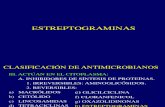
5ta Clase - Macrólidos, Clindamicina, Estreptograminas. Cloranfenicol, Linezolid
Cost-Effectiveness Analysis of Linezolid, Daptomycin, and Vancomycin in Methicillin-Resistant...
-
Upload
mark-bounthavong -
Category
Documents
-
view
222 -
download
1
Transcript of Cost-Effectiveness Analysis of Linezolid, Daptomycin, and Vancomycin in Methicillin-Resistant...

P
V A L U E I N H E A L T H 1 4 ( 2 0 1 1 ) 6 3 1 – 6 3 9
avai lable at www.sc iencedirect .com
journal homepage: www.elsevier .com/ locate / jva l
Cost-Effectiveness Analysis of Linezolid, Daptomycin, and Vancomycinin Methicillin-Resistant Staphylococcus aureus: Complicated Skin andSkin Structure Infection Using Bayesian Methods for EvidenceSynthesisMark Bounthavong, PharmD1,2,*, Amir Zargarzadeh, PharmD3, Donald I. Hsu, PharmD3,4, David J. Vanness, PhD5
1Veterans Affairs San Diego Healthcare System, San Diego, CA, USA; 2University of California, San Diego, Skaggs School of Pharmacy andharmaceutical Sciences, San Diego, CA, USA; 3Western University of Health Sciences, College of Pharmacy, Pomona, CA, USA; 4St. Joseph Hospital,
Orange, CA, USA; 5Department of Population Health Sciences, University of Wisconsin-Madison, Madison, WI, USA
A B S T R A C T
$ctswotDpKimc
Background: Methicillin-resistant Staphylococcus aureus (MRSA) com-plicated skin and skin structure infection (cSSSI) is a prominent infec-tion encountered in hospital and outpatient settings that is associatedwith high resource use for the health-care system. Objective: A deci-sion analytic (DA) model was developed to evaluate the cost-effective-ness analysis (CEA) of linezolid, daptomycin, and vancomycin in MRSAcSSSI. Methods: Bayesian methods for evidence synthesis were usedto generate efficacy and safety parameters for a DA model using pub-lished clinical trials. CEA was done from the US health-care perspec-tive. Efficacy was defined as a successfully treated patient at the test ofcure without any adverse reaction. Primary outcome was the incre-mental cost-effectiveness ratio between linezolid and vancomycin,daptomycin and vancomycin, and linezolid and daptomycin in MRSAcSSSI. Univariate and probabilistic sensitivity analyses were performed
linezolid, daptomycin, and vancomycin were $18,057, $20,698, and O
o repmicse Dri
al So
doi:10.1016/j.jval.2010.12.006
23,671, respectively. The cost-effectiveness ratios for linezolid, daptomy-in, and vancomycin were $37,604, $44,086, and $52,663 per successfullyreated patient, respectively. Linezolid and daptomycin were dominanttrategies compared to vancomycin. However, linezolid was dominanthen compared to daptomycin. The model was sensitive to the durationf daptomycin and linezolid treatment. Conclusion: Linezolid and dap-omycin are potentially cost-effective based on the assumptions of theA model; however, linezolid appears to be more cost-effective com-ared to daptomycin and vancomycin for MRSA cSSSIs.eywords: Bayesian methods, complicated skin and skin structure
nfections, cost-effectiveness analysis, daptomycin, decision analysisodel, linezolid, methicillin-resistant Staphylococcus aureus, vancomy-
in.
to test the robustness of the model. Results: The total direct costs of Copyright © 2011, International Society for Pharmacoeconomics and
utcomes Research (ISPOR). Published by Elsevier Inc.Introduction
Complicated skin and skin structure infections (cSSSIs) are com-monly encountered in both the community as well as the nosoco-mial settings and encompass a wide spectrum of infections fromsuperficial impetigo and mild cellulitis to severe infections involv-ing deeper fascia (e.g., abscess and surgical site infections) [1].cSSSIs are primarily caused by gram-positive bacteria, includingStaphylococcus aureus and �-hemolytic streptococci [1,2]. Methicil-lin-resistant S. aureus (MRSA) has become the predominant patho-gen in cSSSIs [3,4]. The impact of cSSSIs caused by MRSA has beenassociated with increased length of hospital stay and resource usecompared to infections caused by methicillin-sensitive strains [5].
Although vancomycin is still considered by many to be the goldstandard in the management of MRSA cSSSIs, several studies havedemonstrated the superiority of alternative agents such as linezolidand daptomycin [6–8]. More specifically, Weigelt et al. [6] reportedbetter overall outcomes for linezolid compared to vancomycin (88.6%
Conflicts of interest: The authors have no conflicts of interest t* Address correspondence to: Mark Bounthavong, Pharmacoecono
Veterans Affairs San Diego Healthcare System, 3350 La Jolla VillagE-mail: [email protected].
1098-3015/$36.00 – see front matter Copyright © 2011, Internation
Published by Elsevier Inc.
vs. 66.9%, P � 0.001) for a subgroup of patients with cSSSI caused byMRSA. Furthermore, in a meta-analysis of linezolid and vancomycinfor the management of MRSA cSSSIs, a higher rate of microbiologicaleradication was observed for patients managed with linezolid thanwith vancomycin (odds ratio 2.90; 95% confidence interval 1.90–4.41)[7]. Similarly, Davis et al. [8] described a more rapid resolution ofsymptoms and clinical cure for patients managed with daptomycincompared to a vancomycin historical control. It should also be notedthat, in this study, a shorter median antibiotic-related length of stay(LOS) was observed with the daptomycin arm compared to the van-comycin arm (4 days vs. 8 days, P � 0.01).
We previously evaluated the cost-effectiveness of linezolidversus vancomycin for the management of MRSA cSSSIs [9]. Al-though inpatient intravenous (IV) vancomycin therapy with tran-sition to outpatient IV therapy was determined to be the mostcost-effective strategy, for payers with a higher willingness-to-paythreshold (WTP), IV linezolid therapy with transition to outpatientoral therapy would be more cost-effective given its associated
ort.Clinical Specialist, Pharmacoeconomics/Formulary Management,ve (119), San Diego, CA 92161, USA.
ciety for Pharmacoeconomics and Outcomes Research (ISPOR).

