Complications of Bariatric Surgery: What You Can Expect to ... · Roux-en-Y gastric bypass (RYGB)...
Transcript of Complications of Bariatric Surgery: What You Can Expect to ... · Roux-en-Y gastric bypass (RYGB)...
RE
VIE
W1640
The American Journal of GASTROENTEROLOGY VOLUME 112 | NOVEMBER 2017 www.nature.com/ajg
CLINICAL AND SYSTEMATIC REVIEWS
INTRODUCTION
Th e increasing prevalence of obesity and its associated co-mor-
bidities has resulted in a substantial increase in the number of
bariatric procedures performed worldwide ( 1–5 ). In fact, bariatric
surgery has become one of the fastest growing operative proce-
dures and has gained acceptance as the leading option for sus-
tained weight-loss in the treatment of morbid obesity ( 3 ). As this
fi eld continues to expand, gastroenterologists will see an increas-
ing number of patients with surgically altered anatomy. Th ere
are a number of unique complications that arise in this patient
population that require specifi c knowledge for proper manage-
ment. Furthermore, conditions unrelated to the altered anatomy
typically necessitate a diff erent management strategy. As such, a
basic understanding of surgical anatomy, potential complications,
and endoscopic tools and techniques for optimal management is
essential for the practicing gastroenterologist. It is important to
co-manage these conditions with a surgical team, as endoscopic
approaches may not always be successful, and surgical reinterven-
tion may not always be suffi cient. For all of the endoscopic pro-
cedures discussed, it is critical to use carbon dioxide insuffl ation
to minimize complications and post-procedural pain. Further-
more, there should be a low threshold for anesthesia consultation,
as bariatric patients may have complicated airways, obstructive
sleep apnea, require more medication, or may be at other risk of
conscious sedation. Th is review will cover these topics and focus
on major complications that gastroenterologists will be most
likely to see in their practice.
ROUX-EN-Y GASTRIC BYPASS
Roux-en-Y gastric bypass (RYGB) has traditionally been the
most common bariatric procedure, accounting for almost half of
all bariatric surgeries performed worldwide ( 3 ). Th is procedure
involves stapling the stomach to create a small gastric pouch,
along with diversion of oral intake and biliopancreatic digestive
enzymes to the distal small bowel, via creation of a Roux limb
( Figure 1a ).
Various hormonal mechanisms are implicated depending on
surgical technique employed ( 6–8 ). Foregut theories suggest the
role of a hormone that is released from the duodenum and contrib-
utes to insulin resistance. Th is substance is no longer thought to be
secreted following gastric bypass surgery in the foregut hypothesis.
In addition, gastric inhibitory peptide (GIP), which is secreted
from the duodenum, is thought to have a role. In hindgut theory,
bile and undigested food are thought to stimulate L-cells to pro-
duce glucagon-like peptide-1 (GLP-1) and Peptide YY (PYY) as
well as other substances which cross the blood brain barrier and
enhance satiety signaling, slow gastric emptying, and increase
insulin production. It is likely that numerous mechanisms actually
contribute to the metabolic eff ect of this surgical procedure.
Th ere are several variants of the RYGB. In procedures performed
via a laparoscopic approach, the pouch is completely transected
and separated from the gastric remnant, whereas in the prior
open approach, a staple line merely separates the stomach. Gastro-
jejunal anastomosis (GJA) can be created with circular or linear
staplers, or using a hand-sewn. When sutures are used, these can
Complications of Bariatric Surgery: What You Can
Expect to See in Your GI Practice
Allison R. Schulman , MD 1 , 2 and Christopher C. Th ompson , MD, MSc, FASGE, FACG AGAF 1 , 2
Obesity is one of the most signifi cant health problems worldwide. Bariatric surgery has become one of the fastest
growing operative procedures and has gained acceptance as the leading option for weight-loss. Despite improvement
in the performance of bariatric surgical procedures, complications are not uncommon. There are a number of
unique complications that arise in this patient population and require specifi c knowledge for proper management.
Furthermore, conditions unrelated to the altered anatomy typically require a different management strategy. As
such, a basic understanding of surgical anatomy, potential complications, and endoscopic tools and techniques for
optimal management is essential for the practicing gastroenterologist. Gastroenterologists should be familiar with
these procedures and complication management strategies. This review will cover these topics and focus on major
complications that gastroenterologists will be most likely to see in their practice.
Am J Gastroenterol 2017; 112:1640–1655; doi: 10.1038/ajg.2017.241; published online 15 August 2017
1 Division of Gastroenterology, Hepatology and Endoscopy, Brigham and Women’s Hospital , Boston , Massachusetts , USA ; 2 Harvard Medical School , Boston ,
Massachusetts , USA . Correspondence: Christopher C. Thompson, MD, MSc, FACG, FASGE, AGAF, Division of Gastroenterology, Hepatology and Endoscopy,
Brigham and Women's Hospital , 75 Francis St, ASB II , Boston , Massachusetts 02115 , USA . E-mail: [email protected] Received 27 January 2017 ; accepted 27 June 2017
CME
Complications of Bariatric Surgery
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
RE
VIE
W
1641
be absorbable or non-absorbable. In some procedures, a silastic
ring is placed at the level of the GJA in an eff ort to enhance dura-
bility. In addition, placement of the Roux limb can be performed
antegastric (“antecolic”) or retrogastric (“retrocolic”). Jejunojeju-
nal anastomosis can be constructed in an end-to-side or side-to-
side confi guration. Furthermore, limb lengths vary considerably
depending on the operator. All of these variants have specifi c
implications to the risk profi le of the RYGB ( Table 1 ).
Anastomotic ulceration
Ulceration at the GJA, also known as marginal ulceration, is
a common complication of RYGB, occurring in up to 16% of
patients. It can occur anytime postoperatively. It is diagnosed by
upper endoscopy and is typically located on the jejunal aspect of
the GJA ( Figure 2a ). Patients are oft en asymptomatic, suggesting
the incidence may be much higher. When symptoms do occur,
they can include epigastric pain, obstructive symptoms, or gastro-
intestinal bleeding. Further complications include stenosis and
rarely perforation.
Th e etiology of marginal ulceration is likely multifactorial
( 9–12 ). While the mechanisms underlying the development of this
complication have not been fully elucidated, there is substantial
evidence that acidity plays a signifi cant role in the disease patho-
physiology. Poor local tissue perfusion from ischemia or tension at
the site of the anastomosis, in addition to foreign materials (e.g.,
suture, staple), microvascular ischemia from smoking or poorly
controlled diabetes, and medications including but not limited to
non-steroidal anti-infl ammatories (NSAIDs) also play an impor-
tant role in ulcer development. Furthermore, surgical technique
may be relevant, with the majority of studies demonstrating higher
rates of marginal ulceration with the use of circular staplers and
non-absorbable sutures ( 13,14 ). However, the incidence varies
greatly between clinical series utilizing the same surgical tech-
nique, further supporting a multifactorial etiology to the devel-
opment of marginal ulceration. While the relationship between
Helicobacter pylori infection and the development of marginal
ulceration is controversial, a recent nationwide analysis suggests a
strong association ( 15–21 ). A complete list of predisposing factors
is shown in Table 2 .
Th e majority of patients with marginal ulceration respond to
medical therapy which includes high dose proton pump inhibi-
tors (PPIs) and oft entimes the addition of sucralfate solution (not
tablets), especially as adjunctive therapy or in patients already tak-
ing a PPI at the time the ulcer is discovered ( 22 ). Administration
of a soluble or open capsule form of PPI is essential as it allows
enhanced absorption in the Roux limb and common channel due
to increased gastrointestinal transit time post-RYGB, and this
method of administration has been shown to signifi cantly decrease
time to ulcer healing and overall healthcare utilization ( 23 ). Smok-
ing cessation and indefi nite discontinuation of NSAIDs are also
important to promote healing. Removal of foreign material such as
sutures and staples should also be performed if RYGB surgery was
Laparoscopicadjustablegastric banding(LAGB)
Roux-en-Ygastric bypass(RYGB)
a
b c
d e f
Retrocolicgastric bypass Antecolic
gastric bypass
Sleevegastrectomy
Verticalbandedgastroplasty
Figure 1 . Overview of bariatric surgeries. Bariatric surgeries including Roux-en-Y gastric bypass ( a ) with retrocolic ( b ) and antecolic ( c ) anatomy, gastric
banding ( d ), sleeve gastrectomy ( e ), and vertical banded gastroplasty ( f ) ( 136 )*. * with permission.
