Chromosome Abnormalities in Pediatric Solid Tumors · Genetics/Basic Defects 1. Somatic mutation...
Transcript of Chromosome Abnormalities in Pediatric Solid Tumors · Genetics/Basic Defects 1. Somatic mutation...

Chromosome Abnormalitiesin Pediatric Solid Tumors
Harold Chen
ContentsSynonyms and Related Disorders . . . . . . . . . . . . . . . . . . 1
Genetics/Basic Defects . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1
Clinical Features . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5
Diagnostic Investigations . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7
Genetic Counseling . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 14
References . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 17
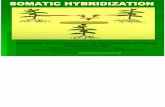
Consistent chromosome abnormalities have beendescribed in many pediatric solid tumors. Thesefindings led to direct molecular investigation anda better understanding of tumor pathogenesis.Clinical correlation often produced useful prog-nostic information (Karnes et al. 1992).
Synonyms and Related Disorders
CNS primary tumor; Ewing sarcoma; Fibrosar-coma; Neuroblastoma; Osteosarcoma; Otherpediatric solid tumors; Rhabdomyosarcoma; Ret-inoblastoma; Sarcomas; Wilms’ tumor
Genetics/Basic Defects
1. Somatic mutation theory of cancer (Mertenset al. 1994):1. Resulting from the accumulation of specific
genetic changes2. Several lines of evidence:
1. Monoclonal origin of most tumors,suggesting that they derive from a singleprogenitor cell
2. Several tumors occurring not only spo-radically but also as familial hereditarytraits
3. Mutagenic nature of most carcinogenicagents, at least in experimental systems
H. Chen (*)Perinatal and Clinical Genetics, Department of Pediatrics,LSU Health Sciences Center, Shreveport, LA, USA
Medical Genetics, Shriners Hospitals for Children,Shreveport, LA, USAe-mail: [email protected]
# Springer Science+Business Media New York 2015H. Chen (ed.), Atlas of Genetic Diagnosis and Counseling,DOI 10.1007/978-1-4614-6430-3_42-2
1

4. Acquired genetic changes in the tumorcells, many of which are detectable at thechromosome level and several of thesemutations have been shown to be tumor-igenic in experimental animals
2. Chromosome abnormalities in neoplastic cells:1. Technical improvement in basic cytoge-
netic techniques:1. Use of colchicine to arrest dividing
cells in metaphase and hypotonic solu-tions to improve spreading of thechromosomes:1. Description of the correct chromo-
some number in humans2. The first specifically neoplasia-
associated chromosome aberration,the Ph1 chromosome in chronic mye-loid leukemia
2. Introduction of chromosome bandingtechniques:1. Possible to identify individual chro-
mosome pairs2. To detect and characterize even subtle
rearrangements2. Clonal chromosome aberrations in
neoplasms:1. Primary aberrations:
1. Nonrandomly associated with partic-ular tumor types.
2. Sometimes observed as the sole kar-yotypic deviation.
3. Thought to constitute early and essen-tial events in carcinogenesis.
4. Increased genomic instability thoughtto be one of the consequences of theacquisition of a primary cancer chro-mosome rearrangement.
5. Many primary aberrations affect cel-lular oncogenes, often fusing themwith other genes to encode hybridproteins or disrupting the normal con-trol sequences of the oncogene, caus-ing its inappropriate expression.
2. Secondary aberrations:1. Occurrence of new abnormalities
facilitated by primary aberrations
2. Nonrandom3. Distribution of the secondary aberra-
tions dependent on both the primaryabnormality and the tumor type inwhich they occur
3. Cytogenetic noise:1. Resulting from acquired instability2. Random changes with little or no
selective value3. Mechanisms by which chromosomal aberra-
tions arise (Albertson et al. 2003):1. Aberrations that lead to aneuploidy:
1. Polyploidy2. Aneuploidy3. Reciprocal translocation4. Nonreciprocal translocation5. Amplification (double minutes)6. Amplification (HSR)7. Amplification (distributed insertions)
2. Aberrations that leave the chromosomeapparently intact:1. Loss of heterozygosity (LOH) (somatic
recombination)2. Loss of heterozygosity (duplication/loss)
4. Identification of specific chromosomerearrangements in neoplasms:1. Leukemia and lymphoma:
1. Crucial for more detailed studies utiliz-ing molecular genetic techniques
2. Possible to compare cytogenetic findingswith morphologic, immunologic, andclinical parameters such as the responseto therapy and survival
3. Diagnostic and prognostic implicationsof karyotyping
2. Solid tumors:1. In general, more complex karyotypes
observed in solid tumors2. Have distinct patterns of primary and
secondary aberrations closely associatedwith histopathologic entities
3. Identification of only a few genes as aconsequence of recurrent structuralrearrangements
4. Fusion of transcription factor gene withother loci, a common feature
2 H. Chen

5. Tumor suppressor genes:1. Important in solid tumors2. Thought to encode inhibitors of unre-
strained growth3. Behave in a recessive manner at the
cellular level (i.e., loss or structuraldisruption of both wild-type allelesis required to unleash a neoplasticphenotype)
5. A new unifying concept called cellular pliancyas a possible explanation for susceptibility tocancer and the developmental origin of pediat-ric solid tumors (Chen et al. 2015):1. Diversity of pediatric solid tumors:
1. Cellular diversity:1. Remarkably diverse in histologic
features2. To define the genetic lesions in differ-
ent pediatric solid tumors, the inter-and intra-tumor heterogeneity, andthe order of events that cause malig-nant transformation during the devel-opment of the retina, bone, neuralcrest, muscle, and other cellularlineages
2. Clinical diversity: can provide importantclues about the developmental origins ofpediatric solid tumors
3. Genetic diversity4. Reprogramming the tumor genome:
needs a detailed understanding of thegenomic landscape of pediatric solidtumors that has emerged with next-generation sequencing over the past5 years
2. Epigenetics: emerged as a major focus areain pediatric solid tumor research because of:1. Striking changes in the epigenetic land-
scape after inactivation of tumor sup-pressor genes such as RB1
2. Identification of recurrent mutations inepigenetic modulators such as BCORand ATRX
3. Cellular pliancy (unify the findings in pedi-atric solid tumor genomic and integratethem with our understanding of
developmental competence and lineagespecification)
4. Clinical genomics: important to incorporatewhole-genome sequencing, whole-exomesequencing, and RNA sequencing in futureclinical genomics efforts to identify poten-tially druggable mutations and to advanceour understanding of the genetic underpin-nings of pediatric solid tumors
6. Retinoblastoma (RB) (Mertens et al. 1994):1. A prototype tumor for understanding basic
concepts in cancer genetics2. Genetics of retinoblastoma:
1. Thought to be a single-gene disordercaused by mutation of the RB1 gene(Carlson and Desnick 1979)
2. Sporadic, nonhereditary form in mostcases:1. Unilateral or unifocal retinoblastoma2. A mutation in the RB1 locus which
occurred later in embryogenesis3. Hereditary form (one third of tumors):
1. Bilateral or multifocal retinoblastoma2. Predisposition inherited as an autoso-
mal dominant trait3. Mutations inherited from a carrier
parent in 25 % of the cases4. A new mutation occurring very early
in embryogenesis in 75 % of cases5. Overall estimates of the penetrance of
the trait: 85–95 %3. Retinoblastoma gene, RB1:
1. The first cancer predisposition gene to becloned
2. Chromosome map: 13q143. More than 100 different mutations
reported to date:1. Missense mutations2. Nonsense mutations3. Splice-site mutations4. Small and large deletions
4. Knudson’s “two-hit hypothesis” of tumori-genesis (Knudson 1971; Horsthemke 1992):1. In the unaffected individual, both RB1
genes are intact and serve as guardians ofthe retina.
Chromosome Abnormalities in Pediatric Solid Tumors 3