t Stap
632 V A L U E I N H E A L T H 1 4 ( 2 0 1 1 ) 6 3 1 – 6 3 9
greater efficacy [9]. Similarly, in a cost-effectiveness analysis ofdaptomycin versus vancomycin for MRSA cSSSIs using a decisionanalysis (DA) model, we reported potential cost savings with dap-tomycin [10]. Currently, no study exists that comparatively evalu-ates the effectiveness of linezolid and daptomycin for the man-agement of MRSA cSSSIs. Available studies have compared thesenovel agents either to vancomycin or beta-lactams (e.g., oxacillin/nafacillin).
Indirect treatment comparison using Bayesian hierarchical mod-els provides a unique method to compare treatments in the absenceof head-to-head trials [11–14]. Bayesian hierarchical models usingMarkov chain Monte Carlo (MCMC) simulations can be applied toprovide indirect comparison of linezolid and daptomycin through acommon comparator (e.g., vancomycin) [11–14]. An advantage of us-ing the Bayesian random-effects indirect treatment comparisonmodel is the production of absolute probabilities for each treatmentthat can then be incorporated into a DA model. Although no directcomparison exists, Bayesian methods for evidence synthesis providea useful tool to generate parameters for a DA model [12]. This was thefirst study to apply Bayesian methods for evidence synthesis in acost-effectiveness analysis comparing vancomycin, linezolid, anddaptomycin for MRSA cSSSIs in a DA model.
Methods
DA Model
A DA model was built to evaluate the cost-effectiveness analysis ofvancomycin, linezolid, and daptomycin in MRSA cSSSIs. Themodel possessed three main branches, one for each of the treat-ment strategies. Each arm of the model represented a clinical
Table 1 – Description of the pathways used in the model.
Strategy
MRSA (�)/success/no ADR Patients were scultures werewere positivecomplete the
MRSA (�)/success/ADR/switched to tigecycline Patients were scultures on dexperiencedmg IV for 14 d
MRSA (�)/failure/switched to tigecycline Patients were scultures on ddetermined tdays with an
MRSA (�)/switched to oxacillin � dicloxacillin Patients were snegative on ddischarged w
ADR, adverse reaction; IV, intravenously; MRSA, methicillin-resistan
Fig. 1 – Decision analysis model. The squares represent the destrategies is made (linezolid, daptomycin, and vancomycin). Cthe pathway that a trial simulation will travel. Triangles repreof the pathway are collected. cSSSI, complicated skin and skin st
Staphylococcus aureus; MRSA (−), negative culture for methicillin-respathway that a patient can experience, which is described in Table1. A schematic diagram of the decision analysis model is illus-trated in Figure 1. Treatment doses were based on the clinicalliterature: vancomycin 1000 mg every 12 hours, linezolid 600 mgevery 12 hours, and daptomycin 4 mg/kg/day for an 80-kg patient[1]. Patients with a diagnosis of cSSSI were treated empirically forMRSA cSSSIs. Culture for MRSA was performed on the day of sus-pected cSSSI (day 0) and confirmed at day 2. It was assumed thatMRSA was present in 59% of patients with cSSSIs [15]. Oxacillin anddicloxacillin were used for patients who had a negative culture ofMRSA.
Success was defined as clinical resolution of signs and symptomof MRSA cSSSI infection at the test of cure. This was interpreted fromthe clinical trials as all patients who were clinically assessable, whichwas defined as all patients in the intention-to-treat population whoreceived the study drug, adhered to the protocol, and had sufficientdata available to make inferences about the study drug with clinicaloutcome. Discontinuation due to an adverse reaction (ADR) to thestudy drug was also modeled in the simulation. Vancomycin infu-sion was assumed to be 60 minutes for every gram, and the totallength of linezolid therapy (IV followed by oral formulation) was 15days [16].
Meta-analysis
Literature searchBuilding on the previous work of two meta-analyses [9,17], weperformed a literature search to identify other studies that maynot have been included. A PubMed search was performed frominception to May 2010 using the following combination of keywords: linezolid, daptomycin, vancomycin, skin and soft tissue
Description
on intravenous (IV) antibiotic empirically on day 1. Microbiologicalormed on day 1, and results were available on day 2. MRSA culturespatients would continue on IV antibiotic treatment. Patients wouldntibiotic course and not experience a relapse at the test of cureon IV antibiotic empirically on day 1, and had positive MRSA
Patients were continued on their IV antibiotic course butand had to be switched. Patients were switched to tigecycline 50ith an initial dose of 100 mg and assumed to respondon IV antibiotic empirically on day 1 and had positive MRSA
Patients were continued on their IV antibiotic course but wereonresponders on day 5 and switched to tigecycline 50 mg IV for 14l dose of 100 mg and assumed to respondon IV antibiotic empirically on day 1, but MRSA cultures were
Patients were then switched to IV oxacillin for 5 days anddays of dicloxacillin
hylococcus aureus.
n mode where the decision to use one of the three treatmentrepresent the chance node where probabilities determine
the terminal nodes where the total direct costs and benefitsre infection; MRSA (+), positive culture for methicillin-resistant
tartedperf
, andir IV atarteday 2.ADRs
ays wtarteday 2.o be ninitia
tarteday 2.ith 10
cisioirclessentructu
istant Staphylococcus aureus; ADR, adverse reaction.

tdstmoabw(pouhetbtawsftCmtj
aci
banetlarocpt
633V A L U E I N H E A L T H 1 4 ( 2 0 1 1 ) 6 3 1 – 6 3 9
infection, skin and skin structure infection, and methicillin-resistant Staphylococcus aureus. Studies that were prospectivetrials, with two or more of the study drugs, using an adult sam-ple (age 18 years and older), and had clinical efficacy as an out-come measure were included.
Clinical outcomesBayesian indirect treatment comparison was used to determinethe probabilities of success for the study therapies (e.g., linezolid,daptomycin, and vancomycin), which were incorporated into theDA model. A central assumption of indirect or mixed treatmentcomparison analysis is that the direct estimate of a treatmenteffect between C and B, dBC, is equivalent to the difference inreatment effects between B, C, and A, their common comparator:BC � dAC � dAB [14]. In assessing dBC, strength is borrowed fromtudies in which dAC or dAB is assessed. When multiple interven-ions are linked by a connected network of evidence, indirect or
ixed treatment comparison allows for treatments to be rank-rdered in terms of their effectiveness on an absolute (e.g., prob-bility) scale for all connected interventions. Joint posterior distri-utions of the absolute treatment effect of each study therapyere estimated with MCMC using the WinBUGS software package
WinBUGS v1.4; Imperial College and MRC, London, UK) [18]. Vagueriors were used to reduce the influence of previous distributionn the observed results and provide information similar to thatsing a conventional frequentist approach [19]. To reflect potentialeterogeneity between studies, a normally distributed random-ffects model on the log-odds scale was used to model the relativereatment effects [20]. A uniform distribution was selected for theetween-study variance, which provided the least influence onhe posterior distribution [21]. Convergence was visually assessedfter a burn-in of 5000 iterations; 10,000 subsequent iterationsere used for inference [22]. Discontinuation due to ADR to the
tudy therapies was estimated using a similar approach. Drawsrom the MCMC were exported using the Convergence Diagnos-ic and Output Analysis (CODA v0.30; MRC Biostatistics Unit,ambridge, UK) function and then incorporated into the DAodel to maintain correlation in the joint posterior distribu-
ion. WinBUGS code is presented in Appendix A at doi:10.1016/.jval.2010.12.006.
