Fatty liver
Transcript of Fatty liver

PRESENTED BY:
BINDU JACOB

INTRODUCTION
•Normal liver contains 4% as total lipids, three-fourths of which is phospholipids (PL) and one-fourths of which as neutral fats (TG).
•This amount of lipid content in the liver is the resultant of several influences, some acting in conjuction with and some in opposition to other.

FACTORS REGULATING FAT CONTENT OF LIVER

• Normal levels of Lipids in the Liver are the result of maintenance of a proper balance between the above mentioned factors.
• A relative increase or decrease in the rate of one or other of these processes can result in accumulation of abnormal quantity of lipids in the Liver, producing FATTY LIVER.


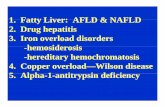
TYPES OF FATTY LIVER• Type-1 Overfeeding of fat
• Type-2 Oversynthesis of fats from carbohydrates
• Type-3 Over mobilisation from depots to liver
• Type-4 Under mobilisation from liver to depots
• Type-5 Under utilisation in the liver

• Overfeeding of fats produce increase in circulating chylomicrons:
• Liver can take up by pinocytosis, leading to increased TG in Liver cells.
• Circulating chylomicrons are acted by Lipoprotein lipase, which produces increase in FFA by hydrolysis of TG of chylomicrons. Leads to influx of FFA in liver, synthesis of TG is enhanced and formation and secretion of more VLDL.
• Lipids deposited in type-1, reflects the composition of dietary Lipids.

Ingestion of carbohydrates in excess of caloric requirement, overloads the capacity
of the cells which normally store glycogen. Surplus carbohydrates are channeled to
synthesis of FA and TG (lipogenesis) in Liver and adipose tissue.
Plasma lipids: Increase in plasma TG ↑ and VLDL ↑, which in turn increases LDL level.
Causes: Oversynthesis from carbohydrates can result from:
1. Forced overfeeding of carbohydrates,
2. Experimentally,
• By administration of excessive amounts of certain B-vitamins viz. thiamine, riboflavin and biotin, and
• Administration of amino acid cystine.

• This type of fatty liver is referred as physiological fatty liver. This represents an exaggeration of normal process, excessive mobilisation of FFA from depot to Liver. Liver responds to increase synthesis of TG and VLDL and increases the plasma level of LDL.
• Causes: Fatty liver of this type develops in conditions involving greatly increased utilisation of fats as “fuel” and where there is interference with oxidation of carbohydrates. (Non-utilisation of carbohydrates for energy). Thus, it occurs in:• Diabetes mellitus: Human or experimental of thehypoinsulin, hyperpituitary or hyperadreno cortical type,• Starvation and• Carbohydrate deprivation.
• Owing to the non-utilisation of carbohydrates, adipose tissue cannot esterify FFA due to lack of α-glycero-P, thus aggravating the hyperlipaemia. In addition to fatty liver and hyperlipaemia, this condition is characterised by ketosis and in advanced cases acidosis.

• Fatty Liver of this type is designated as Pathological fatty liver. It is accompanied by a decrease↓ in plasma lipids (hypolipaemia), which affects mainly PL and Ch-esters.
• The pattern of liver lipids is also abnormal, Fatty Livers of this type, if not treated, eventuates in cirrhosis liver and there may be associated haemorrhagic lesions in the kidneys.
• Causes: They appear to be caused by agents or conditions, which produce either absolute or a relative deficiency in certain of the ingredients used by the Liver for synthesis of VLDL. Such as the:• Protein: Apoprotein itself or• The building blocks of its structural lipid moieties, such as cholesterol esters and PL viz. Inositol phosphatides, choline and the polyunsaturated FA• Factors interfering with secretory mechanism.

• Causative agents: Fatty livers of Type-4 may be roughly classified according to the causative agent or phenomenon as follows:
• 1. Deficiency of EFA
• 2. Imbalance of Vitamin-B Complex Group

Type 5: Underutilisation in the Liver
1. It is possible that the fatty livers of pantothenic acid deficiency are of this type, i.e underutilisation. Deficiency of pantothenic acid leads to decrease↓ in availability of CoA-SH. Hence, activation of FA and its oxidation suffers.
2. Poisoning by salts of rare earth elements (e.g. Cerium) also appears to cause underutilisation, by inhibition of the mitochondrial system which oxidises FA.

SYMPTOMS
Fatigue
Abdominal discomfort
Poor appetite
Weakness
Tiredness

DIAGNOSIS• Physical Exam
If the liver has become inflamed, your physician can detect it by examining the abdomen. An extensive history may reveal fatigue or loss of appetite as well. A thorough history will include alcohol use and other medications or supplements.
• Blood TestsHigher than normal liver enzymes may be found on a routine blood test. This does not confirm a diagnosis of fatty liver. Further analysis will look for the cause of inflammation.
• UltrasoundThe fat on your liver will show up as a white area on the image. Other imaging studies may be done as well such as a CT (computed tomography) scan or MRI (magnetic resonance imaging). Imaging studies can detect fat in the liver, but will not be able to confirm any further damage.
• Liver BiopsyA needle is inserted into the liver to remove a piece of tissue for examination (after giving a local anesthetic to lessen the pain). This is the only way to know for certain if you have fatty liver. The biopsy will also help your doctor learn the exact cause.

TREATMENT