Digoxin and ouabain induce the efflux of … and heart...Digoxin and ouabain induce the efflux of...
Transcript of Digoxin and ouabain induce the efflux of … and heart...Digoxin and ouabain induce the efflux of...

Biochem. J. (2012) 447, 301–311 (Printed in Great Britain) doi:10.1042/BJ20120200 301
Digoxin and ouabain induce the efflux of cholesterol via liver X receptorsignalling and the synthesis of ATP in cardiomyocytesIvana CAMPIA*, Valentina SALA†, Joanna KOPECKA*, Christian LEO†, Nico MITRO‡, Costanzo COSTAMAGNA*,Donatella CARUSO‡, Gianpiero PESCARMONA*§, Tiziana CREPALDI†, Dario GHIGO*, Amalia BOSIA*§ and Chiara RIGANTI*§1
*Department of Genetics, Biology and Biochemistry, University of Torino, via Santena 5/bis, 10126 Torino, Italy, †Department of Anatomy, Pharmacology and Forensic Medicine,University of Torino, corso Massimo D’Azeglio 52, 10126 Torino, Italy, ‡Department of Pharmacological and Biomolecular Sciences, University of Milano, via Balzaretti 9, 20133Milano, Italy, and §Research Center on Experimental Medicine (Ce.R.M.S.), University of Torino, via Santena 5/bis, 10126 Torino, Italy
Cardioactive glycosides exert positive inotropic effects oncardiomyocytes through the inhibition of Na+ /K+ -ATPase. Weshowed previously that in human hepatoma cells, digoxinand ouabain increase the rate of the mevalonate cascade andtherefore have Na+ /K+ -ATPase-independent effects. In thepresent study we found that they increase the expression andactivity of 3-hydroxy-3 methylglutaryl-CoA reductase and thesynthesis of cholesterol in cardiomyocytes, their main targetcells. Surprisingly this did not promote intracellular cholesterolaccumulation. The glycosides activated the liver X receptortranscription factor and increased the expression of ABCA1 (ATP-binding cassette protein A1) transporter, which mediates the effluxof cholesterol and its delivery to apolipoprotein A-I. By increasing
the synthesis of ubiquinone, another derivative of the mevalonatecascade, digoxin and ouabain simultaneously enhanced the rateof electron transport in the mitochondrial respiratory chain andthe synthesis of ATP. Mice treated with digoxin showed lowercholesterol and higher ubiquinone content in their hearts, anda small increase in their serum HDL (high-density lipoprotein)cholesterol. The results of the present study suggest thatcardioactive glycosides may have a role in the reverse transportof cholesterol and in the energy metabolism of cardiomyocytes.
Key words: ATP-binding cassette protein A1 (ABCA1),cholesterol, digoxin, liver X receptor, ubiquinone.
INTRODUCTION
Cardioactive glycosides are used in the treatment of atrialfibrillation and chronic heart failure. Owing to their inhibitionof Na+ /K+ -ATPase (EC 3.6.3.9), they increase the intracellularconcentration of Na+ , decrease the extrusion of Ca2 + viathe Na+ /Ca2 + exchanger and exert a positive inotropic effectin cardiomyocytes [1]. They also exert effects independentlyof Na+ /K+ -ATPase inhibition [2,3], in that they control thetranscription of specific genes [4] and modulate the synthesisof steroid hormones [5,6]. In human hepatoma cells, we observedthat digoxin and ouabain increased the synthesis of cholesterol byup-regulating both the activity and the expression of HMGCR (3-hydroxy-3-methylglutaryl-CoA reductase) (EC 1.1.1.34), whichis the rate-limiting enzyme of the mevalonate pathway. This eventwas mediated by the activation of the SREBP (sterol-regulatory-element-binding protein)-2 and of the SCAP (SREBP-cleavage-activating protein) [7].
The mevalonate pathway mediates the synthesis of sterols,such as cholesterol, and non-sterol isoprenoid metabolites, whichare incorporated in the tail of ubiquinone. Both cholesteroland ubiquinone have critical roles in cardiovascular disease[8,9]. Ubiquinone (or CoQ10), the electron shuttle betweenNADH dehydrogenase (Complex I, EC 1.6.5.3), or succinate-CoQ reductase (Complex II, EC 1.3.5.1), and ubiquinol-cytochrome c reductase (Complex III, EC 1.10.2.2) [10], isnecessary for mitochondrial respiration and ATP synthesis.Ubiquinone is lower in the cardiomyocytes of patients with
ventricular dysfunction [11] and low serum levels of ubiquinoneare predictive of higher mortality in chronic heart failure [12].Dietary supplementation with CoQ10 has improved systolicfunction and haemodynamic parameters in those patients [13].
Modulating the synthesis of cholesterol and ubiquinone in car-diomyocytes might thus have important implications on cardiacmetabolism and function. Since digoxin and ouabain activate themevalonate pathway in liver cells [7], we set out to investigatewhether they may also affect the levels of cholesterol andubiquinone in cardiomyocytes, the main targets of this class ofdrugs.
EXPERIMENTAL
Materials
FBS (fetal bovine serum) and culture medium were supplied byBioWhittaker; plasticware for cell cultures was from Falcon.Mevastatin was purchased from Calbiochem. Electrophoresisreagents were obtained from Bio-Rad Laboratories. Digoxin,ouabain, zaragozic acid and the BCA (bicinchoninic acid) kitfor protein measurement were from Sigma. When not otherwisespecified, all of the other reagents were purchased from Sigma.
Cells
H9c2 cells, a rat cardiomyocyte cell line which expresses α1, α2and α3 subunits of Na+ /K+ -ATPase (Supplementary Figure S1
Abbreviations used: ABC, ATP-binding cassette; ABCA1, ABC protein A1; apoA-I, apolipoprotein A-I; DR-4, direct repeat response element-4; EMSA,electrophoretic mobility-shift assay; FBS, fetal bovine serum; GAPDH, glyceraldehyde-3-phosphate dehydrogenase; HDL, high-density lipoprotein;HMGCR, 3-hydroxy-3-methylglutaryl-CoA reductase; HMGCS, 3-hydroxy-3-methylglutaryl-coA synthase; LDH, lactate dehydrogenase; LDL, low-densitylipoprotein; LXR, liver X receptor; LXRE, LXR response element; RT-PCR, real-time PCR; RXR, retinoid X receptor; SR-BI, scavenger receptor class B,type I; SREBP, sterol-regulatory-element-binding protein.
1 To whom correspondence should be addressed (email [email protected]).
c© The Authors Journal compilation c© 2012 Biochemical Society

