DL n Interpret Unisma 2014
-
Upload
edwin-pasha-jr -
Category
Documents
-
view
11 -
download
1
description
Transcript of DL n Interpret Unisma 2014
-
Maimun ZA/ Agustin IskandarLaboratorium Patologi Klinik FK UB/RSUD dr. Saiful Anwar Malang
*
-
COMPLETE BLOOD COUNT Consists of series of tests:HemoglobinHematocritMean corpuscular volume (MCV)Mean corpuscular hemoglobin (MCH) Mean corpuscular hemoglobin concentration (MCHC)Red blood cell distribution width (RDW)White blood cells countRed blood cells countPlatelets countReticulacytes countErithrocyte sedimentation rate Blood smear evaluation
Complete Blood count
*
-
The hemoglobinHemoglobin (Hb) is the life-giving substance of every red cell, the oxygen-carrying component of the red cell. Each red blood cell is nothing more than a fluid-filled sac, with the fluid being hemoglobin. In 4 months, or 120 days, red cells with normal hemoglobin content submit to the rigors of circulation.Molecule consists of two primary structures:
Heme portion & globin portion*
*
-
HemoglobinThe Hemoglobin concentration (Hb) of a solution may be estimated by measurement of its:Color, ex:
- Hb Sahli - Cyanmethaemoglobin (internationally recommended method)Power of combining with oxygen and carbon monoxide impractical for routine purposesIron content impractical
*
-
Hematocrit/Packed CellVolume (PCV)As a simple screening test for anemiaThe hematocrit X 1000 is about 3 times the hemoglobin expressed in g/l
*
-
Hematocrit is the volume of erythrocytes expressed as a percentage of the volume of whole blood in a sample. The venous hematocrit agrees closely with the hematocrit obtained from a skin puncture; both are greater than the total body hematocrit. *
*
-
Principle: A small tube (Wintrobe tube) filled with blood and sealed at one end is centrifuged at high speed in a centrifuge. The height of the resulting column of red cells is measured, and calculated as a fraction of the height of the entire column of blood.
*
-
*Erythrocyte index
*
-
*
*
-
Red Cell Distribution Width (RDW)Examination of erythrocyte volume heterogenity, reflect the range of erythrocyte shape.Normal Range = 11.6 to 14.6 %Correlates with the degree of anisocytosis.May differentiate thalassemia from iron deficiency.
*
-
Erythrocyte sedimentation rate (ESR)
The erythrocyte sedimentation rate (ESR) is the rate at which red blood cells precipitate in a period of 1 hour. When anticoagulated blood is allowed to stand undisturbed for a period of time, the erythrocytes tend to sink to the bottom. Two layers are formed, the upper plasma layer and the lower one of red blood cells.
*
-
Test based on: inflammatory and necrotic processes cause an alteration in blood proteins aggregation of RBCs heavier and more likely to fall rapidly Referance values:
Men : 0-15 mm/h Women : 0-20 mm/h Child : 0-10 mm/hIncreased by any cause: acute and chronic inflammation, including infections, cancers, and autoimmune diseases
Erythrocyte sedimentation rate
*
-
LeukocyteWhite cell counts that are reported on the CBC are
directly counted from an automated instrument or by manual method. The age of the patient directly influences whether this number is within or outside of the reference range. Pediatric reference ranges show more variability than do ranges for adults. Some of the peculiarities of the newborn include highest white counts at 3 months.
*
*
-
*Table 1. Leukocyte counts at the different ages
*
-
Abnormal White Blood Cell Count
Leukocytosis (abnormally high count). This may be caused by: a. Systemic or local infections (usually due to bacteria). These counts are highly variable and not diagnostic. b. Dyscrasia of blood-forming tissues. This is not caused by any known bacteria, but is due to a malfunctioning of the marrow and lymph tissues,resulting in extremely high white cell counts, which sometimes exceed 1,000,000/mm3. This is commonly known as leukemia*
*
-
*Table 2.Manual differential reference range for adults and infantsType of the Leukocytes
*
-
*
-
Eos*
-
BasophilIn circulation basophil only 0.5 - 1% of all leukocytes. In allergic condition, their granules are broken, substances that trigger allergic reaction are released into circulation.Basophilia (increased basophil) occurs in:Chronic myelocytic leukemia (CML)Policythemia veraMyelofibrosis
*
*
-
The basophil population increase in case of: Acute basophilic leukaemia CML
Basophilia
*
-
EosinophilThe percentage of eosinophil in circulation is 1-3% of leukocytes. Increasing number occurs in allergic condition, Hodgkins disease, worm infestation and CML. Eosinophil plays an important role in relieving allergic reaction by means of neutralizing active substances excreted by mast cell.
