Cataract Art Science
description
Transcript of Cataract Art Science


I

II
OUTLINE OF MAJOR SUBJECTS
Chapter 1: Surgical Anatomy of the Human Lens
Chapter 2: Indications and Preoperative Evaluation
Chapter 3: IOL Power Calculation In Standard
and Complex Cases - Preparing for Surgery
Chapter 4: Preventing Infection and Inflammation
Chapter 5: Proceeding with the Operation
Chapter 6: Phacoemulsification - Why So Important?
Chapter 7: Preparing for the Transition
Chapter 8: Instrumentation and Emulsification Systems
Chapter 9: Mastering Phacoemulsification -
The Advanced, Late Breaking Techniques
Chapter 10: Focusing Phaco Techniques on the Hardness
of the Nucleus
Chapter 11: Complications of Phacoemulsification
Intraoperative - Postoperative
Chapter 12: Cataract Surgery in Complex Cases
Chapter 13: Manual Extracapsular Techniques of Choice
Planned ECCE - Small Incision ECCE
Chapter 14: The New Cataract Surgery Developments
This book was created and written byProfessor Boyd at Miramar Plaza Towers,overlooking the Panama Canal, the PacificOcean and the city of Panama.
Project Director: Andres Caballero, Ph.DProduction Manager: Kayra MejiaPage Design andTypesetting: Kayra Mejia
Laura DuranArt Design: Eduardo ChandeckSpanish Translation: Cristela F. Aleman, M.D.Medical Illustrations: Stephen F. Gordon, B.A.
Trina Fennell, M.S. Samuel Boyd, M.D.
Sales Manager: Tomas MartinezMarketing Manager: Eric PinzonCustomer ServiceManager: Miroslava BonillaInternationalCommunications: Joyce Ortega
ISBN Nº 9962-613-03-5
©Copyright, English Edition, 2001.Highlights of Ophthalmology Int'lP.O. Box 6-3299, El DoradoCity of KnowledgeClayton, Bldg. 207Panama, Rep. of Panama
Tel: (507)-317-0160FAX: (507)-317-0155E-mail: [email protected]
All rights reserved and protected byCopyright. No part of this publication may be repro-duced, stored in retrieval system or transmitted inany form by any means, photocopying, mechanical,recording or otherwise, nor the illustrations copied,modified or utilized for projection without the prior,written permission of the copyright owner.
Printed: Bogota, ColombiaSouth America

III
ACKNOWLEDGMENTS
All the text in this Volume has been written by the author. I am very much indebted
to the Master Consultants and to all Guest Experts who are listed in this Front Section
of the ATLAS. They are all highly recognized, prestigious authorities in their fields and
provided me with most valuable information, perspectives and insights.
The production of this ATLAS is a major enterprise. In addition to our dedicated
staff at HIGHLIGHTS, three of my most valuable collaborators have been vital to its
success: Robert C. Drews, M. D., as Co-Editor of the English Edition; Cristela
Ferrari de Aleman, M.D., an expert in phacoemulsification who advised me in all the
technical stages of the step-by-step small incision surgical procedures and Samuel
Boyd, M.D., for his strong support, valuable advice derived from his expertise in all the
vitreoretinal techniques related to cataract surgery.
Among my closest collaborators in HIGHLIGHTS, Andres Caballero, Ph.D., the
Project Director and Kayra Mejia, my editorial right hand Production Manager of many
years have gone the extra mile to accomplish a very difficult task in production of this
work.
To each person mentioned in this page, on behalf of the thousands of readers of
HIGHLIGHTS, I express my profound recognition and gratitude.

IV
DDDDDEDICATION
This 25th Volume of the Atlas and Textbooks of HIGHLIGHTS isdedicated to my colleagues in 106 nations worldwide who faithfully read theHIGHLIGHTS in seven major languages.
May "THE ART AND THE SCIENCE OF CATARACT SURGERY"contribute to your further understanding of what is best for your patients.May it also help you to master the "state of the art" techniques in yourcontinuous quest for the right answers. May it provide you with insights inyour efforts to rehabilitate vision to millions of people who are still blindfrom cataract, a curable disease.
"The Art and the Science of Cataract Surgery" is also dedicated to thecountless ophthalmic surgeons who, through combined efforts with leadersand scientists in industry, have made of modern cataract surgery the safestand most effective major operation in the field of medicine.
And, by all means, to the great innovators each of whom developed anew era for cataract surgery in their time. Symbolically, IGNACIOBARRAQUER, M.D., whose innovation of intracapsular extraction bymechanized suction in 1917 resulted in the first practical and efficientmethod to remove a cataract without vitreous loss. To JOAQUINBARRAQUER, M.D., for his pioneering work in rendering ophthalmicsurgery under the microscope a feasible and practical new method leadingto the era of microsurgery. To CHARLES KELMAN, M.D., who, byproviding us with phacoemulsification, started the new era of small incisionsurgery. And to HAROLD RIDLEY, M.D., the symbol of intraocular lensimplantation.
The recognition to the great innovators is for their ingenuity and fortheir courage. All innovators stimulate opposition. They all encounteredstrong opposition but they overcame it through their courage and results.
BENJAMIN F. BOYD, M.D., F.A.C.S.

V
AUTHOR AND
EDITOR-IN-CHIEF
BENJAMIN F. BOYD, M.D., D.Sc. (Hon), F.A.C.S.
Doctor Honoris CausaImmediate Past President, Academia Ophthalmologica Internationalis
Honorary Life Member, International Council of Ophthalmology
Recipient of the Duke-Elder International Gold Medal Award (Interna-tional Council of Ophthalmology), the Barraquer Gold Medal (Barcelona),the First Benjamin F. Boyd Humanitarian Award and Gold Medal for theAmericas (Pan American), the Leslie Dana Gold Medal and the NationalSociety for Prevention of Blindness Gold Medal (United States), MoacyrAlvaro Gold Medal (Brazil), the Jorge Malbran Gold Medal (Argentina),the Favaloro Gold Medal (Italy).
Recipient of The Great Cross Vasco Nuñez de Balboa Panama's HighestNational Award.
Founder and Chief Consultant, Ophthalmology Center of Clinica Boyd, Panama,R.P.; Editor-in-Chief, Highlights of Ophthalmology's ten Editions (Brazilian, Chinese,English, German, Indian, Italian, Japanese, Middle East and Spanish); Author, Highlights ofOphthalmology's Atlas and Textbooks (25 Volumes); Diplomate, American Board ofOphthalmology; Past-President (1985-1987) and Executive Director ((1960-1985) PanAmerican Association of Ophthalmology; Fellow, American Academy of Ophthalmology;Fellow, American College of Surgeons; Guest of Honor, American Medical Association,1965; Guest of Honor, American Academy of Ophthalmology, 1978 and Barraquer Institutein Barcelona, 1982 and 1988; Doctor Honoris Causa of Five Universities; Recipient of theGreat Cross of Christopher Columbus, Dominican Republic's highest award, for "Contribu-tions to Humanity"; Founding Professor of Ophthalmology, University of Panama School ofMedicine (1953-1974); Former Dean and Chief, Department of Surgery, University ofPanama School of Medicine (1969-1970); O'Brien Visiting Professor of Ophthalmology,Tulane University School of Medicine, New Orleans, 1983; Honorary Professor of Ophthal-mology at Four Universities; Past-President, Academy of Medicine and Surgery of Panama;Honor Member, Ophthalmological Societies of Argentina, Bolivia, Brazil, Canada, Colom-bia, Costa Rica, Chile, Dominican Republic, Guatemala, Mexico, Paraguay, Peru; Recipientof the Andres Bello Silver Medal from the University of Chile for "ExtraordinaryContributions to World Medical Literature."

VI
MASTER CONSULTANTS
JOAQUIN BARRAQUER, M.D., F.A.C.S., Director and Chief Surgeon,Barraquer Ophthalmology Center; Barcelona, Spain. Professor of Ophthalmology,Autonomous University of Barcelona, Spain. Chair, Academia OphthalmologicaInternationalis.
MICHAEL BLUMENTHAL, M.D., Director, Ein Tal Eye Center, Israel.Professor of Ophthalmology, Sidney A. Fox Chair in Ophthalmology, Tel AvivUniversity. Past President, European Society of Cataract and Refractive Surgery.
EDGARDO CARREÑO, M.D., Assistant Professor of Ophthalmology,University of Chile; Director, Carreño Eye Center, Santiago, Chile.
VIRGILIO CENTURION, M.D., Chief of the Institute for Eye Diseases, SaoPaulo, Brazil.
JACK DODICK, M.D., Chief, Department of Ophthalmology, Manhattan Eyeand Ear Hospital, New York. Clinical Professor of Ophthalmology, ColumbiaUniversity College of Physicians and Surgeons, New York.
CRISTELA FERRARI ALEMAN, M.D., Associate Director, Cornea andAnterior Segment, Boyd Ophthalmology Center. Clinical Professor, Universityof Panama School of Medicine, Panama, Rep. of Panama.
I. HOWARD FINE, M.D., Clinical Associate Professor of Ophthalmology,Oregon Health Sciences University. Founding Partner, Oregon Eye SurgeryCenter.
HOWARD V. GIMBEL, M.D., MPH, FRCSC, Professor and Chairman,Department of Ophthalmology, Loma Linda University, California; ClinicalAssistant Professor, Department of Surgery, University of Calgary, Alberta,Canada; Clinical Professor, Department of Ophthalmology, University of California,San Francisco, California; Founder and Director, Gimbel Eye Centre in Calgary,Albert, Canada.
RICHARD LINDSTROM, M.D., Medical Director, Phillips Eye Center forTeaching and Research. Clinical Professor,, University of Minnesota, Minneapolis.
MAURICE LUNTZ, M.D., Chief of Glaucoma Service, Manhattan Eye and EarHospital, New York. Clinical Professor of Ophthalmology, Mt. Sinai School ofMedicine, New York.
OKIHIRO NISHI, M.D., Director of Jinshikai Medical Foundation, Nishi EyeHospital, Osaka, Japan.
MIGUEL A. PADILHA, M.D., Professor and Chairman, Department ofOphthalmology, School of Medical Sciences of Volta Redonda, Rio de Janeiro.Professor, Graduate Course of the Brazilian Society of Ophthalmology andDirector, Central Department of Ophthalmology, Brazilian College of Surgeons.Former President, Brazilian Society of Cataract and Intraocular Implants.

VII
CO-EDITORENGLISH EDITION
Robert C. Drews, M.D., F.A.C.S., F.R.C.Ophth.
Professor Emeritus of Clinical Ophthalmology, Washington University School ofMedicine, St. Louis, Missouri.
President Elect of the American Ophthalmological Society
Gold Medal of Pan-American Association of Ophthalmology; Rayner Medal, UnitedKingdom Intraocular Implant Society; Binkhorst Medal, American IntraocularImplant Society; Gold Medallion of the National Academy of Science of Argentina;The Montgomery Medal, Irish Ophthalmological Society; Gold Medal of theUniversity of Rome; Gold Medal of the Missouri Ophthalmological Society.
Former Chief of Surgery, Bethesda General Hospital, St. Louis, Missouri, andFormer Chief of the Section of Ophthalmology, Bethesda General Hospital, St. Louis andSt. Luke's Hospital, St. Louis, Missouri. Past Chairman of the Council of the AmericanOphthalmological Society, Former member of the American Board of Ophthalmology,and of the Board of Trustees, Washington University in St. Louis. Past President of thePan American Association of Ophthalmology, International Ophthalmic MicrosurgeryStudy Group, International Intraocular Implant Club, American Intra-Ocular ImplantSociety, Southern Medical Association, Section on Ophthalmology, MissouriOphthalmological Society, Missouri Association of Ophthalmology, St. LouisOphthalmological Society, St. Louis Society for the Blind, Past Vice President, AmericanAcademy of Ophthalmology.
Named Lectures: the Luedde Memorial Lecturer, St. Louis University School ofMedicine; Rayner Lecture, United Kingdom Intraocular Implant Society; BinkhorstLecture, American Intraocular Implant Society; C. Dwight Townes Memorial Lecture,Louisville Kentucky; The Montgomery Lecture, Dublin, Irish Ophthalmological Society;Boberg-Ans Lecture, Copenhagen, Denmark, ESCRS; G. Victor Simpson Lecture,Washington DC; Gradle Lecture, PAAO; Joseph P. Bryan Glaucoma Lecture, Durham,North Carolina.

VIII
GUEST EXPERTS
EVERARDO BAROJAS, M.D., Dean, Prevention of Blindness and Rehabilitationof Sight Society, Mexico, D.F.
PROF. RUBENS BELFORT JR., M.D., Professor and Chairman, Departmentof Ophthalmology, Federal University of São Paulo (Escola Paulista de Medicina-Hospital São Paulo), Brazil; Chair, Academia Ophthalmologica Internationalis.
RAFAEL CORTEZ, M.D., Director, Ophthalmic Surgery Center (CECOF),Caracas, Venezuela.
FRANCISCO GUTIERREZ C., M.D., Ph.D, Anterior Segment Surgery andPediatric Ophthalmologist Specialist, Department of Ophthalmology, HospitalGeneral de Segovia, Spain. Former Fellow of Ramon Castroviejo, M.D.
FRANCISCO MARTINEZ CASTRO, M.D., Associate Professor ofOphthalmology, Autonomous University of Mexico. Consultant in Uveitis, Instituteof Ophthalmology "Conde de Valenciana" and Seguro Social Medical Center,Mexico, D.F.
JUAN MURUBE, M.D., Professor of Ophthalmology, University of Alcala andChairman, Department of Ophthalmology, Hospital Ramon y Cajal, Madrid, Spain.
DAVID McINTYRE, M.D., Head, McIntyre Clinic and Surgical Center, Bellevue,Washington.
CARLOS NICOLI, M.D., Associate Professor of Ophthalmology, University ofBuenos Aires, Argentina. Director, "Oftalmos" Institute.
FELIX SABATES, M.D., Professor and Chairman, Department of Ophthalmology,University of Missouri, Kansas City School of Medicine, Missouri.
JUAN VERDAGUER, M.D., Academic Director, Los Andes OphthalmologicalFoundation, Santiago, Chile; Professor of Ophthalmology, University of Chile;Professor of Ophthalmology, University of Los Andes; Past President, Pan AmericanAssociation of Ophthalmology.
LIHTEH WU, M.D., Associate Surgeon in Vitreoretinal Diseases, Instituto deCirugia Ocular, San Jose, Costa Rica. Consultant in Vitreoretinal Diseases,Department of Ophthalmology, Hospital Nacional de Niños, San Jose, Costa Rica.

IX
CONTENTS
FOCUSING AND OVERVIEW OF WHAT IS BEST
Tackling the ChallengesRole of Small Incision Manual ExtracapsularsIOL's of ChoiceThe Best Phaco Techniques
CHAPTER 1
SURGICAL ANATOMY OF THE HUMAN LENSCLINICAL APPLICATIONS
Behaviour of Different Cataracts 5Anatomical Characteristics of Different Types of Cataract 7How Cataracts Respond Differently 7Incidence and Pathogenesis 8
CHAPTER 2
INDICATIONS FOR SURGERY -PREOPERATIVE EVALUATION
INDICATIONS 11Role of Quality of Life 11The Role of Visual Acuity 11Contrast Sensitivity and Glare Disability 12
Contrast Sensitivity Characteristics 13Relation of Glare to Type of Cataract 14Evaluation of Macular Function 15
PREOPERATIVE GUIDELINES IN COMPLEX CASES 21How to Proceed in Patients with Retinal Disease 21
The Importance of Pre-Op Fundus Exam 21Cataract Surgery in Diabetic Patients 21
Evaluating Diabetics Prior to Cataract Surgery 21Importance of Maintaining the Integrity of the Lens Capsule 24Significant Increase in Complications Following Cataract Surgery 24Appropriate Laser Treatment 25Main Options in Management of Co-existing Diabetic 27
Retinopathy and CataractCataract Surgery and Age-Related Macular Degeneration 28
RETINAL BREAKS AND RETINAL DEGENERATIONS 28 PRIOR TO CATARACT SURGERY
Cataract Surgery in Patients with Uveitis 31Method of Choice 32Diagnosing the Type of Uveitis in the Pre-Operative Phase 32Preoperative Management 32The Intraocular Lens 33
Cataract Surgery in Adult Strabismus Patients 33Preoperative Judgment 33

X
CHAPTER 3
PREPARING FOR SURGERY 37
Making Patients Confident 37Patients Encounter with the Physician 37Ingredients of a Strong Relationship 38Evaluating the Patient's Cataract 38Approaching the Day of Surgery 39Patient's Expectations 39
IOL POWER CALCULATION IN STANDARD 39
AND COMPLEX CASES
Postop Refractive Errors No Longer Admissible 40The Challenge of the Complex Cases 43The Most Commonly Used Formulas 44Main Causes of Errors 44
Targeting Post-Op Refraction 45Monocular Correction 45Binocular Correction 46
Good Vision in the Non-Operated Eye 46When Cataracts in Both Eyes 46
IOL POWER CALCULATION IN COMPLEX CASES 47Specific Methods to Use in Complex Cases 47Practical Method for Choosing Formulas in Complex Cases 47High Hyperopia 47
The Use of Piggyback Lenses in Very High Hyperopia 48High Myopia 49DETERMINING IOL POWER IN PATIENTS WITH 49 PREVIOUS REFRACTIVE SURGERY
Methods Most Often Used 52The Clinical History Method 52The Trial Hard Contact Lens Method 53 Example as Provided by Holladay 53The Corneal Topography Method 54
THE IMPORTANCE OF DETECTING IRREGULAR 54 ASTIGMATISMIOL POWER CALCULATION IN PEDIATRIC CATARACTS 54
Different Alternatives 55Alternatives of Choice 55
IOL POWER CALCULATION FOLLOWING VITRECTOMY 57
CHAPTER 4
PREVENTING INFECTION AND INFLAMMATION
Use of Antiseptics, Antibiotics and Antiinflammatory Agents 63Effective Preoperative Antibiotic Treatments 63Regimens Recommended 64Gills Formulas to Prevent Infection 64
1) For High Volume Cataract Surgery 642) Non-Complex, Effective and Safe Alternative for 65
Prevention of Infection

XI
CHAPTER 5
PROCEEDING WITH THE OPERATION
PREPARATION, SEDATION AND ANESTHESIA 71Preparation of Patient 71Sedation 71Pupillary Dilation 72
ANESTHESIA 72Topical 72Selection of Anesthetic Method 72Unassisted Topical Anesthesia 74The Anesthetic Procedure of Choice 75
Technique for Irrigation of Lidocaine in AC 75Injection of Viscoelastic 75What Can be Done with the Combined Anesthesia 75Side Effects of the Combined Anesthesia 75How to Manage Patients Who Feel Pain and Discomfort 75
PHOTOTOXICITY IN CATARACT SURGERY 75
CHAPTER 6
PHACOEMULSIFICATION - WHY SO IMPORTANT?
COMPARING PLANNED EXTRACAPSULAR WITH 83PHACO EXTRACAPSULAR
ADVANTAGES OF THE PHACO TECHNIQUE 83MAIN TECHNICAL DIFFERENCES ASSOCIATED WITH PHACO 84LIMITATIONS OF PHACOEMULSIFICATION 86
CHAPTER 7
PREPARING FOR THE TRANSITION
GENERAL OVERVIEW AND STEP BY STEP CONSIDERATIONS 93Equipment - Dependent and Phase-Dependent Technique 93Mental Attitude 93
UNDERSTANDING THE PHACO MACHINE 94Becoming Familiar with the Equipment 94Two Hands, Two Feet and Special Sounds 95Main Elements of Phaco Machines - Their Action on Fluid Dynamics 95
COMPARISON OF SURGICAL TECHNIQUES FOR 96TRANSITION VS EXPERIENCED SURGEONSTechniques Which Are the Same for the Transition and for 96Advanced SurgeonsTechniques that Vary According to the Skill of the Surgeon 96

XII
SURGICAL TECHNIQUE IN THE TRANSITION 97Anesthesia 97The Incision 97How to Make a Safe Transition from Large to Small Incision 97Role of Conjunctival Flap 101Anterior Capsulorhexis 102Hydrodissection 104
THE MECHANISM OF THE PHACO MACHINE 106Getting Ready to Use Phaco During Transition 106Optimal Use of the Phaco Machine 106The Rationale Behind It - Main Functions 106Parameters of the Phaco Machine 112How to Program the Machine for Optimal Use 114Fluid Dynamics During Phaco 114Fluidics and Physics of Phacoemulsification 116Importance of and Understanding the Surge Phenomenon 119Lessening Intraoperative 121Complications from the Surge 121
NUCLEUS REMOVAL - APPLICATION OF PHACO 123FRACTURE AND EMULSIFICATION 123
The Divide and Conquer Technique 124Emulsification of the Nuclear Fragments 126
FINAL STEPS 126Aspiration of the Epinucleus 126Aspiration of the Cortex 126Intraocular Lens Implantation 128Removal of Viscoelastic 128Closure of the Wound 129What to Do if Necessary to Convert 130Testing the Wound for Leakage 131Immediate Postoperative Management 131
CHAPTER 8
INSTRUMENTATION AND EMULSIFICATION SYSTEMS
INSTRUMENTATION 137Eye Speculum 137Fixation Ring 137Knives and Blades 137
Hydrodissection Cannula 140Cystotomes or Capsulorhexis Forceps 141Nuclear Manipulators or Choppers (Second Instrument) 142Forceps and Cartridge Injector Systems for Insertion of 144 Foldable Intraocular Lenses
THE PHACO PROBES AND TIPS 147Phaco Tips 148Surgical Principles Behind the Different Phaco Tips 149
PHACOEMULSIFICATION SYSTEMS 150The Alcon Legacy 150The Allergan Sovereign 150The Bausch & Lomb - Storz Millennium 150

XIII
The Pulse and Burst Modes 151Differences Between Them 151
Clinical Applications of the Pulse Mode 152Clinical Applications of the Burst Mode 154
Its Role in Transition to Chopping 154Advances with the Sovereign Phaco System 154
CHAPTER 9
MASTERING PHACOEMULSIFICATIONThe Advanced, Late Breaking Techniques
General Considerations 159Trauma-Free Phacoemulsification 159Faster Operations 160
Do They Sacrifice Patient Care? 160Readiness and Know-How to Become Efficient 160
THE ADVANCED, LATE-BREAKING TECHNIQUES 160Anesthesia 160Fixation of the Globe 161THE INCISIONS 161The Primary Incision 161
Essential Requirements for a Self-Sealing Corneal Incision 162Position of the Clear Cornea Tunnel Incision 162Reservations About the Clear Corneal Incision 164Advantages to the Temporal Approach 164Importance of the Length of the Tunnel 166Placing and Making the Primary Incision 166Surgeon's Position 167Controversy Over the Strength and Safety of the Wound 167Testing the Wound for Leakage 167
Closing a Leaking Wound Without Sutures 167THE ANCILLARY INCISION 169ANTERIOR CAPSULORHEXIS 169
Key Role 169Technique for Performing a First Class CCC 170Size of the Capsulorhexis 170
STAINING THE ANTERIOR CAPSULE IN WHITE CATARACTS 172HYDRODISSECTION - HYDRODELAMINATION 175
Technique of Hydrodissection 175Hydrodelamination 175
MANAGEMENT OF THE NUCLEUS 176
General Considerations 176Concepts Fundamental to All Techniques 176
The Essential Principles 177
THE ENDOCAPSULAR TECHNIQUES 177
THE HIGH ULTRASOUND ENERGY AND LOW VACUUM GROUP 177THE GROOVING AND CRACKING METHODS 177

XIV
The Divide and Conquer Four Quadrant Nucleofractis Technique 177Principles of the Divide and Conquer Techniques 180The Role of D & C Techniques in Cataracts of 180
Different Nucleus ConsistencyPresent Role of Original Four Quadrant Divide and Conquer 181
THE LOW ULTRASOUND ENERGY AND HIGH VACUUM GROUP 181THE CHOPPING TECHNIQUES 183
Main Instruments Used 183Surgical Principles of the Original Phaco Chop 184Chopping Techniques Presented in this Volume 184THE STOP AND CHOP TECHNIQUE 184
Surgical Principles 184Absolute Requirements to Perform the Stop and Chop 188Importance of the Phaco Chopper 188Highlights of the Stop and Chop Technique 189FUNDAMENTAL DIFFERENCES BETWEEN CHOPPING 190AND DIVIDE AND CONQUER (D & C) TECHNIQUESTHE CRATER PROCEDURES 191
The Crater Divide and Conquer (Mackool) 191The Crater Phaco Chop for Dense, Hard Nuclei 191
THE NUCLEAR PRE-SLICE OR NULL PHACO CHOP 194 TECHNIQUE
Disassembling the Nucleus 194How Is the Null-Phaco Chop Done 194Potential Complications 198Contributions of this Technique 198
THE CHOO-CHOO CHOP AND FLIP 198 PHACOEMULSIFICATION TECHNIQUE
Origin of the Name “Choo-Choo” 199Comparison With Other Techniques 202Fine's Parameters 202
THE TRANSITION TO CHOPPING TECHNIQUES 204REMOVAL OF RESIDUAL CORTEX AND EPINUCLEUS 205INTRAOCULAR LENS IMPLANTATION 207
The Increased Interest in Foldable IOL's 207The Most Frequently Used IOL's 207
MONOFOCAL FOLDABLE LENSES 208THE FOLDABLE ACRYLIC IOL'S 208THE FOLDABLE MONOFOCAL SILICONE IOL's 209OTHER MONOFOCAL LENSES 210
The Hydrogel, Foldable Monofocal IOL 210The Foldable Toric Lens 210Bitoric Lens But Not Foldable 210
THE FOLDABLE MULTIFOCAL IOL 211The Array Multifocal Silicone Lens 211
How Does the Array Foldable Multifocal Lens Work? 212Quality of Vision with Array Multifocal 212Patient Selection and Results 212

XV
Specific Guidelines for Implanting the Array Lens 213Special Circumstances for Array Implantation 213Need for Spectacle Wear PostOp 214Halos at Night and Glare 214SURGICAL PRINCIPLES AND GUIDELINES FOR 214 IOL IMPLANTATION
PREFERRED METHODS OF IOL IMPLANTATION 214Use of Forceps vs Injectors 214
Advantages and Disadvantages 214New Trends for Folding and Insertion of IOL's 214
Guidelines for Insertion of Different Types of Lenses 218Surgical Technique with Array Lens 218
Carreño's Technique of Acrylic IOL Implantation 218Through a 2.75 mm IncisionDodick's AcrySof's Implantation Technique 220Implantation Technique for Silicone Foldable IOL's 222Using Cartridge-Injector System
TESTING THE WOUND FOR LEAKAGE 223
CHAPTER 10
FOCUSING PHACO TECHNIQUES ON THEHARDNESS OF THE NUCLEUS
MULTIPLICITY OF TECHNIQUES 229The Essential Criteria for Success 229
DIFFERENT NUCLEUS CONSISTENCY - 229 TECHNIQUES OF CHOICE
Representative Experts 230LINDSTROM'S PROCEDURES OF CHOICE 230
Advantages of the Supracapsular 231Disadvantages of the Supracapsular 232Contraindications of Supracapsular 232
HIGHLIGHTS OF THE SUPRACAPSULAR 233 IRIS PLANE TECHNIQUECENTURION'S TECHNIQUES RELATED 234 TO NUCLEUS CONSISTENCYCARREÑO'S NUCLEAR EMULSIFICATION TECHNIQUE 237 OF CHOICE (PHACO SUB 3)Adjusting the Equipment Parameters to Remove Cataracts 237 of Various Nuclear DensityThree Sets of Values Programmed Into Memory 237Technique of Choice and Consistency of Cataract 238NISHI'S TECHNIQUES OF CHOICE FOR 245 NUCLEI OF DIFFERENT CONSISTENCIES

XVI
CHAPTER 11
INTRAOPERATIVE COMPLICATIONS 249-268
General Considerations 249Main Intraoperative Complications 249Incidence 249Facing the Challenges 250COMPLICATIONS WITH THE INCISION 250COMPLICATIONS RELATED TO ANTERIOR 254 CAPSULORHEXISCOMPLICATIONS WITH HYDRODISSECTION 258COMPLICATIONS DURING NUCLEUS REMOVAL 259COMPLICATIONS DURING REMOVAL OF THE CORTEX 260COMPLICATIONS DURING FOLDABLE IOL's IMPLANTATION 260COMPLICATIONS WITH POSTERIOR CAPSULE RUPTURE 262Pars Plana Vitrectomy for Dislocated Nucleus 266
POSTOPERATIVE COMPLICATIONS 269-290
MEDICAL 269Cystoid Macular Edema 269
Diabetes and Cystoid Macular Edema 273PHOTIC MACULOPATHY 273AMINOGLYCOSIDE TOXICITY 275
POSTERIOR CAPSULE OPACIFICATION 277Overview 277Role of IOL in PCO 277Role of Continuous Curvilinear Capsulorhexis in PCO 278Main Factors that Reduce PCO 278
PERFORMING THE POSTERIOR CAPSULOTOMY 279Size of Capsulotomy 279Posterior Capsulotomy Laser Procedure 279Complications Following Nd:YAG Posterior Capsulotomy 281
POSTOPERATIVE ASTIGMATISM IN CATARACT PATIENTS 281MANAGEMENT 281Procedure of Choice 282Highlights of AK Procedure 283
EXPLANTATION OF FOLDABLE IOL'S 284RETAINING THE BENEFIT OF THE SMALL INCISION 284RETINAL DETACHMENT 286
POSTOPERATIVE ENDOPHTHALMITIS 286INTRAOCULAR LENS DISLOCATION 288
COMPLICATIONS OF PHACOEMULSIFICATION

XVII
CHAPTER 12
CATARACT SURGERY IN COMPLEX CASES
Aims of this Chapter 295Broadening of Indications 295
Complex Cases Already Discussed in Previous Chapters 296FOCUSING ON THE MAIN COMPLEX CASES 296
THE DIFFERENT TYPES OF VISCOELASTICS 296Their Specific Roles 296Cohesive and Dispersive Viscoelastics 296The Cohesive VES - Specific Properties 296The Dispersive VES- Specific Properties 297
PHACOEMULSIFICATION AFTER PREVIOUS 298 REFRACTIVE SURGERYPHACOEMULSIFICATION IN HIGH MYOPIA 298CHALLENGES OF PHACOEMULSIFICATION IN HYPEROPIA 299REFRACTIVE CATARACT SURGERY 299Why and When Do Refractive Cataract Surgery 299 TECHNIQUE FOR REFRACTIVE CATARACT SURGERY 300
CATARACT AND GLAUCOMA 302
Overview - Alternative Approaches 302COMBINED CATARACT SURGERY AND 303 TRABECULECTOMYIndications 303Evolution of the Incision for Combined Cataract Extraction 303 and TrabeculectomyA. Extracapsular Cataract Extraction with Trabeculectomy 304B. Phacoemulsification with Trabeculectomy 308Intraocular Lens Implants 308Preoperative Preparation 308SURGICAL TECHNIQUES STEP BY STEP 310ECCE and Trabeculectomy With Single, Unbroken Tunnel Incision 310Phacoemulsification With Trabeculectomy 315Antimetabolites in Combined Procedures 318Results of Combined Cataract Surgery and Trabeculectomy 320
PHACOEMULSIFICATION IN DISEASED CORNEAS 322
PHACOEMULSIFICATION AND IOL IMPLANTATION 322 IN THE PRESENCE OF OPAQUE CORNEAOverview 322Padilha’s Timing and Technique 322Specific Recommendations 324PHACOEMULSIFICATION, IOL IMPLANTATION 325 AND FUCHS’ DYSTROPHYPreoperative Evaluation 325 Special Precautions During Phacoemulsification 325

XVIII
PHACOEMULSIFICATION IN SMALL PUPILS 328
Pharmacological Mydriasis 328Mechanical Dilatation with Viscoelastics 328Mechanical Strategies 328
TRAUMATIC CATARACTS 333
Overview 333Assessment of the Injured Eye 333
Highlights of Examination 333Diagnostic Imaging 333Combined Injuries of Anterior and Posterior Segment 334
Traumatic Cataracts in the Presence of Anterior 334 Segment Penetrating WoundsMANAGEMENT OF TRAUMATIC CATARACT 334HIGHLIGHTS OF SURGICAL TECHNIQUE 334The Incision 334Anterior Capsulorhexis 334Lens Removal 334Role of Intracapsular Tension Ring in Traumatic Cataracts 335Removal of Cortex 336Selection of IOL 339IOL Implantation 339Selection of Viscoelastic in Traumatic Cataracts 339Phacoemulsification Advantages in Traumatic Cataract 340
PHACOEMULSIFICATION IN SUBLUXATED CATARACTS 340
Strategic Management 340MANAGEMENT DEPENDING ON SIZE OF 340ZONULAR DIALYSIS
Special Precautions with Subluxated Cataracts 342Increasing the Safety of Posterior Lens Implantation in 344 Extensive Zonular Disinsertion
Fixation of the Anterior Capsule to the Ciliary Sulcus 345
CATARACT SURGERY IN CHILDHOOD 347
Previous Controversies Now Resolved 3471) Age and Timing for Surgery 347
Bilateral Cataracts 347Unilateral Cataracts 347
Preoperative Evaluation 348History 348Examination 349The Special Case of Lamellar Cataracts 350Rubella Cataracts 350The Need for Close Monitoring 350Preoperative Considerations 350
The Decision to Implant IOL’s in Children with Cataract Surgery 351Surgical Technique 351The Posterior Approach to Cataract Extraction in Children 355
CATARACT SURGERY IN UVEITIS 355

XIX
CHAPTER 13
THE PRESENT ROLE OF MANUAL EXTRACAPSULARS
Overview 359PERFORMING A FLAWLESS PLANNED EXTRACAPSULAR 361CATARACT EXTRACTION (with an 8 mm Incision and
Posterior Chamber IOL Implantation)General Anesthesia 361Local Anesthesia 362Technique for Extracapsular Cataract Extraction 364with an 8 mm Incision (ECCE)
THE MANUAL, SMALL INCISION EXTRACAPSULARS 375
THE MINI-NUC TECHNIQUE 375SURGICAL TECHNIQUE 376
Anesthesia, Paracentesis, ACM 376Capsulorhexis 377Conjunctiva 377Sclerocorneal Pocket Primary Incision and Tunnel 378Hydrodissection and Nucleus Dislocation 378Nucleus Expression Using Glide and High IOP 381Epinucleus and Cortex Extraction 383IOL Implantation 384Pupil Enlarged by Increased IOP 386Advantages of the Continuous Flow of BSS 387 during Manual ECCEComplications 387
THE SMALL INCISION PHACO SECTION 389MANUAL EXTRACAPSULAR TECHNIQUE
Overview 389Evolution of Technique 389Indications 389PHACO SECTION MOST IMPORTANT FEATURES 389Capsulorhexis 390Completing the Tunnel Incision 390Anterior Chamber Maintainer 391Aspiration of the Anterior Cortex and Epinucleus 392Phacosection 393Transition from Extracapsular Extraction to Phacosection 395
THE SMALL INCISION MANUAL PHACOFRAGMENTATION 400
Benefits of (MPF) 400Experiences with Other Phaco Fragmentation Techniques 400
Why Use Gutierrez' Technique? 400Surgical Technique 402
Complications 405

XX
CHAPTER 14
THE NEW CATARACT SURGERY DEVELOPMENTS
Overview 409 DODICK’S PHOTOLYSIS SYSTEM 409
THE CATAREX SYSTEM 411Aziz PhacoTmesis 411Water Jet Technology 411

Fo c u s i n g a n d O v e r v i e w o f W h a t i s B e s t
1
FOCUSING AND OVERVIEW OF WHAT IS BEST
Modern cataract surgery is definitely re-lated to lens removal through small, short,valve like incisions and implantation of fold-able intraocular lenses implanted through theseshort incisions.
Tackling the Challenges
In this Volume we present what is bestfor our patients and how to tackle the chal-lenges with vigor. We present the new devel-opments in preoperative evaluation, the ex-pansion of the indications as the outcomeshave improved, the new, sometimes complexproblems brought by refractive andvitreoretinal surgery in calculating IOL power.And we illustrate the steps that remain ratherconstant and which apply either to the surgeonin the process of transition or the experiencedsmall incision surgeon, vs the methods that dochange and require the skill of an experiencedsurgeon.
We also present the anesthetic methodsof choice, the understanding of the phacomachine, how it works and what the rationaleis behind its optimal use. How to undergo thesafe and successful transition from plannedextracapsular to phaco. The incisions ofchoice for most surgeons, the methods thatenhance the performance of capsulorhexis incomplex cases, the modern techniques ofhydrodissection, hydrodelineation and cortexremoval that have stood the test of time and theadvantages and disadvantages of the differentmethods of nucleus removal in phacoemulsifi-cation.
Role of Small Incision ManualExtracapsular
Although we provide special emphasison how to master phacoemulsification andfoldable IOL implantation, including an in-depth analysis of how to prevent and manageintraoperative and postoperative complications,we also present to you the small incision manualextracapsular techniques of proven and lastingvalue. For those surgeons who are preventedby practical considerations, or who simplyprefer to not take the significant step of enter-ing into small incision surgery, the chapter onhow to perform a flawless planned extracapsu-lar with 8 mm incision and its merits is superblyas presented by one of the world's master sur-geons.
IOL's of Choice
In modern cataract surgery it is essentialto discuss the IOL's of choice and their merits.Selecting the correct lens implant (size of optic,chemical material, foldable vs non-foldable,mono vs multifocal) may play a more impor-tant role in the final patient's final visual out-come and satisfaction than the specific tech-nique used for phacoemulsification of thenucleus.
The Best Phaco Technique
The best phacoemulsification tech-nique to use is based on the relation of the type

THE ART AND THE SCIENCE OF CATARACT SURGERY
2
of cataract to a specific method of nucleusremoval for that specific stage of cataract. Thedivide and conquer in four quadrants continuesto be the procedure of choice for the beginnerin the transition period or for the surgeon whodoes not have a large volume of cataract sur-gery. The technique for nucleus removal withone hand continues to be fundamental for eachphaco surgeon to learn. We will also presentthe phaco sub-3, phaco chop, phaco pre-chop,choo-choo chop and flip and the phaco burst,all of which are techniques for the moreadvanced or experienced surgeons. Each hasits merits, effectiveness and limitations.
The Complex Cases
Small incision cataract surgery has sig-nificantly changed the approach and manage-ment of the complex cases. It is the mostimportant contribution made in years to a suc-cessful and safe combined glaucoma-cataract
operation, to management of traumatic cata-racts and cataract surgery in patients with cor-neal dystrophies.
Pediatric cataracts have not been resolvedwith the improved management options andalmost risk-free capabilities of the magnitudethat we have available in adult patients. This,in part, may be related to the fact that thepostoperative care depends more on the par-ents than on the surgeon. The previouslyhighly controversial point of implanting in-traocular lenses in children has shifted to apositive decision on the part of most surgeonswho now agree to implant IOL's in childrenwhen the selection of cases has been doneprudently.
Let us now proceed to discuss each oneof the highlights of modern cataract surgery.The field is exciting and a source of greatsatisfaction to the surgeon who does it well andwith full dedication to the benefit of his or herpatients.

C h a p t e r 1: S u r g i c a l A n a t o m y o f t h e H u m a n L e n s
5
SURGICAL ANATOMY OF THE HUMAN LENS
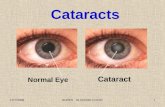
Clinical Applications - Behaviourof Different Cataracts
Understanding the three-dimensionalityand concentric anatomy of the lens as origi-nally conceived by Henry Clayman, M.D. forHIGHLIGHTS is fundamental for having aclear picture of some of the main steps inperforming phaco. I refer to the dissection ofthe different structures of the nucleus withfluid, that is, hydrodissection of the anteriorand posterior capsule from the cortex, separa-tion of the nucleus and epinucleus with fluidand the different tissue reactions to the forcespresented during phacoemulsification of thenucleus.
The normal crystalline lens is an avascu-lar structure. As pointed out by HowardGimbel, M.D., lens fibers are surrounded bythe lens capsule which is the basement mem-brane of the lens epithelial cells (Fig. 1). Lensepithelial cells are located just inside the cap-sule and exist as a single layer. The epithelialcells can differentiate into lens fibers, and thisprocess occurs in an area just posterior to thelens equator. As new lens fibers are formed, thecentral fibers are compacted, forming thenucleus of the lens. The surrounding denselypacked fibers form the cortex (Fig. 1). Due tothe anatomical arrangement of cells and fibers,the Y sutures are formed within the lensnucleus.
For a surgeon not experienced in smallincision extracapsular techniques, there maybe difficulties recognizing the hidden anatomyof the morbid cataract. It may be difficult to
distinguish what is really anterior capsule, whatis cortex and where the posterior capsule is.
When removing the cortex, we must keepin mind that its substance is three dimensional(Fig. 1). As described in this figure, the nucleusis the pit of the avocado. The pit in the avocadodoes not drop out because it is held in byadhesions between the flesh of the avocado andthe pit. Figure 1 also shows that the cortex (C)adheres to the epinucleus and the nucleus. Inorder to remove the nucleus by whatever tech-nique you prefer, these nuclear-cortical adhe-sions have to be broken and out comes thenucleus, whether by phacoemulsification or byplanned extracapsular.
The residual cortex, which is the flesh ofthe avocado, is wrapped around, three dimen-sionally, inside the skin of the avocado, whichis the capsule (Fig. 1). When aspirating thecortex, it is prudent not to attack the cortex righton but to get a free edge, which you may attractto the aspiration port, and peel from its capsulesupport.
In Fig. 1 you may see a conceptual crosssection of the anterior globe, with all the struc-tures of the human lens involved in the maneu-vers hereby described. The capsule is like theskin of an avocado, both anterior (A) andposterior (P). The flesh of the avocado iscomparable to the cortex (Fig. C). The pit ofthe avocado is comparable to the lens epi-nucleus and nucleus (Fig. E-N). In (1) thecortex (C), epinucleus (E) and nucleus (N) areshown removed from the capsule. (2) Showsthe cortex (C) removed from the nucleus andepinucleus (E and N). The nuclear-cortical

THE ART AND THE SCIENCE OF CATARACT SURGERY
6
Figure 1: Three-Dimensionality of the Lens - Clinical Applications
Figure 1 presents a conceptual cross section of the anterior globe and the three dimensional nature of the lensanatomy, with all the structures of the human lens involved in the surgical maneuvers. Think of the lens as if it werean avocado. The capsule is like the skin of an avocado, both anterior (A) and posterior (P). The flesh of the avocadois comparable to the cortex (Fig. C). The pit of the avocado is comparable to the lens epinucleus and nucleus (Fig.E-N). The pit in the avocado does not drop out because it is held in by adhesions between the flesh of the avocadoand the pit. The cortex (C) adheres to the epinucleus (E) and the nucleus (N). The residual cortex, which is the fleshof the avocado, is wrapped around, three dimensionally, inside the skin of the avocado, which is the capsule (Fig. A-P). When aspirating the cortex, it is prudent not to attack the cortex directly but to get a free edge, which you may attractto the aspiration port, and peel it from its capsule support. In (1) the cortex (C), epinucleus (E) and nucleus (N) areshown removed from the capsule. (2) Shows the cortex (C) removed from the nucleus and epinucleus (E and N). Thenuclear-cortical adhesions have to be broken down before the nucleus can come out (2 and 3). In (E) the epinucleusis shown as an entity distinct from the nuclear core. This figure allows us to better understand the anatomical basisfor the formation of grooves across the nucleus skillfully utilized by the surgeon in the technique ofphacoemulsification.

C h a p t e r 1: S u r g i c a l A n a t o m y o f t h e H u m a n L e n s
7
adhesions have to be broken down before thenucleus can come out (2 and 3). In (E) theepinucleus is shown as an, entity distinct fromthe nuclear core. This figure allows us to betterunderstand the anatomical basis for theformation of grooves across the nucleus skill-fully utilized by the surgeon in the technique ofphacoemulsification.
Anatomical Characteristics ofDifferent Types of Cataract
The lens in cross section is made up of aconcentric series of elliptical rings. Each oneof these rings represents growth of the lens andthe laying down of additional lens materialfrom the epithelial cells located on the under-side of the anterior capsule. In soft to mediumdensity cataracts, the concentric lamellae ofcataract tissue are not densely packed, so muchof the space inside the cataract is taken up by
moisture. Medium to firm-density cataractshave concentric lamellae of tissue that aredensely packed together, packed so tight thatthere is no room for moisture between lamel-lae.
How Cataracts Respond Differently
Paul Koch, M.D. emphasizes that eachone of these different types of cataracts re-sponds differently, so surgical forces need tobe applied differently. In breaking the nucleusthe surgeon needs to individualize the opera-tion to take advantage of the natural tendenciesof each type of cataract. Soft to mediumdensity cataracts are malleable and compli-ant. We can hold them in the capsular bag andsqueeze them from between neighboring pieces.Medium to firm density cataracts are morelike rocks. They have rigid form and are muchmore demanding of the surgeon's skill. If we
Figure 2: Dense, Nuclear BrunescentCataract
In dense, nuclear brunescentcataracts, as shown in Fig. 2, there is lesswater content, the capsule is dehydratedand there is a significant increase in thedensity and opacity of the nucleus (C).These nuclei are more like rocks, and arethe hardest to manage with phacoemulsi-fication in the transitional stage or bysurgeons inexperienced in phaco. Diffi-culties during surgery may arise that canbe characteristic in this type of cataractsuch as difficulty in identifying thecapsulorhexis or with the hydrodissection.

THE ART AND THE SCIENCE OF CATARACT SURGERY
8
rub them against the capsule, the capsule canbreak. If we pull them up into the anteriorchamber, the capsulotomy may split. If theytouch the corneal endothelium, they abrade it.
Understanding this surgical anatomy ofthe lens and its clinical applications helps sig-nificantly in recognizing that each type of cata-ract acts differently and that our approachshould vary depending on the individual pa-tient (Fig. 2).
INCIDENCE ANDPATHOGENESIS
It is widely known that cataracts consti-tute the major source of curable blindness world-wide. Not only do they seriously affect largesegments of the population in developing orless economically fortunate regions but alsothe peri-urban areas of large and developedcities which are equipped with highly trainedophthalmologists and the latest technology.For psychological or social reasons difficult tounderstand, many blind or almost blind per-sons living in these peri-urban "belts" do notseek medical advice and treatment when easilyavailable. This is one of the mysteries ofpeople whose quality of life is significantlylimited by partial or complete opacification ofthe crystalline lens. Figure 2 shows abrunescent, advanced, hard cataract which be-comes sometimes very difficult to treat byphaco, even in skillful hands. Many patientsallow their cataracts to become this much ad-vanced even if they live near medical facilitiesthat may provide proper care at a much moreadvantageous time.
As pointed out by Howard Gimbel, M.D.,there are a variety of causes and types ofcataracts. By definition, all cataracts share thecommon feature of opacification of some por-tion of the crystalline lens which, if within theto cataract formation.
BIBLIOGRAPHY
Assia, EI., Legler, UFC., Apple, DJ.: The capsularbag after short and long term fixation of intraocularlenses. Ophthalmology, 1995; 102:1151-7.
Boyd, BF.: Cataract/IOL Surgery. World AtlasSeries of Ophthalmic Surgery, published byHIGHLIGHTS, Vol. II, 1996; 5:5-13.
Boyd, BF.: Cataract/IOL Surgery. World AtlasSeries of Ophthalmic Surgery, published byHIGHLIGHTS,Vol. II, 1996; 5:34-38.
Boyd, BF.: New developments for small incisioncataract surgery. Highlights of Ophthalm. Jour-nal, Volume 27, Nº 4, 1999;45-46.
Gimbel, HV., Anderson Penno, EE: Cataracts:Pathogenesis and treatment. Canadian Journal ofClinical Medicine, September 1998.
Koch, PS.: Simplifying Phacoemulsification, 5thed., published by Slack; 1997; 7:85-86.
Lens and Cataract, Basic and Clinical ScienceCourse, Section 11. American Academy of Oph-thalmology, 1998-99.

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
11
INDICATIONS AND PREOPERATIVE EVALUATION
INDICATIONS
To date there is no established medicaltreatment for the prevention or treatment ofcataract formation and thus the treatment ofcataracts remains surgical. Contrary to thecommonly held belief that cataracts must reacha certain degree of density or become "ripe"prior to considering cataract surgery, today thecrystalline lens can be removed at virtually anystage. In fact, refractive lensectomy in whichthe clear crystalline lens is removed may beused to surgically eliminate or significantlyreduce the need for glasses in patients withvery high myopia or hyperopia. In the lattercondition, this may be achieved by implantingseveral piggyback lenses within the capsularbag following clear lensectomy.
Role of Quality of Life
Cataract/IOL surgery improves qualityof life better than any other medical procedureknown to mankind. Cataract surgery is indi-cated when the patient's quality of life is beingaffected by visual impairment, when there is adiminution in vision if the patient is exposed tolight or at night, and when the preoperativeevaluation indicates that the potential for resto-ration of sight is good. How much a patient'squality of life is impaired from a cataract isrelative, varying with the patient's occupationand age. The key factor is not to wait until anuclear cataract becomes hard. With time, thelens fiber density becomes a hard nuclearbrunescent cataract (Fig. 2) . With most mod-ern phacoemulsification techniques it may be-
come increasingly difficult to perform surgeryif the lens becomes extremely dense orbrunescent.
Waiting too long may require that thesurgeon operate on dense nuclear cataracts,which increases the risk of posterior capsuletears, whether we perform planned extracapsu-lar or a phacoemulsification. This complica-tion may lead to other rather serious problemssuch as dislocated nucleus, retinal detachment,macular edema, bullous keratopathy and in-flammation.
The Role of Visual Acuity
There are very few strict criteria for rec-ommending cataract surgery. In the UnitedStates, however, many professional revieworganizations have indicated that the reductionof Snellen distance acuity to 20/40 or worse asa result of cataract is sufficient indication inand of itself for cataract surgery. This isgenerally the minimum standard for driving. Insome of the advanced, developed countries,being unable to obtain a driver's license mayseriously affect a person's life because he/shemay be disqualified to drive to the market orshop to purchase food and other materials es-sential to daily existence. However, in manycases surgery may be indicated without reduc-tion of visual acuity to the level of 20/40 if thepatient has difficulty performing activities ofdaily living. Because patients have varyingoccupational and recreational needs, some pa-tients may need cataract surgery prior to havingtheir vision reduced to 20/40 by standard tests.In addition, near vision in some cases may be

THE ART AND THE SCIENCE OF CATARACT SURGERY
12
compromised more than distance acuity par-ticularly in the case of central posterior subcap-sular cataracts. The trend toward early re-moval of cataract offers the advantage ofoperating on a younger age group, many ofwhom are still productive members of society.Their need for early return to their usual life-style is extremely important. The older popu-lation, often living alone, also benefits fromearly visual recovery. These high expectationsand needs require that the ophthalmic surgeonperform superior surgery to obtain excellentpostoperative visual acuity and early visualrehabilitation.
As emphasized by Gimbel, symptoms ofcataracts include complaints of a yellowing ofvision, glare, halos, decreased night vision, andgenerally blurred vision in adults. Nuclearsclerosis which is a typical form of age-relatedcataracts may also induce a myopic shift andpatients may give a history of having changedtheir glasses several times within a short periodof time. In children cataracts may present asleukocoria and may result in strabismus and/oramblyopia if not treated promptly.
Contrast Sensitivity and GlareDisability
In evaluating a patient with cataract andin the process of deciding when that personrequires cataract/IOL surgery, it is fundamen-tal to keep always in mind that standard Snellenacuity measurements do not give any informa-tion with regard to symptoms of disablingglare. As a matter of fact, very good visualacuity with the Snellen chart in the physician'sexamining room may lead the ophthalmologistto making the wrong decision and recommen-dations unless he or she takes other factors intoconsideration. In later years, we have become
increasingly aware that diminished contrastsensitivity which interferes with sharp visionunder different color backgrounds or targetluminance, is an essential element of sight anda highly limiting factor in the presence ofcataract. This is perceived by the patient forexample when he or she is unable to read acomputer screen at the airport if the back-ground is light blue and the print is light yelloweven though visual acuity in the physician'srefracting lane was 20/30 or 20/25. The samefor disabling glare.
These are two additional very importantissues in determining when the cataract shouldbe removed. For many years this judgment hasbeen based on Snellen visual acuity. But apatient can score quite well on Snellen acuitywhile suffering in real life. Posterior subcap-sular cataracts are notorious for interferingwith reading, even when distance vision isgood, and may induce a great deal of glare.Snellen acuity may be 20/20 or 20/25, butagainst oncoming headlights while driving atnight, for instance, the glare may diminish thefunctional vision to 20/100 or even 20/200.People with nuclear sclerosis, the most com-mon form of cataract, tend to be bothered bydecreased contrast sensitivity rather than glare.
Although glare disability and contrastsensitivity are distinctly different, the termsoften are erroneously interchanged. The test-ing characteristics of each, however, may over-lap, and a reduction in one function often leadsto a diminution in the other, further adding tothe confusion of their differences. As clarifiedby Samuel Masket, M.D., glare disability isa light-induced visual symptom. Contrastsensitivity testing is a means of vision analysis,analogous to a markedly expanded form ofSnellen acuity evaluation at varied amounts oftarget luminance.

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
13
Contrast SensitivityCharacteristics
Like audiometry, which measures thesensitivity of the hearing apparatus to stimuli atdifferent audio frequencies, contrast sensitiv-ity analysis determines the ability of the visualsystem to perceive objects of differing con-trasts as well as sizes.
A patient who has a reduction in contrastsensitivity might perceive the small, highlycontrasted targets on a Snellen test line but beincapable of identifying larger objects at re-duced contrast. There are alterations in thevisual system that can cause visual loss that arenot detected by the determination of Snellenvisual acuity but may be evaluated by testing ofcontrast sensitivity function. This is unlike
Figure 3 A (above left): Importance of Testing forContrast Sensitivity
The Contrast Sensitivity Test is used clinicallyto evaluate cataracts, glaucoma, diabetic eye disease,contact lens performance and refractive surgery. In thepresence of cataract the clouding of the lens causeslight scatter on the retina. This reduces image contrastand causes dimness of vision. One of the more difficultproblems in evaluating how a cataract is affecting thepatient's visual function is that many cataract patientspreserve good visual acuity as tested in the refractinglane (Snellen chart) but complain about their visualdisability. The true “real-world” vision of cataract pa-tients can be established as a functional acuity scoreusing contrast sensitivity and glare testing.
Figure 3 B (below right): Contrast SensitivityRecording Chart
The contrast sensitivity recording chart pro-vides four (4) rows of wave gratings. At the recom-mended test distance of 8 ft (2.5 meters), thesegratings test the spatial frequencies of 3, 6, 12 and18 cycles/degree. This chart provides a full con-trast sensitivity curve. The functional acuity is de-termined by the lowest level of contrast sensitivity(gray band) that can be detected by the patient. Thefunctional acuity score is shown in a bracket nextto the contrast sensitivity score.

THE ART AND THE SCIENCE OF CATARACT SURGERY
14
disabling glare, which determines the effect ofextraneous light on visual performance. Con-trast sensitivity evaluation is a measurementof the resolving power of the eye at variedcontrasts between image and background(Fig. 3 A-B).
A number of useful contrast and glaresensitivity testing methods have been devised(Fig. 3 A-B). They are accessible and inexpen-sive. Unfortunately, standardization of thesetechniques has not yet been achieved. It isessential that the clinician be fully aware ofthese two factors that may impinge on thepatient's real vision or quality of vision, inaddition to the Snellen acuity test.
Relation of Glare to Type ofCataract
Neumann et al. have determined thatnuclear cataract is more likely to be associ-ated with nighttime glare disability, while cor-tical cataract formation is associated withdaylight glare, and posterior subcapsular cata-racts may induce glare disability associatedwith bright, direct sunlight or bright centrallight sources. Cortical cataracts seem morelikely to cause glare symptoms than nuclearcataracts. Masket points out that frequently,patients with dense central posterior subcapsu-lar cataracts frequently retain excellent dis-tance Snellen acuity as measured in the refract-ing lane, yet they perform poorly on any of theavailable glare testing devices. Such patients
may have severely lower visual function dur-ing daylight driving although they do well withthe Snellen acuity chart. In essence, the Snellenchart evaluates quantity of vision. Contrastsensitivity tests evaluate quantity and qualityof vision. The equipment to perform the test isaccessible and inexpensive. It is basically achart about 0.3 meters in size and it costs aboutUS$200.00
Preoperative Considerations
In addition to determining visual acuityby the Snellen chart, contrast sensitivity andglare disability testing as outllined, all patientswith cataracts should have a thorough historytaken including any systemic or ocular medica-tions being used and any systemic disease forwhich they receive treatment. A family historyis also included. The ophthalmologic exami-nation should include intraocular pressure(IOP) measurements, keratometry, pupil exam,routine motility testing, and dilated slit-lampand funduscopic examinations including indi-rect ophthalmoscopy to examine the centraland peripheral retina. Ancillary testing such asvisual fields, topography, specular microscopyfor endothelial cell counts, and fluoresceinangiography should be considered in selectedcases. There are many causes for decreasedvision and ,especially in older patients, thesecauses may exist concurrently. Age-relatedmacular degeneration is possibly the most im-portant and difficult to detect because of theexisting opacity of the cataract.

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
15
Evaluation of Macular Function
The main preoperative tests to determinecentral visual acuity are: 1) the PotentialVisual Acuity Meter (PAM) and 2) the SuperPinhole. They permit evaluation of the macu-lar function in patients in whom examinationof the macula is difficult due to media opaci-ties. They are more useful when they areintegrated into the total evaluation of the pa-tient.
One of the major problems that all of usconfront as clinical ophthalmologists is that ofpatients with cataracts who correct to 20/100 or20/200 and on whom we are planning tooperate but cannot see the fundus, particularlythe macula. This is aggravated when the pa-tient has a few old small corneal opacities. Theever-present question is: what is the visualprognosis if we operate, either by a cataractextraction or combined with a corneal trans-plant? What can we anticipate for the patient orhis/her family about future, postoperative vi-sion even if we do not have any significantoperative or postoperative complications? Ul-trasonography and clinical tests will give usonly a partial and limited answer.
Since we cannot see the state of themacula or papilla, we are limited as to theprognosis. Sometimes we have the pleasantsurprise of obtaining more vision postopera-tively than we predicted; in other cases, we facethe unpleasant reality of finding macular de-generation or other lesions in the macula oroptic nerve that result in poor central vision inspite of a beautifully performed operation.
Any well trained ophthalmologist candiagnose major lesions of the optic nerve orretina preoperatively. The major problem iswith the subtle lesions that nevertheless limitthe patient's capacity to read or distinguishclear images at distance postoperatively.
One of the most important tests forevaluating macular function in the presence ofa lens opacity dense enough to make our clini-cal examination of the macula unreliable is theGuyton-Minkowski Potential Visual AcuityMeter (PAM).
The Super Pinhole developed by DavidMcIntyre, M.D., is another highly practicaland useful method to evaluate macular func-tion. The Laser Interference-Fringe Methodhas also been previoulsy used but it is lesspractical. Most clinical ophthalmologists pre-fer the PAM test or the Super Pinhole.
The PAM
The Potential Acuity Meter (PAM) is aninstrument which attaches to a slit lamp. Itserves as a virtual pinhole by projecting aregular Snellen visual acuity chart through avery tiny aerial pinhole aperture about one-tenth of a millimeter (0.1 mm) in diameter. Thelight carrying the image of the visual acuitychart narrows to a fine 0.1 mm beam and isdirected through clearer areas in cataracts (orcorneal disease), allowing the patient to readthe visual acuity chart as if the cataract orcorneal disease were not there (Figs. 4 and 5Aand B). The PAM is taken from its stand andplaced directly onto the slit lamp in the same

THE ART AND THE SCIENCE OF CATARACT SURGERY
16
Figure 4 : Concept of the Guyton-Minkowski Potential Acuity Meter With Cataractous Lens (PAM)
The beam (arrow) of the projected Snellen chart is shown passing through a cataract (C) and forming the imageof the chart on the retina (R). The beam of light can only strike the retina when the beam is able to pass through thelens, between opacities. With the chart successfully projected onto the retina, the patient can respond and we candetermine the potential visual acuity as if the cataract were not there. The PAM serves as a superpinhole by projectingthe regular Snellen chart along a tiny beam 0.1 mm in diameter.
manner as the detachable type of Goldmanntonometer. The examination takes from two tofive minutes per eye, depending on the densityof the cataract.
As pointed out by Guyton, for the PAMto work adequately, there must be some smallhole in the cataract for the light beam to passthrough. You may find such a hole even incataracts which have media clouding of up to20/200 and better. When you find it, then you
can avoid the light scattering produced by theopacities. It is this light scattering which washesout the retinal image and decreases vision be-hind cataracts. By projecting the image of thevisual acuity chart through one tiny area, weavoid that scattering effect, and the patient cansee the chart (Figs. 6 A-B and 7 A-B).
How is the instrument operated by theclinician or an assistant? The device is mountedon a slit lamp so that the operator can see

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
17
Figure 5 A (above left): Concept of thePotential Acuity Meter (PAM) in Casesof Corneal Opacities and Cataract
In Fig. 5-A the tiny beam of light(arrow) of the projected Snellen chart isshown striking a corneal opacity and failingto penetrate the cornea.
Figure 5 B (below right): Concept of thePotential Acuity Meter (PAM) in Casesof Corneal Opacities and Cataract
In Fig.5-B, by moving the beam toa point between the corneal opacities, theprojected Snellen chart can pass on throughthe cornea and onto the retina (arrow) sothat the patient can see it and we candetermine the visual acuity. The test asshown in Figs. 4-A and 4-B is particularlyimportant if we are considering a com-bined cataract extraction and penetratingkeratoplasty.

THE ART AND THE SCIENCE OF CATARACT SURGERY
18
exactly where the light beam is passing. Thelight beam is directed to various parts of thepupil (Fig. 4, 6-A, 6-B, 7-A, 7-B). It can befocused in between lens opacities. It is easy tosee when the beam is going in because itpractically disappears (Fig. 6-B). When it hitsan opacity, you can see the opacity light up(Fig. 6-7). When you move the beam with theslit lamp control to lucent, non-opaque areas,you see the beam pierce through (Figs. 6-B and7-B). It is valuable to observe this because ifyou know you are getting the beam throughand the patient still reads poorly, you can befairly confident that there will be a poorresult after surgery. If you are not surewhether the beam is penetrating and the patientreads poorly, results of surgery will be uncer-tain. So, the slit lamp monitoring of the lightbeam is important.
It is sometimes difficult to find a smallhole in a cataract with density greater then20/200, although holes have been found incounting-fingers cataracts. If you obtain goodvision behind any cataract, you have the infor-mation you need. As to the visual prognosisbehind very dense cataracts, if you cannotobtain a good reading, you still do not knowquite where you are.
The instrument is best operated in a dark-ened room because it is easier to see the lightbeam. The best results are obtained with adilated pupil because you have a better chanceof finding an appropriate hole in the cataract.Ninety percent of patients whose best correct-able vision is 20/200 and better preoperatively,achieve the predicted vision or within two lines
Figure 6-A: How the PAMWorks - Slit Lamp View
In Fig. 6-A the ophthal-mologist directs the small beam oflight through different parts of thedilated pupil in a patient with lensopacities. One can see here thatthe beam of light (arrow) is hittinga lens opacity. This light is stronglyscattered by the opacity, lightingup the opacity, leaving little or nolight remaining to penetrate onthrough to the retina.

