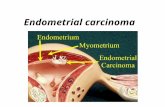
Endometrial carcinoma
-
Upload
aboubakr-mohamed-elnashar -
Category
Health & Medicine
-
view
209 -
download
0
Transcript of Endometrial carcinoma
Incidence
-Endometrial carcinoma is the most common
gynecologic malignancy.
-The disease predominantly affects perimenopausal
and postmenopausal women, whose median age at
diagnosis is 61 years. Only 5% of patients are
younger than 40 years.
-It is twice as common as ovarian cancer and three
times more common than invasive carcinoma of the
cervix.
ABOUBAKR ELNASHAR
Mortality
unlike ovarian cancer, endometrial cancer has a
hallmark early symptom--perimenopausal or
postmenopausal bleeding--which prompts the
physician to take an endometrial biopsy. This
biopsy leads to a diagnosis at a favorable stage in
most patients reducing mortality
ABOUBAKR ELNASHAR
Risk Factors
Most endometrial cancers arise from a background
of endometrial hyperplasia and are the consequence
of unopposed endogenous or exogenous estrogen
on a hormonally responsive endometrium.
1. Obesity (Davies et al, 1981).
Women who are overweight by up to 22.7 kg have a
threefold increased risk for this malignancy. The
risk jumps to ninefold for women overweight by
more than 22.7 kg.
ABOUBAKR ELNASHAR
Obesity increases the risk by increasing estrogen
production and bioavailability.
A. In postmenopausal women, the ovaries and
adrenals secrete negligible amounts of estrogen.
Most estrogen is in the form of estrone, which is
produced in the peripheral conversion of
androstenedione in muscle and adipose tissue.
Increased production of estrone has been
documented in obese women (Judd et al, 1980).
B. obese women have lower levels of sex-hormone-
binding globulin, which accounts for the increased
bioavailability of circulating estrogen (Gambone et al, 1982).
ABOUBAKR ELNASHAR
2. Total intake of calories derived from saturated or
unsaturated fats is a risk factor independent of body
weight.
A. Women reporting a high intake of animal fat and
fried food have a 2.1-fold increased risk for
endometrial carcinoma.
B. Women with a high intake of complex
carbohydrates, predominantly breads and cereals,
have a decreased risk (RR = 0.6) after controlling for
body mass (Potischman et al, 1993).
ABOUBAKR ELNASHAR
3. History of infertility, nulliparity, early menarche, and
late menopause (Elwood et al, 1977; Kelsey et al, 1982).
4. Hypertension and diabetes mellitus are often
associated with obesity, but they may represent
independent risk factors.
5. Chronic anovulatory states, such as PCOS
ABOUBAKR ELNASHAR
6. Functional ovarian neoplasms, such as certain
epithelial ovarian cancers and granulosa cell tumors,
may also increase risk by the endogenous production
of unopposed estrogen.
7. In women with postmenopausal bleeding, the most
significant risk factor for endometrial cancer (and
complex endometrial hyperplasia) is age. Patients
who are older than 70 have a risk for endometrial
cancer-complex atypical hyperplasia that is six to ten
times higher than in younger women (Feldman et al, 1994).
ABOUBAKR ELNASHAR
8. unopposed estrogen replacement therapy (Mack et al, 1976; Weiss et al, 1979).
Risk increases with estrogen dose and duration of
use. Widespread use of unopposed estrogen in the
1960s might have been responsible for the temporal
rise in the endometrial cancer rate that peaked in
1979.
The risk for endometrial cancer can be effectively
eliminated with the addition of a progestin.
Progesterone reduces estrogen-receptor synthesis
and increases the conversion of estradiol to the less
potent metabolite estrone.
Women on combined estrogen and progestin
replacement therapy actually have lower risk for
endometrial cancer than do untreated patients.
ABOUBAKR ELNASHAR
Patients on cyclic combined regimens of estrogen
and progesterone should be administered
progesterone at least 12 to 13 days each month (Paterson et al, 1980).
The trend is to use continuous combined regimens
because this eventually eliminates bleeding in most
women.
Current recommendations suggest that patients on
unopposed estrogen should undergo annual
endometrial biopsy. In addition, women who have
bleeding before day 11 of a cyclic progestin regimen
should undergo endometrial biopsy (Padwick et al, 1986).
