Critical Transitions in Intensive Care Units: A Sepsis ...
Transcript of Critical Transitions in Intensive Care Units: A Sepsis ...

Critical Transitions in Intensive Care Units: A SepsisCase StudyPejman F. Ghalati1,+, Satya S. Samal1,3,+, Jayesh S. Bhat1, Robert Deisz2, Gernot Marx2,and Andreas Schuppert1,*
1Joint Research Center for Computational Biomedicine, RWTH Aachen University, 52074 Aachen, Germany2Klinik fur Operative Intensivmedizin und Intermediate Care, Universitatsklinikum Aachen, 52074 Aachen, Germany3Currently at: BASF SE, Carl-Bosch-Strasse 38, 67056 Ludwigshafen am Rhein, Germany*[email protected]+these authors contributed equally to this work
ABSTRACT
Progression of complex human diseases is associated with transitions across dynamical regimes. These transitions are oftenphase transitions that generate early-warning signs and provide insights into the underlying disease-driving mechanism(s). Inthis paper, we propose a computational method to discover indicators of such transitions in a multivariate time series dataset ofcritical care patients (MIMIC-III database). Our main motivation is to model the dataset mathematically and to quantify thedeterioration of the model’s forecast performance relative to its past performance. Our data-sampling strategy around putativetime-points of critical transitions offer early differentiation capability between septic shock and non-sepsis patients.
1 Introduction
Certain biological systems exhibit nonlinear dynamics that undergo sudden regime shifts at tipping points35, 38 or they presentphase transitions20. In medical context, these critical transitions often indicate changes in clinical phenotypes, e.g., disease-onset45. Such phenomena were studied mathematically with techniques from singularity theory of dynamical systems2, 44, 48. Inaddition, data-driven methods model the dynamics of the system approaching transitions via statistical indicators known asearly-warning signals7, 9, 10, 13, 14, 19, 31, 39. In systems medicine, modelling of such transitions is important in several applications:monitoring health29, predicting disease-onset as well as gaining a better understanding of the underlying disease progression23, 33.
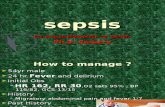
Sepsis is a common complication in the Intensive Care Unit (ICU) and this paper showcases a concept of regime shifts inseptic dynamics. As stated in the third international consensus definitions of sepsis and septic shock (Sepsis-3): “sepsis is alife-threatening organ dysfunction caused by a dysregulated host response to infection” and “septic shock is a subset of sepsisin which underlying circulatory and cellular/metabolic abnormalities are profound enough to substantially increase mortality40.”Worldwide, it is attributed with one of the highest in-hospital mortality. For instance, with 75000+ annual deaths, it has becomeone of the main causes of death in Germany. Despite advances in clinical treatment, it costs billions in the healthcare sector(In 2012, 8.2 billion Euros in German hospitals) due to rising incidence rate and prolonged hospital stay5, 15. Aggressive andearly administration of antibiotics is a crucial step in the treatment and delays significantly increase mortality16. Every hourdelay in the diagnosis of septic shock decreases survival chance by 7.6%30. However, diagnosis remains a challenging task forphysicians due to heterogeneity of infectious agents and multiple comorbidities.
With the availability of large longitudinal observational data, it is now possible to develop automatic screening tools thatcould reduce recognition delays and improve accuracy as compared to manual screening5. These emerging methods are expectedto support physicians in various use-cases: to diagnose infection; to stratify risk; to detect sepsis and quantify its severity; todifferentiate bacterial from viral or fungal infection, as well as systemic sepsis from local infection. These modern methodscould supplement traditional laboratory markers (e.g., WBC, CRp, PCT, Neutrophils count) that clinicians routinely use todiagnose infection and mitigate some of their shortcomings: delayed test results due to transport and processing time; sparseavailability; expensive sampling; unspecific to discriminate infection from inflammation induced by operation/trauma/burn.
To detect and recognise sepsis early, numerous illness severity scores or early-warning signals exist: Acute Physiologyand Chronic Health Evaluation (APACHE II); Simplified Acute Physiology Score (SAPS II); Sepsis-related Organ FailureAssessment Score (SOFA); Modified Early Warning Score (MEWS); Simple Clinical Score22. In general, these scores are goodpredictors of disease severity and mortality but cannot estimate the risk of developing sepsis with reasonable sensitivity andspecificity22. To improve accuracy, innovative computational methods were hence developed and several studies investigatedtheir performance in the early detection of sepsis and septic shock.
1
arX
iv:1
902.
0576
4v1
[q-
bio.
QM
] 1
5 Fe
b 20
19