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
19
than the predicted vision after surgery. Whenthe preoperative visual acuity is worse than 20/200, only about 60% achieve vision withinthree lines of the vision predicted by the PAM.
The vision obtained after surgery isgenerally equal to, or better than the visionpredicted with the Potential Acuity Meter. Falsepositives occur in 10-15% of cases. When thetest is done in cases of cystoid macular edema,the instrument occasionally indicates better
Figure 6-B: How the PAM Works- Slit Lamp View
In Fig. 6-B the beam (ar-row) is successfully penetrating thelens at a point where no lens opaci-ties are present, and the beam dis-appears into the vitreous cavity (V).As the light beam broadens out,passing into the vitreous, it is nolonger visible to the doctor. Theexaminer thus can be certain thatthe light beam of the projectedSnellen chart is getting in to theretina. With the beam successfullyprojecting the Snellen chart imageon the retina, the patient can re-spond accordingly so that the ex-aminer can determine the potentialvisual acuity irrespective of the len-ticular opacities.
potential vision than the patient can achievewith best refractive correction postoperatively.
No single test of visual function, how-ever, is sufficient to mandate surgery. Instead,it is the visual needs of the patient in combina-tion with careful estimation of the potential forthe return of visual function after surgery thatfinally serves as the basis for the ophthalmolo-gist to decide whether surgery is indicated anduseful.

THE ART AND THE SCIENCE OF CATARACT SURGERY
20
Figure 7 A: How the PAM Works -Cross Section View
Figures 7 A and 7 B demon-strate in cross-section the views shownin Figs. 6 A-B. In (A), the light beam(arrow) can be seen striking a lens opac-ity (C) and thus does not penetrate thelens. The patient in this case cannot seethe projected Snellen chart.
Figure 7 B: How the PAM Works -Cross Section View
In Fig. 7-B the light beam isdirected to another part of the pupilwhere it is focused between lensopacities so that the projected Snellenchart passes to the posterior pole.Hence the patient will see the chartand respond so that we can determinethe effective potential visual acuity.

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
21
PREOPERATIVE GUIDELINES FOR CATARACT SURGERY INCOMPLEX CASES
HOW TO PROCEED IN PATIENTSWITH RETINAL DISEASE
The Importance of Pre-Op FundusExam
Thorough peripheral retinal examinationshould be done before cataract extraction. Weare all proud to be first class clinical ophthal-mologists and not think of cataract surgeryonly as a mechanical, technical procedure. Aspatients live longer, they are apt to have morepreoperative diseases sometimes difficult todiagnose unless we are on the alert for them.Because the patient with an even moderatedegree of cataract has reduced clarity of vision,it is easily possible that recent abnormalitiesmay not have been observed or reported by thepatient. This is particularly the case withretinal diseases.
CATARACT SURGERY INDIABETIC PATIENTS
Because of the increasing importanceof diabetic retinopathy, both in incidence andseverity, we provide special emphasis to thisdisease in considering cataract surgery in com-plex cases. Cataract and retinovascular com-plications often co-exist in diabetic patients.The combination can present problems in de-termining the cause of decreased vision. Cata-ract surgery can also result in rapid pro-gression of diabetic retinopathy that mayneed treatment with photocoagulation(Figs. 8 and 9)..
Diabetic patients are very predisposed todeveloping cataracts. This is especially true ofyounger diabetic patients, who are also highlypredisposed to developing diabetic retinopathy(diabetes Type I). In a series of diabetic retin-opathy and maculopathy patients 15 yearsafter laser treatment, only 22% of the eyesmaintained clear lenses (Figs. 10 and 11).Cataracts will often form following vitrectomysurgery for diabetic retinopathy.
Rarely retinopathy can cause cataracts.An example would be prolonged vitreouscavity hemorrhage that results in a partialopacification of the lens. (Very high risk pro-liferative diabetic retinopathy - Fig. 12)
Evaluating Diabetics Prior toCataract Surgery
Clinically significant macular edema(CSME) and less obvious macular changes innon-proliferative retinopathy may be the causeof decreased vision in addition to the cataract(Fig. 13).
It is important to listen to the patient'shistory when evaluating the cause of visualdeterioration. This can be helpful in decidinghow much of the visual loss may be due tocataract as opposed to visual damage caused byretinovascular conditions.
A good fundus examination through adilated pupil is essential. In diabetic patients asin all patients, cataract should be removedwhen a patient's visual function does not meethis/her visual needs and the visual loss is con-sistent with the cataract. It is very rare that

THE ART AND THE SCIENCE OF CATARACT SURGERY
22
Figure 9: Significant Regression of Retinal Neovascularization Following Scatter Photocoagulation
You may observe that the large nets of vessels shown in Fig. 8 have regressed following treatment with scatterphotocoagulation of the proliferative neovascularization existing before cataract surgery. You may observe the laser burns. Ifthe fundus is adequately visible in spite of the cataract, it is preferable to perform photocoagulation before doing cataract surgery.(Photo courtesy of Prof. Rosario Brancato, M.D., from Milan, Italy, reproduced from "Practical Guide to Laser Photocoagu-lation", Italian Edition by Brancato, Coscas and Lumbroso, published by SIFI).
Figure 8 : Scatter Photocoagulation to Ischemic Retinal Area Invaded by Vessels in Diabetic Retinopathy
Cataract extraction does not cause retinopathy to develop when it was not present before cataract removal, but itdefinitely may worsen pre-existent retinopathy, particularly if there is a proliferative retinopathy already present. This figureshows an ischemic area of the retina being treated with scatter photocoagulation. Please observe the large nets of vessels. (Photocourtesy of Prof. Rosario Brancato, M.D., from Milan, Italy, reproduced from "Practical Guide to LaserPhotocoagulation", Italian Edition by Brancato, Coscas and Lumbroso, published by SIFI).

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
23
Figure 10 (above right): Focal Photo-coagulation for Diabetic MaculopathyPrevious to Cataract Surgery
The laser applications are di-rected to the microvascular alterationsresponsible for chronic, leaking fluidwhich gives rise to macular edema. (Photocourtesy of Prof. Rosario Brancato,M.D., from Milan, Italy, reproduced from"Monografie della Societa OftalmologicaItaliana", Italian Edition by Brancato andBandello, published by ESAM).
Figure 11 (below left): Grid Treatment with Photocoagulation for Diabetic Maculopathy
Ophthalmoscopic appearance after grid pattern treatment of the macula in whichdiffuse rather than focal leakage is identified on the fluorescein angiogram. Only 22% ofthese eyes maintain clear lenses 15 years after laser treatment, particularly younger diabetics.(Photo courtesy of Prof. Rosario Brancato, M.D., from Milan, Italy, reproduced from"Monografie della Societa Oftalmologica Italiana", Italian Edition by Brancato and Bandello,published by ESAM).

THE ART AND THE SCIENCE OF CATARACT SURGERY
24
cataracts need to be removed so that treatmentof the diabetic retinopathy can be performed.Occasionally, cataracts need to be removedwhen performing vitrectomy.
It is important that we consider variousdiabetic factors in planning cataract surgerybecause the retinopathy can influence theresult. We may see increased bleeding andfibrin formation, especially in the younger pa-tients with active retinopathy and compromisedretinal perfusion.
Importance of Maintaining theIntegrity of the Lens Capsule
Cataract surgery may not only result inrapid progression of diabetic retinopathy, butit may also complicate its management andtreatment. Rapid deterioration often occurs
when the lens capsule and zonular integrityare sacrificed by the cataract surgery suchas with rupture of the posterior capsule.Retained lens material may produce increasedinflammation, which may further acceleratethis process. While it is important to maintainan intact posterior lens capsule, it is equallyimportant to have an easily dilatable pupil anda clear capsule to allow a good fundus viewthrough which laser treatment can be performed.
Significant Increase in ComplicationsFollowing Cataract Surgery
The progression of retinopathy follow-ing cataract surgery may take several forms.We may see a patient with non-proliferativeretinopathy rapidly develop macular edema(CSME) (Figs. 10, 11 and 13). Macular edema
Figure 12: Severe, Advanced ProliferativeDiabetic Retinopathy, Very High-Risk - AProlongued Vitreous Cavity HemorrhageMay Result in Partial Opacification of Lens
Artistic rendition of severe, advanced,proliferative, very high risk diabetic retinopa-thy. (A) Shows a fundus view of a severe caseof proliferative diabetic retinopathy. There arepreretinal hemorrhages (H) in several loca-tions. Note the extensive active fibrovascularproliferation causing a traction detachment (D)nasally due to traction from the fibrovasculartissue (A) on the retina. There is also activefibrovascular proliferation along the retinalvessel arcade (V) with detachment of the macu-lar area. Note the active fibrovascular stalk (S)which obscures the optic nerve. (B) Shows thesame eye with the surgeon's view as seen throughthe pupil, and accompanying cross section viewof the tissue pathology. Note hemorrhage (H),traction (arrows) of the posterior hyaloid (C),traction detachment of the retina (D), and ac-tive fibrovascular stalk (S) on the optic nerve.

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
25
may progress from being diffuse to being cys-tic. Rafael Cortez, M.D., has observed thatdiabetic patients with proliferative retinopathy(Fig. 12), or non-proliferative retinopathy(Fig. 13) or even without retinopathy, have ahigher risk of developing a vitreous hemor-rhage, rubeosis of the iris and neovascularglaucoma postoperatively. This risk is particu-larly high in those patients with proliferativeretinopathy (Fig. 12).
Appropriate Laser Treatment
Most diabetic retinopathy complicationscan be prevented by appropriate laser treat-ment before cataract surgery. Eyes with non-proliferative retinopathy that have clinically
significant macular edema (Figs. 13 and 14)should receive focal or grid laser treatment(Figs. 10, 11 and 14) to seal the leakage whichis detectable through fluorescein angiography.Eyes with severe, non-proliferative (pre-pro-liferative) diabetic retinopathy (Fig. 15) andproliferative retinopathy (Fig. 16) shouldreceive panretinal laser photocoagulation(Fig. 17) before cataract surgery. This treat-ment will reduce additional proliferation anddeterioration.
Even with a cataract, laser treatment canusually be performed with good pupillary dila-tation. Krypton red wavelengths are oftensuccessful in penetrating somewhat densenuclear sclerotic lenses (Fig. 14). Retrobulbaranesthesia may be necessary.
Figure 13: Diabetic Macular Edema
(A) Shows the fundus view of diabeticmacular edema. Notice thickening of the macu-lar area (F). From the oblique cross section (B),an area of the retina and choroid is magnified in(C) to show its relationship to the clinical oph-thalmoscopic fundus view above. In (C), there ispooling of fluid (D) within the inner layers of theretina. This fluid is trapped between the gan-glion cell layer (G) and the outer plexiform layer(P). Notice there is almost complete loss of theintermediary neurons (N) in this area.

THE ART AND THE SCIENCE OF CATARACT SURGERY
26
Figure 14 (above right): Prevention of Dia-betic Retinopathy Complications by LaserTreatment before Cataract Surgery
Most diabetic retinopathy complicationscan be prevented by appropriate laser treatmentbefore cataract surgery. Eyes with non-prolif-erative retinopathy that have retinal thickeningfrom edema near the macula should receivefocal treatment of the macular aneurysms toerase fluorescein leakage. As shown in thisfigure, even with a cataract, krypton red wave-lengths are often successful in penetrating fairlydense nuclear sclerotic lenses. Laser treatmentmust be performed with good pupillary dilata-tion.
Figure 15 (center): Severe Non-Proliferative Dia-betic Retinopathy (Pre-Proliferative).
This photo shows a characteristic severe, non-proliferative diabetic retinopathy, previously knownas pre-proliferative. Please observe prominent softexudates, dot blot hemorrhages, venous beading, andmicroaneurysms. (Photo courtesy of Lawrence A.Yannuzzi, M.D., selected from his extensive retinalimages collection with the collaboration of Kong-Chan Tang, M.D.)
Figure 16 (below right): Proliferative DiabeticRetinopathy
This photo shows the next stage in severityof the disease. Please observe a large subretinalhemorrhage surrounding soft cotton exudates at thelower temporal arcade. There are also multipleintraretinal hemorrhages with neovascularizationelsewhere (NVE), which is defined as a proliferativeretinopathy anywhere in the retina which is greaterthan 1 disc diameter from the optic disc margin. Themacula is not shown. (Photo courtesy of SamuelBoyd, M.D., Clinica Boyd, Panama).

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
27
Main Options in Management ofCo-existing Diabetic Retinopathy andCataract
The first and most successful is to deferthe cataract surgery until laser treatment can beperformed. If there is extensive vitreous hem-orrhage or traction retinal detachment, you
Figure 17 (above right): Panretinal Laser Photocoagula-tion Before Cataract Surgery
In treating diabetic retinopathy, panretinal photoco-agulation covers all of the periphery and mid-periphery of theretina from the ora serrata to the vascular arcades, sparing onlythe posterior pole. (Photo courtesy of Prof. Rosario Brancato,M.D., from Milan, Italy, reproduced from "Practical Guide toLaser Photocoagulation", Italian Edition by Brancato, Coscasand Lumbroso, published by SIFI.
may need to combine the cataract removal witha vitrectomy (Fig. 18).
Intraocular lenses do not present a prob-lem when a patient is going to have a vitrec-tomy. The visual results of pseudophakic eyeswith diabetic retinopathy complications thathave vitrectomy surgery are essentially identi-cal to those of phakic eyes.
Figure 18: Need to Combine Cataract Removalwith Vitrectomy (Vitreous Hemorrhage andTraction Retinal Detachment)
The first indication for vitrectomy in thecase of proliferative diabetic retinopathy is thepresence of vitreous hemorrhage (H). This isconditional, however, depending on several factorssuch as status of retinopathy, visual loss, adequacyof previous photocoagulation, frequency ofhemorrhage, vision in the fellow eye, advancing irisneovascularization, response to vitreous surgery infellow eye, and systemic factors. In general, surgeryfor retinopathy is more likely to be indicated withhemorrhage in the presence of active fibrovascularproliferation or traction retinal detachment. This isthe second indication for vitrectomy, namely atraction retinal detachment, but only when the macula(M) is detached as shown. Note contraction (arrows)of posterior hyaloid (P) causing a non-rhematogenousretinal detachment (D) due to traction from thefibrovascular tissue (A) on the retina.

THE ART AND THE SCIENCE OF CATARACT SURGERY
28
CATARACT SURGERY ANDAGE-RELATED MACULARDEGENERATION
Felix Sabates, M.D., has best outlinedthe precautions we must take when consideringextracapsular extraction or phacoemulsifica-tion in eyes with already present age-relatedmacular degeneration already present. Theseprinciples are: 1) It is important to study themacular area in detail prior to cataract surgeryto detect the presence of age-related maculardegeneration. 2) If cataract surgery is per-formed in the presence of age-related maculardegeneration, special care should be taken toreduce the possibility of inflammation evenif it would require immediate use of anti-inflammatory drugs. 3) Cystoid macular edemashould be aggressively treated, with carefulfollow-up emphasized. 4) Cataract surgeryshould not be performed on the patient withactive "wet" macular degeneration (Fig. 19)until it has been brought to a dry stage (Fig. 20).If there is bleeding from a neovascular mem-brane, cataract surgery should be postponeduntil at least six (6) months after the blood hascompletely reabsorbed and there has beenno recurrence of the bleeding has been present.5) In patients with macular scars (Fig. 20) andopaque cataracts, surgical removal of the opaci-fied lens with intraocular lens implantationmay be of benefit in recovering some degree ofpericentral or peripheral vision. The smallerthe macular scar, the better the prognosis. Nocataract surgery should be performed unlessthe cataract is opaque enough so that when it isremoved, the patient will probably perceive thebenefit of the operation.
RETINAL BREAKS AND RETINAL DE-GENERATIONS PRIOR TO CATARACTSURGERY
The preoperative treatment of these reti-nal lesions has traditionally come into consid-eration as a possible means of preventing reti-nal detachments after cataract extraction, espe-cially in myopes. I refer only to those periph-eral retinal degenerations which can be clini-cally defined and identified, and which havestatistically been linked with retinal detach-ment following posterior vitreous detachments.This, therefore, excludes senile retinoschisis,which has a higher prevalence in the generalpopulation than among patients with a retinaldetachment. What needs to be clarified is theeffect of cataract surgery on the risk retinalbreaks and degenerations present and whatrecommendations should be given in regard totheir management prior to cataract surgery.This requires therapeutic proof that prophylac-tic treatment significantly lowers this risk be-low that which the natural course of untreatedlesions would present. There is an increasingtendency to support the concept that retinaldetachments generally are associated with re-cent, not old, retinal breaks. At the present timethe picture is not clear. We lack solid reportssupporting the prophylactic treatment of pre-existing retinal breaks prior to cataract surgery.
What happens to an eye with lattice de-generation when cataract extraction is per-formed? Again, we face a lack of valid reportsin the literature to support preventive treatmentprior to cataract surgery. About 90% of eyeswith lattice degeneration do not detach aftersmall incision cataract extraction even when

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
29
Figure 19 (above right): Anatomy and Pathology ofExudative, ("Wet") Macular Degeneration withExtrafoveal Neovascularization
Cataract surgery should not be performed inthese cases. Wait until it has been brought to dry stage asshown in Fig. 20. Fundus view (A) shows an example ofexudative "wet" macular degeneration with an extrafovealneovascular membrane (N) and limited subretinalhemorrhage (H) just at the margin of the paramacularretinal vessels surrounding the fovea (F). From theoblique cross section (B), an area is magnified in (C) toshow the direct relationship between clinicalophthalmoscopic fundus view above and its correspondingcellular pathology. Pathology reveals that the retina isslightly elevated over a neovascular membrane (N). Notevessels emanating from the choriocapillaris (J), into theneovascular membrane (N) and into the sub-RPE andsubretinal spaces, passing through small breaks (T) in theretinal pigment epithelial cell layer (E). There is someatrophy of photoreceptors in this area (P). Subretinalblood (H) is seen to either side of the neovascularmembrane. Large choroidal vessels (K).
Figure 20 (below left)): Anatomy and Pathology ofNon-Exudative, Geographic ("Dry") MacularDegeneration
In these patients, surgical removal of the opacifiedlens with IOL implantation may be of benefit in recoveringsome degree of peripheral vision. Fundus view (A) showsan example of non-exudative, geographic atrophic "dry"macular degeneration where atrophy of the retinal pigmentepithelium predominates. The smaller the macular scar,the better the prognosis for cataract surgery. Notice theclinical signs of drusen (D) which can appear as discretesubretinal bodies, confluent masses or hard glinting lesions,usually yellowish in color. Darker intraretinal pigment (I)may or may not be present. Retinal pigment epitheliumatrophy (E) is identified by prominence of the underlyingchoroidal vessels. From the oblique cross section (B), anarea is magnified in (C) to show the direct relationshipbetween the clinical ophthalmoscopic fundus view aboveand its corresponding cellular pathology. Pathologyincludes subretinal drusen (D) and atrophy of the RPE (E).Compare the disorganized RPE cell layer at (E) on theright to the more normal configuration at (N) on the left.Most importantly, though not clinically visible, there isdefinite loss of photoreceptors (P) in the area ofdegeneration (compare with normal photoreceptor layeron the left). Other anatomy: inner limiting membrane (L),choriocapillaris (J) and large choroidal vessels (K).

THE ART AND THE SCIENCE OF CATARACT SURGERY
30
YAG laser capsulotomy is later performed.Those that do develop a retinal detachmentfrequently do not detach from retinal breaksadjacent to or within the lattice lesions, butfrom unrelated areas which previously lookedclinically normal. This has now been observedby numerous investigators.
Sabates thinks that each case must beindividualized. If a patient has a history ofretinal detachment in one eye and latticedegeneration with retinal holes in the other eye,he performs cryosurgery or laser surgery andcloses those holes in the second eye. Usuallycryosurgery is required because the cataract
may preclude the use of laser. The type of tearpresent and other factors including the locationof the tear and the existence of high myopiawould influence the ophthalmologist's judg-ment in deciding when to treat. Fig. 21 showsthe typical retinal tear that he treats, sealedwith cryotherapy.
Since seven to eight percent of the popu-lation has lattice degeneration, it is obvious thatnot all patients with lattice degeneration shouldbe treated. Regardless of whether the patient istreated prior to cataract surgery, those patientsshould be followed closely with careful exami-nation of the peripheral retina postoperativelyfollowing cataract removal.
Figure 21: Creating the Chorioretinal Ad-hesion of Retinal Tear with CryotherapyBefore Performing Cataract Surgery
This figure presents the treatment withcryotherapy of a retinal tear that needs to besealed prior to cataract surgery. The freezingand defrosting is observed with the indirectophthalmoscope. (A conceptual slit beam hasbeen added to this illustration to enhance the3-dimensional nature of the view).

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
31
CATARACT SURGERY IN PATIENTSWITH UVEITIS
Rubens Belfort Jr.,M.D., in Sao Paulo,Brazil and Martinez Castro in Mexico haveconducted extensive research on these patients.Cataracts develop frequently in patients withuveitis, either as a result of inflammation, thetreatment of inflammation or both. There hasbeen much controversy as to what to do, howto do it and when to operate in patients withcataract and uveitis, and whether intraocularlenses should be implanted in these patients.
Professor Rubens Belfort Jr. consid-ers that uveitis is one of the last categoriesfor which surgeons have advised «don’t do it»when cataract surgery is considered. Cataractsurgery has been regarded as contraindicatedbecause of the initial bad results with in-traocular lenses (IOLs) in patients with uvei-tis. Until about 10 years ago, most surgeonsavoided cataract surgery with or without IOLimplantation in these patients.
There was concern about superim-posing IOL implantation, with the inflamma-tion which used to accompany it in manycases, on a seriously compromised and al-ready inflamed eye. This concept has nowchanged. The development of current tech-niques for small incision cataract surgery,new types of IOLs, and advances in themanagement of patients with uveitis havechanged the prognosis. The change is fortu-nate because cataracts are the major cause ofloss of vision in patients with chronic uveitis(Fig. 22). Moreover, cataracts are potentiallydangerous for patients with uveitis becausethey interfere with visualization of the fun-dus, denying the ophthalmologist the op-portunity to identify macular lesions andto treat them adequately. When these pa-
Figure 22: Uveitic Cataract
Cataracts caused by an inflammatory uveitic processgenerally occur with pigment deposits (P) on the anterior cap-sule of the lens (C) related to anterior synechiae that can im-mobilize the pupillary sphincter. The intensive use of topicalsteroids for the management of the uveitis can hasten the for-mation of such cataracts. Cataracts are the major cause ofloss of vision in patients with chronic uveitis. Current tech-niques for small incision surgery, new types of IOL's and ad-vances in management of uveitis enable their removal wherepreviously this was contraindicated.

THE ART AND THE SCIENCE OF CATARACT SURGERY
32
tients finally undergo long-postponed sur-gery, usually with good anatomic success,central vision may not be recovered becauseof irreversible macular damage that haddeveloped from chronic cystoid macularedema. Therefore it is critical for both thesurgeon and the patient with uveitis to realizethere is another reason for cataract surgery inaddition to improving vision as much aspossible. Removal of the cataract enables thethe ophthalmologist to examine and treat themacula in order to forestall damage.
Method of Choice
In theory, removal of the lens as awhole (intracapsular) could lead to lessinflammation. In fact, careful extracapsularsurgery with adequate cleaning of the lensmaterial during surgery usually provides abetter outcome. Most surgeons now preferphacoemulsification to a classic extracapsu-lar extraction of the cataract even in patientswith uveitis. Belfort believes phacoemulsifi-cation leads to faster results and lessinflammation, and he advocates phaco-emulsification with or without an IOL.Intracapsular technique is no longer usedexcept in some rare cases of lens-induceduveitis, in which inflammation is caused bythe leakage of protein material from the lens.
Diagnosing the Type of Uveitis in thePre-Operative Phase
Belfort emphasizes that in the preop-erative phase, it is very important for thesurgeon to determine the exact type of uveitisthe patient has in order to better predict thesurgical outcome and minimize reaction. For
instance, patients with ocular sarcoid have amuch worse postoperative course than otherpatients. Therefore, a patient with sarcoidosisand uveitis, even in the absence of importantuveitis, must be approached more carefullythan patients with other types of uveitis.Other types of uveitis that can be effectivelymanaged are Fuchs’ heterochromic cyclitis,intermediate uveitis, and posterior uveitis aswell as most of the anterior essential uveities.Behcet’s disease and other vascular inflam-mations, which in the past were considered tohave a bad prognosis, have shown muchbetter results with current techniques.
Preoperative Management
In general, the less inflamed the eye atthe time of surgery, the better the prognosis.Ideally, every patient should be operated onlyafter being inflammation-free for at least 3months, although this is not possible in manycases. Uveitis is chronic, no matter what doseof steroids is used, and many patients must beoperated even in the presence of some activeuveitis. The goal is to have the eye as littleinflamed as possible. Preoperative steroids, aseyedrops or even systemically, as well asimmunosuppressive drugs have to be used inmore severe cases. In patients who do notrespond to steroids alone, Belfort uses sys-temic oral cyclosporin and oral prednisonetherapy. In 20% of patients the use of anIOL is not advisable. This includes patientswith granulomatous uveitis such as sarcoid,Vogt-Koyanagi-Harada syndrome, and sym-pathetic ophthalmia. Belfort also advisesagainst using IOLs in patients with juvenilerheumatoid arthritis, who tend to have achronic disease and may develop long-termcomplications.

Chapter 2: Ind ica t i ons and P reopera t i ve Eva lua t i on
33
The Intraocular Lens
Currently, IOLs can be used in at least80% of patients with both uveitis and cata-ract. Selecting the right type of IOL is veryimportant. Although PMMA lenses are welltolerated by the eye with uveitis, they maylead to more posterior capsule opacificationthan other lenses. Belfort recommends notusing silicone in cases of uveitis becausesilicone lenses by themselves can causeuveitis and may aggravate previous intraocu-lar inflammation, especially in heavily pig-mented people. Belfort therefore prefers touse acrylic lenses in these patients. We donot yet have clinical trials or studies thatestablish conclusively the superiority of onelens material over another. Results appear notto be better with heparin-coated IOLs thanwith PMMA lenses in patients with uveitis.Considering that heparin-coated lenses arealso more expensive, Belfort does not advo-cate using them in uveitis.
CATARACT SURGERY IN ADULTSTRABISMUS PATIENTS
Preoperative Judgment
The treatment of co-existing cataract andstrabismus traditionally has been managed withseparate operations. Usually the cataract ex-
traction has been done first, followed later by asurgical correction of strabismus. As a matterof fact, we may even hesitate to remove acataract in a patient who has had a deviated eyefor a long period for two reasons: First, cataractremoval may result in postoperative diplopia,and second, it is difficult to predict whetheramblyopia may be present in the deviated eye,leaving us with a questionable prognosis.
Successful combined cataract and stra-bismus surgery is highly feasible. The idealpatient for a combined approach must fill cer-tain prerequisites: one, he or she must have acongenital strabismus rectifiable by surgery ona single muscle in each eye. Second, the patientmust have an alternating deviation and equalfusion potential in each eye, determined eitherby knowing the patient's vision before the onsetof the cataracts or by the results of the potentialacuity meter (PAM) that should be about equalin both eyes (see figures 3 through 7). An equalpotential acuity meter measurement in botheyes would seem to exclude amblyopia, therebyimproving the chances for an optimal visualoutcome.
During combined cataract and strabis-mus surgery, if the patient continues to blink orsqueeze the eyelids following the combinedtopical and intracameral anesthesia, you canobtain anesthetic control this a sub-Tenon'sinjection of lidocaine as illustrated in Figs. 33and 34. The effect is almost instantaneous, andsurgery can continue without delay.

THE ART AND THE SCIENCE OF CATARACT SURGERY
34
BIBLIOGRAPHY
Boyd, BF.: Cataract Surgery in Diabetic Patients.World Atlas Series of Ophthalmic Surgery, pub-lished by HIGHLIGHTS,Vol. IV, 1999; 9:153-54.
Boyd, BF.: Undergoing cataract surgery with amaster surgeon: A personal experience. Highlightsof Ophthalm. Journal, Vol. 27, Nº 1, 1999;2-3.
Charlton, Judie: Cataract surgery and lens implan-tation. Editorial Overview, Current Opinion inOphthalmology, 2000, 11:1-2.
Fine, IH.: Cataract surgical problem: Consultationsection. J Cataract Refractive Surg, 1997; 23:704.
Gimbel, HV., Anderson Penno, EE: Cataracts:Pathogenesis and treatment. Canadian Journal ofClinical Medicine, September 1998.
Gimbel HV., Basti S., Ferensowicz MA., DeBroffBM: Results of bilateral cataract extraction withposterior chamber intraocular lens implantation inchildren. Ophthalmology, 1997; 104:1737-1743.
John K., Fenzl R.: Preoperative Workup. CataractSurgery: The State of the Art. Edited by Gills, JP.,Slack; 1998; 1:1-8.
Lacava, AC., Caballero, JC., Medeiros, OA., Cen-turion, V.: Biometria no alto miope. Rev Bras deOft. 1995;54:619-622.
Masket S.: Preoperative evaluation of the patientwith visually significant cataract. Atlas of Cata-ract Surgery, Edited by Masket S. & Crandall AS,published by Martin Dunitz Ltd., 1999, 1:3-5.
Neumann D., Weissmann OD., Isenberg SJ., et al:The effectiveness of daily wear contact lenses forcorrection of infantile aphakia. Arch Ophthalmol.1993;111:927-9.

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
37
IOL POWER CALCULATIONIN STANDARD AND COMPLEX CASES
PREPARING FOR SURGERY
Making Patients Confident
From the minute the patient considersundergoing surgery, fear is present. There isfear of the unknown and fear of someone oper-ating on your eye. Jack Dodick, M.D., fromNew York, believes in the important influenceof office personnel and environment on mak-ing patients confident and comfortable. Dodickstrongly advocates hiring and training high-level professional staff. When patients interactwith highly competent staff at every encounter,they tend to conclude that the doctor must bevery good because he has selected and trainedhis staff so well. Many doctors pay too littleattention to the impressions staff make on theirpatients. They are tempted to cut corners byhiring clerks at low pay if they fail to realizethat patients’ impressions of staff are integralto their impressions of their physician.
In addition, the office environmentshould be tasteful. The impression patientshave when they enter the office influencestheir feelings about their physician. An officethat is dirty and cluttered reflects poorly onthe practice. Dodick believes that once pa-tients feel respected and comfortable with theexpertise of the physician and his/her staff,they relax and decide they have come to theright place.
Patients Encounter with thePhysician
And in the encounter with the physicianpatients should feel respected and important.Even though the waiting room is busy, every-thing should seem unhurried when the pa-tient is sitting in the chair across from thephysician. The ophthalmologist should con-vey the impression that, at this time, thepatient is the most important person.
The physician’s ability to project a con-fident manner is also critical to success.Dodick believes it is an art to convey thisconfidence and professionalism to patients. Itis partly done through certain inflections inthe voice; perhaps it is easier to explain inreverse. Sometimes the doctor who does notfeel totally secure in his ability to produceresults may become a little defensive, andgive more emphasis to potential complica-tions than the real positive benefits of theoperation. “Well, you have a cataract. As youknow, you can have it operated on or not, andthere are some complications that sometimesoccur. For example. . .” Although potentialcomplications are in fact true, the chance thatthese complications will occur is minimal.Dodick does not dwell on these rare potentialcomplications. Instead, he emphasizes the

THE ART AND THE SCIENCE OF CATARACT SURGERY
38
very high probability of positive results whencommunicating with patients. He retains aposition of objectivity in order that his ownperspective will not unduly influence the pa-tient. The patient must be informed of poten-tial risks but with modern small incisioncataract surgery, they are very unusual.
Ingredients of a Strong Rela-tionship
The physician’s ability to instill confi-dence and trust in patients, and an ability toarticulately convey his confidence throughthe spoken word are the basic ingredients of astrong relationship between physician andpatient.
A fundamental question is how shouldthe ophthalmologist approach patients whomeasure well on Snellen acuity, but stillcomplain about their vision because of thevery important factors of contrast sensitivityand glare we have already discussed. Dodickfollows these basic steps. He first listens tothe patient and tries to make a historicaldetermination about how happy or incapaci-tated they are because of their vision. Ifpatients claim to be very happy with theirvision, Dodick goes no further. He merelyinstructs them that they, like everyone over50, have some lens changes. He explains thebasic anatomy of the human eye (Fig. 1-A),with its clear windows inside and outside, andthe tendency of the inside window to becomecloudy. The treatment, of course, is to replacethe cloudy window with a clear window andthereby restore their vision.
In approaching the question of when acataract should be removed, Dodick rein-forces the concept that in nearly all condi-tions, cataract surgery is 100% elective. Thetime to remove a cataract is the time that
patients decide they are unhappy withtheir vision. Most people understand this, butoften Dodick hears the question, “Whatwould you do in my position?” Dodickhandles this by looking the patient in the eyeand responding: “This is a very simple ques-tion. If I were very happy with my visionright now, I would do nothing. If I wereunhappy, I would decide in a minute to havecataract surgery.” Then patients fully realizethat cataract surgery is truly an elective proce-dure.
Evaluating the Patient's Cataract
Of course, giving patients this choice ispredicated upon the fact that the ophthal-mologist has conducted a thorough examina-tion. With slit lamp biomicroscopy posteriorsubcapsular cataracts which strongly inter-fere with vision by inducing a great deal ofglare are very easy to evaluate, whereasnuclear sclerotic cataracts are often difficultto evaluate on the slit lamp. People withposterior subcapsular cataracts can measure20/20 or 20/25 on Snellen acuity because theyare really looking through the little pinholesof the posterior subcapsular cages (Fig. 23-A-B). The minute they see oncoming head-lights while driving at night, for instance, theglare may diminish their functional visionto 20/100 or even 20/200. On the other hand,people with nuclear sclerosis, the most com-mon form of cataract, tend to complain aboutcontrast sensitivity rather than glare (Fig. 23-C-D).
Over the years Dodick has found that agood way to evaluate lenticular or mediachanges is to examine the red reflex of thepatient by holding an ophthalmoscope about12 to 14 inches from the eye and determiningwhether it is a bright red reflex, a gray reflex,

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
39
Figure 23 A-D: Posterior Subcapsular Cataract (top, left and right). Cataract with Nuclear Sclerosis (bottom, left andright)
Figures 23 A and B are three dimensional photographs of a characteristic posterior subcapsular cataract, seen with theslit lamp (top-left) and with indirect illumination also using the slit lamp (top-right). Patients with posterior subcapsularcataracts can measure 20/20 or 20/25 on the Snellen visual acuity chart in the examining room, because they are seeing throughthe little pinholes of the posterior subcapsular cages. When they are exposed to oncoming headlights while driving at night,the glare may diminish their functional vision to 20/100 or even 20/200.
Figures 23 C and D are three dimensional photos of nuclear sclerotic cataract, viewed with diffuse illumination (left)and with the slit lamp beam (right). This is the most common form of cataract. Patients tend to be hindered more by loss ofcontrast sensitivity rather than glare. (Reproduced with permission from AAO's Basic and Clinical Science Course, Lens andCataract, 1999, pp.42, 48, enhanced by HIGHLIGHTS).

THE ART AND THE SCIENCE OF CATARACT SURGERY
40
or a dark black reflex. This provides a goodindicator of opacity. In some circumstances anuclear cataract can be better evaluated withthis technique than with the slit lamp. Dodickdoes not rely on tests for contrast sensitiv-ity when evaluating cataracts. Althoughconditions of glare can be simulated in aclinical setting, Dodick relies on thepatient’s real life test experience instead.
Approaching the Day ofSurgery
Once Dodick and his patient havereached the mutual understanding that cata-ract surgery may be beneficial, the patient isin essence turned over to a series of highlytrained, dedicated, professional staff whowork closely with him. The next person thepatient sees is a highly trained technician. Thetechnician explains that a measurement isneeded to determine the correct lens to im-plant into the eye, and they undergo anultrasonography scan. When the test is com-pleted, the patient is turned over to the surgi-cal counselor, who has become a master atmaking patients comfortable and ready toapproach the day of cataract surgery.
Patient's Expectations
It is essential to clarify to the patientwhat he/she may expect and what not toexpect. Postoperative patient satisfaction isbased on this pre-op surgeon-patient commu-nication and understanding. What are thepatient's daily needs and what final uncor-rected visual acuity for distance and near hewould prefer? Does he want to read withoutglasses? If so, then he must know he wouldnot see perfectly clearly for distance. If he/she are myopes and consequently read with-
out glasses, by all means do not sacrifice theirnear vision just for providing 20/20.
The availability of foldable multifocalIOL's makes this surgeon-patient understand-ing even more critical so that the visualadvantages of these lenses need to be fullyappreciated versus the disadvantages whichexist but may be less significant. A similarsituation presents with the alternative ofmonovision. If the surgeon contemplatesusing this method, which is a good alterna-tive for many patients, it is important to makesure the patient understands how this worksand be enthusiastic with this alternative. Fi-nal visual satisfaction with these methods,multifocal IOL's and monovision, will de-pend a great deal on the selection by thesurgeon of the right patient for these alterna-tives. With multifocal IOL's patients arehappier with bilateral implantation. Withmonocular implantation, it is preferable not todelay surgery in the fellow eye unless there isa major reason, because most patients feelvery insecure with monocular vision and hav-ing only one eye operated.
DETERMINING IOLPOWER (BIOMETRY)
Ocular biometry must be performedprior to cataract surgery. There is noquestion that when well selected and prop-erly done the ultrasonic methods afford usthe best way of achieving the desired postop-erative refraction. Determination of intraocu-lar lens power through meaningful keratom-eter readings and axial length measurementthrough A-Scan ultrasonography has be-come a "standard of care". It is a challengingtechnique and crucial to the visual result andpatient satisfaction.

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
41
Postop Refractive Errors NoLonger Admissible
This is particularly true considering thehigh patient's expectations and the minimalastigmatism created by small incision cataractsurgery, particularly phacoemulsification.Patients look forward to wearing spectaclespostoperatively only under special circum-stances. As emphasized by Centurion andZacharias, postoperative refractive errors are
no longer admissible. In small incision tech-niques, cataract surgery has attained the statusof refractive surgery. Therefore, exact deter-mination of the IOL power to end up with thespecific planned postoperative refraction isessential. The advent of multifocal foldableIOL's makes this even more of an important,though complex subject, as well as operatingon eyes with different axial lengths: normal(Fig. 24), short as in hyperopia (Fig. 25 A-B),long as in myopia (Fig. 26).
Figure 24: Determination of IOL Power inPatients with Normal Axial Length (Nor-mal Eyes) - Mechanism of How UltrasoundMeasures Distances and Determines AxialLength
The use of ultrasound to calculate theintraocular lens power takes into account thevariants that may occur in the axial diameterof the eye and the curvature of the cornea. Theultrasound probe (P) has a piezoelectric crys-tal that electrically emits and receive highfrequency sound waves. The sound wavestravel through the eye until they are reflectedback by any structure that stands perpendicu-larly in their way (represented by arrows).These arrows show how the sound wavestravel through the ocular globe and return tocontact the probe tip. Knowing the speed ofthe soundwaves, and based on the time it takesfor the sound waves to travel back to the probe(arrows), the distance can be calculated. Thespeed of the ultrasound waves (arrows) ishigher through a dense lens (C) than througha clear one. Soft tipped transductors (P) arerecommended to avoid errors when touchingthe corneal surface (S). The ultrasound equip-ment computer can automatically multiply thetime by the velocity of sound to obtain theaxial length. Calculations of intraocular lenspower are based on programs such as SRK-II,SRK-T, Holladay or Binkhorst among others,installed in the computer.

THE ART AND THE SCIENCE OF CATARACT SURGERY
42
Figure 25 A (above right): IOL PowerCalculation in Patients With Very ShortAxial Length (Hyperopia)
In eyes with short or very shortaxial lengths as shown in Fig. 25 the thirdgeneration formulas such as Holladay 2and Hoffer-Q seem to provide the bestresults. Holladay has discovered that thesize of the anterior and posterior segmentsis not proportional in extremely short eyes(<20.0 mm). Only 20% of short eyespresent a small anterior segment(nanophthalmic eyes); 80% present a nor-mal anterior segment and it is the posteriorsegment that is abnormally short as shownhere. (P) represents probe, (S) representscorneal surface.
Figure 25-B (below left): Concept of thePiggyback High Plus Intraocular Lenses
In cases of very high hyperopia, aclear lens extraction may be done combinedwith the use of piggyback high-plusintraocular lenses. One (A), or two (B) or,some surgeons suggest, three or moreintraocular lenses can be implanted insidethe capsular bag (C). This piggybackimplantation technique may solve theproblems of having to implant a lens of over+30 diopters with its consequent opticalaberrations, but the procedure may give riseto postoperative complications. Someprestigious surgeons have their reservations(see text).

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
43
The Challenge of the ComplexCases
The use of refractive surgery on thecornea using a variety of techniques: excimer(Fig. 27), RK (Fig. 28), Intracorneal RingSegments (INTACS - Fig. 29) makes ocularbiometry even more complex. These refrac-tive corneal refractive techniques change theparameters in these special cases as comparedwith those we use for normal eyes and makethese special cases. Computerizedvideokeratography provides additional im-portant data.
The current acceptance of implantingIOL's in children following pediatric cata-ract surgery (Fig. 31) and the frequent useof vitrectomy with the use of silicone oil
(Fig. 32) frequently in Europe and infre-quently in the U.S., also add unique anddifferent difficult challenges, in performingan exact biometry in every individualpatient's condition. When using ultrasound,axial length is determined by measurement ofthe reflection of the eye tissue interfaces withthe ultrasonic beam (Fig. 24 - arrows). TheA-scan must be carefully calibrated and thebeam velocity must correspond to whether ornot the patient is phakic, pseudophakic, oraphakic and may need to be modified in thespecial cases previously described. The ultra-sound probe (T) has a piezoelectric crystalthat electro-mechanically emits and receiveshigh frequency sound waves. The soundwaves travel through the eye until they arereflected back by any structure that stands in
Figure 26: IOL Power Calculation in High Myopia
In high myopia with axial lengths higherthan 27.0 mm the use of the SRK II formula withan individual surgeon's factor has shown good pre-dictability of the refractive target. Probe (P), cor-neal surface (S).

THE ART AND THE SCIENCE OF CATARACT SURGERY
44
their way (represented by arrows). Assumingthe average velocity of the sound waves in theeye being measured, and based on the time ittakes for the sound waves to travel back tothe probe (arrows), a distance can be calcu-lated. The ultrasound equipment's computercan automatically multiply the time by thevelocity of sound to obtain the axial length.At least three scans should be obtained whichare within 0.15 mm of each other. Gimbelrecommends that the A-scan should be mea-sured twice by independent technicians if theaxial length is unusually short (Fig. 25) (hy-peropia) or long (Fig. 26) (myopia) (<22 mmor >25 mm), or if the difference between thetwo eyes is more than 0.3 mm, if the axiallength measurement does not correlate withthe refraction or the patient has difficulty withkeeping the eyes open or with fixation.
The Most Commonly Used For-mulas
The most commonly used IOL formulawas developed by Sanders, Retzlaff and Kraffand is known as the SRK formula, wherep = A - 2.5L - 0.9K. "P" refers to lens implantpower to produce emmetropia, "L" refers toaxial length, "K" refers to averagekeratometric readings in diopters and "A" is aconstant that is specific to the lens implantthat is to be used. Several second and thirdgeneration lens power calculation formulashave been developed including the SRK2 andSRK/T, Hoffer Q, and the Holladay 2 formu-las. Gimbel emphasizes that to avoid errorsin lens power calculations not only must thebiometry be accurate and the correct "A"
constant used, but also the estimated anteriorchamber depth (depending on the formula),preop refraction and age must be taken intoaccount. Adjustments can also be made for aspecific surgeon's technique.
In the search for continuous refinementand accuracy of results, new methods basedon laser interferometry may replace ultra-sonography in the future.
Main Causes of Errors
Zacharias and Centurion have pointedout that most postoperative refraction errorsoccur not due to errors in the formulas but toimprecise preoperative measurements. Foreach millimeter of error in biometry there isa -2.5 diopter error in the calculation of theIOL power. If more than one error occurs inthe same examination there may be signifi-cant postoperative refractive errors.Keratometry in both eyes should be repeatedwhen:
• corneal curvature is less than 40.00 Dor more than 47.00 D;
• the difference of the corneal cylinderis more than 1.00 D between both eyes;
• the corneal cylinder correlates poorlywith the refraction cylinder.
During the examination, the patient sitsin front of the skilled technician performingthe ultrasound test. He/she is asked to fixateat a point straight ahead. The ultrasound softprobe is positioned axially, touching the cor-neal epithelium as lightly as possible so as notto compress and thereby shorten the eye. It isuseful to visualize the procedure laterally tomake sure that the cornea is not being com-pressed (Fig. 24).

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
45
Targeting Post-Op Refraction
This parameter is the only one that thephysician must decide upon by himself andfeed into the computer. All the other param-eters are measured or assumed values overwhich he has no control. When selecting a lensimplant power Gimbel generally recommendsthat the surgeon target mild myopia and thusavoid inadvertent postoperative hyperopia. Apatient who is hyperopic postoperatively willneed spectacles for clear vision at any range,whereas a patient who is slightly myopic willhave a range of clear vision corresponding tothe degree of myopia. In all cases the patientmust be counselled with regard to expectationsof refractive changes and they should be coun-selled that they will generally need readingglasses or bifocals postoperatively as the im-plant has no power of accommodation, unlessthe patient's targeted postop refraction is around-2.00 on purpose.
Monocular Correction
Holladay has pointed out that with mo-nocular correction, there are two major consid-erations for determining what would be thebest postoperative refraction for any patient. Ifwe are only considering one eye (i.e., the othereye is amblyopic), targeting the postoperativerefraction for approximately -1.00 to -1.50diopters is probably the best choice.
This is usually best because most peoplehave visual needs for both distance and near;that is, they want to be able to drive and to readwithout having to wear glasses. If we target thepatient's post-op refraction for -1.00 to -1.50,the patient will have 20/20 vision at approxi-mately 2 to 3 feet, 20/30 vision in the distance,and 20/30 at 14 inches. With a normal sizepupil of approximately 3 mm in the cataract age
group, these visual acuities are adequate withno additional glasses required. At times whenthey might need finer acuity, they can wearregular bifocals, which will correct them fordistance and near.
In older, more sedentary patients, twodiopters of myopia may be a better goal. Forthese patients reading without glasses may bepreferred to distance vision without glasses.
The second reason for targeting the post-op refraction to approximately -1.00 to -1.50,sometimes -2.00 diopters, is that, statistically,between 70% and 90% of patients will fallwithin + or -1.00 diopter error of this desiredpostoperative refraction. The errors, as men-tioned previously, are primarily a result of ourinability to make exact measurements on theliving eye.
Therefore, the patient will fall betweenplano and -2.00 diopters 90% of the time. Thiswill assure most patients of useful vision with-out glasses. Hence, the error of the ultrasoundmeasurement is best handled by choosing thepostoperative refraction of -1.00. On the otherhand, if we target for plano, which is the targetthat some physicians try to obtain, 90% of thepatients will be between -1.00 and +1.00 diopt-ers. When the patient's refraction is on the +1side, he has less useful vision at any distancebecause he is hyperopic and does not have theability to accommodate.
Consequently, because it is very unde-sirable to have a hyperopic correction, tar-geting for -1.00 not only optimizes the bestvision at all distances but also minimizes thechance for hyperopia that can result from theinaccuracies of ultrasonic measurements.
Holladay's recommendation for choos-ing -1.00 to -1.5 as the postoperative refractionis based on one eye only, i.e. monocular condi-tions. When the vision in the other eye is good,its refraction must be considered for binocularvision.

THE ART AND THE SCIENCE OF CATARACT SURGERY
46
Binocular Correction
In patients with Binocular Correction:one overriding rule when choosing an IOLpower is that one should never aim for spec-tacles which give the patient a difference in thepower between the right and left lens greaterthan three diopters. The reason for this is thateven though the patient may have 20/20 visionin primary gaze, when the patient looks up ordown, the induced vertical prism difference inthe two eyes is so large that it will create doublevision. Therefore, avoid anisometropia.
Good Vision in the Non-Operated Eye
In a patient who has good vision in thenon-operative eye, one must target the in-traocular lens power for a refraction withintwo diopters of his/her present prescription inthe non-operative eye. This measurementshould be two diopters, not three, due to our 1diopter A-scan variability. For example, if wehave a patient who is hyperopic and has +5diopters correction in each eye, we cannottarget the intraocular lens for a postoperativerefraction of -1 diopter because this wouldproduce a 6 diopter difference between the twolenses, resulting in double vision or confusion.
Holladay recommends selecting theintraocular lens power to obtain a refractionwhich is approximately two diopters less thanthe non-operative eye. Consequently, on ourpatient who is +5 diopters in both eyes, weshould target the postoperative refraction in theeye with the cataract for +3, so ther e is a90% probability that there will be less than a3 diopter difference.
In contrast, if the patient were highlymyopic in each eye, for example, -10.00 in botheyes, we should target the intraocular lenspower to produce refraction of approximately
-8.00. We have limited the difference in thespectacle lenses to a two diopter difference inthe final prescription. Again, we are advised totarget for a two diopter difference, not a threediopter difference, because there is approxi-mately a one diopter tolerance in the accuracyof the ultrasonic measurement.
When Cataracts in Both Eyes
If the operation on the second eye is to bedone shortly after the first, the IOL calculationis made as if he were monocular, as in ourprevious discussion.
For example, with a patient +5 in botheyes, if the second eye is cataractous and it isplanned that the patient would also need cata-ract surgery in that second eye within a shortperiod of time, it would be wise to target for-1 in the first eye. When the vision in theoperated eye exceeds the vision in the othereye, -1 lenses in both should be prescribed untilthe second eye is operated. Soon. This is notonly true with intraocular lens surgery; it is truein all forms of refraction. The patient needs tounderstand what we are doing and to be a partof the decision process. One should never givea patient more than a three diopter difference inhis/her spectacles unless he has previouslyworn such a prescription. One exception is achild who is under five or six years of age andwho can adjust to this difference by turning hishead rather than moving his eyes. Another isthe patient with an alternating strabismus.
We must continue in our efforts to avoidcreating astigmatism by our surgery. If thepatient is already astigmatic, try to avoid toomuch astigmatic imbalance (high plus at 90º inone eye and high minus at 90º in the other). Thisresults in a vertical prism effect in reading andthe need for prescribing a slab off prism. Thisproblem has fortunately been significantly di-minished with small incision surgery, particu-

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
47
larly phaco, and with the application of refrac-tive cataract surgery by placing the incision inthe correct axis at the time of cataract surgery.This we will discuss under the major heading of"The Incision."
IOL POWER CALCULATIONIN COMPLEX CASES
Specific Methods to Use inComplex Cases
Considering that there are no specificmethods on which there is full agreement as towhat to do in these patients, and after consult-ing different authorities in this field, we herebyrecommend the use of third generation formu-las, preferably more than one and that thehighest resulting IOL power should be used forthe implant. These formulas are preferably theHolladay 2, the SRK/T or the Hoffer formulas.Do not use a regression formula (e.g., SRK I orSRK II). We also recommend that you usecentral topography's flattest curve as akeratometric method unless you are fortunateto have all the information needed in order touse the "historical method." This reading isfed to the computer utilizing the selected for-mulas. The computer will then provide youwith the power of the IOL to use.
The modern formulas hereby recom-mended are already available in most of thecomputers available today to calculate IOLpower. You just select the formulas you be-lieve adequate which should be present withinyour equipment.
The reason behind all these sophisticatedand very careful IOL calculations in highlymyopic patients with cataract is, of course,that although the cataract removal by itself cansomewhat compensate for the high myopia, the
advantages of modern technology, the smallincision extracapsulars and careful inspectionof the peripheral retina allow us to perform asafe lens removal and provide an IOL implan-tation with a sufficiently desirable power toprovide a specific patient with the very highquality of vision that we must demand of our-selves for the benefit of our patients.
Practical Method for ChoosingFormulas in Complex Cases
From a practical standpoint, if severalformulas are available to the clinician, the firstchoice as recommended by Zacharias andCenturion are as follows:
• short eyes: L <22.00 mm: Holladay 2 orHoffer Q. These constitute 8% of cases.
• L (axial length) between 22.00 and24.50 mm; 72% of the cases: mean of the threeformulas: Hoffer, Holladay and SKR/T.
• L between 24.50 mm and 26.00 mm;15% of the cases: Holladay 2 or SRK/T
• L higher than 26.00 mm; 5% of thecases: SRK/T
High Hyperopia
In eyes with short or very short axiallengths (Fig. 25) the third generation formulassuch as Holladay 2 and Hoffer-Q seem toprovide the best results. Observing high refrac-tive errors in extremely short eyes (<20.0 mm),Holladay has discovered that the size of theanterior and posterior segments is not propor-tional, and has devised certain measurementsto be used to calculate the parameters in theseeyes. Assembling data from 35 internationalresearchers Holladay concluded that only 20%of short eyes present a small anterior segment(nanophthalmic eyes); 80% present a normalanterior segment and it is the posterior segment

THE ART AND THE SCIENCE OF CATARACT SURGERY
48
that is abnormally short. This means that theformulas that predict a small anterior segmentin a short eye provoke an 80% error margin, asthey will predict an abnormally shallow ante-rior chamber which, in turn, can lead to hyper-opic errors of up to 5 diopters. The Holladay 2formula comprises the seven parameters previ-ously described for IOL calculation: axiallength, keratometry, ACD (anterior chamberdepth), lens width, white-to-white corneal hori-zontal diameter, preoperative refraction, andage. This new formula has reduced 5 D errorsto less than 1 D in eyes with high hyperopia.
Although biometry is easy to perform,most errors in hyperopic patients occur be-cause of probe compression. Zacharias andCenturion emphasize that only the cornealepithelium should be touched, without anyresulting indentation (Fig. 25-A).
The Use of Piggyback Lenses inVery High Hyperopia
For very short eyes (<22.00 mm inlength) even though the Holladay 2 or theHoffer Q formulas are a significant advance incalculating the IOL power needed, we do nothave IOLs easily available with a power higherthan +34 diopters because a higher diopter lenswould have a marked, almost spherical curva-ture, that would cause major optical aberra-tions. Such lenses can be customized but stillmay cause undesirable optical aberrations. Inthese cases the piggyback method is employed,i.e., the implantation of more than one IOL ina single eye, dividing the total power amongthe different lenses, placing 2/3 of the power inthe posterior lens and 1/3 in the anterior lens(Fig. 25-B).
Gayton (1994) was the first to place twolenses in a single eye. He observed that placingmultiple lenses in a single eye produces im-
proved optical quality because there are fewerspherical aberrations than with very high di-opter lenses.
Measuring the position of piggybacklenses, Holladay observed that contrary towhat he supposed -- that the anterior lens wouldoccupy a more anterior position -- what effec-tively happens is that the anterior lens pre-serves its normal position while the posteriorlens moves backwards because of the disten-sible nature of the capsular bag. The latter mayaccommodate more than two IOLs and thereare cases of patients with four piggyback lensesin the same eye.
Holladay's recommendation for calcu-lating the power of lenses with the piggybackprocedure in high hyperopic patients is to add3 diopters to the total value of the pre-op IOLpower calculation and divide the total by 3,placing 2/3 of the power in the posterior lensand 1/3 in the anterior lens. This facilitatesthe replacement of the anterior lens, if neces-sary, as it is the thinnest lens. The 3 dioptersadded to the total value are meant to roughlycompensate the hyperopic error resulting fromthe space behind the posterior lens. This iscalculated more precisely with the Holladay 2formula.
Joaquin Barraquer, M.D., in Barcelona,who often attends very complex anterior seg-ment diseases referred to him from differentparts of the world, has observed a substantialincrease in depth of focus with the piggybackprocedure as compared to the implantation of asingle custom made lens. He has done bothprocedures. Barraquer as well as I. H. Fine,M.D., another master surgeon, are still cau-tious about the piggyback method. Theyfeel that it is not yet clear how Elschnig pearlsbetween the lenses will behave in the postop-erative period if there is progressive capsularfibrosis. Recently, John Gayton, David

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
49
Apple et al described the presence ofinterlenticular opacification in two pairs ofpiggyback lenses that had to be explanted from2 patients with significant visual loss related toopacification between the optics. They weresubmitted for pathological analysis. Gross andhistopathological examinations were per-formed, and photomicroscopy was used to docu-ment the results.
Gross examination showed accumula-tion of a membrane-like white material be-tween the lenses. Histopathological examina-tion revealed that the tissue consisted of re-tained/proliferative lens epithelial cells (blad-der cells or pearls) mixed with lens corticalmaterial.
They recommended three surgical meansthat may help prevent this complication: me-ticulous cortical cleanup, especially in the equa-torial region; creation of a relatively large con-tinuous curvilinear capsulorhexis to sequesterretained cells peripheral to the IOL optic withinthe equatorial fornix; insertion of the posteriorIOL in the capsular bag and the anterior IOL, inthe ciliary sulcus to isolate retained cells fromthe interlenticular space.
Echobiometry in highly hyperopic eyes,especially microphthalmic and nanophthalmiceyes, is still far from desirable.
High Myopia
According to Zacharias and Centurion'sexperience, results of cataract surgery in highlymyopic eyes with axial lengths higher than31.0 mm with implantation of low or negativepower IOLs may be successful, without anymore operative or postoperative complicationsthan normal eyes. The use of the SRK IIformula with an individual surgeon's factorshowed good predictability of the refractivetarget (Fig. 26). However, better formulas
without the use of a personalized correctionfactor have yet to be developed. Zacharias andCenturion emphasize that there are technicaldifficulties in performing the echobiometry ofpatients with high myopia, especially whenthey have a posterior staphyloma. In thosecases they obtain extremely irregular retinalechoes that cannot provide certainty in termsof really correct results of the IOL calculation.In addition, a posterior staphyloma may notalways coincide with the macula, so the highermeasurement is not necessarily the correct one,as is the case with normal eyes.
In these patients it is useful to perform Btype ultrasound to identify the existence of astaphyloma and its relation with the macula.Equally important is to have an ultrasoundprobe with a fixation light. The patient is askedto fixate at the light -- which he will do with themacula -- facilitating the measurement.
Lacava and Centurion studied 27 myo-pic eyes with an axial length of more than26.50 mm, and found that 88% of the patientswith whom they used the SRK/T formula werewithin the emmetropic criteria established byGeorge Waring.
DETERMINING IOL POWERIN PATIENTS WITH PREVI-OUS REFRACTIVE SURGERY
Patients who have undergone excimerlaser procedures, radial keratotomy or INTACShave had modifications to their corneal curva-tures (Figs. 27, 28, 29). Accurate keratometricreadings are fundamental in calculating IOLpower. IOL power calculation for cataractsurgery in patients previously submitted torefractive surgery by modification of thecorneal curvature is a new challenge for thecataract surgeon basically because of two

THE ART AND THE SCIENCE OF CATARACT SURGERY
50
Figure 27: IOL Power Calculation inPatients After Excimer Laser Procedure
In this group of patients even withthe most advanced ultrasonic equipment,there is a degree of variation in the resultsof the IOL power calculation. This is theresult of the varying modification in thecurvature of the cornea after the excimerlaser ablation (A). There is no universallyaccepted formula to calculate these pa-tients' IOL power accurately. The standardmethods used in normal eyes are inad-equate in these patients. For alternativemethods, consult text.
Figure 28: IOL Power Calculation inPatients After Radial Keratotomy
Patients operated with radialkeratotomy undergo corneal curvaturechanges that cannot be measured reli-ably with the standard methods. Thedata of the corneal curvature obtainedfrom corneal topography are fed into acomputer using third generation formu-las to establish a more dependable calcu-lation of the intraocular lens power. Thisillustration shows the correct way ofusing the ultrasound transducer (P) onthe cornea placing it on the opticalcenter midway between the cornealincisions (RK). For alternative methodsof calculation see text.

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
51
features. 1) Patients who previously decided toundergo refractive surgery are morephychologically resistant to using spectacles tocorrect residual ametropia. Consequently, theirexpectations for cataract surgery are unusuallyhigh. 2) So far there is no universally ac-cepted formula to calculate these patients'IOL power accurately. Routine keratometryreadings do not accurately reflect the true cor-neal curvature in these cases and may result in
errors if used for IOL calculations. Therefore,standard keratometry readings should not beused for IOL calculations in these patients. Ifdone, the standard IOL power-predictive for-mulas based on such readings commonly resultin substantial undercorrection with postopera-tive hyperopic refraction or anisometropia bothof which are very undesirable.
Jack Holladay, M.D., a recognizedauthority on IOL power calculations and in all
Figure 29: IOL Power Calculation After an Intracorneal Ring Segment Procedure
As with other refractive procedures on the cornea, this technique for correction of low myopia also modifies thecentral corneal curvature (arrows). Due to the limited correction power the INTACS can handle (miopias up to -2.5 D),it is presumed that the variability in the reduction of the central corneal curvature should not be very significant.Topography determines the present corneal curvatures. The surgeon uses the flattest keratometric reading as areference in cases where the pre-refractive procedure keratometry cannot be obtained. This data is fed into thecomputer and with the use of the programs outlined in the text the power of the intraocular lens is determined. In thisillustration we can see the ultrasound transducer (P) on the central cornea inside the area in which the intracornealrings (IC) are placed.

THE ART AND THE SCIENCE OF CATARACT SURGERY
52
optical-refractive subjects in ophthalmology,considers that accurate determination of thecorneal power in these patients is difficult andis usually the determining factor in the accu-racy of the predicted refraction following cata-ract surgery. Providing this group of patientswith the same accuracy of intraocular lenspower calculations as we have provided ourstandard cataract patients presents an espe-cially difficult challenge.
Methods Most Often Used
There are three methods to determine theeffective power of the cornea in these complexcases: 1) the clinical history method, alsotermed by Holladay "the calculation method";2) the contact lens method; and 3) the topog-
raphy method. Holladay believes that thecalculation or "clinical history" method and thehard contact lens trial are the two more reliableof the three, because the corneal topographyinstruments presently available do not provideaccurate central corneal power following PRK,LASIK and RKs with optical zones of 3 mm orless. In RKs with larger optical zones, thetopography instruments become more reliable.The great majority of cases, however, have hadRK with an optimal zone larger than 3 mm, sothey should also qualify for this method.
The Clinical History Method
The "clinical history" method is the mostoften used. In the "historical or calculationmethod", however, the keratometry reading
Figure 30: Posterior Capsulorhexis in Pediatric Patients
Following the conventional steps of phacoemulsification, an appropriate intraocular lens for childrenis inserted (IOL) with the required power in compliance with the criteria of the practitioner following theguidelines in the text. Once the intraocular lens is located in the bag, and properly protecting the tissues withviscoelastics, a cystotome (C) is introduced through the limbal incision (I), and directed behind the IOL toperform a posterior capsule tear or posterior capsulorhexis (PC). This opening in the posterior capsule at thetime of the phaco procedure can provide permanent improved vision to the child.

