Current Medicinal Chemistry, 2015, 22, 2539-2557 2539 ...€¦ · Jagat R. Kanwar1,*, Kislay Roy1,...
Transcript of Current Medicinal Chemistry, 2015, 22, 2539-2557 2539 ...€¦ · Jagat R. Kanwar1,*, Kislay Roy1,...

Send Orders for Reprints to [email protected]
Current Medicinal Chemistry, 2015, 22, 2539-2557 2539
0929-8673/15 $58.00+.00 © 2015 Bentham Science Publishers
Nucleic Acid-Based Aptamers: Applications, Development and Clinical Trials
Jagat R. Kanwar1,*, Kislay Roy1, Nihal G. Maremanda1, Krishnakumar Subramanian2, Rakesh N. Veedu3, Raj Bawa4,5,6 and Rupinder K. Kanwar1
1Nanomedicine-Laboratory of Immunology and Molecular Biomedical Research (NLIMBR), Centre for Molecular and Medical Research (C-MMR), School of Medicine (SOM), Deakin University, Victoria, Australia; 2Vision Research Foundation, Sankara Nethralaya, Chennai-India; 3Center for Compara-tive Genomics, Murdoch University and Western Australian Neuroscience Research Institute, Perth, Australia - 6150; 4Adjunct Professor, Department of Biological Sciences, Rensselaer Polytechnic Insti-tute, Troy, New York, USA; 5Patent Agent, Bawa Biotech LLC, Ashburn, Virginia, USA and; 6Founding Director, American Society for Nanomedicine, Ashburn, Virginia, USA
Abstract: Short single-stranded oligonucleotides called aptamers, often termed as chemical antibodies, have been developed as powerful alternatives to traditional antibodies with respect to their obvious ad-vantages like high specificity and affinity, longer shelf-life, easier manufacturing protocol, freedom to introduce chemical modifications for further improvement, etc. Reiterative selection process of aptamers over 10-15 cycles starting from a large initial pool of random nucleotide sequences renders them with high binding affinity, thereby making them extremely specific for their targets. Aptamer-based detection systems are well investigated and likely to displace primitive detection systems. Aptamer chimeras (combination of aptamers with another aptamer or biomacromolecule or chemical moiety) have the potential activity of both the parent molecules, and thus hold the capability to perform diverse functions at the same time. Owing to their extremely high specificity and lack of immunogenicity or pathogenicity, a number of other ap-tamers have recently entered clinical trials and have garnered favorable attention from pharmaceutical companies. Promis-ing results from the clinical trials provide new hope to change the conventional style of therapy. Aptamers have attained high therapeutic relevance in a short time as compared to synthetic drugs and/or other modes of therapy. This review fol-lows the various trends in aptamer technology including production, selection, modifications and success in clinical fields. It focusses largely on the various applications of aptamers which mainly depend upon their selection procedures. The re-view also sheds light on various modifications and chimerizations that have been implemented in order to improve the stability and functioning of the aptamers, including introduction of locked nucleic acids (LNAs). The application of vari-ous aptamers in detection systems has been discussed elaborately in order to stress on their role as efficient diagnostic agents. The key aspect of this review is focused on success of aptamers on the basis of their performance in clinical trials for various diseases.
Keywords: Antibodies, aptamers, chimeras, detection, locked nucleic acid (LNA), modifications, SELEX.
1. INTRODUCTION
Therapeutic vehicles that are used for drug delivery have various life-threatening side effects [1, 2]. Antibodies and their derivatives or chimeric forms have been commonly used for targeting applications [3]. Significant progress has been made in developing and fabricating recombinant anti-bodies to target antigens expressed in cancer [3, 4]. How-ever, factors such as (i) use of animal models for antibody production limiting the generation of antibodies to only those molecules that are not toxic to animals, (ii) limited *Address correspondence to this author at the Nanomedicine-Laboratory of Immunology and Molecular Biomedical Research (NLIMBR), Centre for Molecular and Medical Research (C-MMR), Deakin University, Geelong, Geelong Technology Precinct (GTP), Deakin University, Pigdons Road, Waurn Ponds, Geelong, Victoria 3217, Australia; Tel: 0061-3-5227 1148; Fax: 0061-3-5227 3402; E- mail: [email protected]
applicability of these antibodies in therapeutic and diagnos-tic assays because of their non-human origin, (iii) laborious, time-consuming and expensive methods for production and purification of monoclonal antibodies, (iv) batch to batch variation in antibody-target interaction, (v) denaturation of antibodies at high temperatures, have limited their applica-bility [5, 6]. Improved ligand selection technologies have made use of various moieties such as carbohydrates, nucleic acid ligands or peptide ligands called aptamers. The term aptamer has been derived from the Latin word, aptus which means “to fit” [7]. Tuerk and Gold invented aptamers, their selection procedure and their binding capability [8]. The nucleic acid aptamers are single-stranded (ss) DNA or RNA of 20-80 nucleotides length [9] that fold into unique 3-dimensional conformations due to intra-molecular interac-tions [10] which are capable of binding the target with high affinity and specificity [11].
Please provide corresponding author(s)
photographsize should be 4" x 4" inches

2540 Current Medicinal Chemistry, 2015, Vol. 22, No. 21 Kanwar et al.
The reason aptamers are highly specific is because their iterative selection systems help to isolate the aptamer with the highest specificity from a pool of random DNA or RNA sequences. Thus, owing to their high binding affinity and specificity, aptamers are important in diagnostics, analysis, imaging and therapeutics [12-14]. Pegaptanib sodium, an anti-vascular endothelial growth factor (VEGF) aptamer, was the first aptamer to be approved by the US Food and Drug Administration (FDA) for clinical use; several others are currently in clinical trials [15]. For example, a recent study with aptamers against anti-MPT64 antibodies for Mycobac-terium tuberculosis showed that point mutations of highly conserved nucleotides were able to effectively bind to poly-clonal anti-MPT64 antibodies from tuberculosis (TB) pa-tients with high specificity and sensitivity, whereas antibod-ies generated against a specific antigen fail to recognize the variant form of the antigen.
Increased clinical and bio-analytical applicability of ap-tamers is due to factors such as (i) an increased stability and resistance to high temperatures, (ii) ease of synthesis with highly reproducible chemical procedures without batch-to-batch variations, (iii) ease of introducing modifica-tions/functional groups for increasing stability (against nu-cleases) and also for use as signalling probes (fluorophores), (iv) reduced immunogenicity and toxicity (hence improved biocompatibility), (v) the ability to generate large volumes of highly specific aptamers to a wide range of target molecules [16]. Aptamers have half-life ranging from minutes to hours in the bloodstream, mainly due to nuclease degradation, and hence are cleared rapidly from the bloodstream [17]. This phenomenon has been exploited for in vivo diagnostic imag-ing. The half-life, however, can be increased to days or even weeks by inducing modifications, rendering aptamers useful for therapeutic purposes.
2. APTAMER APPLICATIONS
In recent years, several aptamers have been developed against targets with potential therapeutic applications. Owing to their extremely high specificity and lack of immunogenic-ity or pathogenicity, a number of aptamer candidates have recently entered clinical trials and gained interest from phar-maceutical companies. Aptamers have found their way into food safety and food inspection as NeoVentures Biotechnol-ogy Inc. has successfully commercialized the first aptamer-based detection system for analysis of mycotoxins in grain (http://neoventures.ca/products/mycotoxin-testing/). Biosen-sors based on aptamers, also known as aptasensors, have become highly successful due to their high specificity and sensitivity [18]. Aptamers that can bind to cell surface recep-tors have also been exploited to deliver drugs and a variety of cargoes into target cells [19]. Aptamer-based Western blotting strategy has also been much appreciated as it re-duces the procedure to a single step and easily detects the target protein using only one aptamer. A quantum dot conju-gated aptamer is employed instead of the two antibodies and, therefore, this procedure requires less time, no antibodies, no radiolabelling and also introduces the possibility of detecting more than one target protein [20]. Apart from the above mentioned applications, aptamers have also been widely used in chromatographic techniques and aptamer-based af-finity chromatography system has been reported to isolate
recombinant human L-selectin-Ig fusion protein from Chi-nese hamster ovary (CHO) cells [21]. Aptamers that bind to flavin adenine dinucleotide (FAD), nicotinamide adenine dinucleotide (NAD) and pyrroloquinoline quinone (PQQ) have been synthesized using in vitro methods. Their redox abilities have been tested and this aptamer-cofactor complex has found a possible application in biofuel cells [22]. Both DNA and RNA aptamers have been extensively used for imaging, diagnosis, biomarker identification and targeted delivery for cancer therapy [23-74] (Table 1).
2.1. Aptamer-Based Imaging
Aptamers allow easy modifications with fluorophores for target cell detection and imaging. The small size of aptamers allows cellular permeation and their ability to target an ex-tensive array of target molecules makes them extremely suit-able as imaging probes [75]. An array of DNA aptamers were selected using the Cell-systematic evolution of ligands by exponential enrichment (SELEX) method to specifically differentiate between T-cell leukemia and B-cell lymphoma. Aptamer sgd5 was highly specific to Toledo cells (B-cell lymphoma cell line), while aptamers sgc8, sgc3, sgc4, sgd2, and sgd3 were specific to CCRF-CEM cells (T-cell acute lymphoblastic leukaemia cell line). Such aptamers can be used as molecular probes for detection and identification of the type of neoplastic cells in blood samples from patients [76, 77]. Another study reported the development of DNA aptamers TD05 that specifically bound to the immunoglobin heavy mu chain of the B cell antigen receptor on Ramos cells (Burkitt’s lymphoma cell line) [78, 79]. Aptamers immobi-lized on magnetic nanoparticles for detection of cancer cells from a complex sample have also been developed. A dual signal amplification platform using iron oxide nanoparticles along with gold nanoparticles that bind specifically to CCRF-CEM cells with the help of aptamers was reported by Zhang et al. This strategy showed a detection limit of 10 cells [80]. A similar study reporting the use of aptamer con-jugated gold nanoparticles for detection of CCRF-CEM cells [81]. An in vivo imaging probe using sgc-8 aptamers was developed by Shi et al. referred to as activatable aptamer probe (AAP). The fluorophores conjugated on these aptamer probes were quenched when present in a free state, whereas upon binding to target cells the probes showed fluorescence recovery by undergoing conformational changes. In vivo studies with these AAP molecules showed fluorescence en-hancement at the site of the tumor compared to that of non-tumor areas [82]. Use of superparamagnetic iron oxide nanoparticle-aptamer (A10) conjugates to target prostate-specific membrane antigen (PSMA) expressed on prostate cancer cells has been reported for magnetic resonance imag-ing [83]. The aptamer A10 has also been used in conjugation with gold nanoparticles to develop a computed tomography platform for imaging PSMA expressing prostate cancer cells [84]. Radiolabelled aptamers have also been reported for use as molecular probes. TTA1, an RNA aptamer that targets tenascin-C was radiolabelled for in vivo imaging and bio-distribution studies in brain and breast cancer xenografts. Tenascin-C is an extracellular matrix protein that has been reported to be expressed during tumor growth and angio-genesis. [70, 85]. Radiolabelled DNA aptamers targeting MUC1 (mucin 1), a glycoprotein that is known to be over-

Nucleic Acid-Based Aptamers Current Medicinal Chemistry, 2015, Vol. 22, No. 21 2541
Table 1. List of various DNA and RNA aptamers, their targets and their functions.
S.No Aptamer Sequence Target
(Localization) Cell Line Function Reference
DNA Aptamers
1 MUC1 GCAGTTGATCCTTTGGATACCCTGG
Mucin (Cell surface)
OVCAR-3 (ovarian cancer cells), A549 ( human lung cancer cells),
pancreatic, prostate, MCF-7 (breast cancer cells); HepG2
(human liver cancer cells)
Cancer cell imaging; therapy
[23-27]
2 S1.3/S2.2 GGGAGACAAGAATAAACGCTCAAG-CAGTTGATCCTTTGGATACCCTGGT-TCGACAGGAGGCTCACAACAGGC
Mucin (Cell surface)
MCF-7 (human breast cancer cell line)
Cancer therapy [28, 29]
3 5TR-1 GGGAGACAAGAATAAACGCTCAA-GAAGTGAAAATGACAGAACA-CAACATTCGACAGGAGGCTCA-CAACAGGC
Mucin (Cell surface)
MCF-7 (human breast cancer cell line)
Cancer therapy [28]
4 SGC8 ATCTAACTGCTGCGCCGCCGGGAA-AATACTGTACGGTTAGA-(CH2)6-NH2
Protein tyrosine kinase 7 (PTK7)
(Cell surface)
CCRF-CEM, (T-cell leukaemia cell line)
Cell imaging; diagnosis; cell
sorting; tar-geted therapeu-
tic delivery; biomarker
identification
[30-33]
5 C8FL Modified SGC8 aptamer with two PEG spacers instead of nucleo-tides A23–T30, and LNA at both ends
Protein tyrosine kinase 7 (PTK7)
(Cell surface)
CCRF-CEM, (T-cell leukaemia cell line)
Cancer cell detection
[34]
6 SGA16 TTTAAAATACCAGCTTATTCAATTA-GTCACACTTAGAGTTCTAGCTGCTGC-GCCGCCGGGAAAATACTGTACGGA-TAGATAGTAAGTGCAATCT
Protein tyrosine kinase 7 (PTK7)
(Cell surface)
CCRF-CEM, (T-cell leukaemia cell line)
Cancer diagno-sis
[34, 35]
7 SYL3C
SYL1
SYL2
SYL3
SYL4
CACTACAGAGGTTGCGTCTGTCCC-ACGTTGTCATGGGGGGTTGGCCTG AGCGTCGAATACCACTACAGTTTG-GCTCTGGGGGATGTGGAGGGGGGTATGGGTGGGAGTCAATGGAGCTCGT-GGTCAG AGCGTCGAATACCACTACAGAGCTC-GGGGTTTTTTGGGGTTTTTTGGGGTTTTGGTGGGGCTAATGGAGCTCGT-GGTCAG AGCGTCGAATACCACTACAGAGGTT-GCGTCTGTCCCACGTTGTCATGGGGGGTTGGCCTGCTAATGGAGCTCGTG-GTCAG AGCGTCGAATACCACTACAGAGCT-CCGGGGTTTTTGGGGGTTTTTCTGGGGTTTTTTGGGGCTAATGGAGCTCGT-GGTCAG
EpCAM (Cell surface)
MDA-MB-231 (breast carcinoma cell line); Kato III (human gastric cancer cell line); HT-29 (colorec-
tal adenocarcinoma cell line); T47D (ductal breast epithelial cell
line)
Cell sorting [36]
8 TDO5 AACACCGGGAGGA-TAGTTCGGTGGCTGTTCAGGGTCTCCTCCCGGTG-(CH2)6-NH2 IgG receptors
(Cell surface) Ramos cells (B-cell lymphoma
cell line)
Cancer cell imaging; diag-
nosis; cell sorting; tar-
geted therapeu-tic delivery
[31, 37-39]

