Early Detection of Breast & Genital Tract Malignancies.
-
Upload
clarissa-cobb -
Category
Documents
-
view
221 -
download
2
Transcript of Early Detection of Breast & Genital Tract Malignancies.

Early Detection of Breast &
Genital Tract Malignancies

Screening…?
• Organized identification
– High coverage of a target population
– Continuous quality assessment.
– Feasibility of treatment & follow up
• Of a pre - clinical disease state
• By a test that is repeated at a given interval

OR…
• Screening can be defined as
– The application of diagnostic tests or
procedures
– To asymptomatic people
– For the purpose of dividing them into two
groups:
• those who have a condition that would benefit
from early intervention
• and those who do not.

An Ideal Screening Program…• Features of the disease
– Significant impact on public health
– Asymptomatic period during which detection is possible
– Outcomes improved by treatment during asymptomatic period
• Features of the test – Sufficiently sensitive to detect disease during asymptomatic
period
– Sufficiently specific to minimize false-positive test results
– Acceptable to patients
• Features of the screened population – Sufficiently high prevalence of the disease to justify screening
– Relevant medical care is accessible
– Patients willing to comply with further work-up and treatment

To screen or To screen not ?
• Recommended
Screening
– Cervical Carcinoma
– Breast Carcinoma
– Colorectal Carcinoma
• Not yet , for…
– Ovarian Cancer
– Bronchogenic
Carcinoma
– Skin cancer
– Oral Cancer
– Endometrial Cancer

Effective Screening Program
• Should be tailored to suit the principles for national cancer control programs. We Should NOT copy other’s programs...
Otherwise… Too much money & effort will be spent with
minimal impact on the incidence & mortality from the disease.

Cervical Carcinoma
• Second in frequency among women cancers.• It is still the most frequent cancer in the
developing countries.
• 400,000 new cases identified each year
– 80% of new cases in developing countries
• At least 200,000 women die each year • Screening programs reduced the mortality from
cancer cervix in developed countries by 70%.

Incidence And Mortality For Cervical Cancer Vs Breast Cancer, [United States,
2000]192,000
12,900
40,200
4,400
0
50,000
100,000
150,000
200,000
New Cases Per Year Deaths Per Year
Breast CervicalBreastCervical
Source: American Cancer Society, 2000

Natural History Of Cervical Cancer
Source: PATH, 2001
HPV Infection
LSIL HSIL
Invasive Cancer
years
1%
35%
11%57%
>10%

HPV infection
• Condyloma Accuminata
– Exophytic
– Frond like surface
– Lesion may be single or multiple
– Located within or outside the transformation zone

HPV infection
• Subclinical HPV
– Flat lesions undetectable naked eye
– Best assessed after acetic acid application
– Shinny, snow-white lesions
– Irregular outline
– Satellite lesions beyond the transformation zone
– Strong or partial uptake of Lugol’s iodine

What Makes the Cervix Vulnerable?

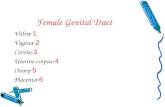
HPV and Genital Cancer
Normal Cx
Mild Dysplasia(CIN I)
Moderate Dysplasia
(CIN II)
Severe Dysplasia (CIN III /
CIS)
Invasive Disease

Elements of Screening of Cervical Cancer
Visual Inspection of the cervix / VIA
Colposcopy and Biopsy
History&
Raising Awareness
Pap smear

History Taking• Ask the client if she has experienced any of the
following symptoms: – Abnormal vaginal discharge– Contact bleeding– Irregular vaginal bleeding
• Ask about risk factors.– Start of sexual intercourse at a young age– Multiple sexual partners (ask in special circumstances: need
extra skills).– Male sexual partner having other partners (ask in special
circumstances: need extra skills)– Clinical history of infection by human papilloma virus or the
presence of condylomata acuminate
• Note all findings in the medical record



Acetic Acid –enhanced Visual Inspection of the Cervix “VIA”
1. Acetic acid coagulates mucus, which becomes easier to remove.
-allows a better view of the cervix
2. Acetic acid constricts the superficial vessels and blows up the columnar papillae so that they become pale.
allows a better view of the squamocolumnar junction
3. Acetic acid causes dehydration of the cells and coagulation of cellular proteins, thereby reducing the transparency of the epithelium
allows a better recognition of dysplastic epithelium

Abnormalities Seen After Acetic Acid• Aceto-white
• Margins and surface
• White gland openings
• Mosaic & punctation
• Abnormal vessels

What May Be Acetowhite• NOT All acetowhite lesions are cancer
• Any of these epithelial changes can become acetowhite– Healing or regenerating epithelium– Congenital transformation zone– Inflammation– Immature squamous metaplasia– HPV infection– SIL– Adenocarcinoma– Invasive squamous cell carcinoma
























VIA: Conclusions
• Alternative to cytology or HPV testing • Effective in identifying precancerous disease• Identify cancers • Effective in ruling out disease• Specificity of VIA is likely to depend on:
– training intervention– presence of STDs in population screened– importance placed on picking up diseased cases
• Positive predictive value of VIA can be increased through sequential or risk-based triage screening

Visual inspection with Lugol’s iodine Visual inspection with Lugol’s iodine ((VILI)VILI)
Original source: Alliance for Cervical Cancer Prevention (ACCP)www.alliance-cxca.org

What does VILI involve?
• Performing a vaginal speculum exam during which a health care provider applies Lugol’s iodine solution to the cervix.
• Viewing the cervix with the naked eye to identify color changes on the cervix.
• Determining whether the test result is positive or negative for possible precancerous lesions or cancer.