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
53
and refraction before refractive surgery mustbe known along with an accurate postoperativerefraction which is not often the case. It is alsoimportant to keep in mind that at present, farmore patients have had RK than PRK andLASIK combined. Also, our long-term fol-low-up of RK patients is much greater. Thelong-term studies of RK patients reveal thatsome have hyperopic shifts in their refractionand develop progressive against-the-rule astig-matism which may complicate the final visionof the patient operated for cataract, unlessdetected at the time of preoperative evaluationand corrected. The long-term refractive changesin PRK and LASIK are unknown, except forthe regression effect following attempted PRKcorrections exceeding 8 D. Whichever proce-dure the patient has had, the stability or insta-bility of the refraction must be determined.When using the "clinical history or calculationmethod" a subtraction of the spherical equiva-lent (SEQ) change after refractive surgery fromthe original K-reading is done to determine thenew "accurate" corneal curve. This, however,is not information easily found. It is useful andcan be applied whenever refraction and the K-reading before the keratorefractive procedureare available to cataract surgeons. If thisinformation is not available, which is notunusual, we recommend that thekeratometry be measured with corneal to-pography and use the flattest curve of thisreading as the new corneal curve to feed thecomputer that will then automatically provideus with the IOL power to use.
Another downfall of the history methodis that cataracts frequently cause induced myo-pia. This method, however, requires an accu-rate and stabilized refraction after thekeratorefractive procedure and at the time weare contemplating cataract surgery. In many
cases, calculation is complicated by the pro-gressive flattening that occurs in about 25% ofRK patients. It is nearly impossible to separatethese two factors and determine the impact ofeach on the refraction before cataract surgery.
The Trial Hard Contact LensMethod
The second method often used, which isthe trial hard contact lens method, requires aplano hard contact lens with a known basecurve and is limited to patients whose cataractdoes not prevent them from being refracted toapproximately +0.50 D. This usually requiresa visual acuity of better than 20/80. The patient'sspheroequivalent refraction is determined bystandard refraction. The refraction is thenrepeated with the hard contact lens in place. Ifthe spheroequivalent refraction does not changewith the contact lens, then the patient`s corneamust have the same power as the base curve ofthe plano contact lens, since the base curve andfront curve are the same in a plano contact lens.If the patient has a myopic shift in the refractionwith the contact lens, then the base curve of thecontact lens is stronger than the cornea by theamount of the shift. If there is a hyperopic shiftin the refraction with the contact lens, then thebase curve of the contact lens is weaker than thecornea by the amount of the shift.
Example as Provided by Holladay
The patient has a current spheroequivalentrefraction of +0.25 D. When a plano hardcontact lens with a base curve of 35.00 D isplaced on the cornea, the spherical refractionchanges to -2.00 D. Since the patient had amyopic shift with the contact lens, the corneamust be weaker than the base curve of the

THE ART AND THE SCIENCE OF CATARACT SURGERY
54
contact by 2.25 D. Therefore, the cornea mustbe 32.75 D (35.00 - 2.25), which is slightlydifferent from the value obtained by the histori-cal or calculation method. This method islimited by the accuracy of the refractions, whichmay be limited by the cataract.
The Corneal TopographyMethod
Current corneal topography instrumentsprovide greater accuracy, compared tokeratometers, in determining the power of cor-neas with irregular astigmatism. The computerin topography instruments provides a veryaccurate determination of the anterior surfaceof the cornea. The limitation of this method isthat the computer in corneal topography pro-vides no information about the posterior sur-face of the cornea. In order to accuratelydetermine the total power of the cornea, thepower of both surfaces must be known.
The Importance of DetectingIrregular Astigmatism
Holladay has strongly recommended thatbiomicroscopy, retinoscopy, corneal topog-raphy and endothelial cell counts be per-formed in all of these complex cases. The firstthree tests are primarily directed at evaluatingthe amount of irregular astigmatism. Thisdetermination is extremely important preop-eratively because the irregular astigmatismmay be contributing to the reduced vision aswell as the cataract. The irregular astigma-tism may also be the limiting factor in thepatient's vision following cataract surgery. Theendothelial cell count is necessary to recog-
nize any patients with low cell counts from theprevious surgery who may be at higher risk forcorneal decompensation or prolonged visualrecovery.
The potential acuity meter (PAM), superpinhole and hard contact lens trial are oftenhelpful as secondary tests in determining therespective contribution to reduced vision bythe cataract and the corneal irregular astigma-tism. The patient should be informed that onlythe glare from the cataract will be eliminated.Any glare from the keratorefractive procedurewill essentially remain unchanged.
IOL Power Calculation inPediatric Cataracts
How to optically correct patients withbilateral congenital cataracts and monocularcongenital cataract has been a major subject ofcontroversy for many years. Some distin-guished ophthalmic surgeons 20 years ago werestrongly against performing surgery in mo-nocular congenital cataract followed by treat-ment of amblyopia with a contact lens. Visualresults were so bad that children with thisproblem must be amblyopic by nature, theythought, and the psychological damage to thechildren and the parents by forcing such treat-ment was to be condemned.
Surgery of bilateral congenital cataractsat a very early age followed by correction withspectacles and sometimes with contact lensesusually ended with no better than 20/60 visionbilaterally. This was again a source for beliefthat congenital cataracts either unilateral orbilateral were by nature associated with am-blyopia, profound in cases of monocular casesand fairly strong in bilateral cataracts.

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
55
When posterior chamber IOL implanta-tion in adults became established as the proce-dure of choice, strong influences within oph-thalmology were adamantly opposed to theiruse in children for the following reasons: 1) theeye grows in length with consequent signifi-cant change in refraction. It was consideredimpossible to predict such change and conse-quently, the accurate IOL power adequate foreach child. 2) There was opacification ofposterior capsule in most cases. This requireda second operation for posterior capsulotomyand the presence of an IOL would impedeproper surgical maneuvers.
You will not find this concise history inany other book. I lived through it and thereforeshare it with you.
The situation has now significantlychanged. The previous failures with spec-tacles and contact lenses, the new develop-ments in technology and surgical techniquesand the fresh insight of surgeons of a newgeneration has led us to discard the previousthinking and very definitely implant posteriorchamber IOL's in children. This has been madepossible from the surgical point of view by thefollowing developments: new medications thateffectively prevent and/or control inflamma-tion; the introduction of posterior capsulecapsulorhexis introduced by Gimbel inNorth America promptly followed byEverardo Barojas in Mexico and LatinAmerica (Fig. 30); high viscosity viscoelasticsto facilitate intraocular surgery in smaller eyes;new, more appropriate IOL's for children andimplantation in their capsular bag; more re-fined technology that leads to a less difficultcalculation of the IOL power.
Different Alternatives
The limitations in calculating these lensespowers (Fig. 31) is due to the fact that the eyegrows after cataract surgery and therefore re-fraction will change. Two main methods ofchoosing an IOL power for pediatric patientsare available: 1) Make the eye emmetropic atthe time of surgery and thereby treat amblyopiaimmediately taking advantage of a much bettervisual acuity. This is followed later by an IOLexchange because of increasing myopia(growth of the eye).
Even though there are more practical andefficient techniques for IOL exchange, as de-vised by Jack Dodick, M.D., this alternative issecond choice.
2) Proceed with incomplete overcorrec-tion of the eye at the time of surgery (treatedwith glasses or contact lenses) taking advan-tage of the trend toward emmetropizationwhich will occur as the eye grows. By "in-complete" we mean leaving the eyes hyper-opic. As the eye grows in length with age (axialgrowth), the myopization that takes place in aneye artificially rendered hyperopic will lead toemmetropia or close to normal refraction. Thismeasure avoids myopic anisometropia that maylead to an undesirable change of IOL surgi-cally. In the meantime, the temporary hypero-pia is managed with standard spectacles orcontact lenses.
Alternatives of Choice
In the IOL power calculation in childrenyounger than 1 year, keratometry is difficultand fortunately less important because the

THE ART AND THE SCIENCE OF CATARACT SURGERY
56
values change very rapidly during the first sixmonths. Thus keratometry may be replaced bythe mean adult average keratometry value of44.00 D. Children less than two years old maybe incompletely corrected +3.00 D to even+4.00 D; between three and four years oldincompletely correct them +3.00 D in thosecloser to three and +2.50 D in those closer tofour. In children closer to six or seven, whohave little chance of recovering from any am-blyopia present but who are the ones that more
frequently suffer from a unilateral traumaticcataract, overcorrect them by +1.00 D.
3) A new method of management inpediatric cataracts is to render the eyesemmetropic from the very start and when axiallength grows and makes the eye myopic,proceed to implant a second IOL with negativeor minus power utilizing the piggyback tech-nique and placing the new IOL in front of theprimary IOL (Fig. 25- B).
Figure 31: IOL Power Calculation in PediatricCataract
The growth of the ocular globe isecographically registered until 18 years of age. How-ever, the lens continues growing throughout the life ofthe individual. In normal conditions, anterior cham-ber (A) depth is reduced as the lens increases in size.In pathological conditions such as the presence of cata-racts the opposite may happen: the anterior chamberdepth may increase due to reduction in the volume ofthe lens (C). In this illustration we can see the changesin the size of the globe through the shaded images thatoutline the growth of the eye by stages. At birth theaxial diameter in the normal patient may measure ap-proximately 17.5 mm, at three years of age it maymeasure 21.8 mm (X), at ten years 22.5 mm identi-fied in (Y) and in normal adulthood nearly 24 mm(Z). In selecting the lens power to be used, some sur-geons choose to make the child hyperopic (arrows) withthe intention that his growth will compensate hypero-pia with the passage of time and will be eventuallycloser to achieving an emmetropic eye. Others preferto calculate an intraocular lens closer to emmetropiawith the intention of keeping the child emmetropicduring his growing years and prescribing eyeglassesin the future.

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
57
IOL Power CalculationFollowing Vitrectomy
For the most part, IOL power calcula-tion in eyes that develop a cataract followingvitrectomy is straightforward. The intravitrealgas is reabsorbed and slowly replaced byaqueous. If silicone oil was used instead ofperfluorocarbons, when the oil is removed,aqueous fills the vitreous cavity. Since therefractive indices of aqueous and vitreous areidentical (1.336), no corrections are needed inthe calculation of the IOL power.
But what if silicone oil is present inthe vitreous cavity? Lihteh Wu, M.D., haspointed out that anywhere from 60% to 100%of eyes have been reported to develop cata-ract following silicone oil tamponade. Up to25% of eyes with silicone oil tamponade,especially those with retinal detachment sec-ondary to necrotizing retinitis, will requirepermanent tamponade. Several authorshave reported unpredictable refractions fol-lowing cataract extraction in silicone-filledeyes when traditional formulas are used. Inone study the axial length was measured priorto silicone oil tamponade, and the IOL powerwas calculated using the traditional formulas.In these eyes the average postoperative re-fraction was about +4.00 diopters (with arange of +2 to +6 D). These results weremore hyperopic than had been predicted andthe change is associated with the differentrefractive index of silicone oil. If the siliconeoil was later removed then the postoperativerefraction was only off by 0.5 to 1 D.
Drs. Melissa Meldrum, TomAaberg, Anil Patel, and Janet Davis havedescribed and proposed correction factors for
the calculation of an intraocular lens implantin a silicone filled eye (Fig. 32). They recom-mend: (1) the use of a modified ultrasoundvelocity in silicone oil in the calculation ofaxial length, (2) the use of convexoplanoIOL's, and (3) the addition of a constant tocompensate for the refractive index of sili-cone oil.
The velocity of sound in a medium isinversely related to the medium’s refractiveindex. Since silicone oil has a higher index ofrefraction than vitreous, it slows down soundvelocity. For instance, sound velocity in sili-cone oil is 986 m/s compared to 1532 m/s inaqueous. If we recall, the velocity of sound ispreset in the computer in the ultrasoundmachine. If no modification is made, the eyeappears to be longer than it actually is. Conse-quently, the wrong IOL may be implanted.
Drs. Meldrum, Aaberg, Patel, andDavis also explain why the choice of IOL isimportant. When convexoplano lenses areused, the anterior surface of the lens is solelyresponsible for the refractive power of thelens. Thus the presence of silicone oil in thevitreous cavity has no effect on the refractivepower of the IOL. On the other hand, whenbiconvex lenses are used, the posterior sur-face also contributes to the refractive powerof the lens. The refractive power of the poste-rior surface depends on the difference be-tween the refractive indices of the IOL andthe vitreous or vitreous substitute. Since sili-cone oil has a higher index of refraction thanvitreous, the posterior refractive power of thelens is reduced. The use of a biconvex lensrequires further correction.
Meldrum, Aaberg, Patel, and Davismake the following recommendations.

THE ART AND THE SCIENCE OF CATARACT SURGERY
58
• Measure the axial length using the velocity ofsound in silicone oil.
• Calculate the IOL power to achieve emmetro-pia using the traditional formulas. To this IOLpower, a correction factor must be added toobtain the IOL power to achieve emmetropiain silicone oil. The correction factors rangefrom 2.79 D to 3.94 D, for axial lengths from20 mm to 30 mm.
• Choose a convexoplano IOL if possible. Ifanother type of le1ns is used, another correc-tion factor must be added to obtain the totalpower of the IOL in the presence of silicone
Figure 32: IOL Power Calculation in Pa-tients After Vitrectomy Procedure WithSilicone
If the patient is in the process ofundergoing this procedure it is recom-mended to calculate the intraocular lensbefore using silicone in the vitreous cavity(V) and extracting the lens (C).Polymethylmethacrylate lenses (PMMA)are recommended. Silicone foldable IOL'sare not recommended because the siliconeoil in the vitreous cavity sticks to theintraocular lens and sometimes causesopacities. In the calculation of these lenspowers there may be differences in excessof 5-7 diopters. Errors can be frequentbecause if the vitreous cavity (V) is notfilled completely with silicone (S), themovement of the bubble can induce errorsin the calculation of the lens. In addition, inthe eye filled with silicone, the ultrasoundwaves travel slower (arrows). This affectsthe axial diameter measurement during IOLpower calculation. For alternative methodsof IOL power calculation, see text.
oil. For a convexoplano lens no additionalcorrection factor is required.
For instance, let us suppose that a patientrequires indefinite intraocular tamponade with sili-cone oil and develops a cataract. Using the tradi-tional formulas, assuming that the IOL power iscalculated to be 22 D based on a measured axiallength of 23 mm. To this 22D we must add acorrection factor of 3.64D (Meldrum et al) to cor-rect for the axial length. Thus, for this patient a 25.5D convexoplano lens should be implanted in orderto achieve emmetropia in the presence of siliconeoil. No additional correction factor for the IOLdesign is necessary.

C h a p t e r 3: IOL Power Calculation in Standard and Complex Cases - Preparing for Surgery
59
RECOMMENDED READING
Mendicute J, Cadarso L, Lorente R., Orbegozo J,Soler JR: Facoemulsificación, 1999.
BIBLIOGRAPHY
Boyd, BF.: Undergoing cataract surgery with a mastersurgeon: a personal experience. Highlights of Ophthalm.Bi-monthly Journal, Volume 27, Nº 1,1999;3.
Brady, KM., Atkinson, CS., Kilty, LA., Hiles, DA:Cataract surgery and intraocular lens implantation inchildren. Am J. Ophthalmol, 1995;120:1-9.
Buckley, EG., Klombers, LA., Seaber, JH., et al: Man-agement of the posterior capsule during intraocular lensimplantation. Am J Ophthalmol, 1993;115:722-8.
Dahan, E., Drusedan, MUH.: Choice of lens and dioptricpower in pediatric pseudophakia. J Cataract RefractSurg, 1997;23:618-23.
Gayton, JL.: Implanting two posterior chamber intraocu-lar lenses in microphthalmos. Ocular Surgery News,1994:64-5.
Gayton JL., Apple DJ., Peng Q., Visessook N., SandersV., Werner L., Pandey SK., Escobar-Gomez, M.,Hoddinott D., Van Der Karr M.: Interlenticular opacifi-cation: Clinicopathological correlation of a complica-tion of posterior chamber piggyback intraocular lenses.J Cataract Refract Surg, 2000; 26:300-336 ©ASCRSand ESCRS.
Gimbel, HV: Posterior continuous curvilinearcapsulorhexis and optic capture of the intraocular lens toprevent secondary opacification in pediatric cataractsurgery. J Cataract Refract Surg, 1997;23:652-656.
Gimbel, HV., Basti, S., Ferensowicz, MA., DeBroff,BM.: Results of bilateral cataract extraction with poste-rior chamber intraocular lens implantation in children.Ophthalmology, 1997; 104:1737-1743.
Grinbaum A., Treister G., Moisseiev J.: Predicted andactual refraction after intraocular lens implantation ineyes with silicone oil. J Cataract Refract Surg, 1996;22:726-729.
Grusha YO., Masket, S., Miller, KM: Phacoemulsifica-tion and lens implantation after pars plana vitrectomy.Ophthalmology 1998;105:287-294.
Holladay, JT: Intraocular lens power in difficult cases.Atlas of Cataract Surgery, Edited by Masket & Crandal,Published by Martin Dunitz, 1999, 19:147-158.
Holladay JT., Gills, JP., Leidlein, J., Cherchio, M.:Achieving emmetropia in extremely short eyes with twopiggyback posterior chamber intraocular lenses. Oph-thalmology, 1996; 103:1118-1123.
Hoffer, KJ: Intraocular lens power calculation for eyesafter refractive keratotomy. J Refract Surg,1995;11:490-3.
Hoffer, KJ.: The Hoffer Q formula: A comparison oftheoretic and regression formulas. J Cataract Surg.,1993; 19:700-711.
Hoffer, KJ: Ultrasound velocities for axial length mea-surement. J Cat Refract Surg, 1994;20:554-562.
Kora, Y., Shimizu, K., Inatomi, M., et al: Eye growthafter cataract extraction and intraocular lens implanta-tion in children. Ophthalmic Surg, 1993;24:467-75.
Lacava AC., Centurion, V.: Cataract surgery after re-fractive surgery, Faco Total, Editora Cultura Medica,2000;269-276.
Lyle WA, Jin GJC.: Intraocular lens power prediction inpatients who undergo cataract surgery followingprevious radial keratotomy. Arch Ophthalmol 1997;115:457-61.
McCartney, DL., Miller, KM., Stark, WJ., et al: In-traocular lens style and refraction in eyes treated withsilicone oil. Arch Ophthalmol 1987; 105:1385-1387.

THE ART AND THE SCIENCE OF CATARACT SURGERY
60
Meldrum, LM., Aaberg, TM., Patel A, Davis, JL.:Cataractextraction after silicone oil repair of retinal detachmentsdue to necrotizing retinitis. Arch Ophthalmol1996;114:885-892.
Olsen T., Thim K., Corydon L.,:Theoretical versus SRKI and SRK II calculation of intraocular lens power. J.Cataract Refract Surg, 1990;16:217-225.
Sanders DR, Retzlaff J, Kraff MC, Gimbel, H., Raanan,M.: Comparison of the SRK/T formula and othertheoretinal and regression formulas. J Cataract RefractSurg., 1990; 16(3):341-346.
Wu, L: IOL power calculation after vitrectomy. GuestExpert, Boyd’s, BF, The Art and the Science of CataractSurgery, HIGHLIGHTS OF OPHTHALMOLOGY,2001.
Zacharias W., Centurion, V.: Biometry and the IOLcalculation for the cataract surgeon: Its importance.Faco Total, 2000; 66-88.

C h a p t e r 4: P revent ing In f ec t i on and Inflammation
63
PREVENTING INFECTIONAND INFLAMMATION
dure of choice for a large number of surgeonswell trained in phaco, the key factors to con-sider are that most infections come from thepatient's own flora. Consequently, we musteffectively kill bacteria in the skin, lids andocular surface before making an incision in theeye itself. For this purpose, you may place 5%Betadine solution inside the fornix and leave itthere for 2 minutes before washing it out of theeye. This is followed by painting the lids with10% povidone-iodine solution.
Peter McDonnell, MD., has pointed outthat endophthalmitis is difficult to study scien-tifically, because it occurs so rarely. AlSommer, M.D., the Dean of the School ofPublic Health at Johns Hopkins University,has emphasized that to do a prospective, ran-domized trial in order to prove that a specificmanagement lowers the risk of endophthalmi-tis, is close to impossible. There are almost noscientific data proving that various strategiesclearly reduce the risk of this complication.Such data are even harder to obtain now be-cause, as incision sizes have gotten smaller, therisk of endophthalmitis has dropped. But asincision sizes have dropped, so has the timethat it takes for surgery. This, of course,reduces the risk.
Henry Perry, M.D., has also broughtout another important point: In patients wherethe posterior capsule breaks or there is need fora vitrectomy, those patients should be treatedwith extra antibiotics because the risk for infec-tion significantly increases depending onwhether it is just the capsule that has rupturedor whether you actually had to do a vitrectomy.
Use of Antiseptics, Antibioticsand Antiinflammatory Agents
Endophthalmitis following cataract sur-gery is a rare complication. When it occurs,however, it becomes the most serious postop-erative complication. We will discuss its pre-vention in this chapter and its management inthe chapter on Complications from CataractSurgery.
The use of preoperative, intraoperativeand postoperative antibiotics and antiinflam-matory agents and the very careful cleaning ofthe lids are generally accepted as the standardof care in patients undergoing cataract surgery.
Effective Preoperative AntibioticTreatments
There is no agreement as to which is themost effective type of antibiotic as well as thedosage and route of administration to preventpostoperative infectious endophthalmitis. Wedo know, however, that aminoglycosides aretoxic to the healing cornea whilefluoroquinolones are not. The former havealso gaps in the antibacterial spectrum of activ-ity and the latter (i.e. ciprofloxacin andofloxacin) are more potent for a wide spectrumof bacteria with less toxicity.
With regard to prophylaxis in an era ofincreasing use of small incision cataract sur-gery where corneal incision without conjuncti-val protection over it is becoming the proce-

THE ART AND THE SCIENCE OF CATARACT SURGERY
64
Regimens Recommended
Considering that there are so many alter-native regimens for minimizing the develop-ment of infection, depending on the personalchoices of different successful surgeons, I amhereby presenting what I consider two alterna-tives that appear to be effective and safe.
Gills Formulas to Prevent Infec-tion
1) For High Volume CataractSurgery
As proposed by James Gills, M.D., afteryears of profound clinical analysis of this sub-ject on many thousands of his own patients.Gills' regime is complex particularly when itcomes to the preparation of two antibiotic mix-tures with two antiinflammatory agents(NSAIDS) for injection into the anterior cham-ber at the end of the operation. The accuratepreparation, mixture and exact dilution of avariety of medications that needs to be donewith absolute accuracy and in very small dosesfor injection routinely into the anterior cham-ber is a big step forward in minimizing endoph-thalmitis, based on Gills' extensive experi-ence. The disadvantage is, however, that suchmultiple steps of preparing these mixtures byoperating paramedical personnel in some largeinstitutions where not only ophthalmic surgeryis performed may be somewhat risky. A smallhuman error is feasible, particularly on the sideof mistakenly applied larger doses, which maylead to toxicity of the ocular tissues. In largeprivate eye centers, where the paramedicalpersonnel is exclusively dedicated to high tech-
nology ocular surgery, Gills outline is an excel-lent measure to follow. The following is hisstep by step procedure.
1) Gills considers that filtering all theirrigating solutions through a 0.2 micronmillipore filter is a major step forward inminimizing infection, particularly endoph-thalmitis. Following his use of filtration, theincidence of endophthalmitis at Gills Institutehas significantly reduced from 1-2 per 1000,which was the same as the national average inthe U.S. to an overall incidence of 1 in 8000 to10,000.
2) After years of successfully usingantibiotics (gentamicin and vancomycin) in theirrigating solution, Gills has changed to whathe considers maximum security, which is asfollows:
A) Preoperatively, 15 minutes prior totransfer to the operating room:
a) Neosynephrine 10% one drop.b) Ocuflox 0.3% mixed with Indocin,
one drop.This combination of Ocuflox (a
fluoroquinolone) and Indocin (a non-steroidal)is prepared as follows: Reconstitute 1 mg ofIndocin with Ocuflox. Reinject into Ocufloxbottle and use one drop of this mixture.
B) In the Operating Rooma) Tetracaine: 0.5% 1 gtt x 3 (3 min.
apart with final drop instilled just prior tobeginning).
b) Betadine BSS: 1 gtt x 3 (2 gtts at thebeginning of the case, 1 gtt at the end).
Preparation: Draw up into the syringe5 cc of BSS followed by 5 cc of Betadinesolution 10%.
Change needle to 18 gauge filter needlewil filter and inject into sterile empty vial. Usethe drops on the eye as outlined above butobtained from this prepared mixture.

C h a p t e r 4: P revent ing In f ec t i on and Inflammation
65
c) Cyloxan (antibiotic): Instill one dropat the end of the operation.
d) Intraocular anesthesia (Intracam-eral): Irrigated inside the anterior chamber(see Chapter 6).
Gills no longer uses antibiotics in theirrigating solution. Instead, he feels there is amore effective control by using a combinationof antibiotics and antiinflammatory drugs di-rectly injected into the anterior chamber at theend of the operation. This combination ofdrugs is obtained as follows:
f) Post-op Anterior Chamber Injec-tion of Indomethacin, Solucortef and TwoAntibiotics
• Draw up 14.4 ml BSS into a syringe andinject 12.4 ml of this BSS into an empty sterilebottle.
• Use the remaining 2 ml to reconstitutetwo 1 mg vials of Indomethacin.
• Add both of the 1 ml vials of In-domethacin solution to the 12.4 ml bottle con-taining BSS making 14.4 ml of total volume.
• Add 8 gtts of Solucortef 125 mg/ml(8 minims using TB syringe), 0.06Cephtazidime 50 mg/ml.
• 0.1 ml Vancomycin 500 mg/10 ml tothe 14.4 ml bottle of Indomethacin solution.
• Dosage per patient: 0.50 ml of thismixture is injected into the anterior chamber atthe end of the operation.
g) Recovery Room: Polytracin oint-ment x 1.
In doses higher than those described inthis outline, Vancomycin and Cephtazidimewould interact and precipitate out of solution.Gills states that he has no problems with theminute concentrations used for intraocular in-jection. At the end of the operation, topicalBetadine® drops are instilled in the eye.Betadine eliminates flora in the cul-de-sac so
they cannot enter the soft eyes that may occurwithin the first hour after surgery. During thiscritical period it is important to make sure thatthe eye is clear and clean.
C) Oral Medications: These are in-stilled before the antibiotic ointment.
Ibuprofen 200 mg ÷ tablet given pre-opand ÷ tablet postop unless contraindicated.
2) Non-Complex, Effective andSafe Alternative for Prevention of In-fection
The regimen that follows is practical andeffective, one which every ophthalmic surgeonmay use with excellent results.
1) AsepsisFollow the same routine previously
outlined for thorough cleaning of lids and skinwith soap and 10% povidone iodine solutions.The same applies for use of 5% Betadine 1 droptopically, Betadine 5% solution inside thefornix leaving it there for 2 minutes beforewashing it out of the eye.
2) Preop antibiotics: none.3) Filtration of irrigating solution
If the micropore filter is available,by all means use it as recommended by Gills.
4) Intracameral irrigation at end ofoperation
Yes. Irrigate the anterior chamber withan effective mixture of:
A) One antibiotic and one steroidal anti-inflammatory mixture containing:
a) Gentamicin 0.5 ml drawn froma vial containing 40 mg / ml.
b) Prednisolone acetate (Depomedrol)0.5 ml solution from a vial containing 40 mg /ml.

THE ART AND THE SCIENCE OF CATARACT SURGERY
66
This combination is easy to use, it pro-vides very little risk of confusion and is mosteffective.
5) Topical instillation after intracam-eral irrigation
In cataract surgery there are many waysto reduce the ocular surface flora which is themain source of contamination that may lead toendophthalmitis. It is also quite clear theusefulness of Povidone-Iodine as an antisepticin the skin and lids and Betadine gtts topicallypreoparatively as outlined previously. The useof preoperative antibiotics has never been asubject of consensus essentially because thereis no fundamental evidence that they reallycontribute to minimize the risk of infection.
Antibiotics Most Commonly Used
As to the use of postoperative antibioticswhich is the subject we discuss here, the sub-conjunctival injection of antibiotics is notrecommended by the majority of experts.The general consensus, however, is that imme-diately following cataract surgery, the postop-erative use of antibiotics and antiinflammatoryagents applied topically is an important com-ponent of the formula for successful results.Antibiotic ointment used immediately at theend of surgery is certainly the preference ofmost surgeons.
The antibiotics most commonly used to-day in the form of drops are Ciprofloxacine(Ciloxan from Alcon) or Ofloxacine (Ocufloxin some countries or Oslox in others , manufac-tured by Allergan). The routine use of antibi-otic drops q.i.d. for seven days is the dosage
recommended. Both of these antibiotics arevery effective. You may use one or the other.They may be instilled immediately followingsurgery and started four times a day within onehour of surgery.
Antimicrobials should be used only forthe shortest period of time needed to obtain thedesired effect and should never be taperedbut simply discontinued. Do not prescribethem at a frequency of less than four timesdaily.
Antibiotics in the first seven days may beused in combination with a steroid. However,once you discontinue the topical application ofthe antibiotic within seven days, if everythinglooks well, the patient has to continue withsteroids.
Most Frequently Used Anti-in-flammatory Agents
The most frequently used antiinflamma-tory agents applied topically are PrednisoloneAcetate 1%, commercially known as PrednefrinForte by Allergan or Econopred by Alcon.These may be started promptly following sur-gery, so that the medication starts its effectsimmediately and continued depending on theclinical findings and the surgeon's individualpreference.
In cataract surgery, there is an inherentdifficulty in establishing consensus guidelines.Those outlined above are the most generallyaccepted by advanced surgeons. It is importantthat the antibiotics, particularly thefluoroquinolone family, which are indeed veryeffective as an antimicrobial medication, beused no more than seven days, unless there is aspecific indication to continue the antibiotic.

C h a p t e r 4: P revent ing In f ec t i on and Inflammation
67
Antibiotics in Irrigating Solutions
The previously widely used practice ofusing antibiotics in irrigating solutions are ofquestionable value. Their use has not beenproven to be effective, mainly because theconcentration and the duration or the exposureof the antibiotic to the bacteria is insufficient toachieve a killing effect. A much better proce-dure is to instill within the anterior chamber acombination of antibiotic and antiinflamma-tory agent as outlined previously. There alsoseems to be a general consensus not to useVancomycin in the irrigating solutions or forirrigation of the anterior chamber immediatelyfollowing surgery. Prospective studies seem toindicate some potential toxicity particularly aclinical significant cystoid macular edema anddecreased best corrected visual acuity in cata-ract patients receiving Vancomycin in the irri-gating solutions as compared with controls.This is not a proven fact but it is a potential forconcern that has been expressed by the Centersof Disease Control in the United States.
Patching
Following phacoemulsification, patch-ing is not used unless the patient lives very faraway and may be at risk for trauma during histrip back home. Practically all patients todayare operated in outpatient surgical centers oreye clinics that have their own operating roomand they go home without patching and startusing the topical antibiotics and antiinflamma-tory agents immediately after getting home sothat the medication will start with their effectimmediately.
Postoperative AntiinflammatoryAgents
We already described the use of antiin-flammatory agents by irrigation into the ante-rior chamber immediately following the op-eration. Gills uses a combination of non-steroidal antiinflammatory agents (Indometha-cin) and a steroidal medication within the ante-rior chamber, mixed with two antibiotics. Inthe other more simple and very effective alter-native which we have outlined, 0.5 ml of Pred-nisolone Acetate (Depomedrol) combined with0.5 ml of antibiotic (Gentamycin) are irrigatedintracamerally immediately following the op-eration.
Postoperatively, the most effective anti-inflammatory agents is a combination of Pred-nisolone Acetate 1% q.i.d. gradually taperedover eight weeks and a non-steroidal antiin-flammatory drug such as Voltaren® q.i.d. fortwo weeks. Either Voltaren or Acular® are twocommonly used and effective medications. Itis also known that topical diclofenac can re-duce pain, burning and inflammation. It mayalso be effective in reducing photophobia afterpupil dilation. The mechanism is not known.However, the use of diclofenac alone is notsufficient to eradicate all inflammation. Supple-mental topical steroid is necessary to com-pletely control inflammation.
This combination of postoperative medi-cations applied topically not only contribute tothe prevention of inflammation and infectionbut also significantly contribute in the patient'spostoperative comfort.

THE ART AND THE SCIENCE OF CATARACT SURGERY
68
BIBLIOGRAPHY
Boyd, BF.: Cataract/IOL Surgery, Section V-A,World Atlas Series of Ophthalmic Surgery, High-lights of Ophthalmology, Vol. II, 1996; 5:17.
Chitkara DK., Jayamanne DGR., Griffiths PG.,Fsadni, MG.: Effectiveness of topical diclofenac inrelieving photophobia after pupil dilation. J Cata-ract Refract Surg 1997; 23:740-744.
Gills, JP.: Pharmacodynamics of cataract surgery,Cataract Surgery: The State of the Art. Slack;1998; 3:19-22.
Lane, S., et al: Antibiotic prophylaxis in oph-thalmic surgery, Ocular Surgery News, SpecialSupplement, Jan. 2000.
O'Brien, TP, et al: Antibiotic update, current treat-ment modalities in ophthalmic surgery, OcularSurgery News, Special Supplement, May 1998.
Perry, HD., Hoffman, J. et al: Choosing an antibi-otic for perioperative use, Ocular Surgery News,Supplement on Antibiotics, July 1998.

C h a p t e r 5: P roceed ing Wi th the Opera t i on
71
PROCEEDING WITH THE OPERATION
PREPARATION, SEDATIONAND ANESTHESIA
Preparation of Patient
Unless the patient is scheduled for gen-eral anesthesia or is likely to be operated undervery heavy sedation (non-airway supported) itis unnecessary to keep these usually older,fragile patients fasting for a large number ofhours. This only contributes to fatigue andanxiety. It is also contraindicated to have thepatients remove all their clothes. This inter-feres with the patient's sense of privacy andcontributes to further anxiety as to what is tocome.
The patient is made comfortable in theholding area, where he or she is met by theattending nurse, who then explains what isgoing to transpire. Presurgical checks areconducted, and the nurse instillsNeosinephrine 10% and tropicamide 1% twodrops each in order to dilate the pupil and onedrop of antibiotic and of Betadine solution,depending on the surgeon's preference. Thissubject is discussed in Chapter 4. Longacting pupillary dilating agents such ascyclopentolate, atropine, homatropine or sco-polamine have no role in today`s smallincision surgery.
The patient is then transported to an-other holding area in the operating room suiteeither by walking or on a lounge chair onwheels. There the patient is met by the anes-thesiologist, who explains that an intravenousline will be started and administers sedative
agents which vary according to theanesthesiologist's and surgeon's choice. Inthe holding area, Jack Dodick, M.D. in NewYork, applies a prudent amount of ocularcompression to the eye and orbit for 10-15minutes. He finds this very beneficial inlowering the intraocular pressure. This ma-neuver lowers the volume of the fluid insideof the eye and orbits thereby leading to ahypotensive eye. This creates a more favor-able surgical environment. This maneuverwas previously done using Honan's ballon inconjunction with peribulbar or retrobulbarinjection of local anesthetic, procedures nolonger used in small incision cataract surgery.The patient is made comfortable in the re-clining chair which is very much like a firstclass seat on an airplane that reclines in analmost 180 degree position. Other surgeonsprefer to place the patient on an operatingtable specially adapted to their needs andwhether they operate from above or on theside.
Sedation
What sedation to administer depends onthe individual patient's emotional profile,which the surgeon should have detected dur-ing his preoperative evaluation. In mostcases, 5 mg of Valium per mouth on arrival tothe clinic leads to sufficient relaxation so thathe or she feels comfortable during surgery.Dodick prefers for the anesthetist to adminis-ter a small dose, 1 mg, of Versed intrave-nously. Versed, like Valium, is a member ofthe benzodiazepine family, but it has a much

THE ART AND THE SCIENCE OF CATARACT SURGERY
72
shorter half-life. Whereas valium takes up to24 hours to be metabolized by the liver,Versed is totally out of the body in less than 2hours. The patient is totally sedated for about10 minutes and the patient is wide awakeand alert after 10-15 minutes, which is thetime the operation lasts. The drug is gonefrom the system within 2 hours. With valium,on the other hand, patients sometimes feelgroggy for a day or two.
Pupillary Dilation
Pupillary dilation is critical to the suc-cess of ECCE, especially phacoemulsifica-tion. Cycloplegic/mydriatic drops, adminis-tered preoperatively, effectively dilate the pu-pil, while topical nonsteroidal antiinflamma-tory drops can help to maintain dilation dur-ing surgery. These medications are instilledtopically at the time of preparation of thepatient before entering the operating room.
ANESTHESIA
Topical
All patients have two or three drops ofproparacaine or tetracaine instilled in the eye,regardless of the type of anesthesia thesurgeon decides to use. One drop everyminute x 3 is a standard protocol (Fig. 35).
Selection of Anesthetic Method
There are a variety of anesthetic meth-ods known to all of you. We will list themhere and proceed to identify those that nolonger have a place in small incision cataractsurgery. They are:
1) Blocks by Injection Anesthesiawith Sharp Metal Needles
a) Retrobulbar: no longer used exceptin exceptional cases.
b) Peribulbar: no longer used.c) Parabulbar: no longer used.d) Van Lint, O'Brien, Nadbath for
controlling lid contraction: no longer used.e) Hyaluronidase: after many years of
recommending its use, it has been finallyshown that hyaluronidase is not an importantfactor in obtaining akinesia more promptly orhaving a more lasting effect.
2) Sub- Tenon's with a FlexibleNeedle
This is a highly effective anesthesiamostly used in combination with topical anes-thesia by surgeons who are either beginningor already are in the transition period ofECCE to phacoemulsification. This combi-nation is also the procedure of choice bysurgeons who perform extracapsular extrac-tion or small incision manual extracapsular.Prospective, randomized studies have con-cluded that single-quadrant, direct sub-Tenon`s injection of anesthetic is as rapid andeffective as retrobulbar injection for cataractsurgery (Figs. 33 and 34). It provides betteranesthesia with comparable akinesia.
The most common complications arechemosis and subconjunctival hemorrhage,but no major complications are encountered.The dispersion of anesthetic fluid underTenon's is effective enough to substantiallydiminish lid discomfort. For these reasons,Sub-Tenon's anesthesia using a flexible can-nula has replaced retrobulbar and peribulbarexcept in very unusual cases.

C h a p t e r 5: P roceed ing Wi th the Opera t i on
73
Figure 33 (above right): Sub-Tenon'sLocal Anesthesia with Flexible Can-nula - Surgeon´s View
Forceps (F) lift the conjunctiva-Tenon´s capsule in the inferior nasal orinferior temporal quadrants between therectus muscles 3 mm from the limbus. Asmall 1 mm buttonhole is cut with scissors(not shown). A Greenbaum flexible can-nula (C) is advanced (arrow) through thebuttonhole until conjunctiva and Tenon´sfits snugly over the hub of the syringe. 2.5cc of local anesthetic is infused quickly,creating a gush of fluid using the "bolus"technique. If additional anesthesia/akine-sia is needed during surgery, the cannulamay be re-introduced.
Figure 34 (below left): Sub-Tenon'sLocal Anesthesia with Flexible Cannula- Cross Section View
This cross section view of the lefteye shows the position of the flexibleGreenbaum cannula during infusion of an-esthetic. The cannula (C) is directed poste-riorly and fluid infused (white arrow) in thesub-Tenon´s space. Inset 1 shows the flex-ible nature (black arrow) of the cannulawhich provides virtually no risk of globeperforation or retrobulbar hemorrhage. In-set 2 shows the rounded, blunt tip with D-shaped port of the half-round cannula.

THE ART AND THE SCIENCE OF CATARACT SURGERY
74
Technique for Performing Sub-Tenon's
When performing a Sub-Tenon's localanesthesia, 1.5 ml of lidocaine is injected.Under topical anesthesia, a small incision ismade in the fused conjunctiva/Tenon's cap-sule 3 mm from the limbus (Fig. 33). If thesurgeon is right handed, it is easier to performthe incision at the inner lower quadrant be-tween the rectus muscles in the right eye andat the lower temporal quadrant in the left eye.If the surgeon is left handed, it would be theopposite. The surgical plane of Tenon's at-tachment to the sclera is carefully dissectedand the cannula is advanced through thisapperture (Fig. 34). It is very importantthat the cannula is always in sub-Tenon'splane. Otherwise, if it is only under theconjunctiva, the flushed anesthetic solutionwill backflush or will infiltrate all throughoutthe subconjunctival space, where it becomesineffective and creates chemosis.
The cannula is advanced under Tenon'suntil the conjunctiva/Tenon's fits snugly overthe hub of the 3 cc syringe. 1.5 cc of thelocal anesthetic is infused using the "bolus"technique. The anesthetic is infused quicklycreating a gush of fluid that spreads through-out the retro and parabulbar spaces (Fig. 34).
Unassisted Topical Anesthesia
Most ophthalmic surgeons, when usingunassisted topical anesthesia, in whichonly drops are administered, use it only whenperforming phacoemulsification and IOL im-plantation through a clear cornea tunnelincision. The increased acceptance of topicalanesthesia is directly related to the somewhat
wider popularity of the clear corneal tunnelincision as first emphasized by I. HowardFine, M.D., (Oregon, USA).
Most surgeons who use this incisionnow do it from the temporal side, whichrequires a series of readjustments in theoperating room. This procedure requiresthe use of a foldable IOL. A corneal tunnelsutureless valve incision no larger than3.0 mm is recommended. Otherwise, cornealcomplications may arise and the incision wouldnot be self-sealing.
Advantages of Unassisted TopicalAnesthesia
This term refers to the use only of anes-thetic drops to obtain sufficient anesthesia toperform the cataract operation. EdgardoCarreño, M.D., Professor of Ophthalmologyat the Funcacion Los Andes, Santiago, Chileand a phacoemulsification expert, considersthat the use of topical anesthesia using a clearcorneal tunnel self-sealing valve incision is asignificant advance in cataract surgery. Withtopical anesthesia, visual recovery is immedi-ate. Other advantages as outlined by Carreño:
1) It prevents the well-known complica-tions of retrobulbar and peribulbar injections
2) It lowers the time of operating roomuse thereby lowering costs.
3) There is no immediate postoperativeptosis, which with retrobulbar or peribulbarand Van-Lint-O'Brien infiltrations lasts from6-8 hours due to temporary akinesia of the lids(as contrasted with the late postoperative pto-sis which is related to the bridle suture on thesuperior rectus). It provides for immediatepostoperative visual recovery which, again, isits main advantage.

C h a p t e r 5: P roceed ing Wi th the Opera t i on
75
Disadvantages of Unassisted Topi-cal Anesthesia
Many surgeons who have performedcataract surgery utilizing "unassisted" topicalanesthesia, that is, topical drops alone, agreewith Paul S. Koch, M.D., that pure, unassistedtopical anesthesia is fairly disappointing. Heestimates that one out of four patients havesome sensation during the operation. Some-times, patients feel pressure build up in the eyeduring injection of viscoelastic. Some feel irismanipulation. Others are aware of the sensa-tion of the lens being implanted into the eye.Koch found that he felt uncomfortable operat-ing on these people, because he never knew inadvance who would be comfortable and whowould not.
Other disadvantages and limitations asoutlined by Carreño are:
1) Only a highly experienced surgeonshould operate with topical anesthesia. Theeye can move, which makes the operation moredifficult. If the eye movement occurs whilecapsulorhexis is being done, an undesirablecapsular tear may take place leading to failureof this important stage of the operation.
2) The most controversial argumentagainst topical anesthesia is an intraoperativecomplication. Consequently, the surgeon mustbe highly skilled so as to:
a) expect as few intraoperative com-plications as possible. b) be able to convert toanother method of anesthesia during the intra-operative stage. Topical anesthesia by itselfmay be insufficient for the surgeon to ad-equately handle intraoperative complications.
3) Topical anesthesia is not indicated inall patients. This is particularly true inanxious, stressed patients, people with hearinglimitations, children and very young patients.
4) The presence of a very opaque cata-ract is a contraindication to the use of topicalanesthesia (Fig. 1-B). This is because thesurgeon depends on the patient's capacity tovisually concentrate on the operating micro-scope light in order to avoid eye movementduring the operation. If he/she cannot fixatewell on the microscope light and maintain thatfixation, the eye will move. This may lead tocomplications.
In essence, adequate selection of patientsis fundamental when considering the use oftopical anesthesia.
The Anesthetic Procedure ofChoice
It is the general consensus today amongsurgeons experienced with phacoemulsifica-tion that a combination of topical anesthesia(proparacaine 1% or tetracaine 1%) and 0.5 ccof 1% unpreserved lidocaine irrigated into theanterior chamber through a 30-gauge cannula(Figs. 35 and 36) is the anesthetic procedure ofchoice for small incision cataract surgery, par-ticularly phacoemulsification. This importantbreakthrough in ophthalmic anesthesia wasintroduced by James Gills, M.D. in 1997.
Technique for Irrigation of Lidocainein AC
Dodick first makes a clear cornea inci-sion using a 2.7 mm diamond knife. He believesthat the non-preserved lidocaine irrigated intothe anterior chamber anesthetizes the nervesof the iris and the ciliary body. The pressurewaves that ensue during irrigation and aspira-tion in the midst of the phaco operation cansometimes impinge upon those nerve fibersand lead to discomfort. In addition, Dodick has

THE ART AND THE SCIENCE OF CATARACT SURGERY
76
observed that this anesthesia inside the eyehelps dull the patient’s sensitivity to the brightlight of the microscope by temporarily block-ing some photoreceptor cells. The rest of theoperation is continued through the same clearcornea incision.
Intraocular unpreserved lidocaine irri-gated into the anterior chamber as outlined hasbeen proven safe and convenient.
Even though a few researchers (i.e. Gillowet al, Boulton et al) have concluded that theroutine use of intracameral lidocaine as a supple-ment to topical anesthesia in routinephacoemulsification does not have a clinicallyuseful role, these experiences constitute a sig-nificant minority and are based on postoperativequestioning of patients concerning discomfortor by well documented trials but in medium
number of patients and by different surgeons.In papers published based on monitoring pa-tient discomfort, not by a subjectivequestionaire, but by objectively measuring vi-tal signs during surgery. the data support theconclusion that patients operated with anteriorchamber irrigation of unpreserved lidocainefeel comfortable during the procedure, despitehaving had no intravenous sedation and re-gardless of sex or age and dismiss the subjectivenature of postoperative questioning patientsconcerning discomfort. In view of the smallcontroversy existing, we must rely on the provenextensive experience of well known, presti-gious, cataract surgeons such as James Gills,M.D., and Paul Koch, M.D., here presented.
An alternative technique for intracam-eral irrigation of 0.5 cc of 1% lidocaine is the
Figure 35: Topical Anesthesia
Unaided topical anesthesia is nowa commonly used method in small inci-sion cataract surgery because it is userfriendly and comfortable for the patient.Only expert small incision surgeonsshould use it without the aid of anothermethod. Most surgeons prefer to use topi-cal anesthesia combined with intracam-eral anesthesia (Fig. 36) in small incisioncataract surgery. This illustration showsthe use of anesthetic drops (A) such asproparacaine or tetracaine, one drop ev-ery 10 minutes, 30-45 minutes preopera-tively.

C h a p t e r 5: P roceed ing Wi th the Opera t i on
77
one proposed by Paul S. Koch, M.D (Fig. 36).He uses a 15º blade in his left hand and .12forceps in the right hand. The blade is placedwhere he wants the sideport entry incision andthe forceps 180º away from that, resting on theperipheral cornea (Fig. 36). The forceps areonly pressed against the cornea. They do notgrab it, because the purpose of the forceps isonly to provide counter pressure for the inci-sion. The blade is then used to make an incisionapproximately 1 mm wide and 1 mm long,beginning in the peripheral clear cornea.
That incision is completely comfortable,because it is no more than a corneal manipula-tion, and the cornea is still anesthetized fromthe original drops given in the holding unit.
Then, 0.5 cc of 1% unpreserved lidocaineis irrigated into the anterior chamber through a
30-gauge cannula (Fig. 36). Most of the time,the patient does not feel anything, but some-times, either because of intraocular pressurechanges or the effect of direct flow onto the iris,the patient may feel a little discomfort. This isnot a matter of concern because in a matter ofseconds the discomfort dissapears.
Koch squirts the little extra lidocainethat remains in the syringe on the surface of thecornea, providing additional topical effect. Theeye is not paralyzed, and an occasional patientmay move it, but this is not nearly the problemthat it is with topical anesthesia. The lack ofdiscomfort makes it unnecessary for the patientto want to move the eye, and Koch as well asGills have found that cooperation in keepingthe eye still is excellent.
Figure 36: Use of Intracameral Anesthesia
After instilling anesthetic drops on theconjunctiva and cornea (Fig. 35) the surgeon en-ters the anterior chamber through the ancillaryincision (I) (Fig. 41-A) using an insulin syringewith a 30 gauge cannula (C). This maneuver is
done with the aid of fine toothed forceps (F)in the contralateral side of the ancillary inci-sion acting as counterpressure. One dose of0.5 ml of 1% unpreserved lidocaine is irri-gated into the anterior chamber. The prelimi-nary marking of the main incision is shownin (A).

THE ART AND THE SCIENCE OF CATARACT SURGERY
78
Injection of Viscoelastic
The eye anesthetizes quickly, and theanesthesia is very profound. Usually in lessthan 10 seconds, the eye is already anesthe-tized, and the viscoelastic injection is performedquite comfortably.
What Can be Done with the Com-bined Anesthesia
Because the combination of topical andintracameral irrigation anesthesia is so effec-tive, the surgeon can perform cataract surgery,lens implantation, iris manipulation, and evenvitrectomy if a complication arises usuallywithout any further injection of anesthetic. If apatient does feel some discomfort, a secondirrigation may be performed. Patients withmental retardation and those with deafnesshave been successfully operated with this anes-thetic combination as long as the surgeon takesthe time to explain prior to surgery that hewanted them to look at the light and keeplooking at the light.
Side Effects of the CombinedAnesthesia
Lidocaine has an effective duration of upto 4 hours. Patients may not see very wellimmediately after the operation, but then a fewhours later the vision really improves. Kochhas concluded that patients have a temporary,neuro-sensory, retinal blockade causing tran-sient blurring of vision following the operation.He has postulated that the anesthetic may dif-fuse back to the retina and perhaps has a directeffect on the ganglion cells. Gills had a patientwith an open posterior capsule who had signifi-cant vision loss for about 24 hours after the
operation. This clinical observation may sup-port Koch's hypothesis, because in the absenceof a posterior capsule the lidocaine could dif-fuse back toward the retina that much moreeasily. As the lidocaine wears off, the visualacuity and contrast sensitivities recover.
How to Manage Patients Who FeelPain and Discomfort
If the patient continues to blink or squeezethe eyelids following the combined topical andintracameral anesthesia, you can control thiswith the sub-Tenon's injection of lidocaine asillustrated in Figs. 33 and 34. The effect isalmost instantaneous, and surgery can con-tinue without delay.
PHOTOTOXICITY INCATARACT SURGERY
Since all cataract surgery is doneunder the microscope, we should clarify herethe practical and clinical aspects of light orphototoxicity from the surgical microscope. Ithas been demonstrated that in some patientsand under specific circumstances, toxicity fromthe light of the microscope can affect the macula.This is seen with fluorescein angiography,which shows an area of pigment abnormalityusually below the fovea. The visual field inthese patients shows that in this area there issevere to moderate phototoxic damage to thephotoreceptors. Without these tests,phototoxicity can be difficult to determine andto see.
The major factors involved withphototoxicity are the time of exposure, thetilt and the illumination intensity. (It isimportant to realize how hard it is to get awayfrom the macular area if we are centered overthe pupil).

C h a p t e r 5: P roceed ing Wi th the Opera t i on
79
The microscope has three light sources:the two side lights and the coaxial beam. Eachof these light sources produces a focal point ofillumination on the retina. It is not the timelength of the operation that is important. It isthe time the light is focused on one particu-lar area of the retina which is critical.
In addition, within the period which anyone operation lasts, sequential light exposureto the same retinal area is additive. If we turnon the light on one spot for three minutes, turnit off and then turn it on that same spot foranother four minutes, the effects of those expo-sures are additive. If, in a certain patient andwith a certain intensity of light from the micro-scope, we expose one macular area duringthree minutes, we may have no lesion whatso-ever but if the total exposure extends to sevenand a half to eight minutes, a lesion may occur.In the human eye, with the standard surgicalmicroscopes on maximum intensity of light,it probably only takes four to eight minutesto produce a retinal lesion. Most phototoxicburns are seen in the inferior part of the fovea.We should leave the light source on thelowest setting.
The potential for trouble related tophototoxicity in cataract surgery is not oftenrecognized. The patient may have 20/25 visionpostoperatively and still complain that he doesnot see adequately. Only after fluoresceinangiography and a visual field can we thenexplain why these patients complain. Even themost experienced of us need to be aware of thepotential for phototoxicity and take the steps toavoid it.
BIBLIOGRAPHY
Anders, N., Heuermann, T., Ruther K., Hartman,C: Clinical and electrophysiologic results after in-tracameral lidocaine 1% anesthesia. Ophthalmol-ogy 1999; 106:1863-1868.
Boulton JE., Lopatatzidis A., Luck J., Baer RM.:A randomized controlled trial of intracamerallidocaine during phacoemulsification under topicalanesthesia. Ophthalmology, 2000; 107:68-71.
Boyd, BF.: Cataract/IOL Surgery. World AtlasSeries of Ophthalmic Surgery, HIGHLIGHTS OFOPHTHALMOLOGY, Vol. II, 1996; 5:21-22.
Boyd, BF: Significant developments in local anes-thesia. Highlights of Ophthalmol. Bi-Monthly Jour-nal, Vol. 23, Nº 6, 1995 Series, pp 55-62.
Carreño E.: Phacoemulsification Sub-3 technique.Guest Expert, Boyd’s BF., The Art and the Scienceof Cataract Surgery, Highlights of Ophthalmol-ogy, 2001.
Fichman RA: Use of topical anesthesia alone incataract surgery. J Cataract Refract Surg, 1996;22:612-614.
Gillow T., Scotcher SM., Deutsch J., While A.,Quinlan MP: Efficacy of supplementary intracam-eral lidocaine in routine phacoemulsification undertopical anesthesia. Ophthalmology, 1999; 106:2173-2177.
Gills JP., Cherchio M., Raanan MG.: Unpreservedlidocaine to control discomfort during cataract sur-gery using topical anesthesia. J Cataract RefractSurg. 1997; 23:545-550.
Gills JP., Martin RG., Cherchio M.: Topical anes-thesia and intraocular lidocaine. Cataract Surgery:The State of the Art, Slack; 1998; 2:9-17.
Koch, PS.: Anesthesia. Simplifying Phacoemulsi-fication, 5th ed., Slack; 1997; 2:12-26.

THE ART AND THE SCIENCE OF CATARACT SURGERY
80
Koch, PS.: Anterior chamber irrigation withunpreserved lidocaine 1% for anesthesia duringcataract surgery. J Cataract Refract Surg. 1997;551-554.
Koch, PS.: Preoperative and postoperative medica-tions of anesthesia. Current Opinion in Ophthal-mology 1998; 9;1:5-9.
Koch, PS.: Preoperative Preparation . SimplifyingPhacoemulsification, 5th ed., Slack; 1997; 1:1-11.
Masket S.: Ocular anesthesia for small incisioncataract surgery. Atlas of Cataract Surgery, Editedby Masket-Crandall, Published by Martin DunitzLtd., 1999; 15:111-114.
Naor J., Slomovic AR.: Anesthesia modalities forcataract surgery. Current Opinion in Ophthalmol-ogy, Vol. 11 Nº 1, Feb. 2000.
Tseng SH., Chen FK: A randomized clinical trial ofcombined topical-intracameral anesthesia in cata-ract surgery. Ophthalmology 1998; 105:2007-2011.

C h a p t e r 6: Phacoemuls i f i c a t i on - Why So Impor t an t ?
83
Phacoemulsification is the "state of the
art" operation of choice for cataract surgery inacademic institutions and private eye centersworldwide. Ophthalmologists in training (Resi-dencies and Fellowships) receive training inphacoemulsification first and manual extra-capsular as a second choice.
COMPARING PLANNEDEXTRACAPSULAR WITH PHACO
EXTRACAPSULAR
With planned extracapsular extractionan 8-9 mm limbal incision is performed,preceded by a conjunctival flap (either limbalbased or fornix based). The anterior capsule isusually opened with a "can opener"capsulorhexis technique. Some surgeons havedeveloped the expertise to do a continuouscircular capsulorhexis. The nucleus is thenexpressed with gentle pressure inferiorly suchthat the lens is subluxated in its entirety into theanterior chamber and out of the eye through asuperior limbal incision (Fig. 37). Aspirationis used to remove the remaining cortex fromthe capsular bag and viscoelastic is irrigatedinto the anterior chamber and capsular bag(Fig. 38). A PMMA intraocular lens im-plantation is performed (Fig. 39) and thewound is sutured.
In planned extracapsular, which is stillably and successfully performed by a signifi-cant number of ophthalmic surgeons, the final
visual recovery takes place slowly through aperiod of 5 to 6 weeks.
In small incision manualextracapsulars such as with Blumenthal'sMINI NUC and Gutierrez manualphacofragmentation, a foldable IOL may beimplanted. Both of these procedures are fullypresented in the Section on Manual Extracap-sular Extraction in this same Volume follow-ing Phacoemulsification. Visual recovery ismuch more rapid.
ADVANTAGES OF THE PHACOTECHNIQUE
The phacoemulsification technique of-fers the following benefits and advantages overplanned extracapsular as outlined by EdgardoCarreño: 1) it is performed through an inci-sion 3mm or less in size which is self-sealingand watertight thereby improving safety dur-ing the procedure. 2) It is significantly lessinvasive thereby leading to much less oculartrauma and consequently less postoperativeinflammation. 3) It results in minimal or noinduced astigmatism. 4) It provides muchmore rapid visual and physical recovery andprompt refractive stability. The visual recov-ery is immediate if topical anesthesia is used.All these advantages lead to an important in-crease in the patient's quality of life. In addi-tion, a smaller incision also may reduce the riskof endophthalmitis.
PHACOEMULSIFICATIONWHY SO IMPORTANT?

THE ART AND THE SCIENCE OF CATARACT SURGERY
84
MAIN TECHNICAL DIFFERENCESASSOCIATED WITH PHACO
The opening of the anterior capsule isdone as a continuous curvilinear capsulorhexis(CCC) as described by Gimbel et al (see Figs.43, 44, 45). An ultrasonic probe (Figs. 50-Aand B) is used to emulsify the nucleus anddraw it out of the eye through an aspirationport (Chapter 8). This allows the removal of a10 mm cataract through a 3 mm incision (orless). Because the integrity of the anteriorchamber is maintained throughout the proce-dure, the intraocular pressure is subject to lessfluctuation and poses much less of a risk forsuprachoroidal hemorrhage.
Figure 37: Planned Extracapsular
With planned extracapsular, the anteriorcapsule is opened with a "can opener"capsulorhexis technique. The nucleus is ex-pressed with gentle pressure inferiorly. Pressure(black arrow) is applied on the posterior woundlip. The nucleus (N) is slid out of the eye (whitearrow). The incision shown here is medium insize (5-6 mm) and allows implantation of a PMMAIOL. A full incision extracapsular is 8-9 mm inarc.
Removal of the lens by phacoemulsifica-tion is followed by placement of a posteriorchamber foldable intraocular lens implantthrough a 3 mm incision. The wound mayrequire one or no sutures. Variations oftechnique may involve a superior limbal inci-sion with dissection of a sclero corneal tunnelto form a self-sealing valve incision, a clearcorneal incision with corneal tunnel and self-sealing valve incision (with experienced sur-geons) and the scleral tunnel incision which isused increasingly less but is a safe procedurefor difficult cases (Figs. 40, 41, 42). The limbaland the corneal incision are either placed at 12o'clock or in the superior temporal quadrant.The limbal incision and tunnel is the proce-

C h a p t e r 6: Phacoemuls i f i c a t i on - Why So Impor t an t ?
85
Figure 38 (above right): Irrigation withViscoelastic
Before insertion of the intraocularlens, fluid in the anterior chamber and withinthe capsular bag is replaced with a vis-coelastic liquid. A cannula (C) is placedinto the capsular bag at position (B) andviscoelastic (V) injected (arrows). The can-nula is inserted across the anterior chamberto a position (A) and as the cannula iswithdrawn, viscoelastic (V) is injected (ar-rows). Replaced fluid (F) flows out throughthe incision. The viscoelastic will help toprotect corneal endothelium, posterior cap-sule and iris during insertion and intraocularmanipulation of the lens implant.
Figure 39 (below left): IOL Implantation inPlanned Extracapsular
Following aspiration of the remain-ing cortex from the capsular bag and deepening theanterior and posterior chambers with viscoelasticas shown in Fig. 38, the intraocular lens is insertedinto the capsular bag. The inferior loop is directedinto the capsular bag inferiorly (arrow). The supe-rior loop shown here is then inserted into thesuperior capsular bag.

THE ART AND THE SCIENCE OF CATARACT SURGERY
86
dure of choice for surgeons in the transitionstage or who do not have a large cataractsurgical volume because it allows conversioninto extracapsular if necessary. Enlargement ofa corneal incision in order convert to an extra-capsular extraction, often results in intolerablepostoperative astigmatism.
Both standard polymethylmethacrylate(PMMA) or foldable (acrylic, silicone or hy-drophilic) intraocular lenses may be used. Afoldable lens allows for an even smaller inci-sion and less risk of postoperative astigmatismas a result of wound construction. Because ofthe watertight wound construction of thismethod and the stability of the anterior cham-ber during phacoemulsification, this techniqueis amenable to topical anesthesia in a coopera-tive patient (Fig. 35) or a combined topical andsub-Tenon's local anesthesia, (Figs. 33, 34) ora combined topical and intracameral anesthe-sia ( Fig. 36) advised by Gills. The choicemainly depends on the experience and skill ofthe surgeon , but there may be special consid-erations such as difficulty in communicationwith the patient and in cases complicated by apatient's poor general health.
LIMITATIONS OFPHACOEMULSIFICATION
Surgeons who have a successful clinicalpractice, ample experience and well earnedprestige and are using planned extracapsularare understandably reticent and apprehensiveabout shifting from a technique they alreadymaster to one which depends a great deal on theunderstanding of how the phaco machine func-tions. 50% of the success in doing phacoemul-sification depends on the proper use of theequipment at each stage of the operation. Oph-thalmic surgeons are used to depend on theirsurgical skill. It is part of their self-esteem. Asemphasized by Centurion, phacoemulsifica-
tion is equipment and instrument-dependent aswell as team-dependent, because the team as-sisting with surgery must fully understand allthe steps of the operation and, by all means,how the phaco machine works.
The Importance of Mental Attitude
Understanding the workings of the phacomachine requires a complete change in mentalattitude and the undergoing of a rigorous train-ing not only in the surgical technique, butlearning to use two feet (microscope andpedal) instead of one (microscope). The sur-geon must also be attentive to the perception ofdifferent sounds emitted by the machine, eachone signaling a different function and param-eters which in turn the surgeon must act upon.It is essential for the physician to understandexactly how to obtain the optimal use of themachine, the rationale behind it, the fluid andphacodynamic processes within the machineand the eye and how to manage safely theequipment, safely, including the varioushandpieces and, of course, the phaco power,and the irrigation and aspiration (see Figs. 49-A through 65).
Motivation to Undertake this Task
This is not an easy task. The multiplemechanical functions of the equipment are not"friendly" to those physicians who , althoufhexcellent surgeons, are not mechanicallyminded. Only the knowledge that such achange, if successfully done, will be best forhis/her patients can serve as the motivation toundertake such a significant step.
For all these reasons, many excellentsurgeons decide not to enter into phaco, andmany others have the equipment available intheir eye center or hospital but allow it toremain idle.

