community willamette valley medical center...
Transcript of community willamette valley medical center...
community newsspring 2010willamette valley medical center
Reaching Further with Helping Handsquality & satisfaction surveys • health care reform provisions
called to care
cec Zander, rn, with a young patient in Kenya.
In This Issue1–3 community newsnew program director at wound care center
aguiar and ford Join Board of trustees
ophthalmologist Joins hospital staff
Board certified internists Join staff
new Joint care coordinator appointed
Board certified orthopedists Join staff
George wiley appointed chief financial officer
4–9 called to carereaching further with helping hands
how you can help
10-11 survey resultsquality and satisfaction survey results
about the on-site survey
12–13 health care reformsummary of major health reform provisions, from the desk of rosemari davis, ceo
wound care and hyperbaric medicine director appointed
Jill Addison has been appointed Program Director at Willamette Valley Medical Center’s Wound Care and Hyperbaric Medicine Center.
Addison graduated from Corban College in Salem, Oregon with a degree in healthcare administration. She has an extensive background in healthcare services, including acting as director of in-home care for the Sun Retirement Corporation. She also owned and served as vice president of customer relations and marketing for BHS Long Term Care Pharmacy, where she worked as liaison for long-term facilities to ensure proper medication management for seniors and disabled individuals. She also served as sales and marketing director for Bi-Mart Health Solutions Pharmacy.
She is a member of the Board of Directors for BHS Pharmacy and Advisory Board for OASIS. She has also served as Chairperson for March of Dimes BHS team and volunteered for the Alzheimer’s Association.
hospital board appoints new trustees
Angel Aguiar Jr., mortgage banker for Sunset Residential Mortgage, and W. Glenn Ford, Vice President for Finance and Administration and Chief Financial Officer at Linfield College, have been appointed to the hospital’s Board of Trustees.
Aguiar attended Glendale Commu-nity College in Glendale, California, and obtained his real estate licenses and certifications in Los Angeles. His professional career includes serving as Bank of America’s neighborhood Lending Certified Mortgage Loan Officer, working closely with non-profit organizations that serve the Latino community. He was also owner and operator of Nationwide Lenders, a local mortgage company, and currently owns JARIKA Investments, a real estate development business.
Ford graduated from the University of Idaho with a bachelor’s degree in forest products with a business man-agement option and a master’s of business administration. Prior to his position at Linfield, he served as Vice President for Business and Finance and Chief Financial Officer for Utah State University in Logan, Utah, and Associate Vice President for Business and Finance for Washington State University in Pullman, Washington.
Both new members have been active in their communities. Aguiar has served as a member and chair of the Dayton School District Budget Committee.
Ford is a member of the City of McMinnville Downtown Master Plan Advisory Committee and is participat-ing in the 2009-2010 McMinnville Area Chamber of Commerce Community Leadership Development Program.
1
community news
Jill addison, program directorangel aguiar, board of trusteesglenn ford, board of trustees
Find a physician
online! Visit our
website at
wvmcweb.com
See videos
of new docs at
wvmcweb.com/
physicians
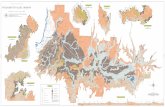
left to right:a building collapsed by the January haitian earthquake,
as seen by peter van patten, md,’s medical team;robert demaster, md, with an operating team in dr congo;
children wait in line for care in guatemala.
2 ophthalmologist Joins staff
Ophthalmologist Ryan Berger, MD,
has joined the staffs of the hospital and McMinnville Eye Clinic.
Dr. Berger earned his bachelor’s degree in liberal arts and sciences at Utah State University, and earned his doctorate of medicine at the George-town University School of Medicine.
He completed his residency in inter-nal medicine at Dartmouth-Hitchcock Medical Center where he was Chief Resident, and his residency in ophthal-mology at the University of Colorado, Rocky Mountain Lions Eye Institute.