302 I. Campia and others
at http://www.BiochemJ.org/bj/447/bj4470301add.htm), was cul-tured in Dulbecco’s modified Eagle’s medium containing10% (v/v) FBS (Sigma), 1 % (v/v) penicillin/streptomycinand 1% (v/v) L-glutamine. The culture medium contained32 μg/ml cholesterol, 8 μg/ml HDL (high-density lipoprotein)cholesterol, 13 μg/ml LDL (low-density lipoprotein) cholesteroland 55 μg/ml triacylglycerols. Total cholesterol, HDLcholesterol and triacylglycerols were measured with theOSR6516, OSR6187 and OSR61118 kits respectively (OlympusSystem Reagent), using an Olympus Analyzer spectrophotometer(Olympus Europa Holding). The results were calculatedaccording to the titration curve of each kit. LDL cholesterol wascalculated with the Friedewald formula.
Measurement of cholesterol and ubiquinone de novo synthesis
The de novo synthesis of cholesterol and ubiquinone wasmeasured by radiolabelling cells with 1 μCi/ml [3H]acetate(3600 mCi/mmol; Amersham GE Healthcare, Piscataway,NJ), or with 1 μCi/ml [14C]mevalonic acid (67 mCi/mmol;Amersham GE Healthcare), as reported in [7]. Cholesterol andubiquinone synthesis was expressed as fmol of [3H]cholesterolor [14C]cholesterol/106 cells and as fmol of [3H]ubiquinone/106
cells, according to the titration curves. For the cholesteroltitration curve, a stock solution of [3H]cholesterol (1 mCi/ml,7 Ci/mmol, PerkinElmer) or [14C]cholesterol (0.04 mCi/ml,60 mCi/mmol) was serially diluted and counted by liquidscintillation. The radioactivity (c.p.m.), subtracted from theradioactivity of the blank (distilled water), was related tothe concentration of each solution, yielding a specific activityof 5852 c.p.m./pmol for [3H]cholesterol and 130 c.p.m./pmolfor [14C]cholesterol. In the absence of commercially available[3H]ubiquinone, the titration curve was performed by incubating106 cells for 24 h with 0.25, 0.5, 0.75 or 1 μCi/ml [3H]acetate.The lipids were extracted and separated by TLC. The spotcorresponding to ubiquinone was isolated and the amount of[3H]ubiquinone was quantified by liquid scintillation. The assaywas linear between 0.25 and 1 μCi/ml (Supplementary Figure S2at http://www.BiochemJ.org/bj/447/bj4470301add.htm), whichfalls in the range of [3H]ubiquinone recovered from H9c2 cellsradiolabelled with [3H]acetate.
Cytotoxicity assays
The release of LDH (lactate dehydrogenase) in the extracellularmedium, a marker of cell damage, and the positivity to annexinV–FITC, a marker of apoptosis, were measured as reportedpreviously [7].
Measurement of HMGCR activity and expression
The activity and expression of HMGCR were measured inmicrosomal fractions collected by centrifugation of cell lysatesat 40000 rev./min in an optima L-90K Beckman Coulterultracentrifuge using a 70.1 Ti rotor for 1 h (4 ◦C), as describedpreviously [7].
RT-PCR (real-time PCR)
Total RNA was extracted with TRIzol® (Invitrogen); a 5 μgportion was reverse-transcribed by 200 units of M-MLV (Moloneymurine leukaemia virus) enzyme (Invitrogen). Quantitative RT-PCR was carried out using IQTM SYBR Green Supermix (Bio-RadLaboratories), according to the manufacturer’s instructions. Therelative quantification of each sample was performed comparing
the PCR products of each gene with the housekeeping geneproduct (actin), with the iQTM 5 Optical System Software (Bio-Rad Laboratories). Results were expressed in arbitrary units. Foreach gene, the expression in untreated cells was considered to be‘1’. Primers sequences are shown in Supplementary Table S1 athttp://www.BiochemJ.org/bj/447/bj4470301add.htm.
Isolation of mitochondria and measurement of Complex I–IIIactivity
The activity of ubiquinone-dependent and ubiquinone-independent Complex I–III was measured on non-sonicatedextracted mitochondria as previously reported [14].
ATP detection assay
The ATP level in mitochondria was measured with the ATPBioluminescent Assay Kit (Sigma), using a Magic Lite Analyzer(Ciba Corning Diagnostic). ATP was quantified as arbitrary lightunits and converted into nmol of ATP per mg of mitochondrialproteins, according to a calibration curve set earlier.
Cholesterol loading and spectrophotometric measurement ofintracellular cholesterol
The cholesterol loading was performed by preparing cholesterol–β-methyl-cyclodextrin complexes as described previously [7].The amount of intracellular cholesterol was measured in celllysates with the OSR6516 kit. The results were expressed as μgof cholesterol per mg of cell proteins.
Measurement of extracellular cholesterol
The amount of cholesterol in the cell culture medium aftercholesterol loading was measured spectrophotometrically bymeans of the OSR6516 kit.
To evaluate cholesterol efflux, cells were incubated with1 μCi/ml [3H]cholesterol for 1 h, washed five times with PBSand grown in fresh medium for 24 h. The cell culture mediumwas collected, cholesterol was extracted in methanol/hexane andresolved by TLC [7]. The amount of [3H]cholesterol recoveredwas quantified by liquid scintillation. In parallel, intracellular[3H]cholesterol was measured in cell lysates. The ratio betweenextracellular [3H]cholesterol and total [3H]cholesterol wascalculated as c.p.m. in medium/(c.p.m. in medium + c.p.m. incells) [15].
To measure the efflux of cholesterol derived from endogenoussynthesis, cells were incubated for 24 h with 1 μCi/ml[3H]acetate, then the cholesterol in the cell culture medium wasextracted and the amount of [3H]cholesterol was quantified asreported above. For both labelling assays, the [3H]cholesterol wasexpressed as pmol/106 cells, according to the titration curve.
Western blot analysis
Cells were lysed in sample buffer [25 mM Hepes/KOH,pH 7.5, 135 mM NaCl, 1% (v/v) Nonidet P40, 5 mM EDTA,1 mM EGTA, 1 mM ZnCl2, 50 mM NaF and 10% (v/v)glycerol] supplemented with protease inhibitor cocktail setIII (Calbiochem), 2 mM PMSF and 1 mM Na3VO4. A 25 μgportion of proteins from whole-cell lysates was separated bySDS/PAGE and probed with the following antibodies: anti-ABCA1 [ABC (ATP-binding cassette) protein A1] (Abcam),
c© The Authors Journal compilation c© 2012 Biochemical Society

Digoxin induces cholesterol efflux and ATP synthesis 303
anti-ABCG1 (Santa Cruz Biotechnology), anti- SR-BI (scavengerreceptor class B, type I) (Novus Biologicals), anti-LXR(liver X receptor) β (Abcam), anti-LXRα (Abcam) and anti-GAPDH (glyceraldehyde-3-phosphate dehydrogenase) (SantaCruz Biotechnology), followed by the secondary peroxidase-conjugated antibody (Bio-Rad Laboratories). Proteins weredetected by enhanced chemiluminescence (PerkinElmer).Densitometric analysis of Western blots was performed usingImageJ software (http://rsb.info.nih.gov/ij/).
Flow cytometry analysis
Cells were washed with PBS, detached with cell dissociationsolution (Sigma), fixed with 0.2 ml of 2 % (w/v) paraformalde-hyde, rinsed with 0.25% PBS-BSA and incubated for 45 min at4 ◦C with the anti-ABCA1 antibody (Abcam). After two washesin PBS-BSA, cells were incubated for 30 min at 4 ◦C withan anti-(rabbit FITC)-conjugated antibody, then washed againand resuspended in PBS-BSA. Control experiments includedincubation with non-immune isotypic antibody, followed by thesecondary antibody. Samples were analysed with a FACS-Caliburflow cytometer (Becton Dickinson), using a 530 nm band-passfilter. For each analysis, 100000 events were collected andprocessed with Cell Quest software (Becton Dickinson).
EMSA (electrophoretic mobility-shift assay)
The probe containing the DR-4 (direct repeat response element-4) for LXR, validated with Genomatix Software (http://www.genomatix.de/; Munich, Germany), was: 5′-GCGACCCCAGTG-ATATCCCGTCGTC-3′. The putative DR-4 site is underlined.The probe was labelled with 50 μCi of [γ -32P]ATP (3000Ci/mmol; Amersham Bioscience), using a T4 polynucleotidekinase (Roche). A total of 10 μg of proteins from nuclearextracts were incubated for 20 min at 4 ◦C with the 32P-labelledprobe, as described previously [7]. As a control of specificity,nuclear extracts from cells stimulated with the LXR activatorTO-901317 were incubated with a mutated labelled probe (5′-GCGACCTATTGTATATCTGTTCGTC-3′) or with the wild-typelabelled probe plus a 100-fold excess of wild-type unlabelledprobe. The DNA–protein complex was separated on a non-denaturing 4% polyacrylamide gel, then the gel was dried andautoradiographed after 72 h.
Chromatin immunoprecipitation
Cells were rinsed with fixation buffer [500 mM Hepes/KOH,pH 7.9, 100 mM NaCl, 1 mM EDTA, 0.5 mM EGTA and 11%(v/v) formaldehyde], washed twice with PBS, centrifuged for5 min at 1000 g at 4 ◦C and resuspended in lysis buffer [50 mMTris/HCl, pH 8.0, 5 mM EDTA and 1 % (w/v) SDS]. Aftersonication (five pulses of 10 s at a power setting of 10, usinga SONOPULS Bandelin instrument), a 200 μl volume of eachsample was taken as input. The remaining lysates were pre-treated for 2 h at 4 ◦C with Protein G–Sepharose magnetic beads(Invitrogen), then divided into three portions (incubated withanti-LXRβ or anti-LXRα, with generic IgG or without anyantibody respectively) and immunoprecipitated overnight at 4 ◦C.The recovered DNA was washed, eluted with the elution buffer[0.1 M NaHCO3 and 1% (w/v) SDS], heated at 65 ◦C for 6 hand incubated with proteinase K for 1 h at 55 ◦C. Samples werecleaned by Qiaquick columns (Qiagen) and analysed by RT-PCR.The putative LXRE (LXR response element) sites on the ABCA1rat promoter, as well as the non-specific sequences upstream of
the promoter, used as negative internal controls, were validatedwith the Genomatix Software (http://www.genomatix.de/). Primersequences are reported in Supplementary Table S1.
Treatment of mice and in vivo assays
The in vivo experiments were performed in conformity withthe Public Health Service Policy on Human Care and Use ofLaboratory Animals and were approved by the InstitutionalReview Board. Mice were housed in an environmentallycontrolled room (24 ◦C, 12 h light/dark cycle) and providedwith food and fresh water ad libitum. A standard diet formouse maintenance was used (Mucedola srl, 4RF21 CertificatePF1610). FVB male mice (1 month old) were injected dailyintraperitoneally with 1 mg of digoxin/kg, diluted in 0.9 % NaClsolution, for 5 or 8 days. Before killing, mice were heparinizedand anaesthetized with 250 mg of tribromoethanol/kg. Blood wascollected through decapitation.
Hearts were excised and rinsed in ice-cold Dulbecco’sPBS. Atria were removed, ventricular tissue and apex werecollected in RNAlater solution (Ambion) or ice-cold 1 M NaCland frozen at − 80 ◦C. RNA was extracted and used forRT-PCR experiments. Lipids were extracted from 50 mg ofventricular homogenates as described previously [16]. Cholesterolwas measured spectrophotometrically with the OSR6516 kit(Olympus System Reagent) and the results were expressed asμg of cholesterol/mg of heart tissue. The amount of ubiquin-one was determined spectrophotometrically [17] and theabsorbance was converted into μmol of ubiquinone/mg of hearttissue, using a calibration curve prepared previously.
Plasma total cholesterol and HDL cholesterol were determinedwith OSR6516 and OSR6187 kits respectively (Olympus SystemReagent) and the results were expressed as mg/100 ml. Plasmadigoxin was quantified with the Access Digoxin Kit (BeckmanCoulter) and the results were expressed as ng/ml.
Intracellular triacylglycerol measurement
The amount of triacylglycerol was measured in mouse hearthomogenates and in H9c2 cell lysates using the TriglycerideQuantification Kit (Abcam). Results were expressed in nmol/mgof cell or tissue proteins, according to the calibration curve setpreviously.
Statistical analysis
All of the data in the text and Figures are provided as means +− S.D.The results were analysed by a one-way ANOVA and Tukey’s test.P < 0.05 was considered significant.
RESULTS
Digoxin and ouabain increase the synthesis of cholesterol andubiquinone in cardiomyocytes by up-regulating the expression ofHMGCR
H9c2 cells were treated with digoxin or ouabain and labelledwith [3H]acetate. Both glycosides increased the de novo synthesisof cholesterol and ubiquinone in a dose- (Figure 1a) and time-(Figure 1b) dependent manner. Since a 24 h incubation with10 nM digoxin or ouabain elicited a detectable increase in themevalonate cascade, but no cytotoxicity, as determined by LDHrelease and annexin V–FITC positivity (Supplementary Figure S3
c© The Authors Journal compilation c© 2012 Biochemical Society

