Diabetes and COVID-19: Risks, Management, and Learnings From … · 2020-06-16 · OR 2.67, 95% CI...
Transcript of Diabetes and COVID-19: Risks, Management, and Learnings From … · 2020-06-16 · OR 2.67, 95% CI...

Diabetes and COVID-19: Risks,Management, and Learnings FromOther National Disastershttps://doi.org/10.2337/dc20-1192
Evidence relating to the impactof COVID-19 inpeoplewithdiabetes (PWD) is limitedbut continuing toemerge.PWDappear tobeat increased riskofmoresevereCOVID-19 infection, though evidence quantifying the risk is highly uncertain. The extent towhich clinical and demographic factors moderate this relationship is unclear, thoughsignals are emerging that link higher BMI and higher HbA1c to worse outcomes inPWDwithCOVID-19.Aswell asposingdirect immediate risks toPWD,COVID-19alsorisks contributing to worse diabetes outcomes due to disruptions caused by thepandemic, including stress and changes to routine care, diet, and physical activity.Countries have used various strategies to support PWD during this pandemic. Thereis a high potential for COVID-19 to exacerbate existing health disparities, andresearch and practice guidelines need to take this into account. Evidence on themanagement of long-termconditions during national emergencies suggests variousways to mitigate the risks presented by these events.
People with diabetes (PWD) have been identified as being at increased risk of seriousillness from COVID-19. COVID-19 also presents substantial indirect risks to PWDthrough disruptions in health care and lifestyle factors. Understanding these risks andbest ways tomitigate them in the short and longer term is key to facilitating informeddecision-making during and after the COVID-19 pandemic.Evidence relating to COVID-19 and diabetes is limited but continuing to emerge.
In this Perspective, we summarize evidence identified through rapid reviews. Weconsider direct and indirect risks posed to PWD by COVID-19 and managementconsiderations for PWD both with and without COVID-19 infection. Recognizinglimitations in evidence related to COVID-19, we also bring together leaders in diabetescare from countries with high rates of COVID-19, highlighting experiences from themost affected countries including Italy, France, China, the U.K., and the U.S.
DIABETES AND RISKS FROM COVID-19
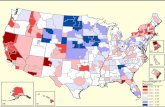
COVID-19 Infection: Contracting the DiseaseIt is unclear if PWD are more likely to contract COVID-19. PWD are considered atincreased risk of infection generally, which has been extended to COVID-19 (1).Community testing for COVID-19 remains limited, hence data predominantly comefromhospitalized cohorts. Systematic reviews primarily consisting of data fromChinahave estimated rates of 8% (95% CI 6–11%) (2), 7.87% (95% CI 6.57–9.28%) (3), and9.7% (95% CI 6.9–12.5%) (4) of diabetes in people hospitalized with COVID-19. Thepercentage hospitalization appears higher in the U.S., where from February 12 to 28March2020, PWDaccounted for 10.9%of all COVID-19patients (similar to theproportionof the U.S. population with diabetes), 24% of hospitalized cases (non–intensive care unit
1Centre for Evidence-Based Medicine, NuffieldDepartment of Primary Care Health Sciences,University of Oxford, Oxford, U.K.2Nuffield Department of Primary Care HealthSciences, University of Oxford, Oxford, U.K.3Medical Sciences Division, University of Oxford,Oxford, U.K.4University of North Carolina School of Medicine,Chapel Hill, NC5Department of Clinical and Experimental Med-icine, Section of Metabolic Diseases and Diabe-tes, University of Pisa, Pisa, Italy6Peking University Diabetes Center, Peking Uni-versity People’s Hospital, China7Federation de Diabetologie, Bichat Hospital, As-sistance Publique–Hopitaux de Paris, Paris, France8INSERM, UMR_S 1138, Centre de Recherche desCordeliers, Paris, France9UFR de Medecine, Universite de Paris, Paris,France10Diabetes Research Centre, University of Leices-ter, Leicester, U.K.
Corresponding author: [email protected]
Received19May2020andaccepted19May2020
This article is part of a special article collectionavailable at https://care.diabetesjournals.org/collection/diabetes-and-COVID19.
© 2020 by the American Diabetes Association.Readersmayuse this article as longas thework isproperly cited, the use is educational and not forprofit, and the work is not altered. More infor-mation is availableathttps://www.diabetesjournals.org/content/license.
Jamie Hartmann-Boyce,1 ElizabethMorris,2
Clare Goyder,2 Jade Kinton,3
James Perring,3 David Nunan,1
Kamal Mahtani,1 John B. Buse,4
Stefano Del Prato,5 Linong Ji,6
Ronan Roussel,7,8,9 and Kamlesh Khunti10
Diabetes Care 1
DIABETES
ANDCOVID-19
Diabetes Care Publish Ahead of Print, published online June 16, 2020

[ICU]), and 32% of ICU admissions (5). Arecent (preprint) U.K. study found uncom-plicated diabetes to be the second mostcommon comorbidity (19%) in patientshospitalized with COVID-19; complicateddiabetes is reported in a figure only butprevalence looks to be approximately6.5% (6).
COVID-19 Infection: Disease SeverityThough issues with study quality andimprecision make it extremely difficultto quantify, current data suggest thatCOVID-19 is associated with worse out-comes in PWD. Reports which aggregatedata frommultiple centers are summarizedin Table 1. There is a notable paucity of dataon what moderates the relationship be-tween diabetes and COVID-19 severity.Increased age, being male, hyperten-sion, and cardiovascular comorbidities
are associated with increased risks forCOVID-19 severity (7) and are likely tobe closely related to diabetes status. It isplausible that BMI (8), ethnicity (9), typeof diabetes, diabetes control, and cer-tain medications (10) all may also play arole. In twocohort studies (FranceandtheU.K., U.K. study preprint) in PWD hospital-ized with COVID-19, higher BMI was pos-itively associated with worse COVID-19outcomes when compared with peoplewith BMI 25–29.9 kg/m2 (11,12). Data ondiabetes type and COVID-19 outcomesare only beginning to emerge, but pre-liminary (not yet peer reviewed) datafrom England (see Table 1) suggests risksmay be higher in people with type 1diabetes compared with type 2 (thoughrisk was increased in all PWD regardlessof type) (12). Data on glucose control andCOVID-19 outcomes are discussed below.
