Dr J King, Dr T Bracey Department of cellular pathology, Derriford Hospital May 2014.
-
Upload
felix-walton -
Category
Documents
-
view
242 -
download
0
Transcript of Dr J King, Dr T Bracey Department of cellular pathology, Derriford Hospital May 2014.

Dr J King, Dr T BraceyDepartment of cellular pathology, Derriford HospitalMay 2014

Introduction
EUS-FNA facilitates the diagnosis of medistinal lymph node disease and retropertioneal lesions
May be the only method of diagnosing pancreatic carcinomas
Go on to have major surgery

RCPath Dataset1
FNA pancreas – Aspiration of pancreatic masses
requires appropriate image guidance. An effective team including the radiology and endoscopy units is thus essential. The effectiveness of the technique is improved by immediate on site assessment of adequacy, which may be performed either by a suitably trained BMS or pathologist. Staff time spent on this activity must be included in job planning

RCPath B7 F N A of lymph node B7.1 Staffing and workload FNA of palpable lymph nodes may be
taken by a variety of clinicians, or by Cytopathologists working in a clinic setting. In this instance, medical and BMS staffing calculations must take this into account. FNA of deep nodes, e.g. Para-aortic nodes, will usually be taken under radiological control. In this instance,it is advantageous for a BMS to attend to prepare the slides and to provide an immediate assessment of adequacy

Introduction ...
Since 2011, introduced poor man cell pellet (PMCB)
Upside down universal container, formalin soaked gauze within the tube and put the sample on the inside of the lid
Formalin vapour fixes the sample overnight
Processed as histology specimen


Standard
No published standards in datasets Adequacy rate without ROSE 61%
Both mediastinal and pancreatic data2
Mediastinal range 84 – 96% With ROSE
Pancreatic range 67-86% Without ROSE

Aim
Review all PMCB cases Compare the outcome with
conventional cytology methods Provide recommendations from the
results found


Method
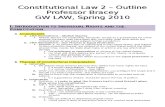
Searches on the pathology database were made: T-C4360 – mediastinal lymph node T-D3300 – mediastinum NOS T-65000 – pancreas NOS T-EA539 – pancreatic cytologic material T-65010 – pancreatic duct NOS

Method ...
Each patient was then looked up on the pathology system in order to retrieve the report.
Data from the reports were inputted into an Excel Spreadsheet
Results were analysed

Data collected:
Site of aspiration operator cytology result PMCB result If any further work was performed on
the cell pellet Date received in the department Date the report was authorised

Categories for cytology and PMCB results
Diagnosis Cytology PMCB
No sample taken C0 PM0
Inadequate C1 PM1
Benign C2 PM2
Atypical probably benign C3 PM3
Suspicious of malignancy C4 PM4
Malignant C5 PM5

Results
A total of 69 cases 13 were excluded 56 cases suitable
23 mediastinal 33 retroperitoneal
PMCB 18 mediastinal 27 retroperitoneal TAT – 2-13 days – includes weekend
days

Overall results
Of the total cytology samples, 67% were adequate (24/36)
Of the total PMCB samples, 78% were adequate (35/45)

Mediastinal casesC0 C1 C2 C3 C4 C5 Total
PM0 3 2 5
PM1 0
PM2 3 8 11
PM3 0
PM4 0
PM5 5 1 1 7
total 8 3 11 0 0 1 23

Mediastinal cases
Total 23 patients 15 had cytology 18 had PMCB 10 had both Cytology – 80% (12/15) were
adequate PMCB – 100% (18/18) were adequate
61% (11/18) benign 39% (7/18) malignant

Mediastinal results ...
One false negative C2 no overt malignant cells PM5 - metastatic moderately
differentiated intestinal type adenocarcinoma
Remaining paired results correlated No false positives


