Contact Lens & Anterior Eye
Transcript of Contact Lens & Anterior Eye

Sk
Ba
b
a
ARRA
KSPIKR
1
cpaeoko
trs
Hf
(
1h
Contact Lens & Anterior Eye 37 (2014) 196–202
Contents lists available at ScienceDirect
Contact Lens & Anterior Eye
jou rna l h om epa ge : w ww.e l sev ier .com/ locate /c lae
cleral contact lenses for visual rehabilitation after penetratingeratoplasty: Long term outcomes
oris Severinskya,∗, Shmuel Behrmanb, Joseph Frucht-Perya, Abraham Solomona
Department of Ophthalmology, Hadassah University Hospital, Jerusalem, IsraelMicrolens Ltd., Tel-Aviv, Israel
r t i c l e i n f o
rticle history:eceived 29 May 2013eceived in revised form 31 August 2013ccepted 4 November 2013
eywords:cleral contact lensesenetrating keratoplastyrregular astigmatismeratoconusecurrent ectasia
a b s t r a c t
Purpose: To evaluate the success rate of highly gas permeable scleral contact lenses (SCL) for visualrehabilitation after penetrating keratoplasty (PK), over a period of up to 9 years.Methods: A total database of 31 consecutive patient fitted with SCL between January 2004 and December2009 was retrospectively reviewed. Demographic data, etiology prior to lens fitting, visual outcomes,follow up time and complications were analyzed.Results: All eyes were fitted due to inadequate spectacle-corrected vision after successful penetratingkeratoplasty or failure of other contact lens modalities. Out of 31 patients fitted, 28 (33 eyes) continue towear SCL for periods between 0.5 and 8.8 years. The mean duration of follow-up after contact lens fittingwas 5.2 ± 2.2 years. The mean age of corneal graft was 17.6 ± 11.4 years (range 4.3–42), and the meaninterval between PK and initial contact lens fitting was 12.2 ± 10.7 years (range 0.7–36.0). The averagesteepest keratometry of our cohort was 55.0 ± 7.5 diopter (D) and the refractive astigmatism was 8.0 ± 4.4D. The mean contact lens corrected visual acuity (BCVAcl) was 0.78 ± 0.25 (range 0.3–1.2). Twenty-three
(82%) patients achieved a functional vision of 0.5 or more.During the studied period, ten (30.0%) eyes presented at least one graft rejection episode and two eyes(6%) had an episode of microbial keratitis. Corneal transplants of 20 years or more show a higher rate ofrefits due to ectasia recurrence.Conclusions: Scleral lenses should be considered as lens of choice in eyes with complex corneal geometry,as besides visual rehabilitation, their use may delay or prevent further surgical involvement.
Briti
© 2013. Introduction
Penetrating keratoplasty (PK) or corneal graft is a surgical pro-edure which has been used for more than a hundred years. Itrovides vision restoration for a variety of corneal dystrophiesnd deformities. Indications for PK may include corneal ectasia,specially keratoconus (KC), corneal scarring, secondary to traumar infection, various forms of keratopathy (pseudophakic bullouseratophaty and herpes simplex keratitis) and congenital cornealpacities (Peter’s anomaly, aniridia).
The main goal of penetrating keratoplasty is visual rehabilita-
ion. However the procedure itself frequently causes abnormality ofefraction, such as high degrees of astigmatism, irregularity or ani-ometropia which prevent the achievement of satisfactory vision∗ Corresponding author at: Department of Ophthalmology, Hadassah Universityospital, POB 12000, Jerusalem 91120, Israel. Tel.: +972 545385865;
ax: +972 775301367.E-mail addresses: [email protected], [email protected]
B. Severinsky).
367-0484/$ – see front matter © 2013 British Contact Lens Association. Published by Elsttp://dx.doi.org/10.1016/j.clae.2013.11.001
sh Contact Lens Association. Published by Elsevier Ltd. All rights reserved.
and create a primary optical challenge [1]. New developments havetaken place with the introduction of the deep anterior lamellarkeratoplasty (DALK) procedure. As an extraocular procedure, DALKhas important theoretic safety advantages in terms of the cornealendothelium survival [2]. Numerous studies indicate that the visualrehabilitation and refractive outcomes of DALK technique are sim-ilar to PK [3,4], however improved graft survival in DALK has yet tobe demonstrated [2].
Spectacles are often impractical to rehabilitate the visual acu-ity (VA) of the grafted eye. In those cases, contact lenses may berequired in order to improve vision and achieve binocularity. How-ever, not all contact lens modalities can be fitted successfully afterPK. The complex shape of the post-graft cornea, frequently fea-tured by the centrally flat and peripherally steep pattern and/orover all asymmetry (i.e. irregular astigmatism) is a challenge to fit.Rigid gas permeable (RGP) contact lenses are commonly used afterPK procedure [5,6]. Despite being considered as “gold standard of
irregular cornea visual rehabilitation” [7] RGP contact lenses maynot always be appropriate. Variable curvatures both centrally andat the donor–host junction [8] are often the reason for rigid lensdecentration or even complete ejection from the cornea. Rigidevier Ltd. All rights reserved.