2542 Current Medicinal Chemistry, 2015, Vol. 22, No. 21 Kanwar et al.
(Table 1) contd….
S.No Aptamer Sequence Target
(Localization) Cell Line Function Reference
9 A1 GGTTGCATGCCGTGGGGAGGGGGGTGGGTTTTATAGCGTACTCAG(CH2)6-NH2
Unknown A549 cells (adenocarcinomic
human alveolar basal epithelial cells)
Targeted drug delivery
[31]
10 AS1411 TTGGTGGTGGTGGTTGTGGTGGTGGTGG
Nucleolin (Cell surface and
nucleolus)
C6 (rat glioma cells), HeLa (hu-man cervical cancer cells), Hep-G2 (human liver cancer cells),
Caco-2 (human colorectal cancer cells), U-87MG (human glioblas-toma cells), F11 (mouse neuro-blastoma cells), C6 (rat glioma
cells), CT-26 (mouse colon cancer cells)
Cancer cell imaging; tar-
geted therapeu-tic delivery
[40-44]
11 GMT4, GMT8
TGACGAGCCCAAGTTACCTTGGT-GATGGTTTTTGGTGGTAACGGGGGCGGGTGAGTAGAATCTCCGCTGCCTACA
Unknown CCRF-CEM, (T lymphoblast cell line); U87, (primary glioblastoma
cell line)
Cancer cell detection
[45]
12 CSC1 ACCTTGGCTGTCGTGTTGTAGGTGGTTTGCTGCGGTGGGCTCAAGAAGAAAG-CGCAAAGGTCAGTGGTCAGAGCGT
Unknown DU145 (Prostate cancer cell line) Photothermal
therapy [51]
13 CSC13 ACCTTGGCTGTCGTGTTGTGGGGTGTCGTATCTTTCGTGTCTTATTATTTTCT-AGGGGAGGTCAGTGGTCAGAGCGT
Unknown Prostate cancer stem cells Photothermal
therapy [51]
14 KDED 2a-3 TGCCCGCGAAAACTGCTATTACGTGT-GAGAGGAAAGATCACGCGGGTTCGT-GGACACGGTTTTTTTTTTT
Unknown DLD-1 (human colorectal adeno-
carcinoma cell line) Cancer cell
imaging [46]
15 KCHA10 ATCCAGAGTGACGCAGCAGGGGAG-GCGAGAGCGCACAATAACGATGG-TTGGGACCCAACTGTTTGGACACGG-TGGCTTAGTTTTTTTTTTT
Unknown HCT 116 (colorectal cancer cell
line) Cancer cell
imaging [46]
16 R13 TCTCTAGTTATTGAGTTTTCTTTTATG-GGTGGGTGGGGGGTTTTT
Unknown A549 (lung cancer cell line) Photodynamic
therapy [47]
17 S6 TGGATGGGGAGATCCGTTGAG-TAAGCGGGCGTGTCTCTCTGCCGCCTTGCTATGGGG
Unknown SK-BR-3 (breast cancer cells
expressing HER-2)
Cancer cell detection and
imaging [48]
18 GBI-10 GGCTGTTGTGAGCCTCCTCCCA-GAGGGAAGACTTTAGGTTCGGTTC-ACGTCCCGCTTATTCTTACTCCC
Tenascin-C (Extracellular ma-
trix)
U251 (human gliobalstoma cell line)
Cancer cell detection
[49]
19 A-1 TAACTCAATAAGCTAGGTGGGTGGGGGACACTACCCGGGGGGTGGTTGGGT
Unknown HepG2, a (human liver cancer cell
line) Cancer cell detection
[50]
20 ADE1
ADE2
EJ2
EJ4
EJ5
EJ7
AGTGGTCGAACTACACATCCTTGAAC-TGCGGAATTATCTAC GAGCCCTATCTCACACCGCACCCGC-AAACTATCCTACAT AGTGGTCGAACTACACATCCTTGA-ACTGCGGAATTATCTAC GAAGACGAGCGGCGAGTTTAT-TACGCTTGGAAACAACCCC TACGGGCTGGATCCACTGTTACGG-CGTGTATCCGCTATCAA GAAGACGAGCGGCGAGTGTTAT-TACGCTTGGAAACAACCCC
Unknown H23 (lung adenocarcinoma cell
line) Cancer cell
sorting [52]

Nucleic Acid-Based Aptamers Current Medicinal Chemistry, 2015, Vol. 22, No. 21 2543
(Table 1) contd….
S.No Aptamer Sequence Target (Localization)
Cell Line Function Reference
21 HCA12, HCC03, HCH07, HCH01
Unknown NCI-H69 (small cell lung cancer cell line)
Cancer cell sorting
[53]
RNA Aptamers
1 A10 GGGAGGACGAUGCGGAUCAGCCA-UGUUUACGUCACUCCUUGUCAAUC-CUCAUCGGC
Prostate-specific membrane antigen
(PSMA) (Cell surface)
LNCaP (human prostate cancer cell line)
Cancer cell imaging;
diagnosis; therapy; cell
sorting
[54-58]
2 A9 GGGAGGACGAUGCGGACCGAAAAA-GACCUGACUUCUAUACUAAGU-CUACGUUCCCAGA
Prostate-specific membrane antigen
(PSMA) (Cell surface)
LNCaP (human prostate cancer cell line)
Cancer therapy; cell sorting
[59]
3 Xpsm-A9 GGGAGGACGAUGCGGACCGAAAA-AGACCUGACUUCUAUACUAAGUCU-ACGUUCCCAGACGACUCGCCCGA
Prostate-specific membrane antigen
(PSMA) (Cell surface)
LNCaP (human prostate cancer cell line)
Cell surface protein anaysis
[60, 61]
4 Ep-DT3-DY647
GCGACUGGUUCCCGGUCG
EpCAM (Cell surface)
MCF-7, breast cancer cell line; SW480, a colon adenocarcinoma cell line; MDA-MB-23, a breast carcinoma cell line; Kato III, a human gastric cancer cell line; HT-29, a colorectal adenocarci-noma cell line; T47D, a ductal
breast epithelial cell line
Cancer cell imaging
[62]
5 CD4 aptamer AAGUGACGUCCUGAUCGAUUGUG-CAUUCGGUGUGACGAUCU
CD4 (Cell surface)
Jurkat (T-cell leukaemia cell line) Cell sorting [63, 64]
6 PSMA aptamer
ACCAAGACCUGACUU-CUAACUAAGUCUACGUUCC
Prostate-specific membrane antigen
(PSMA) (Cell surface)
LNCaP (prostate cancer cell line) Cell imaging [65]
7 EGFR aptamer
GGCGCUCCGACCUUAGUCUCUGUG-CCGCUAUAAUGCACGGAUUUAAUC-GCCGUAGAAAAGCAUGUCAAAGCC-GGAACCGUGUAGCACAGCAGAGAA-UAAAUGCCCGCCAUGACCAG
Epidermal growth factor receptor
(EGFR) (Cell surface)
human glioblastoma cell line Cancer cell isolation
[66]
8 J18 GGCGCUCCGACCUUAGUCUCUG-CAAGAUAAACCGUGCUAUUGAC-CACCCUCAACACACUUAUUUAAU-GUAUUGAACGGACCUACGAAC-CGUGUAGCACAGCAGA
Epidermal growth factor receptor
(EGFR) (Cell surface)
A-431 (human epidermoid carci-noma cell line)
Targeted deliv-ery
[35, 67, 68]
9 A30 GGGAAUUCCGCGUGUGCCAGCGAA-AGUUGCGUAUGGGUCACAUCGCAG-GCACAUGUCAUCUGGGCGGUCCGU-UCGGGAUCCUC
Human EGFR related 3 (Her3)
MCF-7 (human breast cancer cell line)
Cell surface protein analy-
sis; cell sorting; therapy
[35, 69]
10 TTA1 GGAGGACGCUCGCCGUAAUG-GAUGUUUUGCUCCUG
Tenascin-C (Extracellular ma-
trix)
Breast, glioblastoma, lung and colon cancer
Cancer therapy [70-73]
11 E9P2-2 GGGAGGACGAUGCGGUGCCCACU-AUGCGUGCCGAAAAACAUUUCCCC-CUCUACCCCAGACGACUCGCGCGA
Tenascin-C (Extracellular ma-
trix)
U251 (human glioblastoma cell line)
Cell sorting [35, 74]

2544 Current Medicinal Chemistry, 2015, Vol. 22, No. 21 Kanwar et al.
expressed in most tumors of epithelial origin was used for imaging breast cancer [86]. Another group reported the de-velopment of a nanoparticle probe that constituted a nanoparticle-aptamer conjugate that was both fluorescently and radioactively labeled for multimodal in vitro or in vivo imaging. The DNA aptamer used in this study was AS1411; it specifically targets nucleolin which is a nucleolar protein known to control ribosomal biogenesis and is overexpressed in rapidly dividing cells [40].
2.2. Aptamers as Therapeutics
Aptamers, being non-toxic and biocompatible have emerged as potential therapeutic agents for targeted delivery of nanoparticles, drugs and small interfering RNAs (siR, NAs) [87]. Aptamers targeting PSMA expressed on prostate cancer cells have been developed for imaging as well as for therapy [88]. Since the developments of the two RNA ap-tamers (A9 and A10) targeting PSMA by Lupold et al. in 2002, they have been extensively used for developing treat-ment strategies for prostate cancer [60]. McNamara et al. developed an aptamer-siRNA chimera for intracellular deliv-ery of siRNA. The aptamer (A10) portion of the chimeras binds to the PSMA expressing cells leading to intracellular delivery of the siRNA that inhibits cell survival genes polo-like kinase 1 (PLK1) and B cell lymphoma (Bcl2). This ap-tamer-siRNA chimera showed specific inhibition of tumor growth without effecting non-cancerous cells [56]. A trun-cated version of aptamer A10, A10-3.2, was used for intra-cellular delivery of pegylated polyamidoamine based tumor suppressor genes micro-RNA (miR)-15a and miR-16-1 to PSMA expressing LnCAP cells (prostate cancer cell line) [89]. A novel strategy for improving treatment of high-risk localized prostate cancer was developed by Ni et al. using A10-shRNA (short hairpin RNA) chimeras. This chimera increased the sensitivity of PSMA expressing cells to ioniz-ing radiations without damage to surrounding non-cancerous tissue. This was achieved by selecting shRNA that specifi-cally targeted DNA-activated protein kinase, catalytic poly-peptide (DNAPK) which resulted in radiosensitization [90]. A10 aptamers have also been used for therapeutic targeting of prostate cancer using aptamer-nanoparticle conjugates for intracellular drug delivery. Farokhzad et al. demonstrated the use of pegylated poly-lactic acid nanoparticles encapsulated with a fluorescent labelled dextran conjugated with A10 ap-tamers for prostate cancer-specific cell binding and intracel-lular delivery of the drug model (dextran) to cells. It was shown that only PSMA expressing cells efficiently took up the nanoparticle-aptamer conjugates while the non-PSMA expressing cells did not take up the conjugates [91]. Another such example is a novel fluorescent thrombin binding ap-tamer (TBA) conjugated with dansyl probe at 3’-end and a β-cyclodextrin residue at 5’-end. It was found that the folding of this modified aptamer into chairlike, G-quadruplex struc-ture was associated with an enhancement in fluorescence. Hence, the aptamer has immense potential as a diagnostic tool for thrombin recognition [92]. TBA’s have been re-searched for over 20 years with some very encouraging find-ings. TBA’s are aptamer constructs aimed at improving anti-coagulation activity [93].
A truncated version of PSMA aptamer A10, A10-3 was used in conjugation with poly(D,L-lactic-co-glycolic acid)
(PLGA) nanoparticles loaded with docetaxel for in vivo de-livery of the drug to prostate cancer cells, which showed complete tumor regression in five out of seven xenograft nude mice [54]. The same group also compared the efficacy of platinum prodrugs in conjugation with aptamer-targeted pegylated PLGA nanoparticles to that of free cisplatin. This nano-formulation showed a higher anti-tumor efficacy at lower doses compared to that of the conventional cisplatin treatments [94]. A combinatorial drug delivery system using A10 conjugated nanoparticles to deliver docetaxel and cis-platin to prostate cancer cells has also been reported [95]. Aravind et al. recently demonstrated the use of pegylated PLGA-lecithin nanoparticles functionalized with an anti-nucleolin DNA aptamer AS1411 for site specific delivery of an anticancer drug paclitaxel. The antitumor effect of the aptamer-targeted nanoparticles was much higher than the non-targeted delivery in MCF-7 (breast cancer cell line) and GI-1 (human gliosarcoma cell line) cells [41]. Quantum dots-aptamer-drug conjugates for imaging and treatment of cancer were developed by Savla et al. In this case, quantum dots were conjugated with a DNA aptamer MUC1 and doxorubi-cin for targeting mucin expressing A2780/AD multidrug-resistant (MDR) ovarian cancer cells [96].
2.3. Aptamers for Cell Separation
Lack of specific biomarkers for each cancer model and the limited availability of molecular probes for recognizing cell surface receptors has constrained the researchers for understanding the molecular basis of cancer. Development of detection probes for cell surface markers can be of tremen-dous help in cancer diagnosis and therapeutics. Recent ap-proaches involving selection of aptamers for specific cancer cells referred to as cell-SELEX is a promising field for can-cer diagnosis and biomarker identification. Cell-specific ap-tamers have been reported for leukemia cells [77, 97], lym-phoma cells [79], small-cell lung cancer cells, [53, 98], glioblastoma cells [49], liver cancer [99], breast cancer cells expressing HER2 [48].
Use of antibodies as ligands for capturing rare cells on microfluidics is limited only to those few known markers that are specifically expressed in each cancer type for which high-affinity antibodies are available. To overcome this ob-stacle, use of aptamers that can be synthesized for any cell type has been exploited to capture rare cells in microfluidic devices. The ease of immobilization on a variety of sub-strates, their thermal stability, and high specificity to target molecules has made aptamers attractive targets for biosen-sors and microfluidics-based CTC capture studies [100, 101]. The first study reporting the use of aptamers for enrichment of CTCs in a microfluidic device was carried out by Phillips et al. Here, DNA aptamers sgc8 were coated on the micro-channels of a PDMS based chip to capture T cells from an acute lymphoblastic leukemia cell line. Effect of various parameters such as flow rates, aptamer concentration and cell density on cell capture was evaluated. The sensitivity and specificity obtained using aptamers was as good as using antibodies without the need for pre-treatment of cells [101]. This study was further extended for multiplexed cancer cell detection on a single chip using three different DNA aptam-ers, namely, Sgc8, TD05 and Sgd5/ each specific to a leu-kaemia cell line. A PDMS based S-shaped channel was used

