CORONAVIRUS CHEAT SHEET - WordPress.com
13
CORONAVIRUS CHEAT SHEET Compiled by Deborah Passey, PhD Edited by Peggy Dial 1 COVID-19 Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a strain of coronavirus that causes the coronavirus disease 2019 (COVID-19), which is the respiratory illness responsible for the global pandemic. • Symptoms take 2-14 days to appear after exposure (i.e. incubation period): fever, cough, chills, shortness of breath, aches, runny nose, headache, fatigue, sore throat, loss of smell/taste, “covid toes”, or nausea, diarrhea, and loss of appetite. • COVID-19 infection can cause acute respiratory distress syndrome ( ARDS), pneumonia, and many other symptoms. Research suggests that COVID-19 may result in damage to the lungs, heart, digestive tract, and brain/neurological system. • The median time from illness onset to death is about 19 days, so the deaths we are seeing now are from infections that started almost three weeks ago HOW COVID-19 IS SPREAD The coronavirus is thought to spread from person to person through respiratory droplets produced when an infected person coughs or sneezes. These droplets can land in the mouths or noses of people who are nearby or possibly be inhaled into the lungs. • The SARS-CoV-2 virus can survive in the air and on surfaces: viable virus could be detected up to three hours later in the air, up to four hours on copper, up to 24 hours on cardboard and up to two to three days on plastic and stainless steel. • Spread is more likely when people are in close contact with one another (within about 6 feet). It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes.
Transcript of CORONAVIRUS CHEAT SHEET - WordPress.com
Edited by Peggy Dial
1
COVID-19
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a strain of coronavirus that causes the
coronavirus disease 2019 (COVID-19), which is the respiratory illness responsible for the global pandemic.
• Symptoms take 2-14 days to appear after exposure (i.e. incubation period): fever, cough, chills,
shortness of breath, aches, runny nose, headache, fatigue, sore throat, loss of smell/taste, “covid toes”,
or nausea, diarrhea, and loss of appetite.
• COVID-19 infection can cause acute respiratory distress syndrome (ARDS), pneumonia, and many
other symptoms. Research suggests that COVID-19 may result in damage to the lungs, heart, digestive
tract, and brain/neurological system.
• The median time from illness onset to death is about 19 days, so the deaths we are seeing now are
from infections that started almost three weeks ago
HOW COVID-19 IS SPREAD
The coronavirus is thought to spread from person to person through respiratory droplets produced when an
infected person coughs or sneezes. These droplets can land in the mouths or noses of people who are nearby
or possibly be inhaled into the lungs.
• The SARS-CoV-2 virus can survive in the air and on surfaces: viable virus could be detected up to
three hours later in the air, up to four hours on copper, up to 24 hours on cardboard and up to two to
three days on plastic and stainless steel.
• Spread is more likely when people are in close contact with one another (within about 6 feet). It may be
possible that a person can get COVID-19 by touching a surface or object that has the virus on it and
then touching their own mouth, nose, or possibly their eyes.
HOW A PERSON BECOMES INFECTED
Research suggests that airborne transmission is the primary mode of spread. Airborne transmission occurs
when viable virus particles are expelled by an infectious person and stay suspended in the air for several
hours.
1. A SARS-CoV-2 particle enters a person's nose or mouth and floats in the airway until it brushes against
a lung cell that has an ACE2 receptor on the surface.
2. The virus binds to that cell, slips inside and uses the cell's machinery to help make copies of itself.
They break out, leaving the cell for dead, and penetrate other cells.
3. Infected cells send out alarms to the immune system to try to neutralize or destroy the pathogens, but
the viruses can prevent or intercept the signals, buying time to replicate widely before a person shows
symptoms (see Scientific American guide to SARS-CoV-2).
https://www.avert.org/infographics/what-covid-19-and-how-it-spread
• Wash your hands and/or use alcohol-based hand sanitizer
• Wear a face mask when out in public
• Avoid crowded indoor areas, especially if masks are not required
• Stay healthy – eat plenty of fresh fruits/vegetables, get enough sleep, and drink plenty of fluids
• Make sure the people in your circle are also taking precautions
• Regularly clean and disinfect high touch surfaces in your workspace and home
• If you believe you were exposed to someone with COVID-19, isolate at home for 14 days and monitor for symptoms
• Avoid dining in, and opt for takeout or delivery from your favorite local restaurant or café
• For outdoor gatherings, wear a face mask and keep physical distance from others
Edited by Peggy Dial
COVID-19 TESTING
1. Molecular tests detect active infections. This is the test you want if you think you’ve been exposed to
the coronavirus or are exhibiting symptoms of COVID-19. The PCR antigen test involves sticking a 6-inch
swab deep into your nose to collect virus samples to test. The swab is inserted 3 inches or so to reach the
cavity where the nasal passages meet the pharynx. Positive results do not rule out bacterial infection or co-
infection with other viruses. But no test is 100% accurate all of the time. Some things that may affect the
test’s accuracy include:
A. You may have the virus, but the swab might not collect it from your nose or throat
B. The swab or mucus sample may be accidentally contaminated by the virus during collection or
analysis.
