Epiphyseal injury
-
Upload
sunnysmartraj -
Category
Health & Medicine
-
view
1.282 -
download
3
Transcript of Epiphyseal injury

Seminar on
“ Fracture Healing and Epiphyseal injuries”
Moderator: Presenter:
Dr. C B Patil Dr Somnath Machani Professor Post GraduateVIMS & RC. VIMS & RC
.
13 – 10 - 2011

Bone healing in adults
Fracture healing can be divided in to two types Primary- direct healing by internal remodelling Secondary- Indirect healing by callus
Stages Inflamation Soft callus Hard callus remodelling

Stage of inflamation 1 to 7 days Hematoma, inflamatory
exudates Cytokines role Collagen formation Necrotic bone removal

Soft callus formation 2- 3 weeks Decreased pain and swelling Prone to angulation Progenitor cells in cambium
layer Hematoma replaced

Hard callus formation 3 to 4 months Firmly united by new bone Enchondral ossification Bone callus begins at the
periphery of the fracture site- low strain
Initial bone bridge forms externally of within medullary canal and later joins original cortex

Remodelling Woven bone replaced by
lamellar bone. Few months to years till the
meduallary canal is replaced

Difference
Cancellous Less formation of significant external callus After inflamatory stage – intramembranous ossification In unusual cases interfragmentary motion leads to intermediary soft
tissue formation and soon replaced by bone

Need to study child fracture healing
Changing structure and function Different failure pattern Fracture after insignificant trauma 15% of childhood fractures are physeal injuries Physis has longitudinal and diametric growth Salter harris type 1 MC in infants Salter harris type 2 to 4 when 2nd ary ossification centre
enlarges

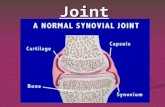
Anatomic regions of child bone
Epiphysis Physis Metaphysis Diaphysis

Epiphysis
@ birth except distal femur Cartilagenous
chondroepiphysis 2nd ary ossification centre
enlarges until replaced by bone
Lucent physeal lines

External surface has perichondrium or articualar cartilage
Pericondrium has ligament and muscle attachments- centrifugal enlargement of the epiphysis
Thick perichondrium- mechanical strength to zone of Ranvier

Physis / growth plate
Rapid longitudinal and diametric growth
Appreciated by growth of the secondary centre
Epiphyseal blood vessels penetrate to reach physis(fig 2)


Vessel damage leads to uneven growth
Patterns of response to ischemia of the epiphyseal (A, B) versus metaphyseal (C, D) circulatory systems. Metaphyseal ischemia is usually transient; epiphyseal ischemia is usually severe and permanent.
Histologic section showing an area of central ischemic growth arrest (arrow). The infarcted area of cartilage is left behind as the rest of the physis continues longitudinal growth.

Metaphysis
Contoured flare at the end of diaphysis
Less cortical and more trabecular bone
Te99m scan shows increased bone turnover
Cortical fenestration (solid arrows) of a metaphysis. Note the interdigitation of periosteal (Ps) tissue with the fenestrations. The periosteum blends into the perichondrium (Pc). Extensive vascularity is often present in this region (open arrows). (E, epiphysis; P, physis; Z, zone of Ranvier; L, ring of Lacroix.)

Fibrovascular connections is the cause for torus or buckle fractures
Extensive modeling and remodeling of the medial (M) versus the lateral (L) cortex of the distal femur may create irregularities that have been misinterpreted as fracture, stress fracture, infection, and tumor. Note the well-formed subchondral bone at the periphery of the epiphyseal ossification center.

Transverse lines of park and harris
Histologic section (A) and x-ray study (B) of a distal femur showing a typical Harris line (arrows). This formed during an acute illness and chemotherapy for leukemia. The child then resumed a more normal pattern of growth until her death from leukemia about 14 months later.

Diaphysis
Extremely vascualar Periosteum- thicker in child
and easily elevated Greater osteogenic potential
and less likely to injure periosteum
Simulated type 1 epiphyseal (E) displacement from the metaphysis (M). Note the thick periosteum (arrow) and its contiguity with the cartilage of the epiphysis (radiopaque here because of the cartilage and air contrast). In the body, however, the similar soft-tissue radiodensities of cartilage, ligament, muscle, and so forth blend together, making them radiolucent.

