Diffusion tensor imaging of deep gray matter in children treated for brain malignancies
Transcript of Diffusion tensor imaging of deep gray matter in children treated for brain malignancies

ORIGINAL PAPER
Diffusion tensor imaging of deep gray matter in childrentreated for brain malignancies
Alena Horská &AnnaNidecker & Jarunee Intrapiromkul &Firouzeh Tannazi & Siamak Ardekani & Larry J. Brant &Moody Wharam Jr & E. Mark Mahone
Received: 18 September 2013 /Accepted: 28 October 2013# Springer-Verlag Berlin Heidelberg 2013
AbstractPurpose PreviousDTI studies reportedmicrostructural changesin white matter of patients receiving treatment for brain malig-nancies. The primary aim of this prospective pilot longitudinalstudy was to examine if DTI can detect microstructural changesin deep gray matter (as evaluated by the apparent diffusioncoefficient, ADC) between pediatric patients treated with cranialradiation therapy and typically developing healthy children. Therelationship between ADC and neurobehavioral performancewas also examined.Methods ADCwas measured at 1.5 T in the caudate, putamen,globus pallidus, thalamus, and hippocampus in nine patients(mean age 11.8 years) and nine age-matched healthy controls.The study was designed with four visits: baseline, 6-month,15-month, and 27-month follow-ups.
Results Patients had 24 % higher overall mean ADC in thehippocampus compared with controls (p =0.003). Post hocanalyses revealed significantly elevated ADC at baseline(p =0.003) and at the 27-month follow-up (p =0.006). Never-theless, patients performed normally on a verbal memory testconsidered to be a hippocampus-related function. Relative tocontrols, patients' performance on the tests of the visual–spatial working memory decreased over time (group by visit,p =0.036). Both patients and controls showed a decline inmotor speed with increasing ADC in the globus pallidus andputamen.Conclusions Childhood brain malignancies and their treat-ment may affect gray matter microstructure as measured bywater diffusion. Significant findings in the hippocampus butnot other regions suggest that differences in tissue sensitivityto disease- and treatment-related injury among gray matterregions may exist. ADC in basal ganglia may be associatedwith motor performance.
Keywords Radiation therapy . Children . Brain . Basalganglia . Hippocampus . Diffusion tensor imaging
Introduction
Long-term survival of pediatric patients with brain malignan-cies has markedly increased over the last two decades due toadvances in treatment with cranial radiation therapy (CRT),surgery, and chemotherapy. While survival rates haveincreased, so have concerns about the neurotoxic effectsof these treatments on healthy brain tissue. Effects oftreatments involving CRT manifest as vascular and glialpathologies and are categorized based on the time oftheir onset [1]. Acute reactions, which are mostly transient andresponsive to medication [2], occur within 1–6 weeks aftertherapy [1]. Early–delayed reactions occur within 3 weeks to
A. Horská (*) :A. Nidecker : J. Intrapiromkul : F. TannaziRussell H. Morgan Department of Radiology and RadiologicalScience, Division of Neuroradiology, Johns Hopkins UniversitySchool of Medicine, 600 N. Wolfe Street,Baltimore, MD 21287, USAe-mail: [email protected]
S. ArdekaniCenter for Imaging Science, Johns Hopkins University, 324B ClarkHall, 3400 North Charles Street, Baltimore, MD 21218, USA
L. J. BrantNIH/NIA/Gerontology Research Center, 5600 Nathan Shock Dr.,Baltimore, MD 21224, USA
M. Wharam JrDepartment of Radiation Oncology and Molecular RadiationSciences, Johns Hopkins University School of Medicine,401 North Broadway, Suite 1440, Baltimore, MD 21231, USA
E. M. MahoneDepartment of Neuropsychology, Kennedy Krieger Institute,1750 East Fairmount Ave, Baltimore, MD 21231, USA
Childs Nerv SystDOI 10.1007/s00381-013-2315-1

several months, and neurotoxic late–delayed effects of treat-ments typically manifest within several months to years aftertreatment completion [1]. More than 40 % of survivors ofchildhood brain tumors develop cognitive deficits attributed tothe tumor or the treatments [3]. Awell-established, influentialfactor related to development of cognitive impairment is CRT,particularly if administered at younger ages and with higherdoses. Tumor type, size and location, surgery, and systemicchemotherapy may also contribute to neurocognitive impair-ment, with potentially synergistic effects [3, 4]. Long-termneurocognitive impairment can negatively impact quality oflife and socioeconomic achievement in surviving patients [5].
