DWC TargeTs Improper DenIals BaseD on laCk of ...Office visit notes/report satisfying the American...
Transcript of DWC TargeTs Improper DenIals BaseD on laCk of ...Office visit notes/report satisfying the American...

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N �
DWC TargeTs Improper DenIals BaseD on laCk of DoCumenTaTIon
In This Issue…
Case Management ...............................p. 10
2008 Question Resolution Logs .............p. 18
©2008 – Flahive, Ogden & Latson A P R I L 2 0 0 8 n V O L U M E � 3 , N O . 3
A P R I V I L E G E D AT T O R N E Y - C L I E N T C O M M U N I C AT I O N B Y F L A H I V E , O G D E N & L AT S O N
The DWC is targeting carriers who improperly deny medical bills based upon the claim that the bill lacks adequate documentation. The Division has elevated this issue to a high profile in its enforcement efforts. We expect the agency to begin recommending increased fines against carriers who improperly deny medical bills based on lack of documentation.
While the defense that a bill is not properly documented is a proper defense in many cases, documentation is not always required by Division rules. Where documentation is not required, and carriers deny a bill because of the lack of documentation, the DWC intends to pursue enforcement actions. The agency announced that it has identified many instances in which carriers have improperly utilized the defense. Accordingly, it is vital that carriers understand when documentation is required and when it is not required. This is a training point for carriers and health care providers.
Moreover, where documentation is required and is requested by the carrier when processing the bill, it is critical that every request for documentation adhere to
seven specific provisions contained in Rule 133.210(d). Under that rule, any request made by the insurance carrier for additional documentation to process a medical bill must:
• Be in writing;• Be specific to the medical bill or the
bill’s related episode of care;• Describe with specificity the clinical
or other information to be included in the response;
• Be relevant and necessary for the resolution of the medical bill;
• Be for information that is contained in or in the process of being incorporated into the injured employee’s medical or billing record maintained by the health care provider;
• Indicate the specific reason for which the insurance carrier is requesting the information; and
• Include a copy of the medical bill for which the insurance carrier is requesting additional documentation.
Two things have caused the Division’s anticipated increase in enforcement in this area: provider complaints and the agency’s implementation of eBilling. Provider complaints have attracted the attention
Continued on p. 5

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N2
Flahive, Ogden & Latson, a 24 lawyer firm, defends contested workers’ compensation cases statewide every day. The firm has represented insurance companies and employers before the Texas Workers’ Compensation agency for more than
50 years. For general questions concerning the newsletter call: (512) 435-2234.
Flahive, Ogden & LatsonP.O. Box 13367
Austin Texas 78711
An electronic copy of FOLIO, our monthly client newsletter, is now available for
clients. If you are interested in receiving FOLIO by email, please let us know.
FOLIO is prepared for the exclusive use of Flahive, Ogden & Latson clients only. It contains privileged communications and further sharing of this newsletter
(in either hard copy or electronic format) outside your company without the express written consent of Flahive,
Ogden & Latson is not permitted.
Our regular office hours are 8:15 a.m. to 4:45 p.m. If you need to call after 4:45,
please call Patsy Shelton at (512) 435-2234. She will be on duty until 6:00 p.m. daily.
fo&l offICe HoursDon’t wait until the last hour of the day for deadline filing. Any faxes with information due must be received by 3:30 p.m. for any deadline handling for same day delivery to the Division, and faxed according to the fax directory listed on the last page of FOLIO.
Furthermore, if you have a last minute deadline, call our office by 3:00 p.m. and
speak with Tillie Aguirre or Patsy Shelton to advise that a last minute filing is necessary to meet a deadline. We will be watching and waiting for the fax. Otherwise, last
minute faxes could delay receipt. Our last daily run to the Division will be at 4:00 p.m.,
in order to get across town to meet their 5:00 closing time.
TDI Delays Tpa annual reporT for many
Workers’ CompensaTIon aDmInIsTraTors
The obligation that many Texas TPAs file an Annual Report (Form 2A LHL080) has been delayed by the Department of Insurance. The annual reporting obligation was imposed by the legislature after the implementation of HB 472 last session. Until very recently, most administrators understood that they would be required to file an annual report no later than June 30, 2008.
When licensed TPAs began to prepare for the filing of their annual reports, they encountered a problem. The Department has not completed its revision of the forms required to report workers’ compensation transactional data.
As a result, the Department has advised us that the annual report obligation will be delayed until June 2009 for any administrator who became licensed on or after September 1, 2008. Administrators who held Texas TPA licenses before September 1, 2008 must still comply with their annual reporting obligation.
The Department has described this change in the following way:
“...For entities who are subject to HB 472 and who did not hold a certificate of authority from the Department to act as an administrator under the Insurance Code Chapter 4151 prior to September 1, 2007: Reporting related to workers’ compensation is not required for the annual report that is due June 30, 2008. Reporting related to workers’ compensation will be required for the annual report due June 30, 2009.
For entities who hold a certificate of authority to act as an administrator
Continued on p. 13

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N 3
memoranDum
DATE: March 26, 2008 TO: All Workers’ Compensation System Participants FROM: Amy Morehouse, Enforcement Allen McDonald, Information Management Services RE: Improper Denials Based on Lack of Documentation
The Texas Department of Insurance, Division of Workers’ Compensation (TDI-DWC), has received several complaints about insurance carriers and bill review companies that are improperly denying payment for medical services for lack of documentation (denied in a manner which is inconsistent with the provisions of the Texas Labor Code).
The Texas Administrative Code (TAC), including 28 TAC §133.210, defines the types of services that require medical documentation to be submitted along with medical bills and the process to request additional medical documentation when necessary. Workers’ compensation health care networks established under Texas Insurance Code Chapter 1305 may decrease any of the documentation requirements.
An insurance carrier may request additional medical documentation after receipt of a medical bill, provided the request complies with the regulatory requirements. Texas Labor Code §408.027(b) allows an insurance carrier to request additional documentation necessary to clarify the provider’s charges. Under 28 TAC §133.210(d), any request made by the insurance carrier for additional documentation to process a medical bill shall:
• be in writing; • be specific to the medical bill or the bill’s related episode of care; • describe with specificity the clinical or other information to be included in the response; • be relevant and necessary for the resolution of the medical bill; • be for information that is contained in or in the process of being incorporated into the
injured employee’s medical or billing record maintained by the health care provider; • indicate the specific reason for which the insurance carrier is requesting the information;
and • include a copy of the medical bill for which the insurance carrier is requesting additional
documentation.
In accordance with the Texas Labor Code, insurance carriers shall not deny payment for services based on the failure to provide documentation unless the TAC provisions specifically require documentation to be submitted with the medical bill for the services rendered; or, the health care provider has failed to respond to an insurance carrier’s request for documentation submitted in accordance with 28 TAC §133.210(d). The last page of this memorandum contains a list of some of the documentation required to be submitted with a medical bill.
electronic medical Billing and required Documentation With the implementation of electronic medical billing (eBill), the need to properly associate documentation with the electronic medical bill transaction has become increasingly important. While attaching documentation to a paper bill is relatively simple, the submission of documentation that is not required complicates the eBill process for both health care providers and insurance carriers. In addition, health care providers may submit medical documentation to the insurance carrier using different methods, including facsimile (fax), email or another electronic format.

