Chest.11 2604.full
-
Upload
amoor010 -
Category
Health & Medicine
-
view
196 -
download
0
Transcript of Chest.11 2604.full

DOI 10.1378/chest.11-2604; Prepublished online April 19, 2012;Chest
RussellAnthony C. Gordon, Nan Wang, Keith R. Walley, Deborah Ashby and James A. NOREPINEPHRINE IN SEPTIC SHOCKVASOPRESSIN COMPARED TO THE CARDIO-PULMONARY EFFECTS OF
http://chestjournal.chestpubs.org/content/early/2012/04/18/chest.11-2604
can be found online on the World Wide Web at: The online version of this article, along with updated information and services
) ISSN:0012-3692http://chestjournal.chestpubs.org/site/misc/reprints.xhtml(without the prior written permission of the copyright holder.reserved. No part of this article or PDF may be reproduced or distributedChest Physicians, 3300 Dundee Road, Northbrook, IL 60062. All rights
ofbeen published monthly since 1935. Copyright2012by the American College is the official journal of the American College of Chest Physicians. It hasChest
Department at (847) 498-1400 or [email protected]. appear online. For inquriires, please contact the AACP Media Relations
Papers in Press are not under media or public embargo once theCHEST (DOI) and date of in-press publication. references to an in-press article must include the digital object identifiernonsubstantive changes. These articles are indexed by PubMed, but any edited or typeset. The final version may contain substantive ornot yet been published in an issue of the journal and have not yet been
Papers in Press are peer-reviewed, accepted articles that haveCHEST
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

1
Word count: 2706
Abstract word count: 249
THE CARDIO-PULMONARY EFFECTS OF VASOPRESSIN COMPARED
TO NOREPINEPHRINE IN SEPTIC SHOCK.
Running head: Cardio-pulmonary effects of vasopressin
Authors: Anthony C Gordon1 MD, Nan Wang
2 PhD, Keith R Walley
3 MD, Deborah
Ashby2 PhD, James A Russell
3 MD
Emails: [email protected]
Institutions:
1. Section of Anaesthetics, Pain Medicine and Intensive Care, Faculty of
Medicine, Imperial College London, UK.
2. Imperial Clinical Trials Unit, School of Public Health, Faculty of Medicine,
Imperial College London, UK.
3. Critical Care Research Laboratories, Institute for Heart + Lung Health, St.
Paul’s Hospital and University of British Columbia, Vancouver, British
Columbia, Canada V6Z 1Y6.
Corresponding author:
Dr Anthony Gordon
Clinical Senior Lecturer & Consultant, Critical Care Medicine
11N, Imperial College / Charing Cross Hospital
Fulham Palace Road
Page 1 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

2
London W6 8RF,
UK
Tel: +44 20 3313 0657
Fax: +44 20 3311 1975
Email: [email protected]
KEY WORDS: Vasopressin, norepinephrine, septic shock, hemodynamics, cardiac
output
Conflicts of interest:
Drs. Russell, Walley, and Gordon have previously served as officers for and hold
stock in Sirius Genomics, which has submitted a patent, owned by the University of
British Columbia and licensed to Sirius Genomics, that is related to the genetics of
vasopressin. The University of British Columbia has also submitted a patent related to
the use of vasopressin in septic shock. Drs. Russell, Walley, and Gordon are named as
inventors on this patent. Drs. Russell and Walley have received consulting fees from
Ferring, which manufactures vasopressin.
Drs Wang and Ashby have no conflicts of interest.
Page 2 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

3
Abstract
Background: Vasopressin is known to be an effective vasopressor in the treatment of
septic shock but uncertainty remains about its effect on other hemodynamic
parameters.
Methods: We examined the cardio-pulmonary effects of vasopressin compared to
norepinephrine in 779 adult patients who had septic shock recruited to the
Vasopressin and Septic Shock Trial (VASST). More detailed cardiac output data was
analyzed for the subset of 241 patients managed with a pulmonary artery catheter and
data was collected for the first 96 hours after randomization. We compared the effects
of vasopressin versus norepinephrine in all patients and also according to severity of
shock (< or ≥ 15µg/min of norepinephrine) and cardiac output at baseline.
Results: Equal blood pressures were maintained in both treatment groups with a
significant reduction in norepinephrine requirements in the vasopressin treated
patients. The major haemodynamic difference between the two groups was a
significant reduction in heart rate in the vasopressin treated patients (p < 0.0001) and
this was most pronounced in the less severe shock stratum (treatment x shock stratum
interaction, p = 0.03). There were no other major cardio-pulmonary differences
between treatment groups, including no difference in cardiac index or stroke volume
index between vasopressin and norepinephrine treated patients. There was
significantly greater use of inotropic drugs in the vasopressin group compared to the
norepinephrine group.
Conclusions: Vasopressin treatment in septic shock is associated with a significant
reduction in heart rate but no change in cardiac output or other measures of perfusion.
(Controlled Trials number, ISRCTN94845869.)
Page 3 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

4
Abbreviation list
APACHE – Acute Physiology and Chronic Health Evaluation
AVP – Arginine vasopressin
CI – Cardiac Index
COPD - chronic obstructive pulmonary disease
CVP - central venous pressure
ECG – Electrocardiogram
FiO2 – Fraction of inspired oxygen
HR – Heart rate
LVSWI – left ventricular stroke work index
MAP – mean arterial pressure
MPAP - mean pulmonary artery pressure
NE- norepinephrine
NYHA - New York Heart Association
PA – Pulmonary Artery
PaO2 – Arterial partial pressure of oxygen
PAOP - pulmonary artery occlusion pressure
RPP – Rate pressure product
SBP - Systolic blood pressure
SIRS - Systemic inflammatory response syndrome
SVI – stroke volume index
SvO2 – Mixed venous oxygen saturation
VASST - Vasopressin and Septic Shock Trial
Page 4 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

5
Introduction:
When cardiovascular failure develops due to sepsis, mortality rates are high1.
As well as treating the underlying infection with antibiotics and source control, the
mainstay of treatment of septic shock is cardiovascular resuscitation using
intravenous fluid, and vasopressor and/or inotropic drugs2. In recent years there has
been increasing interest in vasopressin treatment as an adjunct to other catecholamine
vasopressors.
The rationale behind its use is that there is commonly a relative vasopressin
deficiency in septic shock3 and patients appear sensitive to administration of low-dose
vasopressin infusions4. In several small studies, often unblinded, vasopressin infusion
has invariably been shown to increase blood pressure and spare catecholamine use5-8
.
The effect of vasopressin on cardiac output is less clear with reports that it may
reduce8, increase
7 or have no effect on cardiac output
5,6,9. There have also been
concerns that higher doses of vasopressin (generally > 0.05 U/min) are associated
with cardiac arrest10
. In contrast norepinephrine, the most commonly used
catecholamine vasopressor11
, has both α and β-adrenoreceptor effects and so
increases blood pressure but also may increase heart rate, cause arrhythmias and has
been associated with mesenteric and cutaneous ischemia12,13
.
The Vasopressin and Septic Shock Trial (VASST) was a large double-blind
randomized, controlled trial comparing low-dose vasopressin to norepinephrine in
addition to standard vasopressors in the treatment of established adult septic shock14
.
In the whole study population there was no significant difference in mortality rates
between the treatment groups (28-day mortality, 35.4% in the vasopressin group vs.
39.3% in the norepinephrine group, p=0.26). However, in the a priori stratum of less
severe shock (defined as 5-15µg/min of norepinephrine at baseline) there was a
significantly lower 28-day mortality in vasopressin group compared to the
Page 5 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

6
norepinephrine group (26.5% vs. 35.7%, respectively, p=0.05). In the more severe
shock stratum (≥15µg/min of norepinephrine at baseline) there was no difference in
mortality rates (44.0% vs. 42.5%, p=0.76 in the vasopressin and norepinephrine
groups respectively).
We, therefore, planned to study the cardio-pulmonary effects of vasopressin
compared to norepinephrine in VASST. Specifically we tested the hypothesis that
there is no difference in cardiac output and other measures of hemodynamics between
vasopressin and norepinephrine. To further explore efficacy and safety questions
about vasopressin and norepinephrine, we also compared hemodynamics of
vasopressin versus norepinephrine in the strata of patients who had less and more
severe septic shock (as defined originally in VASST). Finally, because vasopressors
may decrease cardiac output especially in patients who have a low cardiac output, we
compared the effects of vasopressin versus norepinephrine in patients according to
cardiac output at baseline.
Page 6 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