C h a p t e r 6: Phacoemuls i f i c a t i on - Why So Impor t an t ?
87
In order to overcome these negative as-pects of phacoemulsification, it is fundamentalto have a smooth transition into phaco. In orderto achieve it, it is essential that you read and re-read the next chapter (Chapter 7), which pre-sents the very best ways to achieve a successfultransition with little stress or apprehension.
Comparison of Costs - Phaco vs ECCE
One of the strong limitations of phacohas been the cost of not only the phaco equip-ment but also the supplies related to its use.This is important for a significant number ofophthalmologists when operating on patientswho are not economically advantaged.
Fixed Costs with ECCE
Let us analyze, however, the updatedsituation related to costs of performing pha-coemulsification, and compare it with the costsof the supplies needed to perform extracapsu-lar extraction. With the latter, there is the costof very fine sutures, which are unnecessary inphaco; there is the cost of local anesthesiainvolved with either a retrobulbar or a paraocularinjection versus phaco in which only topicalsometimes with intracameral anesthesia is uti-lized. The cost of the postoperative injection ofsteroid in the fornix often done following ext-racapsular is also unnecessary with phaco al-though the trend now is to inject steroid in theanterior chamber (see Chapter 5). The cost ofeven a fairly short stay in the recovery roomfollowing the often used sedation needed withan extracapsular extraction for anxiety is higherthan in patients with phacoemulsification whohave had only topical anesthesia without seda-tion and walk to their home within a fewminutes following surgery.
The significant economical savings tothe patient from lost working hours with ECCEvs almost immediate recovery with phaco andthe improved quality of life with phaco areother major important contributions. All theseare important features to consider when the so-called expenses for both operations are takeninto account.
Phaco's Progressively DecreasingInvestment
What about the high expenses with phacoequipment? There was a time when the equip-ment or phaco machine required a significantinvestment. The supplies or tubing needed foreach patient was also a heavy expense whenperforming several cases. All this has changeddue, in great part, to the ingenuity and under-standing by the industry that these high ex-penses and initial investment were a signifi-cant barrier which prevented more ophthalmicsurgeons from adopting phaco.
At present, most of the companies thatmanufacture phaco units are helping physi-cians and hospitals to acquire the equipmentand supplies. The equipment is made availableat much more reasonable prices than their realsales cost, with the understanding that therewill be a monthly utilization by the surgeon ofthe phaco supplies of that particular manufac-turer. In addition, the manufacturer providesadvice and hands-on-training by experts to thesurgeon so that he/she will be able to enter intothe transition period (Chapter 7) utilizing his/her own personal equipment acquired fromthat manufacturer.
The "tubing" which previously had to bediscarded after each operation is no longer aproblem cost-wise. Now it may be used for asmany as 60 cases in the same day. No re-

THE ART AND THE SCIENCE OF CATARACT SURGERY
88
sterilization is needed. The tubing may beused without replacement for a complete dayof phaco surgery. Upon completion of all thephaco cases in one day, the tubing must bediscarded. Therefore, by programming thesurgeon´s cases accordingly, a great deal ofsavings can be made.
All of this makes the phaco techniquemore accessible to a larger number of surgeons.We still have to cope, however, with the needsof surgeons in countries in which the grossnational product is very low.
Major Limitations in Non-Eco-nomically Advantaged Countries
Experts in programs for rehabilitation ofsight in large numbers of indigent patients--such as Francisco Contreras, M.D. in Peru,Everardo Barojas, M.D. in Mexico, JuanBatlle, M.D. in the Dominican Republic,Newton Kara, M.D., in Brazil,-- all of whomare magnificent surgeons with a large privatepractice but also do a great deal of service to thecommunities, have stated that most patients inthis category earn no more than US$1.00 (onedollar) a day and that the maximum that can becharged to a patient for a cataract operationshould be what that particular patient earns inone month.
This is important information that needsto be appreciated by cataract surgeons through-out the world interested not only in the progressof the technology of our profession but also inthe humanitarian aspects of what we do bestwhich is ophthalmology.
It is also of great interest as outlined byContreras that the number of phaco opera-tions being performed has increased in thosecountries with the highest gross national prod-uct per person. In countries where earnings bypatients are low, phaco is still behind. In manycountries, only 5 to 10% of the population canafford phacoemulsification in spite of the fa-cilities that we have outlined. Of the rest,thirty percent of the population has a mid-levelof income, 30% are very poor, and 30% of thepopulation are in extreme poverty.As we continue to progress in the technologicaldevelopments of ophthalmology, which is ablessing, we also need to be aware of thelimitations existing in the populations of manycountries throughout the world.
An exemplary case is that achieved byProfessor Arthur Lim, M.D., in Singapore,who has put together significant funds fromprivate organizations and has trained large num-bers of young ophthalmologists to learn thesemodern techniques to combat blindness in SouthEast Asia and China.

C h a p t e r 6: Phacoemuls i f i c a t i on - Why So Impor t an t ?
89
BIBLIOGRAPHY
Centurion V: Importance of mental attitude andmotivation in phacoemulsification. Faco Total,pp. 57.
Centurion, V.: The transition to phaco: a step bystep guide. Ocular Surgery News, Slack, 1999.
Carreño E.: Phacoemulsification Sub-3 technique.Guest Expert, Boyd’s BF., The Art and the Scienceof Cataract Surgery, Highlights of Ophthalmol-ogy, 2001.
Drews, RC: Medium-sized and small incision ext-racapsular extraction without phaco. World AtlasSeries of Ophthalmic Surgery of Highlights, byBoyd, BF, Vol. II, 1995; 5:54-56.
Gimbel, H: Posterior Continuous Curvilinear Cap-sulorhexis (PCCC). World Atlas Series of Oph-thalmic Surgery of Highlights, by Boyd, BF, Vol.II, 1995; 5:96-97.

THE ART AND THE SCIENCE OF CATARACT SURGERY
90

C h a p t e r 7: P repar ing f o r t he Trans i t i on
93
PREPARING FOR THE TRANSITION
GENERAL OVERVIEW AND STEPBY STEP CONSIDERATIONS
Complete comprehension of what ispresented in this chapter is essential for thesuccessful undertaking of phacoemulsification.Before you read it, we strongly recommendthat you first read Chapter 6 which refers notonly to the unquestionable advantages of phacobut to its limitations, most of which are relatedto the challenge of understanding how thephaco machine works and how to attain itsoptimal use.
Equipment - Dependent andPhase-Dependent Technique
The transition from planned extracapsu-lar extraction to phacoemulsification funda-mentally refers to the gradual change that theophthalmic surgeon who already masters theplanned extracapsular must undertake in orderto dominate the new technique of phaco, whichis equipment-dependent. This transition shouldbe progressive and atraumatic. As the surgeonadvances step by step, he or she should nevergo on to the following step if he has notdominated the previous step. This operationis also a phase-dependent technique, as em-phasized by Centurion. Each phase must becompleted with the precision of a watch maker.If you pass on to the following step withoutmastering the previous step, complications mayarise with consequent failure and grief. Thislearning curve is achieved with effort, dedica-
tion and proper training to perform each phaseof the transition well.
Outlining the steps necessary in thetransition from extracapsular surgery to pha-coemulsification, we will present you a de-tailed picture of what it really takes to enterinto the transition and to master the learningcurve. We will describe and fully illustrateeach one of the steps in sequence.
For young ophthalmologists who enterdirectly into phacoemulsification in their train-ing, this "bitter pill" of changing from plannedextracapsular to phaco is an experience theywill fortunately miss. But when they laterteach others who have not been trained inphaco, but learned and have spent their careerdoing extracapsular instead, they need to rec-ognize - as we do in this presentation - thedifficulties their colleagues face, and teachaccordingly. Extracapsular surgeons still con-stitute the majority of ophthalmologists world-wide.
Mental Attitude
The surgeon must be absolutely con-vinced that changing from planned extracapsu-lar to phacoemulsification will be best for hispatients, particularly because of a very rapidvisual recovery and physical rehabilitation backinto normal life. As long as the surgeon is notcompletely persuaded of the reasons why hewants to take this crucial step in his profes-sional development, he will never attain apositive experience during the transition with

THE ART AND THE SCIENCE OF CATARACT SURGERY
94
maximum safety, low risk and high benefits forthe patient and minimal stress for him/herself.The fact that phaco also significantly shortensthe waiting period for cataract surgery in thesecond eye, that it has 50% fewer complica-tions than ECCE and that the operation can bedone while the cataract is still in its early stages(20/40 vision, lowered contrast sensitivity andglare intolerance) should be another strongincentive to adopt phaco (See Chapter 6). Theusual reasoning that the planned extracapsularsurgeon assumes are thoughts like: "If I do sowell with planned extracapsular, why change?".This is particularly true when your practice ismostly composed of private patients, some ofthem important persons in the community andno risks can be taken. The successful extracap-sular surgeon continues to find reasons for notmaking the change, such as: "I have very littlepostoperative astigmatism with planned extra-capsular, so why get into the problem of oper-ating with a smaller incision and the difficultiesthat may arise?" "The visual recovery compar-ing the two techniques after several weeks isabout the same; I am not in a hurry for mypatient to attain a prompt visual result as longas the final visual recovery will be the same.""It is better for the patient to have a goodplanned extracapsular than a bad phaco." "Iknow that with planned extracapsular I willhave practically no complications, but I am notso sure that such will be the case with phaco,particularly in the early cases."
In essence, the surgeon has to make his/her decision rationally and on his or her owninitiative. This will provide the stimulus andthe perseverance in order to enter into thelearning curve and the perseverance to eventu-ally master what is considered one of the best
operations in the field of medicine. Once thedecision is made, it must be followed throughwith firmness and resolve.
UNDERSTANDING THE PHACOMACHINE
A successful phacoemulsification de-pends essentially on two factors: 1) the surgeon'sskill; 2) the surgeon's and his team's under-standing of how the phaco machine works.
It is fundamental for the surgeon to havea thorough and practical knowledge regardingthe specific equipment that he is using and howthe technology of phaco machines in generaloperates.
Becoming Familiar with theEquipment
Becoming first familiar with the phacomachine in an experimental laboratory first, isthe best way to learn and understand how theequipment works. This has been reemphasizedonce and again by Virgilio Centurion M.D.,one of the world's best cataract surgeons whohas dedicated a great deal of his valuable timeto teach the transition through courses andpublications. His recommendation is to prac-tice first in the laboratory the use of both handsand the four positions of the phaco machinefoot pedal so as to become familiar, comfort-able, and adept with the parameters of themachine (Figs. 52, 53). For more sensitivecontrol of the phaco machine foot pedal, use ashoe with a thin sole (keep it in the operatingroom) and use your dominant foot (equivalentto the dominant hand). Control the surgicalmicroscope with the non-dominant foot.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
95
Practice using both hands can be attainedwith pig eyes and synthetic eyes in syntheticheads, often coached by the company repre-sentative from whom you acquired the phacomachine and equipment. The surgeon can alsopractice with a human ocular globe supplied bylarge Eye Banks or with pig eyes removed soonafter the animal is sacrificed. These globesshould be refrigerated, not frozen, with thecornea protected with a sponge. When placedin a 700 W microwave oven for 4 seconds, thelens develops a subcapsular cataract. After 9seconds, 50% of the lens will be opaque andhard.
Two Hands, Two Feet and SpecialSounds
The surgeon should dedicate appropri-ately extensive time in the laboratory towardsacquiring complete self-assurance in the use ofthe machine, coordinating his or her hands andthe two foot pedals. Additional time may beused to practice how to make the new, smallerincision, the capsulorhexis and other surgicalsteps. Phaco is mostly a two-handed tech-nique, so you must become trained and developreflexes to use both of your hands and both ofyour feet, together.
During training in the laboratory, thesurgeon grasps how the machine works duringeach step of the operation, learns the methodfor introduction of the phaco tip and the mostcomfortable position in which to place thehandpiece; why and when to elevate or lowerthe height of the fluid bottle, when to increaseor decrease the flow of fluid or the vacuum andwhen to increase or decrease the power of thephaco. These parts of the learning curve aremastered in the laboratory so as to reallyunderstand and become fully adept with thefunctions of the equipment before entering thepatient's eye.
While learning to use the machine's footpedal you must also perceive the significanceof the sounds of the machine which varydepending on the surgical step or stage, such asthe balance of flow when the phaco tip is notoccluded (Figs. 57, 58), and the sounds alertingthe surgeon to changed in fluid dynamics whenthere is occlusion of the tip. In each instance,the surgeon receives a sonic feedback, con-stantly informing him about the state of thefluid dynamics in the eye (Figs. 59, 60). So thesurgeon must learn to use both hands, both feet,and to listen to the phaco machine.
In essence, experimental training first inthe laboratory is the best investment the sur-geon can make to shorten and successfullytransverse the learning curve. It is a necessaryexperience to learn the workings of the equip-ment fully. Its main aim is not that of learningthe surgical technique at this stage. That comeslater. We must not improvise or try to learnthe use of a phaco machine in the operatingroom. The surgeon should not begin learningthe use of the machine directly on a patient'sseeing eye.
Main Elements of Phaco Machines -Their Action on Fluid Dynamics
In this chapter we will thoroughly dis-cuss the optimal use of the phaco machine andthe rationale behind it, the three elements ofmost phaco systems (irrigation, aspiration andultrasonic energy), fluidics and phacodynam-ics, the importance of and understanding of theSurge Phenomenon. The rationale behind highvacuum - low ultrasound power technology,the new technology of the peristaltic pump,particularly in the three main equipment sourcesavailable such as the Alcon's Legacy 2000,Allergan's Prestige (and the Sovereign) andStorz Millennium and some useful informa-

THE ART AND THE SCIENCE OF CATARACT SURGERY
96
tion about the new phaco tips and their contri-bution toward a better operation.
COMPARISON OF SURGICALTECHNIQUES FOR TRANSITIONVS EXPERIENCED SURGEONS
There are several techniques in pha-coemulsification that remain practically thesame for the surgeon who is undergoing thetransition and those who are more experienced.On the other hand, there are stages of theoperation in which there are definite variationsfor the experienced surgeon, some of themminor, others moderate and others major.
We have divided the subjects into two(2) groups: 1) those that are the same for allsurgeons and 2) those that vary depending onthe skill of the surgeon for this particular opera-tion.
Techniques Which Are the Samefor the Transition and forAdvanced Surgeons
Capsulorhexis
These parts of the technique are practi-cally the same for both groups, with slightindividual variations (Figs. 43, 44, 45). Themain feature that may vary is the size of thecapsulorhexis. Some very advanced surgeonsdo a small capsulorhexis, while in the transi-tion a somewhat larger capsulorhexis is advis-able, depending on the size of the IOL to beimplanted.
Hydrodissection and Hydrodelin-eation
These techniques remain essentially thesame for the transition and in advanced sur-geons (Figs. 46, 47, 48).
Epinucleus Removal
This technique does not vary substan-tially in the transition from that used by ad-vanced surgeons (Fig. 69).
Cortex Removal
The technique is the same for both groups(Figs. 70, 71). It is important not to feel overconfi-dent at this stage and by all means avoid beingaggressive.
Techniques that Vary Accordingto the Skill of the Surgeon
Anesthesia
In the transition, the surgeon may useparabulbar or Sub-Tenon's (flush) anesthesiausing Greenbaum's cannula (Figs. 33, 34), par-ticularly because conversion to ECCE may beneeded. It is only advanced surgeons who mayuse topical anesthesia alone or combined withintracameral irrigation anesthesia (Figs. 35,36).
Fixation of the Globe
In the transition, the surgeon does needto fixate the globe, passing a suture through thesuperior rectus, versus the experienced sur-geon who does not need to do so.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
97
The Incision
Sclero corneal tunnel, limbal tunnel, cor-neal tunnel: these three types of incisions de-pend on the skill and experience of the surgeon.In the transition it is important to use thestepped incision starting at the limbus andperforming a sclero corneal tunnel based on alimbal incision, in case there is need to revertto a ECCE. During the transition, it is alwaysimportant for the surgeon to know that he/shemay revert to ECCE whenever they feel un-comfortable with the surgery at any specificstage. Only more advanced surgeons should dothe corneal incision and tunnel (Figs. 40, 41,42).
Type of IOL
Foldable lenses should only be usedby advanced surgeons. PMMA oval lenses5.0 x 6.0 mm are the standard in the transition(Fig. 72-A).
Nucleus Removal
There are many different techniques thatmay be utilized by advanced surgeons. Theywill be discussed in a separate chapter. For thetransition, the basic technique to use whenbeginning phaco is the "divide and conquer"into four quadrants. "Divide and conquer" isusually done with two hands (Fig. 56). Thesurgeon must also learn, however, how to per-form this technique with one hand.
SURGICAL TECHNIQUE IN THE TRANSITION
Anesthesia
During the transition it is advisable thatthe surgeon utilize the type of anesthesia withwhich he/she feels more safe and in bettercontrol (Figs. 33, 34). It is unnecessary to adda new source of stress or immediate change atthis stage of the procedure. Nevertheless, whenthe surgeon is in charge of the situation andmasters the phaco technique, it is ideal to usetopical anesthesia because of its ability to pro-vide immediate visual recovery. The com-bined use of topical anesthesia and intracam-eral anesthesia is more effective than topicalanesthesia alone and should be tried before thesurgeon attempts to operate using topical anes-thesia alone (Figs. 35, 36). I recommend that
you consult Chapter 5 on this important aspectof the operation.
The Incision
How to Make a Safe Transition fromLarge to Small Incision
Role of the Ancillary Incision
This is an important step in performingphacoemulsification. Although there are tech-niques to perform it with only one hand, phacois fundamentally a two-handed procedure.
The ancillary incision is made before themain incision is performed. As shown in

THE ART AND THE SCIENCE OF CATARACT SURGERY
98
Fig. 41, this incision serves as an entry for asecond instrument which is necessary for ma-neuvers to remove the nucleus (Fig. 56). Thiswound is also utilized in irrigation of theanterior chamber with intracameral local anes-thetic as explained in Chapter 5 and illustratedin Fig. 36, and for the insertion of viscoelasticprevious to making the main incision and dur-ing several other steps of the operation. How-ever, some advanced phaco surgeons do notperform hydrodelamination and remove theepinucleus usually during the emulsificationof the nucleus.
At the end of surgery, the ancillary inci-sion also serves to inject fluid into AC to test forleaks in the wound (Fig. 73).
The Main Incision
During the early stages of the transition,the surgeon should plan to start the operationas a phaco but learn how to convert to theplanned extracapsular he or she is accustomedto do successfully if this becomes necessary.This will provide additional comfort and con-
fidence. The surgeon may start with a smallstepped limbal valvulated incision slightlylarger than the phaco tip (Fig. 42) even thoughhe knows that he plans to convert to his usualplanned extracapsular. It is not advisable tostart the transition with a corneal incisionbecause, upon enlarging it, the resulting astig-matism may be severe. The more anteriorlylocated the incision, the more astigmatism thepatient may end up with. By starting thetransition with a limbal incision, the surgeonwill use the same area for the incision that he isaccustomed to use in his planned extracapsularbut will make the incision valvulated (stepped)and smaller than th e usual extracapsular(Figs. 40, 41, 42). The surgeon must master thetechnique of the small incision valve like inci-sion at the limbus, so that it can be part of hisarmamentarium in the future (Fig. 40-C). Oncethe surgeon is certain that he will not need toconvert from phaco to planned extracapsularand therefore will not need to enlarge the inci-sion, he may choose to make a corneal incisionif he wishes, but not before (Fig. 40-C). Thisis what we refer to as a safe transition from alarge to a small incision, a transition that must
Figure 40 A-C (See Facing Page 101): Phacoemulsification Incisions - Surgeon’s and Cross Section Views
Figure A - Limbal Incision (left, above and below): The incision of choice during the transition period and which may continueto be utilized successfully by the surgeon is a stepped limbal incision, slightly larger than the size of the phaco tip, (L-above left). Theincision is placed in this location so that if the surgeon feels uncomfortable with the surgery at any stage of the transition into phaco,the limbal incision may be extended to convert to ECCE in his/her first steps of transition without complications. The cross sectionview below, left, shows the stepped limbal tunnel incision, valvulated and self-sealing. Unless it is made larger, no suture may be neededor perhaps one suture. The three steps to make a valvulated incision starting at the limbus are the same than those shown in Fig. B belowfor the scleral tunnel incision, except that the length of point 2 in the second plane or tunnel is shorter.
Figure B - Scleral Tunnel Incision (center above and below): The scleral tunnel incision involves a three step entry into theanterior chamber creating a 5.5 mm long valvulated self-sealing wound. The first step (1) is a straight or “frown” shaped verticalgroove scleral incision at about 1.5 mm posterior to the limbus. The second plane of the incision (2) is dissected at constant depth (300

C h a p t e r 7: P repar ing f o r t he Trans i t i on
99
microns) toward and into the clear cornea for about 1 mm. The blade should be parallel to the iris plane. The third stepis a penetrating incision into the anterior chamber (3) with the blade obliquely to the iris plane. This type of incisionis no longer frequently used. It used to be the most popular incision, but then we learned that the self-sealing valvulatedaction of the incision is not related to the length of the tunnel outside of the cornea but within the cornea.
Figure C - Corneal Tunnel Sutureless Incision (above right): The 3.2 mm long corneal tunnel incision (C) alsocreates a valve which is self-sealing. As seen in the cross section (below right) a vertical groove (1) is made in the clearcornea followed by a second plane incision (2) approximately oblique to the iris plane. This corneal incision shouldnot be used in the transition period but can be used advantageously by more experienced surgeons whose ability toperform each step of phacoemulsification adequately practically assures that there will not be any need to convert toan ECCE. If a corneal incision as shown in (C) is made and the surgeon has to convert, the enlargement of the cornealincision to finish the operation as an extracapsular may lead to major astigmatism.
Figure A (limbal) and C (corneal tunnel) are either performed at 12 o'clock as shown in this plate orlocated in the superior right quadrant. This is preferred by many surgeons who feel that this location facilitatestheir surgical manipulations.

THE ART AND THE SCIENCE OF CATARACT SURGERY
100
Figure 41-A: Making the AncillaryIncision
This is a most important stage ofphacoemulsification since the operationitself is mainly a two-handed technique.The steps involved are: 1) First, mark thelimbal area (A) where the limbal steppedmain incision will be made (Figs. 41 Band 42) between 9 and 12. In thetransition it is recommended to place thestepped incision at 12 o'clock as shownhere. 2) Make the ancillary incision (I)always at 3 o'clock. This is performedwith a special 15 º blade designed forparacentesis (K). 3) Proceed to performthe limbal valvulated stepped incisionand enter the anterior chamber, as shownin Figs. 41-B and 42 (surgeon's views).The ancillary incision serves to intro-duce a second instrument as shown inFig. 67, inject intracameral local anes-thesia as shown in Fig. 36 and irrigateviscoelastic into the anterior chamber.
Figure 41 B: Initial Stages of Self-Sealing, Stepped, Valvulated TunnelIncision at the Limbus - Surgeon's View
This surgeon's view shows theCrescent knife blade (K) entering the firstincision (1) just at the limbus. The bladeis advanced (red arrow) for some distancein the plane of the cornea, and a tunnel(blue arrows) is created. This forms thesecond step (2) in the three-step incision.The knife does not enter the anterior cham-ber at this stage.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
101
be undertaken step by step as the surgeonprogresses in his learning curve (Figs. 40, 41,42).
Later, as he progresses and learns tomaster phacoemulsification, the surgeon isready to make two significant changes in thetechnique: 1) Operate from an oblique positionand make the incision in the upper right quad-rant, temporally as shown in Figs. 41-B and 42;2) Perform a corneal incision (Fig. 40-C) in-stead of a limbal incision (Figs. 40-A, 41-B, 42
Role of Conjunctival Flap
In the early stages of the transition, thesurgeon may prefer to start with a small fornixbased conjunctival flap from 10:00 to 2:00o'clock, and place light cautery under eachedge of the flap. If the limbal incision isextended because one of the initial phaco stepsbecomes a source of problem and there is needfor conversion to ECCE, there will be lessbleeding.
Figure 42: Final Step of Self-Sealing, Stepped, Valvulated Tunnel Incision atthe Limbus Performed with the Diamond Knife - Surgeon's View
A diamond knife blade (D) enters the first incision (1), the second tunnelincision (2), and is then directed slightly oblique to the iris plane and advanced(arrow) into the anterior chamber. This forms the internal aspect of the incision intothe chamber (A). This is the third sted (3) in the three-step self-sealing incision.

THE ART AND THE SCIENCE OF CATARACT SURGERY
102
Anterior Capsulorhexis
This again is a vital step in the transition.Changing from the can opener capsulotomy(Fig. 37) to the anterior continuous circularcapsulorhexis (CCC) is one of the fundamentalsteps in the transition (Figs. 43, 44, 45). Thesurgeon must learn first by practicingcapsulorhexis on the skin of a grape or by usinga very thin sheet of plastic wrap such as the onethat covers some chocolate candies. Once thesurgeon understands the concept of the tech-nique and can do it in the laboratory, he or shemay begin to use it for the patient.
The surgeon must keep in mind that thespace needed to adequately maneuver the cys-totome (Fig. 43) or the capsulorhexis forceps(Figs. 44, 45) in order to do a proper continu-
ous circular capsulorhexis is larger than thewound or paracentesis required to simply in-troduce a cystotome and perform a can openercapsulotomy.
It is highly recommended to make thecapsulorhexis under sufficient viscoelastic .The latter should be injected into the anteriorchamber as a first measure before trying thecapsulorhexis (Fig. 2). It is also fundamentalnot to begin with dense, hard cataracts whereit is difficult to see the edge of the capsulorhexis.It is prudent to try performing this procedureover and over again in cataracts that are lessdense until the surgeon is able to perform themin eyes with poor visualization of the edge ofthe capsule.
Because the surgeon, in the initial stagesthat we are discussing here, will most probably
Figure 43: Continuous Curvilinear AnteriorCapsulorhexis with Cystotome - Step 1
Anterior capsulorhexis is one of the stepsof phacoemulsification that is practically thesame both for the surgeon beginning with thetransition or the more advanced surgeon, withthe exception that some advanced surgeons pre-fer to do a smaller capsulorhexis. The techniqueshown here is the initial step performed with thecystotome-needle (see Fig. 97). In the transition,it is recommended that it be continued withforceps as shown in figures 44 and 45. With anirrigating cystotome, the center of the anteriorcapsule is punctured creating a horizontal V-shaped tear. The tear is extended toward theperiphery and continued circumferentially inthe direction of the arrow. In the surgeon'stransition stage, the cystotome is introducedthrough a 3.5 to 4.0 mm limbal incision. Theinitial puncture of the anterior capsule with thecystotome needle shown here as made in the midperiphery is the technique initially utilized bythe pioneers of capsulorhexis and is shown herein this form for historical reasons. The presentmethod has been modified to start the puncturein the center, as a frontal incision shown in Fig.98. This leads to better results and facilitates themaneuver.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
103
Figure 44 (above right):Continuous Curvilin-ear Anterior Capsulorhexis with Forceps-Step 2
After having made the initial tear of theanterior capsule with an irrigating cystotome inthe center of the anterior capsule, the tear is ex-tended toward the periphery in a circular direction,this time utilizing forceps as shown in this figure.The tear is extended toward the periphery andcontinues circumferentially in a continuous man-ner for the remaining 180 degrees, as initiallydescribed by Gimbel.
Figure 45 (below right): Continuous Curvilin-ear Anterior Capsulorhexis with Forceps -Step 3
The flap of the capsule is flipped over onitself. The forceps engage the underside of thecapsule. The tear is continued toward its radialsegment. In the transition, beginning surgeons areencouraged to use forceps as shown in figures 44and 45 in order to perform the continuous circularcapsulorhecis (CCC). Viscoelastic is essential inthis maneuver. The correct size of the CCC is 5.5mm to 6.0 mm. A larger CCC, would beundesirable because the nucleus may come out ofthe bag too quickly, forcing the surgeon to doemulsification in the anterior chamber which maylead to endothelial damage. For the early steps ofthe transition, when the surgeon may have toconvert to ECCE, it is important to perform tworelaxing incisions radially at 10 and 2 o'clock in theanterior capsule, in order to facilitate the removal ofthe complete nucleus in an ECCE if necessary.

THE ART AND THE SCIENCE OF CATARACT SURGERY
104
need to convert to ECCE, it is important that heperform two relaxing incisions radially in theanterior capsule at 10 and 12 o'clock followingthe CCC, in order to facilitate the removal ofthe complete nucleus with a planned manualextracapsular. If these relaxing incisions in theanterior capsule are not done, the surgeon mayconfront serious problems in removing thenucleus (Fig. 37).
Hydrodissection
Once the surgeon is able to perform acircular continuous capsulorhexis (CCC) with-out problems, he is ready to go into the nextstep, which is hydrodissection (Figs. 46, 47,48). This step should not be undertaken beforemastering the capsulorhexis. If not, tears in theanterior capsule may extend towards the equa-tor when performing the injection with fluid todo the hydrodissection. The surgeon shouldhave clearly in mind the anatomy of the crystal-line lens and what is it that he is after withhydrodissection (Fig. 1). With this maneuver,by using waves of liquid (Figs. 46, 47, 48) wewish to separate the anterior and posterior
capsules from the cortex (Figs. 46, 47) and thenucleus from the epinucleus (Fig. 48). Whenthis is achieved, the nucleus is liberated so thatit will be free for the ensuing maneuvers ofrotation, fracture and emulsification, all ofwhich will come as the next steps in theprocedure (Figs. 55, 56). As long as thesurgeon is not sure that the nucleus has beenfreed of its attachments through thehydrodissection and will rotate easily, he shouldnot proceed to try to rotate it mechanicallybecause this may lead to rupture of the zonules.Also, if the nucleus is not separated from thecortex by hydrodissection (Fig. 48), the sur-geon should not proceed to apply the phacoultrasound to the nucleus because he or shemay well meet with complications by extend-ing the effects of ultrasound not only to thenucleus but peripherally to the cortex. This canlead to the feared rupture of the posterior cap-sule. Instead, the surgeon should decide toconvert to a ECCE. Although Fig. 47 showshydrodissection through a corneal tunnel(surgeon's view), keep in mind that all maneu-vers during the transition are done with alimbal incision, as shown in Figs. 40 A, 41, 42.
Figure 46 : Hydrodissection - Stage 1- Separation of the Anterior and Pos-terior Capsule from the Cortex -Cross Section View
A 25 gauge cannula is placedthrough the continuous circularcapsulorhexis under the anterior lenscapsule (A). Fluid is infused asshown by the pink arrows in order toseparate the anterior capsule from thecortex. A wave of fluid shown by thepink arrows and identified as (W) ex-tends along the posterior capsule, sepa-rating the posterior capsule (P) fromcortex (C).

C h a p t e r 7: P repar ing f o r t he Trans i t i on
105
Figure 47 (above left): Hydrodissection ofthe Lens Capsule from the Cortex DuringPhacoemulsification - Surgeon's View
This is a surgeon's view of what isshown in figure 46 in cross section view.Following circular curvilinear anteriorcapsulorhexis, a cannula (C) is inserted into theanterior chamber. The cannula tip is placedbetween the anterior capsule and the lens cor-tex at the various locations shown in the ghostviews. BSS is injected at these locations (ar-rows) to separate the capsule from the cortex asshown in Fig. 46. The resultant fluid waves (W)can be seen against the red reflex. These wavescontinue posteriorly to separate the posteriorcapsule from the cortex.
Figure 48 (below right): Hydrodissection -Stage 2 - Separation of Nucleus and Epi-nucleus and the Cortex
In this stage, the cannula is advancedbeneath the cortex (C) and the infusion withBSS is started in order to separate the nucleus(N) from the epinucleus (E). The pink arrowsbetween these two structures, nucleus (N) andepinucleus (E), show the flow of fluid. Thegold "ring" of fluid separating the nucleusfrom the epinucleus is here identified as (GR).

THE ART AND THE SCIENCE OF CATARACT SURGERY
106
THE MECHANISM OF THEPHACO MACHINE
Getting Ready to Use PhacoDuring Transition
We have already emphasized the crucialimportance of understanding how the phacomachine works in order for the surgeon toperform phacoemulsification successfully. Thisis a task every cataract surgeon must undertakewhen contemplating the use of phaco in his/her
Figure 49-A: The Principles of How thePhaco Machine Works
This conceptual view shows the threemain elements of most phaco systems. (1)The irrigation (red): Intraocular pressure ismaintained and irrigation is provided by thebottle of balanced salt solution (B) connectedvia tubing to the phaco handpiece (F). It iscontrolled by the surgeon. Irrigation entersthe eye via an infusion port (H) located on theouter sleeve of the bi-tube phaco probe. Heightof the bottle above the eye is used to controlthe inflow pressure. (2) Aspiration (blue):(I) enters through the tip of the phaco probe,passes within the inner tube of the probe,travels through the aspiration tubing and iscontrolled by the surgeon by way of a vari-able speed pump (J). The peristaltic typepump is basically a motorized wheel exertingrotating external pressure on a portion of theflexible aspiration line which physicallyforces fluid through the tubing. Varying thespeed of the rotating pump controls rate ofaspiration. Aspirated fluid passes to a drain(L). (3) Ultrasonic energy (green) is pro-vided to the probe tip via a connection (M) tothe unit. All three of these main phacofunctions are under control of the surgeon byway of a multi-control foot pedal (N).
patients. It must be achieved first in anexperimental laboratory before attempting tooperate on humans with seeing eyes, as empha-sized by Centurion.
Optimal Use of the PhacoMachine
The Rationale Behind It -Main Functions
Edgardo Carreño, M.D., one of SouthAmerica's top phaco surgeons and teacher,describes the three main functions of the

C h a p t e r 7: P repar ing f o r t he Trans i t i on
107
Figure 49-B (previa Fig. 1-1, p.3 libro Seibel on Phacodynamics): The Rationale Behind the Phaco Machine
In this diagramatic figure from Seibel's excellent book on Phacodynamics, you can clearly observe the mechanicalworkings and rationale behind the function of the phaco machine, as explained in Fig. 49-A, its figure legend and the text.The ultrasound energy coming from the handpiece emulsifies the cataract (Fig. 50-B) so that a 10 mm cataract may beremoved by the aspiration port and line through a 3 mm or smaller incision. A fluidic circuit counteracts the heat build upcaused by the ultrasonic needle and removes the fragmented or "emulsified" lens material via the aspiration port andaspiration line while maintaining the anterior chamber. The fluid is supplied via the irrigation port and line by the elevatedirrigating bottle, which is controlled by the surgeon elevating it or lowering it. This fluid circuit is regulated by the aspirationpump. (After Seibel, B.S., Phacodynamics, 3rd Ed., 1999, p. 3, Slack, as modified by HIGHLIGHTS).
phaco machine: 1) irrigation; 2) aspiration;and 3) fragmentation of nucleus. This isclearly shown in Figs. 49-A and 49-B. Irri-gation is done with the irrigation bottle,aspiration with the aspiration pump andfragmentation with ultrasonic energythrough the titanium needle present in the
phaco tip of the hand piece (Figs. 50-A and50-B). Many types of phaco tip shapes havebeen created to more efficiently handlenuclear extraction, as shown in Fig. 51. Acommand pedal, which is controlled by thesurgeon’s foot, guides the machine into thefollowing four positions: 0 (zero) which is at

THE ART AND THE SCIENCE OF CATARACT SURGERY
108
�
�
� �
Figure 50 A (above left): The Phaco Handpiece
This diagramatic figure clearly shows thedifferent components of the phacoemulsificationhandpiece. The phaco needle is manufactured withvarious degrees of bevel, angulations and shapes, asshown in Fig. 51. The probe tip is hollow with thedistal opening functioning as the aspiration port.Irrigation fluid flows through two ports located180º apart on the silicone irrigation sleeve. Theirrigation sleeve hub shown here in blue threads thesleeve onto the handpiece body outer casing. Thephaco needle threads directly into the internal mecha-nism of the handpiece containing the ultrasoundgenerator. The ultrasound power oscillates be-tween 25.000 and 60.000 times a second (Hz). Thisenergy is transmitted along the handpiece into thephaco needle in such a way that the primary oscil-lation is axial.(After Seibel, B.S., Phacodynamics,3rd Ed., 1999, p. 99, Slack, as modified by HIGH-LIGHTS).
Figure 50 B (below right): Mechanism of Actionof Phacoemulsification Probe Tip
Phacoemulsification involves the use of aprobe tip (T) which vibrates very rapidly and actsas a jackhammer and emits heat to break up lensmaterial (L) into fragments (F). Fragments areaspirated from the eye via the center of this probetip which is hollow (black arrow). An outer sleeve(S) provides for passage of infusion fluid. Fluidenters the eye (white arrow) via infusion ports (P)in this outer sleeve. The infusion fluid constantlyreplaces any aspirate removed from the eye tomaintain a stable intraocular pressure.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
109
rest; position 1 for irrigation, position 2 forirrigation-aspiration and position 3 for irriga-tion, aspiration and phacoemulsification(Figs. 52 and 53).
The first function (irrigation) con-trolled by the foot pedal is provided by abottle with BSS. The liquid flows by gravity.The amount of liquid that reaches the anterior
Figure 51: New Phaco Tips
Many types of phaco tip shapes have been created in an attempt to moreefficiently handle nuclear extraction. Different types include various degrees ofbevel, angulations, and shapes of the tip. Examples include: A-straight round tip,B- 15º bevel, C-30º bevel, D-45º bevel, E-bent 45º tip, F-rectangular tip, G-enlarged bevel tip, and H-another enlarged bevel tip. The beveled tips provide anoval shaped aspiration opening with gradually increasing areas of contact (areasshown in blue) to nuclear material. Angled or bent tips attempt to allow accessof the tip to more peripheral locations within the capsular bag.
chamber depends on the height of the bottle,the diameter of the tubing and the pressurealready existing in the anterior chamber(Figs. 49-A, 49-B, 54). The flow rate into theeye is determined by the balance of thepressure in the tubing - regulated by theheight of the bottle, and the back pressure inthe anterior chamber. When the two are

THE ART AND THE SCIENCE OF CATARACT SURGERY
110
Figure 52 (above left): Basic Phaco FootPedal Functions
The foot pedal controls inflow, out-flow, and ultrasonic rates. With the footpedal in the undepressed position, the inflowvalve is closed, the outflow pump is station-ary, and there is no ultrasonic energy beingdelivered to the phaco tip. With initial de-pression of the pedal (1), the irrigation linefrom the raised infusion bottle is opened.Further depression of the pedal (2), startsand gradually increases the flow rate of theaspiration pump to a maximum amountpreset by the surgeon. Further depression ofthe pedal (3) turns on increasing ultrasonicpower to the phaco tip for lens fragmenta-tion.
Figure 53 (below right): New Dual Linear-Lateral Pedal Control
A new pedal control separates the in-flow-outflow and ultrasonic power functions.The inflow (1) - outflow (2) function is con-trolled by pedal depression, with increasingoutflow availability incurred with increasingpedal depression. Inflow will match outflowrates. Increasing ultrasonic power is applied bydoing a lateral rotation of the foot pedal (3). Thelateral rotation of the foot pedal (3) is shown inthe ghost view. Separating these functions al-lows the surgeon to apply varying amounts ofultrasonic power with varying inflow-outflowrates. With the depression only type pedal,ultrasonic power is only engaged with maxi-mum inflow and outflow. There arephacoemulsification maneuvers when this is notdesirable. A low inflow-outflow rate, for in-stance, may be desired when engagingultrasound.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
111
equal, there is no flow. If there is leakage oraspiration of fluid from the anterior chamber,the pressure there drops, and fluid in thetubing flows in to restore the pressure in theAC, and, indirectly thereby, the volume. Thetubing is purposely made wide enough so thatit impedes the flow of the BSS only slightlyunder normal rates of flow. It does limitmaximum flow - during anterior chambercollapse for example, unfortunately, however.
Figure 54: Irrigating Bottle Height Related to Flow Rate -Hydrostatic and Hydrodynamic Stages
Bottle height (C) has the important function of provid-ing constant chamber pressure during all phases of surgery,including during times of sudden changes in outflow rates.Maintenance of safe intraocular pressure is important in both"hydrostatic" (A - no fluid moving within the fluidic circuit)and "hydrodynamic" situations (B - fluid moving within thecircuit). A bottle height of 45cm above the eye will provide anapproximate 30mmHg of intraocular pressure (I) when nofluid is moving in the circuit (hydrostatic state A) when thereis no aspiration taking place and the aspiration pump (E) is off.When the aspiration pump (J-arrows) is turned on, (hydrody-namic state B), the intraocular pressure (M) will go down, forexample to 20mmHg, depending on the outflow rate. Arrowsdepict fluidic inflow (red) and outflow (blue) in the system.This is because the intraocular pressure decreases proportion-ally as the flow rate increases (Bernoulli's equation). Thereforeit is important to maintain a constant IOP, to increase the bottleheight when using a high phaco outflow rate. Likewise, thebottle height should decrease when the aspiration (outflow)rate is decreased. The black arrows on the tube (J) indicatesdrainage.

THE ART AND THE SCIENCE OF CATARACT SURGERY
112
The second function, which is aspira-tion, is provided by a pump, which creates adifference in pressure between the aspirationline and the anterior chamber. The pumpsmay be a peristaltic pump, a Venturi pump, adiaphragm pump, a rotary vane pump, or ascroll pump. The peristaltic pump hasbecome the most widely known and used.Many feel it is safer. Just like inflow, a baselevel of suction occurs whenever the pump isactivated, depending on how hard the pump isworking. When there is occlusion of the tipwith the foot pedal in the aspiration position(position 2), the pump will continue to pumpand crate more and more suction until thematerial which is provoking the occlusion isaspirated, or until the suction in the tubingreaches the maximum that the surgeon haspreset on the control panel (Figs. 59, 60, 61).This latency period before reaching maxi-mum suction level provides a greater securitymargin allowing the surgeon to take immedi-ate action in case the tip grasps (and sucks in)the iris or the posterior capsule instead ofgrasping the lens mass. In order to perceivewhat happens to the fluid dynamics when thephaco tip is not occluded, please see Figs. 57,58. The reason for limiting the maximumsuction pressure is to limit the rush of fluidout of the eye the moment the fragment whichoccluded the tip is aspirated. This providesthe surgeon the opportunity to stop aspirationand avoid collapse of the anterior chamber.
The third function of the phaco ma-chine - the production of ultrasonic vibra-tions leading to fragmentation of the lens -is carried out by a crystal transducer locatedin the handpiece, which transforms high fre-quency electrical energy into high (ultra-sonic) frequency mechanical energy. Thecrystal drives the titanium tip of the phacounit to oscillate in its anterior-posterior axis.
It is precisely the anteroposterior oscillationof the phaco tip which produces the emulsi-fication (Figs. 50-B, 55, 56, 67, 68).
Parameters of the Phaco Machine
What are the phacoemulsification ma-chine parameters? How are they utilized?These parameters need to be set and resetdepending on the type of cataract: soft,medium-hard, very hard, (as shown inFig. 2); the stage of the operation; and also,importantly, the various situations which thesurgeon must solve. These parameters are:
1) the amount of ultrasonic energyapplied to the nuclear material for its emulsi-fication. It is expressed as a percentage of thephaco machine’s available power and it deter-mines the turbulence which is generated inthe anterior chamber during surgery. It isideal to use the least amount of powerpossible during the operation. This is pos-sible by combining other functions of themachine and maneuvers within the nucleus tofacilitate fracture and emulsification of thelens. The use of excess phaco energy mayresult in damage to structures beyond thenucleus, such as the posterior capsule and theendothelium.
2) The aspiration flow rate. Thismeasures the amount of liquid aspirated fromthe anterior chamber per unit of time. Inpractical terms, this determines the speedwith which the lens material is sucked in intothe phaco tip. This is synonymous with thepower of "attraction" or suction of the lensfragments into the irrigation-aspiration hand-piece (Fig. 61). High maximum flow ratesmay result in collapse of the anterior chamberif the irrigation cannot keep up.
3) The third parameter measures thevacuum or negative pressure created in the

C h a p t e r 7: P repar ing f o r t he Trans i t i on
113
Figure 55: Varying Ultrasonic Settings While Proceeding Through a Nucleus of Varying Density During the Creation of aFurrow or Groove
Under surgeon control via the foot pedal, the ultrasonic power can be varied during creation of a trans nuclear groove toaccommodate the varying density of the nucleus encountered at each location. For example, when beginning the furrow (A) 30% poweris all that is required initially in the low density peripheral portion of the nucleus (P). Note slight depression (arrow) of the foot pedal(1) to obtain this power setting. As the phaco tip is progressed toward the central nucleus, ultrasonic power may be increased to 60%as it encounters more dense epinuclear material (E). Note increased foot pedal depression (arrow) to increase power (2). When the phacoenters the densest central portion of the nucleus (N), ultrasonic power may be increased up to 90-100% by further depression (arrow)of the foot pedal (3). As the phaco tip again encounters less dense material on the distal side of the nucleus near the epinucleus (E),ultrasonic power is again reduced to perhaps 60% to efficiently remove that material. The foot pedal depression is reduced to lowerthe power (4). Varying the power to just the minimum level required at each stage avoids excessive intraocular ultrasonic power,provides for a safer extraction, and avoids possible abrupt engagement of the tip with epinucleus and nearby the posterior capsule.

THE ART AND THE SCIENCE OF CATARACT SURGERY
114
aspiration line and actually determines theforce with which the material is fixated ontothe orifice in the phaco tip. This is known asfixation power or grasp and depends on theaspiration force (Figs. 59-60, 61). Thehigher the aspiration pressure, the more rapidthe aspiration flow, and the less the amountof time it takes to obtain the maximumvacuum power. If the occlusion at the tip isbroken or interrupted, due to the negativepressure in the aspiration line, fluid israpidly sucked out of the eye. This may leadto collapse of the anterior chamber with riskof damage to the corneal endothelium as wellas the posterior capsule. This is known as theSurge Phenomenon (Figs. 61-65).
How to Program the Machine forOptimal Use
We have already discussed the phaco-emulsificator’s settings which include the ul-trasonic power, the aspiration flow, which isthe power of attraction and the vacuum,which is the grasping power.
In order to perform a rational phaco,we must know how to program or calibratethe "memory" of the machine. There arethree memories in the machine. Memory 1 isfor sculpting the nucleus( Figs, 55, 56),Memory 2 is for fragmentation, mobilizationand emulsification of the nuclear fragments(Figs, 67, 68) and Memory 3 is for removalof the epinucleus, when this exists (Fig. 69).
In Memory 1: nuclear sculpting, weneed high ultrasound power with low flowand low vacuum since at this stage we do notneed any fixation or attraction power. InMemory 2: nuclear fragmentation, how-ever, we need low ultrasound or phaco power
in order to keep the nucleus fragments closeto the phaco tip and prevent the vibratingeffect from repelling the fragments from thetip opening. We need a higher flow of aspira-tion to bring the fragments of the nucleus tothe tip of the handpiece and make the proce-dure faster.. In this Memory 2, we also needhigher vacuum since here we need to havegood grasping power to hold the fragmentsagainst the phaco tip so that we can proceedto emulsify them. Memory 2 is the memoryfor fragment mobilization and emulsification.
In Memory 3: removal of epinucleus,all the parameters are lowered consideringthat the epinucleus is soft. Memory 3 isspecifically for the epinucleus, whenever itexists.
Fluid Dynamics During Phaco
Michael Blumenthal, M.D., has madeprofound studies on this most important sub-ject. Its understanding really makes a differ-ence between success and failure in smallincision cataract surgery, particularly in pha-coemulsification. There are two factorsspecifically involved: 1) the amount of in-flow and 2) the amount of outflow duringany given period of the surgery. Fluid dy-namics are responsible for the following in-traocular conditions during surgery: a) fluc-tuation in the anterior chamber depth; b)turbulence; c) intraocular pressure.
Blumenthal has pointed out numeroustimes that zero fluctuation is the target to beachieved in surgery, insuring that intraocularmanipulations are most effective and accu-rately performed as well as keeping steadyand natural the intraocular architectureand relationship between various tissues(Figs. 57-60).

C h a p t e r 7: P repar ing f o r t he Trans i t i on
115
Figure 56: Use of Different Phacomachine Parameters to Sculpt the Nucleus for Making Quadrants -Memory 1 - Divide and Conquer Technique
A linear vertical furrow is made in the nucleus from 6 to 12 o'clock. A second furrow in the lens is madeperpendicular to the first using the phacoemulsifier probe. The phaco probe (P) and manipulator (M) engageopposite sides of the furrow inferiorly. Force is applied with the instruments in opposing directions (arrows) tocrack (C) the nucleus along the length of the furrow. Additional manipulations of this type further lengthes anddeepens the crack. The lens is rotated 90 degrees within the capsular bag and a crack is made in the second furrowin the same manner (not shown). (The incision during transition should be limbal based. Corneal incision shownhere is for advanced surgeons.) The parameters of the machine used to create the furrows in the lens are shownin the figures within the rectangular table immediately above this figure. At this stage, the surgeon uses Memory1 which is shown digitally in the machine as 1. The digital figure under U.S. refers to the ultrasound power utilizedat this stage in order to create the furrows in the nucleus. ASP refers to the aspiration flow rate, and the VACshown on the machine refers to the amount of vacuum. These parameters are identified in the rectangle next toFig. 56.
By cracking the lens furrows at their base, the surgeon creates four separate quadrants of nuclear material.Manipulation of each quadrant for individual removal is carefully guided by use of flow and vacuum. Flow is usedto move a quadrant to the phaco tip (P). Once engaged, vacuum is used to impale and manipulate the quadrantfor safe removal.

THE ART AND THE SCIENCE OF CATARACT SURGERY
116
Fluctuation in the anterior chamberdepth is the consequence of the followingconditions: the amount of outflow exceedsthe amount of inflow in a given period. As aresult, the anterior chamber is reduced indepth or collapses (Figs. 62 and 63). Whenthe amount of outflow is reduced below theamount of inflow, the anterior chamber depthis recovered (Fig. 65). This phenomenon,when repeating itself, increases fluctuation.When fluctuation occurs abruptly, as in thesudden release of blockage of the phaco tip inaspiration, this is called Surge (Figs. 61-65).
Fluidics and Physics ofPhacoemulsification
Barry S. Seibel, M.D., in his classicbook Phacodynamics, presents perhaps the
most complete study on the physics on pha-coemulsification and the fluid dynamics in-volved. This must reading for anyone whowants to delve more deeply into this subject.
Seibel points out that phacoemulsifica-tion surgery is essentially the integration oftwo basic elements: 1) you use ultrasoundenergy in order to emulsify the nucleus; 2)you utilize a fluidic circuit in order to removethe emulsified material through a small inci-sion while maintaining the anterior chamberdepth integrity. This fluidic circuit is pro-vided by an elevated bottle of BSS thatproduces not only the volume of fluid withinthe circuit but also provides the pressure inorder to maintain the anterior chamber hydro-dynamically and hydrostatically. When out-flow and inflow are balanced, the pressure ofthe anterior chamber is proportional to theheight of the bottle (Figs. 49-A, 49-B).
Figure 57 : Fluid Dynamics - Balanceof Flow When the Phaco Tip IsUnoccluded - Hydrodynamic Bal-anced System
When the phaco tip isunoccluded (D), the outflow rate offluid from the eye (blue arrows) isdetermined by the rate (G) of pumpingaction of the peristaltic pump (F) undersurgeon control. In the unoccluded"hydrodynamic" balanced system, in-flow (red arrows) from the infusionbottle (B) will replace (C) the aspiratedfluid at the same rate, to maintain theconstant intraocular pressure deter-mined by the height of the bottle abovethe eye. In this unoccluded case, therates of inflow and outflow are equal.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
117
This fluidic circuit is regu-lated by a pump which not onlywashes the emulsified substancesbut also provides a highly usefulclinical purpose. When the tip ofthe phaco handpiece is not oc-cluded, the pump produces certaincurrents within the anterior cham-ber, which are measured in millili-ters per minute, which are respon-sible for attracting the nuclear frag-ments towards the phaco tip. Whena fragment completely occludes thephaco tip, the pump provides avacuum which is measured in mmHg, which holds the fragmentsfirmly against the phaco tip (Figs.57-60).
There are two main types ofpumps utilized during phaco: TheFlow pump and the Vacuum pump.The Flow pump, responsible for the directcontrol of flow, physically regulates the fluidwithin the aspiration line by direct contactbetween the fluid and the mechanism of thepump. Even though the scroll pump is thelatest type of flow pump, the one traditionallyknown as the peristaltic pump is the morecommonly utilized. One of its importantcharacteristic is the capacity to control theflow of fluid as well as the vacuum. Thisallows the aspiration flow to be independentof the height of the bottle of fluid. Neverthe-less, it is dependent on the degree of occlu-sion of the phaco tip. Aspiration flowdiminishes when the degree of occlusion atthe phaco tip increases and aspiration stopscompletely when the occlusion at the phacotip is total (Figs. 59, 60).
These pumps have in common adrainage cassette adapted to the aspirationline. The pumps are connected to the cassetteand produce a suction which in turn propor-
Figure 58: Fluid Dynamics - Balance of Inflow andOutflow During Phacoemulsification - TipUnoccluded - Hydrodynamic Balanced System
This view is a close-up complement of what isillustrated in Fig. 57. The anterior chamber duringphacoemulsification is a closed system in which thereis both intake and output of liquid and where the pressuremust be controlled. With nothing occluding the tip of thephaco handpiece (P), vacuum pressure is zero (tablepoint 1), At this point, the inflow (green arrow) equalsthe outflow (red arrow) of the phacoemulsification probe,and the pressure in the eye is maintained and constant(table levels 2 and 3).
tionally regulates the flow of aspiration whenthe port of aspiration is not occluded. Whenthe port of aspiration is occluded, the flowceases and the suction is transferred to thecassette by means of the aspiration line to theoccluded tip (Figs. 57-60).

THE ART AND THE SCIENCE OF CATARACT SURGERY
118
Figure 59 (above left): Fluid Dynamics - Balan-ce of Flow When the Phaco Tip Is Occludedwith Lens Material - Hydrostatic Closed System
When a piece of nuclear material (N) isdrawn to and blocks (occludes) the aspiration portof the phaco tip, fluid balance is still maintainedwithin the eye. Although the pump (F) is stillrunning, it can no longer providing fluid outflow(D) because the system is blocked, but it is nowproviding vacuum pressure, holding the occlud-ing fragment. In the balanced "hydrostatic" closedsystem, inflow (C) ceases at the same time since itnow has nowhere to move. Controlled intraocularpressure is maintained via the inflow line to thelevel determined by the height of the bottle (B)above the eye. Equal zero rates of inflow andoutflow is revealed by no drainage (G) from theoccluded yet balanced system.
Figure 60 (below right): Fluid Dynamics -Balance of Inflow and Outflow DuringPhacoemulsification - Tip Occluded With LensMaterial - Hydrostatic Closed System
This view is a close-up complement of thefluid dynamics shown in Fig. 59. When the tip ofthe phacoemulsification probe is occluded withnuclear material (L), the vacuum pressure rises toa level to which the machine is set (table - arrow- 1), and the inflow and outflow rates go down(table 2 and 3 - green and red arrows). With theaspiration port occluded, no fluid can enter or exitthe eye.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
119
Importance of and Understand-ing the Surge Phenomenon
The Surge phenomenon occurs when afragment of nuclear material is suddenly dis-placed from occlusion through the aspirationtip at the handpiece of the phaco machine,
thereby giving rise to a sudden elevation ofthe output of fluid from the anterior chamber(Fig. 61). The output of fluid suddenlybecomes larger than the input of fluid. Thisdifferential results in sudden collapse of theanterior chamber and can lead to seriouscomplications (Figs. 62, 63).
Figure 61: Mechanism of theUndesirable Surge Phenomenon
One problem area of theclosed phaco system occurs dur-ing abrupt dislodging of an oc-cluding piece of lens material soothat it no longer occluds theaspiration port of the phaco tip. Asudden drop in intraocular pres-sure occurs as the fluid rate intothe eye fails to immediately matchthe sudden fluid rate out of the eye.This is known as the Surge Phe-nomenon. (A) Shows a piece oflens material occluding the aspira-tion port of the phaco tip and isheld in place by vacuum pressurecreated by the operating pump (D).(Note there is no drainage (E) fromthe blocked system.) Infusion fromthe irrigating bottle (C) has ceased,but is still providing controlledintraocular pressure due to its el-evated position above the eye.With sufficient vacuum pressurefrom the pump and/or emulsifica-tion from the ultrasonic energy,the nuclear piece will abruptlyenter the aspiration port and thefluid system will once again open(B). Because the plastic infusion/aspiration lines and the eye wallsare flexible in absorbing the sud-den inflow-outflow pressure dif-ferential, there occurs a momentwhen the infusion fluid (G-smallarrow) does not effectively enterthe eye fast enough to replace the fluid suddenly moving out of the unblocked system (F-large arrow). Outflow rate fromthe force of the pump is momentarily greater than the replacing infusion rate. This out of balance system (out of balancein not providing constant intraocular pressure) in which the eye momentarily absorbs the inflow/outflow rate differential,may traumatically collapse the eye for a short period. (See Figs. 62 and 63).

THE ART AND THE SCIENCE OF CATARACT SURGERY
120
Figure 62 (above left): Physical ProblemsCaused by Surge
During the Surge Phenomenon when anuclear piece (F) is abruptly aspirated from theeye, the anterior chamber may collapse due toa sudden loss of intraocular fluid. The cornea(C) may cave in, resulting in possible endothe-lial cell damage if it comes near the phacoprobe. The posterior capsule (D) may also bedamaged from anterior displacement towardthe instrument. The fluid outflow rate must bebrought under control, and the inflow rate (smallred arrow) and outflow rate (large blue arrow)are again equalized with the eye repressurized,to reestablish a balanced system with constant,controlled intraocular pressure is not maintained.
Figure 63 (below right): Problem of SurgeDuring Phacoemulsification
This view is a close-up complement ofwhat is shown in Figs. 61 and 62 and explainedin their respective figure legends. Here weperceive more clearly the complications withinthe eye caused by the outflow surgephenomenon. Surge may occur after afragmented piece of lens nuclear material issuddenly no longer occluding the aspirationport. Aspiration occurs abruptly and the vacuumusually goes to 0 (table point 1 - blue arrow).This sudden aspiration of too much liquid fromthe eye (large red arrow within the a.c.) isgreater than the rate at which the inflow canreplace the liquid aspirated (small green arrowin phaco probe). Notice that the table showsthe outflow rate is large at this stage (table -point 3 red cube and arrow) and the inflow rate(table - point 2 green cube and arrow) has notcaught up with it. This differential causes theposterior capsule to move forward (E) and thecorneal endothelium to move inward (D), whichcan result in severe complications.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
121
When the phaco tip is not occluded,excess vacuum is zero (0), (Fig. 58) but theflow of aspiration is very high with a largequantity of flow going in and out from theanterior chamber. Note the distinction be-tween the normal suction, or vacuum, pres-sure which always exists in Positions 2 & 3,and which must exist to produce the normalaspiration flow we speak of, with the extra"vacuum" pressure which builds up whenthere is tip occlusion. When the phaco tip isoccluded with nuclear material, the outflowof fluid stops and the vacuum rises to themaximum level to which the machine wasoriginally calibrated and which we previouslydescribed (Fig. 60). This high vacuum aidsthe rapid emulsification of the nuclear frag-ment with or without ultrasound. When thereis much more sudden outflow of fluid from
the anterior chamber than the inflow, thechamber collapses with possible rupture ofthe posterior capsule and damage to the en-dothelium (Figs. 61-65).
Lessening IntraoperativeComplications from the Surge
As emphasized by Centurion, the latestgeneration of phacoemulsification machinesmake surge control possible (Figs. 64, 65).With these machines it is possible to workwith a high vacuum of more than 300 mmwhile maintaining a steady flow rate. Whenthe last part of the nuclear material goesthrough the phaco tip, a sensor located at theaspiration line signals a micro processor toslow the rate of the pump. Sometimes there issome reflux in the process of maintaining the
Figure 64: Technical Solution to Preventthe Undesirable Surge Phenomenon
One technical solution for eliminat-ing the surge phenomenon involves the useof a high-tech microprocessor. (Fig. A)When a nuclear piece (F) occludes the aspi-ration port and then suddenly (B) is aspi-rated (F-arrow) by the vacuum pressure ofthe pump (P), a sensor (E) located on theaspiration line signals a microprocessor (G)in the unit that an abrupt surge in aspirationflow has begun to take place. Within milli-seconds, the microprocessor directs the motorof the pump (P) to slow down. The reduc-tion in aspiration rate resulting from theslowed pump occurs before the eye cancollapse from any volume differential en-countered between sudden inflow and out-flow rates. The potentially dangerous surgephenomenon is avoided. This eliminationof the surge phenomenon allows the surgeonto safely use higher vacuum rates (necessaryin some situations) with a reduction in theneed to use potentially damaging high ultra-sonic power settings. Surgery becomes saferand faster.

THE ART AND THE SCIENCE OF CATARACT SURGERY
122
same intraocular pressure. This high speedmechanism insures that the pressure is alwaysthe same inside the eye.
As emphasized by Barry Seibel, thesurge phenomenon occurs in positions 2 or 3of the foot pedal when a nuclear fragmenttotally occludes totally the phaco tip.Vacuum builds up in the aspiration line, thelens material is emulsified sufficiently so thatit is quickly drawn within the phaco tip, theocclusion is broken, and there is a suddensurge of aspiration, emptying the anteriorchamber.
The surge phenomenon is more of aconcern when you utilize a conventional tipwith the 0.9 port with high vacuum and flowof aspiration. It is less of a problem when youutilize the irrigation-aspiration tip with thesmaller opening (0.3 mm). In addition, it ispossible to diminish the propensity for surgeduring phaco by utilizing a more resistanttype of tip such as the Microflow or theMicroseal or with the systems ABS which wedescribe in Chapter 8, (Fig. 84).
Figure 65: Advances in Equipment Technology to Prevent the Surge During Phaco
This is a close-up view of the anterior segment showing what is illustrated and explained in Fig. 64 and its figure legend. Thelatest generation of phacoemulsification machines make surge control possible. During the problem period when the last part of thenuclear material is aspirated through the phaco tip, a sensor signals a microprocessor to slow the rate of the vacuum pump. As aconsequence, when the nuclear material no longer occludes the phaco tip and the sensor detects that the vacuum pressure is droppingsuddenly (table point 1 blue arrow and block), the sensor instantly sends a signal to the pump to slow the outflow rate (broken red arrownext to phaco tip). The outflow rate (table point 3 - broken red arrow and block) is thereby moderated to allow the inflow rate timeto catch up (table point 2 green arrow and block ). This control of the pump action allows inflow and outflow rates increase togetherin a more equal fashion during this moment of potential negative surge. This makes surgery much safer, quicker and easier.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
123
NUCLEUS REMOVALAPPLICATION OF PHACO
FRACTURE AND EMULSIFICATION
This is really when the surgeon begins toutilize the ultrasound energy in the phacomachine and apply it within the patient's eye.During the transition period, this is a step thatshould be preceded by a good number of hoursof practice in the experimental laboratory untilthe surgeon is confident in the application ofthe ultrasound energy. It implies that he or she
has been able to successfully perform all theprevious steps over and over again in differentpatients. This experience will serve the sur-geon as the requisite basis for success in theemulsification and removal of the nucleus inthe present patient.
In removing the nucleus the surgeon firstattempts to divide the nucleus by fragmentingit into smaller portions that in due time willthen be emulsified individually (Figs. 55, 56,66, 67, 68). If the fracture or division of thenucleus has been incomplete and has resultedin large pieces or incomplete fractures, thesurgeon will not be able to perform the pha-
Figure 66: The Role of Cavitation inBreaking the Cataract Inside the Bag
There are two forces involved inemulsifying a cataract. One is themechanical force of the ultrasound asshown in Figs. 55 and 56 and explained intheir respective figure legends; and 2.) themechanism of cavitation. The magnifiedsection of cataract presented here showsthat as the phaco tip makes its tinyultrasonic movements, the energy releasesbubbles (B) inside the nucleus creatingcavities (C). The build-up of bubbles insidethe nucleus creates new hollow spaces (C)in the lens structure, the phenomenon ofcavitation. This cavitation facilitates thebreak-up and destruction of the cataract.
Some of the new phaco tips asshown in Fig. 51 are designed to producemore cavitation. The one shown in thisfigure is one of the best, designed byKelman for the Alcon phaco machines. Ithas a very thin tip with a 30 degree bend.It is particularly effective in hard nucleibecause of its enhanced cavitation.