s & A
lsrTictifii
uaoisvoplep
rcmwtdtmtsmolr[
I(dinos2a
fvow
2
SJtc
Dta
B. Severinsky et al. / Contact Len
ens mechanical interaction with irregular or highly toroid cornealurface [9,10], leads to corneal micro-trauma, epithelial and ante-ior stroma disruptions, and consecutive ocular inflammation [11].he use of hydrogel contact lenses after PK is quite limited due tonability of such lens to neutralize irregular or highly astigmaticorneal surface. Increased lens thickness required for optical neu-ralization of irregular cornea or when high astigmatic correction isncorporated into the lens, leads to reduced gas transmission. Insuf-cient oxygen supply may cause corneal ischemia and, therefore,
ncrease the risk of graft rejection [12].In recent years scleral contact lenses (SCL) have gained pop-
larity among contact lens practitioners worldwide. These lensesre used to improve visual functions in patients with keratoconusr other forms of corneal irregularity and to provide relief and anmprovement of corneal integrity in eyes with refractory ocularurface disease [13–15,25,26]. Indications for scleral lens fittingary among authors, but the consensus amongst all is correctionf high or irregular corneal astigmatism after penetrating kerato-lasty [13–15,25]. The first description of fitting scleral contact
enses after PK procedure goes back to the early sixties [16], how-ver, since then, new techniques in the manufacture of rigid gasermeable scleral lenses have been developed [21–24].
Until the last decade of the past century, the advantages of scle-al contact lenses could not be fully realized, because of chronicorneal hypoxia attributed to low gas permeability of polymethylethacrylate (PMMA) and other materials from which the lensesere made [17–19]. The development of rigid gas-permeable plas-
ics greatly reduced the hypoxic complications associated withaily wear corneal lenses and added a new dimension to the poten-ial of scleral lenses for the visual rehabilitation of patients with
arkedly irregular corneas. Ezekiel [20] was the first to describehe use of preformed fenestrated, silicone/acrylate gas permeablecleral contact lenses in fitting patients with keratoconus, severeyopia, aphakia, and corneal scarring. More recent reports based
n a large groups of patients describe an expanding role for scleralenses with respect to corneal ectasia and post keratoplasty visualehabilitation [14,15,25], together with high patient satisfaction26].
A variety of scleral lens designs have sprung up recently.n addition to existing full size scleral lenses, corneo-scleral12.5–15.0 mm in diameter), and mini-scleral (15.0–18.0 mm) [27],esigns were developed. Mini scleral lenses, as a rule, exhibit min-
mal corneal clearance with moderate areas of scleral bearing. Thearrow haptics on mini-SCL provides a smaller area of landingver the sclera, a fact that frequently leads to excessive compres-ion near the limbus. Advantages of full scleral design, 18.1 mm to4+ mm, are complete corneal clearance and broader area of sclerallignment, the second in turn lessens a limbal compression.
In this article we describe our experience with 18.50 mm, pre-ormed gas permeable scleral contact lenses after PK procedure,isual outcomes, and safety associated with their use. To the bestf our knowledge, this study has the longest follow up of patientsith corneal transplant fitted with scleral contact lenses.
. Methods
Clinical data from the records of 31 patients (36 eyes), fitted withCL for visual rehabilitation after PK, in the 6-year period betweenanuary 2004 and December 2009, were retrospectively analyzedo determine the visual outcomes and safety of its use. The dataollection was made from December 2012 to January 2013.
All patients were referred to the contact lens clinic in theepartment of Ophthalmology, Hadassah University Hospital, due
o failure of spectacles, RGP or soft contact lenses to correct visiondequately, or when fitting of such lenses was contraindicated and
nterior Eye 37 (2014) 196–202 197
other surgical options were undesirable. Only eyes fitted with SCLthree or more years prior to data collection were included in thestudy. Collected demographic data includes patient’s age, sex, ini-tial diagnosis, corneal graft age, follow-up period, and indicationsfor fitting. Best manifest refraction, at consultation, and contactlens, at dispensing, visual acuities (BCVArefr and BCVAcl respec-tively) were recorded in the decimal equivalent of the Snellen ratio.Patients manifest refraction in form of spherical component (Sph),and refractive astigmatism (Cyl), steepest keratometry (Kmax) fromcorneal topography measurements (Eye Sys Topography System3000, EyeSys Vision, Inc., Houston, TX) obtained at the time ofthe initial visit were recorded. Contact lens induced complications,episodes of rejection and the number of refits during contact lensuse were evaluated. A statistical analysis was conducted by usingSPSS software (SPSS Inc., Chicago, IL), with the significance level setat p < 0.01.
2.1. SCL features
The lenses fitted were lathe-cut preformed, non-fenestrated,scleral contact lenses with an overall diameter between 18.50and 19.00 mm (Microlens Ltd., Tel Aviv, Israel). The average cen-ter thickness of the lenses was 0.30 mm. All lenses were preparedfrom highly gas permeable polymer: Optimum Extreme (Conta-mac Ltd., Saffron Walden, UK) having a permeability Dk value of125× 10–11 cm 2 mL O2/s mL mm Hg (International Organizationfor Standardization [ISO]/Fatt). Use of hyper-Dk/t RGP lens materi-als (>100 Dk/t) have been shown to supply enough oxygen to thecornea in all day lens wearers, which does not compromise cornealhealth in terms of increased corneal swelling [28].