7
Methods:
Patients and protocol
The VASST study has been previously reported14
and was conducted between
July 2001 and April 2006. Research ethics board approval was granted at the
coordinating center (University of British Columbia / St Paul Hospital, P99-0175) and
all participants or their legal representatives gave informed consent. In summary, this
was a multi-center randomized double-blind controlled trial of vasopressin versus
norepinephrine in addition to standard vasopressors for the treatment of septic shock.
Patients were greater than 16 years of age and had septic shock, defined by the
presence of two or more of the systemic inflammatory response syndrome (SIRS)
criteria15
, proven or suspected infection, new dysfunction of at least one organ, and
hypotension despite adequate fluid resuscitation requiring vasopressor support of at
least 5 µg/min of norepinephrine (or equivalent) for six hours. Important clinical
exclusion criteria were unstable coronary syndromes, severe chronic heart disease
(New York Heart Association class III and IV) and vasospastic diathesis. Patients
were randomized to receive a blinded infusion of study drug, either vasopressin (0.01
- 0.03 U/min) or norepinephrine (5 – 15 µg/min). The study drug and all other
vasopressors were titrated and weaned according to protocols. The initial target mean
arterial pressure was 65 – 75 mmHg. All other cardiovascular management including
cardiac output monitoring, setting of cardiac output goals, fluid and inotropic therapy
were at the local treating physician’s discretion.
Data analysis & statistics
Basic cardio-pulmonary variables (blood pressure, heart rate, central venous
pressure, PaO2/FiO2 and pH) and inotrope use (dobutamine, milrinone and
epinephrine) were collected in all patients in the study and are reported for all patients
in this analysis. If a pulmonary artery (PA) catheter was in situ details of pulmonary
Page 7 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

8
artery pressures, cardiac output and mixed venous saturations were collected for the
first 96 after randomization.
Comparison of baseline data between patients who had or did not have a PA catheter
was carried out by chi-squared test or t-test as appropriate. Longitudinal data were
analyzed using linear mixed effect models (PROC MIXED in SAS Enterprise Guide
4.3) comparing treatment effect over time adjusting for any imbalance at baseline and
without imputation for missing data variables. The analysis was done first for all
patients and then repeated for each shock stratum. The p-values of fixed effects
(treatment, shock stratum and their interaction) were provided by the F-test or two-
sided t-test as appropriate. The numbers of patients receiving inotropes was analyzed
using a generalized linear mixed effect model with logit link (PROC GENMOD in
SAS Enterprise Guide 4.3) and p-values of fixed effects and their interaction (baseline
adjusted) were provided by the Chi-square test. A p-value less than 0.05 was
considered significant.
Page 8 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

9
Results:
In total 779 patients were randomized and infused with the blinded study
drugs. Cardiac output monitoring was used in 156 patients at baseline and was
instituted after randomization in a further 85 patients (total = 241, or 31% of patients
in VASST) and was equally balanced between the two treatment groups (vasopressin
n=123 and norepinephrine n=118, p = 0.97). The baseline characteristics of those
patients managed with and without a PA catheter are shown in table 1. Patients who
had a PA catheter had several markers of more severe organ dysfunction including
more renal dysfunction, lower pH, higher lactate and were receiving higher doses of
norepinephrine and phenylephrine at baseline compared to patients who did not have
a PA catheter.
As specified in the protocol vasopressor drugs were titrated to maintain similar
mean arterial pressure in the vasopressin and norepinephrine treatment groups (table
2). As expected vasopressin treatment resulted in a significant reduction in
norepinephrine requirements. The most noticeable cardiovascular difference in the
whole population was a rapid and significant drop in heart rate after starting the
vasopressin infusion (table 2). This was most pronounced in the less severe shock
stratum (table 4) and the interaction statistic examining the treatment x shock stratum
interaction was significant (p=0.03).
There was no difference in cardiac index, stroke volume index or left
ventricular stroke work index associated with vasopressin treatment in the whole
population or in either the more or less severe shock strata. Similarly there was no
difference in markers of oxygen delivery, namely SvO2, pH or serum lactate levels
between treatment groups (tables 2-5). However, there was significantly greater use of
inotropic drugs in the vasopressin group compared to the norepinephrine group,
particularly in the more severe shock stratum where significantly more patients were
Page 9 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

10
treated with inotropic agents and there was a trend for a higher mean dose of
dobutamine (the most commonly used inotrope) to be infused in the vasopressin
group compared to the norepinephrine group.
As any deterioration in cardiac function is likely to be most clinically
important in those who have a low cardiac output we also divided the patients by
cardiac index quartile at baseline. There was no difference in cardiac index over time
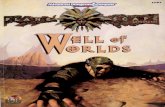
between treatment groups in any of the quartiles (Figure 1A-D) including those who
had the lowest cardiac outputs (1st quartile CI ≤2.9l/min/m
2).
Details of other cardio-pulmonary variables are shown in tables 2-5. There
was no difference in mean pulmonary artery pressure (MPAP), pulmonary artery
occlusion pressure (PAOP) or central venous pressure (CVP) between treatment
groups other than a higher CVP in the vasopressin treated patients in the less severe
shock stratum. Although this difference was statistically significant the actual
difference was small (generally < 1mmHg between vasopressin and norepinephrine
patients).
In view of the complexities and inter-relationship of changes in heart rate,
cardiac output, and inotrope use between vasopressin and norepinephrine treatment
we calculated the rate-pressure product (HR x SBP) as an indicator of myocardial
workload and oxygen consumption. This fell rapidly and was significantly lower in
the vasopressin treated patients compared to the norepinephrine-treated patients and
this decline in rate-pressure product was more marked in the less severe shock
stratum, although the interaction statistic did not reach significance (p = 0.10).
Page 10 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

11
Discussion:
The effect of vasopressin on cardiac output is one of the main concerns about
using vasopressin in the treatment of septic shock, especially in those patients with
poor cardiac function. In this study we have demonstrated that vasopressin therapy
was not associated with a significant decrease in cardiac output compared to
norepinephrine but there was greater use of inotropic drugs in the vasopressin
compared to the norepinephrine treatment group, particularly in the more severe
shock subgroup. The main cardiovascular effect of vasopressin infusion was a
marked decrease in heart rate rather than a reduction in stroke volume index, and this
reduction in heart rate was most striking in the less severe shock stratum. There were
no differences between vasopressin and norepinephrine in the other cardio-pulmonary
variables measured including markers of global perfusion, cardiac filling pressures,
pulmonary artery pressures and oxygenation.
In general, maintenance of a high cardiac output in critical care16
and
specifically sepsis17
is associated with a better outcome and is one of the important
targets of early goal directed therapy18
. However, the use of inotropic drugs to boost
cardiac output and oxygen delivery in established septic shock has been shown to lead
to an increased mortality rate19
. Tachycardia is also thought to have adverse effects on
the myocardium as it both increases myocardial oxygen demand as well as reducing
myocardial oxygen supply due to the reduction in myocardial perfusion in the
shortened diastole. In previous studies a high heart rate has been associated with
higher mortality rates in septic shock20,21
. It is interesting that the greater decrease of
heart rate was seen in vasopressin patients in the less severe shock stratum in whom
there was a significant reduction in mortality with vasopressin compared to
norepinephrine treatment.
Page 11 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