Dr. Berger has also served as an instructor at Dartmouth Medical School and as attending physician in internal medicine at Dartmouth- Hitchcock Medical Center and the White River Junction Veterans Affairs Medical Center in Vermont.
A member of the American Board of Internal Medicine, he joins Michael Passo, MD, Nicholas Grinich, MD and David Hayes, MD at the McMinnville Eye Clinic. To make an appointment with Dr. Berger, please call the clinic at 503.472.4688.
board certified internists Join staff
Christopher Cirino, DO, board certified in Internal Medicine and Infectious Disease, and Yojana Dange, MD, board certified in Internal Medicine, have joined the staffs of the hospital and McMinnville Internal Medicine.
Dr. Cirino earned his bachelor’s degree in microbiology at Miami University of Ohio in Oxford, Ohio, and his doctorate of osteopathic medicine from Ohio University College of Osteopathic Medicine in Athens, Ohio. He earned a master’s degree in public health at George Washington University, where he also completed a residency in internal medicine and fellowships in infectious diseases and
general internal medicine.His professional experience includes
working as a consultant of infectious disease at St. Vincent Health Center in Erie, Pennsylvania. He also worked overseas as a medical volunteer.
Dr. Dange earned her bachelor’s degree in medicine and surgery from Grant Medical College in Mumbai, India and her master’s degree in Pharmacology and Toxicology from the Medical College of Virginia in Richmond. She completed her residency in internal medicine at the Atlanticare Regional Medical Center in Atlantic City, New Jersey. Her professional experience includes serving as attending physician at the Union Memorial Hospital, Good Samaritan Hospital and Overlea Health and Rehabilitation Center in Maryland.
McMinnville Internal Medicine is located at 375 SE Norton Lane, Suite A. To make an appointment, call 503.472.9002. Dr. Cirino’s and Dr. Dange’s practices are open to Medicare and Medicaid patients and accept most insurance plans.
reed named Joint replacement institute coordinator
Natalie Reed, MSPT, CCI was appointed Joint Care Coordinator for the Joint Replacement Institute at Willamette Valley Medical Center, which is scheduled to open this summer.
Reed, bilingual in English and Spanish, graduated from Pacific University in Forest Grove with a bachelor’s of science degree in biology and a master’s of science in physical therapy, also from Pacific.
Her professional career includes serving as staff physical therapist at the Life Care Center of McMinnville, where she designed and implemented a community-centered total joint replacement class and balance screen-ing program. She also served as staff
ryan berger, mdchristopher cirino, do
yojana dange, md
physical therapist at Willamette Valley Medical Center, where she developed and implemented a body mechanics, ergonomic and injury prevention program at Cascade Steel Mill.
Reed’s duties as Joint Care Coordina-tor include teaching pre-and post-op joint recovery classes and acting as liaison between department heads.
board certified orthopedists Join staff
Board certified Orthopedic Surgeon James Ruf, MD, and Orthopedic Spe-cialist in Hip and Knee Replacement Michael Vessely, MD, have joined the staffs of Willamette Valley Medical Center and McMinnville Orthopaedic and Hand Surgery.
Dr. Ruf earned his bachelor’s degree in chemistry at Purdue University in West Lafayette, Indiana, and earned his doctorate of medicine at Creigh-ton University School of Medicine in Omaha, Nebraska. He completed his orthopedic surgery residency at the University of Michigan Department of Orthopedic Surgery in Ann Arbor.
Prior to arriving at McMinnville Orthopedic and Hand Surgery, Dr. Ruf worked as a general orthopedic surgeon at Multicare Orthopedics and Sports Medicine in Covington, Washington, and at Northwest Orthopedic Surgery and Sports Medicine in Hillsboro.
Dr. Vessely earned his bachelor’s degree in human biology from Stanford University in Palo Alto, California and his doctorate of medi-cine from Oregon Health and Science University in Portland. He completed his internship in general surgery at the Los Angeles County-University of Southern California Medical Center and his residency in orthopedic surgery at the University of Missouri Hospital and Clinics in Columbia.