C. The nasal or throat swab may not be kept at the correct temperature before it can be analyzed.
D. The chemicals used to extract the virus genetic material and make copies of the virus DNA may not
work correctly.
2. Antigen tests provide results diagnosing an active coronavirus infection faster than molecular
tests, but antigen tests have a higher chance of missing an active infection. If an antigen test shows
a negative result indicating that you do not have an active coronavirus infection, your health care provider
may order a molecular test to confirm the result.
3. Antibody tests detect the presence of antibodies in the blood. Antibody tests may provide quick
results but should not be used to diagnose an active infection. Antibody tests only detect antibodies the
immune system develops in response to the virus, not the virus itself. It can take days to several weeks to
develop enough antibodies to be detected in a test. They can have 20-30% false-negatives.
Edited by Peggy Dial
VACCINE DEVELOPMENT
There are three main types of vaccines that are being developed by research groups around the world.
1. Whole-Pathogen Vaccines: Traditional vaccines consist of entire pathogens that have been killed or
weakened so that they cannot cause disease. Such whole-pathogen vaccines make the body have a
protective immune response. Many of the vaccines in clinical use today fall into this category.
2. Subunit Vaccines: Instead of the entire pathogen, subunit vaccines include only the components, or
antigens, that stimulate the immune system. Although this design can make vaccines safer and easier
to produce, it often requires the incorporation of adjuvants to elicit a strong protective immune response
because the antigens alone are not sufficient to induce adequate long-term immunity.
3. Nucleic Acid Vaccines: Another investigational approach to vaccination involves introducing genetic
material encoding the antigen against which an immune response is sought (e.g. mRNA vaccine). The
body’s own cells then use this genetic material to produce the antigens. Potential advantages of this
approach include the stimulation of broad long-term immune responses, excellent vaccine stability and
relative ease of large-scale vaccine manufacturing.
Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases (NIAID) has remained
consistent in his estimation of the timeline: 12 to 18 months from the start of the pandemic, or roughly the late
spring of 2021. It remains to be seen how fast vaccines can be manufactured and distributed once approved
for general use. Officials are also grappling with which Americans will get access first. So it’s unclear how long
a person would have to wait to get vaccinated.
HOW EFFECTIVE ARE MASKS?
Although they capture fewer particles than surgical and N95 masks, data shows that DIY masks made with a
single layer of cotton clothing or a tea towel can remove around 50-60% of virus-sized particles. Data shows
masks work incredibly well, and they’re also really cheap. The DIY masks using dish towel fabric captured
fewer particles than the surgical mask, but they still managed to capture 69% of virus-sized particles (read
more here). Thus, DIY masks still managed to capture particles while people were actually wearing them.
Based on this data, the researchers concluded that homemade masks would be better than nothing.
Edited by Peggy Dial
HOW TO USE AND HANDLE A MASK
1. HOW TO PUT ON A MASK
Any mask worn for day-to-day protection against COVID-19 is going to be imperfect, at least for now. Supplies
of N95 respirators—the most effective mask type—should find their way to those in daily close contact with
infected people. This requirement leaves the rest of us reusable cloth face coverings and single-use paper
surgical masks. (The latter are also in high demand for frontline folks, so if you’re looking to buy, try to acquire
fabric masks.) Information from Scientific American, images by Brown Bird Design
2. HOW TO WEAR A MASK
The mask should fit without gaps and fully cover your nose and mouth. Take special care to ensure a snug fit
across the bridge of the nose. If your mask doesn’t have a flexible wire built in, you may be able to MacGyver a
pipe cleaner, a tie for a coffee bag or another object into the role.
CORONAVIRUS CHEAT SHEET Compiled by Deborah Passey, PhD
Edited by Peggy Dial
3. HOW TO TAKE OFF A MASK
There is not a lot of data on how long a mask can be effectively worn. According to the World Health
Organization, a face covering should be replaced when you have breathed through it enough for it to become
damp. That effect is only likely to happen after several hours: For a trip to the grocery store, one mask will
probably do. If you will be out longer, bring a spare if possible.
4. HOW TO CLEAN A REUSABLE MASK
• Placing a cloth mask in a paper bag immediately after taking it off has two purposes: the container
isolates the mask from accidental handling, and the paper allows it to dry out. Before wearing the
covering again, let it sit in a warm spot—still in that paper bag—for two or three days (coronavirus is
undetectable on fabric after 2 days)
• You can pop a used mask straight into the washing machine with the regular laundry. A bag for
washing delicates will keep mask ties from making a knot of the whole load.