Development of adverse neurocognitive effects has beenattributed mainly to injury of healthy white matter; however,therapies may impact all brain tissues [4]. The most commonlyobserved neurocognitive deficits in surviving children involveattention, memory, and processing speed [4, 5], functions in-fluenced by circuits comprising deep gray matter structures—basal ganglia, thalamus, and hippocampus. Frontal–basal gan-glia–thalamic circuits are involved in control of movement andprocesses leading to movements [6] and may also contribute toencoding and retrieval of declarative memories [7], functionsmediated by the medial temporal lobe. Considering therelevance of deep gray matter to neurocognitive domainsthat are impaired by treatment, studies of deep gray mattertissue with concurrent neuropsychological evaluation mayfurther improve our understanding of pathogenesis of neu-ropsychological dysfunction [3].
An earlier study reviewed patterns of abnormalities typicallyassociated with acute, early–delayed, and late–delayed effectson brain parenchyma as detected on clinical MRI scans [1].Advanced neuroimaging techniques may detect tissue impair-ment even in regions with normal appearance on conventionalMRI [8]. Diffusion tensor imaging (DTI), a technique thatprobes tissue microstructure by measuring microscopic motionof water molecules, has been used extensively in studies ofbrain development and has also been applied to study treatmenteffects in patients diagnosed with brain malignances. In healthydeveloping brain, DTI revealed age-related differences in frac-tional anisotropy (FA) and mean diffusivity, parameters char-acterizing microstructure, and directionality of white mattertracts and deep gray matter regions that function as their relaystations [9]. In pediatric medulloblastoma patients treated withsurgery, chemotherapy, and CRT, DTI detected white matterimpairment (low FA) even in regions demonstrating no abnor-malities on conventional MRI [10]. In patients with posteriorfossa tumors, administration of adjuvant therapy leads to amore pronounced damage to white matter microstructure thantreatment with surgery alone [11]. In childhood cancer survi-vors, white matter FA has been related to motor [12] andprocessing speed [12, 13]. To date, DTI studies focused mostlyon white matter, which is considered more sensitive to neuro-toxic treatment effects than gray matter [1, 14]. However, in a
recent pilot DTI study in children previously treated for medul-loblastoma, measurements were also performed in deep graymatter nuclei [15]. Apparent diffusion coefficient (ADC) was amore sensitive parameter than FA to detect differences betweenpatients and healthy controls in all selected white matter regionsand deep nuclei (thalamus and putamen) [15]. In the studycohort, higher mean ADC was associated with lower IQ; norelationship between mean FA and IQ was detected [15].
The main goal of this pilot prospective longitudinal studywas to use DTI to evaluate deep gray matter microstructure inpatients receiving CRTwith or without adjuvant chemotherapyearly in treatment (after surgery, if performed) and 6, 15, and27 months post-CRT. ADC in the thalamus, globus pallidus,putamen, caudate, and hippocampus was measured, and con-current neuropsychological evaluation was performed in pedi-atric patients diagnosed with brain malignancies (primarybrain tumors and leukemia) and a control group of healthychildren. We hypothesized that in patients, ADC would in-crease and corresponding neuropsychological performancewould decline following treatment. To determine if the impair-ment of deep gray matter microstructure is associated withdeficits in neuropsychological performance, correlation analy-ses between neuropsychological test scores and ADC in cor-responding gray matter regions were carried out.
Methods
Table 1 shows the demographic and clinical information onthe nine pediatric patients who received brain radiation (sevenboys; mean age 11.8±3.7 years, all right-handed). Over aperiod of 2.3 years, consecutive patients with brain malignan-cies who completed at least three MRI scans were selected.The control group consisted of nine typically developingchildren (two boys; mean age 11.2±1.8 years, five right-handed). The study was planned to include a baselineexamination (in patients, after surgery and before radiation)and 6-month, 15-month, and 27-month follow-up visits(in patients, after completion of CRT). All participants werefree of psychiatric disease based on assessments using theDiagnostic Interview for Children and Adolescents, fourthedition. Institutional Review Board approval and a signedwritten informed consent were obtained.
