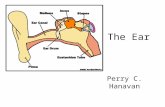
The Ear The ear consists of : 1-THE EXTERNAL EAR 2-THE MIDDLE EAR, OR TYMPANIC CAVITY
Ear Mathes
-
Upload
1lluminatt1 -
Category
Documents
-
view
220 -
download
3
Transcript of Ear Mathes

C H A P T E R
1 Reconstruction of t h e Auricle
CONGENITAL DEFORMITIES History of Auricular Reconstruction Anatomy Practical Embryology and Understanding the
Middle Ear Problem Et~ology Diagnosis Associated Deformities Complete Microtia (Hypoplasia)- Methods of Microtia Repair , . First Stage of Reconstruction Other Stages of Aur~cular Construction Variations in Total Ear Reconstruction Technique
Secondary Reconstruction Bilateral Microtia The Constricted Ear Cryptotia The Prominent Ear
ACQUIRED DEFORMITIES Replantation of the Amputated Auricle Deformities without Loss of Auricular Tissue Deformities with Loss of Auricular Tissue ,, ,*LA Partial Auricular Loss Specific Regional Defects Tumors of the Auricle
CONGENITAL DEFORMITIES cartilage under mastoid skin, then separated it from
Total auricular reconstruction with autogenous tissues is one of the greatest technical feats a reconstructive surgeon may encounter. Whereas an inherent under- standing of sculpture and design influences one's surgical success, strict adherence to basic principles of plastic surgery and tissue transfer is of equal importance.
During the years, ear reconstruction has stimulated the imagination of many surgeons who have provided countless contributions. Various techniques that have stood the test of time are documented, and guidelines for management of a variety of ear deformities are provided.
History of Auricular Reconstruction Ear reconstruction was first referred to in the Sushruta Samhita,' which suggested a cheek flap for repair of the earlobe. As early as 1597, Tagliacozzi described repair of both upper and lower ear deformities with retroauricular flaps2 In 1845, Dieffenbach described repair of the ear's middle third with an advancement flap (see Fig. 74-55)3; this may occasionally have appli- cation today. This early work focused mainly on trau- matic deformities. However, by the end of the 19th century, surgeons began to address congenital defects- particularly prominent ears.4
The origin of microtia repair had its significant beginnings in 1920, when Gillies5 buried carved costal
the head with a cervical flap. Ten later, Pierce6 modified this method by lining the new sulcus with a skin graft and building the helix with a tubed flap. In 1937, Gillies7 repaired more than 30 microtic ears with use of maternal ear cartilage; these were found to pro- gressively resorb.$ Experiencing the same frustration as others?-l2 Steffenseni3 used preserved rib cartilage to produce excellent results but later reported pro- gressive resorption of the same cartilage frameworks.I4
Amajor breakthrough came in 1959,when Tanzeri5 rekindled use of autogenous rib cartilage, which he carved in a solid block. His excellent results have per- sisted duringthe years.I6In an effort to circumvent large operations, Cronin" introduced silicone ear frame- works but found that like other inorganic implants (e.g., polyethylene, nylon mesh, Marlex, polyester net, and Teflon), they suffered a high incidence of extru- sion.18,19 Initially, Cronin20 minimized this problem by providing fascia lata or galeal and fascia1 flaps for extra autogenous rim coverage, but when he found later that the alloplastic frames still extruded, he discontinued this practice. -mrnr-.--a .TI .~flr,i!LI
In spite of some investiga'fir? ?n&i&as'iwith MEDPOR frame~orks,2~'~* these foreign substances seem to encounter the same problems that have plagued silicone. Most recently, a patient came to my consultation with an infectedsinus track that had been draining from her MEDPOR implant for 2 years; another patient presented with three separate exposed areas of MEDPOR in his reconstructed ear. On the other
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

634 1 1 1 + THE HEAD AND NECK
hand, an autogenous ear framework in a microtia patient is rarely or never lost; only one has been lost from trauma in a patient with poor compliance to post- operative instr~ct ions.~ To date, more than 70 of my reconstructed ears have survived major trauma.
For many years, there has been considerable inter- est in development of a"prefabricated" framework from autogenous cartilage to circumvent the necessity of fab- ricating an ear framework during a prolonged recon- structive procedure and to attempt to eliminate the variability of the surgeon's artistry in providing a real- istic ear framework from rib cartilage. Young24 and
first conceived the idea of framework prefabri- cation before the actual auricular reconstruction in the 1940s. This innovative technique was accomplished by means of"diced" pieces of autogenous rib cartilage that were placed in a fenestrated two-piece, ear-shapedvital- lium mold, which in turn was banked in the patient's abdominal wall. After several months, they retrieved the banked mold, opened it, and harvested the frame- work of cartilage chips, which had united by connec- tive tissue that had grown through the mold's openings. However, the results were not consistent, perhaps because contraction of the fibrous tissue surrounding the multiple cartilage islands distorted the resultant framework.
Interest in this prefabrication concept has been rekindled through modern "tissue engineering" tech- niques in which cartilage cells are grown in the lab- oratory and seeded on a synthetic, biodegradable ear form that is then implanted beneath the skin of a mouse.26 The early results are interesting, but the trial work is not being carried out under the same condi- tions as in a clinical human ear reconstruction- the investigators' frameworks are being placed under the loose skin of an animal's back, whereas in human ear repair, the new framework must be placed under- neath snug skin just in front of the hairline in the ear region.
Although these new laboratory studies are intrigu- ing, unless a firm, substantial three-dimensional framework can be produced from autogenous tissues, it is likely to suffer the same consequences of frame- works created by Young's and Peer's method, that is, flattening out under the restrictive, two-dimensional skin envelope under which the framework must be placed to complete the ear reconstruction. The other obvious limitation of prefabricated ear frameworks is the difficulty in accommodating the great variation in size and shape that must be produced to match the opposite, normal ear. In sculpting directly from rib car- tilage, these limitations do not exist because the surgeon develops the required specific size and shape each time.
However, there has long been an interest in devel- opment of a living prefabricated ear framework. Research has begun2' to explore the possibilities of
bioengineeringfirrn, autogenous cartilage frameworks to see whether some of the limitations can be over- ~ o m e . ~ ~ u t o ~ e n o u s costal cartilage is grown in varying- sized molds made from "idealized" frameworks that are sculpted and cast; but to fill these molds with chon- drocytes obtained by digesting a large volume of rib cartilage would merely be reproducing Young's and Peer's work by newer technology. The goalis to exploit the technology by using a small piece of cartilage (perhaps obtained by biopsy from the microtia patient at age 3 to 4 years, when neochondrogenic potential is high), then to efficiently extract the chondrocytes, to expand them in culture, and to infuse them into the idedmatricial substrate within the ideal ear frame- work mold for that specific patient. Once generated to satisfaction, the engineered framework would be "banked" under the patient's hairless ~eriauricular skin as the first reconstructive surgical phase. For this tech- nique to be successful, the major problems that must be overcome are replicating sufficient chondrocytes from a small cartilage sample (25 to 50 million cellslml are needed for neocartilage formation in a construct, and the ear mold volume is about 5 mL) and the ability of those chondrocytes to regeneratefirm cartilage matrix so that the engineered framework can withstand the pressure caused by the constraints of a two-dimensional skin cover that is taut, inelastic, and restrictive.
Until tissue engineering evolves beyond these prob- lems, sculpted autogenous rib cartilage remains the most reliable material that produces results with the least complication^.'^'^^^^^^^^ Furthermore, rib cartilage provides the most substantial source for fabricating a total ear framework. Although contralateral concha1 cartilage has been used for this purp0se,3~.~~ it seems best to reserve auricular cartilage for repair of partial ear defects, for which considerably less tissue bulk is needed.
Anatomy The ear is difficult to reproduce surgically because it is composed of a complexly convoluted frame of del- icate elastic cartilage that is surrounded by a fine skin envelope (Fig. 74- l).The denuded cartilage framework conforms almost exactly to the ear's surface contours except for its absence in the earlobe, which consists of fibrofatty tissue rather than cartilage. In most microtic vestiges, the presence of this lobule tissue is a valuable asset in the repair (see Fig. 74-8). When the lobule is lost in total ear avulsions, it is best recreated by shaping the bottom of the carved ear framework to resemble the lobe.
The ear's rich vascular supply comes from the superficial temporal and posterior auricular vessels, which can nourish a nearly avulsed ear even on sur- prisingly narrow tissue pedicles. The sensory supply
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-1. Anatomy of the auricle.
Auricular tubercle Cruro of antihelix
Triongulor fossa
Crus of he/ix Cymba o f conch
Concha o f aur ic le 31 Cavum o f concha Ext . auditory m,*s
/nterfrogic notch
is chiefly derived from the inferiorly coursing great auricular nerve. Upper portions of the ear are sup- plied by the lesser occipital and auriculotemporal nerves, whereas the conchal region is supplied by a vagal nerve branch.
Understanding this anatomy facilitates blocking of the ear with local anesthetic solution (Fig. 74-2). First, the great auricular nerve is blocked by injecting awheal
Lesser occioita/ n. J U L / B S Mastoid branch o f lesser
occipjto, n.
Greater our~cu/ar n -1
74 + RECONSTRUC~ION OF ME AURICLE
r f f e l i x
Greater auricu/or n. +I
B FIGURE 74-2. Sensory nerve supply of the auricle.
underneath the lobule. After awalsmg its effect, one continues injecting upward along the auriculocephalic sulcus, around the top of the ear and down to the tragus. Finally, the vagal branch can be anesthetized without discomfort by traversing the conchal cartilage with a needle placed through the already anesthetized auricu- locephalic sulcus to raise a wheal of solution just behind the canal.
Practical Embryology and Understanding the Middle Ear Problem At consultation, parents of a microtic infant are usually most concerned with the hearing problem. They believe either that the child is completely deaf on the affected side or that hearing can be restored by merely opening a hole in the skin. Because these are misconceptions, the physician can do much to allevi- ate parents' anxieties by fundamentally explaining ear embryology. Because the human ear's receptive (inner) portion is derived from different embryologic tissue than the conductive (external and middle) portion (Fig. 74-3), the inner ear is rarely involved in micro- tia, and these patients have at least some hearing in the affected ear. The problem is conduction, which is blocked by the malformed middle and external ear complex. Typically, these patients have a hearing threshold of 40 to 60 dB on the affected side. By com- parison, normal function allows us to hear sounds beginning between 0 and 20 dB.
Tissues of both the middle ear and external ear are derived chiefly from the first (mandibular) and second (hyoid) branchial arches. The auricle itself is formed from six ''ldloclts" of tissue that lie along these arches and can first be seen in the 5-week embryo (Figs. 74- 4 and 7 4 - ~ ) . ~ ~ " ~ 0 n the other hand, the inner ear first
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
Auditory ossicles Preosseus embedded i n Ext. acoustic
t~t#b?a'dl b o ~ a tb1212t?tli~t? tzssua meatus
tube cavity ectodermal plate
appears at 3 weeks and is derived from tissues of dis- tinctly separate ectodermal origin. Perhaps this explains why it is usually spared the developmental mishap that almost invariably involves the middle ear of microtic patients. Refinements in radiographic technique (poly- tomography and computed tomography scans) have only occasionally demonstrated dysplasia and hypopla- sia of the inner Inner ear abnormalities are found in approximately 10% of microtia and atresia patients, but the abnormalities are usually slight (e.g., a dilata- tion of the lateral semicircular canal). Interestingly, in evaluating approximately 1500 microtic cases during a 25-year period, the author has seen onlythree patients
FIGURE 74-4. Development of the auricle in a 5-week human embryo: 1 to 6, elevations (hillocks) on the mandibularand hyoid arches; ov, oticvesicle. (AfterArey.)
FIGURE 74-3. Partly schematic section of the ear in a 3-month embryo. (From Arey LB: Developmental Anatomy, 6th ed. Philadelphia, WB Saunders, 1954.1
who were totally deaf. Remarkably, these were patients with unilateral microtia who had no family history of microtia. Because of their normal inner ear, even patients with bilateral microtia usually have servicea- ble hearing with use of bone-conductive hearing aids to overcome the transmission block. If they are referred to an audiologist so that aids can be used as soon as possible, these patients usually develop normal speech. There is no point in waiting several months. Hearing aids should be applied within weeks of birth. Because these bone-conductive aids are cumbersome and label the childUdifferent" from his or her peers, it is optimal to correct the hearing deficit surgically to eliminate the aids. However, surgical correction of this conduc- tive problem is difficult because the middle ear beneath the closed skin is not normal.
Exploration involves one's cautiously avoiding the facial nerve while drilling a canal through solid bone. One must usually provide a tympanum with tissue grafts; the distorted or fused ossicles may be irrepara- ble. Because skin grafts do not take well on the drilled bony canal, chronic drainage is a frequent complica- tion and meatal stenosis is common. Finally, unless the surgeon can closethe functional difference between the repaired and normal ear to within 15 to 20 dB (an elusive feat inmost surgeons' hands), binaural hearing will not be achieved. However, in the hands of a com- petent otologist with a large volume of experience, restoration of middle ear function surgically can be rewarding-even if only one ear is in~olved.~'-'~
Because many microtia patients do well without middle ear surgery-eight of nine patients have
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
- \ . E s m m Adult
FIGURE 74-5. The retardation of growth of the auricular component of the mandibular arch and the expansion and forward rotation of the component of the hyoid arch. (After Streeter; from Patten M: Human Embryology, 3rd ed. New York, McCraw-Hill, 1968.)
unilateral microtia, and they are born "adjusted" to the monaural condition-most surgeons presently believe that potential gains from middle ear surgery in unilateral microtia are outweighed by potential risks and complications of the surgery itself and that this surgery should be reserved for children with bilateral microtia. It is the author's conviction that if the oto- logic surgeon is not comfortable with the unilateral cases, he or she should certainly not be operating on patients with bilateral microtia either.
When middle ear surgery is contemplated, a team approach must be planned with an experienced, com- petent otologist. In these patients, the auricular con- struction should precede the middle ear surgery; once an attempt is made to "open the ear," the virgin skin is scarred, which compromises a satisfactory auricu- lar construction. In the future, implantable acoustic devices may offer a solution for these patients.
occurrence is estimated at 1 in 4000 in Japanese and as high as 1 in 900 to 1200 births in Navajo I n d i a n ~ . ~ ~
HEREDITARY FACTORS In a superb study conducted by R~gers,~morphologic, anatomic, and genetic interrelationships were shown to exist between microtia, constricted ears, and pro- truding ears. In this thorough investigation, he demon- strated that these deformities are interrelated and can be hereditary.
Preauricular its and sinuses and a combination of pits, preauricular appendages, cupping deformity, and deafness are hereditarily dominant.'^^' Both dominant and recessive character&cs have been revealed in deaf- ness associated with several auricular abn~rmalities.~' Ear deformities frequently recur in families of mandibulofacial dysostosis (Treacher Collins syn- d r ~ m e ) . ~ ~ In the author's exverience, these are fre- quentli constricted ear defoimities, an abnormality
Etiology that is known to be hereditary."*50-52 Hanharf" found a severe form of microtia associated with a cleft or high
INCIDENCE palate in 10% of family members studied, and Tanze13 According to an extensive study conducted by found that approximately 25% of his 43 microtia Grabb,44 microtia occurs once in every6000 births. The patients had relatives with evidence of the first and
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
second branchial arch syndrome (craniofacial micro- sornia); microtia was present in four instances.
In 4.9% ofthe author's 1008 mlcrofia family histories revealed that major auricular deformities occurred within the immediate family (i.e., parents, siblings, aunts, uncles, or grandparent^)?^ When "distant" relatives were included, the percentage jumped up to 10.3%. In 6% of the patients, preauric- ular skin tags or minor auricular defects were observed in the immediate family. This number also rose to 10.3% when a l l relatives were included. Immediate family members of 1.2% of patients had normal auricles but underdeveloped jaws or facial nerves.=
In a thorough, intensive survey of 96 families of their 171 microtic patients, Takahashi and Maeda54 ruled out chromosome aberrations and concluded that inheritance must be multifactorial and that the recur- rence risk is 5.7%. In previous studies, others have found multifactorial inheritance between 3% and 8% in first- degree relatives. If a couple has two children with micro- tia, the riskof recurrence in future offspring is thought to be as high as 15%.
SPECIFIC FACTORS McKenzie and Craig55 and Poswillo" theorized that the cause of developmental auricular abnormalities is in utero tissue ischemia resulting from either an oblit- erated stapedial artery or a hemorrhage into the local tissues. This speaks in favor of the deformity's arising from a mishap during fetal development rather than from a hereditary source. In support of this, the author has treated 12 microtia patients who have an identical twin with normal Only one set of the author's identical twin patients have had concordance for outer ear deformities. Of interest is that each of these male twins with microtia also had signs and symptoms of pyloric stenosis within 2 days of each other and were operated on at 6 weeks of age.
The occurrence of deafness and occasional micro- tia resulting from rubella during the first trimester of pregnancy is well known. Also, certain drugs during this critical period may be causative; the author has seen at least three cases of microtia that resulted from the mother's ingestion of the tranquilizer thalido- mide.57.58 Isotretinoin has also been cited as causing ear deformities when it is ingested during the first t r ime~ter .~~ In the author's series, several mothers had been unaware of this problem and had used this drug to control acne. Other medications that reportedly cause microtia are clomiphene citrate6" and retinoic acid:'
Diagnosis CLASSIFICATION Rogers4 noted that one could classify most types of auricular hypoplasia in a descending scale of severity.
TABLE 74-1 + CLINICAL CLASSIFICATION OF AURICULAR DEFECTS (TANZER)
Anotia Complete hypoplasia (microtia)
With atresia of external auditory canal Without atresia of external auditory canal
Hypoplasia of middle third of auricle Hypoplasia of superior third of auricle
Constricted (cup and lop) ear Cryptotia Hypoplasia of entire superior third
Prominent ear
This corresponds to Streeter's depiction of embryologic patterns of auricular de~elopment.~~ Rogers divides developmental ear defects into four groups: microtia; lop ear, that is, folding or deficiency of the superior helix and scapha; "cup" or constricted ear, with a deep concha and deficiency of the superior helix and antihelical crura; and the common prominent or protruding ear.
Using a system that correlates with embryologic development, Tanzer classifies congenital ear defects according to the approach necessary for their surgical correction (Table 74-1).62
Associated Deformities As discussed previously, embryologic development dic- tates that the microtic ear is usually accompanied by middle ear abnormalities. In full-blown, classic micro- tia, one usually finds canal atresia and ossicular abnor- malities. The middle ear deformity may range from diminished canal caliber and minor ossicular abnor- malities to fused, hypoplastic ossicles and failure of mastoid cell vneumatization.
Because the auricle develops from tissues of the mandibular and hyoid branchial arches, it is not sur- prisingthat a sigdicant percentage of microtic patients exhibit deficient facial components that originate from these embryologic building blocks. These deformities are compiled underahemifacial microsomia" (first and second branchial arch syndrome) (Fig. 74-6), and an obvious facial asymmetry was noted in 35% of the author's 1000 microtia patienkZ3 The most complete genetic expression of this condition includes defects of the external and middle ear; hypoplasia of the mandible, maxilla, zygoma, and temporal bones; macrostomia and lateral facial clefts; and atrophy of facial muscles and parotid gland.4863p64 Furthermore, Brentz3 found that 15% of his 1000 patients had paresis of the facial nerve. Dellon et aP5 have shown that the palatal muscles are rarely spared in this syndrome.
Urogenital tract abnormalities are increased in the presence of mi~ro t i a ,~~ particularly when the patient
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
TABLE 74-2 + DEFORMITIES ASSOCIATED WITH MICROTIA*
FIGURE 74-6. Patient with unilateral craniofacial microsomia (first and second branchial arch syndrome] displaying microtia; macrostomia; hypoplasia of the zygoma, maxilla, and mandible; and soft tissue hypoplasia.
is afflicted with other manifestations of the first and second branchial arch syndrome (Table 74-2).67
Complete Microtia (Hypoplasia) CLINICAL CHARACTERISTICS Microtia varies from the complete absence of auric- ular tissues (anotia) to a somewhat normal but small ear with atretic canal. Between these extremes, one finds an endless variety of vestiges, the most common being a vertically oriented sausage-shaped nubbin (Figs. 74-7 and 74-8; see also Fig. 74-26). Microtia is nearly twice as frequent in boys as in girls, and the right-left-bilateral ratio is roughly 6 : 3 : 1 (Table 74-3) .23,29,68
In most instances, the microtic lobule is displaced superiorly to the level of the opposite, normal side, although incomplete ear migration occasionally leaves it in an inferior location. Approximately one third to half the patients exhibit gross characteristics of
Branchial arch deformities Obvious bone and soft tissue deficit, 36.5%
Family perceives it as "significant," 49.4% Overt facial nerve weakness, 15.2%
Of these, more than one branch involved, 42.6% Macrostomia, 2.5% Cleft lip and/or palate, 4.3% Urogenital defects, 4.0% Cardiovascular malformations, 2.5% Miscellaneous deformities, 1.7%
"Author's series of 1000 patients.
hemifacial microsomia, although Converse et a169*70 have demonstrated tomographically that skeletal deficien- cies exist in all cases. Whatever the deformity, the author has been impressed with its potential for psychologi- cal havoc among the entire family, varying from the patient's emotional insecurity to the parents' deep- seated guilt feelings.
GENERAL CONSlDERATlONS Duringthe initial consultation, it is imperative to real- istically describe to the patient and family the tech- nical limitations involved in surgical correction of microtia and to outline alternative methods of man- aging each individual's particular deformity. The author strongly favors autogenous rib cartilage for auricular construction. Although its use necessitates an operation with significant morbidity of the patient, it must be noted that unlike a reconstruction using alloplastic materials, a successful construction with autogenous tissue is less susceptible to trauma and therefore eliminates a patient's overcautious concern during normal activities.
The age at which an auricular construction should begin is governed by both psychological and physi- cal considerations. Because the body image concept usually begins forming around the age of 4 or 5 years," it would be ideal to begin construction before the child enters school and is psychologically trau- matized by peers' cruel ridicule. However, surgery
TABLE 74-3 + MICROTIA: AUTHOR'S SERIES OF 1000 PATIENTS
Patients Total No. of Ears
Right 582 (58.2%) 582 Boys 63 1 (63.1 %) Left 324 (32.4%) 324 Girls 369 (36.9%) Bilateral 94 (9.4%) 188
1000 100.0% 1094 1000 100.0%
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