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N�
Insurance carriers must ensure that they have established the technical ability and administrative processes to match any incoming medical documentation with the associated medical bill. An insurance carrier is considered to have received the medical documentation when it is received by the insurance carrier’s agent; including an eBill agent, clearinghouse, bill review vendor, utilization review agent, or adjuster. In these situations, the health care provider may charge for subsequent requests for the same documentation consistent with 28 TAC §134.120(b). As stated in 28 TAC §133.210(e):
It is the insurance carrier’s obligation to furnish its agents with any documentation necessary for the resolution of a medical bill. The Division considers any medical billing information or documentation possessed by one entity to be simultaneously possessed by the other.
enforcement TDI-DWC will take appropriate enforcement action if an insurance carrier improperly denies medical bills or requests documentation in violation of agency rules. Insurance carriers should be prepared to demonstrate that their requests for additional documentation were made in compliance with 28 TAC §133.210(d) and to provide the basis for any denials related to the failure of a health care provider to submit documentation with their medical bill.
Texas Labor Code §415.002 provides that an insurance carrier commits an administrative violation if the insurance carrier fails to process claims promptly in a reasonable and prudent manner or violates a rule adopted by the Commissioner of Workers’ Compensation.
How to file a Complaint Health care providers may file complaints regarding inappropriate denials or other potential administrative violations by submitting the complaint by facsimile (fax) to Complaint Resolution at 512-490-1030. Health care providers may also submit complaints using the TDI-DWC on-line complaint form located at http://www.tdi.state.tx.us/consumer/complfrm.html#wc
Questions regarding this memorandum may be directed to Allen McDonald, Director of Information Management Services, at 512-804-4530 or [email protected].
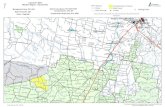
list of required medical Documentation The following table outlines many of the documentation requirements and provides some service identification information to assist insurance carriers in reviewing any bill processing edits complying with the regulatory framework:
Service Description Required Documentation Possible Service Identifier
The two highest Evaluation and Management office visit codes for new and established patients (28 TAC §133.210(c)(1))
Office visit notes/report satisfying the American Medical Association requirements for use of those CPT codes
CPT Code 99204, 99205, 99214, or 99215
Surgical services rendered on the same date for which the total of the fees established in the current Division fee guideline exceeds $500 (28 TAC §133.210(c)(2))
A copy of the operative report CPT Codes 10000 through 60000 series, depending on reimbursement amount
Return to work rehabilitation programs as defined in 28 TAC §134.202 (28 TAC §133.210(c)(3))
A copy of progress notes and/or SOAP (subjective/objective assessment plan/procedure) notes, which substantiate the care given, and indicate progress, improvement, the date of the next treatment(s) and/or service(s), complications, and expected release dates
CPT Code 97545 with modifier “WC”; CPT Code 97546 with modifier “WC”; CPT Code 97545 with modifier “WH”; CPT Code 97546 with modifier “WH”; 97799 with modifier “MR”; or, CPT Code 97799 with modifier “CP” Note: CARF accredited Programs will add “CA” as a second modifier

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N �
Service Description Required Documentation Possible Service Identifier
Procedures/services which do not have an established Division maximum allowable reimbursement (28 TAC §133.210(c)(4))
Any supporting documentation for and an exact description of the health care provided
Varied miscellaneous services not valued by Medicare.
Hospital services (28 TAC §133.210(c)(5))
An itemized statement of charges Hospital bills with the type of bill/type of facility code of “1” (Hospital)
Functional Capacity Evaluations (FCEs) (28 TAC §134.204(g))
All documentation related to the FCE
97750 with modifier “FC.”
Certification statement of costs for separately reimbursed surgically implanted devices (28 TAC §§133.402(e)(4), 134.403(g), and 134.404(g))
Certification of the amount which represents actual cost of surgically implanted, inserted, or otherwise applied devices.
ASC bill with claim notes and attachments; or, Hospital bill with bill notes and attachments
Required Medical Examinations (28 TAC §126.6)
Medical report CPT Code 99456 with modifier “RE”
Designated Doctor Examinations (28 TAC §126.7)
Narrative report and forms, as applicable
Modifiers “W5”, “W6”, “W7”, “W8”, and “W9”
Treating Doctor Examination to Define Compensable Injury (28 TAC §126.14)
Narrative report Modifier “TX”
Work Status Reports (28 TAC §129.5)
Work Status Report CPT Code 99080 with modifier “73” and with modifier “RR” or “EC,” if applicable
MMI/IR Examinations and Determinations (28 TAC §130.1)
Form and narrative report (when applicable)
CPT Code 99455 with Modifiers “MI”, “V1”, “V2”, “V3”, “V4”, or “V5”
Note: This table may not represent an all-inclusive list of services which require documentation. It is possible that other potential documentation requirements exist, such as those required by CMS payment policies.
of agency enforcement staff; eBilling implementation staff members have focused their efforts on the education of system stakeholders.
In an email to many system participants in late March 2008, the agency noted that it has received complaints that insurance carriers and bill review companies are improperly denying payment for medical services for lack of documentation in a manner that is inconsistent with the provisions of the Texas Labor Code.
Moreover, in a system stakeholder meeting regarding the agency’s eBilling
DWC Targets Improper Denials Based on Lack of Documentation – continued from p. 1
initiative, Allen McDonald, head of Information Management Services for the Division, emphasized that carriers who request unnecessary documentation to support provider billing are creating significant impediments to successful eBilling implementation.
Staff from the enforcement and information management departments jointly authored a memorandum, which expresses the agency’s disapproval of improper denials of medical bills based on lack of documentation. The memo also contains a table that describes when medical bills require documentation and when they do not. We have reprinted the Division’s memorandum and its attached table in its entirety in this issue of FOLIO.