How VILI works:
• Squamous epithelium contains glycogen, whereas precancerous lesions and invasive cancer contain little or no glycogen.
• Iodine is glycophilic and is taken up by the squamous epithelium, staining it mahogany brown or black.
• Columnar epithelium does not change color, as it has no glycogen. • Immature metaplasia and inflammatory lesions are at most only
partially glycogenated and, when stained, appear as scattered, ill-defined uptake areas.
• Precancerous lesions and invasive cancer do not take up iodine (as they lack glycogen) and appear as well-defined, thick, mustard or saffron yellow areas.

What infrastructure does VILI require?
• Private exam room• Examination table • Trained health professionals• Adequate light source• Sterile vaginal speculum • New examination gloves, or HLD surgical gloves• Large cotton swabs• Lugol’s iodine solution and a small bowl• Containers with 0.5% chlorine solution• A plastic bucket with a plastic bag• Quality assurance system to maximize accuracy

Categories for VILI test results:
VILI Category Clinical Findings
Test-negativeSquamous epithelium turns brown and columnar epithelium does not change color; or irregular, partial or non-iodine uptake areas appear.
Test-positiveWell-defined, bright yellow iodine non-uptake areas touching the squamo-columnar junction (SCJ) or close to the os if SCJ is not seen.
Suspicious for cancer
Clinically visible ulcerative, cauliflower- like growth or ulcer; oozing and/or bleeding on touch.

VILI: test-negative
• The squamous epithelium turns brown and columnar epithelium does not change color.
• There are scattered and irregular, partial or non-iodine uptake areas associated with immature squamous metaplasia or inflammation.
Photo source: IARC

VILI: test-positive
• Well-defined, bright yellow iodine non-uptake areas touching the squamocolumnar junction (SCJ).
• Well-defined, bright yellow iodine non-uptake areas close to the os if SCJ is not seen, or covering the entire cervix.
Photo source: IARC

VILI: Suspicious for cancer
• Clinically visible ulcerative, cauliflower-like growth or ulcer; oozing and/or bleeding on touch.
Photo source: IARC

Management options if the VILI result is positive:
• Offer to treat immediately, (without colposcopy or biopsy, known as the “test-and-treat” or “single-visit” approach).
• Refer for colposcopy and biopsy and then offer treatment if a precancerous lesion is confirmed.

Management options if the VILI result is suspicious for cancer:
• Refer for colposcopy and biopsy and further management. Further management options include:– Surgery– Radiotherapy– Chemotherapy– Palliative care

Strengths of VILI:
• Simple, easy-to-learn approach that is minimally reliant upon infrastructure.
• Low start-up and sustaining costs.• Many types of health care providers can perform
the procedure.• High sensitivity results in a low proportion of
false negatives.• Test results are available immediately.• Decreased loss to follow-up.

Limitations of VILI:
• Moderate specificity may result in over-referral and over-treatment in a single-visit approach.
• Less accurate when used in post-menopausal women.
• There is a need for developing standard training methods and quality assurance measures.
• Rater dependent.

The Alternative…Downstaging !!!
The detection of the disease at an
earlier stage when still curable…
Just
Insert a speculum and look at the
cervix

Warning signs of early cervical cancer
1. Yellowish and friable epithelium
2. Abnormal contour
3. Ulceration
4. Atypical vessels
5. Very severe colposcopic atypia
6. Large, significant lesion
7. Canal lesion, going out of range
8. Perimenopausal and post radiation

Mimics of cervical cancer
1. Severe cervicitis e.g., herpes, syphilis
2. Benign ulceration e.g., trauma
3. Foreign body reaction
4. Granulomatous cervical conditions
5. Granuloma inguinale
6. Lymphogranuloma venereum
7. Schistosomiasis
8. Cervical condylomata• Cololposcopy aids differentiation.
• Histology is the gold standard



ACCP/ACS Guidelines for Screening
• When to Start Screening– Initiate cervical cancer screening about 3
years after the onset of vaginal intercourse.– Screening should begin no later than 21 years
of age.– The need for cervical cancer screening should
not be the basis for the onset of gynecologic care.
(CA: A Cancer Journal for Clinicians 53(1):27-43, 2003)