1 - ' &&- .:.::-
lib
FIGURE 74-7. Long-term stability of ears constructed with autogenous rib cartilage grafts. First patient, an 8-yedr- old girl with microtia shown preoperatively and then at 1.4, and 12 years postoperatively. Second patient, a 13-year- old boy shown preoperatively, at 1 year, and at 10 years postoperatively, comparing both ears. Third patient, a 6-year-old girl shown preoperatively and then at 1 and 8 years postoperatively; ear growth is particularly obvious in this patient. Fourth patient, an &year-old boy shown preoperatively and immediately after cartilage grafting and then at 2 and 8 years postoperatively. Fifth patient, a 6-year-old girl shown preoperativefy, at 1 year, and at 12 years postoperatively, comparing both ears. (From Brent B: Auricular repair with autogenous rib cartilage grafts: two decades of experience with 600 cases. Plast Reconstr Surg 1992;90:355.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-8. Lobule transposition. noove, leR, The microtic vestige. Above, IeR center, The healed ear several months after framework insertion. Above, right center, By incision around it, the lobule has been mobilized as an infe- riorly based flap; an incision has been made at the proposed superior inset margin. Above, right, through below, l e t center. The skin overlying the lower ear region has been loosened and slid under the elevated framework's tip to surface the "floor" beneath it. Note that connective tissue has been carefully preserved over the cartilaginous tip. Below, right center, The lobule has been filleted and wrapped around the framework tip in a two-layered wound closure; the former lobule site is closed, and the vestigial tissue is excised from the triangular fossa region. Below, right, The healed repair. [From Brent B: Auricular repair with autogenous rib cartilage grafts: two decades of experience with 600 cases. Plast Reconstr Surg 1992;90:355.)
should be postponed until rib growth provides substantial cartilage to permit a quality framework fabrication.
In the author's experience with more than 1500 microtia patients from age 1 month to 62 years, the patients and their families consistently stated that their psychological disturbances rarely began before age 7 years and usually became overt from ages 7 to 10 years. The family is anxious to have the ear repaired as soon as possible, but it is important for the surgeon to wait until it is technically feasible. There usually is enough rib cartilage to serve as the sculpting medium by 6 years of age, allowing ear reconstruc- tion; however, if the patient is small for age or the opposite, normal ear is large, it is prudent to post- pone the surgery for several years. The optimal age to begin is about 8 years. At this age, the child is more aware of the problem and usually wants it resolved as much as the family does. The child can also be more cooperative than a younger child during the postop- erative care phase.
At age 6 years, the normal ear has grown to within 6 or 7 mm of its full vertical height," which permits one to construct an ear that will have reasonably con- stant symmetry with the opposite normal ear. In his follow-up mail su~ey ,Ta~ lze r~~ '~ found that an ear con- structed from autogenous rib cartilage grows at the same rate as the normal ear, with the possible excep- tion of patients operated on at 6 to 7 years of age, in whom he noted that 50% of the ears lagged several millimeters behind in growth; the roles played in the growth of his patients' surgically constructed ears by soft tissues and by cartilage have not been determined. .
In evaluation of "lay" data from my first 500 unilat- eral microtia patients operated on between the ages of 5 and 10 years with a minimum 5-year follow-up (76 patients) ,29 48% of the constructed ears grew at an even pace with the opposite,normal ear; 41.6% grew several millimeters larger; and 10.3% lagged several millime- ters behind the normal side. From the limited number of long-term patients in this age group (it is particu- larly difficult to get patients and their families to fly
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
out for a visit once the surgical repair is complete), most constructed ears have grown, and many of these have not only kept up with the little residual growth in the opposite ear but have slightZy overgr~wn.'~ Few have shrunk, softened, or lost their detail (see Fig. 74- 7). On the basis of these observations, one should try to match the opposite side duringthe preoperative plan- ning session, regardless of age. There is certainly no reason to construct the ear larger, as some investiga- tors have previously thought, and one might even con- sidermakingthe framework several millimeters smaller in the youngest patients, in whom normal, in situ costal cartilage can be expected to exceed normal auricular cartilage growth.
Methods of Microtia Repair STAGING THE AURICULAR CONSTRUCTION The cartilage graft is the "foundation" of an auricular construction, and as in construction of a house, it should be built and well established under ideal con- ditions before further stages or refinements are under- taken. By implanting the cartilage graft as the first surgical stage, one takesadvantage of the optimal elas- ticity and circulation of an unviolated, virgin skin "pocket." For these reasons, the author prefers to avoid initial lobule transposition or vestige division; the resulting scars cannot helv but inhibit the circulation w
and restrict the skin's elasticity, which in turn dirnin- ishes its ability to safely accommodate a three- dimensional cartilage graft. In the author's experience, it seems easier both to judge the earlobe's placement and to "splice" the lobule correctly into position with reference to a well-established, underlying framework. Although Tanzer transposed the lobule simultaneously with implantation of the cartilage graft in the last three patients of his clinical practice74 and Nagata routinely does this in his t e ~ h n i a u e , ~ ~ the author finds that there
L '
is far less risk of tissue necrosis and that it is far more accurate to transpose the lobule as a secondary pro- cedure (see Fig. 74-8).75-TOne can safely transpose the lobe and simultaneously elevate the ear from the head with skin graft if the earlobe vestige is short because its small wound closure will not compromise the ear's anterior circulation (see Fig. 74-16).~~,'~
During the third stage, the ear is separated from the head and surfaced on its underside with a skin graft to create an auriculocephalic sulcus.
In general, the fourth stage combines tragus con- struction, conchal excavation, and simultaneous con- tralateral otoplasty, if indicated. By combination of these procedures, tissues that are normally discarded from an otoplasty can be employed advantageously as free grafts in the tragus construction.
PREOPERATIVE CONSULTATION
Duhg the itid consultation, surgical expectations and psychological considerations should be discussed with the patient and the family, emphasizing goals of the reconstruction. Although costal cartilage can be carved to form a delicate framework, the volume and projection of the furnished three-dimensional frame- work are limited by the two-dimensional skin flap under which it is placed. Furthermore, because the retroauricular-mastoid skin that covers the framework is somewhat thicker than normal, delicate anterolat- era1 auricular skin, it blunts the details of a carved framework. It is important for these limitations to be stressed to patient and family, lest they have unrealis- tic expectations of what can or cannot be produced by surgery. Hence, the plastic surgeon's aim is to achieve accurate representation, that being to provide an acceptable facsimile of an ear that is the proper size, in the proper position, and properly oriented to other facial features.
During the consultation, surgical discomforts and inconveniences should be described, including the expected chest pain, duration of dressings, and limited activities for 4 to 6 weeks. Finally, risks and possible complications of the surgery are discussed thor- oughly. These include pneumothorax, cartilage graft loss secondary to infection, skin flap necrosis, and hematoma. It should be stressed that with proper precautions, these risks are comparatively less severe than the emotional trauma associated with an absent ear.
PLANNING, PREPARATION, AND CORRELATION WITH THE CORRECTION OF OTHER FACIAL DEFICIENCIES The result of a total ear reconstruction depends not only on a surgeon's meticulous surgical technique but on careful preoperative planning. It is essential that one practice carving techniques on a volume of human cadaver cartilage before any live-patient application. An acrylic or plaster replica of a normal ear serves as an excellent model for practice carvings.
During the patient's second office consultation, pre- operative study photographs are obtained and an x- ray film pattern is traced from the opposite, normal ear. This pattern is reversed, and a framework pattern is designed for the new ear (Fig. 74-9). After steriliza- tion, these patterns serve as guidelines for framework fabrication at the time of surgery.
The reconstructed ear's location is predetermined by first noting the topographic relationship of the oppo- site, normal ear to facial features and then duplicat- ing its position at the proposed reconstruction site. First, one compares the vestige's height from the front view with that of the opposite, normal ear. From the
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
FIGURE 74-9. A to C, Preoper- ative determination of auricular location. The ear's axis is posi- tioned to match the opposite side, roughly parallel to the nasal profile; the helical root is positioned equi- distant from the lateral canthus. The reversed auricular pattern is traced 6 mm below the lobule, as determined by frontal measure- ment.
side, it should be noted that the ear's axis is roughly parallel to the nasal p r~ f i l e .~~ '~ ' Finally, one notes and records the distance between the lateral canthus and the normal ear's helical root.
The ear's location is established in the office by first taping the reversed film pattern to the proposed construction site and then adjusting its position until it is level to and symmetric with the opposite normal ear. The pattern is traced on the head, noting the ear's axial relation to the nose, its distance from the lateral canthus, and its lobule's position, which is usually superiorly displaced. The ear's new position is straight- forward and easy to plan in a pure microtia, but much more difficult when severe hemifacial micro- somia exists. Not only are the heights of the facial halves asymmetric, but the anteroposterior dimen- sions of the affected side are foreshortened as well. In these patients, one best plans the new ear's height by lining it up with the normal ear's upper pole- its distance from the lateral canthus is somewhat arbitrary.
In pure microtia, the vestige-to-canthus distance mirrors the helical root-to-canthus distance of the opposite, normal side. However, in patients with severe hemifacial microsomia, the vestige is much closer to the eye. If one places the new ear's anterior margin at the vestige site, the ear appears too close to the eye
if one uses the measured distance of the normal side as a guide, the ear looks too far back on the head. In these patients, it is best to compromise by selecting a point halfway between these two positions.
When both auricular construction and bone repairs are planned, integrated timing is essential. Most often the family pushes for the ear repair to begin first, which helpfully ensures the auricular surgeon unscarred skin. The craniomaxillofacial surgeon argues that by going first, the facial symmetry will be cor- rected, thus making ear placement ea~ier.7~ This is unnecessary when the described guidelines are followed.
If the bone work is done first, it is imperative that scars be peripheral to the proposed auricular site. When a coronal incision is used to approach the upper face or to harvest cranial bone grafts, special care must be taken so that the scar does not precariously lie over the future region of the upper helix.
First Stage of Reconstruction Almost invariably, the author's first-stage"foundation" in correction of microtia is fabricating and inserting the cartilaginous ear framework. As discussed previ- ously, scars can be a significant handicap; the author rarely employs a preliminary procedure.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