ABOUBAKR ELNASHAR
9. Tamoxifen has been used extensively in the
treatment of estrogen receptor-positive breast
cancer in postmenopausal women. While taking
tamoxifen, these women had reductions in new
malignancies forming in the contralateral breast (Kedar et al, 1994).
Tamoxifen has antiestrogenic and estrogenic
properties. It has been shown to reduce the risk for
osteoporosis while increasing rates of endometrial
hyperplasia and neoplasia.
ABOUBAKR ELNASHAR
The risk for endometrial cancer is reduced by
1. Combied oral contraceptive pill. (50%)
Most modern preparations are progestin dominant,
and the degree of risk reduction is related to
duration of use and total progestin dose. The
protective effect may be greatest in non- obese,
nulliparous women.
ABOUBAKR ELNASHAR
2. Smoking:
A.It increases concentrations of sex-hormone-
binding globulin, thereby lowering levels of
bioavailable estrogen.
B. It has been linked to early menopause.
Such benefits of smoking, however, are clearly
outweighed by the marked increase in risk for lung
cancer and cardiovascular disease (Friedman et al, 1987).
ABOUBAKR ELNASHAR
No identifiable risk factors
Not all endometrial adenocarcinomas arise as a
result of physiologic conditions of relative estrogen
excess. There is a subset of adenocarcinomas that
arise in women with no identifiable risk factors.
These tumors may be of high grade and of
unfavorable histologic type (for example, papillary
serous, clear cell, or adenosquamous variants). T
hey develop de novo, not in an environment of
endometrial hyperplasia, and are often aggressive
tumors.
ABOUBAKR ELNASHAR
Hereditary forms of endometrial cancer
Rare
including the Lynch II family cancer syndrome.
This syndrome includes nonpolyposis colorectal
cancer, ovarian, and endometrial cancer (Lynch et al, 1989).
A careful family history should always be obtained
from patients with cancer.
ABOUBAKR ELNASHAR
Clinical picture
1. The most common symptom of endometrial
cancer, abnormal vaginal bleeding, occurs in
more than 80% of patients. When this hallmark
symptom occurs in postmenopausal women, it is
dramatic, disturbing, and likely to prompt an
immediate response from patient and physician.
The amount of bleeding is not correlated with the
likelihood of cancer because even a small
amount of spotting may represent cancer .
2. Late symptoms: pain, pressure symptoms, urinary
symptoms, cachexia
ABOUBAKR ELNASHAR
Signs:
1. The patient is usually obese, hypertensive,
diabetic, infertile with lng history of menstrual
disorders.
2. There may be pallor due to increased blood loss.
3. Palpation of the uterus:
a. Enlagement:
b. Fixation at late stages
c. Secondaries in vagina, ovary
ABOUBAKR ELNASHAR
Screening
Cytological screening:
•50% of patients with endometrial cancer have
abnormal results on Papanicolaou smear.
•This makes the test unsatisfactory for screening.
•Evaluation of endometrial cytologic preparations has
not gained broad acceptance because of the
difficulty in interpretation (Meisels and Jolicoeur, 1985).
ABOUBAKR ELNASHAR
1. Routine screening is not recommended
2. High risk groups:
A. Detection of endometrial cells on a Papanicolaou
smear in a postmenopausal woman indicates the
need for endometrial biopsy (Zucker et al, 1985).
ABOUBAKR ELNASHAR
B. Gronroos et al (1993)
mass screening (Ultrasonography & endometrial
biopsy) of women, 45 to 69 years of age, who have
diabetes mellitus and hypertension.
Among women with diabetes, 6.3% were found to
have neoplasia.
Among women with hypertension, 1.3% were found
to have neoplasia.
Eighty percent of women ultimately bleed, and 75%
have highly curable stage 1 disease at this first sign
of abnormality. Because of this, it is unclear how
much benefit would be gained by screening women
with diabetes mellitus and hypertension, especially
in light of the costs of screening the 90% of patients
who do not have cancer at the time of screening.
ABOUBAKR ELNASHAR
C. Women taking tamoxifen for breast cancer have
an increased risk for endometrial neoplasms.
This increased risk is partly a result of the estrogen
agonist effects of tamoxifen on the endometrium.
