Chapter 8 Study Guide - WordPress.com … · Web view11. Understand treatment of overweight and...
Transcript of Chapter 8 Study Guide - WordPress.com … · Web view11. Understand treatment of overweight and...

Chapter 8 Study Guide
1. Know the average gestation for a full-term and preterm infant.— 88% are born full term, 37-42weeks, 5.5-8.5lbs, 18.5-21.5inches
2. Know how motor development occurs in infants: Motor development: ability to control voluntary muscles Motor development is top down— controls head first and lower legs last Muscle development from central to peripheral
3. Which conditions reflect the immaturity of the gastrointestinal tract?—Fetus swallows amiotic fluid which stimulates intestines maturation and growth. Conditions that reflect the immaturity of the gut are, colic, gastroesophageal reflux (GER), unexplained diarrhea, and constipation.
4. What is the AVERAGE caloric need of infants in the first six months of life per kg ofbody weight, based on growth in breast-fed infants.—Energy needed for infants in the first 6 months of life is 108 cal per kg daily.
*5. What are the two essential fatty acids required in an infant’s diet?— The first is alpha-linolenic acid (LNA or ALA) , and it belongs to the omega-3 family of fatty acids. Linoleic acid (LA) is the other essential fatty acid, belonging to the omega-6 family of fatty acids.*short and medium chain fatty acids found in breast milk.
6. What foods/liquids should be recommended for a baby suffering constipation?— Adequate fluids.
7. Know what vitamin supplement an infant needs if they don’t get much sunlight.—Vitamin D
8. Know unsafe foods to give a one-year old. Popcorn Peanuts Raisins, whole grapes Stringy meats Gum & gummy-textured candy, hard candy or jelly beans Hot dogs Hard fruits or vegetables
9. Know the recommended age for weaning an infant from the breast or bottle to a cup.— The recommended for weaning to a cup at 12 to 24 months.
10. The FIRST step in correcting failure to thrive (FTT) is: to determine whether a child's weight is in fact below normal.*nutrition assessment
11. What is nonorganic failure to thrive and what are possible causes.— Nonorganic—meaning not based on medical diagnosis. Organic—diagnosed medical illness

12. What are good feeding practices to limit baby bottle caries and ear infections? Limit use of bedtime bottle Offer juice in cup Only give water bottles at bedtime Examine and clean emerging teeth
13. Plot a newborn’s weight at birth. Know if she is SGA, LGA or AGA.• (SGA) and “intrauterine growth retardation” (IUGR) <10th % wt/age• “Large for gestational age” (LGA) >90th % wt/age• “Appropriate for gestational age” (AGA)
14. A child with diarrhea and an allergy to lactose would most likely be given which formula.—Formula with Hydrolyzed proteins
15. Healthy newborns typically double their birthweight within 6 months.
16. Should intake of fat or cholesterol be limited in infants?— Fat and cholesterol should NOT be limited in infants.-Beast milk has a 55% of calories from fat-Cholesterol is needed for gonad and brain development
Possible case study:Know when a child is ready for solids (cues), what solids should a person start with, quantity, and foods to avoid.• Cues infants may give for feeding readiness include:
Watching the food being opened in anticipation of eating Tight fists or reaching for spoon Irritation if feeding too slow or stops temp. Playing with food or spoon Slowing intake or turning away when full Stop eating or spit out food when full
• Food offered from spoon stimulates muscle development.

• Only one new food over 2-3 days.
• 4-6 months- pureed foods
• 6-8 very soft, lumpy foods
• 8-10 soft mashed foods
• Salt
Honey Spinach, beets,
turnips, collard greens and carrots
Nuts Cow's milk Unpasteurized milk Wheat Fish, egg and citrus

Chapter 9 Study Guide
1. Know the primary components of a nutrition evaluation in a baby with special needs.— Vitamin D and Fluoride
2. Know under what conditions infants need additional calories and under what health conditions they require less calories.—+ require additional calories: difficult breathing, temperature regulation, fever, and recovery from surgery - required less calories: spina bifida and Down syndrome.
3. The DRI for protein for typically infants is— Normal growth- protein intakes would be 2.2 g/kg Premature protein intakes of 3.0-3.5 g/kg ELBW, high protein intakes as much as 4 g/kg
4. Why is it difficult for a preterm baby to digest protein? Think organ.—Because preterm baby’s organs are not fully developed yet.
5. Know what macronutrients are used in formulas for VLBW babies.—Mixture of amino acids, carbohydrates, fats, vitamins, and minerals.
6. How do we evaluate weight changes in preterm breastfed infant?• Evaluate weight gain and breastfeeding every 2–4 days• Interpretation of growth is based on a pattern of weight gain.
7. Know how to calculate gestation-adjusted age.— Subtract GA at birth from 40 weeks.
8. Know Table 9.6— end
9. What are nutrition concerns for babies with Down syndrome?— Weak muscles in the face, and overall- cause feeding dificult High risk of overweight- close monitoring of growth Constipation Low amount of movement- lower caloric needs
10. What are preterm babies hard to feed?— Fatigue, Low tolerance of volume CNS does not signal hunger Unstable feeding position Oral hypersensitivity
Chapter 10 Study Guide
1. What are some behavioral characteristics of preschool children?— increasing autonomy experiencing broader social circumstances, preschool or staying with relatives increasing language skills Expanding self-control

