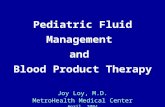
Coagulation and Hemostasis Joy Loy, M.D. MetroHealth Medical Center December 2006.
-
Upload
clemence-terry -
Category
Documents
-
view
216 -
download
0
Transcript of Coagulation and Hemostasis Joy Loy, M.D. MetroHealth Medical Center December 2006.
Coagulation Coagulation and and
HemostasisHemostasis
Joy Loy, M.D.Joy Loy, M.D.MetroHealth Medical CenterMetroHealth Medical Center
December 2006December 2006
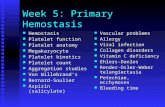
• Hemostatic processHemostatic process
• Coagulation cascadeCoagulation cascade
• FibrinolysisFibrinolysis
• Laboratory studiesLaboratory studies
• MedicationsMedications
• Coagulation disordersCoagulation disorders
HemostasisHemostasis PurposePurpose
Ensure that coagulation mechanisms Ensure that coagulation mechanisms
areare
activated when there is injuryactivated when there is injury
not unnecessarily activatednot unnecessarily activated
Restore tissue blood flow after repair of Restore tissue blood flow after repair of
injury (fibrinolysis) injury (fibrinolysis)
Hemostatic ProcessHemostatic Process
3 main steps3 main steps
Primary hemostasis: local vasoconstriction Primary hemostasis: local vasoconstriction
& platelet plug formation& platelet plug formation
Coagulation cascadeCoagulation cascade
FibrinolysisFibrinolysis
Hemostatic ProcessHemostatic ProcessPlatelet Plug FormationPlatelet Plug Formation
• • vascular injuryvascular injury
• • release and binding of vWF to exposed release and binding of vWF to exposed
blood vessel collagenblood vessel collagen
• • glycoprotein IB on platelet surface glycoprotein IB on platelet surface
membrane binds to vWFmembrane binds to vWF
• • TxATxA2 2 →→ vasoconstriction & platelet vasoconstriction & platelet
adhesionadhesion
• • platelet factor 3 (PF3) phospholipid layer platelet factor 3 (PF3) phospholipid layer
(procoagulant)(procoagulant)
Platelet Activation & AggregationPlatelet Activation & Aggregation
exposed endothelial surfaceexposed endothelial surface
platelets exposed to collagenplatelets exposed to collagen
““activated”activated”
release contents of cytoplasmic granulesrelease contents of cytoplasmic granules
adenosine diphosphate (ADP)adenosine diphosphate (ADP) thromboxane thromboxane
(Tx A(Tx A22))
accelerates platelet accelerates platelet vasoconstriction vasoconstriction aggregation/activationaggregation/activation ↑ ↑ ADP release from ADP release from plateletsplatelets
Hemostatic ProcessHemostatic ProcessCoagulation CascadeCoagulation Cascade
to stabilize and reinforce the weak to stabilize and reinforce the weak
platelet plugplatelet plug
fibrinogen fibrinogen → → fibrinfibrin
3 main steps:3 main steps:
1.1. formation of prothrombin activatorformation of prothrombin activator
2.2. conversion of prothrombin into thrombinconversion of prothrombin into thrombin
3.3. conversion of fibrinogen to fibrinconversion of fibrinogen to fibrin
Coagulation CascadeCoagulation Cascade
TF =tissue factorPK = prekallikreinHK=high molecular kininogena = activated
Roberts HR, et al. Current Concepts for Hemostasis. Anesthesiology 2004;100:3. 722-30.
Coagulation MechanismCoagulation Mechanism
activation of clotting factorsactivation of clotting factors
requires a phospholipid surfacerequires a phospholipid surface tissue factor (TF) extrinsic to the bloodtissue factor (TF) extrinsic to the blood
activated platelet (platelet factor 3 activated platelet (platelet factor 3
phospholipid) intrinsic to blood phospholipid) intrinsic to blood
vitamin-K dependent factors (II, VII, IX, X)vitamin-K dependent factors (II, VII, IX, X)
formation of reaction complexformation of reaction complex labile factors : factors V and VIIIlabile factors : factors V and VIII
Factor VIIIFactor VIII
extrahepatic originextrahepatic origin
2 components (separate genetic control)2 components (separate genetic control)
1.1. VIII R : Ag VIII antigen + vWFVIII R : Ag VIII antigen + vWF
2.2. VIII : C coagulant activity VIII : C coagulant activity
*absence *absence →→ hemophilia Ahemophilia A
von Willebrand factor (vWF)von Willebrand factor (vWF)
•• mediates adhesion of platelets to surface collagenmediates adhesion of platelets to surface collagen
• • carrier of VIII:Ccarrier of VIII:C
• • vWD: vWD: appears to have defect in primary appears to have defect in primary
hemostasis & hemophilia Ahemostasis & hemophilia A
Factor VIIIFactor VIII
F VIII:CF VIII:C F VIII:vwFF VIII:vwF
hemophilia Ahemophilia A decreasedecrease ----------------
vWD type 1vWD type 1 decreasedecrease decreasedecrease
vWD type 2vWD type 2 normalnormal decreasedecrease
Coagulation CascadeCoagulation Cascade
TF =tissue factorPK = prekallikreinHK=high molecular kininogena = activated
Roberts HR, et al. Current Concepts for Hemostasis. Anesthesiology 2004;100:3. 722-30.
