Chemotherapeutic tumor microparticles elicit a neutrophil ... · 7/11/2020 · 1 Chemotherapeutic...
Transcript of Chemotherapeutic tumor microparticles elicit a neutrophil ... · 7/11/2020 · 1 Chemotherapeutic...

1
Chemotherapeutic tumor microparticles elicit a neutrophil response targeting
malignant pleural effusions
Pingwei Xu1,6
, Ke Tang1,6
, Jingwei Ma1, Huafeng Zhang
1, Dianheng Wang
1, Liyan
Zhu1, Jie Chen
1, Keke Wei
1, Jincheng Liu
1, Haiqing Fang
1, Liang Tang
1, Yi Zhang
2,
Jing Xie2, Yuying Liu
2, Rui Meng
3, Li Liu
3, Xiaorong Dong
3, Kunyu Yang
3, Gang
Wu3, Fei Ma
4, Bo Huang
1,2,5*
1Department of Biochemistry and Molecular Biology, Tongji Medical College,
Huazhong University of Science and Technology, Wuhan 430030, China.
2Department of Immunology, Institute of Basic Medical Sciences & State Key
Laboratory of Medical Molecular Biology, Chinese Academy of Medical Sciences
and Peking Union Medical College, Beijing 100005, China.
3Cancer Center, Union Hospital, Tongji Medical College, Huazhong University of
Science and Technology, Wuhan 430022, China.
4National Cancer Center, State Key Laboratory of Molecular Oncology, Cancer
Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College,
Beijing 100005, China.
5Clinical Immunology Center, Chinese Academy of Medical Sciences, Beijing 100005,
China
6 These authors contributed equally
Running title: Microparticles elicit a neutrophil response to kill tumors
Keywords: microparticles, neutrophils, malignant pleural effusions
*Correspondence: Bo Huang, Chinese Academy of Medical Sciences, 5 Dong Dan
San Tiao, Beijing 100005, China. Phone: 86-10-69156447; Fax: 86-10-65229258;
E-mail: [email protected]
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

2
Abstract
Malignant pleural effusion (MPE) is a frequent complication of various cancers and
often leads to a poor quality of life, prognosis, and life expectancy, and its
management remains palliative. New approaches that can effectively treat MPE are
highly desirable. Here, we show that methotrexate (MTX)-packaging, tumor
cell–derived microparticles (MTX-MP) act as an effective immunotherapeutic agent
to treat patients with MPE by mobilizing and activating neutrophils. We find that
MTX-MPs perfusion via a pleural catheter elicits the recruitment of neutrophils in
patients through macrophage-released CXCL1 and CXCL2. By performing ex vivo
experiments, we find that the recruited neutrophils are activated and release reactive
oxygen species (ROS) and neutrophil extracellular trap (NET) to kill tumor cells.
Neutrophil-released NETs were also able to seal-off the damaged endothelium,
facilitating MPE resolution in vitro and in tumor-bearing mice. These findings reveal
the potential for use of cell-derived materials to package drugs as an
immunotherapeutic agent against MPE.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

3
Introduction
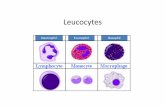
Despite adaptive antitumor immunity, the mobilization of the innate immune system
in cancer immunotherapies is lagging. Neutrophils, the most abundant innate immune
cells, represent 50–70% of all leukocytes, and more than 1011
neutrophils undergo
death daily in our body (1). Maintaining this innate cell death without activation is
presumed to prevent ubiquitous infections. However, this physiological process
presents an opportunity to modulate neutrophils to exert an antitumor effect before
their death. Indeed, antitumor responses from neutrophils can be elicited by Coley
toxin and Bacillus Calmette-Guérin in certain cancer patients (2,3). However,
neutrophils can also be polarized to become tumor-promoting in particular tumor
microenvironments, where factors such as inhibitory cytokines, hypoxia, low pH and
potassium overabundance can redirect neutrophils, thus limiting the treatment
efficiency (4). Studies have revealed the double-edged sword role of neutrophils in
tumor microenvironments (5,6) but mobilizing neutrophils in cancer immunotherapy
remains a challenge.
Solid tumor cells are likely to metastasize to the pleura through the bloodstream and
invade the visceral pleura, resulting in an effusion in the pleural cavity, referred to as
malignant pleural effusion (MPE)(7,8). About 40% of lung cancer patients develop
MPE (9). Patients with refractory MPE commonly suffer dyspnea, followed by chest
discomfort, coughing, and poor quality of life and may have a reduced life span. Lung
cancer patients with MPE display a decreased rate of survival compared with patients
without pleural effusions (9,10). Despite the progress in cancer treatment, the current
management of MPE remains palliative. Thus, approaches that can efficiently target
MPE with minimal side effects are highly desirable. MPE is stemmed from the
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

4
damaged blood vessels, where a relatively physiological state with average oxygen
pressure, pH value, and electrolyte balance may be present. The increased capillary
permeability may facilitate the entry of leukocytes into the effusions. Thus, we asked
whether we could use this to mobilize neutrophils into malignant effusions where the
neutrophils could avoid malignant re-education and exert an antitumor effect.
Tumor cells are able to release extracellular vesicles, which are labeled as tumor
microparticles (T-MPs)(11). We previously reported that T-MPs can stimulate DCs
using the cGAS/STING pathway and function as a vaccination platform (12,13), but
such T-MPs also stimulate M2 macrophage polarization to exert a tumor-promoting
effect (14). We also found that T-MPs can function as natural carriers to deliver
chemotherapeutic drugs or oncolytic viruses to tumor cells, effectively killing
malignant cells (15,16). T-MPs, packaged with chemotherapeutic drugs, can
reprogram M2 macrophages toward M1 phenotype (17). Thus, the incorporation of
drugs into T-MPs may yield chemo-immunotherapeutic, dual-functional MPs. In this
study, we provide evidence that methotrexate (MTX)-packaging T-MPs recruited
neutrophils to the pleural cavity where they exerted a therapeutic effect against MPE
in cancer patients.
Materials and Methods
Patient recruitment and study design
The clinical trial was registered in the Chinese Clinical Trial Register (No.
ChiCTR-ICR-15006304), as a multicenter, randomized, double-blind,
parallel-treatment study. The trial was conducted in accordance with the Declaration
of Helsinki, the relevant International Conference on Harmonization Good Clinical
Practice guidelines, and all applicable regulatory and ethical requirements. The
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

5
Clinical Trials Ethics Committee of the Huazhong University of Science and
Technology approved the clinical trial (NO: [2015] 0702-2). Sixty-two patients, who
completed the whole treatment schedule (Supplementary Table S1) were used for
sample collection. The main inclusion criteria were age 18-70 years and diagnosed
with non-squamous non-small cell lung cancer with primary malignant pleural
effusion and pathologically confirmed non-squamous advanced non-small cell lung
cancer with pleural effusion cytology showing tumor cells. Main exclusion criteria
included pregnancy, lactation, allergy to multiple drugs, severe comorbidities,
psychological diseases, severe infection including pleural infection, previously
received chemotherapy or local intrathoracic administration, and participation in other
clinical trials within the past three months. All patients were recruited from the Hubei
Cancer Hospital or Union Hospital affiliated to Tongji Medical College of Huazhong
University of Science and Technology. Patients were received pemetrexed (PEM, 500
mg/m2,Nanjing Pharmaceutical, China) and cisplatin (DDP, 75 mg/m
2,Qilu
Pharmaceutical, China) i.v. administration at day 1 in 21-day cycles according to
NCCN guidelines, and treated with 50 mL methotrexate tumor cell–derived
microparticles (MTX-MPs; 5×107 MPs containing 25 μg MTX preparation discussed
below) or 50 mL saline at day 5, 7, 9, 11, 13, and 15 by intrathoracic (i.t.) injection
every other day (QOD), see schedule in Fig. 1A. MPE was collected at day 5 (before
MTX-MP treatment) and day 7 (after first time of MTX-MP treatment) for cell
population analysis. 10 mL MPE were collected at 2, 4, 8, 12, 24, and 48 hours after
MTX-MP or saline treatment (n=6) for chemokine detection. All MPE samples were
transferred to the lab for analysis no more than 1 hour after drainage. All patients
signed informed consent forms to participate in the study.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