The studies employed machine learning (ML) methods, such as multivariate logistic regression, support vector machine,and principal component analysis, to predict sepsis onset8, 34, 43. Rothman et al.37 used structured information from electronichealth records (EHR) to identify sepsis on admission or to predict its onset during hospitalisation. For septic shock prediction,Ghosh et al.17 proposed an integrative model combining sequential contrast patterns with coupled hidden Markov models.Henry et al.22 developed a targeted real-time early-warning score by training a Cox regression model to identify patients at highrisk of developing septic shock. Additionally, Horng et al.27 argued that combining free-text patient data with other predictorfeatures improve the performance of ML models significantly.
This study hypothesises that a ”surrogate-biomarker”, continuously and automatically calculated from continuous patient-monitoring data, can function as a real-time sepsis diagnostic tool that supports clinical decision-making. Ideally, it shouldwarn hours before the onset of sepsis, thereby supporting timely therapy. It could accompany the development of a ”watchdogalgorithm” that helps to improve diagnostic speed or accuracy of sepsis detection.
In this paper, we propose a computational method to identify and characterise signals indicative of regime shifts inmultivariate time series data. Based on a forecast breakdown scheme with surprise loss (SL), these signals identify onset ofinstability in complex systems18. The SL concept determines potential or putative tipping-points in time series, i.e., criticaltransitions, by computing forecast error of a mathematical model. The performance of the forecast is measured for a fixed lossfunction in a moving time-window manner. Clements et al.12 discussed the SL concept as forecast failure in econometric dataand also provided a taxonomy of possible sources of such failures11.
We performed retrospective analysis by computing the SL and its moving average for each patient in an unsupervisedmanner. In septic shock patients, prior to clinically annotated disease-onset, moving average of SL intensified, suggesting itsrole as an early-warning indicator to detect putative regions of regime shifts. Additionally, statistical hypothesis tests, conductedat regions of relatively higher values of average SL, revealed significant differences in variable values in our septic shock patientcohort compared to similar regions in the non-sepsis cohort. Therefore, our proposed approach envisages a novel biomarkerand an unsupervised data-sampling strategy.
2 Materials and methods
2.1 Data sourceWe sourced patients’ EHR from the publicly available MIMIC-III database v1.428, which contained longitudinal data of 46,520de-identified patients from 58,976 distinct ICU admissions. For ease of interpretation, we considered these admissions asdistinct patients.
In the ICU, clinical staff make swift decisions or take prompt actions during patient management. They prioritise timelyand correct treatment over consistent documentation about their processes, thereby limiting the reliability of clinical annotationfor retrospective analysis. Furthermore, the execution of guidelines for identifying imminent disease varies across hospitals.Hence, we restricted our data analysis to predominantly machine-recorded quantitative variables.
Decision rules for retrospective annotation of the sepsis syndrome have evolved over the decades as knowledge of itspathophysiology and epidemiological impact increased1. Whereas earlier definitions (19916, 200132) focused on uncontrolledsystemic inflammation as the major indicator, the latest 201640 definition, popularised as Sepsis-3, emphasised organ dysfunctionas the leading effect of the sepsis syndrome and proposed to update the ICD coding system36, 41 (ICD-9: 995.92, 785.52;ICD-10: R65.20, R65.21). SOFA scoring system graded the extent of organ dysfunction and calculated every 24 hours duringICU stay46, 47.
Because ICD-9 codes in our data were not compatible with Sepsis-3, we annotated the patients in accordance with Table 2from the 2016 consensus definition40. Figure 1 illustrates a general schematic of our annotation framework.
The annotation framework was applied to all 58,976 patients, which resulted in 22,547 (38.2%) sepsis patients and 3208(5.4%) septic shock patients. Out of the 3208 patients, we analysed only adults (18+ years old at admission) with at least36-hours stay and at most 144-hours preceding onset, which generated a cohort of 630 patients. Our non-sepsis cohortcomprised of 6,236 patients, who lacked Sepsis-3 annotation or sepsis-specific ICD-9 codes and who stayed between 36 to 144hours in the ICU. As a result, in both cohorts T ∈ [36, ...144] (Sect. 2.2). Table 1 shows the demographic information of thetwo cohorts.
Based on availability and relevance to sepsis, we preselected groups of variables: laboratory variables included bicarbonate,creatinine, blood urea nitrogen (BUN), haematocrit, haemoglobin, platelet count, white blood cell count (WBC), potassium, andsodium; vital signs and physiological variables comprised of body temperature, heart rate, respiratory rate, oxygen saturation(spO2), arterial blood pressure (systolic, mean, diastolic), and urine output; two septic markers contained shock index (ratio ofheart rate over systolic blood pressure), and BUN to creatinine ratio22. Table 2 shows the mean sampling rate of the variables inthe respective patient cohorts, and their distribution can be seen in Figure A2.
2/16

ICU exit
24 hours 24 hours 24 hours
ICU admit
Body fluid culture sampling (BFCS)
Antibiotics administration (AA)
Onset
t
SOFA >= 2
Lactate > 2 and
MAP < 65 and
Vasopressor
Sepsis
yes
no Go to next
infection suspicion
Septic Shock
yes
no
1st AA 3rd AA 2nd AA
Assess Sepsis-3 Criteria
Sepsis-3 Criteria
Figure 1. Over the length of a patient’s ICU stay, all timestamps of body fluids (blood, urine, spinal) sampling and antibioticsadministration were retrieved. For each of the timestamps, an infection was suspected if antibiotics were administered within72 hours of any prior body fluids sampling (irrespective of culture finding), or if any body fluids were sampled within 24 hoursof prior antibiotics administration. Sepsis-3 criteria were independently evaluated over time-windows around theinfection-suspected timestamps (IST). Each time-window began 48-hours prior to IST until 24-hours post IST. If the criteriawere satisfied over a time window, then the beginning of the window was annotated as onset time. In the schematic, the 2nd
antibiotics event falls within 72 hours of previous body fluid sampling and thus an infection suspected.
Septic shock Non-sepsisNumber Age Number Age
Male 380 65 ± 15 3536 61 ± 16Female 250 66 ± 15 2700 63 ± 19Total 630 65 ± 15 6236 62 ± 17
Table 1. Demographic data of the septic shock and non-sepsis cohorts
2.1.1 Missing value imputation and time binningData representation is a crucial step in analysing time series. Continuous EHR suffer from missing values due to insufficientdata collection and lack of documentation. Additionally, high heterogeneity in variable type and irregular sampling intervalsmake handling such data difficult. To tackle the missing data problem and data sparsity, we standardised and regularisedour time series into 30-minute time bins by imputing values at the bins with univariate Stineman interpolation and averagingmeasurement values over the bins42.
2.2 State space modelUsing state space model (SSM) approach3, 21, we model the multivariate time series in a hierarchical manner: the biologicalprocesses are represented by hidden states, and the clinical variables (observables) are weighted linear combinations of thehidden states. Different sources of variability, such as biological and measurement stochasticities, are represented. SSM isalso popular in structural time series analysis, where a given time series is decomposed into trend, seasonal, and irregularcomponents21. Moreover, dynamic factor analysis can use the SSM-derived trend component26, 49. We assume that thebiological processes, represented by hidden states, i.e., trends, are disease states and we formulate our SSM model in (1).
xt = xt−1 +wt where wt ∼ MV N(0,Q), x0 ∼MV N(π,∧)yt = Zxt +a+ vt where vt ∼ MV N(0,R)
(1)
where the indices of the time series are from t = 1, . . . ,T ; e is the number of hidden trends; x is an e×T matrix of hiddenstates; y is a n×T matrix of n observables; w is an e×T matrix of process error. The process error at time t is multivariate
3/16

