Dpp4i earlier the better ! (1)
-
Upload
faraz-farishta -
Category
Health & Medicine
-
view
42 -
download
4
Transcript of Dpp4i earlier the better ! (1)

DPP4 is: Earlier the better!DR FARAZ FARISHTA
CONSULTANT ENDOCRINOLOGISTMEDWIN HOSPITAL
MD OF SPARSH ENDOCRINOLOGY & DIABETIC CENTERSPRESIDENT OF DIABETES AWARENESS FOUNDATION
ASSISTANT PROFESSOR IN MIMS

AgendaDiabetes-Global concernChallenges associated with achieving optimal
glycemic goals Clinical inertiaConventional management approachWhat guidelines say?What DPP4 inhibitors brought?Vildagliptin efficacyVildagliptin value propositionSummary

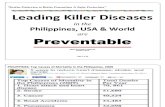
Diabetes is a huge and growing problem, and the costs to society are high and escalating
382 million people have diabetes
By 2035, this number will rise to 592 million
Ref. IDF atlas 06, 2013

Almost half of all people with diabetes live in just three countries
ChinaIndiaUSA
Ref. IDF atlas 06, 2013

| Presentation Title | Presenter Name | Date | Subject | Business Use Only
5Ref. IDF atlas 06, 2013

The ominous octet
DEFRONZO, DIABETES, VOL. 58, APRIL
2009DEFRONZO, DIABETES, VOL. 58, APRIL 2009

The natural course of HbA1c
Ferrannini et al. J Clin Endocrinol Metab 2005

Hafner SM et al. JAMA 1990;263: 2893-2898
Type 2 Diabetes is a Global Cardio-metabolic Risk (CMR)
The ticking clock

HbA1c=haemoglobin A1c.Diabetes Trials Unit. UKPDS Post Trial Monitoring. UKPDS 80 Slide Set. Available at: http://www.dtu.ox.ac.uk/index.php?maindoc=/ukpds/. Accessed 12 September, 2008; Holman RR, et al. N Engl J Med. 2008; 359: 1577–1589; UKPDS 33. Lancet. 1998; 352: 837–853.
Med
ian
Hb
A1c
(%
)
06
7
8
9
UKPDS 1998
ConventionalMetformin
Holman et al 2008
Legacy effect
1997
Difference in HbA1c was lost after first year but patients in the initial intensive arm
still had lower incidence of any complication:• 24% reduction in microvascular complications
• 15% reduction in MI• 13% reduction in all-cause mortality
2007
Achieving early glycaemic control may generate a “good legacy effect“

ADA/EASD1 AACE/ACE2 IDF3
HbA1c <7.0% (general goal)
≤6.5% <6.5%
Preprandial capillary plasma glucose
70–130 mg/dL
(3.9–7.2 mmol/L)
<110 mg/dL
(<6.0 mmol/L)
<110 mg/dL
(<6.0 mmol/L)
Peak postprandial capillary plasma glucose
<180 mg/dL
(<10.0 mmol/L)
<140 mg/dL
(<7.7 mmol/L)
<145 mg/dL
(<8.0 mmol/L)
ACE=American College of Endocrinology; ADA=American Diabetes Association; HbA1c=hemoglobin A1c; IDF=International Diabetes Federation.Adapted from: 1ADA / EASD consensus statement: Nathan DM, et al. Diabetes Care, 2009; 32:193–203;2American Association of Clinical Endocrinologists, American College of Endocrinology. Endocr Pract. 2007; 13 (Suppl 1): 3–68;3International Diabetes Federation. Global Guideline for Type 2 Diabetes. Brussels: International Diabetes Federation; 2005.
Current Treatment Goals for Glycemic Control

Challenges associated with achieving optimal glycaemic goals
2001 2002 2003 2004 2005 2006 20076.5
7.0
7.5
8.0
8.5
9.0
2001 2002 2003 2004 2005 2006 20073.5
4.0
4.5
5.0
5.5
6.0Type 1 diabetes
Type 2 diabetes + insulin
YearYear
Mean
Hb
A1c (%
)
Mean
Tch
ol
(mm
ol/
l)
In patients with type 1 diabetes or type 2 diabetes on insulin, there was a 0.1% relative improvement in HbA1c vs. improvements in total cholesterol of 15% and
29%, respectively between 2001 and 2007
Currie et al. Diabetic Medicine 2010; 27:938-948

Clinical inertia in T2DM
• Retrospective cohort study of over 80,000 people• Time to treatment intensification from first HbA1c above 7.5%, by
number of OADs and type of intensification
Khunti K, et al. Diabetes Care 1013;Epub ahead of print.
*Proportion of people with HbA1c >7.5% having any intensification to their treatment at end of follow-up according to number of OADs
Median: 1.5 years Median: >7.2 years Median: >6.1 years
Cut-off HbA1c 7.5% (58 mmol/mol)