MRI was performed at 1.5 Tesla using the standard circu-larly polarized birdcage transmit–receive head coil. DTI datawere acquired using a single-shot diffusion-weighted spin-echoecho-planar imaging sequence with the following parameters:TE=93.7 ms, matrix size 96×96, field-of-view 240 mm, twob=0 s/mm2 images, maximum b=1,000 s/mm2, 15 noncol-linear diffusion gradient directions, two acquisitions, 24axial slices parallel to the anterior commissure–posteriorcommissure plane, 5 mm slice thickness, no gap; 4 min48 s scan time. The position and orientation of the DTI
Childs Nerv Syst

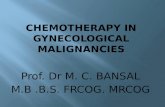
slices on a midsagittal image was used to prescribe thefollow-up examinations. Diffusion tensors were computedusing DTI Studio (cmrm.med.jhmi.edu); FA and ADC werecalculated. The FA maps were used to draw ROIs, whichwere superimposed on the ADC maps using the program“DSX” (godzilla.kennedykrieger.org). Since the diffusion ofwater molecules in gray matter is isotropic [16] and FA, ameasure of directionally restricted diffusion of watermolecules would be difficult to interpret, only ADC wasanalyzed. Mean ADC was evaluated in five regions-of-interest (ROIs) in both hemispheres: (1) thalamus, (2)globus pallidus, (3) putamen, (4) caudate head, and (5)hippocampal head. The ROIs were drawn at a correspond-ing level for all participants, encompassing the largestportion of the cross-sectional area according to a template(Fig. 1). This approach has been shown to have excellentinter-rater and intra-rater reproducibility [17]. The measure-ments were performed by a single reader, a neuroradiologist,two times and the measurements were averaged. The agreementbetween the twomeasurements was excellent (pooled data fromthe baseline visit, intraclass correlation coefficient=0.944). Tominimize partial volume effects with the cerebrospinal fluid, allpixels with FA values less than 0.15 were eliminated from theanalyses [18]. The ROIs in patients showed predominantlynormal appearance on conventional MRI. T2 abnormalities inproximity to or only partially involving an ROI were noted onlyin patient 2 (bilaterally in the hippocampus), patient 3 (unilat-erally in the caudate), and patient 5 (bilaterally in the thalamus).
Mean radiation doses to each particular region of the brain(Table 1) were calculated using the Pinnacle software (version 9)after overlaying the ROIs with the radiation treatment plan.
Neurobehavioral assessment was designed to provide adelineation of select neuropsychological functions usingnationally standardized tests with good test-rest reliabilitythat have been validated in the age range of interest. Weemphasized assessment of memory and motor speed whichconsidered to be most sensitive to radiation effects. Workingmemory was assessed using the Bead Memory Test (Stanford-Binet Intelligence Scale, fourth edition), a measure of visual–spatial working memory, and Auditory Working Memory(Woodcock Johnson-III), an assessment of auditory verbalmemory. Working memory tests are considered to be depen-dent on dorsolateral prefrontal–striatal circuitry, which in-cludes the caudate nucleus. Verbal memory was assessed usingthe Memory for Words Test (Woodcock Johnson-III), a mea-sure of short-term auditory verbal learning and declarativememory and considered to be dependent on subcortical sys-tems including the thalamus and the hippocampus. Motorspeed was assessed using Purdue Pegboard. The two-handtrial was analyzed for the present study given the group differ-ences in handedness. Measures of motor speed are consideredto be dependent on frontostriatal circuitry involving the motorcircuit, which includes the putamen and globus pallidus.T
able1
Clin
icalinform
ationon
patientsandradiationdosesto
theregionsof
interest
Sex
Age
(years)
Diagnosis
Tum
orlocatio
nTreatmentp
rior
toCRT(tim
eof
administrationbefore
CRT,
months)
Radiatio
ndose
(Gy)
Surgery
Chemotherapy
Steroids
THAL
GP
PUT
CAUD
HIPPO
1M
10.2
Tcellacutelymphocytic
leukem
iaNoCNStumor
(mediastinal
mass)
No
Tcellinductionchem
otherapy
(1.1)
Pred
(0.7)
18.6
18.6
18.7
18.6
18.7
2M
15.3
Recurrent
ependymom
aLefttem
poral(originaltumor:
lower
spine)
Yes
(0.9)
No
Dexa(0.8)
44.5
47.3
47.4
45.1
47.7
3M
11.8
Malignant
glioneuraltumor,
otherw
iseunclassifiable
Leftfrontal
Yes
(5.7)
No
No
53.6
50.8
48.6
50.5
46.2
4F
18.6
Germinom
aSuprasellar
Yes
(4.1)
CsPt/V
P-16/CTX/VCR(3.1)
HC(3.7)
23.1
25.7
24.8
27.0
23.7
5M
11.8
Undiagnosed
pinealmass
Pinealregion
No(V
Pshunt,open
biopsy)
No
No
54.3
44.6
29.5
26.3
20.3
6M
11.6
Craniopharyngioma
Suprasellar
Yes
(5.1)
No
Pred(4)
11.6
31.0
27.6
25.4
40.0
7M