Association Between Blood GlucoseControl and COVID-19 Outcomes
There are limited data to date on theassociation between blood glucose con-trol and COVID-19 outcomes. A retro-spective study of 451 people with COVID-19with diabetes and/or hyperglycemiafrom the U.S. reported that people withuncontrolled hyperglycemia had longerlength of stay and higher mortality com-pared with people without diabetes oruncontrolledhyperglycemia (13).Anotherretrospective study of people with type 2diabetes from China reported that well-controlled blood glucose correlated withimproved outcomes in infected patients(14). Worse infection may predispose tomore difficulty managing blood glucose,so the causal mechanism behind correla-tions between glucose control and worseCOVID-19 outcomes is unclear.
Table 1—Aggregated data (across studies or centers) on COVID-19 severity in PWD*
Study design CountryNumberof studies
Number ofparticipants Outcome measure Risk estimate
Systematic review andmeta-analysis (2)
Multiple 8 3,076 Risk of diabetes in severe patientscompared with nonsevere patients
OR 2.07, 95% CI 0.89–4.82
Systematic review andmeta-analysis (63)**
Multiple 9 2,103 Risk of diabetes in severe patientscompared with nonsevere patients
OR 2.67, 95% CI 1.91–3.7
Systematic review andmeta-analysis (4)
Multiple 6 1,527 Risk of diabetes in severe/ICU patientscompared with nonsevere (non-ICU)patients
RR 2.21, 95% CI 0.88–5.57
Meta-analysis (64) China 12 2,018 Diabetes rate ratio among patients withmore severe versus those with lesssevere infection
Rate ratio 2.26, 95% CI1.47–3.49
Chinese Centers forDisease Control andPrevention report (65)
China n/a 72,314 Case fatality rate 7.3% in PWD (comparedwith 2.3% overall)
U.S. Centers for DiseaseControl and Preventionreport (5)
USA n/a 74,439 Not hospitalized PWD5 6% of all COVID-19 casesHospitalized, not in ICU PWD524%of all COVID-19 casesAdmitted to ICU PWD532%of all COVID-19 cases
Multicenter cohort study(66)
China n/a 191 Risk of in-hospital death in PWDcompared with those without(unadjusted)
OR 2.85, 95% CI 1.35–6.05
Retrospective review (67) China n/a 1,590 Likelihood of reaching composite endpoint (admission to ICU, intensiveventilation,ordeath) inPWDcomparedwith thosewithout (age- and smoking status–adjusted)
HR 1.59, 95% CI 1.03–2.45
Retrospective cohortstudy (15)**
U.K. n/a 17,425,445(5,683 deathsattributed toCOVID-19)
Risk of in hospital death inPWDcomparedwith those without (age-, sex-, andcomorbidities-adjusted)
HbA1c , 7.5% (58 mmol/mol);HR 1.50, 95% CI 1.40–1.60.HbA1c $ 7.5% (58 mmol/mol);2.36 (2.18–2.56)
Population cohort study(12)**
U.K. n/a 61,414,470(23,804 COVID-19–relateddeaths)
Risk of in-hospital death in PWDcompared with those without(adjusted for age, sex, deprivation,ethnicity, geographical region)
Type 1 diabetes OR 3.50 (95%CI 3.15–3.89); type 2 diabetesOR 2.03 (95% CI 1.97–2.09)
HR, hazard ratio; OR, odds ratio; RR, risk ratio. *Definition of severe disease was often not clear; we report here what was reported in the primaryliterature.Many of the systematic reviews include overlapping studies and have issueswith quality and reporting. **Preprintdmethods and data havenot been subject to peer review.
2 Diabetes and COVID-19 Diabetes Care

Two recent U.K. studies (both preprint)reported that diabetes was independentlyassociated with a higher risk of deathwhich increased with higher HbA1c (12,15).Comparedwith peoplewithout diabetes,one study reported that PWDwith HbA1c.7.5% (58 mmol/mol) had a higherchance of in-hospital death than thosewith HbA1c,7.5% (,7.5% HR 1.50 [95%CI 1.40–1.60], $7.5% HR 2.36 [2.18–2.56]) (15). In a separate analysis, PWDwith HbA1c .10% (86 mmol/mol) had ahigher risk of in-hospital death related toCOVID-19 than those with an HbA1c of6.5–7% (48–53mmol/mol) (HbA1c.10%compared with HbA1c 6.5–7% adjustedHR 2.19 [95% CI 1.46–3.29] for type 1diabetes, 1.62 [95% CI 1.48–1.79] fortype 2; in type 2 diabetes patients asignificant difference was also detectedwhen comparing HbA1c values .7.5%[59 mmol/mol] to the reference cate-gory) (12). These data suggest that di-abetes control preinfection has a role toplay in COVID-19outcomes. In contrast, aFrench observational study in PWD hos-pitalized with COVID-19 did not find anassociation between long-term glucosecontrol and COVID-19 outcomes but hada smaller sample (11).
Indirect Risks to PWD Posed byCOVID-19Health care services, and in some casesaccess to medication and supplies, havebeen disrupted by COVID-19. Evidencefrom other national emergencies showsthat such disruptions can lead to worsediabetes outcomes during and after theseevents (16–18). Diet and physical activityaremainstays of diabetes self-managementand can reduce risk of worse outcomes inPWDandthosewithcardiometabolicmulti-morbidities (19). Though yet to be ad-dressed by the COVID-19 literature, thepandemic presents significant disruptiontoboth: aU.S. surveyof PWD foundmorethan a third of respondents reportedtheir diet is now less healthy, and halfreport exercising less (20). The currentpandemic and social isolation are likely toincrease rates of anxiety and depression,which may also lead to poor adherence ofmedications and worsening of risk factorcontrol (21,22).
MANAGINGDIABETES DURINGTHECOVID-19 PANDEMIC
Reducing Risk from COVID-19There is little evidence on how PWD canreduce their risk during the COVID-19
pandemic beyond following general in-fection control guidance within eachcountry. More frequent blood glucosemonitoring (in people who self-monitor)has been suggested, though it is unclearwhat evidence was used to make theserecommendations (1).
Considerations for DiabetesManagement in All PWDFigure 1 summarizes specific considera-tions for diabetes management duringnational emergencies.
Self-management
There is little information on the effective-ness of self-management/self-educationduring the pandemic. A variety of onlineservices have been implemented buthave yet to be assessed (see EXPERIENCES
FROM COUNTRIES WITH HIGH RATES OF COVID-19).Thewider literatureon care of long-termconditions during national emergenciessuggests a role for educationalmaterials(23). Evidence for interventions aimingto optimize self-management in PWDthat are potentially feasible in disastercontexts include mobile phone apps (24),web- or computer-based interventions(25), text messaging (26,27), and self-monitoring of blood glucose (28,29).The latter two show the most promisebased on the available literature. How-ever, the interventions tested may notbewidely available ormay require healthcare resources to be set up. In addition,choice of format should be tailored topatient preferences, which will vary byage and sociodemographic group (30).
