Cefpodoxime vs Cefixime in LRTI, IndianJPediatr
-
Upload
vikramsobti -
Category
Documents
-
view
344 -
download
0
description
Transcript of Cefpodoxime vs Cefixime in LRTI, IndianJPediatr
-
Indian Journal of Pediatrics, Volume 71June, 2004 517
Special Article
Correspondence and Reprint requests : Dr. A.K. Moharana, V-7,Naveen Shahdara, Delhi-110032. Fax : 91-11-26429471
Acute lower respiratory tract infections in children are aworldwide public health problem with an estimated 4million potentially preventable deaths every year.1 Untilrecently, penicillin and related drugs were the treatmentof choice for empiric therapy of pediatric lowerrespiratory tract infections. However, concerns over theemergence of penicillin and macrolide resistant strains ofStreptococcus pneumoniae, and beta-lactamase-producingstrains of Haemophilus influenzae and Moraxella catarrhalishave led physicians to turn increasingly towardsalternatives, such as third generation cephalosporins.2
Third generation cephalosporins retain sufficient activityto warrant use in selected pneumococcal infections, eventhose caused by completely penicillin-resistant strains.
Cefpodoxime proxetil is an orally administeredprodrug which is absorbed and de-esterified by theintestinal mucosa to release the third generationcephalosporin, cefpodoxime. Cefpodoxime is highlyactive against both Haemophilus influenzae and Moraxellacatarrhalis including -lactamase producing strains, with aminimum inhibitory concentration for 90% of testedstrains (MIC90) 1mg/L. It has also excellent coverageagainst Streptococcal spp, especially S. pneumoniae (bothpenicillin sensitive and resistant strains).3 Cefpodoximehas a similar potency to that of cefixime against gram verods, but with greater activity against gram +ve cocci; alsothe spectrum of activity is greater than that of cefuroxime,
Comparative Evaluation of Cefpodoxime Versus Cefiximein Children with Lower Respiratory Tract InfectionsJayati Sengupta, A.K. Mondal1, Piyush Jain2, P.D. Garg3, N.C. Mathur4 and A.K. Moharana5
Amri Hospitals, Kolkata, 1District Hospital, Howrah, Kolkata, 2Genesis Clinic, Delhi, 3Holy Child Hospital, Delhi,4Aditya Hospital, Hyderabad and 5Ranbaxy Laboratories Ltd, Delhi.
cefaclor (2nd generation cephems) and cephalexin (1st
generation cephem) against these microorganisms.Moreover, cefpodoxime is more active against H.influenzae including -lactamase producing strains thanamoxicillin/clavulanic acid.3
Cefpodoxime is stable towards the most commonlyfound plasmid mediated -lactamases and its broadspectrum of anti-bacterial activity encompassing bothgram negative and gram positive bacteria renders it apossible option for empirical use in a wide range of com-munity acquired infections in both adult and pediatricpatients. The extended plasma half life of cefpodoxime(1.9 to 3.7 h) permits twice daily administration.4 Inchildren aged 2 months to 18 years, the recommendeddose of 10 mg/kg/day of cefpodoxime suspension for 10days for the treatment of respiratory and urinary tractinfections and as well as those of the skin and soft tissueshas demonstrated a good bacteriological and clinicalefficacy. Cefpodoxime is well tolerated by pediatricpatients, with mild gastro-intestinal disturbances that areconsistent with those reported for other oralcephalosporins.5
Cefixime is another oral third generationcephalosporin, used in Respiratory Tract Infections inpediatric population. However, cefixime has poor efficacyagainst staphylococcus, and streptococci. Therefore, itshould be avoided if staphylococci or pneumococci cannot be ruled out.6 The present study was designed toassess the clinical cure and bacteriological eradicationrates and tolerability of cefpodoxime suspension and to
Abstract. Objective: The emergence of penicillin and macrolide resistant strains, responsible for Acute Lower RespiratoryTract Infections in children has offered third generation cephalosporins the platform to perform. The aim of the present studywas to evaluate two third generation oral cephalosporins for their empirical use in community acquired lower respiratory tractinfections in pediatric patients. An assessment of the clinical cure and bacteriological eradication rates and an overall tolerabilitywas made. Methods : It was a prospective, open, comparative, multicentric study. 776 children (Mean age 10 years) with LRTIswere included and randomly allotted to two groups respectively. A total of 396 children were given cefpodoxime susp 5 mg/kg b.i.d. and 380 patients on cefixime 4 mg/kg b.i.d. for 10-14 days. Results : At the end of therapy, the clinical success withcefpodoxime was 97% as against 86.8% with cefixime. Bacterial eradication was 93.4% with cefpodoxime and 82.9% withcefixime. Conclusion : Cefpodoxime has been found to be a well-tolerated and superior alternative to cefixime synergisticallydocumenting the extended spectrum of activity. [Indian J Pediatr 2004; 71 (6) : 517-521]E-mail : [email protected]
Key words : Cefpodoxime; Cefixime; LRTIs
-
Jayati Sengupta et al
518 Indian Journal of Pediatrics, Volume 71June, 2004
compare it with another cefixime in children with LowerRespiratory Tract Infections (LRTIs) like, AcuteExacerbations of Chronic Bronchitis (AECB) andCommunity Acquired Pneumonia (CAP).