Clinical inertia and CV events
105477 newly diagnosed T2DM (11.3% previous CVD)5.3 years median follow-up
6 month delay in first 2 years of treatment with HbA1c > 7.0%
MI Stroke HF Any CVE
All patients 1.38 (1.16-1.82)
1.07 (0.89-1.29)
1.28 (1.10-1.48)
1.25 (1.13-1.39)
No Previous CVD
1.21 (1.00-1.47)
1.07 (0.87-1.31)
1.28 (1.07-1.52)
1.20 (1.07-1.35)
Previous CVD 1.91 (1.40-2.60)
1.08 (0.73-1.61)
1.27 (0.95-1.70)
1.42 (1.15-1.75)
Paul S et al. Poster presented at EASD 2013.
Values in table correspond to HR (95% CI)

1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 166.0
6.5
7.0
7.5
8.0
8.5
9.0
9.5
Consequences of delayed intervention – Interpreting the VADT results
Time (years since diagnosis)
Hb
A1c
(%
)
Bad glycaemic“legacy”
Before entering VADT intensive treatment arm
After entering VADT intensive treatment arm
Drive risk for complications
Adapted from: Del Prato S, et al. Diabetologia 2009;52:1219-1226.

Earlier and Appropriate Intervention MayImprove Patients’ Chances of Reaching Goal
OAD=oral antidiabetic agent. Del Prato S et al. Int J Clin Pract. 2005;59:1345–1355.
Published Conceptual Approach
Hb
A1
c G
oal
Mean HbA1c
of patients
Duration of Diabetes
OAD monotherapy
Diet andexercise
OAD combination
OAD up-titration
OAD + multiple daily
insulininjections
OAD + basal insulin
Conventional stepwisetreatment approach
Earlier and more aggressive intervention approach
6
7
8
9
10

1 Gastrointestinal2 Thiazolidinedione
Adapted from DeFronzo RA. Br J Diabetes Vasc Dis. 2003;3(suppl 1):S24–S40
Conventional Oral Therapies Do Not Address the Multiple Defects in Type 2 Diabetes
Sulfonylureas
Glinides
Impaired insulinaction
Inadequate glucagon
suppression(-cell
dysfunction)
Glucoseinflux from
GI1 tract
α-Glucosidaseinhibitors
TZDs2
Metformin
Chronicβ-cell
decline
Plasma glucose and disease progression
Acuteβ-cell
dysfunction
unmet need unmet need

Metformin1
TZDs1-3
α-glucosidase inhibitors1
CHF=congestive heart failure; GI=gastrointestinal; SU=sulfonylurea; T2DM=type 2 diabetes mellitus; TZD=thiazolidinedione aRole uncertain1Inzucchi SE. JAMA. 2002; 287: 360–372; 2Avandia US Prescribing Information; 3Dormandy JA, et al. Lancet. 2005; 366: 1279–1289; 4Buse JB, et al. Diabetes Care. 2004; 27: 2628–2635; 5DeFronzo RA, et al. Diabetes Care. 2005; 28: 1092–1100; 6Kendall DM, et al. Diabetes Care. 2005; 28: 1083–1091; 7Kolterman OG, et al. Am J Health-Syst Pharm. 2005; 62: 173–181; 8Byetta US Prescribing Information.
Incretin mimetics4-8
Weight gain, edema, CHF, bone fractures (pioglitazone, rosiglitazone)
GI effects (flatulence, diarrhea)
GI effects (nausea, diarrhea), lactic acidosis (rare)
GI effects (nausea, vomiting, diarrhea), pancreatitis, hypoglycemia (in add-on to SU)
SUs1
Meglitinides1
Hypoglycemia, weight gain, hyperinsulinemiaa
Major Adverse Events of Traditional Treatments for T2DM- Limits Efficacy

What did the major guidelines say...?

Reference: A. Garber et. al., ENDOCRINE PRACTICE Vol 19 (Suppl 2) May/June 2013
AACE’ 2013 Treatment Algorithm

23
T2DM Anti-hyperglycemic Therapy: When goal is to avoid hypoglycemia
Diabetes Care, Diabetologia. 19 April 2012

24
T2DM Anti-hyperglycemic Therapy: When goal is to avoid weight gain
Diabetes Care, Diabetologia. 19 April 2012

| Presentation Title | Presenter Name | Date | Subject | Business Use Only25

Concluding remarks on guidelines
In AACE/ ACE guidelines priority has been given to Incretin based therapies most likely because of glycemic control along with added benefit like weight reduction with GLP1-RA (weight neutral with DPP4-i), and extra glycemic effects like triglyceride reduction, reduced hepatic fat and reduction in systolic and diastolic blood pressure.
In ADA/EASD 2012 guidelines : guide the clinician in choosing agents which may be most appropriate under certain situations: to avoid weight gain, to avoid hypoglycemia, and to minimize costs
Reference: Timothy Bailey, The American Journal of Medicine (2013) 126, S10-S20 Diabetes CDiabetes Care, Diabetologia. 19 April 2012 are, Diabetologia. 19 April 2012