Variable Sampling Rate per DaySeptic Non-Sepsis
BUN 1.7 1.1Creatinine 1.7 2.6
Haemoglobin 1.9 5.0Bicarbonate 1.7 1.5
Respiratory Rate 20.5 4.4Heart Rate 20.2 9.8
Haematocrit 2.2 8.2WBC 1.5 9.2SpO2 20.1 8.1
Platelets 1.6 5.3Systolic BP 19.8 9.3
Urine Output 12.1 10.2Temperature 6.7 9.1
Sodium 2.0 3.2Diastolic BP 19.8 10.4
Mean BP 20.0 6.6Potassium 2.5 3.8
Table 2. Mean sampling rate of the preselected clinical variables in septic shock and non-sepsis cohorts. For a single patient,the sampling rate was the ratio between the number of observations recorded in the ICU and the length of stay (in days). Therate was then averaged over all the patients in the respective cohorts.
normal (MVN), with mean 0 and e× e covariance matrix Q; y is a n×T matrix of the observables; v is a n×T matrix ofobservation error. The observation error at time t is multivariate normal, with mean 0 and n× n covariance matrix R; Z isn×m parameter matrix; a is a vector of offsets; π is a matrix of e× 1 means; ∧ is an e× e covariance matrix. The set ofparameters can be represented in compact form as θ = (Q,R,Z,x1,...,T ,π,∧) and their estimate θ . yt and yt+λ are the estimateand λ -step-ahead forecast of the given observables, yt , respectively.
Our implementation incorporated MARSS R-package25, 26, along with its recommended initial conditions that ensureparameter identifiability.
2.3 Perturbations in the dynamics2.3.1 Early-warning indicatorPatients in ICUs undergo several perturbations due to medical interventions or disease progression, which result in non-constancy of the underlying biological mechanisms and changes in the dynamical regimes. Therefore, our SSM model is notexpected to have constant parameters and is likely to be misspecified with respect to the highly complex disease mechanism.Clements et al.11 discussed a taxonomy of possible sources of uncertainties. Consequently, our proposed computationalmethod is based on surprise loss (SL)18, which determine points in the time series where forecast error, i.e., out-sampleerror, of the SSM model is worse than its in-sample performance. The performance is measured for a fixed loss function in amoving time-window manner. SL computation is unsupervised, i.e, class labels, such as septic shock or non-sepsis, are notrequired. Despite inaccurate model-fit (or forecast), SL quantifies the deterioration of the forecast performance relative to itspast performance. Therefore, a relatively high positive value of SL is likely to indicate transitions across dynamical regimes.
With a moving time-window width m, the SSM model (1) was fitted for time indices t −m+ 1, . . . , t. yict denotes the
observables of a given patient i with c clinical condition at time index t. The in-sample error is a quadratic loss functionthat averages the squared differences between the estimated and the given observables, and it is denoted as L j(θ
ict ) =
1n ∑
nk=1(y(k)
icj − y(k)ic
j )2 where y(k)ic
j is the kth element of column vector yicj . Similarly, the out-sample error is a quadratic loss
function that averages the squared differences between the λ -step-ahead forecast and the given observables, and it is denoted asLt+λ (θ
ict ) = 1
n ∑nk=1(y(k)
ict+λ− y(k)ic
t+λ)2. The SL is then the difference between the out-sample and the in-sample error (2).
SLict+λ
= Lt+λ (θict )− 1
m
t
∑j=t−m+1
L j(θict ) for t = m, . . . ,T ic −λ (2)
To remove short-terms fluctuations, a moving-average filter smoothens the SL (3).
4/16

Wilcoxon rank sum test
y1
y2
y3
yn
SLMean
m
t Ttmax
Non-sepsis patient
y1
y2
y3
yn
SLMean
m
t TtmaxSeptic shock patient
Figure 2. A schematic diagram illustrating our data-sampling strategy using SLMean. Observables at high magnitudeSLMean values were selected from septic shock and non-sepsis patients. Wilcoxon rank-sum test determined statistical
significance of the change among the observables.
SLMeanict =
t
∑j=t−(m+δ )+1
SLicj
jfor t = m+δ , . . . ,T ic (3)
Prior to clinically annotated onset of disease c, for a given patient i, a relatively high SLMeanict suggest putative transitions
across dynamical regimes and serves as an early-warning indicator. The maximum of SLMeanic occurs at time-index t icmax. A
simulated example using synthetic data is shown in Figure 4.
2.3.2 Uncertainty in SLMeanUncertainty in out-sample forecast and in-sample performance disperses the precise location of t ic
max. Let t icmax(up) and t ic
max(low)be the time indices corresponding to the mode of upper and lower bounds of 95% prediction interval of SLMean, respectively.Our approach is considered robust if the deviations of tmax from t ic
max(up) and t icmax(low) are close to zero.
2.4 Statistical hypothesis testsGiacomini et al.18 introduced the SL concept to assess reliability of a forecast model . However, we restrict the use of SL todetermine regions of interest that are indicative of transitions across dynamical regimes (Figure 4). In the clinical context, wedemonstrate that observables at such regions, i.e., high magnitude SLMean, have disease-specific signature as compared torandom selection of observables at random regions. Between two distinct clinical conditions, septic shock and non-sepsis,Wilcoxon rank-sum test24 compared observables at these regions and identified variables that underwent significant change(Figure 2). A bootstrap test assessed our data-sampling strategy and established superiority of our approach. (Sect. 2.5).
The Wilcoxon rank-sum test, i.e., a statistical significance test, examined the extent of difference for the observations yictmax
between septic shock and non-sepsis patients. tmax closer to disease-onset was selected if multiple high values existed. Wedefine a n× v variable matrix Sc = [y1c
tmax , . . . ,yictmax ] where i ≤ v. We considered c ∈ {0,1} i.e., exactly two distinct clinical
conditions, non-sepsis and septic shock, in the determination of disease-specific signature. For each variable, over the patients,the list of p-values is formulated in (4).
p =(
pval(S01,S
11), . . . , pval(S0
n,S1n))
(4)
5/16

