Colorectal cancer following negative colonoscopy: is 5-year screening the correct interval to...
Transcript of Colorectal cancer following negative colonoscopy: is 5-year screening the correct interval to...
Colorectal cancer following negative colonoscopy: is 5-yearscreening the correct interval to recommend?
Steven K. Nakao • Steven Fassler • Iswanto Sucandy •
Soo Kim • D. Mark Zebley
Received: 23 April 2012 / Accepted: 13 August 2012 / Published online: 10 October 2012
� Springer Science+Business Media, LLC 2012
Abstract
Background Despite the high sensitivity of screening
colonoscopy, polyps and cancers can still go undetected.
With the polyp-to-cancer transformation cycle averaging
7–10 years, present guidelines recommend repeat colon-
oscopy within 10 years after negative screening. However,
not all colorectal malignancies follow this decade-long
progression. This study evaluates the incidence and
pathology of colorectal cancers following a previous neg-
ative screening colonoscopy.
Methods Records of patients who underwent a colectomy
at our institution, from 1998 to 2009, were reviewed ret-
rospectively. A total of 1,784 patient records were screened
using exclusion criteria for inclusion in this study. The
patients were divided as follows: Group 1 included patients
with a negative colonoscopy within the previous 5 years;
Group 2 included patients without a previous colonoscopy
or with a previous colonoscopy more than 5 years prior.
Group 1 patients were evaluated by colonoscopy for ane-
mia, diverticulitis, signs of obstruction, and bleeding. Age,
tumor location, operation performed, and pathology find-
ings were recorded. The v2 test and paired t test were used
for statistical analysis.
Results A total of 233 patients were included in this
study. Group 1 contained 43 patients with a mean age of
73 years (range = 35–94, median = 75). Group 2 had 190
patients with a mean age of 68 years (range = 19–91,
median = 70). Group 1 consisted of 18 male and 25 female
patients, and Group 2 included 94 male and 96 female
patients. Both groups were further classified into the
following age categories: \50 years, 50–80 years, and
[80 years. Eighteen percent of the total study population
had newly discovered colorectal cancer within a 5-year
colonoscopy screening period. There were no significant
differences in the distribution of the T and N stages
between the two groups and no statistically significant
differences when the rate of lymphovascular invasion (19
vs. 17 %; p = 0.39) and perineural invasion (7 vs. 11 %;
p = 0.58) were compared.
Conclusions Within 5 years, 18 % of our study popula-
tion developed colorectal cancer. Most of these malig-
nancies were found within the 50–80-year age group and
located predominantly in the right colon and distally in the
sigmoid and rectum. While distal cancers may be visual-
ized by flexible sigmoidoscopy, those located more prox-
imally may be missed, necessitating the need for a full
colonoscopy. Although staging was similar between the
two groups, Group 1 tumors were less aggressive despite
having appeared within 5 years. As a result of our inci-
dence of colorectal cancer within a 5-year interval, a
shorter period for routine colonoscopy may be considered.
Keywords Colorectal cancer � Endoscopy
Colon cancer remains the third most common cancer
diagnosis and is the second leading cause of cancer-related
death in the US annually [1]. Early detection through
Presented at the SAGES 2012 Annual Meeting, March 7–March 10,
2012, San Diego, CA.
S. K. Nakao � I. Sucandy
Department of Surgery, Abington Memorial Hospital, Abington,
PA, USA
e-mail: [email protected]
S. Fassler (&) � S. Kim � D. M. Zebley
Department of Surgery, Division of Colorectal Surgery,
Colon and Rectal Associates, 1235 Old York Road, Suite G20,
Abington, PA 19001, USA
e-mail: [email protected]
123
Surg Endosc (2013) 27:768–773
DOI 10.1007/s00464-012-2543-6
and Other Interventional Techniques
evidence-based screening protocols can lead to the identi-
fication of early disease [2–5]. Initial screening for colon
cancer can be grouped into two categories: stool-based and
structural tests. Stool-based tests are noninvasive, inex-
pensive, and can be performed in the office; however, they
are highly variable and less sensitive for detection of colon
cancer [2]. Due to the variability in detection, annual or
biennial fecal screening is recommended to detect any stool
changes indicative of colon cancer. Structural tests such as
sigmoidoscopy and colonoscopy are more sensitive in
detecting early disease and can be therapeutic.
