Cluster of Mycobacterium Chelonae Keratitis Cases ... keratitis with pics.pdf · Cluster of...
Transcript of Cluster of Mycobacterium Chelonae Keratitis Cases ... keratitis with pics.pdf · Cluster of...
-
Cluster of Mycobacterium Chelonae KeratitisCases Following Laser In-situ Keratomileusis
NAVEEN S. CHANDRA, MD, MARK F. TORRES, MD, KEVIN L. WINTHROP, MD,DAVID A. BRUCKNER, SCD, DAVID G. HEIDEMANN, MD, HELENE M. CALVET, MD,
MITCHELL YAKRUS, MS, MPH, BARTLY J. MONDINO, MD,AND GARY N. HOLLAND, MD
PURPOSE: To describe a cluster of Mycobacteriumchelonae keratitis cases involving patients who under-went laser in-situ keratomileusis (LASIK) at a singlerefractive surgery center. DESIGN: Descriptive case series of four patients andcohort study to identify disease associations. METHODS: Examination schedules, diagnostic tests,and therapy were based on best medical judgment. Iso-lates from three patients were compared by pulsed-fieldgel electrophoresis. Epidemiologic studies were per-formed to identify the source of infection. RESULTS: Seven of eight eyes developed M. chelonaekeratitis following bilateral simultaneous LASIK. Eachpatient was thought to have diffuse lamellar keratitisinitially, but all seven eyes were noted to have opacitiessuggestive of infectious keratitis by 13 to 21 days aftersurgery. All eyes had undergone hyperopic LASIK overfour days in April 2001 by one surgeon in a community-based refractive surgery center. A cohort study of allpatients undergoing LASIK at the same center in April2001 revealed that M. chelonae keratitis occurred onlyin persons undergoing correction of hyperopia (seven of
14 eyes vs. none of 217 eyes undergoing myopic LASIK,P < .001). The only difference identified betweenprocedures was use of masks created from a soft contactlens in hyperopic LASIK. Three isolates (three patients)were indistinguishable by pulsed-field gel electrophoresis.Eyes were treated with a combination of antimicrobialagents, including topical azithromycin in three patients,with resolution of infection in all eyes over 6 to 14weeks. The source of infection was not identified onenvironmental cultures. CONCLUSION: Postoperative nontuberculous myco-bacterial keratitis can occur in an epidemic fashionfollowing LASIK. Topical amikacin, azithromycin, clar-ithromycin, ciprofloxacin, or a combination of theseagents, appears to be effective treatment for these in-fections. (Am J Ophthalmol 2001;132:819830. 2001 by Elsevier Science Inc. All rights reserved.)
I NFECTIOUS KERATITIS AFTER REFRACTIVE SURGERY ISuncommon. Nevertheless, there have been several re-ports of bacterial, fungal, and mycobacterial keratitisafter laser in-situ keratomileusis (LASIK).118 Rapidlygrowing mycobacteria (one group of the nontuberculous oratypical mycobacteria) account for a substantial propor-tion of these cases, with Mycobacterium chelonae being themost frequently reported species.1,4,5,9,16 To date, all re-ports of nontuberculous mycobacterial keratitis afterLASIK in the medical literature have described singleisolated cases.1,4,5,9,16
In May 2001, on behalf of the Centers for DiseaseControl and Prevention (CDC), the American Academyof Ophthalmology issued an alert to its members regardingnontuberculous mycobacterial infections after LASIK, inresponse to a reported cluster of cases from a singlecommunity-based refractive surgery center in SouthernCalifornia (published in the American Academy of Oph-thalmologys EyeNet magazine, July 2001, pages 60 to 61).The cluster involved four patients (seven eyes) whodeveloped M. chelonae keratitis after undergoing bilateral,
Accepted for publication Sep 5, 2001.From the Ocular Inflammatory Disease Center, Jules Stein Eye Insti-
tute, and Department of Ophthalmology, UCLA School of Medicine, LosAngeles, California (Drs Chandra, Torres, Mondino, and Holland); TheEpidemic Intelligence Service, Centers for Disease Control and Preven-tion, Atlanta, Georgia (Dr Winthrop), National Center for InfectiousDiseases, Centers for Disease Control and Prevention, Atlanta, Georgia(Mr Yakrus); The California Department of Health Services, Berkeley,California (Dr Winthrop); The Division of Laboratory Medicine, Depart-ment of Pathology and Laboratory Medicine, UCLA School of Medicine,Los Angeles, California (Dr Bruckner); Michigan Cornea Consultants,Southfield, Michigan (Dr Heidemann); The Department of Health andHuman Services, Long Beach, California (Dr Calvet).
Supported in part by Research to Prevent Blindness, Inc., New York,New York (Drs. Mondino and Holland), The Skirball Foundation, LosAngeles, CA (Dr. Holland), and The David May II Endowed Professor-ship (Dr. Holland). Dr. Holland is a recipient of a Research to PreventBlindness-Lew R. Wasserman Merit Award. Drs. Chandra and Torres areDavid May II Fellows in Cornea-External Ocular Disease and RefractiveSurgery.
Reprint requests to Gary N. Holland, MD, Jules Stein Eye Institute,100 Stein Plaza, UCLA, Los Angeles, CA 90095-7003; fax: (310)794-7906; e-mail: [email protected]
2001 BY ELSEVIER SCIENCE INC. ALL RIGHTS RESERVED.0002-9394/01/$20.00 819PII S0002-9394(01)01267-3
-
simultaneous hyperopic LASIK by one surgeon during afour-day period.
To provide the ophthalmic community with additionalinformation about these cases, we present a description oftheir clinical findings, course of disease, and response totreatment (Figures 13), as well as information regardingattempts to identify the source of infection. We alsodescribe the use of topical azithromycin as a possiblyeffective agent for treatment of nontuberculous mycobac-terial keratitis.
SUBJECTS AND METHODS: Disease assessment wasbased on slit-lamp biomicroscopic examination at frequen-cies dictated by best medical judgment. Medical andsurgical treatments, including changes in therapy, werebased on best medical judgment. Indications for surgicalexcision of lamellar keratectomy flaps were nonadherenceof the flap or lack of clinical improvement, as judged by thetreating ophthalmologist.
Initial specimens for culture were obtained by scrapingthe surface of the cornea with a Kimura spatula in areas ofepithelial defects. Subsequent specimens for culture wereobtained by scraping the corneal stroma with a Kimuraspatula after elevation of the lamellar keratectomy flap.Specimens were placed directly on the following culturemedia: blood agar, chocolate agar, thioglycolate broth,Sabouraud agar, and Middlebrook 7H11 agar. Specimenswere also placed on glass slides for microscopic examina-tion using the following stains: Gram, Giemsa, ZeihlNielson, and fluorochrome.