2. Know typical weight gain at six months and weight gain at a year double their birth weight at 6months 3plet at 1 year
3. What is the “rule of thumb” for toddler portion sizes?— 1 tablespoon of food per year of age.
4. Why is preschool a good time to teach children about foods?— Love to cooperate Can use utensils and cups Appetite increases prior to the spurts of growth Include child in meal selection and preparation
5. How many exposures may a child need before accepting a new food?—About 8 to 10 exposures to a new food
6. What are common nutrition problems among young children?— Iron-deficiency Dental caries Constipation Lead poisoning Food security Food safety
7. What are nutrition interventions for preventing anemia among children?— Limit milk consumption to 24Oz/day
Iron supplements Counseling Repeating screening
8. Fiber recommendations for 5 years old are:1-3 years old- 19g/day4-8 years old- 25g/day
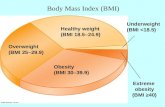
9. Know how to plot BMI on CDC chart; know what the percentiles mean in terms of normal weight, at risk for overweight, and overweight.—
BMI-for-age percentile of 85th to 94th is defined as overweight BMI-for-age >95th is defined as obesity < 2 years of age, weight-for-length > 95th percentile is overweight.
10. Know Ellyn Satter’s division of responsibility.— Parents and caretakers are responsible for what children are offered to eat and the environment
in which the food is served Children are responsible for how much they eat or even whether they eat at a particular meal or
snack.
11. What will result when a family praises a child for cleaning their plate?—Overeating
12. Food jags and consequences on health.—Food jags may cause a nutrition deficiency because children consume less variety of foods.

13. How does appetite change among toddlers and preschool children?—As for toddlers are:• Decrease appetite• Slowing growth • Preferences and dislikes• Food jags
As for preschools are: Make foods attractive Prefer familiar foods Strong flavor/spicy NOT accepted Adjust cal intake to meet cal needs
14. Know temperament differences and how they influence intake.— Easy (40%)- adapts to regular schedules & accepts new foods Difficult (10%)- slow to adapt and may be negative to new foods Slow-to-warm-up (15%)- slow adaptability, negative to new foods but can learn to accept new
foods Intermediate low to high (35%) – a mixture of behaviors
Chapter 11 Study Guide
1. % of children with disabilities with nutritional problems.— 90% of children with disabilities have a nutrition problem
2. Which conditions require more calories?— Cystic dibrosisRenal diseaseAmbulatory children with displegiaPediatric AIDSBronchopulmonary Dysplasia (BPD)
3. Why are overweight and obesity common in Down’s Syndrome?—Because of the lower caloric needs due to low muscle mass, lower mobility, and short stature.
4. What is cystic fibrosis?Condition in which a genetically changed chromosome 7 interferes with all the exocrine functions in
the body, but particularly pulmonary complications, causing chronic illness
5. What behavioral disorders impact nutrition?—Autism and ADHD (Attention Deficit Hyperactivity Disorder)
6. When can FTT occur?— Failure to thrive- Inadequate wt or ht gain w growth declines >2% growth Occurs at the age when appetite typically decreases and control issues at mealtime are expected May result from: Digestive problems, asthma, pediatric AIDs, neurological conditions
7. Looking at growth declines in percentiles, when is FTT diagnosed?—>2 growth percentile decrease.
8. How is celiac disease managed?— Restriction of any foods with gluten, a component of wheat, barley, or rye as additive
9. How do breathing problems impact nutrition?— ↑ nutrient needs ↓Interest in eating- can slow growth
10. How common are food allergies? What are the most common food allergens?• True food allergies seen in ~2% to 8% of children.