Diabetes Services
Guidelines for routine diabetes care duringthe COVID-19 pandemic vary by country.Themes are summarized in Table 2. Studiesof remote consultations have generallyfound positive results, though their gen-eralizability to the current pandemicmaybe limited (31). Within diabetes, there islittle evidence to support or oppose re-mote support (32,33).
MentalHealthandDiabetes-RelatedDistress
There are overarching concerns aboutthe impact of the COVID-19 pandemic onmental health and wellbeing (34,35).PWD are more prone to mental healthissues than the general population (36).Adherence to treatment can worsenwhen people are distressed or have de-pression (21), as seen both during andafter disasters (37,38). We found no ev-idencedirectlypertaining tomanagement
of diabetes-related anxiety or distressduring this pandemic. In the generalliterature, there is mixed evidence oninterventions to reduce diabetes-relateddistress, and the vast majority of inter-ventions tested involve face-to-face con-tact; an unsuitable format in the currentcontext (39).
Managing COVID-19 in PWDManagement of PWD with COVID-19generally follows standard sick-day rules.Considerations that may be specific toCOVID-19 are summarized below.
Medication
MostCOVID-19–relatedconsensus state-ments recommend stopping metforminand sodium–glucose cotransporter 2 in-hibitors (SGLT2i) during acute illness andfollowing the sick-day rules. Dipeptidylpeptidase 4 inhibitors (DPP-4i), glucagon-like peptide 1 receptor agonists (GLP-1RA),and insulinarethepreferredoptionsin particular for hospitalized patients(see Fig. 2) (40,41). There has been somediscussion regarding use of ACE inhibitorsand angiotensin receptor blockers (ARBs)being associatedwithworse outcomes inCOVID-19, particularly in PWD. However,in view of data showing potential bene-fits, the current recommendation is tocontinue with these therapies (40).
A number of studies are currentlytesting chloroquine/hydroxychloroquinefor prevention ormanagement of COVID-19.Careful glucose monitoring will be re-quired in PWD due to these drugs’ anti-diabetic properties, with the potential riskof hypoglycemia that is associated with in-creased risk of cardiac arrhythmia, cardio-vascular events, and mortality (42).
Management in Hospital
Guidance emphasizes the importance ofreferring to local specialist diabetes teamsand of managing hyperglycemia (43). Anarrative review suggests insulin is thepreferred agent for control of hypergly-cemia in this context (1). In the U.S., amajor early focus for hospital manage-mentwas tomove inpatient care for PWDto “virtual” formats where possible, toreduce the need for personal protectiveequipment. This included use of electronichealth records to interrogate data, tele-phone communication between diabetescare providers and inpatients andhospitalstaff, expanded “diabetes self-managementprotocols” allowing selected inpatients tomonitor their own glucose and self-administer insulin with oversight and advice
care.diabetesjournals.org Hartmann-Boyce and Associates 3

from the virtual care team, and, in someinstitutions, initiating inpatient continuousglucose monitoring and/or flash systems.To minimize the need for ICU beds, severalinstitutions launched subcutaneous insulinprotocols for the treatment of diabeticketoacidosisonfloorswithadequatenurs-ing staffing. Virtual diabetes care teamsfocused on supporting transitions to lowerlevels of care or outpatient settings.
EXPERIENCES FROM COUNTRIESWITH HIGH RATES OF COVID-19
We summarize here experiences fromfive countries that have had significantCOVID-19 outbreaks.
ChinaDuring the outbreak in China, many PWDwere unable to access health care pro-viders (HCPs) or medical supplies due tostay-at-home orders or quarantine. Hos-pitals reduced the number of appoint-ments drastically. Tomitigate the impactof those changes on diabetes manage-ment, several organizations issued guid-ance to PWD on how to cope with thesituation (44,45). The guidance devel-oped by the Chinese Geriatric EndocrineSociety mainly focused on preventionand early discovery of hyperglycemic cri-ses and management of medications andprovided detailed instructions on how toget access to certified internet-basedmedical services through smartphones(45). If PWD urgently needed to see anHCP in hospital, detailed guidance on
how to prepare for consultations beforeleaving home and minimize exposure tothe virus were given en route and duringthe hospital visit. Guidance was pro-moted in the form of reading materialand lectures given by medical professio-nals through internet-basedpublicmediasuch as Baidu Health (an equivalent ofGoogle in China) and theWeChat mobileapp. An expert recommendation on in-sulin treatment of hyperglycemia in patientsaffected with COVID-19 was developed(46).
FranceOn 12March, President Macron orderedmost people to stay at home, especially“at-risk” groups, including PWD. ManyPWD were struck by the announcementand were not expecting to be publiclyidentified as such, without answers tobasic questions. On 18March, a group ofHCPs and researchers from the Federa-tion of Diabetology, launched aweb app,CoviDIAB, to provide PWDwith diabetes-specific, scientifically-based informationand to provide support. This free serviceincludes access to a frequently updatedmedia library and to live webinars withnurses, physicians, and experts. Twice aweek, registrants also receive short ques-tionnaires about COVID-19 symptoms andtests for anxiety/depression. If indicated,registrants automatically receive a noticesuggesting medical contact, and phonecalls may follow. At the time of writ-ing, tens of thousands of patients were
registered. Empathy was a driving prin-ciple in design, and comments suggestthat the service helps people to under-standandself-manage their individual riskand to limit disruption in lifestyle and care.An evaluation will indicate to what extentit reduces the burden of disease. Recom-mendations have been formulated bythe French-speaking Diabetes Society(Societe Francophone du Diabete) topromote the intensification of glycemiccontrol by remote support by professio-nals and frequent self-monitoring. How-ever, extremely limited evidence wasavailable to guide both patients andHCPs. In response, a group of physiciansand researchers from50Frenchhospitalsdesigned and launched a large registerto collect data on PWD hospitalized withCOVID-19 and their prognosis (COVID-19and Clinical Outcomes [CORONADO],NCT04324736, ClinicalTrials.gov). Re-cruitment has exceeded expectation;early results are now available (11).