6
Healthy donor
Following informed consent, peripheral blood samples (10 mL) were collected from
healthy volunteers (n=9). Blood samples were transferred to the lab for analysis no
more than 15 minutes after blood draw.
Animals and cell lines
Female wild-type C57BL/6 and BALB/c mice (6-8 weeks) were purchased from the
Center of Medical Experimental Animals of Hubei Province (Wuhan, China). Female
nude mice (6-8 weeks) were purchased from Beijing Vital River Laboratory Animal
Technology Co. Ltd. C57BL/6 CD45.1 mice (B6.SJL-PtprcaPepcb/BoyJ) were
purchased from Peking University Health Science Center. All animal experiments
were conducted in accordance with a protocol approved by the Animal Care and Use
Committee of Tongji Medical College.
The human tumor cell line A549 was purchased from ATCC. Murine
hepatocarcinoma cell line H22, Lewis murine lung carcinoma (LLC) cell line, and
human umbilical vein endothelial cell (HUVEC) line CRL-1730 were purchased from
the China Center for Type Culture Collection (Beijing, China). A549, H22, and
CRL-1730 cells were cultured in RPIM-1640 medium (Thermo Fisher Scientific) with
10% fetal bovine serum (Gibco), and Lewis cells were cultured in MEM medium
(Thermo Fisher Scientific) with 10% fetal bovine serum (Gibco). Cells were tested for
mycoplasma detection, interspecies cross contamination, and authenticated by
isoenzyme and short tandem repeat (STR) analyses in the Cell Resource Centre of
Peking Union Medical College before the beginning of the study and spontaneously
during the research, and the cells were kept in culture for no more than 10 passages.
All cells were cultured in a humidified atmosphere containing 5% CO2 at 37 °C.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

7
Preparation of MTX packaging MPs
MTX-MPs were prepared according to our previously published paper (15). In brief,
2×108 A549 cells containing 2 mg/mL MTX (Heng Rui Pharmaceutical, China) were
exposed to ultraviolet irradiation (UVB, 300 J/m2) for one hour in biosafety cabinet
(Thermo Fisher Scientific), and then cultured in RPIM-1640 medium for 18 hours.
The supernatants were collected for centrifugation: first 5 minutes at 500 × g, and
then 2 minutes at 14,000 × g to clear cell debris. The supernatants were then
centrifuged for 60 minutes at 14,000 × g to pellet MTX-MPs. The pellets were
washed and resuspended in saline (0.8~1.5 × 106/mL) for injection. The size, drug
concentration, and sterility of MTX-MPs were analyzed as described previously (18).
For clinical trials, the process was conducted according to the good manufacturing
practice (GMP) quality standard. For each preparation, equal amounts of MTX treated
the same number of tumor cells under the same conditions. This was done to maintain
the stability and reproducibility of MTX packaging MPs.
CT imaging of patient
Computed Tomography (CT) was carried out at day -1 (before PEM and DDP
treatment) and day 43 by DiscoveryTM
CT750 HD (General Electric Company, GE).
MPE volumes were analyzed through three-dimensional imaging by GE Advance
Workstation 4.5.
Tumor models
In the ascites model, H22 cells (3×105 cells were suspended in 200 μL PBS) were
injected into the peritoneal cavity. Three days later, the mice were i.p injected with
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

8
MTX-MPs (1×107) or neutrophils (1×10
6, bone marrow derived), and the control
group were i.p injected with PBS once per day for 5 days. Part of mice (n=5) were
sacrificed for analysis of ascites volume. The remaining mice (n=10) were used for
long-term survival analysis.
For the establishment of the MPE model, mice were anesthetized using isoflurane
before all procedures. LLC (1×105 cells suspended in 50 μL PBS) were injected into
the pleural cavity through the left tenth or eleventh intercrostal space at the
midaxillary line. The animals were observed until complete recovery. The procedure
was not associated with any mortality or morbidity.Three days later, the mice were
intrapleurally injected with MTX-MPs (5×106) or PBS (50 μL) once per day for 5
days. A portion of mice (n=5) were sacrificed for analysis of MPE volume. The
reamining mice (n=10) were used for long-term survival analysis.
For neutrophil depletion, mice were i.p injected with H22 cells, and three days later,
the mice were i.p injected with Ly-6G antibody (100 μg per mouse, twice a week,
#100763, Biolegend). IgG (#400565, Biolegend) was used as control.
BrdU (Bromodeoxyuridine) incorporation
BrdU (1mg/20g) was i.v injected to BALB/c mice, and 24 hours later, MTX-MPs
were i.p injected. 24 hours later, neutrophils were isolated (as described below) from
peritoneal cavity, peripheral blood (retro-orbital collection), and bone marrow
(harvested from tibias and femurs) and fixed with 4% polyformaldehyde (PFA). Cells
were then washed with HBSS, resuspended to 1×106/100 μL, and incubated with
0.5% Triton-X 100 (X100PC, Sigma-Aldrich) for 15 minutes at room temperature.
After washing with HBSS, cells were labeled with APC-conjugated BrdU (#364114,
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

9
Biolegend), then analyzed by flow cytometry (Canto II, BD), and the data were
analyzed by FlowJo (version 7.6.1).
Neutrophil isolation
For isolating human neutrophils from MPE and peripheral blood, the MPE or
peripheral blood was centrifuged, and the sediments were washed in Hank’s balanced
Salt Solution (HBSS) three times. Neutrophils were isolated by Ficoll Hypaque
solution (#LTS1092P, TBD) according to the manufacturers’ instructions. Mouse
neutrophils were isolated from mouse bone marrow by using Percoll (#17-0891-01,
GE) gradient density centrifugation.
Neutrophil negative magnetic sorting
Female wild-type BALB/c mice (6-8 weeks) were sacrificed, and tibias and femurs
were harvested. After lysis of RBCs, bone marrow neutrophils were sorted by
MojoSort™ mouse neutrophil isolation kit (#480058, Biolegend) according to the
manufacturer’s guidelines.
Neutrophil adoptive transfer
2×106 neutrophils were isolated from bone marrow of CD45.1 mice and injected to
CD45.2 mice via tail vein, followed by intrapleural injection of 1×107 MTX-MPs or
PBS. 18 hours later, the CD45.1 neutrophils in pleural cavity were analyzed by flow
cytometry.
Isolation of human monocytes
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

10
Human peripheral blood mononuclear cells (PBMCs) were isolated from human
peripheral blood using Ficoll density gradient separation. Monocytes were purified by
human CD14 Micro-Beads (#130-50-201, MACS), according to the manufacturer’s
guidelines (~98% were monocytes), and then cultured in complete RPMI 1640
medium containing recombinant human M-CSF (20 ng/mL; #300-25, PeproTech) for
the induction of macrophages. Seven days later, human macrophages were harvested
and stimulated with A549 cells derived MTX-MPs at a ratio 1:20 (cell:MP) for 2
hours, the using of cells and supernatant described below.
CD45 – cell isolation
Total cells were collected from MPE, washed with PBS three times, and CD45- cells
were purified using human CD45 Micro-Beads (#130-045-801, MACS) according to
the manufacturer’s guidelines (~98% were CD45-negative). Cytology examination by
H&E staining was performed as described below.
Flow cytometric analysis
For a phenotype analysis of cells, human cells were stained with surface antibodies:
CD3 (#300318), CD4 (#357404), CD8 (#980904), CD11b (#301308), CD15
(#125606), CD66b (#305116), CD68 (#333806), CD56 (#318304), CD45 (#368508),
CD44 (#338806), CD62p (#304904), CD62e (#330012), CD162 (#328806), CD62L
(#304810), EpCAM (#324204), CD54 (#353120), CD31 (#303106). Mouse cells were
stained with antibodies: Ly6G (#127606), NK1.1 (#108707), CD19 (#152403), F4/80
(#123127), CD3 (#100236), CD138 (#142505), PD-1 (#135214), CD45.1 (#110713),
CD45.2 (#109806), Ki67 (#151212), CD11b (#101255), IL12 (#505203) or CD31
(#102510).
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

11
For intracellular cytokine staining, lymphocytes prepared from mouse peritoneal
cavity using CD4/CD8 (TIL) MicroBeads (#130-117-114, MACS) according to
manufacturer’s guidelines. Cells were restimulated with phorbol 12-myristate
13-acetate (PMA; 20 ng/mL, #P1585, Sigma-Aldrich) and ionomycin (1μg/mL,
#I3909, Sigma-Aldrich) in vitro for 4 hours with monensin (1 μg/mL, #1445481,
Sigma-Aldrich), and then stained for surface CD3 and CD8. After surface staining,
cells were treated with Fix/Perm solution (#426803, Biolegend) and stained with
anti-IFNγ (#505808) and IL10 (#112706). All antibodies were purchased from
Biolegend, and flow cytometric was performed with BD Canto II.
Confocal microscopy
Neutrophils (2×106) isolated from MPE were cocultured with 1×10
5 CD44-labeled
A549 (described above) tumor cells on glass-bottom cell culture dishes (#801001,
NEST Biotechnology) for 2 hours, washed with HBSS. 100μL HBSS was added, and
cells were then incubated with Sytox green (5 nM; #425303, Biolegend)) for 30
minutes at temperature. Cells were visualized by two-photon fluorescent microscopy
(ZEISS 780). All groups were assessed with same threshold and parameters.
Neutrophil extracellular trap staining
1×106 neutrophils from healthy mouse bone marrow were cocultured with 1×10
7
Lewis derived MTX-MPs for 2 hours in the presence or absence of DPI (10μM,
#D2926, Sigma-Aldrich), and NETs were analyzed using Sytox green (#425303,
Biolegend) staining. For endothelial cell assays, 1×105 HUVEC were labeled with
CD31, and seeded on glass bottom cell culture dishes for 24 hours in RPIM-1640
medium with 10% FBS, and neutrophils from patient MPE after MTX-MP or saline
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