Susceptibility testing was performed in the UCLAClinical Laboratories according to National Committee forClinical Laboratory Standards guidelines.19 Isolates weresusceptible to amikacin (mean inhibitory concentration[MIC]: 8 g/ml) and clarithromycin (MIC: 0.5 g/ml)in vitro. There are no standards for susceptibility testing toazithromycin in vitro. Clarithromycin is used as the classagent for the newer macrolides when performing suscepti-
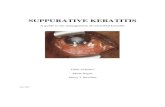
FIGURE 1. (Left) The right eye of case 1, 26 days after LASIK, showing focal and diffuse infiltrates at the interface below thelamellar keratectomy flap. (Right) The same eye, 1 month later. There is complete necrosis and nonadherence of the lamellarkeratectomy flap, which was subsequently excised. A portion of the central white material is precipitated clarithromycin that isadherent to necrotic tissue.
FIGURE 2. (Left) The left eye of case 2, 23 days after LASIK, showing diffuse infiltrates at the interface below the lamellarkeratectomy flap. (Right) The same eye, 2 months later, after resolution of infection. There is a central, nonvascularized scar at thelevel of the interface that also involves the lamellar keratectomy flap. The surrounding cornea is clear.
AMERICAN JOURNAL OF OPHTHALMOLOGY820 DECEMBER 2001
-
bility testing; organisms susceptible to clarithromycin areconsidered to be susceptible to azithromycin.20
All positive culture isolates from patients were sent tothe CDC for molecular analysis. Isolates were comparedusing pulse-field gel electrophoresis.
Topical fortified amikacin (50 mg/ml) was prepared bylocal pharmacies from drug for intravenous injection,according to routine procedures. A commercially availablepreparation was used for topical ciprofloxacin (Ciloxan,Alcon Laboratories, Inc., Fort Worth, TX). Topical clar-ithromycin (10 mg/ml) was prepared as a suspension fromclarithromycin granules for oral suspension (Abbott Lab-oratories, Inc., North Chicago, IL), as described by Fordand associates.21 Topical azithromycin was prepared fromlyophilized drug for intravenous injection (Pfizer Inc., NewYork, NY) according to the following procedures. One vialof drug was reconstituted with 4.8 ml of sterile water perthe manufacturers instructions. The resulting solution wasdiluted further with normal saline to achieve a concentra-tion of 2 mg/ml. This solution was then filtered through a
0.22 m filter into a sterile ophthalmic dropper vial.Patients were instructed to refrigerate the solution betweenapplications. According to the manufacturers packageinsert, azithromycin solution containing 2 mg/ml of drugwill be stable for 7 days when refrigerated.
When initial culture results from the patients suggesteda common source of infection related to surgery, the localhealth department (the Department of Health and HumanServices, Long Beach, CA) was notified. That agency thencontacted the California Department of Health Services inBerkeley, CA and the Epidemic Intelligence Service,Centers for Disease Control and Prevention (CDC) forassistance in epidemiologic studies to identify the source ofinfection.
A case was defined as any patient who developedkeratitis after LASIK by the identified surgeon. Thesurgeon agreed to alert the CDC regarding any new casesof M. chelonae keratitis that were discovered during post-operative care of all surgical patients. To help identifyother possible cases, an e-mail alert was sent to all
FIGURE 3. The right eye (top left) and left eye (top right) of case 4, shown 20 days after bilateral, simultaneous LASIK. The righteye shows focal round corneal opacities at the interface below the lamellar keratectomy flap. The left eye shows a similar focalinfiltrate in front of the inferior pupillary margin, as well as early diffuse cellularity at the interface. The right eye (bottom left) andleft eye (bottom right) of case 4, 1 month after photographs shown in top left and top right. A hypopyon has developed in the righteye, and there is substantial irritation (corneal epitheliopathy, conjunctival redness and chemosis, eyelid swelling and redness)attributed to topical clarithromycin. Increased diffuse opacity at the level of the interface can be seen in the left eye. Precipitatedclarithromycin that is adherent to mucus strands can be seen in both eyes.
CLUSTER OF MYCOBACTERIUM CHELONAE KERATITIS CASESVOL. 132, NO. 6 821
-
members of the American Academy of Ophthalmology,asking for information about any recent cases of nontuber-culous mycobacterial corneal infection throughout thecountry. Similar alerts were posted on the CDC e-maillist-server Epi-X and on a national e-mail list-server forclinical microbiology laboratories, ClinMicroNet.
On May 8, 2001 (24 days after the last procedureassociated with a known M. chelonae infection), physiciansfrom the CDC, as well as from state and local healthagencies, visited the surgical practice in question. Thesurgeon and refractive surgery center staff were interviewedregarding the reported cases and the details of the LASIKprocedures performed. Included were questions about thehandling of surgical instruments during and between sur-gical procedures. Information was requested from thesurgeon about all surgical procedures performed 2 weeksbefore and 2 weeks after the week during which casepatients had undergone LASIK. For each procedure, thefollowing information was obtained: patient demographicdata, type of procedure (hyperopic LASIK, myopicLASIK), date of procedure, postsurgical examination find-ings, and staff present during procedures.
Investigators returned to the refractive surgery center onMay 19, 2001 (the date of the next scheduled hyperopicLASIK) to observe in detail all presurgical, surgical, andpostsurgical practices at the center. As part of this inves-tigation, the sterilizer at the refractive surgery center wasevaluated. Routine procedures employed by the staff inusing the sterilizer were reviewed and compared with themanufacturers instructions. The sterilizer was tested threetimes with Bacillus subtilis spore strips (SGM Biotech,Bozeman, MT) to assess efficacy. The first test involvedone instrument and three spore strips; the second testinvolved a full load of instruments and four spore strips,and the third test included trephines as well as instrumentsand five spore strips. Two spore strips, left unopened andnot placed in the sterilizer, were used as controls. All sporestrips were incubated and cultured according to manufac-turers instructions.
Environmental cultures from potential contaminants inthe surgical center were performed at the time of the initialvisit on May 8, 2001. Because the case patients had beendiagnosed with diffuse lamellar keratitis, the surgeon hadreplaced some materials related to the surgeries, includingdistilled water, dish soap used for cleaning surgical instru-ments before sterilization, and balanced salt solution usedintraoperatively, before resuming LASIK procedures onApril 18, 2001. The stocks of distilled water and dish soapused during the outbreak time-period were still stored atthe surgeons office, however, and samples from thesestocks were obtained for culture. One bottle of balancedsalt solution used during the outbreak time period was alsoavailable and was obtained for culture. Four packages ofgentian violet corneal ink used during the outbreak time-period were also obtained for culture. Because tap water isa common habitat for nontuberculous mycobacteria, tap
water samples from the sink outside the operating roomwere obtained for culture on May 21, 2001. The sink drainwas also swabbed for culture at that time.