ItalyThe first cases COVID-19 in Italy wererecorded early in February. Tragically,Italy has suffered among the highestnumbers of deaths in the world (47). Atthe time of this writing, the death rate inItaly was estimated at 122.52 per 1,000infections, i.e., a 10-fold higher rate thanin Germany (14.14 per 1,000 infections)(48). This could be due to demographicfeatures of the Italian population, whichinclude a large proportion (23%) of peo-ple aged$65 (49). From 9 March, socialconfinement rules were issued includ-ing restricted access to outpatient clin-ics. Access to diabetes clinics has beenlimited to urgent cases, and remotecontacts via telephone or video telecon-sultation have been officially approvedand reimbursed by the National HealthSystem. Prescriptions of glucose-loweringagents requiring specialist approval(DPP-4i, SGLT2i, GLP-1RA, and new basalinsulin analogs) were automatically re-newed until the end ofMay. Special jointrecommendations have been promptlyissued by the Italian Society of Diabetes(SID), the Association of Italian Diabetol-ogists (AMD), the Italian Society of En-docrinology (SIE), and the Italian Societyof Pediatric Endocrinology (SIEDP) (50).The same organizations have opened aFacebook page entitled “One hour withAMD, SID, and SIEDP” allowing PWD andtheir relatives to contact specialists (51).
Figure 1—Considerations for diabetes management during national emergencies. T1D, type 1diabetes.
4 Diabetes and COVID-19 Diabetes Care

A government web page providing sim-ple and pragmatic recommendationshas been created focusing on disrup-tions to physical activity and diet as aresult of social confinement (52). At thetime of writing, discussions were ongoingregarding restarting clinical activities andhow toorganize post-COVIDdiabetes clinics.
U.K.
Over 90%of PWD in theU.K. aremanagedin primary care, by enhanced diabetes-skilled primary care physicians, nurses,and health care assistants. These modelshave shown to be effective in reducinghospitalizations, outpatient attendance,and admissions for diabetes-relatedcomplications (53). In March, the govern-ment issued guidance on social distanc-ing and self-isolation (54). In England,people considered especially clini-cally vulnerable (including some butnot all PWD) were contacted by thegovernment with advice on shielding.All people at high risk, including PWD,
were advised to only leave the housefor limited periods for essential shop-ping and one form of exercise (55). ThePrimary Care Diabetes Society and theAssociation of British Clinical Diabetolo-gists have issued guidance on managingPWD in primary care (56). The nationalcharity Diabetes UK has been active ingiving advice to PWD through their web-site and social media. Both primary andsecondary care are providing emergencyand routine follow-up using telephoneor video consultations including supportfor mental well-being, though there aresome regional variations. Social mediachannels have been set up where HCPsare sharing experience in managing peo-ple in the community and hospital andexchanging new guidance. A number ofself-management education programshave been made freely available. Thereare also discussions regarding longer-term plans to phase in face-to-face con-sultations for routine chronic diseasemanagement.
U.S.
The lack of universal health coverageposes additional challenges to PWD andtheir care providers during the COVID-19 pandemic in the U.S. There has beenan almost wholesale switch to virtualcare for outpatient appointments butmany failings in this approach. Phonevisits provide a much lower rate ofreimbursement than video visits, butmany of the most vulnerable patientshave inadequate equipment or connec-tivity to support video visits. Contactswith certified diabetes educators byphone or video are not reimbursed.Additional efforts have been made tocommunicate with PWD at home toensure that they are safe. Laboratoryand physical exam monitoring of com-plications has virtually ceased for mostpatients as long as they symptomaticallyremain well. Many patients have lostinsurance coverage. Prescription fillsfor diabetes medications are down 10%;a survey of PWD found one in six
Table 2—Selection of guidance and recommendations relating to routine care in PWD during COVID-19 pandemic
Service Recommendations
Inpatient diabetes services c Inpatient diabetes services will need to continue and potentially increase capacity, with need forteam approach re: glycemic control and nutritional status, and consideration of “virtual visits” forreviews (see MANAGEMENT in HOSPITAL) (68).
Urgent/acute diabetes care (outpatient) c Face-to-face consultations should continue in the following circumstances: a new diagnosis ofT1D; urgent insulin start where symptomatic, HbA1c.10% (86 mmol/mol), or ketones detected;teaching blood glucose monitoring for urgent reasons; or in cases where physical examination isessential (e.g., foot ulcer, infection, some points in pregnancy) (69).
c Virtual (telephone, video, or e-mail) consultations should be used in the following circumstances:follow-up of new T1D diagnoses; vulnerable patients (recent hospital admission, recurrent severehypoglycemia, HbA1c.11% (99 mmol/mol); intensive follow-up in high-risk situations; or whererisk of attending an appointment face-to-face is greater than the benefits (69).*
Routine diabetes care c Consider routine diabetes care delivered virtually in the context of broader long-term conditionmanagement and prioritization, taking into account individual risk factors and clinical needs (68).
c The following should be deferred: routine appointments where diabetes is stable and well-managed; face-to-face structured group education courses; flash glucose monitoring startsessions; where the risk of attending an appointment is greater than the benefits; and wheredeferring appointments will not compromise clinical care (69).
Foot services for PWD c Mayneedtocontinueat full capacitywithconsiderationofmovingsupport to remote formswherepossible (68); many of these services are essential (70).
c Access to in-person support should continue for those with acute or limb-threatening problems(70) or where physical examination is essential (69).
c All new referrals should ideally be reviewed within 24 h (70).
Pregnancy services for PWD c Mayneedtocontinueat full capacitywithconsiderationofmovingsupport to remote formswherepossible (68).
c In-person support will be essential for physical examinations and/or teaching blood glucosemonitoring at some points in pregnancy (69).
Blood tests for PWD c Urgentbloodtestmonitoringshouldcontinue(e.g., decliningrenal function, raisedpotassium, lowsodium) (69).
Eye screening for PWD c This was not mentioned in the guidance reviewed but we understand in most affected countrieseye screening has been halted in view of high risk of transfer. Of note, evidence indicates that riskstratifying is possible (71).
*PWD may be concerned about the need to visit hospital; they should be encouraged to contact their physician in case of any signs or symptomsrelated to acute diabetes complications.
care.diabetesjournals.org Hartmann-Boyce and Associates 5

respondents needing insulin experi-enced a problem. A similar proportionreported issues with obtaining teststrips, and a quarter of respondentsreported issues with obtaining pumpor continuous glucose monitoring sup-plies (20). Many pharmaceutical com-panies have stepped in to increaseaccess to otherwise unaffordable med-ications. In data available through theend of March, relatively early in the U.S.COVID-19 course, approximately 80%of clinicians reported serious strainand nearly two-thirds were uncertainwhether they would be able to keeptheir practices open due to insuffi-cientfinancial resources and lowvolumeof reimbursable work. Overall visits(virtual and face-to-face) for chronicasymptomatic care were down ;50%(57). As the future course of the epi-demic in the U.S. is uncertain and seemslikely to persist for many weeks, thethreat to PWD is grave. The hope is thatnew government initiatives and inno-vationon thepart of stakeholderswillfillthe emerging cracks in an already frag-mented system.