THE ART AND THE SCIENCE OF CATARACT SURGERY
124
coemulsification successfully or he will needto use so much ultrasound energy that theremay be endothelial damage. Present tech-niques of phacoemulsification are preciselygeared to avoiding the use of large amounts ofultrasound energy.
There are different techniques for thefracture of the nucleus. In the end, the surgeonwill decide which one he prefers or feels moresecure with. Often, it depends on the type andmaturity of the cataract. At this stage of thetransition, when the surgeon is only beginningin his experience in fracturing and dividing thelens to apply the ultrasound, the most recom-mended procedure is to divide it into fourquadrants, the well known "divide and con-quer" first presented by Gimbel (Fig. 56).Later, the surgeon will be able to utilize othermodern techniques which also use high vacuumand low phaco but which may be too difficultin the transition.
At this stage of division or fracturing ofthe lens in the transition, it is recommendedthat the surgeon use Memory 1 of the phacomachine (Fig. 56) which implies a discretelyhigh amount of ultrasound, low or no vacuum,low aspiration and the conventional height ofthe bottle (65-72 cms).
The Divide and Conquer Technique
In the "divide and conquer" technique,the phacoemulsification instrument is used tocreate a deep tunnel in the center or the upperpart of the nucleus. The nucleus is split intohalves, sometimes fourths, and even occasion-ally into eighths. Splitting the nucleus is saferfor the endothelium and easier to learn, espe-cially for the less experienced ophthalmologistconverting from planned extracapsular surgeryto phacoemulsification. It is easier to keepsmaller particles away from the endothelium
without having to push them against the poste-rior capsule than it is to emulsify a large,cumbersome nucleus.
The nuclear fracturing techniques devel-oped by Gimbel are in part possible because ofthe CCC (capsulorhexis) technique that Gimbeland Neuhann originated. The mechanicalfracturing of the lens causes extra physicalstress within the capsule, and that cannot bedone without great risks of tears extendingaround posteriorly unless you have a properCCC. There is almost an interdependence ofthese two methods. The fracturing techniqueshave not only provided more efficiency inphacoemulsification in routine cases; they havealso made phacoemulsification in difficultcases safer and more feasible.
Gimbel clarifies that not only are therelamellar cleavage planes corresponding to thedifferent zones of the lens, but also there areradial fault lines corresponding to the radialorientation of the fibers, as first described byDrews. Until the development of these nuclearfracturing techniques we had not taken advan-tage of this construction (Figs. 55,56,67,68).The lens fractures quite readily in radial or pie-shaped segments (Fig. 67). To accomplish thisradial fracturing, the surgeon must sculpt deeplyinto the center of the nucleus and push out-wards (Fig. 56). Sculpting is used to create atrench or trough in the nucleus. Then thesurrounding part is divided into twohemisections. The separation must occur in thethickest area of the lens located at the center ofthe nucleus (Figs. 103 and 104).
An additional consideration with thesetypes of nuclear fractures is whether the seg-ments should be left in place until all thefracturing is complete or whether they shouldbe broken off and emulsified as soon as they areseparated. With a lax capsule and particularlywith a dense, or brunescent nucleus (Fig. 2),

C h a p t e r 7: P repar ing f o r t he Trans i t i on
125
Fig. 68 (below right): Emulsificationof Lens Fragments
In this cross-section view youcan see the loose quadrants ready foremulsification by phaco as illustratedthrough a surgeon's view in Fig. 67.Here you see a viscoelastic (V) beinginjected via a cannula (C) into thecleavage created by hydrodissection ofthe posterior nucleus from the posteriorcortex and epinucleus as shown in Fig.47 (blue arrow). The "viscoelastic sand-wich" helps protect the posteriorcapsule to prevent its rupture when thenucleus is undergoing manipulation andemulsification. Note viscoelastic liquidfilling the anterior chamber (blue arrow).The parameters of the phaco machineat this stage of emulsification of lensquadrants with aspiration-fragmentation of the nucleus are shownwithin the rectangular table immediatelyabove this figure. Memory 2 is showndigitally in the machine and by sound as2. U.S. refers to the ultrasound powerused. ASP is identified as the flow rate and VAC as the amount of vacuum, all specifically at this stage.
Figure 67 (above left): Emulsification of LensFragments
This surgeon's view shows themanagement of the lens quadrants. The apex ofeach of the four loose quadrants is lifted, theultrasound phaco tip is embedded into the poste-rior edge of each and by means of aspiration thesurgeon centralizes each quadrant foremulsification.

THE ART AND THE SCIENCE OF CATARACT SURGERY
126
Gimbel considers that it is safer to leave thesegments in place to keep the posterior capsuleprotected. The segments are easier to fractureif they are held loosely in place by the rest ofthe already fractured segments still in the bag(Fig. 105).
Emulsification of the NuclearFragments
If the surgeon has been successful in thefragmentation of the nucleus, the next step is toemulsify the pieces of segments of the dividednucleus. He may do this with the linear con-tinuous mode or with the pulse mode. Thelatter done during the transition provides moresecurity for the surgeon and allows him to useless ultrasound which is the definite tendencyat present.
The surgeon may later slowly begin toutilize other more specialized techniques knownas the different "chop" techniques which wewill discuss later. These techniques facilitatemuch more the emulsification of the segmentsor pieces of the fractured nucleus than thedivide and conquer but they are a little morecomplex. During this step of emulsification ofthe nuclear fragments, the surgeon may useMemory 2 in the machine which delivers lowultrasound, high vacuum, and a larger flow ofaspiration, with a conventional height of thebottle of fluid (Figs. 67, 68).
FINAL STEPS
Aspiration of the Epinucleus
It is during this specific step that there isa higher incidence of rupture of the posteriorcapsule for the surgeon in the period of transi-
tion. This is due to his lack of familiarity withhandling large fragments of epinucleus andcortex since in the planned extracapsular ex-traction he is accustomed to remove a large andcomplete nucleus that includes all the epi-nucleus and a significant amount of cortex.During the transition, the surgeon has to man-age safely the irrigation-aspiration handpiece.Later, when he masters the technique, he mayaspirate the epinucleus and cortex by maintain-ing the aspiration with the tip of the phacohandpiece. For this stage of the aspiration ofthe epinucleus, the surgeon will use Memory 3which means very low or no ultrasound power,a moderate to high vacuum, and high flow ofaspiration, with the bottle of fluid maintained atthe conventional height (Fig. 69).
Aspiration of the Cortex
This step is closely related to the previ-ous one (Figs. 70, 71). There can also be alarger incidence of posterior capsule ruptureduring this stage since the surgeon does nothave the epinucleus as a barrier which up to afew seconds before was protecting the poste-rior capsule. The surgeon should use a largerquantity of viscoelastic whenever required withthe purpose of protecting the posterior capsule.During the transition period, he may help hismaneuvers by using the Simcoe cannula withwhich the planned extracapsular surgeon usu-ally feels safe. This cannula may be introducedthrough the ancillary incision. The Simcoecannula has the disadvantage, though, that theaspiration hole or aperture is smaller than thatof the irrigation-aspiration handpiece of thephaco machine. Consequently, the aspirationof the masses of cortex may become moredifficult and slow. During this stage, the sur-

C h a p t e r 7: P repar ing f o r t he Trans i t i on
127
Figure 69 (right): Epinucleus Removal
Once the nucleus has been extracted,similar flow and vacuum presets are used toremove the epinucleus. Moderated control offlow, then vacuum are essential to a successfuland safe removal as identified in the parametersabove this figure. Higher flow and vacuumrate are inappropriate for engaging theepinucleus located so close to the posteriorcapsule (R) and iris. Too low a flow andvacuum will fail to engage the epinucleus. Amoderate flow rate is used to draw (arrow) thedistal epinucleus (C) to the phaco tip (P) withoutpulling in the capsule or iris. Once the phacohas engaged the epinucleus, moderate vacuumis used to maintain its grip on the epinucleus toremove it as a whole, as centrally in the pupilas possible. Too high a vacuum may abruptlybreak away a piece of the epinucleus andpenetrate the epinuclear bowl and threaten theposterior capsule beneath. Too low a vacuumsetting during removal may lose its grip on theepinucleus and lengthens surgery. During thetransition stage, use a limbal incision. Thecorneal incision in this figure is for experiencedsurgeons. During epinuclear removal useMemory 3, as shown.
Figure 70 (left): Phacoemulsification - Re-moval of Residual Cortex in Transition
The ultrasound tip is exchanged for anirrigation-aspiration tip (I/A), which is smallerand finer than the ultrasound tip. The anterior edgeof cortex is engaged at the 6 o’clock position. Theinstrument peels cortex from the posterior capsuleand removes it using the Memory 4 setting. Theparameters are shown in the rectangle above thisfigure. Please observe that the vacuum is signifi-cantly increased and the aspiration and flow rateare moderately higher than the step shown in Fig.69.
This figure shows (for didactic purposes) alarger amount of cortex than the experienced sur-geon has to deal with. This mass of cortex is whatmay be seen during the transition phase which isthe step of the operation we discuss in this chapter.
The experienced surgeon performs a moreeffective hydrodissection and frequently does notneed to perform irrigation/aspiration because littlecortex remains. He/she remove the epinucleususually during the emulsification process.

THE ART AND THE SCIENCE OF CATARACT SURGERY
128
geon should use Memory 4 in the setting of themachine which means zero phaco power, maxi-mum vacuum and the highest flow of aspira-tion as compared with all the previously men-tioned memories. The fluid bottle is main-tained at the conventional height.
Intraocular Lens Implantation
For the surgeon in the stage of transition,it is advisable to begin by implanting PMMAIOLs either of the ovoid shape (Fig. 72-A) orwith round optics of a fairly small diameter.The ovoid 5 x 6 lens shown in Fig. 72-A is justright.
Enlarging the Incision and Im-planting the Lens
In order to accomplish this the surgeon needs toextend the small incision with which he started,
to 5.2 mm. A 5.2 mm knife blade will do thismost accurately. In extending the arc of theincision, the surgeon must maintain the valve-like, auto-sealing characteristics present in theoriginal small incision. The PMMA IOL im-plantation is performed as shown in Fig. 72-B.After this stage has been mastered, the surgeonmay then change to implantation of the fold-able lenses but this must be done only after thesurgeon is completely satisfied with his phacotechnique.
Removal of Viscoelastic
Throughout the different stages of thisprocedure, the presence of viscoelastic in theanterior chamber is always a measure to keepin mind in order to prevent or minimize damageto the surrounding structures during surgicalmaneuvers, particularly the corneal endothe-lium. When removing viscoelastic from theanterior chamber, the phaco machine must be
Figure 71: Phacoemulsification - Irrigation/Aspiration of Residual Cortex
Residual cortex (C) is removed from thecapsular bag using curved Irrigation/Aspirationprobes. A slightly curved tip is used to gentlyaspirate residual cortex nasally and temporally.Residual cortex located in the hard-to-reach as-pects of the superior capsular bag are reachedwith a very curved I/A probe tip. The machineparameters used at this stage are shown with Fig.70, and correspond to Memory 4. The cornealincision shown here is for surgeons experiencedenough that no conversion to extracapsular isexpected. For surgeons in their transition period,a limbal incision is more prudent.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
129
in zero phaco or ultrasound, high vacuum, verylow aspiration and the bottle of fluid should besignificantly lower. After all the surgical stepshave been accomplished, it is important, as weall know, to remove the viscoelastic in order toavoid a high intraocular pressure postopera-tively, with subsequent corneal edema, blurredvision and pain during the first postoperativedays.
Even though this measure of removingall the viscoelastic has been emphasized overand over again in lectures and published pa-pers, there are still surgeons who are not fullyaware of the importance of taking this step andthe consequent complications.
Closure of the Wound
If a good incision has been made, valve-like, auto-sealing and waterproof, no suturewill be absolutely necessary even in thosecases where the wound has been extended to anarc of 5.2 mm for the PMMA IOL implantationas shown in Figs. 72-A and B. As long as thesetwo requisites are met, that is, extending theincision to 5.2 mm with a special knife blade ofthat size and maintaining a valve-like, auto-sealing incision, there is little danger of com-plications without sutures. Nevertheless, ifthe surgeon is not sure he has made a valvulated
Figure 72 A: The Ovoid PMMA IOL forImplantation During the Transition
During the transition period, the limbalincision is enlarged to 5.5 mm size and a 5 x6 mm ovoid PMMA lens (Fig. 72-A) isimplanted through this incision. The opticalzone should not be smaller.

THE ART AND THE SCIENCE OF CATARACT SURGERY
130
incision from the beginning (3 steps -Fig. 40-A and 42 A-B), even a 3 mm incisionwith no sutures will leak. If so, to leave thepatient without any sutures would be to take anunnecessary risk. It is more prudent to placetwo or three 10-0 nylon sutures in the woundand they may be removed early in the postop-erative stage. This decision really depends onthe ability of the surgeon to create a valve-like,self sealing incision.
What to Do if Necessary to Convert
When the surgeon decides to convertfrom phaco to extracapsular,, viscoelastic isplaced in the anterior chamber. The incision is
enlarged to one side and 2 or 3 sutures areplaced (pre or post placed). The incision iscompleted to the other side and 2 or 3 moresutures are put in place (pre or post placed ).The two superior sutures are placed at eitherend of the "valve incision", so that irrigation-aspiration (I + A) can be performed unhin-dered at that site. These two sutures are tiedwith a slip knot prior to I & A, and thenloosened to place the IOL. The other suturesare tied and knots buried before I & A. At theend of the operation an additional suture canbe placed if the incision is not secure. Toreduce risks, the surgeon may preplace the 310-0 nylon sutures across a grove on each sidefirst, before enlarging the incision.
Figure 72 B: PMMA IOL Implantation inTransition Period
Before implanting the PMMA IOL,the surgeon should irrigate, with machineparameters of U.S. zero power, ASP 50 andVAC 500. After irrigation, the surgeon intro-duces viscoelastic in the A.C. and bag beforeIOL implantation. Lubricate the lips of theincision with viscoelastic first. The use offoldable IOL's introduced through a clearcorneal incision is a goal to be tried and attainedlater, when the surgeon feels more comfortablewith his surgical technique.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
131
Testing the Wound for Leakage
Before considering that the surgery isover, it is important to be sure that no leakageexists either through the main incision orthrough an ancillary incision, under the micro-scope. This is done by cleaning and drying theincision with a Weck-cell sponge, removingthe viscoelastic and slightly overfilling theanterior chamber with BSS after the viscoelas-tic is removed and exerting mild pressure overthe cornea with the sponge (Fig. 73) or usingfine forceps to lightly "dance on" the cornea.At this time one can observe if there is anywound leak (Fig. 73). If the surgeon finds thatthere is a leak, the best way to solve it is byinjecting BSS into the lips of the incision tohydrate the tissues and force the incision closed.This works even better for the small ancillary
incision. The small conjunctival flap is thenadvanced over the incision.
Immediate PostoperativeManagement
After instilling antibiotic ointment andtopical antiinflammatory drops, the eye may bepatched if local anesthesia such as retrobulbar,peribulbar or sub-Tenon's were used. If onlytopical anesthesia or topical combined withintracameral irrigation anesthesia was used(Figs, 35, 36), you may leave the patient with-out any patch. This facilitates the postopera-tive use of antiinflammatory drops by thepatient.
The use of subconjunctival or parabul-bar injection of antibiotics and steroids imme-diately following surgery, is no longer acceptedas necessary, as was outlined in Chapter 4.
Figure 73: Evaluation of Leak ProofIncision
This figure shows the surgeonchecking to test if the incision is really leakproof, by doing the following: 1) after dryingthe lips of the incision, exhert light pressureover the cornea with Weck sponge. The"shadow" image represents the spongedelicately "dancing" over the cornea. Lookfor any fluid escaping through the wound.2) inject fluid through the paracentesis andobserve if any drops of fluid come out throughthe previous incision. If a leak is found, thesurgeon must suture the wound.

THE ART AND THE SCIENCE OF CATARACT SURGERY
132
RECOMMENDED READINGS
Seibel, BS: Phacodynamics: Mastering the Toolsand Techniques of the Phacoemulsification Surgery,Third Edition, 1999.
BIBLIOGRAPHY
Barojas, E: Importance of hydrodissection in phaco.Guest Expert, Boyd’s BF The Art and the Scienceof Cataract Surgery of HIGHLIGHTS, 2001.
Benchimol, S., Carreño, E: The transition fromplanned extracapsular surgery to phacoemulsifica-tion. Highlights of Ophthalmol. International En-glish Ed., Vol. 24, 1996, Nº 3.
Carreño, E.: From can opener to capsulorhexis: thecrucial step in the phaco transition. Course on Howto shift successfully from mannual ECCE to ma-chine-assisted small incision cataract. AAO, Oct.1999.
Carreño, E.: Hydrodissection and hydrodelineation.Guest Expert, Boyd’s BFThe Art and the Scienceof Cataract Surgery of HIGHLIGHTS, 2001.
Centurion, V.: The transition to phaco: a step bystep guide. Ocular Surgery News, Slack, 1999.
Drews, RC.: YAG laser demonstration of theanatomy of the lens nucleus. Ophthalmic Surgery1992. 23:822-824.
Koch, PS: Hydrodissection. Simplifying Pha-coemulsification. Fifth Edition, Slack, 1997, 8:87-98.

C h a p t e r 7: P repar ing f o r t he Trans i t i on
133

THE ART AND THE SCIENCE OF CATARACT SURGERY
134

C h a p t e r 8: Instrumentation and Emulsification Systems
137
INSTRUMENTATION ANDEMULSIFICATION SYSTEMS
INSTRUMENTATION
Phacoemulsification uses many of thesame instruments that are used in conventionalextracapsular cataract surgery. We will notrefer to them in this chapter because everycataract surgeon is fully familiar with suchinstruments.
This chapter is exclusively focused to-ward those instruments especially created forphacoemulsification surgery or those that mayhave common features for both techniques,extracapsular and phaco, but that have requiredmodifications for the surgeon to undertakesuccessful phacoemulsification surgery.
There are multiple variations of eachtype of instrument. Consequently, rather thanreferring to the instruments by the name of theircreators or proponents, we will focus here onthe specific characteristics needed for phacosurgery. These instruments are:
Eye Speculum
It is very important to have the right eyespeculum (Fig. 74). Since topical anesthesia isutilized by most experienced phaco surgeons,the speculum must have a lock to prevent thelids from closing and squeezing during sur-gery.
The speculum should not interfere withthe surgeon's movements and instrumentationwhen operating in the upper temporal quad-rant, which is the approach mostly utilizedtoday.
Fixation Ring
Its use is optional but it may be quitehelpful during the construction of the limbal orthe clear cornea tunnel incision because it pro-duces fixation of the globe throughout thecircumference of the ring. The most popularfixation ring is the Fine-Thornton (Fig. 75). Ifthe surgeon prefers not to use the fixation ring,the globe may be fixed with very fine 0.12toothed forceps.
Knives and Blades
There are two options for the knives andblades (Figs. 76-77): 1) utilize stainless steeldisposable knives (Fig. 76); 2) use diamondknives which can be re-sterilized (Fig. 77).Both types of knives and blades have theiradvantages and disadvantages. The selectionreally depends on the preference of the sur-geon. The disposable stainless steel blades andknives have reached a very high level of qualityand precision. They may be re-sterilized for asmall number of cases, certainly no more thanfour or five. They require a lower initialinvestment and less care when handling by thenurses and assistants. Nevertheless, when weare going to make a clear corneal incision andtunnel, it is recommended to use a diamondknife which can be calibrated (Fig. 77). Thoseknives and blades can be manufactured withdifferent parameters. Those for paracentesis(Fig. 76 B) have an angulation of 30 degrees.

THE ART AND THE SCIENCE OF CATARACT SURGERY
138
Figure 74 (left): Eye Speculum
Phaco surgery using topical anesthesiarequires that the eye speculum design offer suffi-cient aperture for operating from the side, which isalways done from 9 to 12 o’clock, whether right orleft eye. The speculum has a lock and strong armsto keep the eye open in case that the patientsqueezes the lids.
Figure 75 (right): The Fine-ThorntonFixation Ring
Some surgeons find this fixationring useful, particularly during the con-struction of the limbal or the clear corneatunnel incision. Other surgeons prefer tofixate the globe with a forceps.

C h a p t e r 8: Instrumentation and Emulsification Systems
139
Crescent knives (Fig. 76-C) have a roundedpoint which is fundamental in the constructionof the tunnel in the incision as shown in Fig. 41-B, Chapter 8. The disposable knives with sharppoints range from 2.6 to 3.2 mm (Fig. 76-A).They are particularly useful in the small inci-sions when utilizing different sized phacoprobes and tips as shown in Figs. 82 A and B.The 5.2 mm blunt point blades as shownin Figs. 76-D may be highly useful to enlargethe incision in case of PMMA 5.5 mmintraocular lens implantation or larger asshown in Fig. 72 A. There is, however, anincreasing tendency to utilize diamond knivesbecause the surgeon is able to obtain a perfectincision. The knives also last for a long time.
Figure 76: Stainless Steel DisposableKnives for Phacoemulsification
(A) Knife to make a 3.2 mmprimary incision. (B) Blade with a 30degrees angulation for paracentesis orsideport incision to allow introductionof the second instrument (manipulatoror chopper) and other purposes such asviscoelastic injection. (C) Crescent knife.The rounded point is fundamental in theconstruction of the tunnel incision. (D)This 5.2 mm blunt point blade may behighly useful to enlarge the incision incase of PMMA 5.0 x 6.0 mm optics asthe one shown in Fig. 72-A intraocularlens implantation or larger .
Consequently, for surgeons who do a majoramount of surgery, the diamond knife may be,in the end, economically more efficient.
In Fig. 77 you may see diamond knivesdesigned for various purposes, 77-A for para-centesis or side port incision (also shown dur-ing surgery in Fig. 41-A); Fig. 77-B for a3.2 mm incision or slightly smaller as inCarreño's Phaco Sub-3 technique, also shownin Fig. 40 C. Fig. 77-C shows the crescent typeof knife, also seen in the surgical steps inFig. 41-B and Fig. 42. Very narrow sharppointed blades are being developed toperform the 1 (one) mm incisions to be usedwith Dodick's PhotoLysis recently ap-proved by the FDAusing a special ND-YAGlaser.

THE ART AND THE SCIENCE OF CATARACT SURGERY
140
Hydrodissection Cannula
This special cannula is shownin Fig. 78-A and in Figs. 46 - 48. Thesecannulas are especially made with a rect-angular and 27 G diameter that facili-tates the injection of liquid to separatethe anterior capsule from the cortex. Theyare re-sterilizable. They should be con-nected to a 3 or 5 cc syringe to allow abetter effect from dispersion of liquid.For hydrodissection, there are also otherspecial cannulas in the form of "J" whichmay be useful for specific maneuvers asshown in Fig. 47.
Figure 77 (left): Diamond Knives
(A) Utilized for side port or paracentesisincision (also shown during surgery in Fig. 41-A).(B) This blade is used for 3.2 mm incision orslightly smaller as in Carreño's Phaco Sub-3. Thisknife is also shown in Fig. 42. (C) Crescent dia-mond knife with rounded point fundamental in theconstruction of the tunnel incision( also shown inFigs. 41-B and 42).
Figure 78 A (right): Hydrodissection Can-nula Under the Anterior Capsule.
For this purpose it is recommended touse a 25 G flat tip cannula. Observe how thecannula enters below the edge of thecapsulorhexis performed on the anterior cap-sule. The surgeon then injects the BSS to sepa-rate the capsule with the cortex from the nucleus.

C h a p t e r 8: Instrumentation and Emulsification Systems
141
Cystotomes or Capsulorhexis Forceps
There are several alternatives to the se-lection of cystotomes. One group is alreadydesigned and manufactured for this purpose,with 25, 27 and 30 G calibers. Some surgeonsprefer to bend the tip of an insulin needle,which provides a very sharp point. The maincharacteristic of the cystotome is that it must bevery sharp to facilitate the creation of the firstcapsular flap during capsulorhexis and enablethe surgeon to continue performing a curvilin-ear capsulorhexis. These cystotomes must beeasily adjustable to the needs and comfort ofthe surgeon in his/her maneuvers.
As to the capsulorhexis forceps (Fig. 78B-C) there is a large variety and types ofdesigns. The best known is the Utratta-Kershnerforceps (Fig. 78-B left). The main characteris-tic of all capsulorhexis forceps is that theyhave very fine, resistant arms and tips thatprevent trapping of the iris. Curved ends arehighly useful so that the surgeon can manipu-late more comfortably within the anterior cham-ber. In any case, they must be easily connectedto a syringe that contains air or balance saltsolution for injection in addition to the conven-tional viscoelastic, when the surgeon feels it isneeded. There are other very usefulcapsulorhexis forceps such as the ones de-signed by Gimbel (Fig. 78 C), the Masket,the Corydon and several designed by Buratto.
Figure 78 B-C: Capsulorhexis Forceps
(A) The Utratta-Kershner's forceps. (B) TheGimbel's forceps. All capsulorhexis forceps have veryfine, resistant arms and the end of the tips are slightlycurved (see inset) that will prevent trapping of the iris.Please observe the special design that is highly usefulto manipulate more comfortably within the anteriorchamber. Other popular capsulorhexis forceps carrythe name of Masket, Corydon and Buratto.

THE ART AND THE SCIENCE OF CATARACT SURGERY
142
Nuclear Manipulators or Choppers(Second Instrument)
These ancillary instruments are abso-lutely essential in order to adequately performthe maneuvers necessary to remove the nucleus,as described and illustrated in Chapter 9. Thereis a large variety of types and designs. Theseinstruments are introduced into the anteriorchamber through the ancillary or side portincision. The purpose of this second instru-ment, either the manipulator shown in Fig. 79
or the chopper shown in Fig. 80, is to facilitatethe bimanual maneuvering and rotation of thenucleus, as well as allowing the chopping of itintofragments that are going to be emulsified.In Fig. 79 we show two well known lensmanipulators: 79-A is the Lester instrumentand Fig. 79-B is the Osher. In Fig. 80, you maysee different types of choppers: 80-A theFukasaku chopper and 80-B the Dodick-Kamman chopper.
Some of these instruments have a blunttip, some longer or shorter length tips. All ofthem must have angulation as a common char-
Figure 79: Nuclear Manipulators
(A) Shows the Lester nuclear manipula-tor. (B) The Osher manipulator. These are two ofthe most popularly used ancillary instruments es-sential to perform the bimanual maneuvers toremove the nucleus, as described in Chapter 9.These nuclear manipulators are essentially used inthe non-chopping techniques.

C h a p t e r 8: Instrumentation and Emulsification Systems
143
Figure 80: Choppers
In this illustration you may see two of themost popularly used choppers (second or ancil-lary instruments) ustilized by the surgeon in thebimanual technique of removal of the lens nucleuswith the chopping method as described in Chap-ter 9. (A) Shows the Fukasaku chopper. (B)shows the Dodick-Kamman chopper. Pleaseobserve that all the tips have a small diameterangulation (0.25 - 0.50 mm). they have a blunt tipwhich is able to cut or slice the nucleus. Theymust have sufficient strength in the tip to createand lead the forces of traction and rotation of thenucleus. All surgeons have available both typesof ancillary instruments, the nuclear manipula-tors and the choppers, to use in the procedure thathe/she decides for a specific patient.
acteristic, with the angulated tip being of verysmall diameter (0.25 - 0.50 mm). The tip is ableto cut or slice the nucleus. They must havesufficient strength or resistance in the tip tocreate and lead the forces of traction and rota-tion of the nucleus and they must be smooth andblunt on the posterior surface in order to avoiddamage to the surrounding tissues. Some sur-geons have available both types of instru-ments, manipulators and choppers, dependingon the type of surgery they are doing, because
although the surgeon has his procedure ofchoice, he/she is not bound to rigorously followthat same procedure in all cataracts. The sur-geon has to adapt to different circumstancesand situations.
Other commonly known choppers arethose of Seibel, Nagahara, Nichamin. Thereare some hooks that are specifically utilized forrotation of the nucleus. They need to beangulated and have the shape of a shirt button.The best known is the Lester.

THE ART AND THE SCIENCE OF CATARACT SURGERY
144
Forceps and Cartridge Injector Sys-tems for Insertion of Foldable In-traocular Lenses
Small incremental advancements con-tinue to take place for placement of foldableIOL’s through small incisions. There is adefinite trend toward the development of sepa-rate instruments for folding and inserting IOL’srather than using the insertion device to fold theIOL.
The majority of foldable lenses are in-serted either by forceps designed by out-
Figure 81: Forceps for Insertion of FoldableIOL's
There is a large variety of instrumentsdesigned for this purpose. The right design isrelated to the type of IOL you will be using. Herewe present the Osher-Seibel folding forceps (A)with a curved design to easily fold most softintraocular lenses. For the insertion, we shows theBlaydes angled lens forceps (B) that will help thesurgeon to gently insert the IOL in the bag.
standing cataract surgeons for this purpose(Fig. 81) or by a combination of instrumentsdesigned by the manufacturer to facilitate fold-ing and insertion known as cartridge injectorsystems. Examples of often used forceps areshown in Fig. 81 and injectors in Fig. 82.Dodick prefers to use forceps to implantAlcon's AcrySof (acrylic foldable IOL). Othervery popular and useful forceps are the FineUniversal III forceps (Rhein Medical, Tampa,Fla.) and the Buratto insertion forceps (Ameri-can Surgical Instruments. Westmont, Illinois).The latter is used specifically for the acryliclens.

C h a p t e r 8: Instrumentation and Emulsification Systems
145
Figure 82 AB (right): Injectors for Insertion of FoldableIOL's
(A) The Allergan Unfolder. Sapphire Series Fold-able IOL Implantation System: With very soft tip anddesign, the Unfolder Sapphire offers excellent control duringthe implantation of Allergan’s acrylic foldable intraocularlens. In this surgeon´s view we are presenting the Sapphiremodel for the acrylic IOL. Once the IOL is unfolding inside thecapsular bag, the cartridge should be rotated with the tipaperture facing down to permit a smoth ejection of the IOL.
(B) The Alcon Monarch Model. Foldable IOL Im-plantation System: The Monarch system´s design allows theacrylic foldable IOL to blossom out of the tip aperture in asafe, controlled way with no haptic harm. The injector tip isintroduced through the phaco incision asobserved here, ro-tated and advanced to the center of the capsular bag were thelens is slowly injected and unfolded on one plane into thebag. Alcon is also continuing to develop finer injection throughits high technology capabilities.
Figure 82 C (left): Alcon’s Acrylic System to Fold IOL's
This special device allows the surgeon to carefullyfold the acrylic IOL previous to its insertion. The IOL is posi-tioned in the top center of the Acrypack. The optics of theIOL is shown here. Once in position the two arms of theAcrypack are slightly compressed and allow the surgeon tofold the IOL like a Mexican “taco” or a cigar. With the help ofthe insertion forceps (Fig. 81) you may then catch the lens nothalfway but slightly closer to the folded part of the lens.

THE ART AND THE SCIENCE OF CATARACT SURGERY
146
Cartridge Injector Systems
Some of the newest advances in lensinsertion technology surround the use of car-tridge injector systems. Fine, Lewis andHoffman believe that there are many perceivedadvantages of implanting foldable IOLs withinjector systems, as compared with foldingforceps. These advantages include the possi-bility of greater sterility, ease of folding andinsertion, and implantation through smallerincisions.
Greater sterility with injector systems isbelieved to occur because the IOL is broughtdirectly from its sterile package to its sterilecartridge and inserted into the capsular bagwithout ever touching the external surface ofthe eye, as is the case for lenses in foldingforceps. Although this advantage would sug-gest a lower rate of endophthalmitis with injec-tor systems, recent clinical studies have shownno significantly different rate of bacterial con-tamination of the anterior chamber after im-plantation of silicone lenses with a forcepsversus an injector.
Perhaps the most appealing advantage ofinjector systems is that the lens can be loadedby a nurse or technician without the use of anoperating microscope, further streamlining theprocedure. In addition, inserting foldable lenseswith a cartridge device is generally felt to beeasier than insertion with forceps, and theselenses can usually be implanted through asmaller incision when delivered by means of aninjector, compared with an insertion forceps.
Allergan's foldable three piece siliconelens (monofocal or multifocal - AMO Array)with PMMA haptics may be implanted withAMO's Unfolder Phacoflex injector system.Allergan's acrylic foldable IOL (Sensar andClariflex lenses) may be implanted with a newinjector now available and known as theUnfolder Sapphire, as described by Centu-rion (Fig. 82-A). These injectors are re-sterilizable (as are the forceps, of course).
Alcon’s popular 5.5 mm AcrySof IOLmay be implanted with one of its injectors suchas the Monarch (Fig. 82) or with a standardcartridge through a 3.0 mm incision. Somehave reported injecting this lens through a 2.8mm incision. Many surgeons use Alcon’sAcrypack (Fig. 82) when implanting theAcrySof lenses. The Acrypack serves to firstfold the IOL. The surgeon then uses a forceps(Fig. 81) to implant the already folded IOL.
The Alcon AcrySof lens, which requires3.5 to 4.0 mm incisions for 6.0 mm optics and3.2 to 3.5 mm incisions for 5.5 mm optics, isnow packaged in a wagon wheel dispenser.The easiest folding instrument to use for theselenses is the Rhein folder, because its tips havebeen extended to make it easier to remove thelens from the wagon wheel package. Theforceps can be turned with the tips down in thenondominant hand. The tips go into the slots onboth sides of the optics, so that the lens can bepicked up and placed on a drop of viscoelastic.The forceps are then turned so that the tabs aredown. The lens is grasped and folded, and thenthe insertion device in the dominant hand isused to insert the lens.

C h a p t e r 8: Instrumentation and Emulsification Systems
147
THE PHACO PROBES AND TIPS
In Fig. 83 you can see two different typesof phaco probes and tips. In Fig. 83 (left), thereis a larger caliber probe with a straight tip.This is particularly used when the incision ispredominantly limbal. The incision is slightlylarger than the one mostly utilized today whichis the corneal incision shown in Fig. 83 (right).The probe in Fig. 83 (left) using a standard
phaco tip emits more heat which could harmthe corneal lips. The phaco probe and tip,shown in Fig. 83 (right), is narrower and can,therefore, be utilized in smaller corneal inci-sions such as the 2.6 mm shown in Fig. 83(right). The popular angled Kelman tip shownhere has a high capacity to cut the tissues and isvery useful in more dense cataracts. It allowsthe use of a finer probe because there is lesscontact with the lips of the wound and less heatdamage.
Figure 83: Phaco Probe and Tip - Diverse Design and Diameters
Here we may observe and compare a standard phaco tip (A) with 3.2 mm in diameterand a 3.5 mm incision width usually employed in scleral or limbal tunnel incisions. In (B)we present the angled Kelman phaco tip attached to a finer phaco probe inserted througha 2.6 mm corneal tunnel incision.This tip allows a smaller incision with less peri-incisionalfluid escape. It also gives rise to less heat transmission to the lips of the wound.

THE ART AND THE SCIENCE OF CATARACT SURGERY
148
Phaco Tips
The different components of the phacoprobe are shown in Fig. 84 left . Please observethe standard tip (T). The probe is also shown indetail in Figs. 50-A and 50-B in Chapter 7.With the advent of chopping techniques inphacoemulsification, there has been increasinginterest in the development of new tips fordifferent uses and purposes. There is a largevariety of phaco tips, and each one has itsreason for being. Chopping procedures arefacilitated by selecting the right tips from a
variety of them as shown in Figs. 51 and 84.Depending on the surgeon’s technique andcircumstances of the case, they all can contrib-ute to better control in maneuvering of thenucleus.
In figure 84 (right) and Fig. 51, you maysee the most important tips. Fig. 84 A is theMicroflow tip, 84 B is the Mackhool-Kelmanphaco tip, 84 C is the Aspiration BypassSystem (ABS), 84 D the flare head phaco tip,and 84 E is the popular Kelman angled phacotip. Their specific features are presented in thecaption of Fig. 84.
Figure 84: The Phaco Probe and Tips - Several Modelsfor Different Uses
The phacoemulsification probe and its components isshown in detail to the left. Standard Tip (T). The Standardtip (T), attached to it, is employed in cataracts withmoderately dense nucleus. Its large diameter (5.2 mm)requires a wider incision. Probe’s Aspiration port (AP),Irrigation port (IP), silicone Sleeve (S), Handpiece (H),Irrigation line (I), Aspiration line (AL) and the Ultrasoundline (U). It is important to understand its mechanism inorder to manipulate this instrument with extreme accuracy.
To the right you find several phaco tips for differentpurposes related to the type of cataract and the techniqueutilized.
The Micro-Flow Tip (A) has some spiral grooves thatalways provides cool fluid that flows around the needle,thereby diminishing the heat around the incision. TheMackool-Kelman tip (B), has a teflon coat to diminish theheat that could harm the cornea. This is one of the latestgeneration phaco instruments. The transformation of en-ergy always involves some dispersion which generatessome heat.
The Aspiration Bypass System (ABS) shown in (C),is also a new model 3.2 mm in diameter with a 0.25 mm sidehole (encircled in red) which contributes to prevent thecollapse of the anterior chamber (this micro-hole also aidsin controlling the temperature diminishing the heat over the
structures in the anterior chamber). The Surge phenomenon or A.C. collapse might be produced with larger aperture side holes(0.85 mm) in the tip. This does hot happen with these new devices. The Flare tip (D) was designed to perform faster and bettercontact with the nucleus while making the groove (D & C procedures) and the chopping techniques. The broader angle ofcontact between this tip and the nucleus is more effective in softer nucleus. The Kelman angled phaco tip (E), optimizes theultrasound effect during the procedure and permits a better cavitation. It is more efficient in hard nuclei. The curved tip modelallows more contact with the tissues (internally and externally) and less possibilities of traction to the zonule.

C h a p t e r 8: Instrumentation and Emulsification Systems
149
they offer more safety and control. The mostpopular are:
1) Kelman's Turbosonics andMiniturbosonics
These tips have a curved shape that at-tains larger contact with tissue surface, internaland external, leading to more cavitation eventhough the ultrasound energy used may be thesame as compared when using the standard tip.Higher cavitation allows destruction of thenucleus beyond the area of touch.
The miniturbosonics is essentially thesame style of tip but with lesser diameter.
The main advantages of these tips are: 1)US energy is optimized leading to increasedcavitation. 2) Better cutting and slicing oftissues in very hard nuclei.
2) Micro Tips
They all have smaller internal and exter-nal diameters as compared with conventionaltips. Main Advantages: You can work withsmaller incisions and attain greater stability ofthe anterior chamber because these tips havemore resistance to the passing of lens frag-ments leading to less risk of the Surge phenom-enon. They do require, however, more vacuumin order to obtain similar tissue fixation thanwhen using a conventional tips.
These micro tips are the ones indicatedfor use with the Mackool cassette system thatby definition has tubes with narrower innersurfaces and thicker outer surfaces, facilitatingthe use of higher vacuum and reducing Surge.
Surgical Principles Behind theDifferent Phaco Tips
The different uses for each of thesedifferent tips are described in the caption ofFig. 84.
The main variations in phaco tips arerelated to :1) Angulation. 2) Shape. 3) Size and4) Thickness. And 5) The existence or not of aprotective insulated cover that facilitates cool-ing so as to minimize the transfer of heat to thesurrounding tissues, essentially the corneal lipsof the wound.
The Importance of Angulation andBeveling
The more beveled is the tip the larger thecutting surface and the larger the area whichmust be occluded at the tip. Those rangingfrom 0º to 15º do not cut much but they occludemore easily. They are, therefore, ideal for softcataracts and for some chopping techniques inwhich a maximum capacity for occlusion andhigh vacuum is necessary.
Tips with more angulation and bevelsuch as 45 degrees have a high capacity to cutthe tissues and are very useful for the maneu-vers of phacofracture in dense cataracts and inthe Divide and Conquer techniques.Nevertheless,these tips offer a higher risk ofposterior capsule rupture precisely because theyare so sharp and highly cutting.
Importance of Shape and Size
New developments are oriented tomicrotips and the Mackool system because

THE ART AND THE SCIENCE OF CATARACT SURGERY
150
PHACOEMULSIFICATION SYSTEMS
In the past three years, there have beendramatic improvements in the technology ofphacoemulsification, involving every aspectof phaco systems. These range from the phacoprobes and tips all the way down to the footpedal. Improvements in the generation andcontrol of ultrasonic power, fluidics, handpiecesand tips have been made which are extremelyadvantageous to the cataract surgeon. We areall indebted to the manufacturers of our instru-ments and equipments who have investedheavily in financing this research and haveattracted the best designers and engineers tocarry on these developments.
Figure 85: Shown above are the three most advanced phacoemulsification machines andsystems. (A) the well known Alcon Legacy 20,000. (B) Allergan’s Sovereign, that is nowtheir “top of the line” and most efficient equipment. (C) Storz Millennium, which deliversall the advances described in this Chapter.
These systems are able to provide muchmore reproduceable energy at each powersetting regardless of the mass and density ofthe nuclear material at the phaco tip. Since thisload is continually changing, the system mustbe able to adjust. If not, the efficiency of theequipment is immediately affected.
The main systems available today forphacoemulsification are provided by the majorplayers in industry and have very advancedtechnology. These systems are the well knownAlcon Surgical LEGACY 20,000 equipment(Fig. 85-A), the AMO (Allergan) Sovereign(Fig. 85-B) and the Bausch & Lomb - Storz

C h a p t e r 8: Instrumentation and Emulsification Systems
151
Millennium (Fig. 85-C). Allergan's Sovereignis the top of the line at Allergan. The equipmentknown as Diplomax made available for severalyears by Allergan is still a useful machine,more portable and of lower price than theSovereign.
How to Select the RightEquipment for You
In answer to the many questions that wereceive from colleagues throughout the worldas to which machine or equipment to purchase,we strongly recommend that the first priorityshould be to select one of these three, but basedon the quality and availability of service andtechnical support that you will be able toobtain in your community. It is useless tohave a superb phaco machine if that particularmanufacturer provides inadequate technicalsupport in the area where you practice. Eachone of these three major systems makes avail-able power modulations and advantages such
as auto pulse phaco, burst mode phaco andocclusion mode phaco which are most impor-tant in modern phacoemulsification surgery.
The Pulse and Burst Modes
Differences Between Them
This is one of the most important techno-logical advances in phaco systems, as empha-sized by I. Howard Fine, M.D., in the U.S. aswell as by Edgardo Carreño, M.D., one ofSouth America’s top phaco surgeons. Whenyou contemplate acquiring a new machine, becertain that it offers these two modalities.
What is the difference between them? InPulse Mode we have linear power for afixed interval of the application of that power(Fig. 86). In Burst Mode, we have fixedpower with a variable interval in the applica-tion of that power (Fig. 87). Therefore, Pulseis a fixed short interval, Burst is a variableinterval.
Figure 86: Concept of Pulse Mode in Phacoemul-sification
Pulse mode provides a great advantage inmobilizing and removing tissue. In pulse mode,the ultrasonic energy can be increased while thepulse rate or application rate of the energy remainsconstant. One chooses a certain number of pulsesper second (P), say 2 pulses per second, which re-mains fixed during the surgeon's ability to increasethe ultrasonic energy level as the foot pedal (F) isdepressed in position 3. Note the constant pulserate (P) as depicted by two pulses shown in frontof each tip. Note increasing energy which can beapplied, as represented by the enlarging size of thephaco tip and arrow (E), as the foot pedal (F) isdepressed. Graph A (Pulse Rate - P/S) shows thatpulse rate remains constant (horizontal line) dur-ing increased depression of the foot pedal. GraphB (Energy Level) shows that energy application (E)increases in a linear fashion, to a preset maximum,with depression of the foot pedal. Burst Mode, asdisplayed in the next illustration, is the reverse ofPulse Mode.

THE ART AND THE SCIENCE OF CATARACT SURGERY
152
Clinical Applications of the PulseMode
Pulse mode provides a great advantage inmobilizing and removing tissue (Fig. 86). Inthe chopping techniques (Chapter 9), at a fixedpulse rate of 2 pulses per second, the surgeonchops by stabilizing the nucleus with the chopinstrument in the golden ring. Fine likes topull to the side of the phaco needle rather thanto the top of the needle so that after the secondchop, the initial tissue segment is alreadylolipopped. (Editor's Note: lolipopped refersto securely engulfing the tip of the phaco intothe nucleus, like a lollipop or candy sucker ona stick. The phaco tip is analogous to the stickand the nucleus is the round candy portion -Fig. 88) He does not have to search for thenucleus, or manipulate it: it’s already engaged
on the phaco tip. The vacuum provides sub-stantial control for holding the tissue betweenapplications of phaco power, with almost nopotential for chattering. (Editor's Note: chat-tering refers to when the nucleus bouncesagainst the phaco tip at a high rate of speedwithout emulsifying it as desired, like whenone’s teeth chatter when cold - Fig. 89).
When using the LEGACY 20,000 equip-ment, for instance, Fine can specifically cus-tomize the application of the parameters ofphaco power based on differences in thedensity and type of cataract tissue he isremoving. This technological advance is alsoavailable in the other outstanding equipmentalready mentioned, particularly Allergan's Sov-ereign and Storz (Bausch & Lomb) Millen-nium.
The power levels used by Fine are verylow -- very frequently in the low teens. It is rare
Figure 87: Concept of Burst Mode in Pha-coemulsification
Burst Mode provides more control ofthe ultrasonic energy level, which is advan-tageous during certain maneuvers. In burstmode, one chooses the ultrasonic energy leveldesired on the control panel, and it remainsfixed. As you depress the foot pedal in posi-tion 3, the pause between bursts of the fixedenergy decreases from intermittent bursts tomore frequent bursts, toward ultimately con-tinuous phaco. Note the constant energy level(E) as represented by the constant size of thephaco tip and arrow. Note increasing burstrate (P) as depicted by the increasing num-ber of bursts shown in front of each tip, asthe pedal (F) is depressed. Graph A (PulseRate - P/S ) shows that burst rate increasesduring increased depression of the foot pedal.Graph B (Energy Level) shows that energylevel (E) remains constant (horizontal line),with depression of the foot pedal.

C h a p t e r 8: Instrumentation and Emulsification Systems
153
Figure 88 (right): Concept of"Lollipopping" the Nucleus
Lollipopping the nucleus refers to se-curely engulfing the tip of the phaco into thenucleus, like a candy sucker on a stick. Thephaco tip (P) is analogous to the stick andthe nucleus (N) is the round candy portion.This technique provides a secure, controlledhold on the nucleus during the chopping andother maneuvers.
Figure 89 (left): Concept of "Chattering"during Application of Phaco Power
(Top) An undesirable condition duringphacoemulsification is when the phaco tipbounces (arrows) against the nucleus or lenspiece when attempting to emulsify it. Thiscondition wastes time and presents unneededultrasonic energy into the eye with no result-ing emulsification and extraction. The chat-tering effect is represented by a bouncing ballagainst the ground. (Below) Increased vacuumcan provide the additional control for holdingthe tissue between applications of phaco power,so that chattering does not occur. Here the tis-sue is efficiently extracted (arrow) as repre-sented by the smoothly rolling ball.

THE ART AND THE SCIENCE OF CATARACT SURGERY
154
for him to have an effective phaco time greaterthan 20 seconds and an average phaco power ofmore than 20 percent. Meanwhile, the vacuumis high, 340 mmHg. He minimizes power andallows high vacuum to do the job.
Clinical Applications of the BurstMode
Its Role in Transition to Chopping
Fine believes the easiest way for sur-geons to make the transition to chopping (Chap-ter 9) is to use the burst mode set for single-bursts with the panel control (Fig. 87). Heprefers a burst of 150 ms with vacuum of 400mmHg. Also, by using Burst mode and aBiModal sub-mode, Fine can use a higheraspiration flow rate to attract the epinuclearring out of the capsular fornix.
Advances with the Sovereign PhacoSystem
Just as there are significant advances andtechnological contributions with the prestigiousLEGACY 20,000 machine manufactured byAlcon Surgical, Allergan has recently broughtinto the market its Sovereign. This is really thetop of the line for Allergan in this type ofsurgery. It takes into consideration and actu-ally participates in what all surgeons wantwhich is better and more predictable surgicaldynamics for their cataract patients. Thisequipment has superb fluidics and capacity forprogramming and provides increasing ease ofcataract removal.
The Sovereign utilizes very effectivelythe micro-processor controls and an on-boardcomputer regulation of all the components,
such as fluidics, ultrasonics, footpedal, andbottle height.
With respect to fluidics, the Sovereignhas a digital peristaltic pump that, because ofits sophistication, is capable of mimicking ev-ery other pump system. Its highly developedresponsive fluidics monitoring system, calledthe Intellesis, monitors the fluidics 50 timesper second. There is a sensitive control of whatis happening to the vacuum in the anteriorchamber. It also has the ability to respondrapidly because the pump can reverse, in addi-tion to move forward, slow, and stop. An inor-dinately stable anterior chamber can beachieved, with a reduced tendency for vaultingof the capsule or fluctuations in chamber depth(See Chapter 7 - Figs. 62, 63, 65). This newlevel of control offers optimum safety.
The foot pedal has an on-board com-puter and is capable of multiple functions(Figs. 52, 53, 55, Chapter 7). The foot pedalcan be used with either the toe or heel depend-ing on the surgeon's height. Using the footpedal, even remote parameters such as bottleheight, can be changed.
Another important feature is the ultra-sonics which has expanded from a two-crystalto a four-crystal handpiece. This four-crystalhandpiece is adaptable to technology frommanufacturers other than Allergan. Manymachines are not designed to use tips fromcompanies other than the parent company. Finelikes to use a Kelman bent tip for certaincases and he can use it with the Sovereign(Figs. 83-B and 84-E.)
The ophthalmologist acquiring a newunit is naturally concerned whether the Sover-eign can be programmed and used withoutextensive study and training in the system. Ofcourse, every surgeon must understand thefundamentals of how phaco machines in gen-eral work, as presented in Chapter 7. Accord-

C h a p t e r 8: Instrumentation and Emulsification Systems
155
ing to Fine, extensive study is not requiredbecause there is a sensor that monitors thedelivery of ultrasound energy. It is difficult tokeep a system that has a changing mass, shape,and density of material at the tip at its resonancefrequency. But this system monitors, throughits microprocessors, 50 different functions thatare impacting resonance frequency, 500 timesa second, and changes and corrects themautomatically.
Pulse and Burst Modes on theSovereign
We have already outlined the great sig-nificance and importance of the Pulse andBurst Modes applicable with Alcon's LEGACY20,000 equipment, which is a superb machine(Figs. 86, 87). Fine often combines Pulse andBurst modes also when using the Sovereign.Because the power is intermittent and the
vacuum is constant, one advantage of powermodulation is that nuclear material tends to bekept at the tip. Nuclear material seldom chat-ters (Fig. 89) and almost never shoots into theanterior chamber, where it can threaten theendothelium. Fine feels that the Sovereignrepresents a new level of finesse and controlthat leads to safety and ease of operation.
Fine’s Phacoemulsification Parametersincluding the Pulse and Burst Modes for Alcon’sLegacy 20,000, Allergan’s Sovereign and StorzMillennium, are presented in specially designedTables in pages 202-203.
Edgardo Carreño’s Adjustable BurstMode Parameters using Alcon’s Legacy 20,000are presented in this page.
In essence, we have a wonderful newmenu of remarkably sophisticated, helpfulphaco instrument choices. Each surgeon willneed to make his or her own decision, remem-bering to consider local service and support.

THE ART AND THE SCIENCE OF CATARACT SURGERY
156
RECOMMENDED READINGS
Buratto, L: Phacoemulsification: Principles andTechniques, 1998.
Mendicute, J., Cadarso, L., Lorente, R., Orbegozo,J., Soler, JR: Facoemulsificación, 1999.
Seibel, BS: Phacodynamics: Mastering the Toolsand Techniques of Phacoemulsification Surgery,Third Edition, 1999.
BIBLIOGRAPHY
Davidson J.: A comparison of technologically ad-vanced ultrasonic tips. Advances in Technique &Technology, Alcon Surgical - April 1999, Part 2 of2.
Fine, IH., Lewis JS, Hoffman, RS: New techniquesand instruments for lens implantation, CurrentOpinion in Ophthalmology 1998, 9:20-25.
Fine, IH., Lewis JS, Hoffman, RS: Recent advancesin phacoemulsification systems. Cataract Surgery:The State of the Art, Edited by Gills, H., Slack,1998.
Fine, IH.: Total control phaco chop. Advances inTechnique & Technology - Alcon Surgical, Part 2of 2, April 1999.
Koch, PS.:Blades. Simplifying Phacoemulsifica-tion, Fifth Edition, Slack, 1997, 3:21-26.
Piovella M., Camesasca, F.: New phaco tips andhandpieces. Atlas of Cataract Surgery, Masket &Crandall, 1999, 5:42-47.
Salvitti, E.R: Flared tip technology. Advances inTechnique & Technology, Alcon Surgical - April1999, Part 2 of 2.
Seibel, B.: New phaco tips. Phacodynamics -Mastering the Tools & Techniques of Phacoemul-sification Surgery, Third Edition, Section One:104-111.
Technical advances in phacoemulsification sys-tems, Ocular Surgery News, Feb. 2000.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
159
MASTERING PHACOEMULSIFICATION
The Advanced, Late Breaking Techniques
General Considerations
We have presented the step-by-step tech-nique of phaco during the transition includingthe fundamental understanding of how the phacomachine works (Chapter 7). The specific in-strumentation, equipments and best systemsused for phacoemulsification are discussed inChapter 8.
Regarding instruments and use of equip-ment, it is essential to keep in mind that weshould first train in order to thoroughly under-stand and command the subtleties of ourphacoemulsifier before its clinical use. Asfrequently emphasized by Centurion, we willnot be able to improvise or try to master it in thesurgical suite.
Advantages of Phaco
It is also generally accepted that the mainreasons why phacoemulsification has stimu-lated so much interest is because of the follow-ing advantages, all of which improve results: 1. Less ocular trauma induced. 2. Less postoperative inflammation. 3. Astigmatism induced is minimal or nil. 4. Postoperative refraction is more promptlystabilized. 5. Less risk of endophthalmitis. 6. Topical anesthesia can be effectively used. 7. Immediate physical and visual rehabilita-tion is attained.
Now let us consider fundamental con-cepts, measures, methods and techniques nec-essary to follow in order to master phacoemul-sification.
Trauma-FreePhacoemulsification
Considering that this procedure is verymuch device-dependent, Centurion establishesa tripod: physician-technician-machine. Byindividually organizing and interrelating thephysician's role, his/her technician's importantinput and coordination, the functioning of themachine and the technique, we are able toperform the procedure free of trauma to ourpatients and less stress to the surgeon. Thismay be accomplished without changing theOperating Center's routine.
In this "trauma-free phaco," it is alsoimportant to achieve the following: 1) nodelays of patients, anesthesiologists or the sur-gical team. 2) Perform a limited number ofdaily procedures with predictable results moredays in the week which is preferable to aschedule of longer but less frequent operatingdays with a much larger volume of operationsin one single day.
Perform 4 (four) cataract surgeries inone hour is as much as we should aim for. Theobjective is not to operate quickly but to takeadvantage of the results of a well-trained teamthat has adapted well to this system.

THE ART AND THE SCIENCE OF CATARACT SURGERY
160
Faster Operations
Do They Sacrifice Patient Care?
If the operating team is really effi-cient, speed should not necessarily leadto lesser results. The key lies in theadroitness and perfect coordination amongCenturion's "tripod: surgeon-technician-ma-chine". Making an operation safe and effectiveshould be our primary goal. It is important tobalance time, speed and safety, because in theend we all should aim for safe operations.
Readiness and Know-How to BecomeEfficient
Stephen Lane, M.D., has very posi-tively emphasized that if you want to go faster,ignore what is happening inside the eye andconcentrate on what is happening in the oper-ating room (OR). Make sure that the OR staffis proficiently getting the cases in and out andmoving the patients with readiness. If thesurgeon is only working in one room, there ismore time wasted moving a patient from oneroom to another, getting a room cleaned up, andgetting the next patient in, than during the
cataract operation itself. There are a series ofsteps to make the process flow efficiently.
I. Howard Fine, M.D., has pointed outthat there is an emphasis today of cataractsurgery being likened to a foot race. Somesurgeons show videos with stopwatches. Justlooking at their hands reflects how they rushrather than doing maneuvers that are appropri-ate for working inside the eye. Racing theclock is definitely not good for the patient.
In our teaching, it is important to conveythat endothelial cell loss, iris trauma, incisionsthat do not heal, or broken capsules, may resultbecause of a desire to do faster procedures. Asa matter of fact, complications should be lessbecause of the advanced technology we cur-rently possess. If you have one or two operat-ing rooms, efficiency is more connected to theturnover, not necessarily the individual case.The most practical method to obtain speed withefficiency is the one recommended by Centu-rion: use two operating rooms with exactly thesame equipment disposition -- they are clonedrooms. This saves time because it is notnecessary to change equipment; provides sav-ings in maintenance and, most important: op-erating room staff can concentrate on theneeds of the patient and the surgical team.
THE ADVANCED, LATE-BREAKING TECHNIQUES
Anesthesia
Advanced or experienced phaco surgeonsmay use topical anesthesia alone or combinedwith intracameral irrigation anesthesia (Figs.35, 36). You may find as in-depth discussionof this subject in Chapter 5. The other alterna-tive, of course, is to have the assistant or anes-thesiologist use peribulbar anesthesia, gener-ally Xylocaine 2% + Marcaine 0.50%. This
type of anesthesia has the great advantage ofenabling the surgeon to operate without anyintense emotional involvement or requiring themore active cooperation needed with topicalanesthesia. It is very comfortable to arrive atthe operating room where two or three patientsare already anesthetized and ready to beginsurgery.
The advantages of topical combined withintracameral vs peribulbar are amply discussed

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
161
in Chapter 5. For experienced surgeons, thecombined topical-intracameral approach ismuch preferred because of immediate visualrecovery.
Fixation of the Globe
The experienced surgeon does not needto fixate the globe with sutures. Fixation bygrasping the superior rectus muscle with for-ceps and placing a 6-0 silk suture through it,repeating the same maneuver with the inferiorrectus, is completely outmoded for phacoemul-sification. Besides, it leads to postoperativeptosis in a good number of cases.
Many surgeons utilize the Fine-Thorntonfixation ring (Fig. 75 - Chapter 8), particularlyduring the construction of the limbal or theclear cornea tunnel incision. Other surgeonsprefer to fixate the globe with a forceps.
THE INCISIONS
Phacoemulsification is a two-handed pro-cedure in most cases. Consequently there aretwo incisions done:
1) The Primary Incision.2) The Ancillary Incision.
The Primary Incision
For experienced surgeons, the procedureof choice is a self-sealing clear corneal, steppedvalvulated incision, performed temporally(Figs. 90-95). This incision is self-sealing andheals without sutures. It is shown in Figs. 90and 91 (surgeon's view). Most surgeons do atwo-step clear corneal tunnel incision as shownin Fig. 92, cross section view. Others prefer thethree step corneal tunnel incision because theyfeel i t may add a factor of safety (shown in
Figure 90: Initial Stages of Self-Sealing,Corneal, Stepped, Valvulated TunnelIncision - Surgeon's View
This surgeon's view shows the Crescentknife blade (K) entering the first incision (1) justat the limbus. The blade is advanced (red arrow)for some distance in the plane of the cornea, anda tunnel (blue arrows) is created. This forms thesecond step (2) in the three-step incision. Theknife does not enter the anterior chamber at thisstage.

THE ART AND THE SCIENCE OF CATARACT SURGERY
162
Fig. 93, cross section view). When performinga two-step incision, the length of the tunnel isslightly larger to ensure that the incision will beself-sealing. A short tunnel may not self-seal(Fig. 92).
Essential Requirements for a Self-Sealing Corneal Incision
To be safely performed, the clear corneatunnel incision must be done with a sharpdiamond knife (Figs. 77, 90, 91, 92, 93)although the presently available stainlesssteel disposable knives are also very sharpand useful (Fig. 76, Chapter 8). SergioBenchimol, M.D., in Brazil, who was one ofthe first surgeons to popularize this incision inSouth America, starts the surgery with a self-sealing, small, 1 mm paracentesis side portincision (Fig. 41) and pressurizes the eye with
viscoelastic or saline solution through this sideincision. Then he proceeds to perform theprimary self-sealing corneal incision, as shownin Figs. 90-93. The two-incision process, thesharpness and precision of the diamond knifeand even the stainless steel blades, and thepresence of viscoelastic in the pressurized eyemake it possible for a valve-like self-sealingincision to be made in the cornea withoutdamaging its structure.
Position of the Clear Cornea TunnelIncision
The trend today is to make the clearcornea incision on the temporal side as intro-duced by I. Howard Fine and Kimiya Shimizu,although Shimizu is inclined to perform a singleplane incision, which is not generally acceptedbut he was a pioneer in the introduction of theclear cornea incision.
Figure 91: Final Step of Self-Sealing,Corneal, Stepped, Valvulated TunnelIncision Performed with the DiamondKnife - Surgeon's View
A diamond knife blade (D) entersthe first incision (1), the second tunnelincision (2), and is then directed in a slightlyoblique direction to the iris plane andadvanced into the anterior chamber (ar-row). This forms the internal aspect of theincision into the chamber (A). This is thethird step (3) in a three-step self-sealingincision.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
163
Figure 92 (above left): The Two Step ClearCornea Tunnel Incision - Cross Section View
This cross section shows the location,direction and length of the two step clear corneatunnel incision. (1) The incision is started inclear cornea just inside the limbus. (2) It ex-tends through the stroma for 1.75 to 2.0 mmbefore entering the anterior chamber. Thislength of tunnel is important to ensure that theincision will be self-sealing. A short tunnel, bycomparison (dotted line), may not self seal.
Figure 93 (below right): The Three Step Cor-neal Tunnel Incision - Cross Section View
The three step corneal tunnel incisionbegins (1) with a perpendicular corneal incision1 mm inside the corneo-scleral limbus (L). This3.0 mm long first pass incision is made to a depthof about 300 microns. (2) The second passconsists of an incision made parallel to the cor-nea which tunnels for 1.75 mm to 2.00 mm. (3)The third step enters into the anterior chamber.This will form the internal lip of the incision justlike the internal valve lip of a traditional corneal-scleral tunnel incision.