However, women with a history of breast cancer are
also at increased risk for ovarian or endometrial
cancer, regardless of tamoxifen use. In addition,
some studies of women taking tamoxifen report an
excess number of malignancies that carry poor
prognoses, among them clear cell carcinoma and
papillary serous carcinoma (Cohen et al, 1993; Magriples et al, 1993).
Given these findings, yearly endometrial biopsies,
or intermittent progesterone treatment of patients on
long-term tamoxifen therapy, should be considered.
ABOUBAKR ELNASHAR
Pathology
Most forms of cancer arising in the endometrium are
adenocarcinomas.
There are distinct histopathologic types that evince
very different biologic behaviors.
Endometrioid adenocarcinomas are the most
common.
These lesions may be papillary, secretory, or
ciliated.
Squamous differentiation is a common feature.
When the squamous tissue is anaplastic, it is
designated as an adenosquamous variant. Variants
that have been described are mucinous, clear cell,
and pure squamous carcinoma.
ABOUBAKR ELNASHAR
The degree of carcinoma differentiation may be
based on cytologic or architectural criteria. For
endometrial carcinomas, FIGO has established
architectural criteria that may be applied to most cell
types.
A grade 1 tumor is defined as a tumor that has less
than 5% solid area.
A grade 3 tumor is more than 50% solid.
Tumor grade predicts the biologic behavior of
endometrial cancer.
ABOUBAKR ELNASHAR
Well-differentiated lesions tend to be associated with
superficial invasion and have little propensity for
nodal spread.
Poorly differentiated lesions are often deeply invasive
and metastatic. Clear cell carcinoma and papillary
serous carcinoma are two particularly virulent forms
of endometrial cancer.
They represent less than 15% of all endometrial
cancers combined, but they encompass a large
proportion of the treatment failures (Kurman and Scully, 1976; Christopherson et al, 1982).
ABOUBAKR ELNASHAR
ENDOMETRIAL CARCINOMA
1) Endometrioid :
Usually diffuse thickening of the endometrial
surface
Often a shaggy, ulcerated surface with an
underlying friable white gray mass
Deep myometrial invasion and extension into the
cervix indicate more advanced disease.
Grading of the tumor depends on the architectural
features.
Well differentiated tumors are composed of back to
back glands with low nuclear grade.
ABOUBAKR ELNASHAR
A variation of well differentiated endometrioid
carcinoma is the papillary or villoglandular type with
usually slender fibrovascular cores and lack of
stratification and nuclear pleomorphism
Poorly differentiated tumors have a solid growth
pattern. | lo mag | hi mag
Variants: secretory and ciliated
ABOUBAKR ELNASHAR
2) Serous:
5 - 10 % of all endometrial carcinomas.
Aggressive with tendency to deep myometrial
invasion.
Complex papillary fronds that are usually broad.
Budding and tufting of the papillae.
Often the lining cells have a high nuclear gradewith
marked nuclear pleomorphism and prominent
nucleoli.
Mitoses are common.
High propensity to invade lymphatics.
Psammoma bodiesoften present. ABOUBAKR ELNASHAR
3) Clear cell:
4 % of all endometrial carcinomas.
Aggressive.
Often associated with an advanced stage of
disease and thus, poor prognosis.
Solid, tubular or papillarypatterns of growth
Large clear cells and hobnail cells.
Nuclear grade is usually high.
4) Mucinous:
Primary adenocarcinoma of endometrium in which
most of the cells contain prominent intracytoplasmic
mucin and resemble colonic epithelium. ABOUBAKR ELNASHAR
5) Squamous:
Pure squamous carcinomas of endometrium are
rare.
Associated with steam treatment of endometritis in
pre-antibiotic era.
Should be diagnosed only in the absence of a
cervical primary.
6) Adenocarcinoma with squamous
differentiation:
Squamous differentiation is very common | lo-mag
hi-mag
Prognosis related to differentiation of glandular
component ABOUBAKR ELNASHAR
7) Undifferentiated carcinoma:
Relatively uncommon.
Variety of patterns: small cell type with
neuroendocrine differentiation ( lo-mag| hi-mag ,
giant cell, or spindle cell types.
8) Mixed:
Combination of the types described above.
ABOUBAKR ELNASHAR
Pretreatment Evaluation
1. Complete history and physical examination should
be performed. Often, patients with endometrial
cancer are obese and have hypertension or
diabetes and possibly significant intercurrent
medical problems.
