Enzymatic modification of plasma densitylipoproteins ...90-95% of the phosphatidylcholine content of...
Transcript of Enzymatic modification of plasma densitylipoproteins ...90-95% of the phosphatidylcholine content of...
Proc. Natl. Acad. Sci. USAVol. 90, pp. 3476-3480, April 1993Applied Biological Sciences
Enzymatic modification of plasma low density lipoproteins inrabbits: A potential treatment for hypercholesterolemiaREGINE LABEQUE*t, CLAUDY J. P. MULLON*t, JOAO PAULO M. FERREIRA*, ROBERT S. LEES§,AND ROBERT LANGER*§¶*Department of Chemical Engineering, Massachusetts Institute of Technology, Cambridge, MA 02139; and §Harvard-Massachusetts Institute of Technology,Division of Health Sciences and Technology, Cambridge, MA 02139
Communicated by Judah Folkman, January 4, 1993 (received for review February 6, 1992)
ABSTRACT Phospholipase A2 (EC 3.1.1.4) hydrolyzescertain phospholipids of low density lipoprotein (LDL). Plasmaclearance of phospholipase A2-modified human LDL is up to 17times faster than that of native human LDL in hypercholes-terolemic rabbits. Modification of blood lipoproteins of hyper-cholesterolemic rabbits was performed by using an extracor-poreal circuit containing immobilized phospholipase A2. After90-min treatments, nearly 30% decreases in plasma cholesterolconcentrations were observed. Erythrocyte, leukocyte, andplatelet counts showed no net change after treatment. Thistechnique does not require any fluid replacement or sorbentregeneration and offers a potential approach for loweringserum cholesterol and LDL levels.
Coronary heart disease accounts for more deaths annuallythan any other disease, including all forms of cancer com-bined (1). Epidemiologic studies have established that thehigher the total plasma cholesterol and low density lipopro-tein (LDL) cholesterol levels, the greater the risk ofcoronaryheart disease (2, 3). Plasma cholesterol may be reduced bydrugs, diet, and direct removal of LDL from the blood.However, drug therapy may have side effects which limit itsuse. For example, drugs that decrease cholesterol synthesis,such as lovastatin, may cause liver and muscle injuries andfetal abnormalities (4). Moreover, many familial hypercho-lesterolemic patients are resistant to diet and drug therapy.Plasmapheresis, the direct removal of the patient's high-cholesterol plasma and replacement with donor albumin,although a successful therapy (5, 6), is expensive and re-moves a wide range of circulating proteins in addition toLDL. Alternative extracorporeal techniques have been de-veloped to improve LDL specificity and to lower cost.Removal of LDL can be accomplished with columns ofheparin-agarose (7), dextran sulfate-cellulose (8), or anti-body-agarose (9-12) or by LDL precipitation at acidic pH(13). However, the limited capacity of the adsorbents makesthese techniques cumbersome and very expensive. We reporthere that a particular phospholipase modifies plasma LDL, sothat it may be removed by an individual's own metabolicprocesses. A small extracorporeal filter containing immobi-lized phospholipase A2 (PLA2; EC 3.1.1.4) caused a 13-28%decrease in plasma cholesterol concentration in cholesterol-fed rabbits after a 90-min treatment.
MATERIALS AND METHODSMaterials. All reagents were analytical grade. Agarose gel
beads activated with N-hydroxysuccinimide (Affi-Gel 15)were from Bio-Rad. Heparin (sodium form, for injection,10,000 USP units/ml) was from Elkins-Sinn (Cherry Hill,NJ). Bovine serum albumin (99% free of fatty acids) and
soybean type II-S phosphatidylcholine were from Sigma.Na125I (17.4 Ci/mg in 0.1 M NaOH; 1 Ci = 37 GBq) was fromNew England Nuclear. Rabbit Chow containing 0.5% cho-lesterol was purchased from Purina.PLA2. PLA2 from Crotalus atrox venom (Miami Serpen-
tarium, Salt Lake City, UT) was purified as reported (14).The protein concentration was determined by the method ofLowry et al. (15) with bovine serum albumin as a standard.PLA2 was immobilized to Affi-Gel 15 according to themanufacturer's protocol. The enzymatic activity of solubleand immobilized PLA2 was measured by the method ofNieuwenhuizen et al. (16), and 1 unit of enzyme was definedas the amount that hydrolyzes 1 ,umol of phosphatidylcholineper minute at pH 8.9 and 25°C. One gram of the agarosesupport had 60-70 units of enzymatic activity. ImmobilizedPLA2 was stable, with no detectable loss of activity, evenafter 2-3 months of storage at 4°C. For control studies, PLA2was inactivated at 160°C for 15 min.