304 I. Campia and others
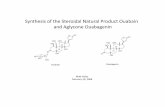
Figure 1 Effect of digoxin and ouabain on cholesterol and ubiquinonesynthesis
(a) H9c2 cells were incubated for 24 h in the absence (CTRL) or presence of variousconcentrations (1, 10, 100 nM) of digoxin (DGX) or ouabain (OUA). (b) Cells were incubatedfor 6, 24 or 48 h in the absence or presence of 10 nM digoxin or ouabain. In both cases, thecells were labelled with 1 μCi/ml [3H]acetate, then the de novo synthesis of cholesterol (openbars) and ubiquinone (striped bars) was measured in duplicate as described in the Experimentalsection. Results are means +− S.D. (n = 3). *P < 0.05 compared with control. (c) Cells weregrown for 6, 24 or 48 h in the absence or presence of digoxin (10 nM) or ouabain (10 nM),then the HMGCR activity was measured in duplicate in the microsomal fraction. Results aremeans +− S.D. (n = 3). *P < 0.01 compared with the respective control.
at http://www.BiochemJ.org/bj/447/bj4470301add.htm), this ex-perimental condition was chosen for all of our assays.
Both drugs induced a time-dependent increase in the enzymaticactivity of HMGCR (Figure 1c), which paralleled an increase ineither HMGCR RNA (Figure 2a) or protein (Figure 2b).
To ascertain whether the effects of digoxin and ouabain werelimited to HMGCR, we studied other genes of the mevalonatepathway, under the transcriptional control of SREBP-2 [18]. Bothdrugs up-regulated HMGCS (3-hydroxy-3-methylglutaryl-CoAsynthase) (Figure 2c), although to a lower extent than HMGCR.We did not detect other effects exerted by either digoxin andouabain in the analysed genes (Figure 2c).
To confirm that glycosides specifically modulate the firststeps of the mevalonate pathway, we measured the synthesisof cholesterol in cells labelled with [3H]acetate (Figure 2d),a substrate upstream of the HMGCR enzyme, or with[14C]mevalonic acid (Figure 2e), the product of HMGCR, inthe absence or presence of the HMGCR inhibitor mevastatin.As expected, mevastatin decreased the synthesis of cholesterolin cells labelled with [3H]acetate, but not in cells labelledwith [14C]mevalonic acid. Mevastatin prevented the increase ofcholesterol triggered by digoxin and ouabain in cells labelled with[3H]acetate (Figure 2d) and had no effect in cells labelledwith [14C]mevalonic acid (Figure 2e). The squalene synthase
inhibitor zaragozic acid [19], which blocks the mevalonatecascade downstream of HMGCR, also prevented the glycoside-elicited cholesterol increase, without a change in the increase inubiquinone (Supplementary Figure S4 at http://www.BiochemJ.org/bj/447/bj4470301add.htm).
Overall, these data suggest that digoxin and ouabain up-regulatethe mevalonate pathway probably by acting on HMGCS andHMGCR.
Digoxin and ouabain enhance the efficiency of the mitochondrialelectron transport chain and ATP synthesis
Besides cholesterol, digoxin and ouabain also increased thesynthesis of another mevalonate pathway derivative, ubiquinone(Figure 1), the only electron carrier between mitochondrialComplexes I or II and Complex III. Therefore glycosidesenhanced the electron flow in mitochondria of H9c2 cells(Figure 3a); this increase was found both in the presence ofthe Complex I inhibitor rotenone (when the electron transportrelies entirely on ubiquinone) and in its absence (i.e. whenthe electron flow depends on Complex I plus ubiquinone). Theenhanced electron flow resulted in increased levels of ATP, aneffect prevented by the F1Fo-ATP synthase inhibitor oligomycin(Figure 3b).
Digoxin and ouabain prevent the intracellular accumulation ofcholesterol
When cholesterol levels rise in mammalian cells, HMGCRactivity is down-regulated [20]. When loaded with exogenouscholesterol (Figure 4a), H9c2 cells had a low activity of HMGCR(Figure 4b). Unexpectedly, in spite of the increased endogenouscholesterol synthesis (Figures 1 and 2), we detected low levels ofintracellular cholesterol after treatment with digoxin and ouabain(Figure 4a). Moreover, when cells were treated with glycosidesplus cholesterol, they showed lower amounts of intracellularcholesterol than cells treated with cholesterol alone (Figure 4a).HMGCR activity remained high in the presence of digoxin andouabain (Figure 4b), which was consistent with the low level ofintracellular cholesterol.
Of note, we observed a progressive cholesterol accumulation inthe culture medium from cells treated with digoxin and ouabain(Figure 4c).
Digoxin and ouabain promote the efflux of cholesterol via theABCA1 transporter
To investigate whether digoxin and ouabain stimulate theefflux of intracellular cholesterol, we pulsed H9c2 cells with[3H]cholesterol and we measured the amount of [3H]cholesterolrecovered after 24 h in the culture medium (Figure 5a): bothdigoxin and ouabain increased the efflux of [3H]cholesterolfrom H9c2 cells. This increase was further enhanced byapoA-I (apolipoprotein A-I), a constituent of HDL particles,and was prevented by glyburide (Figure 5a), an inhibitorof the ABCA1 transporter [21]. The amount of intracellular[3H]cholesterol in H9c2 cells did not change significantlyunder all of the experimental conditions (Supplementary FigureS5a at http://www.BiochemJ.org/bj/447/bj4470301add.htm). Therelative amount of cholesterol effluxed by H9c2 cells was verysmall compared with the total labelling (Supplementary FigureS5b), which is consistent with mammalian cells in general[21,22].
c© The Authors Journal compilation c© 2012 Biochemical Society