where pval(.) returns p-value for the null hypothesis that two distributions do not differ by location shift. In the alternativehypothesis, they differ by some location shift. Benjamini and Hochberg correction method adjusted the p-values4. S0
j and S1j
denote the jth row vectors of S0 and S1 matrices, respectively. Figure 3 illustrates the calculation of SLic , SLMeanic and t icmax.
2.5 BootstrappingA bootstrap test discriminated the tmax p-values (4) from p-values that were obtained from random points in our time series. Fora randomly selected time-index t with its corresponding observation yic
t , where t ∈ (1,T ic), the trandom p-values were calculatedby replacing tmax with t. The test was repeated 1000 times. Bootstrap frequency (BF) denotes the fraction of times whereintmax p-values were less than trandom p-values. In addition, we tested the changes in the BF by randomly sampling points fromspecific regions in the time series of septic shock patients. Specifically, we computed BF on data sampled on all times as wellas 36h and 18h before the onset of septic shock.
2.6 Data normalisationOur observables had different scales and measurement units. Data normalisation is thus needed to facilitate comparison ofSL among variables, and to prevent ill-conditioned SL prior to the calculation of SLMeanic . Z-score normalisation, a hardrequirement of the MARSS package25, transformed the observables to a specific range. Before in-sample normalization, thewhole sequence values were also z-score transformed to address different measurement units.
y1
y2
y3
yn
SL
SLMean
m
!Moving Window(SL Calculation)
Moving Window(Mean of SL)
t Ttmax = Time index at max(SLMean)
Statistical Hypothesis TestsEWI(Early Warning Indicator)
Figure 3. A Schematic for calculation of SL, SLMeanic , and tmax. With a moving time-window of length m, the SSM model,which was fit over the illustrative blue area, calculated SL of subsequent time point. Another sliding window of length δ ,
illustrative green area, computed SLMean. Whereas T denotes disease-onset in septic shock patients, it is discharge/deceasetime in non-sepsis patients. tmax is the time index where SLMean maximises, and it was used in our sampling approach for the
statistical significance test.
6/16

0 50 100 150
45
67
89
1011
Points
Var
iabl
e of
inte
rest
(a) Synthetic Data
0 50 100 1500
5010
015
0
Points
Sur
pris
e Lo
ss
(b) SL
0 50 100 150
05
1015
Points
Sur
pris
e Lo
ss M
ean
(c) SLMean
Figure 4. SLMean simulated using synthetic data that was generated by concatenating 50 points, drawn independently fromthree univariate normal distributions with different means (5, 10, 15) but same standard deviation (0.5). Computed with a
moving time-window of length 30 and number of trends set to 1, the magnitude of SL intensified at the 50th and 100th
time-points, where the parameters of the data generating process changed, i.e., a proxy for transitions across differentdynamical regimes.
2.7 SoftwareTo support reproducible research, our computational method is available at https://github.com/JRC-COMBINE/SL-MTS.
3 Results
3.1 SLMean as an early-warning indicatorOver a moving time-window (m = 36, i.e., 18 hours; e = 3; λ -step-ahead = 1, i.e., 30 minutes; δ = 6, i.e., 3 hours), the fittedSSM (Sect. 2.3) computed SL and SLMean for each patient. Fig. 5a shows median of SLMeanic
t for all septic shock patients (c= 1 in Sect. 2.4). As the moving time-window approached disease-onset, the median intensified. The largest SLMeanic
t need notnecessarily occur exactly at the time of disease-onset. A positive SLMeanic
t indicates a higher out-sample error than in-sampleerror, signalling putative transitions in the underlying dynamics.
3.2 Data samplingFor septic-shock patients, the location of time index tmax from the onset time (T ) is shown in Figure 5b. We compared thep-values for data sampled at tmax to those obtained via random sampling ((4) and Sect. 2.5). In addition to 36h and 18h beforethe onset of septic shock T , the bootstrap test was performed for all time-indices and the bootstrap frequencies were denoted asBF (Full), BF (36 hours) and BF (18 hours), respectively. The different BF computations tests the association of BF (Full)value in some variables to high SLMean. Figure 6a plots BF (Full) against p-values computed at trandom and at high SLMean(i.e., tmax). Figure 6b plots BF (Full), BF (36 hours), and BF (18 hours) of all the variables. P-values and the correspondingbootstrap test values of all variables are shown in appendix Table A1. Our uncertainty in SL calculation (Sect. 2.3.2) hadnegligible deviation in tmax (median of deviation = 0, IQR = 5.4 hours).
3.3 Method robustnessWe assessed the robustness of our method to perturbations in the model parameters. We changed the moving time-windowlength, m ∈ (24,30), and the number of trends in the SSM model (e ∈ (4,5)) and compared the changes in the tmax with respectto the reference setting i.e., m = 36 and e = 3. Figure A1, in the appendix, summarises the differences in tmax due to theperturbations. Zero median of such differences confirmed the robustness of our approach. The outliers in Figure A1 were dueto multiple similarly valued high SLMean, thereby rendering tmax sensitive to the parameter perturbations.
7/16