2. Retinoblastoma develops as a result oftwo separate mutations.
3. Sporadic tumors: two separate mutationsoccurring somatically in the sameretinal cell.
4. Heritable retinoblastoma: the first muta-tion is germinal and the second somatic.
5. Inherited form of retinoblastoma:1. Critical gene for retinoblastoma located
in band 13q14, suggested by cytogeneticanalyses of tumor cells and lymphocytes
2. Homozygous loss of DNA markers from13q14 in tumor cells from individualswith familial retinoblastoma versus het-erozygous loss of these DNA markers innormal cells, suggested by moleculargenetic investigations
7. Neuroblastoma (NB):1. A malignant tumor derived from undiffer-
entiated neural crest cells that are commit-ted to differentiate into the sympatheticnervous system
2. Inheritance:1. Sporadic in most cases2. A few clustered familial cases reported
indicating an autosomal dominant inher-itance with incomplete penetrance
3. Molecular biology (Lee et al. 2003):1. The amplification (i.e., increased num-
ber of DNA copies) of the oncogeneMYCN (N-myc), located on chromo-some 2p24, and changes in the normaldiploid chromosomal content:1. Both are correlated with disease prog-
nosis and disease recurrence.2. The amplification can be in the form
of the double-minute chromosomes,which are extragenomic segments ofDNA, or in homogeneously stainingchromosomal regions.
2. Variable DNA content ofneuroblastoma:1. Near-triploid DNA index regardless
of any clinical or biologic featurespredicts a smaller risk of progressionto higher-stage diseases.
2. Diploid/tetraploid index tends to pre-dict higher risk of progression or mul-tiple relapses.
3. Other molecular markers (receptors fornerve growth factors) associated withneuroblastoma:1. Trk A: associated with favorable
neuroblastomas2. Trk B: expressed in unfavorable
neuroblastomas8. Wilms’ tumor (WT):
1. Biological pathways leading to the devel-opment of Wilms’ tumor:1. Complex2. Involvement of several genetic loci:
1. Two genes on chromosome 11p: oneon chromosome 11p13 (the Wilms’tumor suppressor gene, WT1) andthe other on chromosome 11p15 (theputative Wilms’ tumor suppressorgene, WT2)
2. Loci at 1p, 7p, 16q, 17p (the p53tumor suppressor gene), and 19q(the putative familial Wilms’ tumorgene, FWT2)
2. Inheritance:1. Sporadic in majority of cases
(>95 %).2. Familial predisposition to Wilms’ tumor
is rare, affecting only1.5 % of patientswith Wilms’ tumor.
3. Association with specific genetic disordersor recognizable syndromes:1. WAGR syndrome:
1. Large constitutional deletions ofchromosome 11p13
2. Tumor suppressor gene: WT13. Mechanism of gene inactivation:
hemizygous deletion4. Wilms’ tumor incidence: >30 %5. Associated features: aniridia and gen-
itourinary abnormalities6. Mental retardation7. Associated aniridia: caused by dele-
tion of the PAX6 gene in the 11p13region in close proximity toWT1 gene
4 H. Chen

2. Denys-Drash syndrome:1. Chromosomal loss: 11p132. Tumor suppressor gene: WT13. Mechanism of gene inactivation:
mutation (DNA-binding domain)4. Wilms’ tumor incidence: >90 %5. Associated features: pseudohermaph-
roditism, mesangial sclerosis, andrenal failure
3. Beckwith-Wiedemann syndrome:1. Chromosomal loss: 11p152. Tumor suppressor gene: (WT2/BWS)3. Mechanism of gene inactivation:
unknown4. Wilms’ tumor incidence: 5 %5. Associated features: organomegaly,
hemihypertrophy, umbilical hernia,neonatal hypoglycemia, and othertumors such as hepatoblastoma
4. Perlman syndrome:1. Renal dysplasia2. Multiple congenital anomalies3. Gigantism4. Wilms’ tumor
5. X-linked Simpson-Golabi-Behmelsyndrome:1. Overgrowth disorder2. Caused by mutations in the GPC3
gene located on Xq263. Overlapping physical features with
Beckwith-Wiedemann syndrome4. Wilms’ tumor and other embryonal
tumors9. Primary tumors of the central nervous system
(Mertens 1994):1. Primitive neuroectodermal tumors
(PNETs):1. Homozygous inactivation of the TP53
gene, a tumor suppressor gene locatedin 17p, secondary to i(17p): implicatedin the development of several tumortypes
2. Molecular analyses indicating the exis-tence of a second tumor suppressor gene,distinct from and distal to the TP53locus, which might be pathogenetically
involved in a subset of primitiveneuroectodermal tumors
2. Gliomas:1. A tumor suppressor gene in 22q impli-
cated as an essential event in the gene-sis of a number of neurogenicneoplasms.
2. A candidate for such a role is NF2,thought to be mutated in neurofibroma-tosis type 2, a dominantly inherited dis-order predisposing for gliomas,neurinomas, and meningiomas.
Clinical Features
1. Only retinoblastoma, neuroblastoma, andWilms’ tumor will be discussed here:
2. Retinoblastoma (Mertens 1994; Aertset al. 2006):1. The most common malignant ocular tumor
in childhood that affects approximately 1 in18,000 children under 5 years of age in theUSA (Devesa 1975)
2. A rare malignant tumor arising from cells ofthe embryonal neural retina
3. Develops only in infants and youngchildren
4. Unifocal retinoblastoma: presence of a sin-gle retinoblastoma
5. Multifocal retinoblastoma: presence ofmore than one tumor (Lohmann and Gallie2013):1. Unilateral: occurrence of multiple RB
tumors in one eye2. Bilateral: occurrence of RB tumors in
both eyes3. “Trilateral” retinoblastoma: occurrence
of bilateral retinoblastoma plus apinealoma
6. Presenting signs:1. White papillary reflex (leukocoria): the
most common presenting sign2. Strabismus: the second most common
presenting sign
Chromosome Abnormalities in Pediatric Solid Tumors 5

3. Less common signs:1. Poor vision2. Orbital swelling3. Unilateral mydriasis4. Heterochromia iridis5. Glaucoma6. Orbital cellulitis7. Uveitis8. Hyphema or vitreous hemorrhage9. Nystagmus
7. Retinoma-associated eye lesions rangingfrom retinal scars to calcified phthisicaleyes resulting from spontaneous regres-sion of retinoblastoma (include benignretinal tumors called retinocytoma orretinoma)
8. Patients with germline RB1 mutations: at anincreased risk of developing tumors outsidethe eye:1. Pinealomas2. Osteosarcomas3. Soft tissue sarcomas4. Melanomas
3. Neuroblastoma (Davidoff and Hill 2001; Leeet al. 2003):1. The most frequently occurring solid tumor
in children2. Responsible for 8–10 % of all cancers in
children and approximately 15 % of allpediatric cancer deaths
3. 40 % of cases diagnosed in children under1 year of age who have a very goodprognosis
4. 60 % in older children and young adult whohave a poor prognosis despite advancedmedical and surgical management
5. Amplification of MYCN gene found inneuroblastomas:1. A powerful prognostic indicator2. Associated with:
1. Advanced stages of disease2. Rapid tumor progression3. Poor outcome
6. Clinical presentation:1. Variable presentation (Brodeur
et al. 1997):
1. Localized disease (one third to onefourth of cases)
2. Metastatic disease (two thirds to threefourths of cases)
3. Asymptomatic in a small number ofpatients
2. Retroperitoneal and abdominal tumors(62–65 %):1. A palpable mass2. Abdominal pain (34 %)3. Weight loss (21 %)4. Anorexia5. Vomiting6. Symptoms related to mass effect
3. Thoracic tumors (14 %):1. Dysphagia2. Cough3. Respiratory distress
4. Pelvis (5 %) and paraspinal tumors thatcompress the spinal cord:1. Urinary dysfunction2. Constipation3. Fetal incontinence4. Lower extremity weakness
5. Neck tumors:1. Horner syndrome: present in patients
with lesions in the cervical orupper thoracic sympathetic ganglia(1.7 %)
2. Airway distress6. Liver metastasis:
1. Hepatomegaly2. Jaundice3. Abnormal liver function tests4. Abdominal pain
7. Bone metastases and bone marrowinvolvement:1. Bone pain2. Palpable bony nodules3. Anemia4. Purpura
8. Fever (28 %)9. Lymph node metastases: palpable
lymphadenopathy10. Retrobulbar and orbital metastases:
periorbital ecchymoses
6 H. Chen