Schulman and Thompson
The American Journal of GASTROENTEROLOGY VOLUME 112 | NOVEMBER 2017 www.nature.com/ajg
RE
VIE
W1642
Table 1 . Complications of common bariatric procedures
Type of
Surgery
Complication Symptom(s) *Time of
onset since
surgery
Diagnostic tips Management strategies
RYGB
Anastomotic ulceration Epigastric pain
N/V
Bleeding
Often
asymptomatic
Early or late Do not advance endoscope deeply
beyond area of ulceration
H. pylori stool antigen or serology
High-dose PPI (soluble form) +/−
sucralfate
Stop smoking
No NSAIDs
Consider suture removal
Anastomotic stenosis Dysphagia
N/V
Malnutrition
Late Upper endoscopy
Avoid UGI series given aspiration risk
Look for concomitant ulceration
Stepwise endoscopic balloon dilation
Do not over-dilate (≤15 mm)
Carefully direct wire into distal Roux
limb
Foreign body removal
LAMS for concomitant ulceration
Gastrogastric fi stula Weight regain
Epigastric pain
Refl ux
N/V
Anytime Upper GI series sensitive
EGD important to confi rm and rule
out ulceration
If asymptomatic: PPI+dietary
counseling
If symptomatic: closure (endoscopic
[<1 cm] vs. surgical)
Surgical leaks Tachycardia
C-reactive protein
Leukocytosis
Post-operative
or early
Cross-sectional imaging
High false negative rates for all
studies
Depends on location of leak and
timing since surgery; see text
Stents for acute pouch and GJ leaks
Clips for JJ leaks
Chronic walled-off leaks treat like
necrosectomy
Intestinal obstruction Abdominal pain (often
intermittent)
N/V
Anytime Cross-sectional imaging while the
patient is symptomatic
Surgery
Endoscopy is not indicated for extra-
luminal causes of obstruction
Choledocholithiasis Right upper quadrant
abdominal pain
Late RUQ u/s
Cross-sectional imaging
MRCP
Device-assisted enteroscopy, laparo-
scopic-assisted ERCP, possible EUS
directed ERCP
Dilated gastrojejunal
anastomosis
Weight regain Late Upper endoscopy
Dilation confi rmed with GJA>15 mm
Endoscopic revision (TORe)
APC for compliant yet not markedly
dilated GJA
LAGB
Refl ux esophagitis GERD Late Upper endoscopy High-dose PPI +/− sucralfate
Band defl ation
Esophageal dilitation Dysphagia
Refl ux
Epigastric discomfort
Late Upper endoscopy
Upper GI series
Band defl ation
Surgical replacement or conversion
Band erosion Pain
N/V
Weight loss
Sepsis
Late Upper endoscopy Endoscopic removal of band if
buckle is visible, with surgical
removal of port
Band slippage Vomiting
Epigastric pain
Late UGI Surgery
Sleeve gastrectomy
Sleeve stenosis Dysphagia,
N/V
Abdominal pain
Anytime Distinguish between stenosis and
twisting; consider imaging
Endoscopic pyloric dilation (hydro-
static to 20 mm) and pneumatic
balloon dilation of sleeve (starting at
30 mm)
Twisted sleeves less likely to respond
Sleeve leaks Tachycardia
C-reactive protein
Leukocytosis
Post-operative
or early
Cross-sectional imaging Depends on timing since surgical
procedure; see text
Acute: stent
Chronic: treat like necrosectomy
Esophageal pathology GERD Late Upper endoscopy High dose PPI +/− sucralfate
Surgical conversion to RYGB
Table 1 continued on following page
Complications of Bariatric Surgery
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
RE
VIE
W
1643
performed at least six weeks prior, and this can be accomplished
by the use of biopsy or rat-tooth forceps, or endoscopic scissors
( 24 ). Testing for H. pylori is also recommended, and should be
accomplished by fecal antigen, or serology in immunocompetent
patients who are treatment naïve, as in our experience pouch biop-
sies and breath tests are less reliable in this patient population as
the majority of the stomach where H. pylori resides is inaccessible.
Independent of etiology, we recommend repeat endoscopy in two
to three months to confi rm ulcer healing. Of note, marginal ulcer-
ation complicated by stenosis is particularly diffi cult to manage,
and more likely to require surgical intervention.
Endoscopic suturing techniques in the treatment of recalcitrant
marginal ulceration have demonstrated technical feasibility, safety,
and effi cacy in small series, although additional studies regard-
ing durability are needed ( 25 ). Surgical revision is performed in a
small percentage of patients who do not improve with maximum
medical management, in whom endoscopic techniques are not
successful, or in whom perforation has occurred ( 26 ). Unfortu-
nately, reoperation carries signifi cant morbidity and a 7.7% recur-
rence rate ( 27 ).
Anastomotic stenosis
Stenosis of the GJA is perhaps the most common complications
in RYGB and has been reported in as many as 20% of patients,
however, the majority of studies report incidence in the single dig-
its ( 28–39 ) ( Figure 2b ). Patients can present from weeks to years
post-operatively with progressive dysphagia, nausea, vomiting,
and malnutrition. Some patients may paradoxically have weight
gain as they convert to higher calorie full liquid diets. While the
exact mechanism of stenosis is unknown, ulceration and ischemia
at the GJA, in addition to subclinical anastomotic leak, and
smaller diameter circular staplers used during the initial surgery
are likely contributory factors ( 37–39 ).
Although there is no precise defi nition for stomal stenosis, the
diagnosis is typically made when a patient is symptomatic and
a standard upper endoscope is unable to pass through the GJA.
Endoscopic balloon dilation is fi rst-line for management of this
condition ( Figure 3 ). As the GJA is an end-to-side anastomosis
with a thin jejunal wall directly behind the gastric aspect, care
must be taken to advance the balloon into the Roux limb proper
without traumatizing the adjacent jejunum or blind portion of
the Roux limb. If resistance is met despite careful repositioning,
a fl exible wire may be used as a guide, and rarely an ultrathin
upper endoscope may be required to assist in wire advancement.
Some patients will require multiple procedures to achieve dura-
ble results, and the procedure is safe with a complication rate of
<3% ( 31–33,35,40 ). Dilation should be performed with the goal
of achieving symptom resolution and a durable stomal diameter
of roughly 8–12 mm. Dilation above 15 mm should be performed
in rare circumstances where the patient remains symptomatic
despite having achieved a stable anastomotic diameter that
allows endoscope passage without resistance. Dilation to larger
diameters is associated with increased complications including
perforation and weight regain. It is important to exercise cau-
tion in the setting of coexistent marginal ulceration because this
may increase the risk of perforation and are more likely to require
surgical revision.
Other therapeutic techniques to treat stomal stenosis have also
been described including needle-knife electroincision, intral-
esional steroid injection, and placement of lumen apposing metal
stent ( 41–43 ), the latter of which is particularly helpful in concom-
itant ulceration ( Figure 3 ). Surgical revision for refractory stenosis
is required in approximately two percent of cases ( 44 ).
Gastrogastric fi stula
An abnormal connection between the gastric pouch and the
excluded stomach is known as a gastrogastric fi stula (GGF)
( Figure 2c ). Th ere are several postulated etiologies for the
development of this complication, including surgical technique
without complete division or transection of the gastric pouch,
marginal ulceration, anastomotic leak, and foreign body ero-
sion ( 45–47 ).
Table 1 . Continued
Type of
Surgery
Complication Symptom(s) *Time of
onset since
surgery
Diagnostic tips Management strategies
VBG
Anastomotic stenosis Dysphagia
N/V
Malnutrition
Late Upper endoscopy Endoscopic balloon dilation
Staple line dehiscence Weight regain Anytime Upper endoscopy Surgery
Band erosion Pain
N/V
Weight loss
Sepsis
Late Upper endoscopy Endoscopic removal if band is
silastic
APC, argon plasma coagulation; GERD, gastroesophageal refl ux disease; GJA, gastrojejunal anastomosis; LAGB, laparoscopic adjustable gastric banding; MRCP, mag-
netic resonance cholangiopancreatography; RUQ, right upper quadrant; RYGB, Roux-en-Y gastric bypass; UGI, upper gastrointestinal series.
*Post-operative: immediate post-operative period; early: <30 days; late: ≥30 days.
Schulman and Thompson
The American Journal of GASTROENTEROLOGY VOLUME 112 | NOVEMBER 2017 www.nature.com/ajg
RE
VIE
W1644
persistent symptoms clearly attributable to the fi stula. Tradition-
ally, this has been accomplished with surgical revision. However,
newer per-oral approaches using endoscopic suturing systems
carry decreased morbidity, and sustain successful closure in ~20%
of patients at 12 months ( 49,50 ). Endoscopic repair is especially
eff ective when the fi stula is less than one centimeter ( 50,51 ). Sur-
gical revision following unsuccessful suturing appears to be safe.
Use of over-the-scope clips has also been reported, but should be
used with caution, as unlike with endoscopic suturing techniques,
these may interfere with subsequent revision surgery should it be
required ( 52–54 ).
Surgical leaks
Leaks are among the most serious complications and typically
occur within days of the procedure, but can also present in a
more delayed fashion. Th e incidence ranges from 0.1 to 5.6 per-
cent, and is much higher following revision surgery ( 55–58 ).
Th e typical presenting symptom is weight regain or inability to
lose weight as food does not bypass the remnant stomach. Pain,
refl ux, nausea, emesis, and marginal ulceration are also oft en
reported ( 43,48 ). Th e diagnosis is most reliably made by upper gas-
trointestinal series or upper endoscopy, although cross-sectional
imaging can also demonstrate this fi nding ( Figure 4a,b ). Never-
theless, there is a high false positive rate with this approach, as con-
trast can refl ux into the remnant stomach from the duodenum. A
defi nitive diagnosis should be reserved for when an actual fi stula
is seen, and not just contrast in the remnant stomach. Once con-
fi rmed, high dose PPI should be administered to prevent gastric
acid production in the remnant stomach from entering the gastric
pouch and jejunum through the GGF, as this can lead to abdomi-
nal pain and development of marginal ulceration, and potential
stenosis ( Figure 2d ).
GGF may be managed conservatively with PPI therapy and
dietary counseling. Closure is indicated when the patient has
a b
c d
>30 mm
e f
Figure 2 . Endoscopic examples of gastric bypass complications. Endoscopic examples of complications of gastric bypass including marginal ulceration
( a ), stenosis of the gastrojejunal anastomosis ( b ), gastrogastric fi stula (single arrow) with gastrojejunal anastomosis (double arrow) ( c ), gastrogastric fi stula
(triple arrows) complicated by marginal ulceration leading to stenosis of gastrojejunal anastomosis (single arrow) ( d ), staple line leak in gastric pouch ( e ),
and dilated gastrojejunal anastomosis ( f ).
Complications of Bariatric Surgery
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
RE
VIE
W
1645
Tachycardia, leukocytosis, and elevated C-reactive protein are
the most common presenting fi ndings, and any one of these
should trigger appropriate supportive care and an expedited
evaluation ( 59 ).
Th ese leaks can occur at multiple points along any staple line
including the gastric pouch ( Figure 2e ), the GJA, the blind por-
tion of the Roux limb, the jejunojejunal anastomosis, and the rem-
nant stomach ( Figure 5 ). Before any therapy is undertaken, it is
important to identify the location of the leak using cross sectional
imaging or combined endoscopic and fl uoroscopic interrogation
of possible sites, as that will dictate the appropriate management.