• Common food allergies include: Milk, Eggs, Wheat, Peanuts, Walnuts, Soy, and Fish.
10. How is anaphylactic shock treated?— For children at risk of anaphylaxis, parents and caregivers should given instruction in emergency lifesaving procedures and use of an injection form of epinephrine.
12. Is there a relationship between asthma and food allergies?— Asthma does not necessarily required nutrition services, but some children have asthma as a result of food allergies. (Pg. 306)
Chapter 12 Study Guide
1. What % of U.S. children live in extreme poverty (in 2006).—About 8% children live in extreme poverty.
2. Know BMI cut-offs for normal weight, at risk for overweight and overweight among children.— Overweight = BMI-for-age from 85th to 95th% Obese= BMI-for-age >95th%.
3. Know what is needed to estimate energy requirements for children.— Energy needs vary by activity level and body size.
4. Know fiber recommendations for children between the ages of 4 and 8.— 1-3 years old- 19g/day4-8 years old- 25g/day (pg 324)
5. Know which foods would be MOST likely to promote dental caries.—Sugary snacks, soft drinks, sports drink, and candy (pg 318)
6. Know potential health consequences of obesity in children.— Increase risk of cardiovascular disease and type 2 diabetes mellitus (pg 319)-Hyperlipidemia, higher concentrations of liver enzymes, hypertension, and abnormal glucose tolerance, occur with increased frequency in obese children than in children of normal weight.
7. Of children and adolescents with type 2 diabetes, what percentage are overweight or Obese when diagnosed?—About 85% of affected children being either overweight or obese at diagnosis. (pg.319)
8. Know predictors of childhood obesity (including most significant).—Maternal obesity, low family income and lower cognitive stimulation
Age at onset of BMI rebound – Normal increase in BMI after decline– Early BMI rebound, higher BMIs in children later
Home environment- Parental obesity predictor of childhood obesity
9. Why does watching television contribute to obesity? — Resting energy expenditure decreases while viewing TV
10. According to the DRIs, the Acceptable Macronutrient Distribution Range (AMDR) for fat is 25 to 35% of energy for children 4 to 18 years of age.
11. Understand treatment of overweight and obesity (page 321-322) including weight loss recommendations based on BMI scores.—

Overweight treatment should be weight maintenance or slowing of the rate of weight gain until a BMI-for-age percentile < 85th is achieved. For children with BMI-for-age percentiles of 95th to 98th, weight maintenance or gradual weight loss of no more than 2lbs/wk until the BMI-for-age < 85th. Recommended components include parent training, dietary counseling/nutrition education, physical activity and addressing sedentary behaviors, and behaviors, and behavioral counseling. (pg 322)12. Know 5 tenets of the School Lunch program:
• Lunches based on nutrition standards• No discrimination between those who can and cannot pay• Operate on a non-profit basis• Programs must be accountable• Must participate in commodity program
Chapter 13 Study Guide
1. What do you tell parents of a child with cystic fibrosis who has recurrent illnesses about how to feed their child?—
Just be flexible with your child and don’t force them to eat the things that they don’t feel like eating it.
2. Why do children with chronic conditions have more difficulty meeting the DRI for vitamins and minerals? Chewing or other feeding problems Side effects from prescribed medications Food refusals Treatment of condition that includes restriction of certain foods
3. In what condition are fat-soluble vitamin supplements recommended?—Cystic fibrosis requires fat-soluble vitamins 4. What does nutrition intervention for cystic fibrosis include?— monitoring growth assessing dietary intake increasing calories and protein by 2-4 times the usual recommended to compensate for malabsorption.
5. Why do many children with cerebral palsy have constipation?—They have low levels of physical activity due to their impaired muscle activity and coordination 6. What are nutritional concerns in ADHD? ↑ calories needed Medications
– Ritalin or Adderal: ↓appetite & growth– Medication peak activity is aimed at school hours– Appetite returns to normal when meds are not given such as on weekends & school holidays
No evidence of nutrition as a cause and treatment but families may choose herbal medicines anyway
7. What diet has been shown to be effective in reducing the incidence of seizures in children?—Ketogenic diet- severely low CHO diet with increased calories from fat, adequate in calories and proteins
Chapter 14 Study Guide
1. What is the difference between assessing nutrient needs in adolescents and adults? sexual maturation Increases in height and weight