GLP1 (7-36)agonist
DPP4 inhibition rationale in T2DM treatment
Oral glucoseor mixed
meal GLP1 (9-36)inactive
GLP1actions
>80% of total pool
Intestinal wall
Ahrén et al. Diabetes Care 2003; 26: 2860–2864;Deacon et al. Diabetes 1995;44:1126–1131;
Deacon, Holst. Biochem Biophys Res Commun 2002;294:1–4;Demuth et al. Biochem Biophys Res Commun 2002;296:229–232;
Drucker. Diabetes Care 2003;26:2929–2940
L-cell
DPP4

HGO= Hepatic Glucose OutputAdapted from Unger RH. Metabolism. 1974;23:581.
Insulin
Glucagon
IMPROVED GLYCEMIC CONTROL
Incretin Activity
Prolonged
Improved islet function
DPP-4 Inhibitor
Insulin
Glucagon
HYPERGLYCEMIA
Incretin Response Diminishe
d
Further impaired islet function
T2DM
DPP-4 Inhibition enhances the physiological effects of incretin hormones

Non Glucose dependent action of Sulphonylurea (Sus)
Glucose dependent action of
DPP4 inhibitors (DPP4i)
High risk of hypoglycemia & Beta cell stress/exhaution in Sulphonylurea
Lesser risk of hypoglycemia & Beta cell preservation in DPP4 inhibitors
The Glucose dependent action of DPP4i Vs SUs
Lesser chances of Hypoglycemia & lesser Beta cell stress

DPP4-i addresses the unmet need in the management of diabetes
Adapted from Drucker. Diabetes Care 2003;26:2929–2940
Physiological levels of GLP1 – multiple effects on plasma glucose
• Improves glucose uptake in fat andmuscle tissue
Insulinresistance
• Suppresses glucagon secretion
Inadequate glucagon
suppression (-cell dysfunction)
• Improves insulin secretion
Acuteβ-cell
function
• Increases insulinbiosynthesisa
• Promotes β-cell differentiationa
• Decreases β-cell apoptosisa
Chronicβ-cell
function
aPreclinical data.GLP1=glucagon-like peptide-1.

ED50
Insulincapacity
Glucose Concentration (mmol/L)
Insu
lin S
ecre
tory
Res
pons
e
4.5 5.0 5.5 6.0 6.5 7.0
Glucose sensitivity
Can we increaseinsulin secretion capacity?
Short-term effect
Increasedglucosesensitivity
Glucose-dependent stimulation ofinsulin secretion
No danger ofhypoglycemia
ED50
Insulincapacity
Effect of GLP-1 on Insulin Response to Glucose in Patients with T2DM
ED50=effective dose at 50%; GLP-1=glucagon-like peptide-1; T2DM=type 2 diabetes mellitus.Holst JJ. Diabetes Metab Res Rev. 2002;18:430–441;Zander M, et al. Lancet. 2002;359:824–30.

Sustainability of β-cell Function: No sustainability of Glycemic Control with Sulfonylureas
DeFronzo (Diabetes 2009; 58:773-795)
ADA/EASD Algorithm: • As the progressive decline in beta cell function is a key factor limiting long-term glycaemic
control, more consideration should be given to drugs with beta cell-preserving properties
Schernthaner G et al Diabetologia (2010) 53:1258–1269

Sustainability of β-cell Function :Vildagliptin versus glimepiride over 2 years
33
Initial response was defined as a reduction from baseline in HbA1c ≥0.5% or a HbA1c ≤6.5% during the first 6 months of treatment. Sustainability was defined as the time (in days) from initial response (when the patient reached their lowest HbA1c level within the first 6 months), until an increase of >0.3% above that initial response was detected.
Vildagliptin Glimepiride250
260
270
280
290
300
310
320
309
270
Mean Sustainability of Initial Response
(IR) in days
Day
s
Mathews etal, Diabetes, Obesity and Metabolism 12: 780–789, 2010

* * *
0 12 24 52
Time (Week)
* * †
0 12 24 52
Time (Week)
pm
ol/
L 3
0 m
in/(
mm
ol/
L)
0 12 24 52
Time (Week)
* *
mL
· m
in-1 ·
m -2
0.050
0.040
0.045
0.025
0.030
0.035
300
250
275
200
225
14
10
12
6
8
InsulinSecretio
n
Insulin Sensitivit
y
Adaptation
Index
Effects of vildagliptin treatment on -cell function and insulin sensitivity over 52 Weeks
Patients on Stable Metformin Therapy
*P <0.05 vs placebo; †P <0.01 vs placebo.Adapted from Ahrén B, et al. Diabetes Care. 2005; 28: 1936–1940.
Vildagliptin 50 mg daily / metformin
Placebo / metformin
nm
ol C
-pe
pti
de ·
mm
ol g
luc
os
e-1 ·
m
L-1 ·
m-2