Radioiodination of PLA2. C. atrox PLA2 was radiolabeledwith the lodo-Beads technique (Pierce). After 5 min ofincubation of Na'251 solution (1 mCi) with 4-6 beads, 2-3 mgof enzyme in 100 mM phosphate buffer (pH 7.4) was addedand the reaction proceeded for 15 min. The mixture waspassed through a gel-filtration column (Econo-Pac 10 DG,Bio-Rad) and the protein fractions pooled were dialyzedagainst water. Final labeling efficiencies were 4-7 ,ACi/mg ofprotein, with no loss of enzymatic activity.
Lipoprotein Preparation. LDL (density, 1.025-1.05 g/ml)was isolated from serum of normolipidemic human donors bysequential flotation (17). LDL protein content was quantified(15) with bovine serum albumin as a standard. LDL wasiodinated with Na1251 by the method of McFarlane (18), asmodified for lipoproteins (19). Labeling efficiencies were45-60%. The fraction of radioactivity precipitable by 10%to(wt/vol) trichloroacetic acid ranged from 94% to 97%, andlipid-associated radioactivity was <8%. The specific activityranged from 200 to 400 cpm/ng of protein (apolipoprotein B).Native and iodinated LDL were modified in vitro by PLA2 asfollows (20): LDL (3-4 mg, 6 nM LDL protein) were incu-bated with 80-100 units ofenzyme in 1 mM borate buffer (pH8) containing 4 mM Ca2+ and 1% bovine serum albumin, at37°C for 60 min. The reaction mixture was loaded on aSephadex G-100 column equilibrated with an isotonic salinesolution containing 1 mM EDTA at pH 9. Approximately90-95% of the phosphatidylcholine content of LDL was
Abbreviations: LDL, low density lipoprotein(s); PLA2, phospholi-pase A2; PLA2-LDL, PLA2-modified LDL; NZW, New ZealandWhite; HNZW, hypercholesterolemic NZW; WHHL, Watanabeheritable hyperlipidemic.tPresent address: Procter & Gamble, European Technical Center,Strombeek-Bever, Belgium.tPresent address: W. R. Grace & Co.-Conn, Lexington, MA 02173.$To whom reprint requests should be addressed at: MassachusettsInstitute of Technology, E25-342, 77 Massachusetts Avenue, Cam-bridge, MA 02139.
3476
The publication costs of this article were defrayed in part by page chargepayment. This article must therefore be hereby marked "advertisement"in accordance with 18 U.S.C. §1734 solely to indicate this fact.
Dow
nloa
ded
by g
uest
on
May
15,
202
0
Proc. Natl. Acad. Sci. USA 90 (1993) 3477
hydrolyzed to lysophosphatidylcholine, as measured byquantitative phospholipid analysis and thin-layer chromatog-raphy (21); this is consistent with previous reports (22, 23).Quantitation of malondialdehyde production (24) followingPLA2 modification of both native and radioiodinated LDLshowed that PLA2-modified LDL (PLA2-LDL) was not ox-idized. These findings are important because oxidized LDLis rapidly removed from the blood (25, 26).In Vivo LDL Clearance. All animal care was in accordance
with the National Institutes of Health guidelines and ap-proved by the Massachusetts Institute of Technology Com-mittee on Animal Care. New Zealand White (NZW) rabbitswere purchased from Hazelton Biologics (Denver, PA), andWatanabe heritable hyperlipidemic (WHHL) rabbits werefrom the National Institutes of Health (Bethesda, MD).