CONSIDERATIONS FORMANAGEMENT OF LONG-TERMCONDITIONS DURING NATIONALEMERGENCIES
Evidence on the management of long-term conditions during national emer-gencies suggests variousways tomitigatethe risks presented by these events,which predominantly fall under two phases:planning and response (23). These strate-gies are outlined in Table 3.
AFTER COVID-19
There is much uncertainty as to how theCOVID-19 pandemic will end and whatwill be left in its wake. Disruptions thatarise due to national emergencies canlead to increased HbA1c in those affectedup to 16 months later, with some evi-dence that this is particularly the case forpeople of lower socioeconomic statusand those treated with insulin (18,23). Alack of access to routine health care is aleading cause of morbidity and mortalityafter disasters; stroke, acute myocar-dial infarctions, and diabetes complica-tions are all shown to increase after the
immediate threat has dissipated (26,58).Services such as diabetes clinics may alsorethink their organization to minimize riskof ongoing transmission.
CONCLUSIONS
The need for decisive action creates animportant tension when evidence is lim-ited. An example here is the classificationof PWD as being at increased risk fromCOVID-19 and therefore subject to in-creased preventive measures. Thoughrisk is clearly increased, quantification isscant. There is little to no evidence onpotentially moderating factors, despitethe fact that these data are routinelycollected in data sets used for existinganalyses; the results presented are oftenunadjusted and use single disease cate-gories, ignoring potential differences be-tween type 1 and type 2 diabetes andmultimorbidities, which are associatedwith worse outcomes (59).
In the face of a limited evidence baserelating directly to COVID-19, decisionscan be informed by international ex-periences to date and, to some extent,from the literature as it relates to other
Figure 2—Possibleflowchart formanagement of people hospitalizedwith diabetes andCOVID-19, reproducedwith permission fromCeriello et al. (49).ACEi, ACE inhibitors; AGIs,a-glucosidase inhibitors; BNP, brain natriuretic peptide; CAD, coronary artery disease; CGM, continuous glucosemonitoring;CK, creatine kinase; CKD, chronic kidney disease; CRP, C-reactive protein; eGFR, estimated glomerular filtration rate (mL/min/ 1.73m2);MI, myocardialinfarction; NT-proBNP, N-terminal prohormone of brain natriuretic peptide; OADs; oral antidiabetes drugs; PAD, peripheral arterial disease; RF, riskfactor; SUs, sulfonylureas; TIA, transient ischemic attack.
6 Diabetes and COVID-19 Diabetes Care

national emergencies. This latter sourceof evidence shows the toll of disruptionsto diabetes care is often most pro-nounced after the acute phase of theemergency or disaster has passed. Insome cases, the excess morbidity andmortality in the aftermath of nationalemergencies is higher than the toll dur-ing the emergency itself. History issues astark warning here when considering thebalance between diverting resources to-ward the acuteCOVID-19 crisis andmain-taining routine care for people livingwithlong-term conditions.Finally, in reviewing what has been
written on the topic of diabetes andCOVID-19, we have been struck by twonoticeable absences. The first is theabsence of literature on wider contextualfactors. PWD are likely to be impacted byCOVID-19 just asmuchoutside thehealthcare setting as within it, with particularconcerns relating to disruptions to dietand physical activity, increased stress,and burdens on mental health and well-being, yet the literature to date focusesalmost exclusively on clinical management.The other unspoken issue in the literaturewe reviewed is that of inequality. COVID-19is not an equal-opportunity disease. Theburden will disproportionally be borne bypeople from less-advantaged groups (60).Emergingdata also suggests thatCOVID-19may pose more of a risk to nonwhite ethnicgroups (9). Diabetes discriminates in similarways, and the intersection of diabetesand COVID-19 creates a maelstrom inwhich existing health disparities risk ex-acerbation with profound and long-lasting
consequences. COVID-19 holds a mirrorto our health care systems and care ofPWD; may we do all we can now to makethat reflection favorable in hindsight.
Acknowledgments. Parts of this article arebased on Rapid Reviews conducted for the Centrefor Evidence-Based Medicine’s COVID-19 EvidenceService (23,61,62).Funding. This work was not funded. E.M. isfunded by a Wellcome Trust fellowship. J.B.B. issupported by grants from the National Institutesof Health (UL1TR002489 and P30DK124723). K.K.acknowledges support from the National Insti-tute for Health Research (NIHR) Applied ResearchCollaboration East Midland (NIHR ARC-EM) andthe NIHR Leicester Biomedical Research Centre.The views expressed are those of the authors
andnot thoseof the universities, theNIHR, or theU.K. Department of Health and Social Care.Author Contributions. J.H.-B., E.M., C.G., D.N.,K.M., and K.K. were involved in concept anddesign. J.H.-B., E.M., C.G., J.K., and J.P. reviewedstudies for inclusion and extracted relevant data.J.B.B., S.D.P., L.J., R.R., and K.K. contributedexperiences from individual countries. J.H.-B.drafted the remainder of the article. All authorsedited and approved the finalmanuscript. J.H.-B.had full access to all data and final responsibilityfor the decision to submit for publication.Duality of Interest. J.B.B. reports nonfinancialsupport and other from Adocia, AstraZeneca,Dance Biopharm, Dexcom, Eli Lilly, Fractyl, GIDynamics, Intarcia Therapeutics, Lexicon, Mann-Kind, Metavention, NovaTarg, Novo Nordisk,Orexigen, PhaseBio, Sanofi, Senseonics, vTv Ther-apeutics, and Zafgen; grants and nonfinancialsupport from AstraZeneca, Eli Lilly, Intarcia Ther-apeutics, Johnson & Johnson, Lexicon,Medtronic,NovaTarg, Novo Nordisk, Sanofi, Theracos, Toler-ion, and vTv Therapeutics; personal fees fromCirius Therapeutics Inc. and CSL Behring; andpersonal fees and other from Mellitus Health,Pendulum Therapeutics, PhaseBio, and StabilityHealth, outside the submitted work. R.R. reports
grants, personal fees, and nonfinancial supportfrom Sanofi, personal fees and nonfinancialsupport from Merck Sharp & Dohme, personalfees from AstraZeneca, grants and personal feesfrom Novo Nordisk, personal fees from Janssen,personal fees from Eli Lilly, personal fees fromAbbott, personal fees from Medtronic, grantsand personal fees from Diabnext, and personalfees from Mundipharma, outside the submittedwork. K.K. has received grants from BohringerIngelheim, AstraZeneca, Novartis, Novo Nordisk,Sanofi, Eli Lilly, Merck Sharp & Dohme, andServier, outside the submitted work. K.K. hasserved as a consultant, speaker, or an advisoryboard member for AstraZeneca, Bayer, NappPharmaceuticals, Eli Lilly,Merck Sharp&Dohme,Novartis, Novo Nordisk, Roche, Berlin-ChemieAG/Menarini Group, Sanofi, Servier, and Boeh-ringer Ingelheim. No other potential conflicts ofinterest relevant to this article were reported.