5.5
Pilocytic
astrocytom
aRight
frontalsuprasellar/optic
Yes
(42.7)
CaPt(35.0),TMZ(16.5)
No
12.8
16.7
15.4
26.7
a
8F
8.7
Medulloblastoma
Posteriorfossa
Yes
(1.1)
No
Dexa(0.8)
42.4
34.7
29.8
25.3
32.4
9M
12.7
Medulloblastoma
Posteriorfossa
Yes
(0.8)
No
Dexa(0.7)
40.0
28.2
26.5
24.7
39.3
THALthalam
us,GP
globus
pallidus,PUTputamen,CAUD
caudatehead,HIPPO
hippocam
pus,CaP
tcarboplatin
,CsPtcisplatin
,CTX
cytosan,
Dexadexamethasone,HC
hydrocortisone,
Pred
prednisone,V
CRvincristine,TM
Ztemozolom
ide,VP-16etoposide
aThe
radiationdose
tothehippocam
palhead
inpatient
no.7
couldnotbe
measured(due
toasurgicalresectionon
oneside
andsevere
compression
bythetumor
onthecontralateralside).Age
atthe
baselin
evisit(patient
9,endof
CRT)isreported
Childs Nerv Syst

To account for heterogeneity and correlations in the out-come variable (ADC) resulting from individual repeated mea-surements over time and in different ROIs, linear mixed-effects models (LME) analyses were applied for statisticalevaluations . Differences in ADC between patients and con-trols at the four visits were examined, controlling for age andsex. The main LME analysis included fixed effects of group,sex, age, region, hemisphere, visit, and the interaction termsgroup × region, group × age, and group × visit. Post hocanalyses in individual ROIs included all significant terms ofthe main analysis (except those involving “region”) and theinteraction term group × visit. In individual ROIs, LME wasalso applied to examine differences in ADC among patientsreceiving radiation doses <20, 20–50, and >50 Gy, controllingfor visit and age. Post hoc comparisons in individual ROIs atthe four visits were performed using GLM ANOVA control-ling for age and side. LME analyses were also used to assessthe difference in neurobehavioral performance between patientsand controls (using raw scores of the neuropsychological tests)and among the visits controlling for age. Main effects (groupand visit) and the interaction terms group × visit and group ×age were used. To evaluate the relationship between neuropsy-chological test scores and ADC values, LME analyses of theneuropsychological scores with the terms group, visit, ADC,group × ADC, visit × ADC, and group × visit were applied. Toexamine if differences exist in the relationship between theneuropsychological test scores and ADC in the left and righthemispheres, the term “hemisphere” was also included in theseanalyses. To account for the effect of age, standard or z-scoreswere used. Statistical significance for all main analyses was setto p <0.05 and reduced to p <0.01 in all post hoc tests toaccount for multiple comparisons (five regions). Data are pre-sented as means ± standard deviations.
Results
The following number of DTI and neuropsychological (NP)datasets were obtained: at visit 1 (baseline), 8/9 (patients/controls) for both DTI and NP; at visit 2, 7/8 for DTI and 9/8
for NP; at visit 3, 7/8 for both DTI and NP; at visit 4, 8/9 forDTI and 7/9 for NP. Four patients hadDTI andNP data from allvisits. Data from the second visit of patient 6 could not be usedbecause of artifacts due to braces. The NP tests were completedwithin 3 months of the MRI examination in each subject. Dueto scheduling difficulties, in six patients, the baseline examina-tion was performed before the start of radiation (Table, patients1, 2, 3, 5, 6, and 7) and in two patients after the radiationtreatment was completed [after 2 and 8 days (patients 4 and 8)].Patient 9 missed the baseline examination. There was no sig-nificant difference in age between the patient group and thecontrol group at baseline (T test, p =0.26). The mean timeinterval between the baseline and each follow-up visit were:visit 2, 0.60/0.57 years (patients/controls); visit 3, 1.4/1.4 years;and visit 4, 2.3/2.5 years.
Mean ADC in examined ROIs: group differences
Figure 2 compares mean ADC values in patients and controlsin the five ROIs at each of the four visits. The main LMEanalysis included ADC data from the five ROIs in both hemi-spheres, in all subjects and at all visits, a total of 636 observa-tions (statistical power=0.63, correlation ρ =0.4). Mean ADCin patients (0.793±0.237⋅10−3 mm2/s) was 7.6 % higher than inthe control group (0.737±0.243⋅10−3 mm2/s; p =0.01). MeanADC and the group differences in mean ADC varied amongregions (region, p <0.0001; group × region, p <0.0001). ADCdecreased with age (p =0.004) and a 2.8 % higher meanADC was detected in the left hemisphere than in theright hemisphere (p =0.041). No overall ADC differencesbetween boys and girls (sex, p =0.48) and among visits(p =0.067) were detected.