Table 2 – Cost of items in the decision analysis model.
Item Cost ($US) �25%
Drug cost per dayIV vancomycin (1 g BID) 14.00 3.5IV linezolid (600 mg BID) 240.22 60.0PO linezolid oral (600 mg BID) 183.95 45.9IV daptomycin (80-kg patient) 272.70 68.1IV oxacillin (2 g every 6 hr) 103.08 25.7PO dicloxacillin (500 mg every 6 hr) 4.80 1.2Tigecycline treatment cost 1102.50 275.6Hospitalization (1 day) 2132.51 533.1Vancomycin trough 6.70 1.6Microbiological culture 43.78 10.9Platelet monitoring 9.16 2.2SCr monitoring 2.03 0.5
BID, twice daily; IV, intravenous; LL, lower limit; PO, oral; SCr, serum* A 25% variance of the point estimate was used in the probabilistic† Lower limit and upper limit were used in the univariate analysis.‡ Health Economic Resource Center, 2006 report. All costs were adju
§ Decision Support Services, 2008 report. All costs were adjusted for 2009Economic analysisThis analysis was conducted from the perspective of the UShealth-care payer; therefore, US dollars were used. All costs wereadjusted for 2009 based on the medical component of the Con-sumer Price Index (Table 2). Total direct costs included acquisitioncosts of the study medications, laboratory analysis, microbiology,and a night of hospital stay. Acquisition costs of the study thera-pies were determined from the Drug Red Book [23]. Costs of dailyhospital stay, vancomycin levels (trough), platelet monitoring, re-nal panels, and microbiological cultures were based on the Deci-sion Support System (DSS) database. DSS is the Veterans Affairs(VA) national database that provides resource utilization directedat patient care. Information was pulled from VA hospitals acrossthe country and itemized for easy interpretation of resource utili-zations. Cost parameters and resource utilization were modeledusing gamma and triangular distributions, respectively [24].
The primary outcome of interest was the incremental cost per onedditional treatment success, otherwise known as the incrementalost-effectiveness ratio (ICER). ICERs were calculated using the follow-ng equation: (CTreatment A � CTreatment B)/(ETreatment A � ETreatment B),where C is the total direct costs of the treatment, E is the effect or
enefit of the treatment, Treatment A is the study drug of interest,nd Treatment B is the comparator [24,25]. Average cost-effective-ess ratios were calculated as total direct costs divided by thefficacy (C/E) for each of the study comparisons [24,25]. Cost-effec-iveness was evaluated for the following pairwise comparisons:inezolid versus vancomycin, daptomycin versus vancomycin,nd linezolid versus daptomycin because these were the mostelevant comparisons to decision makers. A dominant strategy isne in which the incremental cost of the study drug is less than theomparator and the incremental efficacy is greater than the com-arator [24,25]. Discounting was not applied because of the shortime frame of the study.
AssumptionsPatients who had a culture negative for MRSA on day 2 wereswitched to an oxacillin/dicloxacillin regimen and presumed torespond to the alternative therapy. Gram-negative coverage wasassumed to be similar between treatment arms and not includedin the analysis. Patients receiving vancomycin would have an ini-tial serum creatinine laboratory value obtained as well as a fol-
LL ($US)† UL ($US) Distribution Ref.
10.50 17.50 Gamma [21]180.17 300.28 Gamma [21]137.96 229.94 Gamma [21]204.53 340.88 Gamma [21]77.31 128.85 Gamma [21]3.60 6.01 Gamma [21]
826.88 1378.13 Gamma [21]1599.38 2665.64 Gamma HERC‡
5.03 8.38 Gamma DSS§
32.84 54.73 Gamma DSS6.87 11.45 Gamma DSS1.52 2.54 Gamma DSS
tinine; UL, upper limit.tivity analysis.
for 2009 US Dollars ($US).
*
069870338591
creasensi
sted
US dollars ($US).

634 V A L U E I N H E A L T H 1 4 ( 2 0 1 1 ) 6 3 1 – 6 3 9
low-up on day 3. In addition, a vancomycin trough would be drawnevery 3 days to simulate blood serum monitoring. Linezolid wouldbe monitored for thrombocytopenia at least once while on ther-apy. Patients in whom therapy was considered a failure wereswitched to tigecycline 50 mg IV for 14 days (with an initial dose of100 mg on day 1) and assumed to be complete responders [26]. Allclinical outcomes were assumed to be reported at the test of cure.Death was not included in our model as a possible clinical path-way because we assumed that the contribution to the outcome ofcSSSIs was minimal.
Patients receiving linezolid for empirical therapy were as-sumed to receive 5.4 days of IV therapy and then discharged on 9.6days of oral linezolid for a total of 15 days of treatment (Table 3)[16]. Patients started on daptomycin empirically were assumedto receive their entire course of therapy in the hospital (6.1 days)until resolution of signs and symptoms [27]. Patients started onvancomycin empirically were assumed to receive their entirecourse of therapy (14 days) in the hospital until resolution ofsigns and symptoms [16,28]. In addition, patients had the van-comycin trough monitored every 3 days.
Sensitivity analysesIn the indirect treatment comparison evaluating discontinuationdue to an ADR, the point estimates used in the DA model weresmall. We wanted to investigate the upper limit of the 95% credibleinterval (CrI), the Bayesian analogue to the standard confidenceinterval, and performed a sensitivity analysis using the higher val-
Table 3 – Resource utilization.
Point estimate
Antibiotic-related LOS, daysVancomycin 14Linezolid 5.4Daptomycin 6.1Oxacillin 5
Duration of PO linezolid, days 9.6Duration of PO dicloxacillin, days 10No. of days until clinical response 5
LL, lower limit; LOS, length of stay; PO, oral; UL, upper limit.* Lower limit and upper limit were used in the univariate analysis.