*
*
-
The eosinophil population increase in case of: Paracytic infection: Ankylostomiasis, ascariasis, Oxyure, Taenia... Allergic disease: rhinitis, asthma, urtikaria, eczema... Malignancy: Lymphoma, CML, Chronic eosinophilic leukemia
Eosinophilia
*
-
NeutrophilNeutrophil is the most abundant leukocyte in circulation and bone marrow. Neutrophilic series: myeloblast, promyelocyte, myelocyte, metamyelocyte, stab and segmented neutrophil. The ability to proliferate only till myelocyte, while in stab and segmented neutrophil the maturation is completed. Normally, in circulation is only found stab and segmented neutrophilThe normal range of absolute neutrophil value in adult is 2,500 7,000/L or 50 - 70% in differential counting.
*
*
-
*Table 3. The causes of neutrophlia and neutropenia
NeutrophiliaNeutropenia Bacterial infectionInflammation processCMLSuddent bleedingPost splenectomyCorticosteroid treatmentPregnancyAplastic anemia Post radiationHypersplenismLupus erythromatosusRheumatoid arthritis Cytostatic drugsViral diseases
*
-
LymphocytosisLymphocytosis is a feature of certain infections, particularly infections in children. It may be especially marked in pertussis, infectious mononucleosis, cytomegalovirus infection, infectious hepatitis, tuberculosis, and brucellosis. Lymphocytosis is also a common transient reaction to severe physical stress. Elderly patients with lymphoproliferative disorders, including chronic lymphocytic leukaemia and lymphomas
*
*
-
Monocytosis A slight to moderate monocytosis may be associated with some protozoal, rickettsial, and bacterial infections including malaria, typhus, and tuberculosis.High levels of monocytes (monocyte count >1 109/l) in an elderly patient suggest chronic myelomonocytic leukaemia or, sometimes, atypical chronic myeloid leukaemia. Because these conditions fall into the myeloproliferative/myelodysplastic group of disorders
*
*
-
Platelets Platelets are small fragments of cytoplasm derived from megakaryocytes. On average they are 1.53.5 m in diameter but may be larger in some disease states. They do not contain a nucleus and are bounded by a typical lipid bilayer membrane. Beneath the outer membrane lies the marginal band of microtubules, which maintain the shape of the platelet and depolymerise when aggregation begins.
*
*
-
The central cytoplasm is dominated by the three types of platelet granules: the granules, granules, and lysosomal granules.Platelets are not complete cells, but actually fragments of cytoplasm from megakaryocyte. Platelets play a vital role in blood clotting. Normal range varies slightly between laboratories but is in the range of 150,000 to 400,000/cmm (150 to 400 x 109/liter).
*
*
-
Normal platelets populationThrombopoesis
*
-
Platelet aggregates
Optical detection
*
-
MacroplateletsMacroplatelet detection
*
-
Reticulocyte The reticulocyte count is the most effective means of assessing red cell generation or response to anemia.Reticulocytes are red cells that are nonnucleated and that contain remnant RNA material, reticulum. Reticulum cannot be visualized by Wrights stain
*
*
-
Erythropoesis - ReticulocytesReticulocyte Count = 0.5 to 2.5 %
*
-
Anemia diagnosis:
micro-macrocytic anemia regenerative or non regenerative anemiaperipheral or central anemia Post chemotherapy follow up Bone marrow regeneration follow up Dialysis disease follow up: EPO treatment
Reticulocytes pathologies
*
-
Morphologic changes of erythrocyte
Hemoglobin level abnormalitiesNormochrome: 1/3 centre area of erythrocytes looks pale (central pallor area). This occurs in normal erythrocyte.Hipochrome: More than 1/3 centre area of erythrocyte looks pale, reflected by decreased of MCH level.Annulocyte: Central pallor area of erythrocyte is very wide, like ring. Hipochrome erythrocyte and annulocyte can occur in severe Fe deficiency anemia and thalassemia.
*
*
-
2. Size abnormalitiesNormocytic: normal size, similar to nucleus of the small lymphocyte.Macrocytic, if the size of erythrocyte bigger than normal, reflected by increased of MCV level. Macrocytic erythrocyte can be found in megaloblastic anemia, reticulocytosis, and liver disease.Microcytic, if the size of erythrocyte smaller than normal, reflected by decreased of MCV level. Microcytic erythrocyte can be found in Fe deficiency anemia, thalassemia, and hereditary spherocytosis. Anisocytosis, if the size of erythrocyte vary from small to large. This condition is reflected by increased RDW
*
*
-
3. Shape abnormalityThe shape of normal erythrocyte is biconcave-disc. Poikilocyte, if erythrocyte has vary in shape.Spherocyte, if erythrocyte is small, round, and darker than normal color, like marble. This cell occurs in hereditary spherocytosis and autoimmune hemoytic anemia (AIHA).Schistocyte or fragmentocyte. Abnormal shape, maybe triangle, boat, or helmet cell. These erythrocytes can be found in thalassemia, microangioapthy hemolytic, and disseminated intravascular coagulation (DIC).
