Ebola virus disease
-
Upload
tarek-tawfik-amin -
Category
Health & Medicine
-
view
175 -
download
1
description
Transcript of Ebola virus disease

Professor Tarek Tawfik AminEpidemiology and Public Health
Faculty of Medicine, Cairo University [email protected]
“ Infection Preventionists: Ready for Disasters ”
Ebola Virus Disease: The Outbreak
The 22nd Annual Conference of the Egyptian Society for Infection Control (ESIC) (APIC/Egypt Chapter)
& The 5th Conference of the Eastern Mediterranean Regional Network for Infection Control (EMRNIC)
04/10/231 Tarek Amin

Objectives Recognize the epidemiological features
of Ebola Virus Disease (EVD). Appreciate the role of infection control
procedures in controlling EVD. Recognize the guidelines and
procedures implied for infection control at different stages of patient’s management.
04/10/232 Tarek Amin

Causative agents 1 Family Filoviridae, three genera:
Cuevavirus, Marburgvirus, and Ebolavirus. Five species of Ebola: - Zaire, Bundibugyo, Sudan, Reston
(Philippines) and Taï Forest (Cote de Ivories) .
- Bundibugyo, Zaire, and Sudan associated with large outbreaks in Africa.
- The 2014 West African outbreak belongs to the Zaire.
04/10/233 Tarek Amin

04/10/234 Tarek Amin

04/10/235 Tarek Amin

Reservoirs
Non-human primates, duikers, bats, small rodents, and shrews.
Past outbreaks, human contact with wild animals hunting, butchering and preparing meat from infected wild animals (“bush meat”).
In 2014 epidemic the majority of cases are a result of human to human transmission.
04/10/236 Tarek Amin

04/10/23Tarek Amin7

04/10/238 Tarek Amin

Transmission 2 Fruit bats (Pteropodidae family) are natural
hosts. Contact with blood, bodily fluids:
chimpanzees, gorillas, fruit bats, monkeys, forest antelope and porcupines “ ill or dead or in the rainforest”.
Human-to-human transmission via direct contact with blood, bodily fluids, or contaminated surfaces and materials.
HCPs infected while treating patients through close contact.
Burial ceremonies, Corpse remains infectious for six days.
Semen for up to seven weeks 3 .
04/10/239 Tarek Amin

Hypothesis: Ebola transmission
04/10/2310 Tarek Amin

Hypothesis : Marburg transmission
04/10/2311 Tarek Amin

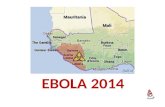
Historical outbreaks 4 EVD in 1976 in two simultaneous outbreaks, Nzara,
Sudan, and Yambuku, DR Congo (former Zaire), near Ebola river.
West African is the largest and most complex outbreak (2014).
Started in Guinea then spreading across borders to Sierra Leone and Liberia, air to Nigeria, and land to Senegal.
Guinea, Sierra Leone and Liberia: weak health systems, lacking human and infrastructural resources, and facing long of conflict and instability.
On August 8th , the WHO Director-General declared this outbreak a Public Health Emergency of International Concern.
04/10/2312 Tarek Amin

Year CountryEbola virus
species CasesDeaths
Case fatality
2012 DR Congo Bundibugyo 57 29 51%2012 Uganda Sudan 7 4 57%2012 Uganda Sudan 24 17 71%2008 DR Congo Zaire 32 14 44%2007 Uganda Bundibugyo 149 37 25%2007 DR Congo Zaire 264 187 71%2005 Congo Zaire 12 10 83%2004 Sudan Sudan 17 7 41%2003 Congo Zaire 35 29 83%2003 Congo Zaire 143 128 90%2001-2002 Congo Zaire 59 44 75%2001-2002 Gabon Zaire 65 53 82%2000 Uganda Sudan 425 224 53%1996 Gabon Zaire 60 45 75%1996 Gabon Zaire 31 21 68%1995 DR Congo Zaire 315 254 81%1994 Cote d'Ivoire Taï Forest 1 0 0%1994 Gabon Zaire 52 31 60%1979 Sudan Sudan 34 22 65%1976 Sudan Sudan 284 151 53%1976 DR Congo Zaire 318 280 88%
04/10/2313 Tarek Amin

Ebola and Health care settings:
04/10/23Tarek Amin14
Of the 2 870 Marburg and Ebola cases documented between June 1967 and June 2011, 270 (9%) were health-care providers.3
Started as small scattered outbreaks, usually spread within health care facility ‘Amplification”
Family members and HCPs are at the highest risk of infection.