11. Severe diarrhea refractory to standardtreatment due to production of vasoac-tive intestinal peptide by tumor cells(4 %)
12. Acute cerebellar encephalopathy (2 %):1. Cerebellar ataxia2. “Dancing eyes and dancing feet syn-
drome” (involuntary eye flutteringand muscle jerking)
3. Myoclonic jerks13. Symptoms related to high catechol-
amine levels (0.2 %):1. Hypertension2. Palpitations3. Flushing4. Sweating5. Malaise6. Headache
4. Wilms’ tumor (Mertens 1994):1. The most common kidney cancer in
childhood2. Represents about 6 % of all childhood can-
cers in the USA3. Clinical presentation (Paulino 2014):
1. Presence of an asymptomatic abdominalmass – the most common presentation:1. Usually affects one kidney with mul-
tiple tumor foci in 8 % of cases2. Bilateral in 6 % of cases
2. Hypertension, gross hematuria, andfever observed in 5–30 % of patients
3. Hypotension, anemia, and fever in asmall number of patients who havehemorrhaged into their tumor
4. Rare respiratory symptoms related to thepresence of lung metastases in patientswith advanced-stage disease
4. Association with congenital malformations:1. Found in 60 % of the bilateral cases and
4 % of the unilateral cases2. WAGR3. Denys-Drash syndrome4. Beckwith-Wiedemann syndrome5. Perlman syndrome6. X-linked Simpson-Golabi-Behmel
syndrome
5. Likelihood of developing Wilms’ tumor inaniridia patients:1. Aniridia patients without other anoma-
lies: 1–2 %2. Aniridia patients withWAGR syndrome:
25–40 %
Diagnostic Investigations
1. Cytogenetic and molecular genetic tech-niques used in analyzing tumor materialsfrom patients (Cooley et al. 2009):1. Conventional and molecular cytogenetic
techniques most commonly used(Varella-Garcia 2003):1. Metaphase cytogenetics or karyotyping
(G-, Q-, and R-bandings):1. Protein digestion and/or special dye
generating banding pattern specificfor each chromosome
2. Identification of numerical andstructural chromosomal anomalies
2. Fluorescence in situ hybridization(FISH):1. A small, labeled DNA fragment
used as a probe to search for homol-ogous target sequences in chromo-some or chromatin DNA
2. Identification of the presence, num-ber of copies per cell, and localiza-tion of probe DNA
3. Applicable to interphase cells3. Comparative genomic hybridization
(CGH):1. Comparative hybridization of differ-
entially labeled total genomic tumorDNA and normal reference DNA tonormal human metaphases used astemplates
2. Detection of variant DNAcopy numbers at the chromosomelevel
3. Applicable to fresh or preservedspecimens
Chromosome Abnormalities in Pediatric Solid Tumors 7

4. Multicolor karyotyping (M-FISH,SKY):1. Hybridization with 24 differentially
labeled, chromosome-specificprobes allowing the painting ofevery human chromosome in a dis-tinct color
2. Detection of rearrangements involv-ing one or more chromosomeswithin individual metaphase spreads
3. Accurate origin identification of allsegments in complex rearrangements
4. Clarification ofmarker chromosomes2. Other techniques:
1. Flow cytometry2. Reverse transcriptase-polymerase
chain reaction (RT-PCR)3. Quantitative PCR4. Southern blot analysis of gene
rearrangements5. Loss of heterozygosity (LOH) analysis6. Clinical utilization of high-resolution
single-nucleotide polymorphism(SNP)-based oligonucleotide arrays indiagnostic studies of pediatric patientswith solid tumors (Doughertyet al. 2012)
7. Restriction landmark genome scanning8. Representational difference analysis9. cDNA gene expression microarrays10. Proteomic methods:
1. Matrix-assisted laser desorption/ionization-time of flight (MALDI-TOF)
2. Surface-enhanced laser desorption/ionization-time of flight (SELDI-TOF)
2. Cytogenetic studies in retinoblastoma:1. Cytogenetically visible changes of 13q14:
infrequent in retinoblastoma2. Deletions or unbalanced translocations
leading to loss of 13q14 band (10 %)3. Monosomy 13 (10 %)4. i(6p), mostly detected as a supernumerary
isochromosome (one third of cases)5. Gain of 1q material (one third of cases)
6. Bone marrow cytogenetic (Barroset al. 2012):1. Del(13q), i(6p), +1, monosomy 16, dup
(5q), dic(15;22), and add(14q).2. These complex chromosome abnor-
malities may be related to the aggres-siveness of the disease.
7. Cytogenetic aberrations in retinoblastoma:1. Secondary to RB1 mutations2. More related to tumor progression than
to tumor establishment3. Other studies for retinoblastoma:
1. Indirect ophthalmoscopy to examine thefundus of the eye to detect retinomas, pref-erably by a retinal specialist
2. Imaging studies (CT, MRI, ultrasonogra-phy) to support the diagnosis and stage thetumor
3. Histopathological examination to confirmthe diagnosis
4. Direct DNA testing of the RB1 gene inWBC DNA:1. Identify a germline mutation in about
80 % of individuals with a hereditarypredisposition to retinoblastoma
2. Probability of detection of the RB1gene mutation in an index case depen-dent on the following:1. Whether the tumor is unifocal or
multifocal2. Whether the family history is posi-
tive or negative3. The sensitivity of the testing
methodology4. Cytogenetic studies in neuroblastoma (Maris
and Matthay 1999; Davidoff and Hill 2001;Lee et al. 2003; Schwab et al. 2003):1. Identification of multiple cytogenetic
abnormalities in neuroblastoma:1. Allelic losses on chromosomes 1p (par-
ticularly 1p36), 11q, 14q, 7q, 2q, 3p,and 19q.
2. Allelic gains on chromosomes 17q,18q, 1q, 7q, and 5q.
3. Aberrations involving chromosomesX,3, 19, and del(1p) could be consid-ered early events, whereas those
8 H. Chen