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N�
GQ CORnER
Q: The claimant had an injury on the job on December 1, 2007. Carrier received First Written Notice of Injury
on that same day. Claimant also underwent a drug screen, which he failed. The employer terminated the claimant on December 7, 2007 once it received the results from the positive drug screen. Carrier has not received any records of medical treatment beyond the initial visit and has not been able to contact the claimant since he has been terminated to know whether or not there is any lost time. The carrier is now past the 15-day dispute deadline. As such, can the carrier still deny the claim in its entirety and, if so, does it owe any income benefits since the denial would come after the 15-day deadline, but before the 60-day deadline?
A: Since the carrier is still within the initial 60 days after receiving First Written Notice of Injury, it may dispute the
entire claim based upon intoxication and any other defenses it may have. Carrier would obviously owe for any medical and income benefits that have accrued through the date prior to your filing a notice of dispute. In these facts, you would certainly owe for the initial medical treatment, but you have provided no facts that the injury claimant indeed had lost time from work as a result for the alleged compensable injury. Without such evidence, carrier would not owe temporary income benefits. If evidence is later provided that he did have lost time during the time prior to your filing of the denial, then income benefits would be owed for the period established by the facts but not beyond the day before you file your notice of dispute.
Q: Carrier received a request for reimbursement on a DWC-26 from a healthcare insurer. Is the carrier
required to send its response to the DWC-26 by verifiable means and does it have to send a copy of the response to the Texas Department of Insurance?
A: Carriers should treat responses to DWC-26s as it would with a medical bill. There is no requirement that the
carrier send its response by verifiable means, but in order to avoid compliance issues, it is suggested that the carrier document the date that its response was sent to the healthcare insurer. Additionally, there is no requirement that a copy of the carrier’s response to the DWC-26 be sent to the Texas Department of Insurance.
Q: Claimant moved out of the State of Texas. She is living in Pennsylvania. Carrier received a copy of an off
work slip from a doctor that she visited in Pennsylvania. Is the carrier able to suspend temporary income benefits until it receives an off work slip from an approved physician?
A: The Approved Doctors List is no longer in effect as of September 1, 2007 except for those doctors that
were previously removed from the list. When it comes to establishing disability, it does not matter whether the doctor was on or off of the ADL list. Any off work slip from any healthcare professional in good standing is some evidence of disability period. In fact, the Division of Workers’ Compensation has found that it is sufficient for a hearing officer to find disability based upon the injured worker’s own lay testimony about his inability to perform his pre-injury job. Therefore, the carrier will need evidence that the injured worker has an ability to return to his pre-injury job before it can begin considering suspension of temporary income benefits.

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N �
Q: Carrier understands that there have been some changes regarding when lifetime income benefits begin to
accrue. When does the carrier’s potential exposure for lifetime income benefits begin?
A: Previously, Rule 131.1 indicated that lifetime income benefits were payable back to the first date of disability. The
Appellate Court in Mid-Century Ins. Co. vs. Texas Workers’ Compensation Commission held that lifetime income benefits accrue and become payable on the date that the injured worker suffers from one of the conditions listed in Section 408.161 (a) and not before. Once an injured worker is adjudicated to be eligible to receive lifetime income benefits, then lifetime income benefits should be paid retroactively to the date that the injured worker first became eligible.
Q: Injured worker returned to work in a light duty capacity and is earning some post-injury earnings. He is earning
approximately 85% of his average weekly wage through his light duty work. Is the carrier required to pay temporary income benefits if the employee’s post-injury earnings are greater than the maximum rate for temporary income benefits?
A: If the injured worker’s post-injury earnings are less than his average weekly wage, then carrier will owe
some temporary income benefits. The minimum and maximum temporary income benefits rates are limited to those amounts paid by the carrier as temporary income benefits. Those minimum and maximum rates do not apply to the injured worker’s post-injury earnings.

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N8
TenTaTIve TImeTaBle for TDI proDuCTIon of WC neTWork reporT CarD
anD HB 7 BIennIal reporT To THe legIslaTure
February 15, 2008 – Data Call Sent to all WC Networks
March 4, 2008 – Reminder Sent out to Networks re: Data Call Deadline
March 7, 2008 – Deadline for Network Data Call
April, 2008 – TDI to:1) Review Data Call Submissions to
Determine Which Networks Are Included in Report Card, Separate Out New Claims, Determine Whether Claims are Lost-Time or Medical-Only, and Refine Survey Sampling Plan
2) Secure Survey Administration Contract with University Survey Center
3) Draw/Provide Final Survey Sample to University Survey Center
Late April – Early July – University Survey Center to Administer Telephone Survey to Network and Non-Network Injured Workers
July-August 2008 – TDI to Compile and Calculate Report Card Measures Using Survey Data and DWC Administrative Data; TDI Also to Compile Measures for Biennial Report
Late August/September 2008 –Provide Individual Networks Copies of Their Results
September 2008 – Publish Final WC Network Report Card/Distribute Press Release
September 2008 – TDI to Compile Initial Draft of Biennial Report for Internal Review
December 1, 2008 – Publish Biennial Report to the Legislature on the Impact of Networks on Medical Costs and Quality of CareNo late than December 1, 2008 – Commissioner of Insurance to hold a WC rate hearing to examine the impact of HB 7 on the availability and affordability of WC coverage for employers.
DWC repeals THe InTerloCuTory
orDer rule
The Division of Workers’ Compensation has repealed its rule describing the process for requesting interlocutory orders. The repeal follows legislation passed in 2007 setting out more specific guidelines for the request and granting of interlocutory orders. That legislation permitted certain agency staff to order both the payment and the suspension of benefits.
Section 410.032 of the Labor Code now contains the Division’s authority for, and describes the procedure by which, interlocutory orders should be requested and granted.
remInDer: upDaTe your ComplIanCe ConTaCT
InformaTIon
Last November, we announced that the Division of Workers’ Compensation had agreed to make changes in its notification process on compliance matters. Carriers are now entitled to designate a compliance contact person for each underwriting company.
Future notices of Enforcement Management Conferences as well as notices of proposed Consent Orders are now sent to that compliance contact person. The Division will retain its practice of sending a copy to the