Digoxin induces cholesterol efflux and ATP synthesis 305
Figure 2 Expression of HMGCR and synthesis of cholesterol in cells treated with digoxin, ouabain and mevastatin
H9c2 cells were cultured for 24 h in fresh medium (CTRL), digoxin (DGX; 10 nM) or ouabain (OUA; 10 nM), then subjected to the following investigations. (a) Total RNA was extracted,reverse-transcribed and amplified by RT-PCR to check HMGCR levels, as indicated in the Experimental section. Measurements were performed in triplicate and data are presented as means +− S.D.(n = 3). *P < 0.05 compared with fresh medium. (b) Western blotting experiments were performed on the microsomal fraction using an anti-HMGCR antibody and an anti-calreticulin (CRT) antibodyas a control for equal protein loading. The Figure is representative of three experiments with similar results. (c) The expression of the following SREBP-2 target genes was evaluated by RT-PCR:HMGCS, mevalonate kinase (MVK), mevalonate pyrophosphate decarboxylase (MPD), isopentenyl pyrophosphate isomerase (IPI), farnesyl pyrophosphate synthase (FPPS), squalene synthase(SQS), lanosterol 14 α-demethylase (CYP51), NADP(H) sterol dehydrogenase-like (NSDHL) and 7-dehydrocholesterol reductase (DHCR7). Measurements were performed in triplicate and resultsare means +− S.D. (n = 4). *P < 0.05 compared with CTRL. (d and e) Cells were incubated as reported above, in the absence or presence of mevastatin (MVS; 10 μM), and radiolabelled with1 μCi/ml [3H]acetate (d) or 1 μCi/ml [14C]mevalonic acid (e). The synthesis of cholesterol was measured in duplicate as described in the Experimental section. Results are means +− S.D. (n = 4).*P < 0.02 compared with fresh medium; ◦P < 0.05 compared with digoxin or ouabain.
In a parallel set of experiments, we labelled cells with[3H]acetate and measured [3H]cholesterol, as an index of de novosynthesized cholesterol, in the medium after 24 h (Figure 5b).Under these circumstances, digoxin and ouabain also promotedcholesterol efflux. Moreover, apoA-I protein further enhanced theefflux and glyburide decreased it.
ABCA1 was expressed in H9c2 cells at baseline and wasincreased by digoxin and ouabain, both in whole-cell lysates(Figure 5c) and on the cell surface (Figure 5d). ABCG1 andSR-BI, two other transporters involved in cholesterol efflux, wereeither only slightly increased by digoxin and ouabain (ABCG1)or not affected at all (SR-BI) (Supplementary Figure S6 athttp://www.BiochemJ.org/bj/447/bj4470301add.htm).
Digoxin and ouabain increase the transcription of ABCA1 byactivating LXR
To find out how glycosides increased the expression of ABCA1and ABCG1, we investigated which transcription factors may up-regulate these transporters.
The promoters of ABCA1 [23,24] and ABCG1 [25]contain sterol-responsive elements, which are activated by theheterodimers LXRα–RXR (retinoid X receptor) and LXRβ–RXR. The total amount of LXRβ and LXRα was not affectedby either glycosides or mevastatin (Figure 6a). LXR did not bindto its DNA target sequence in untreated H9c2 cells (Figure 6b).Conversely, digoxin and ouabain promoted the binding of LXR
c© The Authors Journal compilation c© 2012 Biochemical Society

306 I. Campia and others
Figure 3 Effects of digoxin and ouabain on mitochondrial Complex I–IIIactivity and ATP synthesis
H9c2 cells were grown for 24 h in the absence (CTRL) or presence of digoxin (DGX; 10 nM)or ouabain (OUA; 10 nM). (a) Cells were lysed and the mitochondrial fractions were isolated,then the rate of reduction of cytochrome c (cyt c) in the absence (open bars) or presence(striped bars) of 0.05 mM rotenone was detected [14]. The measurements were performed induplicate and results are means +− S.D. (n = 3). *P < 0.05 compared with control. (b) Cellswere cultured under the same experimental conditions indicated in (a). When indicated, the ATPsynthase inhibitor oligomycin (OLI; 1 μM) was added. The mitochondrial ATP was measuredby a bioluminescence assay, as described in the Experimental section. Results were collectedin duplicate and are means +− S.D. (n = 5). *P < 0.05 compared with control; ◦P < 0.005compared with digoxin or ouabain. prot, protein.
to DNA, an event prevented by mevastatin and mimickedby the LXR activator TO-901317 [24] (Figure 6b). As shown bychromatin immunoprecipitation assays, glycosides induced thebinding of either LXRα and LXRβ to the LXRE sequence ofthe ABCA1 promoter (Figure 6c).
Mice treated with digoxin have a lower amount of cholesterol and ahigher amount of ubiquinone in their hearts
The effects of digoxin were studied in mice treated for 5 and8 days with 1 mg of the drug/kg per day. At the end of thesetime periods, blood digoxin levels were significantly higher whencompared with untreated mice (Table 1) and within the acceptedhuman therapeutic range [26,27]. The drug increased HMGCRmRNA in a time-dependent fashion (Figure 7a) and decreasedcholesterol content (Figure 7b) in heart tissue. We did not detectsignificant differences in the serum levels of cholesterol in treatedand untreated mice; however, HDL cholesterol was slightly higherin the treated group (Table 1). A high degree of variability wasobserved in the levels of cardiac ubiquinone, in digoxin-treatedmice and in controls. Individual variability notwithstanding, thehearts of animals treated with digoxin in general showed higherlevels of ubiquinone.
Since LXR may increase the expression of several genesinvolved in the synthesis of fatty acids and triacylglycerols[28], we set out to see whether these genes were activated
Figure 4 Effect of glycosides on HMGCR activity and cholesterol content incells loaded with cholesterolH9c2 cells were grown for 24 h in the absence (CTRL) or presence ofcholesterol/β-methyl-cyclodextrin (CHOL; 100 μM), digoxin (DGX, 10 nM) or ouabain (OUA,10 nM), in different combinations. (a) The intracellular content of cholesterol was measuredspectrophotometrically in cell lysates. Results are means +− S.D. (n = 3). *P < 0.02 comparedwith control; ◦P < 0.01 compared with cholesterol/β-methyl-cyclodextrin. (b) HMGCR activitywas measured in duplicate in the microsomal fraction. Results are means +− S.D. (n = 3).*P < 0.05 compared with control. (c) At the end of incubation with digoxin or ouabain(zero time) and after 6, 24 and 48 h, the cell culture medium was collected and analysedspectrophotometrically for the cholesterol amount as described in the Experimental section.Results are means +− S.D. (n = 3). *P < 0.01 compared with control. prot, protein.
c© The Authors Journal compilation c© 2012 Biochemical Society

Digoxin induces cholesterol efflux and ATP synthesis 307
Figure 5 Effect of digoxin and ouabain on cholesterol efflux and ABCA1 amount
H9c2 cells were grown for 24 h in the absence (-) or presence of digoxin (DGX; 10 nM), ouabain (OUA; 10 nM), apoA-I (apo; 10 μg/ml), a component of HDLs, or glyburide (GLY; 100 μM), aninhibitor of the ABCA1 transporter, in different combinations, then subjected to the following investigations. (a) Cells were labelled for 1 h with [3H]cholesterol (chol), washed and grown for afurther 24 h. The [3H]cholesterol content in the culture medium was quantified in duplicate as described in the Experimental section. Results are means +− S.D. (n = 3). *P < 0.001 compared withcontrol. ◦P < 0.001 compared with digoxin or ouabain. (b) Cells were labelled with [3H]acetate and then treated as in (a). The amount of [3H]cholesterol in the culture medium, resulting from theintracellular synthesis, was measured in duplicate. Results are means +− S.D. (n = 3). *P < 0.001 compared with control. ◦P < 0.001 compared with digoxin or ouabain. (c) Western blot analysisof ABCA1 in whole-cell lysates. The expression of the housekeeping protein GAPDH was measured as a control for equal protein loading. Left-hand panel: the Figure is representative of threeexperiments with similar results. Right-hand panel: band density ratio between ABCA1 and GAPDH, expressed in arbitrary units (means +− S.D.; n = 3). The ratio corresponding to CTRL (absence ofdigoxin or ouabain) was normalized to 1. (d) Flow cytometry analysis of ABCA-1 protein (grey peak) was performed as described in the Experimental section. Negative controls with non-immuneisotypic antibodies are represented with the bold black outline. The Figures shown are representative of three similar experiments, performed in triplicate.
in the hearts of digoxin-treated animals. We did not observeany changes in the expression of lipogenic genes (acetyl-CoA carboxylase, fatty acid synthase, glycerol-3-phosphateacyltransferase and stearoyl-CoA desaturase 1); only SREBP-1cwas decreased after digoxin treatment (Figure 7d). Intracellulartriacylglycerol levels were highly variable, but did not differin each experimental group (Figure 7e). Similar findings wereobtained in vitro in H9c2 cells after a 24 h incubation with digoxinor ouabain (Supplementary Figure S7 at http://www.BiochemJ.org/bj/447/bj4470301add.htm).
DISCUSSION
Cardioactive glycosides are specific inhibitors of Na+ /K+ -ATPase and positive inotropic drugs [1]. The impact ofcardioactive glycosides on cholesterol metabolism in cardiactissue has not been investigated. We used H9c2 cells, which sharesome ultrastructural features with skeletal muscle [29–31], butretain the key electrophysiological and biochemical properties ofcardiomyocytes [29,32], making them a useful tool for the in vitroinvestigation of cardioactive drugs.
c© The Authors Journal compilation c© 2012 Biochemical Society

