ED4 - Diabetes
Transcript of ED4 - Diabetes
-
7/29/2019 ED4 - Diabetes
1/22
APM Diabetes Session
Rhonda Fruhling, MS, ARNP, CDE
Judy Sigler, BSN, CDE(updated 8/11)
-
7/29/2019 ED4 - Diabetes
2/22
Correlation: A1c and Estimated
Average glucoseA1c (%) eAG
Estimated Average Glucose (mg/dl)
6 126
7 154
8 183
9 212
10 240
11 269
12 298
American Diabetes Association, 2011
-
7/29/2019 ED4 - Diabetes
3/22
Goals for Outpatient Blood GlucoseControl
Pre-meal blood glucose levels
70-130 mg/dl
Post-prandial
-
7/29/2019 ED4 - Diabetes
4/22
Key Concepts in Setting
Glycemic Goals Individualize
Certain populations need special considerations
Less intensive goals may be indicated in personswith severe or frequent hypoglycemia
More stringent goals may be appropriate (a
normal A1c, < 6 %) Postprandial glucose may be targeted if A1c
goals not met
American Diabetes Association, 2007
-
7/29/2019 ED4 - Diabetes
5/22
Continuous Glucose Monitoring
(CGM) Measures interstitial glucose
Require calibration with SMBG (treatment
decisions should be based on SMBG notCGM readings).
BG meter readings and sensor readings
will rarely match exactly. Focus on trends
Focus on direction and speed of thesensor glucose change.
-
7/29/2019 ED4 - Diabetes
6/22
-
7/29/2019 ED4 - Diabetes
7/22
Insulin Therapy Principles
Basal insulin
Controls glucose production by the liver
Bolus insulin
Food insulin
Use and store carbohydrates eaten
Correction (supplemental) insulin Treat an acute elevation in blood glucose
-
7/29/2019 ED4 - Diabetes
8/22
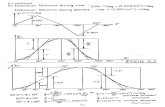
Glucose & insulin concentration
Basal
Bolus
-
7/29/2019 ED4 - Diabetes
9/22
Insulin Preparations
Rapid-acting Insulin Analogs Lispro (Humalog), Aspart (Novolog), Glulisine (Apidra)
Short-acting Insulin Regular
Intermediate-acting Insulin NPH
Long-acting Insulin Analog Detemir (Levemir), Glargine (Lantus)
-
7/29/2019 ED4 - Diabetes
10/22
Insulin Action Patterns
InsulinPreparation
Onset ofAction
PeakAction
EffectiveDuration
Rapid-acting
Analogs
5-15
minutes
30-90
minutes
3-5 hours
Short-acting 30-60minutes
2-3 hours 5-8 hours
Intermediate-
acting
2-4 hours 4-10 hours 10-16 hours
Long-acting
(glargine)
2-4 hours Peakless 20-24 hours
Long-acting
(detemir)
2-4 hours(dose-related)
6-14 hours(relatively flat)
16-20 hours(dose-related)
-
7/29/2019 ED4 - Diabetes
11/22
Pre-Mixed Insulins
Humalog Mix 50/50 50 % lispro protamine and 50 % lispro
Humulin 70/30 (human) 70 % NPH and 30 % Regular
Humalog Mix 75/25 (analog) 75 % lispro protamine and 25 % lispro
NovoLog Mix 70/30 (analog) 70 % aspart protamine suspension and 30 % aspart
-
7/29/2019 ED4 - Diabetes
12/22
-
7/29/2019 ED4 - Diabetes
13/22
NPH and Fast-Acting Insulin
-
7/29/2019 ED4 - Diabetes
14/22
-
7/29/2019 ED4 - Diabetes
15/22
Syringes 1 cc (holds 100 units)
1/2 cc (holds 50 units)
1/3 cc (holds 30 units)
-
7/29/2019 ED4 - Diabetes
16/22
Insulin PensAdvantages
Convenient
Accurate
Often used by person on multi-dose regime
Disadvantage
Usually more expensive (exception is a personon a small dose insulin)
Injection force
-
7/29/2019 ED4 - Diabetes
17/22
Insulin Storage Keep current vial in refrigerator or at room
temperature (once opened, it is good for
28 days). Keep extra vials in the refrigerator
Avoid temperatures extremes (86
degrees) Not in direct sunlight
Never let freeze
-
7/29/2019 ED4 - Diabetes
18/22
-
7/29/2019 ED4 - Diabetes
19/22
Insulin Resistance
Among Patients Lack of confidence/self-efficacy
Concern regarding the ability to handle insulin
therapy Fears and Concerns
Insulin will restrict lifestyle
Hypoglycemia
Diabetes has become more severe
Fear of pain, fear of giving injections
Kruger, D. (2007). Tying It All Together: Matching Insulin Regimens to
Individual Patient Needs. The Diabetes Educator, 33(Suppl. 4) 91-95.
-
7/29/2019 ED4 - Diabetes
20/22
Insulin Resistance
Among Patients Personal failure
The need for insulin is a result of not taking care of
his or her diabetes This sense of failure may be exacerbated by providers
who threaten patients with insulin
Perceived lack of benefit
Do not consider insulin efficacious
Kruger, D. (2007). Tying It All Together: Matching Insulin Regimens toIndividual Patient Needs. The Diabetes Educator, 33(Suppl. 4) 91-95.
-
7/29/2019 ED4 - Diabetes
21/22
Insulin Resistance
Among Healthcare Providers Denial, avoidance, procrastination, wishful
thinking
Fear of alienating the patient Insulin therapy is time-consuming
Fear of hypoglycemia
Peragallo-Dittko,V. (2007). Removing Barriers to Insulin Therapy. TheDiabetes Educator, 33(Suppl.3) 60-65.
-
7/29/2019 ED4 - Diabetes
22/22
Diabetes Education
Inpatient survival skills teaching
Contact by EPIC consult Int Med Diabetes
Nurse or contact by pager 7215 Outpatient (consult on EPIC)
Group Diabetes Self-Management Classes
Individual Diabetes Education appointment