Dr. Vessely’s fellowship experience includes a research fellowship in Adult Reconstructive Surgery in the Depart-ment of Orthopedic Surgery at the Mayo Clinic in Rochester, Minnesota,
and a surgical fellowship in hip and knee replacement at New England Baptist hospital in Boston.
Both are members of the American Academy of Orthopaedic Surgeons, and join George Zakaib, MD, at McMinnville Orthopaedic and Hand Surgery.
george wiley appointed chief financial officer
George Wiley has been appointed Chief Financial Officer (CFO) at Willamette Valley Medical Center.
Wiley graduated from Weber State University in Ogden, Utah with a bachelor’s of science degree in account-ing, and University of Phoenix, with a master’s of business administration and healthcare administration. Prior to Willamette Valley Medical Center, Wiley served as the CFO at Phoenix Baptist Hospital in Phoenix, Arizona.
A CFO with 19 years experience, his professional career includes serving as vice president and CFO for Raleigh General Hospital in Beckley, West Virginia. He also served as CFO for Georgetown Community Hospital in Georgetown, Kentucky and LifePoint Bluegrass Community Hospital in Versailles, Kentucky.
In addition to his tenure as CFO, Wiley’s community service includes serving as treasurer for Habitat for Humanity in Castle Country, Utah. He has also served as member, treasurer and board member of the Healthcare Financial Management Association.
natalie reed, mspt, cciJames ruf, mdmichael vessely, mdgeorge wiley, cfo
called to careWhen you ask Cecilia “Cec” Zander why she
spent her time off from working as a nurse at Willamette Valley Medical Center to work as a nurse in Kenya, she may tell you about the listless boy who perked up after being treated with IV fluids and anti-biotics, or the woman in labor whose life and that of her newborn were saved, or she may tell you of the bad roads filled with beautiful people whose smiles greeted her medical team as they arrived by foot at a rural village in Western Kenya.
Zander described the back-breaking toil of the short-hoe rural farmers and the village women who carry heavy water on their head and children on their back as performing “work that is really, really hard.” Some might say the same of Zander and the other physicians and nurses who take “vacation time” and pay their own travel costs to work in difficult conditions, often surrounded by poverty in makeshift clinics that are understaffed and lack sufficient equipment, resources and medicines. Although there is much that is differ-ent about their stories of service—located in places as diverse as Honduras, Kenya, Ethiopia, Guatemala, Peru and Salem, Oregon—all seem to share a sense that they are called to do this work.
Zander’s most recent Kenya trip was organized by Mercy Medical Teams from The Lutheran Church- Missouri Synod. Her husband, a pastor, accompanied
the medical team as chaplain. Zander, who called her two trips to Kenya “toe-dipping opportunities,” said she may consider a longer trip when she retires. “It was a blessing to me,” she said.
Dolly Palacios, a surgical technologist who trav-eled with Medical Teams International to Ethiopia, admitted that she found the extreme poverty very dis-turbing, especially emergency room conditions and the orphaned children often abused in the city streets.
“We take much for granted…how incredibly fortunate we are to have the medical advancements we do,” said Palacios.
Palacios went to Ethiopia at a time when her own father was diagnosed with terminal cancer. She consid-ered cancelling, but her father encouraged her to go. “He said he wanted me to go, and that he was proud of me.” He died before Palacios returned from the 16-day medical trip.
In spite of the difficult conditions, she is hoping to be able to make future mission trips. “It’s a calling,” she said. “The Ethiopians are a very kind, gentle and humble
ReacHIng FuRTHeR wITH
helpinG hands
shannon seehawer, rn and cindy hall, rn
wayne hurty, md, with colleagues from food for the hungry and
guatemalan villagers;John neeld, md, carrying medical
supplies in guatemala;peter van patten, md (in white),
with medical staff in haiti.