involving chromosomes 9, 13, 15, 18,20, and 21 were often late events (Bettset al. 2005).
2. Hyodiploid, triploid, or “near-triploid”, or“near-tetraploid” in modal chromosomenumber:1. Majority (55 %) with triploid or “near-
triploid” (a chromosome numberbetween 58 and 80)
2. Remainder with “near-diploid” (35–57chromosomes) or “near-tetraploid”(81–103 chromosomes)
3. Frequent partial 1p monosomy (70–80 %of cases) with most commonly deletedregion being between 1p32 and 1p36
4. Gain on the long arm of chromosome17 (17q):1. Probably the most common genetic
abnormality in neuroblastomas2. Occurring in approximately 75 % of
primary tumors3. Most often resulting from an unbal-
anced translocation of this region toother chromosomal sites, most fre-quently 1p or 11q
4. A powerful independent finding ofadverse outcome
5. Deletions of the long arms of chromo-somes 11 (11q) and 14 (14q):1. Appears to be common in
neuroblastomas2. Both inversely related to MYCN
amplification6. Frequent presence of extrachromosomal
double-minute chromatin bodies (DMs)or homogeneously staining regions(HSRs):1. Cytogenetic evidence of gene
amplification2. Amplified region derived from the distal
short arm of chromosome 2 (2p24) thatcontains the MYCN proto-oncogene
7. Chromosome imbalances and alterationsof AURKA and MYCN genes in childrenwith neuroblastoma (İnandıklıoğluet al. 2012):
1. Some 72 % of the cells had structuralaberrations and only 28 % had numer-ical changes in patients.
2. Structural aberrations consisted of dele-tions, translocations, breaks, and fragil-ity in various chromosomes, 84 % and52 % of the patients having deletionsand translocations, respectively.
3. Among these expressed chromosomeabnormalities, there was a higher fre-quency at 1q21, 1q32, 2q21, 2q31,2p24, 4q31, 9q11, 9q22, 13q14,14q11.2, 14q24, and 15q22 in patients.
4. Thirty two percent of the patients hadchromosome breaks, most frequently inchromosomes 1, 2, 3, 4, 5, 8, 9, 11,12, 19, and X.
5. Aneuploidies in chromosomes X,22, 3, 17, and 18 were most frequentlyobserved.
6. Numerical chromosome abnormalitieswere distinctive in 10.7 % of sexchromosomes.
7. Fragile sites were observed in 16 % ofpatients.
5. Other studies for neuroblastoma:1. Imaging studies:
1. Chest radiography2. Ultrasound3. CT4. MRI5. Radionucleotide bone scan
2. Blood tests:1. Elevated urinary and serum catechol-
amine metabolites:1. Homovanillic acid (HVA)2. Vanillylmandelic acid (VMA)
2. Abnormal liver function tests3. Molecular genetic testing (Castel
et al. 2007):1. Array CGH analysis: a pangenomic
technique allowing insights into gainsand losses with high resolution
2. Multiplex ligation-dependent probeamplification (MILPA)
6. Cytogenetic studies in Wilms’ tumor:1. A near-diploid chromosome count.
Chromosome Abnormalities in Pediatric Solid Tumors 9

2. Triploid-tetraploid karyotypes in a fewcases with tendency to have an anaplasticmorphology.
3. Numerical aberrations:1. Trisomy 12: particularly frequent2. Followed by trisomies 8, 6, 7, 13,
20, and 174. Structural rearrangements:
1. Involve all chromosomes except the Ychromosome
2. Recombinations of 11p (>20 %):1. Vast majority of the breakpoints
assigned to 11p13 and 11p15, indi-cating these loci are important insporadic Wilms’ tumor
2. Loss of heterozygosity studies indi-cating that alleles from 11p13 and11p15 are often lost inWilms’ tumor
3. Loss of the long arm of chromosome16 occurring in about 20 % of Wilms’tumors: associated with poor prognosisindependent of stage or tumor histology
5. SNP-based arrays complement classiccytogenetics in the detection of chromo-somal aberrations in Wilms’ tumor(Zin et al. 2012).
7. Other studies in Wilms’ tumor:1. Renal ultrasound to monitor Wilms’ tumor2. Abdominal CT scanning to determine the
tumor’s origin, lymph node involvement,bilateral kidney involvement, and invasioninto major vessels (e.g., inferior vena cavaor liver metastases)
3. Chest radiography to detect lungmetastases
4. Histopathological examination to confirmthe diagnosis
5. Further studies of certain patients witheither Wilms’ tumor or associated anoma-lies (Coppes and Egeler 1999):1. Hemihypertrophy/Beckwith-
Wiedemann syndrome: uniparentaldisomy studies to evaluate constitu-tional or somatic alterations of 11p15.
2. WAGR syndrome: molecular evalua-tion of the 11p13 region if chromo-somal studies do not reveal a deletion:
1. Fluorescence in situ hybridization(FISH)
2. Pulsed-field electrophoresis3. Denys-Drash syndrome: molecular
evaluation of WT1 to determinewhether the patient indeed carries aconstitutional mutation. If the mutationis present, family members need to bescreened.
4. Aniridia:1. Cytogenetic analysis and molecular
evaluation of the WAGR region byFISH or pulsed field to rule out con-tiguous deletion of Pax6 and WT1
2. No further screening for Wilms’tumor if Pax6 mutation is identifiedin isolated cases of aniridia
8. Cytogenetic studies of primary tumors of thecentral nervous system (Mertens 1994):1. Primitive neuroectodermal tumors:
1. Near-diploid in most tumors2. I(17q): the most consistent
rearrangement2. Gliomas:
1. Mostly astrocytomas and ependymomas2. No specific structural rearrangement
found3. Loss of 1p and gain of 1q found in a
subset of tumors4. Loss of chromosome 22 common in
childhood gliomas5. Loss of material from chromosome
22, either numeric or structural aberra-tions, found recurrently in rhabdoidtumors, meningiomas, and neurinomas
6. Single-nucleotide polymorphism(SNP) arrays (Paxton et al. 2015):1. Allow for a whole-genome view of
complex copy number changes andloss of heterozygosity
2. Enable observations of the genomiclandscape beyond 1p19q deletionsand EGFR amplification
9. Cytogenetic studies in hepatoblastoma(Mertens et al. 1994):1. Trisomy 2 or duplications of part of 2q:
detected in half of the cases
10 H. Chen

2. Trisomy 203. Duplication of 8q through either i
(8q) formation or trisomy 810. Cytogenetic studies in sarcomas (Bennicelli
and Barr 1999; Esparza 2012):1. Ewing sarcoma/primitive neuroectodermal
tumor (Davidoff and Hill 2001):1. Reciprocal translocation t(11;22)(q24;
q12):1. Characteristic primary rearrangement.2. Found in nearly 90 % of the
tumors.3. Causing a fusion of the transcription
factor gene FLI1 on chromosome11 with EWS on chromosome22 (FLI1-EWS, a fusion transcript).Only the chimeric gene expresses onthe derivative chromosome 22 whichcontains a sequence encoding aDNA-binding domain from FLI1.
2. t(21;22)(q22;q12) and ERG-EWS3. t(7;22)(p22;q12), ETV1-EWS4. t(17;22)(q12;q12), E1AF-EWS5. t(2;22)(q33;q12), FEV-EWS
2. Additional chromosome changes:1. Trisomy 82. Der(16)t(1;16)(a10-q21;q10-13), lead-
ing to gain of 1q and loss of 16q3. Congenital or infantile fibrosarcoma
(Mertens et al. 1994):1. t(12;15)(p13;q25), ETV6-NTRK32. Hyperdiploid with few or no structural
rearrangements3. Nonrandom numerical changes:
1. Trisomies 11 and 20, the most fre-quent changes
2. Trisomies 17 and 84. Osteosarcoma (Mertens et al. 1994):
1. Highly complex karyotypes in themajority of cases
2. Chromosome number in the triploid-tetraploid range
3. Most common numeric aberrationsinvolving �3, �10, �13, and �15
4. Structural rearrangements involvingchromosome arms 1p, 1q, 3p, 3q, 7q,11p, 17p, and 22q
5. Presence of many undefined chromo-some markers
5. Rhabdomyosarcoma (Mertens et al. 1994):1. The most common soft tissue sarcoma
in childhood2. Alveolar subtype:
1. Most contain one or two recurringtranslocations, namely, t(2;13)(q35-37;q14) or the rare t(1;13)(p36;q14), shown to juxtapose thePAX3 gene on chromosome 2 withthe FKHR gene on chromosome13, leading to the formation of ahybrid transcription factor (PAX3-FKHR).
2. Found in about 70 % of the alveolartumors.
3. Only occasionally described in othersubtypes.
3. Embryonal subtype: numerical changeswith +2, +8, +11, and +20, found in35–50 % of cases
11. Other common, recurrent translocation/chro-mosome abnormalities in solid and softtissue tumors of childhood (Davidoff andHill 2001; Tien et al. 2014):1. Alveolar soft part sarcoma: t(X;17)(p11;
q25), ASPL-TFE32. Inflammatory myofibroblastic tumor:
2p23 translocations, ALK-TPM33. Desmoplastic small round cell tumor:
1. t(11;22)(p13;q12), WT1-EWS2. t(11;22)(q24;q12), FLI1-EWS, ERG-
EWS4. Synovial sarcoma:
1. t(X;18)(p11.23;q11.2), SSX1-SSXT2. t(X;18)(p11.21;q11), SSX2-SSXT
5. Malignant melanoma of soft part (clearcell sarcoma): t(12;22)(q13;q12), ATF1-EWS
6. Myxoid liposarcoma:1. t(12;16)(q13;p11), CHOP-TLS(FUS)2. t(12;22)(q13;q12), CHOP-EWS
7. Ewing sarcoma:1. t(11;22)(q24;q12)2. t(2;11;22)(q35;q24;q12), add(17)(p11.2)3. +12
Chromosome Abnormalities in Pediatric Solid Tumors 11