1 1 1 + THE HEAD AND NECK
OBTAINING THE RIB CARTILAGE
Rib cartilages are obtained en bloc from the side con- tralateral to the ear being constructed to use natural rib configuration. The rib cartilages are removed through a horizontal or slightly oblique incision made just above the costal margin.Mter division of the exter- nal oblique and the rectus muscles, the film pattern is placed on the exposed cartilages to determine the nec- essary extent of rib resection.
The helical rim is fashioned separately with cartilage from the first free-floating rib (Fig. 74-10). Excision of this cartilage facilitates access to the
synchondrotic region of ribs six and seven, which sup- plies a sufficient block to carve the framework body. Extraperichondrial dissection is preferable in obtain- ing an unmarred specimen. One can significantly decrease well-documented chest deformitiess0381 by pre- serving even a minimal rim of the upper margin of the sixth rib cartilage where one obtains the basic shape of the ear (see Fig. 74-10). This precautionary measure retains a tether to the sternum so that the rib does not flare outward to distort the chest as the child grows. If the synchondrotic region seems inadequate in width, one can compensate for frame- work width by bowing the helix away from the
FIGURE 74-1 0. Rib cartilage harvest for ear framework fabrication. Note that the upper border of the sixth cartilage is preserved; this will help prevent subsequent chest deformity as the child grows. The entire "floating carti- lage" will be used to create the helix. To produce the acute flexion necessary to form the helix, the cartilage is delib- erately warped in a favorable direction by thinning it on its outer, convex surface. The thinned helix is affixed to the main sculptural block with horizontal mattress sutures of 4-0 clear nylon; the knots are placed on the framework's undersurface.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
framework body (the "expansile" design),s2 rather than violating the sixth rib margin and sacrificing chest wall integrity.
In cases in which the delicate pleura is entered during this dissection, there is no great reason for concern because a leak in the lung has not been produced. However, when a pleural tear is discovered, a rubber catheter is inserted well into the chest through the pleural opening; the chest wound is then closed inlayers bythe assistant while the surgeon fabricates the frame- work, thus conserving operative time. When skin closure is complete, the catheter is attached to suction, the lung is expanded, and the catheter is rapidlywith- drawn. As a final precaution, every patient receives a portable upright chest radiograph in the overating room.
FRAMEWORK FABRICATION In fabricating an ear framework, the surgeon's aim is to exaggerate the helical rim and thedetails of the anti- helical complex (Fig. 74-11). This is achieved with
FIGURE 74-1 1 . A right ear framework, sculpted from autogenous rib cartilage as illustrated in Figure 74-1 0.
scalpel blades and rounded woodcarving chisels. To minimize possible chondrocytic damage, the use of power tools for sculpting is strictly avoided-one should keep in mind that cartilage sculpting differs from basic woodcarving in that a good long-term result ultimately depends on living tissue.
The basic ear silhouette is carved from the previ- ously obtained cartilage block (see Fig. 74-10). It is necessary to thin little if any of the basic form for a small child's framework, but it is essential for frame- work fabrication in most older patients. When thinning is necessary, care is taken to preserve the peri- chondrium on the lateral, outer aspect of the frame- work to facilitate its adherence ("take") and subsequent nourishment from surrounding tissues.
Because warping must be takeninto con~ideration,8~ one sculpts and thins the cartilage to cause a deliber- ate warping in a favorable direction. This allows one to produce the acute flexion necessary to form a helix, which is fastened to the framework body with hori- zontal mattress sutures; the knots are buried on the frame's undersurface.
FRAMEWORK MODIFICATIONS IN OLDER PATIENTS Adult rib cartilages are often fused into a solid block, which invites one to sculpt the ear framework in one piece-not unlike doing a woodcarving (Fig. 74-12). In my experience, this is advantageous because adult cartilage is often calcified; it is difficult if not impos- sible to create a separate helix that will bend without breaking. If a one-piece carving produces insufficient helical projection, one can detach the helix and slide it up the framework body to augment the protrusion of the rim. This improved contour is maintained by reattaching the helix to the frameworkwith several per- manent sutures (Fig. 74-13).
FRAMEWORK IMPLANTATION A cutaneous pocket is formed with meticulous tech- nique to provide an adequate recipient vascular cov- ering for the framework. Because several hours can lapse during the rib removal and framework fabrica- tion, the auricular region is prepared and scrubbed just before the cutaneous pocket is made. If two sur- geons well versed in ear reconstruction are working together, one can develop the cutaneous pocket while the other finishes the cartilage sculpture.
Through a small incision along the back side of the auricular vestige, a thin flap is raised by sharp dissection, with care taken to preserve the subdermal vascular plexus. To evaluate the flap's vascular status and to ensure accurate hemostasis, epinephrine- containing solutions are avoided. With great care, one dissects the skin from the gnarled, native cartilage remnant, which then is excised and discarded. Finally,
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
FIGURE 74-1 2. Framework modifications in the adult patient. Above, left, When a solid, fused cartilage block is encountered, the framework is sculpted in one piece. Above, center, Cartilage block marked for carving. Above, right, Completed framework sculpted from the block. Below, left, A 60-year-old man with traumatic total ear loss. Below, center and right, Result achieved with a one-piece sculpture from a fused cartilage block, 1 year postoperatively. Sim- ulation of the absent earlobe was achieved by sculpting its likeness in the framework's inferior pole. (From Brent B: Technical advances in ear reconstruction with autogenous rib cartilage grafts: personal experience with 1200 cases. Plast Reconstr Surg 1999; 104:319.)
the pocket is completed by dissecting a centimeter or two peripherally to the projected framework mark- ings (Fig. 74-14).
Insertion of the framework into the cutaneous pocket takes up the valuable skin slack that was made when the native cartilage remnant was removed. The framework displaces this skin centrifugally in an advantageous posterosuperior direction to displace the hairline just behind the rim. This principle of ante- rior incision and centrifugal skin relaxation, intro- duced by Tanzer,I5 not only permits advantageous use of the hairless skin cover but also preserves cir- culation by avoiding incisions and scars along the helical border.
Although T a n ~ e r l ~ ~ ~ * initially suggested the use of bolster sutures to coapt the skin flap to underlying framework, the author h d s it far safer to do this with suction, which simultaneously prevents fluid collec- tion and minimizes the risk of flap necrosis along the helical margin. Silicone catheters are used to attain skin coaptation by suction, or perforated drains are fash- ioned from infusion catheters with the needles inserted into rubber-toppedvacuum tubes (see Fig. 74- 14), the tubes being retained on a rack to observe changes in quantity and quality of drainage. Although a dressing is applied that accurately conforms to the convolu- tions of the newly formed auricle, firm pressure is dangerous and unnecessary and must be avoided.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
FIGURE 74-1 3. Maximizing rim projection in adult patient with sliding helical advancement. Above, IeR: A and B, Harvesting fused rib cartilage block and separating the inflexible helical portion; C, sculpting body of framework: D, sliding and reattaching the helix to maximize its projection. Above, right, A 50-year-old man with ear loss from a dog bite. Below, left, second from IeR, and third from left, Construction of the framework by use of the technique illus- trated in the drawings. Below, right, The completed repair. This patient had his hairline "idealized" by laser treatment before the rib cartilage graft (see Fig. 74-22). (From Brent B: Technical advances in ear reconstruction with autoge- nous rib cartilage grafts: personal experience with 1200 cases. Plast Reconstr Surg 1999; 1043 19.)
Hemostasis and skin coaptation are provided by the suction drain.17*29~75~n
IMMEDIATE POSTOPERATIVE CARE AND MANAGEMENT OF COMPLICATIONS The new ear's convolutions are packed with petrola- tum gauze, and a bulky, noncompressive dressing is applied. Because the vacuum system provides both skin coaptation and hemostasis, pressure is unnecessary and contraindicated. The first day, the tubes are changed by the ward nurses every few hours, then every 4 to 6 hours thereafter or when a tube is one-third full. Although the patient leaves the hospital inseveral days, the drains remain in place another 2 to 3 days until the test tubes contain only drops of serosanguineous
drainage. Postoperatively, the ear is checked and the protective head dressing is changed several times. The protective head dressing is removed after about 12 days.
Attentive postoperative management is imperative for asuccessful ear reconstruction that remains unham- pered by disastrous complications. The newly con- structed auricle is scrutinized frequently and carefully for signs of infection or vascular compromise. Early infection is usually manifested by neither auricular pain nor fever but through local erythema, edema, subtle fluctuation, drainage, or a combination of these. Hence, frequent observations and the immediate insti- tution of aggressive therapy can deter an ovenvhelm- ing infection. Immediately when an infection is suspected, an irrigation drain is introduced below the flap, and continuous antibiotic drip irrigation is
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
FIGURE 74-1 4. A to F, The cuta- neous "pocket." Thevestigial native cartilage is excised and then a skin pocket is created. To provide tension-free accommodation of the framework, the dissection is per-
.'formed well beyond the proposed auricular position. With use of two silicone catheters, the skin is coapted to the framework by means of vacuum tube suction.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECON~TRUC~ION OF THE AURICLE
F FIGURE 74-1 4, cont'd.
begun. Appropriate adjustments are made in both the antibiotic drip irrigation and in the systemic therapy when sensitivities are available from the initial culture. Cronin" has salvaged Silastic-frame reconstructions impressively by this technique, and the author has had success in managing the rare infection in cartilage graft reconstructions.
Skin flap necrosis results from excess tension in an inadequate-sized pocket, tight bolster sutures, or damage to the subdermal vascularity during the flap dissection. This complication is best avoided by meticulous technique; however, once skin necrosis
becomes evident, appropriate steps must be taken without delay. Although at times a small local flap may be required to cover exposed cartilage, small local- ized ulcerations may heal with good local wound care. Wound care consists of continuous coverage with antibiotic ointment to prevent cartilage desiccation and restraints to prevent the patient from lying on the ear during sleep. However, major skin flap necro- sis merits a more aggressive approach if the frame- work is to be salvaged. The necrotic skin is excised early, and the framework is covered by transposition of a local skin flap or by use of a small fascial flap and skin graft.
L I I
> 1
POSTOPERATIVE ACTIVITIES AND CARE Once it is initially healed, no specific care is necessary for an ear constructed with autogenous tissues. To avoid flattening of the helical rim, the patient is instructed to sleep on the opposite side. A soft pillow ensures pro- tection if the patient should sleep on the affected site.
Two weeks postoperatively, the patient may return to school; however, running and sports are discour- aged an additional 3 weeks while the chest wound heals. This is the case in any major surgical procedure where wound strength is essential.
The ear itself withstands trauma well because it, like the opposite, normal ear, houses a framework of autogenous cartilage. To date, the author has witnessed numerous traumatic episodes in reconstructed ears (e.g., baseball and soccer blows, a bee sting, and a dog bite). They have all healed wellz9 For these reasons, no conspicuous, protective headgear is recommended, except in sports such as football and wrestling, in which such equipment is used routinely.
Other Stages of Auricular Construction Major stages in auricular construction subsequent to the initial framework implantation are lobule rotation, separation of the ear with a skin graft, deepening of the concha, and formation of a tragus. These stages can be planned independently or in various combi- nations, depending on which best achieves the desired end result.
ROTATION OF THE LOBULE The author prefers to perform earlobe transposition as a secondary procedure because it seems easier both to judge placement of the earlobe and to splice the lobule correctly into position with reference to a well- established, underlying framework. Although the author has occasionally transposed the lobule simul- taneously with implantation of the cartilage graft, it is safer and far more accurate to transpose the lobule as a secondary procedure.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
FIGURE 74- 1 5. Total ear construction, stage 2: lobule transposition. A, Healed stage 1 repair and proposed lobule transposition. The appropriate lobule pcdtion will be de-epithelialized to receive the transpased earlobe. 8, Completed procedure. The lobule has been transposed as an inferiorly based flap.
The "rotationn or repositioning of this normal but displaced structure is accomplished essentially by Z- plasty transposition of a narrow, inferiorly based tri- angular flap (Fig. 74-15). Na&ata3' and Firminm transpose the earlobe and use from the lobule's posterior surface to b e the framework's tragal strut during the first-stage surgery. This does produce an excellent tragal appearance? but the price paid is greater riskof skin necrosis and earlobes that are at cimes com- promised in appearance and often unable to accom- modate earrings. This problem is no small h u e for y m g female patients, who often submit to surgery with eventual earlobe piercing as their hi-t prior- ity? If the lobe vestige is short so that a substantial skin bridge can be preserved above it during its trans- position, one can safely move the earlobe while simul- taneously separating the auricle from the head to form the auriculocephalic sulcuPg9 and preserve sufficient posterior earlobe skin to permit the use of earrings (Fig. 74- 16).
TRAGAL CONSTRUCTION AND CONCHAL DEFINITION One can form the tragus, excavate the concha, and mimic a canal in a single operation. This is accom- plished by placing a thin elliptical chondrocutaneous composite graft beneath a J-shaped incision in the con& region (Fig. 74-17)?"" The main limb of the J is placed at the proposed posterior tragal margin; the crook of the J represents the intertragal notch. Mraneous soft tissues are excised beneath this tragal flap to deepen the concha; this excavated region looks quite like a meatus when the newly constructed t r a p casts a shadow on it.
It is advantageous to harvest the composite graft fmm the normal ear's anterolated conchal surface
because of its ideal shape and the paucity of subcuta- neous tissue ktyvegn the debate ater~hrd ah a d adjacent cartilage. This technique is particularly ideal when a prominent concha exists in the normal donor ear, closure of the donor site facilitates an otoplasty, which often is needed to gain frontal symmetry.
An alternative method consists of design of the tragus as an integral strut of the original framework during its initial fabrication. A small piece of rib car- tilage is first htened to the frame to simulate the antitragal eminence. The strut is thinned on one side, then curved around and abed by its distal tip with a dear nylon suture that stretches across to the frame's crus helix. The result is a delicate t r a p that flows naturally from the main framework through an arched intertragal notch (Fig. 74- 18). This method of tragus construction is particularly advantageous in bilateral microtia, where there is no source for specid composite tissue grafts. Nagata also creates the tragus with an extra cartilage piece attached to his main framework (see Fig. 74-23) and lines it with skin from the earlobe vestige during the first stage of surgery.
Another option for tragus construction in bilateral rnicrotia is the modified Kirkham method, which con- sists of an anteriorly based conchal flap doubled on itself. '
DETACHING THE POSTERIOR AURICULAR REGION Auricular separation with skin grafting is used solely to eliminate the cryptotic appearance by defining the ear through formation of a sulcus. This procedure will not project a framework that has been carved with insuflicient depth.
The posterior auricular margin is defined by sepa- rating the ear from the head and covering its under- surface with a thick split-skin graft. This should not be attempted until the edema has markedly subsided and the auricular details have become well defined. When this occurs, an incision is made several mil- limeters behind the rim, with care taken to preserve a protective connective tissue layer on the cartilage frame- work. The retroauricular skin is then advanced into the newly created sulcus so that the only graft require- ment is on the ear's undersurfice. A medium split- t h i e b skin graft is hanrested from a hidden region (usu;$Upundemearh the bathing suit area) and sutured to the w o d , withthe sutures left long; tbese are tied over a bolster to tamponade h e graft to the recipient bed (Fig. 74- 19).
Greater p~ojection of the auricle can be obtained by pla&gawedge of rib cartilage behind the elevated ear, k t &is must be co~ered with a tissue fla for the S skin graft to take over the cartilage. Nagata accom- plishes this with an axial flap of temporoparietal fascia
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECON~TRUCTION OF THE AURICLE
FIGURE 74-1 6. Augmenting ear projection with a scalp-banked rib cartilage graft and fascial flap; simultaneous earlobe transposition. Above, left, Healed first-stage repair of a microtic ear. Note banked rib cartilage behind the ear framework (arrow). Above, second from left, Stage 2: retroauricular scalp undermined to retrieve banked cartilage; earlobe transposition begun. Above, second from right, Banked cartilage wedged behind the elevated ear to augment its projection; lobule suspended on the inferior pedicle. Above, right, Retroauricular fascial flap raised; earlobe trans- position complete. Below, left, Fascial flap turned over the cartilage wedge to provide a nourishing cover for skin graft. Below, second from left, Complete skin graft "take" on the elevated ear. Below, second from right, Preoperative view of the patient. Below, right, Healed postoperative appearance. (From Brent B: Technical advances in ear reconstruc- tion with autogenous rib cartilage grafts: personal experience with 1200 cases. Plast Reconstr Surg 1999; 104:319.)
(Fig. 74-20). However, use of that fascial flap is not without a certain morbidity, and this fascia should be reserved for significant traumatic and secondary reconstruction cases in which there is no other option for their solution.29 Like ~ i r m i n ' ~ and ~ e e r d a , ' ~ the author prefers instead to cover the cartilage wedge with a turnover"book flap" of occipitalis fascia from behind the ear (see Fig. 74- 16).23 When this cartilage-wedging technique is used, there is no need to subject the patient to a second uncomfortable chest operation to harvest rib cartilage anew, as does Nagata." Instead, an extra piece of cartilage can be banked underneath the chest incision during the initial first-stage procedure. When the wedge is needed during the elevation procedure, it can easily be retrieved by incising through the orig- inal chest scar. Alternatively, this cartilage wedge is banked underneath the scalp, just posterior to the main
pocket where the completed ear framework is placed (see Fig. 74- 16).'~ This site is particularly advantageous in that one can more conveniently retrieve the nearby banked cartilage when later lifting the new ear from the head; furthermore, this scalp site seemingly pro- vides better nourishment for the banked cartilage than does the subcutaneous chest region.
When harvesting this cartilage wedge material during the first-stage procedure, I split the cartilage in situ, which allows a wider portion of cartilage to be obtained to achieve maximum projection of the ear. This technique consists of shaving the outer cartilage from the rib and deliberately violates Gibson's balanced cross-sectional prin~iples,8~ causing the cartilage wedge to warp into an ideal shape for the posterior conchal wall that it will form (Fig. 74-2 1). This method of tissue
Text continued on p. 656
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
Undermined
FIGURE 74-1 7. A to H, Stage 4, tragus construction and conchal excavation. Harvested from the opposite normal ear's conchal region, a chondrocutaneous composite graft is placed under a thin J-shaped flap to form the tragus. Before the floor of the tragal region is surfaced with a full-thickness skin graft [FTSC) harvested from behind the oppo- site earlobe, extraneous soft tissues are excised to deepen the region.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCT~ON OF THE AURICLE
FTSG ' H
Bolster
F
FIGURE 74-1 7 , cont'd.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

654 111 + THE HEAD AND NECK
FIGURE 74-1 8. Ear framework fabrication with integral tragal strut. Above, Construction of the frame. The floating cartilage creates a helix, and a second strut is arched around to form the antitragus, intertragal notch, and tragus. This arch is completed when the tip of the strut is affixed to the crus helix of the main frame with horizontal mattress suture of clear nylon. Below, Actual framework fabrication with the patient's rib cartilage. (From Brent B: Technical advances in ear reconstruction with autogenous rib cartilage grafts: personal experience with 1200 cases. Plast Reconstr Surg 1999; 1 04:3 19.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
FIGURE 74-1 9. A to D, Stage 3, separating the surgically con- structed ear from the head with skin graft. An incision is made several millimeters peripheral to the sur- C gically constructed ear, and the auricle is sharply elevated from its fascia1 bed. The scalp is advanced to the newly created sulcus both to decrease graft requirements and to hide the graft by limiting its place- ment mostly to the ear's undersur- face. Long silk sutures are tied over a bolus dressing.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