July 2020 10
• You can also WASH A MASK BY HAND: soak it in bleach suitable for disinfection for five minutes and then rinse
it thoroughly. Face coverings should be decontaminated after each use—so have a few on hand if you are going
out more often than your decontamination schedule allows.
COMMON MYTHS ABOUT COVID-19
Myth: The virus is just a mutated form of the common cold
No, it's not. Coronavirus is a large family of viruses that includes many different diseases. SARS-CoV-2 does
share similarities with other coronaviruses, four of which can cause the common cold. All five viruses have
spiky projections on their surfaces and utilize so-called spike proteins to infect host cells. However, the four
cold coronaviruses — named 229E, NL63, OC43 and HKU1 — all utilize humans as their primary hosts.
SARS-CoV-2 shares about 90% of its genetic material with coronaviruses that infect bats, which suggests that
the virus originated in bats and later hopped to humans.
Myth: The virus was probably made in a lab
No evidence suggests that the virus is man-made. SARS-CoV-2 closely resembles two other coronaviruses
that have triggered outbreaks in recent decades, SARS-CoV and MERS-CoV, and all three viruses seem to
have originated in bats. In short, the characteristics of SARS-CoV-2 fall in line with what we know about other
naturally occurring coronaviruses that made the jump from animals to people.
Myth: Pets can spread the new coronavirus
Although pets may contract COVID-19 in rare cases, there is no evidence they can spread it to people. There
have been a few reports of cats and dogs that became infected with COVID-19 after contact with their sick
owner. For example, in April, two pet cats in New York tested positive for COVID-19, and the owner of one of
these cats was confirmed to have COVID-19 before the cat showed symptoms. Even if pets do occasionally
become infected, the Centers for Disease Control and Prevention (CDC) says there is no evidence that they
are playing a significant role in the spread of the virus. And so far, there have been no confirmed reports of
people contracting the disease from pets.
Myth: Kids can't catch the coronavirus
Children can definitely catch COVID-19, although reports of serious illness in children are rare. A CDC study of
more than 1.3 million cases of COVID-19 in the U.S. from January through May found that the rate of
confirmed infections in children under age 9 was 52 cases per 100,000 people in that population of children;
that’s compared with an average of 400 cases (of any age) per 100,000 people in the U.S. population as a
whole.
Another CDC study found that among 52,000 reported COVID-19 deaths from February through May, just 16
deaths were reported in people under age 18. Still, not all children are spared from COVID-19. In rare cases,
children with a current or previous COVID-19 infection have developed so-called multisystem inflammatory
syndrome (MIS-C). Symptoms of this syndrome can vary, but patients seem to have symptoms similar to those
found in two rare conditions: toxic shock syndrome and Kawasaki disease, Live Science previously reported.
Toxic shock syndrome is a life-threatening condition that's caused by toxins produced by certain types of
bacteria; Kawasaki disease is a childhood illness that causes inflammation in blood vessel walls, and in serious
cases can cause heart damage.
Myth: The coronavirus is less deadly than the flu
Edited by Peggy Dial
11
Though the death rate for COVID-19 is unclear, almost all credible research suggests it is much higher than
that of the seasonal flu, which has a death rate of around 0.1% in the U.S. Among reported COVID-19 cases in
the U.S., about 4% have died, according to data from Johns Hopkins University. This is what's known as the
case fatality rate, which is determined by dividing the number of deaths by the total number of confirmed
cases. But the case fatality rate is limited for a few reasons. First, not everyone with COVID-19 is being
diagnosed with the disease — this is in part due to testing limitations in the U.S. and the fact that people who
experience mild or moderate symptoms may not seek out testing. As the number of confirmed cases goes up,
the fatality rate may decrease. Many studies estimate that around 0.5% to 1% of people infected with COVID-
19 will die from the disease, according to Nature News. Even a death rate around 1% is still 10 times higher
than that of the flu.
Myth: Vitamin C supplements will stop you from catching COVID-19
Researchers have yet to find any evidence that vitamin C supplements can render people immune to COVID-
19 infection. In fact, for most people, taking extra vitamin C does not even ward off the common cold, though it
may shorten the duration of a cold if you catch one. That said, vitamin C serves essential roles in the human
body and supports normal immune function. As an antioxidant, the vitamin neutralizes charged particles called
free radicals that can damage tissues in the body. It also helps the body synthesize hormones, build collagen
and seal off vulnerable connective tissue against pathogens. So yes, vitamin C should absolutely be included
in your daily diet if you want to maintain a healthy immune system. But megadosing on supplements is unlikely
to lower your risk of catching COVID-19, and may at most give you a "modest" advantage against the virus,
should you become infected. No evidence suggests that other so-called immune-boosting supplements —
such as zinc, green tea or echinacea — help to prevent COVID-19, either.