Efficacy as Monotherapy compared to Metformincomparable efficacy at 2 yrs
At 1 yr (52 weeks) At 2 yrs (104 weeks)
Intention-to-treat population.*Non-inferiority end point not met, confidence interval = 0.28–0.65 (non-inferiority margin is defined by confidence interval upper limit of 0.4%).*Not non-inferior; **P <0.001 vs metformin (Fisher’s exact test). Schweizer A, et al. Diabet Med. 2007; 24: 955–961. Göke B, et al. Horm Metab Res. 2008; 40: 892–895.

Rationale for the fixed dose combination of vildagliptin plus metformin used as initial therapy
1. The Mechanistic Rationale –
• Vildagliptin offers a clinically important outcome when added to metformin with a twice daily dose regimen, taking advantage of its tight binding and slow dissociation characteristics that lead to a sustained overnight effect
• Synergistic Effect – Higher intact GLP-1 levels with combination
2. The Clinical Rationale –
• Equivalent or superior HbA1c lowering without the GI tolerability issues associated with higher doses of metformin
• Comparable overall tolerability profile and low risk of hypoglycaemia
3. The Compliance Rationale • Single pill Combination tends to improve patient compliance.

Initial combination of Vildagliptin + MetforminEffective across the hyperglycemia spectrum
37

Preferred term, %
Mono vilda
n=297
Mono met
n=295
Low-dose vilda + met
n=290
High-dose vilda + met
n=292
Diarrhoea 2.4 11 7.2 6.5
Headache 5.4 4.5 6.2 5.5
Nasopharyngitis 3.7 4.8 5.5 7.5
Dizziness 2.7 4.1 4.8 5.1
Nausea 2.4 5.8 4.8 6.5
Pain in extremity 1.7 2.4 3.1 1.4
Upper respiratory tract infection 3.4 2.7 3.1 1.4
Fatigue 2.0 5.1 2.4 2.4
Dyspepsia 1.0 1.7 2.1 3.4
Asthenia 1.3 1.4 1.4 3.1
Cough 2.7 3.1 1.4 1.7
Vomiting 0.3 2.4 1.4 3.1
Back pain 2.0 3.8 1.0 3.8
Hypertension 2.4 3.4 1.0 2.1
Abdominal pain 2.0 3.4 0.7 0.7
Constipation 3.4 1.7 0.7 2.1
High-dose vildagliptin + metformin (50/1000 mg bid); low-dose vildagliptin + metformin (50/500 mg bid).Met=metformin; vilda=vildagliptin. Data on file, Novartis Pharmaceuticals, LMF237A2302.
Initial Combination of Vildagliptin + Metformin:incidence of AEs > in any group

Vildagliptin in combination with insulin
42
40% fewer incidences of hypoglycemia, no severe hypoglycemia
BL=baseline; HbA1c=hemoglobin A1c. *P <0.001; **P <0.05 between groups.Fonseca V, et al. Diabetologia. 2007; 50: 1148–1155.

43
Vildagliptin role in hypoglycemia situations – emerging data
43

44
Possible mechanism for low risk of hypoglycemia

Response to meal (−80%)
0
400
600
1000
Response to hypoglycemia (+38%)
200
0
40
60
Placebo
10Glu
cag
on
ΔA
UC
0-12
0 (
ng
/L*m
in)
VildagliptinPlacebo
*
800
20
30
50
Δ g
luca
go
n (
ng
/L)
**
Vildagliptin
Vildagliptin inhibits glucagon at high glucosebut increases glucagon at low glucose
*P=0.025; **P=0.039
Ahrén, et al. J Clin Endocrinol Metab 94:1236, 2009

Vildagliptin has specific role at low glucose
IncreasedGIP levels
Increased glucose sensitivity in islet
α- and β-cells
Potential mechanisms to Mitigate the risk of Hypoglycaemia

Insulin Glucagon
↑ Insulin secretion ↓ Glucagon at high glucose
↑ Glucagon at low glucose
GLP-1
GIP ()
Vildagliptin increases both GLP-1 and GIP and therefore lowers glucose with low risk of hypoglycemia
GLP-1 and GIP: dual effects on islet hormone secretion