harvest leaves the inner cartilage lamella intact, once again maximizing chest wall integrity and minimiz- ing deformity
MANAGING THE HAIRLINE Low hairline is one of the most common and trou- blesome problems in auricular construction. Because the normal hairline is usually lower than the apex of a normal ear, and sometimes considerably lower in microtia, insertion of the framework beneath the peri- auricular skin often places hair on a portion of the new auricle. In trying to avoid hairy skin over the supe- rior helix, the surgeon may be tempted to place the ear too low. Another complication arises when the framework is displaced anteriorly by the hairline, which acts as a constricting band at the juncture between the thin, hairless retroauricular skin and the thick scalp skin. This can be avoided by limiting the anterior dissection of the cutaneous pocket and by checking the framework's position before closing the incision.
Historically, Letterman and Hardinf used aUscalp roll" and free skin graft to provide a hairless skin cover; however, this new cover lacks the elasticity of virgin skin. Instead, the author usually first implants the framework and later eradicates any undesirable hair. This canbe done with electrolysis, by laser,or byreplac- ing the follicular skin with a graft.29 Before placement of an ear framework, if one predicts a tight pocket and a hairline that will cover half the new ear, a primary fascial flap may be ~onsidered.'~
Dealing with this unwanted hair depends on how much ear is actually involved. If hair is limited to the helix, electrolysis or clipping is clearly the method of choice. If hair covers a third or more of the ear, the ear is often resurfaced with a skin graft9 (with or without a fascial flap). Regardless of hair quantity, it is ideal to eradicate the hair by nonsurgical means, which elim- inates a "patchwork" appearance and preserves the normal aesthetic and protective qualities of the local skin. Such a depilatory method would be even better if it simultaneously thinned the follicle-containing scalp skin to provide the new ear with finer skin coverage. Perhaps in the future both of these goals will be achieved without surgery.
In recent years, lasers have become useful adjuncts for treating the skin and its appendages." In treat- ment of axillary hidradenitis with the laser, it has been found that not only is the condition improved by elimination of the apocrine sweat glands?' but by reduction of the bulk these epidermal appendages con- stitute, the skin also becomes h e r and softer?' By virtue of the same principle, I am hopeful that sig- nificant reduction of the hair follicles may likewise alter the scalp skin so that when it does cover a portion of the ear framework, it will be somewhat thinner and
h e r , resulting in enhanced detail of the completed ear.
Although it is still not consistently producing per- manent results at this writing, laser treatments can favorably alter hair growth to make it both finer and slower. Furthermore, as contrasted to needle electrol- ysis, patients can tolerate laser treatment of much larger areas during a given session. The two schools of treat- ment concentrate on targeting the melanin (and thus the heavily pigmented follicles) within the depth of the dermis93 versus targeting only the follicles by loading
Temporal parietal fascia
B FIGURE 74-20. A to E, Separating and projecting the surgically constructed ear, Nagata technique. The surgi- cally constructed ear is separated from the head at the second stage. Projection is supplemented by wedging a piece of rib cartilage (harvested anew from the chest), then covering it with a temporal vessel-containing fascial flap and skin graft.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
E FIGURE 74-20, cont'd.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
them with carbon particles through a gel transport medium and then focusing the laser on the The trick is to deliver enough energy density through the laser to destroy the hair follicles without damag- ing the skin, which causes scarring or hypopigmenta- tion. Presently, laser treatments decrease hair density and texture so that only a fewMmaintenance treatments" are needed per year. Laser technology continues to improve with such advances as better coolant tech- niques, which permit a higher fluence of energy to be delivered safely. Soon, it should consistently be possi- ble to achieve permanent hair removal without inju- rious side effects to the surrounding skin.% It is my vision to "pre-treat" ear reconstruction patients with the laser and thus create the ideal hairline before ini- tiating the surgical ear repair (Fig. 74-22). To aid the laser technician (who often may be at a great distance from my practice), a template is provided that makes it easy to precisely relocate the exact target area during the serial treatments (see Fig. 74-22)r
Variations in Total Ear Reconstruction Technique Numerous variations in technique have evolved during the years and wiU continue to emerge. One of the current popular variations is the Nagata technique, in which the ear reconstruction is accomplished in two stages.'2887 In this method, the cartilage frame- work implantation, tragus construction, and lobule transposition are performed in the first stage; the ear is separated from the head at the second stage with a block of cartilage (harvested by entering the chest for a second time), which is covered by a fascial flap and skin graft.
Although this eliminates several stages of surgery, all the soft tissue manipulation in the initial stage dra- matically increases the risk of tissue necrosis; the com- plication rate with this procedure is 14% (by contrast, the author's technique has experienced a complica- tion rate of less than 0.25% duringthe past 1000 cases). This combination of procedures also sacrifices the earlobe quality by lining the traps with the lobe's valu- able back-side skin. In the author's opinion, the final appearance and quality of the earlobe are far more important than forming a t raps duringthe initial first stage.
Because the Nagata technique produces the anti- helical complex by wiring an extra piece of cartilage to the base block (Fig. 74-23), the ears produced are thick,and more rib cartilage is needed and excised from the chest with attendant chest wall donor def~rmity.~~"' The numerous wire sutures that are used to apply these two pieces together (as well as to attach the helix) are placed on the lateral cartilage surfaces and lie precar- iously under the thin auricular integument (see Fig. 74-23), and thus they bear great risk of frequent
extrusion through the skin?' Tanzer reported wire extrusions b2Q ~f his 44 and he used one fourth as many sutures per ear as does Nagata.
To achieve ear projection, the Nagata technique uses the superficial temporal vessel-containing fascial flap in every case (see Fig. 74-20), with its attendant scalp scar and its risk of hair thinning in the donor site.29 Because Nagata enters the chest again (to obtain the cartilage wedge) during this procedure, the patient is subjected to a second uncomfortable operation.
Finally, the Nagata technique does not address frontal symmetry of the two ears, and for the tech- nique to deal with this and to be complete, a third stage is really required?' In the author's technique, the symmetry is dealt with during the tragus con- struction when the grafts for the tragus are harvested from the opposite ear (see Fig. 74-17). This allows one to adjust the donor ear to the reconstructed ear and to achieve frontal symmetry; by doing this as the final stage, the healed final position of the elevated ear has occurred so one knows where to set the oppo- site ear during the tragus construction so that sym- metry can be accomplished.
The Nagata technique has produced some interesting and useful variations in ear reconstruction and continues to e~o lve .~ , "~ Other variations will emerge as the quest for improved ear reconstruction continues.
FIGURE 74-21. Augmenting ear projection with split cartilage graft and retroauricular turnover fascial flap. Above, Broad cartilage wedge harvested by splitting rib cartilage. Chest wall integrity is maintained by preserv- ing inner cartilage lamella; the harvested outer lamella predictably warps to favorably shape the posterior conchal wall wedge. Second row, lefi, Splitting the rib car- tilage in situ. Second row, center, Outer cartilage lamella predictably begins to warp. Second row, right, The har- vested wedge. Note presetved inner cartilage lamella of the chest wall. The curved cartilage graft is banked subcutaneously until needed for projecting the surgically constructed ear. Third row, Scheme of separating the surgically constructed ear from the head, placing the pro- jection-maintaining cartilage wedge and covering it with turnover flap of retroauricular fascia, then applying split- skin graft. Below, lee, Projection of elevated ear augmented with the banked split-cartilage graft. Note how the pur- poseful warp has remained and produced an ideal shape for the new posterior conchal wall (inset). This particular graft had been subcutaneously banked beneath the orig- inal chest incision. Below, second from right, The fascial flap turned over the cartilage wedge, before skin graft is applied. Below, right, The healed repair. Note maintenance of projection and auriculocephalic sulcus. (From Brent 6: ~echnical advances in ear reconstruction with autogenous rib cartilaee grafts: personal experience with 1200 cases. Plast ~econ$r surg 1999; 10413 19.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

"' A THE HEAD AND NECK
FIGURE 74-22. "Hairline idealization" by presurgical laser treatment. Above, lett, Microtia with typical low hairline, which would cover the upper portion of the proposed auricular construction. Above, center, Crescent-shaped area des- ignated for laser de-epilation before embarking on surgical ear repair. Above, right, Film template to aid in relocating the exact crescent during serial laser treatments. Note aids in applying the template: cut-out area slips over vestige; eyebrow, lateral canthus, and oral commissure are marked on film. Below, left, The laser treatment in progress. Below, right, The same microtia after several laser treatments. The hairline is now ideal, and surgical construction of the ear will begin. (From Brent B: Technical advances in ear reconstruction with autogenous rib cartilage grafts: personal expe- rience with 1200 cases. Plast Reconstr Surg 1999; 104:319.)
Secondary Reconstruction The difficulties in surgically constructing &I ear are substantiated by the often disheartening result that emerges despite the surgeon's persistent efforts. Dis- couragingly, at times the end result bears no resem- blance to an auricle, other than for its location. Furthermore, the scars that result from multiple pro- cedures may extend the defect well beyond the origi- nal deformitv. The irn~act of such failures is emotionallv devastating ;o the pAtient and proportionately frui- trating for the surgeon.
TanzeP8 managed secondary reconstruction by first excising the scar and skin grafting the defect, then waiting for the graft to mature before implanting a new cartilage framework. However, this approach is often beset with compromises in that skin-grafted tissues have limited elasticity as a cutaneous pocket, and a detailed framework with depth cannot be
introduced without significant tension. Furthermore, deeply scarred tissue beds may be so severely damaged that this approach is not even possible, and, seem- ingly, the patient is left with no solution to the problem.
In an effort to resolve this skin coverage impasse, Brent and ByrdS9 implemented amore optimal method for secondary ear reconstruction: excision of the entire auricular scar area and immediate placement of a sculpted autogenous rib cartilage graft, which is covered with a temporoparietal fascia1 flap and skin graft (Figs. 74-24 and 74-25).
Bilateral Microtia Although relatively rare, bilateral microtia frequently afflicts patients with such conditions as Treacher Collins-Franceschetti syndrome, bilateral craniofacial
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

14 + RECONSTRUCTION OF THE AURICLE
A
IX Costal cartilage
FIGURE 74-23. Ear framework fabrication with appliquk of car- tilage components. Above (A and B) , Spina first applied a separate antihelical com~lex to the base block in 1971: (Redrawn from Spina V, Psillakis JM: Total recon- struction of the ear in congenital microtia. Plast Reconstr Surg 197 1 ;48:349.) Below, Nagata re- vived Spina's technique and added his own modifications. The num- erous wire sutures used in this method lie precariously under the AH thin auricular skin. H, helix; CH, crus of helix; AH, antihelix; T, tragus. (Redrawn from Nagata S: Modification of the stages in total reconstruction of the auricle. Plast T
Reconstr Surg 1994;93:221.) See text. I1
microsornia, and other uncommon craniofacial mal- formations (see Chapter 103).The reconstructive prin- ciples for management of bilateral microtia are the same as for the unilateral deformity.
For optimal function and aesthetics in bilateral microtia, one must plan to integrate surgical proce- dures so that one does not compromise the other. In these cases, the auricular construction must precede the middle ear surgery; once an attempt is made to "open" the ear, chances of obtaining a satisfactory auric- ular repair are severely compromised because the invaluable virgin skin has been scarred.
In bilateral microtia, cartilage graft procedures are performed on each side several months apart because each hemithorax contains sufficient cartilage for only one good ear framework. Simultaneous bilateral recon- struction necessitates bilateral chest woundswithatten- dant splinting and respiratory distress. Furthermore,
the first auricular repair might be jeopardized on turning the head to do the second side. For these reasons, it is preferable to perform the first stage of each ear on separate occasions.
Several months after the second cartilage graft, both earlobes are transposed during a single procedure. Once this stage is healed, one can either separate the ears from the head with skin grafting or pursue the middle ear surgery. Nine of 10 patients with microtia have only unilateral involvement, and most do well without middle ear surgery because they are born "adjusted" to their monaural condition.
To ensure that the gains of middle ear surgery out- weigh the risks and complications of the procedure itself, this surgery is reserved for cases in which the patient is highly motivated and there is favorable radi- ologic evidence of middle ear development. Then, it must be thoughtfully planned in a "team approach""
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
FIGURE 74-24. Ear reconstruction with autogenous rib cartilage surfaced by a skin graft-covereu ~alrlporopariew~ fascial flap. A, A patient with a scarred auricular region. Doppler vessels, the flap extent, and the Y-shaped incision are indicated. B, Scar excision, framework fabrication, and scalp dissection are begun. C, Raising a fascial flap that contains the superficial temporal vessels. D, Fascial flap draped over the ear framework. E, Scalp wound sutured. F; Skin graft applied over the fascia-covered ear framework. (From Brent B, Byrd HS: Secondary ear reconstruction with cartilage grafts covered by axial, random, and free flaps of temporoparietal fascia. Plast Reconstr Surg 1983:72: 14 1 .)
enced in atresia surgery. In the team approach, the plastic surgeon initiates
the procedure by lifting the ear from its bed while care- fully preserving connective tissue on the framework's undersurface. Then the otologist proceeds, first drilling a bony canal, completing the ossiculoplasty, and then repairing the tympanum with a temporal fascial graft. Finally, the plastic surgeon resumes by excising soft tissues to exteriorize the meatus through the conchal region and harvesting a skin graft, which the otologist
uses to line the new canal and complete the repair (Fig. 74-26).
The Constricted Ear Tanzer has applied "constricted ear" to a group of ear anomalies in which the encircling helix seems tight, as if constricted by a pursestring (Fig. 74-27). Once loosely termed cup or lop ears, these deformities collectively have helical and scaphal hooding and varying degrees of flattening of their antihelical complexes.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
FIGURE 74-25. Secondary ear reconstruction with a rib cartilage graft surfaced with a superficial temporoparietal fascial flap and skin graft. A, A patient with a scarred auricular region after multiple failed procedures. B, Result achkyed . in one surgical stage with rib cartilage graft and fascia1 flap by the techniques outlined in Figure 74-24. I - ---*
Although Tanzer gave these ears a numerical clas- sification that corresponds to each deformity's sever- i e 2 in practical surgical terms, one needs to determine whether the ear can be repaired by reshaping the exist- ing tissues or whether slun coverage or the support- ing cartilage must be supplemented.
One must individualize constricted ear repairs for each specific ear deformity. If helical lidding is the main defect and the height discrepancy is minimal, the over- hanging tissue can merely be excised. At times, the car- tilage lid can be used as a "banner flap" to increase ear height (Fig. 74-28). Moderate height discrepancies necessitate augmentation of the cartilage height by modifying the ipsilateral ear ~ a r t i l a g e ~ ~ ' ~ ~ or employ- ing contralateral concha1 cartilage grafts.76 The key to repair of these moderate deformities is to visualize the defective cartilage armature, which is possible only after one "degloves" the skin envelope (Figs. 74-29 and 74- 30).
When constriction is severe enough to produce a height difference of 1.5 cm, one must add both skin and cartilage and essentially correct the deformity as if it were a formal microtia (Fig. 74-31).
Cryptotia
Cryptotia is an unusual congenital deformity in which the upper pole of the ear cartilage is buried beneath the scalp (Fig. 74-32). The superior auriculocephalic sulcus is absent but can be demonstrated through gentle finger pressure. This has stimulated Japanese physicians to correct this deformity nonsurgi~al ly~~~ because it occurs in Japan as frequently as 1 in 400 births.'02
This nonsurgica rocedure is accomplished through application I-- -n external conforming splint. If the s p l i t is applied before 6 months of age, it may successfully mold a permanent retroauricular s ~ l c u s . ~ ~ ~ Tan et allo4 have successfully applied such nonsurgical splinting techniques for constricted ears as well (Fig. 74-33). Yotsuyanagi et allo5 have success- fully employed these nonsurgical methods to correct a variety of ear deformities in children oIder than neonates.
Surgical repairs entail addition of skin to the deficient retroauricular sulcus by skin grafts and Z- plasties,V-Y advancement flaps,'" orrotational flaps.lo3
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

664 111 + THE HEAD AND NECK
FIGURE 74-26. Team approach to bilateral microtia. Above, left, Initial auricular repair, after framework placement and lobule transposition. Above, left center, Team approach to middle ear. The plastic surgeon lifts constructed auricle from bed, taking care to preserve connective tissue on cartilage framework; next, the otologic surgeon drills bony canal and completes middle ear repair. Above, right center, The plastic surgeon then raises a concha1 skln flap and removes intervening soft tissues to exteriorize canal. Above, right, With use of the flap to circumvent atres~a by breaking up contractual forces, it is dropped into the introitus of the canal, which is skin grafted to complete the repair. Alterna- tively, the skin flap could have been based anteriorly and doubled on itself for a Kirkham tragal construction. Below, center, Preoperative views of the same bilateral microtia patient. Below, lee and right, Bilateral results of the external and middle ear team repair. (From Brent B: Auricular repair with autogenous rib cartilage grafts: two decades of expe- rience with 600 cases. Plast Reconstr Surg 1992;90:355.)
FIGURE 74-27. Varying types of constricted ears. A, Involvement of the helix only. 6, Involvement of the helix and scapha (left auricle). C, Severe cupping deformity coupled with incomplete migration of the auricle.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
FIGURE 74-28. Correction of grade I ear constriction. A, The incision for exposure of the skeletal deformity. B, The deformed cartilage has been filleted from its soft tissue cover. The line of detachment of the angulated segment is marked. C, The deformed cartilage is lifted on a medially based pedicle and rotated into an upright position. D, The repositioned cartilage is sutured to the scapha. E, The skin is redraped, and the helical sulcus is maintained by through- and-through sutures tied over gauze pledgets. (From Tanzer RC, Edgerton MT, eds: Symposium on Reconstruction of the Auricle. St. Louis, CV Mosby, 1974: 141 .)
When a cartilage deformity accompaniestheskin defi- ciency, various remodeling techniques are needed to facilitate the repair.'023'07
The Prominent Ear PATHOLOGY During the third month of gestation, the auricle's pro- trusion increases; by the end of the sixth month, the helical margin curls, the antihelix forms its fold, and the antihelical crura appear. Anything that interferes with this process produces prominent ears.
The most common deformity arises from the anti- helix's failing to fold. This widens the conchoscaphal angle as much as 150 degrees or more (Fig. 74-34), which flattens the superior crus and, in severe forms, the antihelical body and inferior crus. In extreme cases, the helical roll may be absent, which produces a flat, shell-like ear with no convolutions.
Producing protrusion of the ear's middle third, conchal widening may occur as an isolated deformity or in conjunction with antihelical deformities described before. This abnormality is usually bilateral and is fre-
rt% ed in siblings and the'parents.
TREATMENT In repair of prominent ears, symmetry is most impor- tant and, paradoxically, may be more difficult to achieve in unilateral than in bilateral cases. The repaired ear convolutions should appear smooth and unoperated on. The most lateral point of the com- pleted repair should be between 1.7 and 2.0 cm from the head, and the helix should be visible behind the antihelical body when one sees the ears from the frontal view.'0s
To attain these goals, a great number of tech- niques have heen described, many of which prodace
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