−120 −100 −80 −60 −40 −20 0
0.05
0.10
0.15
0.20
0.25
0.30
Time (t−T) [hours]
Med
ian
of S
LMea
ni c
(a)
tmax−T
Se
ptic P
atie
nts
[%
]
−120 −100 −80 −60 −40 −20 0
05
10
15
20
(b)
Figure 5. a) Median of SLMeanic for all septic shock patients (c = 1 in Sect.2.4) prior to disease-onset; T is the length of timeseries and t−T is the time before onset of septic shock. Number of samples per time-point was different due to heterogeneouslength of stay (Sect. 2.1). As the maximum length of stay was 144 hours, with a moving time-window length of 18 hours andan average window of 3 hours, the minimum of t−T was -123 hours. b) Distribution of tmax−T in septic patients. SLMean
maximises at tmax.
4 DiscussionsUtilisation of continuously monitored health data provides great promise to health care, driven by the massively increasingavailability of long time series of health data collected either by wearables or by monitoring systems such as those establishedin the ICU. The unprecedented sampling rates across long time spans give rise to the hope for new paradigms in individualhealth surveillance, clinical trial design, and preventive care. However, significant challenges remain unresolved. A majordrawback is the restriction of data availability to variables that are easy to collect by non-invasive sensors. They provide onlycorrelated surrogates of the primary disease-driving processes. Hence, sensor signals are rarely specific on their own but requireadvanced computational processing to unravel relevant signals, thereby enabling improved therapies.
Focusing data analysis on the prediction and identification of critical states, i.e., tipping points that switch phenotypes amongstable states, may complement established scoring methods in the classification of stable states. Although tipping-points-specificpatterns differ qualitatively with the scores in classifying stable states, they provide an independent assessment of the healthstatus. Because it is sufficient to identify the evolution of individual longitudinal time series, compared to established scoresbased on absolute variable values, markers for detection of critical states are relatively robust to normalisation and datastandardisation issues.
This study applied the surprise loss concept, a critical state detection marker developed for economic time series analysis,to ICU patient monitoring. Despite its inherent sensitivity to random fluctuations in the data and to signals triggered by amultitude of interventions in the ICU, our moving time-window SL-based averaging method demonstrates a monotonicallyincreasing signal that begins around 24h before the onset of septic shock (Figure 5a). The observed median monotonic increaseunderlines the expectation that SL, an example for tipping-point related biomarker, may provide a strategy for personalisedprediction of patient fate and an early-warning indicator for the onset of the septic shock. In majority of our patients’ data,the highest SLMean occurred near septic shock onset (In 60% of the patients, the signal occurred less than 48 hours prior toonset as in Figure 5b). However, in some patients, the signal was observed beyond onset time. An explanation could be lack ofrecords or low sampling rate of variables few days before the onset of septic shock, which results in insignificant SLMean. Thehighest SLMean, on average, occurred 46 hours prior to the appearance of septic shock symptoms.
Our study also provided an efficient data-sampling strategy to discriminate non-sepsis from septic shock patients throughsurprise loss. Figure 6a demonstrates the discrimination capability through the bootstrap frequency (BF) (Sect. 2.4). Fora majority of variables, a high BF(Full) was achieved, improving sensitivity to differentiate septic shock from non-sepsis.Moreover, from a systems theory point of view, mechanisms that control the system in homeostasis begin to collapse around atipping point. Consequently, variables under tight control within stable states may be more sensitive to systemic variability
8/16

0.1
0.2
0.3
5
0.4
2
0.7
5
0.7
5
0.7
5
0.8
2
0.8
5
0.8
6
0.9
1
0.9
4
0.9
7
0.9
8
0.9
9
0.9
9
0.9
9 1 1
−Log10 p−values at highest SLMean
Median of −log10 p−values of random points
Bootstrap Frequency (Full)
−lo
g1
0 p
−va
lue
s
0
20
40
60
80
100
Bic
arb
onate
Uri
ne O
utp
ut
Pla
tele
ts
Sodiu
m Respirato
ry R
ate
Heart
Rate
WB
C
Pota
ssiu
m
Dia
sto
lic B
P
Hem
oglo
bin
SpO
2
Cre
atinin
e
Mean B
P
BU
N
Hem
ato
cri
t
Shock Index
Tem
pera
ture
BU
N−
Cre
atinin
e
Systo
lic B
P
(a)
Bic
arb
onate
Uri
ne O
utp
ut
Pla
tele
ts
Sodiu
m
WB
C
Dia
sto
lic B
P
Hem
oglo
bin
SpO
2
Cre
atinin
e
BU
N
Respirato
ry R
ate
Heart
Rate
Pota
ssiu
m
Mean B
P
Hem
ato
cri
t
Shock Index
Tem
pera
ture
BU
N−
Cre
atinin
e
Systo
lic B
P
BF (Full)
BF (36 hours)
BF (18 hours)
BF
valu
e
0.0
0.2
0.4
0.6
0.8
1.0
(b)
Figure 6. a) A statistical significance test (see Sect. 2.4) was performed to test whether the values of the clinical variables atlargest SLMean were able to differentiate septic shock patients from non-sepsis. −log10(P− value) of each variable at tmaxwere compared with the median −log10(P− value) of randomly selected points from the whole sequence. A bootstrap test
(denoted as BF Full) was performed to quantify the number of times the p-values at tmax is lower to those at trandom. b) Anotherbootstrap test, performed via randomly sampling points at 18-hour and 36-hour windows prior to the onset of septic shock,
tested whether low p-values at tmax is an effect of time or a characteristic of regions with high SLMean.
around an unstable point. Our data analysis supports this hypothesis (Figure 6a): some variables under tight control, e.g., bloodpressure and body temperature, showed significant improvement in p-values compared to random sampling.
However, merely sampling data close to onset-time of septic shock can result in better separability from non-sepsis andthe high SLMean are not necessarily located close to the onset time (Figure 5b). In order to test it, BF (Full) was modified toselectively sample random data from 36 hours and 18 hours before the onset of sepsis and represented them as BF (36 hours)and BF (18 hours), respectively (Table A1). As the random sampling strategy changed, either to 36 or 18 hours in Figure 6b,BF reduced for six variables (WBC to BUN), but it was preserved for nine variables (respiratory rate to systolic blood pressure),i.e., the differences were small among BF (Full), BF (36 hours), and BF (18 hours). Four variables, bicarbonate till sodium,had low BF (Full), BF (36 hours), and BF (18 hours).
SL can hence inform about the robustness of system’s homeostasis, which can be used for optimised data sampling strategies.Compared to routine data-sampling, an SL-biased sampling strategy may improve the quality of patient classification, evenwith reduced samples.
Conceptually, SL is calculated based on the premise that the underlying system has a stable stationary state and all observeddeviations can be explained by its stochastic perturbations. In that sense, the SL quantifies the homeostasis of the system aroundthe steady state. Hence, the model should be based on observable data that are involved in the control of the respective state.The model, in our study, was trained on data with high relevance to the progression of sepsis (Table A1). The SL calculatedfrom these data alone cannot analyse the development of any arbitrary critical syndrome but syndrome-specific analysis shouldbe undertaken. In future applications, machine learning technologies may significantly support the selection of respectiveoptimal models.
9/16