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N �
company’s corporate representative, but the corporate representative’s letter will show that a copy has been sent to the compliance officer, as well as to identify that person.
If you have not yet designated a compliance contact person for your company or your underwriting companies please contact Patsy Shelton at [email protected]. Moreover, if your compliance contact information has changed since you last notified the Division, please let Patsy know and we will submit updated information to the agency.
If you have any questions or suggestions about this process, please contact James Sheffield or Bobby Stokes.
Zurek nameD To DWC polICy anD researCH
posT
Matt Zurek, currently Director for Health Care Policy at the Texas Division of Workers’ Compensation, will become DWC Executive Deputy Commissioner for Policy and Research effective Tuesday.
Zurek, who joined the agency in August. will be responsible for policy areas including implementation of ebilling, disability management and fee guidelines.
Before joining the agency Zurek served as vice president for clinical quality with HealthSouth Corp. He also has served as reimbursement chairman for workers’ compensation issues at the Texas Physical Therapy Association.
Zurek received a bachelor of science degree in physical therapy from the University of Texas Health Science Center at Dallas and a B.S. in biology and health from Eureka College.
DIvIsIon aCCepTIng puBlIC CommenT
on Informal anD volunTary neTWork
rules
AUSTIN, TX –The Texas Department of Insurance, Division of Workers’ Compensation (TDIDWC) is accepting public comment on proposed rules regarding notification to health care providers of contractual agreements with informal networks and voluntary networks, and reporting requirements. The proposed rules may be viewed on the TDI website at http://www.tdi.state.tx.us/wc/rules/proposedrules/toc.html. The deadline to submit public comments is Monday, April 7, 2008 at 5 p.m.
Submit public comments to TDI-DWC by e-mailing them to [email protected], or mailing or delivering them to Victoria Ortega, TDI-DWC, Legal Services, MS-4D, 7551 Metro Center Drive, Suite 100, Austin, Texas 78744-1609.
The proposed amended and new rules will be published in the Texas Register on March 7, 2008:
CHAPTER 133 — General Medical Provisions Subchapter A General Rules for Medical Billing and Processing §133.2 Definitions (amendment)§133.4 Written Notification to Health Care Providers of Contractual Agreements for Informal and Voluntary Networks (new)§133.5 Informal Network and Voluntary Network Reporting Requirements to the Division (new)

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N�0
Case managemenT
The function of case management in the Texas workers’ compensation system is to effectively coordinate care and to facilitate the injured worker’s timely and productive return to work. Case management consists of either team conferences or telephone calls with an interdisciplinary team, which may include the employer. Although the treating doctor is primarily responsible for case management, a referral provider may participate in and bill for these specified case management activities.
An interdisciplinary team may not include employees of the coordinating provider. A health care provider in a Return to Work Rehabilitation Program may not initiate case management because reimbursement for the program includes coordination of care. However, a health care provider outside the RTW program may initiate case management with a health care provider in the RTW program. In this case, both the health care provider outside the RTW program and the health care provider inside the RTW program can be reimbursed for reasonable and medically necessary case management activities.
Team conferences and telephone conversations should be triggered by a documented change in the condition of the injured worker. Documentation for case management activities must include the purpose and outcome of conferences and telephone calls, and the name and specialty of each individual attending the team conference or engaged in the telephone conversation.
Team conferences may occur, and be billed for, more than once every 30 days if the conferences are for the purposes of: (1) coordinating return to work options with the employer, employee, or an assigned medical or vocational case manager; (2) developing or revising a treatment plan; (3) altering or clarifying previous instructions; or (4) coordinating the care of employees with catastrophic or multiple injuries requiring multiple specialties.
Billing and reimbursement for case management services is as follows:
CPT Code
Description Treating Doctor Modifier
Treating doctor
Contributing HCP (no Modifier)
99361 Medical conference by a physician with interdisciplinary team of health professionals or representative of community agencies to coordinate activities of patient care (patient not present); approximately 30 minutes.
W1 $113 $28
99362 Medical conference by a physician with interdisciplinary team of health professionals or representative of community agencies to coordinate activities of patient care (patient not present); approximately 60 minutes.
W1 $198 $50
99371 Telephone call by a physician to a patient or for consultation or medical management or for coordinating medical management with other health care professionals (e.g., nurses, therapists, social workers, nutritionists, physicians, pharmacists); simple or brief (e.g., to report on tests and/or laboratory results, to clarify or alter previous instructions, to integrate new information from other health professionals into the medical treatment plan or to adjust therapy).
W1 $18 $5

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N ��
CPT Code
Description Treating Doctor Modifier
Treating doctor
Contributing HCP (no Modifier)
99372 Telephone call by a physician to a patient or for consultation or medical management or for coordinating medical management with other health care professionals (e.g., nurses, therapists, social workers, nutritionists, physicians, pharmacists); intermediate (e.g., to provide advice to an established patient on a new problem, to initiate therapy that can be handled by telephone, to discuss test results in detail, to coordinate medical management of a new problem in an established patient, to discuss and evaluate new information and details, or to initiate new plan or care).
W1 $46 $12
99373 Telephone call by a physician to a patient or for consultation or medical management or for coordinating medical management with other health care professionals (e.g., nurses, therapists, social workers, nutritionists, physicians, pharmacists); complex or lengthy (e.g., lengthy counseling session with anxious or distraught patient, detailed or prolonged discussion with family members regarding seriously ill patient, lengthy communication necessary to coordinate complex services of several different health professionals working on different aspects of the total patient care plan).
W1 $90 $23
DIsCounT raTe anD InTeresT raTe DeTermIneD
for aprIl 1, 2008 THrougH June 30, 2008
AUSTIN, TX—The Texas Department of Insurance, Division of Workers’ Compensation has determined, pursuant to the authority and direction given under the Texas Workers’ Compensation Act (Texas Labor Code, Section 401.023), that any interest or discount provided for in the Act shall be at the rate of 4.82 percent. This rate is computed by using the treasury constant maturity rate for one-year treasury bills issued by the United States Government, as published by the Federal Reserve Board on March 17, 2008, (1.32 percent) plus 3.5 percent as required by Section 401.023. The rate shall be effective April 1, 2008 through June 30, 2008.
For more information regarding the rate calculation, please call Matt Jung at 512-322-4322.
Issued in Austin, Texas on March 25, 2008.
Albert Betts,Commissioner of Workers’ Compensation

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N�2
CommIssIoner BeTTs approves 12 CompanIes To self-Insure for Workers’ CompensaTIon ClaIms
AUSTIN, TX – Twelve companies with approximately 32,500 employees in Texas recently were approved to self-insure for workers’ compensation claims for a one-year period under the Texas Department of Insurance, Division of Workers’ Compensation Self Insurance Program.
Commissioner of Workers’ Compensation Albert Betts approved initial applications for Certificates of Authority to Self-Insure for both E.I. du Pont de Nemours and Company, headquartered in Wilmington, DE and Associated Wholesale Grocers, Inc., which has its headquarters in Kansas City, KS.
Under Texas law, certain large, private companies can self-insure for workers’ compensation claims, while retaining the protection of the Texas Workers’ Compensation Act for the company and for its employees. To qualify, a company must have a minimum workers’ compensation insurance unmodified manual premium of $500,000 and meet other requirements subject to annual review.
The following ten companies received renewals of existing self-insurance certificates: Ameron International Corporation, Pasadena, CA Ascension Health, St. Louis, MO Cooper US, Inc., Houston, TX Jacobs Engineering Group Inc., Houston, TX Louisiana-Pacific Corporation, Portland, OR Mount Vernon Mills, Inc., Mauldin, SC PACCAR Inc., Bellevue, WA The Procter & Gamble Company, Cincinnati, OH Textron, Inc., Providence, RI Weyerhaeuser Company, Federal Way, WA
For more information on applying to the Self-Insurance Program, visit TDI’s website at www.tdi.state.tx.us/wc/si/index.html.