The contact lens fragments used as masks in eachhyperopic LASIK case (see description in Results sectionbelow) had been discarded at the end of each procedure,and therefore could not be cultured. A copy of thesurgeons lens ordering and shipment information wasobtained, and the State of California Food and DrugBranch obtained 25 soft contact lenses of the same lotnumber as those used during the outbreak time period fromthe lens manufacturer.
Water and sink drain cultures were performed at theLong Beach (CA) Department of Health and HumanServices Laboratory. All other environmental cultureswere performed at the California Department of HealthSciences Microbial Diseases Laboratory (Berkeley, CA).Tap and distilled water samples were filtered through 45m filters. Filters were placed into Bactec media and onLowensteinJenson slants. Sink drain swabs were inocu-lated directly into the same media. Samples of gentianviolet corneal ink, dish soap, and balanced salt solutionwere inoculated directly into Bactec, LowensteinJensen,and Middlebrook 7H10 media. Lens packaging fluid fromthe 25 contact lens containers and five ground contactlenses were plated onto Middlebrook 7H10 media andinoculated into MGIT broth media. All cultures wereincubated at 35C and held for 6 weeks.
Ground contact lenses and packaging fluid were alsosent to CDC for polymerase chain reaction (PCR) analy-sis, using mycobacteria-specific PCR probes.
We performed a MEDLINE literature search to identifypreviously published cases of infectious keratitis followingrefractive surgery. A separate MEDLINE literature searchrevealed no previous publications describing the use oftopical azithromycin for the treatment of nontuberculousmycobacterial keratitis in any setting.
STATISTICAL ANALYSIS: Relative risk (RR), 95% con-fidence intervals, and P values (Fisher exact test) werecalculated using Epi Info 2000 software version 1.1 (CDC,Atlanta, GA). A per eye analysis was performed becauseone patient had a unilateral infection; such an analysismight allow identification of factors related to infectionbetween first and second procedures on an individualpatient.
REPRESENTATIVE CASE REPORT: A 57-year-oldwoman (case 4) with no history of ocular problemsunderwent bilateral, simultaneous hyperopic LASIK. Shewas in good general health. On the second postoperativeday, diffuse lamellar keratitis was diagnosed in both eyes,and therapy with prednisolone acetate 1% hourly whileawake was initiated. Oral prednisone (60 mg/d) was addedto her treatment regimen on the third postoperative day.On examination 2 weeks after surgery, the diffuse lamellar
AMERICAN JOURNAL OF OPHTHALMOLOGY822 DECEMBER 2001
-
keratitis had resolved in both eyes, and the topical corti-costeroid therapy was tapered but not stopped. Examina-tion during the third postoperative week revealed multiplewhite anterior stromal granular opacities (each less than0.5 mm diameter) in the central cornea at the level of theinterface below the lamellar keratectomy flap in the righteye (Figure 3 [top left]), and a single similar lesion in theleft eye (Figure 3 [top right]). She had no ocular or visualsymptoms. She was referred to the Jules Stein Eye Institutefor evaluation and management. Visual acuity withoutcorrection was 20/20 in both eyes. The lamellar keratec-tomy flap was lifted in the right eye to obtain specimens byscraping for culture and microscopic examination. Acid-fast bacteria were seen on smears, and cultures on Middle-brook 7H11 agar grew M. chelonae 1 week later. Based onthe presence of acid-fast bacteria on smears, corticoste-roid therapy was stopped and topical therapy usingamikacin (50 mg/ml), ciprofloxacin (0.3%), and clar-ithromycin (10 mg/ml) hourly around the clock wasinitiated. She was also given oral doxycycline (100 mgtwice daily). Despite treatment, there was enlargementof the focal infiltrates and increased diffuse infiltrationand haze at the interface in both eyes. There was alsonecrosis and thinning of the inferotemporal portion ofthe flap, although it remained adherent to the underly-ing stroma. After 2 weeks of therapy, there was someevidence of decreased inflammatory signs and the fre-quency of topical medications was reduced to one dropevery 2 hours while awake. There was a subsequentincrease in inflammatory signs in both eyes over thenext week, with development of a hypopyon in the righteye (Figure 3 [bottom left]). At the same time, thepatient began to report intolerance to instillation oftopical clarithromycin in both eyes and developeddiffuse, coarse epitheliopathy; diffuse, increased con-junctival redness and swelling; and eyelid margin red-ness in both eyes. Topical instillation of clarithromycinwas discontinued, with immediate improvement in com-fort, as well as improvement in corneal epithelial,conjunctival, and eyelid margin signs. Topical azithro-mycin (2 mg/ml; hourly while awake), and oral clar-ithromycin (500 mg twice daily) were added to hertreatment regimen. Focal corneal infiltrates resolved inthe right eye over the next week, and diffuse inflamma-tion and haze at the interface decreased in both eyesover the next 4 weeks. There was progressive ingrowthof superficial corneal vessels in both eyes during thisinterval. At 5 weeks after the change in therapy, therewere no signs of active inflammation in either cornea,and all medications were discontinued 1 week later.There was no evidence of recurrent infection in eithereye during 3 weeks of additional observation. There wasstable anterior scarring and superficial vascularization,which was worse in the right eye. Visual acuity withspectacle correction at 19 weeks after LASIK was RE:20/80 and LE: 20/25.
RESULTS
AS OF AUGUST 22, 2001, FOUR INDIVIDUALS MEETING THE
case definition had been identified. All were female, witha mean age of 58 years (range 56 to 64 years). All hadundergone bilateral, simultaneous hyperopic LASIK dur-ing the period April 1114, 2001. Three patients devel-oped bilateral M. chelonae keratitis and one patient (case1) developed unilateral infection, involving the first eyethat underwent LASIK. Two patients had surgery consec-utively on April 11, 2001 (case 1, followed by case 2); onepatient had surgery on April 12, 2001 (case 3); and onepatient had surgery on April 14, 2001 (case 4). Thesurgeon performed LASIK on 54 eyes during this 4-dayperiod; no additional hyperopic LASIK was performedduring this period.
During the period April 428, 2001, the same surgeonperformed LASIK on 231 eyes (120 patients) in the samerefractive surgery center. The majority of patients (113patients, 217 eyes) underwent myopic LASIK. Seven(50%) of 14 eyes undergoing hyperopic LASIK during thisperiod developed M. chelonae keratitis, in contrast to noneof 217 eyes undergoing myopic LASIK (P .001; RR isundefined statistically because no myopic LASIK caseswere associated with infection). All hyperopes underwentbilateral simultaneous LASIK (seven patients), while 104myopes underwent bilateral simultaneous LASIK and ninemyopes underwent unilateral LASIK. A per patient anal-ysis also revealed a significant association between hyper-opic procedures and infection (P .001).