Screening protocols are tailored for average-risk patients
who do not have a documented family history or predis-
posing history of colon cancer. Studies have shown that
patients who are over the age of 50 years have a higher
incidence of colon cancer than younger patients. Current
guidelines recommend that screening colonoscopy should
begin at age 50 in these average-risk patients and follow-up
depends on the pathology found on examination [3].
Positive and negative examinations are determined by the
presence of adenomatous polyps found on colonoscopy,
and recommendations for repeat screening ranges from 3 to
5 years for a positive exam and 10 years for a negative
exam [4, 5].
While the typical polyp-to-cancer transformation cycle
takes an average of 10 years, not all polyps will follow this
decade-long progression. Therefore, a 10-year interval may
prove too long a period for repeat surveillance after a
negative colonoscopy in normal-risk patients. This study
evaluates the incidence and pathology of colorectal cancers
that arose within 5 years after a negative screening
colonoscopy.
Methods
Medical records of patients who underwent colon resection
from 1998 to 2009 were reviewed retrospectively. Initially,
1,784 patients were included in our database. Those who
were included initially had resection performed at two area
hospitals by the same three colon and rectal surgeons.
Review showed that resection had been performed for
complications from anemia, diverticulitis, Crohn’s disease,
ulcerative colitis, foreign body insertion, high-risk family
history, or new onset cancer. Inclusion criteria for the study
were as follows: those patients operated on at a single
teaching hospital, with no documented family history, and
who were not at a higher risk for colorectal cancer. Using
those criteria, 563 patients were included for initial review
in this study. Of these 563 patients, 300 charts had docu-
mented previous colonoscopic surveillance. Those without
a documented previous colonoscopy were excluded from
the study. Of these 300 patients, 67 were noted to have had
a colonoscopy for continued surveillance after previous
colon cancer resection and also were excluded from the
study. The remaining 233 patients had a documented pre-
vious colonoscopy for reasons other than suspected cancer,
as manifested by pain, bleeding, or signs of obstruction and
made up the study group.
Colonoscopic examinations were performed by two
groups at our institution; both sets of physicians were fel-
lowship-trained gastroenterologists or colorectal surgeons.
The gastroenterology group had an average of 9 years of
clinical and endoscopic experience per physician prior to
the start of this study. The colorectal surgeons had a
minimum of 3 years of clinical and endoscopic experience
prior to the start of this study. The annual endoscopic
experience per physician within each group averaged
[1,000 colonoscopies per doctor. Colonoscopic examina-
tion was considered complete with cecal intubation and, on
average, a 7-min withdrawal time, which had been docu-
mented within the chart review.
Patients who met the criteria for inclusion in the study
were then divided as follows: Group 1 patients had a
documented previously negative colonoscopy within the
last 5 years and were noted to have benign or no pathology
on previous reports. Group 2 patients had a documented
previous colonoscopy more than 5 years prior with similar
benign pathology. Benign pathology was considered as no
polyp found on examination or polyps that did not show
adenomatous features upon histologic evaluation.
The two groups were then divided further into subsets
by age, location, and stage. Male and female ratios were
calculated. Age was categorized as \50 years of age,
between 50 and 80 years of age, and[80 years, with mean
and median points. Tumor location was also identified as
originating in the right, transverse, left, sigmoid colon, or
rectum. Tumor stage, nodal metastasis, and evidence of
distant metastasis were also noted for each of the preceding
locations. Overall clinical stage was then tabulated for each
location and age group. The v2 test and the paired t test
analyses were used to determine statistical significance of
the location and clinical stages between the two groups.