THE ART AND THE SCIENCE OF CATARACT SURGERY
164
Reservations About the ClearCorneal Incision
Some surgeons have reservations about theclear-cornea incision, particularly because ofpostoperative astigmatism and endophthalmi-tis. These used to be two major complicationsof clear cornea incisions. These problems havebeen almost solved by making the wound assmall as 3.2 mm or less at the temporal site andby using intracameral antibiotics as discussedin Chapter 4.
Advantages to the Temporal Approach
1) The approach to the anterior chamberis easier, especially in patients with a narrowpalpebral fissure (Fig. 94).
2) As inferior duction of the eyeball is notrequired with the temporal approach, the irisplane is always kept at right angles to themicroscope to provide good visibility.
3) As pointed out by Kimiya Shimizu,the cornea is oval and the optical center of thecornea deviates to the nasal area from the
Figure 94: Advantages of the Temporal Ap-proach Corneal Incision
There are several advantages to the tem-poral approach. First, the optic center (C) isslightly further away from the temporal limbus(distance E) as compared to the 12 o'clocklimbus (distance D). Therefore, a temporalcataract incision is farther away from the opticcenter of the eye, and any resulting post-opcorneal edema around the incision is less likelyto affect the immediate visual rehabilitation.Second, by utilizing a temporal approach thereis no restriction of instrument movement causedby the speculum, as does exist with the 12o'clock approach. Note portion of speculum (S)at 12, and none temporally (T). Third, theeyebrow and somewhat more protruding su-praorbital rim can restrict instrument movementusing the 12 o'clock approach. Compare poste-riorly directed arrow at 12 (representinginstrument approach) to temporal arrow (T),(representing unrestricted instrument approachin the plane of the iris). Therefore, more easeofaccess to the anterior chamber structures, alongwith the unrestricted movement of instruments,is gained using the temporal approach.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
165
anatomic center. Therefore, in the temporalapproach, the incision's, the distance is about 1mm more from the optical center as comparedwith a superior incision (Fig. 94). Thus, theoperative invasion to the corneal center is mini-mal in the temporal incision. As a result,surgically induced astigmatism is small andrecovery of visual acuity is fast. In addition,when working on clear cornea at the 12 o'clockposition (closer to the optical axis than thetemporal position) if there is a small amount ofedema near the edge of the incision, beingcloser to the optic center of the cornea, maytemporarily interfere with the immediate vi-sual recovery aimed at with topical anesthesiaand clear corneal incision.
4) The wound will not separate whenblinking. The temporal incision, therefore,facilitates good adaptation of the wound.
5) In addition, there is more space forthe surgeon's hands. The temporal approachmakes the phacoemulsification itself easierbecause the eyebrow is not a barrier, and freermovements are possible.
Additional Patient's Comfort withCorneal Incision
Jack Dodick definitely prefers to do aclear cornea incision rather than the scleraltunnel procedure. Although he considers thatboth incisions are excellent and lead to thesame outcome, patients tend to be more com-fortable and satisfied with the clear corneaincision.
Using the scleral tunnel procedure, thesurgeon cuts into the sclera, conjunctiva,Tenon's membrane, and some blood vessels,which takes perhaps 1 to 2 weeks to heal.
Although patients do not report having muchpain, they do report a greater sense of aware-ness or discomfort for at least a week or soafter the scleral tunnel procedure. With theclear cornea incision, on the other hand, theepithelium regenerates within 24 hours, muchlike it does after a corneal abrasion. Thosepatients who undergo a clear cornea incisionreport awareness of a sandy sensation which isvirtually gone within 24 hours as the cornealepithelium is reepithelialized.
In many cases Dodick and many sur-geons have done a scleral tunnel operation thatturns out perfectly with 20/20 vision, and thepatient still complains months and maybe evenyears later of an awareness or irritation in thateye. Creating a scleral tunnel wound leaves ascar at or near the limbus (Fig. 40), whichDodick believes interferes with tear film distri-bution. Eventhough it heals beautifully, theinterference with tear flow leaves patients witha vague awareness or irritation in the eye.
With a clear cornea incision, the limbusis never invaded, and a vascular scar is nevercreated. Therefore, tear film distribution isnever disturbed. The final reason Dodickchooses the clear corneal tunnel is that it is amuch more cosmetic procedure. With thescleral tunnel incision, patients often have a redeye. No change is apparent in patients whohave had the clear cornea incision just a fewhours after the operation.
A postoperative photograph showing thebarely visible scar of the corneal tunnel inci-sion on the temporal side is shown in Fig. 95.
In Edgardo Carreño's experience,phaco through clear cornea is less traumatic,considering that there is no need for conjuncti-val dissection nor the use of cautery related toscleral tunnel dissection. There is also nopossibility of hyphema and there is less postop-

THE ART AND THE SCIENCE OF CATARACT SURGERY
166
erative inflammation because there is lesstrauma.
The postoperative cosmetic appearanceof the globe is better, the eye looks as if nevertouched (Fig. 95). The patient feels morecomfortable because there are no sutures, nocautery has been done and there is no pain. Theintraoperative time is less because several tra-ditional stages of the operation have been elimi-nated. Therefore, the cost is reduced.
Importance of the Length of theTunnel
Ideally, the part of the corneal tunnelitself should be about 1.75 mm (Fig. 93). Ashorter tunnel (dotted line in Fig. 92) decreasesthe self-sealing rate, although the surgeon'svisibility becomes better. Too long of a tunnelincreases the self-sealing, but corneal foldssometimes disturb surgeon's visibility. Cor-neal endothelial damage also becomes greateras the distance between the phaco tip and
corneal endothelium becomes shorter. Thus,when the surgeon performs a corneal incisionfor the first time, it is recommended to makea rather shorter tunnel and to place 11-0 nylonsingle knot without being concerned with self-sealing.
Placing and Making the PrimaryIncision
As emphasized by Kimiya Shimizu, theproper placement of the incision is important.If it is too anterior, the corneal tunnel becomesshorter, and the self-sealing effect is decreased.In contrast, if it is too posterior, conjunctivalbleeding and/or chemosis sometimes occur.
So, before incising the cornea, dry theincision site, make the vertical first step justanterior to the terminal conjunctival vessels,then insert and advance the keratome straightabout 1.75 mm into the corneal stroma. Next,direct the keratome slightly downwards in theiris plane to perforate Descemet's membrane.
Figure 95: Minimal Scar Following ClearCorneal Temporal Incision
With slit lamp retroillumination wecan see the very fine scar in the postoperativestage after performing phacoemulsificationutilizing a clear corneal incision done on thetemporal side of the left eye. With daylight oreven a pen light frontal illumination, this scaris barely seen. Please also observe that thescar is very regular, almost like drawn onpaper. This, of course, leads to practically noastigmatism postopertaively. (Courtesy ofEdgardo Carreño, M.D.)

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
167
When the tip of the keratome appears in theanterior chamber, remove the Merocel spongeand release the counterpressure. After that,advance the keratome, swinging it to both rightand left sides. By doing this, the incision maybe conducted safely without causing the col-lapse of the anterior chamber. The length of thecorneal tunnel is usually 1.75 mm, but if it is acomplicated or hard nucleus case, it should beshorter. On the other hand, when the patienthas good mydriasis or a shallow anterior cham-ber, the incision site should be a little anterior,and the corneal tunnel should be longer toprevent iris damage and/or iris prolapse.
Surgeon's Position
When the operator is right-handed andhe/she is operating the right eye, sit at the 10.30position. When operating on the left eye, sit at4:00.
Controversy Over the Strength andSafety of the Wound
One of the most controversial criticismsof clear corneal incisions has been their relativestrength compared to limbal or scleral inci-sions. Mackool has demonstrated that once theincision width is 3.5 mm or less and the lengthof the tunnel 1.75 to 2 mm, there is an equalresistance to external deformation in clear cor-neal incisions as compared to scleral tunnelincisions. Ernest work as well has revealedthat as incision sizes get increasingly smaller,3mm or less, the force required to cause failureof these incisions becomes very similar forlimbal and clear corneal incisions. This furtherdocuments the safety of corneal incisions.
The real issue for these various inci-sions is not healing but sealing. Fine feelsthat as long as an incision is sealed at the
conclusion of surgery and remains sealed, thetime before complete healing of the incision isaccomplished is almost irrelevant, especiallysince there is still a 6-day period in whichlimbal incisions are not healed. An analogycan be drawn to the sealing that takes placeduring LASIK, in which there is no fibrovascu-lar healing of the clear corneal interface, whichhas little effect on the strength, effectiveness,or safety of the wound, and, in fact, is anadvantage by limiting scarring and an inflam-matory healing response.
Clear corneal cataract incisions are be-coming a more popular option for cataractextraction and IOL implantation throughoutthe world. Through the use of clear cornealincisions and topical and intracameral anesthe-sia, we have achieved surgery that is the leastinvasive of any kind in the history of cataractsurgery with visual rehabilitation that is almostimmediate. Clear corneal incisions have had aproven record of safety with relative astigmaticneutrality utilizing the smaller incision sizes.In addition, corneal incisions result in an excel-lent cosmetic outcome.
Testing the Wound for Leakage
There are several methods to test the sealof the incision. For the most practical one, werefer you to Fig. 73, Chapter 7, and the explana-tory text in the same page under this title.
Closing a Leaking WoundWithout Sutures
Professor Juan Murube, M.D.(Madrid), has demonstrated the effectivenessof a very comfortable maneuver in order toclose-shut a leaking wound instead of having tosuture it. Although a self-sealing, steppedvalvulated corneal tunnel incision, 3.0 mm or

THE ART AND THE SCIENCE OF CATARACT SURGERY
168
less in size, is very unlikely to leak, there isalways the possibility for this to occur. Themain causes are related to making the cornealincision larger than 3.0 mm and excessivetrauma to the lips of the wound during surgeryparticularly with the phaco probe. These fac-tors may give rise to a continuous loss ofaqueous humor. This may be detected thefollowing day by means of a positive Seideltest in which several drops of fluorescein areinstilled over the wound and examination isperformed with ultraviolet light.
Because the aqueous humor escapesthrough the wound continuously, the wound iskept open. Unless this is corrected immedi-ately, the surgeon may have to suture the wound.
The very comfortable and effective ma-neuver recommended by Professor Murube inorder to close-shut a leaking wound is to place
a Honan balloon over the eye for 30 minutes at35 mm Hg pressure. At the same time, thepatient is administered orally one tablet of 250mg of Acetazolamide (Diamox). The way thisworks is that the significant intraocularhypotony produced by the combined use of theHonan balloon and Diamox results in theproduction of a significantly reduced amountof aqueous humor that is produced with suffi-cient continuity to reform the anterior chamberbut not in sufficient quantity to seep throughthe wound. After a few minutes, the walls ofthe wound have had a chance to adhere to eachother, thereby sealing the wound. No furtherpositive Seidel test is observed even though thenormal intraocular pressure is reestablished.This maneuver is innocuous and simple as wellas highly effective (Fig. 96).
Figure 96: Murube's Method of Seal-ing a Leaking Wound with Honan'sBalloon
The combined use of HonanBalloon’s compression for 30 minutes at35 mg Hg pressure and one 250 mg tabletorally of Acetazolamide lead to sealing ofthe leaking wound.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
169
THE ANCILLARY INCISION
This is an important step in performingphacoemulsification. Although there are tech-niques to perform phaco with only one hand,phacoemulsification is fundamentally a two-handed procedure.
The ancillary or side-port incision is madebefore the main incision. It serves as an entryfor a second instrument which is necessary formaneuvers to remove the nucleus, either nuclearmanipulators (fig. 79) or choppers (Fig. 80).The location and technique of making the an-cillary incision is shown in Fig. 41 A.
In addition to serving as the mode ofentry for the essential second instrument theancillary incision is utilized in irrigation of theanterior chamber with intracameral local anes-thetic as presented in Chapter 6 and illustratedin Fig. 36. It is also the route for the insertionof viscoelastic previous to making the primaryincision.
At the end of surgery, the ancillary inci-sion is used to inject fluid into the anteriorchamber to test for leaks in the wound, asshown in Fig. 73.
Making the Ancillary Incision
The steps involved in performing theancillary incision are:
1) First, mark the corneal location wherethe clear corneal stepped main incision wouldbe made, which is always between 9 and 12, asshown in Figs. 41 B and 42. This measureserves the surgeon for orientation as to exactlywhere to place the two incisions.
2) Make the ancillary incision at 3 o'clock.This is performed with a special 15 degreesblade designed for paracentesis (Figs. 76 and77).
ANTERIORCAPSULORHEXIS
Key Role
This procedure is also presented inChapter 7 for the transition period and illus-trated in Figs. 43, 44 and 45. It is generallyagreed that a well performed anterior continu-ous capsulorhexis is an essential step for thesuccess of phacoemulsification. The key rea-sons for being so important is that capsulorhexisprevents IOL decentration. In cotrast with theextracapsular extraction and can opener capsu-lotomy, even when the surgeon was sure thathe/she placed the IOL within the bag duringsurgery, sometimes 30 to 40% of cases aftertwo or three months would have one of the lensloops protruding out of the capsular bag andreaching to the sulcus, thereby leading todecentration. On the other hand, by perform-ing the continuous circular capsulorhexis fol-lowed by implantation of the lens within thebag, the IOL will permanently remain wellcentered within the capsular bag. This has beenemphasized time and again by EverardoBarojas, M.D., one of Mexico's most presti-gious cataract surgeons and a good number ofother experts on the subject.
The Role of Viscoelastic in CCC
One of the key steps in achieving a firstclass capsulorhexis is to do it with viscoelasticin the anterior chamber rather than with BSS.The high density viscoelastic is used not only toprotect the endothelium and other surroundingtissues but also serves as a third hand thatamplifies the working space and facilitates themaneuvers of the surgeon's manuevers. It also

THE ART AND THE SCIENCE OF CATARACT SURGERY
170
helps to flatten the anterior capsule. This lastmeasure facilitates the correct performance ofthe procedure.
Technique for Performing a FirstClass CCC
Beginning surgeons should be encour-aged to use forceps as shown in Figs. 44 and 45.All cases should be performed with injection ofviscoelastic material in the anterior chamber.The experienced surgeon may perform the pro-cedure with a cystotome-needle which is a No.26 needle with the tip bent into a square angleas shown in Fig. 97.
The CCC utilizing the cystotome needleand viscoelastic is more safely and effectivelyperformed using the central punch technique.This makes the first incision in the center, asshown in Fig. 98 and not in the periphery, aswas the tendency when the procedure wasdeveloped (shown in Fig. 43). Using thecentral punch technique, there are fewer possi-bilities that a tear will spread to the periphery.The continuation of the capsulorhexis tear,once the central punch is done, may be doneclockwise or counter clockwise, as is morecomfortable for the surgeon. Usually, it iscontinued in a circular fashion in a counterclockwise direction as shown in Fig. 99, care-fully completing a circle from outwards inwardobtaining a completely closes rhexis (Fig. 100).
It is fundamental to advance the capsulartear in a well controlled manner. This is achievedby placing the cystotome-needle against thesurface of the anterior capsule and re-graspingthe tear as many times as necessary to continuethe circular teaar until completing the circle.
A very important part of the first step inCCC is to be able to obtain the flipping of theresultant capsular flap once the cystotome-needle engages the anterior capsule centrally.
It is important for the surgeon to see the under-side surface of the anterior capsular flap asshown in Fig. 98.
Some surgeons find that in order to per-form the procedure more safely, upon finishingeach one of the circular tears with the Uttrataforceps and before completing the circle, in-stead of leaving the capsulorhexis folded, takeit back to the way it was, that is, unfolded. Thismakes the next step easier to perform, that is theanterior capsule, easier to grasp in order toengage and disengage to provide the best con-trol for creation of a circular opening (Figs. 99,100).
Size of the Capsulorhexis
For experienced surgeons mastering pha-coemulsification, it is generally advisable touse a 5.5 mm central and completely enclosedrhexis. This is close to the ideal phacoemulsi-fication technique performed safely within thecapsular bag.
The size of the capsulorhexis, however,may be better determined by the type of in-traocular lens model to be implanted. Carreñoemphasizes that upon using Alcon's foldableacrylic implant with a 5.5 mm optic, he prefersa 4.5 mm or 5.0 mm rhexis so that the edge ofthe optic is completely covered by the ante-rior capsule. This helps in preventing fibrosiswhich may be produced when both capsulescome into contact. It is also helpful in reducingglare especially in younger patients who havemore of a tendency for pupillary dilation atnight or in the darkness.
On the other hand, upon using thesilicone foldable lenses, Carreño prefers a5.0 mm to 5.5 mm rhexis to prevent contractionof the capsular sac, which may accompany thistype of implant when the diameter of thecapsulorhexis is smaller.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
171
Figure 97 (above left): Cystotome - NeedleAdjusted for CCC
The experienced surgeon often prefersto perform CCC with a cystotome-needle. Manysurgeons use a 26 gauge needle with the tip bentinto a square angle. Others use a 23 gaugeneedle. The needle is prepared with two separatebending motions as follows: 1) the tip of astraight 26 or 23 gauge needle (N) is graspedwith a needle bender (B). 2) The tip of the needleis bent downward 90º in a vertical motion (ar-row).
Figure 98 (center): Continuous Curvilinear Anterior Cap-sulorhexis Performed with the Cystotome-Needle (Step 1)
The first step is to engage the cystotome-needle intothe central region of the anterior capsule superiorly at the X andflip the resultant capsular flap over. Please observe that thesurgeon can see the underside of the capsular flap (C). Thecystotome-needle (N) engages the underside of the capsularflap (C) and moves it in the direction of the blue arrow whichin this case is counter clockwise in order to produce a circulartear in the capsule (red arrows). A fixation forceps providesstability which is essential during the performance of the CCC.
Figure 99 (below left): Continuous Cur-vilinear Anterior CapsulorhexisPerformed with the Cystotome-Needle(Step 2)
After injection of viscoelastic, thesurgeon starts with the puncture of the cap-sule and proceeds to make the first smallflap. When this first flap is turned over, thetint is clearly seen because the color is de-tected in the internal face of the capsule andnot in the epithelium.

THE ART AND THE SCIENCE OF CATARACT SURGERY
172
Another factor which influences the sizeof the capsulorhexis, is the degree of hardnessof the cataract. In cases where the nucleus istoo hard, Carreño feels that it is more prudentto perform a rhexis which is not too small,certainly no less than 5.0 mm in diameter, toease performing the phaco chop techniques,which are the most highly recommended fortreating hard nucleus.
STAINING THE ANTERIORCAPSULE IN WHITE CATARACTS
As shown in Figs. 98, 99 and 100, a wellperformed CCC allows the coaxial light of the
microscope to provide the red reflex of thefundus. Over this red reflex the anterior cap-sule and the border of the progressively per-formed continuous circular capsulorhexis canbe very well visualized. This allows the comple-tion of the circle (Fig. 100) under adequatevisual control. On the other hand, when thesurgeon is dealing with white, hypermaturecataracts that have either been allowed to getinto that advanced stage or have been producedby trauma, the details and border of the CCCcannot be well visualized because this whitecataract interferes with fundus reflex . Conse-quently, the step by step progress in the perfor-mance of the CCC is not well visualized.Accidentally, the edge of the anterior capsule
Figure 100: Continuous Curvilinear Anterior Capsulorhexis Performedwith the Cystotome-Needle (Step 3)
The cystotome needle continues to be engaged on the underside of theflipped anterior capsular flap and is moved in a direction (blue arrow) tocomplete the circular tear (red arrow). The capsular flap is then removed fromthe eye.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
173
flap could be displaced toward the peripheryand the lens equator. From here, upon perform-ing the maneuvers inherent to phacoemulsifi-cation, damage to the posterior capsule couldbe inflicted thereby allowing passage of thevitreous to the anterior chamber or a luxation ofthe nucleus into the vitreous or a displacementof the intraocular lens once inserted. Theseimportant considerations have led to the devel-
opment of a very effective technique to controlthe performance of the CCC in white cataracts.It consists in staining the anterior capsule of thelens in order to adequately visualize the detailsduring the performance of the CCC (Fig. 101).
Without the dye it is nearly impossible tosee the anterior capsule. These cataracts arerisky. It is very difficult to distinguish theanterior capsule from the underlined cortex.
Figure 101 (above right): Murube's Techniqueof Staining the Anterior Capsule in White Cata-racts to Perform Adequate CCC
White cataracts (L) present a problem be-cause the red reflex is not present making thecapsulorhexis quite difficult and risky. A vis-coelastic is first injected into the anterior chamberimmediately followed by the injection of a bubbleof air which partially displaces the viscoelasticfrom the anterior chamber. This leaves the cornealendothelium lubricated with the viscoelastic.
A hydrodissection cannula (H) is intro-duced through the corneal incision over the anteriorcapsule (C). Two drops of Trypan Blue are in-stilled. Wait for ten seconds.
Figure 102 (below left): Anterior CapsuleStained with Trypan Blue in White Cataractsto Facilitate Performance of Adequate CCC -Murube's Technique
After waiting for ten seconds, the ante-rior capsule in the white cataract is fully stained.Viscoelastic is then injected into the anteriorchamber to remove the air (air exchange). Theanterior capsule is a little blue. The surgeon cannow proceed with the capsulorhexis now that he/she sees the capsule clearly.

THE ART AND THE SCIENCE OF CATARACT SURGERY
174
Staining Substances and Methods
There is a variety of staining substancesand methods of how to perform the staining.They have been presented by prestigious oph-thalmologists since 1998: in Japan throughNagoya University School of Medicine; inSpain, Oscar Asis, M.D.; in Holland, JerritmMelles, M.D.; in the U.S., Thomas Oettingand Rick Nearhing. The most practical andeffective method now being popularized is theone presented by Prof. Juan Murube (Madrid).The different staining substances analyzed byMurube are the following:
1) Fluorescein 2%. This is obtained bymixing 1 ml of 10% fluorescein for intravenoususe with 2 ml of BSS.
2) Indocyanine Green (ICG): This isobtained by mixing 25 mg of ICG in 0.5 ml ofan aqueous solvent which might be obtainedfrom Akorn in Buffalo Grove, Illinois. Thismixture is then diluted in 4.5 ml of BSS.
3) Trypan Blue: Prepared by mixing 1 mlof trypan blue 0.4% (obtained from Life Tech-nology, Grand Island, New York) in 3 ml ofBSS.
4) Gentian Violet: solution at 0.01 con-centration diluted with BSS.
5) Methylene Blue: solution at 0.01 mixedwith BSS.
Murube's research has led him to selectTrypan Blue as the staining solution of choice.This has been confirmed through the clinicalresearch of Carlos Nicoli, M.D., in Argentina,one of South America's top phacoemulsifica-tion surgeons. Nicoli emphasizes that Methyl-ene Blue and Gentian Violet are very difficultto prepare because they must have very spe-cific concentrations. It is fundamental that thestain used not be toxic to the corneal endothe-lium. Therefore, it should be prepared at ex-actly the right concentration. For instance,
Methylene Blue, if used, should be a 1% solu-tion while Gentian Violet should be at one partper thousand. The new research by the Japa-nese in Nagoya refers to the use of 0.05%Indocyanine Green solution. The problemwith the latter is that it is very costly. TheTrypan Blue solution is being currently mar-keted as a nontoxic stain.
Technique for Injection of Stain-ing Solutions
Murube first irrigates a viscoelastic intothe anterior chamber. This is immediatelyand partially displaced by an air bubble inthe anterior chamber in order to leave thecorneal endothelium slightly lubricated andprotected by the viscoelastic. A cannula isinserted through the corneal incision as shownin Fig. 101 and two drops of Trypan Blue aredeposited over the anterior capsule. The sur-geon waits ten seconds. This is followed byinjection again of viscoelastic in order to elimi-nate the air bubble from the anterior chamber,the so-called "air exchange". At this timetinting is not yet detected until the first flap ofthe rhexis is done because the tissue absorbingthe tint is not the capsular epithelium but theinternal face of the capsule, visible enough forthe surgeon to see the capsule very clearly andto proceed to perform the capsulorhexis ad-equately. Utilizing this technique, when per-forming the capsulorhexis (Figs. 98, 99, 100)the surgeon can see that the epithelium behindthe anterior capsule is selectively stained. It isimportant to keep in mind that the epithelium isbehind the anterior capsule. When the surgeonlifts the flap gently, he/she can see the epithe-lium perfectly stained so he/she may safelyproceed to complete the capsulorhexis.
This technique is considered of greatvalue, a breakthrough in this step of phacoemul-sification.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
175
HYDRODISSECTION -HYDRODELAMINATION
This next step is of great importance. Itsobjective is to separate the capsule from thecortex and the cortex from the nucleus (Figs.46, 47, 48). Its significance is related to theliberation of the adherences which attach thenucleus to the cortex or the cortex to the cap-sule, facilitating aspiration (Figs. 1, 46, 47, 48).The hydric chamber created withhydrodissection also plays a role in the protec-tion of the posterior chamber and the posteriorcapsule during the phacoemulsification ma-neuvers.
Technique of Hydrodissection
Using a 3 ml syringe with a maximum of1.5 ml infusion fluid, a 25 G flat tip cannula isintroduced underneath the capsulorhexis (Fig.78-A). Following Fine and Centurion's rec-ommendations, the anterior capsule is raisedand BSS is infused with light pressure. Thefluid will distribute itself along the posteriorcapsule and will drain through the oppositeside. The liquid wave can be seen in the centerof the red reflex (Fig. 46, 47). This process isrepeated at 6, 3 and 9 o'clock keeping in mindthat after infusing, we should press the cataractagainst the capsule to avoid elevation of pres-sure within the capsular bag.
After the liquid wave reaches the area ofthe pupillary opening, the syringe is with-drawn and the center of the nucleus is com-pressed in an attempt to release the adherencesof the cortex to the capsule on the side opposite
to where hydrodissection was begun. After thismaneuver, the surgeon attempts to rotate thenucleus. If the nucleus was released by com-plete hydrodissection, it will rotate freely. Ifthere is no rotation, try a new hydrodissectionlocated opposite the site of the initial one.Centurion recommends that after the nucleusis released, it be rotated four or five times 360º.This releases possible cortex or epinucleus orcapsule adherence. Thus, at the end of nucleusemulsification there is practically no need toaspirate cortical remains.
Following hydrodissection, it is essentialto confirm that the nucleus is completely sepa-rated from the cortex before proceeding withthe next step, which is management of thenucleus with the different phaco techniques.(For the do's and particularly don'ts related tohydrodissection, it is important to read the texton this subject in Chapter 7, next to Figs. 46, 47,48).
Hydrodelamination
Hydrodelamination is the separation ofthe nucleus from the soft epinucleus (Fig. 48).This technique is done after completinghydrodissection. The same needle (Fig. 78-A)is introduced beneath the cortex and into thelens stroma while infusing BSS, which willdelaminate sheets of cataracts, isolating thenucleus from the epinucleus, forming the goldenring (Fig. 48 GR).
With present techniques, many surgeonsdo not used to perform hydrodelamination fol-lowing a very well done hydrodissectgion.They remove the epinucleus usually during theemulsification of the nucleus.

THE ART AND THE SCIENCE OF CATARACT SURGERY
176
MANAGEMENT OF THE NUCLEUS
General Considerations
At this stage, we proceed with the culmi-nating phase of the operation. The previousmethods of emulsification of the nucleus firstwithin the anterior chamber and later in the irisplane are somewhat outmoded with the excep-tion of the supracapsular otherwise known asthe “tilt and tumble” iris plane technique, whichis still Lindstrom’s first choice. It is lessdemanding. At present, though, the most oftenused phacoemulsification techniques in han-dling the nucleus are performed in the posteriorchamber within the capsular bag. These areall identified as endocapsular techniques.They have the advantage of reduced risk ofdamaging the endothelium. They also enablethe surgeon to work with a larger opening in thecapsulorhexis which is definitely useful in pa-tients whose pupillary dilatation is not ad-equate. These methods have the disadvantagethat nucleus manipulation is done closer to theposterior capsule and more stress is placed onthe zonular fibers, to their consequent risk.
The almost universal use of endocapsu-lar phacoemulsification has been made pos-sible because of innovations in technique andequipment.
Concepts Fundamental to AllTechniques
Surgical Principles
Almost every contemporary cataract sur-geon uses some form of chopping, and allsurgeons who perform chopping use some formof ultrasound to facilitate the chop. Whether itbe a groove-and-chop, divide and conquer, or atechnique like Fine's quick chop (the choo-
choo chop and flip technique presented in Figs.122- 126), some form of ultrasound is used forchopping.
All modern techniques are oriented to-ward breaking up or disassembling the nucleusto facilitate its removal from the eye. Thesetechniques, which rely on mechanical energy,have been developed to reduce the amount ofultrasound energy necessary to break up thehard part of the lens nucleus. In addition,disassembling the nucleus removes it from thecapsular recesses of the bag, thereby facilitat-ing its removal with the phaco probe.
Nuclear disassembling techniques usesome ultrasound at the beginning of the proce-dure to create multiple troughs or grooves. Asecond instrument such as a spatula or choppercan then be used to crack or break the nucleus.
In this chapter we present the three groupsof techniques mostly used in advanced pha-coemulsification methods for nucleus removal.You will find the fundamental concepts whichare applicable to all methods and a descrip-tion of the principles that make these methodshighly successful, all of which have been de-veloped by highly prestigious cataract sur-geons. It is by understanding these conceptsthat the surgeon will be able to develop one ortwo essential techniques and use them as themethods of choice adapting his/her chosenprocedure to virtually any situation and thedifferent types of cataract encountered, eithersoft, standard or medium-density and the veryhard cataract.
The surgeon will find in this Volumeprecisely what he needs to understand and toadopt the method which he feels more comfort-able with and most suitable for his patients. Ifa more complete description of the techniques

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
177
available is desired, we suggest that you referto the carefully selected, short list of recom-mended books and bibliography presented atthe end of the chapter for the method's origina-tors and proponents.
The Essential Principles
1) A general principle for all techniquesto remove the nucleus in phacoemulsification,either the original four quadrants divide andconquer and its derivative divide and conquer(D & C) methods, and the relatively recentchopping techniques is that it is first essential todebilitate the core of the nucleus so that thenucleus can be split into halves, sometimesfourths (Figs. 67, 103 through 106) and occa-sionally into eighths. This allows emulsifi-cation and aspiration of nucleus segments(Fig. 105) instead of attempting to carve theentire nucleus without a planned strategy. Thissplitting of the nucleus is safer for the endothe-lium because it is easier to keep smaller par-
ticles away from the endothelium without hav-ing to push them against the posterior capsule.These essential principles are illustrated in Fig.103 (The Cracking Effect), Fig. 104 (The Di-viding Effect through Opposing Forces), Fig.105 (The Slicing Process) and Fig. 106 (theDividing Process).
2) Smooth sculpting which avoidsnuclear movement and zonular stress is criti-cal to all methods. Well-controlled deep andcentral sculpting facilitates cracking in seg-mentation methods and rim removal in one andtwo-handed methods. By using just enoughultrasound power to embed the phaco tip andthen backing off to the I/A position (standardpedal position 2), the nucleus can be positivelyengaged for rotation and manipulation. Thisversatility of the phaco tip is especially impor-tant for one-handed techniques as well as chop-ping techniques.
The principles of mechanical advan-tage apply to all methods; safety is maxi-mized by using the minimum force and move-ment required to accomplish a given task.
THE ENDOCAPSULAR TECHNIQUES
THE HIGH ULTRASOUND ENERGY AND LOW VACUUM GROUP
THE GROOVING AND CRACKINGMETHODS
The Divide and Conquer FourQuadrant NucleofractisTechnique
The first group of endocapsular opera-tions was based on the principle of utilizinglarge amounts of phaco energy and low vacuum.
The classical and less complicated techniqueof this first group is the Four Quadrants"Divide and Conquer" described in 1987 byHoward Gimbel. The principles of this methodare presented and described in figures 56 and67 in Chapter 7. In order to debilitate andremove the nucleus, a linear vertical sulcus orgroove is done in the nucleus from 6:00 to12:00 o'clock and a second groove perpendicu-lar to the first is done, both using the pha-coemulsifier probe. The carving of these fur-rows results in the nucleus being seen with across as shown in Figs. 56 and 67. A second

THE ART AND THE SCIENCE OF CATARACT SURGERY
178
Figure 103 (above right): Pha-coemulsification - Cracking Effect
Once the desired thinning ofthe nucleus core is done (a furrow or acrater), a second instrument, a chopperor a manipulator is used to divide (ar-rows) the nucleus in half pulling theinstrument from periphery to the cen-ter. The phaco tip is impaled on oneside of the already deep groove and themanipulator in the equator of thenucleus, adjacent to the tip. The depthat which the phaco tip is impaled is 1.5times the width of the phaco tip.
Figure 104 (below left): Phacoemulsifi-cation - Dividing Effect
Opposing force (arrows) is appliedto both sides of the cracking with the phacoprobe and the help of the chopper. Divid-ing the nucleus in small pieces will facilitateits removal with the phacoemulsifier em-ploying less ultrasound and higher vacuum.
instrument known as the "manipulator" whichis introduced through the ancillary or side portincision engages the opposite side of the grooveinferiorly (Figs. 67 and 79). The phaco tip isimpaled on one side of the already deep grooveand the manipulator on the opposite side of the
sulcus (Figs. 103 and 104) Both must bepositioned beyond half the depth of the groove.The sulcus should have been carved with awidth equal to 1.5 diameters of the phacosleeve. The depth at which the phaco tip isimpaled is 1.5 times the width of the phaco tip(Fig. 103).

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
179
Cracking the Nucleus
Force is applied with the instruments inopposing directions in order to crack the nucleusalong the length of the groove (Figs. 103, 104,106 below). Additional manipulations of thistype further lengthen and deepen the cracks.The lens is rotated 90º within the capsular bagand a crack is made in the second groove in thesame manner. The need to rotate the lens 90º,which is done in all techniques of phaco, isbecause the maneuvering by the surgeon isalways done in the lower half of the field.Doing such maneuvering in the upper half istechnically very difficult and cumbersome.
In the Divide and Conquer technique, themaneuver of rotating the nucleus 90º is re-peated three times until the nucleus becomesdivided in four sections (Figs. 67 and 105).After this is done, the lens fragments are emul-sified as shown in Fig. 67. The apex of each of
the four loose quadrants is lifted with the ma-nipulator and the ultrasound phaco tip is em-bedded into the posterior edge of each segment(Fig. 105). By means of aspiration the surgeoncentralizes each quadrant into the phaco tipand proceeds to emulsify each piece, whichrequires the use of a somewhat high amount ofultrasound power. When operating on a softercataract, these fractured pieces are reasonablylarge, perhaps several clock hours in diameter,and as they are broken free they are emulsifiedimmediately.
In very dense cataracts, the piecesshould be much smaller. These pieces areleft in place until the surgeon has worked allthe way around the nucleus, so that as the rimis manipulated and spun around, the capsularbag will stay fully expanded as the nuclear rimis manipulated and spun around. Only afterthe last piece is broken are they removed byemulsification.
Figure 105: Phacoemulsification - Slicing Pro-cess
This cross section view shows the pha-coemulsification probe removing the nucleusfragments within the capsular bag. Note the apexof one of the fragments created in the nucleusbeing lifted with the second instrument (arrow)and the ultrasound tip embedded into the posterioredge of each segment ready for emulsification.The epinucleus and cortex will then be removedduring the phaco process. If we operate on a softercataract, the freed fractured pieces are emulsifiedimmediately.

THE ART AND THE SCIENCE OF CATARACT SURGERY
180
Relation Between Divide and Con-quer and the Continuous Circular Cap-sulorhexis
As pointed out by Paul Koch, M.D., thenuclear fracturing divide and conquer tech-niques developed initially by Gimbel and allthe phacoemulsification techniques that aredesigned to move the nucleus through the cap-sulorhexis are in part possible because of thedevelopment of the continuous circular capsu-lorhexis that Gimbel and Neuhann originatedindividually (Figs. 43-45, 98, 99, 100). TheCCC made nearly obsolete all the existingphacoemulsification procedures, because eachof them required that the nucleus be prolapsedout of the capsular bag for each removal, eitherin the iris plane or in the anterior chamber(although the iris-plane tilt and tumble tech-nique is still used by Lindstrom with signifi-cant success - Editor). Now that the capsularbag could be kept intact with a very strong formof capsulotomy, new techniques were neededto get the nucleus out of the bag. The mechani-cal fracturing of the lens causes extra physicalstress within the capsule and cannot be donewithout great risk of tears of the anterior cap-sule extending around posteriorly unless wehave a proper CCC. There is an interdepen-dence of these techniques.
Principles of the Divide and ConquerTechniques
Gimbel developed the Divide & Con-quer techniques to meet the challenge and theopportunity created by the CCC: to operate
within the capsular bag. There are actually twosubdivisions: the trench Divide & Conquer andthe crater Divide & Conquer, but they bothfollow two very simple principles:
1) Weaken the radii of the nucleus. Thiscreates a space in the middle of the cataract inwhich other instruments can be introduced toforce (crack) apart the sections of the nucleus(Figs. 56, 67, 103, 104, 106).
2) Break apart the nuclear parts includingthe rim of the nucleus (Figs. 104, 105, 106).
Koch has pointed out that the distinctionbetween a trench and a crater is not clear-cut.There is actually a continuum extending fromtrue trench to true crater.
The Role of D & C Techniques inCataracts of Different NucleusConsistency
Softer Cataracts (Trench D & C)
Softer cataracts need preservation offirm tissue so that the cataract can be manipu-lated. If we remove much of the central nucleus,all of the firm tissue would be removed, andany attempt to manipulate it would be difficult.The instruments we use would go like throughcheese in the remaining soft tissue. Some of therelatively hard central core is necessary toresist the instruments, give them something topress against, and, ultimately, something tomanipulate. Recognizing this, Gimbel recom-mended the creation of a trench that is really anarrow pass down the middle of the cataract.This freed up a little space, but preserved wallsof central nucleus for manipulation. The trenchD & C is indicated for softer cataracts.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
181
Dense Cataracts (Crater D & C)
In these cases the strategy is entirelydifferent. We want to remove as much of thehard center core of the cataract as possibleduring this sculpting phase, leaving only a thinand soft nuclear rim for later removal. Forthese cataracts, a crater Divide and Conquer isrecommended when using D & C techniques.
The nucleus is held in place firmly in thebag. We can sculpt into the cataract with theultrasound energy and remove all of the hard,dense nuclear core without the cataract mov-ing. That keeps the phaco tip and all of thedebris far away from the endothelium andallows safe and extensive nucleus removal. Italso allows us to stay away from the posteriorcapsule.
As pointed out by Paul Koch, M.D., wecan judge the depth of the sculpting from fairlydistinctive changes in the red reflex. The firstclue to depth is the color of the cataract. Wenormally begin with a red reflex, but as soon aswe start emulsifying the epinucleus, the reflexchanges and becomes either burgundy or gray.As we sculpt down toward the middle of thecataract, we reach the gray center, and as we getthrough that, the reflex starts turning burgundyagain (Fig. 69). Once we reach the posteriorepinucleus, the color is back to red.
If we monitor the color changes as wesculpt, we can work our way very deep into thecatarac t without the risk of cutting the poste-rior capsule. We slow down as the colorbrightens.
The primary goal of crater creation isto remove the very dense nuclear core, leavingonly a much softer nuclear rim, thereby con-verting the cataract from a dense one into a softone. The secondary goal is to create a space
below the level of the anterior capsule intowhich the rim tissue can be pulled for emulsi-fication. (Editor’s Note: this technique is notto be confused with the original crater-bowlprocedure used years ago).
Steps Following the Trench or theCrater D & C
Once the nucleus is prepared with eitherthe trench or the crater, the nuclear rim isbroken apart using a unique and clever methodof fracturing it. The phacoemulsification tip isdriven into the remaining broad nuclear rimand held there with aspiration. A Barraquerspatula or manipulator (Fig. 79) is placed nextto the phaco tip and poked into the rim rightnext to it (Fig. 67). The two instruments areseparated, breaking the rim apart (Fig. 104).The nucleus is rotated around a bit, reengagedwith th e phaco tip and the Barraquer spatula,and broken again (Fig. 106 below).
Present Role of Original FourQuadrant Divide and Conquer
The original, four quadrant "Divide andConquer Technique" illustrated in Figs. 56 and67, 103, 104 and 106 below is now the tech-nique of choice for those surgeons who are lessexperienced and are converting from plannedextracapsular surgery to phacoemulsification.It is the easiest method. The debilitation of thenucleus is achieved by high doses of ultrasoundenergy and the "eating" or emulsification of thequadrants also requires high ultrasound en-ergy. For this reason we included this tech-nique as the one of choice in Chapter 7 thatcovers the stage of Transition.

THE ART AND THE SCIENCE OF CATARACT SURGERY
182
The original four quadrant divide andconquer technique has the significant impor-tance of having served as the basis for theproliferation of many variations of the divideand conquer. Many of them are still useful. Italso provided the insight needed for the
Figure 106: Phacoemulsification - DividingProcess Chopping vs Divide and Conquer
(Top) The opposing forces in the chop-ping techniques are shown in vertical arrows.Please observe the chopper (Fig. 80) biting thenucleus fibers from the periphery towards thecenter, with phaco tip deeply impaled creatingfixation and steadiness of the nucleus. This issincronized move of the phaco probe and thechopper. (Below) Shows the opposing forces(arrows) cracking the nucleus after the deepgroove has been made with the ultrasound(D & C technique). In this stage, the movementis from the center to the periphery (arrows).
development of the chopping techniques, be-ginning with Nagahara's Phaco Chop. Thelatter, though, are based on different prin-ciples and constitute the group of low ultra-sound energy - high vacuum procedureswhich at present are the techniques of choice.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
183
THE LOW ULTRASOUND ENERGY ANDHIGH VACUUM GROUP
sharp needles to engage and cut nuclear mate-rial. The aspiration mode played a secondaryrole, after the material had been emulsified.
The trend now is the opposite, that is, touse low ultrasound power and high vacuum.These chopping techniques emphasize the as-piration aspect while the ultrasound power isutilized as an aid to fragment the hard portionsof the nucleus and to facilitate aspiration of thenuclear material. This is a significant advancewhich allows much more control by the sur-geon.
In all modern techniques, the surgeonuses only sufficient but very small amounts ofultrasound power to fragment the nuclear ma-terial that is occluding the tip of the phaconeedle. The advances in technology that havemade this possible are presented in Chapter 8,under “Emulsification System,” and illus-trated in Fig. 85.
The techniques described in the first groupare known as the grooving and cracking meth-ods. Now it is important for the surgeon toevolve into the second group, which are thechopping methods, because chopping enablesyou to reduce ultrasound energy in the eye byusing greater mechanical forces - mechanicalforces that will not harm the eye. I. HowardFine, M.D., emphasizes that the easier we canmake it to help surgeons transition to chopping,the better we will be serving our patients.
Innovations in technique have under-gone a rapid and important evolution driven byadvances in technology. At the time when theinitial four quadrant technique was introducedby Gimbel in 1987, the early phacoemulsifica-tion machines vibrated at a constant powerwith constant aspiration requiring the use of alarge amount of ultrasound power in order toobtain rapid sculpting of the nucleus using
THE CHOPPING TECHNIQUES
They are all based on the concept of thePhaco Chop technique initially devised byNagahara in 1993. Since then a multiplicityof techniques that stem from the principles ofthe phaco chop have been developed but areless complex than the original Phaco Chop.
The lens substance, including the nucleus,has a concentric lamellar and radial structure.It can be fractured along the direction of thelens fibers that run from one side of the equatortowards the opposite side, passing through thecenter of the nucleus (Fig. 106 above).
Main Instruments Used
In the chopping techniques, two instru-ments are utilized: 1) the phaco chopper intro-duced through the ancillary or side port inci-sion, which serves as an ax (Fig. 80). Thephaco tip serves as a chopping block (Fig. 106above). The nucleus is easily fractured with thephaco chop technique. The latter is more effec-tive for standard to moderately hard nuclei thana soft one.

THE ART AND THE SCIENCE OF CATARACT SURGERY
184
Surgical Principles of the OriginalPhaco Chop
The surgical principle of the originalphaco chop technique is first, after hydrodis-section, the phaco tip is placed into the eye andtouches the nucleus as far superiorly as pos-sible, inside the limits of the capsulotomy.Using a quick burst of phaco energy the tip isburied securely into the nucleus.
The chopper is inserted through the side-port incision, and placed on the nucleus as farinferiorly as possible, again right inside thecapsulotomy. It is buried right into the cataractand then pulled up toward the phaco tip, divid-ing the cataract . This technique, which was thebasis for all chopping techniques that laterdeveloped, presented two problems: unlikeprevious experiences with Divide & Conquerand In-Situ Fracture, there was no space in themiddle of the cataract for manipulation. Whenthe surgeon finished chopping the four quartersand was ready to emulsify one of them, he hadno room to allow it to slide toward the phacotip. It was wedged in place in the capsular bagand did not move easily.
The surgeon had to engage the fragmentand pull it into the anterior chamber for re-moval, converting the case from one that waspurely endocapsular, to one that was three-quarters endocapsular and one-quarter ante-rior chamber phaco.
The surgeon had divided the nucleusinto fragments, but had no space for maneuver-ability in order to remove them.
Even though the Phaco-Chop techniqueof Nagahara initiated a new era in phacoemul-sification, the original procedure had to bemodified in order to overcome the problemshere outlined.
Chopping Techniques Presentedin this Volume
From the large variety of chopping tech-niques now available, we have chosen five forpresentation in Chapters 9 and 10. They wereall originated by highly prestigious, experi-enced phacoemulsification experts and repre-sent the direction in which this surgery is ori-ented. These procedures are: 1) The Stop andChop (Paul Koch); 2) The Crater PhacoChop (MacKool); 3) The Null Phaco Chopalso referred to as Pre-Slice (Jack Dodick); 4)The Choo-Choo Chop and Flip (I. HowardFine). 5) The Stop and Karate Chop Tech-nique as advocated by Edgardo Carreño, oneof the top phaco surgeons in South America.His insights are somewhat different than thetop surgeons in North America.
THE STOP AND CHOPTECHNIQUE
Surgical Principles
This is the main variation of the phacochop technique. It is widely used, and waspopularized by Paul Koch. Its most importantcontribution is that it facilitates one of thesignificant difficulties encountered with theoriginal phaco chop which is the fragmentingof the first half of the nucleus and removal ofthe first fragment.
A superior quality CCC and a goodhydrodissection are fundamental before man-aging the nucleus, as in all other phaco opera-tions. After the hydrodissection is completed(Figs. 46-48, 78-A), Koch usually does notperform hydrodelineation for this procedure,

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
185
because he is able to chop the nucleus into bite-sized pieces. Because he constantly pulls piecesinto the middle of the capsular bag, he does notneed the cushion of epinucleus. All he wouldbe doing if he created one would be adding onemore step at the end -- removal of epinucleus.
Koch's method is to sculpt a centralgroove as if we were doing the classical Nucle-ofractis or divide and conquer technique butonly one groove is done and not the classicalcross. This creates a space in the center (Figs.107, 108) which is essential for nucleus ma-nipulation. In softer cataracts, the surgeondoes a lighter furrow or trench while in thestandard two to three plus or even four plus
cataracts, a center crater is done instead of afurrow.
The deep nuclear sculpting is performedfrom 12 o'clock to 6 o'clock, creating a verticaltrough (Fig. 107). A second instrument de-signed for phaco chop (chopper) is insertedthrough the ancillary incision (Figs. 108, 80).The chopper is inserted underneath theanterior capsular edge in the lower right quad-rant (Fig. 108), advanced out to the peripheryof the capsule (Fig. 109), embedded in theperipheral nucleus (Fig. 110), and pulled backto the central groove. This creates a small freewedges of nucleus, which are easily emulsifiedand aspirated (Fig. 111).
Figure 107: Stop and Chop Technique -Stage 1 - Sculpting the One Central Groove
After instillation of viscoelastic, thephaco probe is introduced through the primaryincision size (3.2 mm) at 10.30 o'clock and thechopper at 3 o'clock. This side view showshow the phato tip is impaled in the lens sub-stance, sculpting a central groove as if we weredoing the classical nucleofractures but onlyone groove is done and not the classical cross.This creates a space in the center which isessential for nucleus manipulation. The groove(G) is extended toward the periphery of thenucleus with the phaco probe (P). This maneu-ver debilitates the central core of the lenspermitting its easier fracturing with the chop-per.

THE ART AND THE SCIENCE OF CATARACT SURGERY
186
Figure 108 (above right): Stop and Chop Tech-nique - Stage 2 - Insertion and Role of SecondInstrument
Once the groove has been sculpted deepenough (half the diameter of the phaco probe) in the12 o'clock to 6 o'clock direction, the second instru-ment (chopper) is inserted through the ancillaryincision and placed underneath the anterior capsu-lar edge in the right lower quadrant. It is thenadvanced out to the periphery of the capsule, em-bedded in the peripheral nucleus and pulled back tothe central groove, creating small free wedges ofnucleus which are emulsified.
Figure 109 (center): Stop and ChopTechnique - Stage 3 - Rotation of theNucleus
A space had been produced forthe ultrasound tip and the ancillary chop-per to fracture the nucleus. The surgeonstops, rotates the nucleus through 90 de-grees, fixates the lower half of the nucleuswith the ultrasound tip and creates a crackwith the hook exherting traction in theopposite direction.
Figure 110 (above right): Stop and Chop Tech-nique - Stage 4 - Creating Free Wedges of Nucleus
The same piece of nucleus is again stabi-lized with the phaco tip while the chopper isadvanced out to the periphery and pulled centrally.The surgeon uses the chopper (C) to crack therotated nucleus in small pieces starting at the pe-riphery. Observe how the chopper is pulled fromthe 6 o'clock position under the capsulorhexis to-wards the center while the phaco probe (P) maintainsthe nucleus in a fixed position for firm support.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
187
Fracturing of the Nucleus
The ultrasound tip and the ancillary chop-per fracture the nucleus into two parts byexerting force toward each other. The surgeonholds the ultrasound tip steady, which serves asthe firm block holding the nucleus and thechopper slices the nucleus from the peripherytowards the center of the nucleus. Numerousbites are performed with the choopper creatingsmall free wedges to be emulsified (Fig. 111).
Fixating, Rotating and CreatingSmall Free Wedges of Nucleus forEmulsification and Aspiration
At this point, the surgeon stops, rotatesthe nucleus through 90 degrees (Figs. 108, 109,110). He fixates the lower half of the nucleuswith the ultrasound tip and cracks it with a
hook, exerting force toward the ultrasound tip(Figs. 111, 106 above). The same piece ofnucleus is again stabilized with the phaco tip,while the phaco chop instrument is advancedout to the periphery and pulled centrally(Figs. 110, 111), creating another small freewedge of nucleus for emulsification and aspi-ration. The process is repeated until the entirefirst nuclear half is removed. The other nuclearhalf is rotated into the inferior capsular bag,and the entire process is repeated (Figs. 108through 111).
From these four initial fragments, whichcan be easily mobilized from the capsular bag,each piece is further divided into smaller piecesand eaten with the ultrasound. Thereby, theimportance of the burst action in the phacomachine, because the surgeon cuts small piecesand emulsifies, again cuts small pieces andemulsifies them (See Chapter 8 for Burst Modeand Pulse Mode). The whole procedure occurswith no sculpting .
Figure 111: Stop and Chop Technique- Stage 5 - Chopping and Emulsifica-tion
At this point the inferior half ofthe nucleus has been cracked and beginsto be emulsified. With the chopper thesurgeon pulls from the periphery towardthe center to divide and create additionalsmall free wedges of nucleus which arethen emulsified and aspirated. The pro-cess is repeated until the entire remainingnuclear half is removed.

THE ART AND THE SCIENCE OF CATARACT SURGERY
188
This is the essence of the stop and chop,one of the most important of the advancedtechniques.
Absolute Requirements toPerform the Stop and Chop
Although this technique is much lesscomplex than the original phaco chop, in orderfor it to be successful, the following principlesmust be attained:
1) Hydrodissection: this stage of theprocedure must be very well done (Figs. 46-48,78-A). A great deal of the success of thistechnique depends on the ability to easilymobilize the nucleus (Figs. 108-110). Wemust be sure that the nucleus can be completelyrotated before beginning its phacoemulsifica-tion. The ease with which the nucleus can berorated depends on a very well done hydro-dissection. Before beginning phacoemulsifi-cation of the nucleus, the surgeon should ro-tate the nucleus two or three times inside thebag. If the rotation is not easy, then there wasa failure in the hydrodissection maneuver. Thesurgeon must not attempt to mobilize thenucleus mechanically or by force.
2) The Initial Groove: done to createthe space inside the nucleus for it to befractured (Figs. 107 - 108). This groove mustbe well done to be useful. It allows thesurgeon to free the two sectors easily (Fig. 106above).
3) Fracturing the Nucleus: when thesurgeon has reached a good depth with the twoinstruments, that is, the phaco tip and the ma-
nipulator or chopper, he should attempt tofracture the nucleus (Figs. 103, 104, 106 above).It is easy to split the nucleus into two partsbecause the chopper or manipulator does abetter job separating the nucleus halves thanthe olive tip spatula previously used for thispurpose. If there are difficulties and the frac-ture line is not seen, the initial groove in thecenter of the nucleus can be deepened but thesurgeon must pay great attention to the color ofthe red reflex to be sure he/she is not too closeto the posterior capsule.
The fracture of the nucleus into two partsfirst is the key to the success of the operation.Only after this will the surgeon be allowed toproceed making smaller free segments orwedges by additionally fracturing with the chop-per (Fig. 111).
Fracturing with the chopper dependslargely on the instrument insertion depth. Nor-mally, the phaco probe and tip as well as thechopper should be inserted at a depth about2/3 the diameter of the phaco tip. Once thenuclear fragments have been made, the proce-dure is continued with the usual maneuvers(Figs. 105 - 111). At the end of nuclear re-moval, there is a small quantity of residualmaterial which is then aspirated.
Importance of the PhacoChopper
This ancillary instrument is absolutelyessential to perform the chopping technique.There is a large variety of these phaco chop-pers. They all look like a golf club and the most

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
189
effective ones have a somewhat sharp point1.5 mm in length (Fig. 80). In figures 103through 121 you may observe the chopperbeing used in different techniques. The chop-per is inserted through the side port or ancil-lary incision. The hook or chopper is posi-tioned at 6:00 o'clock underneath the anteriorcapsule as far peripheral and deep as possible(Figs. 105, 110, 111). The shape of the pointis most important. We can chop a soft nucleususing a sharp point; a wedge shaped tip facili-tates chopping of a hard nucleus.
Highlights of the Stop and ChopTechnique
1) It provides excellent stabilization ofthe nucleus by fixation with the phaco tip andslicing and biting with the chopper. The latterhas more of an active role in the procedure thanthe ancillary instruments in other endocapsulartechniques. The surgeon uses the two hands inharmony during the entire phaco nuclear re-moval.
This also means that the surgeon shouldpay very close attention to the chopper, whichneeds as much control as the ultrasound tip.
2) Throughout the entire procedure, theultrasound energy transmitted to the nucleus isnot transmitted to the epinucleus and the cor-tex. Therefore, it is not passed on to theposterior capsule and the zonules because it is
absorbed by the external cortex and the separa-tion induced through hydrodissection
3) How useful is this procedure is incataracts of different nuclear consistencydepends on the ability of the surgeon to adapthis technique to the type of cataract he/she isoperating. The size of the nuclear wedgescreated can vary based on nuclear consistency.This technique is even useful in hard nucleiusing less ultrasound and more aspiration. Hardnuclei require smaller wedges while softernuclei can yield with larger wedges.
The stop and chop technique is useful inmost cataracts with different consistency:in hard nuclei, in soft and in cataracts withnuclei of standard consistency. It is a methodthat lends itself to wide use. There is greaterease in dealing with very hard nuclei ascompared with most other techniques.
4) The advantages of this procedure overthe conventional divide and conquer methodsinclude reduced stress on the capsular bag andzonular fibers because the use of the choppersimplifies the fracture.
5) The operation decreases phaco time.6) It creates less turbulence and conse-
quent complications.7) Any remaining epinucleus and cortex
is removed in standard fashion.8) By dividing the nucleus in two halves,
the stop and chop technique facilitates the moredifficult maneuvering encountered by the sur-geon in phaco chop.

THE ART AND THE SCIENCE OF CATARACT SURGERY
190
FUNDAMENTAL DIFFERENCES BETWEEN CHOPPINGTECHNIQUES AND DIVIDE AND CONQUER (D & C) TECHNIQUES
The two main groups of techniques uti-lized in modern, endosacular advanced meth-ods for managing of the nucleus in phacoemul-sification are the chopping techniques and itsderivatives and the cracking techniques (divideand conquer and its derivatives). There arefundamental differences in regards to theirsurgical principles.
Chopping tends to stabilize the nucleusbetween the phaco tip and the chopping instru-ment. Furthermore, mechanical force is di-rected centripetally as the chopping instrumentcleaves the nucleus (Fig. 106 above). There-fore, minimal force is directed outwardagainst the capsule periphery. This is incontrast to cracking methods, during whichthe nuclear periphery is pushed outwardagainst the capsule by the cracking instruments(Figs. 104, 106 below). As a consequence, anydefect in the capsulorhexis is at greater risk andmay have a tendency to extend to the peripheryand posteriorly with cracking as opposed tochopping.
Chopping is also a more productivemethod than cracking with respect to the needto use ultrasound power because chopping usesmechanical force for nuclear segmentation asopposed to sculpting grooves which are donewith ultrasound, even though modified D & Ctechniques do allow the use of low total ultra-sound energy because it is not used continu-ously.
Ultrasound is used more efficiently dur-ing chopping because it is applied in the moreeffective occlusion mode.
Finally, chopping is a more time produc-tive method than cracking in that a segmentingchop can be made with a single instrumentmovement (Figs. 104 above, 111) as opposedto multiple ultrasonic sculpting passes requiredfor a groove (Figs. 56, 67). Also, the smallerchopped fragments are more readily emulsi-fied with less repositioning required as com-pared to larger quadrants.
In the chopping techniques, the chop-ping direction is from the equator to the center(Fig. 104 above). In the divide and conquerprocedures, the cracking is from the centertoward the equator (Fig. 104 below). There-fore, in the divide and conquer procedures, thesurgeon must begin sculpting the center of thenucleus and debilitating the nucleus at thatstage, making a trench or a crater with ultra-sound to start the cracking from the center,as shown in Figs. 106 below, and 104. In thechopping techniques, the surgeon sticks thephaco tip into the nucleus and insert the phacochopper into the space between the equator andthe capsule at the 6 o'clock position (Figs. 105,110, 111). Then the phaco chopper is drawn tothe phaco tip to crack the nucleus. There is noneed of sculpting during this stage of the proce-dure which is the reason why the phaco energycan be significantly reduced.
Sculpting with the ultrasound energy isthe easiest and safest step of the operation andthat is why we recommend the divide andconquer original four quadrant technique forthe transition. There is no ultrasound sculptingin the stop and chop.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
191
THE CRATER PROCEDURES
The Crater Divide and Conquer(Mackool)
This procedure is based on Gimbel'sDivide and Conquer surgical principles. It isa modification of the original four quadrantdivide and conquer. Because it is used mostlyfor hard nuclei, the center of the nucleus isweakened in the shape of a small crater byapplying ultrasound energy and proceeding tocrack the nucleus in two halves. This is fol-lowed by further cracking into four piecesusing the ultrasound energy with the help of theancillary instrument. The pieces are then emul-sified.
The Crater Phaco Chop for Dense,Hard Nuclei
The crater phaco chop is essentially usedin harder, more dense and brunescent cataracts(Fig. 2) in which a trench or trough or groovecannot be used because it does not weaken theentire lens nucleus sufficiently to easily frac-ture the nucleus. The resulting segments wouldbe too large to manage safely. This is becausethe epinucleus of a hard nucleus is thin and ahard nucleus has a dual structure consisting ofan outer soft and inner hard nucleus or core.Also, a hard nucleus is thicker than a softnucleus and the posterior part is harder andmore elastic. In these lenses, the phaco chop ofNagahara or even the stop and chop of Kochmay not be sufficient.
Instead, a small, central crater is sculptedwith controlled amounts of ultrasound energy,leaving a dense peripheral rim (Fig. 112). Afterthe central core of the nucleus is removed, themaneuvering of fracturing can be accomplishedby first placing the chopping instrument underthe anterior capsule at the 6 o'clock position(Fig. 113). Keeping the phaco tip placed intothe bulkhead of the nuclear rim (Fig. 113), thevacuum of the tip is used to stimulate divisionof the nucleus. No ultrasound is used. Thechopping instrument which has been intro-duced through the ancillary incision pulls to-ward the incision (arrow), slightly away fromthe phaco tip and gently towards the posteriorcapsule. This results in a fracture through thenuclear rim and any remaining thin nuclearplate (Figs. 114). The nucleus is then rotated inorder to accomplish additional fracturing ofsmall segments (Figs. 114, 115). Fracturing isdone with much less ultrasound energy than inthe D & C Crater Procedure.
In the Crater Chop technique, again weinitially debilitate the nuclear core with ultra-sound energy. When weakened, the phaco tipis impaled or firmly buried in the central nucleus(Figs. 113, 114). Multiple wedges are createdby the continuous process of biting tissue usingthe chopper. These small pieces are thenemulsified (Fig. 116).
This Crater Chop technique is not to beidentified as the Crater-Bowl procedure de-scribed previously in which a substantial amountof ultrasound energy was used to debilitate thecentral tissue.

THE ART AND THE SCIENCE OF CATARACT SURGERY
192
Figure 112 (above left): Crater ChopTechnique - Stage 1 - Creation of theSmall Crater
The central epinucleus and ante-rior cortex are removed. The phaco tip(P) is used for sculpting at the center. Asmall central crater is sculpted with con-trolled amounts of ultrasound energy,leaving a dense peripheral rim. Thiscreates a thin central nucleus suitable toeasier fracturing with the chopper.
Figure 113 (center): Crater Chop Tech-nique - Stage 2 - Fracturing the Nucleus
With coordinated movements thephaco probe (P) is impaled and buriedthrough the thickness of the dense pe-riphery. At that time the chopoper (C) isemployed to start the fracture deeply andvertically from the periphery to the cen-ter toward the phaco tip in the directionof the primary incision.
Figure 114 (below left): Crater ChopTechnique - Stage 3 - Slicing theNucleus into Small Wedges
Small, controlled and smoothmovements are required to slice por-tions of the nucleus into wedges withouttearing the posterior capsule. Portionsof the nucleus are attracted and rotatedtoward the center with the phaco probe(P) in ultrasound mode, fracturing thewedges into small pieces with the helpof the chopper (C) and rendering themfor emulsifiction and aspiration.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
193
When to Remove Nuclear Seg-ments Immediately vs When Leavethem in Place
The entire lens is fractured before anypieces are removed, maintaining the disten-tion of the capsule which helps to preventan inadvertent capsule rupture, as shown inFig. 115). With a dense or brunescent nucleus,it is safer to leave the segments in place tomaintain the shape of the bag, without thepotential for collapse. The segments are easierto fracture if they are held loosely in place bythe rest of the segments still in the bag.
Figure 115 (above ): Crater Chop Technique - Stage4 - Fracturing and Chopping Process
During the fracturing process, the phaco tip isburied in the dense nuclear periphery while the continu-ous action of the chopper bites the nucleus into piecesbringing them to the center. Here we may observe thiscombined maneuver using the chopper (C) and thephaco probe (P) for rotation and cutting of fragments.
Figure 116 (below): Crater Chop Technique - Stage 5- Attacking the Final Quadrant
The phaco tip is brought in contact with the lastfragment. Tip occlusion is maintained using short burstsof low energy ultrasound. While keeping the tip oc-cluded the fragment is advanced toward the center of thecapsular bag with the help of the chopper (C) for com-plete aspiration with the phaco probe (P).