1 1 1 4 TWE HEAD AND NECK
FIGURE 74-29. Repair of a moderately constricted ear. A, Preoperative appearance. B, "Deg~ov~ng" the ear to expose the distorted cartilage. C, The cartilage is expanded, the antihelix is formed, and a contralateral concha1 car- tilage graft repairs the deficient upper third. D, Skin redraped to complete the repair. See Figure 74-30B. (From Brent B: The correction of microtia with autoqenous cartilage grafts. II. Atypical and complex deformities. Plast Reconstr Surg 1980;
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCT~ON OF THE AURICLE
acceptable results. However* the author recommends that the smgeon direct efforts toward correding the specific problem areas of each individual ear rather thao foflowing a routine "cookbook recipe."
If the upper third of the ear protrudes becauee of an absent or weak antihelix, one must form an exag- gerated antihelix. If themiddle third is too prominent, one must recess the concha byeither cartilage excision or suture 6mti0n.'~~ Finally, if the lobule protrudes, one must either resect or retroposition the d a d - nous tail of the cauda helicisU0 or excise retrolobular skin.
CONCHAL ALTERATION Dieffenbach3 is credited with me first otoplastic attempt in 1845. This consisted of his excising skin &om the auriculocephalic sulcus and then suturing conchal d g e to the mastoid periosteum.
In addition to narrowing the auriculocqhalic sulcus, Ely4 (18811 and others excised astrip of conchal wall, a procedure that is attributed to Momtin"' in 1903. This old methad of t a c h back the concha to mastoid periostem b,s been re4ved throughout the years (~ig. 74-35). 10% 12-iL5
Also, one can correct the wide concha bv excising a cartilaginom ellipsebeneath the antihelical body. T ~ E may create a redundant skinfold, which then may require excision.
RESTORING OF THE ANTIHELICAL FOLD Luckett (1910) first conceptualized that prominent ears result from the antiheWs failure to fold. He restored this fold by excising a crescent of medial skin and car- tilage (Fig. 74-%).'"Themajorityof subsequent oto- plasty procedures have focused on making a smoother antihelix than is p rodud by employing Luckett's sharp cartilage-breaking t e c h ~ i q u e . ~ ~ " ~ - " ~
ALTERING THE MEDIAL CARTIIAGE SURFACE To permit its smooth molding, one can recontour the scaphal cartilageby a number of techniques. McEvittlm and Paletta1l3 weakened the sapha With multiple par- allel cuts; Chnperse et al'" used burr abrasion.
Becker,'u.'u Cop~erse;~' and T a n ~ e r ' ~ ~ used paral- lel cuts and permanent sutures to form a smooth, cor- nucopia-like an&&(Pig. 74-37) .Advantageously, this cartilage tube encases substantial scar to lock the cartilage into position and prevent recurrence of deformity. FIGURE 74-30. Repair of a moderately constricted ear
Re~galong-forgo~ensuBesrion of MOrd,~ by the technique shown in Figure 74-29. (From Brent B: The correction of microtia with autogenous cartilage grafts. i'4~stafde'~~'" formed the antihelix by inserting Pel II. Atypical and complex deformities. Plast Reconstr Surg manent mattress sutures throu* the cartilage without 1980;66: 13.) using any actual cartilage incisions. The author finds
this technique particularly useful in the pliable ear
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

668 111 + THE HEAD AND NECK
FIGURE 74-3 1 . Repair of sevc, , tar constriction by the classic microtia technique. A, A patient with a severely con- stricted ear. B, Appearance after insertion of total ear framework of rib cartilage. C, Use of the vestige to form the earlobe and tragus. D, Final result after separation from the head with a skin graft. (From Brent B: The correction of microtia with autogenous cartilage grafts. 11. Atypical and complex deformities. Plast Reconstr Surg 1980;66:13.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 4 RECONSTRUCTION OF THE AURICLE
FIGURE 74-32. Cryptotia.
cartilage of children. Surgeons who criticize this technique mention recurrence of the deformity, pre- sumablv because the sutures tear through the carti- " lage. I have circumvented this technical problem by hydrodissecting the anterolateral skin from the car- tilage with saline injected through a 30-gauge needle just before passing each permanent suture. This has worked well in preventing recurrent deformities (Fig. 74-38).
ALTERING THE LATERAL CARTILAGE SURFACE Exploiting cartilage's tendency to warp when one surface is cut," Chongchet'*' scored the anterior scaphal cartilage with multiple cartilage cuts to roll it back and form an antihelix. While Chongchet did this under direct vision using a scalpel, StenstromlZ8 pro- duced thesameeffect byusinga short-tined rasp instru- ment to"blind1y"score the antihelical region through a posterior stab incision near the cauda helicis. The lateral cartilage surface has also been morselized or abraded under direct vision through a lateral incision.lZ9
Finally, Kaye130 advocates an otoplasty method that combines both lateral cartilage scoring and fixation with permanent sutures. Heaccomplishes both of these maneuvers through minimal incisions (Fig. 74-39).
ACQUIRED DEFORM ITlES Total auricular reconstruction in the acquired defor- mity presents special problems not encountered in microtia. These merit separate consideration.
The lackof skin coverage is much more critical than in microtia; an existing meatus precludes use of the anterior incision, and extra skin, as usually gained by removing the crumpled microtic cartilage, is not available. This factor compounds the previously men- tioned hairline problem. If one can use the existing skin, the cutaneous pocket is best developed by inci- sions above or below the proposed auricular site. If the local tissues are heavily scarred or restrict the surgeon
FIGURE 74-33. A, Neonate with lop ear. B, Custom splint used to correct helical fold. C, Follow-up photograph taken 2 months after completion of 10 weeks of splinting. (From Tan ST, Abrarnson DL, MacDonald DM, Mulliken JB: Molding therapy for infants with deformational auricular anomalies. Ann Plast Surg 1997;38:263.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-34. A, Cross section of a normal ear. B, Prominent ear resulting from an increased con- choscaphal angle. YIC
al-I 1 8 I ~ r h q w, , -.. y ," I - " L m p ~ , ~ " '" "
from deve opmg an ample s h poc t e repair must be supplemented with fascial flap coverage (see Figs. 74-24 and 74-25).89 Skin expanders have also been employed to stretch the covering skin but bear risks of extrusion and scar capsule formation.
Replantation of the Ampu Auricle &%A ' A
Replantation of amputated segments of the auricle was practiced in the 17th century. Cocheril13' cites the memoirs of Strafford written during the reign of the
English king Charles I. To punish Puritan and colonist opposition to the regime, the victim's ear was fre- q u d y nailed to a wooden post and then amputated. Three of these many victims have been specifically documented: Burton, a minister in the government; Prynne, a lawyer; and Bartwick, a physician.13' Prynne had earlier published a book that was considered offen- sive to the queen and consequently had his ears ampu- tated. When he appeared before the Tribunal a second +;me, the presiding judge was surprised to see Prynne
ith two normal-appearing ears. Prynne's ears were exposed but showed the signs of mutilation Having been condemned to have his ears amputated a second time, Prynne retrieved the amputated ears, hoping to have them sutured back to their original site as had been done previously. No information is available about the fate of Burton's ears. We know that Bartwick's wife collected his amputated ears and placed them carefully into a handkerchief, hoping to have them replanted. AU this took place between 1630 and 1640.
Cocheril cites many examples of successful replan- tations during the 19th century and states, "It is diffi- cult to doubt the good faith of these authors: the prestige attached to their names; the clarity of their reports; the official approval given to their reports should suffice to consider them as veracious. The vascularity of the auricle, the rapid healing of wounds of this structure, the fact that the vessels remain gaping, ready to receive nourishing fluid-all mitigate in favor of the veracity of the reports." The only information missing in all of these reports is the size of the amputated parts.
To the modem plastic surgeon, choosing a salvage procedure is influenced by the size of the amputated
FIGURE 74-35. Technique of reducing prominence by conchomastoid sutures.A, Cross section of the auricle showing placement of the sutures to reduce the conchomastoid angle and to restore the antihelical fold. B, Correction of the prominence. C, View of the medial surface of the auricular cartilage after correction of the prominence. (From Spira M , McCrea P, Cerow F, Hardy B: Analysis and treatment of the protruding ear. Transactions of the 4th International Congress of Plastic Surgery. Amsterdam, Excerpta Medica, 1969.1
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
A B C FIGURE 74-36. Evolution of the tubing principle for correction of prominent ears. A, Luckett; B, Barsky; C, Becker.
FIGURE 74-37. Complete corrective otoplasty (Tanzer modification of Converse procedure).
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
I:;'
J of antihelical foids. Previous treatment of the cartilage by mattress sutures resulted only in recurrence. B to D, Cor- rection by cartilage tubing to form an antihelical fold and elliptical excision of excess concha.
portion; the condition of the tissues of the amputated segment; and the condition of the stump and sur- rounding tissues, particularly in the retroauricular area. A clean-cut amputation gives the surgeon a better chance for success. When the ear and its surrounding tissues are mangled and avulsed and bone is exposed, the reconstruction is difficult if not insurmountable. Small amputated segments are replaced as composite grafts with some hope of success. Larger amputated segments and subtotal amputation require further consideration.
REPLANTATION OF AURICUIAR TISSUE AlTACHED BY A NARROW PEDICLE Because an ear is richly vascularized and has major
! vessels extending through its periphery, one can suc- cessfully replace the partly avulsed auricular tissue ' even though the remaining attachment is tenuous -
I\: 'q
REPIANTATION OF AURICULAR TISSUE AS A COMPOSITE GRAFT
! ' Even when the piece of auride is large, the completely ' detached ear tissue may survive when replaced as a
composite graft, although few successful cases have been reported in the plastic surgery literature (Figs. 74-41 and 74-42).13*-13'
REPLANTATION OF AURICULAR CARTILAGE Because a cartilaginous framework is difficult to reproduce, the salvage and use of denuded auric- ular cartilage were recommended by numerous sur- g e o n ~ . ' ~ ~ - ' ~ ~ Various techniques have been employed to preserve cartilage from an avulsed ear. The slun may be removed and the cartilage buried in an abdominal pocket,139 buried in a cervical pocket,140 or placed under the skin of the retroauricular area.I4' The orthotopic cartilage replantation can be employed only if regional cutaneous tissues are in good condition.
Although logical, the author finds this procedure futile; the flimsy ear cartilage almost invariably flat- tens beneath the snug, discrepant two-dimensional skin cover. Furthermore, when amputated ear cartilage has been"banked" in the retroauricular region, it hampers later reconstructive attempts by producing an irregu- lar, amorphous structure that is adherent to the over- lying regional skin.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-39. The Kaye method to correct flattening of the antihelix. A, A subperichondrial tunnel is made on the lateral surface of the cartilage through a medial incision near the cauda helicis; a sharp-tined instrument produces curling by multiple vertical striations. B and C, The proper amount of antihelical roll is maintained by several mattress sutures introduced through tiny incisions along the concha1 crest and carried across the antihelical fold through holes in the skin. (From Kaye BL: A simplified method for correcting the prominent ear. Plast Reconstr Surg 1967;40:44. Copyright O 1967, The Williams & Wilkins Company, Baltimore.)
REPLANTATION OF THE DERMABRADED AMPUTATED AURICLE Mladick et and Mladick and C a r r a ~ a y ' ~ ~ have advocated first dermabrasion and then reattachment of the amputated ear to its stump. The reattached ear is then buried in a subcutaneous postauricular pocket, which allows revascularization through the exposed dermis of the dermabraded auricle (Fig. 74-43). Several weeks later, the ear is exteriorized by blunt dissection from its covering flap, which is allowed to slide behind the helical rim. At this time, the subcu- taneous attachments of the medial auricular surface are left intact. The exposed raw auricular surface is dressed, and epithelialization begins within several days.
Rather than separate the medial auricular attach- ments from their bed several weeks later to allow spon- taneous re-epithelialization as Mladick originally suggested, the author thinks it is safer to wait several months before separating the ear frame from the head.
At that time, one can skin graft the new retroauricu- lar sulcus as in a classic ear reconstruction.
REPIANTATION OF THE AMPUTATED AURICLE ON REMOVAL OF POSTAURICULAR SKIN AND FENESTRATION OF CARTILAGE Almost invariably, the replantation of large compos- ite parts is doomed to unless one increases the vascular recipient area. Instead of employing derm- abrasion to achieve this, BaudetI4' removed the skin from the postauricular portion of the amputated part, fenestrated the cartilage, and placed the auricular segment into a raw area established by raising a flap of retroauricular-mastoid skin (Fig. 74-44). The car- tilaginous windows allowed direct contact of the auricular skin with the recipient site, thus facilitating its revascularization. Although some distortion of the superior helical border occurred (Fig, 74-45), the result was satisfactory.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