Results
A total of 1,784 patients were initially included in this
study; however, after exclusion criteria were applied, only
233 patients qualified for inclusion (Fig. 1). These 233
patients were divided into two groups depending on their
previous colonoscopy status. Group 1 included those who
had a colonoscopy within the last 5 years and a negative
pathology report; there were 43 patients, with a mean age
of 73 years (range = 35–94, median = 75) and a male-to-
female ratio of 18:25. Two patients were younger than age
Surg Endosc (2013) 27:768–773 769
123
50 years, 28 patients were between 50 and 80 years, and 13
were older than 80 years (Fig. 2).
Location and stage of each tumor were categorized for
each age group as follows: 2 right-sided cancers in the\50-
year age group; 11 right-sided, 1 transverse colon, 2 left-
sided, 7 sigmoid colon, 6 rectal, and 1 synchronous
malignancy (right and left colon) in the 50–80-year age
group; 9 right-sided, 1 sigmoid colon, and 3 rectal tumors in
the[80-year age group (Fig. 3). In the\50-year age group,
100 % of the tumors were characterized as stage I. In the
50–80-year age group, 42.9 % were stage I, 25 % were
stage II, 25 % were stage III, and 7.1 % were stage IV. In
the[80-year group, 30.8 % were stage I, 30.8 % were stage
II, and 38.4 % were stage III (Fig. 4).
In Group 2, there were 190 patients with a mean age of
68 years (range = 19–91, median = 70) and a male-to-
female ratio of 94:96. There were 20 patients\50 years of
age, 133 between 50 and 80 years, and 37 patients
[80 years of age (Fig. 2). There were 6 right-sided, 3 left-
sided, 4 sigmoid colon, and 7 rectal tumors in the\50-year
subset. In patients aged between 50 and 80 years, 44 right-
sided, 5 transverse colon, 12 left-sided, 21 sigmoid colon,
47 rectal, and 4 synchronous tumors were found. In those
[80 years, there were 23 right-sided, 5 left-sided, 1 sig-
moid colon, and 8 rectal tumors (Fig. 3). In the \50-year
age group, 30 % of the tumors were stage I, 20 % were
stage II, and 50 % were stage III. In patients aged
50–80 years, 33.9 % of the tumors were stage I, 35.3 %
were stage II, 29.3 % were stage III, and 1.5 % were stage
IV. In patients[80 years, 32.4 % of the tumors were stage
I, 32.4 % were stage II, and 35.2 % were stage III (Fig. 4).
When comparing tumors in the 50–80-year subset of
both groups, there were no significant differences in their
location in the colon. In Group 1, tumor location was on the
right side in 39.3 %, in the transverse in 3.6 %, on the left
side in 7.1 %, in the sigmoid in 25 %, in the rectum in
21.4 %, and synchronous (right and left sides) in 3.6 %. In
group 2, 33 % were right-sided (p = 0.27), 3.6 % were
transverse (p = 0.01), 9 % were left-sided (p = 0.63),
15.8 % were sigmoid (p = 0.14), 35.2 % were in the
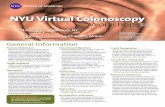
Fig. 1 Algorithm for inclusion in the study
Fig. 2 Age distribution
Fig. 3 Tumor location
Fig. 4 Tumor stage
770 Surg Endosc (2013) 27:768–773
123
rectum (p = 0.9), and 3.6 % were synchronous
(p = 0.001) (Table 1). Tumors in Group 1 were 42.9 %
stage I, 25 % stage II, 25 % stage III, and 7.1 % stage IV.
Tumors in Group 2 were 33.9 % stage I (p = 0.19), 35.3 %
stage II (p = 0.86), 29.3 % stage III (p = 0.68), and 1.5 %
stage IV (p = 0.01) (Table 2). There were no significant
differences in the distribution of the T and N stages
between the two groups. There also were no significant
statistical differences between the two groups when the
rates of lymphovascular invasion (19 vs. 17 %; p = 0.39)
and perineural invasion (7 vs. 11 %; p = 0.58) were
compared.