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N �3
reImBursemenT of valID HCpCs (CpT) CoDes
WITHouT an assIgneD value
The Division of Workers’ Compensation recently published a health care module, which explains the agency’s view of carrier’s payment obligations for medically necessary health care in the workers’ compensation system. This module explains how carriers should reimburse validly billed CPT Codes that do not have an assigned value under CMS.
The Division noted initially that insurance carriers are responsible for correctly reimbursing medically necessary workers’ compensation treatments and services.
With the adoption of the 2002 Medical Fee Guideline (§134.202), the Texas workers’ compensation system began using Medicare coding, billing, reporting, and reimbursement methodologies, models, and values or weights for reimbursement of professional medical services provided on or after August 1, 2003. This requirement remains the same for the new Medical Fee Guidelines, §134.203 and §134.204. Reimbursement values for most Healthcare Common Procedure Coding System (HCPCS) codes used in Texas workers’ compensation may be found by using the Medicare Physician Fee Schedule Data Base or the fee calculator on the TrailBlazer Health Enterprises, LLC website at www.trailblazerhealth.com
If a valid CPT code does not have a relative value assigned by CMS, or a reimbursement amount assigned by CMS or the Division, and there is no negotiated contract between an insurance carrier and a health care provider, reimbursement shall be the lesser of a health care provider’s usual and customary charge or a fair and reasonable reimbursement amount.
Additionally, if payment for HCPCS codes for durable medical equipment, medical supplies and home health services are not specified by CMS, Texas Medicaid or the
Division, and there is no negotiated contract between an insurance carrier and a health care provider, reimbursement shall be the lesser of health care provider’s usual and customary charge or a fair and reasonable reimbursement amount.
Division §134.1 provides that fair and reasonable reimbursement must be consistent with reimbursement r similar procedures provided in similar circumstances, and be based on nationally recognized published studies, published Division medical dispute decisions, and values assigned for services involving similar work and resource commitments, if available.
under the Insurance Code Chapter 4151 issued by the Department prior to September 1, 2007: Reporting for the annual report that is due June 30, 2008, shall follow the format required by the TPA Annual Report (Form 2A LHL080), currently posted on the Department’s website....”
In addition, TDI has advised us that Oversight of the TPA Section of the Texas Department of Insurance (TDI) is in the process of being transferred to the Financial Program of TDI.
We encourage anyone having questions regarding this filing obligation to contact Steve Tipton or Bobby Stokes in our office to discuss.
TDI Delays TPA Annual Report for Many Workers’ Compensation Administrators – continued from p. 2

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N��
fIve mosT frequenTly uTIlIZeD Drug suBClasses ToTal numBer of presCrIpTIons
presCrIpTIon year 2006
The Texas Workers’ Compensation Commission, Division of Workers’ Compensation has identified five drug subclasses, which make up 56 percent of all the drugs dispensed in the Texas workers’ compensation system. The largest subclass is made up of Hydrocodone combinations. In 2006 309,000 prescriptions for Hydrocodone were written for Texas workers’ compensation claimants.
Hydrocodone Combinations:
309K
Central Muscle Relaxants: 224K
Nonsteroidal Anti- Inflammatory Agents:
200K
Anticonvulsants: 83K
Opioid Agonists: 114K
0 50,000 100,000 150,000 200,000 250,000 300,000 350,000
Number of Prescriptions

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N ��
fIve mosT frequenTly DenIeD Drug suBClasses presCrIpTIon year 2006
The Texas Department of Insurance, Division of Workers’ Compensation has identified the five most frequently denied drug subclasses for prescription year 2006. These five subclasses make up more than 130,000 prescriptions for the year.
The most frequently denied drug subclass is Hydrocodone in its various combinations. More than 20,000 prescriptions for the Hydrocodone combination subclass were written and denied in 2006.
Other Subclasses *
71K
Hydrocodone Combinations: 20K
Nonsteroidal Anti- Inflammatory Agents:
18K
Opioid Agonists: 6K
Central Muscle Relaxants: 17K
0 10,000 20,000 30,000 40,000 50,000 60,000 70,000 80,000
Number of Prescriptions

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N��
mosT frequenTly DenIeD presCrIpTIons By THerapy ClassIfICaTIon groups
presCrIpTIon year 2006
In a recently released study, the Texas Department of Insurance, Division of Workers’ Compensation identified the most frequently denied prescriptions by therapeutic classification groups for prescription year 2006. Opioid analgesics made up 20 percent of the denied drugs for the year.
The total number of injured employees includes duplicates since each employee could receive prescriptions from multiple therapeutic classification groups.
TherapeuticClassification Group
number ofDenied
Prescriptions
number ofInjured
EmployeesW/Denied
Prescriptions *
Total DeniedCharges
OTHER GROUPS 71,219 (42%) 13,020 $23,732,524
ANALGESICS – OPIOID 34,020 (20%) 14,062 $3,038,485
ANALGESICS - ANTI-INFLAMMATORY 22,729 (13%) 11,515 $1,988,809
MUSCULOSKELETAL THERAPY AGENTS 18,020 (11%) 8,267 $1,781,442
ANTIDEPRESSANTS 9,183 (5%) 3,506 $1,051,773
ANTICONVULSANTS 6,618 (4%) 2,889 $1,170,175
HYPNOTICS 5,123 (3%) 2,285 $602,530
ANTIANXIETY AGENTS 3,610 (2%) 1,630 $250,892
Total 170,522 57,174* $33,616,630