Nucleic Acid-Based Aptamers Current Medicinal Chemistry, 2015, Vol. 22, No. 21 2545
for multiplexed capture of different cancer cells in different areas of the channel by immobilizing specific aptamers at specific regions. The results showed that this device was able to sort cells with 96% purity while maintaining the viability of the captured cells [102]. Sheng et al. developed a micro-fluidic device consisting of several micropillars coated with DNA aptamers to efficiently capture cancer cells from un-processed whole blood samples. Isolation of colorectal can-cer cells DLD-1 and HCT 116 spiked in whole blood sam-ples by using specific DNA aptamers KDED2a-3 and KCHA10 respectively with >90% capture efficiency with >80% purity and high sensitivity was seen [46]. Capture and enumeration of prostate cancer cells spiked in whole blood samples using PSMA specific aptamers coated on a high-throughput microsampling unit (HTMSU) have been re-ported. This study showed efficient capture of cancer cells from the large background of blood cells even at low cell concentrations [65]. Use of gold nanoparticles conjugated with DNA aptamers sgc8 for efficient capture of leukaemia cells was reported by Sheng et al. Capture efficiency in-creased from 49% to 92% by using gold nanoparticle-aptamer conjugates in comparison to aptamers alone. This approach was further validated in a flat channel with her-ringbone structures that cause microvortexing within the channels to improve interactions between cells and channel surface [103]. Zhu et al. designed a microfluidic device that allows temperature mediated release of captured cells for subsequent culture and analysis. This approach involved specific capture of leukemia cells on a sgc-8 modified PDMS based device followed by efficient release of cells while maintaining their viability using integrated heaters and tem-perature sensors [104]. Anti-epidermal growth factor recep-tor (EGFR) RNA aptamers have been used for efficient iso-lation of human glioblastoma cells and genetically modified murine glioma cells overexpressing EGFR [66]. This study was further extended for increasing surface roughness of the PDMS chip by nano-texturing. A 2-fold increase in capture efficiency was seen as a result of efficient functionalization of aptamers on the substrate [105]. Effect of surface rough-ness on capture efficiency was also evaluated by Wang et al. Comparison of capture efficiencies of RAMOS cells on sur-faces with TD05 aptamers immobilized on gold nanoparticle layers with varying roughness and with TD05 aptamers linked to the gold particle layers via a spacer poly (oligo(ethylene glycol)methacrylate) in serum-free and se-rum-containing media was carried out [106].
2.4. Aptamers and Immune Response Affected cells such as the tumour cells generally vary
from healthy normal tissues and the differences between the two types of cells can be recognized by the immune system to induce an anti-tumour response [107]. The intensity of the generated immune response may get enhanced via induction of secondary signaling by co-stimulatory receptors. Although it is well established that aptamers lack immunogenicity due to their nucleic acid nature, it has also been found that ap-tamers can enhance immune responses through activation of specific target receptors. It has been shown that a dimerized OX40 (CD134), a member of the tumour necrosis family of immune co-stimulatory molecules, can enhance in vitro and in vivo immune response through OX40 receptor activation [107]. Another study reported the development of an aptamer
that binds to 4-1BB (a major co-stimulatory receptor that promotes the survival and expansion of activated T cells) expressed on the surface of mouse T cells and activated the CD8+ T cells that further mediated tumour rejection in mice [108]. These studies laid the foundation that aptamer-receptor binding can favor immune response activation and, therefore, more research was focused in the same direction. In fact, it was reported recently that dimerized CD28 (main co-stimulatory receptor responsible for activation of T lym-phocytes) aptamers upon binding to CD28 receptors provide an artificial co-stimulatory signal capable of enhancing the cellular immune response against a lymphoma idiotype and also prolonged the survival of mice [109].
2.5. Role of Aptamers in Detection Systems Kanwar et al. [110] have reported various mechanisms of
aptamer conjugation with a drug-loaded nanocarrier, its in-ternalization, biodistribution and detection systems. They examined functions of various aptamers, their targets, and the action strategies. The role of aptamers in cancer, eye dis-eases and inflammation and aptamers as therapeutics and biosensors has also been examined. This highlights the im-portance of aptamers in targeted delivery systems. Various detection systems have been developed over the years, but most of the other targeting methods such as carrier peptide, antibody, and nanoparticle-based systems lack target speci-ficity. It is very difficult to generate antibodies against every antigen or biomolecule with a very high specificity. Aptam-ers, having obvious benefits over antibodies, easily improve the efficiency of detection systems (Fig. 1). Aptamers have been used to detect anthrax spores [111], the hepatitis C vi-rus (HCV) core antigen [112], adenosine [113], ATP [114], thrombin [115, 116], the HIV1 transactivator of transcription (tat) protein [117], lysozyme [118], human IgE [119], mucin1 (MUC1) for breast, pancreatic and ovarian cancer therapy [120], glycoprotein 130 receptor for treatment of myasthenia gravis [121], transcription factor 1 (TCF1) for treatment of colon cancer, tenascin-C for brain cancer detec-tion [122] and many other targets such as prostate-specific membrane antigen (PSMA) [123], cocaine [124], C-reactive protein (CRP) [125] and mercury (Hg).
Using SELEX, a DNA aptamer was synthesized against non-pathogenic spores of Sterne strain (low virulence as it is non-capsulated) Bacillus anthracis. This was performed us-ing an electro-chemiluminiescence (ECL) sandwich system comprising an aptamer coated onto magnetic beads followed by anthrax spores- and the biotinylated aptamer, the detec-tion of ECL was done, which indicated presence of the Ba-cillus anthracis spores [111].
Quantum dots (QD) in combination with aptamers have been widely employed in aptamer-based detection systems to detect various biomolecules such as PSMA in prostate can-cer. An anti-PSMA aptamer was coated onto the surface of QD and doxorubicin (an anticancer drug) that was also bound non-covalently to the aptamer. This complex was able to bind to PSMA receptors expressed on prostate cancer cells and release doxorubicin over time [123]. Another PSMA detection system included bioconjugate nanoparticles with A10 aptamer (specific against PSMA) and 57 basepair nu-clease stabilized 2’ fluoropyrimidine RNA modified with C-18 amine at the 3’ end of the RNA sequence [126]. In yet

2546 Current Medicinal Chemistry, 2015, Vol. 22, No. 21 Kanwar et al.
Fig. (1). Aptamer-based detection systems. Aptamer coating on glass or polymeric chips are used for detection of single or multiple targets. The aptamers are mainly used in detection systems that are based on microscopy, microfluidics or aptamer ELISA. another study, an aptamer-QD molecule was tagged to a co-caine binding aptamer to form a cocaine-aptamer-aptamer-QD complex. In the presence of cocaine, the anti-cocaine aptamer dissociates from the complex leading to the release of a QD bound aptamer. The amount of QD released is di-rectly proportional to the cocaine concentration in the sam-ple [124]. Aptamers have been used in several studies for imaging as well. Confocal laser microscopy has been used to study cellular internalization of an anti-angiogenin ap-tamer in realtime protein imaging in cancer cells [127]. In a different study, an anti-C reactive protein (CRP) RNA ap-tamer was immobilized onto streptavidin-coated magnetic beads, and in the presence of CRP the aptamer selectively binds to it. The amount of binding was estimated using differential pulse voltammetry (DPV) by the addition of a biotinylated aptamer which binds to the CRP bound ap-tamer giving an enzymatic reaction [125]. Selenome-thionine (SeMet) encapsulated nanoparticles tagged with aptamers (120nm size) have been synthesized to inhibit mercury (Hg) toxicity. In this study, the thymine (T) rich aptamers used were specific for metals as they formed metal bridged thymine base pairs in the presence of metals (T-metal-T) [128]. The nanoparticles protected the aptamer from biodegradation and achieved effective release of Se-Met to diminish Hg toxicity. Aptamers have also been used to facilitate the entry of nanoparticles into various target cells. The detection of AS1411 (anti-nucleolin aptamer) bound to rhodamine labelled cobalt chloride nanoparticles internalized in cells was peerformed by magentic resonance imaging (MRI). Aptamer immobilized gold nanorods and silica nanoparticles have been used to detect cancer cells through covalent linkage of fluorophore-labeled aptamers on their surfaces [129].
Aptamer-based detection systems are ready to take over primitive detection systems. A clear example is the use of a peptide aptamer-based enzyme-linked immunosorbent assay (ELISA) for detection of cathepsin E (catE) from both tis-
sues and plasma samples. This process was named as an en-zyme on peptide (EOP) mode peptide ELISA where the pep-tide aptamer pa4043 was used for detection of catE in plasma samples from rat spleen and gastric mucosa [130]. Another technology used to generate aptamers and simulta-neously discover various biomarkers is known as aptamer-facilitated biomarker discovery (AptaBiD). It is based on the selection of aptamers from a pool of nucleotides against dif-ferential molecular targets on the cells [131].
3. APTAMERS DEVELOPMENT The aptamers are engineered in such a way that they form
tertiary structures which lock perfectly with the target mole-cule. These aptamers can be prepared by directed evolution techniques also known as in vitro evolution, this involves preparation of large libraries of random DNA or RNA mole-cules from which the sequence specific to target ligands are selected based on competitive binding followed by enrich-ment and amplification. This process is called SELEX [100]. The advantages of using aptamers include features such as low molecular weight, high binding affinity and specificity, ease of synthesis and modifications, low toxicity, increased thermal stability and tissue penetrating ability [99].
3.1. Aptamers Selection
Generally, there are two ways of aptamer selection: (i) the virtual aptamer screening procedure, and (ii) the compu-tational design of structured random pools for selection of advanced aptamers. Due to lack of efficient screening tech-niques, aptamer applications were previously limited. Re-cently, many screening methods have been introduced which are starting to impact the field. The virtual screening process of aptamers contains three main steps: 1. Ascertain the target molecule, 2. add the known length of oligonucleotides SS DNA or
RNA, and

Nucleic Acid-Based Aptamers Current Medicinal Chemistry, 2015, Vol. 22, No. 21 2547
3. use the immobilized or free target for screening and se-lection of aptamers from the DNA or RNA pool [132]. The first method of selecting ligands from a nucleic acid
pool was termed as SELEX [8, 133]. SELEX is an iterative procedure for selection and amplification of SS nucleic acids that bind to the respective targets with high affinity and specificity. The most suitable length for aptamers is between 20-80 nucleotides. The very first step is the synthesis of a large library of randomly sequenced oligonucleotides 20-80 in length with fixed primer regions at 5’ and 3’ ends for PCR amplification [134]. The target molecules are then incubated with this pool of oligonucleotides and then bound or un-bound sequences are separated by means of affinity chroma-tography. Once the bound oligonucleotides have been iso-lated they are put through repeated rounds of selection and amplification (6-20 cycles) and the stringency of the selec-tion by affinity chromatography is increased to isolate the aptamer with very high specificity and affinity for the target molecule. Finally, the oligonucleotides that are most specific towards the target, are cloned in plasmids, amplified and sequenced. Thus, from a very large pool of random oligonu-cleotides, a desired quantity of highly specific aptamers is obtained [135].
Other procedures include negative SELEX, used for the isolation of aptamers that can adsorb the targets, [136], counter SELEX, [137] that includes exchange of matrices with the analogues of the target, subtractive SELEX [138] that removes SS DNA or RNA sequences and can bind to a non-specific part of a complex target with various binding sites, Capillary electrophoresis (CE) SELEX where high-affinity aptamers can be obtained only after two rounds of selection [139] and the most recent method known as Cell-SELEX where the whole living cell is used as a target [140].
With the increase in applications of aptamers, the need for design, identification, and selection of a better variety of aptamers has become more apparent. It has been demon-strated that random RNA/DNA oligonucleotide pools are not structurally diverse and favor the formation of simple struc-tures such as stem-loops [141]. Carothers et al. [142] have shown that increasing the structural diversity of the starting oligonucleotide pool can enhance the possibility of finding better aptamers. A computational approach for designing structured RNA pools was developed by Schlick et al. which functions by modeling the pool generation process using mixing matrices [143]. Other methods developed to improve the structural complexity and diversity of the oligonucleotide pools include random filtering to selectively increase the number of 5-way junctions and genetic filtering to design RNA/DNA pools with any desired structure distribution, including a uniform structure distribution, i.e., 20% 1-way, 2-way, 3-way, 4-way and 5-way junctions [144]. Other methods have been developed that propose a computational approach for designing a starting pool of RNA sequences for the selection of aptamers for specific analyte binding. This approach consists of three steps: (i) selection of RNA se-quences based on their secondary structure, (ii) generating a library of 3D structural RNA molecules and (iii) high-throughput virtual screening of the library to select aptamer with highest binding affinity to the target [145]. One such example is the aptamer against phospholipid phosphatidyl-
serine (PS), an early marker exploited for detecting apopto-sis. An in silico approach, entropic fragment-based approach (EFBA) was used to design the aptamer templates that selec-tively bind to PS [146]. However, Tseng et al. have also de-veloped an aptamer selection procedure without going through the SELEX, based on information-driven theoretical approach that allows the design of aptamer templates de-pendent solely on the structural information about bio-molecular targets [147]. Another study showed synthesis, selection, characterization and binding of kinked peptide-nucleic acids-DNA chimera duplex, where the oligonucleo-tide contains a N-(2-amino-ethyl)-glycine unit replacing the sugar-phosphate backbone which enhances the resistance of the chimera towards exonuclease degradation [148].
3.2. Aptamers Modifications
Even though aptamers hold the capacity to distinguish between closely related but non-identical targets as well as between the different functional, conformational forms of the same target [110] and can withstand a wide range of temperature, pH (4-9), various organic solvents without the loss of potential activity; they are susceptible to nuclease degradation in vivo. Most chemical modifications are intro-duced either at the nucleobase, the phosphate group or at the sugar backbone [149]. Some typical sugar-modified nucleotides include 2’-F, 2’-NH₂, 2’-OCH₃, 2’-methoxy-ethane, 2’-Oxy-dimethyl allyl etc. Nucleotides carrying modifications of the phosphate residues such as phos-phorothioate, methyl phosphonate and the nucleotides car-rying the modifications of nucleobases such as propenyl, 5-(N-aminoalkyl) carbamoyl uracil, methyl, trifluoromethyl, phenyl and 2-thiopryimidine are some other types of ap-tamer modifications that have been used in order to provide stability and resistance from nuclease degradation [150]. Iodide (I), bromide (Br), chloride (Cl), amino (NH₂) and azide (N₃) groups are used for modification of pyrimidines at the 5th position and amino (NH₂), fluoro (F) and methoxy (OCH₃) groups are used for modification at the 2nd position. Other modifications include substitution of 4-thiouridine, 5-bromouracil, backbone modification, methy-lation, use of isobases like isocytidine and isoguanosine [151] and 3’ capping [152] etc.
Post SELEX modifications is followed mainly because many of the chemically-modified nucleotides are not sub-strates of polymerases hence they cannot be directly utilized in SELEX. However, there are modified nucleotides such as 2’-F, 2’-NH₂, 2’-OCH₃ that are successfully employed in SELEX. The Spiegelmer technology is a screening method for obtaining modified aptamers. Here the aptamers of the chiral target from the dextrorotatory oligonucleotide pool are screened first. From this, the complementary levorotatory oligonucleotides are synthesized and finally the chemical modifications are induced. Such modified aptamers have the ability to bind the target with a higher affinity and possess better stability [153]. One of the first examples of application of modified aptamers was in 1994 by Latham et al. who sub-stituted the canonical dT by 5-pentynyl-dU in a thrombin aptamer [154]. Another report showed selection of aptamers against tumour necrosis factor receptor superfamily member 9 (TNFRSF9) by inducing six different modifications at C5 of deoxyuridine using benzyl and indole groups. The modi-