308 I. Campia and others
Figure 6 LXR is translocated into the nucleus by digoxin and ouabain and binds to the ABCA1 promoter
(a) H9c2 cells were incubated for 24 h in the absence (CTRL) or presence of digoxin (DGX; 10 nM), ouabain (OUA, 10 nM) or mevastatin (MVS, 10 μM), in different combinations, then whole-celllysates were prepared as reported in the Experimental section and analysed for the amount of LXRβ and LXRα. The expression of the housekeeping protein glyceraldehyde-3-phosphate dehydrogenase(GAPDH) was measured as a control for equal protein loading. The Figure is representative of three experiments with similar results. (b) EMSA detection of LXR bound to its DNA consensus sequencewas performed on nuclear extracts of cells incubated as reported in (a). The Figure is representative of three experiments with similar results. In each experiment one lane was loaded with distilledwater (-) in place of cell extracts. The LXR activator TO-901317 (TO; 100 nM for 24 h) was added as a positive control. As a control of specificity, the nuclear extracts of TO-901317-stimulated cellswere incubated with a mutated probe (TO mut) or with a 100-fold excess of non-radioactive wild-type probe (TO cold). (c) Chromatin immunoprecipitation assays. The binding of LXRα and LXRβ
to the ABCA1 promoter was measured as described in the Experimental section; the immunoprecipitated DNA was analysed by RT-PCR, using primers for the LXREs in the ABCA1 promoter or for anupstream region, chosen as a negative control. Results are means +− S.D. (n = 4). *P < 0.01 compared with control.
Digoxin and ouabain enhanced the activity of the mevalonatepathway in a dose- and time-dependent manner in these cells.This increase was accompanied by the up-regulation of the rate-limiting enzyme HMGCR, which is under the transcriptionalcontrol of SREBP-2. Although SREBP-2 induces a transcrip-tional activation of several enzymes involved in cholesterolbiosynthesis [18], in H9c2 cells only the HMGCR and HMGCSgenes were up-regulated by both digoxin and ouabain. Suchspecificity suggests that glycosides may act not only by simply
activating SREBP-2 [7], but also by recruiting other transcriptionfactors and/or co-activators, which in turn co-operate withSREBP-2 on HMGCR and HMGCS promoters.
The effects of glycosides on the HMGCR step, or on one of thefirst steps in the mevalonate cascade, were confirmed by functionalassays: the increase in cholesterol was indeed prevented by theHMGCR inhibitor mevastatin in cells labelled with [3H]acetate(i.e. the metabolite upstream of HMGCR), but not in cellslabelled with [14C]mevalonic acid (i.e. the product of HMGCR)
c© The Authors Journal compilation c© 2012 Biochemical Society

Digoxin induces cholesterol efflux and ATP synthesis 309
Table 1 Plasma values of digoxin, total cholesterol and HDL cholesterol inmice treated with digoxin
DGX, digoxin. *P < 0.001.
TreatmentNumber ofanimals
Digoxin(ng/100 ml)
Cholesterol(mg/100 ml)
HDL cholesterol(mg/100 ml)
Control 10 0.29 +− 0.02 95.60 +− 6.41 60.07 +− 3.17DGX, 5 days 6 2.05 +− 0.10* 94.80 +− 3.00 69.80 +− 1.82DGX, 8 days 6 1.78 +− 0.01* 96.20 +− 4.17 68.30 +− 2.73
or treated with the inhibitor of squalene synthase, zaragozicacid.
Both cholesterol and ubiquinone, the mevalonate pathwayproducts increased by digoxin and ouabain, play an undisputedrole in cardiovascular disease and therapy [8,9,11,13].
Glycosides increased the synthesis of ubiquinone in H9c2 cells,thus enhancing the efficiency of mitochondrial electron transportand ATP synthesis. Both adequate intracellular Ca2 + levels anda constant supply of ATP are necessary to support an efficientcontractile performance. The increase of intracellular Ca2 + is awell-documented effect of digoxin [1–3]; the increase in aerobicmetabolism and ATP synthesis observed in the present study mayrepresent an additional mechanism by which digoxin exerts itspositive inotropic effects.
Cholesterol levels also affect other crucial cellular functionsin cardiomyocytes: increased plasma membrane cholesterolmodifies the affinity of Na+ /K+ -ATPase for inhibitors and altersthe activity of Ca2 + -ATPase, Na+ /Ca2 + -exchanger and Na+ /K+ -ATPase, three pumps that critically affect intracellular Ca2 + levels[8]. As digoxin and ouabain increase the synthesis of cholesterol,one might expect that these cells ‘fill up’ with cholesterol.Such occurrence, however, has never been described in patients
Figure 7 Effects of digoxin on HMGCR expression, cholesterol and ubiquinone content in mouse heart
Male FVB mice (1 month old) were treated with 1 mg of digoxin/kg for 5 days (n = 6) or 8 days (n = 6). The control group (CTRL; n = 10) was treated with saline solution. Animals were killed at theend of treatment, and heart tissue was homogenized, frozen and subjected to the following investigations. (a) Total RNA was extracted, reverse-transcribed and amplified by RT-PCR to check HMGCRexpression. Results are means +− S.D. *P < 0.05 compared with control. Amounts of cholesterol (chol) (b) and ubiquinone (ubiq) (c) were measured spectrophotometrically in heart homogenates,after the appropriate extraction [16,17]. *P < 0.05 compared with control. (d) Expression of the following lipogenic genes was evaluated by RT-PCR: acetyl-CoA carboxylase (ACC), fatty acidsynthase (FAS), glycerol-3-phosphate acyltransferase (GPAT), stearoyl-CoA desaturase 1 (SCD1) and SREBP-1c (SREBP1). Measurements were performed in triplicate, and results are means +− S.D.Compared with *P < 0.05 control. (e) The intracellular amount of triacylglycerols was detected fluorimetrically as reported in the Experimental section. Results are means +− S.D.
c© The Authors Journal compilation c© 2012 Biochemical Society