12
We calculated the rate-pressure product in an attempt to summarize the
balance of myocardial workload and oxygen consumption, a higher number
particularly >11,00022
, being associated with an increased risk of myocardial
ischemia23
. There was a significant reduction in the rate-pressure product and the
proportion of patients who had a rate-pressure product >11,000 in the vasopressin-
treated patients (compared to norepinephrine-treated patients) and this may reflect an
improvement in the balance of myocardial oxygen supply and demand. However,
there were no differences in myocardial ischemia or infarction between treatment
groups in the primary VASST analysis or in subsequent post-hoc subgroup analyses
of troponin levels or ischemic ECG changes24,25
.
These effects of vasopressin vs. norepinephrine on hemodynamics agree with
many of the previously published smaller studies. Vasopressin has been associated
with a reduction in heart rate in several studies7,8
. There are two possibilities for this
effect. If the normal baroreceptor response is still intact (particularly in the less severe
shock stratum) the normal physiological response to the vasopressin-induced
vasoconstriction would be a drop in heart rate if stroke volume is maintained,
therefore balancing cardiac output in order to maintain the same blood pressure. The
other explanation may be due to the well-described catecholamine-sparing effect of
vasopressin. Although norepinephrine is described as an α-adrenoreceptor agonist it
does have some β-adrenoreceptor activity and thus a reduction in the rate of infusion
of norepinephrine may lead to a reduction in heart rate. This may be an important
characteristic of vasopressin. Recent work has demonstrated that increased
catecholamine vasopressor load is associated with mortality and other adverse events
once a mean arterial pressure of 70mmHg is obtained21
. At the time of recruitment
into VASST the average mean arterial pressure was ~72mmHg and the mean
norepinephrine infusion rate was ~20µg/min. Norepinephrine requirements reduced
Page 12 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

13
significantly in the vasopressin treated patients. The idea of decatecholaminization,
reducing both endogenous and exogenous adrenergic stimulation, is now thought to
be an important treatment strategy26
and the use of beta-blockers in septic shock is
being considered27,28
. The early use of vasopressin or specific V1a receptor agonists
in early septic shock may be another possible treatment strategy29
. Adhering to the
lower limits of a blood pressure targets may also help reduce vasopressor load30
.
A reduction in cardiac output associated with vasopressin has previously been
reported8 although other controlled trials have shown no effect
5,6,9 and others even an
increase in cardiac output7. The divergent results between studies may reflect
differences in doses and methods of vasopressin administration, concomitant
intravenous fluid resuscitation and inotropic infusions. We administered low-dose
vasopressin (maximum dose 0.03U/min) by continuous infusion after adequate fluid
resuscitation, and then titrated up the infusion while decreasing catecholamine
vasopressors to maintain the target blood pressure. The fact that there was no
difference in stroke volume index between treatment groups suggests that vasopressin
treatment is not significantly decreasing cardiac contractility and that any effect on
cardiac output is due to an effect on heart rate. Reassuringly there was no associated
fall in cardiac output with vasopressin in those patients who had poor cardiac function
(as defined by the lowest cardiac index quartile at baseline); however, it is important
to note that there was a significantly greater proportion of patients who received
inotropic agent infusions amongst vasopressin treated patients. While this greater use
of inotropic agents could have been due to changes in cardiac output or markers of
perfusion, our data do not show such a difference between the vasopressin and
norepinephrine groups. This is in agreement with another recent study that reported
that infusions of vasopressin or terlipressin, in addition to norepinephrine in septic
shock, did not affect microcirculatory flow31
. Despite previous reports that low-dose
Page 13 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

14
vasopressin may reduce pulmonary artery pressures32
, we saw no effect of
vasopressin on these pressures.
There are of course strengths and limitations of this study. The data come
from a large multi-center double-blind randomized controlled trial in which infusion
and weaning of vasopressin and norepinephrine was controlled by protocol, and thus
provide us with the most extensive data set to date in which to compare the effects of
vasopressin to norepinephrine infusion in septic shock. However, PA catheters were
only inserted in a small subgroup (31%) of patients, and their use and the use of
inotropic agents was uncontrolled. As can be seen clearly from table 1, PA catheters
were inserted in sicker patients with higher APACHE II scores, more organ
dysfunction and requiring higher doses of vasopressors. Therefore they are not
representative of the whole population of patients with septic shock. However, if there
are any adverse hemodynamic effects of vasopressin they are more likely to be
present in these sicker patients. This is a post-hoc subgroup analysis and therefore
should only be hypothesis-generating, informing further research studies, rather than
used to inform clinical practice. It is also important to consider the inclusion and
exclusion criteria for the trial. Patients were recruited who had established and treated
septic shock for at least 6 hours. Patients had already been fluid resuscitated and the
blinded study drug (vasopressin or norepinephrine) was substituted for existing
vasopressors and thus it is not a direct comparison of the two vasopressors on
systemic hemodynamics when used as initial therapy in septic shock. Adequate fluid
resuscitation prior to starting vasopressin or any vasopressin analogue is important
and detrimental cardiovascular effects might occur if the patient is fluid deplete. Also
patients with severe chronic heart disease and patients with acute coronary syndromes
were excluded from VASST. Further evidence about the effect of vasopressin
infusion in these groups of patients is required.
Page 14 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

15
Conclusions:
Vasopressin treatment in septic shock is associated with a significant reduction in
heart rate but no change in cardiac output or measures of perfusion. Nonetheless,
more patients in the vasopressin-treated than the norepinephrine-treated group also
received inotropic agent infusions. Any effect of vasopressin on cardiac output seems
due to this decrease in heart rate rather than an effect on stroke volume index. Finally,
there were no adverse effects on cardiac output of vasopressin versus norepinephrine
even in those patients with the poorest cardiac function (as reflected by lowest cardiac
index quartile at baseline).
Page 15 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

16
Acknowledgments:
Funding: Dr Gordon is a UK National Institute for Health Research (NIHR) Clinician
Scientists award holder, and is grateful for funding from the NIHR comprehensive
Biomedical Research Centre funding stream. The VASST trial was funded by a grant
(MCT 44152) from the Canadian Institutes of Health Research.
Author contributions: All authors provided intellectual input to the research and
manuscript. Dr Gordon acts as a guarantor of the paper, taking responsibility for the
integrity of the work as a whole.
Drs Gordon, Walley and Russell contributed to the study conception and design,
acquisition of data, analysis and interpretation of data, statistical analysis, drafting of
the manuscript, and critical revision of the manuscript for important intellectual
content.
Drs Wang and Ashby contributed to the analysis and interpretation of data, statistical
analysis, and critical revision of the manuscript for important intellectual content.
Page 16 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

17
References:
1 Alberti C, Brun-Buisson C, Goodman SV, et al. Influence of systemic inflammatory
response syndrome and sepsis on outcome of critically ill infected patients.
American Journal of Respiratory and Critical Care Medicine 2003; 168:77-84
2 Dellinger RP, Levy MM, Carlet JM, et al. Surviving Sepsis Campaign: international
guidelines for management of severe sepsis and septic shock: 2008. Critical
care medicine 2008; 36:296-327
3 Landry DW, Levin HR, Gallant EM, et al. Vasopressin deficiency contributes to the
vasodilation of septic shock. Circulation 1997; 95:1122-1125
4 Landry DW, Levin HR, Gallant EM, et al. Vasopressin pressor hypersensitivity in
vasodilatory septic shock. Crit Care Med 1997; 25:1279-1282
5 Malay MB, Ashton RC, Jr., Landry DW, et al. Low-dose vasopressin in the
treatment of vasodilatory septic shock. J Trauma 1999; 47:699-703; discussion
703-695
6 Patel BM, Chittock DR, Russell JA, et al. Beneficial effects of short-term
vasopressin infusion during severe septic shock. Anesthesiology 2002;
96:576-582
7 Dunser MW, Mayr AJ, Ulmer H, et al. Arginine vasopressin in advanced
vasodilatory shock: a prospective, randomized, controlled study. Circulation
2003; 107:2313-2319
8 Lauzier F, Levy B, Lamarre P, et al. Vasopressin or norepinephrine in early
hyperdynamic septic shock: a randomized clinical trial. Intensive Care Med
2006; 32:1782-1789
9 Morelli A, Ertmer C, Rehberg S, et al. Continuous terlipressin versus vasopressin
infusion in septic shock (TERLIVAP): a randomized, controlled pilot study.
Crit Care 2009; 13:R130
10 Holmes CL, Walley KR, Chittock DR, et al. The effects of vasopressin on
hemodynamics and renal function in severe septic shock: a case series.
Intensive Care Med 2001; 27:1416-1421
11 Torgersen C, Dunser MW, Schmittinger CA, et al. Current approach to the
haemodynamic management of septic shock patients in European intensive
care units: a cross-sectional, self-reported questionnaire-based survey.
European journal of anaesthesiology 2011; 28:284-290
Page 17 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