2548 Current Medicinal Chemistry, 2015, Vol. 22, No. 21 Kanwar et al.
fied aptamers were highly specific to the target when com-pared to the non-modified aptamers [155]. 3.3. Chimeric Forms of Aptamers
Through the process of natural recombination or chemi-cal engineering, two different aptamers or an aptamer and other biomolecules are joined together leading to the pro-duction of a chimera [156]. Chimeric aptamers have the potential activity of both parent molecules and thus holds the capability to perform diverse functions at the same time. The selection of chimeric aptamers is done by chi-meric SELEX where libraries are used for chimeric ap-tamer production with more than one desired feature. Each of the parent library molecules is selected distinctly. Then the selected molecules are fused randomly in a way that the chimera gets the novel properties [157]. Multiple SELEX is
another selection procedure where two biomolecules spe-cific for a common target are fused together. Two parent library pools of 40-60 molecules each are fused together with a common target and after 5-6 rounds of selection and amplification, the molecules which are both highly specific to the common target are isolated and fused together to form the chimera [158]. Common chimeras are aptamer-aptamer, aptamer-antibody, aptamer-enzyme, and aptamer-siRNA chimera [87, 157-174]. Selected aptamer chimeras, their target, and their mechanism of action have been listed in Table 2.
Chimerization, however, has not been able to overcome the nuclease degradation problem even though it imparts stability and exceptional qualities to an aptamer. Thus, the concept of locked nucleic acids (LNA’s) was introduced.
Table 2. List of selected chimeric aptamers, targets and their mode of action.
S. No Chimeric Aptamer Target Mechanism Reference
1 Adenosine DNA aptamer - malachite green aptamer Adenosine Disscociation of aptamers produces fluorescence [157]
2 P66 antibody-A8 aptamer Listeria monocytogenes P66 antibody is therapeutic part whereas A8
aptamer is targeting moiety [158]
3 α L-iduronidase-anti-transferrin patamer Fibroblast cells Tansferrin aptamer is targeting moiety and deliver-
ing the enzyme [159]
4 A10 aptamer-siRNA (PLK1 & Bcl2) PLK1 and Bcl2 A10 aptamer for targeting prostatecancer cells and
siRNA for gene silencing [160]
5 PLK1aptamer-siRNA Malignant mesothe-
lioma cells Inhibit tumour proliferation [161]
6 PSMA aptamer-smg1 siRNA Prostate cancer Stimulate anti-tumour immunity [162]
7 PSMA aptamer-PLK1 siRNA Prostate cancer Induce apoptosis [163]
8 siRNA- fluoro-modified aptamer with boranophos-
phate modification Prostate cancer Boron neutron capture therapy [164]
9 PSMA aptamer-Dox-ShRNA Bcl-xL synergistic and selective cancer cell death [165]
10 siRNA-anti-trans activating responsive (TAR) ap-
tamer HIV
Achieving higher affinity and resistance to RNAses
[166]
11 Anti-gp120 aptamer - siRNA HIV Prevents HIV infectivity [167, 168]
12 the anti HIV reverse transcriptase aptamer (HIV-
1RT)-azidothymidine triphosphate (AZTTP) HIV
Inhibition of DNA polymerization by HIV reverse transcriptase
[169]
13 CD4 aptamer-siRNA HIV Knockdown gene expression in CD4 positive cells
to reduce HIV infection [170]
14 Anti αVβ3 aptamer-siRNA(eukaryotic elongation
factor 2) Eukaryotic elongation
factor 2 Induces apoptosis [171]
15 Doxorubicin- Epithelial cell adhesion (EpCAM)
aptamer Retinoblastoma
Targets EpCAM and induces apoptosis specifi-cally in retinoblastoma cells
[172]
16 Doxorubicin-Mucin 1 (Muc-1) aptamer A549 cells Muc-1 acts as targeting and delivery agent [173]
17 Iron saturated lactoferrin (FebLf)-LNA Nucleolin-
LNA EpCAM Colon and Breast cancer
cells Tumour specific targeting using two LNA aptam-
ers and therapy by FebLf [87]
18 LNA Nucleolin-LNA EpCAM Colon and Breast cancer
cells Tumour specific targeting [174]

Nucleic Acid-Based Aptamers Current Medicinal Chemistry, 2015, Vol. 22, No. 21 2549
3.4. Locked Nucleic Acids
Locked nucleic acid (LNA) nucleotide (Fig. 2) is one of the most promising and successful nucleotide analog re-ported to date [175, 176]. In LNA, the furanose ring of the ribose sugar is locked by the introduction of a 2’-O, 4’C-methylene bridge which conformationally restricts the LNA nucleotides to adopt N-type sugar puckering (Fig. 2).
Fig. (2). LNA. Structural representation of a locked nucleic acid nucleotide monomer.
Due to its conformational restriction, LNA exhibits a high degree of thermal stability and resistance to nuclease degradation accounting for an improved plasma stability of LNA-containing oligonucleotides. Veedu et al. extensively investigated the enzymatic recognition capabilities of LNA nucleotides towards the scope of LNA aptamer development by SELEX methods [177-179]. It has been shown that the introduction of LNA nucleotides into a known aptamer, sig-nificantly improves its stability and in some cases, affinity. For example, Schmidt et al. [73] described the capability of LNA modifications to improve the in vivo stability of aptam-ers and their targeting function. Recently, Hernandez et al. reported that the incorporation of one LNA nucleotide to avidin binding DNA aptamer significantly improved the binding affinity [180]. In another work, LNA incorporation
in a 39-mer oligonucleotide TTA1 (RNA aptamer) improved the plasma stability and maintained the high binding affinity of the aptamer towards its target [181]. In another report, LNA improved the stability, binding affinity and nuclease resistance [182]. Furthermore, it is noteworthy that the re-markable properties of LNA nucleotides has also been util-ized in nanotechnology by conjugating LNA to nanoparticles (LNPs) whereby it has been determined that LNPs were more stable and imparted better effects on the target when compared to non-modified aptamer-nanoparticle conjugates [182] (Fig. 3). All of the above-mentioned applications fur-ther reinforce and direct us towards the applicability of LNA nucleotides in aptamer-based therapeutic development.
4. APTAMERS IN CLINICAL TRIALS
Aptamers have been successful in a wide range of clini-cal trials owing to their extremely high specificity and lack of immunogenicity or pathogenicity. With time, more num-bers of aptamers have reached clinical trials and gained the trust of several pharmaceuticals. The first aptamer was approved by the FDA in 2005, since then nearly 12 aptamers are in clinical trials. Vascular endo-thelial growth factor (VEGF) is known to be the major cause of visual loss in the age-related macular degeneration (AMD) and macugen blocks vegf165 (Fig. 4). The results from clinical trials had demonstrated that macugen stabilized vision and reduced risk of severe visual loss in the majority of patients with AMD and some patients also showed visual improvement. Thus, macugen went on to get FDA approval in 2005 [15].
Coronary thrombosis generally leads to both ischemia and bleeding and REG1 uniquely minimizes the risk of both ischemia and bleeding simultaneously. In phase 1 it was
Fig. (3). LNA-chimeric-aptamer-Np conjugate. The LNA aptamer chimeras are highly stable and nuclease resistant as compared to aptam-ers alone. Hence the LNA-chimeric-aptamer-Np conjugate has a better chance of internalization in the target cells as compared to aptamer-Np conjugates.

2550 Current Medicinal Chemistry, 2015, Vol. 22, No. 21 Kanwar et al.
Fig. (4). Macugen, the first FDA approved aptamer. VEGF binds to VEGF receptors and leads to angiogenesis. In the presence of Macugen there is no angiogenesis as Macugen attaches with the VEGF and prevents the binding of VEGF to its receptors (as suggested by Ng, E. W. et al. [15]). well-tolerated by the patients and a dose-dependant predict-able complete or partial reversal of the disorder was seen. In Phase IIb, the results confirmed a consistent reduction in ischemic events and a consistent dose-related reduction in major bleeds. Regado is currently preparing for a single phase III trials [183].
EYE001 which prevents the formation of new blood ves-sels by blocking VEGFR was tested in 15 patients with sub-foveal choroidal neovascularization in phase 1A trials. The results revealed that 80% of patients showed stable or im-proved vision after 3 months of treatments and 27% of eyes demonstrated a three-line or greater improvement in vision. Currently, EYE001 is undergoing phase II/III trials [184, 185].
E100300 also known as fovista was tested in 22 patients in phase I/IIa where no adverse effects were reported and all patients showed 86% regression of neovascular AMD. In phase IIb, it was tested on 449 patients in combination with Lucentis and the results showed a mean +10.6 letters of vi-sion improvement at six months and a 62% improvement when compared to Lucentis alone [186, 187].
The phase I/IIa clinical trials of ARC1905 was conducted in 43 patients with wet AMD and the results showed im-proved vision acuity at all timepoints [188, 189].
The ARC1779 was tested on 47 healthy volunteers as phase I trial and demonstrated dose-and concentration de-pendent inhibition of von willebrand factor (vWF) activity and platelet function. Currently, it is being tested on 300 patients suffering from acute coronary syndrome in phase IIa trials [190, 191].
Baxter’s ARC19499 which blocks the tissue factor path-way inhibitor (TFPI) and improves blood clotting is also undergoing phase I/II clinical trials in patients with hemo-philia A and B [192].
Nu172 was tested in healthy volunteers in phase 1 clini-cal trials where it produced a dose-dependent increase in anti-coagulation, measured by activated clotting time (ACT). Currently, Nu172 is undergoing phase II studies in 30 pa-tients undergoing primary, elective, off-pump coronary ar-tery bypass surgery [193, 194].
The largest prevent or clinical trial phase III was con-ducted for E₂F where 1404 patients with critical limb ische-mia were treated with E₂F. The results were quite successful and most patients showed a statistically significant im-provement [195, 196].
A phase I trial of AS1411 (binds to nucleolin on cancer cells and induces apoptosis) in 30 patients with advanced cancer showed significant improvement in patient condition and the phase II trials were conducted in 71 patients with acute myeloid lymphoma (AML). The results showed that AS1411 was well tolerated and showed promising anti-cancer activity in patients. Currently, it is undergoing phase III trials with 90 patients suffering from AML [197, 198].
In phase 1 LY2181308 was given to 14 patients with ad-vanced solid tumors and results showed an extensive tissue distribution with a long terminal half-life, the disease was stable in patients. In phase II, 154 patients with castration-resistant prostate cancer (CRPC) were tested with LY2181308. The results were not very encouraging. How-ever, it was also tested in combination with Docetaxel in patients with locally advanced or metastatic non-small cell lung cancer (NSCLC) in phase II where it showed promising results and is currently undergoing phase III trials in patients with NSCLC [199, 200].
Emapticap pegol also known as Nox-E36 successfully completed phase 1 trial in patients with renal impairment and, is now undergoing phase IIb trials with 75 patients suf-fering from diabetes mellitus [201].

Nucleic Acid-Based Aptamers Current Medicinal Chemistry, 2015, Vol. 22, No. 21 2551
Table 3. Aptamers in clinical trials.
Aptamer Company Disease Target Mode of Action Clinical Trail
Phase Reference
Macugen (Pegaptanib)
Eyetech Pharmaceuticals/Pfizer
AMD, Diabetic Retinopathy
VEGF-165 Competitive inhibition of
VEGF FDA
Approved [15]
REG1 (RB006 & RB007)
Regado Biosciences Arterial thrombosis Factor IXa Controls blood thinning Phase III [183]
EYE001 Gilead Sciences, Inc. Neovascular AMD VEGFR Prevents formation of new
blood vessels Phase II/III [184, 185]
E100300 Ophthotech Corporation
Neovascular AMD PDGF Prevents binding of PDGF
to PDGF-β Phase III [186, 187]
ARC1905 Ophthotech Corporation
AMD C₅ Factor Prevents formation of
membrane attack complex Phase II [188, 189]
ARC1779 Archemix Corporation Acute coronary
syndromes
A1 domain of Von Willebrand Factor
(vWF)
Inhibits binding of platelet receptor glycoprotein Ib
Phase II/III [190, 191]
ARC19499 Baxter Biosciences Haemophilia Anti-tissue factor inhibitor (TFPI)
Improves blood clotting Phase I/II [192]
Nu172 ARCA
Biopharma/Archimex Corp
Heart diseases Thrombin Prevents blood clotting Phase II [193, 194]
E₂F (edifo-ligide)
Corgentech and Bristol Myers Squibb
Vein graft failure of heart and leg
- - Phase III [195, 196]
AS1411 Antisoma/Archimex AML Nucleolin Inhibits DNA replication
to cause cell death Phase III [197, 198]
LY2181308 Oxford Cancer
Research Non-small cell lung
cancer (NSLC) Survivin mRNA
Inhibits survivin expres-sion
Phase III [199, 200]
Nox-E36 NOXXON Pharma Type 2 diabetes
mellitus and diabetic nephropathy
CCL2 (Monocyte chemotactic pro-
tein-1MCP-1) Inhibits MCP-1 Phase IIb [201]
Nox-A12 NOXXON Pharma Various types of cancer Stromal cell de-rived factor-1 (SDF-1 alpha)
Inhibits SDF-1 Phase IIa [202]
Nox-A12 which sensitizes cancer cells to chemotherapy
has successfully completed phase I trials and undergoing phase IIa trials for the treatment of chronic lymphocytic leu-kemia in 28 patients [202].
The clinical trial results have all been very promising and it gives a new hope to change the conventional style of ther-apy. Aptamers have attained high therapeutic levels in a very short time as compared to synthetic drugs or other modes of therapy. Some of the aptamers undergoing clinical trials with promising results are mentioned (Table 3).
CONCLUSION
The commercial success of macugen has made it clear that aptamers are safe to use as they are non-toxic, non-immunogenic and non-pathogenic. The most important fea-
ture of aptamers is their high specificity that can potentially be used to target many diseases. Aptamers can be widely used and their production costs are far less when compared to any synthetic drug. It has been estimated that the current cost of goods for aptamer synthesis at the kilogram scale is estimated at $500/g and is expected to be lowered to $100/g via technology, a number that is significantly less when compared to antibodies and proteins. Aptamers with high specificity can be generated for any antigen, including small molecules, proteins, nucleic acids, cells, tissues and even whole organisms. They have a good shelf life (can be stored for more than 1 yr). As a result of these benefits, the phar-maceutical companies are interested in them. From this and other reviews it’s clear that aptamers in clinical trials have been successful and well tolerated by patients suffering from a wide range of diseases such as age-related macular degen-eration (AMD), diabetic and neovascular retinopathy, arterial