“We take much for granted…how incredibly fortunate we are to have the medical advancements we do.”
people, and just so thrilled when we help. They were very gracious.”
“You come home and feel like you’re the one with the reward,” said Palacios.
This sentiment was echoed by Emergency Room Nurse Kathy Galer. “It is hard work, but the re-wards outweigh sitting by a pool or walking on the beach. There’s nothing wrong with that—we all need that —but what makes me tick is my love for people,” she said. “How can you tell someone about the love of Christ if you don’t help them physically?”
Galer has traveled with many different groups. Her first trip was 19 years ago to Africa. Since then, she’s been to Mexico, Guatemala, the Dominican Republic and the Philippines. She called her mission trips “life changing.”
“What’s so amazing to me is seeing people—the poorest of the poor—laughing, enjoying their chil-dren, just like we do,” she said. “It’s not all about toys we have…they have happiness also, and sometimes our media doesn’t portray that.”
Dr. John Neeld, a gynecologist and obstetri-cian, had his first experience with an overseas medical project in March 2008 when he and nurse practitioner Nancy Manley went to the villages of Guatemala with a medical team organized by Faith in Practice.
Working in makeshift exam rooms made from rope and tarps, Neeld and Manley provided primarily gyne-cological care for up to 30 patients each per day, and focused on cervical cancer prevention. Because the villages see physicians so rarely, Manley said they had to turn away thousands of people hoping to receive medical attention. And those they were able to treat, they had to do so with accelerated care—meaning treating any lesion as if it was cancer, without tak-ing the step to biopsy it. Although accelerated care is not common or necessary in the U.S., in Guatemala, if the women had to wait for teams of physicians to return to their village, it would give the cancer time to
develop and endanger their lives. “We [Americans] expect perfection from our
system. There, they are grateful for anything they can get,” said Neeld. He added, “It feels good to be able to treat people who are underserved.”
Cardiologist Dr. Wayne Hurty was also struck by the gratefulness of the people he served. In February, he spent a week in Pompeche, Guatemala, serving in a medical clinic and making home visits for those too sick to travel to the clinic.
His trip was organized by Food for the Hungry which bases its programs on the philosophy, “if you give a man a fish he will eat for a day. If you teach a man how to fish he will eat for a lifetime.” In addition to medical treatments, Hurty and the nine-member medical team instructed community members on how to: develop and maintain clean water sources (since contaminated water is the source of much illness), practice good hygiene, wear footwear to prevent infec-tion, and practice good nutrition. “We are all very similar—we pray to the same God, sleep under the same moon and I felt very blessed for what I have. In the U.S., we are often rich financially but impover-ished spiritually. There, they are poor financially but, for the most part, happy people.”
.
Dr. Marion Hull, family practice physician, also had her first experience with mission trips in Guate-mala. “Then I noticed the need in my own backyard,” she said. Living in Salem, Oregon, at the time, Hull co-founded the Salem Free Clinic. A self-described “start-up” person, Hull said she was helping her church with outreach and making home visits when the need became apparent. The clinic was a coopera-tive effort of the Foursquare Church and Walker Middle School. “We began by setting up exam rooms in the school gym with PVC pipe and shower curtains,” she said.
News of the free clinic traveled by word of mouth. The clinic served the working poor, the mentally ill
—Robert DeMaster, MD anesthesiologist
—Kathy galer, Rnemergency Room nurse
7
It is hard work, but the rewards outweigh sitting by a pool or walking on the beach. There’s nothing wrong with that—we all need that—but what makes me tick is my love for people.
Kathy galer, rn, with a patient in ghana.
robert demaster, md, with a patient in peru.
“What’s so amazing to me is seeing people—the poorest of the poor—laughing, enjoying their children…”
“We expect perfection from our system. There, they are grateful for anything they can get.”
“In the U.S., we’re often financially rich but impoverished spiritually. There, they are poor financially but…happy people.”
“We began by setting up exam rooms in the school gym with PVC pipe and shower curtains.”