In addition, it is important to treat downstream obstruction and
remove foreign material from the leak site. Th is includes staples,
sutures, and drains that may be in close proximity.
Endoscopic placement of self-expandable metal stents is eff ec-
tive in the treatment of proximal leaks of the pouch or GJA that
occur in the acute setting ( 60–70 ). Stent migration occurs in
16.9% of patients with rare serious complication ( 58 ). Optimal
time for stent removal is between 6 and 8 weeks, with leak reso-
lution rate of 87.8% ( ref. 58 ). Stents are the preferred treatment
method for leaks in these locations, as it is eff ective and there
is less evidence for the use of other modalities. In chronic leaks
with a walled-off cavity, these modalities are less eff ective, and
treating the collection as walled-off necrosis and ultimately plac-
ing plastic double pigtail stents between the cavity and the gastric
lumen (as detailed below in the sleeve gastrectomy section) is
oft en required ( 71,72 ).
Leaks at other locations are typically not amenable to stent-
ing. Other therapeutic options include clips, over-the-scope clips,
endoscopic suturing, tissue sealants and biochemical matrices.
Th ese modalities have variable results, and the evidence for their
use is limited to case series ( 68,73–75 ).
Table 2 . Etiology of Marginal Ulceration
Predisposing factors
Surgical Technique
Smoking
NSAID use
Alcohol
Lack of PPI use
Factors implicated in the physiopathology
H. pylori
Infl ammation
Foreign body reaction
Acid secretion
Bile refl ux
Fistula
Ischemia
NSAID, non-steroidal anti-infl ammatory.
*Reproduced from Fernandez-Esparrach G, Guarner-Argente C, and Bordas
JM. Ulceration in the Bariatric Patient. Bariatric Endoscopy . Springer
Science+Business Media; 2013, with permission.
a b
c d e
Figure 3 . Management of stenosis of the gastrojejunal anastomosis in gastric bypass. Endoscopic management of stenosis of the gastrojejunal anastomosis
without ulceration ( a ) with balloon dilation ( b ); endoscopic management of stenosis of the gastrojejunal anastomosis with ulceration ( c ) placement of a
lumen apposing metal stent ( d ), and resolution of stenosis and subsequent ulcer healing ( e ).
Schulman and Thompson
The American Journal of GASTROENTEROLOGY VOLUME 112 | NOVEMBER 2017 www.nature.com/ajg
RE
VIE
W1646
Intestinal obstruction
Early post-operative bowel obstruction following gastric bypass
occurs at similar rates to other abdominal surgeries. Late bowel
obstruction will be more commonly seen in a gastroenterology
practice, and includes ventral incisional and internal hernias,
adhesions, and intussusceptions ( 76,77 ).
Adhesions and ventral incisional hernias occur more commonly
following open gastric bypass surgery. Both of these entities pre-
sent with pain or obstructive symptoms, with the latter classically
also causing a visible bulge. Internal hernias, on the other hand,
are more common following a laparoscopic surgical approach, and
have a reported incidence of 3–16% ( ref. 78–81 ). Th ere are three
mesenteric defects created during RYGB through which hernias
occur including the jejuno-jejunostomy, the space between the
transverse mesocolon and Roux-limb mesentary (i.e., Peterson’s
defect), and in the transverse mesocolon in patients with a retro-
colic Roux-limb. Computed tomography (CT) may demonstrate
swirled vessels or fat at the root of the mesentary ( Figure 4c ), a
fi nding which is known to have the highest sensitivity and speci-
fi city for making the diagnosis. However, these oft en occur inter-
mittently making radiographic detection diffi cult, and therefore
imaging should be performed while the patient is symptomatic
and there should be a low threshold for re-exploration is indicated
in bariatric patients with unexplained pain or symptoms of bowel
obstruction ( 82 ). If left undetected, bowel necrosis can occur
requiring large segment bowel resection.
a
b
c d
Figure 4 . Radiographic examples of gastric bypass complications. Computed tomography ( a ) and upper gastrointestinal series ( b ) demonstrating evidence
of gastrogastric fi stula; computed tomography demonstrating internal hernia ( c ) with arrows showing swirled vessels and fat at the root of the mesentary
and ( d ) intussusception with arrows showing telescoping of bowel.
Gastric pouch
1
5
4
2
3Remnantstomach
Roux limb
Biliopancreaticlimb (75–150 cm)
Commonlimb
Cecum
Duodenum
Commonbile duct
Gastrojejunostomy
Blind limb
Jejuno-jejunal anastomosis
Ligamentof Treitz
Figure 5 . Multiple points of gastric leak following RYGB.
Complications of Bariatric Surgery
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
RE
VIE
W
1647
Intussusception is most commonly seen at the jejunojejunal
anastomosis, where the common limb telescopes through in a
retrograde fashion (distal to proximal) ( Figure 4d ). Th e reported
incidence rates range from 0.1 to 1%, and it oft en presents with sig-
nifi cant weight loss ( 80,83,84 ). Th e etiology is not well understood
but appears to be multifactorial, possibly involving a lead point
(suture lines, food boluses or adhesions), motility disturbances,
or thinning of intestinal mesentery that occurs with weight loss
and allows increased mobility of the bowel and an unstable region
around the site of the Roux limb ( 80,83,84 ). Endoscopy is not typi-
cally useful in these patients.
Cholelithiasis
Gallstone disease is common following RYGB. It is estimated
to occur in 28 to 71 percent of patients within six months fol-
lowing surgery, and as many as 40 percent of these patients are
symptomatic ( 85 ). Rapid weight loss may increase the choles-
terol saturation in the bile and the gallbladder mucin concentra-
tion, increasing the risk of gallstone development. Postoperative
anatomical changes and compromised gallbladder emptying
may also play a role ( 85–90 ). In addition, cholecystectomy is less
commonly performed in the era of laparoscopic RYGB. As such,
gastroenterologists are seeing these patients more frequently.
Endoscopic retrograde cholangiopancreatography (ERCP) is
particularly arduous in RYGB anatomy due to the relative inac-
cessibility of the duodenum and ampulla, making treatment
of choledocholithiasis challenging. Surgical technique plays in
important role in likelihood of success, as long a Roux limbs and
side-to-side jejunojejunal anastomosis poses even more diffi -
culty to the endoscopist. Oft entimes the procedure is attempted
using a pediatric colonoscope, spiral overtube, balloon-assisted
enteroscope, or a duodenoscope back-loaded onto a guidewire.
Balloon-assisted enteroscopy is the most well described pro-
cedure, with pooled procedural success rates of 62% ( ref. 91 ).
Alternative approaches include passage through a gastrogastric
fi stula if present with dilation if necessary, placement of a pro-
phylactic gastrostomy tube into the bypassed stomach, or EUS-
directed gastrostomy ( 92 ). A controversial emerging procedure is
the endoscopic ultrasound-directed transgastric ERCP (EDGE)
procedure, where a lumen-apposing metal stent is placed through
the gastric pouch and into the remnant stomach to allow access.
Th is stent is later removed and carries a risk of a persistent gastro-
gastric fi stula ( 93,94 ).
Failure to lose weight or weight regain
RYGB is associated with 15–35% failure, defi ned as inability to
achieve signifi cant weight loss (>50% loss of excess weight) or
excessive weight regain aft er initial adequate weight loss ( 8,95–98 ).
A signifi cant minority of these patients experience substantial
weight regain even two years post-surgical aft er RYGB ( 8,96–99 ).
In addition, studies have demonstrated that, on average, patients
have regained one third of the maximum weight lost 10 years fol-
lowing RYGB ( 100 ). Dietary non-compliance is contribute known
risk factor for weight regain. It has also been demonstrated that
anatomical changes such as dilation of the GJA ( Figure 2f ), and
development of gastrogastric fi stula ( Figure 2c,d ) play a signifi -
cant role in promoting weight regain ( 101 ).
Endoscopic suturing, plication devices, argon plasma coagula-
tion and other forms of thermal therapy ( 102–106 ) used to tighten
the stoma and reduce pouch volume have proven to be technically
feasible and safe, with recent studies showing sustained weight loss
at three years, and suturing demonstrating level I evidence in a
randomized sham-controlled trial ( 107 ). Th ese endoscopic thera-
pies off er a less invasive treatment option for post-bypass weight
regain, with minimal morbidity.
Nutritional abnormalities
Metabolic and nutritional defi ciencies are not uncommon fol-
lowing RYGB, as reconfi guration of gastrointestinal anatomy,
alteration in motility, pH and enzymatic profi les can lead to
derangements. Th ere should be a low threshold to evaluate and
treat nutritional defi ciencies aggressively. Common nutritional
defi ciencies and clinical symptoms are shown in Table 3 .
Dumping syndrome
Dumping syndrome following RYGB occurs when large quanti-
ties of simple carbohydrates are ingested. Early dumping occurs
within 15 min of ingestion and has been attributed to rapid fl uid
shift s from the plasma into the bowel due to hyperosmolality of
the food. Symptoms include both gastrointestinal complaints
(abdominal pain, diarrhea, bloating, and nausea) and vasomotor
changes (fl ushing, palpitations, perspiration, tachycardia, hypo-
tension, and syncope). Treatment includes avoidance of foods that
are high in simple sugar content, in addition to small frequent
meals in which liquids and solids are separated. Late dumping
results from hyperglycemia and the subsequent insulin response
leading to hypoglycemia, and occurs several hours aft er eating
with resultant symptoms due to low serum glucose (perspiration,
palpitations, weakness, confusion, tremor, and syncope). Treat-
ment includes similar dietary modifi cation, with medications
such as acarbose, an alpha-glucosidase inhibitor, reserved for
non-responders. Each of these conditions may present as a spec-
trum of symptoms captured by the Sigstad scoring system ( 108 ).
Abdominal pain
Abdominal pain is one of the most common reasons for gastro-
enterology consultation in the post-surgical population and is
not unique to gastric bypass. A standard abdominal pain work-
up evaluating potential etiologies unrelated to bariatric surgery
should be pursued as appropriate. Th ere are also several etiolo-
gies specifi c to post-surgical anatomy that must be considered.