Cardio Vascular
Renal
Elderly
Fasting Patients
Vildagliptin – Safety

Odds ratio [95% CI]
p-value
Major CV event1 0.71 [0.59, 0.86] < 0.001
Acute MI 0.64 [0.44, 0.94] 0.023
Stroke 0.77 [0.48, 1.24] 0.29
Mortality 0.60 [0.41, 0.88] 0.008
CV mortality 0.67 [0.39, 1.14] 0.14
Meta-analysis of 70 short- and medium-term trials, with 41,959 patients and mean follow-up of 44.1 weeks
DPP4 inhibitor better
Comparator better
Cardiovascular Safety:In a large meta-analysis of CV events, DPP-4is were better than the comparator in terms of CV safety
AMI, acute myocardial infarction; CV, cardiovascular; DPP4i, dipeptidyl peptidase-4 inhibitors; MACE, major CV events; MH–OR, Mantel–Haenzel odds ratio.1.Analysis of MACE as serious adverse events supports the safety of DPP4 inhibitors, but does not demonstrate their efficacy in reducing CV risk ion a long-term basis.Monami M, et al. Diabetes Obes Metab. 2013;15:112–120.
0.0 1.0 10.0

53
Cardiac safety: Vildagliptin vs Competition
Monami et al, Diabetes, Obesity and Metabolism 15: 112–120, 2013
Benefit was only significant with Vildagliptin and Saxagliptin
Significant (p=0.005) 39% reduction in MACE with Vildagliptin

SAVOR-TIMIPrimary End-point: Composite of CVD death, MI or ischemic stroke
Secondary end-point: Primary + hospitalisation for unstable angina, coronary revascularization or HF
Scirica BM et al. N Engl J Med 2013. DOI: 10.1056/NEJMoa1307684
16,492 T2DM with CVD or at riskSaxagliptin vs placeboMedian follow-up 2.1 years
More patients on saxagliptin had hospitalisation with HFHR 1.27 (95% CI 1.07 to 1.51)

Placebo + Current therapy
Vildagliptin (50 mg qd2 or bid3) + Current therapy
Run-in Double-blind Treatment
52 weeks2 weeks
Screening Randomization
Stable dose of current therapy1
● This was a multi-center, randomized, double-blind clinical trial to evaluate the safety of vildagliptin versus placebo when given as monotherapy or as add-on therapy to other anti-diabetic drugs for 52 weeks in patients with T2DM and CHF (NYHA class I-III).
Stratification occurred at Visit 2 for baseline CHF status (NYHA class I, II or III) 1Patients remained on their current anti-diabetic therapy (for at least 8 weeks prior to Visit 1 and on a stable dose for at least 4 weeks prior to Visit 1).
2Patients who were taking background sulfonylurea therapy were instructed to take one tablet (vildagliptin 50 mg or vildagliptin 50 mg matching placebo) before the breakfast meal every day.
3Patients who were not taking background sulfonylurea therapy were instructed to take one tablet (vildagliptin 50 mg or vildagliptin 50 mg matching placebo) before breakfast and one tablet before the evening meal every day.
N=128
N=126
CHF, congestive heart failure; NYHA, New York Heart Association; T2DM, type 2 diabetes mellitus.
Vildagliptin In Ventricular Dysfunction Diabetes Study

PPS: †p=0.667 (95% CI=-2.21, 3.44); FAS ‡p=0.670 (95% CI=-1.97, 3.06). Indicates non-inferiority to comparator at the 2.5% alpha level. Non-inferiority margin is -3.5. FAS, full analysis set; LVEF, left ventricular ejection fraction; PPS, per protocol set.Study 23118, Novartis Data on file, CSR Table 11-6.
Primary endpoint: Change in LVEF from baseline to Week 52 endpoint
.
VildagliptinPlaceboBetween-treatment difference
Full analysis setPer protocol set
N= 89 90 N= 114 111

*p=0.04, indicates statistical significance at 5% level. #Full analysis set. BL, baseline.Study 23118, Novartis Data on file, CSR Table 11-8.
-0.4
-0.3
-0.2
-0.1
0
0.1
0.2
-0.21
0.15
-0.36*
Ad
jus
ted
me
an
(S
E)
ch
an
ge
in H
bA
1c
, %
N = 115 107BL = 7.8 7.8
Strictly Confidential. Proprietary information of Novartis. For internal use ONLY.
Secondary endpoint: Change in HbA1c from baseline to rescue-censored 52 week endpoint#
VildagliptinPlaceboBetween-treatment difference

Similar incidence of SAEs, discontinuations due to AEs, or death for vildagliptin and comparators
n (%)Vilda
50 mg bidN=6116
Total comparators
N=6210
Any AE 4225 (69.1) 4228 (69.0)
Drug-related AEs 961 (15.7) 1349 (21.7)
SAEs 545 (8.9) 557 (9.0)
Discontinuation of study drug due to AEs 347 (5.7) 400 (6.4)
Deaths 24 (0.4) 23 (0.4)
AEs=adverse events; bid=twice daily; PBO=placebo; SAEs= serious adverse events; vilda=vildagliptin.All-study safety (excluding open-label) population.Schweizer A. et al, Vasc Health Risk Manag 2011(accepted version)