2552 Current Medicinal Chemistry, 2015, Vol. 22, No. 21 Kanwar et al.
thrombosis, acute coronary syndromes, hemophilia, heart diseases, vein graft failure of heart and leg, acute myeloid lymphoma (AML), non-small cell lung carcinoma (NSLC), type 2 diabetes and various types of cancers. With currently available efficient aptamer selection technologies most anti-body-based systems can be replaced by aptamer-based sys-tems that are likely to offer superior results. Aptamers can be used for better imaging as well as for the detection of various bioanalytes.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest and have no affiliation or financial involvement with any organization or entity discussed in this manuscript. This in-cludes employment, consultancies, honoraria, grants, stock ownership or options, expert testimony, patents (received or pending) or royalties. No writing assistance was utilized in the production of this manuscript and the authors have re-ceived no payment for its preparation.
The findings and conclusions in this review reflect the current views of the authors. They should not be attributed, in whole or in part, to the organizations with which they are affiliated, nor should they be considered as expressing an opinion with regard to the merits of any particular company or product discussed herein.
ACKNOWLEDGEMENTS
The authors would like to thank the Australia–India Stra-tegic Research Fund (AISRF, BF030016) and National Health and Medical Research Council (NHMRC, APP1050286) for providing the funding for this project.
REFERENCES [1] Langer, R. Drug delivery and targeting. Nature, 1998, 392(6679),
5-10. [2] Ferrari, M. Cancer nanotechnology: Opportunities and challenges.
Nat. Rev. Cancer, 2005, 5(3), 161-171. [3] Guillemard, V.; Saragovi, H.U. Novel approaches for targeted
cancer therapy. Curr. Cancer Drug Targets, 2004, 4(4), 313-326. [4] Zhang, X.Q.; Wang, X.L.; Zhang, P.C.; Liu, Z.L.; Zhuo, R.X.;
Mao, H.Q.; Leong, K.W. Galactosylated ternary DNA/polyphosphoramidate nanoparticles mediate high gene trans-fection efficiency in hepatocytes. J. Control. Release, 2005, 102(3), 749-763.
[5] Chames, P.; Van Regenmortel, M.; Weiss, E.; Baty, D. Therapeutic antibodies: successes, limitations and hopes for the future. Br. J. Pharmacol., 2009, 157(2), 220-233.
[6] Jayasena, S.D. Aptamers: An emerging class of molecules that rival antibodies in diagnostics. Clin. Chem., 1999, 45(9), 1628-1650.
[7] Ueyama, H.; Takagi, M.; Takenaka, S. A novel potassium sensing in aqueous media with a synthetic oligonucleotide derivative. Fluo-rescence resonance energy transfer associated with guanine quartet-potassium ion complex formation. J. Am. Chem. Soc., 2002, 124(48), 14286-14287.
[8] Tuerk, C.; Gold, L. Systematic evolution of ligands by exponential enrichment - RNA Ligands to bacteriophage-T4 DNA-polymerase. Science, 1990, 249(4968), 505-510.
[9] Huang, D.B.; Vu, D.; Cassiday, L.A.; Zimmerman, J.M.; Maher, L.J. 3rd; Ghosh, G. Crystal structure of NF-kappaB(p50)2 com-plexed to a high-affinity RNA aptamer. Proc. Natl. Acad. Sci. USA, 2003, 100(16), 9268-9273.
[10] Fitzwater, T.; Polisky, B. A SELEX primer. Methods Enzymol., 1996, 267, 275-301.
[11] Hermann, T.; Patel, D.J. Adaptive recognition by nucleic acid aptamers. Science, 2000, 287(5454), 820-825.
[12] White, R.R.; Sullenger, B.A.; Rusconi, C.P. Developing aptamers into therapeutics. J. Clin. Invest., 2000, 106(8), 929-934.
[13] Tombelli, S.; Minunni, A.; Mascini, A. Analytical applications of aptamers. Biosens. Bioelectron., 2005, 20(12), 2424-2434.
[14] Charlton, J.; Sennello, J.; Smith, D. In vivo imaging of inflamma-tion using an aptamer inhibitor of human neutrophil elastase. Chem. Biol., 1997, 4(11), 809-816.
[15] Ng, E.W.; Shima, D.T.; Calias, P.; Cunningham, E.T.; Guyer, D.R.; Adamis, A.P. Pegaptanib, a targeted anti-VEGF aptamer for ocular vascular disease. Nat. Rev. Drug Discov., 2006, 5(2), 123-132.
[16] Song, K.-M.; Lee, S.; Ban, C. Aptamers and their biological appli-cations. Sensors, 2012, 12(1), 612-631.
[17] DeAnda, A. Jr.; Coutre, S.E.; Moon, M.R; Vial, C.M; Griffin, L.C; Law, V.S; Komeda, M; Leung, L.L.K; Miller, D.C. , Pilot study of the efficacy of a thrombin inhibitor for use during cardiopulmonary bypass. Ann. Thorac. Surg., 1994, 58(2), 344-350.
[18] Cho, E.J.; Lee, J.W.; Ellington, A.D. Applications of aptamers as sensors. Annu. Rev. Anal. Chem., 2009, 2, 241-264.
[19] Min, K.; Jo, H.; Song, K.; Cho, M.; Chun, Y.S.; Jon, S.; Kim, W.J.; Ban, C. Dual-aptamer-based delivery vehicle of doxorubicin to both PSMA(+) and PSMA(-) prostate cancers. Biomaterials, 2011, 32(8), 2124-2132.
[20] Shin, S.; Kim, I.H.; Kang, W.; Yang, J.K.; Hah, S.S. An alternative to Western blot analysis using RNA aptamer-functionalized quan-tum dots. Bioorg. Med. Chem. Lett., 2010, 20(11), 3322-3325.
[21] Romig, T.S.; Bell, C.; Drolet, D.W. Aptamer affinity chromatogra-phy: combinatorial chemistry applied to protein purification. J. Chromatogr. B., 1999, 731(2), 275-284.
[22] Emahi, I.G. P.R; Freitag, L; Baum, D.A. Investigating the Redox Abilities of DNA Aptamers Bound to Redox Cofactors for Possible Application in Biofuel Cells. 225th ECS Meeting: Orlando, Fl, 2014.
[23] Yu, C.; Hu, Y.; Duan, J.; Yuan, W.; Wang, C.; Xu, H.; Yang, X.-D. Novel aptamer-nanoparticle bioconjugates enhances delivery of anticancer drug to MUC1-positive cancer cells in vitro. PLoS One, 2011, 6(9), e24077.
[24] Tan, L.; Neoh, K.G.; Kang, E.T.; Choe, W.S.; Su, X. PEGylated anti-‐MUC1 aptamer-‐doxorubicin complex for targeted drug deliv-ery to MCF7 breast cancer cells. Macromol. Biosci., 2011, 11(10), 1331-1335.
[25] Chang, K.; Pi, Y.; Lu, W.; Wang, F.; Pan, F.; Li, F.; Jia, S.; Shi, J.; Deng, S.; Chen, M. Label-free and high-sensitive detection of hu-man breast cancer cells by aptamer-based leaky surface acoustic wave biosensor array. Biosens. Bioelectron., 2014, 60, 318-324.
[26] Zhao, J.; Ma, Y.; Cui, S.; Cao, J.; Achilefu, S.; Gu, Y. MUC1 ap-tamer based near infrared fluorescence probes for tumor diagnosis. SPIE BiOS, 2013, 8596, 859614-859619.
[27] Liu, N.; Zhou, C.; Zhao, J.; Chen, Y. Reversal of paclitaxel resis-tance in epithelial ovarian carcinoma cells by a MUC1 aptamer-let-7i chimera. Cancer Invest., 2012, 30(8), 577-582.
[28] Bruno, J.G. Aptamer–biotin–streptavidin–C1q complexes can trigger the classical complement pathway to kill cancer cells. In Vi-tro Cell. Dev. Biol. Anim., 2010, 46(2), 107-113.
[29] Baouendi, M.; Cognet, J.A.; Ferreira, C.S.; Missailidis, S.; Coutant, J.; Piotto, M.; Hantz, E.; Hervé du Penhoat, C. Solution structure of a truncated anti-‐MUC1 DNA aptamer determined by mesoscale modeling and NMR. FEBS J., 2012, 279(3), 479-490.
[30] Chang, Y.M.; Donovan, M.J.; Tan, W. Using aptamers for cancer biomarker discovery. J. Nucleic Acids, 2013, 817350. doi: 10.1155/2013/817350.
[31] Lu, Y.; Wu, P.; Yin, Y.; Zhang, H.; Cai, C. Aptamer-functionalized graphene oxide for high efficient loading and cancer cell-specific delivery of antitumor drug. J. Mater. Chem., B., 2014, 2, 3849-3859.
[32] Zhu, G.; Zheng, J.; Song, E.; Donovan, M.; Zhang, K.; Liu, C.; Tan, W. Self-assembled, aptamer-tethered DNA nanotrains for tar-geted transport of molecular drugs in cancer theranostics. PNAS, 2013, 110(20), 7998-8003.
[33] Zhang, J.; Sheng, W.; Fan, Z.H. An ensemble of aptamers and antibodies for multivalent capture of cancer cells. Chem. Commun., 2014, 50, 6722-6725.
[34] Shangguan, D.; Tang, Z.; Mallikaratchy, P.; Xiao, Z.; Tan, W. Optimization and modifications of aptamers selected from live can-cer cell lines. Chembiochem., 2007, 8(6), 603-606.