Clearance rates and biodistributions were determined innormal NZW rabbits, hypercholesterolemic NZW (HNZW)rabbits (NZW rabbits fed a 0.5% cholesterol diet for 2-3weeks), and WHHL rabbits (27-29). Cholesterol feeding inNZW rabbits produces changes in LDL removal from plasmathat are similar to those observed in receptor-deficient rabbits(30).The animals were injected with either 125I-LDL or 1251_
PLA2-LDL (1.5-2 mg ofprotein, 200-350 ,Ci). Plasma decaykinetics were determined in terms of trichloroacetic acid-precipitable radioactivity in plasma. The fractional catabolicrates for native LDL and PLA2-LDL were calculated asdescribed by Matthews (31) and Bilheimer et al. (32, 33), byassuming a two-compartment model.The biodistribution studies of 1251-LDL were performed as
described by Lees et al. (34). Eighteen different tissues weresampled.LDL Atherogenicity Study. PLA2-LDL was tested for ath-
erogenicity with the balloon-deendothelialized rabbit aortamodel (35, 36). The aortas of 16 NZW rabbits were deendo-thelialized in situ with a balloon catheter via the right femoralartery (36). Four weeks after deendothelialization, the ani-mals were injected intravenously with 125I-PLA2-LDL (10rabbits) or 125I-LDL (6 rabbits) and killed by an overdose ofintravenous pentobarbitol 1-6 hr after injection. The aortaswere fixed with trichloroacetic acid, washed, and processedas reported by Shih et al. (36).
Bile Metabolism Study. HNZW rabbits (six experimental,four control) and WHHL (five experimental, three control)received active PLA2 (200-500 units) or heat-inactivatedPLA2 (control) through the marginal ear vein over a 1-hrperiod. Bile samples were collected as follows: after therabbits were anesthetized with ketamine (40 mg/kg) andxylazine (10 mg/kg), the abdomen was opened throughtransverse skin and muscle incisions. The cystic duct wasligated and the common bile duct was cannulated with apolyethylene catheter (Intramedic, Clay Adams; i.d., 0.045inch; OD, 0.062 inch). A second catheter of similar dimen-sions was placed in the duodenum. The free ends of bothtubes were connected to allow bile circulation and to restoreenterohepatic circulation. Bile (0.5-1 ml) was collected every15 min for determination of flow, bile salts, cholesterol,protein, and phospholipids. Bile salts were quantitated en-zymatically by the method of Turley and Dietschy (37). Thetotal amount of phospholipids was directly measured byquantitating the amount of phosphorous present, as de-scribed by Bartlett (21). Cholesterol concentrations weremeasured by a modification ofthe method of Allain et al. (38).Proteins secreted into the bile were quantitated (15) andanalyzed by SDS/polyacrylamide gel electrophoresis.Procedure for in Vivo Reactor Studies. HNZW rabbits were
used. Two catheters were implanted chronically in thejugularvein (7-12 cm) and carotid artery (5-10 cm) 1 week before theextracorporeal treatments. During that procedure, the ani-mals were anesthetized with ketamine and xylazine at initial
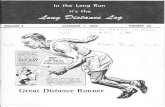
doses of40 mg/kg and 10 mg/kg, respectively. The catheterswere connected by three-way plastic stopcocks and 16-gaugeblunt needles (Becton Dickinson) to the extracorporeal cir-cuit. The circuit (Fig. 1) consisted of a plasma separator(Enka polypropylene fibers, n = 600 fibers, i.d. = 300 gm,housed in a Miniflo Path chamber, Amicon), a column(Bio-Rad Econo-Column, 1.5 x 10 cm, with a water jacketfilled with flowing water at 37°C), and two Masterflex pumpsand tubing (Masterflex size 14, Cole-Parmer). Agarose beads(control experiments) or enzyme-bead conjugates werepacked into the column. Before each experiment, the circuitwas rinsed with a sterile isotonic saline solution at pH 7.4,containing 20 units of heparin per ml and 0.05% rabbit serumalbumin. The rabbits were injected with heparin (200 units/kgof body weight). Blood was pumped through the plasmaseparator at 5-10 ml/min, and the filtered plasma (0.5-1.0ml/min) was perfused through the reactor. Treated plasmaand blood were recombined and returned to the animal. Eachtreatment lasted 60-90 min. Blood samples for biochemicaldeterminations were drawn from the sampling ports (Fig. 1).The rabbits were fully awake during the perfusion. Plasmacholesterol concentrations were measured as before (38). Theplasma concentration of high density lipoproteins was mea-sured after LDL or PLA2-LDL precipitation with heparin/manganese chloride (17), and plasma phospholipid concen-trations were quantitated by thin-layer chromatography (21).
RESULTSIn Vivo Clearance of Native LDL and PLA2-LDL. The
feasibility of reducing plasma cholesterol by PLA2 treatmentwas first tested by injecting rabbits intravenously with human125I-PLA2-LDL. Clearance rates and biodistributions weredetermined in NZW, HNZW, and WHHL rabbits. Theplasma concentration curves are presented in Fig. 2. Human125I-LDL was used as a control. The fractional catabolic ratesof apolipoprotein B for PLA2-LDL were calculated from theplasma concentration curves (31-33) and compared with thevalues for native LDL (Table 1). The results indicated thatPLA2-LDL was degraded 17, 10, and 6 times faster thannative LDL in NZW, WHHL, and HNZW rabbits, respec-tively.