MATERIALS AND METHODS
Study DesignIt was a prospective, open, comparative multicentricstudy. In addition, the Institutional Review Board orIndependent Ethics Committee of each site approved thestudy protocol and the legal guardians of all participatingpatients provided written informed consent prior toenrollment.
PatientsChildren (6 months to 12 years) of either sex withdiagnosis of Lower Respiratory Tract Infections (LRTIs),which included patients with Community AcquiredPneumonia, and Acute Exacerbations of ChronicBronchitis were included in the study.
The Lower Respiratory Tract Infection wascharacterized by increased cough, sputum productionand dyspnoea. Sputum had to be purulent or had toshow a change in the character of sputum from the steadystate level (i.e., patient status before current episode ofLower Respiratory Tract Infections). Fever could bepresent. Patients with a history of hypersensitivity tocefpodoxime, cefixime or any other member ofcephalosporin class of antimicrobial agents were excludedfrom the study.
Study ProcedurePatients fulfilling the inclusion criteria received eithercefpodoxime suspension 5 mg/kg b.i.d or cefixime 4 mg/kg b.i.d for 10-14 days without regard to meals. Patientswere evaluated on 1st day through the end of therapy (on10th day).
Patients requiring antacids containing aluminium andmagnesium salts were administered 8 hours before orafter cefpodoxime or cefixime administration. If thesymptoms were not controlled or worsened, additionalmedications could be given depending at the discretion ofthe investigator and this rescue medication was recordedin the Case Record Form.
Patients were considered to be compliant with thestudy medication if at least 80% of study medicationswere taken according to the prescribed regimen.Otherwise patient was considered to be non-compliant.
Evaluation VisitsThe physician examined the patient and recorded foradherence to therapy, any adverse drug reactions and theclinical response on the following days:
Visit 0: Day 0, study admission visit ; Visit 1: Day 5-7,midtherapy visit ; Visit 2: Day 10-14, end of therapy.Symptoms of LRTI and fever were assessed at each visit.Patients were also monitored for any complications.
Efficacy AssessmentThe main outcome measures were:
1. Bacteriological and clinical response of signs andsymptoms of respiratory tract infections determined atend of therapy determined. 2. No. of cases in whichchange of antibiotics was needed. 3. Physician Globalevaluation of patient condition (using a 5-point scale) ;1=Excellent, 2=Very Good, 3 = Good, 4= Fair, 5 =Poor
Clinical Outcome was defined as follows:Clinical cure (Defined as complete resolution of signs
and symptoms); Improved (If clinical signs & symptomsdiminished but did not completely resolve); Failure (if thesigns and symptoms worsened, persisted or reappeared).
Safety AssessmentPatients were closely monitored for clinical adverseevents. The severity of clinically adverse events wascategorized by the investigators as mild, moderate, orsevere. The investigators also classified the relationship ofadverse events to the study drugs as either certainly,probably, or possibly drug related; not drug related; orwith an unknown relationship to the study drug. Globalassessment of overall tolerability was also recorded on a5-point scale (1=excellent, 2 =very good, 3=good, 4=fair,5=poor).