18
12 Krejci V, Hiltebrand LB, Sigurdsson GH. Effects of epinephrine, norepinephrine,
and phenylephrine on microcirculatory blood flow in the gastrointestinal tract
in sepsis. Critical care medicine 2006; 34:1456-1463
13 Hayes MA, Yau EH, Hinds CJ, et al. Symmetrical peripheral gangrene: association
with noradrenaline administration. Intensive Care Med 1992; 18:433-436
14 Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion
in patients with septic shock. N Engl J Med 2008; 358:877-887
15 Bone RC, Sibbald WJ, Sprung CL. The ACCP-SCCM consensus conference on
sepsis and organ failure. Chest 1992; 101:1481-1483
16 Shoemaker WC, Appel PL, Kram HB, et al. Prospective trial of supranormal
values of survivors as therapeutic goals in high-risk surgical patients. Chest
1988; 94:1176-1186
17 Abraham E, Bland RD, Cobo JC, et al. Sequential cardiorespiratory patterns
associated with outcome in septic shock. Chest 1984; 85:75-80
18 Rivers E, Nguyen B, Havstad S, et al. Early goal-directed therapy in the treatment
of severe sepsis and septic shock. N Engl J Med 2001; 345:1368-1377
19 Hayes MA, Timmins AC, Yau EH, et al. Elevation of systemic oxygen delivery in
the treatment of critically ill patients. N Engl J Med 1994; 330:1717-1722
20 Parker MM, Shelhamer JH, Natanson C, et al. Serial cardiovascular variables in
survivors and nonsurvivors of human septic shock: heart rate as an early
predictor of prognosis. Critical care medicine 1987; 15:923-929
21 Dunser MW, Ruokonen E, Pettila V, et al. Association of arterial blood pressure
and vasopressor load with septic shock mortality: a post hoc analysis of a
multicenter trial. Critical care 2009; 13:R181
22 Roy WL, Edelist G, Gilbert B. Myocardial ischemia during non-cardiac surgical
procedures in patients with coronary-artery disease. Anesthesiology 1979;
51:393-397
23 Robinson BF. Relation of heart rate and systolic blood pressure to the onset of pain
in angina pectoris. Circulation 1967; 35:1073-1083
24 Mehta S, Granton J, Cook D, et al. Troponin and CKMB trends in patients with
septic shock randomized to vasopressin (VP) or Norepinephrine (NE). Am J
Respir Crit Care Med 2009; 179:A1564
Page 18 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

19
25 Gordon AC, Mehta S, Lapinsky S, et al. Comparison of vasopressin- versus
norepinephrine-associated ischemic ECG changes in septic shock. Intensive
Care Med 2009; 35:S114
26 Brame AL, Singer M. Stressing the obvious? An allostatic look at critical illness.
Critical care medicine 2010; 38:S600-607
27 Rudiger A. Beta-block the septic heart. Critical care medicine 2010; 38:S608-612
28 http://clinicaltrials.gov/ct2/show/NCT01231698:Accessed 30-January 2012
29 Rehberg S, Ertmer C, Vincent JL, et al. Role of selective V1a receptor agonism in
ovine septic shock. Critical care medicine 2011; 39:119-125
30 Takala J. Should we target blood pressure in sepsis? Critical care medicine 2010;
38:S613-619
31 Morelli A, Donati A, Ertmer C, et al. Effects of vasopressinergic receptor agonists
on sublingual microcirculation in norepinephrine-dependent septic shock.
Critical care 2011; 15:R217
32 Holmes CL, Patel BM, Russell JA, et al. Physiology of vasopressin relevant to
management of septic shock. Chest 2001; 120:989-1002
Page 19 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

20
Legend
Figure 1 Cardiac index over time in patients who had PA catheters by cardiac index
quartile at baseline. A - 1st quartile CI ≤2.9 l/min/m
2 at baseline. B- 2
nd quartile CI
2.91-3.7 l/min/m2 at baseline. C - 3
rd quartile CI 3.71-4.5 l/min/m
2 at baseline. D - 4
th
quartile CI >4.5 l/min/m2 at baseline. The grey circles represent the vasopressin-
treated patients and the black squares norepinephrine-treated patients. The treatment
(vasopressin vs. norepinephrine) effect on CI over time was p=0.99 in the first
quartile, p=0.26 in the second quartile, p=0.43 in the third quartile, p=0.36 in the
fourth quartile.
Page 20 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

21
TABLE 1. DEMOGRAPHICS AND BASELINE CHARACTERISTICS OF PATIENTS WHO HAD OR DID NOT
HAVE PA CATHETERS
CHARACTERISTIC
NO PA
CATHETER N (%)
(N = 538)
PA
CATHETER N (%)
(N = 241)
P-VALUE
Age (years) 59.9 ± 16.5 62.0 ± 15.6 0.10
Sex – Male 329 (61.2) 146 (60.6) 0.88
Recent surgical history 185 (34.4) 98 (40.7) 0.09
APACHE II score 26.6 ± 7.6 28.2 ± 6.4 0.004
Ethnicity – Caucasian 453 (84.2) 203 (84.2) 0.99
Pre-existing conditions
Ischemic Heart Disease 85 (15.8) 48 (19.9) 0.16
Congestive Heart Failure 43 (8.0) 15 (6.2) 0.38
COPD 93 (17.3) 34 (14.1) 0.27
Chronic Renal Failure 60 (11.2) 28 (11.6) 0.85
Diabetes 110 (20.4) 55 (22.8) 0.45
Liver Disease 66 (12.3) 22 (9.1) 0.20
Alcoholism 75 (13.9) 33 (13.7) 0.93
Injection Drug Abuse 29 (5.4) 5 (2.1) 0.04
Cancer 131 (24.3) 58 (24.1) 0.93
Immunocompromised 100 (18.6) 39 (16.2) 0.42
Solid Organ Transplant 25 (4.6) 6 (2.5) 0.15
Steroid use 109 (20.3) 59 (24.5) 0.19
Recent Trauma 25 (4.6) 14 (5.8) 0.49
New Organ Failure
Respiratory 465 (86.4) 218 (90.5) 0.11
Renal 344 (63.9) 178 (73.9) 0.006
Hematology/Coagulation 130 (24.2) 72 (29.9) 0.09
Neurologic 134 (24.9) 56 (23.2) 0.62
Cardio-pulmonary variables
Systolic Blood Pressure (mmHg) 109 ± 16 109 ± 17 0.84
Mean Arterial Pressure (mmHg) 72.9 ± 9.9 72.4 ± 8.6 0.52
Arterial pH 7.32 ± 0.10 7.30 ± 0.10 <0.001
Central venous pressure (mmHg) 14.2 ± 4.9 15.4 ± 5.1 0.002
Serum lactate (mmol/L) 3.1 ± 2.9 4.2 ± 3.5 <0.001
PaO2/FiO2 (mmHg) 207 ± 94 192 ± 92 0.05
More severe shock subgroup (>15µg/min
norepinephrine at randomization)
256 (47.6) 145 (60.2) 0.001
Vasoactive Drug Dosage at randomization
Norepinephrine (µg/min) 19.1 ± 19.7 24.0 ± 20.8 0.003
Phenylephrine (µg/min) 139 ± 81 182 ± 80 0.002
Epinephrine (µg/min) 14.5 ± 18.0 9.0 ± 7.7 0.18
Dobutamine (µg/kg/min) 5.4 ± 4.8 6.5 ± 4.1 0.30
Milrinone (µg/kg/min) 0.40 ± 0.37 0.30 ± 0.13 0.36
Plus-minus values are means ± SD. PA denotes pulmonary artery catheter, COPD - chronic
obstructive pulmonary disease, and APACHE II - Acute Physiology and Chronic Health
Evaluation II
Page 21 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