2. A complete blood count to rule out anemia
secondary to vaginal bleeding should be performed.
ABOUBAKR ELNASHAR
3. Abnormal liver function test results may suggest
occult metastatic disease.
4. A chest x-ray should be obtained to rule out
pulmonary metastases.
5. Intravenous pyelography, gastrointestinal series,
and barium enema are not required in asymptomatic
patients. A bone scan adds little to the initial
evaluation.
ABOUBAKR ELNASHAR
6. Magnetic resonance imaging has proven to be
accurate in the evaluation of myometrial invasion and
lymph node involvement (Yazigi, 1989).
7. Transvaginal sonography has been used to assess
myometrial invasion but with less success (Yamashita, 1993).
These modalities are expensive and less accurate
than data derived from surgical staging. They may be
helpful in evaluating patients in whom comorbid
disease precludes surgical staging, but they are not
required for surgical staging.
ABOUBAKR ELNASHAR
8. Although originally described as a tumor marker
for ovarian cancer, serum levels of CA-125 have
been shown to be elevated among patients with
endometrial cancer (Niloff et al, 1994).
It is unusual for early-stage disease to cause an
abnormal level, and because most patients seek
treatment at an early stage, it is not indicated as a
routine test. In most studies, more than 80% of
patients with elevated CA-125 levels are found to
have extrauterine disease at the time of exploratory
laparotomy (Pastner and Mann, 1988).
ABOUBAKR ELNASHAR
Endometrial cancer is a surgically staged disease.
Therefore, imaging to assess the depth of
myometrial invasion and tumor markers to suggest
disseminated disease are not required before
exploration.
ABOUBAKR ELNASHAR
Staging
In 1988 FIGO abandoned the clinical staging system
after the completion of prospective surgical staging
trials (Boronow et al, 1984; Creasman et al, 1987).
These studies establish the importance of cell type,
histologic grade, depth of myometrial invasion, and
nodal, adnexal, or peritoneal spread as prognostic
variables.
The previous clinical staging system, which
determined uterine size and endocervical
involvement at a fractional D & C, is now used only
for patients treated with primary radiation therapy.
ABOUBAKR ELNASHAR
Surgical staging begins with a vertical abdominal
incision. Any collection of free pelvic fluid should be
aspirated for cytologic evaluation. If no fluid is
present, saline washings should be obtained.
Thorough exploration of the abdomen, including
palpation of the diaphragm, bowel mesentery, and
para-aortic nodal groups, is essential.
Biopsy specimens should be taken of suspicious
areas. Total extrafascial hysterectomy and
adnexectomy are then performed. In selected
patients, para-aortic or pelvic lymph nodes may be
sampled, and any enlarged lymph nodes must be
removed. ABOUBAKR ELNASHAR
Omentectomy or omental biopsy is indicated for
patients with the papillary serous variant.
Para-aortic or pelvic lymph node sampling may lead
to morbidity and may be technically difficult in an
obese patient.
Nodal involvement risk is predictable based on
histologic cell type, tumor grade, and depth of
myometrial invasion.
Stage I, grade 1 lesions with superficial invasion
rarely metastasize to the pelvic or para-aortic nodes,
whereas up to 45% of women with deeply invasive
grade 3 lesions have nodal metastasis.
ABOUBAKR ELNASHAR
Therefore, for patients with presumed stage I
endometrial cancer, gross or frozen-section
evaluation of the depth of myometrial invasion at the
time of hysterectomy is invaluable in guiding
intraoperative decision making. Lymph node
sampling should be strongly considered for patients
with presumed stage I, grade 3 lesions or for lesions
of any grade with significant myometrial invasion.
Patients with stage II or III disease or with disease of
an unfavorable histologic type should also undergo
para-aortic and pelvic lymph node sampling.
Vaginal hysterectomy remains an appropriate
alterna- tive to abdominal surgery for stage I, grade
1 endometrial cancer. ABOUBAKR ELNASHAR
Recent advances in operative laparoscopy have led
to innovative approaches to the surgical staging of
endometrial cancer. Childers and Surwitt (1993)
report their experience with laparoscopically
assisted surgical staging of endometrial cancer,
including laparoscopic nodal sampling and vaginal
hysterectomy. Preliminary data suggest that this
investigational technique is well tolerated and that it
significantly reduces hospital stays. Laparoscopy
allows for upper abdominal exploration, node biopsy,
and salpingo-oophorectomy. These procedures are
not possible using a purely vaginal approach.