Biodistributions of Native and PLA2-LDL. Table 2 showsthe biodistributions of injected radioactivity per organ in bothWHHL and NZW rabbits. PLA2-LDL accumulated to agreater extent in the liver than native LDL (P < 0.002); inNZW rabbits, the percent injected doses of radioactivity for
Red blood cells
Peristaltic/ pump
Plasma Plasmaseparator
Immobilized _ WaterPLA2 ~~~~jacket
22gPeristaltic WEi amlpump ~~Exit sample
IT t X port
Entry sampleport
Rabbit
FIG. 1. Circuit for extracorporeal treatment with PLA2. Bloodwas pumped through a plasma separator at 5-10 ml/min, and thefiltered plasma was perfused at 0.5-1 ml/min through a columncontaining immobilized PLA2. Treated plasma and blood cells wererecombined and returned to the animal.
Applied Biological Sciences: Labeque et aL
Dow
nloa
ded
by g
uest
on
May
15,
202
0
3478 Applied Biological Sciences: Labeque et al.
1.00
0.80
0.600*°0 0.40'.4
Cuu 0.20
8 0.00
q0
01
0.80 1
Z 0.80-
A
20 40 60Time (min)
i4
0 20 40 60Time (min)
FIG. 2. (A) Normalized plasma concentrations for PLA2-LDL (e,averages of 15 animals) and native LDL (o, averages of 10 animals)in NZW rabbits. (B) Normalized plasma concentrations for PLA2-LDL in HNZW rabbits (m, 3 animals), PLA2-LDL in WHHL rabbits(*, 6 animals), and native LDL in both HNZW and WHHL rabbits(0, 3 and 6 animals, respectively). Plasma cholesterol concentrationsin NZW rabbits were within 20-30 mg/dl and the average concen-trations of WHHL and HNZW rabbits were, respectively, 450 and770 mg/dl.
the liver (mean ± SEM) were 36 ± 4 and 19 ± 2, respectively,for the modified and native LDL; in WHHL rabbits, thenumbers were 26 ± 3 and 12 ± 1, respectively. A significantincrease in radioactivity (10-20%) was also seen in theadrenals, kidneys, bile, and urine. A slight increase in thedelivery to bone marrow was observed, a fact that deservesfurther studies on potential alterations on hematopoietic cellfunction. No increase was observed in the spleen, whichsuggests that monocytes/macrophages were not involved inthe removal of PLA2-LDL.PLA2-LDL was tested for atherogenicity by measuring its
distribution in rabbits with ballooned healing aortic lesions,a well-characterized model of atherosclerosis (35). The con-tent of iodinated native LDL or PLA2-LDL in the wall of theballooned and healing abdominal aorta was, respectively, 4.6± 0.8% and 3.4 ± 0.5% ofthe plasma concentration. The datasuggest (P < 0.09) that, in this model, PLA2-LDL may be lessatherogenic than native LDL.
Extracorporeal Treatment. Having demonstrated thatPLA2-LDL was rapidly removed from the blood pool, wedesigned an extracorporeal circuit containing an immobilizedPLA2 reactor (Fig. 1).
Table 1. Comparison of clearance rates for PLA2-LDL andnative LDL in NZW and WHHL rabbits
Clearance rate, hr-1
Rabbits PLA2-LDL Native LDL*
NZW 1.16 ± 0.05 0.069HNZW 0.16 ± 0.ost 0.029tWHHL 0.22 ± 0.04 0.02-0.024
*Data forNZW and WHHL are from ref. 20 and forWHHL from ref.30.tAverage plasma cholesterol of 770 mg/dl.tAverage plasma cholesterol of 205 mg/dl.