8. Extraskeletal myxoid chondrosarcoma:t(9;22)(q22;q12), CSMF-EWS
9. Dermatofibrosarcoma protuberans andgiant cell fibroblastoma: t(17;22)(q22;q13), COLIAI-PDGFB
10. Lipomas: t(2;12)(q23;q15)11. Leiomyomas: t(12;14)(q13;15),HMGI-C
(Cooper 1996)12. Other primary chromosome changes in solid
tumors (Sandberg and Turc-Carel 1987;Sandberg 1988):1. Benign tumors:
1. Meningioma and acoustic neuroma:1. �222. 22q�
2. Mixed tumors of salivary glands:1. t(3;8)(p21;q12)2. t(9;12)(p13-22;q13-15)
3. Colonic adenomas:1. 12q� and/or +72. 12q� and/or +8
4. Cortical adenoma of the kidney:1. +72. +173. �Y
2. Adenocarcinomas:1. Bladder:
1. i(5p)2. +73. �9/9q�4. 11p�
2. Prostate: del(10)(q24)3. Lungs (small cell carcinoma): del(3)
(p14p23)4. Colon:
1. 12q�2. +73. +84. +125. 17(q11)6. 17p-
5. Kidney: del(3)(p11p21)6. Uterus: 1q�7. Ovary:
1. 6q�2. t(6;14)(q21;q24)
8. Endometrium:1. Trisomy 1q2. +10
3. Embryonal and other tumors:1. Testicular (germ cell tumors): i(12p)2. Malignant melanoma:
1. Del(6)(q11q27)2. i(6p)3. Del(1)(p11p22)4. t(1;19)(q12;q13)
3. Mesothelioma: del(3)(p13p23)4. Glioma: �22
13. Potential prognostic markers of neoplasticdisease (Barcus et al. 2000):1. Breast cancer: allelic loss at 1p22-p31
(lymph node metastasis and tumor size>2 cm)
2. Bladder cancer:1. LOH RB (high grade/muscle invasion)2. Genomic alterations (2q�, 5p+, 5q�,
6q�, 8p�, 10q�, 18q�, 20q+) (highergrade)
3. Cervical carcinoma: LOH on chromosome(advanced stage)
4. Colorectal cancer:1. LOH at 18q21 or p53 expression
(recurrence/poor survival)2. MSI (microsatellite instability) and
K-ras mutations in normal-appearingcolonic mucosa (predictive of colorec-tal cancer)
3. P16 hypermethylation (shorter survivalin Stage T3N0M0 tumors)
5. Gastric cancer:1. LOH p53 (invasive disease)2. LOH of 7q (D7S95) (poor prognosis
(in Stage III/IV))6. Glioma: chromosome 22q loss (astrocy-
toma progression)7. Head and neck squamous cell carcinoma:
1. LOH of 14q (poor outcome)2. LOH on 2q (poor prognosis)3. LOH on 17p (chemoresistance)
8. Melanoma: LOH in plasma (advancedstage/tumor progression)
9. Neuroblastoma:
12 H. Chen

1. N-myc amplification (poor prognosis)2. TrkA expression (good prognosis)3. High telomerase expression (aggres-
sive behavior)10. Neuroblastomas, 4s: N-myc amplifica-
tion, 1p deletion, 17q gains, and elevatedtelomerase activity (poor prognosis)
11. Non-small cell lung cancer:1. Allelic imbalances on 9p (poor
prognosis)2. LOH of 11p (poor prognosis)
12. Primitive neuroectodermal tumor:1. LOH of 17p (metastatic disease)2. C-myc amplification (poor
prognosis)13. Prostate cancer: LOH on 13q (advanced
stage)14. Retinoblastoma: LOH at RB1 locus
(tumoral differentiation, absence of cho-roidal invasion)
14. Chromosome abnormalities observed insome solid tumors (Cooley et al. 2009):1. Genitourinary:
1. Renal:1. Renal cell carcinoma (RCC): �3 or
del(3p), del(3p) with gain 5q, del(3p) with loss 5q, and �14/del(14q)
2. Papillary RCC: +7, +17, �Y, and9p�
3. t(Xp11.2) RCC: (X;17)(p11.2;q25),t(X;17) (p11.2;q23), and t(X;1)(p11.2;p34)
4. t(6;11) RCC: t(6;11)(p21;q12)5. Chromophobe RCC: losses 1, 2,
6, 10, 13, 17, and 216. Oncocytoma: 1p� and t(11q13)7. Rhabdoid: �22/22q�8. Congenital mesoblastic nephroma:
t(12;15)(p12;q25), +11, +17, and+20
2. Bladder, papillary: del(9)(p21), 8p�,+7, and +17
3. Wilms’ tumor: 16q�, +1q, 1p�, �22,and 17p�
4. Prostate: +17q31, 8p22�, +8q24,10q�, and 17p13�
2. Gastrointestinal:1. Liver:
1. Hepatoblastoma: +20, +2, +8, andt(1q12q21)
2. Hepatic mesenchymal hamartoma:t(11;19)(q13;q13.4) and t(19q13.4)
2. Salivary gland:1. Pleomorphic adenoma: t(3;8)(p21;
q12)2. Mucoepidermoid cancer: t(11;19)
(q21;p13)3. Warthin tumor: t(11;19)(q21;p13)
3. Breast:1. Invasive intraductal: dmin (double
minute) and HSR (homogeneouslystaining region)
2. Secretory breast: t(12;15)(p13;q25)4. CNS:
1. Astrocytic tumors: +7, �10/10q�,9p21�, and 19q�
2. Glioblastoma: +7, 10q�, and 9p�3. Anaplastic: 1p�, 19q�, and der(1;19)
(q10;p10)4. Mixed oligoastrocytoma: +7, �10/
10q�, and 15q�5. Oligoastrocytoma: 19q� and 1p�
5. Ependymoma:1. Spinal: +7, �22q, and 14q�2. Intracranial: +1q, 6q�, +7, and 9p�
6. Mudulloblastoma: i(17q), 17p�, �10/10q�, and +7
7. Supratentorial primitive neuroectodermaltumor: +1q, 16q�, and 19p�
8. Atypical teratoid/rhabdoid tumor: �22 ordel(22q11.23)
9. Meningioma: �22 or del(22q11.2), 1p�,and �14/14q�
10. Choroid plexus tumors:1. Carcinoma: losses 2, 3, 4, 5, 6, 8, 10,
11, 13, 14, 15, 16, 17, 18, 19, and 222. Papilloma: gains 7, 8, 9, 12, 14, 15,
17, 18, 19, and 2011. Small round cell tumors:
1. Alveolar RMS: t(2;13)(q37;q14), t(1;13)(p36;q14), t(X;2)(q13lq35),and t(2;2)(q35;p23)
Chromosome Abnormalities in Pediatric Solid Tumors 13