Newer Concepts of Coagulation ReactionsNewer Concepts of Coagulation Reactions
2 main functions of tissue factor (TF) 1) to activate factor X to Xa 2) to activate factor IX to IXa
Control MechanismsControl Mechanisms
1) TF pathway inhibitor
2) Protein C system
3) Antithrombin (e.g. AT III)
4) Glycoaminoglycans
APC: activated protein CAT : antithrombinGAG: glycoaminoglycansT : thrombinPC : protein CS : protein STF : tissue factorTM : thrombomodulin
Antithrombin III (AT III)Antithrombin III (AT III)
naturally-occuring anticoagulantnaturally-occuring anticoagulant
binds to factors IXa, Xa, XIa, XIIa (slow)binds to factors IXa, Xa, XIa, XIIa (slow)
accelerated by accelerated by heparinheparin manyfold manyfold
Implication:Implication:
Heparin has almost Heparin has almost NONO anticoagulant anticoagulant
action action without without AT III AT III
Coagulation FactorsCoagulation Factors
FACTORSFACTORS PLASMA t ½PLASMA t ½
(hrs)(hrs)
Fibrinogen (I)Fibrinogen (I) 72-12072-120
Prothrombin Prothrombin (II)(II)
60-7060-70
VV 12-1612-16
VIIVII 3-63-6
VIIIVIII 8-128-12
IXIX 18-2418-24
XX 30-4030-40
FACTORSFACTORS PLASMA t ½ PLASMA t ½
(hrs)(hrs)
XIXI 5252
XIIXII 6060
Protein CProtein C 66
Protein S Protein S (total)(total)
4242
Tissue factorTissue factor ----
ThrombomodulThrombomodulinin
----
antithrombinantithrombin 7272
Roberts HR, et al. Current Concepts for Hemostasis. Anesthesiology 2004;100:3. 722-30.
FibrinolysisFibrinolysis
Plasminogen Plasminogen →→ plasmin plasmin
Release of tPA by the Release of tPA by the
endotheliumendothelium
Lysis of clotLysis of clot→ → FDPs or FSPsFDPs or FSPs
Reopening of blood vesselReopening of blood vessel
Laboratory MonitoringLaboratory MonitoringProthrombin Time (PT)Prothrombin Time (PT)
test of test of extrinsicextrinsic pathway activity pathway activity
measures vitamin K - dependent factors measures vitamin K - dependent factors
activity (factors II, VII, IX, X)activity (factors II, VII, IX, X)
thromboplastin + Cathromboplastin + Ca+2+2 to plasma = clotting to plasma = clotting
timetime
normal values: 12-14 secondsnormal values: 12-14 seconds
International Normalized Ratio (INR)International Normalized Ratio (INR)
▪ ▪ standardizes PT reportingstandardizes PT reporting normal values: 0.8 -1.2 secondsnormal values: 0.8 -1.2 seconds
Laboratory MonitoringLaboratory Monitoring Prothrombin Time (PT)Prothrombin Time (PT)
monitors coumadin therapymonitors coumadin therapy
most sensitive to alteration in F VII levelsmost sensitive to alteration in F VII levels
prolonged: 55 % prolonged: 55 % ↓ ↓ of normal F VII activityof normal F VII activity
antithrombotic activity: reduction of factor antithrombotic activity: reduction of factor
II and factor X activity (after several days)II and factor X activity (after several days)
Laboratory MonitoringLaboratory Monitoring Activated Partial Prothrombin Time (aPTT)Activated Partial Prothrombin Time (aPTT)
test for test for intrinsicintrinsic and and commoncommon pathways pathways
dependent on activity of all coagulation dependent on activity of all coagulation
factors, except VII and XIIIfactors, except VII and XIII
normal values: 25 -35 secondsnormal values: 25 -35 seconds
monitors heparin tx & screen for hemophiliamonitors heparin tx & screen for hemophilia
Laboratory MonitoringLaboratory Monitoring Activated Prothrombin Time (aPTT)Activated Prothrombin Time (aPTT)
prolonged: heparin, thrombin inhibitors, prolonged: heparin, thrombin inhibitors,
fibrin degradation products (FDP)fibrin degradation products (FDP)
citrated plasma + surface activators + citrated plasma + surface activators +
phospholipid phospholipid
prolonged only if coagulation factors prolonged only if coagulation factors
reduced to < 30 % of normalreduced to < 30 % of normal
Laboratory MonitoringLaboratory Monitoring Activated Clotting Time (ACT)Activated Clotting Time (ACT)
monitors heparin anticoagulation in the monitors heparin anticoagulation in the
OR (cardiac and vascular surgeries)OR (cardiac and vascular surgeries)
normal values: 90 - 120 seconds normal values: 90 - 120 seconds
Laboratory MonitoringLaboratory MonitoringThrombin Clotting Time (TCT)Thrombin Clotting Time (TCT)
reflects abnormalities in fibrinogen reflects abnormalities in fibrinogen → → fibrinfibrin
plasma + excessive amount of thrombinplasma + excessive amount of thrombin
prolonged: heparin, thrombin inhibitors, prolonged: heparin, thrombin inhibitors,
low fibrinogen, dysfibrinogenemialow fibrinogen, dysfibrinogenemia