The effectiveness of the treatment was verified in vivo withHNZW rabbits (body weight of 2.5-3.5 kg and average initialplasma cholesterol concentration ranging from 300 to 500mg/dl). The reactors contained 1.5-3 g (wet weight) ofagarose-enzyme conjugate, or agarose as a control. Table 3shows that 33-95% of the plasma phospholipids were mod-ified after 60-90 min of treatment with the PLA2 reactor.Control experiments with NZW and HNZW rabbits showedno phospholipid modification (Table 3). The average de-creases in plasma cholesterol concentrations were 13-28%,at the end of the 90-min treatments. In contrast, in the controlstudies no significant drops in plasma cholesterol were ob-served (P < 0.05).Blood samples at the end of treatment revealed no signif-
icant net change in erythrocyte counts, leukocyte counts,platelet counts, or hematocrit. The concentrations of albu-min, uric acid, bilirubin, and liver enzymes remained withinthe normal range. Plasma levels of free hemoglobin were<0.2 g/dl. The level of high density lipoproteins, measuredafter LDL or PLA2-LDL precipitation with heparin/manganese chloride (17), showed no significant change withtreatment.
Metabolism of PLA2-LDL. As an approach to understand-ing the metabolism of the products of the reactions, smallquantities of active PLA2 (200-400 units) or heat-inactivatedPLA2 were slowly infused intravenously (at a constant flowrate over a 1-hr period) into hypercholesterolemic rabbits(HNZW and WHHL). Ninety-five percent of plasma phos-phatidylcholine was hydrolyzed to lysophosphatidylcholine10 min after the injection of PLA2. Plasma cholesterol con-centrations, measured 3 hr after the injection of PLA2,decreased by an average of 32 ± 17% (seven HNZW rabbitswith initial plasma cholesterol concentrations ranging from250 to 650 mg/dl, and five WHHL rabbits with initial plasmacholesterol concentrations ranging from 390 to 500 mg/dl).Control hypercholesterolemic rabbits (HNZW and WHHL),which received injections of inactivated PLA2, had no changein their blood cholesterol (n = 8, P < 0.005). BecausePLA2-LDL accumulates predominantly in the liver, whichmetabolizes lipoproteins, the bile composition was moni-tored. After an initial 1-hr period to determine the basal bileflow rate, bile samples were collected every 15 min over a5-hr period. Thirty minutes after the injection of active PLA2was initiated, the bile phospholipid composition was 90-95%lysophosphatidylcholine, as compared to >90% phosphati-dylcholine before injection (Fig. 3); total phospholipid massincreased by 10%. In contrast, no biliary lysophosphatidyl-choline was detected in control experiments. Thus, PLA2infusion induced a radical change in biliary phospholipidcomposition. In addition, the secretion of biliary bile saltsincreased from =290 ,umol in control animals to =360 ,umolin experimental animals during the 2 hr following the begin-ning of injection. In contrast, biliary cholesterol secretionremained constant. A 25% increase in bile protein (mainlyserum albumin, as detected by SDS/polyacrylamide gelelectrophoresis) was observed. However, PLA2 was notsecreted in the bile, as determined with iodinated PLA2 (datanot shown), which indicated that the lysophosphatidylcho-line in the bile originated from the plasma. In confirmation ofthis, the time course of excretion of biliary lysophosphati-dylcholine correlated with the time course of formation ofplasma lysophosphatidylcholine.
DISCUSSIONThe objective of our study was to use an enzyme to modifyLDL so that it would be rapidly removed from the blood pooland metabolized endogenously. PLA2, which hydrolyzes theester bond in position 2 of phosphatidylglycerols, was se-lected because the enzymatic modification of LDL does not
Proc. Natl. Acad. Sci. USA 90 (1993)
Dow
nloa
ded
by g
uest
on
May
15,
202
0
Proc. Natl. Acad. Sci. USA 90 (1993) 3479