t 111 + IHE HEAD AND NECK
F r'- -
F . 7 I w mold for 4 months.
I FIGURE 74-40. Repair of a major auricular avulsion. A, The avulsed ear remains attached by a narrow pedicle, which maintains its viability; the canal is transected. 6, Result after repair of the canal and maintenance of an acrylic
FIGURE 74-41. Replantation of auricular tissue as a composite graft. A, Loss of a portion of the scapha and helix resulting from a dog bite. B, The amputated segment was retrieved and sutured in position as a composite graft, with this result 2 years later. (Patient of Dr. Andries Molenaar.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRVCTCON OF THE AURICLE 675
FIGURE 74-42. Replantation of a totally amputated auricle as a composite graft. A, The stump of the amputated auricle 5'12 hours after the accident. B, The amputated part includes the pinna, the earlobe, and part of the concha. C and D, The final result after reattachment. (From Clemons JE, Connelly MV: Reattachment of a totally amputated auricle. Arch Otolaryngol 1973;97:269.]
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
FIGURE 74-43. Reattachment of thesevered auricle by dermabrasion and subcutaneous "pocketing." A, The ampu- tated stump. B, The severed part. C, The dermabraded reattached part is buried in a postauricular pocket; a traction suture (arrow) from the helix flattens out the auricle to gain better apposition of the tissues. D, The ear has been exte- riorized and is almost completely epithelialized (see text for details); onegranulatingarea is seen at the superior margin. E, One month after injury, the ear has a red flush over the reattached segment. F, Appearance at 5 months. (From Mladick R, Carraway J: Ear reattachment by the modified pocket principle. Plast Reconstr Surg 1973;51:584. Copy- right O 1973, The Williams & Wilkins Company, Baltimore.)
REPLANTING THE EAR CARTILAGE AND IMMEDIATELY COVERING IT WITH A FASCIAL FLAP AND SKIN GRAFT In selected cases in which the wounds are clean, the scalp is intact, and the patient's general condition is stable, one might be tempted to remove the ampu- tated ear's skin and to cover the filleted cartilage imme- diately with a fascial flap and skin graft. Because poor results in filleted ear cartilages that have been subcu- taneously banked are frequently observed, it is prefer- able to use Baudet's fenestration technique initially and to reserve the fascia for secondary reconstruction should this effort fail.
MICROSURGICAL EAR REPLANTATION Although there have been several reports of success- ful microsurgical replantation of this pro- cedure tends to fail because of such small vessels within the amputated ear. Therefore, what initially appears to be a successful replantation often fails as venous congestion ensues. However, such cases have been sal- vaged by application of leeches to the congested replant.14'
With this in mind, the author believes that one should accomplish the anastomosis end-to-side in the temporal vessels rather than sacrificing them for an end-to-end repair. An axial-pattern fascial flap is
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-44. Replantation of the ampu- tated auricle after removal of the posteromedial auricular skin and fenestration of the cartilage (after B a ~ d e t ' ~ ~ ) . A and B, The extent of the amputation. C, Skin removed from the medial aspect of the amputated part. D, Windows cut through the cartilage. E, Reattachment of the amputated part; the denuded portion of the auricle is applied against the raw surface in the auriculomastoid area. F, Technique of fenestra- tion suggested by Brent to prevent the defor- mity seen in Figure 74-450.
preserved for a future reconstruction should the replant fail.
Deformities without Loss of Auricular Tissue IRREGULARITIES IN CONTOUR The most common traumatic auricular deformities without actual tissue loss result from faulty approxi- mation of full-thickness lacerations, which manifest the helical border's distortion and notching.
Meticulous approximation of sutures is essential in primary repair of lacerations or in secondary repair of maladjusted tissues. Z-plasties, stepping, halving, and dovetailing of cartilage edges and soft tissue wounds are important measures in preventing recurrence of contour irregularities.
OTOHEMATOMA: "CAULIFLOWER EAR" Frequently found in pugilists, this deformity results from a direct blow or excessive traction that produces a hemorrhage. Blood collects between the perichon- driumand cartilage, which produces a fibroticclot that thickens and obliterates the ear's convolutions. This is similar to the process that produces thickening of the septa1 cartilage, which is frequent in boxers and wrestlers.
Immediately after hematoma has occurred, one must drain the blood clots and serum. Whereas mere
needle aspiration is followed almost invariably by recur- rent fluid collection, a small incision will permit evac- uation of the hematoma under direct vision. The incision should be long enough to permit retraction, inspection, and application of a large suction tip for the aspiration of blood clots. Conforming, compres- sive gauze bolsters are placed on either side of the auricle and are maintained for 7 to 10 days by horizontal mat- tress sutures (4-0 nylon) that traverse the bolsters as well as the ear.
Late treatment ofthe cauliflower ear deformitycon- sists of carving out the thickened tissue to improve the auricular contour. Exposure is obtained by raising a skin flap through carefully placed incisions. After the carving is completed, similar dressings must be applied to ensure coaptation of the soft tissues to the carti- laginous framework and to prevent hematoma.
8 8
STENOSIS OF THE EXTERNAL L .
AUDITORY CANAL . . -. I . WSII. The concha is elongated inikiidty h e ezeza;;"di: tory canal through an opening, the meatus, through which lacerations may extend and ultimately produce stenosis.
Whenever possible, one must carefully suture cir- cular lacerations involving the canal and keep the canal packed tightly during the hea1ingperiod.A small, pros- thetic appliance should be prepared to keep the canal open. This is made by taking an impression with dental
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-45. Replantation of the amputated auricle after removal of the posteromedial auricular skin and fen- estration of the cartilage. A, Appearance of the stump of the amputated auricle. B, The denuded medial aspect of the cartilage; the outlines of the windows to be cut through the cartilage are indicated. C, The auricle immediately after reattachment. D, Final appearance. (Courtesy of Dr. J . Baudet.)
compound and creating a perforated mold of acrylic bands.14' In severe stenosis, when the meatus is closed resin. This prosthetic support should be worn for 3 or and the canal is filled with scar tissue, the cicatricial 4 months until the tendency toward stenosis disap- tissue must be excised; the skin defect is repaired by pears (Fig. 74-46). means of the skin graft inlay technique, for which
Cicatricial stenosis of the external auditory meatus a full-thickness retroauricular graft is uniquely suit- and canal is remedied by Z-plasties of the cicatricial able. To facilitate this grafting, one should take two
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE 679
FIGURE 74-46. Traumatic stenosis of the external auditory canal. A, Stenosis of the external auditory canal result- ing from laceration. B, Acrylic mold worn after skin grafting. C, Result obtained; the canal remains patent. (From Con- verse JM: Reconstruction of the auricle. Plast Reconstr Surg 1958;22: 150 copyright O 1958, Williams & JhlilkinS Company. Baltimore.) rr h w
- .- 8 I ' r-wlr
, L.
impressions of the canal with dental compound. o n 4 impression serves to apply the graft firmly within the canal until the skin graft has taken; the other irnpres- sion is duplicated in clear acrylic and should be worn by the patient for a period of 3 or 4 months to coun- teract the tendency for secondary contraction of the graft and subsequent stenosis (see Fig. 74-46). A detail worth noting is to prepare the mold in such a manner that the mold's distal portion itself fills the concha; this precaution ensures prosthesis stability.
Deformities with Loss of Auricular Tissue These deformities may result from loss of skin, loss of cartilage, or full-thickness loss of auricular tissue.
LOSS OF AURICULAR SKIN Auricular trauma that results only in a skin loss is usually secondary to burns. Loss of retroauricular skin results in adhesions between the ear and the mastoid region, whereas skin loss from the anterolateral surface may cause forward folding of the ear. When a burn destroys the skin, the cartilage becomes involved also, the result being a full-thickness defect of the auricle (see Chapter 65 for early treatment of the burned ear). However, partial-thickness burns that are adequately treated may heal with only varying degrees of con- traction and thinning of the helical border.
- - - -
--* kr-.- FULL-THICKNESS DEFECTS 01 THE AURICLE For purposes of classification, full-thicmess defects of the ear may be divided into six groups: defects of the upper third, middle third, and lower third; partial and total loss; and loss of the lobule (or lobe) of the ear.
MAJOR AURICULAR LOSS AFTER TRAUMA Loss of a major portion of the auricle or of the entire ear itself may result from a razor slash, flying glass, gunshot wound, flame or radiation burns, and human or dog bites. Complete traumatic loss of the auricle is an unusual occurrence, for a portion of the concha and the external auditory canal are usually preserved even in cases of severe injury. When a large portion of the auricle or the entire ear has been destroyed, a number of obstacles must be surmounted in succes- sive stages. These include (1) a suitable skin covering devoid of hair follicles; (2) a framework of cartilage to maintain the upright position of the reconstructed auricle and to represent its characteristic convolutions; and (3) a covering of skin for the posteromedial aspect of the auricular framework after it is raised from the mastoid area. Additionalc'retouching" procedures may be necessary to achieve a satisfactory repair ofthe recon- structed auricle.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD AND NECK
THE SKIN COVERING
The presence of supple and well-vascufarid skin is a sine qua non for success in auricular reconstruction. The quality of the residual local soft tissues varies in traumatic defects. When amputation of the auricle is by means of a clean-cut laceration, the local residual skin remains relatively unscarred and thus may be used. Likewise, minimally scarred skin after healed partial- thickness burns may be of sufficiently good quality to avoid skin grafting. To the contrary, if the auricle has been avulsed, destroyed by a burn, or injured by a gunshot, the area may show multiple linear or surface scars, thus necessitating excision and replacement with a skin graft before the auricular reconstruction begins. Should this be necessary, a fd-thickness graft from ,hhe contralateral retroauricular region or supraclavic- d a r area is most suitable for this purpose, although Ef this is not available, a thick split graft will suffice. It - -
is essential that the skin overlying a cartilage graft have an adequate blood supply and be sufficiently loose to permit insertion of a good three-dimensional frame- work. Therefore, the skin graft must be allowed to mature for a nhmber of "months before cartilage replacement.
At times, the local skin will be irreparably scarred or grafts will mature inadequately t ~ - ~ e r m i t frame- work placement without supplementing the soft tissue cover. Under these circumstances, one must employ a fascial flap.89 First, all heavy scars and unus- kble tissues are excised while great care is taken to preserve the temporal vessels, which may be entan- gled in the traumatically scarred tissues. Rib cartilage is then harvested, and a framework is sculpted as for correction of a virgin microtia (see Figs. 74-10, 74-11, 74-18, and 74-23). Finally, the fascial flap is raised.
To realize how large a fascial flap is needed for ade- quate coverage, one must first assess the periauricular skin. At times. the scar excision will be so extensive that total fascih flap coverage of the hamework is nec- essary. However, at other times, the framework's lower portion can beUpocketed" beneath available skin, and therefore only a variable portion of the upper frame- work will need fascial flap coverage.
In using this fascial flap, one must be familiar with the course of the superfid temporal vessels. The artery remains beneath the subcutaneous tissue and within the temporoparietal fascia until a point approximately 12 cm above the anterosuperior auriculocephalic attachment. Here the artery emerges superficially and interlinks with the subdermal vascular plexus.'50 Con- sequently, this is the limit of fascial vascular domain, continued distal dissection would interrupt the fascial circulation.
After the vessels are first mapped with a Doppler probe, exposure to the fascia is gained through a
Y-shaped incision that extends superiorly above the proposed auricular region. The dissection begins just deep to the hair follicles and continues down to a plane where subcutaneous fat adheres to the temporopari- etal fascia. Because initial identification of this plane can be difficult, care must be taken to damage neither the follicles nor the underlying axial vessels. Although tedious, once the scalp dissection is accomplished, the inferiorly based temporoparietal fascial flap is raised easily from the underlying deep fascia that envelops the temporalis musculature.
Subsequently,the fascial flap is first draped over the framework (see Fig. 74-24) and then coapted to it by means of suction by a small infusion catheter. The flap is then a f f~~ed to the peripheral skin in a "vest-under- pants" fashion to secure a tight closure. Finally, a pat- terned thick split-skin graft is sutured on top of the fascia-covered framework. The new ear's convolutions are then packed with petrolatum gauze; last, a head dressing is applied.
AURICULAR PROSTHESES The auricular prosthesis should be reserved for instances in which surgical reconstruction is imprac- tical or contraindicated or when an experienced surgeon is unavailable. For the most part, an auricu- lar prosthesis has no practical value for children and is worthwhile for older persons who have undergone ablative cancer surgery or who have extensive burns. Even so, many adults find them undesirable after a short trial experience; there is always a constant fear of the prosthesis becoming dislodged at embarrassing moments and the psychological discomfort of wearing an "artificial part." The innovation of osseointegrated percutaneous implants has offered a solution to the retention of ear prostheses.151
Additional problems that arise from local skin irri- tation from the adhesive glue frequently necessitate discontinuance of the prosthesis for a time, which in turn causes the patient further embarrassment. Fur- thermore, obvious color contrast calls attention to the prosthetic ear in climatic changes when the prosthetic part remains a constant color while the surrounding skin varies as the patient passes from indoor to outdoor environmental surroundings.
When an auricular prosthesis has been elected for the younger patient, a trial period should ensue, with the realization that surgical reconstruction may be desired later. It is wise to avoid preliminary ex- cision of the microtic lobule or other remnants merely to "gain an improved surface for adherence of the prosthesis," as has been advocated. Should the patient desire surgical reconstruction later, which has often been my experience, the missing lobule, short- age of skin, and existing scar become a significant handicap.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

Partial Auricular Loss Most auricular deformities encountered in everyday practice are acquired partial defects. They present the surgeon with an unlimited variety of unique problems. Reconstruction is influenced by the etiology,location, and nature of each residual deformity.
USE OF RESIDUAL TISSUES In management of acute auricular trauma, initial metic- ulous reapproximation of tissues and appropriate wound care will greatly facilitate the reconstructive task ahead. Likewise, the innovative use of residual local tissues in a post-traumatic deformity will greatly sim- plify the reconstruction and contribute to a pleasing outcome.
STRUCTURAL SUPPORT Contralateral Conchal Cartilage A variety of tissues are available to provide the struc- tural support required for an auricular reconstruction. Although the quantity of cartilage needed to fabricate a total ear framework necessitates the use of costal car- tilage, often one is not compelled to employ this tissue in a small, partial auricular reconstruction. Because it is often possible to use an auricular cartilage graft, which is obtained most frequently from the contralateral concha under local anesthesia, the correction of partial losses is less extensive than the procedure to correct total auricular losses. Auricular cartilage, used as an orthotopic graft in ear reconstruction, is superior to costal cartilage in that it provides a delicate, flexible, thin support.
The conchal cartilage graft can be obtained by a posteromedial incision, as described by ad am^'^^ and Gorney?' or through an anterolateral approach, which the author uses more frequently. The anterolateral approach, performed through an incision several mil- limeters inside the posterior conchal wall-inferior crus contour line, is a simple method of obtaining a precise graft with direct visual exposure.153
lpsilateral Conchal Cartilage In certain partial reconstructions, it is more advanta- geous to employ an ipsilateral rather than a contralateral conchal cartilage graft. However, it is imperative that an intact antihelical strut be present to permit removal of an ipsilateral conchal cartilage graft without sub- sequent collapse and further deformity of the ear.
An ipsilateral conchal cartilage graft is particularly advantageous when a retroauricular flap is being raised to repair a major defect in the helical rim. Elevation of the flap provides the required conchal cartilage expo- sure without the necessity of an additional incision, and removal of this cartilage graft subsequently lowers the ear closer to the mastoid region. In effect, this
produces a relative gain in length, thus enabling the flap to cover the cartilage graft once it is spliced onto the rim and eliminating the need for a skin graft in the flap's donor bed.
Furthermore, the ipsilateral concha may be used occasionally as a composite flap of skin and cartilage (Fig. 74-47). This innovative technique, proposed by Davis," is applicable to defects of the auricle's upper third and again should be employed only when the antihelical support remains intact.
Composite Crafts Small to moderate-sued defects may be repaired with composite grafts from the unaffected ear, particularly if it is large and pr~truding.'"~'"-~~ A wedge-shaped composite graft of less than 1.5 cm in width is resected from the scapha and helix of the unaffected ear and transplanted to a clean-cut defect on the contralateral ear (Fig. 74-48). The success rate of composite grafts can be enhanced by removing a portion of the skin and cartilage, thus converting part of the "wedge" to a full-thickness skin graft, which is readily vascular- ized by a recipient advancement flap mobilized from the loose retroauricular skinL5' A strut of the helical cartilage is preserved within the graft for contour and support (Fig. 74-49).
Despite a slight inclination toward shrinkage after transplantation, the composite graft offers a simple and expeditious reconstructive technique for partial auric- ular defects.
Specific Regional Defects HELICAL RIM Acquired losses of the helical rim may vary from small defects to major portions of the helix. Small defects usuallyresult from tumor excisions or from minor trau- matic injuries and are best closed by advancing the helix in both directions as described by Antia and B~ch '~ ' (Fig. 74-50). The success of this excellent tech- nique depends first on totally freeing the entire helix from the scapha by an incision in the helical sulcus that extends through the cartilage but not through the skin on the ear's back surface. Second, the postero- medial auricular skin is undermined, dissecting just superficial to the perichondrium until the entire helix is hanging as a chondrocutaneous component of the loosely mobilized skin (Fig. 74-50Cand D). Extra length can be gained by a V-Y advancement of the crus helix (Fig. 74-SOB), and surprisingly large defects can be closed without tension.
Although this technique was originally described for upper third auricular defects (Fig. 74-51),15' the author has found that it is even more effective for middle third defects and is equally applicable in repair of earlobe 10sses.'~' Reconstruction of larger helical
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

682 " 1 + THE HEAD AND NECK
Raw area I
FIGURE 74-47. Upper auricular defect repaired with a composite flap of conchal skin and cartilage. A, The defect. 5, The composite conchal flap elevated. C, The final appearance. D and E, Diagram of the procedure indicating the incisions and the raw surfaces to be grafted. The anterior cutaneous pedicle (crus helicis) maintains the blood supply. (After Davis.34)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
FIGURE 74-48. Reconstructio~~ of an auricular defect with a com- posite graft from the contralater ear. Left: above, an auricular defe~ resultingfrom a human bite; cente appearance of the ear 3 years aftt, reconstruction with a composite graft; below, appearance of the donor ear 14 days after the surgi- cal procedure. Right, The sequence of repair, top to bottom; the donor ear is at the left, and the defecti\ ear being reconstructed is on the right. (From Nagel F: Reconstruc- tion of a partial auricular loss. Plast Reconstr Surg 1972;49:340. Copy- right Q 1972, The Williams & Wilkins Company, Baltimore.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

684 111 + THE HEAD AND NECK
FIGURE 74-49. Enhancement of composite graft revascularization by decreasing "composite bulk." A, Auricular defect with residual chondrodermatitis. B, The bulkiness of the composite graft is decreased by removing the pos- teromedial auricular skin and cartilage while preserving a cartilage strut in the helical rim. A retroauricular flap is advanced to serve as a recipient bed fnr t h e rerrlaining anterolateral cutaneous portion of the wedge-shaped graft. C, The final result.
FIGURE 74-50. Helical defect repaired by advancement of auricular skin cartilage. A, Defect of the upper portion of the auricle. B, Lines of incisions through skin and cartilage. C, The incisions completed; note the downward exten- sion into the earlobe. D, The skin-cartilage flaps mobilized. E, The repair completed. (After Antia NH, Buch VI: Chon- drocutaneous advancement of flap for the marginal defect of the ear. Plast Reconstr Surg 1967;39:472. Copyright O 1967, The Williams & Wilkins Company, Baltimore.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-51. A, Traumatic defect of the superior helical region. 8, Repair by helical advancement as illustrated in Figure 74-50. (After Antia NH, BuchVI: Chondrocutaneous advancement of flap for the marginal defect of the ear. Plast Reconstr Surg 1967;39:472. Copyright0 1967,The Williams & Wilkins Company, Balti- more.)
74 + RECONSTRUCTION OF THE AURICLE
defects requires a more sophisticated procedure that recreates the absent rim with use of an auricular car- tilage graft covered by an adjacent flap as previously described in the text. Although advancement flaps of local soft tissues have also been employed to provide helical contour, the author finds that these flaps often suffer a disappointing long-term result unless a strut of cartilage has been incorporated into the repair (Figs. 74-52 and 74-53).
Another sophisticated method of helical recon- struction is the use of thin-caliber tubes that can suc- cessfully form a fine, realistic helical rim when meticulous technique is used in conjunction with careful case selection (Fig. 74-54). Minor burns often destroy the helical rim yet leave the auriculocephalic sulcus skin intact, thus providing a superb site for tube constr~ction"~ and minimizing tube migration, risk of failure, and secondary deformity.
UPPER THIRD AURICULAR DEFECTS Upper third defects may be reconstructed by five major methods. Minor losses are usually confined to the rim and are repaired either by helical advancement, as pre- viously described (see Fig. 74-50), orbya readily acces- sible preauricular flap.
Intermediate losses of the upper third are repaired with a banner flap, as described by Cr ike l a i~ '~~ which is based anterosuperiorly in the auriculocephalic sulcus. This flap should be used in conjunction with a small cartilage graft to ensure a good long-term result.
Major losses in the superior third are most suc- cessfully reconstructed with a contralateralconchal czu- tilage graft as classically described by dams.'" In using this technique, it is imperative that the cartilage graft
FIGURE 74-52. Technique for restoring the helical margin. A, Outline of the incisions for an advancement flap from the retroauricular area. B, The advancement flap sutured in position. C, In a second stage, the pedicle of the advancement flap has been sectioned, the flap rolled into a tube, and the resulting defect covered by a split- thickness skin graft. See results produced in Figure 74- 53. (After Padgett and Stephenson, 1948.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