monitors hirudin, bivalirudin, LMWH txmonitors hirudin, bivalirudin, LMWH tx
INR & PT may be normal or INR & PT may be normal or ↑ ↑
TTCT prolonged with adequate therapeutic CT prolonged with adequate therapeutic
levelslevels
Laboratory MonitoringLaboratory Monitoring
Thromboelastography (TEG)Thromboelastography (TEG) continuous profiles during all phases of continuous profiles during all phases of
clot formationclot formation
provides more accurate picture of in vivo provides more accurate picture of in vivo
coagulation processcoagulation process to evaluate:to evaluate:
• • hypo / hypercoagulable state hypo / hypercoagulable state
• • hemophiliahemophilia
• • dilutional coagulopathydilutional coagulopathy
• • rare coagulation disorders anticoagulation txrare coagulation disorders anticoagulation tx
• • coagulation problems with liver coagulation problems with liver transplantationtransplantation
Bleeding timeBleeding time
monitors platelet functionmonitors platelet function
not specific indicator of platelet not specific indicator of platelet
functionfunction
not very reliablenot very reliable
very operator - dependentvery operator - dependent
variable from each institutionvariable from each institution
Bleeding timeBleeding time
other factors: degree of venostasis, depth other factors: degree of venostasis, depth
and direction of incisionand direction of incision
no evidence as no evidence as
• • a predictor of risk of hemorrhagea predictor of risk of hemorrhage
• • useful indicator of efficacy of antiplatelet useful indicator of efficacy of antiplatelet
therapytherapy
insensitive to mild platelet defects insensitive to mild platelet defects
Laboratory MonitoringLaboratory Monitoring Platelet Function Analyzer (PFA) - 100Platelet Function Analyzer (PFA) - 100
relatively new global test of platelet relatively new global test of platelet
adhesion and aggregationadhesion and aggregation
advantagesadvantages noninvasive, simple, easy to performnoninvasive, simple, easy to perform
very sensitive in detecting platelet defectsvery sensitive in detecting platelet defects
associated with vWDassociated with vWD
sensitive to dx of acquired platelet defects sensitive to dx of acquired platelet defects
(ASA, NSAID, dietary factors: excessive (ASA, NSAID, dietary factors: excessive
cocoa intake)cocoa intake)
monitors pro-hemostatic treatmentmonitors pro-hemostatic treatment
DDAVP & platelet transfusionsDDAVP & platelet transfusions
Laboratory MonitoringLaboratory Monitoring
PFA-100PFA-100
LimitationsLimitations
■ ■ inflexibilityinflexibility
■ ■ results should be interpreted in the results should be interpreted in the
context of either a simultaneously or context of either a simultaneously or
recently drawn full blood countrecently drawn full blood count
■ ■ platelet count < 80,000 or Hct < 30% platelet count < 80,000 or Hct < 30%
will prolonged CT even if no platelet will prolonged CT even if no platelet
abnormalabnormal
LABORATORY LABORATORY
TESTTESTCOMPONENTS COMPONENTS
MEASUREDMEASURED
NORMAL NORMAL VALUESVALUES
Bleeding timeBleeding time platelet functionplatelet function
vascular integrityvascular integrity
3 - 10 3 - 10 minsmins
PTPTI, II, V, VII, IX, XI, II, V, VII, IX, X
12 - 14 12 - 14 secssecs
PTTPTTI, II, V, VIII, IX, X, XI, XIII, II, V, VIII, IX, X, XI, XII
24 - 35 24 - 35 secssecs
Thrombin timeThrombin time I, III, II 12 - 20 12 - 20 secssecs
Implications for TherapyImplications for Therapy
Congenital & acquired factor Congenital & acquired factor
deficienciesdeficiencies historyhistory
medicationsmedications
congenital factors: vWD, hemophilia, platelet disorderscongenital factors: vWD, hemophilia, platelet disorders
acquired disorders: multifactor-renal, hepatic, DICacquired disorders: multifactor-renal, hepatic, DIC
Antiplatelet medicationsAntiplatelet medications
AnticoagulantsAnticoagulants
Drugs affecting CoagulationDrugs affecting Coagulation
HEMOSTATICHEMOSTATIC
PROCESSPROCESS
AFFECTEDAFFECTED
CLASS OF CLASS OF
DRUGSDRUGS SPECIFICSPECIFIC
DRUGSDRUGS
1º platelet plug 1º platelet plug formation inhibitionformation inhibition
antiplatelet drugsantiplatelet drugs reversible: NSAIDreversible: NSAID
irreversible: ASAirreversible: ASA
coagulation coagulation cascadecascade
IV anticoagulantsIV anticoagulants
oral anticoagulantsoral anticoagulants
standard and LMW standard and LMW heparinsheparins
warfarinwarfarin
fibrinolysisfibrinolysis fibrinolytic agentsfibrinolytic agents StreptokinaseStreptokinase
UrokinaseUrokinase
t-PAt-PA
Prostaglandin SynthesisProstaglandin Synthesis