Table 2. Biodistributions of 1251-PLA2-LDL and 125I-LDL in NZW and WHHL rabbitsPercentage of injected radioactivity
NZW WHHL
Organ(s) PLA2-LDL Native LDL PLA2-LDL Native LDLPlasma 49 ± 2 68 ± 1 61 ± 3 76 ± 3Spleen 0.09 ± 0.03 0.07 ± 0.003 0.00 ± 0.00 0.06 ± 0.03Liver 36 ± 4 19 ± 2 26 ± 3 12 ± 1Adrenals 0.10 ± 0.02 0.07 ± 0.02 0.05 ± 0.005 0.03 ± 0.00Lungs 1.1 ± 0.2 1.2 ± 0.2 3.5 ± 0.5 2.7 ± 0.8Kidneys 1.00 ± 0.09 0.8 ± 0.03 1.5 ± 0.2 1.2 ± 0.1Urine 6 ± 1 3.5 ± 0.4 3.1 ± 0.5 1.9 ± 0.5Bile 0.053 ± 0.002 0.05 ± 0.009 0.05 ± 0.01 0.02 ± 0.01Bone marrow 5.3 ± 0.4 2.1 ± 0.1 7 ± 2 4.5 ± 0.5Small bowel 1.3 ± 0.2 1.6 ± 0.2 2.3 ± 0.5 2.4 ± 0.5Large bowel 1.09 ± 0.05 1.4 ± 0.1 1.9 ± 0.3 1.1 ± 0.8Muscle 2.6 ± 0.3 2.9 ± 0.3 5 ± 3 4.2 ± 1.8Heart 0.071 ± 0.003 0.08 ± 0.03 0.12 ± 0.05 0.21 ± 0.04Stomach 0.85 ± 0.06 0.44 ± 0.009 0.68 ± 0.09 1.3 ± 0.8Adipose 0.008 ± 0.004 0.0033 ± 0.0009 0.004 ± 0.001 0.012 ± 0.006Brain 0.034 ± 0.002 0.012 + 0.005 0.03 ± 0.01 ND
Values for NZW rabbits are means ± SEM of 15 and 10 animals, respectively, for PLA2-LDL and native LDL; valuesfor WHHL rabbits are means ± SEM of 6 animals, for both PLA2-LDL and native LDL. ND, not determined.
significantly change the basic structural features of the par-ticle, including solubility (23). PLA2 is present in most animaland human tissues. It is abundant in the mammalian pancreasand in the venoms of several snakes and bees. The presentstudy shows an accelerated plasma clearance of PLA2-LDLin rabbits, with the liver being the main removal site. Thesefindings are consistent with an observation made by Boren-sztajn and Kotlar (39), who studied the removal of PLA2-modified chylomicrons from the circulation of rats. Fiveminutes after injection, they observed that about 80% of theinjected modified chylomicrons were cleared from theplasma, compared with 10% of native chylomicrons, with theliver as the major removal site.
Clearance and degradation rates of PLA2-LDL in HNZWand WHHL rabbits were lower than in normal NZW rabbits.The different rates may be attributed to the animal models, tothe transport mechanism between PLA2-LDL and tissues,and to the differences in the initial LDL pool sizes (30).Hypercholesterolemic rabbits had much higher plasma cho-lesterol concentrations than normolipidemic ones (250-600mg/dl vs. 40 mg/dl). However, the similar clearance andcatabolic rates in HNZW and WHHL rabbits may be ex-plained by the study of Wiklund et al. (30), who reported thatcholesterol feeding in NZW rabbits produced changes in the
Table 3. Lipid measurements during C. atrox PLA2 and controlextracorporeal treatment
C. atrox PLA2 HNZW1 HNZW2 HNZW3
Enzyme, units 400Treatment,min 60
% modificationof PC 95
Chol, mg/dlInitial 188Final 135(% change) (-28
Control
Chol, mg/dlInitialFinal
HNZW4 HNZW5
164 182 267 120
90 90 90 90
33 91 89 ND
178147(-17)
312254(-19)
362259
(-28%)
516449(-13)
NZW1 NZW2 HNZW3 HNZW4 HNZW5
PC, phosphatidylcholine; Chol, total cholesterol.
plasma decay of lipoproteins that were similar to thoseobserved in receptor-deficient, WHHL rabbits. The biodis-tribution of PLA2-LDL showed that it did not accumulate inthe spleen, which suggests that monocytes/macrophageswere not involved in the removal of PLA2-LDL.
Rabbits with deendothelialized aortic lesions made byballoon catheter were used to compare the accumulation ofPLA2-LDL and native LDL in the abdominal aorta. Accord-ing to previous studies (35), lipoprotein species which accu-mulate at the leading edges ofregenerating endothelial islandsare considered atherogenic. When the animals were sacri-ficed 1 hr after injection of 125I-PLA2-LDL, 70-75% (Table 2)ofthe radioactivity had been cleared from the plasma, and thecenters of regenerating endothelial islands showed a lowerlevel of activity than when native LDL was used. Thissuggests that PLA2-LDL may be less atherogenic than nativeLDL.