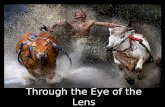
Each lens was designed to barely clear the steepest point of thecornea and to provide the most uniform thickness profile of thefluid accumulated between the lens and the cornea. The desiredclearance after lens settling (settling was minimal and inconsis-tent) was 30–50% of a thickness of a healthy average cornea, i.e.200–300 �m. By maintaining the minimal thickness of this reser-voir, we optimized the oxygen transmissibility of the lens–corneasystem [29] and minimized the degradation of vision that occursif excessive tear debris accumulates inside. Liquid reservoir under-neath the lens bathes the ocular surface with unpreserved saline orartificial tears, therefore masking any irregular corneal astigmatism(Fig. 1).
2.2. Fitting procedure
A single examiner (B.S.) fit the lenses for all patients. An indi-vidual lens design was determined by an on-eye evaluation ofdiagnostic scleral lenses with known parameters, after the lens hadbeen placed on the eye and had been in the position for at least2 h. Corneal clearance was evaluated by slit lamp examination toestablish the optimal sagittal height of each lens.
In an average lens, the internal optic zone of 12.5 mm was asingle curve surrounded by a 1.5–2.0 mm wide multi-curve tran-sitional zone vaulting the limbus and merging seamlessly into theposterior haptic surface. The haptic parameters of individual lenseswere determined by observing the vascular compression patternsof the bulbar conjunctiva, using a series of diagnostic lenses ofdifferent haptic designs aimed at minimizing lens induced com-pression of conjunctival blood vessels and enabling unobstructedblood circulation.
The patients were advised to wear the lenses on a daily basis.The patients were also instructed to take short breaks every 6 h for
cleaning and refilling the lens with fresh, unpreserved saline. Lenscare consisted of cleaning, wetting, and disinfecting with standardrigid gas-permeable lens solution systems. If there were excessiveCL deposits a peroxide based cleaning was added on a weekly base.
198 B. Severinsky et al. / Contact Lens & Anterior Eye 37 (2014) 196–202
F
Acc
2
tal
3
fiwwg
cTs(
adese
Table 1Indications for penetrating keratoplasty.
Indications for PK Eyes (%)
Keratoconus 27 (75%)Failed PK for KC 4 (11%)Cohan’s syn. 2 (6%)Post LASIK ectasia 1 (3%)HSK scar 1 (3%)
ig. 1. Optical section is used to define pre-corneal tear reservoir thickness profile.
fter dispensing, the patients were monitored periodically at theornea and contact lens clinics for the status of the corneal graft,ontact lens fit and complications associated with the CL wearing.
.3. Indications for success/failure
We considered the fitting of SCL to be successful when wearingime of 10 h a day or more was achieved. Partial success was defineds ability to wear the lenses between 6 and 10 h a day. Wearing timeess than 6 h a day was considered to be a failure.
. Results
36 eyes of 31 patients were fitted with SCL, 26 patients weretted in one eye and five patients in both. The male/female ratioas 26:5. The mean age ± standard deviation (SD) at time of fittingas 43.0 ± 14.2 years (range 19–74 years). The mean age of corneal
raft was 17.6 ± 11.4, and ranged from 4.3 to 42 years.Keratoconus, other forms of primary keratoectasia, and failed
orneal grafts for KC were the most common indications for PK.ogether, these groups accounted for 31 (86%) of the 36 eyes in thetudy. The remaining indications occurred relatively infrequentlyTable 1).
The most common reason for contact lens fitting was irregularstigmatism 24 (67%) eyes, followed by significant graft toricity,
efined as refractive cylinder of 5 or more diopters (D), 16 (44%)yes. Seven eyes (19%) were found to have significant spherical ani-ometropia with a difference of 3 or more diopters of the sphericalquivalent between the eyes. Two eyes with irregular astigmatismAlkaline burn 1 (3%)Total 36 (100%)
also had therapeutic indications for SCL fitting, one eye receivedcorneal graft due to corneal descemetocele secondary to alkalineburn and the other developed an ingrowth of irregular epitheliumcells. Listed above categories are not absolute, as many patientswere found to have multiple indications.
Three patients (3 eyes) failed to wear SCL for the first few weeksafter dispensing, due to an inability to increase wearing time or tofollow wearing schedule and therefore were excluded from furtherstatistical analysis. Regarding the other 28 patients (33 eyes) con-tinued with SCL, the duration of contact lens wearing period rangedfrom 0.5 to 8.8 years, with the mean follow-up time of 5.2 ± 2.2years. The mean interval between PK and initial contact lens fittingwas 12.2 ± 10.7 years (range 0.7–36.0 years).
The majority of our patients underwent corneal graft proceduredue to keratoconus. Penetrating corneal grafts for keratoconus,counting for their third decade of life, have a tendency to reveala decline in graft survival rates [30], and develop late-phase com-plications like progressive astigmatism [31] or recurrent ectasia[32,33]. We performed a separate analysis for a subgroup of ourcohort, 12 patients (15 eyes) consisted of patients with cornealgrafts older than 20 years of age (Group II). Eyes with cornealtransplants aged less than 20 years were listed as group I. Therewas no statistically significant difference in manifest refractionsphere and astigmatism values between the groups. However eyesin group II demonstrated a trend to higher K max values, 57.0 ± 7.6vs. 53.2 ± 6.8 D, but this was not statistically significant (Table 2).