Patient history and physical examination are oft en essential in
making the diagnosis. Careful evaluation for a Carnett’s sign is
important, as abdominal wall pain is common. Carnett’s sign is
elicited by having the patient lie fl at on an examination table, and
identify the point of maximal abdominal tenderness ( 109 ). Th e
physician then focally compresses this area with continuous pres-
sure and instructs the patient to lift their legs off the table, tens-
ing abdominal musculature. If the focal pain intensifi es, this is a
positive sign suggesting an abdominal wall syndrome. Th e most
Schulman and Thompson
The American Journal of GASTROENTEROLOGY VOLUME 112 | NOVEMBER 2017 www.nature.com/ajg
RE
VIE
W1648
line diagnostic study. Endoscopy may also be therapeutic if pain
is due to retained foreign body such as suture material ( 24 ). If the
pain is intermittent, positional, or severe, cross-sectional imaging
should be initially performed to evaluate for potential intestinal
obstruction such as volvulus, intussusception, or internal hernia.
common treatment for abdominal wall pain is trigger point injec-
tion, whereby a local anesthetic is injected directly into the site of
pain. Prioritization of diagnostic studies depends on presenting
symptoms. If consistent mid-epigastric pain is present suggesting
marginal ulceration, upper endoscopy is recommended as a fi rst
Table 3 . Common nutritional defi ciencies and symptoms in Roux-en-Y gastric bypass
Defi ciency Common symptoms
Fat-soluble vitamins
Vitamin A Conjunctival dryness
Retinopathy
Night blindness
Dermatologic changes
Immune system impairment
Vitamin D Often asymptomatic (if mild-moderate)
Demineralization of bones, osteomalacia (if severe)
Weakness
Fracture
Vitamin E Neuromuscular disorders
Hemolytic anemia
Vitamin K Impaired coagulation leading to bruisability, mucosal bleeding.
Prolonged prothrombin time (PT)
Water-soluble vitamins
Thiamine (vitamin B1) Wernicke encephalopathy (encephalopathy and confabulation, oculomotor
dysfunction, ataxia)
Vitamin B12 Pernicious (megaloblastic) anemia
Folate Megaloblastic anemia
Vitamin C Petechiae
Gingivitis
Arthralgias
Poor wound healing
Trace minerals
Iron Hypochromic, microcytic anemia
Zinc Impotence
Impaired immune function
Hair loss
Copper Microcytic anemia
Neutropenia
Ataxia
Selenium Skeletal muscle dysfunction
Cardiomyopathy
Other
Calcium Metabolic bone disease
Secondary hyperparathyroidism
Protein Protein energy malnutrition
Complications of Bariatric Surgery
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
RE
VIE
W
1649
Th is imaging should ideally be performed when the patient is
symptomatic, which increases the sensitivity. Right upper quad-
rant pain may warrant ultrasound, cross-sectional imaging, or
magnetic resonance cholangiopancreatography (MRCP) to evalu-
ate for cholelithiasis or cholodocholithiasis as a fi rst line test.
For diff use or lower abdominal discomfort, abdominal bloating,
and change in bowel habits, hydrogen or methane breath tests to
evaluate for small intestinal bacterial overgrowth (SIBO) should
also be part of the work-up. Th ese studies may be fraught with false
positives, as there is also faster transit time in RYGB patients ( 110 ).
As such, transit time to the colon should be estimated by small
bowel follow-through, and the breath test evaluated in light of
patient specifi c results. If the pain is generalized or predominantly
in the left upper quadrant, enteroscopy to the remnant stomach
may also be considered to look for remnant gastropathy or other
gastric remnant pathology. Th is is critical in patients that also
have unexplained anemia. For patients without anemia and who
are high risk for procedural intervention, we recommend obtain-
ing cholescintigraphy (99mTc-heapto-iminodiacetic acid (HIDA)
scanning), which allows for a radiolabeled substance to be taken
up selectively by hepatocytes and excreted into bile, thereby pro-
viding information about bile fl ow. Pooling of bile in the remnant
stomach suggests a positive test. Recent studies suggest that this
may off er a non-invasive alternate diagnostic strategy for iden-
tifying increased risk for bile acid gastropathy ( 111 ). If refl ux to
the remnant stomach is noted, then use of ursodiol, in addition
to PPI therapy, has been shown to eff ectively treat this condition
in small studies, and we have found it to be a useful management
strategy ( 111 ).
Surgical management
For chronic marginal ulceration or gastro-gastric fi stula, revision
of RYGB reconstituting the normal RYGB anatomy is being per-
formed more commonly and safely. Reversal of RYGB is an option
for patients with excessive weight loss, dumping syndrome, per-
sistent nausea and emesis. Esophagojejunostomy is reserved for
persistent leaks in the proximal pouch as it is a relatively morbid
procedure. Surgical revisions for weight regain, including Roux
limb distalization, are also performed when less invasive options
are not successful.
LAPAROSCOPIC ADJUSTABLE GASTRIC BANDING
Laparoscopic adjustable gastric banding involves the insertion of
an adjustable, prosthetic band over the cardia of the stomach to
form a gastric pouch with roughly 15 ml capacity ( Figure 1b ). Th e
mechanism of action for this procedure is primarily restrictive in
nature. Th e gastric band consists of a silicone ring connected to
an infusion port, the latter of which remains in the subcutaneous
tissue and can be easily accessed for fl uid injection to increase the
degree of restriction, thus rendering it fl exible to meet the chang-
ing needs of the patient. While this procedure has the lowest peri-
operative complication rate and mortality among all bariatric
procedures, there are several disadvantages including presence of
a foreign body.
Refl ux esophagitis
Acid refl ux and esophagitis are common following banding
procedures ( 112–115 ) ( Figure 6a ). A systematic review demon-
strated newly developed refl ux symptoms aft er gastric banding in
up to 50% of patients without prior symptoms, and new esophagi-
tis confi rmed in up to 38.4% ( ref. 113 ). Treatment involves acid-
suppression therapy with or without sucralfate, as well as referral
to a surgeon for potential defl ation of the band.
Esophageal dilation
An achalasia-like syndrome can occur in less than ten percent
of patients and results from esophageal dilation proximal to the
band ( 116–119 ) ( Figure 6b ). Excessive fi lling of the band can
precipitate this condition and cause symptoms of refl ux, epigas-
tric discomfort, and inability to tolerate oral intake. Treatment
involves fl uid removal via the subcutaneous port (“band holiday”)
with reevaluation in 6 weeks ( 120 ). If this is not eff ective, replace-
ment of the band in a new location, or conversion to an alternative
bariatric procedure, is the typical course of action.
Band erosion
Band erosion, or intragastric migration, occurs in less than
6.8 percent of patients ( 121 ). Mean time to occurrence of 22.5
months post operatively, with a range of weeks to years ( 121,122 ).
Early erosions are usually attributed to undetected perforations
during surgery or early infection, while late erosions may be the
a b c
Figure 6 . Endoscopic examples of laparoscopic adjustable gastric banding complications. Severe refl ux esophagitis ( a ), pseudoachalasia following lap-
band placement ( b ) and lap band erosion ( c ).
Schulman and Thompson
The American Journal of GASTROENTEROLOGY VOLUME 112 | NOVEMBER 2017 www.nature.com/ajg
RE
VIE
W1650
( refs 129,130 ). Over-sewing the staple line or use of a bougie that
is too small both predispose to narrowing at these locations. Rota-
tion of the stomach during stapling can also lead to a twisted and
narrowed sleeve.
Symptoms of obstruction can occur depending on the sever-
ity of the narrowing. Th is diagnosis is typically made by endo-
scopy or upper gastrointestinal series, and endoscopic dilation
is the primary mode of management. We recommend starting
with a hydrostatic balloon, and dilating both the pylorus and the
incisura to 20 mm. If there is no symptomatic improvement, use
of a pneumatic dilation balloon is then recommended at the level
of the gastric stenosis. We recommend starting with a 30 mm bal-
loon. Depending on resistance, maximal PSI may not be reached
in the fi rst session. In two weeks the procedure is repeated with
the same size balloon if maximum PSI was not reached, or with
a balloon fi ve mm greater in size. Th is process is repeated every
two weeks as needed until symptoms resolve ( Figure 7 ). A recent
study has demonstrated 96% effi cacy when using this algorithm
( 131 ). It is important to ensure the pneumatic balloon is not span-
ning the gastroesophageal junction or the pylorus to minimize risk
of perforation. If the sleeve is twisted, this technique is oft en less
eff ective.
Sleeve leaks
One complication that is common and particularly bothersome
is leak following sleeve gastrectomy. Th is complication has been
reported in up to 5.3 percent of patients, and usually occur along
the superior aspect of the staple line just below the gastroesopha-
geal junction ( 132 ). Th ese patients present in a more delayed fash-
ion than aft er RYGB.
Endoscopic approaches have proven successful, and off er a
less invasive fi rst line therapy for many patients. Th e timing of
presentation for sleeve leaks aff ects management strategy and
the literature supports diff erent time cut-off s in this regard.
If the leak occurs early (i.e., within six weeks following sleeve
gastrectomy) we recommend stent placement with simultane-
ous dilation of the pylorus to treat downstream obstruction. If
the leak is delayed and the collection is walled-off ( Figure 8 ),
we instead recommend dilation of the pylorus and distal sleeve,
and approach the collection in a manner similar to endoscopic
necrosectomy technique ( 71,72 ). In this approach, an endo-
scope is advanced into the collection and is used to mechani-
cally debride non-viable tissue and perform antibiotic lavage
with subsequent placement of pigtail stents for ongoing drain-
age. Other centers report use of a needle-knife fenestration
technique ( 133,134 ). Both of these approaches allow healing by
secondary intention.