Table 4 – Characteristics of the studies.
Study Drugs Age in years ofexperimental
Age in yecompar
Davis et al.,2007 [8]
Daptomycin vs. vancomycin Median 45(range 19–67)
Median 45(range 1
Arbeit et al.,2004 [34]
Daptomycin vs. comparators* Mean 51.5(range 18–91)
Mean 51.9(range 1
Katz et al.,2008 [35]
Daptomycin vs. vancomycin Mean 43.5(range 18–77)
Mean 41.0(range 1
Pertel et al.,2009 [36]
Daptomycin vs. vancomycin Median 54(range 125–79)
Median 48(range 1
Stevens et al.,2002 [37]
Linezolid vs. vancomycin Mean 63.9(SD 16.1)
Mean 59.8(SD 20.2
Weigelt et al.,2004 [38]
Linezolid vs. vancomycin Mean 60(SD 16)
Mean 60(SD 18)
Weigelt et al.,2005 [6]
Linezolid vs. vancomycin Mean 52(SD 18)
Mean 52(SD 18)
Kohno et al.,2007 [39]
Linezolid vs. vancomycin Mean 68.4(SD 16.4)
Mean 67.5(SD 16.3
Wilcox et al.,2009 [40]
Linezolid vs. vancomycin Mean 53.7(SD 18.1)
Mean 53.8(SD 17.6
CE, clinical evaluation; MRSA, methicillin-resistant Staphylococcus au
* Comparators include penicillinase-resistant penicillin or vancomycin.ues as the point estimates (scenario 1). In scenario 2, we investi-gated the change in ICER when the LOS of patients treated withvancomycin was reduced from 14 to 8 days [8,29]. In scenario 3, weinvestigated the change in ICER when the duration of IV linezolidwas reduced from 5.4 to 1.8 days to take advantage of linezolid’s100% bioavailability [29]. In scenario 4, we investigated the changein ICER when the duration of IV daptomycin was reduced from 6.1to 4 days based on the results from one study [8].
Univariate (one-way) sensitivity analysis was performed for allparameters in the base-case DA model for the comparison of lin-ezolid and daptomycin. Mean probabilities generated from theBayesian random-effects meta-analysis was used along with thecalculated 95% CrI. Probabilistic sensitivity analysis (second-orderMonte Carlo simulation) was performed for all comparisons using10,000 trial simulations and plotted on a cost-effectiveness plane[30,31]. Uncertainties of the cost-effectiveness for the treatment ofinterest versus the comparator based on the cumulative densityfunction with increasing WTP were presented as acceptability curves[31–33]. Analyses were performed using TreeAge Pro Suite 2009 (re-lease 1.5.1; TreeAge Software, Inc., Williamstown, MA, USA).
Results
A total of 9 studies were used to generate efficacy and discontin-uation due to ADR probabilities based on the Bayesian method ofindirect treatment comparison [6,8,34–40]. Characteristics of each
LL* UL Distribution Refs.
3 19 Triangular [8, 27]1 10 Triangular [26, 27]4 14 Triangular [8, 33, 44, 46]3 7 Triangular [35]4 15 Triangular [26, 27]5 15 Triangular [35]2 7 Triangular [44, 45]
CE results ofexperimental
CE results ofcomparator
MRSA ofexperimental
MRSA ofcomparator
41/53 (77.4%) 89/212 (42.0%) NR NR
372/446 (83.6%) 384/456 (84.2%) 21/28 (75.0%) 25/36 (69.4%)
32/39 (82.1%) 37/39 (94.9%) 22/31 (71.0%) 24/28 (85.7%)
)22/28 (78.6%) 16/22 (72.7%) NR NR
9/17 (52.9%) 5/10 (50.0%) 13/18 (72.2%) 4/10 (40.0%)
53/57 (93.0%) 48/55 (87.3%) 41/49 (83.7%) 28/49 (57.1%)
39/45 (86.7%) 31/39 (79.5%) 42/48 (87.5%) 34/39 (87.2%)
64/99 (64.6%) 54/87 (62.1%) 27/34 (79.4%) 22/30 (73.3%)
439/476 (92.2%) 402/454 (88.5%) 124/140 (88.6%) 97/145 (66.9%)
ars ofator
9–73)
7–94)
8–86)
18–86
)
)
)
reus.

635V A L U E I N H E A L T H 1 4 ( 2 0 1 1 ) 6 3 1 – 6 3 9
study and data used in the meta-analyses are presented in Table 4.Four studies were used for daptomycin [8,34–36], and five studieswere used for linezolid [6,37–40]. All studies used vancomycin asthe comparator except for one study, which used beta-lactamsand vancomycin [34]. The mean age of the experimental drugranged from 43.5 years to 68.4 years, and the mean age of thecomparator ranged from 41.0 years to 67.5 years.
In the Bayesian meta-analysis, linezolid had a higher probabil-ity of success at the test of cure (82%) followed by daptomycin(80.1%) and vancomycin (76.7%). However, daptomycin had alower probability of patients discontinuing empirical therapy dueto an ADR (0.1%) compared to linezolid (0.2%) and vancomycin(0.2%). Mean probabilities with SDs and 95% CrIs are presented inTable 5.
In the base-case analysis, linezolid and daptomycin weredominant compared to vancomycin (Table 6). However, whencompared to daptomycin, linezolid was a dominant strategy.The total direct costs for linezolid, daptomycin, and vancomy-cin were $18,057, $20,698, and $23,671, respectively. The cost-effectiveness ratios for linezolid, daptomycin, and vancomycinwere $37,604, $44,086, and $52,663 per successfully treated pa-tient, respectively. Extended dominance was not observed inthe cost-effectiveness frontier (not shown).
In the one-way sensitivity analyses comparing linezolid todaptomycin, the base-case ICER was sensitive to three model pa-rameters (Table 7). If the duration of IV daptomycin was de-creased, linezolid was no longer a dominant strategy. If the du-rations of linezolid oral and IV therapy were increased, linezolidwas no longer a dominant strategy. For all other parameters, themodel was robust. The model was also robust in most of thedifferent scenarios investigated (scenarios 1, 2, and 3) with theexception of scenario 4, in which the duration of IV daptomycinwas changed from 6.8 to 4 days (Table 8). In scenario 4, linezolidwas no longer a dominant strategy.