The post hoc analyses in individual ROIs revealed asignificant difference in mean ADC between patients andcontrols in the hippocampus (region 5), with an overall24 % higher mean ADC (1.05±0.33⋅10−3 mm2/s) in patients(group, p =0.003) across the visits (group × visit, p =0.25).The group differences remained significant (p =0.005)even after removing data of patient 2 who had abnormalhippocampal appearance on conventional T2-weighted MRI
Fig. 1 Five regions of interestdrawn on the FA map of a12-year-old healthy control.Regions 1 (thalamus) and 4(caudate head) are shown on theleft image , regions 2 (globuspallidus) and 3 (putamen) areshown on the center image , andregion 5 (hippocampal head) isshown on the right image
Childs Nerv Syst

(see Methods, section MRI). At individual visits, significantgroup differences were detected at baseline (37 % higherADC in patients, p=0.003) and at the fourth visit (23 % higher
ADC in patients, p =0.006) (visit 2, p =0.014; visit 3, p =0.087)(Fig. 2). In the thalamus (region 1), globus pallidus (region 2),putamen (region 3), and caudate (region 4) the post hocLME analyses did not reveal any significant differencesbetween patients and controls (group, p =0.73, 0.21, 0.037,and 0.015, respectively).
There was no difference in the mean radiation dosesamong the ROIs (thalamus 33.4±17.0 Gy, globus pallidus33.1±12.3 Gy, putamen 29.8±11.4 Gy, caudate 30.0±10.5 Gy,hippocampus 33.5±11.5Gy) between hemispheres and betweenyounger and older patients. No differences in ADC amongpatients who received radiation doses <20, 20–50, and >50 Gywere detected in any ROI (p=0.14–0.75).
Neuropsychological performance: differencesbetween patients and controls
On the test of visual–spatial working memory (BeadMemory),the main LME analysis detected a decrease in scores in patientsover time [age-adjusted mean scores, 0.20±0.98 (baseline),−0.58±1.36 (visit 4)] and improved performance in controls[age-adjusted mean score, −0.66±1.33 (baseline), 0.20±1.11(visit 4)] (group × visit, p =0.036), with no overall difference inperformance between groups (group, p =0.60). The group dif-ferences in motor speed as assessed by the Purdue Pegboardtest were not significant (group, p =0.08; controls showed atrend to a better performance at all four visits). No significantoverall differences between patients and controls were detectedin verbal working memory or verbal memory nor were thegroup by visit interactions for these variables significant.
Results of LME analyses showing a significant relationshipbetween neuropsychological performance and ADC (ADC orADC × visit, 0.0001<p ≤0.02), including data from all visits,are presented in Fig. 3. These analyses also indicated differ-ences between controls and patients as shown by at least onesignificant term including group (0.002≤p <0.025). Figure 3shows that the test scores on visual–spatial working memory(Bead Memory test), auditory working memory, and motorspeed (Purdue Pegboard) decreased with increasing ADC incontrols. In patients, a negative relationship between motorspeed performance and ADC was also detected, although atoverall lower scores. The relationships between the tests ofvisual–spatial and auditory working memory and ADC didnot follow the trends observed in controls. The overalltrends and statistical significance were confirmed in addi-tional analyses performed without inclusion of the mostextreme values in patients (0.6⋅10−3<ADC<0.8⋅10−3 mm2/s).No relationship between memory performance and hippo-campal or thalamic ADC was detected in either group. Innone of the analyses, the term “hemisphere” (indicating left–right differences) reached statistical significance, suggestingthat data obtained from both hemispheres accounted for theobserved correlations.
Fig. 2 Comparison ofmean ADC values in the thalamus (THAL), globuspallidus (GP), putamen (PUT), caudate (CAUD), and hippocampus(HIPPO) between patients and healthy controls at the four visits. Theerror bars represent standard deviations. Significant group differencesbetween patients and healthy children (hippocampus, main LME analysis,p<0.01) are marked by an asterisk
Childs Nerv Syst

Discussion
In children with brain malignancies treated with CRT, conven-tional MRI showed mostly normal findings in the evaluateddeep gray matter regions both at baseline and post-radiation.However, DTI detected a 24% higher overall mean ADC in thehippocampal region in patients, indicating impairment in tissuemicrostructure. Significantly elevated ADC was detected bothat baseline and 27 months post-CRT. In another DTI studyevaluating long-term treatment effects (more than 1 year aftertherapy) inmedulloblastoma and pilocytic astrocytoma patients,widespread decreases of FA were detected in both patientgroups compared with controls. The abnormalities were lesspronounced in the patients with pilocytic astrocytoma, who didnot receive chemotherapy and CRTwhile the medulloblastomapatients did [11]. Our results thus complement this and otherprevious DTI studies of whitematter [12, 13] by detecting tissueinjury in the gray matter and at an early stage of the treatmentprocess. The data also suggest that combined adverse effects ofthe disease, initial treatment with surgery, and subsequent che-motherapy andCRTmay have contributed to graymatter injury.This explanation is supported by our related volumetric MRIstudy, reporting reduced regional cerebellar volumes at a base-line visit and at similar time points relative to CRT [19].Elevated ADC in the hippocampus in the current study wasnot accompanied by concurrent impairment on memory perfor-mance in the studied patient group. However, in both patientsand controls, performance on the Purdue Pegboard declinedwith increasing ADC in the globus pallidus and putamen,suggesting a relationship between motor function and micro-structure of corresponding regions of the basal ganglia.