Composition of bone

Composition of Cartilage

Zones of physis

Factors influencing bone growth

Fracture healing in children
Usually associated with ligament and soft tissue injury
Physis and epiphysis don't heal by callus formation
Phases Inflamatory Reparative remodelling

Inflamatory phase
Hematoma and local necrosis Bleeding from periosteum and
bone Dissects along diaphysis upto
the zone of ranvierPDGF, VGEF, TGF beta promote osteoblast recruitment and activation

Local necrosis- supply is disrupted for a few mm on either side
Necrosis also releases growth factors
Initial matrix contains type 1,3,5 collagen
Promotes mineralization and primary callus

Reparative phase
Osteogenic cells proliferate from the external callus
10-14 days thick fracture callus enveloping mass of peripheral osteogenic tissue
BMP family- mesenchymal cell differenciation
Till healing goes thro final stages- fracture is still biologically plastic
Clinical union

Remodelling
Resorption of unnecessary and in efficient callus
Trabecular orientation Cancellous bone- the cells
are never far away from the blood vessels
Replacement of bone occur in the trabeculae

Physeal healing
Limted ability to repair Primarily heals by increased endochondral bone 3 types of chondro osseous healing
I- # thro columns II - # thro transition zone III - # injury to all layers of the physis

Mechanism of bone bridge formation
Intramembranous ossification mechanism for bone bridge formation at the growth plate injury site. Histologically (Barbara's histology stain), bony bridge trabeculae start to appear on day 7 postinjury (A), and become well-constructed on day 14 with marrow (B). Prior to and during physeal bar formation, there is no new cartilage formation, no collagen-X synthesis (as examined by immunostaining) at the injury site (C), and no expansion of chondrocyte proliferation (as examined by BrdU labeling) from adjacent physeal cartilage (D).

Starting from day 3 (E) until day 14, there is infiltration of marrow-derived fibroblast-like mesenchymal cells (as examined by vimentin immunostaining), some of which are osteoblast precursor cells displaying positive immunostaining for bone cell differentiation transcription factor cbf-a1 (F) and osteoblast/osteoprogenitor maturation marker alkaline phosphatase (G). During bone bridge formation, bone matrix protein osteocalcin is produced by osteoblasts on bone bridge trabeculae (immunostaining) (H). *, injury site; block arrow, pointing to adjacent growth plate cartilage; small arrow, pointing to bone bridge trabeculae or immunostained positive cells.

Etiology of Physeal injuries
Infection
Standing anteroposterior lower extremity x-ray of a 12-year-old boy with multifocal physeal disturbance from purpura fulminans associated with meningococcemia. X-ray abnormalities are present in the left proximal femur; both distal femoral epiphyses, including partial arrest of the left distal femoral physis; and both distal tibial epiphyses. The patient also has digital amputations and extensive soft-tissue scarring resulting from this septic event.

Tumours
Valgus deformity of the distal femur associated with the presence of an enchondroma of the distal lateral femur involving the lateral physis.

Vascular insultA. The patient's leg was caught under heavy pipes
rolling off a rack, resulting in stripping of the soft tissues from the distal thigh, open comminuted fracture of the distal femur, and popliteal artery injury. B. In follow-up, after arterial and soft tissue reconstruction, the patient has physeal growth arrests of the distal femur and proximal tibia. The mechanism of injury to the proximal tibial physis was presumed to be vascular, because of the associated femoral artery injury.

Repetitive stress Distal radius in gymnast Proximal tibia in soccer

Classification of epiphyseal injuries
Salter Harris- 1963 Poland 1898 Aitken 1936 Petersons 1970

Salter Harris
Type 1
transphyseal plane X ray only shows soft tissue
swelling Diagnosis by MRI and USG Avoid stress x ray # line in zone of hypertrophy Minimal growth disturbance

Type II Metaphyseal and physeal
component Thurston holland fragment
sign Growth disturbance
uncommon

Metaphyseal spike may damage physis
A. Dorsally displaced type II fracture of the distal radius. Note the evidence of impaction of the epiphyseal fragment (with the physis) by the dorsal margin of the proximal fragment metaphysis. B. One year later, there is x-ray evidence of physeal arrest formation in the distal radial physis.

Type III Begins in the epiphysis as a
fracture thro the articular surface
2 fragments- small portion of epiphysis and physis
large with long bone Type 3 fracture fixed with
screw

Type IV Veritical shear Disrrupt articular cartilage Metaphyseal and epiphyseal
cross union is common Reduction and stabilization

Type V Unrecognized compression Normal x ray show a
premature physeal closure later

Poland classification
Poland type I, epiphyseal separation without metaphyseal fragment, or extension into the epiphysis.
Poland type II, physeal fracture line extends into the metaphysis.
Poland type III fracture extends from the articular surface to the physis and continues peripherally through the physis.
Poland type IV, T-condylar fracture of the epiphysis and physis.