Gastroesophageal refl ux disease and Barrett’s esophagus
Sleeve gastrectomy may predispose to esophageal pathology
including gastroesophageal refl ux disease and Barrett’s esopha-
gus. While some studies have failed to consistently demonstrate
an association, new evidence suggests that patients who have
undergone sleeve gatrectomy may be at substantially higher risk
of developing these complications. A recent study found that the
consequence of gastric wall ischemia from an excessively tight
band. Clinical manifestations of this complication can include
refl ux, nausea and vomiting, epigastric pain, excessive weight loss,
and life-threatening sepsis. In addition, if the site of erosion occurs
into the posterior part of the stomach near the cardioesophageal
junction, massive hematemesis can occur from involvement of the
gastric artery ( 123 ). Th e fi nding of abdominal cellulitis (overlying
the port) also indicates likely band erosion and warrants further
investigation. Diagnosis can be made endoscopically ( Figure 6c ),
and if the band buckle is visible, removal may be accomplished at
the time of the procedure, using a stiff guidewire and mechanical
lithotripter ( 124,125 ). Th is requires the patient to be under gen-
eral anesthesia, and that a surgeon is available to remove the sub-
cutaneous port (which can be performed in endoscopy). Th e wire
is fed through the opening of the band and the ends are placed
into the mechanical lithotripter. Th e band is then severed and can
be pulled out through the mouth.
Band slippage
Band slippage leads to prolapse of a portion of the stomach
through the band, and is one of the most common and bother-
some late complications of gastric banding. Patients oft en present
with vomiting and epigastric pain, and should prompt surgical
consultation.
Port infection or malfunction
Th e mechanical port component of the adjustable band device
exposes the patients to infectious complications given the pres-
ence of a foreign body, in addition to the inevitable consequences
of device weathering, which can lead to its failure ( 126–128 ).
Endoscopy is of no therapeutic value in this setting.
Surgical management
Laparoscopic adjustable banding can be easily reversed with
endoscopic or surgical removal of the band. Th is is oft en done for
failure of effi cacy or the aforementioned complications. Conver-
sion to other bariatric procedures such as sleeve gastrectomy or
RYGB is commonly and safely performed.
SLEEVE GASTRECTOMY
Laparoscopic sleeve gastrectomy is a procedure in which a large
portion of the greater curvature of the stomach is removed, leav-
ing just a small conduit along the lesser curvature. In so doing,
this procedure eff ectively removes fundal ghrelin-producing cells
and increases gastric emptying, which is associated with a vari-
ety of metabolic consequences leading to weight loss ( Figure 1c ).
Mechanistically, ghrelin levels decrease following sleeve gastrec-
tomy, and this is believed to aff ect appetite regulation. In addi-
tion, hind gut mechanisms including post-prandial increase in
Peptide-YY and GLP-1 are thought to play a role ( 6–8 ).
Sleeve stenosis
Stenosis following sleeve gastrectomy classically occurs at the
incisura ( Figure 7 ). Th e incidence is reported to be 0.7–4%
Complications of Bariatric Surgery
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
RE
VIE
W
1651
incidence of GERD symptoms signifi cantly increased compared
with preoperative values (68.1% vs. 33.6%). Furthermore, PPI intake
similarly increased following surgery (57.2% vs. 19.1%). Finally,
a signifi cant increase in the incidence and severity of erosive
esophagitis was evidenced, and a signifi cant number of patients
were diagnosed with non-dysplastic Barrett’s esophagus ( 135 ).
As the prevalence of sleeve gastrectomy increases, the develop-
ment of these conditions should be monitored closely.
Surgical management
For complications not amenable to endoscopic or medical therapy,
surgical options are available. For refractory severe erosive
a b
c
Figure 7 . Management of stenosis of the incisura in sleeve gastrectomy. Sleeve gastrectomy complicated by stenosis of the incisura with pooling of bile
acid ( a ) managed by pneumatic balloon dilation under endoscopic ( b ) and fl uroscopic ( c ) guidance.
a b
Figure 8 . Management of late leak in sleeve gastrectomy. Sleeve gastrectomy complicated by late leak presenting with contained walled-off necrosis ( a )
managed by debridement and subsequent stent placement through leak site (arrow) ( b ).
Schulman and Thompson
The American Journal of GASTROENTEROLOGY VOLUME 112 | NOVEMBER 2017 www.nature.com/ajg
RE
VIE
W1652
Financial support: None.
Potential competing interests: C.C. Th ompson—Apollo Endo-
surgery (Consultant/Research Support); Olympus (Consultant/
Research Support); Boston Scientifi c (Consultant); Covidien (Con-
sultant, Royalty, Stock); Medtronic (Consultant, Royalty, Stock);
USGI Medical (Consultant/Research Support). Th e remaining
author declares no confl ict of interest.
REFERENCES 1. Buchwald H , Avidor Y , Braunwald E et al. Bariatric surgery: a systematic
review and meta-analysis . JAMA 2004 ; 292 : 1724 – 37 . 2. Arterburn DE , Olsen MK , Smith VA et al. Association between bariatric
surgery and long-term survival . JAMA 2015 ; 313 : 62 . 3. Buchwald H , Oien DM . Metabolic/bariatric surgery worldwide 2011 .
Obes Surg 2013 ; 23 : 427 – 36 . 4. Perry CD , Hutter MM , Smith DB et al. Survival and changes in comor-
bidities aft er bariatric surgery . Ann Surg 2008 ; 247 : 21 – 7 . 5. Colquitt JL , Clegg AJ , Loveman E et al. Surgery for morbid obesity . In:
Colquitt JL editor(s). Cochrane Database of Systematic Reviews John Wiley & Sons, Ltd : Chichester, UK , 2005 , pp CD003641 .
6. Ramón JM , Salvans S , Crous X et al. Eff ect of Roux-en-Y gastric bypass vs sleeve gastrectomy on glucose and gut hormones: a prospective ran-domised trial . J Gastrointest Surg 2012 ; 16 : 1116 – 22 .
7. Peterli R , Steinert RE , Woelnerhanssen B et al. Metabolic and hormonal changes aft er laparoscopic Roux-en-Y gastric bypass and sleeve gastrec-tomy: a randomized, prospective trial . Obes Surg 2012 ; 22 : 740 – 8 .
8. Magro DO , Geloneze B , Delfi ni R et al. Long-term weight regain aft er gastric bypass: A 5-year Prospective Study . Obes Surg 2008 ; 18 : 648 – 51 .
9. Azagury DE , Abu Dayyeh BK , Greenwalt IT et al. Marginal ulceration aft er Roux-en-Y gastric bypass surgery: characteristics, risk factors, treat-ment, and outcomes . Endoscopy 2011 ; 43 : 950 – 4 .
10. Dallal RM , Bailey LA . Ulcer disease aft er gastric bypass surgery . Surg Obes Relat Dis 2006 ; 2 : 455 – 9 .
11. Rasmussen JJ , Fuller W , Ali MR . Marginal ulceration aft er laparoscopic gastric bypass: an analysis of predisposing factors in 260 patients . Surg Endosc 2007 ; 21 : 1090 – 4 .
12. Coblijn UK , Lagarde SM , de Castro SMM et al. Symptomatic marginal ulcer disease aft er Roux-en-Y gastric bypass: incidence, risk factors and management . Obes Surg 2015 ; 25 : 805 – 11 .
13. Edholm D , Sundbom M . Comparison between circular- and linear-stapled gastrojejunostomy in laparoscopic Roux-en-Y gastric bypass—a cohort from the Scandinavian Obesity Registry . Surg Obes Relat Dis 2015 ; 11 : 1233 – 6 .
14. Sacks BC , Mattar SG , Qureshi FG et al. Incidence of marginal ulcers and the use of absorbable anastomotic sutures in laparoscopic Roux-en-Y gastric bypass . Surg Obes Relat Dis 2006 ; 2 : 11 – 16 .
15. Schirmer B , Erenoglu C , Miller A . Flexible endoscopy in the management of patients undergoing Roux-en-Y gastric bypass . Obes Surg 2002 ; 12 : 634 – 8 .
16. Cleator IG , Rae A , Birmingham CL . Ulcerogenesis following gastric procedure for obesity . Obes Surg 1996 ; 6 : 260 – 1 .
17. Papasavas PK , Gagné DJ , Donnelly PE et al. Prevalence of Helicobacter pylori infection and value of preoperative testing and treatment in patients undergoing laparoscopic Roux-en-Y gastric bypass . Surg Obes Relat Dis 2008 ; 4 : 383 – 8 .
18. Lin Y-S , Chen M-J , Shih S-C et al. Management of Helicobacter pylori infection aft er gastric surgery . World J Gastroenterol 2014 ; 20 : 5274 .
19. Hartin CW , ReMine DS , Lucktong TA . Preoperative bariatric screening and treatment of Helicobacter pylori . Surg Endosc 2009 ; 23 : 2531 – 4 .
20. Rawlins L , Rawlins MP , Brown CC et al. Eff ect of Helicobacter pylori on marginal ulcer and stomal stenosis aft er Roux-en-Y gastric bypass . Surg Obes Relat Dis 2013 ; 9 : 760 – 4 .
21. Schulman AR , Abougergi M , Th ompson CCH . Pylori as a predictor of marginal ulceration: a nationwide analysis . Obesity 2017 ; 25 : 522 – 6 .
22. Carr WRJ , Mahawar KK , Balupuri S et al. An evidence-based algorithm for the management of marginal ulcers following Roux-en-Y gastric bypass . Obes Surg 2014 ; 24 : 1520 – 7 .
23. Schulman AR , Chan WW , Devery A et al. Opened proton pump inhibitor capsules reduce time to healing compared with intact capsules for marginal ulceration following Roux-en-Y gastric bypass . Clin Gastroenterol Hepatol 2016 ; 15 : 494 – 500.e1 .
esophagitis or persistent dysphagia due to a stenosed or twisted
sleeve, conversion to RYGB is a successful option. For patients
who lose inadequate weight or develop weight regain following
sleeve gastrectomy, conversion to RYGB or duodenal switch (i.e.,
sleeve with distal small bowel anastomosis) is a viable option.