arachidonic acidarachidonic acid cyclooxygenasecyclooxygenase
prostaglandin Gprostaglandin G22
peroxidaseperoxidase
prostaglandin Hprostaglandin H22
prostacyclinprostacyclin thromboxanethromboxane
synthetasesynthetase synthetase synthetase
prostacyclinprostacyclin thromboxane Athromboxane A22
PG FPG F1a1a thromboxane Bthromboxane B22
Mechanism of ActionMechanism of ActionASPIRINASPIRIN
arachidonic acidarachidonic acid ASPIRINASPIRIN
cyclooxygenasecyclooxygenase
prostaglandin Gprostaglandin G22
peroxidaseperoxidase
prostaglandin Hprostaglandin H22
prostacyclinprostacyclin thromboxanethromboxane
synthetasesynthetase synthetase synthetase
prostacyclinprostacyclin thromboxane A2thromboxane A2
PG FPG F1a1a thromboxane B2thromboxane B2
Mechanism of ActionMechanism of Action
ASPIRIN and NSAIDSASPIRIN and NSAIDS
arachidonic acidarachidonic acid ASPIRINASPIRIN
cyclooxygenasecyclooxygenase
prostaglandin Gprostaglandin G22 NSAIDSNSAIDS
peroxidaseperoxidase
prostaglandin Hprostaglandin H22
prostacyclinprostacyclin thromboxanethromboxane
synthetasesynthetase synthetase synthetase
prostacyclinprostacyclin thromboxane A2thromboxane A2
PG FPG F1a1a thromboxane B2thromboxane B2
Antiplatelet MedicationsAntiplatelet Medications
DRUGDRUG
SITE OFSITE OF
ACTIONACTION ROUTROUTEE
PLASMPLASMAA
t 1/2t 1/2
META-META-
BOLISBOLISMM
Ø PRIORØ PRIOR
PROCEDURPROCEDUREE
↑ ↑ PT / PT /
PTTPTT
ANTI – ANTI –
DOTEDOTE
AspirinAspirin COX 1COX 1
and 2 and 2 oraloral 20 min20 min hepatihepati
cc 7 days7 days No/NoNo/No nonenone
Dipyrida-Dipyrida-molemole
adenosinadenosinee
oraloral 40 min40 min hepatihepaticc
24 hrs24 hrs No/NoNo/No nonenone
ClopidogrClopidogrelel (Plavix)(Plavix)
ADPADP oraloral 7 hrs7 hrs hepatihepaticc
5 days5 days No/NoNo/No nonenone
TiclodipinTiclodipinee (Ticlid)(Ticlid)
ADPADP oraloral 4 days4 days hepatihepaticc
10 days10 days No/NoNo/No nonenone
AbciximaAbciximabb (ReoPro)(ReoPro)
GPIIb-IIIaGPIIb-IIIa IVIV 30 min30 min renalrenal 72 hrs72 hrs No/NoNo/No nonenone
EptifibatidEptifibatidee
GPIIb-IIIaGPIIb-IIIa IVIV 2.5 2.5 hrshrs
renalrenal 24 hrs24 hrs No/NoNo/No nonenone
TirobanTiroban GPIIb-IIIaGPIIb-IIIa IVIV 2 hrs2 hrs renalrenal 24 hrs24 hrs No/NoNo/No hemo-hemo-dialysisdialysis
Roberts HR, et al. Current Concepts for Hemostasis. Anesthesiology 2004;100:3. 722-30.
Non-steroidal Anti-inflammatory MedicationsNon-steroidal Anti-inflammatory Medications
DRUGDRUG
SITE OFSITE OF
ACTIONACTION ROUTROUTEE
PLASMPLASMAA
t 1/2t 1/2
META-META-
BOLISBOLISMM
Ø PRIORØ PRIOR
PROCEDURPROCEDUREE
↑ ↑ PT / PT /
PTTPTT
ANTI – ANTI –
DOTEDOTE
PiroxicamPiroxicam COX 1 & COX 1 & 22
oraloral 50 hrs50 hrs hepatichepatic 10 days10 days No/NoNo/No nonenone
Indome –Indome –
thacinthacinCOX 1 & COX 1 & 22
oral/oral/
suppsupp 5 hrs5 hrs hepatichepatic 48 hrs48 hrs No/NoNo/No nonenone
KetorolacKetorolac COX 1 & COX 1 & 22
oral / oral /
IVIV 5-7 5-7 hrshrs
hepatichepatic 48 hrs48 hrs No/NoNo/No nonenone
IbuprofenIbuprofen COX 1 & COX 1 & 22
oraloral 2 hrs2 hrs hepatichepatic 24 hrs24 hrs No/NoNo/No nonenone
naproxennaproxen COX 1 & COX 1 & 22
oraloral 13 hrs13 hrs hepatichepatic 48 hrs48 hrs No/NoNo/No nonenone
DiclofenaDiclofenacc
COX 1 & COX 1 & 22
oraloral 2 hrs2 hrs hepatichepatic 24 hrs24 hrs No/NoNo/No nonenone
CelecoxibCelecoxib COX 2COX 2 oraloral 10-1710-17
hrshrshepatichepatic nonenone No/NoNo/No nonenone
Roberts HR, et al. Current Concepts for Hemostasis. Anesthesiology 2004;100:3. 722-30.
Anticoagulants & ThrombolyticsAnticoagulants & Thrombolytics
DRUGDRUG SITE OF SITE OF ACTIONACTION
ROUTROUTEE
PLASMPLASMAA
t 1/2t 1/2
EXCRE-EXCRE-
TIONTIONØ PRIORØ PRIOR
PROCEDURPROCEDUREE
↑ ↑ PT / PT /
PTTPTT
ANTI – ANTI –
DOTEDOTE
UnfractionUnfraction-ated -ated heparinheparin
IIa/XaIIa/Xa IV/SCIV/SC 1.5 hrs1.5 hrs hepatichepatic
6 hrs6 hrs No/No/
YesYesprotaminprotaminee
LMWHsLMWHs XaXa
IIIaIIIa SCSC 4.5 hrs4.5 hrs renalrenal 12-24 hrs12-24 hrs No/NoNo/No protaminprotamin
ee
(partial)(partial)
Strepto - Strepto - kinasekinase
plasmi –plasmi –
nogennogen IVIV 23 23
minsmins hepatichepatic
3 hrs3 hrs Yes/Yes/
YesYesantifibri-antifibri-
nolyticsnolytics
t-PAt-PA plasmi –plasmi –
nogennogen IVIV <5 min<5 min
hepatichepatic 1 hr1 hr Yes/Yes/
YesYesantifibri-antifibri-nolyticsnolytics
OralOral
AnticoaguAnticoagu--
lantslants
vit-K vit-K dep.dep.
factorsfactors
OralOral 2-2-4days4days
hepatichepatic
2-4 days2-4 days Yes/Yes/NoNo
Vit. K, Vit. K, rFVIIarFVIIa
Plasma, Plasma, ProthromProthrom. . complex complex conc.conc.
Roberts HR, et al. Current Concepts for Hemostasis. Anesthesiology 2004;100:3. 722-30.