Discussion
As previously stated, screening for colon cancer can be
approached by one of two methods: fecal or structural-
based. While structural-based tests are the standard for
colon surveillance, lesions can still be missed. Patients who
had previous colonoscopies were included in this study and
divided into groups depending on the interval from previ-
ous colonoscopy. Approximately one in five patients
(18 %) who were diagnosed with colon cancer had a pre-
viously documented negative colonoscopy within the last
5 years. All of these lesions were found in patients who did
not have any previously documented colon cancer or sig-
nificant family history of colon cancer. None of the patients
included in this study had preventative family surveillance
as the reason for colonoscopic screening.
Despite the higher sensitivity of structural screening
examinations, many lesions still go undetected and can
progress to invasive cancer. Typically, lesions found within
3 years after a previously negative colonoscopy are usually
thought to have been missed on the initial screening, while
tumors found more than 3–5 years after the negative
colonoscopy are thought to have appeared de novo [6].
Previous studies have shown that the institution of routine
colonoscopy screening has found adenomas at a rate of
approximately 23 % and that removal of these adenomas
has led to a decrease in the rates of invasive colorectal
cancer [7, 8]. Even the discovery of small adenomas
(\1 cm) on sigmoidoscopy can be a harbinger of high-
grade dysplasia or invasive carcinoma in the remaining
colon, and these patients should be referred for a complete
colonoscopy [9]. These studies show the importance of
colonoscopy screening in average-risk patients to decrease
the rates of invasive colon cancer.
Historically, patients between the ages of 50 and
80 years have had the highest incidence of colorectal
cancer or adenomas found on colonoscopy. After the
implementation of colonoscopic screening for these
patients, the incidence of colon malignancies has
decreased. Although this study included the total number of
new incidences of colon cancer, our data for location and
staging reflect mostly the incidence of colon cancer in the
50–80-year age group. A recent study evaluating the age at
which to begin screening average-risk patients for colon
cancer noticed an increase in the incidence of colon cancer
in patients between 20 and 49 years [10]. Staging of these
tumors has shown that they are often times more aggressive
and advanced at the time of diagnosis, with a significant
number of tumors found in the sigmoid colon and rectum
[11, 12]. However, in our study, patients outside the
screening ages (below 50 years and above 80 years of age)
were shown to have a very low incidence of colon cancer.
This trend is likely due to the higher median age of patients
at our institution.
The distribution of colon malignancies in our study
appears quite different from those that are usually descri-
bed in the literature. Previously reported data show that
cancers detected by colonoscopy are typically seen in the
left colon or distally, while right-sided cancers are not
documented with the same frequency [13]. Previously
reported limitations for decreased detection of right-sided
colon cancers have been attributed to difficulty in cecal
intubation, poor quality of bowel preparation, experience
of the endoscopist, history of colon resection, patient
anatomy, or shortened withdrawal time of the colonoscope
[14, 15]. More recent studies have shown that experience
of the endoscopist factors considerably into the rate of
newly diagnosed tumors found on colonoscopy [16]. Rates
of adenoma detection, polyp removal, or completion of a
colonoscopy in women have been shown to affect the rates
of post-colonoscopy malignancies. Numerous studies have
shown an inverse relationship between the rates of polyp/
Table 1 Tumor location in 50–80-year age group
Group 1 Group 2 p value
Right-sided 39.3 % 33 % 0.27
Transverse 3.6 % 3.6 %
Left-sided 7.1 % 9 % 0.63
Sigmoid 25 % 15.8 % 0.14
Rectum 21.4 % 35.2 % 0.9
Synchronous 3.6 % 3.6 %
Table 2 Tumor stage in 50–80-year age group
Group 1 Group 2 p value
Stage I 42.9 % 33.9 % 0.19
Stage II 25 % 35.3 % 0.86
Stage III 25 % 29.3 % 0.68
Stage IV 7.1 % 1.5 % 0.01
Surg Endosc (2013) 27:768–773 771
123
adenoma detection and colonoscopy completion with
malignancy [17–20]. Studies have also shown a higher
incidence of colon cancer after a previously negative
colonoscopy in women. This has been hypothesized to be
the result of a more tortuous colon, incomplete preparation
of the right colon, or estrogen use [21]. In our study, there
is no statistically significant difference between men and
women and there is an increased incidence of right-sided
lesions in both men and women.