2. Embryomal rhabdomyosarcoma:gains 2, 7, 8, 11, 12, 13, and 20; losses1p, 3p, 9q, 10q, 16q, 17p, and 22
3. Neuroblastoma: del(1p), del(11q)without MYCN amp, del(1p), +17q,MYCN amp, and triploidy withoutabove abnormalities
4. Ewing sarcoma/peripheralneuroectodermal tumor: t(11;22)(q24;q12) and variants, t(21;22)(q22;q12), del(9p), 17p�, and der(1;16)(q10;p10)
5. Desmoplastic small round cell tumor:t(11;22)(p13;q12)
6. Clear cell sarcoma: t(12;22)(q13;q12)7. Retinoblastoma: del(13q14) and gains
1q and 6p8. Lymphomas: specific translocations
12. Bone and soft tissue:1. Congenital fibrosarcoma/congenital
mesoblastic nephroma: t(12;15)(p12;q25), +11, +17, and +20
2. Synovial sarcoma: t(X;18)(p11.2;q11.2)
3. Lipoma: t(3;12)(q27-28;q14-15) andvariants
4. Liposarcoma:1. Myxoid, round cell: t(12;16)(q13;
p11)2. Myxoid: t(12;22)(q13;q12) and
variant3. Well differentiated: rings, markers,
and dmin13. Leiomyoma: t(12;14)(q15;q24):
1. Alveolar soft part sarcoma: der(17)t(X;17)(p11.2;q25)
2. Extraskeletal myxoid chondrosarcoma:t(9;22)(q22;q12), t(9;17)(q22;q11.2),t(9;15)(q22;q21), and t(3;9)(p11;q22)
14. Dermal tumors:1. Dermatofibrosarcoma protuberans:
der (22)t(17;22)(q22;q13.1) or r(22)t(17;22)
2. Giant cell fibroblastoma: t(17;22)(q22;q13.1)
3. Bednar tumor: der (22)t(17;22) (q22;q13.1) or r(22)t(17;22)
4. Hidradenoma: t(11;19)(q21;p13)15. Non-small cell lung cancer: 3p�, +7, and
EGFR high copy number oramplification
16. Dysgerminoma, ovary: i(12p) and 12poverrepresentation
17. Testicular germ cell tumors, seminoma,and nonseminoma: i(12p) and 12pamplification
Genetic Counseling
1. Recurrence risk:1. Retinoblastoma:
1. Predisposition to retinoblastoma whichis caused by germline mutations in theRB1 gene: transmitted in an autosomaldominant fashion.
2. Use RB1 mutation analysis to clarify thegenetic status of at-risk sibs and off-spring when a previously characterizedgermline cancer-predisposing mutationis available.
3. Use indirect testing using polymorphicloci linked to the RB1 gene in somefamilies to clarify genetic status ofat-risk family members if RB1 directDNA testing is not available or isuninformative.
4. Use empiric recurrence risk estimates inall families in which direct DNA testingof RB1 and linkage analysis areunavailable or uninformative.
5. Risk to patient’s siblings:1. When there is an existing family his-
tory: a 45 % chance for siblings ofbilaterally affected cases and a 30 %chance for siblings of unilaterallyaffected cases to develop disease.
2. When there is absence of any familyhistory: 2 % risk for siblings ofbilaterally affected cases and 1 % for
14 H. Chen

siblings of unilaterally affectedcases to develop disease (Draperet al. 1992).
3. There is an additional risk to siblingsin the absence of any family history ordocumented mutation in parental leu-kocyte DNA because of germlinemosaicism. If neither parent has thecancer-predisposing RB1 germlinemutation that was identified in theindex case, germline mosaicism inone parent is possible, and the risk toeach sib of having retinoblastoma is3–5 %.
4. If the index case has mosaicism for anRB1 cancer-predisposing mutation(the mutation arose as a post-zygoticevent) and neither parent has an RB1germline mutation, the risk to the sibsis not increased, and thus it is notwarranted to test the sibs for the RB1mutation identified in the index case.
6. Risk for patient’s offspring:1. About 45 % by the age of 6 years
(consistent with an autosomal domi-nant inheritance with 90 % pene-trance) for the offspring of survivorsof hereditary (multifocal, bilateral)retinoblastoma.
2. About 2.5 % for the offspring of sur-vivors of unilateral retinoblastoma.
3. The low (~1 %), but not negligible,risk to the offspring of index caseswith unifocal disease and a negativefamily history reflect the possibilityof a germline RB1 mutation withlow penetrance or mutationalmosaicism.
2. Implications of somatic and germline mosa-icism in retinoblastoma for genetic counsel-ing (Sippel et al. 1998):1. In a unilateral, simplex case of retino-
blastoma, the absence of a detectedmutation in leukocytes does not reliablypredict that no tumors will arise in thefellow eye in the future.
2. Some bilateral simplex retinoblastomapatients and unilateral, multifocal sim-plex retinoblastoma patients have arecurrence risk among their offspringthat is much less than 45–50 %.
3. It is possible – but not yet proven – thatevery bilateral or unilateral retinoblas-toma patient in whom an initial mutationis identified in tumor cells, but not inleukocytes, has a recurrence risk of zero.
4. If unaffected parents with no previousfamily history of retinoblastoma havean affected child, DNA-based estimatesof the recurrence risk for future childrenshould include, whenever possible, ananalysis of paternal germline DNA.
5. The risk that a patient with unilateralsimplex retinoblastoma will have mutantgerm cells may be much higher than12 %; however, some will be mosaics,and <50 % of their germ cells will bemutant.
3. Genetic counseling for retinoblastoma inthe presence of positive family history(Vogel 1979; Isidro et al. 2011):1. Multiplex disease (>2 affected mem-
bers) – the index patient had retinoblas-toma and one or more close relatives arealso affected:1. Affected individuals definitely carry a
germline mutation.2. A 50 % chance exists that a known
carrier will pass the mutant copy ofthe retinoblastoma gene to each childand there is 50 % penetrance andthere is a 50 % � 90 % = 45 %chance that each child will developretinoblastoma.
2. Multiplex disease (>2 affected mem-bers) – the index patient did not developretinoblastoma as a child, but a parent isknown to be a carrier:1. Approximately 10 % risk that an
asymptomatic son or daughter of aknown carrier is also a carrier.
Chromosome Abnormalities in Pediatric Solid Tumors 15