22
Table 2: Cardio-pulmonary variables over time comparing vasopressin versus norepinephrine in all patients (n=779). 0hrs 6 hrs 12 hrs 24 hrs 36 hrs 48 hrs 60 hrs 72 hrs 84 hrs 96 hrs p
#
MAP (mmHg) NE AVP
73.2 ± 9.9 72.4 ± 9.1
75.5 ± 10.1 73.4 ± 9.1
75.0 ± 10.2 74.2 ± 9.6
75.9 ± 11.8 75.9 ± 10.9
76.7 ± 11.1 75.2 ± 11.3
76.2 ± 12.8 76.4 ± 11.4
80.3 ± 12.7 79.6 ± 12.7
79.2 ± 13.7 80.1 ± 13.6
81.1 ± 14.7 82.7 ± 14.0
82.1 ± 13.7 83.0 ± 14.9
0.80
Total NE infusion rate^ (µ g/min) NE AVP
15.9 (9.0-25.0) 14.0 (8.0- 25.0)
17.0 (12.0-33.0) 8.0 (3.0-17.0)
15.0 (10.0-29.8) 6.0 (2.0-14.4)
12.5 (3.0-22.0) 4.0 (0.0-10.0)
15.0 (7.5-28.9) 6.0 (2.0-14.0)
10.0 (3.1-21.0) 3.1 (0.0-9.6)
7.5 (2.0-19.2) 1.0 (0.0-5.9)
5.0 (0.0-15.0) 0.0 (0.0-2.0)
2.5 (0.0-12.5) 0.0 (0.0-2.0)
0.0 (0.0-9.0) 0.0 (0.0-1.1)
<0.0001
HR (bpm) NE AVP
100 ± 20 100 ± 21
99 ± 19 93 ± 20
96 ± 19 90 ± 21
95 ± 20 90 ± 21
96 ± 19 90 ± 22
95 ± 20 90 ± 21
92 ± 19 88 ± 20
92 ± 19 89 ± 20
91 ± 19 88 ± 19
92 ± 18 90 ± 21
<0.0001
CVP (mmHg) NE AVP
14.4 ± 5.0 14.8 ± 5.0
14.9 ± 5.2 15.0 ± 5.0
14.2 ± 4.9 15.1 ± 5.6
14.4 ± 5.7 15.2 ± 5.3
14.6 ± 5.1 14.9 ± 4.8
14.4 ± 5.5 15.0 ± 5.0
14.0 ± 4.9 15.0 ± 4.9
13.6 ± 4.7 14.4 ± 4.9
13.4 ± 4.5 13.8 ± 4.5
13.1 ± 4.9 13.4 ± 4.9
0.14
pH NE AVP
7.31 ± .10 7.32 ± .10
7.32 ± .11 7.32 ± .11
7.33 ± .10 7.34 ± .09
7.35 ± .09 7.35 ± .08
7.34 ± .10 7.34 ± .09
7.35 ± .09 7.35 ± .09
7.37 ± .09 7.36 ± .09
7.38 ± .07 7.38 ± .07
7.39 ± .08 7.39 ± .07
7.39 ± .08 7.40 ± .08
0.66
Lactate (mmol/l) NE AVP
2.3 (1.5-4.6) 2.3 (1.4-4.0)
2.5 (1.5-4.5) 2.4 (1.7-5.2)
2.2 (1.4-4.0) 2.1 (1.4-3.8)
1.8 (1.2-2.9) 1.8 (1.3-2.8)
1.7 (1.2-2.4) 1.7 (1.2-2.4)
0.63
PaO2/FiO2 (mmHg) NE AVP
199 ± 94 206 ± 93
207 ± 97 217 ± 114
213 ± 94 219 ± 97
217 ± 91 217 ± 91
218 ± 98 222 ± 96
218 ± 89 223 ± 109
231 ± 99 226 ± 94
229 ± 103 227 ± 94
231 ± 100 233 ± 89
227 ± 88 229 ± 93
0.79
N receiving any inotropes (existing / new) NE AVP
74 80
68 (57 / 11) 86 (70 / 16)
73 (58 / 11) 94 (81 / 13)
55 (47 / 8) 88 (83 / 5)
67 (66 / 1) 93 (91 / 2)
56 (48 / 8) 85 (81 / 4)
51 (47 / 4) 78 (73 / 5)
45 (41 / 4) 67 (61 / 6)
55 (48 / 7) 66 (62 / 4)
50 (45 / 5) 53 (52 / 1)
0.02
Mean dose dobutamine§ (µ g/kg/min) NE AVP
5.1 ± 3.7 6.4 ± 5.2
6.2 ± 10.3 6.4 ± 5.0
4.4 ± 3.0 6.9 ± 6.4
4.5 ± 5.2 6.3 ± 6.4
3.7 ± 2.4 6.3 ± 5.0
5.3 ± 7.5 6.5 ± 6.8
3.7 ± 1.9 5.2 ± 4.7
3.4 ± 1.5 5.5 ± 6.2
3.4 ± 1.9 4.9 ± 4.5
3.7 ± 1.8 5.7 ± 4.4
0.06
RPP (/100) NE AVP
109 ± 23 108 ± 24
112 ± 24 100 ± 24
109 ± 25 99 ± 26
109 ± 27 101 ± 28
110 ± 27 99 ± 27
109 ± 27 102 ± 27
110 ± 27 105 ± 31
110 ± 28 108 ± 32
112 ± 30 109 ± 31
115 ± 28 112 ± 35
<0.0001
RPP >110 (%) NE AVP
47.6 44.9
49.3 33.0
46.9 30.9
44.4 34.5
45.7 31.3
44.5 32.0
46.1 35.2
47.2 44.1
48.5 44.0
51.2 48.8
<0.0001
Page 22 of 32
Copyright ©
2012 Am
erican College of C
hest Physicians
at McG
ill University Libraries on June 15, 2012
chestjournal.chestpubs.orgD
ownloaded from

23
Values are means ± SD and median (interquartile range) for NE dose and serum lactate levels. # p-value is comparing difference over time between
treatment groups. The abbreviations are NE – norepinephrine, AVP – vasopressin, MAP – mean arterial pressure, HR – heart rate, CVP – central venous
pressure, RPP – rate pressure product (divided by 100). ^NE dose is calculated for all patients who were receiving NE at baseline.
§Dobutamine dose is
calculated for patients receiving dobutamine at that time point.
Page 23 of 32
Copyright ©
2012 Am
erican College of C
hest Physicians
at McG
ill University Libraries on June 15, 2012
chestjournal.chestpubs.orgD
ownloaded from

24
Table 3 Detailed cardio-pulmonary variables over time comparing vasopressin versus norepinephrine in patients who had a PA catheter (n=241) 0hrs 6 hrs 12 hrs 24 hrs 36 hrs 48 hrs 60 hrs 72 hrs 84 hrs 96 hrs p
#
SvO2 (%) NE AVP
68.6 ± 14.4 67.0 ± 15.7
69.5 ± 14.3 64.0 ± 17.0
68.4 ± 13.8 68.3 ± 13.8
69.8 ± 15.6 66.2 ± 14.6
66.9 ± 14.2 67.7 ± 15.8
66.4 ± 15.9 67.3 ± 13.0
62.9 ± 17.4 65.0 ± 16.8
63.3 ± 17.7 65.4 ± 14.4
65.3 ± 17.1 64.2 ± 14.8
62.3 ± 17.4 65.7 ± 15.0
0.92
CI (l/min/m2) NE AVP
3.95 ± 1.26 3.82 ± 1.31
3.92 ± 1.22 3.51 ± 1.39
3.70 ± 1.14 3.46 ± 1.29
3.67 ± 1.02 3.70 ± 1.57
3.61 ± 1.23 3.46 ± 1.45
3.62 ± 1.27 3.65 ± 1.45
3.46 ± 1.18 3.52 ± 1.46
3.82 ± 1.40 3.59 ± 1.39
3.49 ± 1.15 3.47 ± 1.48
3.53 ± 1.10 3.65 ± 1.61
0.87
SVI (ml/min/m2) NE AVP
39.8 ± 14.3 37.5 ± 12.5
39.9 ± 11.9 37.2 ± 14.3
37.8 ± 11.7 36.3 ± 12.7
40.2 ± 11.9 39.0 ± 14.6
37.5 ± 11.9 37.5 ± 14.9
39.9 ± 14.0 39.1 ± 14.8
38.4 ± 12.9 38.9 ± 15.1
40.4 ± 13.6 39.5 ± 13.7
39.6 ± 11.8 38.7 ± 13.0
39.8 ± 11.9 40.0 ± 13.5
0.53
LVSWI (g/m2) NE AVP
28.5 ± 11.7 26.6 ± 10.3
31.2 ± 11.9 28.8 ± 11.9
29.8 ± 12.5 27.7 ± 11.7
31.7 ± 12.2 30.2 ± 14.0
29.4 ± 12.4 29.3 ± 13.6
31.3 ± 12.8 31.5 ± 14.7
32.5 ± 13.4 31.4 ± 15.3
33.2 ± 13.2 31.5 ± 14.2
32.0 ± 11.5 31.6 ± 10.9
34.8 ± 12.3 32.0 ± 12.5
0.72
PAOP (mmHg) NE AVP
17.3 ± 5.7 20.6 ± 5.9
17.9 ± 5.3 19.2 ± 5.0
17.7 ± 4.8 19.6 ± 6.7
18.9 ± 6.1 20.2 ± 6.0
18.7 ± 5.7 19.0 ± 5.8
19.4 ± 7.2 19.1 ± 5.9
17.9 ± 5.3 19.5 ± 6.4
18.7 ± 6.4 19.5 ± 6.8
19.2 ± 8.3 19.4 ± 5.6
18.9 ± 5.2 19.5 ± 6.3
0.32
MPAP (mmHg) NE AVP
28.0 ± 6.7 30.3 ± 6.7
29.4 ± 6.3 30.2 ± 8.2
29.0 ± 5.9 29.9 ± 8.2
29.4 ± 8.7 29.7 ± 6.3
29.4 ± 6.6 29.8 ± 8.0
29.8 ± 7.1 30.1 ± 7.1
28.6 ± 6.9 29.8 ± 7.8
30.0 ± 7.7 29.9 ± 7.3
28.9 ± 7.8 28.7 ± 6.3
30.4 ± 7.3 29.8 ± 7.4
0.82
Values are means ± SD. # p-value is comparing difference over time between treatment groups. The abbreviations are NE – norepinephrine, AVP –
vasopressin, SvO2 mixed venous saturation, CI – cardiac index, SVI – stroke volume index, LVSWI – left ventricular stroke work index, PAOP –
pulmonary artery occlusion pressure, MPAP – mean pulmonary arterial pressure.
Page 24 of 32
Copyright ©
2012 Am
erican College of C
hest Physicians
at McG
ill University Libraries on June 15, 2012
chestjournal.chestpubs.orgD
ownloaded from