3.1. Efficacy
All treated eyes were fitted due to inadequate spectacle-corrected vision after successful penetrating keratoplasty. Someof those eyes had undergone multiple unsuccessful surgical pro-cedures for reducing the iatrogenic astigmatism. In most of thesecases, the scleral lens provided useful corrected vision, regardlessof the amount or type of corneal astigmatism present.
The mean overall BCVAcl was 0.78 ± 0.25 (range 0.3–1.2). Therewas no clinically significant difference in BCVAcl between treatedgroups, 0.8 ± 0.3 in group I vs. 0.75 ± 0.2 in group II. The meanBCVArefr was 0.30 ± 0.18 (range 0.05–0.7). There was a significantincrease in visual acuity with scleral lenses (Fig. 2) compared to thespectacle corrected VA in all fitted eyes (p < 0.0001, paired t test).Improvement in BCVA, defined as a gain of two or more decimalacuity lines, was observed in 31 eyes (94%). In terms of functionalvision 23 patients (82%) achieved a Snellen visual acuity of 0.5 orbetter.
Out of 28 patients who continued with SCL, 21 (75%) were suc-cessfully fitted as defined by success criteria, i.e. able to wear thelenses for more than 10 h a day, and 5 patients (18%) achieved par-tial success with SCL. Mean wearing time of successful wearersgroup was 13.0 ± 2.0 h a day (range 10–16). The mean wearing timeamong all fitted patients was 11.9 ± 3.5 h a day.
Four patients (4 eyes) discontinued the use of SCL after differ-ent periods of successful wear (average follow up of 1.8 years). Thereasons for discontinuation were development of corneal decom-pensation (2 eyes), graft rejection secondary to lens abuse (one eye),

B. Severinsky et al. / Contact Lens & Anterior Eye 37 (2014) 196–202 199
Table 2Kmax, refractive cylinder and daily wearing time values for post keratoplasty groups (Group I – corneal transplants <20 years of age; Group II – corneal transplants >20 years;SPH, spherical component of manifest refraction; CYL, refractive astigmatism; Kmax, steepest keratometry; D, diopter; F/U, follow-up time).
Groups Eyes (%) SPH ± SD (D) CYL ± SD (D) Kmax ± SD (D) F/U ± SD (years) Daily wearing time ± SD (h)
anow
pItora
3
1dsoaegrte
wtf
4
c
Fi
Group I 18 (54.5%) −2.2 ± 5.6 8.4 ± 5.3
Group II 15 (45.5%) −2.3 ± 5.4 7.6 ± 3.2
Total 33 (100%) −2.2 ± 5.4 8.0 ± 4.4
nd end stage glaucoma (one eye). There was no statistically sig-ificant difference between the mean of refractive cylinder, Kmax
r wearing times of patients who dropped-out lens wear to thoseho continued.
An average of 1.7 lenses per eye was fitted during the studyeriod. There was a trend to more frequent lens refits in the group
I, 1.95 lenses vs. 1.4 in the group I. The primary reason for refit, inhis group, was the gradual decrease of corneal clearance, observedver time in 6 (40%) of 15 eyes. Thinning of the pre-corneal liquideservoir was contributed to progressive steepening of host cornea,s a part of the natural course of the disease or recurrent ectasia.
.2. Complications
During the study period, serious graft complications occurred in2 (36.4%) out of 31 fitted eyes (Table 3). Out of ten (30.0%) eyes thatemonstrated at least one graft rejection episode, eight eyes wereuccessfully treated and controlled by topical corticosteroids. Twother eyes exhibited signs of corneal decompensation and weredvised to discontinue the lens wear. The incidence of rejectionpisodes was higher in group I, 7 (21%) eyes. Two eyes (6%) inroup I had an episode of microbial keratitis (MK) that was probablyelated to patient non-compliance. The other noticeable complica-ions were contact lens induced corneal graft edema (Fig. 3), cornealrosions and compression due to ectasia recurrence (Fig. 4).
One of the benign complications associated with scleral lensear is conjunctival folds (Fig. 5), but clinically it does not seem
o have any effect on either corneal transplant or scleral lens per-ormance.
. Discussion
Contact lenses are used by more than 50% of patients after suc-essful penetrating keratoplasty to achieve better visual functions
R² = 0 .437 4p<0 .00 1
0
0.2
0.4
0.6
0.8
1
1.2
0 0.2 0. 4 0.6 0. 8 1 1.2
BCVA
cl
BCVA refr
Decimal VA: Cont act Lenses vs. SpectacleRefrac�on
VA CL
ig. 2. Graph showing the distribution of manifest refraction vs. contact lens BCVAn eyes dispensed with SCL (n = 33).
