Cerebral palsy
-
Upload
harjot-gurudatta -
Category
Health & Medicine
-
view
3.425 -
download
0
description
Transcript of Cerebral palsy
- 1.Most Common Permanent Disability of Childhood
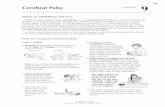
2. CEREBRAL PALSY By: Harjot Singh Gurudatta Moderator: Dr. Rohit Sharma 3. William John Little (18101894) In 1860s, known as "Cerebral Paralysis or Littles Disease After an English surgeon wrote the 1st medicaldescriptions 4. CEREBRAL PALSY (CP) Cerebral- Latin Cerebrum; Affected part of brain Palsy " -Gr. para- beyond, lysis loosening Lack of muscle control 5. CEREBRAL PALSY A motor function disorder caused by permanent, non-progressive brain lesion present at birth or shortly thereafter. (Mosby, 2006) Non-curable, life-long condition According to a recent definition CP describes a group of permanent disorders of the development of movement and posture,causing activity limitation, that are attributed to non-progressive disturbances that occurred in the developing fetal or infant brain. The motor disorders of cerebral palsy are often accompanied by disturbances of sensation, perception,cognition, communication, and behaviour; by epilepsy; and by secondary musculoskeletal problems 6. CEREBRAL PALSY A Heterogenous Group of Movement Disorders 7. In CP Muscles are unaffected Brain is unable to send the appropriate signals necessary to instruct muscles when to contract and relax 8. CAUSES OF CEREBRAL PALSY 9. An insult or injury to the brain Fixed, static lesion(s) In single or multiple areas of the motor centers of the brain Early in CNS developmentSevere deprivationon of oxygen orblood flow to the brain Hypoxic-ischemic encephalopathy or intrapartal asphyxia 10. Etiology Prenatal(MC) I, iron def.,poor nut. Inf, UTI, high fever Chorioamniotis HTN, DM Teratogens Poor ANC Rh ? Twins Fetal vasculopathy Maternal drugs/smoking(>30)Perinatal Birth asphyxia Breach/vacuum/forc Premature / LBW(>60/1000) IUGR Hyperbilirubenemia Intraventricular hemorrrhage Sepsis, pneumonia, meningitis Develop. Malformation, abruptioPostnatal CNS infections Head injuries Seizures Hypoxic damage Hyperpyrexi a damage Stroke 11. TYPES OF CEREBRAL PALSY 12. Classification of CP According to: 1. Neurologic deficits 2. Type of movement involved 3. Area of affected limbs 13. 1. Accdg. to Neurologic Deficits Based on the - extent of the damage - area of brain damage Each type involves the way a person moves 14. 3 MAIN TYPES 1. PYRAMIDAL - originates from the motor areas of the cerebral cortex2. EXTAPYRAMIDAL - basal ganglia and cerebellum3. MIXED 15. 4 MAIN TYPES( Movem ent) 16. Spastic CP Increased muscle tone, tense and contracted muscles Have stiff and jerky or awkward movements. limbs are usually underdeveloped increased deep tendon reflexes most common form 70-80% of all affected 17. Types of Spastic CP A/C LIMB INVOLVED Paraplegia Diplegia LL>UL , mc, normal iq,walks eventually,though delayed Hemiplegia UL>LL, seizures+, sensory changes in ul, limb length discrepancy Quadriplegia only slight H N control loss,low iq, highest hip subluxation,cognitive deficiency, Monoplegia one limb (extremely rare) Whole body with seizure, drooling hn control loss 18. Diplegia/ Paraplegia both legs w/ slight involvement Elsewhere May also have Contractures of hips and kneesand talipes equinovarus (clubfoot).both legs 19. Hemiplegia limbs on only one side 20. Hemiplegia on right side Hip and knee contractures Talipes equinus (tip-toeing- sole permanently flexed) Asteriognosis may be present. (inability to identify objects by touch) 21. Quadriplegia 22. Spastic Quadriplegia Characteristic scissors positions of lower limbs due to adductor spasms. 23. Athetoid/ Dyskinetic CP Fluctuating tone involves abnormal involuntary movements that disappear during sleep and increase with stress. Interferes with speaking, feeding, reaching, grabbing, and any other skills 20% of the CP cases, Wormlike movements Slow, uncontrolled motion, writhing or twisting in character in the face, extremities, and torso.Dystonia - when held as a prolonged posture Grimacing, drooling and dysarthria. Adductor spasm 24. Movements may becomechoreoid (rapid, irregular, jerky) anddystonic (disordered muscle tone, sustained muscle contractions) especially when stressed and during the adolescent years. 