References1. Gupta R, Ghosh A, Singh AK, Misra A. Clinicalconsiderations forpatientswithdiabetes in timesof COVID-19 epidemic. Diabetes Metab Syndr2020;14:211–2122. Yang J, Zheng Y, Gou X, et al. Prevalence ofcomorbidities and its effects in patients infectedwith SARS-CoV2: a systematic review and meta-analysis. Int J Infect Dis 2020;94:91–953. Emami A, Javanmardi F, Pirbonyeh N, AkbariA. Prevalence of underlying diseases in hospi-talized patients with COVID-19: a systematicreview andmeta-analysis. Arch Acad EmergMed2020;8:e354. Li B, Yang J, Zhao F, et al. Prevalence andimpact of cardiovascular metabolic diseases onCOVID-19 in China. Clin Res Cardiol 2020;109:531–5385. CDC COVID-19 Response Team. Preliminaryestimates of the prevalence of selected under-lying health conditions among patients withcoronavirus disease 2019 – United States,February 12-March 28, 2020. MMWR MorbMortal Wkly Rep 2020;69:382–3866. Docherty AB, Harrison EM, Green CA, et al.Features of 16,749 hospitalised UK patients with
Table 3—Strategies suggested for mitigating risks to management of long-term conditions during national emergencies (23)
Phase Suggested strategy
Planning c Collaboration, including the role of community-based partnershipsc Development of culturally adapted resources for people living with LTCs, including print and web-based educational materialsand access to support telephone lines
c Access to online self-management education programsc Monitoring for patients using prescription data on assessing adherence to medicationsc Proactive remote review of patients requiring care for LTCs and their possible needs if health care services are disruptedc Clear point of contact for patient care should disasters/emergencies occurc Improving identification and tracking mechanisms for people living with LTCs
Response c Triage and resource allocationc Transfer of care to allied HCPs including nurses and pharmacistsc Communication between different agenciesc Business continuity plans for pharmacies, and consideration of 30-day supplies from pharmacistsc Ensuring access to appropriate foods where supplies may be limited (for people with LTCs impacted by diet)c Dedicated patient transportation or mobile clinics for patients requiring in-person care who may be affected by transportdifficulties
c Continued guidance from patient support groups
LTCs, long-term conditions.
care.diabetesjournals.org Hartmann-Boyce and Associates 7

COVID-19 using the ISARIC WHO Clinical Char-acterisation Protocol. 28 April 2020 [preprint].medRxiv. DOI: 10.1101/2020.04.23.200760427. Jordan RE, Adab P, Cheng KK. Covid-19: riskfactors for severe disease and death. BMJ 2020;368:m11988. Stefan N, Birkenfeld AL, Schulze MB, LudwigDS. Obesity and impaired metabolic health inpatients with COVID-19. Nat Rev Endocrinol2020;2020:1–29. Khunti K, Singh AK, Pareek M, Hanif W. Isethnicity linked to incidence or outcomes ofcovid-19? BMJ 2020;369:m154810. Aronson JK, Ferner RE.Angiotensin convert-ing enzyme (ACE) inhibitors and angiotensinreceptor blockers in COVID-19. 22 March 2020.Available from: https://www.cebm.net/covid-19/angiotensin-converting-enzyme-ace-inhibitors-and-angiotensin-receptor-blockers-in-covid-19/.Accessed1 May 202011. Cariou B, Samy H, Wargny M, et al. Pheno-typic characteristics and prognosis of inpatientswith COVID-19 and diabetes: the CORONADOstudy. Diabetologia. 29May 2020 [Epub aheadofprint] DOI: 10.1007/s00125-020-05180-x12. NHS England. Type 1 and type2diabetes andCOVID-19 related mortality in England. 20 May2020. Available from: https://www.england.nhs.uk/publication/type-1-and-type-2-diabetes-and-covid-19-related-mortality-in-england/.Accessed21 May 202013. Bode B, Garrett V, Messler J, et al. Glycemiccharacteristics and clinical outcomes of COVID-19patients hospitalized in the United States. J Di-abetes Sci Technol.9 May 2020 [Epub ahead ofprint]. DOI: 10.1177/193229682092446914. Zhu L, She Z-G, Cheng X, et al. Association ofblood glucose control and outcomes in patientswith COVID-19 and pre-existing type 2 diabetes.Cell Metab 2020;31:1068–107715. The OpenSAFELY Collaborative; WilliamsonE, Walker AJ, Bhaskaran KJ, et al. OpenSAFELY:factors associated with COVID-19-related hospi-taldeath in the linkedelectronichealth recordsof17 million adult NHS patients. 7 May 2020 [pre-print]. medRxiv. DOI: 10.1101/2020.05.06.2009299916. Saulnier DD, Brolin Ribacke K, von Schreeb J.No calm after the storm: A systematic review ofhuman health following flood and storm disas-ters. Prehosp Disaster Med 2017;32:568–57917. Fonseca VA, Smith H, Kuhadiya N, et al.Impact of a natural disaster on diabetes: exac-erbationof disparities and long-termconsequen-ces. Diabetes Care 2009;32:1632–163818. Ng J, Atkin SL, Rigby AS, Walton C, KilpatrickES. The effect of extensive flooding in Hull on theglycaemic control of patients with diabetes.Diabet Med 2011;28:519–52419. Chudasama YV, Zaccardi F, Gillies CL, et al.Leisure-time physical activity and life expec-tancy in people with cardiometabolic multimor-bidity anddepression. J InternMed2020;287:87–9920. dQ&A. Impact of COVID-19 on the diabetescommunity in the United States, 2020. Availablefrom https://d-qa.com/impact-of-covid-19-on-the-usa-diabetes-community/?utm_source5Closer1Look1Subscribers12018&utm_campaign54285f7ac19-2020-04-19_WIR_4%2F13-4%2F1704_18_2020&utm_medium5email&utm_term50_c55d924bf1-4285f7ac19-409220105. Accessed 24 April 202021. Grenard JL, Munjas BA, Adams JL, et al. De-pressionandmedicationadherence in the treatment