53.2 ± 6.8 4.5 ± 2.0 11.8 ± 2.457.0 ± 7.6 6.0 ± 2.2 11.9 ± 4.055.0 ± 7.5 5.2 ± 2.2 11.8 ± 3.5
[34]. In our series, vision improvement was the primary indica-tion for SCL fitting, and was achieved in most instances by theestablishment of an optimal anterior optical surface, with an appro-priate refractive correction. Our patients tolerated contact lenseswell with significant improvement of VA, as compared to the best-corrected vision without a SCL. Visual outcomes varied accordingto the pre-existing ocular status and the clarity of the corneal trans-plant, and ranged from 0.3 to 1.2. All of our patients demonstratedhigh degrees of astigmatism or/and corneal irregularity. Studieshave shown that the rates of postoperative astigmatism, higherthan 5.0 D, may vary from 18% to 23% [35]. Irregular astigmatisminduced by a corneal graft misalignment is one of the main reasonswhy contact lenses provide better visual results than spectacles[36]. However, the irregular corneal surface after PK often preventsachieving an optimal fit with corneal lenses [37]. Scleral lenses thatare characterized by excellent centration do not touch any part ofthe cornea and provide good optical correction without the dangerof corneal damage.
A number of surgical procedures were developed to decreasepost-keratoplasty astigmatism or anisometropia [38]. When thegraft astigmatism is of moderate amount and regular, laser refrac-tive surgery has been shown to be effective. LASIK (laser in situkeratomileusis) might be superior to PRK (photorefractive kerate-ctomy) for the treatment of myopia and astigmatism of low degree[39,40]. Correction of high refractive errors requires high energylevels and, therefore, may be associated with corneal haze, scaringor graft rejection. Furthermore, the application of microkeratomeitself may provoke wound dehiscence [40]. Incisional techniques[41,42] have been shown to be effective in correcting post kerato-plasty astigmatism, but the results are frequently unpredictable,since the depths or location of the incisions cannot be calculatedpreoperatively. Additionally, the risk of perforation always exists.
Contrary to surgical options, the safety and efficacy of scleral
contact lenses was previously reported by a number of investiga-tors [13–15,25,43]. Studies performed on a large cohort of patientsdescribed the successful use of SCL for visual rehabilitation ofFig. 3. SCL induced corneal graft edema. Note: contact lens full-thickness crackcorresponded to edematous area.

200 B. Severinsky et al. / Contact Lens & Anterior Eye 37 (2014) 196–202
Table 3Corneal graft complications among groups fitted with SCL (percentage given out of the total number of eyes wearing SCL). Group I – corneal transplants <20 years of age;Group II – corneal transplants >20 years.
Complication Mean graft age (years) Graft rejection Graft–host ectasia Microbial keratitis Corneal edema
GroupsGroup I, eyes 8.8 ± 3.8 7 (21%) 3 (9%) 2 (6%) 1 (3%)Group II, eyes 28.1 ± 8 3 (9%) 6 (18%) 0 1 (3%)Total, eyes 17.6 ± 11.4 10 (30%) 9 (27%) 2 (6%) 2 (6%)
F n (leftc
im
awlcosfp
srtau
that patients with gas-permeable lenses scleral lenses need a breakin 45.5% of the eyes. In the study by Visser et al. [26], nearly half(48.9%) of the patients removed and reinserted their lenses duringdaily wearing.
ig. 4. Subepithelial fibrosis of donor tissue located near to the host–donor junctioorneal profile elevation (recurrent ectasia).
rregular corneas, when keratoplasty was listed as one of the pri-ary indications.Various studies on scleral lenses used different methods to
ssess wearing time. The mean wearing time in the current studyas 11.8 h a day, that similar to reported by Severinsky and Mil-
odot [15] (11.9 h daily wearing time) in the retrospective studyonducted on 97 patients, when nearly all had either ectatic corneasr corneal irregularities following penetrating keratoplasty. In thetudy performed on a larger amount of patients, Pullum et al. [43],ound an average of 10 h or more wearing time in 59% (n = 538)atients.
The performance of scleral lenses is also reflected in the neces-ity to take a break during the day. Scleral lenses are designed toest on bulbar conjunctiva, which is a pliable tissue. In some eyes,
he lens may depress it and cause compression. In this case the par-limbal area will become swollen and injected. Also tears exchangenderneath the lens will decrease significantly [44]. When the lensFig. 5. Superiorly located conjunctival fold (arrow) under well fitted SCL.
). The fibrosis is related to the contact lens corneal bearing (right), as a sequence of
is not fluid-vented or the exchange of liquid reservoir has damp-ened due to a lens seal-off, the cornea will be exposed to a toxicswamp that has accumulated beneath the lens. Stagnation of thefluid in pre-corneal chamber may lead to severe punctate epithe-lial keratophaty (Fig. 6), corneal ischemia and edema. Aspiration ofthe fresh tears under the lens edge provides additional oxygen sup-ply to the cornea, and was shown to be associated with successfulfit and increased wearing time [15]. Thus graft patients should beadvised to have breaks during contact lens wear as often as possi-ble in order to minimize toxicity damage. Tan et al. [45] reported
Fig. 6. Epitheliopathy of corneal transplant.

B. Severinsky et al. / Contact Lens & A
sadi7at
asftappglschig
ra1st
ealic
ttrdfn
Fig. 7. Heavy deposits covering anterior surface of SCL.