Statistical AnalysisAge is presented as mean SD. Symptom assessment wasdone with actual patient numbers. Rest of the data ispresented as percentages. Comparison of signs andsymptoms of disease before and after therapy was doneby paired t-test. The limit of significance was set at pvalue < 0.05.
RESULTS
Patient Characteristics396 patients included in the cefpodoxime arm of thestudy comprised 242 males and 154 females with a meanage of 10.402.85 years and 380 patients in the cefiximearm comprised 221 males and 159 females (Table 1). Allchildren had one or more pretreatment symptoms ofrespiratory tract infection; the most frequent were cough,increased, thickened, foul odour sputum, dyspnoea, andcrepitations or wheeze on auscultation. Many childrenalso had signs of systemic infection: fever, chills and chestpain.
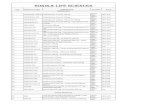
TABLE 1. Demographic Profile and Baseline Characteristics ofPatients Enrolled
Characteristic Cefpodoxime Group Cefixime Group
Total no. of patients 396 380 Male 242 221 Female 154 159
Age (years)* 10.402.85 10.852.86
*Values are mean SD.
-
Comparative Evaluation of Cefpodoxime Versus Cefixime
Indian Journal of Pediatrics, Volume 71June, 2004 519
Efficacy Parameter Assessment
Both cefpodoxime and cefixime caused a significantimprovement in all the signs and symptoms after a 10-14day treatment period. However, between-the-groupcomparisons showed that the reduction in thesesymptoms was better with cefpodoxime arm compared tocefixime group. The percentage decrease in signs andsymptoms at the end of therapy in the two treatmentgroups is shown in Fig 1.
The clinical success (clinical cure + improvement) atthe end of therapy was significantly better withcefpodoxime group: 97% with cefpodoxime versus 86.8%with cefixime (Table 2). Bacteriological eradication(eradication + presumed eradication) was seen in 93.4% ofpatients in cefpodoxime group and 82.9% of patients incefixime group. In 7% of patients, clinical symptomsworsened, and they were shifted to cefpodoxime arm intheir second visit, where they showed excellent response.
Global Assessment
94% physicians rated treatment with cefpodoxime asexcellent to good versus 81% with cefixime (Table 3). Thesame pattern of response was observed in the patientsassessment as well, with 92% patients/patients guardiansrating the treatment as excellent to good in cefpodoximegroup versus 80% in the cefixime group (Table 4).
Adverse Effect ProfileGastrointestinal side effects were the only adverse eventsreported, most of which were mild and self-limiting innature in the cefpodoxime group. Therefore, none of thepatients withdrew from the therapy. However, loosemotion was more commonly reported (13%) in the
Fig. 1. Comparative evaluation of symptom resolution
TABLE 2. Comparative Clinical and Bacteriological Outcomes
Clinical Cefpodoxime Cefiximeoutcome Group Group
Cure 61.3% 43%Improvement 35.7% 43.8%Clinical Success 97.0% 86.8%
(Cure + Improvement)Failure 3.0 % 13.2%
Bacteriological outcomeEradication 93.4% 82.9%
(+presumed eradication)Failure 6.6% 17.1%
TABLE 3. Physicians Global Assessment on Clinical Efficacy.