of chronic diseases in the United States: a meta-analysis. J Gen Intern Med 2011;26:1175–118222. Qiu J, Shen B, ZhaoM,Wang Z, Xie B, Xu Y. Anationwide survey of psychological distressamong Chinese people in the COVID-19 epidemic:implications and policy recommendations. GenPsychiatr 2020;33:e10021323. Hartmann-Boyce J, Mahtani KR. CEBM: Sup-porting people with long-term conditions (LTCs)during national emergencies. Available from:https://www.cebm.net/covid-19/supporting-people-with-long-term-conditions-ltcs-during-national-emergencies/. Accessed 18 April 2020202024. Aminuddin HB, Jiao N, Jiang Y, Hong J, WangW. Effectiveness of smartphone-based self-management interventions on self-efficacy, self-care activities, health-related quality of life andclinical outcomes in patientswith type 2 diabetes:a systematic review and meta-analysis. Int J NursStud. 8 February 2019 [Epub ahead of print]. DOI:10.1016/j.ijnurstu.2019.02.00325. Pal K, Eastwood SV,Michie S, et al. Computer-based diabetes self-management interventionsforadultswith type2diabetesmellitus.CochraneDatabase Syst Rev 2013 3:CD00877626. Huang L, Yan Z, Huang H. The effect of shortmessageservice interventiononglycemiccontrolin diabetes: a systematic review and meta-analysis.Postgrad Med 2019;131:566–57127. Sahin C, Courtney KL, Naylor PJE, E Rhodes R.Tailored mobile text messaging interventionstargeting type 2 diabetes self-management:a systematic review and a meta-analysis. DigitHealth 2019;5:205520761984527928. XuY, TanDHY, Lee JY-C. Evaluating the impactof self-monitoringofbloodglucose frequenciesonglucose control in patients with type 2 diabeteswho do not use insulin: a systematic review andmeta-analysis. Int J Clin Pract 2019;73:e1335729. Malanda UL, Welschen LMC, Riphagen II,Dekker JM, Nijpels G, Bot SDM. Self-monitoringof blood glucose in patients with type 2 diabetesmellitus who are not using insulin. CochraneDatabase Syst Rev 2012;1:CD00506030. Woolley AK, Chudasama Y, Seidu SI, et al.Influenceof sociodemographic characteristics onthepreferred formatofhealtheducationdeliveryin individualswith type2diabetesmellitus andorcardiovascular disease: a questionnaire study.Diabet Med 2020;37:982–99031. The Health Foundation. Using virtual con-sultations in the fight against COVID-19: Inter-view with Professor Trish Greenhalgh, 30 March2020. Available from https://www.health.org.uk/news-and-comment/newsletter-features/using-virtual-consultations-in-the-fight-against-covid-19. Accessed 18 April 202032. Farrell K, Holmes-Walker DJ. Mobile phonesupport is associated with reduced ketoacidosisin young adults. Diabet Med 2011;28:1001–100433. Viana LV, GomesMB, Zajdenverg L, Pavin EJ,Azevedo MJ; Brazilian Type 1 Diabetes StudyGroup. Interventions to improve patients’ com-pliance with therapies aimed at lowering glycatedhemoglobin (HbA1c) in type1diabetes: systematicreview and meta-analyses of randomized con-trolled clinical trials of psychological, telecare, andeducational interventions. Trials 2016;17:9434. World Health Organisation. Mental Healthandpsychosocial considerations during theCOVID-19
outbreak. 18March2020.Available fromhttps://www.who.int/docs/default-source/coronaviruse/mental-health-considerations.pdf. Accessed 18April 202035. Shelvin M, McBride O, Murphy J, et al.Anxiety, depression, traumatic stress, and COVID-19related anxiety in the UK general population suringthe COVID-19 pandemic. 18 April 2020 [preprint].PsyArXiv DOI: 10.31234/osf.io/hb6nq36. The All-Party Parliamentary Group for Di-abetes (APPG Diabetes). Diabetes and MentalHealth. Available from: https://www.diabetes.org.uk/resources-s3/2018-08/Diabetes%20and%20Mental%20Health%20%28PDF%2C%205.7MB%29.pdf. Accessed April 18, 202037. Krousel-WoodMA, Islam T,Muntner P, et al.Medication adherence in older clinic patientswith hypertension after Hurricane Katrina: im-plications for clinical practice and disaster man-agement. Am J Med Sci 2008;336:99–10438. Khan Y, Albache N, Almasri I, Gabbay RA. Themanagement of diabetes in conflict settings:Focus on the Syrian crisis. Diabetes Spectr 2019;32:264–26939. Chew BH, Vos RC, Metzendorf MI, Scholten RJ,Rutten GE. Psychological interventions for diabetes-related distress in adults with type 2 diabetesmellitus.Cochrane Database Syst Rev 2017;9:CD01146940. Ceriello A, Standl E, Catrinoiu D, et al.; Di-abetes and Cardiovascular Disease (D&CVD)EASD Study Group. Issues of cardiovascular risk man-agement in people with diabetes in the COVID-19era. Diabetes Care 2020;43:1427–143241. Bornstein SR, Rubino F, Khunti K, et al.Practical recommendations for themanagementof diabetes in patients with COVID-19. LancetDiabetes Endocrinol 2020; 8:546–55042. Wondafrash DZ, Desalegn TZ, Yimer EM,Tsige AG, Adamu BA, Zewdie KA. Potential effectof hydroxychloroquine in diabetes mellitus: Asystematic review on preclinical and clinical trialstudies. J Diabetes Res 2020;2020:521475143. NHS London Clinical Networks. Managementof diabetes in emergency department duringcoronavirus pandemic. Available from https://www.england.nhs.uk/london/wp-content/uploads/sites/8/2020/04/Covid-19-Management-of-diabetes-in-emergency-department-crib-sheet-updated-150420.pdf. Accessed 18 April 202044. WeiqingW,ZhongyanS,GuangW,etal.Expertrecommendations for diabetes management inprimary care during COVID-19 pandemic. Zhong-hua Neifenmi Daixie Zazhi 2020;36:185–19045. LinongJ,GuangweiL,QiuhongG,etal.Guidanceon diabetes management in elderly during COVID-19 pandemic. Chin J Diabetes 2020;28:1–646. Linong J, Jiajun Z, Zhiguang Z, et al. Recom-mendation on insulin treatment in diabetes pa-tients affected with COVID-19. Chin J Diabetes2020;28:1–547. Remuzzi A, Remuzzi G. COVID-19 and Italy:what next? Lancet 2020;395:1225–122848. Euronews. Coronavirus statistics: latestnumbers on COVID-19 cases and deaths, 2020.Available from https://www.euronews.com/2020/04/04/covid-19-coronavirus-breakdown-of-deaths-and-infections-worldwide. Accessed 20April 202049. Onder G, Rezza G, Brusaferro S. Case-fatalityrate and characteristics of patients dying in rela-tion to COVID-19 in Italy. JAMA 2020;323:1775–1776