Table 5 – Base-case parameters of the decision analysis m
Variable Mean SD
Success*Vancomycin 0.767 0.0Linezolid 0.820 0.0Daptomycin 0.801 0.0Heterogeneity parameter (��) 0.777 0.3
Discontinuation due to ADR*Vancomycin 0.002 0.0Linezolid 0.002 0.0Daptomycin 0.001 0.0Heterogeneity parameter (��) 0.381 0.3
Mean SD
Probability of MRSA (�) 0.590 0.1
ADR, adverse reaction; CrI, credible interval; LL, lower limit; MRSA, m* Bayesian meta-analysis was performed to generate the probabilitie† Lower limit and upper limit were used in the univariate analysis.
Table 6 – Base-case results of probabilistic sensitivity anal
Strategy Total costs SD Incrementalcosts
Efficacy
Vancomycin $23,671 $7069 0.449 0Linezolid $18,057 $4840 �$5614 0.480 0Daptomycin $20,698 $5632 �$2973 0.469 0
CER, cost-effectiveness ratio; DAP, daptomycin; ICER, incremental cost-ef
Results of the probabilistic sensitivity analysis were plotted onan incremental cost-effectiveness plane comparing linezolid andvancomycin, daptomycin and vancomycin, and linezolid and dap-tomycin (Fig. 2). For all comparisons, a majority of the ICER scat-terplots were in the dominant quadrant (less costly and more ef-fective). In the probabilistic sensitivity analysis comparinglinezolid and vancomycin, 75.34% of the ICER scatterplots were inthe dominant quadrant. In the comparison of daptomycin andvancomycin, 57.38% of the ICER scatterplots were in the dominantquadrant. In the comparison of linezolid and daptomycin, 48.08%of the ICER scatterplots were in the dominant quadrant.
Acceptability curves were created for all comparisons: lin-ezolid and vancomycin, daptomycin and vancomycin, and lin-ezolid and daptomycin (Fig. 3). Linezolid was a cost-effectivestrategy across the WTP range investigated compared to vanco-mycin and daptomycin; and daptomycin was a cost-effectivestrategy across the WTP range investigated compared to vanco-mycin. The acceptability curve dropped slightly in the linezolidand daptomycin comparison; however, the curve plateaued andremained greater than 50%, favoring linezolid.
Discussion
Clinical outcomes associated with the management of cSSSIs areinfluenced by multiple factors such as host comorbidities, size ofinfected lesion, surgical intervention, selection of antibiotics, and theinfecting organism(s) [41]. More specifically, MRSA cSSSIs are associ-ated with poorer treatment outcomes compared to infections causedby methicillin-sensitive strains, with an increased risk of concomi-tant bacteremia, need for amputation, and mortality [42–44]. Al-though vancomycin remains the gold standard for the managementof MRSA cSSSIs, intolerance and adverse effects associated with ad-ministration and/or use of the antibiotic often limits its usefulness.
.
2.5% (CrI) 97.5% (CrI) Refs.
0.721 0.811 [7, 17]0.681 0.921 [7]0.609 0.917 [17]0.286 1.618
3.52E-13 0.015 [7, 17]3.93E-13 0.017 [7]2.35E-13 0.011 [17]0.023 1.303
LL† UL
0.150 0.740 [15]
cillin-resistant Staphylococcus aureus; UL, upper limit.success and discontinuation due to ADR for the different treatments.
Incrementalefficacy
CER ICER (vs. VAN) ICER (LIN vs. DAP)
$52,6630.031 $37,604 Dominant Dominant0.020 $44,086 Dominant
odel
23617736
04050437
37
ethis for
ysis.
SD
.101
.113
.114
fectiveness ratio; LIN, linezolid; VAN, vancomycin.

nc
cctccs
cttstw
it; MR
636 V A L U E I N H E A L T H 1 4 ( 2 0 1 1 ) 6 3 1 – 6 3 9
Furthermore, increasing reports of MRSA demonstrating intermedi-ate resistance to vancomycin have raised concerns [45]. As such, al-ternative agents such as linezolid and daptomycin have become in-creasingly more attractive as treatment options for MRSA cSSSIs.
Our study was the first to use Bayesian methods for indirect com-parisons of daptomycin and linezolid. In our investigation, linezolidand daptomycin were cost-effective when compared to vancomycin,primarily because of increased efficacy and reduced hospital LOS.Several studies have shown that the use of linezolid or daptomycinresulted in decreased LOS and increased efficacy compared to van-comycin [6,16,27–29,46]. Reduction in LOS is an important compo-
ent in total direct costs for cSSSIs, and any advantage that a medi-ation can provide to reduce this variable would result in significant
Table 7 – One-way sensitivity analysis results comparing l
Parameter ICER
Low ICER
Duration of IV daptomycin in days �$856,104Duration of IV linezolid in days �$497,403Duration of PO linezolid in days �$81,552Cost of IV daptomycin �$62,844Cost of hospitalization �$59,471Cost of IV linezolid �$57,868Cost of PO linezolid �$55,593Probability of daptomycin success �$57,688Probability of MRSA (�) �$53,533Probability of linezolid discontinuation �$51,871No. of days until response �$41,707Probability of linezolid success �$31,910Probability of daptomycin discontinuation �$36,409Cost of tigecycline regimen �$36,397Cost of platelet monitoring �$36,245Cost of creatinine monitoring �$36,149
A negative incremental cost-effectiveness ratio reflects that linezolidcost-effectiveness ratio reflects that daptomycin is dominant comparedICER, incremental cost-effectiveness ratio; IV, intravenous; LL, lower lim
Table 8 – Results of scenario analyses.
Scenario Total costs SD Incrementalcosts
Efficacy
1Vancomycin $25,964 $149 0.446 0Linezolid $18,450 $1002 �$7514 0.475 0Daptomycin $18,776 $1269 �$7189 0.467 0
2Vancomycin $19,949 $331 0.452 0Linezolid $18,232 $1021 �$1717 0.483 0Daptomycin $18,626 $1284 �$1323 0.472 0
3Vancomycin $25,776 $164 0.452 0Linezolid $14,422 $1305 �$11,354 0.483 0Daptomycin $18,626 $1284 �$7150 0.472 0
4Vancomycin $25,776 $164 0.452 0Linezolid $18,232 $1021 �$7544 0.483 0Daptomycin $16,241 $1513 �$9535 0.472 0
Scenario 1: High end of the 95% credible interval for probability of dilength of stay was changed from 14 days to 8 days. Scenario 3: Linezo4: Daptomycin hospital length of stay was changed from 6.8 days to
CER, cost-effectiveness ratio; ICER, incremental cost-effectiveness ratio; Vost savings. However, decision makers should not be solely con-erned with total costs as an end point when making a conclusion onhe cost-effectiveness of one agent over another in cSSSIs. The effi-acy of the antibiotic needs to be balanced with its costs; moreover,onsideration should be made for the potential for antimicrobial re-istance, which was not modeled in our study.