Myth: Drinking bleach or other disinfectants can protect you from COVID-19
You absolutely should not drink bleach or other household disinfectants, and you should also not spray them
on your body. These substances are poisonous if ingested, and they can also cause damage to the skin and
eyes, according to the World Health Organization. When ingested, sodium hypochlorite (household bleach)
can cause what is called "liquefactive necrosis," or a process that results in the transformation of tissue into a
liquid viscous mass, Live Science previously reported. The bleach can also damage cells as the sodium reacts
with proteins and fats in a person's tissues in a process called saponification (soap), medical doctors reported
in 2018 in a publication by the Emergency Medicine Residents' Association.
Myth: Drinking alcohol and eating garlic can protect you from COVID-19
Consuming certain foods, such as alcohol or garlic, will not protect you from the new coronavirus. Although
alcohol-based hand sanitizers work to disinfect your skin, alcohol does not have this effect on your body when
it is ingested, according to WHO. Indeed, heavy use of alcohol can actually weaken your immune system and
reduce your body's ability to cope with infectious diseases. And although garlic may have some antimicrobial
properties, there is no evidence that it can protect against COVID-19, WHO says.
Myth: 5G networks can spread the new coronavirus
Viruses, including SARS-CoV-2, cannot travel on or transmit through radio waves or mobile networks such
as 5G networks. The new coronavirus is spread mainly through respiratory droplets that are expelled when an
infected person coughs, sneezes or speaks, as well as through contaminated surfaces. WHO also notes that
COVID-19 has been spreading in countries that do not have 5G mobile networks.
Myth: Exposure to high temperatures prevents COVID-19
Exposing yourself to the sun or warm temperatures will not protect you against COVID-19, according to WHO.
You can still catch the disease no matter how hot it is — indeed, the virus is spreading even in areas with very
hot weather, such as Arizona. Taking a hot bath will also not prevent COVID-19, WHO says.
Myth: Wearing masks can cause CO2 poisoning
Wearing medical masks for long periods may be uncomfortable for some, but it does not cause oxygen
deficiency or carbon dioxide (CO2) intoxication (when too much CO2 builds up in the bloodstream), according
to WHO. The same applies for N95 masks and cloth face coverings, according to Healthline. "Rebreathing tiny
amounts of CO2 from wearing either properly fitted N95 respirators or more loosely fitted cloth or surgical
masks is of no concern for the vast, vast majority of people," Darrell Spurlock Jr., the director of the Leadership
Center for Nursing Education Research at Widener University in Pennsylvania, told Healthline. "The 'dose' of
CO2 we might rebreathe while masking is quickly and easily eliminated by both the respiratory and metabolic
systems in the body."
Myth: Hydroxychloroquine cures COVID-19
US President Donald Trump used Twitter to spread footage of a doctor who claims a combination of medicines
including hydroxychloroquine will cure COVID-19. But there is currently no cure for the disease caused by the
novel coronavirus, and the false information the video contains has left social media companies scrambling to
remove it.
Myth: You can get a face mask exemption card so you don’t need to wear a mask.
Fake cards and flyers, claiming that the bearer is exempt from mask-wearing regulations, have shown up in
some areas. The cards, which some people have purchased online, may have official-looking logos or
government insignias on them. They claim that the person carrying them has a physical or mental condition
covered by the Americans with Disabilities Act (ADA) that makes them unable to wear a face mask or covering.
The United States Department of Justice has issued a statement about these fake mask exemptions,
explaining that these cards and flyers are fraudulent.
Myth: Rinsing your nose with nasal saline will prevent the virus
There is some limited evidence that regularly rinsing your nose with saline lowers the duration of a common
cold, according to WHO. But rinsing your nose has not been proven to eliminate the coronavirus or any other
respiratory infection.
Myth: Ultraviolet disinfection lamps kill the virus on your skin.
According to WHO, the best way to clean your hands is by washing them with soap and water. The ultraviolet
light will irritate your skin.
Myth: The virus only affects the elderly.
Edited by Peggy Dial
13
People who are elderly or have compromised immune systems are at a greater risk for severe illness if they
contract the virus, according to WHO. But anyone of any age can contract and spread the virus to others,
which is why it's important for everyone to take precautions and frequently wash their hands.
Myth: Ordering or buying products shipped from China will make a person sick.
There is no evidence to show that there has been transmission through packages. Officials say because of the
poor survivability of these coronaviruses on surfaces, there is likely very low risk of spread from products or
packaging that are shipped over a period of days or weeks at ambient temperatures.