8 Diabetes and COVID-19 Diabetes Care

50. SIE - Societa Italiana di Endocrinologia.Emergenza COVID, 2020. Available from http://societaitalianadiendocrinologia.it/html/cnt/emergenza-covid.asp. Accessed 5 April 202051. SID - Societa Italiana di Diabetologia. Onehour with AMD, SID and SIEDP [in Italian],2020. Available from http://www.siditalia.it/progetto-un-ora-con-amd-sid-siedp. Accessed5 April 202052. Ministero della Salute. Nuovo coronavirus inItalia, 2020. Available from http://www.salute.gov.it/nuovocoronavirus. Accessed 20 April202053. Seidu S, Davies MJ, Farooqi A, Khunti K.Integratedprimary care: is this the solution to thediabetes epidemic? Diabet Med 2017;34:748–75054. Public Health England. Guidance on shield-ing and protecting people who are clinicallyextremelyvulnerablefromCOVID-19,2020.Availablefromhttps://www.gov.uk/government/publications/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19/guidance-on-shielding-and-protecting-extremely-vulnerable-persons-from-covid-19. Accessed 15 April 202055. NHS. People at higher risk from coronavirus,2020. Available from https://www.nhs.uk/conditions/coronavirus-covid-19/advice-for-people-at-high-risk/. Accessed 24 April 202056. Association of British Clinical Diabetologists.COVID-19 (Coronavirus) information for health-care professionals, 2020. Available from https://abcd.care/coronavirus. Accessed 24 April 202057. IQVIA. Monitoring the impact of COVID-19on the pharmaceutical market. Available fromhttps://www.iqvia.com/-/media/iqvia/pdfs/files/iqvia-covid-19-market-tracking-us.pdf?_51587334105503. Accessed 19 April 2020
58. Mokdad AH, Mensah GA, Posner SF, Reed E,Simoes EJ, Engelgau MM; Chronic Diseases andVulnerable Populations inNatural DisastersWork-ingGroup.When chronic conditions becomeacute:prevention and control of chronic diseases andadverse health outcomes during natural disasters.Prev Chronic Dis 2005;2:A0459. Zemedikun DT, Gray LJ, Khunti K, Davies MJ,Dhalwani NN. Patterns of multimorbidity in mid-dle-aged and older adults: An analysis of the UKbiobank data. Mayo Clin Proc 2018;93:857–86660. Royal College of Physicians. COVID-19 andmitigating impact on health inequalities. Avail-able from https://www.rcplondon.ac.uk/news/covid-19-and-mitigating-impact-health-inequalities.Accessed 18 April 202061. Hartmann-Boyce J, Morris E, Goyder C, et al.Diabetes and risks from COVID-19. Availablefrom https://www.cebm.net/covid-19/diabetes-and-risks-from-covid-19/. Accessed 18 April202062. Hartmann-Boyce J, Morris E, Goyder C, et al.Managing diabetes during the COVID-19 pan-demic. Available from https://www.cebm.net/covid-19/managing-diabetes-during-the-covid-19-pandemic/. Accessed 18 April 202063. Chen Y, Gong X, Wang L, Guo J. Effects ofhypertension, diabetes and coronary heart dis-ease on COVID-19 diseases severity: a systematicreview and meta-analysis. 30 March 2020 [pre-print]. medRxiv. DOI: 10.1101/2020.03.25.2004313364. Fadini GP,MorieriML, Longato E, AvogaroA.Prevalence and impactof diabetes amongpeopleinfected with SARS-CoV-2. J Endocrinol Invest2020;43:867–869;65. Wu Z, McGoogan JM. Characteristics of andimportant lessons from the coronavirus disease2019 (COVID-19) outbreak in China: summaryof a report of 72 314 cases from the Chinese
Center for Disease Control and Prevention.JAMA 2020;323:1239–124266. Zhou F, Yu T, Du R, et al. Clinical course andrisk factors for mortality of adult inpatients withCOVID-19 in Wuhan, China: a retrospective co-hort study. Lancet 2020;395:1054–106267. Guan WJ, Liang WH, Zhao Y, et al.; ChinaMedical Treatment Expert Group for COVID-19.Comorbidity and its impact on 1590 patients withCOVID-19 in China: a nationwide analysis. EurRespir J 2020;55:200054768. NHS;RoyalCollegeofPhysicians;AssociationofBritishClinicalDiabetologists. Clinical guide forthe management of people with diabetes duringthe coronovirus pandemic (19 March 2020, Ver-sion 2). Available from https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/speciality-guide-diabetes-19-march-v2-updated.pdf.Accessed 18 April 202069. NHS London Clinical Networks. Outpatientappointmentprioritisation for specialist diabetesdepartments during the coronavirus pandemic.Available from: https://www.england.nhs.uk/london/wp-content/uploads/sites/8/2020/04/4.-Covid-19-Diabetes-Outpatient-Appointment- Prioritisation-Crib-Sheet-27032020.pdf. Accessed 18 April 202070. NHS London Clinical Networks. Clinical strat-egy for servicemanagementofdiabetic footunitsduring the COVID-19 pandemic. Available fromhttps://www.england.nhs.uk/london/wp-content/uploads/sites/8/2020/04/5.-Covid-19-Clinical-Strategy-for-MDFTs-Crib-Sheet-02042020.pdf. Accessed 18April 202071. Leese GP, Stratton IM, Land M, et al.; FourNationsDiabetic Retinopathy Screening StudyGroup.Progression of diabetes retinal status within commu-nityscreeningprogramsandpotential implications forscreening intervals. Diabetes Care 2015;38:488–494
care.diabetesjournals.org Hartmann-Boyce and Associates 9


![December 2009 Issue [File Type: PDF, ~1.91 MB] - Heavy](https://static.fdocuments.in/doc/165x107/62062e968c2f7b1730053154/december-2009-issue-file-type-pdf-191-mb-heavy.jpg)