686 111 + THE HEAD AND NECK
FIGURE 74-53. Helical reconstruction with a postauricular flap, as illustrated in Figure 74-52. A, Acquired loss of the helical rim. 5, The postauricular flap in position over the auricular margin. C, The completed reconstruction, after division of the flap. (From Lewin M: Formation of the helix with a postauricular flap. Plast Reconstr Surg 1950;5:452. Copyright 0 1950, The Williams & Wilkins Company, Baltimore.)
be anchored to the cartilaginous remnant of the helical root by means of a suturiplaced through a small inci- sion at that point. This prevents the cartilage graft from "drifting" and ensures helical continuity.
Should the existing skin be unfavorable for this tech- nique, the entire concha may be rotated upward as a chondrocutaneous composite flap on a small anterior pedicle of the crus helix.34 This is a technically demand- ing procedure, and it is restricted to individual instances in which a large concha exists (see Fig. 74-47).
l4lDDLE THIRD AURICULAR DEFECTS
Major middle third auricular defects are usually repaired with a cartilage graft that is either covered by an adjacent skin flap (Fig. 74-55) or inserted by Con- verse's tunnel procedure (Fig. 74-56).16' Conditions may occasionally favor a specially prepared compos- ite graft as described previously (see Fig. 74-49).
The tunnel procedure16' is an effective technique for moderate-sized defects of the auricle (Fig. 74-57),
FIGURE 74-54. Helical restoration with a fine-caliber tube flap. A, Migra- tion of the supraclavicular tube flap to the ear with helical loss. B, Comple- tion of the helical reconstruction; note the splice of the superior junction by a Z-plasty.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
FIGURE 74-55. Dieffenbach's technique for reconstruction of the middle third of the auricle, drawn from his description ( 1 829-1 834). A, The defect and the outline of the flap. B, The flap advanced over the defect. C and D, In a second stage, the base of the flap is divided and the flap is folded around the posteromedial aspect of the auricle. A skin graft covers the scalp donor site.
and in major defects it has the advantage of preserv- ing the retroauricular sulcus (Fig. 74-58). In employ- ing this technique, one presses the auricle against the mastoid area and draws an ink line on the skin in this area, keeping the line parallel and adjacent to the edge of the auricular defect (Fig. 74-58C). Incisions are made through the skin along the ink line and also through the edge of the auricular defect (Fig. 74-580). The medial edge of the auricular incision is sutured to the anterior edge of the mastoid skin incision (Fig. 74-58E and F). A cartilage graft is then placed in the soft tissue bed and is joined to the edges of the auricular cartilage defect (Fig. 74-58H). The mastoid skin, which has been undermined, is advanced to cover the cartilage graft, and the edge of this skin flap is sutured to the lateral edge of the auricular skin (Fig. 74-581). A healing and vascularization period of 2 or 3 months is permitted; during this period, the cuta- neous tunnel behind the auricle must be cleaned with cotton-tipped applicators. The auricle is detached in a second stage, and the resulting elliptical raw areas on the ear and mastoid region are grafted (Figs. 74- 581 and 74-59).
Middle third auricular tumors are excised and closed either by wedge resection with accessory tri- angles or by helical advancement, as previously described.
LOWER THIRD AURICULAR DEFECTS Lower third losses that encompass more than earlom tissue are an especially complex challenge and must include a cartilage graft to provide the support neces- sary to ensure long-term contour.
Although PreauxL6' has described an impressive technique for repairing lower third defects by means of a superiorly based flap doubled on itself, the author finds that contour and support are provided and main- tained with less risk by primarily inserting a wn- tralateral conchal cartilage graft subcutaneously in the proposed site of reconstruction.
ACQUIRED EARLOBE DEFORMITIES Traumatic clefts and keloids that result from ear vierc- ing are the most common acquired defects of the earlobe. Cleft earlobes, usually occurring from the dra- matic extraction of earrings, can be repaired most effi- ciently by means of pardue's ingenious adjacent flap, which is rolled into the apex of the wedge repair, thus maintaining a tracklined with skin that permits further use of earrings (Fig. 74-60).lQ
Another common occurrence in everyday practice is the earlobe keloid, which heretofore has been treated with varying degrees of success with irradiation and steroid Because there is strong evidence
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

688 111 + THE HEAD AND NECK
FIGURE 74-56. Repair of a defect of the middle third of the auricle: the tunnel procedure. A, Carved costal carti- lage graft. B, The defect. C, Incisions through the margins of the defect. D, Incisions through the edge of the defect are extended backward through the skin of the mastoid area. E, The skin of the mastoid area is undermined between the two incisions. E The medial edge of the incision at the border of the auricular defect is sutured to the edge of the postauricular incision. A similar type of suture is placed at the lower edge of the defect. C, The cartilage graft is placed under the skin of the mastoid area and anchored to the auricular cartilage with sutures. H, Suture of the skin incision. (From Converse JM: Reconstruction of the auricle. Plast Reconstr Surg 1958;22:150, 230. Copyright Q 1958, The Williams & Wilkins Company, Baltimore.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-57. Partial auricular reconstruction with concha1 cartilage graft, as illustrated in Figure 74-56. A, Middle third postsurgical defect. 5, Conchal cartilage graft from contralateral ear. C, Result obtained by tunnel procedure of Converse. Secondary procedures will be necessary to release the ear and to improve helical contour. (From Brent R. The versatile cartilage autograft: current trends in clinical transplantation. Clin Plast Surg 1979;6: 163.)
that pressure plays an important role in keloid therapy,166sL67 a light pressure-spring earring device may be worth a trial in reducing postexcisional recurrence of earlobe ke10ids.I~~
Construction of an earlobe is rarely required in congenital microtia because the lobe is formed by the repositioning of auricular remnants. However, a portion of the lobe or the entire lobe may be missing in traumatic deformities of the ear, and a variety of techniques for its reconstruction have been proposed. As early as 1907, effective techniques were innovated to repair earlobes with local flap tissues.169 Since then, numerous methods have been developed (Figs. 74-61 to 74-65).'70-'72
Tumors of the Auricle BENIGN TUMORS Sebaceous cysts of the auricle are often treated improp- erly or neglected. Most often, one finds them on the medial aspect of the ear, particularly in the lobe, and these should be excised in toto during the quiescent period through the medial surface ofthelobuleto min- imize deformity.
The most common auricular lesion is actinic ker- atosis, which occurs, as does carcinoma, in outdoor workers with fair complexions. Other benign
auricular lesions, such as granuloma pyogenicum, beryllium granuloma, verruca contagiosa, verruca senilis, cylindroma, nevus, papilloma, lipoma, lym- phangioma, leiomyoma, and chondroma, should be surgically excised. Keloid of the earlobe is common; the treatment of this lesion is discussed elsewhere.
MALIGNANT TUMORS More than 5% of skin cancers involve the a~ricle."~ Most of these are cutaneous, usually basal cell or squa- mous cell carcinomas. A lesser percentage are malig- nant melanoma.
When first seen, the cartilage is involved by direct extension in about one third of the cutaneous carci- nomas of the auricle. For this reason, and because car- tilage is an excellent barrier to the tumor's spreading, it is thought that the cartilage must be included in the surgical
The cervical lymph nodes are rarely involved in basal cell carcinoma of the auricle but are involved in approx- imately one third of all squamous cell carcinomas and malignant melanomas.
The majority of these malignant lesions are on the helical rim and can be eradicated with a wedge excision, or a helical advancement, as previously described. Many of the tumors on the lateral and medial
TpXt continued on p. 695
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

690 'I1 + THE HEAD AND NECK
FIGURE 74-58. Repair of a pos- terosuperior auricular defect by the tunnel procedure of Converse. A, The portion of the ear to be restored. B, The auricle is pressed against the mastoid process. C, An ink outline is traced on the skin overlying the mastoid process, parallel to the edge of the auricular defect. D, Incisions are made along the edge of the defect and through the skin of the mastoid area.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

74 + RECONSTRUCTION OF THE AURICLE
FIGURE 74-58, cont'd. E, Suture of the medial edge of the auricular incision to the anterior edge of the mastoid incision. F. The suture has been completed. G, Costal car- tilage graft. H, The costal cartilage graft has been embedded. I, The skin of the mastoid area is advanced to cover the cartilage graft. J, In a second stage, the auricle is sepa- rated from the mastoid area, and full-thickness retroauriculargraftsfrom the contralateral ear cover the defects. (From Converse JM: Reconstruction of the auricle. Plast Reconstr Surg 1958;22: 150,230. Copyright O 1958, The Williams & Wilkins Company, Baltimore.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

692 111 + THE HEAD AND NECK
FIGURE 74-59. A superior auricular defect resultingfrom a burn. A, Preoperative appearance. B, The result obtained by the tunnel procedure shown in Figure 74-58. (From Converse JM: Reconstruction of the auricle. Plast Reconstr Surg 1958;22: 150, 230. Copyright O 1958, The Williams & Wilkins Company, Baltimore.)
FIGURE 74-60. Repair of an earlobe cleft with preservation of the perforation for an earring. A, A flap is prepared by a parallel incision on one side of the cleft; the other side is "freshened" by excision of the margin. B, The flap is rolled in to provide a lining for preservation of the earring track. C, Closure is completed; a small Z-plasty may be incorporated. (After P a r d ~ e . ' ~ ~ )
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-61. Reconstruction of the earlobe. A, The curved line abc outlines the proposed earlobe as measured on the unaffected contralateral auricle. A vertical flap is outlined; line bd is equal in length to line ab, and cd is equal to ca. 13, Incisions are made through the outlined skin and subcutaneous tissue. C, The vertical flap is raised from the underlying tissue as far upward as the horizontal line ac, and the apex of the flap is sutured to point a. D, The operation completed. [After Zenteno Alani~."~]
FIGURE 74-62. Reconstruction of the earlobe by a two-flap technique (Converse). A, The pattern of the planned earlobe. B, The pattern has been placed on the posteromedial aspect of the auricle and an outline made. The outline of the second flap from the retroauricular area is also shown; note the line of the vertical incision for insertion of the lobe. C, Each of the flaps is sutured to an edge of the vertical incision, thus anchoring the new earlobe. D, The two flaps are sutured to each other. E, The operation completed. (From Kazanjian and Converse.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-63. A, Loss of the lower part of the auricle. B, The result obtained with a flap based on the mastoid process and folded on itself. Note the scar of the approximated edges of the flap's donor site. (Patient of Dr. Cary L. Guy.)
FIGURE 74-64. Construction of an earlobe with a reverse contoured flap. A, The earlobe deficiency. B, An auriculomastoid flap outlined. C, The elevated flap hanging as a curtain from the inferior auricular border. D, The flap folded under and sutured and the mastoid defect closed. A small graft is placed over the auricular donor defect. E, The completed earlobe, exaggerated by one third toallow for shrinkage. (From Brent B: Earlobe reconstruction with an auricular-mastoid flap. Plast Reconstr Surg 1976;57:389. Copyright O 1976, The Williams & Wilkins Company, Baltimore.)
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

FIGURE 74-65. Earlobe reconstruction. A, The reverse contour pattern, in which ab is equal to ef, bc to ce, and ad to df. B, Congenital deficiency of lobular tissue. C, Completed construction by the technique illustrated in Figure 74- 64 . (From Brent B: Earlobe reconstruction with an auricular-mastoid flap. Plast Reconstr Surg 1976;57:389. Copy- right O 1976, The Williams & Wilkins Company, Baltimore.)
auricular surfaces can be treated adequately by exci- sion and subsequent skin grafting or by local flap coverage. Others require definitive reconstructive procedures previously detailed in this chapter. Radia- tion therapy is of no value in managing recurrences and metastases and is poorly tolerated by the auricle.
When the cancer is large and includes cartilaginous invasion, one must totally excise the ear with sur- rounding soft tissue. Radical resection of the cervical lymph nodes in continuity with resection of the involved auricle should be performed. In patients with lymph node metastases, one must resect the ear and all cervical lymph nodes. Melanomas require early radical intervention. At times, one's onlyhope of effect- ing a cure in auricular cancer includes resection of the temporal bone.175-177
Patients requiring total auricular ablation are usually older and generally are not candidates for total auricular reconstruction. A prosthesis is often preferred, but if total ear reconstruction is indicated, it is advis- able that reconstruction be postponed until the threat of recurrence is well past.
REFERENCES I. Bhishagratna KKL: An English Translation of the Sushruta
Samhita. Calcutta, Wilkins Press, 1907. 2. Tagliacozzi G: De Curtorum Chirurgia per Insitionem.Venice,
Gaspare Bindoni, 1597. 3. Dieffenbach JF: Die operative Chirurgie. Leipzig, FA
Brockhaus, 1845. 4. Ely ET: An operation for prominence of the auricles. Arch
Otolaryngol1881;10:97.
5. Gillies H: Plastic Surgery of the Face. London, H. Frowde, Hodder & Stoughton, 1920.
6. Pierce GW Reconstruction of the external ear. Surg Gynecol Obstet 1930;50:601.
7. Gillies H: Reconstruction of the external ear with special ref- erence to the use of maternal ear cartilages as the supporting structure. Rev Chir Structive 1937;7:169.
8. Converse JM: The absorption and shrinkage of maternal ear cartilage used as living homografts: follow-up report of 21 of GiUies' patients. In Converse JM, ed: Reconstructive Plastic Surgery, 2nd ed. Philadelphia, WB Saunders, 1977: 308.
9. Brown JB, Cannon B, Lischer CE, et al: Surgical substitution for losses of the external ear: simplified local flap method of reconstruction. Surg Gynecol Obstet 1947;84:192.
10. Dupertuis SM, Musgrave RM: Experiences with the recon- struction of the congenitally deformed ear. Plast Reconstr Surg 1959;23:361.
11. Kirkham HJD: The use of preserved cartilage in ear recon- struction. AM Surg 1940;11:896.
12. PotterEL:A hereditary ear malformation transmittedthrough five generations. J Heredity 1937;28:255.
13. Steffensen WH: Comments on total reconstructionof the exter- nal ear. Plast Reconstr Surg 1952;10:186.
14. Steffensen WH: Comments on reconstruction of the external ear. Plast Reconstr Surg 1955;16:194.
15. Tanzer RC: Total reconstruction of the external ear. Plast Reconstr Surg 1959;23:1.
16. Tanzer RC: Microtia-a long-term follow-up of 44 recon- structed aurides. Plast Reconstr Surg 1978;61:161.
17. Cronin TD: Use of a Silastic frame for total and subtotal reconstruction of the external ear: preliminary report Plast Reconstr Surg 1966;37:399.
18. Curtin JW, Bader KF: Improved techniques for the success^ silicone reconstruction of the external ear. Plast Reconstr Surg 1969;44.372.
19. Lynch JB, Pousti A, Doyle J, Lewis S: Our experiences with Silastic ear implants. Plast Reconstr Surg 1972;49:283.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

+ THE HEAD AND NECK b. 3 4 + '
20. Cr& TD: Use of a Sdastic frame for reconstruction of the auride. InTanzerRC,EdgertonMT,eds: Symposium on Recon- stnation of the Avridn St4 Ls* CY my, 137a3,
21. BresnidcSD,Reinsch RF: Reconstructive techniquesfor salvage of the Medpore ear reconstruction. Presented at Ear Recon- struction '98: Choices for the Future, Chateau Lake Louise, Canada, March 5,1998.
22. Wellisz T: Reconstruction of the burned external ear with a Medpore porous polyethylene pivotingheh framework Plast Reconstr Surg 1993;91:811.
23. Brent B: Technical advances in ear reconstruction with au- togenous rib carthge grafts: personal experience with 1200 cases- Plast Reconstr Surg 1999;104.319. Young F: Cast and precast cartilage grafts. Surgery 1944;l~. 335.
25. Peer LA: Reconstruction of the auride with diced cartilage graftsin avitallium ear mold. Plast Reconstr Surg 1948;3:653.
26. Cao Y, Vacanti P, Paige KT, et al: Transplantation of chon- drocytes utilizing a polymer-cell construct to produce tissue- engineered cartilage in theshape of a human ear. Plast Reconstr Surg 1997;100:297.
27. Ting V, Sims CD, Brecht LE, et al: In vitro prefabrication of human cartilage shapes using fibrin glue and human chon- drocytes. Ann Plast Surg 1998;40:413.
28. Saadeh PB, Brent B, ~ o n ~ a c r e M, et al: Human cartilage engi- neering: chondrocyte extraction, proliferation, and charac- terization for cohstruct development. Ann Plast Surg 1999;42:509.
29. Brent B: Auricular repair with autogenous rib cartilage grafts: two decades of experience with 600 cases. Plast Reconstr Surg 1992;90:355.
30. Firmin F: Ear reconstruction in cases of typical microtia. Per- sonal experience based on 352 microtic ear corrections. Scand J Plast Reconstr Hand Surg 1998;32:35.
31. Fukuda 0: The microtic ear: survey of 180 cases in 10 years. Plast Reconstr Surg 1974;53:458.
32. Nagata S: Modification of the stages in total reconstruction of the auricle. Plast Reconstr Surg 1994;93:221.
33. Osorno G: Autogenous rib cartilage reconstruction of con- genital ear defects: report of 110 cases with Brent's technique. Plast Reconstr Surg 1999;104:1951.
34. Davis J: Reconstruction of the upper third of the ear with a chondrocutaneous composite flap based on the crus helix. In Tanzer RC, Edgerton MT, eds: Symposium on Reconstruction of the Auricle. St. Louis, CV Mosby, 1974247.
35. Gorney M, Murphy S, Falces E: Spliced autogenous conchal cartilage in secondary ear reconstruction. Plast Reconstr Surg 1971;47:432.
36. Arey LB: Developmental Anatomy, 7th ed. Philadelphia, WB Saunders, 1974,
37. His W: Zur Entwickelungdes Acusticofaaalisgebietsbem Men- schen. Arch Anat Phys Anat SuppI 1899.
38. Streeter GL: Development of the auricle in the human embryo. Carnegie Contrib Embryo1 1922;14:111.
39. Nauton R,Valvassori G: Inner ear anomalies: their association with atresia. Laryngoswpe 1968;78:1041.
40. Reisner K: Tomography in inner and middle ear malforma- tions: value, limits, results. Radiology 1969;92:11.
41. Jahrsdoerfer RA, Yeakley JW, Hall JW 111, et al: High- resolution CT scanning and auditory brain stem response in congenital aural atresia: patient selection and surgical corre- lation. Otolaryngol Head Neck Surg 1985;93:292.
42. Jahrsdoerfer RA, HallJWIII: Congenitalmalformationsof the ear. Am J Ot011986;7:267.
43. Jahrsdoerfer RA, Yeakly JW,Aguilar EA, et al: Grading system for the selection of patients with wngenital aural atresia. Am J Otol 1992;13:6.
44. Grabb WC: The first and second branchial arch syndrome. Plast Reconstr Surg 1965;36:485. ' q s , , ,
L5. Aase JM,Twmeier RE: Microtia in New Mexico: evidence for multifactorial causation. Birth Defects 1977:13:113.
h 8agm-P;Microtia, lop, cup and protruding aa! four dimly inherited deformities? Plast Reconstr Sure 1968:41:208.
47. wddervanck~~: ~ e r e d i t a r ~ malformations of the ear in three generations: marginal pits, preauricular appendages, malfor- mations of the auricle and conductive deafness. Acta Otolaryngol1962;54553.
48. Konigsmark BW Hereditary deafness in man. N Engl J Med 1969;281:713.
49. Rogers B: Berry-Treacher Collins syndrome: a review of 200 cases. Br J Plast Surg 1964,17:109.
50. ErichJB%Abu-Jamra FN: Congenital cup-shaped deformity of the ears: transmittedthrough four generations. Mayo Clin Proc 1965;40:597.
51. Hanhart E: Nachweis einer einfach-dominanten, un- komplizierren sowie einer unregelmassig-dominanten, mit Atresia auris, Palatoschisis und anderen Deformationen- verbundenen Anlage zu Ohrmuschel-Verkummerung (Mikrotie). Arch Julius Klaus-Stift 1949;24:374.
52. Kessler L: Beobachtung einer liber 6 Generationen einfach- dominant vererbten Mikrotie 1. Grades. HNO 1967;15: 113.
53. Tanzer RC: Total reconstruction of the auricle: the evolution of a plan of treatment. Plast Reconstr Surg 1971;47:523.
54. Takahashi H, Maeda K: Survey of familial occurrence in 171 microtia cases. Jpn J Plast Surg 1982;15:310.
55. McKenzie J, Craig J: Mandibulo-facial dysostosis (Treacher Collins syndrome). Arch Dis Child 1955;30:391.
56. Poswillo DE: The pathogenesis of the first and second branchial arch syndrome. Oral Surg 1973;35:302.
57. Jorgensen MB, Kristensen HK, Buch NH: Thalidomide- induced aplasiaof theinner ear. J Laryngol Otol1964,78: 1095.
58. Mundrick K: Handbuch Hals- Nasen- Ohrenheilkunde, vol 111, pt 1. Stuttgart, Thieme, 1965:668.
59. JahnAF,GantiK: Major auricularmalformationsdue to Accu- tane (isotretinoin) Laryngoscope 1987;97:832.
60. Jahrsdoerfer RA: Causative agents in microtia-atresia. Dis- cussion at Microtia-Atresia Support Group; Manhattan Day . School, New York, NY; November 2,1997.
61. Lammer EJ, Chen DJ, Hoar RM, et al: Retinoic acid embry- opathy. N End J Med 1985;313:837.
62. Tanzer RC: The constricted (cup and top) ear. Plast Reconstr Surg 1975;55:406.
63. Longacre JJ, de Stefano GA, Holmstrand KE: Thesurgical man- agement of first and second branchial arch syndromes. Plast Reconstr Surg 1%3;31:507.
64. May H: Transverse facial clefts and their repair. Plast Reconstr S u g 1962;29:240.
65. Dellon AL, Claybaugh GL, Hoopes JE: Hemipalatal palsy and microtia. Ann Plast Surg 1983;10:475.
66. Longenecker CG, Ryan RF,Vincent RW Malformations ofthe ear as a due to urogenital anomalies: report of sixadditional cases. Plast Reconstr Surg 1965;35:303.
67. Taylor WC: Deformity of ears and kidneys. Can Med Assoc J 1965;93:107.
68. OginoY,YoshikawaY: Plasticsurgery for the wngenital anomaly of the ear. Keisei Geka 1963;6:79.
69. Converse JM, Horowitz SL, Coccaro PJ, Wood-Smith D: The corrective treatment of the skeletal asymmetry in hemifacial microsomia. Plast Reconstr Surg 1973;52:221.
70. Converse JM, Wood-Smith D, McCarthy JG, et al: Bilateral facial microsomia. Plast Reconstr Surg 1974;54:413.
71. Knorr NJ, Edgerton MT, Barbarie M: Psychologic factors in the reconstruction of the ear. In Tanzer RC, Edgerton MT, eds: Symposium on Reconstruction of the Auricle. St. Louis, CV Mosby, 1974:187.
72. Farkas LG: Growth of normal and reconstructed auricles. In Tanzer RC, Edgerton MT, eds: Symposium on Reconstruction of the Auricle. St. Louis, CV Mosby, 1974:24.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