With the exception of one case patient (case 3), whorelocated to Michigan during the first week after surgery,all patients who underwent LASIK during the period April428, 2001 were examined for at least 3 weeks postoper-atively by the surgeon. Because of the infections that hadoccurred in the four case patients, particular attention waspaid to the other three patients who underwent hyperopicLASIK; each was followed for at least 14 weeks with nosigns of infection.
A representative case history is presented above, andspecific details for each case patient are listed in Table 1.Initial clinical characteristics were similar in all four casepatients. By the second postoperative day, each exhibitedcellularity at the interface below the lamellar keratectomyflap, which was diagnosed as probable diffuse lamellarkeratitis. All patients were treated with prednisoloneacetate 1% (hourly while awake). Signs resolved in twopatients (cases 1 and 2), and their topical corticosteroidtreatments were stopped after 1 week. Oral prednisone (60mg daily) was also prescribed for two patients (cases 3 and4). The patient who relocated to Michigan (case 3)stopped oral prednisone after 6 days, but was still usingtopical prednisolone acetate 1% at the time a diagnosis ofpresumed M. chelonae keratitis was made, as describedbelow. One patient (case 4) was still receiving both oralprednisone and topical prednisolone acetate 1% when
CLUSTER OF MYCOBACTERIUM CHELONAE KERATITIS CASESVOL. 132, NO. 6 823
-
TABLE 1. Characteristics of Mycobacterium chelonae Keratitis in Patients Following Bilateral Laser In-situ Keratomileusis
Case*
Age(years)/Gender
Eye(s)Involved
Clniical Features at Diagnosis
Basis ofM. chelonae
Keratitis Diagnosis
Drug Treatment
Excision ofFlap (Interval
AfterDiagnosis)
Visual Acuity
Final CornealStatus
At DiagnosisFinal
Symptoms
Slit LampBiomicroscopic
FindingsDrug
Combination
Interval FromDiagnosis to
Start ofDrugs
Durationof Drugs Response Uncorrected
ThroughPinholes Uncorrected
BestSpectacleCorrected
1 56/F RE Ache, irritation,
burning,
blurring
Multiple linear
opacities at
level of flap
interface
Positive culture
from flap
interface; AFB in
flap biopsy
specimen
Initial:
Ciprofloxacin,
amikacin,
clarithromycin,
oral
doxycycline
Subsequent:
Ciprofloxacin,
amikacin,
azithromycin,
oral
clarithromycin
Immediate
6 weeks
6 weeks
8 weeks
Persistent stromal
infiltration,
hypopyon,
epithelial toxicity
Resolution of
inflammatory
signs after 6
weeks
Yes
(4 weeks)
20/200 20/40 HM 20/100- Diffuse anterior
stromal scars
and superficial
vessels
2 56/F OU OU:
photophobia,
burning,
blurring
Multiple round
opacities at
level of flap
interface
Positive culture
from flap
interface (LE)
Ciprofloxacin,
amikacin,
clarithromycin,
oral doxcycline
Immediate 6 weeks OU: Resolution of
inflammatory
signs after 5
weeks
No RE: 20/70
LE: 20/50
20/20
20/25
20/50
20/50
20/25
20/25
Focal anterior
stromal scars
3 64/F OU Mild irritation Diffuse
keratitis at
level of flap
interface
Clinical
characteristics
Initial OU:
ciprofloxacin,
amikacin,
clarithromycin
Subsequent OU:
ciprofloxacin,
azithromycin,
oral
clarithromycin
Immediate
6 weeks
6 weeks
9 weeks
OU: Persistent
stromal infiltration,
hypopyon,
epithelial toxicity
OU: Resolution of
inflammatory
signs after 6
weeks
RE: Yes
(4 weeks)
LE: Yes
(7 weeks)
RE: NA
LE: NA
NA
NA
NA
NA
20/200
20/80
RE: stromal scars
and superficial
vessels; focal
stromal
thinning
LE: anterior
stromal
scarring and
superficial
vessels; focal
stromal
thinning
AM
ERIC
AN
JOU
RN
AL
OF
OPH
THA
LMO
LOG
Y824
DEC
EMB
ER2001
-
TABLE 1. Continued
Case*
Age(years)/Gender
Eye(s)Involved
Clniical Features at Diagnosis
Basis ofM. chelonae
Keratitis Diagnosis
Drug Treatment
Excision ofFlap (Interval
AfterDiagnosis)
Visual Acuity
Final CornealStatus
At DiagnosisFinal
Symptoms
Slit LampBiomicroscopic
FindingsDrug
Combination
Interval FromDiagnosis to
Start ofDrugs
Durationof Drugs Response Uncorrected
ThroughPinholes Uncorrected
BestSpectacleCorrected
4 57/F OU Asymptomatic Multiple round
opacities at
level of flap
interface
Positive culture
from flap
interace (RE);
AFB on smear
from flap
interface (RE)
Initial OU:
Ciprofloxacin,
amikacin,
clarithromycin,
oral
doxycycline
Subsequent OU:
Ciprofloxacin,
amikacin,
azithromycin,
oral
clarithromycin
Immediate
6 weeks
6 weeks
8 weeks
OU: Persistent
stromal infiltration,
hypopyon,
epithelial toxicity
OU: Resolution of
inflammatory
signs after 5
weeks
No RE: 20/20
LE: 20/20
NA
NA
20/200
20/30
20/80-
20/25-
RE: Diffuse
anterior
stromal scars
and superficial
vessels
LE: Inferior
anterior
stromal scars
and superficial
vessels
AFB acid fast bacteria; F female; HM hand motion; NA not available.
*Cases are presented in the order of surgery: cases 1 and 2 underwent LASIK on April 11, 2001; case 3 underwent surgery on April 12, 2001; case 4 underwent surgery on April 14, 2001.All drugs listed were administered topically unless otherwise specified.Article prepared at 19 weeks after LASIK procedures were performed.Cases 3 and 4 were being treated with topical prednisolone acetate 1% at diagnosis of M. chelonae keratitis; case 4 was being treated with oral prednisone at diagnosis. Corticosteroids had
been prescribed for presumed diffuse lamellar keratitis.Best corrected visual acuity with spectacles at onset of antimycobacterial drug treatment was RE: 20/40; LE: 20/40.
CLU
STERO
FM
YC
OB
AC
TERIU
MC
HELO
NA
EK
ERA
TITISC
ASES
VO
L.132,
NO
.6
825
-
signs of infectious keratitis developed. Signs of infectiouskeratitis (focal corneal stromal opacities at the level of theinterface) were first noted 13 to 21 days after surgery(mean, 17 days) (Figure 3 [top left and top right]). Thethree patients still in California were referred to the JulesStein Eye Institute for additional evaluation and manage-ment when evidence of infectious keratitis developed.