References1. Edward Abraham. New definitions for sepsis and septic shock: continuing evolution but with much still to be done. Jama,
315(8):757–759, 2016.
2. Vladimir I. Arnold. Singularities, Bifurcations, and Catastrophes. In Catastrophe Theory, pages 1–2. Springer BerlinHeidelberg, Berlin, Heidelberg, 1992.
3. Marie Auger-Methe, Chris Field, Christoffer M. Albertsen, Andrew E. Derocher, Mark a. Lewis, Ian D. Jonsen, and JoannaMills Flemming. State-space models’ dirty little secrets: even simple linear Gaussian models can have estimation problems.Scientific Reports, 6(May):26677, 2016.
4. Yoav Benjamini and Yosef Hochberg. Controlling the False Discovery Rate: A Practical and Powerful Approach toMultiple Testing. Journal of the Royal Statistical Society. Series B (Methodological), 57(1):289–300, 1995.
5. Poushali Bhattacharjee, Dana P. Edelson, and Matthew M. Churpek. Identifying Patients With Sepsis on the HospitalWards. Chest, 151(4):898–907, April 2017.
6. Roger C. Bone, Robert A. Balk, Frank B. Cerra, R. Phillip Dellinger, Alan M. Fein, William A. Knaus, Roland MH Schein,and William J. Sibbald. Definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis.Chest, 101(6):1644–1655, 1992.
7. S. R. Carpenter and W. A. Brock. Rising variance: a leading indicator of ecological transition: Variance and ecologicaltransition. Ecology Letters, 9(3):311–318, March 2006.
8. M. Carrara, G. Baselli, and M. Ferrario. Mortality prediction in septic shock patients: Towards new personalized models incritical care. pages 2792–2795. IEEE, August 2015.
9. Luonan Chen, Rui Liu, Zhi-Ping Liu, Meiyi Li, and Kazuyuki Aihara. Detecting early-warning signals for suddendeterioration of complex diseases by dynamical network biomarkers. Scientific reports, 2:342, 2012.
10. Pei Chen, Rui Liu, Yongjun Li, and Luonan Chen. Detecting critical state before phase transition of complex biologicalsystems by hidden Markov model. Bioinformatics, 32(14):2143–2150, July 2016.
11. Michael Clements and David Hendry. Forecasting economic time series. Cambridge University Press, 1998.
12. Michael P Clements and David F Hendry. Modelling methodology and forecast failure. The Econometrics Journal,5(2):319–344, 2002.
13. V. Dakos, M. Scheffer, E. H. van Nes, V. Brovkin, V. Petoukhov, and H. Held. Slowing down as an early warning signal forabrupt climate change. Proceedings of the National Academy of Sciences, 105(38):14308–14312, September 2008.
14. Vasilis Dakos, Egbert H. van Nes, Raul Donangelo, Hugo Fort, and Marten Scheffer. Spatial correlation as leading indicatorof catastrophic shifts. Theoretical Ecology, 3(3):163–174, August 2010.
15. C Fleischmann, M Hartmann, Cs Hartog, T Welte, S Heublein, D Thomas-Rueddel, U Dennler, and K Reinhart. Epi-demiology of sepsis in germany: Incidence, mortality and associated costs of care 2007-2013. Intensive Care MedicineExperimental, 3(Suppl 1):A50, 2015.
16. David F. Gaieski, Mark E. Mikkelsen, Roger A. Band, Jesse M. Pines, Richard Massone, Frances F. Furia, Frances S.Shofer, and Munish Goyal. Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whomearly goal-directed therapy was initiated in the emergency department*:. Critical Care Medicine, 38(4):1045–1053, April2010.
17. Shameek Ghosh, Jinyan Li, Longbing Cao, and Kotagiri Ramamohanarao. Septic shock prediction for ICU patients viacoupled HMM walking on sequential contrast patterns. Journal of Biomedical Informatics, 66:19–31, February 2017.
18. Raffaellea Giacomini and Barbara Rossi. Detecting and predicting forecast breakdowns. Review of Economic Studies,76(2):669–705, 2009.
19. Vishwesha Guttal and Ciriyam Jayaprakash. Changing skewness: an early warning signal of regime shifts in ecosystems.Ecology Letters, 11(5):450–460, May 2008.
20. Hermann Haken. Synergetics: Introduction and advanced topics. Springer Science & Business Media, 2013.
21. Andrew C Harvey. Forecasting, structural time series models and the Kalman filter. Cambridge university press, 1990.
22. K. E. Henry, D. N. Hager, P. J. Pronovost, and S. Saria. A targeted real-time early warning score (TREWScore) for septicshock. Science Translational Medicine, 7(299):299ra122–299ra122, August 2015.
10/16