Of the deep gray matter regions examined, ADC differencesbetween patients and controls were observed only in the hip-pocampus. In an earlier longitudinal study on medulloblastomapatients, a decline in hippocampal volume was observed overthe first 2 years post-treatment, followed by volume increase.
�Fig. 3 Relationship between neuropsychological performance andADC in subcortical gray matter. Data from all subjects at all visitsare presented in the figure. The regression lines represent changes inneuropsychological test scores with ADC averaged across the fourvisits in patients and controls. The regression lines were calculatedfrom all significant factors that comprised the final models of therespective LME analyses comparing both groups. Compared withleast squares regression lines, LME regression lines take into account thevariability of the data. In all LME analyses, the p values including the factor“ADC” or the interaction “ADC” by “visit” were ≤0.02. In controls,neuropsychological performance on working memory (a, b) and motor(c, d) tests improved with decreasing ADC. In patients, motor performancedecreased with increasing ADC in the globus pallidus (c) and putamen (d),although at overall reduced scores. For the tests onworkingmemory (a, b),the relationship between the test scores and ADC did not follow the trendsobserved in controls. The calculations of the regression lines for patients in(a) and (b) included only data for ADC<1.1⋅10−3 mm2/s; the outliers arestill shown in the figure
Childs Nerv Syst

The pattern of volume changes was different from growthpattern previously reported in healthy children and could notbe accounted for by tissue atrophy [20]. Since CRT can causeprofound inhibition of hippocampal neurogenesis [21], our datamay be of interest for future studies on short- and long-termeffects of CRT on the hippocampal region and associatedcognitive functions. Data from a larger group of pediatricpatients (N =19) including those examined in this studyshowed that higher radiation doses to the hippocampus orthe temporal lobes have a more pronounced effect onneurocognitive decline than irradiation of the subventricularzone, which also contains neural progenitor cells [22].
DTI is a sensitive technique for studying brain develop-ment and maturation. In normal developing deep gray matter,mean diffusivity of water decreases with age. The age-relateddecreases in diffusivity are most pronounced until 2 years ofage with a more gradual decrease thereafter [16]. Develop-ment of gray matter microstructure as detected by DTI con-tinues until 24 years of age or later [9]. As the age-relateddecreases in water diffusivity in gray matter are related todecrease in water content and increase in macromolecularconcentrations [16] elevated hippocampal ADC values inour patients compared with age-matched healthy controlsmay suggest disruption of these processes.
A previous cross-sectional study reported elevated ADC inthe thalamus (by 53 %) and the putamen (by 42 %) in eightchildren treated with cranio-spinal radiation for medulloblas-toma examined at a mean time of 2.5 years post-diagnosis[15]. In our longitudinal study, no group differences weredetected in the thalamus and the putamen. This discrepancymay be explained by differences between the patient groupsand by controlling for CSF (to account for potential reductionsin tissue volume) in our study. Additionally, differences inradiation doses and treatment plans have to be considered. Ourstudy included patients with both lower (<23.4 Gy) and higherdoses (>36 Gy) to the thalamus than the medulloblastomapatients examined previously [15].
The findings of significant negative associations betweenthe performance on tests of working memory and motor speedand deep gray matter ADC in healthy children are in agree-ment with previousMRI-based studies on functional networksinvolving the frontal, prefrontal, and striatal regions in thedeveloping brain [23–25]. A similar trend of decreasing testscores with increasing ADC was also observed in patients onthe test of motor speed but not on the tests of workingmemory, possibly suggesting disruption of the pathwayslinking the cortical regions with the striatum. None of theanalyses on the relationship between subcortical ADC valuesand verbal memory, including analyses performed in controlsonly provided significant results. However, in studies of adults,a significant correlation between hippocampal diffusivity andverbal memory function was reported in patients with smallvessel disease [26], temporal lobe epilepsy [27], MCI, and early
Alzheimer's disease [28]. In patients with small vessel disease,the relationship between hippocampal diffusivity and verbalmemory performance was highly significant particularly in thesubgroup of patients who had normal hippocampal volumes,suggesting that ADC may be an early marker of underlyingneurodegenerative disease [26]. In the future, it may be inter-esting to examine if abnormal hippocampal ADC detected earlyin the course of treatment for brain malignancies would predictmemory deficits at longer intervals from treatment completion.