*
*
-
Crenation, erythrocyte like durian fruit. This cell is artefact because of blood smear is not immediately dry. Burr cell, erythrocyte with short protusions. It can be found in uremia and carcinomatosis.Tear drop cell, erythrocyte like tear drop. It occurs in myelofibrosis and thalassemia.Target cell: erythrocyte likes arrow target board. It occurs in liver disease, thalassemia, and HbC disease.Cigar cell: erythrocyte like cigar. It occurs in Fe deficiency
*
*
-
4. Inclusion bodiesHowell-Jolly: blue, single or double inclusion, usually inside the erythrocyte, about 1 . It is the remnant of erythrocyte nucleus. Often it is present after splenectomy.Heinz: refractile, 1-2 , in the edge of erythrocyte, easy to observe on supravital stain using methyl-violet. It is origin from polimerization and precipitation of denaturated hemoglobin molecule. It occurs in G6PD deficiency, HbF, and post splenectomy.Basophilic stippling: color drops in erythrocyte. It occurs in lead intoxication and thalassemia.
*
*
-
5. OthersRouleaux phenomena: Erythrocytes agregate similar to stack of coin, resulting from paraprotein in the blood. This condition occurs in myeloma multiple and Waldenstorms disease.Autoagglutination: The clump of erythrocytes on the counting area of blood smear. It occurs in AIHA.
*
*
-
Normochrome-normocyticAnisocytosisAniso-poikilocytosisMacro-ovalocytes
*
-
Spherocyte Cigar cell Target cellsTear drop cell
*
-
HipochromeHipochrome-microcyticOvalocytosisStomatocyte
*
-
Basophilic stipplingP. falciparumGamet P. falciparumNormoblast
*
-
Auto agglutinationRouleaux phenomena
*
-
Anemia There are many causes of anemia, and a logical classification would be according to mechanism: Decreased productionReduced lifespan of red cellsBlood lossSplenic pooling
*
*
-
In practice, if the cause is not readily apparent from the clinical circumstances and an automated blood count is available, classification according to cell size is more practicable. The choice of further investigations is then guided by the mean cell volume (MCV) and red cell morphology in addition to clinical features. Anemia is thus broadly divided into three types: Microcytic (low MCV)Macrocytic (high MCV)Normocytic (normal MCV)
*
*
-
Erythrocytosis Increases in red cells may be one of the following: Relative (pseudopolycythaemia) owing to reduced plasma volumePrimary (polycythaemia vera) as part of the spectrum of myeloproliferative disordersSecondary to chronic hypoxia (e.g., chronic lung disease, congenital heart disease, high-affinity haemoglobins) or aberrant erythropoietin production
*
*
-
Thrombocytopenia Frequent causes of spurious thrombocytopenia include blood clots in the sample, platelet aggregation, and platelet satellitism. Platelet aggregation, which can be seen on the blood film, may occur in vitro as the result of a temperature-dependent or anticoagulant-dependent autoantibody. Small platelet aggregates are also seen in slides that have been made directly from a fingerprick sample
*
*
-
True thrombocytopenia is most frequently the result of anticancer chemotherapy, HIV infection, autoantibodies [(immune thrombocytopenia (ITP), other drugs (such as thiazide diuretics), alcohol excess, hypersplenism, and MDS (in the elderly)].
*
*
-
ThrombocytosisThrombocytosis is often associated with infectious and inflammatory conditions such as osteomyelitis and rheumatoid arthritis. Hematological causes of thrombocytosis include chronic blood loss, red cell destruction, splenectomy, and rebound following recovery from marrow suppression. Under these circumstances, a moderately increased platelet count (e.g., 400800 109/l) does not usually have any pathological consequences.
*
*
-
Primary (essential) thrombocythaemia belongs to the spectrum of myeloproliferative diseases and is characterized by a persistently high platelet count (often arbitrarily defined as greater than 600 109/l) and thrombotic or haemorrhagic complications.
*
*
-
Giant thrombocytesThrombocytosis
*
-
Pancytopenia Pancytopenia (reduction in the white cell count, Hb, and platelet count) is most often the result of anticancer chemotherapy, HIV infection, hypersplenism, folic acid/vit B12 deficiency, aleukemic leukemia, MDS, and bone marrow infiltration or failure. Careful examination of a blood film is important if the reason for the pancytopenia is not apparent from the clinical history. If this does not reveal the cause, bone marrow aspiration and trephine biopsy may be needed.
*
*
-
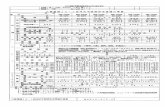
The CBC tests are done by some modern Hematology AutoanalysersABX Pentra DF 120 22 parameters/ 1 minuteSysmex XT-2000i 25 parameters/ 1 minute
*
-
The Complete blood count result by hematology autoanalyser
*
-
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*Eos*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*
*