ACCP/ACS Guidelines for Screening
• When to Stop Screening:– Women aged >70 years with an intact cervix with
>3 documented, consecutive, technically satisfactory/normal/negative cervical cytology tests and no abnormal/positive cytology tests within the 10 years prior to age 70 may stop cervical cancer screening.
• Screening is recommended for 70+ year old women not previously screened and for whom information about previously screening is unavailable and for whom past screening is unlikely.
CA: A Cancer Journal for Clinicians 53(1):27-43, 2003)

ACCP/ACS Guidelines for Screening
• Screening After Hysterectomy – Vaginal cytology screening tests are not
indicated after total hysterectomy for benign gynecologic disease.
– Hysterectomy for CIN2 or greater is not considered benign.
CA: A Cancer Journal for Clinicians 53(1):27-43, 2003)

ACCP Guidelines for Screening
• Screening Interval:– After initiation of cervical screening, perform
annually with conventional cervical cytology smears or every 2 years using liquid-based cytology.
– Women >30 years of age with 3 consecutive, technically satisfactory normal/negative cytology results may be screened every 2 to 3 years unless they have a history of in utero DES exposure, HIV+, or are immunocompromised.
CA: A Cancer Journal for Clinicians 53(1): 27-43, 2003)

Abnormal PAP smear: Colposcopy



Multimodal Spectroscopy

Recent FIGO Recommendations For the Management of Abnormal Smear( Benedet,2000)
Persistent inflam., persistent ASCUS, LSIL, HSIL, AGCUS,Invasive
Colposcopy ± Biopsy
Normal or LSIL HSIL Invasive
6 mo smear x 2 LLETZ Appropriate TT
Normal Persistent
Annual screening

LLETZ Large Loop Excision of the Transformation Zone

Against Breast Cancer

Elements of Screening of Breast Cancer
Clinical Breast Examination
Mammography
History&
Raising Awareness
Breast Self Examination

Approach to the Client• Explain to the client the importance of breast
examination as a tool for early detection of abnormalities especially cancer that results in better prognosis.
• Explain and train all clients to perform breast self-examination and instruct them when, how to do it and abnormalities to look for.
• Maintain good communication channels with the clients whose screening shows suspicious results to ensure that follow-up can be achieved: note the client’s telephone, address and who to contact.
• Respond to all the client Needs and inquiries and provide reassurance while encouraging her to perform extra-necessary procedures

History Taking • Ask about risk factors:
– Family history of breast cancer– Menstruation after age of 55 or before age of 12– Menstrual cycles lasting more than 40 years– Hormone administration– Obesity– Smoking– Previous uterine cancer– First pregnancy after age 30 or no pregnancies
• Ask about symptoms:– Pain– Swelling in breast or armpit– Discharge from nipple– Discoloration of the skin
• Note all findings in the medical record


What changes should She be aware of?
• A change in size – it may be that one breast has become noticeably larger or noticeably lower
• A nipple has become inverted (pulled in) or changed its position or shape
• A rash on or around the nipple• A discharge from one or both nipples• A puckering or dimpling of the skin• A swelling under the armpit or around the collarbone (where the
lymph nodes are)• A lump or thickening in the breast that feels different from the
rest of the breast tissue• Constant pain in one part of the breast or in the armpit.

Clinical Breast Examination• Yearly Done
• Postmenstrually
• Should be part of any
gynecologic examination.
• Refer client to a MOHP
hospital if needed.
• Explain the procedures to
the client, and ask her to
undress to the waist and
stand relaxed.
• Inspection• Ask the client to put her hands on
her waist, and to push inwards to contract the chest muscles.
• Inspect both breasts for any puckering, abnormalities of the skin, change in the nipple such as swelling or retraction, asymmetric appearance or nipple discharge.
• While the client lies on her back, inspect breasts to detect any abnormalities.
• Inspect for any abnormal discoloration of the skin
• Note all findings in the medical record.

Palpation
• Palpate the breast tissue for any breast masses as well as the axilla and supraclavicular area for any enlarged lymph nodes.
• Be sure that all parts are felt carefully.• Milk the nipple after massage of the areola medially to
identify any fluid discharge. • Describe as none, clear, milky, pinkish or dark-bloody
color.• If any abnormality is detected by examination, refer to
specialist for mammography.• Note all findings in the medical record.

Breast Self Examination• Tell the client to conduct breast self-examination once
every month after the end of menstruation starting at the age of 20 years for life.
• Palpation of the breasts during bathing is recommended. – Soap and water on the skin facilitates palpation of the breast
tissue.
• It is important to note the normal consistency of the breasts at the first examination so that she will be aware of any changes in subsequent examinations.




Diagnosis Vs Screening??

Mammography…A debate
• Before the age of 40 and after 70 there is NO recommendations for routine mammographic screening
• Currently, the American Cancer Society and the American College of Radiology encourage mammograms every two years for women ages 40 to 49.
• Yearly mammographic examination are done from the age of 50-70 years.

Other tools..
• Breast Ultrasonography
• MRI• Thermography• BRCA

Thank you!!!