Aitken classification
Type 1 – SH2 Type 2 – SH 3 Type 3 – SH 4

Petersons Classification
Does not accept SH 5 Peterson 2 to 5 like SH 1 to 4 Peterson 1- transverse
metaphyseal fracture with longitudinal extension into physis
Peterson 6- partial physeal loss


Evaluation of physeal injury
Xray CT MRI USG Arthorgraphy to assess the congrugency of articular surface

Treatment
Stabilize first General principles
Children # heal rapidly Cast immobilization Accurate reduction
Complication – growth disturbance, neurovascular compromise

Physeal growth disturbance
Etiology Peterson type 6, Infection, Cyst Blounts disease Purpura fulminans
Evaluation- serial x rays Loss of physeal contour,
radiolucency between physeal and metaphyseal bone Asymmetric growth arrest line that does not taper to the
physis is a strong indication of the presence of physeal growth disturbance without frank physeal arrest. In this case, the asymmetric growth arrest line is noted in the proximal tibial metaphysis on computed tomography scan.

Harris growth arrest line tapering to the physis at the level of the growth arrest can serve as an excellent x-ray confirmation of the presence of the true growth arrest. Although most commonly noted on plain x-rays, these arrest lines can be seen on computed tomography (CT) scans and magnetic resonance images as well. A. Anteroposterior x-ray of the distal tibia after Salter-Harris type IV fracture demonstrates a Harris growth arrest line tapering to the medial distal tibial physis, where a partial physeal arrest has formed. B. Harris growth arrest line as noted on CT. CT scans with coronal (C) and sagittal (D) reconstructions corrected for bone distortion provide excellent images of the location and size of arrest.

Magnetic resonance imaging scan of a patient with traumatic lateral distal femoral partial growth arrest. Note Harris arrest line tapering to the site of the arrest.

Magnetic resonance imaging scan (three-dimensional spoiled recalled gradient echo images with fat saturation) provides excellent visualization of the affected area and some sense of the integrity of the residual physis. This patient has infantile Blount disease.

Physeal arrestsPotential Causes
Traumatic vascular disruptionTransphyseal infectionVascular collapse associated with infection (purpura fulminans)Infantile Blount's diseaseIrradiationUnicameral bone cystEnchondroma
limb shortening, angular deformity, and epiphyseal distortion, depending on the duration of the arrest, the physis affected, and the size of the arrest. A long, standing film of the lower extremities with the hip, knee, and ankle joints included provides an overall assessment of angular deformity and shortening.

Classification of physeal arrests
Central arrests are surrounded by a perimeter of normal physis.
Peripheral arrests are located at the perimeter of the physis.
Linear arrests are through-and-through lesions with normal physis on either side of the arrest area.

Management
Prevention of arrest formation Gentle anatomic and secure
reduction Fat grafting
NSIAD's ??

Physiolysis
Partial physeal arrest resection
Principle- to remove bone between metaphysis and physis and fill defect with bone reformation retardant

Physeal distraction
External fixator is used to span the arrest .
Gradual distraction until arrest separates
Distraction injury may cause complete cessation of normal physeal growth

Repeated osteotomies
Corrective osteotomy of adjacent metaphysis to correct angular deformity
Completion of epiphysisodesis and management of resulting limb length discrepancy
Epiphysiodesis prevents angular deformtiy Limb lengthening can be considered

Physeal arrest resection
Etiology- trauma/ blounts- good prognosisinfection / tumour- unlikely to show growth
Central and linear arrest regrowth more likely Proximal humeral and femoral leisions more difficult to expose-
adequate resection unlikely Arrests affecting >25% of total surface area are unlikely to grow

Preoperative planning
extent and location of the arrest relative to the rest of the physis must be carefully documented
evaluate an arrest is with reconstructed sagittal and coronal CT images to provide views orthogonal to the affected physis
estimation of the affected surface area can be computed with the assistance of the radiologist using a modification of the method of Carlson and Wenger
Reconstructed magnetic resonance images allow estimation of the percentage of surface area of the physis affected by a growth arrest. This workstation reconstruction delineates the perimeter of normal physis (border 2) and that of the physeal arrest (border 1). Surface area affected can be calculated from these reconstructions.