12
treatment were seeded with the HUVEC layer for 2 hours. The cells were then stained
with Sytox green and visualized by two-photon fluorescent microscopy as described
above.
Neutrophil chemotaxis
Neutrophils isolated from patient peripheral blood (5×105) were seeded in the upper
chamber of 24-well plate with a Millicell Hanging Cell Culture Insert. The lower
chamber was MPE double diluted by RPMI 1640 with or without CXCL1
(#MAB275-SP, R&D), CXCL2 (#ab89324, Abcam), GM-CSF (#502319, Biolegend)
or IL1β (#MAB601-SP, R&D) neutralization antibody. After one hour, cells from the
lower chamber were collected and counted by flow cytometry (Accuri C6, BD).
Real-time PCR
Total RNA extraction was prepared with TRIzol reagent (#15596026, Invitrogen), and
cDNA were generated by ReverTra Ace qPCR RT Kit (FSQ-101, Toyobo). Real-time
PCR analysis was performed with 2μg of cDNA as a template. A SYBR Green mix
(Applied Bioscience) and an Agilent Technologies Stratagene M-x3500 Real-time
PCR system were used. Relative quantification was performed using 2-ΔCt
. The
procedure was repeated in at last three biologically independent samples. The primer
sequences are shown as follows: Arginase-1, 5’-TCATCTGGG
TGGATGCTCACAC-3’ (sense) and 5’-GAGAATCCTGGCACATCGGGAA-3’
(antisense); MPO, 5’-GAGCAGGACAAATACCGCACCA-3’ (sense) and 5’-AGAG
AAGCCGTCCTCATACTCC-3’ (antisense); NOS2, 5’-GCTCTACACCTCCAATG
TGACC-3’ (sense) and 5’-CTGCCGAGATTTGAGCCTCATG-3’ (antisense); NOX2,
5’-CTCTGAACTTGGAGACAGGCAAA-3’ (sense) and
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

13
5’-CACAGCGTGATGACAACTCCAG-3’ (antisense); GAPDH,
5’-GTCTCCTCTGACTTCAACAGCG-3’ (sense) and 5’-ACCA
CCCTGTTGCTGTAGCCAA-3’ (antisense). Reduced glyceraldehyde-phosphate
dehydrogenase (GAPDH) was used for normalization.
Cytotoxicity assay
A549 cells were stained with carbox fluorescenceindiacetate succinimidyl ester
(CFSE; Sigma-Aldrich, #21888) and cocultured with neutrophils isolated from patient
peripheral blood or MPE (48 hours after MTX-MPs treatment) at a ratio of 1:20 for
16 hours, with or without N-acetylcysteine (NAC; 20 mM, #A0737, Sigma-Aldrich),
diphenylene iodonium (DPI; 10 μM, #D2926, Sigma-Aldrich), or Cl-amine (10μM,
#S8141, Selleck). CFSE-labeled cells were collected and stained with propidium
iodide (PI) and APC-Annexin V (#640932, Biolegend) to assess apoptosis by flow
cytometry (Canto II, BD) and analyzed by FlowJo 7.6.1.
Detection of hydrogen peroxide and ROS
Hydrogen peroxide (H2O2) in MPE patient was detected by a hydrogen peroxide
detection kit (#s0038, Beyotime biotechnology), and ROS in neutrophils was
measured using the CellROX probe (#C10422, Thermo Fisher Scientific).
Mitochondria-originated ROS was detected with the MitoSOX probe (#M36008,
Thermo Fisher Scientific) according to the manufacturers’ instructions. The cells were
then stained with Hochest (#94403, Sigma-Aldrich) for one hour at room temperature
and visualized by two-photon fluorescent microscopy, as described above.
Evans blue leakage
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

14
1×105 H22 tumor cells were i.p. injected into C57BL/6 mice, and 3 days later, the
mice were i.p injected with 5×106 MTX-MPs, Cl-amidine (1 μg/g), or
MTX-MPs/Cl-amidine (1 μg/g) daily for three days. Normal saline was used as a
control. Twenty-four hours after the last treatment, mice were injected with 1% Evans
blue (5 mg/kg, #E2129, Sigma-Aldrich) via tail vein injection. One hour after the
Evans blue injection, the mice were sacrificed, and 2 mL PBS was used to flush the
peritoneal cavity. The flushed fluid was collected and the supernatant was quantified
spectrophotometrically by microplate reader (Biotek) according to standard curve.
Western blot assay
Protein from MPE patient neutrophils was extracted, the protein concentrations were
determined by BCA kit (#23235, Thermo Fisher Scientific). Then the protein (20 μg)
was run on an SDS-PAGE and transferred to nitrocellulose membranes.
Nitrocellulose membranes were blocked in 5% bovine serum albumin (BSA) and probed
with anti-human arginase 1 (1:1,000 dilution, Cell Signaling Technology, #79404),
anti-human MPO (1:1,000 dilution, Cell Signaling Technology, #79623), anti-human
NOX2 (1:1000 dilution, Cell Signaling Technology, #4312S), iNOS (1:1,000 dilution,
Cell Signaling Technology, #39898) or anti-human β-actin antibodies (1:1,000
dilution, Cell Signaling Technology, #4967) overnight at 4℃, followed by a second
horseradish peroxidase-coupled antibody incubation at room temperature for 1 hour.
Blots were visualized by enhanced chemiluminescence according to the
manufacturer’s instructions (ECL kit, Pierce).
PKH26 labeling
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

15
MPs were suspended in diluent C solution, and incubated with PKH26 (MINI26,
Sigma-Aldrich) for 30 minutes at room temperature followed by quenching with an
equal volume of FBS (Gibco) and washing twice with PBS.
Cellular uptake assay
To investigate the cellular internalization of MPs, we carried out uptake assays using
cells from MPE patients as recipient cells. Briefly, T cells, B cells, macrophages,
neutrophils, and tumor cells in MPE were cocultured with PKH26-labeled MPs for 30
minutes or 2 hours. Cells were then washed with PBS, and analyzed by flow
cytometry. For in vivo uptake assay, PKH26-labeled MPs were intrapleural or i.p
injected, and 2 hours later, the cells were collected, and uptake of MP was analyzed
by flow cytometry.
Cytokine detection assay
Human macrophages were harvested and stimulated with A549 cell-derived
MTX-MPs at a ratio of 1:20 (cell:MP) for 2 hours. The supernatant wascentrifuged at
14, 000 × g for 30 minutes to remove MTX-MPs, and then 50 μL supernatant was
used for ELISAs.
MPE was collected before and 2, 4, 8, 24, and 48 hours after MTX-MPs or saline
treatment. Supernatants were centrifuged at 3000 × g for 8 minutes, then 50 μL was
used for ELISA analysis. CXCL1 and CXCL2 concentrations were assessed using a
human GRO-alpha/MGSA (CXCL1) Mini ELISA kit (#900-M38, PeproTech) and
human GRO-beta (CXCL2) ELISA kit (#900-M120, PeproTech) according to
manufacturer’s instructions.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

16
H&E staining
Neutrophils were collected and fixed in 4% paraformaldehyde (#158127, Sigma-
Aldrich) at room temperature for 15 minutes. 1×105 cells were smeared on glass slide
and dried at 50℃. Hematoxylin staining for one minute and eosin staining for 10
seconds was performed, and samples were analyzed by microscope (Leica, DMi8) at
200× and 400× magnification.
Electron microscopy
Neutrophils were collected and fixed in 4% glutaric dialdehyde solution (#G7651,
Sigma-Aldrich) at room temperature for 2 hours. The pellets were then dehydrated in
a graded ethanol series, treated with propylene oxide, and embedded with Spurr’s
epoxy resin. cut sections were stained with uranyl acetate and lead citrate, and then
imaged using JEM1010 electron microscope (JEOL).
For scanning electron microscopy assay, 1×106 neutrophils were collected from MPE,
and fixed with 4% glutaric dialdehyde solution at room temperature for 2 hours. MPE
was then incubated with 1% osmium tetroxide and dehydrated with an ascending
ethanol series. After critical-point drying, the samples were coated with gold and
analyzed by S4800 scanning electron microscopy (Hitachi).
Endothelial permeability detection
1×105 HUVECs were seeded in the upper chamber of 24-well plate with a Millicell
Hanging Cell Culture Insert (pore size 0.4 μm). 5×105 neutrophils isolated from
patient MPE in saline- or MTX-MP-treated groups after were seeded on the HUVEC
layer for 2 hours in the presence or absence of 10 μM Cl-amidine (CLAM). 100 μL
FITC-dextran (1mg/ml,#FD40, Sigma-Aldrich) was then added into the upper
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