THE ART AND THE SCIENCE OF CATARACT SURGERY
194
THE NUCLEAR PRE-SLICE OR NULLPHACO CHOP TECHNIQUE
This technique has been devised by JackDodick, M.D., from New York, one of theworld's experts in cataract surgery. Almostevery contemporary cataract surgeon uses someform of chopping, and all surgeons who per-form chopping use some form of ultrasound tofacilitate the chop. Whether it be a groove-and-chop, divide and conquer, or a technique likeHoward Fine's quick chop (the choo-choo chopand flip technique presented later in this chap-ter), some form of ultrasound is used for chop-ping.
Disassembling the Nucleus
Importance in Modern Techniques
All modern techniques are oriented to-ward breaking up or disassembling the nucleusto facilitate its removal from the eye. Thesetechniques, which rely on mechanical energy,have been developed to reduce the amount ofultrasound energy necessary to break up thehard part of the lens nucleus. In addition,disassembling the nucleus removes it from thecapsular recesses of the bag, thereby facilitat-ing its removal with the phaco probe.
Nuclear disassembling techniques usesome ultrasound at the beginning of the proce-dure to create multiple troughs or grooves. Asecond instrument such as a spatula or choppercan then be used to crack or break the nucleus.Dodick now routinely uses the nuclear pre-slice or null-phaco chop technique except inhardened, black cataracts. This procedure re-duces the amount of ultrasound needed to re-move cataracts by phacoemulsification. The
actual breaking up of the lens uses no ultra-sound at all.
In this technique, Dodick sections thenucleus into four parts with no ultrasoundusing two specially designed hooks (Figs. 117- 121). It is as safe as any phaco chop, and takesan equal amount of time.
How Is the Null-Phaco Chop Done
The procedure uses two elongatedSinskey hooks, which have a 2 mm bendwith a round polished ball at the endneatly shown in Figs. 119 and 120. Theanterior cortex is vacuumed, and viscoelasticis placed in the eye. The first hook is intro-duced through the paracentesis incision paral-lel to the lens until it is in the capsular bag.Dodick always does the phacoemulsificationat the 11:00 position, which means the para-centesis incision is at about 2:30 (Fig. 117).The hook enters the capsular bag and isrotated 90 degrees so that it engages theequator of the nucleus. The first hook is nowin place and is pointing toward the opticnerve.
Then the second hook is introducedthrough the phacoemulsification incision,again parallel to the lens (Fig. 117). It en-gages the capsular bag and enters it. Thesurgeon then rotates the hook 90 degrees sothat the tip faces the optic nerve and engagesthe equator of the nucleus below. The hooksshould be about 180 degrees apart. Takinggreat care, the surgeon moves the hooks tobring the tips together (Fig. 118). This pro-cess will not tear the posterior capsule, but itis important not to place the hooks in thesulcus. As the two hooks are brought to-gether, they bisect the nucleus (Fig. 118).

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
195
Figure 117: Dodick’s Null-Phaco ChopTechnique - Stage 1 - Insertion andPlacement of Hooks
Two identical elongated hooks (H)which have a 2 mm bend with a roundpolished ball at the end serve as the chop-pers. The first hook is introduced throughthe ancillary incision at 2 - 3 o'clock andthe other one through the primary incision.The hooks are positioned opposite oneanother. They enter the capsular bag andare rotated 90 degrees so that they engagethe equator of the lens. The hooks are 180degrees apart.
Figure 118: Dodick’s Null-Phaco ChopTechnique - Stage 2 - Bissecting the Nucleus
Thesurgeon pulls on the hooks tobring them together and bisect the nucleus.

THE ART AND THE SCIENCE OF CATARACT SURGERY
196
After the first crack a second crack ofeach half is easily made. The 11:00 hook ismoved toward 6:00, and placed in thecapsular bag while the second hook is left inthe trough or groove (Fig. 119). The twohooks are brought together resulting in atrisection. At this point the lens has been cutinto three parts (Fig. 119). The procedure canbe repeated by splitting the next half in asimilar fashion (Fig. 120). Upto this point noultrasound has been used.
Once the quadrants are each broken upinto three or four parts, they are removed withbevel down phaco, with high vacuum of 300mm Hg to 500 mm Hg. This is in a peristalticsystem, with a high flow rate of 30cc to 40 ccper minute. The amount of energy needed isextremely low.Figure 119 (above): Dodick’s Null-
Phaco Chop Technique - Stage 3 - Frac-turing the Inferior Half of the Cataract
The 11 o’clock hook is movedtoward 6 o’clock and placed in the capsu-lar bag. The second hook is left in thegroove. The two hooks are brought to-gether resulting in a trisection (this partof lens is cut into three parts).
Figure 120 (below): Dodick’s Null-Phaco Chop Technique - Stage 4 -Fracturing the Superior Half of theCataract
Once the inferior half is di-vided, the surgeon proceeds with thesuperior half in a similar manner. Thehooks or choppers are placed at 11o’clock and centrally and drawn to-gether toward the visual axis to com-plete the disassembling of the entirecataract.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
197
Dodick disassembles some 1+ 2+lenses with little or no ultrasound, becausethis maneuver not only sections the nucleusinto four parts, it actually dislodges theseparts quite well from the recesses of thecapsular bag (Figs. 120, 121). He brings thelast two quadrants into the pupillary planeand is able to break them up further with theaid of a Sinskey hook through the paracente-sis incision. When he needs ultrasound in 3+or 4+ cataracts, he rarely goes above 30 %ultrasound because the lens is already brokeninto four parts (Fig. 121).
Learning and Adjustment
Performing this technique does requiresome learning and adjustment. The learningcurve required for this technique is to masterthe placement of the two hooks nd to preventrotation of the nucleus while it is beingdivided. Great care must be exercised in theplacement of the hooks into the capsular bag.There is a tendency for the nucleus to rotate,but you soon develop a proprioceptive-likesense of placing those hooks. If you see orfeel internal rotation of the nucleus about tobegin, you simply adjust the hooks.
Figure 121: Dodick’s Null-Phaco ChopTechnique - Stage 5 - Cataract Fracturedin Four Fragments
Once fractured, the four fragments ofthe cataract are removed using mainlyvacuum and aspiration. Once mastered, thistechnique is highly reproducible and takes nolonger than any other chop technique and re-duces the amount of ultrasound energy intro-duced into the eye.

THE ART AND THE SCIENCE OF CATARACT SURGERY
198
Once mastered, this technique is highlyreproducible, it takes no longer than anyother chop technique, and reduces the amountof ultrasound energy introduced into the eye.It may be a very good alternative procedurefor experienced phaco surgeons.
Potential Complications
To critics, this technique appears dan-gerous. The belief is that the capsular bagcan be dislocated. However, Dodick has notfound this to be a problem if the recesses ofthe capsular bag are identified by vacuumingof the anterior cortical material and the hooksare carefully placed in the capsular bag andnot in the sulcus. Critics may point out thatthe tip is back toward the posterior capsule,and the two hooks brought across the nucleusmight rip the posterior capsule. This, accord-ing to Dodick, does not happen.
On the contrary, he thinks that this canactually be a safer procedure, especially ineyes with weak zonules andpseudoexfoliation. Rather than sculpting andapplying pressure toward the zonules, thevector forces from the special hooks pulltoward the center, reducing stress on thezonules.
For more dense cataracts (e.g. 3+), hedoes use low ultrasound, perhaps 15%, maxi-mum 30%, and again high vacuum, 300 to400 mmHg, and a high flow rate. To mini-mize the effect of surge, he uses theMAXVAC high vacuum tubing and the aspi-ration bypass ABS tip.
Contributions of this Technique
Dodick's procedure shows that usingmechanical energy to break up the lens inplace of ultrasound is helpful in reducing the
amount of energy necessary to evacuate thelens. The technique Dodick describes is onemethod of nuclear disassembly. These meth-ods in general dramatically reduce theamount of energy to break up the nucleus,leading to clearer corneas and quicker reha-bilitation of the patient after surgery.
THE CHOO-CHOO CHOP ANDFLIP PHACOEMULSIFICATIONTECHNIQUE
This special technique devised byI. Howard Fine, M.D., head of the OregonEye Institute in Eugene, Oregon and ClinicalProfessor at the Oregon Health Science Uni-versity in Portland, is a chopping techniquethat uses power modulations and highvacuum along with specific maneuvers tominimize the amount of ultrasound energy inthe eye and maximize safety and control. It iseffective in all types of cataracts and allowshardened nuclei to be removed safely in thepresence of a compromised endothelium.
This procedure facilitates the achieve-ment of two goals: minimally invasive cata-ract surgery and maximally rapid visual reha-bilitation. It is designed to take maximumadvantage of various new technologies avail-able, mainly the Alcon 20,000 Legacy, theAMO Sovereign (Allergan) and the StorzMillennium phacoemulsification systems(Fig. 85). These technologies include highvacuum cassettes and tubing, multiple pro-grammable features on all systems, as well asthe Mackool Micro Tip (Fig. 84) with theLegacy and burst mode and occlusion modecapabilities with the Sovereign (Figs. 86, 87).The result is enhanced efficiency, control, andsafety. The procedure is done as shown anddescribed in Figs. 122, 123, 124, 125, and126.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
199
Figure 122: Choo-Choo Chop Technique -Stage 1
Following instillation of high density,cohesive viscoelastic, cortico cleaving, circu-lar capsulorhexis (C), hydrodissection andhydrodelineation of the nucleus are performed.The exposed epinucleus (E) exposed by theCCC is aspirated. To chop the nucleus intotwo hemispheres, a Fine/Nagahara chopper(F) introduced through a side port incisionengages the distal nuclear margin at the goldenring (G) and stabilizes the endonucleus. Si-multaneously, the 30 degree bevel-downphaco tip (P) introduced through a clear cor-neal incision “lollipops” the proximal nucleus.The nucleus is scored by bringing the chop-per proximally (red arrow) to the side of thephaco tip, which provides a countering force(blue arrow).
Origin of the Name “Choo-Choo”
Fine uses high vacuum and shortbursts, or pulses, of phaco ultrasonic power.The name “choo-choo” arises from the re-sulting sound of the pulse mode (Fig. 125).The nucleus is continually rotated so that pie-shaped segments can be scored and chopped,and then removed by high vacuum assisted byshort bursts or pulses of phaco. (Editor’sNote: scoring the nucleus in this instancemeans using the wedge-shaped edge of thechopper instrument to groove and then cut thenucleus in half against the countering resis-tance of the phaco tip which has been se-curely engulfed in the opposite side of thenucleus.)
The short bursts or pulses of ultrasoundenergy continuously reshape the pie-shapedsegments which are kept at the tip, allowingfor occlusion and extraction by the vacuum.The size of the pie-shaped segments is cus-tomized to the density of the nucleus withsmaller segments for denser nuclei. Phaco inburst mode (Fig. 125) or at this low pulse rate(Fig. 86) sounds like “choo-choo-choo-choo”; this is the reason behind the name ofthis technique. (Editor’s Note: for a precisedescription and illustration of the pulse andburst modes, and their clinical applications,see pages 151-156, and Figs. 86, 87).
The term “flip” refers to managementof the epinucleus (Fig. 126). Fine considersit important not to remove the epinucleus too

THE ART AND THE SCIENCE OF CATARACT SURGERY
200
Figure 123 (above): Choo-Choo Chop Tech-nique - Stage 2
This figure shows the resting positionsof the instruments just following completionof the nuclear chop (arrow). The chopper (F)has been brought proximally and slightly tothe side of the phaco tip and the phaco (P) hasbeen held stationary. The hands are then sepa-rated - the chop instrument moving to the leftand slightly down (1), and the phaco tip tothe right and slightly up (2).
Figure 124 (below): Choo-Choo ChopTechnique - Subsequent Chopping of Nu-cleus
In a similar manner to the first chop,the phaco (P) and chopper (F) are used in com-bination to score and chop the heminuclei.First the nucleus is rotated into position asshown. Here the chopper is directed fromposition 1 to position 2 toward the side of thebevel-down phaco tip to score (3 - arrow) thehemisphere. These smaller pieces can thenmore easily be extracted from the eye withreduced use of ultrasonic power by usingpower modulations. The second nuclearhemisphere (H) is dealt with in the same fash-ion.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
201
Figure 125 (above left): Choo-Choo ChopTechnique - Use of Burst Mode UltrasonicPower
The chopper (F) is used to assist inholding the nuclear pie-shaped segmentsagainst (arrow) the phaco (P) aspiration port.Using high vacuum and short bursts, or pulses,of phaco ultrasonic power (thus the name“choo-choo” from the resulting sound of thepulse mode), the nuclear material is frag-mented and aspirated with minimal or no chat-tering of the piece against the phaco tip. Thismakes for a more efficient and timely removalof the nucleus.
Figure 126 (below right): The EpinuclearFlip Technique
Following removal of the endonucleus,the rim of the distal epinucleus (E) is engagedwith the phaco tip (P) in the bevel-up position.The chopper (F) is used to assist in flipping (ar-row) the epinucleus. In this more centrally lo-cated position, the entire epinuclear rim andfloor can be evacuated from the eye safely andcompletely. This is followed by foldable IOLimplantation and removal of viscoelastic andany residual cortex.

THE ART AND THE SCIENCE OF CATARACT SURGERY
202
early, to avoid leaving a large amount ofresidual cortex after evacuation of the epi-nucleus. The epinuclear rim of the fourthquadrant is utilized as a handle to flip theremaining epinucleus.
Comparison With Other Techniques
The choo-choo chop and flip techniqueutilizes the same hydro forces to disassembleof the nucleus as in cracking techniques, butsubstitutes mechanical forces (chopping) for
ultrasound energy (grooving) to further disas-semble the nucleus.
High vacuum is utilized to removenuclear material rather than utilizing ultra-sound energy to convert the nucleus to anemulsate that is evacuated by aspiration.
Fine's Parameters
The parameters used by Fine for thistechnique and applied to the three main pha-coemulsification equipments are the follow-ing:

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
203
These Parameters are adjusted depending on the hardness of the nucleus. They can be pro-grammed in the corresponding “Memory” of the equipment.

THE ART AND THE SCIENCE OF CATARACT SURGERY
204
THE TRANSITION TOCHOPPING TECHNIQUES
In the transition to chopping, Fine rec-ommends the following steps:
Impale the nucleus on the phaco tipsuperiorly. If you have not lollipoped theprobe tip deep enough (Fig. 88), return toposition 2 and then go back into position 3.(Editor’s Note: lollipoping refers to securelyengulfing the tip of the phaco into thenucleus, like a lollipop or candy sucker on astick. The phaco tip is analogous to the stickand the nucleus is the round candy portion.) A burst takes place each time you enterposition 3.
When you have lollipoped deeplyenough (Fig. 88), score the nucleus. (Editor’sNote: scoring the nucleus means using thewedge-shaped edge of the chopper instrumentto groove the nucleus deeply, against thecountering resistance from the lollipopedphaco on the opposite side of the nucleus.)Place the chop instrument in the golden ring(Fig. 75), go from foot position 2 into footposition 3 and floor it (Editor’s Note: push-ing the pedal fully all the way to the bottomsetting, as when applying full gas pedal pres-sure in a car). You can chop the nucleuswithout having to worry about what your footis doing because your foot is on the floor —the vacuum will hold the nucleus as youmanipulate the chop instrument.
Then break the nucleus in half byseparating the two instruments while depress-ing the chopper and slightly elevating thephaco needle. You will not have to worryabout what your foot is doing because you arealready in control of the nucleus — you willnot have to manipulate your foot at all. Thistechnique will allow you a much easier transi-
tion with fewer factors to worry about.For mobilizing the nuclear tissue, Fine
likes a burst width of 80 milliseconds insurgeon control (Fig. 87). Once again, youcan customize your options to control whathappens at the tip. If things are moving alongrapidly, you can depress the foot pedal to footposition 3 and decrease the interval betweenbursts. Or if you feel like things are a littleprecarious or there is a very hard piece ofnucleus and you want to avoid chattering, youcan back off a little bit. (Editor’s Note:chattering is when the nucleus bouncesagainst the phaco tip at a high rate of speedwithout being emulsified as desired, likewhen ones teeth chatter when cold - Fig. 89)
The material will be held very firmly atthe tip with no chatter, and will not emergeinto the anterior chamber. This affords amuch greater level of safety when dealingwith a hard cataract in the presence of endot-helial disease.
Once you have taken care of theendonucleus, you can employ the Bimodal fea-ture using the pedal to vary your aspiration flowrate in foot position 2. This helps you to mo-bilize and bring the epinuclear roof out of thecapsular fornix and position it in such a waythat you can trim it. Fine trims the rim of theepinucleus in three different quadrants and usesthe rim in the remaining quadrant to flip therest of the epinucleus (Fig. 126). He bringsthe handpiece central and then trims the epi-nucleus. Once he goes into foot position 3 thetip clears. As the rim of the epinuclear shell isremoved, the aspiration flow rate causes theresidual cortex to flow over the floor of theepinuclear plate.
Fine does not usually have to removethe cortex as a separate step of phacoemulsifi-cation. In 70 percent of these cases, he has nocortex remaining.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
205
These types of maneuvers can be donebecause there is a stable anterior chamberwith a very low tendency for surge.
The new technology in these advancedmachines and new software allows the sur-geon to put into effect the important advancein performing phacoemulsification, which isfundamentally cutting power. The surgeonreally has little worry about cutting powerhimself because the new software provideshim/her so many more options. With theserecent advances in phacoemulsification sys-tems, the surgeon has indeed a total controlphaco chop. The new type of software de-scribed in Chapter 8, Fig. 85, will advancephacoemulsification in regions of the worldwhere there is a preponderance of hard cata-ract with diseased endothelium.
Figure 127: Irrigation/Aspiration of Residual Cortex Inferiorly
Following emulsification of the nucleus, the ultrasound tip is replaced by theirrigation/aspiration tip (A). The tip is placed into the anterior chamber through theprimary incision and inserted under the anterior capsule in the inferior sector to removethe small amounts of residual cortex. It is important not to be aggressive nor attempt tovacuum clean. This is risky and may result in posterior capsule rupture.
REMOVAL OF RESIDUALCORTEX ANDEPINUCLEUS
The surgeon who is learning this tech-nique usually has more cortex to aspirate andneeds to follow a specific technique for re-moval of the epinucleus. This is discussed indepth and illustrated in Figs. 69, 70 and 71,Chapter 7. If not cautiously done, there is ahigher incidence of rupture of the posteriorcapsule.
The situation differs for the experiencedsurgeon. Due to the importance attributed toa well-performed hydrodissection and rota-tion of the nucleus at the end of it, generallythe epinucleus and the residual cortex are

THE ART AND THE SCIENCE OF CATARACT SURGERY
206
aspirated together with the nucleus segments.The aspiration of cortical remains becomesunnecessary because they were partially ortotally eliminated during nucleus emulsifica-tion. If this does not happen, the tip of thephaco emulsifier aspirates the free epinucleuswith the pedal on position 2, with the help ofthe nucleus manipulator (Figs. 69 and 126).
Once the nucleus has been removed andthe surgeon proceeds to irrigate/aspiratewhatever cortex remains, he/she may becomeover-confident thinking that the operation ispractically finished. It is, if the cortex andepinucleus are then removed with specialcare. Always be certain to check the tip of theI/A phaco tip preoperatively to detect any
little barbs or sharp spots that could rupture ortear the posterior capsule. The Chip and Fliptechnique advocated by Fine may be veryuseful in this phase (Fig. 126). The entireepinuclear rim and floor can be evacuatedsafely and completely.
If some cortical material remains, par-ticularly in the hard-to-reach superior capsu-lar bag underneath the anterior capsuleleaves, the surgeon proceeds to remove thisresidual cortex as shown in Figs. 127 and128. It is very important not to be aggres-sive. Do not attempt to clear the very last bitof cortex remaining because this could lead toaccidental rupture of the posterior capsule.
Figure 128: Irrigation/Aspiration of ResidualCortex Superiorly
In superior areas where it is difficult tomaneuver with the irrigation/aspiration tip (ghostview - A), particularly at 12 o’clock, we may re-move the residual cortex located superiorly using amanual aspiration technique with a curved irriga-tion/aspiration cannula or a standard Simcoe can-nula (S). Here the Simcoe cannula is inserted infe-riorly through an additional paracentesis (P) whichis a third incision performed between 6 and 7o’clock. It is moved superiorly to remove the re-sidual cortex under the anterior capsule leaves.Manual technique allows more accurate control.Another method to attain this is following the pro-cedure shown in figure 71. Again, it is importantnot to be aggressive.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
207
INTRAOCULAR LENSIMPLANTATION
The Increased Interest in Fold-able IOL's
Present trends point to an increasing useof foldable IOL's for the following reasons:
1) Small incision cataract surgery con-tinues to be on the rise. Patients who are in thefinancial, social, business and professional lev-els to afford phacoemulsification look forwardto a very prompt visual rehabilitation. This canbe made possible only by a successful phacowith a small, valvulated, self-sealing 3 mmaverage incision which requires a first classfoldable IOL (Figs. 90, 91).
Surgeons, therefore, no longer acceptthe previous methods of performing a cataractextraction through a small incision followed byan enlargement of the wound in order to inserta 6.0 mm optic PMMA lens. As a consequence,industry rose to this challenge and has devel-oped high quality foldable IOL's .
2) Through the significant clinical andlaboratory research made by R. Lindstrom,I.H. Fine, Ernest and Neuhann, Langernmanand other prestigious colleagues, refractivecataract surgery was developed as a standardprocedure by: a) placing the corneal cataractincision in the right place. b) developing theright architectural design of a small self-seal-ing, valvulated, corneal tunnel incision that canresult in 1.00 D or less of postoperative astig-matism (Figs. 92, 93). This has stimulated theuse of foldable monofocal and multifocal IOL's.
3) Foldable IOL technology has signifi-cantly improved associated with the use ofnon-toxic, highly biocompatible chemicalsand polymers of which the foldable IOL`s aremade. This is particularly important with thedevelopment of second generation siliconelenses which have been proven to be non-toxic,non-inflammatory, non-sensitizing, inert andavailable at lower costs.
The Most Frequently Used IOL's
Even though there is a distinct trent to-wards foldable lenses, PMMA IOL's continueto be the most frequently implanted intraocularlenses throughout the world, (except in theU.S). PMMA IOL’s are used more commonlyeven in Europe, although to an ever-decreas-ing extent, as has been pointed out by TobiasNeuhann, M.D., of Germany, in a classicstudy he made of new foldable IOL's (seebibliography).
The still preponderant use of PMMAlenses is related to the unquestionable realitythat, for a variety of reasons, extracapsularsurgery is still the cataract operation mostlyused throughout the globe. More than 60% ofvery good ophthalmic surgeons perform ECCEin the majority of patients even though theymay recognize that phacoemulsification is abetter operation especially for of very promptvisual rehabilitation.
Special Indications for PMMALenses
Richard Lindstrom, M.D. uses fold-able lens implants in most cataract operations.

THE ART AND THE SCIENCE OF CATARACT SURGERY
208
Nevertheless, he considers that there still areindications for the standard PMMA lenses, forexample the secondary anterior chamber lensimplant (Fig. 129). He also uses standardPMMA intraocular lenses when performing atriple procedure that includes a penetratingkeratoplasty. In these patients there is noreason to use a foldable lens. He may use a7 mm optic modified C loop PMMA lens.
MONOFOCAL FOLDABLELENSES
An extensive variety of excellentmonofocal foldable lenses are produced bymanufacturers in the US, Germany, France,Belgium, Switzerland and other countries. Theyuse the finest technology and front-line engi-neers, biochemists and designers.
The most widely accepted, major groupsof foldable lenses are made of either acrylic orsecond generation silicone (PDMDPS). Eachgroup has advantages and disadvantages. Othermonofocal lenses creating interest are theMemory lens, the hydrogel lenses and the toriclens made by STAAR.
THE FOLDABLE ACRYLIC IOL'S
These lenses have a very high refractiveindex providing crystal clear vision. Chemi-cally they are closely related to the still gener-ally favored PMMA. Mechanically they arebest described as pliable rather than elastic.This is clinically important because acryliclenses are comsidered by many surgeons assomewhat bulky when folded and, conse-quently, difficult to implant through an inci-
Figure 129: Insertion of PMMA AnteriorChamber Lens in Aphakia - Gonioscopic View
A gonioscopic mirror is used to check theposition of the proximal footplates, and to ensurethat there is no iris tuck. The distal footplates arealso checked again with the gonio prism to ensurethat they have not been displaced during place-ment of the proximal haptics.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
209
sion less than 3.5 mm. We have presentedCarreño's technique in which he describeshow to insert the AcrySof lens through a 2.8mm incision in Chapter 8. The most widelyused foldable acrylic lenses are the popularAlcon AcrySof lens model MA30BA, whichhas a 5.5 mm optic and PMMA haptics and theAllergan Sensar AR40 with a 6.0 mm optic.They both come with very practical folding andinjector systems, the "Acrypack" for Alcon'sAcrySof and the "Unfolder Saphire" forAllergan's Sensar.
Specific Advantages of AcrylicFoldables
In addition to providing a very highrefractive index, they are also the first choicelenses to use in higher risk cases such aspatients with diabetic retinopathy (Figs. 8-17),chronic uveitis or any candidates for futurevitrectomy with silicone oil.
Another advantage seems to be thatacrylic lenses have a "tacky" surface.According to Tobias Neuhann, M.D., apositive consequence of this tackiness is amechanical adhesiveness between lens capsuleand IOL, which, in turn, may lead to reductionof secondary cataract (posterior capsule opaci-fication).
A disadvantage of this tackiness, how-ever, is that a multitude of small particles maystick to the lens surface and be pressed into thematerial with the implantation instruments,where they remain forever, since they are notabsorbed. For these reasons, injector implanta-tion or disposable implantation forceps aregaining increasing importance in handling theselenses (Fig. 82 B and C).
Disadvantages of AcrylicFoldables
Foldable acrylic lenses come in a 5.5 anda 6 mm optic size. Lindstrom and some othersurgeons prefer the 6 mm optic because the5.5 mm optic lenses may have problems withedge glare and unwanted visual images.Another limitation with acrylic lenses, accord-ing to Lindstrom, is that none of the foldableacrylic lenses will go through an incision smallerthan 3.5 mm. (they are pliable but not elastic -Editor) In his experience, you have to makeone of two compromises if you use an acryliclens. Either you make the incision larger ormake the optic smaller. 3.5 mm instead of 3.2or 3.0 mm is not a large difference but still,with a clear corneal incision, Lindstrom thinksthe smaller the incision the safer it is as far assealing of the wound. And if you go to a smalleroptics then you get more symptoms of edgeglare, particularly with younger patients whohave larger pupils.
Edgardo Carreño, M.D., on the otherhand, has developed a technique by which heimplants the foldable acrylic Alcon AcrySoflens 5.5 mm optic through a 2.75 mm incision.Carreño's technique is described in this bookin Chapter 8.
THE FOLDABLE MONOFOCALSILICONE IOL's
Second generation silicones are gain-ing in popularity because they are inert and donot give rise to inflammatory reactions. Thissecond generation silicone polymer is identi-fied as the PDMDPS.

THE ART AND THE SCIENCE OF CATARACT SURGERY
210
There was a time when the silicone lensescaused more inflammation or capsular fibrosesbut the newer silicones do not do that at leastbased on the studies made by Lindstrom andothers. Many surgeons like silicone lensesbecause they go through an incision smallerthan other lenses thereby allowing a largeroptic. The favorite lenses are those with 6.0mm optic or larger.
There are now two companies that havea 6.3 mm optic silicone lens. One of them isStaar and the other is Bausch & Lomb. Mostother companies have 6 mm optic siliconelenses. The most popular monofocal foldablesilicone lenses are Allergan's SI 40 NV andBausch & Lomb's LI 61 both of which have a6 mm optic. The Bausch & Lomb LI 63silicone lens has a 6.3 mm optic. Siliconelenses have more elasticity. When the lens isimplanted through an injector, it stretches. Soit can go through a smaller incision. TheAllergan SI 40 NV that has a 6.00 mm optic andthe Bausch & Lomb LI 63 with a 6.3 mm opticwill go through a 3 mm incision with the properinjector nd cartridge made available bythe manufacturer for those spe cific lenses(Fig. 132). This gives you a 6.3 mm or 6.0 mmoptic through a 3 mm incision. The openmodified C loop silicone lenses are better ac-cepted by the surgeon than the plate hapticlenses because of less decentration.
The Importance of Cost
An additional advantage of the siliconelenses is that because many companies makethem, they tend to be less expensive. And so,if you are in an environment where cost is anissue, which is just about anywhere in theworld, the new second generation, high qualitysilicone lenses on the average can be purchasedfor maybe half the price of foldable lenses ofother materials.
OTHER MONOFOCAL LENSES
The Hydrogel, Foldable MonofocalIOL
These lenses swell in water. Their me-chanical properties are pliable rather than elas-tic. Their properties are close to PMMA buthave a hydrophilic surface and may be foldedand inserted through small incisions.
The Foldable Toric Lens
The STAAR toric IOL (AA4203T) com-bines recent toric technology with a flexibleoptic. The toric optic offers three cylindricalpowers (2.5 D, 3.5 D, 4.0 D) as well asspherical (+14D to +26 D) values, and the platehaptic possesses large fenestrations designedfor lens fixation in the capsular bag.
The results of this product are encourag-ing and appear to be stable. This implantextends the range of refractive lens surgery,especially in cases where high ametropia iscombined with astigmatism.
Bitoric Lens But Not Foldable
Although we here emphasize essentiallythe trends towards the increasing use of fold-able lenses, it is important to bring out thedevelopment of the bitoric IOL although it isnot foldable. This lens has been developed byH.R. Koch and manufactured by Dr. SchmidtIntraokularlinsen in Germany. The disk-shaped PMMA implant consists of two toriclenses of the same power, both with oneplanar and one toric side, which counter-rotateto produce a variable degree of astigmaticpower. The direction of the haptic defines theposition of the cylindrical axis, and two addi-tional lines in the optical periphery allow an

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
211
exact intraocular positioning. The range of this6 mm toric IOL is outstanding: spherical powerbetween -3.0 D and +30 D combined withcylindrical power from +1.0 D to +12.0 D. It is12.5 or 13.4 mm in diameter;
THE FOLDABLEMULTIFOCAL IOL
The Array Multifocal SiliconeLens
This is one of the most important devel-opments in rehabilitation of sight and improv-
ing the quality of life following cataract sur-gery. I. Howard Fine, M.D., and RichardHoffman, Javitt and colleagues in the U.S.and Virgilio Centurion, M.D. in Brazil havedone extensive clinical research on the perfor-mance of this foldable multifocal lens and thebenefits of high quality multifocal vision intheir patients. Having used different kindsof multifocal IOLs in the past, Centurion isfamiliar with the complications in their design.This new multifocal lens, however, is a refrac-tive molded lens instead of a diffractive lens(Figs. 130, 131). Its use is recommended byCenturion for surgeons who are confidentwith phacoemulsification and small incisiontechniques.
Figure 130 (left): How the Multifocal Array In-traocular Lens Works - Frontal View
The new multifocal Array intraocular lenshas five refractive zones on the anterior surface. Be-tween each of them there is a narrow aspheric transitionzone. Zones 1, 3 and 5 (red) dominate for distancevision, and zones 2 and 4 (yellow) dominate for nearvision. The optical mechanism of these zones isshown in Fig. 131.
Figure 131 (right): How the Multifocal Array In-traocular Lens Works - Cross Section View
This cross section shows how the steeper areas ofthe lens (yellow zones 2 and 4) are of higher power andfocus on near objects (N). The flatter areas of the lens (redzones 1, 3, and 5) are of lower power and focus far objects(F). Light rays from a distant object (O) which refractthrough zones 2 and 4 (yellow rays) focus at (N). Lightrays from a distant object which refract through zones 1, 3and 5 (red rays) focus at (F). Zones 2 and 4 have smoothtransitions to adjacent zones, and focus light at intermedi-ate distances. These aspheric transitions between theoptical zones greatly reduce the halo effect which wassometimes bothersome using older diffractive designs.

THE ART AND THE SCIENCE OF CATARACT SURGERY
212
How Does the Array Foldable Multi-focal Lens Work?
The lens is manufactured by AllerganMedical Optics. It has a foldable silicone opticthat is 6.0 mm in diameter with haptics made ofpolymethylmethacrylate and a haptic diameterof 13 mm (Fig. 130). The lens can be insertedthrough a clear corneal or scleral tunnel inci-sion that is 2.8 mm wide, using the Unfolderinjector system manufactured by AMO(Allergan) (Fig. 82 A).
There are five zones on the anteriorsurface. Between each of them there is anarrow aspheric transition zone. The 5 domi-nant zones provide the following: 1) a clearimage for distance (2 zones); 2) one zone forintermediate distance, and 3) two zones fornear. The Allergan Array Lens differs fromthe older diffractive lens designs not only inhaving classical optics for the definitivezones, but in having aspheric transition zoneswhich, according to Centurion, provide thepatient with a smooth transition between theimages for distance, intermediate, and nearvision, greatly reducing the halo effect whichwas sometimes so bothersome with olderdesigns. Even those patients who may com-plain of some halos after surgery seldomreport them 2 or 3 months later.
Fine and Hoffman describe the lens ashaving an aspherical component and thuseach zone repeats the entire refractive se-quence corresponding to distance, intermedi-ate, and near foci. This results in vision overa range of distances. The lens uses 100% ofthe incoming available light and is weightedfor optimum light distribution. With typicalpupil sizes, approximately half of the light isdistributed for distance, one-third for nearvision, and the remainder for intermediatevision.
Quality of Vision with Array Multi-focal
Refractive multifocal IOLs, such as theArray, have been found to be superior todiffractive multifocal IOLs by demonstratingbetter contrast sensitivity and less glare dis-ability. The Array does produce a smallamount of contrast sensitivity loss equivalentto the loss of 1 line of visual acuity at the 11%contrast level using Regan contrast sensitivitycharts. This loss of contrast sensitivity at lowlevels is present only when the Array isplaced monocularly. This has not been dem-onstrated with bilateral placement and bin-ocular testing. In addition to relatively nor-mal contrast sensitivity, good random-dot ste-reopsis and less distance and near aniseikoniawere present in patients with bilaterallyplaced implants as compared to those withunilateral implants.
In a study by Javitt and colleagues,41% of bilateral Array subjects were foundnever to require spectacles, as compared to11.7% of monofocal controls. Overall, sub-jects with bilateral Array IOLs reported betteroverall vision, less limitation in visual func-tion, and less use of spectacles than didmonofocal controls.
Studies in different parts of the worldreport that more than 85% of patients have20/40 or better vision without correction afterimplantation with this lens. All of the 456patients in the US Clinical Study have J3 orbetter, and more than 60% are J2 or J1without correction. About half are 20/20without correction.
Patient Selection and Results
Fine and Hoffman emphasize that theadvantages of astigmatically neutral clear

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
213
corneal cataract surgery have allowed forincreased utilization of multifocal technologyin both cataract and clear lens replacementsurgery. Careful attention to patient selec-tion, preoperative lens power calculations, inaddition to meticulous surgical technique,will allow surgeons to offer multifocal tech-nology to their patients with great success.
Researchers working with this lenshave the clinical impression that depth offocus and quality of vision are improved ifthe surgeon does a bilateral implantationand implants the second eye within 4 weeksof the first implantation. The results seem tobe improved if there is a very short intervalbetween the first and second eye. (If thecataract merits removal in both eyes. This isusually the case when modern small incisioncataract surgery is performed. - Editor).
Of the 350 multifocal lens implanta-tions Centurion has done, about half werebilateral, and half were monocular. The mo-nocular implantations involved traumatic orinflammatory cataracts rather than senilecataracts . He has not yet used multifocalIOLs in patients with congenital cataracts, butthey work well for monocular implantationwhen a patient has one normal eye. Gener-ally patients do not depend upon glassesmuch for near vision after the implantation.With bilateral implantation, the quality ofvision and quality of life of patients improveconsiderably. Sometimes they only needglasses to drive at night and to read verysmall print.
Fine and Hoffman point out that themost important assessment for successfulmultifocal lens use, other than patient selec-tion, involves precise preoperative measure-ments of axial length in addition to accuratelens power calculations. They have foundapplanation techniques in combination with
the Holladay II formula and the Holladay IIback-calculation to yield accurate and consis-tent results.
Specific Guidelines for Implantingthe Array Lens
Fine and Hoffman have used the Arraymultifocal IOL over the last 2.5 years exten-sively, in approximately 30% of their cataractpatients and in the majority of their clear lensreplacement refractive surgery patients. As aresult of their experience, they have devel-oped specific guidelines with respect to theselection of candidates and surgical strategiesthat enhance outcomes with this IOL.
AMO recommends using the Arraymultifocal IOL for bilateral cataract patientswhose surgery is uncomplicated and whosepersonality is such that they are not likelyto fixate on the presence of minor visualaberrations such as halos around lights. Ob-viously, a broad range of patients would beacceptable candidates. Relative or absolutecontraindications include the presence ofocular pathological processes (other thancataracts) that may degrade image formationor may be associated with less than ad-equate visual function postoperatively de-spite visual improvement after surgery.Contraindications are age-related macular de-generation, uncontrolled diabetes or diabeticretinopathy, uncontrolled glaucoma, recur-rent inflammatory eye disease, retinal detach-ment risk, and corneal disease or previousrefractive surgery in the form of radial kerato-tomy, photorefractive keratectomy, or laser-assisted in situ keratomileusis.
Fine and Hoffman also avoid the use ofthese lenses in patients who complain exces-sively, are highly introspective and fussy, orobsessed over body image and symptoms.

THE ART AND THE SCIENCE OF CATARACT SURGERY
214
They are conservative when evaluating pa-tients with occupations that involve frequentnight driving or that put high demands onvision and near work (e.g., engineers andarchitects). Such patients need to demon-strate a strong desire for relative spectableindependence in order to be considered forArray implantation.
In their practice, they have reducedpatient selection to a very rapid process.Once they determine that someone is a candi-date for either cataract extraction or clear lensreplacement, they ask the patient two ques-tions: First, "If we could put an implant inyour eye that would allow you to see bothdistance and near without eyeglasses, undermost circumstances, would that be an advan-tage?" Approximately 50% of their patientssay no directly or indirectly. Negative re-sponses may include, "I don't mind wearingglasses," "My grandchildren wouldn't recog-nize me without glasses," "I look terriblewithout glasses," or "I've worn glasses allmylife." These patients receive monofocalIOls. Of the 50% who say it would be anadvantage, they ask a second question: "Ifthe lens is associated with halos around lightsat night, would its placement still be anadvantage?" Approximately 60% of thisgroup of patients say that they do not thinkthey would be bothered by these symptoms,and they receive a multifocal IOL.
Centurion also emphasizes that theselenses should not be used in patients with abasic astigmatism of more than 1.50 diopters.
Prof. Luis Fernandez Vega in Spainrecommends a series of important guidelinesin order to be successful with advanced tech-nology multifocals: 1) Do only bilateralmultifocal implantations in adults. Do notplace a monofocal IOL in one eye and amultifocal in the other. Otherwise, patients
compare the vision between the two eyes andrefer to the differences existing, even thoughthey may have good visual acuity in both. 2)Yes, the multifocal IOL does fullfil its opticalpurpose both for distance and near. Althoughit does not completely prevent the wearing ofspectacles, it does diminish the dependencyon glasses. Clarify this to the patient preop-eratively. 3) Select the patient according tohis/her visual needs. 4) Do a very precisepreoperative biometry; 5) Perfect your cata-ract surgery to end up with less than 1.00 Dastigmatism.
Special Circumstances for Array Im-plantation
There are special circumstances inwhich implantation of a multifocal IOLshould be strongly considered. Alzheimer'spatients frequently lose or misplace theirspectacles, and thus they might benefit fromthe full range of view that a multifocal IOLprovides without spectacles. Patients witharthritis of the neck or other conditions withlimited range of motion of the neck maybenefit from a multifocal IOL rather thanmultifocal spectacles, which require changesin head position. Patients with a monocularcataract who have successfully wornmonovision contact lenses should be consid-ered possible candidates for monocular im-plantation. The same is true for certainprofessionals such as photographers whowant to alternate focusing through the cameraand adjusting imaging parameters on thecamera without spectacles. In these patients,the focusing eye could have a monofocal IOLand the nondominant eye a multifocal IOL.Fine and Hoffman almost always use theArray for traumatic cataracts in young adultsin order to facilitate binocularity at near,

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
215
especially if the fellow eye has no refractiveerror or is corrected by contact lenses.
Need for Spectacle Wear PostOp
Prior to implanting an Array lens, theyinform all candidates of the lens's statistics toensure that they understand that spectacleindependence is not guaranteed. Approxi-mately 41% of patients implanted with bilat-eral Array IOLs will never need to weareyeglasses, 50% wear glasses on a limitedbasis (such as driving at night or duringprolonged reading), 12% will always need towear glasses for near work, and approxi-mately 8% will need to wear spectacles on afull-time basis for distance and near correc-tion.
Halos at Night and Glare
15% of patients were found to havedifficulty with halos at night, and 11% haddifficulty with glare, as compared to 6% and1%, respectively, in monofocal patients.
SURGICAL PRINCIPLES AND GUIDE-LINES FOR IOL IMPLANTATION
Just as there are a large number ofmethods to disassemble the nucleus there is awide variety of techniques to implant theIOL's, particularly the foldable lenses. Whatcounts is the results and the feasibility toachieve a successful implantation.
We present here the surgical principlesand guidelines for implantation of the mostcommonly used types of foldable lenses. Wehave chosen the principles followed byhighly respected, skilled phaco surgeons whodo a great deal of teaching in addition tohaving a large, solid practice in different
geographical and cultural regions. They haveprovided HIGHLIGHTS with the pearls ofthe methods that lead them to successfulimplantation. They are: Jack Dodick, M.D.,from New York, I. Howard Fine, M.D.,from Oregon, and Richard Lindstrom,M.D., from Minnesotta, three different areasof the United States. And Edgardo Carreño,M.D., from South America (Chile).
First, you will find the present status ofthe preferred methods of lens implantation,forceps vs injectors, their pros and cons.Second, the techniques of implantation of 1)the Array Multifocal Foldable Lens(Allergan). 2) The acrylic monofocal lens, inthis case the AcrySof Lens (Alcon). 3) Thesilicone monofocal foldable lens (STAAR).
PREFERRED METHODS OF IOLIMPLANTATION
Use of Forceps vs Injectors
Advantages and Disadvantages
Many surgeons like to use forceps toimplant the foldable lens, others use injectors.Lindstrom reminds us that the original in-struments available for foldable lenses wereall forceps. Consequently, those surgeonsthat used foldable lenses early on got used tothe forceps insertion method (Figs. 133,134). But there is a disadvantage to the for-ceps approach. It adds some mass to theamount of material you are putting into theeye (Fig. 132) thereby requiring a slightlylarger incision. Another disadvantage of us-ing forceps is that you may touch the lens tothe conjuntiva or sclera before placing it intothe incision. Several studies have shown thatthe lens picks up bacteria and mucus and

THE ART AND THE SCIENCE OF CATARACT SURGERY
216
other debris from the surface of the eye whenyou use the typical cross action forceps (Fig.133). This may increase the risk of post-operative inflammation or infection. Forthese reasons, Lindstrom now prefers theinjectors, because you take a sterile lens outof a sterile package, put it into a sterileinjector and place the lens directly inside theeye. With the injector you also have lessbulk, thereby requiring a slightly smaller inci-sion (Fig. 132-A).
The reason a good number of surgeonsdo not like the injectors is: 1) they got usedto folding with forceps, (Figs. 132-B, 133)which are convenient and they are used tothem. 2) All the injectors have a small failurerate. It is very annoying when you load alens into the injector and then after placing itinside the eye, the optic is torn or one of thelens loops is bent or damaged. Some sur-geons do not use injectors because they donot like the lens failures that occassionallyoccur with them. The newer injectors of thebetter companies, however, are performingvery well now.
New Trends for Folding andInsertion of IOL's
The majority of lenses are still foldedand inserted with forceps (Figs. 132-B, 133).Nevertheless, there is a definite trend towardthe development of separate instruments forfolding and inserting IOL’s rather than usingthe insertion device to fold the IOL. Thecombination of instruments designed by themanufacturers to facilitate folding and inser-tion is known as cartridge injector systemswhich are then used to implant the IOL.
Cartridge Injector Systems
Fine, Lewis and Hoffman believe thatthere are many perceived advantages of im-planting foldable IOLs with injector systems,as compared with folding forceps. These ad-vantages include the possibility of greater ste-rility, ease of folding and insertion, and im-plantation through smaller incisions as empha-sized by Lindstrom (Fig. 132).
Greater sterility with injector systems isbelieved to occur because the IOL is broughtdirectly from its sterile package to its sterilecartridge and inserted into the capsular bagwithout ever touching the external surface ofthe eye, as is the case for lenses in foldingforceps. Although this advantage would sug-gest a lower rate of endophthalmitis with injec-tor systems, recent clinical studies have shownno significantly different rate of bacterial con-tamination of the anterior chamber after im-plantation of silicone lenses with a forcepsversus an injector.
Perhaps the most appealing advantage ofinjector systems is that the lens can be loadedby a nurse or technician without the use of anoperating microscope, further streamlining theprocedure. In addition, inserting foldable lenseswith a cartridge device is generally felt to beeasier than insertion with forceps.
There are no irregular surfaces as mayoccur between the surface of the forceps andthe lens. The IOL is lodged inside the cartridgeand injector system.
Allergan's foldable three piece siliconelens (monofocal or multifocal - AMO Array)with PMMA haptics may be implanted withAMO's Unfolder Phacoflex injector system.Allergan's acrylic foldable IOL (Sensar andClariflex lenses) may be implanted with a new

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
217
injector now available and known as theUnfolder Sapphire, as described by Centu-rion (Fig. 82-A). These injectors are re-sterelizable (as are the forceps, of course).
Alcon’s popular 5.5 mm AcrySof IOLmay be implanted with one of its injectors suchas the Monarch (Fig. 82) or with a standardcartridge through a 3.4 mm incision. Carreñoreports injecting this lens through a 2.8 mmincision (Fig. 132). Many surgeons use Alcon’sAcrypack (Fig. 82) when implanting theAcrySof lenses. The Acrypack serves to firstfold the IOL. The surgeon then uses a forceps(Fig. 81) to implant the already folded IOL.
The Alcon AcrySof lens, which requires3.5 to 4.0 mm incisions for 6.0 mm optics and
3.2 to 3.5 mm incisions for 5.5 mm optics,when implanted with forceps is now packagedin a wagon wheel dispenser. The easiest fold-ing instrument to use for these lenses is theRhein folder, as recommended by Fine be-cause the tips have been extended to make iteasier to remove the lens from its wagon wheelpackaging. The forceps can be turned with thetips down in the nondominant hand. The tipsgo into the slots on both sides of the optics, sothat the lens can be picked up and placed on adrop of viscoelastic. The forceps are thenturned so that the tabs are down. The lens isgrasped and folded, and then the insertiondevice is used to insert the lens using thesurgeon’s dominant hand.
Figure 132: Insertion of Foldable IOL - Forceps vs Injector - Comparative Incision Size
The insertion of a foldable intraocular lens may well be done either with forceps or with injectors.There is a difference between the two regarding the size and architecture of the incision.
When injectors are used (A) we may maintain the small size primary incision of 2.8 mm (red arrow).On the contrary, when we use forceps for the insertion of the IOL (B), the diamond blade needs to beextended fully (yellow arrow) in order to enlarge the incision from 2.8 mm to 3.0 mm to accommodate thesilicone IOL insertion and 3.4 mm with acrylic IOL’s . This is due to the added bulk relation of lens andforceps. With the injector, there is no additional bulk.

THE ART AND THE SCIENCE OF CATARACT SURGERY
218
Guidelines for Insertion of Dif-ferent Types of Lenses
Surgical Technique with Array Lens
Fine and Hoffman consider it very im-portant that incision construction be appropri-ate with respect to size and location because themultifocal Array works best when the finalpostoperative refraction has less than 1 D ofastigmatism. They favor a clear corneal inci-sion at the temporal periphery that is 3 mm orless in width and 2 mm long (Fig. 91). Eachsurgeon should be aware of his or her usualamount of surgically induced astigmatism byvector analysis. The surgeon must also con-sider the best meridian in the cornea to place theincision considering the existing preoperativeastigmatism in order to end up with minimumpostop astigmatism. We discuss this subjectunder "Refractive Cataract Surgery" in Chap-ter 12 (Complex Cases).
In preparation for phacoemulsifiction,the capsulorhexis must be round (Figs. 44, 45)and its size should be sufficient so that there isa small margin of anterior capsule overlappingthe optic circumferentially. This is importantin order to guarantee in-the-bag placement ofthe IOL and prevent anteroposterior alter-ations in location that would affect the finalrefractive status. Hydrodelineation and cor-tical-cleaving hydrodissection are crucial inall patients because they facilitatelens disas-sembly and complete cortical cleanup.
Taking the time and care to perform acareful and effective cortical cleanup as shownin Figs. 127 and 128, without being aggressive,may reduce the incidence of posterior cap-sule opacification, the presence of which,even in very small amounts, will inordi-
nately degrade visual acuity in Array pa-tients. Because of these phenomena, patientsimplanted with Array lenses will require YAGlaser posterior capsulotomies earlier than willpatients with monofocal IOLs.
Minimally invasive surgery is key.Techniques that utilize effective phacoemulsi-fication powers of 10% or less are highlyadvantageous and can best be achieved withpower modulations (burst mode or two pulsesper second) rather than continuous phacoemul-sification modes (Figs. 86-89, Chapter 8). TheManagement of Complications with the ArrayLens is discussed in Chapter 11 (Complica-tions).
Carreño's Technique of AcrylicIOL Implantation Through a2.75 mm Incision
Because it is generally considered thatacrylic lenses require a somewhat larger inci-sion (3.4 mm) to be introduced into the anteriorchamber without harming the lips of the wound,we present Carreño's technique by which heimplants the AcrySof lens (acrylic, Alcon)through a 2.75 mm incision. This is one stageof the Phaco Sub 3 method which he advocates.Carreño from Chile, is a highly skilled cata-ract surgeon.
Carreño emphasizes that in order tointroduce the acrylic intraocular lens throughvery small incisions, as is the case in Phaco Sub3, using adequate technique and equipment isimperative. Otherwise, the implantation couldcause severe trauma to the corneal margins ofthe wound and the endothelium as well asleading to an undesired increase in the size ofthe incision. Before implantation, a generousamount of viscoelastic should be injected intothe capsular bag and the anterior chamber.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
219
Foldable Acrylic Lens of Choice
Carreño's experience is based on the useof Alcon's AcrySof lens model MA30BA(5.5mm optic, total length 12.5mm, PMMAhaptics).
Implantation Technique
The lens is folded with forceps (paddle), placedparallel to the haptics (longitudinal implanta-tion technique). The implantation forceps(Buratto) are used to grasp the lens so that thehaptics are perfectly parallel to the fold, goingthrough the center line of the optic, and reach-ing the edge.
Correctly grasping the Buratto for-ceps is critical to penetration with theAcrySof through a 2.75mm incision. If thelens fold is not completely symmetrically, anedge is produced that impedes its introduction.If the jaws of the forceps are at an angle to thelens fold, a separation is created between thefaces, which may make the lens impossible tointroduce through a small incision.
The surgeon proceeds with the Burattoforceps placed in such a way that the lens foldstays on the left. It is very important that thefirst haptic enters the anterior chamber beforethe optic. Otherwise, the lens may be damagedif the haptic is trapped with the optic inside thecorneal tunnel. Then the surgeon inserts theoptic by exerting pressure and using slightlateral movements along the corneal tunnel.The spatula, introduced through the lateralparacentesis, exerts firm and constantcounterpressure. (In order to exert adequatecounterpressure, the lateral paracentesis mustbe placed 60 degrees from the main incision.)This pressure and counterpressure maneuver isanother key aspect of successful implantation
of the AcrySof MA30BA through a 2.75mmcorneal incision without complications.
Before completing the insertion of theoptic, which should be very controlled so as notto penetrate abruptly into the anterior chamberand risking the integrity of the posterior cap-sule, the surgeon puts the haptic under the edgeof the capsulorhexis so it can be placed in thecapsular bag.
Once the optic is in the anterior chamber,the Buratto forceps are rotated 90 degrees inthis position, and they are released so the lensunfolds (Fig. 133). Due to the thin incision, thelens tends to be trapped in the claws of theforceps. To release it, the surgeon pushes gen-tly downward with the spatula. Now the for-ceps may be withdrawn, and the lens continuesto gradually unfold (Fig. 133). The secondhaptic is immediately grasped with Kelman-McPherson forceps to introduce it into theanterior chamber. Aided by the spatula, using abimanual maneuver, the implantation is com-pleted by placing the lens optic first and thenthe second haptic into the capsular bag (Fig.134).
Implantation of the AcrySof MA30BAlens through a 2.75mm corneal incision is noteasy, but Carreño emphasizes that if thedescribed technique is followed step by step,the surgeon can perform it without injuringcorneal tissues. However, when dealing withAcrySof MA30BA lenses stronger than 24diopters, Dr. Carreño prefers to use a slightlylarger incision (3.0mm) because the greaterthickness of these lenses may make them diffi-cult or impossible to implant through a 2.75mmincision. (Editor's Note: as pointed out at thebeginning when describing the acrylic IOL'simplantation, most expert surgeons find it verydifficult or unfeasible to implant an acrylic lensthrough a 3.0 mm incision using forceps with-out harming the lips of the wound - Fig. 132).

THE ART AND THE SCIENCE OF CATARACT SURGERY
220
Once the implantation is complete, theviscoelastic is carefully removed from the an-terior chamber and from the capsular bag. Thesurgeon must take care not to leave viscoelasticmaterial behind the intraocular lens. (It is nec-essary to push the implant optic gently back-ward with the cannula to force the evacuationof the viscoelastic through the capsulorhexisopening.)
Finally, balanced saline solution is in-jected through the lateral paracentesis to en-sure that the incision is perfectly self-sealing.
Dodick's AcrySof's ImplantationTechnique
Special Features AboutAcrySof´s Implantation
When handling the lens, it is importantto keep in mind that especially in high powersup to 30 diopters, this is a thick lens. Thismakes folding more difficult. Jack Dodick,M.D., has found that pre-warming the lensdramatically facilitates the ease of the fold.This is done at his institution (Manhattan Eyeand Ear Hospital) by placing it in a warmenvironment such as on top of a sterilizer thathas an ambient temperature between 100 and105 degrees. This seems to soften the materialand facilitates the gentle folding of the lens,making it much easier to implant especiallyfor high diopter lenses which are more diffi-cult to fold.
It is also important to keep in mind thatif the surgeon performs rapid folding of acold lens, this may leave striae in the lens that
could conceivably interfere with visual acu-ity.
A second measure taken by Dodick tofacilitate this lens' entry into the wound afterfolding and holding it with forceps is to pinchthe lead edge of the lens with a secondforceps, to make the "nose" conform into abullet or missile shape. This facilitates entryinto the eye. Once the nose enters into theeye, the rest of the lens follows with greatfacility (Fig. 133).
Dodick uses folding and insertionforceps to insert the lens. They must be veryfine folding forceps so as to add very littlebulk to the combination of lens and forcepsthat have to enter through the small wound(Fig. 132).
Dodick's Three Stage Implanta-tion
Dodick likes to divide the implantationof the lens into three stages once it is in theanterior chamber. First, when the lead haptic isin the capsular bag, the lens is allowed tounfold. Stage two is the implantation only ofthe optic. Stage three, once the optic is im-planted the surgeon inserts the superior hapticby rotating it in with the Lester hook or placingit with a Kelman-McPherson forceps. Dodickconsiders that a common mistake when im-planting any soft foldable IOL, is to implantit in only two stages. Once the inferior haptic isplaced into the capsular bag, some surgeonsproceed immediately to try to place the opticand the superior haptic in one second stage. Hisexperience has taught him that implantationbecomes simpler and more controlled by divid-ing it into the three stages described.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
221
Fig. 133 (right): Foldable Intraocular LensImplantation Through a Corneal IncisionUsing Forceps - Final Unfolded Position
The lens holding forceps are slowlyopened and the lens is gently unfolded (ar-rows) inside the capsular bag as shown. Widelyused cross-action forceps presented in thisfigure (Buratto’s forceps not shown).
Figure 134 (left): Foldable Intraocular LensImplantation Through a Corneal Incision UsingForceps - Final Unfolded Position
This view shows the final unfolded positionof the foldable intraocular lens and its haptics withinthe capsular bag. Please observe the final appear-ance of the corneal incision (C).

THE ART AND THE SCIENCE OF CATARACT SURGERY
222
Implantation Technique forSilicone Foldable IOL's UsingCartridge-Injector System
Lindstrom prefers to implant these lenseswith a cartridge injector system. Since thesecond generation silicone lenses are very flex-ible, they stretch when implanted through acartridge-injector system, providing the sur-geon with the advantage of inserting the lensthrough a smaller incision (Fig. 132-A).
Carreño's technique for implantation ofsilicone foldable lenses starts with the injectionof viscoelastic in the anterior chamber, thecapsular bag and into the cartridge. Once vis-coelastic has been injected into the cartridge,the lens is loaded carefully so that both sides areinserted into the lateral channels. The car-
tridge is then closed and placed in the injec-tor. In order not to enlarge the incision,Carreño considers that it is essential to intro-duce the tip of the cartridge a few millimetersinto the anterior chamber, as its thickness in-creases towards the back (Fig. 132-A). Withthe injector in place, the lens is advanced throughthe cartridge. Once it begins to unfold in theanterior chamber, it is guided with the firsthaptic under the edge of the capsulorhexis andplaced in the capsular bag. Once it is unfolded,the empty cartridge is removed. Using a spatulaintroduced through the lateral paracentesis, thesecond haptic is gently pushed downward andbackward to be placed in the capsular bag aswell.
For you to have a mental picture of theconcept of foldable lens implantation, we referyou to Fig. 135.
Figure 135: Concept of Foldable Intraocular Lens Implantation
This cross section view shows the movement of the foldable intraocular lens during insertion. Folding forcepsremoved for clarity. (1) Folded lens outside the eye. (2) Folded lens passing through small incision. (3) Folded lensplaced posteriorly into the capsular bag through anterior capsule opening and then rotated 90 degrees. (4) Lens slowlyunfolded in the bag. (5) Final unfolded position of lens within the capsular bag.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
223
TESTING THE WOUND FORLEAKAGE
If the corneal incision has been performedadequately, following the principles outlinedin Figs. 90, 91, 92, 93, the surgeon should havea self-sealing stepped valvulated corneal tun-nel incision. These incisions should not leakbut there is always the possibility that this mayoccur. Consequently, we must test the woundfor leakage as shown in Fig. 73 and explainedits accompanying text.
Following the removal of viscoelasticfrom the anterior chamber and capsular bag,BSS is injected through the paracentesis. If thesurgeon finds that there is a leak (Fig. 73) thereare two ways to seal the incision without hav-ing to suture it: 1) Inject BSS into the lips of theincision to hydrate the tissues and seal thewound. 2) Use Professor Juan Murube'smaneuver for the combined placing of a Honanballoon over the eye for 30 minutes at 35 mmHg pressure and administering orally one tab-let of 250 mg Acetazolamide (Diamox).
The way Murube's clever maneuverworks is explained in Fig. 96 and accompany-ing text. In the remote case that the cornealincision leaks and, even more remote, that thetwo methods for sealing described here do notwork and there is a need to suture the incision,it is recommended that the surgeon place onesingle radial suture.
BIBLIOGRAPHY
Basic and Clinical Science Course: Lens and Cata-ract. American Academy of Ophthalmology, Sect.11, 1998-99;8:108-109.
Barret, GD: New hydrogel lenses: current stylesand future trends. Atlas of Cataract Surgery, Ed-ited by Masket Crandal, published by Martin Dunitz,1999, 22:182-193.
Barojas, E.: How to make a safe capsulorhexis.Guest Expert, The Art and the Science of CataractSurgery, Highlights of Ophthalmology, 2001.
Carreño, E.: From can opener to capsulorhexis: Thecrucial step in the phaco transition, 1999.
Centurion, V: Phacoemulsification: Mastering thetechnique. Guest Expert, The Art and the Scienceof Cataract Surgery, Highlights of Ophthalmol-ogy, 2001.
Christensen1 GD., Simpson WA., Younger JJ et al:Adherence of coagulase-negative staphylococci toplastic tissue culture plates: a quantitative modelfor the adherence of staphylococci to medical de-vices. J Clin Microbiol 1985; 22:996-1006.
Davison JA: Free-hand clear corneal incision withLegacy 20,000 aspiration bypass system. Atlas ofCataract Surgery, Edited by Masket Crandal, pub-lished by Martin Dunitz, 1999, 16:115-127.
Dillman, DM: Techniques, thoughts, challenges.Clear Corneal Lens Surgery, Slack, 1999, 11;131-155.
Dodick J.: Null phaco chop. Advances in Tech-nique and Technology, Alcon Surgical, Part 2 of 2,April 1999.
Ernest PH, Fenzel R., Lavery KT, Sensoli A: Rela-tive stability of clear corneal incisions in a cadavereye model. J. Cataract Refractr Surg. 1995;21:39-42.

THE ART AND THE SCIENCE OF CATARACT SURGERY
224
Ernest PH, Tipperman R., Eagle R, et al: Is there adifference in incision healing based on location? JCataract Refract Surg, 1998;24:482-486.
Rosen, E: Clear corneal incisions and astigmatism.Clear Corneal Lens Surgery, by IH, Fine, Slack,1999, 3:21-42.
Fine, IH.: The choo choo chop and flip phacoemul-sification technique. Operative Techniques in Cata-ract and Refractive Surgery, 1998;1(2):61-65.
Fine, IH.: The choo choo chop and flip phacoemul-sification technique. Clear Corneal Lens Surgery,6:72-79.
Fine, IH., Hoffman, RS.: Controversies regardingclear corneal incisions. Clear Corneal Lens Sur-gery, Slack, 1999;1:1-5.
Fine, IH., Hoffman, RS.: Controversies regardingclear corneal incisions. Clear Corneal Lens Sur-gery, Slack, 1999;2:9-20.
Fine, IH, Hoffman, RS: The AMO Array FoldableSilicone Multifocal Intraocular Lens. Interna-tional Ophthalmology Clinics, Edited by DavisEA, Hardten, DR., Lindstrom RL, Vol. 40 Nº3,Summer 2000.
Fine, IH., Lewis, JS., Hoffman, RS: New tech-niques and instruments for lens implantation. Cur-rent Opinion in Ophthalmol., Vol. 9 Nº 1, Feb.1998.
Gimbel, HV.: Advanced capsulotomy. CataractSurgery: The State of the Art. Slack, 1998, 6:69-74.
Gimbel, HV., Brown, D., Fine HI., Fakasaku, H.,Maloney W., Singer, JA., Thornton SP., Gills JP:Advanced phacoemulsification technique. Cata-ract Surgery: The State of the Art, Slack 1998,9:101-124.
Grabow, HB, Gills, JP, Fish, JR, Van Der Karr, M:Advanced cataract incisions. Cataract Surgery:The State of the Art by J. Gills, Slack, 1998; 4:29-51.
Hoffer, KJ: Clear corneal implant surgical tech-niques. Clear Corneal Lens Surgery, by IH Fine,Slack,, 16:251-261.
Hoffman RS: Making the transition to temporalclear corneal cataract surgery under topical anes-thesia. Clear Corneal Lens Surgery, by IH Fine,Slack,, 4:43-57.
Hunkeler, JD.: Personal clear corneal cataract tech-nique. Clear Corneal Lens Surgery, Slack, 1999,8;95-97.
Javitt JC, Want F, Trentacost DJ, et al: Outcomesof cataract extraction with multifocal intraocularlens implantation - functional status and quality oflife. Ophthalmology, 1997:104:589-599.
Kelman, C: Problem-free cortex removal. Advancesin Technique & Technology, Alcon Surgical, April1999, Part 2 of 2.
Kimiya Shimizu: Clear-cornea cataract incision:astigmatic consequences. Chapter 17, ;Atlas ofCataract Surgery, Edited by Masket Crandal, pub-lished by Martin Dunitz, 1999
Koch, PS:Scleral incisions. Simplifying Phacoemul-sification, Fifth Edition, Slack, 1997, 4:27-50.
Koch, PS:Dense cataract phacoemulsification. Sim-plifying Phacoemulsification, Fifth Edition, Slack,1997, 16:177-189.
Koch, PS.: Divide and conquer. Simplifying Pha-coemulsification, Fifth Edition, Slack, 1997.
Koch, PS.: Phaco chop. Simplifying Phacoemulsi-fication, Fifth Edition, Slack, 1997.
Koch, PS.: Stop and chop. Simplifying Phacoemul-sification, Fifth Edition, Slack, 1997.
Kohnen T., Magnowski G., Koch DD: Scanningelectron microscopy surface analysis of foldableacrylic and hydrogel intraocular lenses. J CataractRefract Surg 1996;22(suppl. 2):1342-50.

