Chapter 7 Severe Malnutrition. Case study: Kanchha Kanchha, a 12-month-old boy brought to district...
-
Upload
annice-ellis -
Category
Documents
-
view
216 -
download
2
Transcript of Chapter 7 Severe Malnutrition. Case study: Kanchha Kanchha, a 12-month-old boy brought to district...
Case study: Kanchha
Kanchha, a 12-month-old boy brought to district hospital from rural area. 8 day history of loose watery stools. 2 days of increased irritability and poor oral intake.
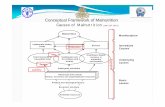
Stages in the management of a sick child (Ref. Chart 1, p. xxii)
1. Triage
• Emergency treatment, if required
2. History and examination
• Laboratory investigations, if required
3. Differential diagnoses
• Main diagnosis
4. Treatment
5. Supportive care
6. Monitoring
7. Plan discharge
• Follow-up, if required
What emergency and priority signs have you noticed from the
history and from the picture?
Temperature: <35.00C, pulse: 130/min, RR: 50/min, Weight: 6 kg, Length: 69cm
Triage
Emergency signs (Ref. p. 2, 6)
• Obstructed breathing• Severe respiratory distress• Central cyanosis• Signs of shock• Coma• Convulsions• Severe dehydration
Priority signs (Ref. p. 6)• Tiny baby• Temperature• Trauma• Pallor• Poisoning• Pain (severe)• Respiratory distress• Restless, irritable, lethargic • Referral• Malnutrition• Oedema of both feet• Burns
Kanchha Lama was well until 5 months of age. At 5 months his mother became pregnant again. His mother had started to wean him from the breast at 3 months, as her milk supply was reduced. From 4 months he was fed formula milk from a bottle with a rubber teat. He was given solid food from four months of age, mostly rice with dahl (lentil soup).
From 5 months he had six episodes of diarrhoea. Each episode lasted for 5-6 days, which was treated locally from a medical shop. During each episode of diarrhoea he was given reduced amounts of fluid and feeds because his mother thought this would reduce the severity of his diarrhoea. On this last occasion he was taken to the hospital, as he became irritable and was not drinking or eating well.
History
Nutrition history
Kanchha was started on formula feed at 4 months of age. The milk was diluted (one scoop of milk per whole bottle of water). His mother would wash his bottles and teats in tap water, and rarely would boil the bottles. He was given weaning food at six months of age, mainly contained rice with dal and only occasional vegetables. He would get meat occasionally, but not for the past 2 months. He usually received two meals and two bottles of milk each day. Kanchha always had to share his plate of food with his other siblings.
Family circumstances
Kanchha lives with his parents in a small cottage. He has three older sisters and two older brothers. They have a small plot of land on which they grow crops, but which is not sufficient to feed their family. Kanchha’s father works as a farmer and his mother as a housemaid where they can earn some more money for food and beverages. Because they are so busy, Kanchha’s older siblings mostly take care of him.
Kanchha was visibly wasted, having skin folds over his arms, buttocks and thighs and visible rib outlines.Vital signs: temperature: <35.00C, pulse: 130/min, RR: 50/min Weight: 6 kg and Length: 69cm, MUAC 10.5cm
□ Use Table 35 p. 386 and assess Kancha’s weight-for-length
Chest: bilateral air entry was normal, no added sounds Cardiovascular: both heart sounds were heard and there was no murmurAbdomen: soft, bowel sound was audible; no organomegalyEars-Nose-Throat: dry mucus membranesEyes: sunken, no tears and dry conjunctivaSkin: decreased skin turgor Neurology: irritable, sick looking; no neck stiffness and no other focal signs
Examination
• List possible causes of the illness
• Main diagnosis
• Secondary diagnoses
• Use references to confirm (Ref. p. 198-199)
Differential diagnoses
Differential diagnoses (continued)
• Primary severe malnutrition (marasmus, kwashiorkor)
• Secondary severe malnutrition in the course of:
-Tuberculosis
-HIV-Pneumonia-Measles-Malabsorption syndrome-Micronutrient deficiency (Vitamin A, zinc)
Additional questions on history
Concerning:
• Recent intake of food and fluids
• Usual diet (before the illness)
• Breastfeeding
• Duration and frequency of diarrhoea and vomiting
• Type of diarrhoea (watery/bloody)
• Loss of appetite
• Family circumstances (social background)
• Chronic cough
• Contact with TB, measles
• Known or suspected HIV
Further examination based on differential diagnoses
On examination, look for:• Severe palmar pallor• Eye signs of vitamin A deficiency• Skin changes of kwashiorkor• Localizing signs of infection• Signs of HIV• Fever or hypothermia• Mouth ulcers• Signs of dehydration• Shock(Ref. p. 199)
Further examination based on differential diagnoses
• Palmar Pallor – indicating severe anaemia (Ref. p. 167). In any child with palmar pallor, determine the haemoglobin or haematocrit level
• Check also conjunctiva and mucous membranes
Further examination based on differential diagnoses
Look for signs of vitamin A deficiency:
• Dry conjunctiva or cornea
• Bitot’s spots
• Corneal ulceration
• Keratomalacia
(Ref. p. 199)
Investigations (continued)
• Blood glucose: 2.4 mmol/L (3-6.5mmol/L)
• Haemoglobin: 70 g/l (105-135)
• Chest x-ray: normal
• Stool microscopy shows trophozoites of giardia
DiagnosisSummary of findings:• Examination: pale, irritable, and ill-looking. He was visibly
wasted, having skin folds over his arms, buttocks and thighs. He had visible rib outlines, hypothermia, sunken eyes with no tears and dry conjunctiva and decreased skin turgor.