Most of the studies reported clinical outcomes at the test ofure rather than the end of treatment. This reporting method cap-ured relapse rates that would not have been seen at the end ofreatment, thereby eliminating the need to model relapse in ourtudy. However, there were two studies evaluating daptomycinhat did not report clinical outcomes at the test of cure. As a result,e had to assume that the outcomes reported were similar at
olid to daptomycin.
erences Range
High ICER LL UL
$181,848 4 14$446,127 1 10$7686 4 15
�$9403 $204.53 $340.88�$12,773 $1599.38 $2665.64�$14,371 $180.17 $300.28�$16,651 $137.96 $229.94�$26,824 0.6088 0.9168�$34,919 0.15 0.74�$35,595 3.97E-13 0.01758�$27,744 2 7�$24,565 0.6814 0.9207�$34,540 2.51E-13 0.01145�$35,846 $826.88 $1378.13�$35,998 $6.87 $11.45�$36,094 $1.52 $2.54
dominant compared to daptomycin therapy. A positive incrementalnezolid. The base-case ICER is �$36,122.77 (linezolid vs. daptomycin).SA, methicillin-resistant Staphylococcus aureus; PO, oral; UL, upper limit.
Incrementalefficacy
CER ICER (vs. VAN) ICER (LIN vs. DAP)
$58,2700.030 $38,831 Dominant Dominant0.021 $40,213 Dominant
$44,1680.031 $37,777 Dominant Dominant0.020 $39,485 Dominant
$57,0680.031 $29,881 Dominant Dominant0.020 $39,485 Dominant
$57,0680.031 $37,777 Dominant $182,7890.020 $34,427 Dominant
inuation due to adverse reactions. Scenario 2: Vancomycin hospitalospital length of stay was changed from 5.4 day to 1.4 days. Scenarios.
inez
diff
is ato li
SD
.013
.036
.045
.013
.036
.045
.013
.036
.045
.013
.036
.045
scontlid h
4 day
AN, vancomycin; LIN, linezolid; DAP, daptomycin.
48.08%, respectively.
637V A L U E I N H E A L T H 1 4 ( 2 0 1 1 ) 6 3 1 – 6 3 9
the test of cure. Pertel et al. [36] did not provide enough infor-mation to determine whether the results were collected at thetest of cure or the end of treatment. Similarly, Davis et al. [8]only reported outcomes at the end of treatment. We applied therandom-effects model in our Bayesian meta-analysis to reflectthis design heterogeneity.
The LOS for each study drug varied depending on the studiesused. In scenario 4, we reported that the model was sensitive tothe changes in daptomycin duration of IV therapy. The variabilityin LOS and duration of IV treatment may be attributed to study sitepolicy and protocol. Observational studies provide real-world dataon how drug therapies are used and may be more robust in a DAmodel. However, the only available observational studies that wefound were based on the Cubicin Outcomes Registry and Experi-ence (CORE) registry for daptomycin [46–48]. In the CORE registry,the median duration of IV daptomycin therapy for cSSSIs was 13 days(range 2–148 days) compared to the base-case number of 6.1 days(range 4–14 days) [48]. The base-case results were sensitive to thesedata and demonstrated the importance of using observational stud-ies in DA modeling. Future analysis should use registry data or ob-servational studies to further improve DA models.
The CORE registry reported variations in the daily dose for pa-tients with cSSSIs ranging from 2.3 mg/kg to 12.0 mg/kg (mean 4.5,SD 1.0 mg/kg) [46]. Although product label dose and frequency fordaptomycin (4 mg/kg/day) were mostly used, 29.7% of patients(29/165) received daptomycin at a dose greater than 4 mg/kg/dayand 7.3% of patients (12/165) had intervals that were greater than24 hours. Reasons for this may be a lack of initial efficacy, per-ceived severity of illness, body weight, and renal insufficiency. Itshould be noted that daptomycin demonstrates concentration-dependent bactericidal activity. As such, the response to dapto-mycin may improve with increasing daily dose. However, the out-come of this relationship has not been firmly established in theliterature. Future research will need to model the higher doses ofdaptomycin in special populations (e.g., hemodialysis and obesepatients) to better elucidate the clinical outcomes of dosing out-side the product labeling.
Several treatment options are available for MRSA cSSSIs. Tige-cycline [49], telavancin [50,51], dalfopristin/quinopristine [52],ceftobiprole [53], ceftaroline [54], and iclaprim [55] have evidenceto support their use in MRSA cSSSIs. Tigecycline, telavancin, anddalfopristin/quinopristine are approved by the US Food and DrugAdministration (FDA), with telavancin being the most recent.Ceftobiprole, ceftaroline, and iclaprim are future potential agentsthat could be used in MRSA cSSSIs; however, they are not currentlyapproved by the FDA (at the time that this article was written). Thenumber of novel agents for MRSA cSSSIs will require decisionmakers to evaluate the cost-effectiveness of each agent relative toanother. However, the lack of direct head-to-head trials for thenewer agents will necessitate the use of Bayesian methods in ev-idence synthesis to generate probabilities to be applied in futureDA models.
Bayesian models provide a useful method to synthesize indi-rect comparisons among treatments that lack head-to-head trials.We applied this method to develop posterior probability estimatesfor linezolid and daptomycin, which were then incorporated into aDA model. This approach to decision modeling has been called“comprehensive decision modeling” [12,56]. Comparative effec-tiveness research requires that evaluation be made between twotreatment strategies that are considered equivalent or standard ofcare. The current practices, however, for FDA approval do not nec-essarily require these types of studies for New Drug Application.Therefore, there is a gap in the literature where relevant direct com-parisons are unavailable, thus, contributing to the uncertainty re-garding the relative efficacy and safety of certain novel medications.Bayesian methods for meta-analysis provide a framework with
Fig. 2 – Probabilistic sensitivity analyses results forcomparisons of linezolid and vancomycin (A), daptomycinand vancomycin (B), and linezolid and daptomycin (C). Adrug is considered dominant if it is less costly and moreeffective than its comparator (southeast quadrant).Scatterplots on the cost-effectiveness plane represent theindividual incremental cost-effectiveness ratios drawn fromthe simulation (10,000 trial simulations). Incremental costwas based on US dollars ($US) and was plotted on the y-axis. Incremental efficacy was based on success of thetreatment and plotted on the x-axis. The distributions ofincremental cost-effectiveness ratios scatter in thedominant quadrant for the comparisons of linezolid andvancomycin (A), daptomycin and vancomycin (B), andlinezolid and daptomycin (C) were 75.34%, 57.38% and
which to estimate the differences in the absence of data. However,

(
[
[
[
[
[
[
[
[
[
[
638 V A L U E I N H E A L T H 1 4 ( 2 0 1 1 ) 6 3 1 – 6 3 9
validation of this method would require a large, prospective studycomparing linezolid and daptomycin.