The failure rate of our study was 19.4%. Four patients hadtopped the use of SCL after different periods of successful wear,nd three individuals failed to wear SCL in the first weeks afterispensing. This number concurs well with the results of other
nvestigators. In a retrospective study, Tan et al. [45] found that1% of the eyes could continue wearing the scleral lens, Pullumnd Buckley [13] described that 22% of their cases failed a scleralrial or stopped wearing their scleral lenses completely.
Most complications associated with SCL wear responded well toppropriate management. Ten (30%) eyes demonstrated at least aingle episode of graft rejection. Whereas eight eyes were success-ully treated by conservative treatment (topical corticosteroids),wo eyes had demonstrated corneal decompensation, which wasttributed to the reduction in endothelial cells density, and theatients were advised to stop SCL use. While it cannot be directlyroven that contact lenses by themselves play a significant role inraft decline, we do believe that factors associated with contactens wear, such as corneal hypoxia, microtrauma, epithelial ero-ions and the toxic effects of preservatives in rigid gas-permeableontact lens solution systems, may all compromise corneal graftealth and cause chronic ocular surface inflammation. This chronic
nflammation may in turn provoke episodes of graft rejection andraft decline.
Corneal graft rejection rate in our cohort coincides with theesults of other researchers. In a longitudinal study Jonuscheit [46]nd colleagues found that of 43 penetrating grafts for keratoconus,5 experienced at least one episode of rejection. Another retro-pective study [32] reports rejection rate of 30% in clear cornealransplants 20 or more years old.
Two of our patients had an episode of microbial keratitis. Thexact etiology of MK remains unknown, but we suggest it was prob-bly related to patient non-compliance to remove and reinsert theenses during the day, contact lens over wear or bacteria aggregatesn precipitates covering contact lens surface as a sequence of poorleaning (Fig. 7).
Most irregular cornea patients are fully dependent on their con-act lenses and therefore wear them all day long. This may leado corneal hypoxia. In our study two eyes (6%) had demonstrated
ecurrent episodes of transient corneal edema. Edema has a ten-ency to appear when oxygen level is below minimal requirementsor normal corneal oxygenation. Mild edema resolves sponta-eously with discontinuation of contact lens wearing. The use ofnterior Eye 37 (2014) 196–202 201
hypertonic saline (5% NaCl) has been shown to accelerate cornealrecovery from hypoxic events [47]. When the episodes of cornealedema persist, we tend to advise topical instillation of 5% NaClsolution during the removal/reinsertion procedure. Additional topositive fluid-venting properties of SCL, a combination of hyper gaspermeable lens materials and minimization of contact lens and pre-corneal fluid layer thicknesses will increase oxygen permeability ofthe lens–cornea system [29].
Conjuntivochalasis is frequent in eyes of contact lens wearersespecially when the ocular surface is compromised [48]. Since con-junctiva is pliable, it may get underneath the space designatedfor “limbal clearance” and create a “conjunctival fold”. The “folds”may block fluid exchange beneath the lens and lead to stagnation.In such cases decreasing limbal vault, i.e. minimizing the spacebetween the lens and the limbus may be helpful.
In our study the major indication for PK was keratoconus. It isknown that penetrating grafts performed for keratoconus exhibitbetter visual outcome and graft survival than grafts performed forother indications. The 20-year graft survival for a penetrating graftfor keratoconus in recipients of all ages stands at 49% [35].
The average initial graft to fit interval in our study was morethan 12 years. This value is relatively high when compared to thedata presented by other researchers [5,6] and may be explained bygood spectacle corrected visual acuity, which is often a rule after asuccessful PK. In an Australian corneal graft registry study in 44%of 4834 total penetrating grafts for keratoconus, spectacles wereused as primary visual correction, while 39% did not use any typeof visual correction at all [35]. As corneal astigmatism progressivelyworsens and the cornea becomes more irregular, spectacles becameimpractical and the need for contact lens correction rises.
Practitioners should be aware of ectasia recurrence when fit-ting corneal transplants, counting for second or third decades oftheir lives. Among our cohort, the average Kmax value was higherin group II, 57.0 ± 7.6 D. Six (40%) of 15 eyes in this group, requiredone or more lens changes due to over time developed SCL bearingon donor cornea or graft–host wound. Elevation of corneal profilemay be explained by progressive misalignment of the graft–hostinterface or steepening of the host cornea (i.e. recurrent ectasia).The rate of graft–host ectasia varies from 11% to 39.6% [32,33] with20-year keratoconus recurrence probability of 10% [49]. However,despite graft ectasia, most of these corneal transplants remain clearand may provide excellent vision. Additionally, as each subsequentcorneal transplant has a higher risk of early failure, delaying surgeryin such cases would be beneficial.
This retrospective study describes prolonged and successful useof scleral contact lenses after penetrating keratoplasty. Our patientsdemonstrated good visual outcomes and sufficient daily wearingtimes. The major complication of concern remains graft rejection.However, its rates were consistent with data provided by other,non-contact lens related, reports. Contact lens mechanical compli-cations such as compression and corneal erosions, which thoughtto be related to the protrusion of corneal profile, were successfullyresolved by changing lens design.