Myth: I’m healthy, so I don’t need to practice social distancing.
While you may be healthy, you could still be a carrier of the virus. You also increase your risk of getting
infected and then spreading it to others who may be at a higher risk for severe illness. While you may not be
experiencing symptoms, it's important to practice social distancing to protect not only yourself but the people
around you.
Myth: The virus cannot survive in warm weather.
While many cold/flu viruses tend to drop out during the warmer months, there is no research to suggest that
this will happen with COVID-19. Warmer areas around the world are experiencing an outbreak of COVID-19,
so no one knows at this time if warmer weather will kill the virus.
Myths Q&A from:
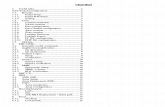
The best way to protect yourself
COVID-19 testiNG
VACCINE DEVELOPMENT
Common Myths About COVID-19
1
COVID-19
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a strain of coronavirus that causes the
coronavirus disease 2019 (COVID-19), which is the respiratory illness responsible for the global pandemic.
• Symptoms take 2-14 days to appear after exposure (i.e. incubation period): fever, cough, chills,
shortness of breath, aches, runny nose, headache, fatigue, sore throat, loss of smell/taste, “covid toes”,
or nausea, diarrhea, and loss of appetite.
• COVID-19 infection can cause acute respiratory distress syndrome (ARDS), pneumonia, and many
other symptoms. Research suggests that COVID-19 may result in damage to the lungs, heart, digestive
tract, and brain/neurological system.
• The median time from illness onset to death is about 19 days, so the deaths we are seeing now are
from infections that started almost three weeks ago
HOW COVID-19 IS SPREAD
The coronavirus is thought to spread from person to person through respiratory droplets produced when an
infected person coughs or sneezes. These droplets can land in the mouths or noses of people who are nearby
or possibly be inhaled into the lungs.
• The SARS-CoV-2 virus can survive in the air and on surfaces: viable virus could be detected up to
three hours later in the air, up to four hours on copper, up to 24 hours on cardboard and up to two to
three days on plastic and stainless steel.
• Spread is more likely when people are in close contact with one another (within about 6 feet). It may be
possible that a person can get COVID-19 by touching a surface or object that has the virus on it and
then touching their own mouth, nose, or possibly their eyes.
HOW A PERSON BECOMES INFECTED
Research suggests that airborne transmission is the primary mode of spread. Airborne transmission occurs
when viable virus particles are expelled by an infectious person and stay suspended in the air for several
hours.
1. A SARS-CoV-2 particle enters a person's nose or mouth and floats in the airway until it brushes against
a lung cell that has an ACE2 receptor on the surface.
2. The virus binds to that cell, slips inside and uses the cell's machinery to help make copies of itself.
They break out, leaving the cell for dead, and penetrate other cells.
3. Infected cells send out alarms to the immune system to try to neutralize or destroy the pathogens, but
the viruses can prevent or intercept the signals, buying time to replicate widely before a person shows
symptoms (see Scientific American guide to SARS-CoV-2).
https://www.avert.org/infographics/what-covid-19-and-how-it-spread
• Wash your hands and/or use alcohol-based hand sanitizer
• Wear a face mask when out in public
• Avoid crowded indoor areas, especially if masks are not required
• Stay healthy – eat plenty of fresh fruits/vegetables, get enough sleep, and drink plenty of fluids
• Make sure the people in your circle are also taking precautions
• Regularly clean and disinfect high touch surfaces in your workspace and home
• If you believe you were exposed to someone with COVID-19, isolate at home for 14 days and monitor for symptoms
• Avoid dining in, and opt for takeout or delivery from your favorite local restaurant or café
• For outdoor gatherings, wear a face mask and keep physical distance from others
Edited by Peggy Dial
COVID-19 TESTING
1. Molecular tests detect active infections. This is the test you want if you think you’ve been exposed to
the coronavirus or are exhibiting symptoms of COVID-19. The PCR antigen test involves sticking a 6-inch
swab deep into your nose to collect virus samples to test. The swab is inserted 3 inches or so to reach the
cavity where the nasal passages meet the pharynx. Positive results do not rule out bacterial infection or co-
infection with other viruses. But no test is 100% accurate all of the time. Some things that may affect the
test’s accuracy include:
A. You may have the virus, but the swab might not collect it from your nose or throat
B. The swab or mucus sample may be accidentally contaminated by the virus during collection or
analysis.
C. The nasal or throat swab may not be kept at the correct temperature before it can be analyzed.
D. The chemicals used to extract the virus genetic material and make copies of the virus DNA may not
work correctly.
2. Antigen tests provide results diagnosing an active coronavirus infection faster than molecular
tests, but antigen tests have a higher chance of missing an active infection. If an antigen test shows
a negative result indicating that you do not have an active coronavirus infection, your health care provider
may order a molecular test to confirm the result.