You’ve got a skill to offer and can provide services they otherwise don’t get and there’s a satisfying feeling that comes with that. Once you’ve been there, you want to go back.
99It’s a calling. The ethiopians are a very kind, gentle and humble people, and just so thrilled when we help. They were very gracious. You come home and feel like you’re the one with the reward. —Dolly Palacios, Surgical Technologist
and many recently released from the correctional sys-tem. The clinic treated diabetes, high blood pressure and a myriad of mental illnesses including bipolar dis-order, depression and anxiety. “The difficult thing was many of the people from the correctional system were mentally ill and were released with only two weeks worth of medications,” said Hull. “It’s not good if they are off their meds; that’s how many of them ended up in jail in the first place.”
The free clinic soon partnered with an organization that provided free medications (nothing narcotic or that can be abused). Other volunteers joined in and provided meals and prayer, and supported the clinic in many ways. Recently a donor funded a two-year lease on a building to house the clinic; and now that the program has malpractice insurance, more physicians and nurses are willing to volunteer. The program today has two psychiatric nurses.
Orthopedist Dr. Peter Van Patten was about to go on a ski vacation when the January earthquake hit Haiti. After talking it over with his wife, he changed his plans and went to Port-au-Prince. Although he didn’t travel with a specific aid organization, once in Haiti he met up with the relief organization Humedica and worked at the Hopital Espoir, the Hospital of Hope. For 12 days he worked in makeshift surgical rooms with minimal functioning equipment. He per-formed surgeries to fix broken and fractured limbs or amputate when necessary. “You have to be flexible,” he
said as he spoke about the primitive conditions. “You can’t do things the way you’re used to doing them.”
Although grateful he could help, he said he was disheartened because of the gravity of the situation, and returned in March to follow up with patients. Even months later, little had changed since his earlier trip—there were still new patients coming in with injuries and the city was still in ruins. He plans on returning to Haiti to continue to help.
Anesthesiologist Dr. Robert DeMaster has been a physician for 30 years, and has practiced locally since 1996. For nearly each of the years that he’s practiced medicine, he’s served on a medical mission trip.
DeMaster administers anesthesia for many of the most common surgeries performed by the medical teams, including cleft lip and palate surgeries, and orthopedic and gynecological surgeries. DeMaster said it is important for American workers to be culturally sensitive and work alongside the countries’ physicians and staff. “You’re only there a short time. It takes a certain level of sensitivity,” he said. “You are going to find frustrations. Standards of care are not the same.”
DeMaster, who has been on many medical mission trips, including to Mexico, Honduras, the Congo, Ethiopia and Peru, is preparing for a trip to Cameroon.
“Once you’ve been there, you want to go back,” he said. Now that his six children are grown, he antici-pates spending even more “vacations,” working.
gabriela rubio, food services
Doing Our Part: How You can Help
clockwise from top:dolly palacios, surgical technologist,
assists ethiopian surgeons;nancy manley, nurse practitioner, with
a patient in guatemala;marion hull, md, examines an elderly
woman in guatemala.
The following charities were featured in our article. We encourage you to support these or other programs that work with causes important to you.
the lutheran church–missouri synod includes many mission groups. Visit http://catalog.lcms.org/GiveNow/Gift–Catalog.asp to choose between grant support, domestic and international projects, art programs and other giving programs.
medical teams international helps people around the world affected by disaster, conflict and poverty. Visit www.medicalteams.org/sf/donate.aspx
to set up planned giving, donate non-cash or stock gifts, support a volunteer, or browse the gift catalog.
faith in practice serves more than 14,000 patients each year. Visit www.faithinpractice.org/general donate.php to donate money or in-kind and learn how you can become a volunteer.
food for the hungry’s mission statement demon-strates their dedication to help churches, leaders and families overcome poverty and build spiritual connec-tions. Visit www.fh.org to donate money or stocks, sponsor a child, or become a volunteer yourself.