We believe that scleral lenses are the best contact lens optionavailable for eyes with complex corneal graft geometry. In additionto successful visual rehabilitation, SCL may delay or prevent furthersurgical involvement.
Conflict of interest and source of funding
Boris Severinsky, Joseph Fruct-Pery and Abraham Solomon have
no financial or proprietary interest in any material or method men-tioned.Mr. Shmuel Berhman is a full time employee of Microlens Ltd.and has a financial interest in manufacturing contact lenses.

2 s & A
A
cs
R
[
[
[
[
[
[
[
[
[
[
[[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
[
02 B. Severinsky et al. / Contact Len
cknowledgments
We would like to thank Microlens Ltd. Laboratory and espe-ially Mr. Shmuel Behrman for his generous technical and didacticupport given during the study period.
eferences
[1] Stainer GAT, Perl T, Binder PS. Controlled reduction of postkeratoplasty astig-matism. Ophthalmology 1982;89:668–75.
[2] Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM.Deep anterior lamellar keratoplasty as an alternative to penetrating kerato-plasty a report by the American academy of ophthalmology. Ophthalmology2011;118(1):209–18.
[3] Sögütlü Sari E, Kubaloglu A, Ünal M, Pinero Llorens D, Koytak A, OfluogluAN, et al. Penetrating keratoplasty versus deep anterior lamellar kerato-plasty: comparison of optical and visual quality outcomes. Br J Ophthalmol2012;96(8):1063–7.
[4] Fontana L, Parente G, Tassinari G. Clinical outcomes after deep anterior lamellarkeratoplasty using the big-bubble technique in patients with keratoconus. AmJ Ophthalmol 2007;143(1):117–24.
[5] Wietharn BE, Driebe Jr WT. Fitting contact lenses for visual rehabilitation afterpenetrating keratoplasty. Eye Contact Lens 2004;30(1):31–3.
[6] Geerards AJ, Vreugdenhil W, Khazen A. Incidence of rigid gas-permeablecontact lens wear after keratoplasty for keratoconus. Eye Contact Lens2006;32(4):207–10.
[7] Jinabhai A, Neil Charman W, O‘Donnell C, Radhakrishnan H. Optical quality forkeratoconic eyes with conventional RGP lens and stimulated, customized con-tact lens correction: a comparison. Ophthalmic Physiol Opt 2012;32(3):200–12.
[8] Manabe R, Matsuda M, Suda T. Photokeratoscopy in fitting contact lenses afterpenetrating keratoplasty. Br J Ophthalmol 1986;70:55–9.
[9] Barr JT, Wilson BS, Gordon MO, Rah MJ, Riley C, Kollbaum PS, et al. Estimationof the incidence and factors predictive of corneal scarring in the CollaborativeLongitudinal Evaluation of Keratoconus (CLEK) Study. Cornea 2006;25:16–25.
10] Bergmanson JPG, Ruben CM, Chu L-W-F. Corneal epithelial response of the pri-mate eye to gas permeable corneal contact lenses: a preliminary report. Cornea1984;3:109–13.
11] Efron N. Contact lens-induced changes in the anterior eye as observed in vivowith the confocal microscope. Prog Retin Eye Res 2007;26:398–436.
12] Mackman G, Polak FM, Sidrys L. Fluorescein angiography of soft contactlens induced vascularization in penetrating keretoplasty. Ophthalmic Surg1985;16(3):157–61.
13] Pullum KW, Buckley RJ. A study of 530 patients referred for RGP scleral contactlens assessment. Cornea 1997;16:612–22.
14] Rosenthal P, Croteau A. Fluid-ventilated, gas-permeable scleral contact lensis an effective option for managing severe ocular surface disease and manycorneal disorders that would otherwise require penetrating keratoplasty. EyeContact Lens 2005;31(3):130–4.
15] Severinsky B, Millodot M. Current applications and efficacy of scleral contactlenses—a retrospective study. J Optometry 2010;3(3):158–63.
16] Ridley F. Scleral contact lenses, their clinical significance. Arch Ophthalmol1963;70(December):740–5.
17] Bleshoy H, Pullum KW. Corneal response to gas-permeable impression sclerallenses. J Br Contact Lens Assoc 1988;11:31–4.
18] Pullum KW, Hobley AJ, Parker JH. Hypoxic corneal changes following sealedgas permeable impression scleral lens wear. J Br Contact Lens Assoc 1990;13:83–7.
19] Pullum KW, Hobley AJ, Davison C. 100 + DK: does thickness make much differ-ence. J Br Contact Lens Assoc 1991;14:17–9.
20] Ezekiel D. Gas permeable haptic lenses. J Br Contact Lens Assoc 1983;6:158–61.21] Ruben CM, Benjamin WJ. Scleral contact lenses: preliminary report on oxygen
permeable materials. Contact Lenses 1985;13:5–10.22] Rosenthal P, Ducharme C. A gas-permeable scleral contact lens for visual reha-
bilitation. Am J Ophthalmol 1990;109:318–22.