2. The risk that his or her offspring willinherit a mutation is about 5 %, andthe risk of the disease is90 % � 5 % = 4.5 %.
3. Simplex disease (only one family mem-ber affected) – the index patient hadmultifocal retinoblastoma:1. The patient very likely has a germline
mutation.2. The risk to each offspring is 50 % for
being a carrier and 45 % for develop-ing the disease.
4. Simplex disease (only one family mem-ber affected) – the index patient hadunifocal retinoblastoma (one tumor inone eye only):1. A 12 % risk exists that the patient
carries a germline mutation (i.e., hashereditary retinoblastoma) and an88 % risk that he or she does not(nonhereditary retinoblastoma).
2. The risk for the first child of theindex patient is 6 % for being acarrier and 5.4 % for developing thedisease.
3. If the first child does not develop ret-inoblastoma, the risk for the nextchild is less.
4. If at least one child developsretinoblastoma, the index patientdefinitely has the hereditary type ofthe disease, and the risk for familymembers is as described for multiplexfamilies.
5. Simplex disease (only one familymember affected) – two unaffectedparents have one child withretinoblastoma:1. The risk of the parents’ second child’s
developing retinoblastoma is about1 % if the first child had unifocaldisease and about 6 % if the firstchild had multifocal disease.
2. These risks decrease with every unaf-fected child that passes the years ofhighest risk (years 0–5) withoutdeveloping the disease.
6. Simplex disease (only one family mem-ber affected) – the index patient is anadult of childbearing age who did notdevelop retinoblastoma, but a siblinghad retinoblastoma:1. A small risk exists that one of the
parents is an asymptomatic carrierand the index patient is also anasymptomatic carrier.
2. The carrier risk for the index patient is0.1 % if the affected sibling had uni-lateral retinoblastoma and 0.6 % if theaffected sibling had bilateralretinoblastoma.
3. The risk that the first child of theindex patient will develop retinoblas-toma is approximately half of thesenumbers, i.e., 0.05 % or 0.3 %,respectively.
4. Neuroblastoma:1. Risk for patient’s sibling: low unless a par-
ent has hereditary form of neuroblastoma2. Risk for patient’s offspring: 50 %
5. Wilms’ tumor:1. Risk for patient’s sibling: low unless a
parent has hereditary form of Wilms’tumor
2. Risk for patient’s offspring: 50 %2. Prenatal diagnosis:
1. Retinoblastoma:1. Prenatal testing is possible if the
germline RB1 mutation in the parent isknown or if RB1 linkage analysis isinformative in the family.
2. Mutation analysis on fetal DNAobtained from amniocentesis or CVS.
3. Use prenatal ultrasonography todetect intraocular tumors if the disease-causing RB1 mutation is identified in thefetus.
2. Adrenal neuroblastoma (Kesrouaniet al. 1999):1. Prenatal diagnosis adrenal neuroblas-
toma by ultrasonography usually madein the third trimester.
2. Sonographic appearance of the adrenalneuroblastoma varies:1. Solid
16 H. Chen

2. Purely cystic (50 %)3. Mixed echo pattern (related to necro-
sis, hemorrhage, or spontaneoustumoral involution)
4. Fetal hydrops5. Hydropic placenta with metastases in
the placenta3. Needle biopsy for selection of the group
with favorable biological parameters(N-myc, DNA index).
4. Frequently producing catecholaminesand hence maternal symptoms could aidthe diagnosis.
5. Elevated catecholamines in the amnioticfluid.
3. Wilms’ tumor (Vadeyar et al. 2000):1. Prenatal ultrasonography:
1. Maternal hydramnios.2. Fetal hydrops.3. A solid echogenic mass with a clearly
defined capsule.4. Areas of hemorrhage and necrosis
may be seen within the mass.2. Fetal renal biopsy (nephroblastoma by
histology)3. Management:
1. Surgeries for most solid tumors2. Determining the genetic changes present
in the tumor of an individual patient:becoming increasingly important formanaging the oncology patient
3. Retinoblastoma (Chintagumpalaet al. 2007):1. Goals of treatment: preservation of sight
and life.2. Management of intraocular disease:
1. Enucleation2. External beam radiation (EBR) therapy3. Brachytherapy: involves the place-
ment of a radioactive implant4. Thermotherapy5. Chemothermotherapy6. Laser photocoagulation7. Cryotherapy8. Chemotherapy
3. Management of extraocular disease:Patients with extraocular disease, havinga very poor prognosis with respect to
survival, may benefit from a combina-tion of conventional chemotherapyand EBR, and those with distantmetastatic disease may benefit fromhigh-dose chemotherapy and EBR inconjunction with bone marrow stemcell transplantation.
4. Neuroblastoma (Lee et al. 2003):1. Localized, low-risk disease:
1. Primary curative surgery2. Minimal therapy: low-dose radiation
or chemotherapy3. Supportive care with surveillance
2. Intermediate-risk patients: combinationtherapy with radiation, chemotherapy,and surgery
3. High-risk patients:1. Combination of radiation,
myeloablative chemotherapy, andsurgery (delayed)
2. Autologous bone marrow transplant3. Research protocols
5. Wilms’ tumor: The usual approach inmost patients is nephrectomy followed bychemotherapy with or without postopera-tive radiotherapy.
Fig. 1 Notice the white firm neoplasm (retinoblastoma)filling the vitreous space of the eye
Chromosome Abnormalities in Pediatric Solid Tumors 17

Fig. 2 (a–c) A 12-month-old boy was seen because of a3-month history of a lazy left eye. One month previously,he was noted to have a white reflex in his left eye. He wasseen by an ophthalmologist who diagnosed him to havegroup E retinoblastoma of the left eye. The right eye wasnormal. MRI of orbits demonstrated a calcified mass (a, b)with mild enhancement (c) in the posterior aspect of the leftglobe. The findings are compatible with retinoblastoma.Mutation screening of RB1 gene on DNA isolated from
lymphocytes demonstrated heterozygous for a single-basesubstitution, g.162367G > A, in the last nucleotide ofexon 23 of the coding sequence of the RB1 gene. Thissingle-base substitution translates to a missense mutation,p.Arg830Lys. Although this novel change has not beenreported in the RB1 mutation database, it has been seenin one other child with unilateral retinoblastoma in theperforming molecular laboratory own database (Courtesyof Dr. Grace Guo)
18 H. Chen

Fig. 3 Large, well-circumscribed ovoid Wilms’ tumor in the upper pole of the kidney. Barely identifiable small areas ofhemorrhage and necrosis are present
Fig. 4 (a, b) A 2-year-old female with a left renal masswas seen on the recent ultrasound. CT scan demonstrated alarge heterogeneous mass arising from the left kidney (a).
A heterogeneous metastatic lesion was present in the rightfront lobe of the brain (b). The masses were confirmed asWilms’ tumors (Courtesy of Dr. Grace Guo)
Chromosome Abnormalities in Pediatric Solid Tumors 19

Fig. 5 Karyotype of a patient with Wilms’ tumor showing 46,XY,der(11)(p11.2q13.5)del(11)(p13p15.1)
Fig. 6 Note a lobulatedmeningioma encroachingthe brain at the inferiorsurface of the leftfrontal lobe
20 H. Chen

Fig. 7 (a, b) Karyotypes of two patients with meningioma showing 46,XX,del(22)(q12) (a) and 44,XX,del(7)(q32q36),-11,der(14)t(11;14)(q12;p11),-22 (b)
Chromosome Abnormalities in Pediatric Solid Tumors 21

