Connective Tissue. 4 Types of Tissue Epithelial Connective Muscle Neural.
Connective tissue present
-
Upload
drbhavna-tyagi -
Category
Health & Medicine
-
view
57 -
download
1
Transcript of Connective tissue present

Connective
tissue

Introduction Functions Composition Types of fibers Connective tissue cells Classification of connective tissue Membranes Connective tissue framework Connective tissue disorders References
contents

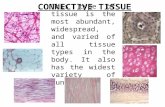
Most abundant basic tissue. Derived from somites during prenatal
development.
Functions Establishing a structural framework Transporting fluids and dissolved materials Protecting delicate organs Supporting, surrounding and
interconnecting tissues Storing energy reserves Defending the body from microorganisms

Cells Fixed Mobile Fibers Collagen fibers -large Reticular fibers-thin Elastic fibers- very fine
Ground substance
Composition

1) PROTEOGLYCANS Glycosaminoglycans.( GAG) 80-90% Protein Core. 10-20%
2) GLYCOPROTEINS Fibronectin Laminin Chondronectin
GROUND SUBSTANCE

Linear chains of repeating disaccharides units.
One of the disaccharides is glucosamine or galactosamine.
The other is glucuronic acid or iduronic acid or galactose.
GLYCOSAMINOGLYCANS

(1) keratin sulfate Galactose-Glucosamine Bone and Cornea
(2) Chondroitin sulfate Glucuronic acid-Galactosamine cartilage, skin , basal lamina.
(3) Dermatan sulfate Iduronic acid-Galactosamine tendon , skin
5 types of glycosaminoglycans.

(4) Heparin sulfate iduronic acid-glucosamine
basal lamina, nerve tissue.
(5) Hyaluronic acid glucuronic acid-glucosamine cartilage , synovial fluid LARGEST , no protein core

Glycosaminoglycans usually attached to a protein core and called as proteoglycan exception is hyaluronate.
o GAGs are linked to protein core like bristles on a hair brush.

Anchor cells to proteoglycans in matrix and to fibers.
Fibronectin – general connective tissue.
Laminin – mainly basement membrane.
extracellular matrix glycoproteins

Facilitate cell migration.
May be important for determining cell shape.
May play a role in blood clotting.
Fuction of fibronectin

Laminin found in basement membrane.
Binds to collagen type 4 heparin sulfate Integrin receptor

(1)Collagen (2)Reticular formed from collagen proteins.
(3)Elastic – formed from the protein elastin.
Connective tissue fibres.

Collagen is tough protein 30% of human body by dry weight. Relatively long (300 nm) and narrow(1.5 nm) 3 polypeptide chain wound together in form
of triple helix.( alpha chains) Made up of repetitive sequences of 3 amino
acids. 25 forms of alpha chains. 12 types of collagen are known. Lots of hydroxyprolines and hydroxylysines.
Collagen fiber


Formation of mRNA for each type of a chain
Sythesis of alpha chains of procollagen with peptides.
Hydroxylation of specific prolyl & lysl residues in rER.( vit C dependent)
Attachment of soluble glucose & galacotose.
Assembling of procollagen to golgi complex via transport vescicles.
Packing of procollagen in secretory vescicles .
Secretory vescicles transported to cell surface via microfilaments & microtubules
Discharge of procollegen molecule to extracellular space.


Randomly oriented and unbranched in loose areolar CT.
Collagen fibers consist of closely packed orderly fibrils and when seen in bundles (as in tendons, aponeuroses) appear white. In histological preparations after regular staining they are acidophilic. Collagen fibers are flexible, but very inelastic with extremely high tensile strength.


Electron micrograph of human collagen fibrils

Collagen type
Pricipal tissue distribution
cells of origin
1 Loose & dense CT, fibrocartilage,bone, dentin.
Fibroblasts & reticular cells ,osetoblast, ondotoblasts
2 Hyaline & elastic cartilage, viterous body of eye.
Chondrocytes and retinal cells.
3 Loose CT, reticular fibres, blood vessels
Fibroblasts & reticular cells, endothelial cells
4 Basement membranes fibroblasts
5 Fetal membranes,placenta membranes,bone
Fibroblasts.
Distributions and origins of five types of collagen

Abundant in lympoid tissue. Reticular fibers are very thin (diameters
between 0.5 - 2m m) and are not visible in normal histological preparations after regular staining (H & E), however they can be visualized and stained black after impregnation with silver salts. This affinity for silver is called argyrophilia.
Reticular fibers are also stainedwith the PAS reaction due to the high content of glycoproteins It is now recognized that reticular fibers are a special form of collagen (Type III).
RETICULAR FIBRES.


Oxytylan fibres: glycoprotein containing microfibirils or microfilaments, 6-10 microm diameter.
Elaunin fibres: gradual deposition of elastin on microfilaments.
Elastic fibres: heavy deposition of elastin
Elastic fibres.