17
chamber. One hour later, FITC-dextran in lower chamber was detected by Microplate
System (Biotek).
Immunofluorescence imaging
1×107 MTX-MPs or PBS were i.p injected to MPE mice for 18 hours, Sytox green
(1:1000 diluted by PBS, 200μL) was injected through tail vein for 2 hours. Mice were,
sacrificed, and frozen sections of pleural vessel were stained with PE-anti CD31
(#102407, Biolegend) and analyzed by fluorescence microscope (Leica).
Endothelium-neutrophil contact detection
2×105 HUVEC were seeded in 24-well culture plate (Corning) for 48 hours, then
1×106 neutrophils were collected from MPE and seeded on HUVEC layer for 24
hours in the presence or absence of 1×107 MTX-MPs. Endothelium-neutrophil contact
was observed by phase contrast microscope after washing.
Quantification and statistical analysis
All experiments were performed at least three times. Results are expressed as mean ±
SEM and were analyzed by Student’s t-test. The survival rates were determined by
Kaplan-Meier survival analysis. The p value < 0.05 was considered statistically
significant. The analysis was conducted using the Graph pad 8.0 software. Sample
exclusion was never carried out.
Results
MTX-MPs efficiently treat MPE, which correlates with neutrophil recruitment
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

18
To assess the treatment efficacy of a pleural injection of MTX-MPs, newly diagnosed
NSCLC patients with MPE were recruited and received routine systemic
chemotherapy in advance. A schematic of the clinical treatment procedure was briefly
depicted in Fig.1A. Because drug-free T-MPs can promote M2 tumor-associated
macrophage development (14,19), we used saline instead of drug-free T-MPs as the
control. MTX-MPs were characterized by multiple aspects, including size, plasma
membrane origin, mitochondrial and genomic DNA fragments, drug concentration,
stability and sterility (Supplementary Fig. S1-2), which was consistent with previous
reports (15). The amelioration of the color and turbidity of malignant fluids was
observed following the initial treatment (Supplementary Fig. S3). In line with this
observation, CD45– tumor cells, which were not mesothelial cells (Supplementary Fig.
S4), were efficiently removed from the MPE in the MTX-MPs treated patients,
whereas abundant CD45+ immune cells were present in the fluids (Fig. 1B and C).
However, in the saline-treated patients, both CD45– and CD45
+ cells were not altered,
but CD45+ cell numbers slightly decreased after saline treatment (Fig. 1D and E).
Four weeks after treatment, analysis of pleural effusions showed that MTX-MP
treatment resulted in a significant decrease of MPE compared to the saline treatment
(Fig. 1F). Given the presence of overabundant immune cells in the MPE after
MTX-MP treatment, we asked which immune cell type(s) were mainly present. The
flow cytometric analysis showed that the number of CD4+ and CD8
+ T cells was
increased, but the number of CD56+ NK cells, CD68
+ macrophages, and
CD11b+CD33
+CD14
– myeloid-derived suppressor cells (MDSCs) was not altered (Fig.
1G). Robust CD11b+CD15b
+ neutrophils were collected in the effusions following the
MTX-MP treatment (Fig. 1H and I). Functionally, CD11b+CD15b
+ neutrophils did
not affect T-cell proliferation, whereas CD11b+CD33
+CD14
- MDSCs inhibited T-cell
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

19
proliferation (Supplementary Fig. S5). 48 hours after the initial MTX-MP treatment,
the neutrophil number showed a correlation with the reduction of MPE in the lung
cancer patients (Fig. 1J), Together, these results suggested that MTX-MPs efficiently
treat MPE, which correlated with CD11b+CD15
+ neutrophil recruitment.
Neutrophil recruitment enhances MTX-MP treatment efficiency
The above treatment efficacy was likely due to direct killing of tumor cells, consistent
with our previous report (18). However, recruiting numerous neutrophils to the MPE
raised a possible role of neutrophils against MPE. We thus tested this using H22
hepatocellular carcinoma-induced ascites in BALB/c mice to mimic a malignant
effusion. Mice were i.p. injected with tumor cells, followed by the intraperitoneal
injection of MTX-MPs. We found that a large number of neutrophils were present in
the ascites (Fig. 2A). However, we did not find alteration of T cells, B cells, NK cells,
and macrophages (Supplementary Fig. S6). 20% of macrophages but not T cells, B
cells, NK cells, or neutrophils underwent apoptosis following MTX-MP treatment
(Supplementary Fig. S6), which might be due to a high uptake of MTX-MPs by
macrophages. BrdU was incorporated into proliferating myeloid progenitors in the
bone marrow that subsequently differentiated into neutrophils (Fig. 2B). These
recruited neutrophils showed low Ki67 staining (Fig. 2C), suggesting that
MTX-MP-recruited neutrophils lost their proliferating capability. We also found that
the recruited neutrophils were not MDSCs through H&E staining (Fig. 2D). Also, the
recruited neutrophils did not suppress CD8+
T-cell proliferation and did not affect the
expression of IFNγ,IL10, and PD-1 in the T cells (Supplementary Fig. S7). Using a
Ly6G-depleting antibody to deplete neutrophils, we found that the therapeutic effect
of MTX-MPs was abrogated, as demonstrated by that the increased volume of ascites
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

20
and decreased survival (Fig. 2E). We isolated neutrophils from healthy mouse bone
marrow and i.p. injected them to the H22 ascites in mice. The ascites volume was
50% reduced and long-term survival was prolonged (Fig. 2F). In line with the Ficoll
isolation method, neutrophils isolated with negative magnetic sorting also showed
antitumor effects (Supplementary Fig. S8). The i.p. injection of MTX-MPs did not
affect the frequency of neutrophils in peripheral blood and bone marrow
(Supplementary Fig. S9). This anti-ascites effect of neutrophils was T
cell-independent, because similar results were also obtained in nude mice (Fig. 2G).
Consistently, MTX-MP treatment also showed antitumor effects in nude mice
(Supplementary Fig. S10). Using a LLC induced MPE, we further demonstrated that
neutrophil depletion impaired the effect of MTX-MPs on the long-term survival of the
mice (Fig. 2H). Intravenous injection of CD45.1+
neutrophils to CD45.2 mice showed
that MTX-MP treatment attracted neutrophils to the pleural effusion (Supplementary
Fig. S11). Together, these results suggested that neutrophil recruitment enhanced
MTX-MP treatment efficacy.
MTX-MPs induce chemokines for neutrophil recruitment
Next, we investigated how neutrophils were attracted to the MPE. We isolated the
cells from the MPE of patients and incubated them with MTX-MPs. We found that
MTX-MPs could be taken up by CD68+ macrophages, CD11b
+CD15
+ neutrophils and
CD45– tumor cells (Fig. 3A). Macrophages showed the strongest fluorescent intensity
(Fig. 3A). These macrophages rather than the neutrophils or tumor cells could take up
the MPs within 30 minutes, as demonstrated by the increased MFI of PKH26 (Fig.
3B). Using a LLC-induced MPE or H22-induced ascites model, a consistent uptake by
macrophages was observed (Supplementary Fig. S12). We then asked if the cells
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

21
following MTX-MP uptake produced neutrophil chemoattractant(s). A trans-well
assay showed that only the supernatants from a two-hour co-incubation of MTX-MPs
with patient MPE macrophages could recruit (Fig. 3C). A 2-hour incubation was
based on the observation that the number and proportion of neutrophils in MPEs
increased 2 hours after MTX-MP injection (Fig. 3D). GM-CSF and IL-1β are known
chemoattractants of neutrophils (20,21). However, the addition of GM-CSF- or
IL-1β-neutralizing antibody did not affect the above supernatant-mediated attraction
of neutrophils (Fig. 3E). Other CXCL chemokines including CXCLs1-3 and
CXCLs5-8 also attract neutrophils (22, 23). CXCL1 and CXCL2 were upregulated in
MTX-MP-treated macrophages (Fig. 3F) and were detected in the supernatants of the
two-hour co-incubation (Fig. 3G). In line with these results, clinical MPE samples
with a high neutrophil infiltration (n=6) also showed increased CXCL1 and CXCL2
two hours after MTX-MP injection (Fig. 3H and I). CXCL1 and CXCL2 were not
detected in the macrophages in the MPE before MTX-MP injection but were induced
2 hours after MTX-MP treatment (Fig. 3J). CXCL1 or CXCL2 neutralization
abrogated the attraction of neutrophils to the lower chamber in the above trans-well
assay (Fig. 3K). Despite the chemokine-mediated effect, recruiting neutrophils also
need endothelial activation, which provides binding molecules for the rolling,
tethering and arrest of neutrophils to the endothelium (23,24). We found that
MTX-MPs not only upregulated CD62e and CD62p in the human vein endothelial
cells (Fig. 3L), but also upregulated P-selectin glycoprotein ligand 1 (PSGL1) in
neutrophils (Fig. 3M). In line with this result, the promotion of neutrophil-endothelial
cell contact by MTX-MPs was observed in H22 ascites (Supplementary Fig. S13).
Also, MTX-MPs promoted the tight contact of patient MPE-derived neutrophils with
endothelial cells in vitro (Fig. 3N). These results suggest that MTX-MPs treatment not
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