“You have to be flexible. You can’t do things the way you’re used to doing them.”
“It takes a certain level of sensitivity. You are going to find frustrations. Standards of care are not the same.”
11The second survey, conducted by the HealthStream Corporation and focused on the satisfaction of employ-ment for hospital employees and medical staff, was equally as positive.
Hospital employees were asked to fill out an anony-mous online survey that covered key aspects of their employment satisfaction, including their overall satis-faction with their jobs, the hospital as an employer, if they would recommend the hospital as the best place to work in town, and if they anticipated staying at the hospital over the next several years. Scores for each ranged in the 90 percent range, com-pared to scores in the 70 to 80 percent range for the aver-age of all other HealthStream hospitals.
The survey also specifically addressed physicians’ levels of job satisfaction, which was reported to be 98 percent, compared to 85 percent nationally. Lash also said the scores of staff competency and the hospital’s commitment to improved care stand out.
When physicians were asked about the ability of the
hospital’s nurses, 94 percent of physicians surveyed are satisfied with the competency of the nursing staff, com-pared to the national average of 81 percent. Scores were
also significant when physi-cians were asked how sat-isfied they were with the hos-pital’s efforts to continually improve care—95 percent respectively, compared to 85 percent nationally.
While the data gathered by The Joint Commission and Healthstream surveys pro-vide very different insights to how the hospital operates, Lash said they accomplish something very similar: they give patients and community members confidence that the hospital employees, adminis-tration and medical providers care about providing quality care at every turn.
“Fundamentally, I think a hospital is a place focused on caring for others from the top down,” said McKeegan. “The administrators care about their patients, but also
very much about their employees. Nobody wants to be in the hospital, but if you have to be, you would want to be in our hospital.”
Patients and community members can rest assured knowing Willamette Valley Medical Center has passed another round of quality and satisfaction surveys.
As a way to measure the hospital’s operation and performance in every area, Willamette Valley Medical Center participated in two voluntary surveys this year. The first, conducted by The Joint Commission, scrutinized the hospital’s operation from the bottom up—literally. Surveyors examined everything from the physical structure of the hospital all the way to the paperwork prepared by medical staff. The second survey, conducted in compliance with stan-dards from the Centers for Medicare and Medicaid Services (CMS), compiled responses from employees and medical staff regard-ing key aspects of their job satisfaction.
The Joint Commission quality check survey was conducted in February and con-sisted of a three-day visit by Joint Commission surveyors. Everything from physical inspections to medical staff and patient interviews took place during the three days.
Chief Quality Officer Carolyn Lash said the quality check survey takes place approximately every three years, but the exact date is unknown, adding an extra level of uncertainty for hospital administration and employees. It
is for that reason that Lash said she is particularly proud of the results.
“They had no significant find-ings, and those that they found were paperwork related and easily fixable,” Lash said. “We are very pleased with
our results. We aren’t perfect, but we work hard to make our processes as perfect as possible so we can provide the best care, and the survey results validate that.”
She added that any results needing improvements must be reported back to The Joint Commission within 45 days, stating the steps they have taken to correct the problem, and providing documentation that they are now in compliance with the standards. Just two months after the initial survey, Lash said they are now com-pliant with standards and are continuing to monitor to assure that they remain in compliance
with the new processes put in place. John McKeegan, local attorney and chair for the hospi-
tal board of trustees, said the results confirm what many people in the community have always believed —that Willamette Valley Medical Center is a first class hospital.
“It’s a top to bottom review, and it’s important that they occur the way they do,” he said. “To pass it with such fly-ing colors is phenomenal.”
Hospital Receives excellent Satisfaction Scores
top marKs
...we work hard to make our processes as perfect as possible so we can provide the best care, and the survey results validate that.
—carolyn Lash chief Quality Officer
Fundamentally, I think a hospital is a place focused on caring for others from the top down. The administrators care about the patients, but also very much about their employees.