3. Antibody tests detect the presence of antibodies in the blood. Antibody tests may provide quick
results but should not be used to diagnose an active infection. Antibody tests only detect antibodies the
immune system develops in response to the virus, not the virus itself. It can take days to several weeks to
develop enough antibodies to be detected in a test. They can have 20-30% false-negatives.
Edited by Peggy Dial
VACCINE DEVELOPMENT
There are three main types of vaccines that are being developed by research groups around the world.
1. Whole-Pathogen Vaccines: Traditional vaccines consist of entire pathogens that have been killed or
weakened so that they cannot cause disease. Such whole-pathogen vaccines make the body have a
protective immune response. Many of the vaccines in clinical use today fall into this category.
2. Subunit Vaccines: Instead of the entire pathogen, subunit vaccines include only the components, or
antigens, that stimulate the immune system. Although this design can make vaccines safer and easier
to produce, it often requires the incorporation of adjuvants to elicit a strong protective immune response
because the antigens alone are not sufficient to induce adequate long-term immunity.
3. Nucleic Acid Vaccines: Another investigational approach to vaccination involves introducing genetic
material encoding the antigen against which an immune response is sought (e.g. mRNA vaccine). The
body’s own cells then use this genetic material to produce the antigens. Potential advantages of this
approach include the stimulation of broad long-term immune responses, excellent vaccine stability and
relative ease of large-scale vaccine manufacturing.
Anthony Fauci, Director of the National Institute of Allergy and Infectious Diseases (NIAID) has remained
consistent in his estimation of the timeline: 12 to 18 months from the start of the pandemic, or roughly the late
spring of 2021. It remains to be seen how fast vaccines can be manufactured and distributed once approved
for general use. Officials are also grappling with which Americans will get access first. So it’s unclear how long
a person would have to wait to get vaccinated.
HOW EFFECTIVE ARE MASKS?
Although they capture fewer particles than surgical and N95 masks, data shows that DIY masks made with a
single layer of cotton clothing or a tea towel can remove around 50-60% of virus-sized particles. Data shows
masks work incredibly well, and they’re also really cheap. The DIY masks using dish towel fabric captured
fewer particles than the surgical mask, but they still managed to capture 69% of virus-sized particles (read
more here). Thus, DIY masks still managed to capture particles while people were actually wearing them.
Based on this data, the researchers concluded that homemade masks would be better than nothing.
Edited by Peggy Dial
HOW TO USE AND HANDLE A MASK
1. HOW TO PUT ON A MASK
Any mask worn for day-to-day protection against COVID-19 is going to be imperfect, at least for now. Supplies
of N95 respirators—the most effective mask type—should find their way to those in daily close contact with
infected people. This requirement leaves the rest of us reusable cloth face coverings and single-use paper
surgical masks. (The latter are also in high demand for frontline folks, so if you’re looking to buy, try to acquire
fabric masks.) Information from Scientific American, images by Brown Bird Design
2. HOW TO WEAR A MASK
The mask should fit without gaps and fully cover your nose and mouth. Take special care to ensure a snug fit
across the bridge of the nose. If your mask doesn’t have a flexible wire built in, you may be able to MacGyver a
pipe cleaner, a tie for a coffee bag or another object into the role.
CORONAVIRUS CHEAT SHEET Compiled by Deborah Passey, PhD
Edited by Peggy Dial
3. HOW TO TAKE OFF A MASK
There is not a lot of data on how long a mask can be effectively worn. According to the World Health
Organization, a face covering should be replaced when you have breathed through it enough for it to become
damp. That effect is only likely to happen after several hours: For a trip to the grocery store, one mask will
probably do. If you will be out longer, bring a spare if possible.
4. HOW TO CLEAN A REUSABLE MASK
• Placing a cloth mask in a paper bag immediately after taking it off has two purposes: the container
isolates the mask from accidental handling, and the paper allows it to dry out. Before wearing the
covering again, let it sit in a warm spot—still in that paper bag—for two or three days (coronavirus is
undetectable on fabric after 2 days)
• You can pop a used mask straight into the washing machine with the regular laundry. A bag for
washing delicates will keep mask ties from making a knot of the whole load.
July 2020 10
• You can also WASH A MASK BY HAND: soak it in bleach suitable for disinfection for five minutes and then rinse
it thoroughly. Face coverings should be decontaminated after each use—so have a few on hand if you are going
out more often than your decontamination schedule allows.
COMMON MYTHS ABOUT COVID-19
Myth: The virus is just a mutated form of the common cold
No, it's not. Coronavirus is a large family of viruses that includes many different diseases. SARS-CoV-2 does
share similarities with other coronaviruses, four of which can cause the common cold. All five viruses have
spiky projections on their surfaces and utilize so-called spike proteins to infect host cells. However, the four
cold coronaviruses — named 229E, NL63, OC43 and HKU1 — all utilize humans as their primary hosts.