Structural and histological differences between right-
and left-sided colon tumors have also been documented.
Right-sided cancers are typically sessile or flat, and the
physiological difference between right- and left-sided
lesions can lead to a difference in progression of a lesion
[22, 23]. In the current study, a higher number of right-
sided colon cancers were detected by colonoscopy in both
Group 1 and Group 2 patients, with fewer left-sided lesions
in Group 1 and an approximately equal number of left-
sided lesions in the Group 2. Patients who present for
routine follow-up colonoscopy demonstrate a higher per-
centage of left-sided and distal colon cancers, which is in
line with previously reported data [23]. Studies have shown
that an increased rate of screening colonoscopy leads to
lower death rates and a decrease in the amount of left-sided
colon cancers that lead to death. More often, right-sided
colon cancers lead to death because of missed lesions on
initial colonoscopy or difference in tumor biology [13–20].
Of those tumors that were detected by colonoscopy,
most that were seen in the Group 1 patients were calculated
to be stage I tumors, with fewer but comparable stage II
and III lesions and few stage IV cancers. Consequently,
those patients who required more frequent colonoscopies
had less invasive tumors at the time of surgery. When
compared to those in Group 2, tumor staging was more
evenly distributed between stages I and III, and this appears
to be more typical of a longer colonoscopic surveillance
[23]. However, there does not appear to be a significant
difference between the stages of colon cancer between the
two groups, implying that neither group had a more
aggressive form of cancer.
This study is limited by several factors. The sample size
from a single institution is, of course, limited and affects
the statistical significance. Second, the patient’s comor-
bidities were not documented in all initial histories thus
limiting any clinical significance to the incidence of colon
cancer. Third, there was no documentation of significant
long-term follow-up after colon cancer resections.
Although current guidelines recommend that colon
cancer screening should commence at age 50 years for
average-risk patients and have a repeat colonoscopy
between 5 and 10 years, our data suggest that this may be
too long an interval, especially with a higher incidence of
right-sided colon cancers. While many of these cancers are
found in lower stages, a decreased screening interval may
lead to earlier detection and thus more complete resection
of colorectal tumors at less invasive states. Having
screening intervals of less than 5 years for benign disease
might be recommended for earlier detection and eradica-
tion of potential colon cancer.
Disclosures Steven K. Nakao, Steven A. Fassler, Iswanto Sucandy,
D. Mark Zebley, and Soo Kim have no conflicts of interest or
financial ties to disclose.
References
1. U.S. Cancer Statistics Working Group (2010) United States Cancer
Statistics: 1999–2007 Incidence and Mortality Web-based Report.
Department of Health and Human Services, Centers for Disease
Control and Prevention, and National Cancer Institute, Atlanta.
http://www.prevent-cancer.org/ColorectalCancerInformation.aspx
2. Smith RA, Cokkinides V, Brawley OW (2008) Cancer screening
in the United States, 2008: a review of current American Cancer
Society guidelines and cancer screening issues. CA Cancer J Clin
58:161–179
3. Whitlock EP, Lin JS, Liles E, Beil TL, Fu R (2008) Screening for
colorectal cancer: a targeted, updated systematic review of the
U.S. Preventative Services Task Force. Ann Intern Med 149:
638–658
4. Walsh JM, Terdiman JP (2003) Colorectal cancer screening: a
scientific review. JAMA 289:1288–1296
5. Lieberman D (2006) Screening for colorectal cancer in average-
risk populations. Am J Med 119:728–735
6. Hosokawa O, Shirasaki S, Kaizaki Y, Hayashi H, Douden K,
Hattori M (2003) Invasive colorectal cancer detected up to
3 years after a colonoscopy negative for cancer. Endoscopy
35(6):506–510
7. Brenner H, Chang-Claude J, Seiler CM, Hoffmeister M (2011)
Long-term risk of colorectal cancer after negative colonoscopy.
