Download poster (PDF)
Transcript of Download poster (PDF)

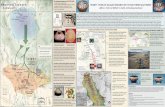
ME THODS
Clinical setting: This observational study took place on a 22-bed critical care unit (CCU).
Study design and duration: This was a comparative e!ectiveness evaluation comparing devices used for heel o"oading in CCU patients with a Braden Scale Score of <10. The evaluation started 11/03/11 and ended 11/30/11.
Device comparisons: Nurses di!erentiated between the two heel protector devices by blue or black color. Each patient received a blue heel protector on one foot and a black heel protector on the other foot.
Surveys and definitions: Nursing sta! was provided a 6-question survey, on which they were asked to circle the preferred device (circle blue heel protector or black heel protector) or declare a neutral opinion. Nurses were trained on appropriate completion of the survey, and questions were as follows:
Question 1: Which of the heel protectors remained on the limb in proper position throughout your shift? • All nurses were trained on application of each heel protector, and hands on application and competency testing demonstrated proper position.
Question 2: Which of the heel protectors e!ectively o"oaded your patient’s heel throughout your shift? • All nurses were trained in appropriate heel o"oading in Skin Management Classes associated with competency testing. Question 3: Which of the heel protectors prevented external rotation of the limb more e!ectively. • Prevention of external rotation is a basic evidence-based nursing skill and is associated with competency testing. Question 4: Which heel protector repelled moisture more e!ectively? • All nurses were trained through a hands-on demonstration of the e!ect of the amount of moisture on the materials of the boots.
Question 5: Which of the heel protectors was compatible with sequential compression device (SCD) tubing? • All nurses were trained on the appropriate application of the heel protector in conjunction with SCDs. The definition of “compatible” was based on the absence of excess pressure associated with application of the heel protector and SCD device at the same time.
Question 6: Which of the heel protectors provided the greatest clinical advantage to prevent heel breakdown? • “Greatest clinical advantage to heel breakdown prevention” was based on the nurse’s opinion after using both devices.
Data collection: Throughout the comparative e!ectiveness evaluation, the following information was collected: patient demographics; Braden Scale score; Braden Subscale scores; number of vasopressor agents. Patient skin observations were made twice daily, throughout the duration of the patient’s length of stay.Prevalon® Pressure Relieving Heel Protector with Integrated Foot and Leg Stabilizer Wedge (Sage Products Inc, Cary, IL) HEELMEDIX ™ Heel Protector (MEDLINE, Mundelein, Illinois)
RESULTS
A total of 15 patients were treated in the CCU with heel protectors during the comparative e!ectiveness evaluation. Patient demographics and information are shown in Table 1. The average age of all patients was 56.2 years of age, with 10 males and 5 females, and an average Braden Scale Score of 9. Of 61 nurses surveyed, 100% returned their surveys. Survey responses are presented in Figure 1, demonstrating the majority of nurses surveyed preferred the blue heel protector to the black heel protector.
DISCUSSION
This comparative e!ective evaluation revealed the majority of nurses preferred the blue heel protector over the black heel protector, although a small percentage remained neutral on product selection.