ABOUBAKR ELNASHAR
Postoperative Care
After primary therapy, patients with endometrial
cancer should be examined at regular intervals with
complete physicals and Papanicolaou smears.
Frequency of visits and duration of follow-up must be
based on the likelihood for disease recurrence in
each patient. Among women with stage IA, grade 1
and stage IB endometrial cancer, hormone
replacement therapy may be initiated after informed
consent is obtained. In these patients, the risk for
tumor recurrence is low and the benefits of
replacement therapy far outweigh the risks (Lee et al, 1990).
Estrogen replacement therapy may be
contraindicated in advanced-stage, high-grade
lesions. ABOUBAKR ELNASHAR
Adjuvant Therapy
After surgical staging and treatment, adjuvant therapy
may be required for patients at significant risk for
disease recurrence in the pelvis or abdomen. Patients
are at high risk if they have been found to have para-
aortic lymph node metastasis or adnexal or peritoneal
spread.
Postoperative radiation to the pelvic and aortic areas
may cure up to half the patients with advanced
disease (Potish et al, 1985).
Radiation treatment of the pelvis remains
controversial. Most studies show a reduction in local
recurrences but no significant impact on survival
rates.
ABOUBAKR ELNASHAR
Prognosis
Overall, 72% of women with stage I adenocarcinoma
of the endometrium survive at least 5 years.
The 5-year survival rate falls to 56% for stage II
disease and 30% for stage III disease.
Unfortunately, only 10% of women with stage IV
lesions survive at least 5 years (Pettersson, 1988).
ABOUBAKR ELNASHAR
Recurrence
Endometrial cancer may metastasize
intraabdominally, hematologically, or through the
lymphatics. The most common site of local
recurrence is the vaginal cuff. Distant metastasis
may be seen in lung, liver, or abdomen. Most
recurrences develop within 3 years of initial
diagnosis. Distant metastasis is associated with a
grim prognosis because of a lack of effective
systemic hormonal therapy or chemotherapy.
However, an isolated vaginal recurrence, without
pelvic extension, may be effectively treated with
surgical excision or local irradiation. As many as 45%
of women with this recurrence survive 10 years (Paulsen and Roberts, 1988).
ABOUBAKR ELNASHAR
Staging of Cancer of the Uterine Corpus
IA G123
Tumor limited to endometrium
IB G123
Invasion to 50% myometrium
IC G123
Invasion to 50% myometrium
IIA G123
Endocervical glandular involvement only
IIB G123
Cervical stromal invasion
ABOUBAKR ELNASHAR
IIIA G123
Tumor invades serosa and/or adnexa and/or there is
positive peritoneal cytology
IIIB G123
Vaginal metastases
IIIC G123
Metastases to pelvic and/or paraaortic lymph nodes
IVA G123
Tumor invasion of bladder and/or bowel mucosa
IVB
Distant metastases including intraabdominal and/or
inguinal nodes
ABOUBAKR ELNASHAR
Treatment of Recurrent Endometrial Cancer
Treatment of patients with distant recurrences of
endometrial cancer is challenging and rarely results
in cure. Local irradiation may control pain or disability
from focal metastases.
To control systemic disease, progestational agents or
cytotoxic chemotherapy may be used.
Response rates to progestin therapy may be as high
as 15% to 20%, particularly in well-differentiated
cancers that are more likely to be estrogen-receptor
and progesterone-receptor positive.
ABOUBAKR ELNASHAR
The role of cytotoxic chemotherapy in the treatment
of endometrial cancer is limited. The reported
complete clinical response rate is only 15%.
Regimens that contain platinum or doxorubicin
hydrochloride have the highest overall response
rates, but these responses tend to be short lived, and
survival is not prolonged (Park et al, 1992).
Given the toxicity associated with cytotoxic
chemotherapy, progestin treatment is a rational first
step in treating recurrent disease. Progestins have
some desirable secondary effects, particularly as
appetite stimulants, and minimal toxicity. If progestin
treatment fails, cytotoxin therapy may be considered.
ABOUBAKR ELNASHAR