22
only induced macrophages in the MPE to release CXCL1 and CXCL2 but also
activated endothelial cells, allowing for neutrophil recruitment.
Attracted neutrophils possess antitumor properties in the MPE of patients
Neutrophils can have a N1 or N2 phenotype to exert an antitumor or protumor effect
(25-27). To investigate this, we analyzed the neutrophils in patients’ MPE after
MTX-MP treatment. We found that the forward scatter (FSC) of neutrophils was
reduced after MTX-MP treatment (Fig. 4A) but was not altered in the saline-treated
patients (Fig. 4B). Lower FSC phenotype may reflect an antitumor property of
neutrophils (28). In addition to the low FSC, the activated phenotype
(CD66b+CD62L
low or CD54
+CD62L
low) might also relate to the antitumor property of
neutrophils (29). We found that neutrophils in the MTX-MP-treated MPE upregulated
the expression of CD11b, CD66b and CD54 but downregulated the expression of
CD15 compared to the cells before MTX-MP treatment (Fig. 4C). However,
neutrophils in the saline group did not show the phenotype alteration (Fig. 4D). In line
with the surface markers, oxidative enzymes NADPH oxidase 2 (NOX2),
myeloperoxidase (MPO), and inducible nitric oxide synthase (NOS2) were
upregulated but arginase 1 was downregulated after MTX-MP treatment (Fig. 4E).
Morphologically, a more vacuolated structure and degranulation in MTX-MP-treated
neutrophils were observed under transmission electron microscope (TEM) (Fig. 4F),
and more cytoplasmic azurophilic granules and hypersegmented nuclei were observed
(Fig. 4G and H), which are a signature for lysosome activation (28), further
suggesting a bias toward an antitumor phenotype (24, 29). Using MTX-MPs to treat
neutrophils isolated from the MPE, we found that the surface markers CD11b, CD66b,
and CD54 and the enzymes iNOS, NOX2, and MPO were upregulated but CD15 and
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

23
arginase 1 were downregulated (Fig. 4I and J). Supernatants from the
MTX-MP-treated A549 cells could stimulate neutrophils to upregulate CD11b,
CD66b, CD54, iNOS, NOX2, and MPO but to downregulate CD15 and arginase 1
(Fig. 4K and L). Together, the injection of MTX-MP not only recruited neutrophils to
the MPE of patients but also conferred antitumor properties.
Attracted neutrophils are cytotoxic to tumor cells by utilizing ROS and NETs
Next, we investigated the antitumor role of attracted neutrophils. We isolated CD45–
tumor cells and neutrophils from the MPE before MTX-MP treatment. We also
isolated neutrophils from the MPE after the treatment in the same patient. Then, we
co-incubated the isolated neutrophils and tumor cells, respectively, and found that
only neutrophils from the treatment setting were able to kill tumor cells (Fig. 5A). We
further found that such neutrophils also eliminated A549 cancer cells in vitro (Fig.
5B). We observed that the tumor cells were surrounded by neutrophils (Fig. 5C),
suggesting that the neutrophil-mediated killing of tumor cells may be in a cell-cell
contact manner (28). Such cell-cell contact was also observed in the MTX-MP-treated
MPE in patients, but not from the saline-treated MPE (Fig. 5D). ROS is a mechanism
neutrophils use to kill tumor cells. In line with the upregulation of iNOS, NOX2, and
MPO, ROS expression in neutrophils was elevated in the MPE of patients treated with
MTX-MPs, but not in the MPE of the saline group (Fig. 5E). We also found that the
H2O2 concentration in the MTX-MP-treated MPE of patients was elevated
(Supplementary Fig. S14). Both the mitochondria and lysosomes are the main
organelles that generate ROS in a cell. However, we only detected minor ROS in
mitochondria of the MTX-MP-treated neutrophils by fluorescent microscopy and flow
cytometry (Fig. 5F), suggesting that the ROS was mainly produced from the
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

24
lysosomes. Consistently, the use of ROS scavenger N-acetylcysteine (NAC) or NOX2
inhibitor diphenylene iodonium (DPI) could lower the ROS levels (Supplementary
Fig. S15) and also inhibited the killing of tumor cells by neutrophils isolated from
clinical MPE samples (Fig. 5G). We found that lysosomal biogenesis was enhanced in
MTX-MP-treated neutrophils (Supplementary Fig. S16).
Besides ROS, neutrophils also use neutrophil extracellular traps (NETs) to induce
tumor cell NETosis. This NET formation is regulated by ROS, especially from
MPO-processed ROS (30), which, however, relies on the NOX2 system-derived H2O2
(31, 32). Using an H22 ascites model, we stained the MTX-MP-treated neutrophils
with Sytox green, a DNA binding dye, which showed presence of extracellular traps,
and 35.8% of neutrophils released NETs (Supplementary Fig. S17). As expected, the
blockade of ROS generation resulted in the inhibition of the NET formation in
MTX-MP-treated murine neutrophils (Supplementary Fig. S18). We also found NETs
surrounding tumor cells in the MTX-MP-treated MPE of patients but not in saline
group (Fig. 5H), which was also confirmed by scanning electron microscopy (SEM)
(Fig. 5I), suggesting that NETs might be involved in the killing of tumor cells. Indeed,
the inhibition of NETs by Cl-amidine inhibited the killing of A549 tumor cells by the
MTX-MP-recruited neutrophils in vitro (Fig. 5J). Together, these results suggest that
neutrophils may use ROS and NETs to kill tumor cells in the MPE of patients
following MTX-MP treatment.
NETs prevent vascular leakage by sealing off the damaged endothelium
The formation of MPE is due to the damage of pleural capillaries caused by tumor
invasion and soluble factors, which leads to excessive plasma leakage through
hyper-permeable pleural vasculature networks (33). Histological analysis of the
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

25
mouse MPE model showed that some vascular endothelial cells from the pleural
vasculature underwent apoptosis, and the structure of endothelium was not integrative
(Fig. 6A). Regarding filamentous net-like structure and the stickiness of NETs, we
further hypothesized that besides the killing of tumor cells, NETs had a repairing
effect on the vascular leakage in pleural cavity. To test this hypothesis, we seeded
human endothelial cells in the upper chamber of transwells, and MTX-MP- or
saline-treated neutrophils were placed on an endothelial cell layer. We found that
saline-treated neutrophils could not prevent FITC-Dextran (molecular 40, 000) from
entering the bottom chamber by crossing the endothelial layer (Fig. 6B). However,
MTX-MP-treated neutrophils effectively prevented this process (Fig. 6C), which was
abrogated by Cl-amidine (Fig. 6D). Using fluorescence staining, we found that NETs
intertwined with the membrane of endothelial cells in the MTX-MP-treated neutrophil
group but not in the saline control group (Fig. 6E). In the MPE mouse model, we also
found that Evans blue i.v. injected could be detected in the MPE of the saline-treated
mice, but very little detected in the MTX-MP-treated mice (Fig. 6F). Similarly, the
administration of NET inhibitors increased the vascular permeability and allowed
Evans blue to enter the pleural cavity (Fig. 6G). In line with these results, the frozen
section analysis showed that neutrophils anchored to blood vessels and abundant NET
were located between the endothelial gap (Fig. 6H). We further evaluated the
therapeutic effect of the NETs on MPE by treating the MPE mice with NET inhibitors
instead of neutrophil depletion. Under this condition, we found that the therapeutic
effect of MTX-MPs on pleural effusions was also inhibited (Fig. 6I) and the mice
survival was reduced (fig. 6J). Together, these results suggest that MTX-MP-recruited
neutrophils may release NETs to seal off the damaged endothelium, thus inhibiting
plasma leakage.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

26
Discussion
A way to effectively mobilize endogenous neutrophils and promote their intrinsic
antitumor activities as an immunotherapeutic approach is not available. In this study,
we showed that tumor cell-derived MPs packaging MTX mobilize neutrophils to the
MPE of NSCLC patients, where the neutrophils display an antitumor phenotype, not
only exerting a tumor cell-killing effect but also releasing NETs to seal off the
damaged endothelium, leading to the effective treatment of MPE with low adverse
effects. During the treatment process, only some patients developed a fever and did
not exhibit other symptoms, consistent with our previous reports (18).
Many factors contribute to the chemoattraction of neutrophils to inflammatory sites
(20-22,34). In this study, we found that CXCL1 and CXCL2, released by
MTX-MP-stimulated macrophages, played a role in the attraction of neutrophils to the
MPE. Macrophages are commonly polarized to tumor-associated M2 macrophages
with anti-inflammatory properties in MPEs. It is unclear how MTX-MP treatment
switches the M2 phenotype to a pro-inflammatory M1 with the release of CXCL1 and
CXCL2 for neutrophil recruitment. However, our previous studies have shown that
drug-packaging tumor cell-derived MPs are able to reset tumor-associated
macrophages towards the M1 phenotype (17). Notably, drug-free tumor cell-derived
MPs promote M2 tumor-associated macrophage development (14). The key point lies
in the very low amount of chemotherapeutic drug in the MPs. Such little drug may not
exert a cytotoxic effect but act as a lysosomal regulator because MPs enter lysosomes
following their uptake. How drug-packaging MPs regulate macrophage M1 phenotype
is under investigation.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