Conclusion
By applying Bayesian random effects, indirect treatment compar-ison, probability estimates among linezolid, daptomycin, and van-comycin were generated and incorporated into a DA model forMRSA cSSSIs. When compared to vancomycin, linezolid and dap-tomycin were dominant strategies in treating MRSA cSSSIs. How-ever, when compared to each other, linezolid was dominant com-pared to daptomycin. Sensitivity analyses reported that the modelwas sensitive to the duration of drug therapy but not to drug costs.Future prospective studies comparing linezolid and daptomycinshould be performed to validate the results of our comprehensivedecision model.
Supplemental Materials
Supplemental material accompanying this article can be found inthe online version as a hyperlink at doi:10.1016/j.jval.2010.12.006,or if hard copy of article, at www.valueinhealthjournal.com/issuesselect volume, issue, and article).
R E F E R E N C E S
[1] Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for thediagnosis and management of skin and soft-tissue infections. ClinInfect Dis 2005;41:1373–406.
[2] Rennie RP, Jones RN, Mutnick AH. Occurrence and antimicrobialsusceptibility patterns of pathogens isolated from skin and soft tissueinfections: report from the SENTRY antimicrobial surveillanceprogram (United States and Canada, 2000). Diagn Microbiol Infect Dis2003;45:287–93.
[3] Swartz MN. Hospital-acquired infections: diseases with increasinglylimited therapies. Proc Natl Acad Sci U S A 1994;91:2420–7.
[4] Frazee BW, Lynn J, Charlebois ED, et al. High prevalence of methicillin-
Fig. 3 – Acceptability curves for comparisons of linezolid anddaptomycin. Willingness to pay was plotted on the x-axis afor an additional benefit gained. The probability of selecting
resistant Staphylococcus aureus in emergency department skin and softtissue infections. Ann Emerg Med 2005;45:311–30.
[5] Abramson MA, Sexton DJ. Nosocomial methicillin-resistant andmethicillin-susceptible Staphylococcus aureus primary bacteremia: atwhat costs? Infect Control Hosp Epidemiol 1999;20:408–11.
[6] Weigelt J, Itani K, Stevens D, et al. Linezolid versus vancomycin intreatment of complicated skin and soft tissue infections. AntimicrobAgents Chemother 2005;49:2260–6.
[7] Bounthavong M, Hsu DI. Efficacy and safety of linezolid in methicillin-resistant Staphylococcus aureus (MRSA) complicated skin and soft tissueinfection. Curr Med Res Opin 2010;26:407–21.
[8] Davis SL, McKinnon PS, Hall LM, et al. Daptomycin versus vancomycinfor complicated skin and skin structure infections: clinical andeconomic outcomes. Pharmacotherapy 2007;27:1611–8.
[9] Bounthavong M, Hsu DI, Okamoto MP. Cost-effectiveness analysisof linezolid s. vancomycin in treating methicillin-resistantStaphylococcus aureus complicated skin and soft tissue infections usinga decision analytic model. Int J Clin Pract 2009;63:376–86.
10] Zargarzadeh AH, Bounthavong M, Hsu DI, Okamoto MP. Cost-effectiveness analysis of daptomycin versus vancomycin incomplicated skin and soft structure infection (cSSSI) using a decisionanalytical model. Presented at the 14th Annual Meeting of theInternational Society for Pharmacoeconomics and OutcomesResearch, May 16–20, 2009, Orlando, FL.
11] Jansen JP, Crawford B, Bergman G, Stam W. Bayesian meta-analysis ofmultiple treatment comparisons: an introduction to mixed treatmentcomparisons. Value Health 2008;11:956–64.
12] Ades AE, Sculpher M, Sutton A, et al. Bayesian methods for evidencesynthesis in cost-effectiveness analysis. Pharmacoeconomics 2006;24:1–19.
13] Lumley T. Network meta-analysis for indirect treatment comparisons.Stats Med 2002;21:2313–24.
14] Sutton A, Ades AE, Cooper N, Abrams K. Use of indirect and mixedtreatment comparisons for technology assessment.Pharmacoeconomics 2008;26:753– 67.
15] Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S.aureus infections among patients in the emergency department.N Engl J Med 2006;355:666–74.
16] Li Z, Willke RJ, Pinto LA, Rittenhouse BE, et al. Comparison of length ofhospital stay for patients with known or suspected methicillin-resistantStaphylococcus species infection treated with linezolid or vancomycin: arandomized, multicenter trial. Pharmacotherapy 2001;21:262–74.
17] Bliziotis IA, Plessa E, Peppas G, Falagas ME. Daptomycin versus otherantimicrobial agents for the treatment of skin and soft tissueinfections: a meta-analysis. Ann Pharmacother 2010;44:97–106.
18] Spiegelhalter D, Thomas A, Best N, Lunn D. WinBUGS User Manual. Version1.4. Cambridge, UK; MRC Biostatistics Unit, 2003.
19] Lambert PC, Sutton AJ, Burton PR, et al. How vague is vague? A
comycin, daptomycin and vancomycin, and linezolid andflects the health-care system’s ability to invest resources
most cost-effective strategy is represented on the y-axis.
vannd rethe
simulation study of the impact of the use of vague prior distributionsin MCMC using WinBUGS. Statist Med 2005;24:2401–28.

[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
639V A L U E I N H E A L T H 1 4 ( 2 0 1 1 ) 6 3 1 – 6 3 9
[20] Smith TC, Spiegelhalter DJ, Thomas A. Bayesian approaches torandom-effects meta-analysis: a comparative study. Stat Med 1995;14:2685–99.
21] Gelman A. Prior distributions for variance parameters in hierarchicalmodels. Bayesian Analysis 2006;1:151–33.
22] Gelman A, Rubin DB. Inferences from iterative simulation usingmultiple sequences. Statistical Science 1992;7:457–72.
23] Red Book Pharmacy’s Fundamental Reference. Montvale, NJ:Thompson Healthcare, 2009.
24] Drummond MF, Sculpher MJ, Torrance GW, et al., eds., Methods for theEconomic Evaluation of Health Care Programmes (3rd ed.). New York:Oxford University Press, 2005.