Nucleic Acid-Based Aptamers Current Medicinal Chemistry, 2015, Vol. 22, No. 21 2553
[35] Li, N.; Ebright, J.N.; Stovall, G.M.; Chen, X.; Nguyen, H.H.; Singh, A.; Syrett, A.; Ellington, A.D. Technical and biological is-sues relevant to cell typing with aptamers. J. Proteome Res., 2009, 8(5), 2438-2448.
[36] Song, Y.; Zhu, Z.; An, Y.; Zhang, W.; Zhang, H.; Liu, D.; Yu, C.; Duan, W.; Yang, C.J. Selection of DNA aptamers against epithelial cell adhesion molecule for cancer cell imaging and circulating tu-mor cell capture. Anal. Chem., 2013, 85(8), 4141-4149.
[37] Wu, Y.; Sefah, K.; Liu, H.; Wang, R.; Tan, W. DNA aptamer–micelle as an efficient detection/delivery vehicle toward cancer cells. PNAS, 2010, 107(1), 5-10.
[38] Fan, Z.H.; Sheng, W.; Chen, T.; Tan, W. Efficient isolation of tumor cells in whole blood using aptamers immobilized in a device. Anal. Chem. 2012, 84(9), 4199-4206
[39] Ray, P.; White, R.R. Aptamers for targeted drug delivery. Pharma-ceuticals, 2010, 3(6), 1761-1778.
[40] Hwang, D.W.; Ko, H.Y.; Lee, J.H.; Kang, H.; Ryu, S.H.; Song, I.C.; Lee, D.S.; Kim, S. A Nucleolin-targeted multimodal nanopar-ticle imaging probe for tracking cancer cells using an aptamer. J. Nucl. Med., 2010, 51(1), 98-105.
[41] Aravind, A.; Jeyamohan, P.; Nair, R.; Veeranarayanan, S.; Na-gaoka, Y.; Yoshida, Y.; Maekawa, T.; Kumar, D.S. AS1411 ap-tamer tagged PLGA-lecithin-PEG nanoparticles for tumor cell tar-geting and drug delivery. Biotechnol. Bioeng., 2012, 109(11), 2920-2931.
[42] Latorre, A.; Posch, C.; Gracimartin, Y.; Celli, A.; Sanlorenzo, M.; Vujic, I.; Ma, J.; Zekhtser, M.; Rappersberger, K.; Ortiz-Urda, S. DNA and aptamer stabilized gold nanoparticles for targeted deliv-ery of anticancer therapeutics. Nanoscale, 2014, 6(13), 7436-7442.
[43] Lee, K.Y.; Kang, H.; Ryu, S.H.; Lee, D.S.; Lee, J.H.; Kim, S. Bio-imaging of nucleolin aptamer-containing 5-(N-benzylcarboxy-amide)-2′-deoxyuridine more capable of specific binding to targets in cancer cells. J. Biomed. Biotechnol., 2010, Article ID 168306, 9 pages, 2010. doi:10.1155/2010/168306.
[44] Kim, J.K.; Choi, K.-J.; Lee, M.; Jo, M.-h.; Kim, S. Molecular imag-ing of a cancer-targeting theragnostics probe using a nucleolin ap-tamer- and microRNA-221 molecular beacon-conjugated nanopar-ticle. Biomaterials, 2012, 33(1), 207-217.
[45] Bayrac, A.T.; Sefah, K.; Parekh, P.; Bayrac, C.; Gulbakan, B.; Oktem, H.A.; Tan, W. In vitro selection of DNA aptamers to glioblastoma multiforme. ACS Chem. Neurosci., 2011, 2(3), 175-181.
[46] Sheng, W.; Chen, T.; Kamath, R.; Xiong, X.; Tan, W.; Fan, Z.H. Aptamer-enabled efficient isolation of cancer cells from whole blood using a microfluidic device. Anal. Chem., 2012, 84(9), 4199-4206.
[47] Liu, Q.; Jin, C.; Wang, Y.; Fang, X.; Zhang, X.; Chen, Z.; Tan, W. Aptamer-conjugated nanomaterials for specific cancer cell recogni-tion and targeted cancer therapy. NPG Asia Mater., 2014, 6(4), e95.
[48] Kang, H.S.; Huh, Y.M.; Kim, S.; Lee, D.-k. Isolation of RNA ap-tamers targeting HER-2-overexpressing breast cancer cells using cell-SELEX. Bull. Korean Chem. Soc., 2009, 30(8), 1827-1831.
[49] Daniels, D.A.; Chen, H.; Hicke, B.J.; Swiderek, K.M.; Gold, L. A tenascin-C aptamer identified by tumor cell SELEX: Systematic evolution of ligands by exponential enrichment. PNAS, 2003, 100(26), 15416-15421.
[50] Ninomiya, K.; Kaneda, K.; Kawashima, S.; Miyachi, Y.; Ogino, C.; Shimizu, N. Cell-SELEX based selection and characterization of DNA aptamer recognizing human hepatocarcinoma. Bioorg. Med. Chem. Lett., 2013, 23(6), 1797-1802.
[51] Wang, J.; Sefah, K.; Altman, M.B.; Chen, T.; You, M.; Zhao, Z.; Huang, C.Z.; Tan, W. Aptamer-conjugated nanorods for targeted photothermal therapy of prostate cancer stem cells. Chem. – An Asian J., 2013, 8(10), 2417-2422.
[52] Jiménez, E.; Sefah, K.; López-Colón, D.; Van Simaeys, D.; Chen, H.W.; Tockman, M.S.; Tan, W. Generation of lung adenocarci-noma DNA aptamers for cancer studies. PLoS One, 2012, 7(10), e46222.
[53] Chen, H.W.; Medley, C.D.; Sefah, K.; Shangguan, D.; Tang, Z.; Meng, L.; Smith, J.E.; Tan, W. Molecular recognition of small-‐cell lung cancer cells using aptamers. Chem. Med. Chem., 2008, 3(6), 991-1001.
[54] Farokhzad, O.C.; Cheng, J.; Teply, B.A.; Sherifi, I.; Jon, S.; Kan-toff, P.W.; Richie, J.P.; Langer, R. Targeted nanoparticle-aptamer
bioconjugates for cancer chemotherapy in vivo. PNAS, 2006, 103(16), 6315-6320.
[55] Bagalkot, V.; Farokhzad, O.C.; Langer, R.; Jon, S. An aptamer–doxorubicin physical conjugate as a novel targeted drug-delivery platform. Angew. Chem. Int. Ed., 2006, 45(48), 8149-8152.
[56] McNamara, J.O.; Andrechek, E.R.; Wang, Y.; Viles, K.D.; Rempel, R.E.; Gilboa, E.; Sullenger, B.A.; Giangrande, P.H. Cell type–specific delivery of siRNAs with aptamer-siRNA chimeras. Nat. Biotechnol., 2006, 24(8), 1005-1015.
[57] Bandekar, A.; Zhu, C.; Jindal, R.; Bruchertseifer, F.; Morgenstern, A.; Sofou, S. Anti–prostate-specific membrane antigen liposomes loaded with 225Ac for potential targeted antivascular α-particle therapy of cancer. J. Nucl. Med., 2014, 55(1), 107-114.
[58] Min, K.; Jo, H.; Song, K.; Cho, M.; Chun, Y.-S.; Jon, S.; Kim, W.J.; Ban, C. Dual-aptamer-based delivery vehicle of doxorubicin to both PSMA(+) and PSMA(−) prostate cancers. Biomaterials, 2011, 32(8), 2124-2132.
[59] Chu, T.C.; Shieh, F.; Lavery, L.A.; Levy, M.; Richards-Kortum, R.; Korgel, B.A.; Ellington, A.D. Labeling tumor cells with fluo-rescent nanocrystal–aptamer bioconjugates. Biosens. Bioelectron., 2006, 21(10), 1859-1866.
[60] Lupold, S.E.; Hicke, B.J.; Lin, Y.; Coffey, D.S. Identification and characterization of nuclease-stabilized RNA molecules that bind human prostate cancer cells via the prostate-specific membrane an-tigen. Cancer Res., 2002, 62(14), 4029-4033.
[61] Farokhzad, O.C.; Karp, J.M.; Langer, R. Nanoparticle-aptamer bioconjugates for cancer targeting. Expert Opin. Drug Deliv. 2006, 3(3), 311-324.
[62] Shigdar, S.; Lin, J.; Yu, Y.; Pastuovic, M.; Wei, M.; Duan, W. RNA aptamer against a cancer stem cell marker epithelial cell ad-hesion molecule. Cancer Sci., 2011, 102(5), 991-998.
[63] Zhang, P.; Zhao, N.; Zeng, Z.; Chang, C.-C.; Zu, Y. Combination of an aptamer probe to CD4 and antibodies for multicolored cell phenotyping. Am. J. Clin. Pathol., 2010, 134(4), 586-593.
[64] Guo, S.; Tschammer, N.; Mohammed, S.; Guo, P. Specific delivery of therapeutic RNAs to cancer cells via the dimerization mecha-nism of phi29 motor pRNA. Human Gene Ther., 2005, 16(9), 1097-1110.
[65] Dharmasiri, U.; Balamurugan, S.; Adams, A.A.; Okagbare, P.I.; Obubuafo, A.; Soper, S.A. Highly efficient capture and enumera-tion of low abundance prostate cancer cells using prostate-‐specific membrane antigen aptamers immobilized to a polymeric microflu-idic device. Electrophoresis, 2009, 30(18), 3289-3300.
[66] Wan, Y.; Kim, Y.-t.; Li, N.; Cho, S.K.; Bachoo, R.; Ellington, A.D.; Iqbal, S.M. Surface-immobilized aptamers for cancer cell isolation and microscopic cytology. Cancer Res., 2010, 70(22), 9371-9380.
[67] Li, N.; Larson, T.; Nguyen, H.H.; Sokolov, K.V.; Ellington, A.D. Directed evolution of gold nanoparticle delivery to cells. Chem. Commun., 2010, 46(3), 392-394.
[68] Master, A.M.; Sen Gupta, A. EGF receptor-targeted nanocarriers for enhanced cancer treatment. Nanomedicine, 2012, 7(12), 1895-1906.
[69] Chi-hong, B.C.; Chernis, G.A.; Hoang, V.Q.; Landgraf, R. Inhibi-tion of heregulin signaling by an aptamer that preferentially binds to the oligomeric form of human epidermal growth factor receptor-3. PNAS, 2003, 100(16), 9226-9231.
[70] Hicke, B.J.; Stephens, A.W.; Gould, T.; Chang, Y.-F.; Lynott, C.K.; Heil, J.; Borkowski, S.; Hilger, C.-S.; Cook, G.; Warren, S.; Schmidt, P.G. Tumor targeting by an aptamer. J. Nucl. Med., 2006, 47(4), 668-678.
[71] Zhou, J.; Rossi, J.J. Cell-specific aptamer-mediated targeted drug delivery. Oligonucleotides, 2011, 21(1), 1-10.
[72] Hicke, B.J.; Marion, C.; Chang, Y.-F.; Gould, T.; Lynott, C.K.; Parma, D.; Schmidt, P.G.; Warren, S. Tenascin-C aptamers are generated using tumor cells and purified protein. J. Biol. Chem., 2001, 276(52), 48644-48654.
[73] Schmidt, K.S.; Borkowski, S.; Kurreck, J.; Stephens, A.W.; Bald, R.; Hecht, M.; Friebe, M.; Dinkelborg, L.; Erdmann, V.A. Application of locked nucleic acids to improve aptamer in vivo stability and target-ing function. Nucleic Acids Res., 2004, 32(19), 5757-5765.
[74] Meyer, M.; Scheper, T.; Walter, J.-G. Aptamers: versatile probes for flow cytometry. Appl. Microbiol. Biotechnol., 2013, 97(16), 7097-7109.

2554 Current Medicinal Chemistry, 2015, Vol. 22, No. 21 Kanwar et al.
[75] Wang, A.Z.; Farokhzad, O.C. Current progress of aptamer-based molecular imaging. J. Nucl. Med., 2014, 55(3), 353-356.
[76] Shangguan, D.; Cao, Z.C.; Li, Y.; Tan, W. Aptamers evolved from cultured cancer cells reveal molecular differences of cancer cells in patient samples. Clin. Chem., 2007, 53(6), 1153-1155.
[77] Shangguan, D.; Li, Y.; Tang, Z.; Cao, Z.C.; Chen, H.W.; Mal-likaratchy, P.; Sefah, K.; Yang, C.J.; Tan, W. Aptamers evolved from live cells as effective molecular probes for cancer study. PNAS, 2006, 103(32), 11838-11843.
[78] Mallikaratchy, P.; Tang, Z.; Kwame, S.; Meng, L.; Shangguan, D.; Tan, W. Aptamer directly evolved from live cells recognizes mem-brane bound immunoglobin heavy mu chain in Burkitt's lymphoma Cells. Mol. Cell. Proteom., 2007, 6(12), 2230-2238.
[79] Tang, Z.; Shangguan, D.; Wang, K.; Shi, H.; Sefah, K.; Mallik-ratchy, P.; Chen, H.W.; Li, Y.; Tan, W. Selection of aptamers for molecular recognition and characterization of cancer cells. Anal. Chem., 2007, 79(13), 4900-4907.
[80] Zhang, K.; Tan, T.; Fu, J.-J.; Zheng, T.; Zhu, J.-J. A novel aptamer-based competition strategy for ultrasensitive electrochemical detec-tion of leukemia cells. Analyst, 2013, 138(21), 6323-6330.
[81] Medley, C.D.; Smith, J.E.; Tang, Z.; Wu, Y.; Bamrungsap, S.; Tan, W. Gold nanoparticle-based colorimetric assay for the direct detec-tion of cancerous cells. Anal. Chem., 2008, 80(4), 1067-1072.
[82] Shi, H.; He, X.; Wang, K.; Wu, X.; Ye, X.; Guo, Q.; Tan, W.; Qing, Z.; Yang, X.; Zhou, B. Activatable aptamer probe for con-trast-enhanced in vivo cancer imaging based on cell membrane pro-tein-triggered conformation alteration. PNAS, 2011, 108(10), 3900-3905.
[83] Wang, A.Z.; Bagalkot, V.; Vasilliou, C.C.; Gu, F.; Alexis, F.; Zhang, L.; Shaikh, M.; Yuet, K.; Cima, M.J.; Langer, R. Superpar-amagnetic iron oxide nanoparticle–aptamer bioconjugates for com-bined prostate cancer imaging and therapy. Chem. Med. Chem., 2008, 3(9), 1311-1315.
[84] Kim, D.; Jeong, Y.Y.; Jon, S. A Drug-loaded aptamer−gold nanoparticle bioconjugate for combined CT imaging and therapy of prostate cancer. ACS Nano, 2010, 4(7), 3689-3696.
[85] Winnard, P.T.; Pathak, A.P.; Dhara, S.; Cho, S.Y.; Raman, V.; Pomper, M.G. Molecular imaging of metastatic potential. J. Nucl. Med., 2008, 49(Suppl. 2), 96S-112S.
[86] Pieve, C.D.; Perkins, A.C.; Missailidis, S. Anti-MUC1 aptamers: radiolabelling with 99mTc and biodistribution in MCF-7 tumour-bearing mice. Nucl. Med. Biol., 2009, 36(6), 703-710.
[87] Kanwar, J.R.; Roy, K.; Kanwar, R.K. Chimeric aptamers in cancer cell-targeted drug delivery. Crit. Rev. Biochem. Mol. Biol., 2011, 46(6), 459-477.
[88] Pei, X.; Zhang, J.; Liu, J. Clinical applications of nucleic acid ap-tamers in cancer. Mol. Clin. Oncol., 2014, 2(3), 341.
[89] Wu, X.; Ding, B.; Gao, J.; Wang, H.; Fan, W.; Wang, X.; Zhang, W.; Ye, L.; Zhang, M.; Ding, X. Second-generation aptamer-conjugated PSMA-targeted delivery system for prostate cancer therapy. Int. J. Nanomedicine, 2011, 6, 1747-1756.
[90] Ni, X.; Zhang, Y.; Ribas, J.; Chowdhury, W.H.; Castanares, M.; Zhang, Z.; Laiho, M.; DeWeese, T.L.; Lupold, S.E. Prostate-targeted radiosensitization via aptamer-shRNA chimeras in human tumor xenografts. J. Clin. Invest., 2011, 121(6), 2383.
[91] Farokhzad, O.C.; Jon, S.; Khademhosseini, A.; Tran, T.-N.T.; LaVan, D.A.; Langer, R. Nanoparticle-aptamer bioconjugates: a new approach for targeting prostate cancer cells. Cancer Res., 2004, 64(21), 7668-7672.
[92] De Tito, S.; Morvan, F.; Meyer, A.; Vasseur, J.-J.; Cummaro, A.; Petraccone, L.; Pagano, B.; Novellino, E.; Randazzo, A.; Giancola, C. Fluorescence enhancement upon g-quadruplex folding: synthe-sis, structure, and biophysical characterization of a dan-syl/cyclodextrin-tagged thrombin binding aptamer. Bioconjug. Chem., 2013, 24(11), 1917-1927.
[93] Musumeci, D.; Montesarchio, D. Polyvalent nucleic acid aptamers and modulation of their activity: a focus on the thrombin binding aptamer. Pharmacol. Ther., 2012, 136(2), 202-215.
[94] Dhar, S.; Kolishetti, N.; Lippard, S.J.; Farokhzad, O.C. Targeted delivery of a cisplatin prodrug for safer and more effective prostate cancer therapy in vivo. PNAS, 2011, 108(5), 1850-1855.
[95] Kolishetti, N.; Dhar, S.; Valencia, P.M.; Lin, L.Q.; Karnik, R.; Lippard, S.J.; Langer, R.; Farokhzad, O.C. Engineering of self-
assembled nanoparticle platform for precisely controlled combina-tion drug therapy. PNAS, 2010, 107(42), 17939-17944.
[96] Savla, R.; Taratula, O.; Garbuzenko, O.; Minko, T. Tumor targeted quantum dot-mucin 1 aptamer-doxorubicin conjugate for imaging and treatment of cancer. J. Control. Release, 2011, 153(1), 16-22.
[97] Shangguan, D.; Cao, Z.; Meng, L.; Mallikaratchy, P.; Sefah, K.; Wang, H.; Li, Y.; Tan, W. Cell-specific aptamer probes for mem-brane protein elucidation in cancer cells. J. Proteome Res., 2008, 7(5), 2133-2139.
[98] Kunii, T.; Ogura, S.-i.; Mie, M.; Kobatake, E. Selection of DNA aptamers recognizing small cell lung cancer using living cell-SELEX. Analyst, 2011, 136(7), 1310-1312.
[99] Shangguan, D.; Meng, L.; Cao, Z.C.; Xiao, Z.; Fang, X.; Li, Y.; Cardona, D.; Witek, R.P.; Liu, C.; Tan, W. Identification of liver cancer-specific aptamers using whole live cells. Anal. Chem., 2008, 80(3), 721-728.
[100] Breaker, R.R. Natural and engineered nucleic acids as tools to explore biology. Nature, 2004, 432(7019), 838-845.
[101] Phillips, J.A.; Xu, Y.; Xia, Z.; Fan, Z.H.; Tan, W. Enrichment of cancer cells using aptamers immobilized on a microfluidic channel. Anal. Chem., 2008, 81(3), 1033-1039.
[102] Xu, Y.; Phillips, J.A.; Yan, J.; Li, Q.; Fan, Z.H.; Tan, W. Aptamer-based microfluidic device for enrichment, sorting, and detection of multiple cancer cells. Anal. Chem., 2009, 81(17), 7436-7442.
[103] Sheng, W.; Chen, T.; Tan, W.; Fan, Z.H. Multivalent DNA nano-spheres for enhanced capture of cancer cells in microfluidic de-vices. ACS Nano, 2013, 7(8), 7067-7076.
[104] Zhu, J.; Nguyen, T.; Pei, R.; Stojanovic, M.; Lin, Q. Specific cap-ture and temperature-mediated release of cells in an aptamer-based microfluidic device. Lab Chip, 2012, 12(18), 3504-3513.
[105] Wan, Y.; Mahmood, M.A.I.; Li, N.; Allen, P.B.; Kim, Y.-t.; Bachoo, R.; Ellington, A.D.; Iqbal, S.M. Nanotextured substrates with immobilized aptamers for cancer cell isolation and cytology. Cancer, 2012, 118(4), 1145-1154.
[106] Wang, Y.; Zhou, F.; Liu, X.; Yuan, L.; Li, D.; Wang, Y.; Chen, H. Aptamer-modified micro/nanostructured surfaces: efficient capture of ramos cells in serum environment. ACS Appl. Mater. Interfaces, 2013, 5(9), 3816-3823.
[107] Maria, D.C. Novel applications of RNA aptamers for enhancement of immune responses. Duke Univ., 2008, 239, 3346758.
[108] McNamara, J.O.; Kolonias, D.; Pastor, F.; Mittler, R.S.; Chen, L.P.; Giangrande, P.H.; Sullenger, B.; Gilboa, E. Multivalent 4-1BB binding aptamers costimulate CD8(+) T cells and inhibit tumor growth in mice. J. Clin. Invest., 2008, 118(1), 376-386.
[109] Pastor, F.; Soldevilla, M.M.; Villanueva, H.; Kolonias, D.; Inoges, S.; de Cerio, A.L.; Kandzia, R.; Klimyuk, V.; Gleba, Y.; Gilboa, E.; Ben-dandi, M. CD28 aptamers as powerful immune response modulators. Mol. Ther. Nucleic Acids, 2013, 2, e98, doi:10.1038/mtna.2013.26.
[110] Kanwar, J.R.; Mohan, R.R.; Kanwar, R.K.; Roy, K.; Bawa, R. Applications of aptamers in nanodelivery systems in cancer, eye and inflammatory diseases. Nanomedicine (Lond.), 2010, 5(9), 1435-1445.
[111] Bruno, J.G.; Kiel, J.L. In vitro selection of DNA aptamers to an-thrax spores with electrochemiluminescence detection. Biosens. Bioelectron., 1999, 14(5), 457-464.
[112] Lee, S.; Kim, Y.S.; Jo, M.J.; Jin, M.; Lee, D.K.; Kim, S. Chip-based detection of hepatitis C virus using RNA aptamers that spe-cifically bind to HCV core antigen. Biochem. Biophys. Res. Com-mun., 2007, 358(1), 47-52.
[113] Kleinjung, F.; Klussmann, S.; Erdmann, V.A.; Scheller, F.W.; Furste, J.P.; Bier, F.F. High-affinity RNA as a recognition element in a biosensor. Anal. Chem., 1998, 70(2), 328-331.
[114] Rupcich, N.; Nutiu, R.; Li, Y.F.; Brennan, J.D. Entrapment of fluorescent signaling DNA aptamers in sol-gel-derived silica. Anal. Chem., 2005, 77(14), 4300-4307.
[115] Xu, H.; Mao, X.; Zeng, Q.X.; Wang, S.F.; Kawde, A.N.; Liu, G.D. Aptamer-functionalized gold nanoparticles as probes in a dry-reagent strip biosensor for protein analysis. Anal. Chem., 2009, 81(2), 669-675.
[116] Huang, H.P.; Zhu, J.J. DNA aptamer-based QDs electrochemilu-minescence biosensor for the detection of thrombin. Biosens. Bioelectron., 2009, 25(4), 927-930.