—John McKeegan chair, Board of Trustees
98%satisfactionreported By responding
physicians
about the On-Site Survey The on-site survey is just one
part of The Joint Commission’s multi-process for hospital accredi-tation. According to Chief Quality Officer Carolyn Lash, the survey process is data-driven, patient-centered and focused on evaluating actual care processes. The purpose of the survey is to evaluate the organization and provide best practice guidance to help improve performance.
“I look at it as the good house-keeping seal of approval,” she said.
The three-day survey begins with a survey planning session, followed by an opening conference, orienta-tion and leadership session.
“An important part of the review is how prepared we are initially,” said Lash. “Do we have materials for the surveyors to read that accurately describe the hospital, and are our hospital administrators there and ready for an open discussion?”
Once the initial briefing is complete, The Joint Commission conducts what it calls tracer methodology. This methodology uses clients, patients or residents to assess the standards of compliance through interviews and observation.
They also complete a competence assessment of all staff, which includes a credentials review to determine the experience and
training of the medical providers. Lash said once the patient and
employee surveys are complete, The Joint Commission also examines the infrastructure of the building, called an environment of care session. This includes a building tour where surveyors examine everything from firewalls to ceilings.
Staff is then briefed in what is called an exit conference. The survey team presents a written summary of the survey findings to staff, and if there are any areas for improvement, the hospital is required to submit an evidence of standards compliance report.
13
Like myself, I am sure many of you have been following the developments of the Patient Protection and Affordable Care Act and the Reconciliation Act of 2010. The act was signed into law by President Obama on March 23, and offers
immediate benefits to millions of Americans. I believe the changes will provide the financial relief many of our community members need, and will allow us to continue to provide quality, local and affordable health care to you. The key provisions of the Act include:
SMALL BUSINESS TAX CREDITS Offers tax credits to small businesses to make em-
ployee coverage more affordable. Tax credits of up to 35 percent of premiums will be immediately available to firms that choose to offer coverage. Effective begin-ning for calendar year 2010. (Beginning in 2014, small business tax credits will cover 50 percent of premiums.)
BEGINS TO CLOSE THE MEDICARE PART D DONUT HOLE
Provides a $250 rebate to Medicare beneficiaries who hit the donut hole in 2010. Effective for calendar year 2010. (Beginning in 2011, institutes a 50 percent discount on brand-name drugs in the donut hole; also completely closes the donut hole by 2020.)
FREE PREVENTIVE CARE SERVICES UNDER MEDICARE
Eliminates co-payments for preventive services and exempts preventive services from deductibles under the Medicare program. Effective beginning January 1, 2011.
HELP FOR EARLY RETIREES Creates a temporary re-insurance program (until
the Exchanges are available) to help offset the costs of expensive premiums for employers and retirees for health benefits for retirees age 55 to 64. Effective 90 days after enactment.
ENDS RESCISSIONS Bans insurance companies from dropping people
from coverage when they get sick. Effective six months after enactment.
NO DISCRIMINATION AGAINST CHILDREN WITH PRE-EXISTING CONDITIONS
Prohibits new health plans in all markets plus grandfathered group health plans from denying cover-age to children with pre-existing conditions. Effective six months after enactment. (Beginning in 2014, this prohibition would apply to all persons.)
BANS LIFETIME LIMITS ON COVERAGE Prohibits health insurance companies from placing
lifetime caps on coverage. Effective six months after enactment.
summary of maJorhealth reformfrom the desk of rosemari davischief executive officer, willamette valley medical center
Have more questions about health care reform?The U.S. Department of Health and Human Services
manages an official U.S. Government website centered on health care reform at www.healthreform.gov. You can sign up for regular e-mail updates, ask questions, and partici-pate in weekly web chats. The site also features specific
information for groups such as seniors, young adults, early retirees, rural Americans, small businesses, and minorities. For further details on how health care reform impacts the state of Oregon, visit http://www.healthreform.gov/reports/statehealthreform/oregon.html.
provisions
BANS RESTRICTIVE ANNUAL LIMITS ON COVERAGE
Tightly restricts the use of annual limits to ensure access to needed care in all new plans and grandfathered group health plans. These tight restrictions will be defined by HHS. Effective six months after enactment. (Beginning in 2014, the use of any annual limits would be prohibited for all new plans and grandfathered group health plans.)