25
Table 4: Cardio-pulmonary variables over time comparing vasopressin versus norepinephrine in all patients in the more and less severe shock strata. 0hrs 6 hrs 12 hrs 24 hrs 36 hrs 48 hrs 60 hrs 72 hrs 84 hrs 96 hrs #
p value *p value
interaction
MAP (mmHg) More severe NE AVP Less severe NE AVP
71.7 ± 10.5 71.4 ± 8.8 74.7 ± 9.1 73.3 ± 9.3
74.5 ± 10.4 72.4 ± 9.5 76.6 ± 9.7 74.4 ± 8.6
74.8 ± 10.3 73.6 ± 10.2 75.2 ± 10.0 74.9 ± 9.0
74.6 ± 11.3 74.8 ± 11.3 77.2 ± 12.2 77.0 ± 10.4
76.0 ± 11.9 73.9 ± 11.9 77.5 ± 10.2 76.5 ± 10.5
74.8 ± 12.6 75.1 ± 11.7 77.6 ± 12.9 77.6 ± 10.9
79.7 ± 11.4 76.9 ± 12.3 80.9 ± 13.8 82.1 ± 12.6
77.8 ± 11.8 78.5 ± 13.6 80.7 ± 15.2 81.3 ± 13.5
79.7 ± 14.0 82.8 ± 14.0 82.4 ± 15.2 82.7 ± 14.0
81.7 ± 12.6 81.7 ± 14.8 82.4 ± 14.8 84.0 ± 14.9
0.73 0.55
0.51
Total NE infusion rate^ (µ g/min) More severe NE AVP Less severe NE AVP
22.7 (16.0-37.8) 24.0 (17.0-35.0) 10.0 (7.0-12.0) 9.0 (6.0-11.0)
27.0 (15.5-45.0) 15.0 (8.0-28.0) 12.5 (7.5-16.6) 5.0 (1.0-8.0)
23.0 (15.0-40.0) 12.7 (4.0-26.2) 10.0 (5.0-15.0) 4.0 (0.0-6.0)
17.6 (7.5-27.0) 6.0 (0.0-18.0) 5.0 (1.5-15.0) 2.0 (0.0-6.0)
21.2 (15.0-37.0) 12.0 (4.0-24.0) 10.0 (5.0-15.0) 3.7 (0.0-7.0)
17.0 (28.6-7.5) 5.7 (0.0-16.0) 5.0 (2.0-15.0) 1.5 (0.0-6.0)
15.0 (4.0-23.0) 2.5 (0.0-10.6) 5.0 (0.0-15.0) 0.0 (0.0-3.9)
6.5 (0.0-17.0) 0.0 (0.0-5.3) 2.5 (0.0-10.0) 0.0 (0.0-2.0)
2.5 (0.0-13.0) 0.0 (0.0-3.7) 1.1 (0.0-11.0) 0.0 (0.0-2.0)
0.0 (0.0-10.0) 0.0 (0.0-2.0) 0.0 (0.0-7.5) 0.0 (0.0-0.5)
<0.0001 <0.0001
0.16
HR (bpm) More severe NE AVP Less severe NE AVP
100 ± 20 100 ± 21 97 ± 19 95 ± 18
99 ± 19 93 ± 20 97 ± 18 88 ± 19
96 ± 19 90 ± 21 96 ± 20 85 ± 19
95 ± 20 90 ± 21 95 ± 21 86 ± 20
96 ± 19 90 ± 22 95 ± 19 84 ± 20
95 ± 20 90 ± 21 95 ± 20 88 ± 21
92 ± 19 88 ± 20 93 ± 19 87 ± 21
92 ± 19 89 ± 20 95 ± 20 89 ± 20
91 ± 19 88 ± 19 94 ± 20 87 ± 19
92 ± 18 90 ± 21 95 ± 20 92 ± 22
0.02 <0.0001
0.03
CVP (mmHg) More severe NE AVP Less severe NE AVP
14.7 ± 5.1 15.6 ± 5.1 14.2 ± 4.8 14.0 ± 4.8
15.5 ± 5.4 15.7 ± 4.8 14.2 ± 4.8 14.3 ± 5.2
14.7 ± 5.0 15.9 ± 6.0 13.7 ± 4.8 14.3 ± 5.0
14.9 ± 5.8 15.9 ± 5.4 13.8 ± 4.8 14.5 ± 5.1
15.1 ± 5.5 15.5 ± 4.9 14.0 ± 4.5 14.2 ± 4.6
15.1 ± 6.0 15.7 ± 5.3 13.6 ± 4.8 14.4 ± 4.7
14.6 ± 5.5 15.1 ± 4.9 13.3 ± 4.1 14.9 ± 4.9
14.1 ± 5.2 14.7 ± 4.7 13.1 ± 4.2 14.1 ± 5.1
14.2 ± 5.0 13.9 ± 4.5 12.6 ± 3.9 13.6 ± 4.7
13.6 ± 5.2 13.6 ± 5.1 12.7 ± 4.4 13.2 ± 4.8
0.57 0.007
0.02
pH More severe NE AVP Less severe NE AVP
7.29 ± 0.11 7.29 ± 0.10 7.35 ± 0.08 7.35 ± 0.08
7.29 ± 0.12 7.29 ± 0.12 7.35 ± 0.09 7.35 ± 0.09
7.31 ± 0.11 7.32 ± 0.10 7.35 ± 0.10 7.36 ± 0.08
7.33 ± 0.10 7.33 ± 0.09 7.36 ± 0.08 7.37 ± 0.07
7.32 ± 0.10 7.32 ± 0.10 7.36 ± 0.09 7.36 ± 0.08
7.34 ± 0.10 7.34 ± 0.10 7.37 ± 0.08 7.37 ± 0.08
7.36 ± 0.09 7.35 ± 0.10 7.38 ± 0.08 7.38 ± 0.08
7.37 ± 0.07 7.37 ± 0.07 7.39 ± 0.08 7.39 ± 0.07
7.38 ± 0.08 7.39 ± 0.07 7.40 ± 0.07 7.40 ± 0.07
7.39 ± 0.08 7.39 ± 0.08 7.40 ± 0.09 7.40 ± 0.08
0.91 0.59
0.76
Lactate (mmol/l) More severe
Page 25 of 32
Copyright ©
2012 Am
erican College of C
hest Physicians
at McG
ill University Libraries on June 15, 2012
chestjournal.chestpubs.orgD
ownloaded from

