ECTOPIC PREGNANCY ECTOPIC PREGNANCY ASSOCIATE PROFESSOR IOLANDA BLIDARU, MD, PhD.
Ectopic pregnancy
-
Upload
fahad-zakwan -
Category
Documents
-
view
47 -
download
2
Transcript of Ectopic pregnancy
ECTOPIC PREGNANCY
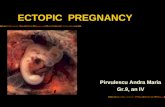
•An ectopic pregnancy, or eccysis , is a complication of pregnancy in which the embryo implants outside the uterine cavity.
•With rare exceptions, ectopic pregnancies are not viable.
• Furthermore, they are dangerous for the woman, since internal haemorrhage is a life threatening complication if rupture occurs.
•An ectopic pregnancy is a potential medical emergency, and, if not treated properly, can lead to death.
•It is an important cause of maternal deaths
SITES OF ECTOPIC IMPLANTATION
Most ectopic pregnancies occur in the Fallopian tube (so-called tubal pregnancies), but implantation can
also occur in the cervix, ovaries, and abdomen
TUBAL PREGNANCY• The vast majority of ectopic pregnancies implant in the
Fallopian tube. Pregnancies can grow in the fimbrial end (5% of all ectopics), the ampullary section (80%), the isthmus (12%), and the cornual and interstitial part of the tube (2%)
•Mortality of a tubal pregnancy at the isthmus or interstitial pregnancy is higher as there is increased vascularity that may result more likely in sudden major internal hemorrhage
NON-TUBAL ECTOPIC PREGNANCY
• Two percent of ectopic pregnancies occur in the ovary, cervix, or are intra-abdominal.
•While a fetus of tubal pregnancy is typically not viable, very rarely, a live baby has been delivered from an abdominal pregnancy.
• In such a situation the placenta sits on the intraabdominal organs or the peritoneum and has found sufficient blood supply
RISK FACTORS/CAUSES1. PID
2. use of an intrauterine device (IUD),
3. previous exposure to DES,
4. tubal surgery,
5. intrauterine surgery (e.g. D&C),
6. smoking,
7. previous ectopic pregnancy, and
8. tubal ligation.
CLASSICAL CLINICAL PRESENTATION
1. Short period of amenorrhea (btw 5 – 8 wks.)
2. +ve pregnancy test
3. Intermittent scanty Vaginal bleeding of dark blood (spotting)
4. Abdominal pain
SIGNS AND SYMPTOMS
Clinical presentation of ectopic pregnancy occurs at a mean of 7.2 weeks after the last normal menstrual period, with a range of 5 to 8 weeks. Later presentations are more
common in communities deprived of modern diagnostic ability.
Signs and symptomsEarly signs include:
Pain in the lower abdomen, and inflammation (Pain may be confused with a strong stomach pain, it may also feel like a strong cramp)
Pain while urinating
Pain and discomfort, usually mild. A corpus luteum on the ovary in a normal pregnancy may give very similar symptoms.
Pain while having a bowel movement
•Vaginal bleeding, usually mild. An ectopic pregnancy is usually a failing pregnancy and falling levels of progesterone from the corpus luteum on the ovary cause withdrawal bleeding. •This can be indistinguishable from an early miscarriage or the 'implantation bleed' of a normal early pregnancy.
Patients with a late ectopic pregnancy typically experience pain and bleeding. This bleeding will
be both vaginal and internal and has two discrete pathophysiologic mechanisms:
External bleeding is due to the falling progesterone levels.
Internal bleeding (haemoperitoneum) is due to hemorrhage from the affected/ruptured tube.
More severe internal bleeding may cause:Lower back, abdominal, or pelvic pain.
Shoulder pain. This is caused by free blood tracking up the abdominal cavity and irritating the diaphragm, and is an ominous sign.
There may be cramping or even tenderness on one side of the pelvis.
The pain is of recent onset, meaning it must be differentiated from cyclical pelvic pain, and is often getting worse.
Signs and symptoms of shock (low BP, high pulse rate and episode of syncope and loss of consciousness
SIGNS• Pallor: moderate to severe
• Shock signs: • Low BP 90/60 mmHg• Weak pulse• Raised pulse rate 110/min• Raised RR> 20• Sweating• Cold skin
• Tender distended abdomen with rebound tenderness
• Signs of intraperitoneal fluid i.e. fluid thrill & shifting dullness.
Threatened abortion
UTI
early normal pregnancy.
PID
acute appendicitis
gastrointestinal disorder,
Twisted ovarian cyst
DIFFERENTIAL DIAGNOSIS
DIAGNOSIS
•An ectopic pregnancy should be considered in any woman with abdominal pain and/or vaginal bleeding who has a positive pregnancy test.
•An ultrasound showing a gestational sac with or without fetal heart in the fallopian tube is clear evidence of ectopic pregnancy. (Empty uterus with these findings adds to the diagnosis)
•A laparoscopy or laparotomy can also be performed to visually confirm an ectopic pregnancy.
•Culdocentesis, in which fluid is retrieved from the cul de sac (pouch of Douglas) may be used to look for internal bleeding.
•Paracentesis (aspiration from the abdominal cavity through the abdominal wall)
•Cullen's sign can indicate a ruptured ectopic pregnancy.
MANAGEMENT
•Resuscitation with intravenous fluids if in shock or clinically unstable.• Normal saline, ringers lactate, Hartman’s solution• Should be given first using cannula
•Blood group & Xmatch
•Blood transfusion may be needed.
•Definitive treatment of the ectopic pregnancy.
DEFINITIVE MANAGEMENT
• Medical
Early treatment of an ectopic pregnancy with methotrexate is a viable alternative to surgical treatment.
If administered early in the pregnancy, methotrexate terminates the growth of the developing embryo; this may cause an abortion, or the tissue may then be either resorbed by the woman's body or pass with a menstrual period. Contraindications include liver, kidney, or blood disease, as well as an ectopic mass > 3.5 cm.
•Surgical
If hemorrhage has already occurred, surgical intervention may be necessary.
laparoscopy or laparotomy to gain access to the pelvis and can either incise the affected Fallopian and remove only the pregnancy (salpingostomy) or remove the affected tube with the pregnancy (salpingectomy).
PROGNOSIS
• Fertility following ectopic pregnancy depends upon several factors,
The treatment choice, whether surgical or nonsurgical,
The rate of intrauterine pregnancy may be higher following methotrexate compared to surgical treatment.
Rate of fertility may be better following salpingostomy than salpingectomy.