04/10/2315 Tarek Amin
CountryTotal Cases
Laboratory-
Confirmed Cases Total Deaths
Guinea 1553 1312 926
Liberia 4665 965 2705
Sierra Leone 3896 3389 1281
Total 10114 5666 4912
Country Total Cases
Laboratory-Confirmed Cases Total Deaths
Mali 1 1 1
Senegal ! 1* 1* 0
Total 2 2 1
Country Total Cases
Laboratory-Confirmed Cases Total Deaths
Nigeria ! 20* 19* 8
Spain 1 1 0
United States 4 4 1
Total 25 24 9
•Countries with Widespread Transmission
•Countries with Travel-associated Cases
•Countries with Travel-associated Cases and Localized Transmission
24th of October 2014, CDC, Current situation
http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/case-counts.html

Case definitio
n 3
Routine surveillance: Suspect case: Fever and no response to treatment for usual causes in the area, and at least one: bloody diarrhea, bleeding gums, purpura, bleeding into eyes, or hematuria. Confirmed Ebola : Laboratory confirmation (Ve+ IgM antibody, Ve+PCR or viral isolation)
Community-based surveillance: Pre-epidemic phase and outbreak. Alert case: fever and no response to treatment of usual causes of in the area, OR bleeding, bloody diarrhea, hematuria OR any sudden death.
During outbreak: SUSPECT CASE: Alive or dead, high fever and contacted a suspected, probable or confirmed case; dead or sick animal. OR: sudden onset of high fever + at least 3: • headaches • vomiting • anorexia / loss of appetite • diarrhea • lethargy • stomach pain • aching muscles or joints • difficulty breathing or swallowing • hiccup OR: inexplicable bleeding OR: sudden, inexplicable death.
04/10/2316 Tarek Amin

04/10/2317 Tarek Amin

Case definition for exclusive use by hospitals and surveillance teams 3:
PROBABLE CASE: Any suspected case evaluated by a clinician OR: Deceased suspected case having an epidemiological link with a confirmed case
LABORATORY CONFIRMED CASE: Any suspected or probable cases with a positive laboratory result. - Virus RNA by RT- PCR, - IgM antibodies.
04/10/2318 Tarek Amin

Contacts 4 Case contacts: With case in the last 21 days preceding the onset of symptoms: Slept in the same household Physical contact with case Physical contact at the funeral, Touched blood or body fluids Touched his/her clothes or linens Breastfed by the patient
Dead or sick animals: With sick or dead animal in the 21 days preceding: Physical contact with the animal Animal’s blood or body fluids Carved up the animal Eaten raw bush-meat
Laboratory contacts: Worked in a laboratory 21 days preceding onset of symptoms: Direct contact with specimens collected from suspected Ebola patients Direct contact with specimens collected from suspected Ebola animal Contact with a hospital where Ebola cases being treated the 21 days.
04/10/2319 Tarek Amin

04/10/2320 Tarek Amin

Timeline of Infection Diagnostic tests available
- Within a few days after symptoms
® Antigen-capture enzyme-linked immunosorbent assay (ELISA) testing
® IgM ELISA
® RT Polymerase chain reaction (RT- PCR)
® Virus isolation
- Later in disease course or recovery
IgM and IgG antibodies
- Deceased patients Immunohistochemistry testing
PCR
Virus isolation
Laboratory diagnosis 5
04/10/2321 Tarek Amin