310 I. Campia and others
treated with digoxin. Indeed, H9c2 cells treated with digoxin andouabain had low levels of intracellular cholesterol and showed atime-dependent cholesterol accumulation in the culture medium.The cholesterol transport assays that use [3H]cholesterol or thecholesterol precursor [3H]acetate suggest that digoxin and ouabainstimulate the efflux of both exogenously added or endogenouslysynthesized cholesterol, thereby preventing any accumulation ofcholesterol in cardiomyocytes. From this perspective, one mightconsider this ‘cholesterol-buffering’ effect of glycosides to be atype of cardioprotective action.
A crucial mechanism of cholesterol efflux in mammalian tissuesis its active transport via the ABC transporter ABCA1, whichtransfers cholesterol from the cytosol to apoA-I and mediates thefirst step of HDL assembly [23,33,34]. Interestingly, both digoxinand ouabain increased the amount of ABCA1 in H9c2 cells. Inaddition, ABCG1, a second transporter which mediates the effluxof cholesterol from the cells, was slightly increased. As we workedwith a culture medium that contains HDLs, we hypothesized thatglycosides might promote the delivery of cholesterol to the apoA-I present in the culture medium through ABCA1. When we usedthe ABCA1 inhibitor glyburide, cholesterol efflux decreased tocontrol levels, even under maximal stimulation (i.e. when digoxinand ouabain were co-incubated with apoA-I): this suggests thatin H9c2 cells, most of the glycoside-induced cholesterol efflux ismediated by ABCA1, whereas ABCG1 plays a secondary role.
Multiple sterol-responsive elements, activated by LXRα–RXRand LXRβ–RXR heterodimers in response to oxysterols, arecontained in the promoter of the ABCA1 gene [23,24]. Givingthe cell a cholesterol load induces the transcriptional activityof LXRs, suggesting that free cholesterol, or a cholesterol-derived metabolite produced within cells, can up-regulate ABCA1[34]. We hypothesize that a similar mechanism might also workwith glycosides, which in our hands increased the synthesis ofcholesterol, the binding of LXR on DNA target sequences and theactivation of the ABCA1 promoter.
To our knowledge this is the first report that showsthat cardioactive glycosides stimulate the reverse transport ofcholesterol by increasing the expression of ABCA1 and thedelivery of cholesterol to apoA-I, and therefore facilitate oneof the first steps in the assembly of HDLs. This event mayhave physiological relevance, since an efficient reverse cholesteroltransport and high levels of HDLs are protective factors againstcardiovascular disease.
The concentration of digoxin used in our in vitro experiments(10 nM) falls within the clinically accepted therapeutic range[26,27]. At these concentrations, the well-known inotropic effectsof glycosides are mainly mediated by their binding to the α2subunit of Na+ /K+ -ATPase [35], which in rats has a higheraffinity for ouabain than α1 subunit [36]. Since α1 and α2 subunitlevels were equal in H9c2 cells, it is likely that in our model theNa+ /K+ -ATPase-dependent effects of glycosides were mediatedby the interaction with the α2 subunit. H9c2 cells mirror rattissues, which have a mix of ouabain-insensitive (i.e. containingsolely the α1 isoform) Na+ /K+ -ATPases and ouabain-sensitive(i.e. containing the α2 and α3 isoforms) ones [37]. Rodents aremore resistant than humans to the effects of digoxin on Na+ /K+ -ATPase [37,38]. Nonetheless, after a few days of treatment, in ouranimal models, digoxin reached the same levels as the acceptedclinically therapeutic ones in humans. As such, it began to exertits effects on the mevalonate pathway in hearts, as the increasedexpression of HMGCR, the progressive decrease in cholesteroland increase in ubiquinone synthesis would indicate. Since inthe liver, LXR up-regulates SREBP-1c and co-operates with itto promote the synthesis of fatty acids and triacylglycerols [28],we set out to investigate whether these events occurred in the
heart as well. Differently from what happens in the liver, in ourmodel digoxin decreased the expression of SREBP-1c. Such adecrease may prevent the up-regulation of lipogenic genes and theaccumulation of triacylglycerols in cardiac myocytes, makingthe onset of a lipid-induced cardiomyopathy an unlikely event.
The present study sheds some new light on the metaboliceffects of glycosides in cardiac myocytes. By enhancing theactivity of the mevalonate pathway, glycosides increase thecellular levels of ubiquinone, the aerobic metabolism and thesynthesis of ATP of the cells, three events critical in thecontrol of contractile performance. In addition, glycosides finelycontrol the levels of cholesterol in the cell. On one hand,they provide cells with a metabolite (cholesterol) necessaryfor the maintenance of membrane homoeostasis and the properconformation and activity of transporters, channels and receptors.On the other, they prevent the intracellular accumulation of thesame metabolite and facilitate its delivery to HDLs. Beside beingused as therapeutic agents, ouabain- and digoxin-like substancesare also endogenously produced; acting at nanomolar/picomolarconcentrations, these endogenous glycosides have beenimplicated in the control of blood pressure and in thecardiovascular remodelling of chronic heart failure [39]. Onecould surmise that the same effects observed with exogenouslyadministered glycosides might be exerted by the ones that areendogenously produced. From this perspective, glycosides mightindeed be novel regulators of cholesterol homoeostasis.
AUTHOR CONTRIBUTION
Ivana Campia performed the in vitro experiments, analysed the data and wrote the paper;Valentina Sala and Christian Leo performed the animal treatment and the in vivoassays; Joanna Kopecka, Nico Mitro and Costanzo Costamagna performed the in vitro exp-eriments; Donatella Caruso and Gianpiero Pescarmona supervised the in vitro experimentsand analysed the results; Tiziana Crepaldi supervised the in vivo experiments and analysedthe results; Dario Ghigo and Amalia Bosia analysed the data and reviewed the paper priorto submission; Chiara Riganti conceived the study and wrote and reviewed the paperprior to submission.
FUNDING
This work was supported by the Fondazione Internazionale Ricerche Medicina Sperimentale(FIRMS), the Compagnia di San Paolo [grant number 3856 SD/CV], the Regione PiemonteRicerca Sanitaria Finalizzata 2009 [grant number 204/30.04.2009] and the GiovanniArmenise-Harvard Foundation.
REFERENCES
1 Kaplan, J. H. (2002) Biochemistry of Na,K-ATPase. Annu. Rev. Biochem. 71, 511–5352 Newman, R. A., Yang, P., Pawlus, A. D. and Block, K. I. (2008) Cardiac glycosides as
novel cancer therapeutic agents. Mol. Interv. 8, 36–493 Prassas, I. and Diamandis, E. P. (2008) Novel therapeutic applications of cardiac
glycosides. Nat. Rev. Drug Discovery 7, 926–9354 Takara, K., Takagi, K., Tsujimoto, M., Ohnishi, N. and Yokoyama, T. (2003) Digoxin up
regulates multidrug resistance transporter (MDR1) mRNA and simultaneouslydown-regulates steroid xenobiotic receptor mRNA. Biochem. Biophys. Res. Commun.306, 116–120
5 Kau, M., Kan, S., Wang, J. and Wang, P. S. (2005) Inhibitory effects of digoxin andouabain on aldosterone synthesis in human adrenocortical NCI-H295 cells. J. Cell.Physiol. 205, 393–401
6 Pu, H., Wang, S., Tseng, C., Huang, H., Lin, C., Hsu, J., Chen, M., Chow, Y. and Wang,P. S. (2006) Mechanisms of digoxin and digitoxin on the production of corticosterone inzona fasciculata-reticularis cells of ovariectomized rats. J. Cell. Biochem. 97, 303–313
7 Campia, I., Gazzano, E., Pescarmona, G., Ghigo, D., Bosia, A. and Riganti, C. (2009)Digoxin and ouabain increase the synthesis of cholesterol in human liver cells. Cell. Mol.Life Sci. 66, 1580–1594
8 Saini, H. K., Arneja, A. S. and Dhalla, N. S. (2004) Role of cholesterol in cardiovasculardysfunction. Can. J. Cardiol. 20, 333–346
c© The Authors Journal compilation c© 2012 Biochemical Society