27
In addition to recruitment, the effect of MTX-MPs also confers neutrophils antitumor
properties, which seems not to be mediated by MTX-MP-triggered CXCL1 and
CXCL2 (35). MTX-MPs can exert an indirect effect on neutrophil activation through
the macrophage pathway. Macrophages upon taking up MTX-MPs may release
soluble factors, thus inducing neutrophil polarization towards a N1 phenotype. These
MTX-MP-triggered neutrophils are not terminally differentiated but are immature
cells, allowing BrdU incorporation. Although we propose that these immature
neutrophils are mobilized from the bone marrow by MTX-MPs, an alternative
possibility is that MTX-MPs induce the differentiation of MDSCs to become
neutrophils with the ability to proliferate. In this regard, whether MTX-MPs induce
MDSC differentiation to become neutrophils is worthy of investigation.
We found in this study that MTX-MP-recruited neutrophils released NETs in the
MPE. NETs comprise a web of fibers composed of chromatin and serine proteases
that trap and kill microbes extracellularly (36) and also serve as a physical barrier,
preventing the further spread of pathogens. Besides the antimicrobial properties,
NETs may have pathological effects on organ injury such as acute lung injury (37,38).
Studies have also shown a proposed role for NETs in cancer (39). In preclinical
models, NETs show a tumor-promoting effect, including facilitating metastasis.
However, in this study we found that NETs have a tumor-inhibiting effect. NETs may
mobilize their DNA fiber, histone structure proteins and the released proteases to
exert this antitumor effect, similar to their bactericidal process. In the MPE of NSCLC
patients, NETs were found to surround tumor cells, which may prevent tumor cells
from migrating and benefit the killing of tumor cells by nearby neutrophils.
Besides the inhibitory effect on tumor cells, NETs are also able to interfere with the
vascular leakage, leading to the effective treatment of malignant fluids. The primary
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

28
cause of MPE lies in the loss of endothelial integrity such as tight junction alteration
and endothelial cell apoptosis. However, MTX-MP treatment may enhance the
interaction of endothelial cells and neutrophils by upregulating the expression of
endothelial E-selectin and P-selectin. Thus, the anchored neutrophils may release and
allow NETs to seal off the damaged endothelium. An important issue about NETs is
the manner of how MTX-MPs trigger neutrophils to release NETs in the MPE of
NSCLC patients. MTX-MPs may stimulate macrophages to produce CXCL1 and
CXCL2. These two chemokines not only attract neutrophils but also facilitate
neutrophils to release NETs.
Malignant pleural effusion poses a significant clinical problem with a poor treatment
efficacy. However, based on the present findings and our previous studies (15,17,18),
we propose that drug-packaging MPs may represent a unique approach, which can
efficiently treat MPEs in NSCLC patients through the processes, as shown in Fig. 7.
All in all, our data showed that drug-packaging MPs, by virtue of their ability to
recruit neutrophils, lead to a robust antitumor innate immunity. These findings
provide insights into the versatile antitumor function of neutrophils, especially in the
control of malignant fluids.
Acknowledgments
This work was supported by National Natural Science Foundation of China
(81788101 , 81530080, 91742112), CAMS Initiative for Innovative Medicine
(2016-I2M-1-007), Young Elite Scientists Sponsorship Program by CAST (YESS20
160166), Program for HUST Academic Frontier Youth Team (2018QYTD01),
National Major Science and Technology Projects of China (2019ZX09301001).
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

29
Author Contributions
B.H. conceived the project. K.T., P.X., J.W., H.Z., D.W., L.Z., J.C., K.W., J. L., H.F.,
Y.Z., J.X. and Y.L. performed the experiments. B.H., P.X., K.T., H.Z. and J.M.
developed methodology. B.H., K.T. and P.X. performed data analysis, provided
administrative, technical, or material support. B.H. and K.T. wrote the manuscript with
input from all authors.
Declaration of Interests
U.S. Patent No. 9,351,931 and China Patent No. ZL201110241369.8 held by Hubei
Soundny Bio-Tech Co. Ltd. cover the pharmaceutical preparation for “Tumor
cell-derived microparticles packaging of chemotherapeutic drugs”. All authors declare
that they have no competing interests.
Reference
1. Dancey JT, Deubelbeiss KA, Harker LA, Finch CA. Neutrophil kinetics in man. J
Clin Invest. 1976;58(3):705-15.
2. Starnes CO. Coley's toxins in perspective. Nature. 1992;357(6373):11-2.
3. Herr HW, Morales A. History of bacillus Calmette-Guerin and bladder cancer: an
immunotherapy success story. J Urol. 2008;179(1):53-6.
4. Powell DR, Huttenlocher A. Neutrophils in the Tumor Microenvironment. Trends
Immunol. 2016;37(1):41-52.
5. Gregory AD, Houghton AM. Tumor-associated neutrophils: new targets for
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

30
cancer therapy. Cancer Res. 2011;71(7):2411-6.
6. Amulic B, Cazalet C, Hayes GL, Metzler KD, Zychlinsky A. Neutrophil function:
from mechanisms to disease. Annu Rev Immunol. 2012;30:459-89.
7. Stathopoulos GT, Kalomenidis I. Malignant pleural effusion: tumor-host
interactions unleashed. Am J Respir Crit Care Med. 2012;186(6):487-92.
8. Davies HE, Lee YC. Management of malignant pleural effusions: questions that
need answers. Curr Opin Pulm Med. 2013;19(4):374–379.
9. Porcel JM, Gasol A, Bielsa S, Civit C, Light RW, Salud A. Clinical features and
survival of lung cancer patients with pleural effusions. Respirology.
2015;20(4):654-9.
10. Antony VB, Loddenkemper R, Astoul P, Boutin C, Goldstraw P, Hott J, et al.
Management of malignant pleural effusions. Eur Respir J. 2001;18(2):402-19.
11. D'Souza-Schorey C, Clancy JW. Tumor-derived microvesicles: shedding light on
novel microenvironment modulators and prospective cancer biomarkers. Genes
Dev. 2012;26(12):1287-99.
12. Zhang H, Tang K, Zhang Y, Ma R, Ma J, Li Y, et al. Cell-free tumor microparticle
vaccines stimulate dendritic cells via cGAS/STING signaling. Cancer Immunol
Res. 2015;3(2):196-205.
13. Ma J, Wei K, Zhang H, Tang K, Li F, Zhang T, et al. Mechanisms underlying
presentation of tumor microparticle antigens to CD8+ T cells by dendritic cells.
Cancer Immunol Res. 2018;6:1057-68.
14. Ma R, Ji T, Chen D, Dong W, Zhang H, Yin X, et al. Tumor cell-derived
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

31
microparticles polarize M2 tumor-associated macrophages for tumor progression.
Oncoimmunology. 2016;5(4):e1118599.
15. Tang K, Zhang Y, Zhang H, Xu P, Liu J, Ma J, et al. Delivery of
chemotherapeutic drugs in tumour cell-derived microparticles. Nat Commun.
2012;3:1282.
16. Ran L, Tan X, Li Y, Zhang H, Ma R, Ji T, et al. Delivery of oncolytic adenovirus
into the nucleus of tumorigenic cells by tumor microparticles for virotherapy.
Biomaterials. 2016;89:56-66.
17. Sun Y, Zheng Z, Zhang H, Yu Y, Ma J, Tang K, et al. Chemotherapeutic tumor
microparticles combining low dose irradiation reprogram tumor-promoting
macrophages through a tumor-repopulating cell-curtailing pathway.
Oncoimmunology. 2017;6(6):e1309487.
18. Ma J, Zhang Y, Tang K, Zhang H, Yin X, Li Y, et al. Reversing drug resistance of
soft tumor-repopulating cells by tumor cell-derived chemotherapeutic
microparticles. Cell Res. 2016;26(6):713-27.
19. Zhang H, Yu Y, Zhou L, Ma J, Tang K, Xu P, et al. Circulating tumor
microparticles promote lung metastasis by reprogramming inflammatory and
mechanical niches via a macrophage-dependent pathway. Cancer Immunol Res.
2018;6:1046-56.
20. Gomez-Cambronero J, Horn J, Paul CC, Baumann MA. Granulocyte-macrophage
colony-stimulating factor is a chemoattractant cytokine for human neutrophils:
involvement of the ribosomal p70 S6 kinase signaling pathway. J Immunol.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