While the limitation of this pilot study to a small number ofpatients with brain malignancies has to be acknowledged,longitudinal design and data sampling in multiple regions inboth hemispheres provided a large number of ADC data.However, a larger group of patients (receiving a wide rangeof radiation doses) examined at a longer follow-up would beneeded to study the effects of radiation doses on deep graymatter nuclei ADC in detail. Although the patient groupincluded more males, no consistent differences in mean diffu-sivity in deep gray matter nuclei between males and femaleswere reported recently [29].
Summary
Presence of brain malignancies and their treatment may leadto disruption of gray matter microstructure. The most interest-ing finding in our study was the detection of abnormal ADC inthe hippocampal region early in therapy. The study resultssuggest that (a) differences in tissue sensitivity to disease- andtreatment-related impairment among deep gray matter regionsmay exist and (b) tissue microstructure of deep gray matternuclei, as measured with DTI, may be associated with neuro-psychological performance (motor function).
Acknowledgments The study was supported by the National Institutes ofHealth R01 NS042851; P30HD024061-16; Johns Hopkins UniversitySchool ofMedicine Institute for Clinical and Translational Research, NationalInstitutes of Health/National Center for Research Resources Clinical andTranslational Sciences Awards Program, UL1-RR025005; Intellectual andDevelopmental Disabilities Research Center, Imaging Core, P30HD024061,National Institute of Child Health and Human Development.
We would like to thank Dr. Todd McNutt for his help with theevaluation of radiation doses and Amanda Barnes, Cynthia Schultz, andCynthia Maranto for their assistance with recruitment of participants anddata acquisition.
Conflict of interest The authors declare that they have no conflict ofinterest.
References
1. Ball WS Jr, Prenger EC, Ballard ET (1992) Neurotoxicity of radio/chemotherapy in children: pathologic andMR correlation. AJNRAmJ Neuroradiol 13:761–776
Childs Nerv Syst

2. Lawrence YR, Li XA, el Naqa I, Hahn CA,Marks LB, Merchant TE,Dicker AP (2010) Radiation dose-volume effects in the brain. Int JRadiat Oncol Biol Phys 76:S20–S27
3. Ullrich NJ, Embry L (2012) Neurocognitive dysfunction in survivorsof childhood brain tumors. Semin Pediatr Neurol 19:35–42
4. Butler RW, Haser JK (2006) Neurocognitive effects of treatment forchildhood cancer. Ment Retard Dev Disabil Res Rev 12:184–191
5. Ellenberg L, Liu Q, Gioia G, Yasui Y, Packer RJ, Mertens A,Donaldson SS, Stovall M, Kadan-Lottick N, Armstrong G,Robison LL, Zeltzer LK (2009) Neurocognitive status in long-termsurvivors of childhood CNS malignancies: a report from theChildhood Cancer Survivor Study. Neuropsychology 23:705–717
6. Haber SN, Calzavara R (2009) The cortico-basal ganglia integrativenetwork: the role of the thalamus. Brain Res Bull 78:69–74
7. Scimeca JM, Badre D (2012) Striatal contributions to declarativememory retrieval. Neuron 75:380–392
8. Robbins ME, Brunso-Bechtold JK, Peiffer AM, Tsien CI, Bailey JE,Marks LB (2012) Imaging radiation-induced normal tissue injury.Radiat Res 177:449–466
9. Lebel C, Walker L, Leemans A, Phillips L, Beaulieu C (2008)Microstructural maturation of the human brain from childhood toadulthood. Neuroimage 40:1044–1055
10. Khong PL, Kwong DL, Chan GC, Sham JS, Chan FL, Ooi GC(2003) Diffusion-tensor imaging for the detection and quantificationof treatment-induced white matter injury in children with medullo-blastoma: a pilot study. AJNR Am J Neuroradiol 24:734–740
11. Rueckriegel SM, Driever PH, Blankenburg F, Ludemann L, HenzeG, Bruhn H (2010) Differences in supratentorial damage of whitematter in pediatric survivors of posterior fossa tumors with andwithout adjuvant treatment as detected by magnetic resonance diffu-sion tensor imaging. Int J Radiat Oncol Biol Phys 76:859–866