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N ��
perCenT of DenIeD presCrIpTIons By DenIal CoDe
presCrIpTIon year 2006
The Texas Department of Insurance, Division of Workers’ Compensation has identified the five most frequently used reasons to deny prescriptions, according to denial codes filed with the agency.
Forty percent of all prescription denials were denied based on the “unnecessary” denial code. The fee code was used 23 percent of the time, while 20 percent of the prescription bills were denied based upon the defense that the bill had not been timely filed with the carrier.
40%
23%
20%
8%
5%
0%
5%
10%
15%
20%
25%
30%
35%
40%
Unnecessary Fee Not Timely Filed Negotiated Contract Unbundling
% of Denied Prescriptions

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N�8
neW Workers’ CompensaTIon CoDes aDopTeD By aCCreDITeD sTanDarDs CommITTee
The Texas Department of Insurance, Division of Workers’ Compensation (TDI-DWC) successfully worked with the International Association of Industrial Accident Boards and Commissions (IAIABC) and the Accredited Standards Committee (ASC X12) to add or revise claim adjustment reason codes for workers’ compensation purposes. The addition and revision of codes will allow health care providers to use existing systems to electronically exchange medical bill data with insurance carriers.
Prior to the adoption of these codes, Texas insurance carriers were required to use non-standard or proprietary codes when paying or denying a medical bill. The use of these non-standard codes caused integration issues with practice management systems, code translators, and data exchanges through clearinghouses.
“The adoption of these codes by the national standard organization represents another step forward in aligning workers’ compensation requirements with those in the health care industry,” said Allen McDonald, Director of Information Management Services at TDI-DWC.
The new or revised codes are available for immediate use. TDI-DWC will remove references to the Texas specific codes from the Texas Clean Claim and eBill Companion Guides after a transition period of at least six months for any necessary adjustments to automated systems. The eight new codes and four revised codes are included in the updated code list available through Washington Publishing Company at: http://www.wpcedi. com/custom_html/claimadjustment.htm.
ASC X12 and IAIABC issued a joint press release on this matter. The release can be found at the ASC X12 website at: http://www.x12.org.
2008 quesTIon resoluTIon logs / polICy poInTs
Prepared by the Office of Policy Advisor
These answers have been reviewed by a representative of Legal Services and members of the Question Resolution Committee. As policy directives change, responses to the questions may change.
2008 Question Resolution Logs / Policy Points
# Date Received
Question / Problem
Date Answered Resolution
08-01 (Re-Address of #07-08)
08-10-07 Medical Billing for Certified Register Nurse Anesthetist (CRNA) ServicesWhich license number should be provided on the CMS 1500 when billing for Certified Registered Nurse Anesthetist (CRNA) services?
Re-Addressed 12/28/2007
The correct modifier for a CRNA and the Texas Board of Nursing registered nurse license number should be provided when billing on the CMS1500 for this type of service. Detailed formatting instructions for a clean bill can be found in the Texas Clean Claim and eBill Workers’ Compensation Companion Guide on the Division’s website: www.tdi.state.tx.us/wc/ebill/index.html#ebcg

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N ��
appeals panel DeCIsIons
no. 072129
For injuries occurring before September 1, 2003, based upon construing § 409.021(a) to require that the carrier take some action within seven days, if there is no evidence of carrier action taken (pay or dispute) within seven days from receipt of written notice of the claim, a compensable injury is defined by the information that could have been reasonably discovered by the carrier’s investigation prior to the expiration of the seven-day period.
faCTs: The carrier received written notice of a right knee injury on August 30, 1996. A medical report dated August 29, 1996, shows a right knee injury at work. Right knee x-ray on August 29, 1996, gives a conclusion of “moderate osteoarthritic changes of the right knee.” A medical report dated September 3, 1996, shows the diagnosis of “acute exacerbation of degenerative arthritis of the right knee.”
A CCH was held on the issues of whether the injury extended to and included the diagnosed of acute exacerbation of degenerative arthritis/osteoarthritis and whether the carrier waived its right to contest compensability of the injury by not timely contesting the injury. There was no evidence that the carrier took any action (pay or dispute) within seven days of receipt of written notice of this claim. The hearing officer found that carrier received written notice of the injury on August 30, 1996; that the compensable injury did not include degenerative arthritis/osteoarthritis; and that the carrier did not waive its right to contest compensability. The claimant appealed all issues. The carrier responded, urging affirmance.
HolDIng: Reversed and rendered. Under § 409.021, the Appeals Panel reversed the waiver finding and rendered a new decision that the carrier waived its right to contest compensability. Section 409.021(a), effective for a claimed compensable injury that occurred before September 1, 2003, provides that a carrier shall, not later than the seventh day after the receipt of written notice of an injury, begin the payment of benefits as required by the 1989 Act or notify the Division and the employee in writing of its refusal to pay benefits. The Appeals Panel cited to its APD 030380-s, and the Texas Supreme Court decision, Continental Casualty Company v. Downs, 81 S.W.3d 803 (Tex. 2002), for the proposition that “taking some action within 7 days is what entitles the carrier to a 60-day period to investigate or deny compensability.”
The Appeals Panel cited its prior decision APD No. 041738-s, for the proposition that when a carrier does not timely dispute the compensability, the injury is defined by the information that could have been reasonably discovered by the carrier’s investigation prior to the expiration of the “waiver” period. In this case, the Appeals Panel noted that two reports (from September 3, 1996, and the x-ray dated August 29, 1996) existed prior to the expiration of the seven-day waiver period. The Appeals Panel concluded that the carrier could have reasonably discovered in its investigation that the disputed condition was part of the claimed injury within this waiver period.