25. Ataxic CP Poor balance and lack of coordination Wide-based gait Depth perception usually affected. Tendency to fall and stumble Inability to walk straight line. Least common 5-10% of cases 26. MIXED CP A common combination isspastic and athetoid Spastic muscle tone and involuntary movements. 25% of CP cases, fairly common 27. DEGREE OF SEVERITY 1. Mild CP- 20% of cases2.Moderate CP50% - require self helpfor assisting their impaired ambulation capacity. 3.Severe CP30%;-totally incapacited and bedridden and they always need care from others. 28. The Peabody Development Motor Scales In-depth assessment 6 Subtests include: Reflexes Stationary Locomotion Object Manipulation Grasping, Visual-Motor Integration. The subtests yield a gross motor quotient a fine motor quotient a total motor quotient. Ages covered: from birth through five years of age 29. Denver Test II Developmental Screening Test Cover 4 general functions: personal social (eg. smiling), fine motor adaptive (eg. grasping & drawing) language (eg. combining words) gross motor (eg. walking)Ages covered: from birth to 6 years 30. Signs and Symptoms; Diagnosis OF CEREBRAL PALSY 31. History + Exam Include all that may predispose an infant to brain damage or CP Risk factors Psychosocial factors Family adaptationOften admitted to hospitals for corrective surgeries and other complications. Respiratory status Motor function Presence of fever Feeding and weight loss Any changes in physical state Medical regimenP osturing / Poor muscle control and strength O ropharyngeal problems(drooling?swallowing?feeding?) S trabismus/ Squint T one (hyper-, hypotonia)Muscle strength testing E volutional maldevelopment R eflexes (e.g. increased deep tendon) *Abnormalities 4/6 strongly point to CP 32. d. c.e.f.b. a.g. h. 33. Early Signs Infancy (0-3 Months) Stiff or floppy posture Excessive lethargy or irritability/ High pitched cry Poor head control Weak suck/ tongue thrust/ tonic bite/ feeding difficulties 34. neonatal reflexes Moros reflexStartle response; Startle reflex; Embrace reflexwhen the infant feels as if it is falling,1st abduct ,2nd adduct,ie embraceAsymmetric tonic neck reflex "fencing position -- head to one side, arm & leg on that side extended, opposite limbs flexedPlacing reflex When the dorsal (back) side of the hand or foot is placed on the edge of a surface, such as a table, the infant will lift the extremity and place it on the flat surface.Landau reflexWhen the infant is held in a horizontal prone position, the infant will lift head and extend the neck and trunk. When the neck is passively flexed, the entire body will flex3m-2y 35. Parachute ReflexWhen held around the waist in a horizontal prone position and then lowering the infant slowly, head first to the surface. By age 6 to 8 months the infant should respond by extending the arms and hands to break the fall. If this response is asymmetrical it indicates an unilateral motor abnormality. 36. CHILD with CP 37. Late infancy Inability to perform motor skills as indicated: Control hand grasp by 3 months Rolling over by 5 months Independent sitting by 7 months Abnormal Developmental Patterns: Hand preference by 12 months Excessive arching of back Log rolling Abnormal or prolonged parachute response 38. Abnormal Developmental Patterns after 1 year of age: W sitting knees flexed, legs extremely rotated Bottom shuffling Scoots along the floor Walking on tip toe or hopping Bleck not sitting independently @4 yrs, not walking @ 8 yrs bad 39. ASSO. CONDITIONS Hearing and visual problems Bladder and bowel control problems, digestive problems Sensory integration (gastroesophageal reflux) problems Failure-to-thrive, Feeding Skeletal deformities, dental problems problems Mental retardation and Behavioral/emotional learning disabilities in difficulties, some