Enteric Gram-negative bacilli (Family: Enterobacteriaceae )
description
Transcript of Enteric Gram-negative bacilli (Family: Enterobacteriaceae )
Enteric Gram-negative bacilli(Family: Enterobacteriaceae)
Gram negative bacilli characterized by:- Grow on ordinary media- Aerobic or facultative anaerobic- Non spore forming- All ferment glucose- All reduce nitrate to nitrite- All catalase positive- All motile except Shigella and Klebsiella.-Some are capsulated. Klebsiella produce large mucoid colonies
Some enteric organisms are part of the normal flora and incidentally cause disease (E. coli). Others arc regularly pathogenic for humans (salmonella)
The family Enterohacteriaceae includes many
genera (twenty) e.g., escherichia shigella salmonella, klebsiella, proteus, pseudomonas. Usually, there are opportunistic pathogen.
ShigellaShigella is the etiological agent of bacillary
dysentery.
The natural habitat of shigella is limited to the intestinal tract of humans.
Morphology Gram negative bacilli, non motile, non capsulated.
Culture:Shiglla produce pale non-lactose fermenting colonies
on MacConkey’s media.
Serological characters: Genus shigella divided into 4 groups.According to the somatic antigen ‘O’.The first 3 groups divided into types by type-specific
antisera. The fourth group divided into types by colicine antibiotic typing.
Biochemical reactions : All ferment mannitol with production of acid except
group A.
All may produce indole from triptophan broth except group D.
Group D is late lactose fermenter.
Toxin production:Endotoxin; which is lipopolysaccharide in the cell
wall. It causes irritation to the bowels wall.Exotoxin; produced only by one type of S.
dysenteriae (type 1) It affect the gut act as verotoxin of E. coil (invading and destruction of intestinal epithelial cells), and affect the CNS and act as neurotoxin causing meningism and coma in sever infections.
Epidemiology and Pathogenesis:The infection occurs by the ingestion of
contaminated food or drinks from cause of carries (large bowel). It is limited to the gastrointestinal tract without blood invasion, Endotoxin acts early producing voluminous non-bloody diarrhea which is followed by invasion of the mucosa of the wall of the large intestine and terminal ileum, leading to necrosis, superficial ulcers, pseudomembrane formation and bleeding. Sh. Dysenteriae has invasive properties. Shigella is the most effective pathogen.
Clinical findings:The incubation period is 1-4 days.There is crampy abdominal pain, diarrhea
composed of blood & mucus, tenesmus and fever. Shiga toxin first effect is small gut then can effect colon causing rectal spasm (Tenesmus ).
S. dysenteriae causes the severest local and systemic manifestations ( Life threatening disease).
Recovery occurs spontaneously.Very few remain as chronic carriers.
Diagnosis:Stool samples are inoculated on MacConkey’s or
DCA media. Non lactose fermenter colonies are identified by; morphology, biochemical reactions & serologically.
Prevention: (similar to Salmonella typhi).
Public health measures: • Safe sewage disposal• Sanitary control of water, food and milk• Fly control• Isolation of patient and disinfect its excrets• Oral vaccine is under investigation.
Treatment:Restoration of fluid & electrolyte balance in severe
cases. Antibiotics; ciprofloxacin, chloramphenicol, ampicillin & tetracycline. Antibiotics are rarely necessary for S. Sonnei.
Escherichia coliThese are normal inhabitants of the intestine of
man however some can cause disease in man. Live only in the intistine, its presence in water indicate contamination with fecal content. Don't live in soil and water.
Morphology: Gram negative bacilli, motile, some strains are
capsulated.
Culture characters : Aerobic or facultative anaerobic, grow on simple
media on MacConkey's medium, they produce pink colonies due to lactose fermentation.
Biochemical activity: They ferment lactose glucose maltose mannitol,
sucrose and salicin with production of acid and gas.They are indole positive methyl red positive VP.
negative & citrate utilization negative.
Serological characters: O (somatic) antigen more than 70 antigen.H (flagellar) antigen more than 50 antigen. K (capsular) antigen more than 1 00 antigen. Virulence factorsPili; mediate adherence to host cells. Capsule; interfere with phagocytosis interfere with the
bactericidal effect of complement.Endotoxin; the somatic lipopolysaccharide. Exotoxins.
Pathogenesis & clinical findings
I - Urinary tract infection: E coli is the most common cause of urinary tract
infection & accounts for approximately 90% of urinary tract infection in young women Certain strains known as uropathogenic E. coli colonize the vagina & periurethral region from where they ascend to the bladder or kidney causing cystitis or pyelonephritis .K antigen & P pilus are important virulant factors in upper urinary tract infection. E coli causes 85 of domestic infection (community) and 50 hospital infection (nonocomial).
1 - Enterotoxigenic E. coli;Causes Traveler’s diarrhea & infantile diarrhea.
Diarrhea is watery and range from mild to severe (cholera-like) and may be fatal.
The organisms adhere to the intestinal epi. Through the epithelume, then they liberate enterotoxins (ST & LT).
ST (heat stable enterotoxin) activates guanylyl cyclase and stimulates fluid secretion.
LT (heat labile exotoxin) consists of 2 subunits A & B.
LT subunit B attaches to epi. cells of small intestine and facilitates the entry of subunit A into the cells.
LT subunit A activates cAMP causes hypersecretion of water and chloride and inhibits reabsorption of sodium.
2 - Enteropathogenic E. coli: Causes outbreaks of neonatal diarrhea. They act
mainly by adhering tightly to intestinal mucosa resulting in loss, thus preventing the normal functions of absorption and secretion.
3 - Enteroinvasive E. coli:Cause dysentery-like diarrhea through invasion of
intestinal epithelial cell lining of the intestinal wall.
4- Enterohaemorrhagic E. coli: Produce 2 antigenic forms of a toxin known as
verotoxin haemorrhagic colitis (severe diarrhea with bloody discharge)
5 -Enteroaggregative E. coli Organisms adhere to
intestinal mucosa and elaborates enterotoxins & cytotoxins. The result is mucosal damage secretion of large amounts of mucus and a secretory diarrhea.
III- Neonatal meningitis; 40% due to E. coil followed by group B streptococci (S. agalactiae) and Listeria monocytogenous. Symptoms: failure to minimal movement, weak cry and anxious.
IV-Specticemia-gramnegative bacteremia (Endotoxic
shock) endotoxin lead to peripheral vasodilatation --- decrease venous return ---> Symptoms: high fever, low cardiac output, hypotension, hypo-glycemia, leucopenia & anoxia ------ shock
V-Hospital acquired infections (noso-comial). VI-wounds: infection usually mixed with anaerobes,
bed-sores, peritonitis, appendicitis & cholecystitis.
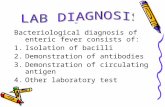
Laboratory diagnosis:1 -- Specimens; urine, stool, pus, CSF sputum…2-- Direct smear; shows Grain negative non spore
forming bacilli. Wet unstained smears show motile bacilli.
3-- Culture; On MacConkey's medium shows pink colonies. The colonies are identified by morphology and biochemical reactions.
4--Serological identification; using slide agglu-tination with known antisera.
Enterotoxigenic E. coil detected by testing for toxin by ELISA or DNA probe