Comparitively thin {1 microm}
Less wavy Occurence: large artries. loose connective
tissue. elastic cartilage

Fibrillin Microfilament glycoprotein important in
elastic fibres. Marfan’s syndrome- defect in fibrillin
syntehesis and elastic fibres. Connective tissue disorder affecting
skeleton, elastic blood vessels and eye. Severe- cardiovascular problems-arteries
cannot stretch.

All connective tissue cells are derived from two types of stem cells
Hematopoetic stem cells. Mesenchymal cells
Connective tissue cells



Fibroblast Macrophages Mast cells Plasma cells Adipose cells Leukocytes Lymphocytes Monocytes Mononuclear,agranulocytes
Netrophils Eosonophil Basophil polymorphonuclear,granulocytes


Most common cell type in connective tissue. Synthesize collagen , reticular and elastic
fibres. Sythesize glycosaminoglycans and
glycoproteins.
fibroblast


10 – 30 mirom in diameter Shape can very trmendously Phagocytosis and digestion of bacteria foreign bodies blood cells dead cells oOppsonization
Macrophages.

Oppsonization

Secretes important enzymes –collagenase, elastase
Produce cytokines such as: Tumour necrosis factor Interlekuins GM-CSF(granulocyte macrophage –
colony stimulating factor)
Other function

Round , oval , 20 – 30 microm Basophilic granules in cytoplasm. Metachromasia- mast cells stain purple with
methylene blue. Due to heparin content in the cell.
Mast cells


Heparin- anticoagulant Histamine – increases capilliary permeability primary mediator of acute inflammatory reaction.o Eosinophil chemotactic factor ECF- Ao Slow reacting substance of anaphylaxis SRS-A leukotrines.
MAST CELL SECRETES


Can occur within seconds. Massive release of histamine from mast
cells Reduces mean arterial blood pressure –
blood enters peripheral capillaries Caused by IgE secretion from plasma cells. Epinephrine can reverse HIS by causing
vasoconstriction.
Immediate hypersensitivity reaction


Eccentric nucleus Dark staining
cytoplasm , lots of RER
10 – 20 micrm Don’t leave the
connective tissue Produce
antibodies.
Plasma cell


1. Loose Connective Tissue:
a. Areolar tissue Widely distributed under epithelia
b. Adipose tissue Hypodermis, within abdomen, breasts
c. Reticular connective tissue Lymphoid organs such as lymph nodes
True or Proper Connective Tissue

1. Areolar CT
◦ consists of all 3 types of fibers, several types of cells, and semi-fluid ground substance
◦ found in subcutaneous layer and mucous membranes, and around blood vessels, nerves and organs
◦ function = strength, support and elasticity
LOOSE Connective Tissue


2. Adipose tissue
◦ consists of adipocytes; "signet ring" appearing fat cells. They store energy in the form of triglycerides (lipids).
◦ found in subcutaneous layer, around organs and in the yellow marrow of long bones
◦ function = supports, protects and insulates, and serves as an energy reserve


3. Reticular CT
◦ Consists of fine interlacing reticular fibers and reticular cells
◦ Found in liver, spleen and lymph nodes
◦ Function = forms the framework (stroma) of organs and binds together smooth muscle tissue cells

2. Dense Connective Tissue: a. Dense regular connective tissue
Tendons and ligaments
b. Dense irregular connective tissue Dermis of skin, submucosa of digestive tract
contains more numerous and thicker fibers and far
fewer cells than loose CT

1. Dense regular Connective Tissue• consists of primarily
parallel bundles of collagen fibers and fibroblasts
• forms tendons, ligaments and aponeuroses
• Function = provide strong attachment between various structures


. Dense Irregular CT
◦ consists of randomly-arranged collagen fibers and a few fibroblasts
◦ Found in fasciae, dermis of skin, joint capsules, and heart valves
◦ Function = provide strength


Supportive Connective Tissue

o Firm, non calcified tissue.o Serves as skeleton tissue in the body.o Avascular
HISTOLOGY OF CARTILAGE Cells and matrix Cells: chondroblast chondrocytes
Cartilage

◦ Jelly-like matrix (chondroitin sulfate) containing collagen and elastic fibers and chondrocytes surrounded by a membrane called the perichondrium.
◦Unlike other CT, cartilage has NO blood vessels or nerves except in the perichondrium.
◦The strength of cartilage is due to collagen fibers and the resilience is due to the presence of chondroitin sulfate.
◦Chondrocytes occur within spaces in the matrix called lacunae.

1. Hyaline cartilage2. Fibrocartilage3. Elastic cartilage

Hyaline Cartilage (most abundant type)
fine collagen fibers embedded in a gel-type matrix. Occasional chondrocytes inside lacunae.
Found in embryonic skeleton, at the ends of long bones, in the nose and in respiratory structures.
Function= flexible, provides support, allows movement at joints


2. Fibrocartilage
contains bundles of collagen in the matrix that are usually more visible under microscopy.
Found in the pubic symphysis, intervertebral discs, and menisci of the knee.
Function = support and fusion, and absorbs shocks.