26
NE AVP Less severe NE AVP
3.0 (1.7-5.4) 3.3 (2.0-6.1) 1.9 (1.3-3.7) 1.6 (1.1-2.5)
2.9 (1.8-5.8) 3.5 (1.9-6.3) 1.9 (1.4-3.2) 2.1 (1.3-2.5)
2.5 (1.6-4.6) 2.9 (1.8-5.6) 1.7 (1.2-2.8) 1.7 (1.2-2.3)
1.8 (1.3-3.1) 2.1 (1.5-3.3) 1.7 (1.2-2.6) 1.6 (1.2-2.1)
1.7 (1.3-2.5) 1.8 (1.3-2.7) 1.6 (1.2-2.2) 1.7 (1.1-2.2)
0.51 0.95
0.69
PaO2/FiO2 (mmHg) More severe NE AVP Less severe NE AVP
188 ± 95 194 ± 95 210 ± 92 217 ± 90
197 ± 101 206 ± 118 218 ± 92 229 ± 108
207 ± 98 209 ± 104 220 ± 89 229 ± 88
211 ± 92 212 ± 91 223 ± 90 223 ± 91
213 ± 100 211 ± 98 224 ± 94 233 ± 93
216 ± 89 224 ± 129 221 ± 90 223 ± 84
229 ± 96 219 ± 98 233 ± 103 232 ± 90
226 ± 95 230 ± 92 231 ± 111 225 ± 95
233 ± 102 237 ± 92 228 ± 98 229 ± 87
229 ± 83 233 ± 93 225 ± 94 225 ± 93
0.74 0.99
0.81
N receiving any inotropes (existing/new) More severe NE AVP Less severe NE AVP
54 62 20 18
53 (44 / 9) 67 (55 / 12) 15 (13 / 2) 19 (15 / 4)
53 (44 / 9) 72 (64 / 8) 20 (14 / 6) 22 (17 / 5)
40 (34 / 6) 65 (62 / 3) 15 (13 / 2) 23 (21 / 2)
50 (49 / 1) 72 (70 / 2) 17 (17 / 0) 21 (21 / 0)
41 (37 / 4) 64 (61 / 3) 15 (11 / 4) 21 (20 / 1)
39 (37 / 2) 56 (54 / 2) 12 (10 / 2) 22 (19 / 3)
30 (29 / 1) 46 (41 / 5) 15 (12 / 3) 21 (20 / 1)
34 (31 / 3) 45 (43 / 2) 21 (17 / 4) 21 (19 / 2)
34 (30 / 4) 37 (37 / 0) 16 (15 / 1) 16 (15 / 1)
0.03 0.27
0.69
Mean dose dobutamine§ (µ g/kg/min) More severe NE AVP Less severe NE AVP
5.1 ± 3.7 7.0 ± 5.7 5.1 ± 4.0 4.1 ± 1.8
6.5 ± 11.9 6.9 ± 5.4 5.3 ± 4.0 4.6 ± 2.3
3.7 ± 1.9 7.1 ± 6.9 5.8 ± 4.4 5.7 ± 3.2
4.5 ± 6.2 6.8 ± 7.1 4.5 ± 1.4 4.3 ± 2.2
3.5 ± 1.9 6.6 ± 5.4 4.3 ± 3.4 4.7 ± 2.2
5.2 ± 8.6 7.1 ± 7.5 5.4 ± 2.0 4.4 ± 2.8
3.6 ± 2.0 5.6 ± 5.1 5.2 ± 9.0 4.0 ± 2.7
3.5 ± 1.6 5.6 ± 4.8 3.1 ± 1.4 5.2 ± 9.0
3.6 ± 2.0 5.6 ± 5.0 3.1 ± 1.6 3.5 ± 2.5
3.7 ± 1.9 6.4 ± 4.9 3.6 ± 1.3 4.1 ± 2.7
0.07 0.66
0.59
RPP (/100) More severe NE AVP Less severe NE AVP
110 ± 24 112 ± 26 108 ± 23 104 ± 23
112 ± 24 103 ± 22 111 ± 24 96 ± 25
109 ± 25 103 ± 26 109 ± 25 95 ± 25
106 ± 25 103 ± 26 111 ± 28 100 ± 29
109 ± 26 103 ± 26 112 ± 27 96 ± 28
105 ± 25 102 ± 25 112 ± 29 103 ± 30
107 ± 25 102 ± 26 114 ± 29 109 ± 5
105 ± 27 106 ± 31 116 ± 28 110 ± 33
108 ± 28 109 ± 30 116 ± 31 109 ± 32
111 ± 27 108 ± 32 118 ± 29 116 ± 37
0.05 <0.0001
0.10
RPP >110 (%) More severe NE AVP Less severe
49.0 50.7
53.8 38.4
47.6 36.3
41.2 38.0
43.9 36.8
40.2 31.4
40.5 32.2
36.5 41.5
41.4 42.9
48.4 44.8
0.04
0.12
Page 26 of 32
Copyright ©
2012 Am
erican College of C
hest Physicians
at McG
ill University Libraries on June 15, 2012
chestjournal.chestpubs.orgD
ownloaded from

27
NE AVP
46.2 39.0
44.5 27.5
46.1 25.6
47.7 31.0
47.5 25.7
48.9 32.6
51.7 38.0
57.7 46.2
55.4 44.8
53.9 52.2
<0.0001
Values are means ± SD and median (interquartile range) for NE dose and serum lactate levels. # p-value is comparing difference over time between
treatment groups; *p-value is testing for a treatment group x shock subgroup interaction. The abbreviations are NE – norepinephrine, AVP –
vasopressin, MAP – mean arterial pressure, HR – heart rate, CVP – central venous pressure, RPP – rate pressure product (divided by 100). ^Median NE
dose is calculated for all patients who were receiving NE at baseline. §Mean dobutamine dose is calculated for patients receiving dobutamine at that time
point
Page 27 of 32
Copyright ©
2012 Am
erican College of C
hest Physicians
at McG
ill University Libraries on June 15, 2012
chestjournal.chestpubs.orgD
ownloaded from