12. Aukema EJ, CaanMW, Oudhuis N, Majoie CB, Vos FM, Reneman L,Last BF, Grootenhuis MA, Schouten-van Meeteren AY (2009) Whitematter fractional anisotropy correlates with speed of processing andmotor speed in young childhood cancer survivors. Int J Radiat OncolBiol Phys 74:837–843
13. Palmer SL, Glass JO, Li Y, Ogg R, Qaddoumi I, Armstrong GT,Wright K, Wetmore C, Broniscer A, Gajjar A, Reddick WE (2012)White matter integrity is associated with cognitive processing inpatients treated for a posterior fossa brain tumor. Neuro Oncol 14:1185–1193
14. Leibel SA, Sheline GE (1987) Radiation therapy for neoplasms of thebrain. J Neurosurg 66:1–22
15. Mabbott DJ, Noseworthy MD, Bouffet E, Rockel C, Laughlin S(2006) Diffusion tensor imaging of white matter after cranial radia-tion in children for medulloblastoma: correlation with IQ. NeuroOncol 8:244–252
16. Mukherjee P,Miller JH, Shimony JS, Philip JV, Nehra D, Snyder AZ,Conturo TE, Neil JJ, McKinstry RC (2002) Diffusion-tensor MRimaging of gray and white matter development during normal humanbrain maturation. AJNR Am J Neuroradiol 23:1445–1456
17. Bonekamp D, Nagae LM, Degaonkar M, Matson M, Abdalla WM,Barker PB, Mori S, Horska A (2007) Diffusion tensor imaging inchildren and adolescents: reproducibility, hemispheric, and age-related differences. Neuroimage 34:733–742
18. Cercignani M, Bozzali M, Iannucci G, Comi G, Filippi M (2001)Magnetisation transfer ratio andmean diffusivity of normal appearingwhite and grey matter from patients with multiple sclerosis. J NeurolNeurosurg Psychiatry 70:311–317
19. Horska A, Laclair A, Mohamed M, Wells CT, McNutt T, Cohen KJ,Wharam M, Mahone EM, Kates W (2010) Low cerebellar vermisvolumes and impaired neuropsychologic performance in childrentreated for brain tumors and leukemia. AJNR Am J Neuroradiol 31:1430–1437
20. Nagel BJ, Palmer SL, Reddick WE, Glass JO, Helton KJ, Wu S,Xiong X, Kun LE, Gajjar A, Mulhern RK (2004) Abnormal hippo-campal development in children with medulloblastoma treated withrisk-adapted irradiation. AJNR Am J Neuroradiol 25:1575–1582
21. Monje M (2008) Cranial radiation therapy and damage to hippocam-pal neurogenesis. Dev Disabil Res Rev 14:238–242
22. Redmond K, Ishaq O, Ford E, Batra S, Terezakis S, McNutt T,Kleinberg L, Wharam M, Mahone E, Horska A (2013) Associationbetween radiation dose to neuronal progenitor cell niches andtemporal lobes and performance on neuropsychological testing inchildren: a prospective study. Neuro Oncol 15:360–369
23. Klingberg T (2006) Development of a superior frontal-intraparietalnetwork for visuo-spatial working memory. Neuropsychologia 44:2171–2177
24. Olesen PJ, Nagy Z, Westerberg H, Klingberg T (2003) Combinedanalysis of DTI and fMRI data reveals a joint maturation of white andgrey matter in a fronto-parietal network. Brain Res Cogn Brain Res18:48–57
25. Ozturk A, Degaonkar M, Matson MA, Wells CT, Mahone EM,Horska A (2009) Proton MR spectroscopy correlates of frontallobe function in healthy children. AJNR Am J Neuroradiol 30:1308–1314
26. van Norden AG, de Laat KF, Fick I, van Uden IW, van OudheusdenLJ, Gons RA, Norris DG, Zwiers MP, Kessels RP, de Leeuw FE(2012) Diffusion tensor imaging of the hippocampus and verbalmemory performance: the RUN DMC study. Hum Brain Mapp 33:542–551
27. Lui YW, Nusbaum AO, Barr WB, Johnson G, Babb JS, Orbach D,Kim A, Laliotis G, Devinsky O (2005) Correlation of apparentdiffusion coefficient with neuropsychological testing in temporallobe epilepsy. AJNR Am J Neuroradiol 26:1832–1839
28. Fellgiebel A, Yakushev I (2011) Diffusion tensor imaging of thehippocampus in MCI and early Alzheimer's disease. J AlzheimersDis 26(Suppl 3):257–262
29. Pal D, Trivedi R, Saksena S, Yadav A, Kumar M, Pandey CM,Rathore RK, Gupta RK (2011) Quantification of age- and gender-related changes in diffusion tensor imaging indices in deep greymatter of the normal human brain. J Clin Neurosci 18:193–196
Childs Nerv Syst