FREE PREVENTIVE CARE UNDER NEW PRIVATE PLANS
Requires new private plans cover preventive services with no co-payments, with preventive services exempt from deductibles. Effective six months after enactment.
NEW, INDEPENDENT APPEALS PROCESS Ensures consumers in new plans have access to an
effective internal and external appeals process to appeal decisions by their health insurance plan. Effec-tive six months after enactment.
ENSURES VALUE FOR INSURANCE PREMIUM PAYMENTS Requires plans in individual and small group mar-
ket to spend 80 percent of premium dollars on medical services, and plans in the large group market to spend 85 percent. Insurers that do not meet these thresholds must provide rebates to policyholders. Effective on January 1, 2011.
IMMEDIATE HELP FOR THE UNINSURED UNTIL EXCHANGE IS AVAILABLE (INTERIM HIGH-RISK POOL)
Provides immediate access to affordable insurance for Americans who are uninsured because of a pre-existing condition through a temporary subsidized high-risk pool. Effective 90 days after enactment.
EXTENDS COVERAGE FOR YOUNG PEOPLE UP TO 26TH BIRTHDAY THROUGH
PARENTS’ INSURANCERequires new health plans and certain grandfathered plans to allow young people up to their 26th birthday to remain on their parents’ insurance policy, at the parents’ choice. Effective six months after enactment.
COMMUNITY HEALTH CENTERS Increases funding for Community Health Centers to
allow for nearly a doubling of the number of patients seen by the centers over the next five years. Effective beginning in fiscal year 2010.
INCREASES PRIMARY CARE DOCTORS Provides investment in training programs to in-
crease number of primary care doctors, nurses, and public health professionals. Effective fiscal year 2010.
PROHIBITS PLANS FROM DISCRIMINATING BASED ON SALARY
Prohibits group health plans from establishing any eligibility rules for health care coverage that have the ef-fect of discriminating in favor of higher wage employees. Effective six months after enactment.
INSURANCE CONSUMER INFORMATION Provides aid to states in establishing offices of
health insurance consumer assistance in order to help individuals with the filing of complaints and appeals. Effective beginning in fiscal year 2010.
CREATES VOLUNTARY, PUBLIC LONG-TERM CARE INSURANCE PROGRAM
Creates a long-term care insurance program to be financed by voluntary payroll deductions to provide home and community-based services to adults who become functionally disabled. Effective January 1, 2011.
1
2
3
4
5
6
7
8
9
10
11
12
15
13
14
16
17
18
Looking for a physician?
family practice
david collins, mdphone: 503.843.4909222 se Jefferson streetsheridan michael Jaczko, dophone: 503.852.6668348 south pine streetcarlton marion hull, mdphone: 503.474.25662700 se stratus avenue, #302mcminnville
c. francis Kenyon, mdphone: 503.474.25662700 se stratus avenue, #302mcminnville
melvin herd, mdphone: 503.472.9002375 se norton lane, suite amcminnville sunita paudyal, mdphone: 503.472.9002375 se norton lane, suite amcminnville richard Kimani, mdphone: 503.472.9002375 se norton lane, suite amcminnville
internal medicine
beata Kopecka, mdphone: 503.472.9002375 se norton lane, suite amcminnville
christopher cirino, dophone: 503.472.9002375 se norton lane, suite amcminnville yojana dange, mdphone: 503.472.9002375 se norton lane, suite amcminnville
2700 se stratus avenuemcminnville, or 97128
The following primary care physicians are currently accepting new Medicare and Medicaid patients.