The arrest must be resected in a manner that minimizes trauma to the residual physis. Central lesions should be approached through either a metaphyseal window or through the intramedullary canal after a metaphyseal osteotomy. Peripheral lesions are approached directly, resecting the overlying periosteum to help prevent reformation
Fluoroscopy is needed to keep the surgeon oriented properly to the arrest and the residual healthy physis.

A high-speed burr worked in a gentle to-and-fro movement perpendicular to the physis usually is the most effective way to gradually remove the bone composing the arrest and expose the residual healthy physis

By the end of the resection, all of the bridging bone between the metaphysis and epiphysis should be removed, leaving a void in the physis where the arrest had been, and the perimeter of the healthy residual physis should be visible circumferentially at the margins of the surgically created cavity

Prevent Re-forming of Bridge between Metaphysis and Epiphysis
A bone-growth retardant or a spacer material should be placed in the cavity created by the arrest resection to prevent re-forming of the bony bridge between the metaphysis and epiphysis.
Four compounds have been used for this purpose either clinically or experimentally: autogenous fat , methylmethacrylate , silicone rubber , and autogenous cartilage. Silione and cartilage not used anymore
Methlymethacrylate is inert but gives structural stability in large resection and in weight bearing areas (tibia in blounts disease)

Metallic markers should implanted in the epiphysis and metaphysis at the time of arrest resection to allow reasonably accurate estimation of the amount of longitudinal growth that occurs across the operated physis, as well as to identify the deceleration or cessation of that growth
Resumption of longitudinal growth may not occur despite technically adequate arrest resection in patients with good clinical indications.
The treating surgeon be alert to those developments, so that proper intervention can be instituted promptly. Embedded metallic markers serve these purposes

Treatment recommendations
On average, approximately 60% of physeal arrests demonstrate clear x-ray evidence of resumption of longitudinal growth of the affected physis after physeal arrest resection.
There is a correlation between the amount of surface area of the physis affected and the prognosis for subsequent longitudinal growth after arrest resection. Physeal arrests affecting less than 10% of the surface area of the physis have a better prognosis than larger arrests.
Langenskiod stage VI infantile Blount disease has results comparable to post-traumatic physeal arrests.
Etiologies other than post-traumatic and infantile Blount disease have poor prognoses for subsequent growth.
Central and peripheral arrests have equivalent prognoses with respect to resumption of growth.
Early growth resumption may be followed by cessation of longitudinal growth before skeletal maturity. As a consequence, patients must be evaluated regularly until skeletal maturity with some reliable method (such as metaphyseal and epiphyseal x-ray markers) to detect such development as promptly as possible.

Growth Deceleration Without Arrest
growth deceleration without frank cessation of growth is characterized by x-ray abnormality of the appearance of an injured physis
clinical or x-ray deformity if the disturbance is severe and long-standing, but without complete cessation of growth in the affected area
The concept of growth deceleration without arrest is most readily appreciated in patients with adolescent Blount disease and the milder stages of infantile Blount disease, infection and physeal fracture
there is no sclerotic area of arrest on plain x-rays
A growth arrest line, if present, may be asymmetric but will not taper to the physis, thereby suggesting growth asymmetry but not complete arrest.

Management
The diagnosis of physeal growth disturbance usually is made incidentally by noting physeal abnormality on x-rays during physeal fracture follow-up or after a diagnosis of frank physeal arrest has been excluded during the evaluation of a patient with angular deformity and physeal abnormality on plain x-rays.
Assess extent of limb length inequality and the calculated amount of potential growth remaining for the affected physis.
If angular deformity is present or progressive, treatment options include hemiepiphysiodesis or stapling and corrective osteotomy, with or without completion of the epiphysiodesis.

Hemiepiphysiodesis or stapling of the affected physis on the convex side of the deformity may result in gradual correction of the deformity. If correction occurs, options include completion of the epiphysiodesis (with contralateral epiphysiodesis if necessary to prevent the development of significant leg length deformity) or removal of staples with careful longitudinal observation for recurrence or overcorrection of deformity.
Corrective osteotomy is the other option for the management of growth disturbance with established angular deformity.
Treating surgeon must decide whether to perform epiphysiodesis of the affected physis (with contralateral epiphysiodesis, if appropriate) to prevent recurrence or to ensure careful longitudinal observation of the growth performance of the affected physis until skeletal maturity.

Conclusion
Physeal injuries are common
Gentle and expert management to maximize restoration of normal limb function and longitudinal growth
Follow up with serial x rays to identify physeal arrest

References
Rockwood and wilkins fractures in children AO trauma manual

Thankyou