Other AnticoagulantsOther Anticoagulants
DRUGDRUG
SITE SITE OFOF
ACTIOACTIONN
ROUTROUTEE
PLASMPLASMAA
t 1/2t 1/2
META-META-
BOLISMBOLISMØ PRIORØ PRIOR
PROCEDURPROCEDUREE
↑ ↑ PT/ PT/ PTT PTT
ANTI – ANTI –
DOTEDOTE
Pentasac- Pentasac-
charidecharide XaXa IVIV 14-17 14-17
hrshrs renalrenal 4 days4 days No/NoNo/No rFVIIa?rFVIIa?
BivalirudinBivalirudin IIaIIa IVIV 25 min25 min hepatichepatic 2-3 hrs2-3 hrs Yes/Yes/
YesYesNoneNone
ArgatrobanArgatroban IIaIIa IVIV 45 min45 min hepatichepatic 4-6hrs*4-6hrs* Yes/Yes/
YesYesNoneNone
HirudinHirudin IIaIIa IVIV 1.5 hr1.5 hr renalrenal 8 hrs*8 hrs* Yes/Yes/
YesYesPMMA PMMA dialysidialysiss
Activated Activated Protein CProtein C
(APC)(APC)
Va/Va/
VIIIaVIIIa IVIV 2 hrs2 hrs hepatichepatic 12 hrs12 hrs No/No/
YesYesnonenone
XimelagatrXimelagatranan
IIaIIa IVIV 3 hrs3 hrs renalrenal 24 hrs24 hrs Yes/Yes/
YesYesnonenone
PMMA= polymethyl-methyl acrylatePMMA= polymethyl-methyl acrylate
*Argatroban &lepirudin may *Argatroban &lepirudin may ↑↑ the normal PT 4-5 secs the normal PT 4-5 secsRoberts HR, et al. Current Concepts for Hemostasis. Anesthesiology 2004;100:3. 722-30.
Oral AnticoagulantsOral AnticoagulantsWarfarinWarfarin
inhibits synthesis of vitamin - k inhibits synthesis of vitamin - k
dependent factors II, VII, IX, X and dependent factors II, VII, IX, X and
protein C & Sprotein C & S
reversal:reversal: stopping medication and waiting for ~4 stopping medication and waiting for ~4
days for PT normalizationdays for PT normalization
vitamin K PO or IV (1-2mg)vitamin K PO or IV (1-2mg)
immediate: rFVIIa, FFP (1-2 units),immediate: rFVIIa, FFP (1-2 units),
prothrombin complex concentrateprothrombin complex concentrate
check PT prior to surgerycheck PT prior to surgery
Oral AnticoagulantsOral AnticoagulantsWarfarinWarfarin
biphasic effect on PT and INRbiphasic effect on PT and INR initial initial ↑↑: : ↓↓ F VII (shortest t ½) to 55 % F VII (shortest t ½) to 55 %
of normalof normal
subsequent subsequent ↑↑: ↓ : ↓ F II and X – therapeutic F II and X – therapeutic
anticoagulantanticoagulant
discontinuationdiscontinuation return to normal: F VII followed by F II & Xreturn to normal: F VII followed by F II & X
caution: INR =/< 1.4 no assurance of caution: INR =/< 1.4 no assurance of
normal coagulationnormal coagulation
Unfractionated HeparinUnfractionated Heparin
negatively charged, water - soluble negatively charged, water - soluble
glycosaminoglycanglycosaminoglycan
extracted from porcine gut or bovine lungextracted from porcine gut or bovine lung
binds and binds and ↑↑ anti - thrombin III (AT III) activity anti - thrombin III (AT III) activity
to 1,000 fold to 1,000 fold →→binds & inactivates factors IIabinds & inactivates factors IIa
and factor Xaand factor Xa
degree of inhibition: F Xa = IIa degree of inhibition: F Xa = IIa
* * LMWH inhibition of Xa > IIaLMWH inhibition of Xa > IIa
lesser inhibition on F XIa, XIa and F XIIalesser inhibition on F XIa, XIa and F XIIa
Unfractionated HeparinUnfractionated Heparin
Low-dose or “minidose”Low-dose or “minidose”
5,000 U SC q 12 hrs for 5,000 U SC q 12 hrs for
thromboprophylaxisthromboprophylaxis
peak action: 40 - 50 minutespeak action: 40 - 50 minutes
duration 4 - 6 hrsduration 4 - 6 hrs
low risk for hemorrhage during anesthesia low risk for hemorrhage during anesthesia
or surgeryor surgery
4 reported cases of SEH with CNB4 reported cases of SEH with CNB
Unfractionated HeparinUnfractionated HeparinStandard DoseStandard Dose
regular doses for therapeutic anticoagulationregular doses for therapeutic anticoagulation
high risk of bleeding during & after surgeryhigh risk of bleeding during & after surgery
stop at least 6 hrs before surgerystop at least 6 hrs before surgery
restarted ~ 12 hrs postop if needed with close restarted ~ 12 hrs postop if needed with close
monitoringmonitoring
immediate reversal: protamineimmediate reversal: protamine
Low Molecular Weight Heparin (LMWH)Low Molecular Weight Heparin (LMWH)
4,000-6,500 daltons (vs. standard heparin 4,000-6,500 daltons (vs. standard heparin
3,000 -30,000 daltons3,000 -30,000 daltons
retains anti-Xa activityretains anti-Xa activity
less anti -IIa than standard heparinless anti -IIa than standard heparin
enhances AT-III interaction with F IIa & F Xaenhances AT-III interaction with F IIa & F Xa
degree of inhibition: F Xa > IIa degree of inhibition: F Xa > IIa
LMWH in the U.S.LMWH in the U.S.