A review of patient demographics and clinical data revealed the patient population was considered extremely high risk for pres-sure-related breakdown, with an average Braden Scale Score of 9. All patients had a Braden Subscale activity score of 1, placing them at high risk for breakdown over bony prominences due to prolonged pressure, friction and shear. On average, patients were receiving 1 or more vasopressors, a known independent risk factor for skin breakdown.4,5 These risk factors are associated with an MICU patient population at high risk for developing hPU. Clinical e!ectiveness evaluations, which are conducted using “head-to-head” comparisons within the clinical environment, are helpful in making product selections that can impact patient outcomes and aid in cost-e!ectiveness analyses.12
REFERENCES 1. Keller P, Wille J, van Ramshorst B, van der Werken C. Pressure ulcers in intensive care patients: a review of risks and prevention. Intensive Care Med. 2002;28(10):1379-1388.2. Shahin ES, DassenT, Halfens RJ. Pressure ulcer prevalence in intensive care patients: a cross-sectional study. J Eval Clin Prac. 2008;14:563-568.3. VanGilder C, Amlung S, Harrison P, Meyer S. Results of the 2008-2009 International Pressure Ulcer Prevalence Survey and a 3-year acute care, unit-specific analysis. Ostomy Wound Manage. 2009;55(11):39-45.4. Cox J. Predictors of pressure ulcers in adult critical care patients. Am J Crit Care. 2011;20(5):364-755. Nijs N, Toppets A, Defloor T, Bernaerts K, Milisen K, Van Den Berghe G. Incidence and risk factors for pressure ulcers in the intensive care unit. J Clin Nurs. 2009;18(9):1258-666. Agency for Healthcare Research and Quality. Statistical Brief #64 - Hospitalizations Related to Pressure Ulcers among Adults 18 Years and Older, 2006. Available at: www.hcup-us.ahrq.gov/reports/statbriefs/sb64.pdf7. Young ZF, Evans A, Davis J. Nosocomial pressure ulcer prevention: a successful project. J Nurs Adm. 2003 Jul-Aug;33(7-8):380-38. Federal Register Tuesday, August 19, 2008, Part II Department of Health and Human Services: Centers for Medicare & Medicaid Services, 42 CFR Parts 411, 412, 413, 422, and 489, pg 484739. Padula WV, Mishra MK, Makic MB, Sullivan PW. Improving the quality of pressure ulcer care with prevention: a cost-e!ectiveness analysis. Med Care. 2011 Apr;49(4):385-9210. European Pressure Ulcer Advisory Panel and National Pressure Ulcer Advisory Panel. Prevention and treatment of pressure ulcers: quick reference guide. Washington DC: National Pressure Ulcer Advisory Panel; 2009.11. Salcido R, Lee A, Ahn C. Heel pressure ulcers: purple heel and deep tissue injury. Adv Skin Wound Care. 2011 Aug;24(8):374-80; quiz 381-2.12. Sox HC, Goodman SN. The Methods of Comparative E!ectiveness Research. Annu Rev Public Health. 2011 Apr 4. [Epub ahead of print] [reference: Salcido R, Lee A, Ahn C. Heel Pressure Ulcers: Purple Heel and Deep Tissue Injury. Adc in Skin and Wound Care 2011; 24 (8): 374-380.]. A comparative e!ectiveness evaluation was conducted to assess the opinions of nurses on the clinical e!ectiveness of two heel protectors in a critical care patient population.
BACKGROUND
Patients who are critically ill are at an increased risk for developing pressure ulcers, with ICU incidence rates ranging from 14 to 42%.1-3 Due to the bony prominences associated with the heel, it is one of the primary anatomical locations for PU development in the critical care population.2
Predictors for pressure-related breakdown in critically ill patientsinclude, but are not limited to,friction/shear, immobility, adminis-tration of vasopressors, and vascular disease.4,5
The development of hPU is associated with increased morbidity and extended length of stay.6 The economic costs associated with hPU ranges from $2,000 to $43,180 for more advanced ulcer stages.7,8 Although the direct and indirect costs associated with hospital-acquired pressure ulcers (HAPU) are di#cult to ascertain, a recent cost-e!ec-tiveness analysis which measured cost per quality-adjusted life-years gained for HAPU prevention reported, “It is more cost e!ective to pay for HAPU prevention compared with standard of care.” 9
E!ective prevention of hPU in critically ill patients requires multiple interventions,10 one of which is heel o"oading with a device that maintains grip of the limb.11 A comparative e!ectiveness evaluation was conducted to assess the opinions of nurses on the clinical e!ectiveness of two heel protectors in a critical care patient population.
Heel Pressure Ulcer Prevention: A Comparative E!ective EvaluationJoanne McGovern BSN, RN, CCRN; Judith A DiPerri MSN, RN, BC, CWOCN
Figure 1. Results of Nursing Surveys (N=61)
Table 1. Patient Demographics and Clinical Information
* Neutral may be interpreted as either not applicable or equivalent
*