J Clin Oncol 29:3761–3767
8. Loeve F, Boer R, Zauber AG, van Ballegooijen M, van Oort-
marssen GJ, Winawer SJ (2004) National polyp study data: evi-
dence for regression of adenomas. Int J Cancer 111(4):633–639
9. Butterly LF (2006) What is the clinical importance of small
polyps with regard to colorectal cancer screening? Clin Gastro-
enterol Hepatol 4:343–348
10. Davis DM, Marcet JE, Frattini JC, Prather AD, Mateka J, Nfonsam
VN (2011) Is it time to lower the recommended screening age for
colorectal cancer? J Am Coll Surg 2(13):352–361
11. Robertson DJ, Greenberg ER, Beach M et al (2005) Colorectal
cancer in patients under close colonoscopic surveillance. Gas-
troenterology 129(1):34–41
12. Strock P, Mossong J, Scheiden R, Weber J, Heieck F, Kerschen A
(2011) Colorectal cancer incidence is low in patients following a
colonoscopy. Dig Liver Dis 43:899–904
13. Bressler B, Paszat LF, Vinden C, Li C, He J, Rabeneck L (2004)
Colonoscopic miss rates for right-sided colon cancer: a popula-
tion-based analysis. Gastroenterology 127(2):452–456
14. Soetikno RM, Kaltenbach T, Rouse RV et al (2008) Prevalence of
nonpolypoid (flat and depressed) colorectal neoplasms in
asymptomatic and symptomatic adults. JAMA 299(9):1027–1035
15. Brenner H, Hoffmeister M, Arndt V, Stegmaier C, Altenhofen L,
Haug U (2010) Protection from right- and left-sided colorectal
772 Surg Endosc (2013) 27:768–773
123
neoplasms after colonoscopy: population-based study. J Natl
Cancer Inst 102(2):89–95
16. Heresbach D, Barrioz T, Lapalus MG, Coumaros D, Bauret P,
Potier P (2008) Miss rate for colorectal neoplastic polyps: a
prospective multicenter study of back-to-back video colonos-
copies. Endoscopy 40(4):284–290
17. Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister
M (2011) Protection from colorectal cancer after colonoscopy.
Ann Intern Med 154:22–30
18. Kaminski MF, Regula J, Kraszewska E, Polkowski M, Wa-
jciechowska U, Didkowska J, Zweirko M, Rupinski M, Nowacki
MP, Butruk E (2010) Quality indicators for colonoscopy and the
risk of interval cancer. N Engl J Med 362:1795–1803
19. Singh H, Nugent Z, Mahmud SM, Demers AA, Bernstein CN
(2010) Predictors of colorectal cancer after negative colonoscopy:
a population-based study. Am J Gastroenterol 105:663–673
20. Baxter NN, Goldwasser MA, Paszat LF, Saskin R, Urbach DR,
Rabeneck L (2009) Association of colonoscopy and death from
colorectal cancer. Ann Intern Med 150:1–8
21. Sugai T, Habano W, Jiao YF et al (2006) Analysis of molecular
alterations in left- and right-sided colorectal carcinomas reveals
distinct pathways of carcinogenesis: proposal for new molecular
profile of colorectal carcinomas. J Mol Diagn 8(2):193–201
22. Azzoni C, Bottarelli L, Campanini N et al (2007) Distinct
molecular patterns based on proximal and distal sporadic colo-
rectal cancer: arguments for different mechanisms in the tumor-
igenesis. Int J Colorectal Dis 22(2):115–126
23. Bressler B, Paszat LF, Chen Z, Rothwell DM, Vinden C, Rabe-
neck L (2007) Rates of new or missed colorectal cancers after
colonoscopy and their risk factors: a population-based analysis.
Gastroenterology 132(1):96–102
Surg Endosc (2013) 27:768–773 773
123