LMWHLMWH TRADETRADE
NAMENAME
MOLECULAMOLECULARR
WEIGHTWEIGHT
(daltons)(daltons)
HALF - LIFEHALF - LIFE
(minutes)(minutes)Anti Xa: Anti Xa: Anti IIaAnti IIa
DaltepariDalteparinn
FragminFragmin 5,0005,000 120120 2:12:1
EnoxapariEnoxaparinn
LovenoxLovenox
4,5004,500 150150 2.7:12.7:1
DanaparoDanaparoidid
OrgaranOrgaran 6,5006,500 1,1001,100 20:120:1
ArdeparinArdeparin NormifloNormiflo
6,0006,000 200200 2:12:1
Standard Standard HeparinHeparin
14,00014,000 60-9060-90 1:11:1
Standard Heparin vs. LMWHStandard Heparin vs. LMWH
PARAMETERSPARAMETERS STANDARD HEPARINSTANDARD HEPARIN LMWHLMWH
MOLECULAR MOLECULAR WEIGHTWEIGHT
3, 000 - 30,000 daltons3, 000 - 30,000 daltons 4,000-6,500 daltons4,000-6,500 daltons
BIOAVAILABILITYBIOAVAILABILITYvariable due to binding to variable due to binding to
plasma protein & plasma protein &
macrophagesmacrophages
predictablepredictable
MONITORINGMONITORING PTTPTT
dose adjusted based on dose adjusted based on
PTTPTT
no need for no need for
monitoring monitoring
no dose adjustmentsno dose adjustments
HALF – LIFEHALF – LIFEvariable; dose-dependent variable; dose-dependent
(30 min for 25 u/kg, 150 (30 min for 25 u/kg, 150
mins with 400 u/kg)mins with 400 u/kg)
4-6 hrs4-6 hrs
CLEARANCECLEARANCE hepatichepatic renalrenal
Standard Heparin vs. LMWHStandard Heparin vs. LMWH PARAMETERSPARAMETERS STANDARD HEPARINSTANDARD HEPARIN LMWHLMWH
EFFECT ON EFFECT ON PLATELETSPLATELETS
Higher incidence of HITHigher incidence of HIT
Inhibition of platelet Inhibition of platelet
functionfunction
Inhibits platelet-Inhibits platelet-
endotheliumendothelium
interactioninteraction
Lower incidence of Lower incidence of
HITHIT
Less inhibitionLess inhibition
No interactionNo interaction
RISK OF RISK OF BLEEDINGBLEEDING
higherhigher LowerLower
ANTI Xa: IIa ANTI Xa: IIa ACTIVITYACTIVITY
1:11:1 2:12:1
REVERSALREVERSAL protamineprotamine Only anti-IIa (90%) but Only anti-IIa (90%) but
not anti-Xa (60%) not anti-Xa (60%)
activity reversed by activity reversed by
protamine (1 mg/100 protamine (1 mg/100
anti-Xa units LMWHanti-Xa units LMWH
COSTCOST inexpensiveinexpensive expensiveexpensive
Recombinant Factor VIIaRecombinant Factor VIIa(NovoSeven)(NovoSeven)
FDA approved for use in hemophilia & patients FDA approved for use in hemophilia & patients
with inhibitorswith inhibitors
enhances the TF pathwayenhances the TF pathway
binds loosely to platelets and directly activates binds loosely to platelets and directly activates
F X F X →→ ↑↑ thrombin generation with F Va present thrombin generation with F Va present
never completelynever completely normalizes thrombin normalizes thrombin
generation but enhances hemostasisgeneration but enhances hemostasis
dose: 90-120 mcg/kg q 2 hrs x 1dose: 90-120 mcg/kg q 2 hrs x 1stst 24 hrs 24 hrs
Recombinant Factor VIIaRecombinant Factor VIIa
variable individual thrombin- variable individual thrombin-
generating capacitygenerating capacity megadoses: 150-300 mcg/kgmegadoses: 150-300 mcg/kg
““off label” use (non - FDA approved)off label” use (non - FDA approved) liver diseaseliver disease
liver transplantliver transplant
traumatrauma
ICHICH
platelet disordersplatelet disorders
Recombinant Factor VIIaRecombinant Factor VIIa
common denominator: defective thrombin common denominator: defective thrombin
generationgeneration
thrombocytopenia ▪ thrombocytopenia ▪ hypothermiahypothermia
↓↓ plasma coagulation proteins plasma coagulation proteins ▪ ▪ hyperfibrinolysishyperfibrinolysis
dilutional coagulopathydilutional coagulopathy
prophylactic use reported for retropubic prophylactic use reported for retropubic
prostatectomy, hepatectomyprostatectomy, hepatectomy
potential use: Jehovah’s witnesspotential use: Jehovah’s witness
Disorders of Hemostatic MechanismDisorders of Hemostatic Mechanism
Classification: depends on involvement ofClassification: depends on involvement of
platelets and/or clotting factorsplatelets and/or clotting factors
and/or presence of inhibitors (such as FDP)and/or presence of inhibitors (such as FDP)
TreatmentTreatment
• • transfusion of platelets and/or clotting factorstransfusion of platelets and/or clotting factors
• • pharmacologic agents affectingpharmacologic agents affecting
Platelets fx (DDAVP, antiplatelet drugs)Platelets fx (DDAVP, antiplatelet drugs)
Clotting factors (vit. K, coumadin, heparin)Clotting factors (vit. K, coumadin, heparin)
Inhibitors (antifibrinolytics, protamine, fibrinolytics)Inhibitors (antifibrinolytics, protamine, fibrinolytics)
Hereditary Platelet DisorderHereditary Platelet Disordervon Willebrand Disease (vWD)von Willebrand Disease (vWD)
most common congenital bleeding most common congenital bleeding
disorderdisorder
quantitative or qualitative abn. of vWFquantitative or qualitative abn. of vWF
Type 1: most common formType 1: most common form