Renal safety of Vildagliptin- 1 year dataSignificant HbA1c reduction
• 1 year safety study adding Vildagliptin 50mg od to background therapy in those with moderate or severe renal failure
• Better HbA1c reduction of 0.6% and 0.8% with Vildagliptin in moderate and severe RI respectively
Kothny et al. Diabetes Obesity Metabolism,2012

No deterioration of renal function with vildagliptin
Renal impairment Moderate Severe
eGFR (MDRD) (mL/min/1.73 m2) Vilda 50mg qd
N=163PlaceboN=129
Vilda 50mg qdN=124
PlaceboN=97
Mean Baseline 39.3 40.3 21.9 20.9
Mean Change from baseline 0.865 0.572 -1.456 -1.121
Median Change from baseline -0.068 -0.067 -1.291 -1.872
Estimated *GFR (MDRD) in patients with severe and moderate RI at 24 wks
* eGFR (MDRD)= GFR estimated using the MDRD formula. Baseline eGFR is defined as the lowest of eGFR (MDRD) values before visit 2 that were calculated using the
serum creatinine value before visit 2 and the age at the associated creatinine measurement date
• The overall incidences of AEs, SAEs, discontinuations due to AEs and deaths were comparable between vildagliptin 50 mg qd and placebo
treatment groups
• No statistically significant or clinically relevant differences for events of identified risk observed for vildagliptin
MDRD = Modification of Diet in Renal DiseaseLukashevich et al. Diabetes Obesity Metabolism,2011

Mechanistic basis of Vildagliptin in T2DM patients with renal impairment
Yan –Ling He-Int J Clin Pharmacol Ther. 2013; 51:693–703
Only ~23% of vildagliptin is excreted unchanged by kidney (main excretion mode is hydrolysis to inactive metabolite)
In Mild/Moderate/severe : similar and minimal increase in Cmax
In moderate and severe RI: 1.7~2 fold increase in exposure of vildagliptin(AUC0-24hrs)
Doubling of exposure (AUC) but no expected increased in concentration (Cmax) in Moderate/Severe RI
Effectively with vildagliptin in RI there is,
• Reduced dose frequency, dose strength unchanged, maintained 24-hour DPP4 blockage (50 mg once daily Vildagliptin in
moderate/severe RI = 50 mg twice daily Vildagliptin in normal renal function)
• A1c reductions with 50 mg OD similar to reduction with 50 mg BD with normal renal function
• 50% reduced therapy cost
In patients with moderate-severe RI with vildagliptin,
How does Vildagliptin add value in terms of Renal safety to T2DM patients
Reduce dose frequency by half

65
Summary and Take Home Messages
• Tight glycaemic control should be targeted from the day of diagnosis
• Intensive glycaemic control:
Reduces risk of micro-vascular complications
Some benefit in reducing cardiovascular events
No reductions in mortality
Clinical inertia a major issue in achieving tight targets
DPP-4 inhibitors are an important therapy option as reflected by current guidelines and clinical evidence
• Vildagliptin is efficacious, weight neutral, with a low risk of hypoglycaemia as monotherapy, and in combination with other anti-diabetic agents including metformin.