Diagnosis of M. chelonae keratitis for the three patientsin California (cases 1, 2, and 4) was based on cultureresults. Initial cultures of specimens obtained from thecorneal surface in areas of epithelial defects overlyingdeeper infiltrates were negative in all three cases. Addi-tional specimens were then obtained from all three pa-tients by lifting the lamellar keratectomy flap of the worseeye and scraping the interface with a Kimura spatula.Acid-fast bacteria were identified on slides prepared withthe same material in case 4 only. Growth was first detectedon Middlebrook 7H11 agar between 3 and 7 days in allcases. All three M. chelonae isolates were indistinguishableby pulsed-field gel electrophoresis (Figure 4). In one
patient (case 1), biopsy of necrotic flap tissue from thesame eye was performed after the flap was raised initially,but before results of the initial cultures were obtained; thisspecimen also contained acid-fast bacteria, and repeat cultureof the interface taken at the same time grew M. chelonae.
Because of the experience with these three patients, thesurgeon contacted the fourth patient (case 3) in Michigan.She was being followed by a local optometrist, still with adiagnosis of presumed diffuse lamellar keratitis. Her find-ings, as described by the optometrist, were similar to thosein the three patients in California, and a presumptivediagnosis of M. chelonae keratitis was made. The sameantimycobacterial treatment being used for the other threepatients was initiated empirically, and the patient waseventually referred to Michigan Cornea Consultants foradditional evaluation and management.
Initial antibiotic therapy for all four patients consisted oftopical ciprofloxacin 0.3%, fortified amikacin (50 mg/ml),and clarithromycin (10 mg/ml), as well as oral doxycycline(100 mg, twice daily). One patient (case 2) responded wellto this treatment regimen, and no further modifications inmedical therapy were made. The other patients had per-sistence of active infection on this treatment regimen anddeveloped irritation and signs of ocular surface toxicitycaused by topical clarithromycin (corneal epitheliopathy,increased conjunctival redness, chemosis, eyelid marginredness, and pain with instillation) (Figure 3 [bottom leftand bottom right]). Oral clarithromycin was substituted fororal doxycycline, and topical azithromycin (2 mg/ml) wassubstituted for topical clarithromycin after 6 weeks oftreatment for each patient. All three patients tolerated thisrevised treatment regimen well, with eventual resolutionof inflammatory signs over the next 5 to 6 weeks. Allmedications were stopped for three patients (cases 1, 2, and4) and there were no clinical signs of recurrent infectionduring 3 to 6 weeks of additional follow-up. One patient(case 3) had no sign of active disease, but was still beingtreated with topical azithromycin and ciprofloxacin at areduced frequency at the time of this writing.
In one patient (case 1), the lamellar keratectomy flapwas removed from the right cornea at week 4, when itbecame diffusely necrotic and nonadherent (Figure 1[right]). In the other two patients being managed at theJules Stein Eye Institute (cases 2 and 4), all four flapsremained adherent, although there were focal areas ofnecrosis and thinning. The flap was excised from the worse(left) cornea of the patient being managed at MichiganCornea Consultants (case 3), because of dense flap infil-trates, lack of appreciable response to medical therapy, andpublished experience suggesting a therapeutic benefit offlap removal.1 Improvement was noted in the left corneaafter flap removal; therefore, excision of the flap from theright cornea was recommended as well, as inflammatorysigns had become more severe in that eye. On the sameday, topical azithromycin was added to the patients
FIGURE 4. Pulsed-field gel electrophoresis results showingidentical M. chelonae isolates from cases 1, 2, and 4 (lanes 5 to7). Other numbered lanes show results for the followingorganisms or references: 1, M. fortuitum (American TypeCulture Collection [ATCC], Rockville, MD); 2, M. mucogeni-cum (ATCC); 3, M. abscessus (ATCC); 4, M. chelonae(ATCC); 8, 48.5 kb DNA ladder.
AMERICAN JOURNAL OF OPHTHALMOLOGY826 DECEMBER 2001
-
treatment regimen. There was subsequent improvement inthe status of both eyes.
Following resolution of infection, findings were remark-ably similar in all seven involved corneas. All had anteriorstromal scarring and superficial vascularization to varyingdegrees. In addition, there were variable amounts ofnecrosis and tissue loss from the lamellar keratectomy flapin all eyes. It is our clinical impression that among thosepatients whose flaps were not excised, stromal scarring andsuperficial vascularization was most severe in areas wherethe overlying flap was absent because of either necrosis orbiopsy. Areas of remaining flap that had been necrotic, buthealed, were diffusely opaque. Both corneas of one patient(case 3) had focal deep stromal loss, with up to 90%thinning (a 2 4 mm peripheral area in the right eye anda 1 mm diameter central area in the left eye).
Epidemiologic studies identified one surgical factor thatwas related to the cluster of infections, but failed toidentify the source of the infecting organisms. Evaluationof the myopic and hyperopic LASIK procedures revealedonly one difference between procedures; during hyperopicLASIK, the surgeon utilizes soft contact lens fragments tomask a portion of the cornea during laser ablation. Threemasks of various sizes (3.5 mm, 4.5 mm, 5.5 mm) arecreated from a single contact lens, using nondisposabletrephines that have been resterilized before each patientsprocedure. During hyperopic LASIK, the three masks areheld with a pair of sterile jewelers forceps at approximately1 cm above the cornea, for approximately 10 seconds each,in succession from smallest to largest, as the laser is appliedto the cornea. All surgical equipment, with the exceptionof the trephines used to create the masks, is the same forboth myopic and hyperopic LASIK.
The surgeon reported using a new contact lens for eachcase patient, but the same masks were used for both eyes ofeach patient. Masks were placed on a sterile tray betweenprocedures on the first and second eyes. Contact lensesfrom two manufacturers were used during the month ofApril 2001. All eyes undergoing hyperopic LASIK duringthe period April 1114, 2001 were masked with contactlenses from a single manufacturer. The surgeon had re-ceived five contact lenses from that manufacturer at thebeginning of April 2001. The surgeon reported using fourof these five lenses to create masks for the four casepatients. The fifth lens was discarded by the surgeon beforeuse, and was not available for examination. All otherhyperopic LASIK procedures were performed using maskscreated from contact lenses obtained from the othermanufacturer, but none of these cases were performedduring the period April 1114, 2001.
The surgeon routinely wears sterile gloves while per-forming LASIK, but does not change instruments or glovesbetween eyes of the same patient. Surgical staff wasconstant throughout the month of April 2001, with thesame individuals being involved in all surgeries. Theyreported that all surgical instruments, including trephines,
had been sterilized between use on each patient. Otherproducts, including gentian violet corneal ink, sterilegloves, and topical medications, were used in all proce-dures throughout the month. The brands of balanced saltsolution, distilled water, and dish soap were switched onapproximately April 18, 2001.