partial partial quantitativequantitative deficiency of vWF deficiency of vWF
autosomal dominantautosomal dominant
mucocutaneous bleedingmucocutaneous bleeding
hematology consult prior to surgeryhematology consult prior to surgery
prolonged bleeding time, normal plateletprolonged bleeding time, normal platelet
Hereditary Platelet DisordersHereditary Platelet Disordersvon Willebrand Disease (vWD)von Willebrand Disease (vWD)
Type 2: Type 2: qualitativequalitative alterations in the vWF structure alterations in the vWF structure
& function& function
Type 3: least common and most severeType 3: least common and most severe
Complete Complete absenceabsence of vWF in plasma or storage of vWF in plasma or storage
organelleorganelle
Autosomal recessiveAutosomal recessive
acquired vWDacquired vWD
Lymphoproliferative disease ▪ cardiac/valvular diseaseLymphoproliferative disease ▪ cardiac/valvular disease
Tumors ▪ medications (valproic acid)Tumors ▪ medications (valproic acid)
Autoimmune diseaseAutoimmune disease ▪ hypothyroidism ▪ hypothyroidism
Hereditary Platelet DisordersHereditary Platelet Disordersvon Willebrand Diseasevon Willebrand Disease
Treatment:Treatment: Desmopressin (DDAVP) Desmopressin (DDAVP)
synthetic analog of vasopressinsynthetic analog of vasopressin
↑↑ both F VIII and vWF 3 - 5x in 30 minsboth F VIII and vWF 3 - 5x in 30 mins
preop prophylactic dose: 0.3 mcg/kg IV in preop prophylactic dose: 0.3 mcg/kg IV in
50 -100 ml NS infused 30-60 mins q 12-24 50 -100 ml NS infused 30-60 mins q 12-24
hrs PRNhrs PRN
duration 8-10 hrsduration 8-10 hrs
intranasal dose: 300 mcg – for home intranasal dose: 300 mcg – for home
treatment, not for preop prophylaxistreatment, not for preop prophylaxis
Hereditary Bleeding DisordersHereditary Bleeding Disordersvon Willebrand Diseasevon Willebrand Disease
DDAVPDDAVP
vasomotor effect: flushing, vasomotor effect: flushing, ↑↑HRHR, , headacheheadache
SE: hyponatremia, seizuresSE: hyponatremia, seizures
not for children < 3 yrs oldnot for children < 3 yrs old
unresponsive to DDAVP (15%)unresponsive to DDAVP (15%)
cryoprecipitatecryoprecipitate
FFPFFP
factor VIII / vWF concentratefactor VIII / vWF concentrate
Acquired Platelet DisordersAcquired Platelet Disorders
Thrombocytopenia : platelets <150,000/mmThrombocytopenia : platelets <150,000/mm33
inadequate production by bone marrowinadequate production by bone marrow
splenic sequestrationsplenic sequestration
consumption coagulopathyconsumption coagulopathy
dilutional thrombocytopeniadilutional thrombocytopenia
immunogenic destructionimmunogenic destruction
Platelet dysfunctionPlatelet dysfunction myeloproliferative and myelodysplastic myeloproliferative and myelodysplastic
syndromessyndromes
renal failure, liver disease, DIC, CPBrenal failure, liver disease, DIC, CPB
drugs: NSAIDS, ASAdrugs: NSAIDS, ASA
* * DDAVP: tx platelet dysfunction due to uremia, liver DDAVP: tx platelet dysfunction due to uremia, liver
disease, and patients on ASA for CABGdisease, and patients on ASA for CABG
Hereditary Factor DeficienciesHereditary Factor DeficienciesHemophiliaHemophilia
x-linked recessive conditions (males only)x-linked recessive conditions (males only)
type A : F VIII:C deficiency (Classical type A : F VIII:C deficiency (Classical
Hemophilia)Hemophilia)
B : F IX deficiency (Christmas disease)B : F IX deficiency (Christmas disease)
C : F XI deficiency C : F XI deficiency
unexplained bruising or bleeding in young unexplained bruising or bleeding in young
males, usually ~ 1 yr of agemales, usually ~ 1 yr of age
joint & muscle bleeding joint & muscle bleeding → → arthropathyarthropathy
Hereditary Factor DeficienciesHereditary Factor DeficienciesHemophiliaHemophilia
■ ■ screening: prolonged PTTscreening: prolonged PTT
■ ■ hemophilia Ahemophilia A
mildmild
moderatemoderate
severe : life-threatening (CNS severe : life-threatening (CNS
bleed)bleed)
treatmenttreatment
factor replacementfactor replacement
rFVIIarFVIIa
Factor VIII Concentrate Necessary for Factor VIII Concentrate Necessary for HemostasisHemostasis
Factor VIII Factor VIII ConcentrateConcentrate
(% of normal)(% of normal)
Spontaneous hemorrhageSpontaneous hemorrhage 1-3 %1-3 %
Moderate traumaModerate trauma 4-8 %4-8 %
Hemarthrosis/deep skeletal Hemarthrosis/deep skeletal
muscle hemorrhagemuscle hemorrhage
10-15 %10-15 %
Major surgeryMajor surgery > 30%> 30%
Acquired Factor DeficienciesAcquired Factor Deficiencies
Vitamin - K deficiencyVitamin - K deficiency
malabsorption syndromesmalabsorption syndromes
pancreatic insufficiencypancreatic insufficiency
biliary obstructionbiliary obstruction
GI obstructionGI obstruction
treatment: vitamin Ktreatment: vitamin K
Platelet Dysfunction, Factor Deficiencies & Platelet Dysfunction, Factor Deficiencies & Presence of InhibitorsPresence of Inhibitors
Liver diseaseLiver disease