Blood sampling: BSL4* 6
Acute phase: whole blood obtained within 7 days of onset. Convalescent sera: collected at least 14 days after onset. Paired serum samples are ideal, usually collected 7-20 days apart.
*Bio-safety level 4: level required for work with dangerous and exotic agents that pose a high individual risk of aerosol-transmitted laboratory infections, agents which cause severe to fatal disease in humans for which vaccines or other treatments are not available, such as Bolivian and Argentine hemorrhagic fevers, Marburg virus, Ebola virus, Lassa virus, Crimean-Congo hemorrhagic fever, and others.
04/10/2322 Tarek Amin

Safety precautions: Category A, BSL4 facilities 7.
Do not separate acute phase sera from blood clots .
Sealed sterile dry Vacutainer tubes. In their original tube and stored at 4 ˚C for
PCR / virus isolation
04/10/2323 Tarek Amin

04/10/2324 Tarek Amin
Phases: opportunity for control

04/10/2325 Tarek Amin
Outbrea measures

04/10/2326 Tarek Amin

Controlling Infection in Health Care Setting: rules 1,2
Strict standard precautions, regardless of diagnosis.
Basic hand, respiratory hygiene, PPE, safe injection practices and safe burial practices.
Extra infection control measures to prevent contact with patient’s blood and body fluids and contaminated surfaces or materials.
In close encounter (1 m) face protection (face shield or medical mask and goggles), a clean, non-sterile long-sleeved gown, and gloves (sterile gloves for some procedures).
Human and animal samples for investigations handled by trained staff and processed in suitably equipped laboratories.
04/10/2327 Tarek Amin

04/10/23Tarek Amin28

04/10/2329 Tarek Amin

DIRECT PATIENT CARE (FOR SUSPECTED OR CONFIRMED PATIENTS) 1,8
PATIENT PLACEMENT, STAFF ALLOCATION AND VISITORS:
04/10/2330 Tarek Amin

04/10/2331 Tarek Amin

Suspected or confirmed cases in single isolation rooms (IRs).
If IRs are unavailable, cohort patients in specific confined area keeping suspected and confirmed cases separate. At least 1 meter distance between patient beds.
Clinical and non-clinical personnel are assigned exclusively to patient care areas.
Restrict all non-essential staff from patient care areas.
Stopping visitor access to the patient, or limit their number.
Do not allow other visitors to enter the isolation rooms/areas and ensure adequate distance for observation (≈3 meters).
Before allowing visitors, screen for of EVD
04/10/2332 Tarek Amin

•HAND HYGIENE, PERSONAL PROTECTIVE EQUIPMENT AND OTHER PRECAUTIONS2,9.
04/10/2333 Tarek Amin

04/10/2334 Tarek Amin

Visitors use PPE and perform hand hygiene (HH) prior entry.
HCPs, PPE before entering isolation areas. Scrub or medical suits NOT personal clothing. HH: 1.before gloving and wearing PPE on entry. 2.before any clean/aseptic procedures performed 3.after any exposure with the patient’s blood and
body fluids, 4.after touching contaminated
surfaces/items/equipment in the patient’s surroundings,
5.after removal of PPE, upon leaving the care area.
04/10/2335 Tarek Amin

HH within the isolation rooms/areas. Before entering the isolation areas, PPE in
dedicated changing zone.Correctly sized gloves. Changing gloves if heavily soiled while
providing care to the same patient (HH immediately after removal).
Change gloves, HH, moving from one patient to another in same room.
Disposable, impermeable gown to cover clothing and exposed skin.
Medical mask and eye protection to prevent splashes.
04/10/2336 Tarek Amin

Rubber boots. If NOT, overshoes, removed while wearing
gloves. Strenuous activity (respirator) or tasks in
which contact with blood and body fluids is anticipated (waterproof apron over the gown).
Avoid aerosol-generating procedures, use a respirator.
Before exiting isolation room/area, carefully remove and dispose PPE into waste containers and perform HH.
Avoid any contact between the soiled items (e.g. gloves, gowns) and any area of the face or non-intact skin.
04/10/2337 Tarek Amin