Cefpodoxime Cefixime
Excellent 50% 36%Very good 33% 20%Good 11% 25%Fair 6% 8%Poor 0% 1%
TABLE 4. Patients Global Assessment on Clinical Efficacy
Cefpodoxime Cefixime
Excellent 48% 32%Very good 31% 24%Good 13% 24%Fair 7% 8%Poor 1% 2%
-120.00%
-100.00%
-80.00%
-60.00%
-40.00%
-20.00%
0.00%
Coug
h
Sput
um Q
uant
ity
Sput
umCo
nsist
ency
Sput
umAp
pear
nce
Dysp
noea
Feve
r
Chills
Foul
Odo
ur
Ches
t Pai
n
Crep
itatio
ns
Whe
eze
Symptoms
% C
hang
e
CepodoximeCefixime
-
Jayati Sengupta et al
520 Indian Journal of Pediatrics, Volume 71June, 2004
cefixime arm, compared to 3.4% in the cefpodoxime arm.Overall tolerability of study medications was assessed
by physicians at the end of the study. 95% rated thetolerability of cefpodoxime as excellent to good versus79% of cefixime. Similarly, 92% of the patients ratedtolerability of cefpodoxime as excellent to good versus78% in cefixime group (Figs. 2 and 3)
DISCUSSION
Acute respiratory infections include acute exacerbationsof chronic bronchitis (AECB), pneumonia, bronchitis,bronchiolitis, sinusitis, of which lower respiratory tractinfections account for high morbidity and mortality.7 Theoverall impact of LRTIs in developing countries is 12times greater than in developed countries.8 In India, acuterespiratory infections (ARIs) are responsible for 1 milliondeaths and it has a reported occurrence of 3-7 attacks ofARIs/child/year, of which 10-15% are due to lowerrespiratory tract infections.9 Choice of antibiotics in
various respiratory ailments was a simple matter untilfew years ago, as gram positive organisms (mainlyS.pneumoniae) were predominantly implicated in LRTIs.However, with increasing recognition of gram negativeorganisms and compromised efficacy of penicillins andmacrolides with emergence of resistant bacterial species,choice of an antibiotic has become more complicated.9
Cefpodoxime proxetil is an oral third generationcephalosporin with a broad spectrum of antibacterialactivity. The drug has in vitro activity against manycommon gram positive and gram negative pathogensassociated with common pediatric infections, making thedrug a useful option for empirical therapy.10
Findings from this multicenter study indicate thatcefpodoxime is an effective antimicrobial agent for LRTIin chidren and its efficacy is comparable to that ofcefixime. There was a marked improvement in all thesigns and symptoms associated with LRTIs over 10-14days of the study. Clinical success was obtained in 97%patients in cefpodoxime group versus 86.8% in cefixime
Fig 3. Global tolerability assessment by patients
Fig. 2. Global tolerability assessment by physicians
30%
39%
23%
7%
1%
11%
35%32%
14%
8%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
Excellent Very good Good Fair Poor
Grading of tolerability
% p
atie
nts
CepodoximeCefixime
32%
43%
20%
4%
1%
14%
33% 32%
13%
8%
0%
5%
10%
15%
20%
25%
30%
35%
40%
45%
Excellent Very good Good Fair Poor
Grading of tolerability
% p
hysi
cian
s
CepodoximeCefixime
-
Comparative Evaluation of Cefpodoxime Versus Cefixime
Indian Journal of Pediatrics, Volume 71June, 2004 521
group and bacteriological eradication was achieved in93.8% patients on cefpodoxime versus 82.9% of patientson cefixime.
The results of this study are in line with those of earliermulticentre, randomized, comparative clinical trialscarried out to assess the efficacy of cefprozil in thetreatment of common pediatric infections. In randomizedcontrolled trials conducted in children with acute otitismedia, oral cefpodoxime proxetil 8 to 10 mg/kg/day for5 to 10 days was at least as effective or better as standardregimens of amoxicillin/clavulanic acid, cefixime,cefuroxime axetil or cefaclor as assessed by either clinicalor bacteriological criteria. The clinical and bacteriologicalefficacy of 5 day treatment with cefpodoxime wasclinically and bacteriologically similar to 10 day course ofpenicillin V in the treatment of children with pharyngitisand/or tonsillitis. In randomized controlled clinical trialsin children with LRTIs, clinical and bacteriologicalefficacy rates achieved with cefpodoxime proxetil treat-ment were similar to those produced by cefuroxime axetiland amoxicillin/clavulanic acid. Cefpodoxime proxetilalso demonstrated clinical efficacy in pediatric patientswith skin and soft tissue infections.11
Schito GC et al12, in their multicentric survey, fromthree European countries tried to monitor the activity ofwidely used oral antibiotics against common respiratorypathogens. Studies were conducted in Italy, Spain, andAustria to monitor resistance patterns among respiratoryStreptococcus pneumoniae, H influenzae, M catarrhalis, Streppyogenes, Staph aureus and K pneumoniae to cefaclor,cefuroxime, cefixime, cefpodoxime and macrolides.Cefpodoxime was more potent than cefaclor and cefixime,against pneumococci, especially strains with decreasedsensitivity to penicillin, and more active than cefaclor andcefuroxime against gram ve respiratory pathogens.Pneumococci and staphylococci displayed a very highlevel of in vitro macrolide resistance. The investigatorssuggested that cefpodoxime represents an appropriatechoice in the treatment of community acquiredrespiratory tract infections in European countries.