• History: several risk factors for malnutrition such as poor socioeconomic status, a large family, non-nutritious family food, early weaning from breast milk, diluted, dirty formula feeding
• Weight-for length: <70% or -3SD• Low haemoglobin• No contact with TB• No signs of HIV• Stool microscopy shows trophozoites of Giardia lamblia
Treatment: Step 1
□Hypoglycaemia (Ref. p. 201):give the first feed of F-75 if it is not quickly available give 50ml of 10% glucose solution orally or by nasogastric tubegive 2-3 hourly feeds, day and night, at least for the first day
Treatment: Step 2
□Hypothermia (Ref. p. 202-203):feed the child immediately
make sure the child is clothed (including the head), use warmed blanket or put the child on the mother's bare chest or abdomen
Treatment: Step 3
□Dehydration (Ref. p. 203-204):give ReSoMal rehydration fluid orally or by nasogastric tube, much more slowly than you would when rehydrating a well-nourished childif rehydration is still occurring at 6 and 10 hours give the same volume of starter F-75 instead of ReSoMal at these times
Treatment: Step 4
□Electrolytes (Ref. p. 206):If electrolytes are not added to the food:
give extra potassium (3-4mmol/kg)
give extra magnesium (0.4-0.6mmol/kg)prepare food without salt
Giving high sodium loads could kill the child
Consider if F-75 is provided there is no need to add electrolytes to food
Treatment: Step 5
□Infection (Ref. p. 207-208):give all severely malnourished children a broad-spectrum antibioticin this case give also treatment for giardiasis (metronidazole: 5mg/kg, 3 times a day, for 5 days (Ref. p. 137))give measles vaccine if the child is not immunized
Treatment: Step 6□Micronutrients (Ref. p. 208-209):If micronutrients are not added to the
food:give daily a multivitamin supplement, folic acid, zinc, coppergive vitamin A orally on day 1once gaining weight, give ferrous sulfategive iron only after the child gains weight, because iron can make infections worse
Consider if F-75 is provided there is no need to add electrolytes to food
Treatment: Step 7
□Initiate feeding (Ref. p. 209-210):give F-75
100kcal/kg/day (protein: 1-1.5g/kg/day; liquid: 130ml/kg/day)continue breastfeeding if possible, but make sure the prescribed amounts of starter formula are given
Treatment: Step 8
□Catch-up growth (Ref. p. 210-215):replace the starter F-75 with F-100 for 2 days or use RUTF, if the child is elder than 6 monthsthen increase each feed by 10ml until some feed remains uneatencontinue breastfeeding if possible and give F-100 as indicated
Treatment: Step 9□Sensory stimulation (Ref. p. 215):
provide tender loving care, a cheerful stimulating environment and maternal involvement as much as possibleprovide structured play therapy for 15-30 minutes a dayphysical activity as soon as the child is well enough
Treatment Step 10: Prepare for discharge and follow-up
Monitoring• Monitor for early signs of heart failure (Ref. p. 214):
Pulse
RR• Monitor urinary frequency and frequency of stools and vomit• Note amounts of feed offered and left over and daily body weight• Standardize the weighing on the ward (Ref. p. 222-223)• Weigh the child the same time of the day, after removing clothes• Calculate weight gain (Ref. p. 215)
Monitoring (continued)• Note the weight gain:
– poor: <5g/kg/day– moderate: 5-10g/kg/day– good:>10g/kg/day
• If weight gain is poor check the following points:– Inadequate feeding– Untreated infection– HIV/AIDS– Psychological problems
Discharge home
If you discharge the child home before the full recovery:The child :• Should have completed antibiotic treatment• Should have a good appetite• Should show good weight gain• Should at least be losing oedema
The mother or carer:• Should be available for child care• Should have received specific training on appropriate feeding• Should have resources to feed the child
Mothers should understand that it is essential to give frequent meals with a high energy and protein content
(Ref. 219-221)
Follow-up
• Make a plan for the follow-up of the child until recovery
• Contact the outpatient department (or nutrition rehabilitation centre, local health clinic, health worker) who will take responsibility for continuing supervision of the child.
• The child should be weighed weekly after discharge.
• If the child does not gain weight over 2-week period or it even losts weight, it should be referred back to hospital.
• Kanchha was discharged before full recovery. • His parents were told to feed him at least 5
times per day. They had to give him high-energy snacks between meals (e.g. milk, banana, bread, biscuits).
• His parents were told to assist and to encourage him to complete each meal, to add electrolytes and micronutrient supplements to each feed and to monitor his intake as well.
• His mother was encouraged to breastfeed him as often as Kanchha wants.
• Follow-up was arranged.• Kanchha still needs continuing care as an
outpatient to complete rehabilitation and prevent relapse.
Progress
Summary
• 12-month-old boy, youngest of family of 6. Several episodes of gastroenteritis since he was five months of age. For the last 8 days he had been having frequent loose watery stools.
• Early weaning, diluted dirty formula, poorly nutritious food, repeated infections
• Alert but severely wasted, with palmar pallor
• Severe malnutrition with hypothermia, hypoglycemia, anaemia, giardiasis























































![€¦ · D Diarrhea (loose, watery stools) C] Coughing, wheezing, shortness of breath Other: How much of the food do you eat before symptoms occur? How soon after eating do symptoms](https://static.fdocuments.in/doc/165x107/5aea8d4d7f8b9ac3618dea57/d-diarrhea-loose-watery-stools-c-coughing-wheezing-shortness-of-breath-other.jpg)