32
2003;171(12):6846-55.
21. Mitroulis I, Kambas K, Ritis K. Neutrophils, IL-1β, and gout: is there a link?
Semin Immunopathol. 2013;35(4):501-12.
22. Kolaczkowska E, Kubes P. Neutrophil recruitment and function in health and
inflammation. Nat Rev Immunol. 2013;13(3):159-75.
23. de Oliveira S, Rosowski EE, Huttenlocher A. Neutrophil migration in infection
and wound repair: going forward in reverse. Nat Rev Immunol.
2016;16(6):378-91.
24. Mayadas TN, Cullere X, Lowell CA. The multifaceted functions of neutrophils.
Annu Rev Pathol. 2014;9:181-218.
25. Fridlender ZG, Sun J, Kim S, Kapoor V, Cheng G, Ling L, et al. Polarization of
tumor-associated neutrophil phenotype by TGF-beta: "N1" versus "N2" TAN.
Cancer Cell. 2009;16(3):183-94.
26. Li YW, Qiu SJ, Fan J, Zhou J, Gao Q, Xiao YS, et al. Intratumoral neutrophils: a
poor prognostic factor for hepatocellular carcinoma following resection. J
Hepatol. 2011;54(3):497-505.
27. Mantovani A, Cassatella MA, Costantini C, Jaillon S. Neutrophils in the
activation and regulation of innate and adaptive immunity. Nat Rev Immunol.
2011;11(8):519-31.
28. Sagiv JY, Michaeli J, Assi S, Mishalian I, Kisos H, Levy L, et al. Phenotypic
diversity and plasticity in circulating neutrophil subpopulations in cancer. Cell
Rep. 2015;10(4):562-73.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

33
29. Eruslanov EB, Bhojnagarwala PS, Quatromoni JG, Stephen TL, Ranganathan A,
Deshpande C, et al. Tumor-associated neutrophils stimulate T cell responses in
early-stage human lung cancer. J Clin Invest. 2014;124(12):5466-80.
30. Souto JC, Vila L, Brú A. Polymorphonuclear neutrophils and cancer: intense and
sustained neutrophilia as a treatment against solid tumors. Med Res Rev.
2011;31(3):311-63.
31. Fuchs TA, Abed U, Goosmann C, Hurwitz R, Schulze I, Wahn V, et al. Novel cell
death program leads to neutrophil extracellular traps. J Cell Biol.
2007;176(2):231-41.
32. Wang Y, Li M, Stadler S, Correll S, Li P, Wang D, et al. Histone
hypercitrullination mediates chromatin decondensation and neutrophil
extracellular trap formation. J Cell Biol. 2009;184(2):205-13.
33. Yano S, Shinohara H, Herbst RS, Kuniyasu H, Bucana CD, Ellis LM, et al.
Production of experimental malignant pleural effusions is dependent on invasion
of the pleura and expression of vascular endothelial growth factor/vascular
permeability factor by human lung cancer cells. Am J Pathol.
2000;157(6):1893-903.
34. Sesma JI, Kreda SM, Steinckwich-Besancon N, Dang H, García-Mata R, Harden
TK, et al. The UDP-sugar-sensing P2Y(14) receptor promotes Rho-mediated
signaling and chemotaxis in human neutrophils. Am J Physiol Cell Physiol.
2012;303(5):C490-8.
35. De Filippo K, Dudeck A, Hasenberg M, Nye E, van Rooijen N, Hartmann K, et al.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

34
Mast cell and macrophage chemokines CXCL1/CXCL2 control the early stage of
neutrophil recruitment during tissue inflammation. Blood. 2013;121:4930-7.
36. Brinkmann V, Reichard U, Goosmann C, Fauler B, Uhlemann Y, Weiss DS, et al.
Neutrophil extracellular traps kill bacteria. Science. 2004;303(5663):1532-5.
37. Huang H, Tohme S, Al-Khafaji AB, et al. Damage-associated molecular
pattern-activated neutrophil extracellular trap exacerbates sterile inflammatory
liver injury. Hepatology. 2015;62:600–614.
38. Liu S, Su X, Pan P, et al. Neutrophil extracellular traps are indirectly triggered by
lipopolysaccharide and contribute to acute lung injury. Sci Rep. 2016;6:37252.
39. Albrengues J, Shields MA, Ng D, Park CG, Ambrico A, Poindexter ME, et al.
Neutrophil extracellular traps produced during inflammation awaken dormant
cancer cells in mice. Science 2018;361(6409).
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

35
Figure legends
Figure 1. MTX-MPs treat MPE and is coordinated with neutrophil recruitment.
(A) Graphical outline of the treatment protocol. MPE patients received intravenous
injection (i.v.) of PEM (500 mg/m2) and DDP (75 mg/m
2) on day 1 (blue
arrow) ,followed by intrapleural treatment with MTX-MPs or saline on days 5, 7, 9,
11, 13 and 15 (red arrow). ; CT images were performed at day –1 and 43 (purple
arrow). (B-E) Cells were collected from the MPE of (B,C) MTX-MP-treated or (D,E)
saline-treated patients on day 5 and 7 and analyzed by flow cytometry (n=16/group).
(F) Left top: CT image thorax of control and treated patients with MPE on day -1 and
day 43 (see purple arrows in A). The white arrows indicate pleural effusion. Left
bottom: Pleural effusion assessment of the same patients by CT analysis. Right: MPE
volume ratio (volume on day 43/volume on day -1) was analyzed (n=32/group). (G-I)
MPE samples (n=16) were analyzed by flow cytometry on day 5 and 7 to assess (G,H)
numbers of CD3+CD4
+ T cells, CD3
+CD8
+ T cells, CD16
+CD56
+ NK cells,
CD11b+CD68
+ macrophages, CD11b
+CD14
–CD33
+ MDSCs, CD11b
+CD15
+CD49d
–
neutrophils and (I) the population of neutrophils. (J) Correlation analysis between
neutrophil number on day 7 and decreased MPE volume (volume on day 43 minus
volume on day -1). For all graphs, data present mean±SEM for at least three
independent experiment. *P<0.05, **P<0.01, ***P<0.001, ns: not significant by
paired Student’s t-test (C, E, G, H, and I) or unpaired Student’s t-test (F).
Figure 2. Neutrophil recruitment is required for MTX-MP treatment efficiency.
(A) H22 tumor cells were i.p. injected into BALB/c mice (n=6), followed by the
intraperitoneal injection of MTX-MPs (MP) or saline (Control: Ctrl) one day later.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

36
After 18 hours, peritoneal CD11b+Ly6G
+ cells were analyzed. (B) BrdU (1 mg/20g)
was i.v. injected into mice (n=6) for 24 hours, followed by saline or MTX-MPs i.p.
injection. Peritoneal neutrophils were analyzed by flow cytometry. Bone marrow
(BM)-derived neutrophils were used as a positive control. (C,D) H22 cells were i.p
injected into mice (n=6), followed by MTX-MPs or saline. 18 hours later, the
neutrophils were analyzed by (C) flow cytometry for Ki67 expression and (D) H&E
stain to assess neutrophils (Neu) and MDSCs. Scale bar 10 μm. (E) H22 cells were i.p
injected into mice, followed by i.p. injected MTX-MPs once every day for 6 times.
Ly6G-depleting antibody was used to deplete neutrophils. IgG acted as a control.
Ascites volume (left, collected on day 15 after tumor inoculation, n=5) and long-time
survival (right, n=10/group) are shown. **P<0.01 versus IgG group, #P<0.05 versus
MP/Ly6G antibody group. (F, G) H22 cells were i.p. injected into (F) wild-type or (G)
nude mice for 3 days. The mice (n=15) were treated by i.p. infusion of BM-derived
neutrophils daily. Some mice (n=5) were used to analyze CD45– tumor cell number
and the ascites volume. The remaining mice (n=10) were used for long-time survival.
(H) LLC cells were i.p. injected into C57BL/6 mice, followed by i.p. injection
MTX-MPs daily. Ly6G-depleting antibody were used, and long-time survival was
analyzed (n=10/group). **P<0.01 versus IgG group, ##P<0.01 versus MP/Ly6G
antibody group. **P<0.01, ***P<0.001, ****P<0.0001 by unpaired Student’s t-test
(C, F, G), one-way ANOVA (E). The data represent mean±SEM for three
independent experiments. The survival rates were determined by Kaplan-Meier
survival analysis.
Figure 3. MTX-MPs induce chemokines for neutrophil recruitment
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