04/10/2338 Tarek Amin

Do not recycle any single-use disposable PPE. Dedicated equipment (e.g. stethoscopes) for
each patient. If NOT decontaminate between each patient
contact. Waste generated should be treated as
infectious waste.Items and equipment should not be moved
between isolation rooms/areas and other areas of HCF.
Patient charts and records should be kept outside the isolation rooms/areas to avoid their contamination.
04/10/2339 Tarek Amin

INJECTION SAFETY AND MANAGEMENT OF SHARPS 3,10
04/10/2340 Tarek Amin

Injection and medication equipment disposed of at point of care.
Limit the use of needles and other sharp objects. Limit the use of phlebotomy and laboratory testing to
minimum.a)Never recapping . b)Never direct the point of a used needle towards any
part of the body. c)Do not remove used needles from syringes by hand,
bend, break or manipulate. d)Dispose sharps in puncture-resistant containers. e)Containers are placed upright to the immediate
(‘point of use’). • Kidney dish or similar to carry to the sharps container. • Containers placed in an area not easily accessible by
visitors, particularly children .04/10/2341 Tarek Amin

ENVIRONMENTAL CLEANING 1,2,11,12
04/10/2342 Tarek Amin

Heavy duty/rubber gloves, impermeable gown
and closed shoes (e.g. boots) when cleaning the environment and handling infectious waste.
Facial protection (mask and goggle or face shield) and overshoes if boots are unavailable.
Respirator: - Blood and body fluids is anticipated (cleaning
surfaces heavily soiled with vomit or blood) or - Cleaning areas closer < 1 meter from a patient
with symptoms like diarrhoea, bleeding or vomiting, etc.).
1- PPE
04/10/2343 Tarek Amin

Environmental surfaces or objects contaminated cleaned and disinfected using (e.g. a 0.5% chlorine solution).
Change cleaning solutions and refresh equipment frequently.
Clean floors and horizontal work surfaces at least once a day with clean water and detergent.
Dry sweeping never be done. Rags not be shaken out and surfaces should
not be cleaned with dry rags. From “clean” areas to “dirty” areas. Do not spray (fog) occupied or unoccupied
clinical areas with disinfectant.
2- CLEANING PROCESS
04/10/2344 Tarek Amin

Handling soiled linen from patients, use PPE and facial protection.
Clearly-labeled, leak-proof bags or buckets at the site of use.
Never be carried against the body. Transported directly to the laundry area
in its container. Washing contaminated linen by hand
discouraged. Burn the linen to avoid any
unnecessary risks.
3- LINEN
04/10/2345 Tarek Amin

•Waste Management 1- PPE PPE and facial protection. Goggles provide greater protection than
visors from splashes.Avoid splashing when disposing of liquid
infectious waste.
04/10/2346 Tarek Amin

2- WASTE MANAGEMENT PROCEDURES
Segregated at point of generation. Puncture resistant waste containers. Solid, non-sharp, infectious waste in leak-proof
waste bags covered bins. Bins should never be carried against the body (e.g.
on the shoulder). Designated pit of appropriate depth (2 m) and filled
to a depth of 1–1.5 m, covered with 10 to 15 cm soil layer.
Controlled access. Feces, urine and vomit, and liquid waste, disposed
sewer or latrine. 04/10/2347 Tarek Amin

NON-PATIENT CARE ACTIVITIES 1,12
04/10/2348 Tarek Amin

A. DIAGNOSTIC LABORATORY ACTIVITIES:
Laboratory sample processing under a safety cabinet or at least a fume cabinet with exhaust ventilation.
No procedures on the open bench. Micro-pipetting and centrifugation are
prohibited. PPE, particulate respirator when
aliquotting, centrifugation. Discard apron or gown immediately. Specimens in clearly-labeled, non-glass,
leak-proof containers . Disinfect all surfaces of specimen
containers. 04/10/2349 Tarek Amin

04/10/23Tarek Amin50

B. MOVEMENT AND BURIAL OF HUMAN REMAINS .
PPE , rubber boots to handle. Plug the natural orifices. Double bag, wipe surface with disinfectant
(e.g., 0.5% chlorine solution) and seal and label.
Immediately move the body to the mortuary.
Remains should not be sprayed, washed or embalmed.
Washing for “clean burials” should be discouraged.
Buried promptly. 04/10/2351 Tarek Amin