66

67
Thank You

Basic Succinct Statement - GALVUS®
Presentation: Tablets containing 50 mg of Vildagliptin.
Indications: ♦Galvus is indicated as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus (T2DM). It is indicated: as monotherapy, IN COMBINATION: with metformin, when diet, exercise and metformin alone do not result in adequate glycemic control. with a sulphonylurea (SU), when diet, exercise and a SU alone do not result in adequate glycemic control. with a thiazolidinedione (TZD), when diet, exercise and a TZD alone do not result in adequate glycemic control. IN TRIPLE COMBINATION: with a sulphonylurea and metformin when diet and exercise plus dual therapy with these agents do not provide adequate glycemic control.
♦Galvus is also indicated in combination with insulin (with or without metformin) when diet, exercise and a stable dose of insulin do not result in adequate glycemic control. ♦Galvus is also indicated as initial combination therapy with metformin in patients with T2DM whose diabetes is not adequately controlled by diet and exercise alone.
Dosage and administration: ♦Adults: The recommended dose is 50 mg or 100 mg daily for monotherapy, and for combination with metformin, with a TZD or with insulin (with or without metformin); 50 mg daily in combination with a SU; 100 mg daily for triple combination with metformin and a SU. Maximum dose is 100 mg/day (in two divided doses of 50 mg).♦Children (under 18 years of age): Not recommended. ♦Special population: In patients with moderate to severe renal impairment or End Stage Renal Disease (ESRD), the recommended dose is 50 mg once daily.
Contraindications: Hypersensitivity to vildagliptin or to any of the excipients.
Warnings and precautions: ♦Galvus should not be used in patients with type 1 diabetes or for the treatment of diabetic ketoacidosis. ♦Not recommended in patients with hepatic impairment including patients with a pre-treatment ALT or AST>2.5X the upper limit of normal. Liver function tests (LFT) to be performed prior to treatment initiation, at three-month intervals during the first year and periodically thereafter. Withdrawal of therapy with Galvus recommended if an increase in AST or ALT of 3X upper limit normal or greater persist. Following withdrawal of treatment with Galvus and LFT normalisation, treatment with Galvus should not be reinitiated. ♦Clinical experience in patients with NYHA functional class III treated with vildagliptin is still limited and results are inconclusive. ♦Not recommended in patients with NYHA Class IV.
Women of child-bearing potential, pregnancy: Should not be used during pregnancy unless the potential benefit justifies the potential risk to the fetus.
Breast-feeding: Should not be used.
Special excipients: Contains lactose
Adverse reactions: Rare cases of angioedema. Rare cases of hepatic dysfunction (including hepatitis) ♦Monotherapy - Common: dizziness - Uncommon: headache, constipation, oedema peripheral. ♦Combination with metformin - Common: tremor, dizziness, headache. ♦Combination with a sulphonylurea - Common: tremor, headache, dizziness, asthenia. ♦Combination with a thiazolidinedione - Common: weight increase, oedema peripheral. ♦Combination with insulin - Common: headache, nausea, gastrooesophageal reflux disease, chills, decreased blood glucose – Uncommon: Diarrhoea, flatulence. ♦Combination with metformin and a sulphonylurea - Common: dizziness, tremor, asthesia, hypoglycaemia, hyperhidrosis. ♦Post-marketing experience - Rare: hepatitis (reversible with drug discontinuation) – Unknown: urticaria, pancreatitis, localized exfoliation or blisters.
Interactions: ♦Vildagliptin has a low potential for drug interactions. ♦No clinically relevant interactions with other oral antidiabetics (glibenclamide, pioglitazone, metformin), amlodipine, digoxin, ramipril, simvastatin, valsartan or warfarin were observed after co-administration with vildagliptin.
Packs: Box of 2 strips of 14 tablets each
Note: Before prescribing, please consult full prescribing information available from Novartis Healthcare Private limited, Sandoz House, Dr. Annie Besant Road, Worli, Mumbai- 400 018, Tel: 022 2495 8888
For the use only of a registered medical practitioner or a hospital or a laboratory.
India BSS dtd 27 Jan 2014 based on international BSS dtd 18 Dec 2013

Basic Succinct Statement – GalvusMet®
Presentation: Tablets containing Vildagliptin/Metformin hydrochloride fixed dose combination: 50 mg/500 mg, 50 mg/850 mg, 50 mg/1,000mg.
Indications: ♦Galvus Met is indicated as an adjunct to diet and exercise to improve glycemic control in patients with type 2 diabetes mellitus (T2DM) whose diabetes is not adequately controlled on metformin hydrochloride or vildagliptin alone or who are already treated with the combination of vildagliptin and metformin hydrochloride, as separate tablets. ♦Galvus Met is indicated in combination with a sulphonylurea (i.e., triple combination therapy) as an adjunct to diet and exercise in patients inadequately controlled with metformin and a sulphonylurea. ♦Galvus Met is indicated in combination with insulin (i.e., triple combination therapy) as an adjunct to diet and exercise to improve glycemic control in patients when stable dose of insulin and metformin alone do not provide adequate glycemic control. ♦ Galvus Met is also indicated for the treatment of Type 2 Diabetes mellitus having HbA1c > 8% where diabetes is not adequately controlled by diet and exercise alone.
Dosage and administration: ♦Do not exceed the maximum recommended daily dose of vildagliptin (100 mg). ♦Should be given with meals. ♦Adults: Starting dose for patients inadequately controlled on vildagliptin or metformin hydrochloride monotherapy: 50 mg/500mg twice daily and gradually titrated after assessing adequacy of therapeutic response. ♦Starting dose for patients switching from combination therapy of vildagliptin plus metformin hydrochloride as separate tablets: 50 mg/500 mg, 50 mg/850 mg or 50 mg/1,000 mg based on the dose of vildagliptin or metformin already being taken. ♦Starting dose for treatment naïve patients: may be initiated at 50 mg/500 mg qd and gradually titrated to a maximum dose of 50 mg/1,000 mg bid after assessing adequacy of therapeutic response. ♦Use in combination with a sulphonylurea or with insulin: the dose of Galvus Met should provide vildagliptin dosed as 50 mg twice daily (100 mg total daily dose) and a dose of metformin similar to the dose already being taken. ♦Children (under 18 years of age): Not recommended.
Contraindications: Known hypersensitivity to vildagliptin or metformin hydrochloride or to any of the excipients ♦renal disease or renal dysfunction ♦congestive heart failure ♦acute or chronic metabolic acidosis including diabetic ketacidosis with or without coma ♦should be temporarily discontinued in patients undergoing radiologic studies involving intravascular administration of iodinated contrast materials.
Warnings and precautions: ♦Risk of lactic acidosis. ♦Monitoring of renal function. ♦Caution with concomitant use of medications that may affect renal function or metformin hydrochloride disposition. ♦Should be temporarily discontinued in patients undergoing radiologic studies involving intravascular administration of iodinated contrast materials. ♦Discontinue treatment in case of hypoxemia. ♦Temporary discontinuation in patients undergoing surgical procedure. ♦Excessive alcohol intake to be avoided. ♦Not recommended in patients with hepatic impairment including patients with a pre-treatment ALT or AST >2.5X the upper limit of normal. Liver function tests (LFT) to be performed prior to treatment initiation, at three-month intervals during the first year and periodically thereafter. Withdrawal of therapy with Galvus Met recommended if an increase in AST or ALT of 3X upper limit normal or greater persist. Following withdrawal of treatment with Galvus Met and LFT normalisation, treatment with Galvus Met should not be reinitiated. ♦Risk of decreased vitamin B12 serum levels. ♦Should not be used in patients with type 1 diabetes or for the treatment of diabetic ketoacidosis. ♦Risk of hypoglycemia. ♦May be temporarily withheld in case of loss of glycemic control. ♦Should only be used in elderly patients with normal renal function. ♦Not recommended in pediatric patients.