VERTICAL BANDED GASTROPLASTY
Vertical banded gastroplasty (VBG) is a purely restrictive proce-
dure that involves the creation of a small proximal gastric pouch
<50 ml lined by a vertical staple line and a tight prosthetic mesh
that is sutured to itself but not the stomach ( Figure 1d ). Th is sur-
gery has the benefi t of providing an outlet diameter that remains
constant.
Familiarity with the complications of this procedure is impor-
tant, despite the fact that VBG has largely been replaced by other
procedures. Staple line dehiscence can result in formation of a fi s-
tula to the fundus, oft en leading to weight gain. Th is type of fi stula
is found in as many as half of all patients on routine post-operative
endoscopy. Stomal stenosis can also occur and present as obstruc-
tive symptoms, and be managed by endoscopically by balloon
dilation, although results are oft en short-lived and revision may
be necessary. Band erosion is a late complication of VBG, and can
be removed via endoscopy if the band is silastic. Removal of mesh
bands is typically not feasible. All of these complications warrant
consideration for surgical revision.
Surgical management
Th is procedure is most commonly converted to a RYGB when
there is inadequate weight loss, as the proximal stomach has been
modifi ed into a pouch.
CONCLUSION
Obesity is one of the most signifi cant health problems worldwide.
Despite improvement in the performance of bariatric surgical
procedures, complications are not uncommon. It is our respon-
sibility as gastroenterologists to be familiar with these procedures
and complication management strategies. In addition, primary
endoscopic therapies for obesity are seeing broader use in the
United States. As obesity is one of the most challenging medical
and economic problems faced by our society, fellowship programs
should place a greater emphasis on the management of this con-
dition and procedure-related complications. Endoscopy is a less
invasive alternative to primary and revisional procedures, and
will have a signifi cant role in the care of these patients moving
forward.
CONFLICT OF INTEREST
Guarantor of the article: Christopher C. Th ompson, MD, MSc,
FACG, FASGE, AGAF.
Specifi c author contributions: Draft ing of the manuscript: Allison
R. Schulman; this author has approved the fi nal draft submitted.
editing of the manuscript: Christopher C. Th ompson; this author has
approved the fi nal draft submitted.
Complications of Bariatric Surgery
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
RE
VIE
W
1653
24. Ryou M , Mogabgab O , Lautz DB et al. Endoscopic foreign body removal for treatment of chronic abdominal pain in patients aft er Roux-en-Y gastric bypass . Surg Obes Relat Dis 2010 ; 6 : 526 – 31 .
25. Jirapinyo P , Watson RR , Th ompson CC . Use of a novel endoscopic sutur-ing device to treat recalcitrant marginal ulceration (with video) . Gastro-intest Endosc 2012 ; 76 : 435 – 9 .
26. Chau E , Youn H , Ren-Fielding CJ et al. Surgical management and outcomes of patients with marginal ulcer aft er Roux-en-Y gastric bypass . Surg Obes Relat Dis 2015 ; 11 : 1071 – 5 .
27. Patel RA , Brolin RE , Gandhi A . Revisional operations for marginal ulcer aft er Roux-en-Y gastric bypass . Surg Obes Relat Dis 2009 ; 5 : 317 – 22 .
28. Schneider BE , Villegas L , Blackburn GL et al. Laparoscopic gastric bypass surgery: outcomes . J Laparoendosc Adv Surg Tech 2003 ; 13 : 247 – 55 .
29. Awad S , Aguilo R , Agrawal S et al. Outcomes of linear-stapled versus hand-sewn gastrojejunal anastomosis in laparoscopic Roux en-Y gastric bypass . Surg Endosc 2015 ; 29 : 2278 – 83 .
30. Sanyal AJ , Sugerman HJ , Kellum JM et al. Stomal complications of gastric bypass: incidence and outcome of therapy . Am J Gastroenterol 1992 ; 87 : 1165 – 9 .
31. Ahmad J , Martin J , Ikramuddin S et al. Endoscopic balloon dilation of gastroenteric anastomotic stricture aft er laparoscopic gastric bypass . Endoscopy 2003 ; 35 : 725 – 8 .
32. Peifer KJ , Shiels AJ , Azar R et al. Successful endoscopic management of gastrojejunal anastomotic strictures aft er Roux-en-Y gastric bypass . Gastrointest Endosc 2007 ; 66 : 248 – 52 .
33. Nguyen NT , Stevens CM , Wolfe BM . Incidence and outcome of anas-tomotic stricture aft er laparoscopic gastric bypass . J Gastrointest Surg 2003 ; 7 : 997 – 1003 ; discussion 1003 .
34. Huang CS . Th e role of the endoscopist in a multidisciplinary obesity center . Gastrointest Endosc 2009 ; 70 : 763 – 7 .
35. Barba CA , Butensky MS , Lorenzo M et al. Endoscopic dilation of gastroesophageal anastomosis stricture aft er gastric bypass . Surg Endosc 2003 ; 17 : 416 – 20 .
36. Podnos YD , Jimenez JC , Wilson SE et al. Complications aft er laparoscopic gastric bypass: a review of 3464 cases . Arch Surg 2003 ; 138 : 957 – 61 .
37. Gould JC , Garren M , Boll V et al. Th e impact of circular stapler diameter on the incidence of gastrojejunostomy stenosis and weight loss following laparoscopic Roux-en-Y gastric bypass . Surg Endosc 2006 ; 20 : 1017 – 20 .
38. Fisher BL , Atkinson JD , Cottam D . Incidence of gastroenterostomy stenosis in laparoscopic Roux-en-Y gastric bypass using 21- or 25-mm circular stapler: a randomized prospective blinded study . Surg Obes Relat Dis 2007 ; 3 : 176 – 9 .
39. Giordano S , Salminen P , Biancari F et al. Linear stapler technique may be safer than circular in gastrojejunal anastomosis for laparoscopic Roux-en-Y gastric bypass: a meta-analysis of comparative studies . Obes Surg 2011 ; 21 : 1958 – 64 .
40. Go MR , Muscarella P , Needleman BJ et al. Endoscopic management of stomal stenosis aft er Roux-en-Y gastric bypass . Surg Endosc 2004 ; 18 : 56 – 9 .
41. Majumder S , Buttar N , Gostout C et al. Lumen-apposing covered self-expanding metal stent for management of benign gastrointestinal strictures . Endosc Int Open 2015 ; 4 : E96 – 101 .
42. Uchima H , Abu-Suboh M , Mata A et al. Lumen-apposing metal stent for the treatment of refractory gastrojejunal anastomotic stricture aft er laparoscopic gastric bypass . Gastrointest Endosc 2016 ; 83 : 251 .
43. Lee JK , Van Dam J , Morton JM et al. Endoscopy is accurate, safe, and eff ective in the assessment and management of complications following gastric bypass surgery . Am J Gastroenterol 2009 ; 104 : 575 – 82 ; quiz 583 .
44. Campos JM , de Mello FST , Ferraz AAB et al. Endoscopic dilation of gastrojejunal anastomosis aft er gastric bypass . Arq Bras Cir Dig 2012 ; 25 : 283 – 9 .
45. Tucker ON , Szomstein S , Rosenthal RJ . Surgical management of gastro-gastric fi stula aft er divided laparoscopic Roux-en-Y gastric bypass for morbid obesity . J Gastrointest Surg 2007 ; 11 : 1673 – 9 .
46. Pauli EM , Beshir H , Mathew A . Gastrogastric fi stulae following gastric bypass surgery—clinical recognition and treatment . Curr Gastroenterol Rep 2014 ; 16 : 405 .
47. Stanczyk M , Deveney C , Traxler S et al. Gastro-gastric fi stula in the era of divided Roux-en-Y gastric bypass: strategies for prevention, diagnosis, and management . Obes Surg 2006 ; 16 : 359 – 64 .
48. Huang CS , Forse RA , Jacobson BC et al. Endoscopic fi ndings and their clinical correlations in patients with symptoms aft er gastric bypass sur-gery . Gastrointest Endosc 2003 ; 58 : 859 – 66 .
49. Mukewar S , Kumar N , Catalano M et al. Safety and effi cacy of fi stula closure by endoscopic suturing: a multi-center study . Endoscopy 2016 ; 48 : 1023 – 8 .
50. Fernandez-Esparrach G , Lautz DB , Th ompson CC . Endoscopic repair of gastrogastric fi stula aft er Roux-en-Y gastric bypass: a less-invasive approach . Surg Obes Relat Dis 2010 ; 6 : 282 – 8 .
51. Haito-Chavez Y , Law JK , Kratt T et al. International multicenter experi-ence with an over-the-scope clipping device for endoscopic management of GI defects (with video) . Gastrointest Endosc 2014 ; 80 : 610 – 22 .
52. Niland B , Brock A . Over-the-scope clip for endoscopic closure of gastro-gastric fi stulae . Surg Obes Relat Dis 2016 ; 13 : 15 – 20 .
53. Flicker MS , Lautz DB , Th ompson CC . Endoscopic management of gastrogastric fi stulae does not increase complications at bariatric revision surgery . J Gastrointest Surg 2011 ; 15 : 1736 – 42 .
54. Law R , Wong Kee Song LM , Irani S et al. Immediate technical and delayed clinical outcome of fi stula closure using an over-the-scope clip device . Surg Endosc 2015 ; 29 : 1781 – 6 .
55. Nelson DW , Blair KS , Martin MJ . Analysis of obesity-related outcomes and bariatric failure rates with the duodenal switch vs gastric bypass for morbid obesity . Arch Surg 2012 ; 147 : 847 – 54 .
56. Gonzalez R , Nelson LG , Gallagher SF et al. Anastomotic leaks aft er laparoscopic gastric bypass . Obes Surg 2004 ; 14 : 1299 – 307 .
57. Almahmeed T , Gonzalez R , Nelson LG et al. Morbidity of anastomotic leaks in patients undergoing Roux-en-Y gastric bypass . Arch Surg 2007 ; 142 : 954 .