Previous approaches utilizing immobilized enzymes ther-apeutically (40-42) caused either the degradation of a toxinor its conversion to a nontoxic substance. The current studyprovides a way of utilizing immobilized enzymes, by modi-fying an existing molecule in the blood so that the body's ownmetabolic processes can more easily eliminate it. The effec-tiveness of the PLA2 treatment was demonstrated in HNZWrabbits. The total plasma cholesterol concentrations of
100-
. 80-
u 60 - %P
'4 4- % LPC400
g 20
0 50 5 0 100 150 20'0 250
Time (min)
FIG. 3. Bile phospholipid composition (mol %) upon i.v. admin-istration of active PLA2. Injection took place at t = 60 min, asindicated by the arrow. PC, phosphatidylcholine; LPC, lysophos-phatidylcholine.
19 58 543 343 116116 54 544 343 1025
Applied Biological Sciences: Labeque et al.
3)
Dow
nloa
ded
by g
uest
on
May
15,
202
0
3480 Applied Biological Sciences: Labeque et al.
HNZW rabbits decreased by nearly 30% after a 90-mintreatment. Furthermore, the drop in plasma cholesterol con-centration increased with the enzymatic activity of the reac-tor (Table 3).Upon i.v. injection of soluble PLA2, lysophospholipids-a
major product of the reaction-were excreted in the bile.Although lysophospholipids are known hemolytic sub-stances, usually transported in blood bound to serum albu-min, hemolysis was not observed during extracorporealtreatments. Quinn et al. (43) have reported that, in vitro andat low concentrations (<100 ,uM), lysophosphatidylcholinehas chemotactic activity for monocytes. The significance ofthis effect in vivo has not been established. In our studies, weobserved a rapid clearance of lysophosphatidylcholine fromplasma, and similar observations were made in rats byAngelico et al. (44).The mechanism of uptake of PLA2-LDL by the liver
remains to be studied. Also, in order to get a closer insightinto the potential effects of the extracorporeal procedure inhumans, an animal model with a closer lipoprotein metabo-lism should be tested. Multiple treatments should be per-formed, with continuous monitoring of plasma protein andlipoprotein levels, liver function, and endothelial cell wallmorphology.
In summary, we have shown that short treatments (60-90min) with an immobilized PLA2 reactor reduce by a third theplasma cholesterol ofHNZW rabbits. In contrast to plasma-pheresis and LDL apheresis, this technique does not requirefluid replacement or column regeneration and appears to bequite specific for very-low- and low-density lipoproteins.This technique may be useful in the treatment of severehypercholesterolemia and may provide a potential applica-tion for the use of immobilized enzymes (40-42) to removetoxic substances from blood.
We thank M. Krieger and A. Klibanov for critical reading of themanuscript, B. M. Clark and C. Tosone for technical assistance, T.Muller and B. Solomon for generous advice and assistance, andW. R. Grace & Co.-Conn. for financial support.
1. Rifkind, B. M. (1984) J. Am. Med. Assoc. 251, 351-361.2. Tyroler, H. A. (1987) in Hypercholesterolemia andAtheroscle-
rosis, eds. Steinberg, D. & Olefsky, J. M. (Churchill Living-stone, New York), pp. 99-116.
3. Goldstein, J. L. & Brown, M. S. (1977) Annu. Rev. Biochem.46, 897-930.
4. The Lovastatin Study Group III (1988) J. Am. Med. Assoc. 260,359-366.
5. Apstein, C. S., Zilversmit, D. B., Lees, R. S. & George, P. K.(1978) Atherosclerosis 31, 105-115.
6. King, M. E., Breslow, J. L. & Lees, R. S. (1980) N. Engl. J.Med. 302, 1457-1459.
7. Lupien, P.-J., Moorjani, S., Lon, M., Brun, D. & Gagne, C.(1980) Pediatr. Res. 14, 113-117.
8. Homma, Y., Mikami, Y., Tamachi, H., Nakaya, N., Naka-mura, H. & Goto, Y. (1987) Metabolism 36, 419-425.
9. Saal, S. D., Parker, T. S., Gordon, B. R., Studebaker, J.,Hudgins, L., Ahrens, E. R., Jr., & Rubin, A. L. (1986) Am. J.Med. 80, 583-589.
10. Stoffel, W., Borberg, H. & Greve, V. (1981) Lancet 1, 1005-1007.
11. Ostlund, R. E., Jr. (1987) Artif. Organs 11, 366-372.12. Ostlund, R. E., Jr. (1988) Artif. Organs 12, 491-505.13. Eisenhauer, T., Armstrong, V. W., Wieland, H., Fuchs, C.,
Sheler, F. & Seidel, D. (1987) Klin. Wochenschr. 65, 161-168.14. Hachimori, Y., Wells, M. A. & Hanahan, D. J. (1971) Bio-
chemistry 10, 4084-4089.15. Lowry, O. H., Rosebrough, N. J., Farr, A. L.& Randall, R. J.