28
Table 5: Detailed cardio-pulmonary variables over time comparing vasopressin versus norepinephrine in patients who had a PA catheter in the more and
less severe shock strata. 0hrs 6 hrs 12 hrs 24 hrs 36 hrs 48 hrs 60 hrs 72 hrs 84 hrs 96 hrs #
p value ##
p
value interaction
SvO2 (%) More severe NE AVP Less severe NE AVP
67.4 ± 16.7 62.2 ± 16.3 69.8 ± 11.6 74.1 ± 11.8
68.9 ± 15.6 58.5 ± 18.1 70.3 ± 12.6 73.4 ± 9.5
67.4 ± 14.2 64.7 ± 14.8 69.9 ± 13.4 72.8 ± 11.0
70.7 ± 13.1 61.2 ± 15.2 68.5 ± 18.9 70.8 ± 12.7
66.9 ± 12.8 64.7 ± 15.2 67.0 ± 16.7 71.4 ± 16.1
67.7 ± 12.6 63.9 ± 14.0 64.7 ± 19.8 71.7 ± 10.2
61.4 ± 16.7 60.6 ± 18.1 66.1 ± 19.0 70.3 ± 13.7
62.5 ± 16.4 59.8 ± 15.5 64.5 ± 20.2 71.9 ± 10.3
61.8 ± 17.5 58.8 ± 15.5 70.3 ± 15.8 73.9 ± 6.4
63.1 ± 14.7 61.4 ± 16.5 60.4 ± 22.9 74.2 ± 5.6
0.99 0.95
0.97
CI (l/min/m2) More severe NE AVP Less severe NE AVP
3.96 ± 1.14 3.76 ± 1.27 3.95 ± 1.41 3.93 ± 1.39
3.67 ± 0.99 3.51 ± 1.37 4.36 ± 1.45 3.50 ± 1.44
3.59 ± 1.26 3.41 ± 1.19 3.86 ± 0.93 3.55 ± 1.45
3.55 ± 1.05 3.65 ± 1.52 3.83 ± 0.99 3.81 ± 1.69
3.41 ± 1.22 3.26 ± 1.31 3.95 ± 1.19 3.80 ± 1.64
3.47 ± 1.28 3.53 ± 1.45 3.83 ± 1.24 3.87 ± 1.45
3.36 ± 1.16 3.31 ± 1.42 3.64 ± 1.23 3.85 ± 1.47
3.54 ± 1.29 3.47 ± 1.25 4.18 ± 1.47 3.74 ± 1.56
3.33 ± 1.16 3.30 ± 1.21 3.72 ± 1.11 3.73 ± 1.82
3.22 ± 0.90 3.64 ± 1.57 4.01 ± 1.26 3.65 ± 1.74
0.32 0.30
0.15
SVI (ml/min/m2) More severe NE AVP Less severe NE AVP
39.8 ± 14.3 37.5 ± 12.5 41.4 ± 16.8 40.8 ± 14.6
39.9 ± 11.9 37.2 ± 14.3 46.9 ± 12.7 38.4 ± 15.7
37.8 ± 11.7 36.3 ± 12.7 40.2 ± 38.6 38.6 ± 14.9
40.2 ± 11.9 39.0 ± 14.6 42.8 ± 11.5 42.7 ± 16.2
37.5 ± 11.9 37.5 ± 14.9 42.3 ± 11.1 42.6 ± 17.5
39.9 ± 14.0 39.1 ± 14.8 42.5 ± 14.7 42.6 ± 16.0
38.4 ± 12.9 38.9 ± 15.1 40.6 ± 11.2 41.9 ± 15.5
40.4 ± 13.6 39.5 ± 13.7 43.4 ± 12.3 41.1 ± 15.3
39.6 ± 11.8 38.7 ± 13.0 41.4 ± 9.2 42.2 ± 16.1
39.8 ± 11.9 40.0 ± 13.5 43.1 ± 10.4 41.0 ± 14.9
0.36 0.86
0.66
LVSWI (g/m2) More severe NE AVP Less severe NE AVP
27.8 ± 11.7 25.3 ± 8.0 29.5 ± 11.8 28.4 ± 12.9
28.8 ± 12.0 27.7 ± 10.6 35.8 ± 10.3 30.9 ± 14.2
28.3 ± 14.5 25.3 ± 8.3 32.1 ± 8.5 31.6 ± 15.4
30.4 ± 14.8 27.1 ± 11.1 33.4 ± 7.9 34.9 ± 16.7
26.7 ± 13.4 26.4 ± 9.9 33.5 ± 9.5 34.2 ± 17.4
30.1 ± 15.1 28.3 ± 12.6 32.9 ± 9.0 37.3 ± 16.7
31.3 ± 14.9 28.4 ± 12.8 34.5 ± 10.7 36.9 ± 18.2
31.2 ± 14.3 30.8 ± 11.9 35.5 ± 11.6 32.5 ± 17.2
31.7 ± 12.4 30.1 ± 9.3 32.3 ± 10.5 34.2 ± 13.1
33.9 ± 14.5 31.6 ± 13.6 36.4 ± 7.45 32.8 ± 10.6
0.62 0.16
0.16
PAOP (mmHg) More severe NE AVP Less severe NE AVP
17.4 ± 6.0 20.6 ± 4.7 17.2 ± 5.3 20.5 ± 7.4
18.1 ± 6.3 19.9 ± 4.2 17.7 ± 6.2 17.7 ± 6.2
18.2 ± 5.4 19.5 ± 4.4 16.9 ± 3.7 19.8 ± 9.6
19.1 ± 7.2 20.6 ± 5.2 18.5 ± 4.4 19.5 ± 7.2
18.9 ± 5.6 18.9 ± 4.9 18.3 ± 5.9 19.0 ± 7.3
19.3 ± 7.8 19.8 ± 5.1 19.6 ± 6.3 17.7 ± 7.0
17.6 ± 4.7 20.6 ± 6.2 18.3 ± 6.2 17.4 ± 6.3
18.1 ± 7.1 19.1 ± 4.2 19.5 ± 5.5 20.0 ± 9.5
19.1 ± 7.7 19.9 ± 6.0 19.4 ± 9.1 18.7 ± 5.2
18.8 ± 5.9 19.2 ± 6.8 19.1 ± 3.5 20.0 ± 5.3
0.20 0.97
0.39
Page 28 of 32
Copyright ©
2012 Am
erican College of C
hest Physicians
at McG
ill University Libraries on June 15, 2012
chestjournal.chestpubs.orgD
ownloaded from

29
MPAP (mmHg) More severe NE AVP Less severe NE AVP
27.3 ± 7.2 29.6 ± 6.4 28.9 ± 6.0 31.2 ± 7.0
29.9 ± 7.4 30.1 ± 7.2 28.7 ± 4.3 30.3 ± 9.7
29.8 ± 6.5 29.2 ± 6.2 27.8 ± 4.6 30.9 ± 10.6
30.7 ± 10.4 29.6 ± 6.0 27.5 ± 4.2 29.8 ± 7.0
30.1 ± 7.5 29.2 ± 7.4 28.2 ± 4.8 30.9 ± 8.8
30.4 ± 8.0 29.6 ± 6.1 28.9 ± 5.6 31.0 ± 8.6
28.7 ± 7.4 29.2 ± 7.2 28.5 ± 6.2 30.9 ± 8.8
29.5 ± 8.6 29.7 ± 7.1 30.6 ± 6.4 30.2 ± 7.6
29.2 ± 8.1 28.2 ± 6.1 28.6 ± 7.4 29.6 ± 6.7
30.5 ± 8.4 27.6 ± 5.6 30.2 ± 4.9 34.3 ± 8.6
0.10 0.12
0.02
Values are means ± SD. # p-value is comparing difference over time between treatment groups; *p-value is testing for a treatment group x shock
subgroup interaction. The abbreviations are NE – norepinephrine, AVP – vasopressin, SvO2 mixed venous saturation, CI – cardiac index, SVI – stroke
volume index, LVSWI – left ventricular stroke work index, PAOP – pulmonary artery occlusion pressure, MPAP – mean pulmonary arterial pressure,
Page 29 of 32
Copyright ©
2012 Am
erican College of C
hest Physicians
at McG
ill University Libraries on June 15, 2012
chestjournal.chestpubs.orgD
ownloaded from

A
B
Figure 1 Page 31 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

C
D
Figure 1 Page 32 of 32
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from

DOI 10.1378/chest.11-2604; Prepublished online April 19, 2012;Chest
RussellAnthony C. Gordon, Nan Wang, Keith R. Walley, Deborah Ashby and James A.
NOREPINEPHRINE IN SEPTIC SHOCKTHE CARDIO-PULMONARY EFFECTS OF VASOPRESSIN COMPARED TO
June 15, 2012This information is current as of
http://chestjournal.chestpubs.org/content/early/2012/04/18/chest.11-2604Updated Information and services can be found at:
Updated Information & Services
http://www.chestpubs.org/site/misc/reprints.xhtmlonline at: Information about reproducing this article in parts (figures, tables) or in its entirety can be foundPermissions & Licensing
http://www.chestpubs.org/site/misc/reprints.xhtmlInformation about ordering reprints can be found online:
Reprints
the right of the online article.Receive free e-mail alerts when new articles cite this article. To sign up, select the "Services" link to
Citation Alerts
slide format. See any online figure for directions. articles can be downloaded for teaching purposes in PowerPointCHESTFigures that appear in Images in PowerPoint format
[email protected]. For inquriires, please contact the AACP Media Relations Department at (847) 498-1400 or
Papers in Press are not under media or public embargo once the appear online.CHEST (DOI) and date of in-press publication. PubMed, but any references to an in-press article must include the digital object identifier version may contain substantive or nonsubstantive changes. These articles are indexed bypublished in an issue of the journal and have not yet been edited or typeset. The final
Papers in Press are peer-reviewed, accepted articles that have not yet beenCHEST
Copyright © 2012 American College of Chest Physicians at McGill University Libraries on June 15, 2012chestjournal.chestpubs.orgDownloaded from