58. Puli SR , Spoff ord IS , Th ompson CC . Use of self-expandable stents in the treatment of bariatric surgery leaks: a systematic review and meta-analysis . Gastrointest Endosc 2012 ; 75 : 287 – 93 .
59. Mickevicius A , Sufi P , Heath D . Factors predicting the occurrence of a gastrojejunal anastomosis leak following gastric bypass . Wideochir Inne Tech Maloinwazyjne 2014 ; 3 : 436 – 40 .
60. Salinas A , Baptista A , Santiago E et al. Self-expandable metal stents to treat gastric leaks . Surg Obes Relat Dis 2006 ; 2 : 570 – 2 .
61. Fukumoto R , Orlina J , McGinty J et al. Use of Polyfl ex stents in treatment of acute esophageal and gastric leaks aft er bariatric surgery . Surg Obes Relat Dis 2007 ; 3 : 68 – 71-2 .
62. Eisendrath P , Cremer M , Himpens J et al. Endotherapy including tempo-rary stenting of fi stulas of the upper gastrointestinal tract aft er laparo-scopic bariatric surgery . Endoscopy 2007 ; 39 : 625 – 30 .
63. Serra C , Baltasar A , Andreo L et al. Treatment of gastric leaks with coated self-expanding stents aft er sleeve gastrectomy . Obes Surg 2007 ; 17 : 866 – 72 .
64. Casella G , Soricelli E , Rizzello M et al. Nonsurgical treatment of staple line leaks aft er laparoscopic sleeve gastrectomy . Obes Surg 2009 ; 19 : 821 – 6 .
65. Eubanks S , Edwards CA , Fearing NM et al. Use of endoscopic stents to treat anastomotic complications aft er bariatric surgery . J Am Coll Surg 2008 ; 206 : 935 – 8-9 .
66. Babor R , Talbot M , Tyndal A . Treatment of upper gastrointestinal leaks with a removable, covered, self-expanding metallic stent . Surg Laparosc Endosc Percutan Tech 2009 ; 19 : e1 – e4 .
67. Edwards CA , Bui TP , Astudillo JA et al. Management of anastomotic leaks aft er Roux-en-Y bypass using self-expanding polyester stents . Surg Obes Relat Dis 2008 ; 4 : 594 – 9-600 .
68. Merrifi eld BF , Lautz D , Th ompson CC . Endoscopic repair of gastric leaks aft er Roux-en-Y gastric bypass: a less invasive approach . Gastrointest Endosc 2006 ; 63 : 710 – 4 .
69. Kriwanek S , Ott N , Ali-Abdullah S et al. Treatment of gastro-jejunal leak-age and fi stulization aft er gastric bypass with coated self-expanding stents . Obes Surg 2006 ; 16 : 1669 – 74 .
70. Ballesta C , Berindoague R , Cabrera M et al. Management of anasto-motic leaks aft er laparoscopic Roux-en-Y gastric bypass . Obes Surg 2008 ; 18 : 623 – 30 .
71. Th ompson CC , Kumar N , Slattery J et al. A standardized method for endoscopic necrosectomy improves complication and mortality rates . Pancreatology 2016 ; 16 : 66 – 72 .
72. Kumar N , Conwell DL , Th ompson CC . Direct endoscopic necrosectomy versus step-up approach for walled-off pancreatic necrosis: comparison of clinical outcome and health care utilization . Pancreas 2014 ; 43 : 1334 – 9 .
73. Jacobsen GR , Coker AM , Acosta G et al. Initial experience with an inno-vative endoscopic clipping system . Surg Technol Int 2012 ; 22 : 39 – 43 .
74. Ritter LA , Wang AY , Sauer BG et al. Healing of complicated gastric leaks in bariatric patients using endoscopic clips . JSLSSoc Laparoendosc Surg 2013 ; 17 : 481 – 3 .
75. Seebach L , Bauerfeind P , Gubler C . "Sparing the surgeon": clinical experience with over-the-scope clips for gastrointestinal perfora-tion . Endoscopy 2010 ; 42 : 1108 – 11 .
Schulman and Thompson
The American Journal of GASTROENTEROLOGY VOLUME 112 | NOVEMBER 2017 www.nature.com/ajg
RE
VIE
W1654
102. Baretta GAP , Alhinho HCAW , Matias JEF et al. Argon plasma coagulation of gastrojejunal anastomosis for weight regain aft er gastric bypass . Obes Surg 2015 ; 25 : 72 – 9 .
103. Abu Dayyeh BK , Jirapinyo P , Weitzner Z et al. Endoscopic sclerotherapy for the treatment of weight regain aft er Roux-en-Y gastric bypass: outcomes, complications, and predictors of response in 575 procedures . Gastrointest Endosc 2012 ; 76 : 275 – 82 .
104. Th ompson CC , Slattery J , Bundga ME et al. Peroral endoscopic reduc-tion of dilated gastrojejunal anastomosis aft er Roux-en-Y gastric bypass: a possible new option for patients with weight regain . Surg Endosc 2006 ; 20 : 1744 – 8 .
105. Mullady DK , Lautz DB , Th ompson CC . Treatment of weight regain aft er gastric bypass surgery when using a new endoscopic platform: initial experience and early outcomes (with video) . Gastrointest Endosc 2009 ; 70 : 440 – 4 .
106. Jirapinyo P , Slattery J , Ryan MB et al. Evaluation of an endoscopic sutur-ing device for transoral outlet reduction in patients with weight regain following Roux-en-Y gastric bypass . Endoscopy 2013 ; 45 : 532 – 6 .
107. Kumar N , Th ompson CC . Transoral outlet reduction for weight regain aft er gastric bypass: long-term follow-up . Gastrointest Endosc 2016 ; 83 : 776 – 9 .
108. Sigstad H . A clinical diagnostic index in the diagnosis of the dumping syndrome. Changes in plasma volume and blood sugar aft er a test meal . Acta Med Scand 1970 ; 188 : 479 – 86 .
109. Carnett J . Intercostal neuralgia as a cause of abdominal pain and tender-ness . Surg Gynecol Obs 1926 ; 42 : 625 – 32 .
110. Abidi W , Chan WW , Th ompson CC . Breath testing for small intestinal bacterial overgrowth in Roux-en-Y gastric bypass patients: the impor-tance of orocecal transit time . Gastroenterology 2016 ; 150 : S688 – 9 .
111. Schulman AR , Th ompson CC . Utility of bile acid scintigraphy in the diagnosis of remnant gastritis in patients with Roux-en-Y gastric bypass . Gastrointest Endosc 2016 ; 83 : AB327 – 8 .
112. Naik RD , Choksi YA , Vaezi MF . Impact of weight loss surgery on esophageal physiology . Gastroenterol Hepatol (N Y) 2015 ; 11 : 801 – 9 .
113. de Jong JR , Besselink MGH , van Ramshorst B et al. Eff ects of adjustable gastric banding on gastroesophageal refl ux and esophageal motility: a systematic review . Obes Rev 2010 ; 11 : 297 – 305 .
114. Gamagaris Z , Patterson C , Schaye V et al. Lap-band impact on the func-tion of the esophagus . Obes Surg 2008 ; 18 : 1268 – 72 .
115. Dixon JB , O’Brien PE . Gastroesophageal refl ux in obesity: the eff ect of lap-band placement . Obes Surg 1999 ; 9 : 527 – 31 .
116. Naef M , Mouton WG , Naef U et al. Esophageal dysmotility disorders aft er laparoscopic gastric banding--an underestimated complication . Ann Surg 2011 ; 253 : 285 – 90 .
117. Dargent J . Esophageal dilatation aft er laparoscopic adjustable gastric banding: defi nition and strategy . Obes Surg 2005 ; 15 : 843 – 8 .
118. Arias IE , Radulescu M , Stiegeler R et al. Diagnosis and treatment of meg-aesophagus aft er adjustable gastric banding for morbid obesity . Surg Obes Relat Dis 2009 ; 5 : 156 – 9 .
119. Khan A , Ren-Fielding C , Traube M . Potentially reversible pseudoacha-lasia aft er laparoscopic adjustable gastric banding . J Clin Gastroenterol 2011 ; 45 : 775 – 9 .
120. Fielding GA . Should the lap band be removed to treat pseudoachalasia? Gastroenterol Hepatol (N Y) 2013 ; 9 : 471 – 3 .
121. Suter M , Giusti V , Héraief E et al. Band erosion aft er laparoscopic gastric banding: occurrence and results aft er conversion to Roux-en-Y gastric bypass . Obes Surg 2004 ; 14 : 381 – 6 .
122. Abu-Abeid S , Keidar A , Gavert N et al. Th e clinical spectrum of band erosion following laparoscopic adjustable silicone gastric banding for morbid obesity . Surg Endosc 2003 ; 17 : 861 – 3 .
123. Png KS , Rao J , Lim KH et al. Lap-band causing left gastric artery erosion presenting with torrential hemorrhage . Obes Surg 2008 ; 18 : 1050 – 2 .
124. Neto MPG , Ramos AC , Campos JM et al. Endoscopic removal of eroded adjustable gastric band: lessons learned aft er 5 years and 78 cases . Surg Obes Relat Dis 2010 ; 6 : 423 – 7 .
125. Blero D , Eisendrath P , Vandermeeren A et al. Endoscopic removal of dysfunctioning bands or rings aft er restrictive bariatric procedures . Gastrointest Endosc 2010 ; 71 : 468 – 74 .
126. Abu-Abeid S , Szold A . Results and complications of laparoscopic adjust-able gastric banding: an early and intermediate experience . Obes Surg 1999 ; 9 : 188 – 90 .
76. Swanson CM , Roust LR , Miller K et al. What every hospitalist should know about the post-bariatric surgery patient . J Hosp Med 2012 ; 7 : 156 – 63 .
77. Carucci LR , Turner MA . Imaging aft er bariatric surgery for morbid obesity: Roux-en-Y gastric bypass and laparoscopic adjustable gastric banding . Semin Roentgenol 2009 ; 44 : 283 – 96 .