(1951) J. Biol. Chem. 193, 265-275.16. Nieuwenhuizen, W., Kunze, H. & de Haas, G. (1974) Methods
Enzymol. 32, 147-154.17. Hatch, F. T. & Lees, R. S. (1968) Adv. Lipid Res. 6, 1-68.18. McFarlane, A. S. (1958) Nature (London) 182, 53.19. Bilheimer, D. W. & Levy, R. I. (1972) Biochim. Biophys. Acta
260, 212-221.20. Goldstein, J. L., Basu, S. K. & Brown, M. S. (1983) Methods
Enzymol. 98, 241-260.21. Bartlett, G. A. (1958) J. Biol. Chem. 234, 466-468.22. Marinetti, G. V. (1965) Biochem. Biophys. Acta 98, 554-565.23. Aggerbeck, J. P., Kezdy, F. J. & Scanu, A. M. (1976) J. Biol.
Chem. 251, 3823-3830.24. Buege, J. A. & Aust, S. D. (1978) Methods Enzymol. 52,
302-310.25. Steinberg, D., Parthasarathy, S., Carew, T. E., Khoo, J. C. &
Witztum, J. L. (1989) N. Engl. J. Med. 320, 915-924.26. Sparrow, C. P., Parthasarathy, S. & Steinberg, D. (1988) J.
Lipid Res. 29, 745-753.27. Watanabe, Y. (1980) Atherosclerosis 36, 261-268.28. Tanzana, K., Shimada, Y., Kuroda, M., Tsujita, Y., Arai, M.
& Watanabe, Y. (1980) FEBS Lett. 118, 81-84.29. Kita, T., Brown, M. S., Watanabe, Y. & Steinberg, D. (1981)
Proc. Natl. Acad. Sci. USA 78, 2268-2272.30. Wiklund, A., Witztum, J. L., Carew, T. E., Pittman, R. C.,
Elam, R. L. & Steinberg, D. (1987)J. LipidRes. 28, 1098-1109.31. Matthews, C. M. E. (1957) Phys. Med. Biol. 2, 36-53.32. Bilheimer, D. W., Stone, N. J. & Grundy, S. M. (1977) J. Clin.
Invest. 64, 524-533.33. Bilheimer, D. W., Goldstein, J. L., Grundy, S. M. & Brown,
M. S. (1975) J. Clin. Invest. 56, 1420-1430.34. Lees, R. S., Garabedian, H. D., Lees, A. M., Scumacher,
D. J., Miller, A., Isaacsohn, J. L., Derksen, A. & Strauss,H. W. (1985) J. Nucl. Med. 26, 1056-1063.
35. Minick, C. R., Stemerman, M. B. & Insuli, W. (1977) Proc.Natl. Acad. Sci. USA 74, 1724-1728.
36. Shih, I.-L., Lees, R. S., Chang, M. Y. & Lees, A. M. (1990)Proc. Natl. Acad. Sci. USA 87, 1436-1440.
37. Turley, S. D. & Dietschy, J. M. (1978) J. Lipid Res. 19,924-928.
38. Allain, C. A., Poon, L. S., Chan, C. S. G., Richmond, W. &Fu, P. C. (1974) Clin. Chem. 20, 470-475.
39. Borensztajn, I. & Kotlar, T. (1981) Biochem. J. 200, 547-553.40. Langer, R., Linhardt, R. J., Hoffberg, S., Larsen, A. K.,
Cooney, C. L., Tapper, D. & Klein, M. (1982) Science 217,261-263.
41. Lavin, A., Sung, C., Klibanov, A. & Langer, R. (1985) Science230, 543-548.
42. Klein, M. D. & Langer, R. (1986) Trends Biotechnol. 4, 179-186.
43. Quinn, M. T., Parthasarathy, S. & Steinberg, D. (1988) Proc.Natl. Acad. Sci. USA 85, 2805-2809.
44. Angelico, M., Alvaro, D., Masella, R., Corradini, S. G. &Cantafora, A. (1987) Biochim. Biophys. Acta 905, 91-99.
Proc. Natl. Acad Sci. USA 90 (1993)
Dow
nloa
ded
by g
uest
on
May
15,
202
0