Tap water from the refractive surgery center sink grewM. gordonae, a common contaminant. All other environ-mental cultures, as well as cultures of ground contact lensesand lens package fluids, were negative. PCR tests of groundcontact lenses and lens package fluid were negative formycobacteria. In all tests, the office sterilizer workedeffectively, as all spore strips that underwent sterilizationfailed to grow B. subtilis during culture, while both controlspore strips did grow B. subtilis during culture.
DISCUSSION
CORNEAL INFECTION IS AN UNCOMMON COMPLICATION OF
LASIK surgery, with reported rates of 1 to 2 cases per 1000eyes.22,23 Isolated case reports have described cornealinfections with a variety of organisms, including Staphylo-coccus aureus, Aspergillus sp., Nocardia sp., and Mycobacteriasp. Nontuberculous mycobacterial keratitis is one of themost common infections to be reported. Among 22 cul-ture-positive cases of post-LASIK infectious keratitis in 18publications since 1995,118 Mycobacterium sp. were iden-tified in six cases (five cases of M. chelonae keratitis1,4,5,9,16and one case of M. fortuitum keratitis5). We were unable toidentify any previous reports describing a cluster of infec-tions from a single refractive surgery center.
There are approximately 50 species within the genusMycobacterium, including M. tuberculosis, M. leprae, andnumerous nontuberculous mycobacterial species. The Ru-nyon classification system categorizes nontuberculous my-cobacteria into four categories, one of which (group IV)contains the rapidly growing mycobacteria (so namedbecause these species usually grow in vitro within sevendays),24 including M. fortuitum, M. chelonae, and M.abscessus. Nontuberculous mycobacteria are ubiquitous insoil, animals, milk, foodstuffs, municipal tap water, andlaboratory water.2528 Runyon group IV organisms multiplyreadily in distilled water, and can remain viable for a year.They are also resistant to chemical disinfectants, such aschlorine.25 Nontuberculous mycobacterial infections arenot transmitted by human-to-human contact.25,29
M. chelonae and M. fortuitum are the most commoncauses of nontuberculous mycobacterial ocular disease.Other species reported to cause keratitis include M.gordonae, M. marinum, M. avium-intracellulare, M. nonchro-mogenicum, and M. asiaticum.21,25,3032
The occurrence of multiple cases of M. chelonae keratitisin a cluster provides an opportunity to understand clinicalfeatures, disease course, and response to therapy. Clinicalfeatures of these four cases were similar. All patients
CLUSTER OF MYCOBACTERIUM CHELONAE KERATITIS CASESVOL. 132, NO. 6 827
-
developed findings suggestive of diffuse lamellar keratitis inthe immediate postoperative period, but findings persisteddespite intense topical, and in some cases oral, corticoste-roid therapy, and patients eventually developed focal,dry-appearing opacities. Clinicians should be alert to thepossibility of nontuberculous mycobacterial keratitis inpatients with persistence of apparent diffuse lamellar ker-atitis, and in those who develop infiltrates at the level ofthe interface.
With regard to diagnostic testing, elevation of thelamellar keratectomy flap appears to be necessary forobtaining culture material. Organisms will grow rapidly onspecific media, such as Middlebrook 7H11 media, butrapidly growing mycobacteria will also grow on blood agar.Acid-fast bacteria may not be seen in smears of materialobtained by scraping of the interface, however.
The course of infection, and late findings were alsosimilar between patients. Late changes in the corneasinclude diffuse and focal anterior scarring, superficial vas-cularization, and variable amounts of tissue loss, especiallyfrom the flap.
Whether the common characteristics in our patients areunique to the specific isolate in this cluster or reflect thenature of nontuberculous mycobacterial keratitis associ-ated with LASIK (because of unique anatomic consider-ations) cannot be determined. The cases reported aresimilar to other previously reported cases of nontubercu-lous mycobacterial keratitis after LASIK, however.1,4,5,9,16In contrast, findings are different than those associatedwith nontuberculous mycobacterial infections after pene-trating injury, radial keratotomy, or penetrating kerato-plasty; such cases are characterized by deep densely opaqueinfiltrates, frequently with severe necrosis and tissueloss.3339 These differences probably reflect the differenttypes of incisions made. Following LASIK, infiltratesdevelop at the level of the interface and inflammatorymaterial spreads along the plane of incision. Ford andassociates21 have speculated that organisms will remainsuperficial unless introduced into deeper layers mechani-cally.
Amikacin has been the traditional drug of choice fortreatment of nontuberculous mycobacterial keratitis, andtopical ciprofloxacin has been shown to be an effectivetreatment in animal studies.4042 A recent clinical reportsuggests that up to 60% of nontuberculous mycobacterialkeratitis cases are nonresponsive to amikacin, and an evenhigher percentage are nonresponsive to ciprofloxacin.21An animal model has also been used to show thatclarithromycin may be effective for treatment of nontuber-culous mycobacterial keratitis.42,43 Based on limited expe-rience, Ford and associates21 suggested that topicalclarithromycin should now be considered the drug ofchoice for nontuberculous mycobacterial keratitis. Topicalclarithromycin has been used to treat several cases of M.chelonae keratitis after LASIK.1,5,9 There is no commer-cially available intravenous formulation of clarithromycin
from which fortified eye drops can be made; and dilution ofa commercially available suspension, marketed for oral use,has been described for use as an eye drop.21 Our patientsfound this topical preparation of clarithromycin to beirritating, which prohibited its extended use. This irrita-tion has also been reported previously.21
Azithromycin was chosen as an alternative macrolide forcontinued treatment of our cases. Although clarithromy-cin appears to be more active in vitro than other macro-lides, susceptibility testing may not reflect its relativeactivity in vivo.20 In contrast, azithromycin is concen-trated in tissues; thus, it has the potential for being moreeffective than clarithromycin in vivo.20 Furthermore, thefact that clarithromycin must be given as a suspension maylimit its efficacy as a topical preparation.
There are no standards for in vitro susceptibility testingwith azithromycin and we found no published reportsdescribing its use topically against M. chelonae keratitis.The concentration of azithromycin was chosen in part forits known stability, and in part on the basis of in vitrosusceptibility testing with clarithromycin, which is be-lieved to reflect susceptibility to azithromycin. It is knownthat dilutions of intravenous azithromycin to 2 mg/ml arestable for 7 days with refrigeration (package insert; PfizerInc., New York, NY); the stability of higher concentrationshas not been shown. Because it is concentrated in tissues,we believed that a solution of 2 mg/ml would achievehigher tissue concentration than the 10 mg/ml suspensionof clarithromycin and would be effective against an organ-ism with an MIC 0.5 g/ml.
Disease was still active when topical azithromycin wasadded to the treatment regimens for three patients, andinfection subsequently resolved in these cases. Azithromy-cin was not used as monotherapy, however, and thus itsefficacy cannot be established conclusively from this series.It was better tolerated than topical clarithromycin.