78. Higa KD , Ho T , Boone KB . Internal hernias aft er laparoscopic Roux-en-Y gastric bypass: incidence, treatment and prevention . Obes Surg 2003 ; 13 : 350 – 4 .
79. Higa K , Ho T , Tercero F et al. Laparoscopic Roux-en-Y gastric bypass: 10-year follow-up . Surg Obes Relat Dis 2011 ; 7 : 516 – 25 .
80. Hamdan K , Somers S , Chand M . Management of late postoperative complications of bariatric surgery . Br J Surg 2011 ; 98 : 1345 – 55 .
81. Blachar A , Federle MP . Gastrointestinal complications of laparoscopic roux-en-Y gastric bypass surgery in patients who are morbidly obese: fi ndings on radiography and CT . AJR Am J Roentgenol 2002 ; 179 : 1437 – 42 .
82. Ma IT , Madura JA . Gastrointestinal complications aft er bariatric surgery . Gastroenterol Hepatol (N Y) 2015 ; 11 : 526 – 35 .
83. Simper SC , Erzinger JM , McKinlay RD et al. Retrograde (reverse) jejunal intussusception might not be such a rare problem: a single group’s experi-ence of 23 cases . Surg Obes Relat Dis 2008 ; 4 : 77 – 83 .
84. Daellenbach L , Suter M . Jejunojejunal intussusception aft er Roux-en-Y gastric bypass: a review . Obes Surg 2011 ; 21 : 253 – 63 .
85. Shiff man ML , Sugerman HJ , Kellum JM et al. Gallstone formation aft er rapid weight loss: a prospective study in patients undergoing gastric bypass surgery for treatment of morbid obesity . Am J Gastroenterol 1991 ; 86 : 1000 – 5 .
86. Shiff man ML , Sugerman HJ , Kellum JM et al. Changes in gallbladder bile composition following gallstone formation and weight reduction . Gastro-enterology 1992 ; 103 : 214 – 21 .
87. Worobetz LJ , Inglis FG , Shaff er EA . Th e eff ect of ursodeoxycholic acid therapy on gallstone formation in the morbidly obese during rapid weight loss . Am J Gastroenterol 1993 ; 88 : 1705 – 10 .
88. Iglézias Brandão de Oliveira C , Adami Chaim E , da Silva BB . Impact of rapid weight reduction on risk of cholelithiasis aft er bariatric surgery . Obes Surg 2003 ; 13 : 625 – 8 .
89. Bastouly M , Arasaki CH , Ferreira JB et al. Early changes in postprandial gallbladder emptying in morbidly obese patients undergoing Roux-en-Y gastric bypass: correlation with the occurrence of biliary sludge and gallstones . Obes Surg 2009 ; 19 : 22 – 8 .
90. Everhart JE . Contributions of obesity and weight loss to gallstone disease . Ann Intern Med 1993 ; 119 : 1029 – 35 .
91. Inamdar S , Slattery E , Sejpal DV et al. Systematic review and meta-analysis of single-balloon enteroscopy-assisted ERCP in patients with surgically altered GI anatomy . Gastrointest Endosc 2015 ; 82 : 9 – 19 .
92. Th ompson CC , Ryou MK , Kumar N et al. Single-session EUS-guided transgastric ERCP in the gastric bypass patient . Gastrointest Endosc 2014 ; 80 : 517 .
93. Kedia P , Kumta N , Widmer J et al. Endoscopic ultrasound-directed transgastric ERCP (EDGE) for Roux-en-Y anatomy: a novel technique . Endoscopy 2015 ; 47 : 159 – 63 .
94. Tyberg A , Nieto J , Salgado S et al. Endoscopic ultrasound (EUS)-directed transgastric endoscopic retrograde cholangiopancreatography or EUS: mid-term analysis of an emerging procedure . Clin Endosc 2016 ; 50 : 185 – 90 .
95. Monaco-Ferreira DV , Leandro-Merhi VA . Weight regain 10 years aft er Roux-en-Y gastric bypass . Obes Surg 2016 ; 27 : 1137 – 44 .
96. Nicoletti CF , de Oliveira BAP , de Pinhel MAS et al. Infl uence of excess weight loss and weight regain on biochemical indicators during a 4-year follow-up aft er Roux-en-Y gastric bypass . Obes Surg 2015 ; 25 : 279 – 84 .
97. Christou NV , Look D , MacLean LD . Weight gain aft er short- and long-limb gastric bypass in patients followed for longer than 10 years . Ann Surg 2006 ; 244 : 734 – 40 .
98. Barhouch AS , Padoin AV , Casagrande DS et al. Predictors of excess weight loss in obese patients aft er gastric bypass: a 60-month follow-up . Obes Surg 2016 ; 26 : 1178 – 85 .
99. Lim CSH , Liew V , Talbot ML et al. Revisional bariatric surgery . Obes Surg 2009 ; 19 : 827 – 32 .
100. Sjöström L , Lindroos A-K , Peltonen M et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years aft er bariatric surgery . N Engl J Med 2004 ; 351 : 2683 – 93 .
101. Abu Dayyeh BK , Lautz DB , Th ompson CC . Gastrojejunal stoma diameter predicts weight regain aft er Roux-en-Y gastric bypass . Clin Gastroenterol Hepatol 2011 ; 9 : 228 – 33 .
Complications of Bariatric Surgery
© 2017 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
RE
VIE
W
1655
132. Burgos AM , Braghetto I , Csendes A et al. Gastric leak aft er laparoscopic-sleeve gastrectomy for obesity . Obes Surg 2009 ; 19 : 1672 – 7 .
133. Mahadev S , Kumbhari V , Campos JM et al. Endoscopic septotomy: an eff ective approach for internal drainage of sleeve gastrectomy-associated collections . Endoscopy 2017 ; 49 : 504 – 8 .
134. Baretta G , Campos J , Correia S et al. Bariatric postoperative fi stula: a life-saving endoscopic procedure . Surg Endosc 2015 ; 29 : 1714 – 20 .
135. Genco A , Soricelli E , Casella G et al. Gastroesophageal refl ux disease and Barrett’s esophagus aft er laparoscopic sleeve gastrectomy: a possible, un-derestimated long-term complication . Surg Obes Relat Dis 2016 ; 13 : 568 – 74 .
136. Jirapinyo P , Th ompson CC . Endoscopic bariatric and metabolic therapy: surgical analogues and mechanisms of action . Clin Gastroenterol Hepatol 2016 ; 15 : 619 – 30 .
127. Keidar A , Carmon E , Szold A et al. Port complications following laparoscopic adjustable gastric banding for morbid obesity . Obes Surg 2005 ; 15 : 361 – 5 .
128. Angrisani L , Furbetta F , Doldi SB et al. Lap Band adjustable gastric band-ing system: the Italian experience with 1863 patients operated on 6 years . Surg Endosc 2003 ; 17 : 409 – 12 .
129. Cottam D , Qureshi FG , Mattar SG et al. Laparoscopic sleeve gastrectomy as an initial weight-loss procedure for high-risk patients with morbid obesity . Surg Endosc 2006 ; 20 : 859 – 63 .
130. Lalor PF , Tucker ON , Szomstein S et al. Complications aft er laparoscopic sleeve gastrectomy . Surg Obes Relat Dis 2008 ; 4 : 33 – 8 .
131. Abidi W , Th ompson CC . Systematic treatment of sleeve gastrectomy stenosis with hydrostatic and pneumatic balloon dilatation is safe and eff ective . Gastroenterology 2016 ; 150 : S828 – 9 .
GASTROENTEROLOGY ARTICLE OF THE WEEK December 14, 2017
Schulman AR, Thompson CC. Complications of bariatric surgery: What you can expect to see in your GI practice. Am J Gastroenterol 2017;112:1640‐1655. 1. True statements regarding sleeve gastrectomy include a. Remove most of the lesser curvature of the stomach b. Removal of ghrelin‐producing cells contribute to the weight loss c. Gastric emptying is delayed, contributing to early satiety and lower intake d. Sleeve gastrectomy has effects on the hind gut secretion of peptide YY and GLP‐1 True or False 2. Erosive esophagitis from acid reflux is a common complication after gastric banding procedure for weight loss 3. Dumping syndrome after bypass surgery usually occurs following ingestion of a high fat meal 4. Balloon dilation of a stenotic gastrojejunal anastomosis to a 18mm size is the mainstay of therapy for anastomotic stenosis 5. Abdominal wall cellulitis after gastric banding may be an indication of band erosion into the gastric lumen 6. A patient with severe dysphagia after lap band surgery should be managed by endoscopic balloon dilation to a diameter not larger than 12mm. 7. Swirled vessels at the root of the mesentery seen on CT are a highly specific sign for internal hernia after gastric bypass 8. Administering the PPI as an open capsule for patients with anastomotic ulceration significantly reduces the time to ulcer healing 9. Visible suture material should not be removed even if the surgery was done months prior to the EGD 10. Marginal ulceration associated with anastomotic stenosis will usually require surgical revision

















![Effect of Roux-en-Y gastric bypass surgery on …...diabetes [1, 2]. Until recently, Roux-en-Y gastric bypass (RYGB) was the surgical procedure of choice, especially when treating](https://static.fdocuments.in/doc/165x107/5f2155ed9d02c317381db1f2/effect-of-roux-en-y-gastric-bypass-surgery-on-diabetes-1-2-until-recently.jpg)









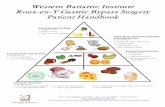



![· Web viewWord count: 3904. Corresponding Author ... (Roux-en-Y gastric bypass [RYGB]) with an intensive lifestyle intervention ... For CPAP vs BS study, large cross-over group.](https://static.fdocuments.in/doc/165x107/5b2f1add7f8b9af0648d60d4/-web-viewword-count-3904-corresponding-author-roux-en-y-gastric-bypass-rygb.jpg)