Women of child-bearing potential, pregnancy: Should not be used in pregnancy unless the potential benefit justifies the potential risk to the foetus.
Breast-feeding: Should not be used during breast-feeding.
Adverse reactions:
♦Vildagliptin: Rare cases of angioedema. Rare cases of hepatic dysfunction (including hepatitis). ♦Vildagliptin monotherapy - Common: dizziness – Uncommon: headache, constipation, oedema peripheral. ♦Metformin monotherapy – Very common: loss of appetite, nausea, vomiting, diarrhoea, abdominal pain. Common: dysgeusia. Very rare: lactic acidosis, hepatitis, skin reactions such as erythema, pruritus and urticarial, decrease of vitamin B12 absorption, liver function test abnormalities. ♦Other effects with combination of Vildagliptin and Metformin - Common: tremor, dizziness, headache. ♦Other effects with combination of Vildagliptin and Metformin with insulin – Common: headache, nausea, gastrooesophageal reflux disease, chills, blood glucose decreased– Uncommon: diarrhoea, flatulence. ♦Other effects with combination of Vildagliptin and Metformin with a sulphonylurea – Common: dizziness, tremor, asthenia, hypoglycemia, hyperhidrosis. ♦Post-marketing experience: - Rare: hepatitis (reversible with drug discontinuation) - Unknown: urticaria, pancreatitis, localized exfoliation or blisters.
Interactions: ♦Interactions with Vildagliptin: low potential for drug interactions, no clinically relevant interactions with other oral antidiabetics (glibenclamide, pioglitazone, metformin), amlodipine, digoxin, ramipril, simvastatin, valsartan or warfarin were observed after co-administration with vildagliptin. ♦Interactions with metformin hydrochloride: furosemide, nifedipine, cationic drugs, drugs tending to produce hyperglycemia, alcohol.
Packs: Box containing 6 strips of 10 tablets each
Note: Before prescribing, consult full prescribing information available from Novartis Healthcare Private Limited, Sandoz House, Dr. Annie Besant Road, Worli, Mumbai- 400 018, Tel: 022 2495 8888
For the use only of a registered medical practitioner or a hospital or a laboratory.
India BSS dtd 31 Jan 2014 based on international BSS dtd 18 Dec 2013, effective from 1 Apr 14.
2/2
Basic Succinct Statement – GalvusMet®

DisclaimerThe views, opinions, ideas etc expressed therein are solely those of the author. Novartis does not certify the accuracy, completeness, currency of any information and shall not be responsible or in anyway liable for any errors, omissions or inaccuracies in such information. Novartis is not liable to you in any manner whatsoever for any decision made or action or non-action taken by you in reliance upon the information provided. Novartis does not recommend the use of its products in unapproved indications and recommends to refer to complete prescribing information prior to using any of the Novartis products.”
Issued in scientific service to medical professionals
For full product information please write to :
Novartis Healthcare Private Limited,
Sandoz House, 7th floor,
Shivsagar Estate, Dr. Annie Besant Road,
Worli, Mumbai, 400 018, INDIA
ScientificPresentation/Galvus/CVM/279309/Aug/2014I
For use of RMP, hospital or lab only