73. Tanzer RC: Correction of microtia with autogenous costal cartilage. In Tanzer RC, Edgerton MT, eds: Symposium on Reconstruction of the Auricle. St. Louis, CV Mosby, 197447.
74. Tanzer RC: Microtia. Clin Plast Surg 1978;5:317. 75. Brent B: The correction of microtia withautogenous cartilage
graftx I. The classic deformity. Plast Reconstr Surg 1980; 661.
76. Brent B: The correction of microtiawith autogenous cartilage grafts: 11. Atypical and complex deformities. Plast Reconstr Surg 1980;66: 13.
77. Brent B: Total auricular construction with sculpted costal car- tilage. In Brent B, ed: The Artistry of Reconstructive Surgery. St. Louis, CV Mosby, 1987:113-127.
78. Broadbent TR, Mathews VI: Artistic relationships in surface anatomy of the face. Plast Reconstr Surg 1957;20:1.
79. Lauritzen C, Munro IR, Ross RB: Classification and treatment of hemifacial microsomia. Scand J Plast Reconstr Surg 1985;19:33.
80. Ohara K, Nakamura K, Ohta E: Chest wall deformities and thoracic scoliosis after costal cartilage graft harvesting. Plast Reconstr Surg 1997;99:1030.
81. Thomson HG, Kim TY, Ein SH: Residual problems in chest donor sites after microtia reconstruction: a long-term study. Plast Reconstr Surg 1995;95:961.
82. Brent B: Ear reconstruction with an expansile framework of autogenous rib cartilage. Plast Reconstr Surg 1974;53:619.
83. Gibson T, Davis W The distortion of autogenous cartilage grafts: its cause and prevention. Br J Plast Surg 1958;10:257.
84. Tanzer RC: An analysis of ear reconstruction. Plast Reconstr Surg 1963;31:16.
85. Firmin F: Controversies in autogenous auricular reconstruc- tion. Presented at Ear Reconstruction '98: Choices for the Future, Chateau Lake Louise, Canada, March 4,1998.
86. Weerda, H: Discussion of personal technique. In Panel by Brent B: Solving problems in autogenous auricular reconstruction. Presented at Ear Reconstruction '98: Choices for the Future, Chateau Lake Louise, Canada, March 5,1998.
87. Nagata S: Two-stage total auricular reconstruction with au- togenous costal cartilage. Presented at Ear Reconstruction '98: Choices for the Future, Chateau Lake Louise, Canada, March 4, 1998.
88. Letterman GS, Harding RL: The management of the hairline in ear reconstruction. Plast Reconstr Surg 1956;1&:199.
89. Brent B, Byrd HS: Secondary ear reconstruction with carti- lage grafts covered by axial, random, and free flaps of tem- poroparietal fascia. Plast Reconstr Surg 1983;72:141.
90. Wheeland RG: Laser-assisted hair removal. Dermatol Clin 1997; 15:469.
91. Dalrymple JC, Monaghan JN: Treatment of hidradenitis sup- uurativa with the carbon dioxide laser. Br J Sura 1987;74:420.
92. Sasaki G: Personal communication, 1998. -
93. LaskG, Elman M, Slatkine M,et al: Laser-assisted hairremoval by selective photothermolysis. Preliminary results. Dermatol Surg 1997;23:737.
94. Littler CM: Laser hair removal in a patient with hypertrichosis lanuginosa congenita. Dermatol Surg 1997;23:705.
95. Nanni CA, Alster TS: Optimizing treatment parameters for hair removal using a topical carbon-based solution and 1064- nm Q-switched neodymium:YAG laser energy. Arch Dermatol 1997;133: 1546.
96. Dieridor CC, Grossman MC, Farinelli WA, Anderson RR: Permanent hair removal by normal-mode ruby laser. Arch Dermatol 1998;134:837.
97. Brent B: Discussion of Nagata S: Modification of the stages in total reconstruction of the auricle. Plast Reconstr Surg 1994;93:267.
98. Tanzer RC: Secondary reconstruction of the auricle. InTanzer RC, Edgerton MT, eds: Symposium on Reconstructiofl of the Auricle. St. Louis, CV Mosby, 1974:238.
99. Cosman B: Repair of moderate cup ear deformities. In Tanzer RC, Edgerton MT, eds: Symposium on Reconstruction of the Auricle. St. Louis, CV Mosby, 19741 18.
100. Cosman B: Repair of the constricted ear. In Brent B, ed: The Artistry of Reconstructive Surgery. St. Louis, CV Mosby, 198299.
101. Matsumoto K: The characteristics of cryptotia and its therapy. Jpn J Plast Reconstr Surg 1977;20:563.
102. OhmoriS,Matsurnoto K: Treatment of cryptotia, usingTeflon string. Plast Reconstr Surg 1972;49:33.
103. Torikai T: Anatomy of the auricular muscles and its applica- tion to surgical treatment of cryptotia. Jpn J Plast Reconstr Surg 1982;25:46.
104. Tan ST,Abramson DL,MacDonald DM, MuUiken JB: Molding therapy for infants with deformational auricular anomalies. Ann Plast Surg 1997;38:263.
105. Yotsuyanagi T, Yokoi K, Urushidate S, Sawada Y: Nonsurgical correction of congenital auricular deformities in children older than early neonates. Plast Reconstr Surg 1998;101:907.
106. FukudaO: Otoplastyofcryptotia. Jpn JPIast Surg 1968;ll: 117. 107. Washio H: Cryptotia-pathology and repair. Plast Reconstr
Surg 1973;52:648. 108. McDoweU AJ: Goals in otoplasty for protruding ears. Plast
Reconstr Surg 1968;41:17. 109. Furnas DW Correction of prominent ears by concha-mastoid
sutures. Plast Reconstr Surg 1968;42:189. 110. Webster GV: The tail of the helix as a key to otoplasty. Plast
Reconstr Surg 1969;@455. 1 11. Morestin H: De la reposition et du plissement cosmetiques du
pavillon de Poreille. Rev Orthop 1903;14:289. 112. OwensN,Delgado DD: The management of outstanding ears.
South Med J 1955;58:32. 113. Paletta E, ShipA,VanNorman R: Double spring release in oto-
plasty for prominent ears. Am J Surg 1963;106:506. 114. Spira M, McCrea R, Gerow FJ, Hardy SB: Analysis and treat-
ment of the protruding ear. Transactions of the Fourth Inter- national Congress of Plastic Surgery. Amsterdam, Excerpta Medica, 1969:1090.
115. Stark RB, Saunders DE: Natural appearance restored to the unduly prominent ear. Br J Plast Surg 1962;15:385.
116. Ludrert WE. A new operation for prominent ears based on theanatomy of the deformity.SurgGyneco1Obstet L910;10:635.
117. Cloutier AM: Correction of outstanding ears. Plast Reconstr Surg 1961;28:412.
118. Erich JB: Surgical treatment of protruding ears. EyeEar Nose Throat Monthly 1958;37:390.
119. Straith RE: Correction of the protruding ear. Plast Reconstr Surg 1959;24:277.
120. McEvin WG: The problem of the protruding ear. Plast Reconstr Surg 1947;2:481.
12 1. Converse JM, Nigro A, Wilson FA, Johnson N: A technique for surgicalcorreaionoflopears.PlastReconstrSurg 1955;15:411.
122. Becker OJ: Surgical correction of the abnormally protruding ear. Arch Otolaryngol 1949;50:541.
123. Becker OJ: Correction of the protruding deformed ear. Br J Plast Surg 1952;5:187.
124. Tanzer RC: The correction of prominent ears. Plast Reconstr Surg 1962;30:236.
125. Mustarde JC: The correction of prominent ears using simple mattress sutures. Br J Plast Surg 1963;16:170.
126. Mustarde JC: The treatment of prominent ears by buried mattress sutures: a ten-year survey. Plast Reconstr Surg 1967;39:382.
127. Chongchet V: A method of anthelix reconstruction. Br J Plast Surg 196316268.
128. Stenstrom SJ: A "natural" technique for correction of con- genitally prominent ears. Plast Reconstr Surg 1963;32:509.
129. Ju DMC, Li C, Crikel& GF: The surgical correction of pro- truding ears. Plast Reconstr Surg 1963;32:283.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7

111 + THE HEAD N O NEW
130. Kaye BL: A simplified method for c o r r ~ g the prominent ear. Plast Reconstr Surg 1967;40:44.
13L Ch&rii RC, Essai 6u krtstawation dupadon de I'oreille [these pour le Doctorat en Medecine]. Lille, L. Danel, 1894.
132. Clemons JE, Connelly MV Reattachment of a totally ampu- tated auride. Arch Otolaryngol 1973;92269.
133. Gifford GH: Replantation of severed part of an ear. Plast Reconstr Surg 197249202.
134. McDowell F: Suamsful replantation of severed halfof ear. Plast Reconstr Surg 1971;48:28 1.
135. Conway H, Neumann CG, Golb J, et al: Reconstruction of the external ear. Ann Surg 1948;128:226.
136. Greeley PW. Reconstruction of theexternal ear. US Naval Med Bull 1944;42:1323.
137. Musgrave RH, Garrett WS: Management of avulsion injuries of the external ear. Plast Reconstr Surg 1967;40:534.
138. Suraci AJ: Plastic reconstruction of acquired defects of the ear. Am J Surg 1944,66:196.
139. W o n RP: Utilization of the amputated ear cartilage. Plast Reconstr Surg 1955;15:419.
140. Conroy CC: Salvage of an amputated ear. Plast Reconstr Surg 1972;49564.
141. Bonanno PC, Converse JM: Reconstruction of the ear. In Kazanjian VH, Converse JM, eds: Surgical Treatment of Facial Iniuries, 3rd ed. Baltimore, Wiiarns & Wilkins, 19741292.
142. Mb%ck RA, ort ton damson JE, Cohen BI: pocket prin- ciple: a new technique for reattachment of a severed ear part. Plast Reconstr Surg 1971;48:219.
143. MladickRA,CarrawayJH: Earreattachment bymodified pocket principle. Plast Reconstr Surg 1973;51:584.
144. Grabb WC, Dingman RO: The fateof amputated tissues of the head and neck following replacement. Plast Reconstr Surg 1972;49:28.
145. Baudet J, Tkamond P, Goumain A: A new technic for the reim- plantation of a completely severed auricle [in French]. Ann Chir Plast 19721267.
146. Juri J, Irigaray A, Juri C, et al: Ear replantation. Plast Reconstr Surg 1987;80:431.
147. ~ e n n i n ~ t o n DG, Lai MF, Pelly AD: Successful replantation of a com~letdv avulsed ear bv microvascular anastomosis. %st ~econ&r s i rg 1980;65:820.
148. Mutimer K, Banis JC, Upton J: Microsurgical reattachment of totally amputated ears. Plast Reconstr ~ u r g 1987;79:535.
149. Steffensen WH: Method of correctingatresia of ear canal. Plast - Reconstr Surg 1946,1:329.
150. Byrd HS: The use of subcutaneous axial fascial flaps in recon- struction of the head. Ann Plast Surg 1980;4191.
151. AlbrekzssonT,BranemarkPI,JacobssonM,ZelistromA: Present dinicalapplicationsofo~~e~integratedpercutanmusimplants. Plast Reconstr Surg 1987;79721.
152. Adams WM: Construction of the upper halfof the auricle uti- lizing a composite concha cartilage graft with perichondrium attached on both sides. Plast Reconstr Surg 1955;16:88.
53. Brent B: The versatile cartilage autograft: current trends in dinid transplantation. Clin Plast Surg 1979;6:163.
1 Day HF. Reconstruction of the ears. Boston Med Surg J 1921;185:146.
155. Nagel P: Reconstruction of a partial auricular loss. Plast Reconstr Surg 197249340.
156. Pegram M, Peterson R: Repair of partial defects of theear.Plast Reconstr Surg 1956;18:305.
157. Brent B: Theacquired auricular deformity. Asystemic approach to its analysis and reconstruction. Plast Reconstr Surg 1977;59:475.
158. Antia NH, BuchVI: Chondrocutaneous advancement flap for themarginaldefect of the ear. Plast Reconstr Surg 1%7;39:472.
159. SteaFanoff DN: Auriculo-mastoid tube pedicle for otoplasty. - . Plast Reconstr Surg 1948;3:352.
160. Crikelair GF: A method of partial ear reconstruction for avulsion of the upper portion of the ear. Plast Reconstr Surg 1956; 12438.
161. ConverseJbtReconst~ctionof theauricle.Plast Reconstr Surg 1958;22:150,230.
162. Preaux J: A simple procedure for reconstruction of the lower part of the auride [in French]. Ann Chir Plast 1971;16:60.
163. Pardue AM: Repair of torn earlobe with preservation of the perforation for an earring. Plast Reconstr Surg 1973;51:472.
164. Cosman B, Wolff M: Bilateral earlobe keloids. Plast Reconstr Surg 1974;53:540.
165. Ramakrishnan KM, Thomas KP, Sundararajan CR: Study of 1,000 patientswith keloids in South India. Plast Reconstr Surg 1974;53:276.
166. Ketchum LD, Cohen IK, Masters FW: Hypertrophic scars and keloids. A collective review. Plast Reconstr Surg 1974;53:140.
167. Snyder GB: Button compression for keloids of the lobule. Br J Plast Surg 1974;22 186.
168. Brent B: The role ofpressure therapy in management of earlobe keloids: preliminary report of a controlled study. AM Plast Surg 1978;1:579.
169. Gavello P: Quoted by Nelaton C, Ombredanne L: Les auto- plastics. Paris, G. Steinheil, 1907.
170. Brent B: Earlobe construction with an auriculomastoid flap. Plast Reconstr Surg 1976;57:389.
171. Guerrero-Santos J: Correction of hypertrophied earlobes in leprosy. Plast Reconstr Surg 1970;46:381.
172. Zenteno Alanis S: A new method for earlobe reconstruction. Plast Reconstr Surg 1970;45:254.
173. AronsMD,Sadin RC: Auricular cancer.Arn J Surg 197 1;122:770. 174. Lewis JS: Cancer of the ear. Laryngoscope 1960;7&55 1. 175. Hoopes JE: Reconstruction of the auricle after tumor resec-
tion. In Tanzer RC, Edgerton MT, eds: Symposium on Recon- struction of the Auricle. St. Louis, CV Mosby, 1974232.
176. Mladick RA, Horton CE, Adamson JE, Caraway JH: The core resection for malignant tumors of the auricular area and sub- jacent bones. Plast Reconstr Surg 1974;53:281.
177. Parsons H, Lewis JS: Subtotal resection of the temporal bone for cancer of the ear. Cancer 1954;7:995.
RoshanKetabMedical Publishers
TEHRAN - IRAN Tel: +98(21)66950639TelFax: +98(21)66963783_7