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N20
The Appeals Panel accordingly reversed the waiver finding and rendered a new decision that the carrier waived the right to contest compensability of degenerative arthritis/osteoarthritis, which the carrier could have reasonably discovered in its investigation prior to the expiration of the waiver period.
no. 072028
For purposes of filing a timely request for a BRC to dispute entitlement to SIBs, under Rule 102.3(a)(3), if the 10th day is not a working day, the period is extended to include the next day that is a working day.
faCTs: Claimant applied for the 11th quarter of SIBs. The self-insured received the claimant’s 11th quarter DWC-52, Application for SIBs, on May 31, 2007. The self-insured filed a request for a BRC on Monday, June 11, 2007. The 10th day after the self-insured’s receipt of the claimant’s 11th quarter DWC-52, was June 10, 2007, a Sunday.
At a CCH on the issues of SIBs entitlement and carrier waiver for untimely filing of BRC request, the hearing officer decided that the claimant was entitled to SIBs for the 11th quarter, and that the self-insured waived its right to dispute entitlement to SIBs for the 11th quarter by failing to timely request a BRC. The self-insured appealed the determinations of entitlement to SIBs and waiver, arguing that the request for BRC was timely filed under Rule 102.3(a)(3).
HolDIng: Affirmed in part and reversed and rendered in part. The Appeals Panel affirmed that the claimant was entitled to SIBs as supported by sufficient evidence. The Appeals Panel reversed the waiver finding. Under § 408.147(b), if a carrier fails to make a request for a BRC within 10 days after receipt of the employee’s DWC-52, the carrier waives the right to contest entitlement to SIBs and the amount of SIBs for that period of SIBs. See also Rule 130.108.
The Appeals Panel noted that under Rule 102.3(a)(3), due dates and time periods shall be computed as follows: “if the last day of any period is not a working day, the period is extended to include the next day that is a working day.” Rule 102.3(b) provides that a working day is any day, Monday-Friday, other than a national holiday as defined by the Texas Government Code, § 662.003(a) and the Friday after Thanksgiving Day, December 24th and December 26th. Use of the term day, rather than working day shall mean a calendar day.
Because the 10th day after the receipt of the claimant’s DWC-52 was Sunday, June 10, 2007, under Rule 102.3(a)(3) and (b), the last date to file a BRC request was Monday, June 11, 2007, the next working day. The appeals panel found that the hearing officer’s calculation of the 10-day deadline was incorrect and reversed the waiver determination and rendered a new decision that the self-insured did not waive the right to contest entitlement to SIBs.

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N 2�
Texas MuTual Ins. Co. v. Havard, no. 01-07000268-Cv, 2008 Wl 598347 (Tex. app.—HousTon [1sT DIsT.]
marCH 6, 2008, no peT. H.).
Where the evidence from the claimant that included a denial of ever using cocaine, expert testimony stating that the urinalysis results did not prove that he suffered from the effects of cocaine while driving, and the claimant’s description of his morning activities showed this, a reasonable fact finder could have concluded that the claimant was not intoxicated at the time of the injury. The evidence was legally sufficient to support the finding of no intoxication.
faCTs: Havard worked as a truck driver for the employer for four years. He had been randomly drug tested during his tenure and all testing had been negative. On the morning of the accident, there was evidence that the claimant inputted various numbers into a control box to enter the facility to get his load, that he maneuvered his truck on a narrow loading ramp, that he loaded asphalt, and that he completed paperwork before leaving the facility. Further a co-worker indicated that the claimant did not appear to be intoxicated when he observed him. After driving about 30 miles on the highway, the claimant lost control of his truck when he choked on his coffee. He hit a guardrail and was thrown from the truck, landing 10-15 below. He told paramedics that he had taken no-doze, ephedra, and “meth.” A urine sample taken at the hospital was positive for benzoylecgonine, which is a cocaine metabolite.
Texas Mutual thus denied its liability for any injury due to the claimant’s intoxication at the time of the injury based on Texas Labor Code § 406.032. At CCH, the hearing officer found that the claimant sustained a compensable injury and was not intoxicated at the time of the injury. The Appeals Panel affirmed the finding, and Texas Mutual took the matter into court. The trial court affirmed the ruling in favor of the claimant, and Texas Mutual appealed. One of its complaints was that the trial court failed to apply the rebuttable presumption regarding intoxication found in Texas Labor Code § 401.013(c).
HolDIng: Affirmed. The Court of Appeals noted first that findings from a bench trial have the same weight as a jury’s verdict, and if those findings are challenged, the court will review using the same standards. That is, if the appealing party attacks the legal sufficiency of an issue on which it bears the burden of proof, it must demonstrate that the evidence conclusively establishes all vital facts in support of the issue.
Workers’ compensation cases are appealed using a modified de novo review. This means that (1) the trial court is informed of the Appeals Panel decision; (2) evidence of the extent of the impairment is limited to that presented to the DWC, unless there is a finding of substantial change in condition; and (3) the court is required to adopt
Case DeCIsIons Texas CourT of appeals

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N22
the specific impairment rating arrived at by one of the doctors in the case. The court does not have to give any specific weight to the AP finding, and the fact finder does not review the AP decision for reasonableness. Instead, the fact finder is to decide the issues independently by a preponderance of the evidence.
Here, Texas Mutual had to prove by a preponderance of the evidence that the claimant was intoxicated when injured. The court’s opinion noted the standards regarding intoxication within the Labor Code. There is no specific threshold level for cocaine to show the loss of use of a person’s mental and physical faculties. However, there is a rebuttable presumption contained within the statute: “on the voluntary introduction into the body of any substance listed under Subsection (a)(2)(B), based on a blood test or urinalysis, it is a rebuttable presumption that a person is intoxicated and does not have the normal use of mental or physical faculties.” So if there is probative evidence of intoxication, the burden shifts to the employee to prove that he was not intoxicated at the time of the injury.
The court found that the record contained nothing to show that the rebuttable presumption was not applied. Instead, the court stated that a reasonable fact finder could have concluded that the claimant was not intoxicated at the time of the injury. The court concluded that the evidence was legally sufficient to support the finding of no intoxication. It stated that the evidence from the claimant that included a denial of ever using cocaine, expert testimony stating that the urinalysis results did not prove that he suffered from the effects of cocaine while driving, and the claimant’s description of his morning activities showed this.
Further, the court concluded that the evidence was factually sufficient to uphold the trial court’s decision. The claimant presented his own testimony and that of an expert. The trial court was free to accept this testimony as proof that the claimant had the normal use of his mental and physical faculties at the time of the accident.

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N 23
praCTICe poInTer general prInCIples regarDIng HealTH Care
reImBursemenT
Unless there is a contractual fee arrangement between an insurance carrier and a health care provider, or an amount specified by the Division, the insurance carrier must reimburse the provider the least of:
• The Maximum Allowable Reimbursement (MAR) amount;• The health care provider’s usual and customary charge; or• A fair and reasonable amount consistent with Division Rule 134.1 [§ 134.203(h)].
Fair and reasonable reimbursement must be consistent with reimbursement for similar procedures provided in similar circumstances, and be based on nationally recognized published studies, published Division medical dispute decisions, and values assigned for services involving similar work and resource commitments, if available [§ 413.011(d)].