Communication Seizures/ epilepsy disorders 40. DIAGNOSIS Physical evaluation, Interview MRI, CT Scan EEG Laboratory and radiologic work up Assessment tools i.e. Peabody Development Motor Skills, Denver Test II 41. Treatment OF CEREBRAL PALSY 42. - No treatment to cure cerebral palsy. - Brain damage cannot be corrected. Crucial for children with CP: Early Identification; Multidisciplinary Care; and Support 43. I. Nonphysical TherapyThe earlier we start, the more improvement can be made -Health worker 44. A. General management - Proper nutrition and personal careB. Pharmacologic Intrathecal, Baclofen - control muscle spasms and seizures, Glycopyrrolate -control drooling Pamidronate -may help with osteoporosis. 45. Baclofen Oral delivery was common but sedation is more, so Intrathecal Baclofen Using a pump Delivered directly to the spinal fluid GABA agonist inhibits release of excitatory neurotransmitter at level of spinal cord It is commonly used in a starting dose of 1.25 - 2.5 mg BD orally To avoid brain effects 46. BOTOLUNIM TOXIN The toxin is produced by the anaerobic sporeforming bacterium Clostridium botulinum, of which eight immunologically distinct serotypes A, B, C1, C2, D, E, F, and G have been identified. Type A and B are used clinically in variousconditions like focal tissue spasms, blepharospam, dystonia, achalia, urology, cerebral palsy, cosmetic surgeries, toe clawing.Relief of athetosis and dystonia - is difficult occasionally levo-dopa for severe athetosis and carbamezepine for dystonia may be helpful. Thalamotomy for athetoid CP, stereotactic dentatomy and chronic cerebellar stimulation via implanted electrode .Multiple injection sites to avoid toxicity. acetylcholine-blocking chemical denervant Requires adjunctive therapy like splints, orthoses, casting, manual stretch, posturing The children in CT receive bilateral Botox injection @12 u/kg with topical anaesthesia and analgesic cover/ sedation 47. C. Surgery -To loosen joints,-Relieve muscle tightness, - Straightening of different twists or unusual curvatures of leg muscles- Improve the ability to sit, stand, and walk. 48. Selective posterior rhizotomy Best for : spastic diplegia, 4-8 yrs, no previous surgery, no contractures, no extra pyramidal signs Not done in hemi/ quadriplegia 49. How it Works The Sensory nerve fibers are exposed, then stimulated and the responses of the leg muscles are observed. Those that have an abnormal or excessive response are severed. Those with a normal response are left intact. Intensive rehabilitation is required after the surgery, usually up to six weeks, followed by physical therapy on an ongoing basis 50. Walker cpD. Physical Aids Orthosis, braces and splints - Keep limbs in correct alignment - Prevent deformities. - Ankle foot orthosis, knee ankle foot orthoses Positioning devices -Enable better postureWalkers, special scooters, wheelchairs - make it easier to move about. Active exercises - Passive ROM exercises - Passive stretching - BracingSpiral thigh brace 51. E. Special Education Rehabilitation - To meet the child's special needs - Improve learning. - Vocational training can help prepare young adults for jobs H. Other Treatment -Therapeutic electrical stimulation, Acupuncture, Hyperbaric therapy Massage Therapy might help 52. Cerebral palsyOrthopedic Procedures Usually multiple deformities at different joints Knowledge of complex effects each deformity has on other lower extremity jointsDiiferentiate between primary deformity : needs treatment compensatory deformity :can improve without intervention 53. Cerebral palsyPrerequisites for effective surgery Type : spastic Extent : hemiplegics / diplegics : good results quadriplegics : minimal improvement Age : 3- 12 years IQ : good Good upper limb function : for walking Underlying muscle power : not weak Walker / non-walker :walkersurgery hardly changes state but improves gait, to get him better from current state 54. Cerebral palsyTiming For Orthop Surgery For structural changes : Early e.g. Hip subluxation , usually 20, abduction