3. Elastic Cartilage
threadlike network of elastic fibers within the matrix.
found in external ear, auditory tubes, epiglottis.
function = gives support, maintains shape, allows flexibility


Has osteocytes◦Depend on diffusion through canaliculi for
nutrients Little ground substance Dense mineralized matrix Surrounded by periosteum Function
◦ Supports and protects organs◦ Provides levers and attachment site for muscles◦ Stores calcium and other minerals◦ Stores fat◦ Marrow is site for blood cell formation
Location ◦ Bones
Bone, or osseous tissue


Description◦ red and white blood cells
in a fluid matrix Function
◦ transport of respiratory gases, nutrients, and wastes
Location◦ within blood vessels
Characteristics◦ An atypical connective tissue◦ Consists of cells surrounded by fluid matrix
Fluid connective tissue.


Membranes
Form a barrierComposed of epithelium and connective tissueFour types Cutaneous
SynovialSerousMucous


1. Mucous membrane = mucosa; it lines cavities that open to the exterior, such as the GI tract.◦ The epithelial layer of the mucous
membrane acts as a barrier to disease organisms.
◦ The connective tissue layer of the mucous membrane is called the lamina propria.
◦ Found as the lining of the mouth, vagina, and nasal passage.

2. Serous membrane = serosa, membrane lines a body cavity that does NOT open to the exterior and it covers the organs that lie within the cavity.
a. pleura = lungsb. pericardium = heartc. peritoneum = abdomen
◦ The serous membrane has two portions:1. parietal portion = lining outside
the cavity.2. visceral portion = covers the organ.



Organs and systems are interconnected
Network of connective tissue proper consisting of◦ Superficial fascia◦ Deep fascia◦ Subserous fascia
The Connective Tissue Framework of the Body


Connective tissue disorders

Perivascular collagen deposition=Collagen Vascular Diseases
Autoimmune diseases-not the primary cause
Exact cause remains obscure Different diseases associated with specific
autoantibodies

Diseases Antibody
Systemic lupous erythematosous
Rhemutoid arthriris Sjogren syndrome Systemic sclerosis Polymyositis/
dermatomyositis Mixed connective
tissue deseases
Anti – dsDNA, Anti-SM
RF, Anti-RA33 Anti RO(SS-A),AntLa(SSB) Anti-Scl-70,anti cetromere Anti-Jo-1,
Anti-U1-RNP

Histopathology: Connective tissue and blood vessel inflammation and abundant fibrinoid deposits
Varying tissue distribution and pattern of organ involvement
Symptoms nonspecific and overlapping Difficult to diagnose

General◦ autoimmune multisystem disease◦ Malar rash first sign in 50%◦ Erythematous maculopapular eruption after sun exposure◦ Oral ulceration◦ 3-5% nasal septum perforation◦ Acute parotid enlargement 10%◦ Xerostomia 15%◦ Larynx and trachea involvement uncommon
Systemic Lupus Erythematosus


Discoid Lupus: Cutaneous manifestations Scar upon healing

Inflammation of the synovial tissue (lymphocytic) with synovial proliferation
Symmetric involvement of peripheral joints, hands, feet and wrists
Occasional systemic effects: vasculitis, visceral nodules, Sjogren syndrome, pulmonary fibrosis
Rheumatoid Arthritis

Rheumatoid Arthritis may involve the TMJ.

Chronic disorder characterized by immune-mediated destruction of exocrine glands
Sicca complex accompanying any of the connective tissue diseases (xerophthalmia, keratoconjuntivitis, xerostomia with/without salivary gland enlargement)
Sjogren Syndrome

Also known as systemic sclerosis
Sclerotic skin changes often accompanied by multisystem disease.
Progressive fibrosis from increased collagen deposition in intersitium and intima of small arteries and connective tissues
May be benign cutaneous involvement or aggressive systemic disease.
Scleroderma

PresentationRaynaud’s
phenomenonedema fingers and
handsskin thickening
visceral manifestationsGI tract, lung, heart,
kidneys, thyroidarthralgias and muscle
weakness often

Proximal muscle weakness
Elevated serum creatinine kinase
Myopathic changes on electromyography
Muscle biopsy with evidence of lymphocytic inflammation
Rash accompanies these in dermatomyositis
Polymyositis and Dermatomyositis

Ham’s histology Fawcets Dental embryology, Histology,and
Anatomy;second edition;Mary Bath Balgoh,Margaret j Fehrenbach;chapter8 ;basic tissues.
Ten cate’s Oral histology;chapter 4 ; cytoskeleton,junction,fibroblast.
Textbook of oral pathology;Shafer, Hine,Levy,
references

o Burket’s Oral Medicine;diagnosis and treatment planning;Greenberg,gGick;tenth edition
o Epidemiology of connective tissue disorders M. Gaubitz, rheumatology.oxfordjournals.org,
(2006) 45 (suppl 3)o Mutations in the human gene for fibrillin-1
(FBN1) in the Marfan syndrome and related disorders.
o Raynaud’s phenomenon, A.D.A.M. Medical Encyclopedia.

Thank you