Nucleic Acid-Based Aptamers Current Medicinal Chemistry, 2015, Vol. 22, No. 21 2555
[117] Tombelli, S.; Minunni, A.; Luzi, E.; Mascini, M. Aptamer-based biosensors for the detection of HIV-1 Tat protein. Bioelectrochem-istry, 2005, 67(2), 135-141.
[118] Collett, J.R.; Cho, E.J.; Ellington, A.D. Production and processing of aptamer microarrays. Methods Enzymol., 2005, 35, 4-15.
[119] Kim, Y.H.; Kim, J.P.; Han, S.J.; Sim, S.J. Aptamer biosensor for lable-free detection of human immunoglobulin E based on surface plasmon resonance. Sensor Actuat. B-Chem., 2009, 139(2), 471-475.
[120] Pieve, C.D.; Perkins, A.C.; Missailidis, S. Anti-MUC1 aptamers: radiolabelling with 99mTc and biodistribution in MCF-7 tumour-bearing mice. Nucl. Med. Biol., 2009, 36, 703-710.
[121] Cho, J.S.; Lee, S.W. Sequence and structural features of RNA aptamer against myasthenic autoantibodies. Oligonucleotides, 2009, 19(3), 273-279.
[122] Lee, S.Y.; Jeong, S. In vitro selection and characterization of TCF-1 binding RNA aptamers. Mol. Cells, 2004, 17(1), 174. [Erratum: 2005; 18(2), 269].
[123] Bagalkot, V.; Zhang, L.; Levy-Nissenbaum, E.; Jon, S.; Kantoff, P.W.; Langer, R.; Farokhzad, O.C. Quantum dot-aptamer conju-gates for synchronous cancer imaging, therapy, and sensing of drug delivery based on bi-fluorescence resonance energy transfer. Nano Lett., 2007, 7(10), 3065-3070.
[124] Zhang, C.Y.; Johnson, L.W. Single quantum-dot-based aptameric nanosensor for cocaine. Anal. Chem., 2009, 81(8), 3051-3055.
[125] Centi, S.; Sanmartin, L.B.; Tombelli, S.; Palchetti, I.; Mascini, M. Detection of C reactive protein(CRP) in serum by an electrochemi-cal aptamer-based sandwich assay. Electroanalysis, 2009, 21(11), 1309-1315.
[126] Wang, A.Z.; Bagalkot, V.; Vasilliou, C.C.; Gu, F.; Alexis, F.; Zhang, L.; Shaikh, M.; Yuet, K.; Cima, M.J.; Langer, R.; Kantoff, P.W.; Bander, N.H.; Jon, S.; Farokhzad, O.C. Superparamagnetic iron oxide nanoparticle-aptamer bioconjugates for combined pros-tate cancer imaging and therapy. Chem. Med. Chem., 2008, 3(9), 1311-1315.
[127] Li, W.; Yang, X.H.; Wang, K.M.; Tan, W.H.; He, Y.; Guo, Q.P.; Tang, H.X.; Liu, J.B. Real-time imaging of protein internalization using aptamer conjugates. Anal. Chem., 2008, 80(13), 5002-5008.
[128] Miyake, Y.; Togashi, H.; Tashiro, M.; Yamaguchi, H.; Oda, S.; Kudo, M.; Tanaka, Y.; Kondo, Y.; Sawa, R.; Fujimoto, T.; Machi-nami, T.; Ono, A. MercuryII-mediated formation of thymine-HgII-thymine base pairs in DNA duplexes. J. Am. Chem. Soc., 2006, 128(7), 2172-2173.
[129] Chiu, T.C.; Huang, C.C. Aptamer-functionalized nano-biosensors. Sensors, 2009, 9(12), 10356-10388.
[130] Kitamura, K.; Biyani, M.; Futakami, M.; Tsuji, S.U.; Suzuki, M.; Kawakubo, T.; Yamamoto, K.; Nishigaki, K. Peptide aptamer-based ELISA-like system for detection of cathepsin E in tissues and plasma. J. Mol. Biomark Diagn., 2011, 2, 1-4.
[131] Berezovski, M.V.; Lechmann, M.; Musheev, M.U.; Mak, T.W.; Krylov, S.N. Aptamer-facilitated biomarker discovery(AptaBiD). J. Am. Chem. Soc., 2008, 130(28), 9137-9143.
[132] Wang, W.; Jia, L.Y. Progress in aptamer screening methods. Chin. J. Anal. Chem., 2009, 37(3), 454-460.
[133] Ellington, A.D.S. J.W. In vitro selection of RNA molecules that bind specific ligands. Nature, 1990, 346, 818-822.
[134] Bock, L.C.; Griffin, L.C.; Latham, J.A.; Vermaas, E.H.; Toole, J.J. Selection of single-stranded-DNA molecules that bind and inhibit human thrombin. Nature, 1992, 355(6360), 564-566.
[135] William, J. Aptamers. In: Encyclopedia of Analytical Chemistry; Meyers, R.A. Ed.; John Wiley & Sons Ltd.: Chichester, 2000, pp. 4848-4871.
[136] Ellington, A.D.S. J.W. Selection in vitro of single-stranded DNA molecules that fold into specific ligand-binding structures. Nature, 1992, 355, 850-852.
[137] Jenison, R.D.; Gill, S.C.; Pardi, A.; Polisky, B. High-resolution molecular discrimination by RNA. Science, 1994, 263(5152), 1425-1429.
[138] Wang, C.; Zhang, M.; Yang, G.; Zhang, D.; Ding, H.; Wang, H.; Fan, M.; Shen, B.; Shao, N. Single-stranded DNA aptamers that bind differentiated but not parental cells: subtractive systematic evolution of ligands by exponential enrichment. J. Biotechnol., 2003, 102, 15-22.
[139] Mendonsa, S.D.; Bowser, M.T. In vitro selection of high-affinity DNA ligands for human IgE using capillary electrophoresis. Anal. Chem., 2004, 76(18), 5387-5392.
[140] Guo, K.T.; Paul, A.; Schichor, C.; Ziemer, G.; Wendel, H.P. Cell-SELEX: Novel perspectives of aptamer-based therapeutics. Int. J. Mol. Sci., 2008, 9(4), 668-678.
[141] Gevertz, J.G. H.H; Schlick, T. In vitro RNA random pools are not structurally diverse: a computational analysis. RNA, 2005, 11(6), 853-863.
[142] Carothers, J.M.; Oestreich, S.C.; Davis, J.H.; Szostak, J.W. Infor-mational complexity and functional activity of RNA structures. J. Am. Chem. Soc., 2004, 126(16), 5130-5137.
[143] Kim, N.; Gan, H.H.; Schlick, T. A computational proposal for designing structured RNA pools for in vitro selection of RNAs. RNA, 2007, 13(4), 478-492.
[144] Luo, X.M.; McKeague, M.; Pitre, S.; Dumontier, M.; Green, J.; Golshani, A.; Derosa, M.C.; Dehne, F. Computational approaches toward the design of pools for the in vitro selection of complex ap-tamers. RNA, 2010, 16(11), 2252-2262.
[145] Chushak, Y.; Stone, M.O. In silico selection of RNA aptamers. Nucleic Acids Res., 2009, 37(12), e87.
[146] Ashrafuzzaman, M.; Tseng, C.Y.; Kapty, J.; Mercer, J.R.; Tuszyn-ski, J.A. A computationally designed DNA aptamer template with specific binding to phosphatidylserine. Nucleic Acid Ther., 2013, 23(6), 418-426.
[147] Tseng, C.Y.; Ashrafuzzaman, M.; Mane, J.Y.; Kapty, J.; Mercer, J.R.; Tuszynski, J.A. Entropic fragment-based approach to aptamer design. Chem. Biol. Drug Des., 2011, 78(1), 1-13.
[148] Musumeci, D.; Bucci, E.M.; Roviello, G.N.; Sapio, R.; Valente, M.; Moccia, M.; Bianchi, M.E.; Pedone, C. DNA-based strategies for blocking HMGB1 cytokine activity: design, synthesis and pre-liminary in vitro/in vivo assays of DNA and DNA-like duplexes. Mol. BioSyst., 2011, 7(5), 1742-1752.
[149] Keefe, A.D.; Cload, S.T. SELEX with modified nucleotides. Curr. Opin. Chem. Biol., 2008, 12(4), 448-456.
[150] Bunka, D.H.; Platonova, O.; Stockley, P.G. Development of ap-tamer therapeutics. Curr. Opin. Pharmacol., 2010, 10(5), 557-562.
[151] Sampson, T. Aptamers and SELEX: the technology. World Pat. Inform., 2003, 25, 123-129.
[152] Kasahara, Y.; Kitadume, S.; Morihiro, K.; Kuwahara, M.; Ozaki, H.; Sawai, H.; Imanishi, T.; Obika, S. Effect of 3 '-end capping of aptamer with various 2 ',4 '-bridged nucleotides: Enzymatic post-modification toward a practical use of polyclonal aptamers. Bioorg. Med. Chem. Lett., 2010, 20(5), 1626-1629.
[153] Eulberg, D.; Klussmann, S. Spielgemers: Biostable aptamers. Chembiochem., 2003, 4, 979-983.
[154] Latham, J.A.; Johnson, R.; Toole, J.J. The application of a modified nucleotide in aptamer selection: novel thrombin aptamers contain-ing5-(1-pentynyl)-2’deoxyuridine. Nucleic Acid Res., 1994, 22(14), 2817-2822.
[155] Vaught, J.D.; Bock, C.; Carter, J.; Fitzwater, T.; Otis, M.; Schnei-der, D.; Rolando, J.; Waugh, S.; Wilcox, S.K.; Eaton, B.E. Expand-ing the chemistry of DNA for in vitro selection. J. Am. Chem. Soc., 2010, 132(12), 4141-4151.
[156] Burke, D.H.; Willis, J.H. Recombination, RNA evolution, and bifunctional RNA molecules isolated through Chimeric SELEX. Rna-a Publication of the Rna Society, 1998, 4(9), 1165-1175.
[157] Xu, W.C.; Lu, Y. Label-free fluorescent aptamer sensor based on regulation of malachite green fluorescence. Anal. Chem., 2010, 82(2), 574-578.
[158] Ohk, S.H.; Koo, O.K.; Sen, T.; Yamamoto, C.M.; Bhunia, A.K. Antibody-aptamer functionalized fibre-optic biosensor for specific detection of Listeria monocytogenes from food. J. Appl. Micro-biol., 2010, 109(3), 808-817.
[159] Chen, C.H.B.; Dellamaggiore, K.R.; Ouellette, C.P.; Seclano, C.D.; Lizadjohry, M.; Chernis, G.A.; Gonzales, M.; Baltasar, F.E.; Fan, A.L.; Myerowitz, R.; Neufeld, E.F. Aptamer-based endocytosis of a lysosomal enzyme. Proc. Natl. Acad. Sci. USA, 2008, 105(41), 15908-15913.
[160] Zhou, J.; Rossi, J.J. Aptamer-targeted cell-specific RNA interfer-ence. Silence, 2010, 1(1), 1-4.
[161] Kawata, E.; Ashihara, E.; Nakagawa, Y.; Kiuchi, T.; Ogura, M.; Yao, H.; Sakai, K.; Tanaka, R.; Nagao, R.; Yokota, A.; Takeuchi, M.; Kimura, S.; Hirai, H.; Maekawa, T. A combination of a DNA-