• • synthesis of coagulation factors (except VIII),synthesis of coagulation factors (except VIII),
anticoagulants, ATIII, protein C & S, plasminogenanticoagulants, ATIII, protein C & S, plasminogen
• • clearance of activated clotting factors, tPA, FDPsclearance of activated clotting factors, tPA, FDPs
DICDIC
Hypercoagulable StatesHypercoagulable StatesFactor V Leiden MutationFactor V Leiden Mutation
glutamine is substituted for arginine at glutamine is substituted for arginine at
position 506position 506→ → resistant to inactivation by resistant to inactivation by
protein Cprotein C
dx: genetic screening dx: genetic screening
↑↑ risk for DVT in lower extremities & brainrisk for DVT in lower extremities & brain
homozygous (20x) >heterozygous (7x)homozygous (20x) >heterozygous (7x)
if asymptomatic: no anticoagulationif asymptomatic: no anticoagulation
Hypercoagulable StatesHypercoagulable States
Factor V Leiden MutationFactor V Leiden Mutation
TreatmentTreatment
▪ ▪ warfarin x 6 mos or until warfarin x 6 mos or until
thrombosis free for 2 mosthrombosis free for 2 mos
▪ ▪ LMWH x 2 wks after warfarin LMWH x 2 wks after warfarin
then retestedthen retested
▪ ▪ long term anticoagulation if long term anticoagulation if
persist persist
or recurrent thrombotic eventor recurrent thrombotic event
Idiopathic Thrombocytopenic PurpuraIdiopathic Thrombocytopenic Purpura(ITP)(ITP)
more commonly found in childrenmore commonly found in children
diagnosis of exclusiondiagnosis of exclusion
petechia <20,000x 10petechia <20,000x 1099/l platelets/l platelets
bleeding <10,000x 10bleeding <10,000x 1099/l/l
medical managementmedical management
Blood Component TherapyBlood Component TherapyPlatelet TransfusionPlatelet Transfusion
1 unit 1 unit ↑ ↑ platelets count 10,000 mmplatelets count 10,000 mm33
adult dose: 1 unit/10 kg BW within 24 hrsadult dose: 1 unit/10 kg BW within 24 hrs indications (NIH)indications (NIH)
▪ ▪ thrombocytopenia with clinical coagulopathythrombocytopenia with clinical coagulopathy
10, 000 in ITP10, 000 in ITP
20, 000 in bone marrow suppression20, 000 in bone marrow suppression
40,000 during massive transfusion40,000 during massive transfusion
▪ ▪ pplatelet dysfunction even with latelet dysfunction even with platelets>100,000platelets>100,000
CPBCPB drugs (ASA, etc)drugs (ASA, etc)
uremiauremia thrombastheniathrombasthenia
Blood Component TherapyBlood Component TherapyTransfusion of FFPTransfusion of FFP
1) replacement of isolated factor deficiency1) replacement of isolated factor deficiency
2) reversal of coumadin2) reversal of coumadin
3) antitrombin III deficiency3) antitrombin III deficiency
4) treatment of immunodeficiencies4) treatment of immunodeficiencies
5) treatment of TTP5) treatment of TTP
6) massive blood transfusion6) massive blood transfusion
Blood Component TherapyBlood Component TherapyCryoprecipitateCryoprecipitate
contains significant levels of factor contains significant levels of factor
VIIIC, factor VIII: vwF, XIII, fibrinogenVIIIC, factor VIII: vwF, XIII, fibrinogen
indications:indications:
1) hemophilia1) hemophilia
2) von Willebrand disease2) von Willebrand disease
3) fibrinogen deficiencies3) fibrinogen deficiencies
4) uremic platelet dysfunction4) uremic platelet dysfunction
ReferencesReferences
Roberts HR, Monroe DM, Escobar MA. Current Concepts of Roberts HR, Monroe DM, Escobar MA. Current Concepts of Hemostasis. Anesthesiology 2004; 100:722-30.Hemostasis. Anesthesiology 2004; 100:722-30.
De Souza GJ. Anticoagulation and Central Neuraxial Anesthesia. De Souza GJ. Anticoagulation and Central Neuraxial Anesthesia. Progress in Anesthesiology. 2000;vol XIV, Chap 9: 132-148.Progress in Anesthesiology. 2000;vol XIV, Chap 9: 132-148.
Petrovich, CT. An approach to the patient who may have a Petrovich, CT. An approach to the patient who may have a bleeding disorder. 2005 ASA nnual Meeting Refresher Course bleeding disorder. 2005 ASA nnual Meeting Refresher Course Lectures. Atlanta, GA. 2006;241:1-6.Lectures. Atlanta, GA. 2006;241:1-6.
Kelly RE, Yao FF. Hemophilia and Coagulation Disorders. Yao & Kelly RE, Yao FF. Hemophilia and Coagulation Disorders. Yao & Artusio’s Problem Oriented Anesthesiology 4Artusio’s Problem Oriented Anesthesiology 4thth Ed. Lippincott Ed. Lippincott Williams & Wilkins. 1998. Chapter 40, pp 763-774.Williams & Wilkins. 1998. Chapter 40, pp 763-774.
Fleisher LA. Evidence-based Practice of Anesthesiology. Saunders. Fleisher LA. Evidence-based Practice of Anesthesiology. Saunders. 2004.2004.
Stoelting RK,Dierdorf, SF. Coagulation Disorders. Anesthesia and Stoelting RK,Dierdorf, SF. Coagulation Disorders. Anesthesia and Co-existing diseases 3Co-existing diseases 3rdrd Ed. Churchill Livingston. 1993. Chapter 25, Ed. Churchill Livingston. 1993. Chapter 25, p 407-426.p 407-426.