POST-MORTEM EXAMINATIONS
Limited to essential evaluations by trained personnel.
Eye protection, PPE. Performing autopsies, particulate respirator . Specimens in clearly-labeled, non-glass, leak-
proof containers. External surfaces of specimen containers
disinfected prior transport. Tissue or body fluids for disposal carefully
placed in clearly marked, sealed containers for incineration.
04/10/2352 Tarek Amin

MANAGING EXPOSURE TO VIRUS THROUGH BODY FLUIDS INCLUDING BLOOD
04/10/2353 Tarek Amin

04/10/23Tarek Amin54
a)Immediately and safely stop any current tasks, b)Leave the patient care area, c)Safely remove PPEd)Wash the affected skin or percutaneous injury site
with soap and water. e)Irrigate mucous membranes with copious amounts of
water. f) Immediately report the incident. g)Medically evaluated (e.g., HIV), receive follow-up
care, including fever monitoring, twice daily for 21 days after the incident.
h)Consultation for exposed person develops fever within 21 days of exposure.
i) Suspected of being infected , isolated, with same management recommendations until a negative diagnosis is confirmed.
j) Contact tracing is essential.

References
1) 1 Interim manual - Ebola and Marburg virus disease epidemics: preparedness, alert, control, and evaluation World Health Organization, Geneva, 2014; Available from: http://www.who.int/csr/disease/ebola/manual_EVD/en/
2) 2 Clinical Management of Patients with Viral Haemorrhagic Fever: A pocket Guide for the Front-line Health Worker. World Health Organization, Geneva, 2014.
3) 3 Guideline for Isolation Precautions: Preventing Transmission of Infectious Agents in Healthcare Settings. Centers for Disease Control and Prevention, Atlanta, GA, 2007; Available from: http://www.cdc.gov/HAI/prevent/prevent_pubs.html
4) 4 Standard precautions in health care AIDE-MEMOIRE. World Health Organization, Geneva, 2007; Available from: http://www.who.int/csr/resources/publications/standardprecautions/en/.
5) 5 Hand Hygiene Posters. World Health Organization, Geneva, 2009. ; Available from: http://www.who.int/gpsc/5may/tools/workplace_reminders/en/
6) 6 Glove Use Information Leaflet. World Health Organization, Geneva, 2009.; Available from: http://www.who.int/gpsc/5may/tools/training_education/en/
7) 7 Infection Prevention and Control Recommendations for Hospitalized Patients with Known or Suspected Ebola Hemorrhagic Fever in U.S. Hospitals. Centers for Disease Control and Prevention, Atlanta, GA; Available from: http://www.cdc.gov/vhf/ebola/hcp/infection-prevention-and-control- recommendations.html
8) 8 Guide to Local Production: WHO-recommended Handrub Formulations. World Health Organization, Geneva, 2010; Available from: http://www.who.int/gpsc/5may/tools/system_change/en/.
9) 9 Hoffman PN, Bradley C, Ayliffe GAJ, Health Protection Agency (Great Britain). Disinfection in healthcare. 3rd ed. Malden, Mass: Blackwell Pub.; 2004.
10) 10 How to safely collect blood samples from persons suspected to be infected with highly infectious blood-borne pathogens (e.g. Ebola) World Health Organization.
11) 11 WHO best practices for injections and related procedures toolkit. World Health Organization, Geneva, 2010; Available from: http://www.who.int/injection_safety/toolbox/9789241599252/en/
12) 12 Management of Hazard Group 4 viral haemorrhagic fevers and similar human infectious diseases of high consequence. Department of Health, United Kingdom, 2012; Available from: http://www.dh.gov.uk/publications.
04/10/2355 Tarek Amin

Thank you
04/10/2356 Tarek Amin


![Ebola virus disease [ bio project ]](https://static.fdocuments.in/doc/165x107/557d5e21d8b42ae1438b4dc3/ebola-virus-disease-bio-project-.jpg)