Corticosteroid use has been implicated as a contributingfactor in the development of nontuberculous mycobacte-rial keratitis in both clinical33 and animal studies.44 Therole of corticosteroids in our cases is uncertain; all patientshad been treated with topical corticosteroids after surgery,and two patients were receiving topical corticosteroids atthe time of diagnosis, including the patient who had areasof 90% stromal thinning in both eyes (case 3). The patientwho developed infection in only 1 eye was treated withtopical corticosteroids for only one week (case 1), althoughinfection was severe in the involved eye. It is interesting tonote that the patient still receiving oral corticosteroids atthe time of diagnosis (case 4) was asymptomatic, while theother three patients were symptomatic.
It has been suggested that removal of the lamellarkeratectomy flap may facilitate resolution of infection byimproving the penetration of topical medications1 and byfacilitating removal of loculated infiltrates at the level ofthe interface.5 Although keratitis improved in case 3 afterflap removal, it cannot be determined whether improve-
AMERICAN JOURNAL OF OPHTHALMOLOGY828 DECEMBER 2001
-
ment was due to flap removal, additional medical therapy,or both. Because the anterior stromal lamellae do not addto the structural integrity of the cornea after separationfrom the posterior stroma by the microkeratome, it isprobably acceptable to remove the flap, if necessary forcontrol of infection. In some cases, the flap becomes totallynecrotic and nonadherent, as occurred in our case 1. In ourpatients with partial loss of flaps because of necrosis, therewas diffuse opacification of necrotic flap tissue that hadremained adherent and healed, while scarring and vascu-larization of the interface bed appeared to be worse whereoverlying flap tissue had been lost.
Surgical extirpation by penetrating keratoplasty of in-fection has been advocated by several authors as treatmentfor nontuberculous mycobacterial keratitis.4,9,16,21,32,33,38,39This procedure may be more applicable for deep cornealinfections. Our series shows that resolution of infection,with good visual outcome in some cases, can result frommedical therapy alone. Although recurrent infection aftermedical therapy has been described in cases of deepinfection,39 we found no reports in the literature ofrecurrent infection in cases of post-LASIK M. chelonaekeratitis that had apparently resolved with medical therapyalone.1,4,5
Isolates were identical on pulsed-field gel electrophoresistesting, indicating a common source. Investigation foundall infections to be associated with LASIK correction ofhyperopia. The contact lens fragments used as masksduring the procedures were implicated as the source ofinfection, although the means by which they were con-taminated, and the route by which organisms were trans-ferred from the lens fragments to the corneas, could not bedetermined. The association of infection with a specificshipment of contact lenses suggested the possibility ofintrinsic contamination of the contact lenses, but myco-bacteria could not be identified from five additional lenseswith the same lot number. Laboratory evaluation of thecontact lens lot was limited by the small sample size tested;average lots contain thousands of lenses, but additionallenses from the same lot were not available for testing atthe time of this writing. It is also possible that the lensfragments were contaminated by the surgeon or surgicalassistant, although observation of the surgeons hyperopicLASIK technique failed to identify a likely mechanism forpreoperative or intraoperative contact lens contamination.Environmental cultures failed to reveal a source of theorganisms, but cultures were not performed until morethan 3 weeks after the case patients had surgery.
This cluster of nontuberculous mycobacterial keratitiscases is not unique. The CDC has received reports of atleast three other recent, independent clusters of nontuber-culous mycobacterial keratitis cases after LASIK; twooccurred in the United States and one occurred in a SouthAmerican country (CDC, unpublished data). Small clus-ters of M. chelonae keratitis have been associated withother ophthalmic procedures. Robin and associates39 de-
scribed two cases following radial keratotomy performed bythe same surgeon in the same outpatient facility. Newmanand associates38 described three cases that occurred after avariety of invasive procedures performed in the same office.The source of infection was not determined for eithercluster.
In summary, nontuberculous mycobacterial keratitis canoccur in an epidemic manner after LASIK through con-tamination of surgical materials. Although the specificsource of infection was not identified in this cluster,nontuberculous mycobacteria are ubiquitous in the envi-ronment, and surgeons must remain meticulous in main-taining sterile techniques during all aspects of LASIK andassociated procedures. In addition, surgeons must be awareof the early signs of infection, which may be mistaken fordiffuse lamellar keratitis. Early diagnosis, with immediateand aggressive antibiotic therapy, can lead to cure ofinfection. Azithromycin is an additional drug that may beuseful for the treatment of nontuberculous mycobacterialkeratitis, and should be investigated further.
ACKNOWLEDGMENTS
The following individuals provided technical assistance inthe epidemiologic investigations described in this article:Bruce K. Fujikawa, DrPH (Department of Health andHuman Services, Long Beach CA), Akiko Kimura, MD(California Department of Health Services, Los AngelesCA), Rachel Ramirez, MS (California Department ofHealth Services, Berkeley CA), S. Benson Werner, MD,M.P.H. (California Department of Health Services, Berke-ley, CA), Andrea Winquist, MD (Centers for DiseaseControl and Prevention, Atlanta, GA), and Duc J. Vugia,MD, MPH (California Department of Health Services,Berkeley, CA).
REFERENCES
1. Chung MS, Goldstein MH, Driebe WJ, Schwartz BH.Mycobacterium chelonae keratitis after laser in situ kerato-mileusis successfully treated with medical therapy and flapremoval. Am J Ophthalmol 2000;129:382384.
2. Chung MS, Goldstein MH, Driebe WJ, Schwartz B. Fungalkeratitis after laser in situ keratomileusis: A case report.Cornea 2000;19:236237.
3. Dada T, Sharma N, Dada VK, Vajpayee RB. Pneumococcalkeratitis after laser in situ keratomileusis. J Cataract RefractSurg 2000;26:460461.
4. Garg P, Bansal AK, Sharma S, Vemuganti GK. Bilateralinfectious keratitis after laser in situ keratomileusis: A casereport and review of the literature. Ophthalmology 2001;108:121125.
5. Gelender H, Carter HL, Bowman B, et al. Mycobacteriumkeratitis after laser in situ keratomileusis. J Refract Surg2000;16:191195.
6. Gupta V, Dada T, Vajpayee RB, et al. Polymicrobial keratitisafter laser in situ keratomileusis. J Refract Surg 2001;17:147148.
7. Hovanesian JA, Faktorovich EG, Hoffbauer JD, et al. Bilat-
CLUSTER OF MYCOBACTERIUM CHELONAE KERATITIS CASESVOL. 132, NO. 6 829
-
eral bacterial keratitis after laser in situ keratomileusis in apatient with human immunodeficiency virus infection. ArchOphthalmol 1999;117:968970.
8. Karp KO, Hersh PS, Epstein RJ. Delayed keratitis after laserin situ keratomileusis. J Cataract Refract Surg 2000;26:925928.