2556 Current Medicinal Chemistry, 2015, Vol. 22, No. 21 Kanwar et al.
chimera siRNA against PLK-1 and zoledronic acid suppresses the growth of malignant mesothelioma cells in vitro. Cancer Lett., 2010, 294(2), 245-253.
[162] Pastor, F.; Kolonias, D.; Giangrande, P.H.; Gilboa, E. Induction of tumour immunity by targeted inhibition of nonsense-mediated mRNA decay. Nature, 2010, 465(7295), 227-230.
[163] McNamara, J.O. 2nd; Andrechek, E.R.; Wang, Y.; Viles, K.D.; Rempel, R.E.; Gilboa, E.; Sullenger, B.A.; Giangrande, P.H. Cell type-specific delivery of siRNAs with aptamer-siRNA chimeras. Nat. Biotechnol., 2006, 24(8), 1005-1015.
[164] Shaw, B.R.; Moussa, L.; Sharaf, M.; Cheek, M.; Dobrikov, M. , Boranophosphate siRNA-aptamer chimeras for tumor-specific down regulation of cancer recpetors and modulators. Nucleic Acids Symp. Ser., 2008, 52, 655-656.
[165] Kim, E.; Jung, Y.; Choi, H.; Yang, J.; Suh, J.S.; Huh, Y.M.; Kim, K.; Haam, S. Prostate cancer cell death produced by the co-delivery of Bcl-xL shRNA and doxorubicin using an aptamer-conjugated polyplex. Biomaterials, 2010, 31(16), 4592-4599.
[166] Lebars, I.; Richard, T.; Di Primo, C.; Toulme, J.J. LNA derivatives of a kissing aptamer targeted to the trans-activating responsive RNA element of HIV-1. Blood Cell Mol. Dis., 2007, 38(3), 204-209.
[167] Zhou, J.H.; Li, H.T.; Li, S.; Zaia, J.; Rossi, J.J. Novel dual inhibi-tory function aptamer-siRNA delivery system for HIV-1 therapy. Mol. Ther., 2008, 16(8), 1481-1489.
[168] Meng, L.; Yang, L.; Zhao, X.X.; Zhang, L.; Zhu, H.Z.; Liu, C.; Tan, W.H. Targeted delivery of chemotherapy agents using a liver cancer-specific aptamer. PLoS One, 2012, 7(4), e33434. doi:10.1371/journal.pone.0033434.
[169] Held, D.M.; Kissel, J.D.; Saran, D.; Michalowski, D.; Burke, D.H. Differential susceptibility of HIV-1 reverse transcriptase to inhibi-tion by RNA aptamers in enzymatic reactions monitoring specific steps during genome replication. J. Biol. Chem., 2006, 281(35), 25712-25722.
[170] Wheeler, L.A.; Vrbanac, V.; Trifonova, R.; Brehm, M.A.; Gilboa-Geffen, A.; Tanno, S.; Greiner, D.L.; Luster, A.D.; Tager, A.M.; Lieberman, J. Durable knockdown and protection from HIV trans-mission in humanized mice treated with gel-formulated CD4 Ap-tamer-siRNA chimeras. Mol. Ther., 2013, 21(7), 1378-1389.
[171] Hussain, A.F.; Tur, M.K.; Barth, S. An aptamer-siRNA chimera silences the eukaryotic elongation factor 2 gene and induces apop-tosis in cancers expressing alphavbeta3 integrin. Nucleic Acid Ther., 2013, 23(3), 203-212.
[172] Subramanian, N.; Raghunathan, V.; Kanwar, J.R.; Kanwar, R.K.; Elchuri, S.V.; Khetan, V.; Krishnakumar, S. Target-specific deliv-ery of doxorubicin to retinoblastoma using epithelial cell adhesion molecule aptamer. Mol. Vis., 2012, 18(283-286), 2783-2795.
[173] Hu, Y.; Duan, J.H.; Zhan, Q.M.; Wang, F.D.; Lu, X.; Yang, X.D. Novel MUC1 aptamer selectively delivers cytotoxic agent to cancer cells in vitro. PLoS One, 2012, 7(2), e31970. doi:10.1371/ jour-nal.pone.0031970.
[174] Kanwar, J.R.; Kanwar, R.K.; Mahidhara, G.; Cheung, C.H.A. Can-cer targeted nanoparticles specifically induce apoptosis in cancer cells and spare normal cells. Aust. J. Chem., 2012, 65(1), 5-14.
[175] Veedu, R.N.; Wengel, J. Locked nucleic acids: promising nucleic acid analogs for therapeutic applications. Chem. Biodivers., 2010, 7(3), 536-542.
[176] Veedu, R.N.; Wengel, J. Locked nucleic acid as a novel class of therapeutic agents. RNA Biol., 2009, 6(3), 321-323.
[177] Crouzier, L.; Dubois, C.; Edwards, S.L.; Lauridsen, L.H.; Wengel, J.; Veedu, R.N. Efficient reverse transcription using locked nucleic acid nucleotides towards the evolution of nuclease resistant RNA aptamers. PLoS One, 2012, 7(4), e35990. doi:10.1371/ jour-nal.pone.0035990.
[178] Veedu, R.N.; Vester, B.; Wengel, J. Polymerase chain reaction and transcription using locked nucleic acid nucleotide triphosphates. J. Am. Chem. Soc., 2008, 130(26), 8124-8125.
[179] Veedu, R.N.; Vester, B.; Wengel, J. Enzymatic incorporation of LNA nucleotides into DNA strands. Chem. Bio. Chem., 2007, 8(5), 490-492.
[180] Hernandez, F.J.; Kalra, N.; Wengel, J.; Vester, B. Aptamers as a model for functional evaluation of LNA and 2 '-amino LNA. Bioorg. Med. Chem. Lett., 2009, 19(23), 6585-6587.
[181] Kanwar, J.R.; Kamalapuram, S.K.; Kanwar, R.K. Targeting sur-vivin in cancer: patent review. Expert Opin. Ther. Pat., 2010, 20(12), 1723-1737.
[182] Seferos, D.S.; Giljohann, D.A.; Rosi, N.L.; Mirkin, C.A. Locked nucleic acid-nanoparticle conjugates. Chem. Bio. Chem., 2007, 8(11), 1230-1232.
[183] Becker, R.C.; Chan, M.Y. REG-1, a regimen comprising RB-006, a factor IXa antagonist, and its oligonucleotide active control agent RB-007 for the potential treatment of arterial thrombosis. Curr. Opin. Mol. Ther., 2009, 11(6), 707-715.
[184] Carrasquillo, K.G.; Ricker, J.A.; Rigas, I.K.; Miller, J.W.; Gragou-das, E.S.; Adamis, A.P. Controlled delivery of the anti-VEGF ap-tamer EYE001 with poly(lactic-co-glycolic) acid microspheres. In-vest. Ophthamol. Vis. Sci., 2003, 44(1), 290-299.
[185] ClinicalTrials.gov, EYE001 to Treat Retinal Tumors in Patients With Von Hippel-Lindau Syndrome, 2008. Available from: http://clinicaltrialsgov/ ct2/show/study/NCT00056199
[186] Jo, N.; Mailhos, C.; Ju, M.; Cheung, E.; Bradley, J.; Nishijima, K.; Robinson, G.S.; Adamis, A.P.; Shima, D.T. Inhibition of platelet-derived growth factor B signaling enhances the efficacy of anti-vascular endothelial growth factor therapy in multiple models of ocular neovascularization. Am. J. Pathol., 2006, 168(6), 2036-2053.
[187] Release Owp, Ophthotech enrolls its first patient in a randomized, controlled phase II study of E10030 in macular degeneration, April 26, 2010. Available from: http://wwwophthotechcom/news
[188] Nozaki, M.; Raisler, B.J.; Sakurai, E.; Sarma, J.V.; Barnum, S.R.; Lambris, J.D.; Chen, Y.; Zhang, K.; Ambati, B.K.; Baffi, J.Z.; Am-bati, J. Drusen complement components C3a and C5a promote choroidal neovascularization. Proc. Natl. Acad Sci. USA, 2006, 103(7), 2328-2333.
[189] ClinicalTrials.gov, A Study of ARC1905(Anti-C5 aptamer) in subjects with dry age-related macular degeneration, Jan 21, 2010. Available from: http://clinicaltrials.gov/show/NCT00950638
[190] Cosmi, B. ARC-1779, a PEGylated aptamer antagonist of von Willebrand factor for potential use as an anticoagulant or anti-thrombotic agent. Curr. Opin. Mol. Ther., 2009, 11(3), 322-328.
[191] ClinicalTrials.gov, ARC1779 Injection in Patients With Von Willebrand Factor-Related Platelet Function Disorders, Jan 8, 2009. Available from: http://clinicaltrialsfeeds.org/clinical-trials/show/ NCT00632242
[192] Updates I, Baxter announces acquisition of all hemophilia-related assets of archemix and an exclusive license of its anti-TPFI ap-tamer technology, Nov 19, 2010. Available from: http://wwwgenengnewscom/industry-updates/baxter-announces-acquisition-of-all-hemophilia-related-assets-of-archemix-and-an-exclusive-licen/101236564/
[193] Wagner-Whyte J, K.S.P. J.R.; Kurz, J.C.; Olson, K.; Hatala, P.; Boomer, R.M.; Fraone, J.M.; Brosnan, N.; Makim, A. Discovery of a potent, direct thrombin inhibiting aptamer. J. Thromb. Haemost. 2007, 5, P-S-067.
[194] ClinicalTrials.gov, Study of NU172 as Anticoagulation in Patients Undergoing Off-Pump CABG Surgery(SNAP-CABG-OFF), July 6, 2009. Available from: http://clinicaltrials.gov/ct2/show/ NCT00808964
[195] Maeshima, Y.; Kashihara, N.; Yasuda, T.; Sugiyama, H.; Seki-kawa, T.; Okamoto, K.; Kanao, K.; Watanabe, Y.; Kanwar, Y.S.; Makino, H. Inhibition of mesangial cell proliferation by E2F decoy oligodeoxynucleotide in vitro and in vivo. J. Clin. Invest., 1998, 101(11), 2589-2597.
[196] Inc, C. From Edifoligide(E2F Decoy) Phase 3 Trial For Peripheral Bypass Graft, Dec 7, 2004. Available from: http://wwwmedicalnewstodaycom/ articles/17439php
[197] Laber, D.A.T. B.S.; Kloecker, G.H.; Bates, P.J.; Trent, J.O.; Miller, D.M. Extended phase I study of AS1411 in renal and non-small cell lung cancers. J. Clin. Oncol., 2006, 24(18), 13098.
[198] Stuart, R.K.; Stockerl-Goldstein, K.; Cooper, M.; Devetten, M.; Herzig, R.; Medeiros, B.; Schiller, G.; Wei, A.; Acton, G.; Rizzieri, D. Randomized phase II trial of the nucleolin targeting aptamer AS1411 combined with high-dose cytarabine in relapsed/refractory acute myeloid leukemia(AML). J. Clin. Oncol., 2009, 2(15)(suppl; abstr 7019).
[199] Tanioka, M.; Nokihara, H.; Yamamoto, N.; Yamada, Y.; Yamada, K.; Goto, Y.; Fujimoto, T.; Sekiguchi, R.; Uenaka, K.; Callies, S.;

Nucleic Acid-Based Aptamers Current Medicinal Chemistry, 2015, Vol. 22, No. 21 2557
Tamura, T. Phase I study of LY2181308, an antisense oligonucleo-tide against survivin, in patients with advanced solid tumors. Cancer Chemoth. Pharm., 2011, 68(2), 505-511.
[200] UK, C. A trial of LY2181308 alongside chemotherapy for non small cell lung cancer, 2010. Available from: http://wwwcancerhelporguk/trials/a-trial-of-ly2181308-alongside-chemotherapy-for-non-small-cell-lung-cancer
[201] ClinicalTrials.gov, NOX-E36 in Patients With Type 2 Diabetes Mellitus and Albuminuria, 2012. Available from: http://clinicaltrialsfeeds.org/clinical-trials/show/NCT01547897
[202] Purschke, W.J. F.; Eulderg, D.; Klussmann, S.; Buchner, K.; Maasch, C.; Dinse, N. SDF-1 Binding nucleic acids and the use thereof. United States Patent Application 20110223127, Sep 15, 2011.
Received: ???????????????? Revised: ???????????????? Accepted: ????????????????








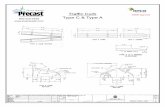


![Campbell, Richard L. - Efficient Viscous Design of Aircraft Config - Aiaa-98-2539 [NASA]](https://static.fdocuments.in/doc/165x107/577d38b91a28ab3a6b985d4d/campbell-richard-l-efficient-viscous-design-of-aircraft-config-aiaa-98-2539.jpg)