25] Gold MR, Siegel JE, Russell LB, Weinstein MC. Cost-effectiveness inHealth and Medicine. New York: Oxford University Press, 1996.
26] Tigecycline. Product label. Wyeth Pharmaceuticals, Inc., Philadelphia,PA. 2010.
27] Fossaceca C. Outcomes analysis of daptomycin use in a communityhospital. Adv Ther 2007;24:517–28.
28] McKinnon PS, Sorenson SV, Liu LZ, Itani KMF. Impact of linezolid oneconomic outcomes and determinants of cost in a clinical trialevaluating patients with MRSA complicated skin and soft-tissueinfections. Ann Pharmacother 2006;40:1017–23.
29] Itani KMF, Weigelt J, Li JZ, Duttagupta S. Linezolid reduces length ofstay and duration of intravenous treatment compared withvancomycin for complicated skin and soft tissue infections due tosuspected or proven methicillin-resistant Staphylococcus aureus(MRSA). Int J Antimicrob Agents 2005;26:442–8.
30] Briggs AH. Handling uncertainty in cost-effectiveness models.Pharmacoeconomics 2000;17:479–500.
31] Briggs A, Sculpher M, Claxton K. Decision Modelling for Health EconomicEvaluation. New York: Oxford University Press, 2006.
32] Fenwick E, Byford S. A guide to cost-effectiveness acceptability curves.Br J Psychiatry 2005;187:106–8.
33] Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptabilitycurves—facts, fallacies, and frequently asked questions. Health Econ2004;13:405–15.
34] Arbeit RD, Maki D, Tally FP, et al. Daptomycin 98-01 and 99-01Investigators. The safety and efficacy of daptomycin for the treatmentof complicated skin and skin-structure infections. Clin Infect Dis 2004;38:1673–81.
35] Katz DE, Lindfield KC, Steenbergen JN, et al. A pilot study of high-dose shortduration daptomycin for the treatment of patients with complicated skinand skin structure infections caused by gram-positive bacteria. Int J ClinPract 2008;62:1455–64.
36] Pertel PE, Eisenstein BI, Link AS, et al. The efficacy and safety ofdaptomycin vs. vancomycin for the treatment of cellulitis anderysipelas. Int J Clin Pract 2009;63:368–75.
37] Stevens DL, Herr D, Lampiris H, et al. Linezolid versus vancomycin for thetreatment of methicillin-resistant Staphylococcus aureus infections. Clin InfectDis 2002;34:1481–90.
38] Weigelt J, Kaafarani HM, Itani KM, Swanson RN. Linezolid eradicatesMRSA better than vancomycin from surgical-site infections. Am J Surg2004;188:760–6.
39] Kohno S, Yamaguchi K, Aikawa N, et al. Linezolid versus vancomycin
for the treatment of infections caused by methicillin-resistantStaphylococcus aureus in Japan. J Antimicrob Chemother 2007;60:1361–9.40] Wilcox MH, Tack KJ, Bouza E, et al. Complicated skin and skin-structure infections and catheter-related bloodstream infections:noninferiority of linezolid in a phase 3 study. Clin Infect Dis 2009;48:203–12.
41] Wilson SE, Solomkin JS, Le V, Cammarata SK, Bruss JB. A severityscore for complicated skin and soft tissue infections derived fromphase III studies of linezolid. Am J Surg 2003;185:369–75.
42] Fejfarova V, Jirkovaska A, Skibova J, Petkov V. Pathogen resistance andother risk factors in the frequency of lower limb amputations inpatients with the diabetic foot syndrome. Vnitr Lek 2000;48:302–6.
43] Holmberg SD, Solomon SL, Blake PA. Health and economic impacts ofantimicrobial resistance. Rev Infect Dis 1987;9:1065–78.
44] Locksley RM, Cohen ML, Quinn TC, et al. Multiple antibiotic-resistantStaphylococcus aureus: introduction, transmission, and evolution ofnosocomial infection. Ann Intern Med 1982;97:317–24.
45] Fridkin SK, Hageman J, McDougal LK, et al. Epidemiological andmicrobiological characterization of infections caused by Staphylococcusaureus with reduced susceptibility to vancomycin, United States, 1997-2001.Clin Infect Dis 2003;36:429–39.
46] Owens RC, Lamp KC, Friedrich LV, Russo R. Postmarketing clinicalexperience in patients with skin and skin-structure infections treatedwith daptomycin. Am J Med 2007;120(Suppl. 10A):S6–S12.
47] Martone WJ, Lamp KC. Efficacy of daptomycin in complicated skin andskin-structure infections due to methicillin-sensitive and -resistantStaphylococcus aureus: results from the CORE Registry. Curr Med Res Opin2006;22:2337–43.
48] Katz DE, Martone WJ. Community-phenotype-methicillin-resistantStaphylococcus aureus infections: a retrospective chart review ofoutcomes after treatment with daptomycin. Clin Ther 2007;29:2440–7.
49] Slover CM, Rodvold KA, Danziger LH. Tigecycline: a novel broad-spectrumantimicrobial. Ann Pharmacother 2007;41:965–72.
50] Wilson SE, O’Riordan W, Hopkins A, et al. Telavancin versusvancomycin for the treatment of complicated skin and skin-structureinfections associated with surgical procedures. Am J Surg 2009;197:791–6.
51] Stryjewski ME, Graham DR, Wilson SE, et al. Telavancin versusvancomycin for the treatment of complicated skin and skin-structureinfections caused by gram-positive organisms. Clin Infect Dis 2008;46:1683–93.
52] Allington DR, Rivey MP. Quinupristin/dalfopristin: a therapeuticreview. Clin Ther 2001;23:24–44.
53] Anderson SD, Gums JG. Ceftobiprole. An extended-spectrum anti-methicillin-resistant Staphylococcus aureus cephalosporin. AnnPharmacother 2008;42:806–16.
54] Zhanel GG, Sniezek G, Schweizer F, et al. A novel broad-spectrumcephalosporin with activity against methicillin-resistant Staphylococcusaureus. Drugs 2009;69:809–31.
55] Krievins D, Brandt R, Hawser S, et al. Multicenter, randomized study ofthe efficacy and safety of intravenous iclaprim in complicated skinand skin structure infections. Antimicrob Agents Chemother 2009;53:2834–40.
56] Cooper NJ, Sutton AJ, Abrams KR, et al. Comprehensive decision
analytical modelling in economic evaluation: a Bayesian approach.Health Econ 2004;13:203–26.