9. Kouyoumdjian GA, Forstot SL, Durairaj VD, Damiano RE.Infectious keratitis after laser refractive surgery. Ophthalmol-ogy 2001;108:12661268.
10. Kuo IC, Margolis TP, Cevallos V, Hwang DG. Aspergillusfumigatus keratitis after laser in situ keratomileusis. Cornea2001;20:342344.
11. Levartovsky S, Rosenwasser G, Goodman D. Bacterial ker-atitis following laser in situ keratomileusis. Ophthalmology2001;108:321325.
12. Mulhern MG, Condon PI, OKeefe M. Endophthalmitis afterastigmatic myopic laser in situ keratomileusis. J CataractRefract Surg 1997;23:948950.
13. Nascimento EG, Carvalho MJ, de Freitas D, Campos M.Nocardial keratitis following myopic keratomileusis. J Re-fract Surg 1995;11:210211.
14. Perez-Santonja JJ, Sakla HF, Abad JL, et al. Nocardialkeratitis after laser in situ keratomileusis. J Refract Surg1997;13:314317.
15. Quiros PA, Chuck RS, Smith RE, et al. Infectious ulcerativekeratitis after laser in situ keratomileusis. Arch Ophthalmol.1999;117:14237.
16. Reviglio V, Rodriguez ML, Picotti GS, et al. Mycobacteriumchelonae keratitis following laser in situ keratomileusis. JRefract Surg 1998;14:3573660.
17. Rudd JC, Moshirfar M. Methicillin-resistant Staphylococcusaureus keratitis after laser in situ keratomileusis. J CataractRefract Surg 2001;27:471473.
18. Watanabe H, Sato S, Maeda N, et al. Bilateral cornealinfection as a complication of laser in situ keratomileusis.Arch Ophthalmol 1997;115:15931594.
19. National Committee for Clinical Laboratory Standards. Sus-ceptibility testing of mycobacteria, Nocardia, and otheraerobic Actinomycetes; tentative standard-second edition.NCCLS document M24-T2 2000;20:159.
20. Inderlied CB, Nash KA. Antimycobacterial agents: In vitrosusceptibility testing, spectra of activity, mechanisms ofaction and resistance, and assays for activity in biologicfluids. In: Lorian V, editor. Antibiotics in laboratory medi-cine, 4th ed. Baltimore: Williams & Wilkins, 1996:127175.
21. Ford JG, Huang AJ, Pflugfelder SC, et al. Nontuberculousmycobacterial keratitis in south Florida. Ophthalmology1998;105:16521658.
22. Stulting RD, Carr JD, Thompson KP, et al. Complications oflaser in situ keratomileusis for the correction of myopia.Ophthalmology 1999;106:1320.
23. Lin RT, Maloney RK. Flap complications associated withlamellar refractive surgery. [Comment In: Am J Ophthalmol2000;130:258259 UI: 20505219 Comment In: Am J Oph-thalmol 1999;127:202204]. Am J Ophthalmol 1999;127:129136.
24. Runyon EH. Anonymous mycobacteria in pulmonary dis-ease. Med Clin North Amer 1959;43:273289.
25. OBrien TP, Matoba AY. Nontuberculous mycobacterial
disease. In: Pepose JS, Holland GN, Wilhelmus KR, editors.Ocular infection & immunity. St. Louis, Missouri: Mosby-Year Book, Inc., 1996:10331041.
26. Dizon D, Mihailescu C, Bae HC. Simple procedure fordetection of Mycobacterium gordonae in water causingfalse-positive acid-fast smears. J Clin Microbiol 1976;3:211.
27. Gangadharam PR, Lockhart JA, Awe RJ, Jenkins DE. My-cobacterial contamination through tap water [letter]. AmRev Respir Dis 1976;113:894.
28. Goslee S, Wolinsky E. Water as a source of potentiallypathogenic mycobacteria. Am Rev Respir Dis 1976;113:287292.
29. Falkinham JO. Epidemiology of infection by nontuberculousmycobacteria. Clin Microbiol Rev 1996;9:177215.
30. Schonherr U, Naumann GO, Lang GK, Bialasiewicz AA.Sclerokeratitis caused by Mycobacterium marinum. Am JOphthalmol 1989;108:607608.
31. Knapp A, Stern GA, Hood CI. Mycobacterium avium-intracellulare corneal ulcer. Cornea 1987;6:175180.
32. Moore MB, Newton C, Kaufman HE. Chronic keratitiscaused by Mycobacterium gordonae. Am J Ophthalmol1986;102:516521.
33. Dugel PU, Holland GN, Brown HH, et al. Mycobacteriumfortuitum keratitis. Am J Ophthalmol 1988;105:661669.
34. Zimmerman LE, Turner L, McTigue JW. Mycobacteriumfortuitum infection of the cornea. A report of to cases. ArchOphthalmol 1969;82:596601.
35. Wunsh SE, Byle GL, Leopold IH, Littman ML. Mycobacte-rium fortuitum infection of corneal graft. Arch Ophthalmol1969;82:602607.
36. Hu FR. Infectious crystalline keratopathy caused by Myco-bacterium fortuitum and Pseudomonas aeruginosa. Am JOphthalmol 1990;109:738739.
37. Lazar M, Nemet P, Bracha R, Campus A. Mycobacteriumfortuitum keratitis. Am J Ophthalmol 1974;78:530532.
38. Newman PE, Goodman RA, Waring GO, et al. A cluster ofcases of Mycobacterium chelonei keratitis associated withoutpatient office procedures. Am J Ophthalmol 1984;97:344348.
39. Robin JB, Beatty RF, Dunn S, et al. Mycobacterium cheloneikeratitis after radial keratotomy. Am J Ophthalmol 1986;102:7279.
40. Stevens RK, Holland GN, Paschal JF, et al. Mycobacteriumfortuitum keratitis. A comparison of topical ciprofloxacinand amikacin in an animal model. Cornea 1992;11:500504.
41. Lin R, Holland GN, Helm CJ, et al. Comparative efficacy oftopical ciprofloxacin for treating Mycobacterium fortuitum andMycobacterium chelonae keratitis in an animal model. Am JOphthalmol 1994;117:657662.
42. Helm CJ, Holland GN, Lin R, et al. Comparison of topicalantibiotics for treating Mycobacterium fortuitum keratitis inan animal model. Am J Ophthalmol 1993;116:700707.
43. Gross RH, Holland GN, Elias SJ, Tuz R. Corneal pharma-cokinetics of topical clarithromycin. Invest Ophthalmol VisSci 1995;36:965968.
44. Paschal JF, Holland GN, Sison RF, et al. Mycobacteriumfortuitum keratitis. Clinicopathologic correlates and cortico-steroid effects in an animal model. Cornea 1992;11:493499.
AMERICAN JOURNAL OF OPHTHALMOLOGY830 DECEMBER 2001