SARS-CoV-2 shares about 90% of its genetic material with coronaviruses that infect bats, which suggests that
the virus originated in bats and later hopped to humans.
Myth: The virus was probably made in a lab
No evidence suggests that the virus is man-made. SARS-CoV-2 closely resembles two other coronaviruses
that have triggered outbreaks in recent decades, SARS-CoV and MERS-CoV, and all three viruses seem to
have originated in bats. In short, the characteristics of SARS-CoV-2 fall in line with what we know about other
naturally occurring coronaviruses that made the jump from animals to people.
Myth: Pets can spread the new coronavirus
Although pets may contract COVID-19 in rare cases, there is no evidence they can spread it to people. There
have been a few reports of cats and dogs that became infected with COVID-19 after contact with their sick
owner. For example, in April, two pet cats in New York tested positive for COVID-19, and the owner of one of
these cats was confirmed to have COVID-19 before the cat showed symptoms. Even if pets do occasionally
become infected, the Centers for Disease Control and Prevention (CDC) says there is no evidence that they
are playing a significant role in the spread of the virus. And so far, there have been no confirmed reports of
people contracting the disease from pets.
Myth: Kids can't catch the coronavirus
Children can definitely catch COVID-19, although reports of serious illness in children are rare. A CDC study of
more than 1.3 million cases of COVID-19 in the U.S. from January through May found that the rate of
confirmed infections in children under age 9 was 52 cases per 100,000 people in that population of children;
that’s compared with an average of 400 cases (of any age) per 100,000 people in the U.S. population as a
whole.
Another CDC study found that among 52,000 reported COVID-19 deaths from February through May, just 16
deaths were reported in people under age 18. Still, not all children are spared from COVID-19. In rare cases,
children with a current or previous COVID-19 infection have developed so-called multisystem inflammatory
syndrome (MIS-C). Symptoms of this syndrome can vary, but patients seem to have symptoms similar to those
found in two rare conditions: toxic shock syndrome and Kawasaki disease, Live Science previously reported.
Toxic shock syndrome is a life-threatening condition that's caused by toxins produced by certain types of
bacteria; Kawasaki disease is a childhood illness that causes inflammation in blood vessel walls, and in serious
cases can cause heart damage.
Myth: The coronavirus is less deadly than the flu
Edited by Peggy Dial
11
Though the death rate for COVID-19 is unclear, almost all credible research suggests it is much higher than
that of the seasonal flu, which has a death rate of around 0.1% in the U.S. Among reported COVID-19 cases in
the U.S., about 4% have died, according to data from Johns Hopkins University. This is what's known as the
case fatality rate, which is determined by dividing the number of deaths by the total number of confirmed
cases. But the case fatality rate is limited for a few reasons. First, not everyone with COVID-19 is being
diagnosed with the disease — this is in part due to testing limitations in the U.S. and the fact that people who
experience mild or moderate symptoms may not seek out testing. As the number of confirmed cases goes up,
the fatality rate may decrease. Many studies estimate that around 0.5% to 1% of people infected with COVID-
19 will die from the disease, according to Nature News. Even a death rate around 1% is still 10 times higher
than that of the flu.
Myth: Vitamin C supplements will stop you from catching COVID-19
Researchers have yet to find any evidence that vitamin C supplements can render people immune to COVID-
19 infection. In fact, for most people, taking extra vitamin C does not even ward off the common cold, though it
may shorten the duration of a cold if you catch one. That said, vitamin C serves essential roles in the human
body and supports normal immune function. As an antioxidant, the vitamin neutralizes charged particles called
free radicals that can damage tissues in the body. It also helps the body synthesize hormones, build collagen
and seal off vulnerable connective tissue against pathogens. So yes, vitamin C should absolutely be included
in your daily diet if you want to maintain a healthy immune system. But megadosing on supplements is unlikely
to lower your risk of catching COVID-19, and may at most give you a "modest" advantage against the virus,
should you become infected. No evidence suggests that other so-called immune-boosting supplements —
such as zinc, green tea or echinacea — help to prevent COVID-19, either.
Myth: Drinking bleach or other disinfectants can protect you from COVID-19
You absolutely should not drink bleach or other household disinfectants, and you should also not spray them
on your body. These substances are poisonous if ingested, and they can also cause damage to the skin and
eyes, according to the World Health Organization. When ingested, sodium hypochlorite (household bleach)
can cause what is called "liquefactive necrosis," or a process that results in the transformation of tissue into a
liquid viscous mass, Live Science previously reported. The bleach can also damage cells as the sodium reacts
with proteins and fats in a person's tissues in a process called saponification (soap), medical doctors reported
in 2018 in a publication by the Emergency Medicine Residents' Association.