Digoxin induces cholesterol efflux and ATP synthesis 311
9 Ghandehari, H., Kamal-Bahl, S. and Wong, N. D. (2008) Prevalence and extent ofdyslipidemia and recommended lipid levels in US adults with and without cardiovascularcomorbidities: the National Health and Nutrition Examination Survey 2003–2004. Am.Heart J. 156, 112–119
10 Teclebrhan, H., Olsson, J., Swiezewska, E. and Dallne, G. (1993) Biosynthesis of the sidechain of ubiquinone: trans-prenyltransferase in rat liver microsomes. J. Biol. Chem. 268,23081–23086
11 Jeejeebhoy, F., Keith, M., Freeman, M., Barr, A., McCall, M., Kurian, R., Mazer, D. andErrett, L. (2002) Nutritional supplementation with MyoVive repletes essential cardiacmyocyte nutrients and reduces left ventricular size in patients with left ventriculardysfunction. Am. Heart J. 143, 1092–1100
12 Molyneux, S. L., Florkowski, C. M., George, P. M., Pilbrow, A. P., Frampton, C. M., Lever,M. and Richards, A. M. (2008) Coenzyme Q10: an independent predictor of mortality inchronic heart failure. J. Am. Coll. Cardiol. 52, 1435–1441
13 Sander, S., Coleman, C. I., Patel, A. A., Kluger, J. and White, C. M. (2006) The impact ofcoenzyme Q10 on systolic function in patients with chronic heart failure. J. Card. Failure12, 464–472
14 Campia, I., Lussiana, C., Pescarmona, G., Ghigo, D., Bosia, A. and Riganti, C. (2009)Geranylgeraniol prevents the cytotoxic effects of mevastatin in THP-1 cells, withoutdecreasing the beneficial effects on cholesterol synthesis. Br. J. Pharmacol. 158,1777–1786
15 Wang, N., Silver, D. L., Costet, P. and Tall, A. R. (2000) Specific binding of ApoA-I,enhanced cholesterol efflux, and altered plasma membrane morphology in cellsexpressing ABC1. J. Biol. Chem. 275, 33053–33058
16 Folch, J., Lees, M. and Stanley, G. H. S. (1957) A simple method for the isolation andpurification of total lipids from animal tissues. J. Biol. Chem. 226, 497–509
17 Karpinska, J., Mikołuc, B. and Piotrowska-Jastrzebska, J. (1998) Application of derivativespectrophotometry for determination of coenzyme Q10 in pharmaceuticals and plasma.J. Pharm. Biomed. Anal. 17, 1345–1350
18 Horton, J. D., Shah, N. A., Warrington, J. A., Anderson, N. N., Park, S. W., Brown, M. S.and Goldstein, J. L. (2003) Combined analysis of oligonucleotide microarray data fromtransgenic and knockout mice identifies direct SREBP target genes. Proc. Natl. Acad. Sci.U.S.A. 100, 12027–12032
19 Bergstrom, J. D., Dufresne, C., Bills, G. F., Nallin-Omstead, M. and Byrne, K. (1995)Discovery, biosynthesis, and mechanism of action of the zaragozic acids: potent inhibitorsof squalene synthase. Annu. Rev. Microbiol. 49, 607–639
20 Espenshade, P. J. and Hughes, A. L. (2007) Regulation of sterol synthesis in eukaryotes.Annu. Rev. Genet. 41, 401–427
21 Kasza, I., Hegyi, Z., Szabo, K., Andrikovics, H., Nemet, K., Varadi, A., Sarkadi, B. andHomolya, L. (2009) Model system for the analysis of cell surface expression of humanABCA1. BMC Cell Biol. 10, 93
22 Wang, N., Lan, D., Chen, W., Matsuura, F. and Tall, A. R. (2004) ATP-binding cassettetransporters G1 and G4 mediate cellular cholesterol efflux to high-density lipoproteins.Proc. Natl. Acad. Sci. U.S.A. 101, 9774–9779
23 Costet, P., Luo, Y., Wang, N. and Tall, A. R. (2000) Sterol-dependent transactivation of theABC1 promoter by the liver X receptor/retinoid X receptor. J. Biol. Chem. 275,28240–28245
24 Tamehiro, N., Shigemoto-Mogami, Y., Kakeya, T., Okuhira, K., Suzuki, K., Sato, R., Nagao,T. and Nishimaki-Mogami, T. (2007) Sterol regulatory element-binding protein-2- andliver X receptor-driven dual promoter regulation of hepatic ABC transporter A1 geneexpression. J. Biol. Chem. 282, 21090–21099
25 Sabol, S. L., Brewer, Jr, H. B. and Santamarina-Fojo, S. (2005) The human ABCG1 gene:identification of LXR response elements that modulate expression in macrophages andliver. J. Lipid Res. 46, 2151–2167
26 Haynes, K., Heitjan, D. F., Kanetsky, P. A. and Hennessy, S. (2008) Declining publichealth burden of digoxin toxicity from 1991 to 2004. Clin. Pharmacol. Ther. 84,90–94
27 Rogers, N. M., Jones, T. E. and Morris, R. G. (2008) Frequently discordant results fromtherapeutic drug monitoring for digoxin: clinical confusion for the prescriber. Intern. Med.J. 40, 52–56
28 Cha, J.-Y. and Repa, J. J. (2007) The liver X receptor (LXR) and hepatic lipogenesis.J. Biol. Chem. 282, 743–751
29 Hescheler, J., Meyer, R., Plant, S., Krautwurst, D., Rosenthal, W. and Schultz, G. (1991)Morphological, biochemical, and electrophysiological characterization of a clonal cell(H9c2) line from rat heart. Circ. Res. 69, 1476–1486
30 Kimes, B. W. and Brandt, B. L. (1976) Properties of a clonal muscle cell line from ratheart. Exp. Cell Res. 98, 367–381
31 Mejıa-Alvarez, R., Tomaselli, G. F. and Marban, E. (1994) Simultaneous expression ofcardiac and skeletal muscle isoforms of the L-type Ca2 + channel in a rat heart musclecell line. J. Physiol. 478, 315–329
32 Watkins, S. J., Borthwick, G. M. and Arthur, H. M. (2011) The H9C2 cell line and primaryneonatal cardiomyocyte cells show similar hypertrophic responses in vitro. In Vitro Cell.Dev. Biol.: Anim. 47, 125–131
33 Oram, J. F. and Heinecke, J. W. (2005) ATP-binding cassette transporter A1: a cellcholesterol exporter that protects against cardiovascular disease. Physiol. Rev. 85,1343–1372
34 Oram, J. F. and Lawn, R. M. (2001) ABCA1: the gatekeeper for eliminating excess tissuecholesterol. J. Lipid Res. 42, 1173–1179
35 Gao, J., Wymore, R. S., Wang, Y., Gaudette, G. R., Krukenkamp, I. B., Cohen, I. S. andMathias, R. T. (2002) Isoform-specific stimulation of cardiac Na/K pumps by nanomolarconcentrations of glycosides. J. Gen. Physiol. 119, 297–312
36 Dostanic-Larson, I., Van Huysse, J. W., Lorenz, J. N. and Lingrel, J. B. (2005) The highlyconserved cardiac glycoside binding site of Na,K-ATPase plays a role in blood pressureregulation. Proc. Natl. Acad. Sci. U.S.A. 102, 15845–15850
37 Hansen, O. (2003) No evidence for a role in signal-transduction of a Na+ /K+ -ATPase interaction with putative endogenous ouabain. Eur. J. Biochem. 270,1916–1919
38 Perne, A., Muellner, M. K., Steinrueck, M., Craig-Mueller, N., Mayerhofer, J.,Schwarzinger, I., Sloane, M., Uras, I. Z., Hoermann, G., Nijman, S. M. B. and Mayerhofer,M. (2009) Cardiac glycosides induce cell death in human cells by inhibiting generalprotein synthesis. PLoS ONE 4, e8292
39 Bagrov, A. Y., Shapiro, J. and Fedorova, O. V. (2209) Edogenous cardiotonicsteroids: physiology, pharmacology, and novel therapeutic targets. Pharmacol. Rev. 61,9–38
Received 2 February 2012/27 July 2012; accepted 30 July 2012Published as BJ Immediate Publication 30 July 2012, doi:10.1042/BJ20120200
c© The Authors Journal compilation c© 2012 Biochemical Society

Biochem. J. (2012) 447, 301–311 (Printed in Great Britain) doi:10.1042/BJ20120200
SUPPLEMENTARY ONLINE DATADigoxin and ouabain induce the efflux of cholesterol via liver X receptorsignalling and the synthesis of ATP in cardiomyocytesIvana CAMPIA*, Valentina SALA†, Joanna KOPECKA*, Christian LEO†, Nico MITRO‡, Costanzo COSTAMAGNA*,Donatella CARUSO‡, Gianpiero PESCARMONA*§, Tiziana CREPALDI†, Dario GHIGO*, Amalia BOSIA*§ and Chiara RIGANTI*§1
*Department of Genetics, Biology and Biochemistry, University of Torino, via Santena 5/bis, 10126 Torino, Italy, †Department of Anatomy, Pharmacology and Forensic Medicine,University of Torino, corso Massimo D’Azeglio 52, 10126 Torino, Italy, ‡Department of Pharmacological and Biomolecular Sciences, University of Milano, via Balzaretti 9, 20133Milano, Italy, and §Research Center on Experimental Medicine (Ce.R.M.S.), University of Torino, via Santena 5/bis, 10126 Torino, Italy
Figure S1 Expression of α subunit isoforms of Na+ /K+ -ATPase in H9c2cells
Total RNA was extracted from H9c2 cells, reverse-transcribed and amplified by RT-PCR, asindicated in the Experimental section of the main text. Measurements were performed in triplicate,and results are means +− S.D. (n = 3). The expression of α1 subunit in untreated cells wasconsidered to be ‘1’; the relative expressions of α2 and α3 subunits were with reference to theα1 experimental dataset.
Figure S2 Linearity of ubiquinone assay
A total of 106 cells were incubated for 24 h with 0.25, 0.50, 0.75 or 1 μCi of [3H]acetate, and thelipids were extracted in methanol/hexane and separated by TLC. The amount of [3H]ubiquinonewas quantified by liquid scintillation as reported in the Experimental section of the main text.
Figure S3 Cytotoxicity of digoxin and ouabain in H9c2 cells
(a) Cells were incubated in the absence (CTRL) or presence of digoxin (DGX) or ouabain (OUA)at different concentrations (1 nM, 10 nM or 100 nM) for 24 h. (b) Cells were incubated in theabsence (CTRL) or in the presence of 10 nM digoxin (DGX) or ouabain (OUA) for 6, 24 or 48 h.(a and b) The measurement of LDH release (open bars) and the flow cytometry analysis ofannexin V–FITC-positive cells (striped bars) were performed in duplicate as described in theExperimental section of the main text. Results are means +− S.D. (n = 3). *P < 0.001 comparedwith control.
1 To whom correspondence should be addressed (email [email protected]).
c© The Authors Journal compilation c© 2012 Biochemical Society