[
[
nterior Eye 37 (2014) 196–202
23] Lyons CJ, Buckley RJ, Pullum K, Sapp N. Development of the gas-permeableimpression-moulded scleral contact lens. A preliminary report. Acta Ophthal-mol Suppl 1989;192:162–4.
24] Winkler TD. Corneo-scleral RGP lenses for post-graft patients. CLAO J1998;24:198.
25] Visser ES, Visser R, van Lier HJ, Otten HM. Modern scleral lenses. Part I: Clinicalfeatures. Eye Contact Lens 2007;33(1):13–20.
26] Visser ES, Visser R, van Lier HJ, Otten HM. Modern sclerallenses. Part II: Patientsatisfaction. Eye Contact Lens 2007;33(1):21–5.
27] Van der Worp E. A guide for scleral lens fitting. Scleral Lens Education Society;2010. p. 2–3. Available online: http://www.commons.pacificu.edu/mono/4
28] Pullum KW, Stapleton FJ. Scleral lens induced corneal swelling: what is theeffect of varying DK and lens thickness. CLAO J 1997;23:259–63.
29] Michaud L, van der Worp E, Brazeau D, Warde R, Giasson CJ. Predicting esti-mates of oxygen transmissibility of scleral lenses. Cont Lens Anterior Eye2012;35(6):266–71.
30] Fukuoka S, Honda N, Ono K, Mimura T, Usui T, Amano S. Extendedlong-term results of penetrating keratoplasty for keratoconus. Cornea2010;29(5):528–30.
31] Szczotka-Flynn L, McMahon TT, Lass JH, Sugar J, Weissman BA, Stiegemeier MJ,et al. Late-stage progressive corneal astigmatism after penetrating keratoplastyfor keratoconus. Eye Contact Lens 2004;30(2):105–10.
32] Felipe AF, Hammersmith KM, Nottage JM, Rapuano CJ, Nagra PK, Cohen EJ, et al.Indications, visual outcome, and ectasia in clear corneal transplants 20 yearsold or more. Cornea 2013;32(5):602–7.
33] Patel SV, Malta JB, Banitt MR, Mian SI, Sugar A, Elner VM, et al. Recurrentectasiain corneal grafts and outcomes of repeat keratoplasty for keratoconus. Br JOphthalmol 2009;93(2):191–7.
34] Smiddy WE, Hamburg TR, Kracher GP, Stark WJ. Keratoconus. Contact lens orkeratoplasty? Ophthalmology 1988;95(4):487–92.
35] Kelly TL, Williams KA, Coster DJ. Corneal transplantation for keratoconus: aregistry study. Arch Ophthalmol 2011;129(6):691–7.
36] Woodward EG, Moodaley LC, Lyons C, Davison C, Buckley RJ, Barbur VA. Postkeratoplasty dimensional and refractive change in contact lens and spectaclecorrected cases. Eye 1990;4:689–92.
37] Kagaya F, Tomidokoro A, Tanaka S, Amano S, Oshika T. Fourier series harmonicanalysis of corneal topography following suture removal after penetrating ker-atoplasty. Cornea 2002;21(3):256–9.
38] Kuryan J, Channa P. Refractive surgery after corneal transplant. Curr Opin Oph-thalmol 2010;21(4):259–64.
39] Bilgihan K, Ozdek SC, Akata F, Hasanreisoglu B. Photorefractive keratectomyfor post-penetrating keratoplasty myopia and astigmatism. J Cataract RefractSurg 2000;26:1590–5.
40] Webber SK, Lawless MA, Sutton GL, Rogers CM. LASIK for post penetratingkeratoplasty astigmatism and myopia. Br J Ophthalmol 1999;83:1013–8.
41] Javadi MA, Feizi S, Yazdani S, Sharifi A, Sajjadi H. Outcomes of augmented relax-ing incisions for postpenetrating keratoplasty astigmatism in keratoconus.Cornea 2009;28:280–4.
42] Ezra DG, Hay-Smith G, Mearza A, Falcon MG. Corneal wedge excision inthe treatment of high astigmatism after penetrating keratoplasty. Cornea2007;26:819–25.
43] Pullum KW, Whiting MA, Buckley RJ. Scleral contact lenses the expanding role.Cornea 2005;24:269–77.
44] DeNaeyer GW. Modern scleral contact lens fitting. Contact Lens Spectrum2010;10:20–5.
45] Tan DHT, Pullum KW, Buckley RJ. Medical applications of scleral contact lenses:2. Gas permeable scleral contact lenses. Cornea 1995;14:130–7.
46] Jonuscheit S, Doughty MJ, Ramaesh K. The corneal endothelium after kerato-plasty for keratoconus. Clin Exp Optom 2013;96(2):201–7.
47] Marisi A, Aquavella JV. Hypertonic saline solution in corneal edema. Ann Oph-thalmol 1975;7(2):229–33.
48] Mimura T, Usui T, Yamamoto H, Yamagami S, Funatsu H, Noma H, et al. Con-junctivochalasis and contact lenses. Am J Ophthalmol 2009;148(1):20–5.
49] Niziol LM, Musch DC, Gillespie BW, Marcotte LM, Sugar A. Long-term outcomesin patients who received a corneal graft for keratoconus between 1980 and1986. Am J Ophthalmol 2013;155(2):213–9.