Myth: Drinking alcohol and eating garlic can protect you from COVID-19
Consuming certain foods, such as alcohol or garlic, will not protect you from the new coronavirus. Although
alcohol-based hand sanitizers work to disinfect your skin, alcohol does not have this effect on your body when
it is ingested, according to WHO. Indeed, heavy use of alcohol can actually weaken your immune system and
reduce your body's ability to cope with infectious diseases. And although garlic may have some antimicrobial
properties, there is no evidence that it can protect against COVID-19, WHO says.
Myth: 5G networks can spread the new coronavirus
Viruses, including SARS-CoV-2, cannot travel on or transmit through radio waves or mobile networks such
as 5G networks. The new coronavirus is spread mainly through respiratory droplets that are expelled when an
infected person coughs, sneezes or speaks, as well as through contaminated surfaces. WHO also notes that
COVID-19 has been spreading in countries that do not have 5G mobile networks.
Myth: Exposure to high temperatures prevents COVID-19
Exposing yourself to the sun or warm temperatures will not protect you against COVID-19, according to WHO.
You can still catch the disease no matter how hot it is — indeed, the virus is spreading even in areas with very
hot weather, such as Arizona. Taking a hot bath will also not prevent COVID-19, WHO says.
Myth: Wearing masks can cause CO2 poisoning
Wearing medical masks for long periods may be uncomfortable for some, but it does not cause oxygen
deficiency or carbon dioxide (CO2) intoxication (when too much CO2 builds up in the bloodstream), according
to WHO. The same applies for N95 masks and cloth face coverings, according to Healthline. "Rebreathing tiny
amounts of CO2 from wearing either properly fitted N95 respirators or more loosely fitted cloth or surgical
masks is of no concern for the vast, vast majority of people," Darrell Spurlock Jr., the director of the Leadership
Center for Nursing Education Research at Widener University in Pennsylvania, told Healthline. "The 'dose' of
CO2 we might rebreathe while masking is quickly and easily eliminated by both the respiratory and metabolic
systems in the body."
Myth: Hydroxychloroquine cures COVID-19
US President Donald Trump used Twitter to spread footage of a doctor who claims a combination of medicines
including hydroxychloroquine will cure COVID-19. But there is currently no cure for the disease caused by the
novel coronavirus, and the false information the video contains has left social media companies scrambling to
remove it.
Myth: You can get a face mask exemption card so you don’t need to wear a mask.
Fake cards and flyers, claiming that the bearer is exempt from mask-wearing regulations, have shown up in
some areas. The cards, which some people have purchased online, may have official-looking logos or
government insignias on them. They claim that the person carrying them has a physical or mental condition
covered by the Americans with Disabilities Act (ADA) that makes them unable to wear a face mask or covering.
The United States Department of Justice has issued a statement about these fake mask exemptions,
explaining that these cards and flyers are fraudulent.
Myth: Rinsing your nose with nasal saline will prevent the virus
There is some limited evidence that regularly rinsing your nose with saline lowers the duration of a common
cold, according to WHO. But rinsing your nose has not been proven to eliminate the coronavirus or any other
respiratory infection.
Myth: Ultraviolet disinfection lamps kill the virus on your skin.
According to WHO, the best way to clean your hands is by washing them with soap and water. The ultraviolet
light will irritate your skin.
Myth: The virus only affects the elderly.
Edited by Peggy Dial
13
People who are elderly or have compromised immune systems are at a greater risk for severe illness if they
contract the virus, according to WHO. But anyone of any age can contract and spread the virus to others,
which is why it's important for everyone to take precautions and frequently wash their hands.
Myth: Ordering or buying products shipped from China will make a person sick.
There is no evidence to show that there has been transmission through packages. Officials say because of the
poor survivability of these coronaviruses on surfaces, there is likely very low risk of spread from products or
packaging that are shipped over a period of days or weeks at ambient temperatures.
Myth: I’m healthy, so I don’t need to practice social distancing.
While you may be healthy, you could still be a carrier of the virus. You also increase your risk of getting
infected and then spreading it to others who may be at a higher risk for severe illness. While you may not be
experiencing symptoms, it's important to practice social distancing to protect not only yourself but the people
around you.
Myth: The virus cannot survive in warm weather.
While many cold/flu viruses tend to drop out during the warmer months, there is no research to suggest that
this will happen with COVID-19. Warmer areas around the world are experiencing an outbreak of COVID-19,
so no one knows at this time if warmer weather will kill the virus.
Myths Q&A from:
The best way to protect yourself
COVID-19 testiNG
VACCINE DEVELOPMENT
Common Myths About COVID-19