37
(A,B) Cells from MPE of patients were incubated with PKH26-labeled MTX-MPs
(cell:MP=1:10) for (A) 2 hours or (B) 30 minutes. MFIs for tumor cells (Tumor),
macrophages (Mac), neutrophils (Neu), T and B cells were analyzed by flow
cytometry. (C) Macrophages, neutrophils and tumor cells from (A,B) were incubated
with MTX-MPs for 2 hours, and cultured supernatants were used for a trans-well
assay. Neutrophil migration to the lower chamber was counted. (D) MPE samples of
patients (n=6) were collected at different time points following the first MTX-MP
injection. CD11b+CD15
+ neutrophils in MPE were analyzed. (E) MPE supernatant
from MTX-MP-treated patients were loaded to the lower chamber with or without
GM-CSF- or IL1β-neutralizing antibody. Neutrophils were in the upper chamber. IgG
was used as control. (F, G) PBMC-derived macrophages were incubated with
MTX-MPs for 2 hours. CXCL1 and CXCL2 was analyzed by (F) real-time PCR
(n=9), and (G) culture supernatants were analyzed by ELISA (n=3). (H,I) MPE was
collected from patients at different times after the first MTX-MP injection. (H)
CXCL1 and (I) CXCL2 was measured by ELISA (n=6). (J) Macrophages isolated
from untreated MPE of patients were incubated with MTX-MPs. Four hours later,
CXCL1 and CXCL2 in the supernatant were analyzed (n=6). (K) MPE supernatants
from patients were collected 48 hours after MTX-MP treatment for the trans-well
experiments (Lower chamber: supernatant with or without anti-CXCL1 or CXCL2.
Upper chamber: peripheral blood derived neutrophils). (L) HUVECs (CRL-1730)
were cocultured with MTX-MPs for 4 hours. CD62p and CD62e were analyzed. (M)
Neutrophils were isolated from the MPE of patients untreated or 24 hours after
treatment. CD162 was analyzed (n=3). . (N) Neutrophils from MPE of patients
without MTX-MPs treatment were added onto the HUVEC layer for 24 hours with or
without MTX-MPs. Endothelium-neutrophil contact was assessed. Scale bar: 20 μm.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

38
**P<0.01, ***P<0.001, ****P<0.0001 by unpaired Student’s t-test (A, B, F, G, J, L,
M and N), or one-way ANOVA (E and K), the data present mean±SEM for three
independent experiments.
Figure 4. Attracted neutrophils possess antitumor properties in the MPE of
patients. (A-D) Neutrophils from MPE of patients (n=16) before and 48 hours after
treatment with (A,C) MTX-MPs or (B,D) saline were analyzed by flow cytometry. (E)
MPO, iNOS (NOS2), NOX2 (CYBB), and ARG1 in neutrophils (n=6) was analyzed by
real-time PCR. (F-H) The above neutrophils were analyzed by (F) TEM and (G,H)
H&E staining. Black arrows: vacuolated structure; red arrows: lobulated nucleus.
Scale bar: 10 μm. (I, J) Neutrophils from the untreated MPE patients (n=3) were
incubated with MTX-MPs for 12 hours. CD11b, CD66b, CD54, and CD15 were
analyzed by (I) flow cytometry and (J) real-time PCR. (K, L) Neutrophils from
untreated MPE patients (n=4) were cocultured with the supernatants of
MTX-MP-treated A549 cells for 12 hours. CD11b, CD66b, CD54, and CD15 were
analyzed by (K) flow cytometry and (L) western blot. *P<0.05, **P<0.01,
***P<0.001, ****P<0.0001 by unpaired Student’s t-test (A-D and H-K), or paired
student’s t-test (E). The data present mean±SEM for three independent experiments.
Figure 5. Recruited neutrophils are cytotoxic to tumor cells by utilizing ROS and
NETs. (A,B) CFSE-labeled (A) tumor cells from untreated MPE patients (n=3) or (B)
A549 cells were incubated with neutrophils from MPE patients for 16 hours. CFSE+
cells were analyzed by flow cytometry. Blank: no neutrophils; Ctrl: neutrophils from
saline-treated MPE; MP: neutrophils from MTX-MP-treated MPE; PBN: neutrophils
from peripheral blood of untreated patients. (C) A549 cells were incubated with
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

39
neutrophils from the treated MPE. Cells were observed under microscope. Blank:
without neutrophils. Scale bar: 20 μm. (D) Fresh MPE from MTX-MP-treated
patients was stained with anti-EpCAM and anti-CD15 for fluorescent microscopic
analysis. Scale bar: 20 μm. (E,F) Neutrophils from MPE patients (control: no
treatment) were collected. MFIs for (E) total ROS and (F) mitochondrial ROS were
analyzed by microscopy and flow cytometry. Scale bars: 10 μm. (G) Neutrophils from
MPE patients (n=3) were incubated with A549 cells with or without of NAC (20 mM)
or DPI (10 μM). Apoptosis of tumor cells was detected by flow cytometry. (H)
Neutrophils from treated MPE patients were incubated with CD44-stained A549 cells
in serum-free medium. NETs stained by Sytox green were analyzed using confocal
microscopy. Scale bar: 30 μm. (I) Neutrophils in MPE were isolated from patients
with or without MTX-MP treatment and observed by SEM. Scale bar: 10 μm. (J)
Neutrophils from treated patients’ MPE (n=3) were incubated with CFSE-labeled
A549 cells with or without Cl-amidine (CLAM). A549 cell apoptosis was analyzed by
flow cytometry. *P<0.05, **P<0.01, ***P<0.001, ****P<0.0001 by unpaired
Student’s t-test (E and F) or one-way ANOVA (A, B, G and J). The data present
mean±SEM for three independent experiments.
Figure 6. NETs prevent vascular leakage by sealing off damaged endothelium. (A)
LLCs were i.p. injected into mice (n=6) for 10 days. The pleural vasculature was
analyzed by H&E staining (normal: healthy mice). Scale bar: 300 μm. (B-D)
HUVECs were seeded on the upper chamber. Neutrophils isolated from MPE (n=5)
from (B) saline- or (C) MTX-MP-treated patients were seeded on the HUVEC layer
for 2 hours (D) with or without Cl-amidine. Dextran was then added into the upper
chamber for colorimetric analysis. (E) Neutrophils from MTX-MP- or saline-treated
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

40
MPE patients (n=6) were added onto the HUVEC layer (anti-CD31) for 2 hours.
NETs were assessed with Sytox green by confocal microscopy. 3D and 2D images are
shown on the left and right, respectively. Scale bar: 20 μm. (F,G) LLCs were
intrapleurally injected into mice (n=4), followed by intrapleural injection of
MTX-MPs (F) without or with Cl-amidine (G). Evans blue dye was i.v. injected 1
hour before mice were scarified. The extravascular Evans blue in pleural cavity was
quantified spectrophotometrically. (H) LLCs were inoculated in the pleural cavity for
10 days, followed by intrapleural injection of MTX-MPs. 18 hours later, Sytox green
was i.v. injected and the mice were scarified 2 hours later. Vessel sections were
stained with PE-labeled CD31 and assessed for NETs (n=5). Scale bar: 100 μm. (I, J)
LLCs were intrapleurally injected into C57BL/6 mice for 3 days, followed by the
treatment of saline or MTX-MPs, Cl-amidine, or MTX-MPs plus Cl-amidine. On day
12, (I) MPE volume was measured (n=5) and (J) the long-term survival was analyzed
(n=10/group), ***P<0.001 versus control group, ###P<0.001 versus MP/Cl-amidine
group, Kaplan-Meier survival analysis was used (J). *P<0.05, **P<0.01,
***P<0.001 by unpaired Student’s t-test (B-D and F) or one-way ANOVA (G and I),
the data present mean±SEM for three independent experiments (B-I).
Figure 7. Schematic diagram for MTX-MP treatment of MPE.
(1) Following the injection into the MPE via pleural catheter, drug-MPs are taken up
by and kill tumor cells. (2) Drug-MPs are taken up by and induce macrophages to
release CXCL1 and CXCL2, thus recruiting neutrophils to the MPE. (3) Neutrophils
are activated in drug-MP-remodeled malignant environments. (4) Activated
neutrophils launch the second wave of killing tumor cells. (5) Neutrophils release
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

41
NETs to seal off the damaged endothelium, facilitating the regression of the MPE.
Red arrows: increased expression. A: steps 1-3; B: steps 4 and 5.
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789

Published OnlineFirst July 13, 2020.Cancer Immunol Res Pingwei Xu, Ke Tang, Jingwei Ma, et al. response targeting malignant pleural effusionsChemotherapeutic tumor microparticles elicit a neutrophil
Updated version
10.1158/2326-6066.CIR-19-0789doi:
Access the most recent version of this article at:
Material
Supplementary
C1
http://cancerimmunolres.aacrjournals.org/content/suppl/2020/07/11/2326-6066.CIR-19-0789.DAccess the most recent supplemental material at:
Manuscript
Authorbeen edited. Author manuscripts have been peer reviewed and accepted for publication but have not yet
E-mail alerts related to this article or journal.Sign up to receive free email-alerts
Subscriptions
Reprints and
To order reprints of this article or to subscribe to the journal, contact the AACR Publications
Permissions
Rightslink site. Click on "Request Permissions" which will take you to the Copyright Clearance Center's (CCC)
.http://cancerimmunolres.aacrjournals.org/content/early/2020/07/11/2326-6066.CIR-19-0789To request permission to re-use all or part of this article, use this link
Research. on September 22, 2020. © 2020 American Association for Cancercancerimmunolres.aacrjournals.org Downloaded from
Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. Author Manuscript Published OnlineFirst on July 13, 2020; DOI: 10.1158/2326-6066.CIR-19-0789