Changes in body composition Accumulation of skeletal mass
2. The struggle for independence that characterizes adolescent psychosocial development may lead to the development of which health-compromising eating behaviors?
– Excessive dieting– Meal skipping– Use of unconventional nutritional and no nutritional supplements– Fat diets
3. Snacks account for 39% of daily energy intakes among adolescents.
4. What is the vegetable most frequently consumed by adolescents?potatoes make up half of the vegetables
5. Know the DRI of fiber for adolescent females.26 g/day for adolescent females
6. What is the best reason for wanting young adolescents to consume foods that provide adequate calcium?Adequate intake of calcium is critical to ensure peak bone mass
7. How can you increase the bioavailability of iron?Heme Iron found in animal products, is highly bioavailable. Bioavailability of nonheme iron, found in both animal and plant-based foods, can be enhanced by consuming it with heme sources of iron or vitamin C. (pg 370)
8. What are the physical activity recommendations for adolescents? – Be physically active every day– Engage in 60 minutes or more physical activity– Include muscle- and bone-strengthening activities at least 3 days a week
9. Know the three levels of influence when planning nutrition interventions for teens.– Personal or individual– Environmental– Macrosystem
10. What are the health advantages for an adolescent consuming a vegetarian diet? – High intake of fiber and relatively high intake of the vitamins and minerals found in plant-based
food.– Consume more fruits and vegetables
• Fewer sweets, salty snacks, and fat.– Best when small amounts of animal-derived foods, such as milk or cheese, are consumed at least
two times per week.
Chapter 15 Study Guide
1. What are risk factors for the development of overweight among children and adolescents?– Having one or more overweight parents– From a low income family– African American, Hispanic, American Indian or Native Alaskan descent– Having a condition that limits mobility

– Inadequate physical activity– Diets high in calories, sugars, & fat
2. A male has a BMI of 25 which is at the 90th percentile for age and gender. Based on age, height and weight, is overweight
3. Know what the four stages of the National guidelines for the treatment of child and adolescent overweight and obesity are.
1. Prevention plus- overweight, no co-morbidity 2. Structured weight management- Stabilize weight3. Comprehensive multidisciplinary intervention- 4. Tertiary care intervention
4. Know treatment of iron-deficiency anemia and side-effects.• Treatment includes:
– Increase intake of foods rich in irons & vitamin C
– Iron supplements• Under age 12—60 mg/day• Over age 12—60 to 120 mg/day
• Common side effects include:– Constipation – Nausea– Cramps
Side Effect of Iron Supplements:• Reduce side effects by
– Taking small, frequent doses– Take with meals
• Factors reduce iron absorption include – Calcium supplements – Dairy products– Coffee– Tea– High-fiber foods
5. Nutrition recommendations for treating hyperlipidemia and hypertension.For hypertension:
• Limit sodium intake• Limit fat to 30% of calories• Consume adequate fruits, vegetables, whole grains, & low-fat dairy• Weight loss if overweight• Dietary recommendations should be encouraged even if meds are prescribed.
For hyperlipidemia:• <35% calories from total fat• <10% calories from saturated fat• Cholesterol intake ≤300 mg/day • Adequate fruits, vegetables, grains, & low-fat dairy
6. Know the contributing factors for eating disorders.• Main groups of contributing factors for eating disorders are:
1. Environmental

2. Familial factors3. Interpersonal factors4. Personal factors
Prevention of Overweight & Obesity• Limit sugar-sweet beverages• Encourage fruits & vegetables• Limit TV• Daily breakfast• Limit fast foods• Limit portionsCalcium rich diets• Diets high in fiber• Follow the DRI for carbs, pro & fat• Promote physical activity• Limit energy-dense foods

Health and Eating-related Behaviors during Adolescence
• The model depicts 3 interacting levels of influence on adolescent eating behaviors
– Personal or individual
– Environmental
– Macrosystem
Overweight and Obesity
• Factors contributing to the increase include:
– Having one or more overweight parents
– From a low income family
– African American, Hispanic, American Indian or Native Alaskan descent
– Having a condition that limits mobility
– Inadequate physical activity
– Diets high in calories, sugars, & fat
National Guidelines for Weight Management Therapy
• Four stages of treatment
1. Prevention plus
2. Structured weight management
3. Comprehensive multidisciplinary intervention
4. Tertiary care intervention
Nutrition Counseling for Hypertension

• Limit sodium intake
• Limit fat to 30% of calories
• Consume adequate fruits, vegetables, whole grains, & low-fat dairy
• Weight loss if overweight
• Dietary recommendations should be encouraged even if meds are prescribed
•
Dietary Recommendations to Reduce Hyperlipidemia
• <35% calories from total fat
• <10% calories from saturated fat
• Cholesterol intake ≤300 mg/day
• Adequate fruits, vegetables, grains, & low-fat dairy













![Pregnancy after bariatric surgery: a narrative literature ......wide are overweight (BMI≥25kg/m2) and 13% are obese (BMI ≥30kg/m2)[1]. It is widely known that obesity is associated](https://static.fdocuments.in/doc/165x107/609256503d5e5b10c55c0fc6/pregnancy-after-bariatric-surgery-a-narrative-literature-wide-are-overweight.jpg)