References
Aerts, I., Lumbroso-Le Rouic, L., Gauthier-Villars, M.,et al. (2006). Retinoblastoma. Orphanet Journal ofRare Diseases, 1, 31–41.
Albertson, D. G., Collins, C., McCormick, F., et al. (2003).Chromosome aberrations in solid tumors. NatureGenetics, 34, 369–376.
Barcus, M. E., Ferreira-Gonzalez, A., Buller, A. M.,et al. (2000). Genetic changes in solid tumors. Seminarsin Surgical Oncology, 18, 358–370.
Barros, J. E. X. S., Soares-Ventura, D. M., Santos, N.,et al. (2012). New cytogenetic aberrations found in acase of aggressive retinoblastoma.Genetics andMolec-ular Research, 11, 1666–1670.
Bennicelli, J. L., & Barr, F. G. (1999). Genetics and thebiologic basis of sarcomas. Current Opinion in Oncol-ogy, 11, 267–274.
Betts, D. R., Cohen, N., Leibundgut, K. E., et al. (2005).Characterization of karyotypic events and evolution inneuroblastoma. Pediatric Blood Cancer, 44, 147–157.
Brodeur, G. M., Maris, J. M., Yamashiro, D. J.,et al. (1997). Biology and genetics of human neuro-blastomas. Journal of Pediatric Hematology/Oncology,19, 93–101.
Carlson, E. A., & Desnick, R. J. (1979). Mutational mosa-icism and genetic counseling in retinoblastoma. Amer-ican Journal of Medical Genetics, 4, 365–381.
Castel, V., Grau, E., Noguera, R., et al. (2007). Molecularbiology of neuroblastoma. Clinical and TranslationalOncology, 9, 478–483.
Fig. 9 N-mycamplification in a patientwith neuroblastoma. Grosscopy number of the orangesignal is noted (LSI®
N-MYC (2p24.1)SpectrumOrange TMprobe)
Fig. 8 Neuroblastomasmear. Note the anaplasticneuroblastic cells mixedwith blood
22 H. Chen

Chen, X., Pappo, A., & Dyer, M. (2015). Pediatricsolid tumor genomics and developmental pliancy.Oncogene, 34, 5207–5215.
Chintagumpala, M., Chevez-Barrios, P., Paysse, E. A.,et al. (2007). Retinoblastoma: Review of current man-agement. The Oncologist, 12, 1237–1246.
Cooley, L. D., Mascarello, J. T., Hirsch, B., et al. (2009).Section E6.5 of the ACMG technical standards andguidelines: Chromosome studies for solid tumor abnor-malities. Genetics in Medicine, 11, 890–897.
Cooper, C. S. (1996). Translocations in solid tumours.Current Opinion in Genetics and Development, 6,71–75.
Coppes, M. J., & Egeler, R. M. (1999). Genetics of Wilmstumor. Seminars in Urologic Oncology, 17, 2–10.
Davidoff, A. M., & Hill, D. A. (2001). Molecular geneticaspects of solid tumors in childhood. Seminars in Pedi-atric Surgery, 10, 106–118.
Devesa, S. S. (1975). The incidence of retinoblastoma.American Journal of Ophthalmology, 80, 263–265.
Dougherty, M. J., Tooke, L. S., Sullivan, L. M.,et al. (2012). Clinical utilization of high-resolutionsingle nucleotide polymorphism based oligonucleotidearrays in diagnostic studies of pediatric patients withsolid tumors. Cancer Genetics, 205, 42–54.
Draper, G. J., Sanders, B. M., Brownbill, P. A.,et al. (1992). Patterns of risk of hereditary retinoblas-toma and applications to genetic counseling. BritishJournal of Cancer, 66, 211–219.
Esparza, S. D. (2012). Childhood cancer, genetics.eMedicine from WebMD. Updated March 5, 2012.Available at: http://emedicine.medscape.com/article/989983-overview
Horsthemke, B. (1992). Genetics and cytogenetics of reti-noblastoma. Cancer Genetics and Cytogenetics, 63,1–7.
İnandıklıoğlu, N., Yılmaz, S., Demirhan, O., et al. (2012).Chromosome imbalances and alterations of AURKAand MYCN genes in children with neuroblastoma.Asian Pacific Journal of Cancer Prevention, 13,5391–5397.
Isidro, M. A., Roque, M. R., Aaberg, T. M. J., et al. (2011).Retinoblastoma. Medscape Reference. Updated29 April 2011. Available at: http://emedicine.medscape.com/article/1222849-overview
Karnes, P. S., Tran, T. N., Cui, M. Y., et al. (1992). Cyto-genetic analysis of 39 pediatric central nervous systemtumors. Cancer Genetics and Cytogenetics, 59,12–19.
Kesrouani, A., Duchatel, F., Seilanian, M., et al. (1999).Prenatal diagnosis of adrenal neuroblastoma by ultra-sound: A report of two cases and review of the litera-ture. Ultrasound in Obstetrics & Gynecology, 13,446–449.
Knudson, A. G. (1971). Mutation and cancer: Statisticalstudy of retinoblastoma. Proceedings of NationalAcademy Science USA, 68, 82–823.
Lee, K. L., Ma, J. F., & Shortliffe, L. D. (2003). Neuro-blastoma: Management, recurrence, and follow-up.Urologic Clinics of North America, 30, 881. http://emedicine.medscape.com/article/988284-overview
Lohmann, D. R., & Gallie, B. L. (2013). Retinoblastoma.GeneReviews. Updated March 28, 2013. Available at:http://www.ncbi.nlm.nih.gov/books/NBK1452/
Maris, J. M., & Matthay, K. K. (1999). Molecular biologyof neuroblastoma. Journal of Clinical Oncology, 17,2264–2279.
Mertens, F., Mandahl, N., Mitelman, F., et al. (1994). Cytoge-netic analysis in the examination of solid tumors in chil-dren. Pediatric Hematology and Oncology, 11, 361–377.
Paxton, C. N., Rowe, L. R., & South, S. T. (2015). Obser-vations of the genomic landscape beyond 1p19q dele-tions and EGFR amplification in glioma. MolecularCytogenetics, 8, 60–66.
Paulino, A. C. (2014). Wilms tumor. eMedicine fromWebMD. Retrieved November 8, 2014. Available at:http://emedicine.medscape.com/article/989398-overview
Sandberg, A. A. (1988). Chromosomal lesions and solidtumors. Hospital Practice October, 15, 93–106.
Sandberg, A. A., & Turc-Carel, C. (1987). The cytogenet-ics of solid tumors. Relation to diagnosis, classificationand pathology. Cancer, 59, 387–395.
Schwab, M., Westermann, F., Hero, B., et al. (2003). Neu-roblastoma: Biology and molecular and chromosomalpathology. The Lancet Oncology, 4, 472–480.
Sippel, K. C., Faioli, R. E., Smith, G. D., et al. (1998).Frequency of somatic and germ-line mosaicism in ret-inoblastoma: Implications for genetic counseling.American Journal of Human Genetics, 62, 610–619.
Tien, J. D. Y., Lau, L. C., Tien, S. L., et al. (2014). Theclinical utility of conventional karyotyping in the detec-tion of cytogenetic abnormalities in soft tissue tumours:An Asian institutional experience.Hong Kong MedicalJournal, 20, 393–400.
Vadeyar, S., Ramsay, M., James, D., et al. (2000). Prenataldiagnosis of congenital Wilms’ tumor(nephroblastoma) presenting as fetal hydrops. Ultra-sound in Obstetrics & Gynecology, 16, 80–83.
Varella-Garcia, M. (2003). Molecular cytogenetics in solidtumors: Laboratorial tool for diagnosis, prognosis, andtherapy. The Oncologist, 8, 45–58.
Vogel, F. (1979). Genetics of retinoblastoma. HumanGenetics, 1, 1–54.
Zin, R., Pham, K., Ashleigh, M., et al. (2012). SNP-basedarrays complement classic cytogenetics in the detectionof chromosomal aberrations in Wilms’ tumor. CancerGenetics, 205, 80–93.
Chromosome Abnormalities in Pediatric Solid Tumors 23