Retroperitoneal casesC0 C1 C2 C3 C4 C5 Total
PM0 1 2 3 6
PM1 4 6 10
PM2 1 1 2
PM3 1 1
PM4 1 1 1 3
PM5 5 1 1 2 2 11
total 12 9 6 2 2 2 33

Retroperitoneal cases
Total 33 patients 21 had cytology 27 had PMCB 16 had both Cytology – 57% (12/21) were
adequate PMCB – 63% (17/27) were adequate
11/27 PM5 3/27 PM4

Retroperitoneal lesions
Comparing the cytology and PMCB: Cytology – inadequate ; PM – spindle cell
GIST 2 false negatives on cytology:
C2 and PM4 – suspicious of adenocarcinoma
C2 and PM5 – well differentiated endocrine lesion
Limitation on paired samples as all of the diagnostic material may have been put into the PMCB


How many used extra tests
16 of the PMCB had extra tests Levels Special stains Immunohistochemistry

Discussion
Cytology PMCB
Overall - 61% 67% 78%
Mediastinal 84-96%
80% 100%
Pancreatic 67-86%
57% 63%
•Small numbers•We hope to add with time•Operators and pathologists are becoming more experienced

Discussion
Overall PMCB greater diagnostic rate 100% in mediastinal nodes
Ability to maintain structure in PMCB Can perform further ancillary tests to
aid diagnosis Potential all histopathologists can
report – not just cytopathologists Technique could be useful elsewhere
- EBUS

recommendations
Continue with PMCB Review SOP for handling such
specimens Liase with operators Re-audit with 2014 data

References1. RCPath . Tissue Pathways for exfoliative cytology and FNA cytology. Jan 2010
2. Rapid on-site evaluation of EUS–FNA by cytopathologist: An experience of a tertiary hospital. R. Shifa Ecka; M. Sharma. Diagnostic Cytopathology. Volume 41, Issue 12, pages 1075–1080, December 2013
3. Clinical utility of endoscopic ultrasound-guided fine-needle aspiration in the diagnosis of mediastinal and intra-abdominal lymphadenopathy. Mehmood S., Loya A., Yusuf M.A. Acta Cytologica, September 2013, vol./is. 57/5(436-442)
4. Comparison of 19- and 22-gauge needles in EUS-guided fine needle aspiration in patients with mediastinal masses and lymph nodes. Songur N., Songur Y., Bircan S., Kapucuoglu N. Turkish Journal of Gastroenterology, October 2011, vol./is. 22/5(472-478)
Utility of liquid-based cytology in the evaluation of endoscopic ultrasound guided fine needle aspiration: Comparison with the conventional smearsMoon S.-H., Seo D.W., Kim J.W., Gong G., Eum J., Song T.J., Park D.H., Lee S.S., Lee S.K., Kim M.-H. Gastrointestinal Endoscopy, April 2010, vol./is. 71/5
Rapid on-site evaluation of EUS–FNA by cytopathologist: An experience of a tertiary hospital. R. Shafia Ecka; M. Sharma. Diagnostic Cytopathology. Oct 2013

references
A 1 year audit of endoluminal ultrasound-guided fine needle aspiration cytology investigations (EUS-FNA) : Diagnostic efficacy and input of on-site cytological assessment. Hegarty S., Lioe T., Mitchell M., McNeice A., Mainie I. Gut, August 2013, vol./is. 62/(A34-A35)
What is the impact of a one-week, intensive, hands-on eus training program on tissue acquisition? Piramanayagam P., Bang J.Y., Varadarajulu S., Palaniswamy K.R. Gastrointestinal Endoscopy, May 2014, vol./Is. 79/5
Endoscopic ultrasound-guided fine-needle aspiration. KJ Chang; KD Katz; TE Durbin et al. Gastrointest Endosc. 1994; 40:694-699
Impact of on-site adequacy assessment for EUS FNA of solid pancreatic lesions. S Chatterjee.; V Wadehra; J Cunningham et al. Gut 2011 239301

Thank you