23. Yoshito Hirata, Nicholas Bruchovsky, and Kazuyuki Aihara. Development of a mathematical model that predicts theoutcome of hormone therapy for prostate cancer. Journal of Theoretical Biology, 264(2):517–527, May 2010.
24. Myles Hollander, Douglas A. Wolfe, and Eric Chicken. Nonparametric Statistical Methods: Hollander/NonparametricStatistical Methods. John Wiley & Sons, Inc., Hoboken, NJ, USA, July 2015.
25. Elizabeth Holmes, Eric Ward, and Kellie Wills. MARSS: Multivariate Autoregressive State-Space Modeling. 2018.
26. Elizabeth E. Holmes, Eric J. Ward, and Kellie Wills. MARSS: Multivariate autoregressive state-space models for analyzingtime-series data. The R Journal, 4(1):30, 2012.
27. Steven Horng, David A. Sontag, Yoni Halpern, Yacine Jernite, Nathan I. Shapiro, and Larry A. Nathanson. Creating anautomated trigger for sepsis clinical decision support at emergency department triage using machine learning. PLOS ONE,12(4):e0174708, April 2017.
28. Alistair E. W. Johnson, Tom J. Pollard, Lu Shen, Li-wei H. Lehman, Mengling Feng, Mohammad Ghassemi, BenjaminMoody, Peter Szolovits, Leo Anthony Celi, and Roger G. Mark. MIMIC-III, a freely accessible critical care database.Scientific Data, 3:sdata201635, May 2016.
29. Eric Kipnis, Davinder Ramsingh, Maneesh Bhargava, Erhan Dincer, Maxime Cannesson, Alain Broccard, Benoit Vallet,Karim Bendjelid, and Ronan Thibault. Monitoring in the intensive care. Critical care research and practice, 2012, 2012.
30. Anand Kumar, Daniel Roberts, Kenneth E. Wood, Bruce Light, Joseph E. Parrillo, Satendra Sharma, Robert Suppes, DanielFeinstein, Sergio Zanotti, Leo Taiberg, David Gurka, Aseem Kumar, and Mary Cheang. Duration of hypotension beforeinitiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock*:. Critical CareMedicine, 34(6):1589–1596, June 2006.
31. T. M. Lenton, V. N. Livina, V. Dakos, E. H. Van Nes, and M. Scheffer. Early warning of climate tipping points fromcritical slowing down: Comparing methods to improve robustness. Philosophical Transactions of the Royal Society A:Mathematical, Physical and Engineering Sciences, 370(1962):1185–1204, 2012.
32. Mitchell M. Levy, Mitchell P. Fink, John C. Marshall, Edward Abraham, Derek Angus, Deborah Cook, JonathanCohen, Steven M. Opal, Jean-Louis Vincent, Graham Ramsay, and SCCM/ESICM/ACCP/ATS/SIS. 2001SCCM/ESICM/ACCP/ATS/SIS International Sepsis Definitions Conference. Critical Care Medicine, 31(4):1250–1256,April 2003.
33. Rui Liu, Pei Chen, Kazuyuki Aihara, and Luonan Chen. Identifying early-warning signals of critical transitions with strongnoise by dynamical network markers. Scientific Reports, 5(1), December 2015.
34. Shannon Mitchell, Katherine Schinkel, Yifeng Song, Yuanbo Wang, John Ainsworth, Travis Halbert, Stephen Strong,Jinghe Zhang, Christopher C. Moore, and Laura E. Barnes. Optimization of sepsis risk assessment for ward patients. pages107–112. IEEE, April 2016.
35. Mitra Mojtahedi, Alexander Skupin, Joseph Zhou, Ivan G. Castano, Rebecca Y. Y. Leong-Quong, Hannah Chang, KalliopiTrachana, Alessandro Giuliani, and Sui Huang. Cell fate decision as high-dimensional critical state transition. PLOSBiology, 14(12):1–28, 12 2016.
36. World Health Organization. ICD-10: The ICD-10 Classification of Mental and Behavioural Disorders: diagnostic criteriafor research. In ICD-10: the ICD-10 classification of mental and behavioural disorders: diagnostic criteria for research.1993.
37. Michael Rothman, Mitchell Levy, R. Philip Dellinger, Stephen L. Jones, Robert L. Fogerty, Kirk G. Voelker, Barry Gross,Albert Marchetti, and Joseph Beals. Sepsis as 2 problems: Identifying sepsis at admission and predicting onset in thehospital using an electronic medical record–based acuity score. Journal of Critical Care, 38:237–244, April 2017.
38. Satya Swarup Samal, Jeyashree Krishnan, Ali Hadizadeh Esfahan, Christoph Lueders, Andreas Weber, and OvidiuRadulescu. Metastable regimes and tipping points of biochemical networks with potential applications in precisionmedicine. bioRxiv, 2018.
39. Marten Scheffer, Jordi Bascompte, William A Brock, Victor Brovkin, Stephen R Carpenter, Vasilis Dakos, HermannHeld, Egbert H van Nes, Max Rietkerk, and George Sugihara. Early-warning signals for critical transitions. Nature,461(7260):53–59, September 2009.
40. Mervyn Singer, Clifford S. Deutschman, Christopher Warren Seymour, Manu Shankar-Hari, Djillali Annane, MichaelBauer, Rinaldo Bellomo, Gordon R. Bernard, Jean-Daniel Chiche, Craig M. Coopersmith, Richard S. Hotchkiss, Mitchell M.Levy, John C. Marshall, Greg S. Martin, Steven M. Opal, Gordon D. Rubenfeld, Tom van der Poll, Jean-Louis Vincent, andDerek C. Angus. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA, 315(8):801,February 2016.
11/16

41. National Center for Health Statistics (US). The International Classification of Diseases: 9th Revision, Clinical Modification:ICD-9-CM. 1991.
42. Russel W Stineman. A Consistently Well Behaved Method of Interpolation. Creative Computing, 6(7):54–57, 1980.
43. Collin H H Tang, Paul M Middleton, Andrey V Savkin, Gregory S H Chan, Sarah Bishop, and Nigel H Lovell. Non-invasiveclassification of severe sepsis and systemic inflammatory response syndrome using a nonlinear support vector machine: apreliminary study. Physiological Measurement, 31(6):775–793, June 2010.
44. Rene Thomas and Richard d’Ari. Biological feedback. CRC press, 1990.
45. Christophe Trefois, Paul MA Antony, Jorge Goncalves, Alexander Skupin, and Rudi Balling. Critical transitions in chronicdisease: transferring concepts from ecology to systems medicine. Current Opinion in Biotechnology, 34:48–55, August2015.
46. J.-L. Vincent, Rui Moreno, Jukka Takala, Sheila Willatts, Arnaldo De Mendonca, Hajo Bruining, C. K. Reinhart, PeterMSuter, and L. G. Thijs. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure.Springer, 1996.
47. Jean-Louis Vincent, Arnaldo De Mendonca, Francis Cantraine, Rui Moreno, Jukka Takala, Peter M. Suter, Charles L.Sprung, Francis Colardyn, and Serge Blecher. Use of the SOFA score to assess the incidence of organ dysfunction/failurein intensive care units: results of a multicenter, prospective study. Critical care medicine, 26(11):1793–1800, 1998.
48. Conrad Hal Waddington. The strategy of the genes. London: Allen, 86, 1957.
49. A. F. Zuur, R. J. Fryer, I. T. Jolliffe, R. Dekker, and J. J. Beukema. Estimating common trends in multivariate time seriesusing dynamic factor analysis. Environmetrics, 14(7):665–685, 2003.
12/16