I. Campia and others
Figure S4 Effect of zaragozic acid on the synthesis of cholesterol andubiquinone in H9c2 cells treated with cardioactive glycosides
Cells were cultured for 24 h with [3H]acetate in the absence (CTRL) or presence of zaragozicacid (ZA; 10 μM), an inhibitor of squalene synthase, digoxin (DGX; 10 nM) or ouabain (OUA,10 nM), in different combinations. The synthesis of cholesterol (open bars) and ubiquinone(striped bars) was measured in duplicate as described in the Experimental section of the maintext. Results are means +− S.D. (n = 4). *P < 0.02 compared with control; ◦P < 0.05 comparedwith digoxin or ouabain.
Figure S5 Intracellular cholesterol and cholesterol efflux in H9c2 cells
Cells were labelled for 1 h with [3H]cholesterol (chol), then extensively washed and grown for 24 h in the absence (-) or presence ( + ) of digoxin (DGX; 10 nM), ouabain (OUA, 10 nM), apoA-I(apo; 10 μg/ml), a component of HDL, or glyburide (GLY; 100 μM), an inhibitor of the ABCA1 transporter, in different combinations. (a) Cells were lysed and analysed for the intracellular amountof [3H]cholesterol. Results are means +− S.D. (n = 3). (b) The ratio between extracellular [3H]cholesterol (reported in Figure 5a in the main text) and total [3H]cholesterol (extracellular cholesterol,reported in Figure 5a of the main text, plus intracellular cholesterol, reported in (a) was expressed as c.p.m. in medium/(c.p.m. in medium + c.p.m. in cells). Results are means +− S.D. (n = 3).*P < 0.05 compared with untreated (-) cells.
c© The Authors Journal compilation c© 2012 Biochemical Society

Digoxin induces cholesterol efflux and ATP synthesis
Figure S6 Expression of ABCG1 and SR-BI in H9c2 cells
H9c2 cells were incubated for 24 h in the absence (CTRL) or presence of digoxin (DGX; 10 nM)and ouabain (OUA; 10 nM). Total extracts were prepared as described in the Experimentalsection of the main text and analysed for the amount of ABCG1 and SR-BI. The expression ofthe housekeeping protein GAPDH was measured as a control for equal protein loading. Upperpanel: the Figure is representative of three experiments with similar results. Lower panel: banddensity ratio between ABCG1 and GAPDH or SR-B1 and GAPDH, expressed in arbitrary units(means +− S.D.; n = 3). The ratio corresponding to the control was normalized to 1.
c© The Authors Journal compilation c© 2012 Biochemical Society

I. Campia and others
Figure S7 Expression of lipogenic genes and amount of triacylglycerols in H9c2 cells
H9c2 cells were incubated for 24 h in the absence (CTRL) or presence of digoxin (DGX; 10 nM) and ouabain (OUA; 10 nM), then subjected to the following investigations. (a)Total RNA was extracted,reverse-transcribed and amplified by RT-PCR, as indicated in the Experimental section of the main text. The expression of the following genes was evaluated: acetyl-CoA carboxylase (ACC), fatty acidsynthase (FAS), glycerol-3-phosphate acyltransferase (GPAT), stearoyl-CoA desaturase 1 (SCD1) and SREBP1c (SREBP1). Measurements were performed in triplicate, and results are means +− S.D.(n = 4). *P < 0.05 compared with control. (b) The intracellular amount of triacylglycerols was detected fluorimetrically as reported in the Experimental section of the main text. Measurements wereperformed in duplicate, and results are means +− S.D. (n = 3).
c© The Authors Journal compilation c© 2012 Biochemical Society

Digoxin induces cholesterol efflux and ATP synthesis
Table S1 Primer sequences used in RT-PCR experiments
Gene Host Forward primer (5′→3′) Reverse primer (5′→3′)
Na+ /K+ -ATPase α1 subunit Rat GGCTGTCATCTTCCTCATTGG CGGTGGCCAGCAAACCNa+ /K+ -ATPase α2 subunit Rat GGTGGCCCTCCGAATGTAC ATGAAGATGAGGAGACTGTAGGGAAANa+ /K+ -ATPase α3 subunit Rat CCATTGTCACTGGTGTGGAG CAATGCAGAGGATGGTGATGHMGCR Rat GCTTGAGCATCCTGACATAC GAACCATAGTTCCCACGTCTHMGCR Mouse CGCAACCTCTATATCCGT GTAGCCGCCTATGCTCHMGCS Rat TTGGTAGTTGCAGGAGACATCGCT AGCATTTGGCCCAATTAGCAGAGCMevalonate kinase (MVK) Rat CCGCAGAGCAATGGGAAAGTG CATCGCCTTGCTCAAGAAAGCCMevalonate pyrophosphate decarboxylase (MPD) Rat AGCGTGGCGACCAGTACCCTG GGGCGTTGAAGCGGTGGACTAIsopentenyl pyrophosphate isomerase (IPI) Rat AGTTGCTGTAGTCATCCATTAAATAACC CGCTTCTGTGCTGCTCGTTFarnesyl pyrophosphate synthetase (FPPS) Rat TATCAGAAGCCGGGCATAGG GGTGCTGTGATGAGGTCGAGASqualene synthase (SQS) Rat GCCACCCGGAGGAGTTCTACA GGCGAAGCTGCGACTGGTCLanosterol 14α-demethylase (CYP51) Rat TTAGGTGACAACCTGACACACGCT TGCTTACTGTCTTGCTCCTGGTGTNADPH steroid dehydrogenase-like (NSDHL) Rat CGGGTGCAGTTCTTCATAGGT ACACTGGCAGAGCTGGTTAAA7-Dehydrocholesterol reductase (DHCR7) Rat TCAGCTTCCAGGTGCTGCTTTACT ACAATCCCTGCTGGAGTTATGGCAFatty acid synthase (FAS) Rat GCCATTTCCATTGCCCTTAGC CTGAGCCAAGCACCGCACACTFatty acid synthase (FAS) Mouse CCTGGATAGCATTCCGAACCT AGCACATCTCGAAGGCTACACAAcetyl-CoA carboxylase (ACC) Rat CAACCACTACGGCATGACTCA CGCAGAAGCAGCCCATTACTTAcetyl-CoA carboxylase (ACC) Mouse CCCAGCAGAATAAAGCTACTTTGG TCCTTTTGTGCAACTAGGAACGTGlycerol-3-phosphate acyltransferase (GPAT) Rat GGCCCATCAGCAAGAACCTAT CGCCAAACCGCTCGCACATGlycerol-3-phosphate acyltransferase (GPAT) Mouse CAACACCATCCCCGACATC GTGACCTTCGATTATGCGATCAStearoyl-CoA desaturase 1 (SCD1) Rat CACTGGTGCCCTGGTACTGCT GGATGTTCTCCCGAGATTGAAStearoyl-CoA desaturase 1 (SCD1) Mouse ACGCCGACCCTCACAATTC CAGTTTTCCGCCCTTCTCTTTSREBP-1c (SREBP1c) Rat GCAAGGCCATCGACTACATC TTTCATGCCCTCCATAGACACSREBP-1c (SREBP1c) Mouse GATCAAAGAGGAGCCAGTGC TAGATGGTGGCTGCTGAGTGABCA1 promoter Rat CGCAGGCTTAGAAGATTGT CGAGGAAATGTATCCGAGGTABCA1 promoter upstream region Rat GTGGTTTTGCAGGCTTT CAGGCATGGTGTGAATATGAAActin Rat AGCCATGTACGTAGCCATCC CTCTCAGCTGTGGTGGTGAAActin Mouse TGAAGTGTGACGTTGACA TAGAAGCACTTGCGGTGCAG
Received 2 February 2012/27 July 2012; accepted 30 July 2012Published as BJ Immediate Publication 30 July 2012, doi:10.1042/BJ20120200
c© The Authors Journal compilation c© 2012 Biochemical Society