Liu P and co-workers13 reported significantly highercefpodoxime concentration in interstitial tissues, likelungs tissues, in their comparative evaluation ofcefpodoxime versus cefixime. Their findings indicate that,taking into account pharmakokinetic/dynamicconsiderations, cefpodoxime is likely to be moreefficacious than cefixime, due to its greater tissuepenetration. Our study findings support this hypothesis,by showing significantly better clinical and bacteriologicaloutcome with cefpodoxime compared to cefixime.
The twice-daily regimen of cefpodoxime also wasacceptable to most patients as with cefixime, andcompliance to these medications was also good. It hasbeen seen that patient compliance is inversely related to
the frequency of dosing and directly related to the efficacyof the drug.14 Most of the other standard antimicobialsused have a thrice or four times daily regimen.
Cefpodoxime was better tolerated than cefixime by ourstudy population. The side effects observed withcefpodoxime were of mild intensity and no patientwithdrew from the study due to adverse events. Thegastrointestinal adverse events seen in the present studycorrelate with those reported in earlier studies. Highergastro-intestinal side effects associated with cefixime, likeloose motion was due to alteration of the normal flora inthe gut.
CONCLUSION
Cefpodoxime proxetil is a well tolerated and superioralternative to the earlier oral third generation cefixime forLRTIs in children. Moreover, its expanded spectrum ofactivity , and better tolerability as compared to cefiximeproves the fact that it should be accepted as a first-lineanti-microbial in pediatric LRTIs.
REFERENCES
1. Klein M. Multicenter trial of cefpodoxime proxetil vs.amoxicillin/clavulanate in acute lower respiratory tractinfections in children. International Study Group. Pediatr InfectDis J 1995; 14(Suppl 4) : S19-22.
2. Geddes AM. Cefpodoxime proxetil in the treatment of lowerrespiratory tract infections. Drugs 1991; 42 (Suppl 3) : 34-40.
3. Frampton JE, Brogden RN, Langtry HD, Buckley MM.Cefpodoxime Proxetil : A review. Drugs 1992; 44(5) : 889-917.
4. Borin MT. A review of the pharmacokinetics of cefpodoximeproxetil. Drugs 1991; 42 (Suppl 3) : 13-21.
5. Fujji R. Clinical trials of cefpodoxime proxetil suspension inpediatrics. Drugs 1991; 42(Suppl 3): 57-60.
6. Bluer K et al. Text Book of Therapeutics, Drugs and DiseaseManagement, 7th edn. Pg 1415.
7. Reddiah VP, Kapoor SK. Acute respiratory infections in ruralunder fives: Indian J Pediatr 1988; 55 : 424-426.
8. Nag VL, Ayyagari A. Indian J Chest Dis Allied Sci 2001; 43(1): 13-17.
9. Arora A, Ajay L, Sinha RK et al. An extended epidemiologicalstudy of prevalence and resistance of respiratory pathogens toantibiotics in AECB patients. The Antiseptic 2003; 4 : 119-122.
10. Geddes AM. Cefpodoxime proxetil in the treatment of lowerrespiratory tract infections. Drugs 1991; 42 : (Suppl.3) : 34-40.
11. Fulton B, Perry CM. Cefpodoxime proxetil: Pediatr Drugs 2001;3(2): 137-158.
12. Schito GC et al. Antibacterial activity of oral antibiotics againstcommunity-acquired respiratory pathogen from threeEuropean countries. J Antimicrob Chemother 2002; 50 (Suppl)7-11.
13. Liu P, Muller M, Grant M et al. Interstitial tissue concentrationsof cefpodoxime. J Antimicrob Chemother 2002; 50 : 19-22.
14. In Sackett DL, Haynes RB, eds. Compliance with TherapeuticRegimens. Baltimore, MD: Johns Hopkins University Press,1976; 293p.