AcknowledgementsThe computing resources were granted by RWTH Aachen University under project rwth0260. S.S.S. was supported by fundingfrom CompSE profile area, RWTH Aachen University.
Author contributions statementP.F.G and S.S.S. developed the idea, conducted the research, and implemented the algorithms. J.S.B helped in the preparationof the data and in proofreading of the article. R.D. and G.M. provided the clinical insights and interpreted the findings. A.S.supervised and supported the research project. All authors have reviewed the manuscript.
Competing interestsThe author(s) declare no competing interests.
13/16

5 Appendix
m = 24 m = 30
−100
−50
050
100
t max
i c (
m)
− t
max
i c (
ref)
(a)
e = 4 e = 5
−100
−50
050
100
t max
i c (
e)
− t
max
i c (
ref)
(b)
Figure A1. The robustness of our procedure was examined by calculating SL of septic patients (c = 1 in sect.2.4) usingdifferent settings of moving time-window (m ∈ (24,30) and e ∈ (4,5)). The corresponding t ic
max for each set of parameters,along with their difference from the reference parameter set (m = 36, e = 3), were obtained. a) The difference between tmax(m)and t ic
max(re f ) shows the effect of moving time-window length on t icmax. b) The difference between t ic
max(e) and t icmax(re f ) shows
the effect of number of trends on t icmax.
14/16

−140 −120 −100 −80 −60 −40 −20 0
10
20
30
40
50
Time (t−T) [hours]
BU
N
−140 −120 −100 −80 −60 −40 −20 0
0.5
1.0
1.5
2.0
Time (t−T) [hours]
Cre
atin
ine
−140 −120 −100 −80 −60 −40 −20 0
10
15
20
25
30
35
40
Time (t−T) [hours]
BU
N_
Cre
atin
ine
−140 −120 −100 −80 −60 −40 −20 0
89
10
11
12
13
14
Time (t−T) [hours]
He
mo
glo
bin
−140 −120 −100 −80 −60 −40 −20 0
25
30
35
40
Time (t−T) [hours]
He
ma
tocri
t
−140 −120 −100 −80 −60 −40 −20 0
50
100
150
200
250
300
Time (t−T) [hours]
Pla
tele
ts
−140 −120 −100 −80 −60 −40 −20 0
135
140
145
Time (t−T) [hours]
So
diu
m
−140 −120 −100 −80 −60 −40 −20 0
3.5
4.0
4.5
5.0
5.5
Time (t−T) [hours]
Po
tassiu
m
−140 −120 −100 −80 −60 −40 −20 0
70
80
90
100
110
Time (t−T) [hours]
He
art
Ra
te
−140 −120 −100 −80 −60 −40 −20 0
40
50
60
70
Time (t−T) [hours]
Dia
sto
lic B
P
−140 −120 −100 −80 −60 −40 −20 0
60
70
80
90
Time (t−T) [hours]
Me
an
BP
−140 −120 −100 −80 −60 −40 −20 0
90
100
110
120
130
140
150
Time (t−T) [hours]S
ysto
lic B
P
−140 −120 −100 −80 −60 −40 −20 0
0.5
0.6
0.7
0.8
0.9
1.0
Time (t−T) [hours]
Sh
ock I
nd
ex
−140 −120 −100 −80 −60 −40 −20 0
10
15
20
25
Time (t−T) [hours]
Re
sp
ira
tory
Ra
te
−140 −120 −100 −80 −60 −40 −20 0
35.0
35.5
36.0
36.5
37.0
37.5
38.0
Time (t−T) [hours]
Te
mp
era
ture
−140 −120 −100 −80 −60 −40 −20 0
18
20
22
24
26
28
30
Time (t−T) [hours]
Bic
arb
on
ate
−140 −120 −100 −80 −60 −40 −20 0
94
96
98
100
102
Time (t−T) [hours]
Sp
O2
−140 −120 −100 −80 −60 −40 −20 0
46
810
12
14
16
18
Time (t−T) [hours]
WB
C
−140 −120 −100 −80 −60 −40 −20 0
050
100
150
200
250
Time (t−T) [hours]
Uri
ne
Ou
tpu
t
Figure A2. Median (dots) and median deviation (lines) of variables in septic shock patients (red) and non-sepsis patients(blue). T is the length of time series, and t−T is the time before the onset of septic shock in septic patients or the time before
discharge/decease in non-sepsis patients.
15/16

Variable −log10(P− value) BF BF (36 hrs) BF (18 hrs)tmax Random Time Points
BUN 92.2 86.9 0.98 0.05 0.00BUN-Creatinine 44.2 37.8 1.00 0.99 0.99
Creatinine 36.0 33.3 0.94 0.14 0.00Hemoglobin 20.2 18.2 0.86 0.81 0.00
Hematocrit 15.1 11.6 0.99 0.99 0.51Shock Index 14.4 8.9 0.99 0.98 0.77
Respiratory Rate 14.3 12.8 0.75 0.95 0.99Heart Rate 12.9 11.6 0.75 0.72 0.50
Systolic BP 9.0 2.1 1.00 0.99 0.99Bicarbonate 6.6 9.4 0.1 0.00 0.00
Platelets 5.3 5.6 0.35 0.00 0.00Temperature 4.8 1.9 0.99 0.93 0.95
Urine Output 4.6 6.0 0.2 0.00 0.00WBC 4.0 3.5 0.75 0.00 0.00
Mean BP 2.6 1.1 0.97 0.83 0.52SpO2 1.9 0.9 0.91 0.00 0.00
Diastolic BP 1.8 1.0 0.85 0.32 0.06Sodium 1.2 1.3 0.42 0.00 0.00
Potassium 0.6 0.2 0.82 0.92 0.98SLMean 19.3 - -
Table A1. A statistical significance test (see Sect. 2.4) was performed to test whether the values of clinical variables at largestSLMean were able to statistically differentiate septic shock patients from non-sepsis patients. −log10(P− value) of eachvariable at tmax were compared with the median −log10(P− value) of randomly selected points. The last three columns showthe corresponding BF (Full), BF (36 hours) and BF (18 hours) of each variable.
16/16