Dislocation of patella
-
Upload
orthoprince -
Category
Business
-
view
696 -
download
2
Transcript of Dislocation of patella

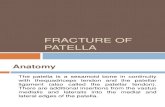
Dislocation of Patella

• Largest sesamoid bone• Thick articular cartilage
proximally• Articular surface
divided into medial and lateral facets by a longitudinal ridge
• Distal pole nonarticular• The patella lies within
the fascia lata and the fibers of the quadriceps tendon

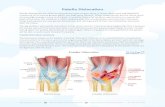
Extraosseous and Intraosseous vascular systems The primary blood supply to the patella is from a dorsal
arterial ring derived from branches of the geniculate anastomotic system around the knee
The arterial ring is made up of a central superior geniculate vessel; medial, lateral superior, and lateral inferior geniculate vessels; and an inferior recurrent tibial vessel
The primary intraosseous blood supply of the patella enters the bone by vessels through the middle of the anterior portion of the body of the patella and through the distal pole vessels
Arterial Blood Supply

The patellar retinaculum derives from the deep investing fascia lata in combination with the aponeurotic fibers from the vastus medialis and vastus lateralis
The retinaculum inserts directly into the proximal tibia Contributions from the lateral aspect of the vastus
lateralis, iliotibial tract, and patellofemoral ligaments of the joint capsule help to complete the retinaculum
The patella tendon originates at the apex of the patella and inserts into the tibial tubercle
The patella retinaculum and the iliotibial track fibers blend into the patella tendon at the insertion on the anterior portion of the proximal tibia.
Anatomy of soft tissue


PATELLA CAN BE DISPLACED UPWARDS-PATELLA ALTA
DOWN WARDS-PATELLA INFERA LATERAL MEDIAL LATERAL COMMON, ALL OTHES RARE

LATERAL DISLOCATION IS THE MOST LIABLE TO RECURRENT DISLOCATION/HABITUAL DISLOCATION.
MORE COMMON IN FEMALES Q ANGLE-MALES 8-10 FEMALES 15 FACTORS THAT INCREASE Q ANGLE CAUSE
RECURRENT PATELLAR DISLOCATION

The Q(quadriceps) angle is measured from the anterior superior iliac spine through the patella and to the tibial tubercle
Q angle

Subluxation or dislocation of the patellofemoral joint most commonly occurs secondary to a rotational or twisting injury with simultaneous contraction of the quadriceps.
Less commonly glancing blows to the knee can cause dislocation of the patella
Mechanism of Injury

Increased Q angle (laterally inserted patellar tendon, excessive tibial external rotation or genu valgum, femoral anteversion or internal rotation)
Patella alta Insufficient lateral trochlea or shallow
patellofemoral groove Vastus medialis atrophy Insufficient medial patellofemoral ligament Genu recurvatum or patellar hypermobility
Predisposing abnormalities

Severe pain, deformity of the anterior knee and flexed position is characteristic of an acutely dislocated patella
Palpation will reveal the abnormal position of the patella
Patellofempral crepitus is palpable Wasting of quadriceps and vastus medialis Frequently patella reduces spontaneous When the patella is reduced by the knee being
straightened manually by an observer, usually a loud pop or crack is noted with significant improvement in pain
Signs and Symptoms

Examination of the reduced patellar dislocation reveals a large effusion and medial patellar tenderness
Occasionally a defect in the medial retinaculum can be palpated
Flexion is limited due to the medial soft tissue injury and the presence of the large effusion
Usually tenderness + in the area of the superior medial pole of the patella

Palpation of the undersurface of the patella and the lateral femoral condylar edge are helpful in identifying an acute osteochondral fracture
In the presence of a loose articular piece > mechanical locking symptoms
With a recurrent patellar dislocation or subluxation, the swelling and pain are usually less than those of the first injury

Anteroposterior, tunnel, lateral and axial patellofemoral views (most commonly the technique of Merchant)
Bilateral views
Radiographic Evaluation

Tunnel views – evaluating loose bodies that can come to lie in the femoral notch
Anteroposterior views – evaluation of patellar shape, partition and evidence of fracture
Lateral view – determination of patellar height, fractures and patellofemoral arthritic changes
Axial views (sunrise view) – evaluating intraarticular fractures, trochlear position of the patella, patellofemoral arthritis and avulsion injury of the medial patellofemoral ligament

Evaluation of patellar height for recognition of patella alta or infera is routinely performed on a lateral view
Insall and Salvati A ratio is measured between the length of the
patella and that of the patellar tendon On average the ratio of LT/LP is 1.02 with a
standard deviation of 0.13 A ratio of 0.80 or less > patella infera, >1.20
patella alta


Conservative management should be used when possible and includes maintenance of quadriceps strength, functional retraining and control of swelling and pain
Surgical techniques should be used for chronic patellar problems only after conservative treatment has failed over a significant time period usually 4 to 6 months
Methods of Treatment

Closed reduction can be performed Extensor mechanism integrity evaluated Quality of reduction assessed Intraarticular fragments looked for
Asymmetrically subluxed or tilted patella or evidence of an intraarticular fragment are indications for operative treatment with repair of the medial patellofemoral ligament, lateral release and removal or internal fixation of the osteochondral fragment
Acute Dislocation

Non Operative treatment includes casting in extension for 6 weeks and early range of motion exercises with functional rehabilitation

LATERAL RETINACULAR RELEASE PROXIMAL EXTENSOR REALIGNEMENT DISTAL EXTENSOR REALIGNMENT PROXIMAL AND DISTAL REALIGNEMENT PATELLECTOMY WITH EXTENSOR
REALIGNEMENT DURING ALL SURGICAL PROCEDURES
THOROUGH LOOK OF ARTICULAR SURFACE NECCESARY

Surgical repair involves EUA followed by a thorough evaluation of the articular surfaces to rule out a chondral or osteochondral fracture
Small patellar fragments should be debrided Large fragments or those that involve the
femoral weight-bearing surface should be reduced and fixed using biodegradable implants
Repair of the medial patellofemoral ligament and torn retinaculum
Overtensioning may cause medial subluxation of the patella

Indications for a lateral release involve preexisting tilt, increased Q angle and lateral patellar subluxation

Thank You















![Total Knee Arthroplasty in a Patient with Neglected ... · Congenital dislocation of patella can be associated with Down’s syndrome, skeletal and cardiac anomalies[1].Total knee](https://static.fdocuments.in/doc/165x107/60362f97798cc36dd262a92a/total-knee-arthroplasty-in-a-patient-with-neglected-congenital-dislocation-of.jpg)