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N2�
InTeresT CalCulaTor
Interest Rate Effective from 04/01/2008 through 06/30/2008: 4.82%
1 Determine number of weeks of continuous payment owed. Find corresponding “X” value on chart.
2 Multiply “X” by weekly compensation rate. This is the approximate amount of interest owed on the ending date of benefits.
3 Determine number of weeks between ending date of payments and date benefits are to be paid. Find corresponding “Y” value on chart.
4 Multiply “Y” by the total benefits owed (not including interest determined in steps 1 and 2 above). This is the approximate amount of interest owed from benefit ending date to payment date.
5 Determine total benefits plus interest owed by adding interest from steps 2 and 4, and adding total benefits to be paid.
TIBs: Calculate interest from the 7th day after first day benefits began, or the 7th day after the first notice, whichever is LATER.
IIBs: Calculate interest from the 5th day after notice of the certification of MMI and impairment, or the date of a CARRIER dispute of MMI or impairment, whichever is EARLIER.
nOTE: For partial weeks, round up to next week (8 2/7ths weeks = 9 weeks).
Accumulated Interest from Beginning to End of Continuous Payment
Accumulated Interest from End of Payment Period to Date Paid
Weeks “X” Value Weeks “X” Value Weeks “Y” Value Weeks “Y” Value1 0.0014 27 0.3499 1 0.0009 27 0.02502 0.0033 28 0.3758 2 0.0019 28 0.02603 0.0060 29 0.4026 3 0.0028 29 0.02694 0.0097 30 0.4303 4 0.0037 30 0.02785 0.0144 31 0.4590 5 0.0046 31 0.02876 0.0199 32 0.4886 6 0.0056 32 0.02977 0.0264 33 0.5191 7 0.0065 33 0.03068 0.0338 34 0.5505 8 0.0074 34 0.03159 0.0421 35 0.5829 9 0.0083 35 0.032410 0.0513 36 0.6161 10 0.0093 36 0.033411 0.0615 37 0.6503 11 0.0102 37 0.034312 0.0726 38 0.6855 12 0.0111 38 0.035213 0.0846 39 0.7215 13 0.0121 39 0.036214 0.0976 40 0.7585 14 0.0130 40 0.037115 0.1114 41 0.7964 15 0.0139 41 0.038016 0.1262 42 0.8352 16 0.0148 42 0.038917 0.1419 43 0.8750 17 0.0158 43 0.039918 0.1586 44 0.9156 18 0.0167 44 0.040819 0.1761 45 0.9572 19 0.0176 45 0.041720 0.1946 46 0.9998 20 0.0185 46 0.042621 0.2140 47 1.0432 21 0.0195 47 0.043622 0.2344 48 1.0876 22 0.0204 48 0.044523 0.2556 49 1.1329 23 0.0213 49 0.045424 0.2778 50 1.1791 24 0.0222 50 0.046325 0.3009 51 1.2262 25 0.0232 51 0.047326 0.3250 52 1.2743 26 0.0241 52 0.0482

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N 2�
flaHIve, ogDen & laTson DIreCTory
attorneys Direct Dial (512)
Direct fax*(512)
e-mail **Initials@fol. paralegal paralegal
(512)
Bobby Stokes 435-2150 867-1705 RDS Anita Drake 435-2249
Carlos Acosta 435-2177 867-1712 CA1 Alanna Bielke 435-2231
Chuck Finch 435-2158 867-1745 CCF Elizabeth Brown 435-2223
Dana Gannon 435-2151 867-1710 DMG Anita Drake 435-2249
Elizabeth Campos 435-2159 867-1715 EBC Sharissa Karol 435-2224
Greg Solcher 435-2175 867-1718 GDS Shannon Morrison 435-2298
Jack Latson 435-2156 867-1701 JWL Patsy Shelton 435-2234
James Sheffield 435-2169 867-1703 JRS Sharissa Karol 435-2224
Jeremy Lord 435-2184 867-1711 JXL Anita Drake 435-2249
Katie Flahive 435-2168 867-1702 KMF Marlyn Mueller 435-2229
Kevin MacEwan 435-2166 867-1706 KEM Cynthia Sherman 435-2274
Kevin Poteete 435-2163 867-1728 KSP Grace Guerrero 435-2242
Lynette Phillips 435-2165 867-1708 LLP Sharon Youso 435-2233
Nancy Ippolito 435-2181 867-1721 NHI Marlyn Mueller 435-2229
Paul Stone 435-2157 867-1716 PBS Karen VanLoo 435-2240
Pamela Peavy 435-2152 867-1736 PEP Shannon Morrison 43.5-2298
Rebecca Strandwitz 435-2160 867-1720 RMS Sonya Burke 435-2257
Rhett Robinson 435-2154 867-1709 SRR Cynthia Carter 435-2228
Rob Dollars 435-2164 867-1707 RAD Karen Vanloo 435-2240
Ron Johnson 435-2178 867-1745 RMJ Elizabeth Brown 435-2223
Roy Leatherberry 435-2179 867-1714 RJL Cynthia Carter 435-2228
Scott Bouton 435-2153 867-1737 SDB Cynthia Sherman 435-2274
Steve Tipton 435-2162 867-1704 SMT1 Mary Casebier 435-2275
Susan Larsen 435-2182 867-1734 SJL Alanna Bielke 435-2231
Tom Wilkins 435-2183 867-1727 TRW Sonya Burke 435-2257
Tricia Blackshear 435-2180 867-1723 PHB Sharon Youso 435-2233
*Attorney’s direct dial fax no. is directed to his/her paralegal.**Alternative e-mail address: first initial+last [email protected] (Example: [email protected])

F O L I O C L I E N T N E W S L E T T E R B Y F L A H I V E , O G D E N & L A T S O N2�
key Task DIreCTory
To help expedite your faxed information to the correct area within FO&L and get it to the responsible person at the earliest time, use the following fax directory. Please remember the 3:30 p.m. receipt deadline for material required to be date stamped at the Commission. Material received after 4:00 p.m. does not permit time to deliver it across town prior to the DWC close.
Task Contact person Direct Dial (512)
fax no.(512)
Administrative Violations – C&P Dianne Townsend 435-2289 867-1724 NRB
BRC Settings (Request For Evidence)
Cindi Friedel 435-2244 477-4987 CAF
Disputed Claims (PLns)
Request for BRC (TWCC-45)Diana Nelson 435-2237 477-4996 DMN
General Questions Receptionist 477-4405 867-1700 GQS
Insurance Coverage (TWCC-20) Patsy Shelton 435-2234 867-1701 PGS
Records Requests/Photostats Katie Jaimes 435-2220 867-1748 KEJ
Medical Dispute Resolution Katie Foster 435-2266 867-1733 KTF
Client Consultant Trina DeCecco 435-2239 867-1700 TAD
Designated Doctor Filings Brandi Senters 435-2299 479-5319 BES
TWC Manual Sales Jordan Kazmann 482-9710 472-9160 [email protected]
Flahive, Ogden & LatsonAttorneys at LawP. O. Box 13367Austin, TX 78711