C h a p t e r 9: Mastering Phacoemulsification - The Advanced, Late Breaking Techniques
225
Lacava, AC., Centurion V: Cataract surgery afterrefractive surgery. Faco Total by V. Centurion.
Langerman DW: Architectural design of a self-sealing corneal tunnel, single-hinge incision. JCataract Refract Surg 1994;20:84-8.
Langerman, DW: Deep groove corneal incision.Clear Corneal Lens Surgery, by IH Fine, Slack,,7:85-93.
Leaming DV. 1996 Practice Styles and Preferencesof ASCRS Members Survey Results. Ocul SurgNews Int 1997; 8:66.
Mackool RJ, Russell RS: Strength of clear cornealincisions in cadaver eyes. J Cataract Refract Surg.1996;22:721-725.
Masket S.: Clear corneal incision: A personalmethod. Clear Corneal Lens Surgery, Slack, 1999,10;121-130.
Murube J.: Cerrando Heridas Fistulizadas - TincionCapsula Anterior . Guest Expert, The Art and theScience of Cataract Surgery, Highlights of Oph-thalmology, 2001.
Murube J.: Using a Honnan balloom to treat ocularaqueous fistulas. Ophthalmic Surgery 1994;25:745.
Neuhann TH: Intraocular folding of an acrylic lensfor explantation through a small incision cataractwound. J Cataract Refract Surg 1996; 22(suppl 2):1383-6.
Neuhann TH: New foldable intraocular lenses.;Atlas of Cataract Surgery, Edited by MasketCrandal, published by Martin Dunitz, 1999, 21:171-172.
Nicoli, C.: Capsulorhexis on a completely opaquecataract. Guest Expert, The Art and the Science ofCataract Surgery, Highlights of Ophthalmology,2001.
Oshika T., Shiokawa Y: Effect of the folding on theoptical qualilty of soft acrylic intraocular lenses. JCataract Refract Surg 1996; 22(suppl 2):1360-4.
Osher, RH: Personal phacoemulsification technique.Phacoemulsification: Principles and Techniquesby L. Buratto, 1998; 31:447-449.
Seibel, B.: Capsulorhexis with shearing and rip-ping. Phacodynamics - Mastering the Tools &Techniques of Phacoemulsification Surgery, ThirdEdition.
Seibel, B.: Nucleus removal technique. Phacody-namics - Mastering the Tools & Techniques ofPhacoemulsification Surgery, Third Edition, Slack,1999.
Seibel, B.: Physics of capsulorhexis. Phacodynam-ics - Mastering the Tools & Techniques of Pha-coemulsification Surgery, Third Edition, Slack,1999.
Snyder, RW: Updates in surgical techniques &therapeutics. Ocular Surgery News, Slack, June 1,2000.
Sugimoto Y., Takayanagi K., Tsuzuki, S., TakahashiY., Akagi, Y.: Postoperative changes over time insize of anterior capsulorrhexis in phacoemulsifica-tion/aspiration. Jpn. J. Ophthalmol, 1998, 42:495-498.
Vaquero-Ruano M, Encinas JL, Millan I, et al:AMO Array multifocal versus monofocal intraocu-lar lenses: log-term follow-up. J Cataract RefractSurg. 1998;24:118-123.
Zacharias W: Biometry: its importance. Faco Totalby V. Centurion.

THE ART AND THE SCIENCE OF CATARACT SURGERY
226

C h a p t e r 10: Focusing Phaco Techniques on the Hardness of the Nucleus
229
FOCUSING PHACO TECHNIQUES ONTHE HARDNESS OF THE NUCLEUS
MULTIPLICITY OFTECHNIQUES
Visiting prestigious eye centers andthrough personal communications with anumber of expert consultants throughout theworld, it is interesting to observe how manydifferent techniques and modifications of thebasic phacoemulsification procedures havebeen developed. They all work well, if usedin skilled hands. In addition, watching videosof phaco procedures performed by outstand-ing cataract surgeons from different regions,cultures, races and economic status of theircountries, surgeons who perform a thou-sand or more cataract operations a year,we find them using techniques that are quitedifferent from each other. Some use lowvacuum, others use high vacuum, one uses a60º phaco tip while the next one uses a 0 (zero)degree tip for the same type of cataract. Onewould do a supracapsular while the otheremphasizes the need to do all cataracts usingan endocapsular technique. Some are crack-ing, some are chopping.
The Essential Criteria for Success
The revealing experience is that the greatmajority of their cases have very good resultsand the operated eyes look very well. Whatwe learn from this experience is that each
surgeon has developed a technique with whichhe/she feels comfortable, that works best forhim/her and that fills the essential criteria ofnot damaging the posterior capsule, theiris and/or the corneal endothelium.
DIFFERENT NUCLEUSCONSISTENCY -TECHNIQUES OF CHOICE
In Chapter 9, in discussing the Manage-ment of Disassembling the Nucleus, we pre-sented the surgical principles of the major,late-breaking techniques mostly used now,showing how they work and how theyare performed. These can be classified as:1) Divide and Conquer (D & C) techniquesand 2) the chopping procedures based onmodifications of the Phaco Chop of Nagahara(Japan). Most of the now extensively usedtechniques that we present in Chapter 9 havebeen developed by pioneers and distinguishedsurgeons from North America (Gimbel fromCanada; and Paul Koch, MacKool, Dodick,and I. Howard Fine, from the U.S.). Manyother prestigious surgeons from all continentshave made substantial contributions to renderthis step of the operation more effective andless risky.
Now let us try to get into the crucialsubject that most ophthalmic surgeons want

THE ART AND THE SCIENCE OF CATARACT SURGERY
230
to know: What are the procedures of choicewhen we need to remove nuclei of differentconsistencies?
The answer is that this is not a math-ematical formula whereupon the techniquescan be categorized based exclusively on howhard a nucleus we are going to operate. But thesubject is sufficiently clear to allow us topresent highly useful guidelines, based on theextensive experience of highly recognized sur-geons. This is what we are providing you here.
In Chapter 9, you can find the guidelinesand surgical principles of the techniques mostsurgeons use now and what consistency ofcataracts do better in general with the majortechniques such as D & C operations, the Stopand Chop, the Crater Chop, the Null-PhacoChop and the Choo-Choo Chop and Flip. Avariety of other procedures not described inChapter 9 are modifications of the fundamen-tal techniques and carry the name of the sur-geon who sponsors the procedure.
Representative Experts
Confronting Nuclei of DifferentHardness
Now let us focus more specifically onthe procedures of choice of some highly repre-sentative experts from different regions of theworld regarding the operation they use whenconfronting nuclei of different consisten-cies. These surgeons are: RichardLindstrom, M.D., from the U.S.; LucioBuratto, M.D., from Europe (Italy); OkihiroNishi, M.D., from Japan, EdgardoCarreño, M.D., (Chile) and VirgilioCenturion, M.D., (Brazil) the latter two rep-resenting different regions and cultures ofSouth America. Each one of these surgeons
has performed many thousand phacoemulsi-fication procedures. They are highly success-ful and their concepts are solid. What wepresent in this Chapter is how each one ofthese five (5) prestigious surgeons performphaco, with emphasis on nucleus removalwhen faced with the five types of cataracts thatwe are all familiar with, based on differentnucleus consistency.
You may observe that each one of themhas a different procedure of choice. I willconfirm that they are all successful. Thisexperience may serve the ophthalmic surgeonas guidelines within which to select the tech-nique he/she feels more comfortable with andthat may serve the patients best. A great dealdepends on where you practice, what equip-ment and facilities you have and the type ofcataracts you mostly do.
LINDSTROM'S PROCEDURESOF CHOICE
1) For Soft and Medium Density (stan-dard) Cataract: the supracapsular iris-planeprocedure (Figs. 136-139).
The supracapsular operation is popu-larly known as the "tilt and tumble" technique.It is performed on the iris plane and is notendocapsular.
2) Posterior capsular cataract or thecataract in a young patient with relativelysoft nucleus without much ultrasound powerneeded: the supracapsular iris plane technique.
3) For Very Hard Nuclei: the Stop andChop (an endocapsular technique) describedin Figs. 107-111).
Lindstrom considers that a clear cor-nea incision is not indicated when doing thestop and chop in very hard nuclei. He uses acorneo-scleral incision and larger amounts of

C h a p t e r 10: Focusing Phaco Techniques on the Hardness of the Nucleus
231
viscoelastic. More ultrasound energy is neededto disassemble these very hard nuclei withmore danger of wound burn and endothelialdamage. The sclera is more resistant to theheating up of the wound than is the cornea. Inaddition, by moving back to the sclera you arefarther away from the corneal endotheliumwith less risk of damage, particularly in pa-tients with borderline corneas.
Advantages of the Supracapsular
Lindstrom notes that supracapsulartechniques enjoy increasing popularity. Aslightly larger anterior capsulorhexis (5.5 to6.0 mm), is necessary. This allows the sur-
geon to bring a part of the nucleus or the wholenucleus in front of the anterior capsular ridge(Figs. 136-137).
In addition, Lindstrom considers thatwith the endocapsular techniques the numberof posterior capsular tears with or withoutvitreous loss is higher for most surgeons be-cause they are working inside the capsularbag. With a supracapsular technique thenucleus is up closer to the anterior chamber sothe incidence of posterior capsule tears is re-duced. It is also a very easy technique to learn.For a beginning surgeon the endocapsular tech-niques are more difficult to teach and need alonger learning curve and more time to per-form (see Chapters 7 and 9).
Figure 136: Lindstrom’s Supracapsular(“Tilt and Tumble”) Technique
Following clear corneal temporalincision (T), superior limbal counterpunc-ture for secondary instrumentation (S), and5.5 or 6.0 mm circular capsulorhexis (C), aPearce hydrodissection cannula (H) is in-troduced between the nucleus (N) and cap-sule. Slow continuous hydrodissection isperformed with BSS (blue arrow) beneaththe anterior capsular rim until a fluid wave(W) is seen. Irrigation is continued untilthe nucleus tilts up on one side (red arrow),out of the capsular bag. This is the “tilt”portion of the “Tilt and Tumble Phaco Tech-nique.” Viscoelastic is introduced beneaththe nucleus and into the chamber (notshown).

THE ART AND THE SCIENCE OF CATARACT SURGERY
232
Disadvantages of the Supracapsular
The disadvantage of the supracapsulartechnique is that you are working much closerto the corneal endothelium. The surgeon mustbe very careful in his technique and should notperform it on a very hard nucleus. With themodern technology available in the phacomachines (Chapter 8) and the adequate use ofviscoelastic we have another margin of secu-rity to protect the endothelium.
Another measure that helps a good dealto protect the endothelium is to do the pha-coemulsification with the bevel of the tip downor to the side. You have the alternative ofplacing the phaco instrument in the eye with the
bevel anterior, bevel to the side, bevel downor bevel close to you. There is a little spraythat comes out of the phaco tip when you aredoing the surgery. We want that spray to goaway from the corneal endothelium so it isimportant to place the bevel to the side or thebevel down technique in using supracapsulartechnique.
Contraindications of Supracapsular
Lindstrom performs the supracapsulartechnique in all cataracts except: 1) Patientswho have cornea guttata, Fuchs' dystrophy orlow endothelial counts. 2) Very hard cata-racts.
Figure 137: Phacoemulsification of the FirstHalf of the Nucleus - Lindstrom’s Supra-capsular (“Tilt and Tumble”)
With the nucleus (N) tilted toward themain incision, the phaco probe (P) emulsifiesand removes one half of the nucleus using anoutside-in approach. During this removal, thenucleus is supported by a second instrument,such as a nucleus rotator (R) introducedthrough the secondary counterpuncture (S).

C h a p t e r 10: Focusing Phaco Techniques on the Hardness of the Nucleus
233
HIGHLIGHTS OF THESUPRACAPSULAR IRIS PLANETECHNIQUE
The main steps are illustrated and ex-plained in Figs. 136-139. The surgeon needsto become quite adept at hydrodissecting untilthe nucleus is lifted, which is the first step
prior to tumbling the nucleus in a supracapsularapproach. Rather than completing the tum-bling of the entire nucleus, Lindstrom sup-ports the nucleus in the plane of the iris andanterior capsular leaflet and then emulsifieshalf of it (Figs. 136-137). With a much smallernuclear remnant, he tumbles the remaining onehalf upside down and completes the emulsifi-cation (Figs. 138-139).
Figure 138 (left): Tumbling the RemainingHalf of the Nucleus - Lindstrom’s Supra-capsular (“Tilt and Tumble”)
One half of the nucleus has been re-moved, the remaining half is tumbled upsidedown (arrow) with the secondary instrument(R). This brings the nucleus into a position tobe attacked from the opposite pole with thephaco probe (P).
Figure 139 (right): Phacoemulsificationof the Second Half of the Nucleus -Lindstrom’s Supracapsular (“Tilt andTumble”)
The remaining nuclear half isemulsified and removed with the phacofrom an outside edge-in direction. Again,the nucleus is supported in the iris planeby the secondary instrument (R) duringphacoemulsification.

THE ART AND THE SCIENCE OF CATARACT SURGERY
234
In this operation, it is important to makea slightly larger anterior CCC (5.5 to 6.0 mm).If a small anterior capsulorhexis is done, thehydrodissection step where the nucleus is tiltedcan be dangerous and rupture the posteriorcapsule during hydrodissection could be pos-sible. If a small anterior capsulectomy isinadvertently created, Lindstrom favors con-verting to an endocapsular phacoemulsifica-tion technique or enlarging the capsulorhexis.If he is unable to tilt the nucleus with eitherhydrodissection or manual technique, he willalso convert to an endocapsular approach.
Occasionally the entire nucleus willsubluxate into the anterior chamber. In thissetting, if the cornea is healthy, the anteriorchamber roomy, and the nucleus soft, he willoften complete the phacoemulsification in theanterior chamber keeping the nucleus awayfrom the corneal endothelium. The nucleuscan also be pushed back inferiorly over thecapsular bag to allow the iris plane tilt andtumble technique to be completed.
CENTURION'S TECHNIQUESRELATED TO NUCLEUSCONSISTENCY
1) For soft nucleus (+) Centurion'sprocedure of choice is the flip and chip (Fine- see Figs. 122-126).
2) For intermediate nucleus (++) (thosenot hard enough to be chopped), Centurionperforms the classical divide and conquer(Figs. 56, 67, 103, 104, 206 below).
Because Centurion does not performhydrodelamination, he usually removes theepinucleus during emulsification of thenucleus. If the hydrodissection was well done,usually irrigation-aspiration (I/A) will not benecessary.
3) For hard nucleus (+ + + and above)Centurion's favorite technique is the PhacoQuick Chop, as developed by Pfeifer. Theparameters he prefers are based on the differ-ent machines that he uses and are presented.
The main difference between this tech-nique and other phaco chop procedures are:1) The placement of the chopper is in thecenter of the lens, and not under the anteriorcapsule. 2) The movement of the chopper isvertical, instead of horizontal as in otherphaco chop techniques.
Highlights of Other Steps inCenturion's Technique
Anesthesia: For routine cases he recom-mends topical anesthesia. Peribulbar is usedfor special situations, such as subluxated lens,white cataract, combined cataract- glaucomasurgery and so on.
The Ancillary Incision: Usually, hesits at the head of the patient, performingfirst the ancillary incision and injecting aviscoelastic substance. This incision isplaced 80º away from the primary incision,which is usually located between 10 and 11o’clock (Fig. 41).
The Primary Incision: Is a one stepincision between 10 and 11 o'clock per-formed with the 3.0 mm clear path (Asico)diamond knife (Figs. 41, 42).
Capsulorhexis: He refills the anteriorchamber with more viscoelastic and per-forms a 5.5 mm capsulorhexis, with a cysto-tome.
Hydrodissection: The next step is thecortical cleaving hydrodissection, as de-scribed by Fine. The nucleus must be totallyor completely free inside the capsular bag. Atthis time, he rotates the nucleus once or twiceclockwise or anti-clockwise.

C h a p t e r 10: Focusing Phaco Techniques on the Hardness of the Nucleus
235
IOL Implantation: he injects vis-coelastic. For routine cases Centurion usesfoldable IOLs. He has been working withsilicone IOL's for many years and is veryconfident with the implantation techniqueusing the unfolder through 3.0 mm incision.
It is not necessary to enlarge the incisionduring the implantation. In his experience,with the acrylic lens it is necessary to enlargeto 3.5 mm to implant the Sensar (Allergan)and 3.75 mm with the AcrySof (Alcon).

THE ART AND THE SCIENCE OF CATARACT SURGERY
236

C h a p t e r 10: Focusing Phaco Techniques on the Hardness of the Nucleus
237
CARREÑO'S NUCLEAREMULSIFICATION TECHNIQUEOF CHOICE (PHACO SUB 3)
For the latest concepts on surgery re-lated to density of cataracts, I also refer youto page 7. Carreño's Phaco Sub 3 is aphacoemulsification procedure performedthrough an incision of 3 mm or less. Thereare other modifications of the phaco tech-nique also identified as "Phaco Sub 3." Hisgoal is to make it as uninvasive as possible.He follows all the parameters appropriatefor the entire spectrum of nuclear densitythat have proven to be efficient, safe, andreplicable by other surgeons. Obviously, inorder to achieve good surgical results, it isimperative that the phaco machine settingsare perfectly adjusted to the needs of eachtype of nucleus and to the requirements ofeach step of the technique. Carreño usesthe Legacy 20,000 equipment (Alcon).
Adjusting the EquipmentParameters to RemoveCataracts of Various NuclearDensity
It is important to keep in mind that thebasic parameters of the phacoemulsifier arethe ultrasound power, the vacuum, and theaspiration flow. These are amply discussedand beautifully illustrated in pages 112-114,119-122 and Figs. 83, 84, 61-65.
Three Sets of ValuesProgrammed Into Memory
Carreño uses the following criteria:three sets of values programmed into thememory in the Legacy 20,000. These param-eters are set according to the degree ofhardness of the cataract. They are:
• Memory 1: Use high ultrasound powerto enable a quick (continuous mode) nuclearsculpt or chisel and lower levels of vacuumand aspiration flow (Fig. 56). There is noneed for great grasping or fixation power, orpower of attraction in this stage of the tech-nique.• Memory 2: For capture, mobilizationand emulsification of nuclear fragments(pulse mode) (Figs. 67, 68) it is necessary tohave high vacuum levels and aspiration flowin order to achieve considerable grasp andfixation power. It is also necessary to havelittle ultrasound power so that the nuclearfragments that are free are not propelled fromthe phaco tip by excessive vibration.• Memory 3: Is intended for the removalof soft material like the epinucleus, and usesmuch lower values in all settings, in pulsemode (Fig. 69).Height of the bottle (infusion): 75 cm to85 cm.Phaco tip: Kelman type (curved) ABS MicroTip with a 30-degree tip (Fig. 84).
If a good hydrodissection is performedwith the cortical cleaving technique, it ispossible to remove the epinucleus along with

THE ART AND THE SCIENCE OF CATARACT SURGERY
238
the nuclear material in the majority of me-dium hard cataracts and in virtually all hardcataracts.
Working with well-programmedmemories is a great advantage when usingthe Phaco Sub 3 Technique. By eliminatingfiltration through the surgical wound, thesmaller incision directs the flow of liquidand nuclear fragments towards the micro tipfor aspiration, making the phacoemulsifica-tion procedure more efficient. That is, thereis no competition between the flow of liquidtoward the surgical incision and the flowtoward the phaco tip, which can occur withlarger, leaking incisions. Also, the morehermetic incision of Phaco Sub 3 reduces theamount of liquid circulating in the eye dur-ing surgery and maintains a deeper and morestable anterior chamber. This helps preservethe integrity of the corneal endothelium andthe posterior capsule, which, undoubtedly,confers greater safety to the technique.(Editor’s Note: see Chapter 7 for a verywell illustrated presentation of the fluidics ofphacoemulsification).
While performing Phaco Sub 3 it isvery important to keep in mind that a lateralmovement of the micro tip must be avoidedso as not to enlarge the incision duringsurgery. It is therefore necessary to alwayskeep the micro tip working from 12o’clock to 6 o’clock without lateral move-ment. This explains the great importance ofa second instrument (manipulator or chop-per), introduced through the lateral paracen-tesis to facilitate rotation, mobilization ma-neuvers, and nuclear fracture.
Before beginning nuclear emulsifica-tion, regardless of the technique used, thesurgeon should always inject viscoelastic inthe anterior chamber to ease the penetration
of the phaco tip and to provide protection tothe corneal endothelium.
Technique of Choice andConsistency of Cataract
SOFT CATARACTS (grade 1 - 2nucleus)
Carreño recommends Fine’s Chipand Flip because the nuclei are not veryhard and generally cannot be fractured (Figs.122-126). With this technique, it is impor-tant to use hydrodissection andhydrodelamination maneuvers. Hydrodis-section makes free nuclear rotation withinthe capsular sac easier, andhydrodelamination clearly outlines the sepa-ration between the harder inner nucleus andthe softer epinucleus that surrounds it. Thegold hydrodelamination ring denotes thelimit to which it is possible to emulsify thenucleus without risking capsular damage(Fig. 48).
First Step (“memory 1”: vacuum 0to 10 mm Hg, aspiration flow 18 cc/min,U/S power 60%).
With a manipulator introducedthrough the lateral paracentesis, the nucleusis gently moved toward 12 o’clock to allowthe micro tip, maintained in a central posi-tion, to emulsify the inner nucleus ring at 6o’clock without the risk of reaching thecapsular fornix. Then, with the manipulator,the nucleus is rotated in order to place othernuclear fragments in position to be emulsi-fied. The microtip must not be advancedpast the gold hydrodelamination ring. Thismaneuver is repeated until the entire innernuclear ring is completely removed.

C h a p t e r 10: Focusing Phaco Techniques on the Hardness of the Nucleus
239
Second Step (“memory 2”: vacuum200 mm Hg, aspiration flow 25 cc/min, U/Spower 40%, 6 - 8 pulses/sec).
The manipulator is inserted into thecleavage plane obtained throughhydrodelamination and is passed behind theresidual nuclear fragment (chip). The chip islifted and taken to the center of the capsularsac. It is here that the chip may be emulsi-fied with greater safety.
Third Step (“memory 3”: vacuum100 mm Hg, aspiration flow 20 cc/min, U/Spower 30%, 6 - 8 pulses/sec).
The center of the epinucleus is pushedtoward 6 o’clock with the manipulator. Slid-ing the epinucleus out of the upper capsularfornix, the microtip can pull the epinucleusup toward the main incision using aspirationonly (phaco pedal in position 2). The epi-nucleus is then folded over itself top-down(flip), using the spatula and the microtip.This moves the nucleus away from the pos-terior capsule. Once the flip maneuver iscompleted, the epinucleus is removed safelyby simple aspiration or using low powerultrasound (Figs. 122 – 126).
MEDIUM DENSITYCATARACTS (grade 2 - 3 nucleus)
For cataracts with a medium-hardnucleus, Carreño prefers to use Shepherd’sQuadrant Nuclear Fracture technique,which is a variation of Gimbel’s original“Divide and Conquer” procedure (Fig. 67)which is a grooving and cracking method.Carreño considers that Shepherd’s tech-nique has become the nuclear fracturetechnique most widely used by phaco sur-geons because of its simplicity and the high
level of safety it provides. The nucleus issoft enough to allow quick sculpting withlow ultrasound. At the same time it is hardenough for the surgeon to create fractureswithout difficulty (keep in mind that softgrade 1 (+) cataracts cannot be fractured).Furthermore, with grade 2-3 nuclei, no ex-cessive pull is exerted on the zonule whilethe fragments are sculpted, which can occurwith harder nuclei.
In general, all of the nuclear fracturetechniques (Fig. 106) aim to divide thenucleus in multiple fragments to allow theirremoval through the small circular apertureof the capsulorhexis and also to make pha-coemulsification more efficient inside thecapsular bag (Fig. 105). Phacoemulsifica-tion of small fragments of nuclear materialis faster than emulsification of an entirenucleus. The procedure is therefore quicker,and the ultrasound time is reduced. Thefragments are mobilized more easily withinthe capsular bag and it is possible to takethem to the center without much difficulty(Fig.111). This allows them to be removedin a safe zone, eliminating the risk of injuryto the posterior capsule or the corneal endot-helium.
In Quadrant Nuclear Fracture, thenucleus is divided into four parts, which arethen moved individually toward the centralsafe zone to be emulsified (Fig. 105).
First Step (“memory 1”: vacuum 10to 20 mm Hg, aspiration flow 25 cc/min,U/S power 70%):
A manipulator is introduced throughthe side port incision to rotate the nucleus(Figs. 56 and 67). Moving the microtipfrom 12 o’clock to 6 o’clock, thin and deepgrooves are carved until a cross is formed(Fig. 67). Ideally, these grooves should

THE ART AND THE SCIENCE OF CATARACT SURGERY
240
extend almost to the edge of thecapsulorhexis (to avoid the peripheral cap-sule), and should be deeper in the middlethan in the periphery (to respect the curve ofthe posterior capsule) (Figs. 103, 104). Theyshould also be slightly thicker than the ultra-sound tip (including the silicone sheath) andshould be 80%-90% of the depth of thenucleus (Fig. 103). The visualization of thered reflex at the bottom of the groove indi-cates adequate depth to the surgeon.
Second Step:Once the cross is formed (Fig. 67), the
nucleus is divided into four quadrants. Thephaco tip and the manipulator are placed atthe bottom of the groove at 6 o’clock and arepushed in opposite directions (with a director crossed maneuver) (Fig. 104). The separa-tion results in a fracture line, which extendsfrom the periphery to the center of the poste-rior nuclear wall (Fig. 104). After thenucleus is rotated 90 degrees, fractures areperformed until the nucleus is divided intofour fragments (Fig. 105). The fractureshould include all the nuclear material; all thefragments must be separated in order toensure a good result. Before continuing to thenext step, the surgeon should mobilize thequadrants with the spatula in the capsular bagto ensure that there are no connections be-tween them (Fig. 105).
Third Step (“memory 2”: vacuum300 mm Hg, aspiration flow 35 cc/min, U/Spower 50%, 6 - 8 pulses/sec) (Fig. 67)
The microtip is directed toward 6o’clock, and the phaco pedal is in position 2(irrigation/aspiration without ultrasound).
The first quadrant is captured by plac-ing the tip in contact with nuclear material togenerate occlusion (Figs. 59, 60). For greater
safety, the surgeon may first lift the cornerof the quadrant with the spatula to distanceit from the posterior capsule. With hardercataracts, sometimes simple aspiration is notenough to occlude the opening of themicrotip. Apply a few ultrasound bursts(phaco pedal in position 3) to grasp thenuclear material and generate occlusion(Figs. 52, 53). Once occlusion is achievedand the phaco pedal is again in position 2,the surgeon should wait until the vacuumreaches the aspiration line. This makes itpossible to hold the quadrant firmly on theopening of the tip. At this precise moment,relying on good grasping force, the surgeoncan pull the quadrant toward the central safezone. The quadrant should be completelycontrolled by the manipulator in order toavoid turbulence and contact. Then thequadrant is emulsified with the machine inpulse mode (Fig. 86). With large and hardfragments, it is useful to use chop maneu-vers (with the same chopper or secondaryinstrument) in order to divide the quadrantinto smaller fragments, to make the surgeryquicker and easier (Figs. 105, 106). Theprocedure described is repeated for the otherquadrants until the entire nucleus is emulsi-fied.
HARD CATARACTS (grade 3-4nucleus)
With hard cataracts, Carreño prefersto use chopping techniques. They offerclear advantages over the divide and con-quer procedures in the management of thistype of nucleus (See pages 177-182). As amethod of nuclear fragmentation, the chop-ping techniques derived from Nagahara’soriginal “Phaco Chop” considerably reduce

C h a p t e r 10: Focusing Phaco Techniques on the Hardness of the Nucleus
241
the power and total time of phacoemulsifica-tion, thereby reducing the tension on thezonules and the posterior capsule and con-fining the entire phacoemulsification proce-dure to the central 3 mm of the pupil (Fig.183).
Three important features of the chop-ping techniques are important to emphasize:
1. Chopping is a completely differ-ent method than nuclear fracture. It basicallyconsists of making cuts following the natu-ral cleavage of the lens ( similar to cutting alog with ax blows) (see page 183).
2. In order to lend itself well to thechop maneuver, the nucleus must have afirm consistency.
3. The conservation of energy gainedby not carving grooves (D & C) makeschopping particularly indicated for the man-agement of hard nuclei.
The Stop and Karate Chop
Carreño’s preferred chopping tech-nique is the “Stop and Karate Chop”, whichis a combination of Koch’s “Stop and Chopand Nagahara’s “Karate Chop.” He finds itis a very safe procedure combining the ad-vantages of both techniques.
Without a doubt, Koch’s “Stop andChop” noticeably simplifies Nagahara’soriginal “Phaco Chop” technique by creatingan initial groove (Fig. 107) which, in turn,creates a space in the nucleus, making thechopping maneuvers, mobilization, andnuclear fragment emulsification mucheasier. This explains its great popularity as achop technique (page 184). At the sametime, “Karate Chop,” which corresponds to amodification introduced by Nagahara to his
original “Phaco Chop,” offers a greater ad-vantage by confining the chop to the centralregion within the limits of the capsulorhexis.This means the surgeon avoids the need toreach dangerously with the chopper under theanterior capsule, toward the lens equator, tocreate the fracture.
The “Stop and Karate Chop” techniquebasically consists of three steps, which arethe sculpting or chiseling of the central sul-cus (Fig. 107, page 185) in order to fracturethe nucleus in two halves, the chopping ofthe two hemi-nuclei, (Fig. 106, page 182)and the mobilization and ulterior emulsifica-tion of the nuclear fragments (Fig. 111).(Editor's Note: from the practical point ofview, these are the same principles of theStop and Chop (pages. 184-188), except thatthe direction of the cut in the “Phaco Chop”technique goes from the equator towards thecenter of the nucleus, while the “KarateChop” goes from the anterior pole to theposterior pole).
First Step (“memory 1”: vacuum20 mm Hg to 30 mm Hg, aspiration flow30 cc/min, U/S power 80%):
The procedure is initiated by chiselinga central sulcus with the microtip toward 6o’clock (as if it were nuclear fracture in fourquadrants) (Fig. 107). The chiseling is com-pleted toward the other extreme after rotatingthe nucleus 180 degrees aided by the chopperintroduced through the side port incision(Fig. 109). Once the desired depth is ob-tained, the nucleus is divided into two halves.It is fractured with the phaco tip, and thechopper is placed in the bottom of the sulcus.The surgeon must ensure that the halves arecompletely separated (Fig. 106). From thistime on, no more sculpting or cracking is

THE ART AND THE SCIENCE OF CATARACT SURGERY
242
done, and the chopping maneuvers areinitiated. (Hence, the “Stop and Chop” des-ignation by Paul Koch).
Second Step (“memory 2”: vacuum400 mm Hg, aspiration flow 40 cc/min, U/Spower 60%, 6 to 8 pulses/sec):
The nucleus is rotated 90 degrees sothat it is in a horizontal position to ease thegrasp of the distal hemi-nucleus with themicrotip. The phaco pedal is in position 2(irrigation-aspiration), the microtip is placedagainst the wall of the sulcus in its centralportion while ultrasonic pulses (phaco pedalin position 3) are applied, and the nuclearmaterial is grasped. Once occlusion isreached, the pedal is returned to pedal posi-tion 2 in order to increase the vacuum andobtain good fixation at the microtip. Nowthe choopper is sunk into the nuclear mate-rial slightly in front of the microtip. Bypulling the instruments in opposite direc-tions (the chopper towards the left and themicrotip toward the right), the surgeon frac-tures the distal hemi-nucleus into two halves(Fig. 111, page. 189). The nucleus is thenrotated 180 degrees, and the procedure isrepeated so as to fracture the other hemi-nucleus in two halves as well. The nucleusends up divided into four quadrants.Carreño prefers not to remove the quad-rants immediately. Keeping all the pieceswithin the capsular bag stabilizes the secondhemi-nucleus at the moment the chop isperformed, making the maneuver easier. Itis very important to ensure that all fourquadrants are completely independent ofeach other. Introducing the chopper directlyinto the nucleus, without having to reach theperiphery to carry out the fracture, as with
the “Phaco Chop,” is what promptedNagahara to call this modification of histechnique the “Karate Chop.”
Third Step (“memory 2” is main-tained: vacuum 400 mm Hg, aspiration flow40 cc/min, U/S power 60%, 6 to 8 pulses/sec):
Once the nuclear division is complete,the quadrants are mobilized. They are cap-tured with the microtip and pulled to thecentral safety zone, where they are emulsi-fied. In order to capture the quadrants, thesurgeon grasps the nuclear material by ap-plying some ultrasonic pulses (Fig. 105)(phaco pedal in position 3). Once occlusionis achieved, the vacuum is increased (phacopedal in position 2) to ensure grasp at themicrotip. The maneuver is repeated until allfragments are removed. As with Shepherd’s“Quadrant Nuclear Fracture,” any largenuclear fragments present should be dividedusing chopping maneuvers to speed the pro-cedure.
The presence of a central sulcus playsa fundamental part in the development of the“Stop and Karate Chop” technique, as spaceis created within the nucleus (Fig. 107).With the occlusion of the tip, it is easier toperform the chop, to move the nucleus poste-riorly, and to remove the fragments.
VERY HARD CATARACTS(4-5 grade nucleus):
In these extremely hard nuclei (rubraand nigra cataracts), that represent a greatchallenge for the phaco surgeon, Carreño’stechnique of choice is “Crater and KarateChop,” which is a combination of Gimbel’s

C h a p t e r 10: Focusing Phaco Techniques on the Hardness of the Nucleus
243
“Crater Divide and Conquer” withNagahara’s previously mentioned “KarateChop.” The key to success with these veryhard nuclei lies in reducing the nuclear vol-ume as much as possible while maintaining aperipheral nuclear ring firm enough to per-form chopping maneuvers geared to creatingthe fractures (See pages. 191-193 for refer-ence of the very similar Crater Phaco ChopTechnique - Editor).
The basic steps for the “Crater andKarate Chop” technique are the sculpting ofa very deep central crater, the chopping ofthe peripheral nuclear ring to create multiplefragments, and finally, the mobilization andemulsification of these fragments (Fig. 112-116 for reference).
First Step (“memory 1”: vacuum 20mm to 30 mm Hg, aspiration flow 30 cc/min,U/S power 90%):
Directing the microtip always towards6 o’clock, the surgeon sculpts a crater in thecentral nuclear zone, using rotation maneu-vers to facilitate and deepen it. (The use ofultrasound for a prolonged amount of timeduring this step of the technique is not riskybecause the nuclear sculpting is performedinside the capsular sac, far away from thecorneal endothelium.) In order to fracture, itis necessary to centrally sculpt very deeply(until the red reflex appears in the bottom)while maintaining enough dense material inthe nuclear periphery.
Second Step (“memory 2”: vacuum400 mm Hg, aspiration flow 40 cc/min, U/Spower 70%, 6 to 8 pulses/sec):
The microtip is placed against the wallof the central crater at 6 o’clock, and ultra-sound pulses are applied (phaco pedal in
position 3). The nuclear material is impaled.Once occlusion is reached, the pedal isplaced in position 2 to increase the vacuumin the aspiration line and firmly attach thenucleus to the opening of the microtip. Thechopper is then introduced into the nuclearedge in front of the microtip (“Karate Chop”technique, without taking the chopper to theequator underneath the anterior capsule.)The instruments are pulled apart to completethe first fracture. The nucleus is rotated, andthe maneuver is repeated in order to makethe second fracture, creating the first frag-ment. The process continues until thenucleus is divided into multiple fragments(five or more). The surgeon must ensure thatthere are no connections between them. Theharder the nucleus, the smaller and morenumerous the fragments must be in order tomake them more manageable. While mak-ing subsequent chopping maneuvers, it isuseful to leave the fragments in place tokeep the capsular bag well-distended. Thisreduces the possibility of an inadvertent cutinto the posterior capsule with the phaco tip.
Third Step (uses “memory 2”:vacuum 400 mm Hg, aspiration flow40 cc/min, U/S power 70%, 6 to 8 pulses/sec):
Once the nucleus is fragmented,Carreño proceeds to move each individualfragment toward the center to emulsify it.(Because very hard fragments are involved,it is advisable to inject viscoelastic to protectthe corneal endothelium). The tip is placedagainst the nuclear fragment at 6 o’clock,and ultrasonic pulses are applied (phacopedal in position 3) to capture the fragment.Then the vacuum is allowed to increase

THE ART AND THE SCIENCE OF CATARACT SURGERY
244
(phaco pedal in position 2) to reach a firmgrasp at the microtip opening. The fragmentis then pulled toward the center, into thesafety zone, to be emulsified. The nucleus
is then rotated in order to place anotherfragment at 6 o’clock. The procedure is re-peated until all the fragments are completelyremoved.

C h a p t e r 10: Focusing Phaco Techniques on the Hardness of the Nucleus
245
NISHI'S TECHNIQUES OFCHOICE FOR NUCLEI OFDIFFERENT CONSISTENCIES
Nishi uses two different techniquesdepending on nucleus consistency.
1) Soft (+), Standard (++):In these groups, Nishi uses a modifi-
cation of the Divide and Conquer procedure(Figs. 56 and 67) and sometimes Fine'sChoo-Choo Chop and Flip technique (Figs.122-126) using high vacuum and low ultra-sound energy from the very beginning(vacuum 170 mm Hg, energy up to 60%using Allergan's Diplomax phaco machine).High energy is not necessary for those nu-clei, and it is cumbersome for the surgeon toswitch on from high vacuum-low energy tolow vacuum-high energy.
2) Moderately Hard to HardNucleus (+++):
In cases with moderately hard andhard nucleus, higher energy up to 80%(even 100%) is used for rock-hard nucleus,taking care not to burn the wound. Thishigh energy is combined with low vacuumfor making a groove or a cross. For makinga groove, the tip is never occluded and highvacuum is not needed. After the nucleus isdivided into 2 or 4 parts, the next step isemulsification. The machine is switched tohigh vacuum low energy, unless higher en-ergy is needed for emulsifying the fracturedquadrants. High vacuum is now needed,because the nucleus fragments must bepulled towards the center by occluding thetip opening.
3) Hard (++++) or Very HardNuclei (+++++):
Nishi uses a chopping technique(Figs. 103, 106, 107-111). Care is taken tostay away from the corneal endothelium.
BIBLIOGRAPHY
Buratto, L: Buratto's elective techniques for pha-coemulsification according to grades of hardness ofnuclei. Phacoemulsification: Principles and Tech-niques by Lucio Buratto, 1998; 6:166-170.
Carreño, E.: Nuclear emulsification technique of choice(Phaco Sub 3). Guest Expert The Art and the Science ofCataract Surgery of HIGHLIGHTS, 2001.
Centurion, V.: Centurion's technique related to nucleusconsistency. Guest Expert The Art and the Science ofCataract Surgery of HIGHLIGHTS, 2001.
Lindstrom, R.: Lindstrom's procedures of choice. GuestExpert The Art and the Science of Cataract Surgery ofHIGHLIGHTS, 2001.
Lindstrom, R: Tilt and tumble phacoemulsification.Clear Cornea Lens Surgery, edited by I. Howard Fine,Slack, 1999;9:99-119.
Lindstrom, R: Tilt and tumble phacoemulsification.Operative Techniques in Cataract and Refractive Sur-gery. Vol. 1, Nº 2 (June), 1998: pp. 95-102.
Nishi, O: Nishi's technique of choice related to nucleusof different consistency. Guest Expert The Art and theScience of Cataract Surgery of HIGHLIGHTS, 2001.

THE ART AND THE SCIENCE OF CATARACT SURGERY
246

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
249
INTRAOPERATIVE COMPLICATIONS
Main IntraoperativeComplications
The main complications are relatedto the following phases of the operation:1) complications related to the incision.2) Those associated with anterior capsulorhexis.3) Complications consequent upon rupture ofthe posterior capsule. 4) Complications re-lated to emulsification and removal of thenucleus through different techniques. We alsoneed to confront the complications related tohydrodissection and/or hydrodelineation, thosethat occur during the process of aspiration ofthe cortex, intraocular lens implantation andthe difficulties of the operation when the pupilis small.
Incidence
As pointed out by Howard Gimbel,M.D., the incidence of intraoperative compli-cations will vary to some degree with thesurgeon’s experience and the type of proce-dure performed as, for instance, when a sclerocorneal tunnel is performed versus a clearcorneal incision. It will also vary dependingon the anatomic characteristics of the indi-vidual eye as in small pupils and hypermaturecataracts. Intraoperative complications arealso related to the type of anesthesia utilizedbut this has been significantly diminished bycombining topical and intracameral local an-esthesia which is used in most cases, or usingthis combination with sub-Tenon’s anesthe-
General Considerations
Even in the most experienced hands com-plications occur. The best management ofcomplications is to avoid them. Whenunpreventable, a well thought out, carefullyexecuted plan can give very good visual re-sults.
When using topical anesthesia, the pa-tient is an active participant in the procedure.Complications can occur when patients movetheir head, body, or eye, cough, or squeeze theireyelids. Consequently, they should be fullyeducated and carefully selected. We shouldprovide proper education in advance aboutwhat will be experienced so that the level ofanxiety will be low. When speaking with thepatient, the surgeon should sound calm and incontrol. If patients sense the surgeon's anxietythey may become more anxious, further limit-ing their ability to cooperate. When patientsbecome over sedated they may fall asleep andmight awake disoriented. The best way to keeppatients from waking up suddenly is to keepthem from falling asleep.
In cases under topical anesthesia, exces-sive globe movement can impair the safecompletion of the operation. If the patient isunable to hold the eye steady, or if they areperceiving discomfort from the surgery, aug-menting the anesthesia with a subtenon, peribul-bar, or retrobulbar block may be helpful. Thiscan be accomplished quite safely when a self-sealing wound is done.

THE ART AND THE SCIENCE OF CATARACT SURGERY
250
sia when desired (Chapter 5). Since retrobul-bar or peribulbar anesthesia are practically nolonger used in phacoemulsification, even bythose who are starting in the transition period,the risks of globe perforation or retrobulbarhemorrhage have practically disappeared.
Facing the Challenges
Virgilio Centurion, M.D. from SaoPaulo, Brazil, one of Latin America’s mostexperienced and didactic anterior segment sur-geons, has dedicated years of research andteaching on how to master phacoemulsifica-tion. This includes being prepared for thechallenges of the intraoperative complications,which are different than those we were accus-tomed to face with planned extracapsular.Centurion emphasizes that each cataract op-eration presents its own challenges, and thateven though we have reached a very advancedlevel of safety and predictability with pha-coemulsification, it is important that we keepin mind the complications that may arise so asto minimize situations that may bring the levelof stress to a peak in the operating room.
COMPLICATIONS WITH THEINCISION
Too Short and Shallow or TooLarge
Lindstrom points out that the most fre-quent complication he has with the clearcorneal incision is that he either makes thewidth of the incision a little bit too short, orthe dissection too shallow or too beveled
(Fig. 140). Or else, he makes the incision alittle bit too large. If it is too shallow orbeveled, it will become a non self-sealing, non-valvulated wound. If it is too large, a persistentiris prolapse may occur. You may try to ignoreit but it keeps coming back.
With a superficial, shallow incision, youmay manage it as shown in Fig. 140. Simplyabort the superficial tunnel, go back to the firstor initial vertical groove of the incision (300microns depth) corresponding to 1/2 the cor-neal thickness and place the blade deeper,forming a second tunnel with the correct depthlocated below the first or superficial tunnel(Fig. 140).
If you are having a very difficult timewith an incision, the best thing to do is to closethat incision with one or two vicryl sutureswhich will eventually dissolve and move overto another nearby spot and start over. With aclear corneal incision, starting over only takesa short additional time (Fig. 141).
Problems from Incorrect Place-ment and Performance of Incision
In Fig. 142 you may see a summary ofthe problems in creating the sclero corneal,limbal and corneal tunnel incisions. Thecorrect placement and structure of each inci-sion is presented in Fig. 40. A key elementin the success of phacoemulsification is toobtain a good internal valve incision.
As Centurion has emphasized, it isonly by experience and extreme care that wedevelop a sense of «feeling» of the idealdepth, that is, the one which will not endangerthe intraocular tissues and will ensure a goodtunnel protection.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
251
Figure 140 (left): Complications while Mak-ing a Clear Corneal Incision - Too Shallowand Short
The corneal tunnel incision should beself-sealing and valvulated, at about 300 mi-crons depth. That is approximately half thecorneal thickness. Here we observe that thefirst incision was too superficial (red) notpermitting a proper valve to function. Thereby,the wound is not self-sealing. One solutionfor this is to abort this tunnel and start againfrom the initial incision, go deeper forming asecond tunnel (arrows) below the first super-ficial tunnel.
Figure 141 (right): Problems From Incor-rect Placement of Tunnel Incisions
The correct placement and performanceof the sclero corneal tunnel, limbal or cornealincision is extremely important. In case of thesclero-corneal, a 5 mm external incision (E) ismade 1-3 mm from the limbus to a depth corre-sponding to 1/2 to 2/3 thickness of the sclera. Ascleral tunnel (T) between 2 to 3 mm in length ismade. With blade directed toward and in a paral-lel path to the pupil, the internal valve (V) openingis created. Common placement errors are shownby blue lines. Also shown is a detachment ofDescemet’s membrane (D), another common er-ror that can be avoided by use of abundantviscoelastic. (Original illustration by HIGH-LIGHTS, based on principles from VirgilioCenturion's book titled "Complicações Durantea Facoemulsificação".)

THE ART AND THE SCIENCE OF CATARACT SURGERY
252
Detachment of Descemet'sMembrane
An occasional but important complica-tion is detachment of Descemet’s membrane,as shown in Fig. 143. The main causes are: 1)ocular hypotension while dissecting the tunnelor while constructing the internal part of thetunnel to make the valve-like incision. Theinjection of viscoelastic through the side portof the incision before performing the primaryincision can prevent this from happening. 2)The introduction of the blade in the wrongdirection when constructing the internal part ofthe incision (Figs. 140, 142 and 143). 3) Theforced introduction of the phaco tip or foldablelenses in a tight incision. This may be avoidedby being very careful during entry of the tip, by
lubricating the tunnel with viscoelastic and byvery careful folding of the IOL and lubricationeither of forceps or the injector, in order toattain a non-traumatic introduction and im-plantation of the IOL.
Important: During the dissection ofthe internal step of the incision which leads tothe formation of the internal valve (V), theintraocular pressure must be either normal orslightly high and the tip of the blade must bedirected towards the pupil and follow aparallel path toward the pupil as shown inFigs. 140, 142 and 143. Use abundant vis-coelastic in order to keep Descemet’s mem-brane where it belongs until the conclusion ofthe surgery.
A detachment of Descemet’s membranediscovered postop, is an important complica-
Figure 142: Complications during Incision - Closing of the Im-proper Incision and Making a New One
If the elected incision site is too superficial and short or toolarge (A) so that it may not provide correct sealing, it is advisable toclose the first incision with vicryl sutures and perform a new andcorrect incision next to the first one (B). The surgeon may choose thehorizontal (S) or radial sutures according to his/her experience.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
253
tion when it occurs because it may befollowed by corneal edema and eveninflammation. If it occurs, topical antiinflam-matory medications are sometimes useful.If the detachment is significant, however,(Fig. 143) there may be corneal decompensa-tion progressing to bullous keratopathy whichmay eventually require a penetrating graft.
Precautions with Closure of theIncision Upon Conversion
Conversion to extracapsular is not infre-quent when you start in the transition periodand may be necessary even in the hands of amore experienced surgeon upon the develop-ment of complications. If the incision is cor-neal, move to the limbus. Other surgeonsprefer the scleral tunnel incision or the tunnelstarting at the limbus or about 1 to 1.5 mmfrom the limbus. When converting, enlarge the
incision for the extracapsular at the limbus.The nucleus and cortex are removed and theIOL implanted. When suturing, it is importantto close the wound by placing the interruptedsutures radially. When you get to the junctionbetween the part of the incision where thetunnel was started and the limbus, suture it asshown in Fig. 144. The arrow shows conver-sion when the initial incision was a sclerocor-neal tunnel. Unless properly sutured, the valvemay leak at this site.
Heating the Wound
Very occasionally, if one is not careful,you can heat the wound. It looks like youcauterized the cornea. That is not such aproblem during the surgery but this woundmay well leak. If that occurs, at the end of theoperation, the surgeon has to close the woundby suturing but will not be able to perfectly
Figure 143: Complications with the Tun-nel Incision - Detachment of Descemet'sMembrane
A detachment of Descemet's mem-brane (D) may be observed during con-struction of the valvulated incision, ma-nipulation of the incision with the phacoprobe in a tight incision or from insertion ofthe intraocular lens. This complicationhappens more frequently when making theincision in a hypotensive eye, or the wrongmaneuver when introducing the knife.

THE ART AND THE SCIENCE OF CATARACT SURGERY
254
approximate the edges of the incision becausethis may induce a large astigmatism. The mostpractical approach is to suture the anterioredges of the tunnel to the posterior surface ofthe wound using a mattress suture. A littlegap will remain in almost every setting but youcan create a sealing incision. You shouldexpect a small to moderate amount of astigma-tism, but the good news is that it will go awaywith time. It is only a temporally inducedastigmatism. The difficulty is to get thatincision to seal.
Management of LeakingIncisions with a Positive Seidel
Infrequently, a clear cornea incision or ascleral tunnel incision larger than 3 mm inwidth may show leaking of fluid one daypostoperatively. This is either secondary to anincision larger than planned and not sutured, orby too much trauma in the lips of the woundusually by the phaco tip.
When this leaking occurs, it may beimmediately detected by instilling a drop offluorescein and observing the patient underultraviolet light. The problem with thesepatients is that the constant escape of aqueoushumor keeps the wound open and may re-quire suturing of the incision which certainlyis a nuisance.
Prof. Juan Murube, M.D., fromMadrid recommends a very ingenious maneu-ver in order to close the leaking woundwithout having to re-suture the incision. Heplaces a Honan balloon (Fig.96) over the eyefor 30 minutes at a pressure of 35 mm Hg andat the same time administers 1 tablet ofacetazolamide, 250 mg orally (Diamox). Thehypotony produced when the Honan balloonis removed makes the aqueous humor (that is
constantly being produced and was causingthe positive Seidel) remain in the anteriorchamber. The anterior chamber has the op-portunity to reform. After a few minutes,when the intraocular pressure returns to nor-mal, the walls of the incision have cometogether and adhered, without any furtherpositive Seidel. This ingenious maneuver issimple and avoids having to re-suture thepatient.
COMPLICATIONS RELATED TOANTERIOR CAPSULORHEXIS
It is generally agreed that this is theprocedure of choice to open the anterior cap-sule. In most cases, it allows the phacotechnique to be performed within the capsularbag and, consequently, the maneuvering andinstrumentation does not affect the surround-ing tissues particularly the corneal endothe-lium. Capsulorhexis also allows an almostperfect positioning of the intraocular lens. Asemphasized by Centurion, when the surgeondominates the technique of capsulorhexis, casesof decentration, capture and/or subluxation ofthe IOL are rare.
Main Complications
The main complications may be relatedto: 1) the size of the capsulorhexis. It may beeither too large or too small. This is due to atechnical mistake either in the judgment of thesurgeon or in performing the technique. Theideal diameter of capsulorhexis ranges from5 to 6 mm. Centurion advises that, when thereis doubt, check the diameter of the capsulo-tomy by holding a compass over the cornea.When the capsulorhexis is too small, less than5 mm (Fig. 145), problems may arise during themanipulation of the nucleus and the IOL im-

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
255
Figure 144: Precautions with Clo-sure of the Incision Upon Conver-sion
The wound is closed with in-terrupted sutures radially. When youget to the junction between the part ofthe incision where the tunnel wasstarted and the limbus, you must placethe suture as shown in this figure. Oth-erwise, the valve may leak. (Courtesyof Virgilio Centurion, M.D., from hisbook titled “Complicaçoes Durante aFacoemulsificaçao”.)
Figure 145: Complications Related toAnterior Capsulorhexis - Too Small
When the anterior capsulorhexis(C) is rather small (less than 5 mm), themanipulation of the nucleus may presentproblems that might compromise the suc-cessful results of surgery, and IOL implan-tation may be more difficult.

THE ART AND THE SCIENCE OF CATARACT SURGERY
256
plantation may be more difficult to the extent ofcompromising the final result of the surgery.
If it is considered to be small, perform asmall lateral cut in the capsulorhexis withVannas scissors at 10 o'clock (Fig. 146).Afterwards, perform a second and wider ante-rior capsulorhexis with the Uttrata forceps at12 o'clock which will prevent or eliminatethe likelihood of stenosis of the opening(Fig. 147). This is also a good option on whatto do if there is some discomtinuity or smalltear identified in the anterior capsulorhexis.
When the capsulorhexis is too large(Fig. 148), larger than 6 mm, some difficul-ties may arise in stabilizing the nucleus afterhydrodissection with a tendency for thenucleus to move into the anterior chamber.Thic could possibly endanger the cornealendothelium and other surrounding structuresand emulsification would need to be done inthe anterior chamber. Maintain sufficientviscoelastic between the lens and the endot-helium.
Lindstrom considers that if thecapsulorhexis is really large (Fig. 148) it isnot a major problem although there is atendency to develop a higher rate of capsularopacity because the border of thecapsulorhexis is not placed over the edge ofthe posterior capsule.
Another problem that Lindstrom hascommonly encountered is the chamber willshallow as you are doing the capsulorhexis,particularly in younger eyes. The way toavoid this is that as you see the chambershallowing, put more viscoelastic in it andput it more centrally in the younger eye.
Another complication is that thecapsulorhexis will tear into the zonules. If
that occurs, Lindstrom goes back to thebeginning, makes a little cut with Vannasscissors at the edge of the rhexis (Fig. 146) inthe other direction from where the extensioninto the zonules occurred and enlarges therhexis around the opposite way (Fig. 147). Inthese cases, the surgeon may have to pre-sume that there was a little radial tear to startand must be very careful with the next step,the hydrodissection, because most probablythere is a weak spot in the anterior capsule.In that case you should probably not use aplate haptic lens.
Preventing Rhexis Complications byTinting
One of the major advances in performingcircular continuous capsulorhexis (CCC) inhypermature cataracts which are either totallywhite or very dark is the tinting of the anteriorcapsule. In these eyes, the fundus reflexcannot be seen by the coaxial light of themicroscope. When the reflex is not present, itis extremely difficult to see in order to com-plete the circular capsulorhexis. Tinting of theanterior capsule through various substancessuch as Fluorescein 2%, Indocyanine Green,Trypan Blue, Gentian Violet, or MethyleneBlue is a new development to improve thevisibility of the anterior capsule during CCC.Professor Juan Murube, M.D., in Madrid andProfessor Carlos Nicoli, M.D., in BuenosAires both definitely prefer the use of TrypanBlue as the best coloring substance for thispurpose. They place the tinting substance overthe anterior capsule when the anterior chamberis full of air as advised by Murube. The tech-nique is shown in (Figs. 101, 102, page 173).

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
257
Figure 146 (above): Management of SmallAnterior Capsulorhexis
If it is considered to be small, perform asmall lateral cut in the capsulorhexis with Vannasscissors at 10 o'clock.
Figure 147 (center): Enlarging a Small Capsulorhexis -Managing a Discontinuity of the Rhexis
Perform a second and wider anterior capsulorhexiswith the Uttrata forceps which will prevent or eliminate thelikelihood of stenosis of the opening. This figure also serves toshow what to do when there is a discontinuity or small tearidentified in the anterior capsulorhexis (C). The best optionfirst is the injection of viscoelastic. Next, try with the forceps(F) to perform a second anterior capsulorhexis (arrow) leavinga regular surface with no weak points in order not to alter thecorrect evolution of the surgery. The white arrow identifies thesmall discontinuity of the rhexis which is being repaired.
Figure 148 (below): Complications Related toAnterior Capsulorhexis - Too Large
The ideal size ranges from 5 to 6 mm. Inthis surgeon's view you may observe a largecapsulorhexis (C). This may induce tears of theposterior capsule during the stage of phacoemul-sification or a tendency for the nucleus to move tothe anterior chamber during the operation.

THE ART AND THE SCIENCE OF CATARACT SURGERY
258
COMPLICATIONS WITHHYDRODISSECTION
What we try to accomplish withhydrodissection is that by irrigating with astream of BSS immediately under the anteriorcapsule, we produce a separation of the rest ofthe lens from the anterior capsule, including thenucleus and cortex, and separation of thecortex from the epinucleus.
If you are doing an endocapsular tech-nique, sometimes it is difficult to get the nucleusloose by hydrodissection. Sometimes surgeonswill stop because they find it is taking themlonger than they expected and are not sure howto proceed. If the surgeon stops to the extent ofdiscontinuing hydrodissection, this makes therest of the operation much more difficult andrisky. Lindstrom emphasizes that one shouldcontinue to hydrodissect and do so in different
areas until one is sure the nucleus is loose andwill rotate. Having a loose nucleus byhydrodissection is one of the keys to successwith the endocapsular technique. If thesurgeon does not get the nucleus loose it leadsto complications in the next step.
Centurion emphasizes that if the nucleusdoes not spin freely within the capsular bag itis due to incomplete hydrodissection. It isimportant not to try to rotate the nucleus me-chanically at this stage but, instead, repeat thehydrodissection maneuver and/or introduce inthe anterior chamber a Sinskey hook throughthe main incision and another hook through anancillary incision as shown in Fig. 149. Thehooks are fixed at opposite sides of the nucleus.In Fig. 149 the arrows indicate the direction ofthe spin of the nucleus when a slight traction isapplied but this is done after a repeathydrodissection. For this procedure, the ante-rior chamber should be filled with viscoelastic.
Figure 149: Freeing a Fixed Nucleus AfterIneffective Hydrodissection
Under viscoelastic, a Sinskey hook (1)is introduced in the anterior chamber throughthe main incision and another hook (2)through the ancillary incision. The hooks arefixed at opposite sides of the nucleus (N).Arrows indicate the direction of spin of thenucleus when a slight traction is applied.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
259
Centurion emphasizes not to proceedto the next stage, which is nucleus removalthrough phaco, without being sure that thenucleus is free. In traumatic or congenitalcataracts be particularly careful when per-forming hydrodissection due to the possiblefragility of the posterior capsule.
COMPLICATIONS DURINGNUCLEUS REMOVAL
Before proceeding with phacoemulsifi-cation of the nucleus, it is assumed that thesurgeon has performed correctly all the previ-ous phases of the operation. Upon enteringthis crucial stage of the operation, the surgeonmay have difficulty in fracturing the nucleus.That usually is caused by having performed
too shallow a groove within the lens, not deepenough to allow fracturing of the remainingnuclear bed.
If the surgeon is using the "Divide andConquer" technique, the reliable point of ref-erence when performing the groove, is the tipof the phacoemulsifier as shown in Fig. 150.The tip of the phacoemulsifier should pen-etrate the central region of the nucleus 1 1/2to 2 times the diameter of the tip of thephacoemulsifier (Fig. 150). The arrows inthis figure show the direction of opposingforces applied to both sides of the groove inorder to fracture the nucleus. As this pro-ceeds, the red reflex becomes redder (Alsosee Figs. 104 page 178, and 106 page 182).The most serious complication of nucleusremoval is rupture of the posterior capsule,which we address separately in this chapter.
Figure 150: Proper Depth of the LensGroove for “Divide and Conquer” Tech-nique
As indicated, the depth of the lensgroove should be 1 1/2 to 2 times thediameter of the tip of the phacoemulsifier(P). Arrows show the direction of oppos-ing forces applied to both sides of thegroove to fracture the nucleus.

THE ART AND THE SCIENCE OF CATARACT SURGERY
260
Surgeon's Fatigue
Lindstrom points out that another pre-ventive measure to avoid complications dur-ing nucleus removal is that in the moredifficult eyes, the surgeon fatigues, or getstired. When this happens, he stops and rests.The minute you think you do not seem totallycomfortable and your movements get a littleawkward he recommends stopping and putsome viscoelastic in the eye. Use two instru-ments to rotate the nucleus into a more favor-able position (Fig. 149) and then start again.In some difficult eyes Lindstrom may restartand stop even two or three times. Maybe thatmeans the case took four minutes longer butthis is not important. In those really difficulteyes it can mean the difference between suc-cess and failure. In some complicationssymposia, if you observe the live surgeryyou can see the tremors of some surgeon'shands when it is taking them a long time indifficult cases, and they get awkward anduncomfortable, they just cannot get thenucleus into the right position. In those casesLindstrom thinks if you just stop and rest fora minute, put a little viscoelastic, take yourtime and be patient until being able to rotatethe nucleus (or other difficult maneuvers) youcan save yourself and the patient a great dealof problems.
COMPLICATIONS DURINGREMOVAL OF THE CORTEX
After the nucleus has been removed, it isimportant that the surgeon remain concentratedon proceeding with skill and attention to everydetail to the end stages of the operation. It isnatural for some surgeons to consider thatimmediately after removing the nucleus, themain steps of the operation have been con-
cluded and it is time to relax. Not so. Anunpleasant rupture of the posterior capsulemay occur during the following step, which isremoval of the cortex.
Lindstrom emphasizes that for mostpeople removing the cortex is "easy" but manyof the series in the world literature will showthat as many posterior capsules are torn duringcortical removal as are during the nucleus re-moval. The hard part is over but do not looseconcentration. Slow down, and make sure youdo this step properly. The cortex usually isquite easy to remove but most of the difficultyand risk occurs when trying to vacuum cleanthe posterior capsule. Lindstrom is not con-vinced that it makes any difference to vacuumclean the posterior capsule because this is notwhere the source of the eventual opacificationof the posterior capsule. He discouragesaggressive vacuuming of the posterior capsule.If you are going to do it be very certain thatthere is no barb or sharp point on the tip of theI/A. He has seen many capsules torn by a littlebarb or sharp tip on the I/A tip particularlyduring the vacuum cleaning.
COMPLICATIONS DURINGFOLDABLE IOL's IMPLANTA-TION
Wrong IOL Power andDecentration
To prevent complications, the key is toget the lens symmetrically into the capsularbag or symmetrically into the ciliary sulcus iffor some reason the surgeon feels insecureabout the capsular bag being intact. This re-quires being very observant that there is a goodcapsular rim and certain that you are placingthe complete lens at the bottom of the capsule.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
261
Also, be sure you have the correct lensand correct lens power. Surgeons who receivemany referrals from other colleagues considerthat the most common reasons they have tooperate in order to change an IOL are: 1) errorin lens power calculation during the previousoperation and 2) late decentration or sublux-ation.
Asymmetric Capsulorhexis
Sometimes, a decentration of the IOLoccurs because there is an asymmetriccapsulorhexis. The margins of the rhexis arenot over the optic on all sides. Consequently,one side gets underneath the lens, it fibrosesand pushes the lens aside. If for some specificreason the haptics were placed in the sulcus,sometimes the sulcus can be very large, as inmyopes, and there can be an area of disinser-tion.
Deficient Intraoperative Handling
Carlos Nicoli, M.D., one of Argentina'smost prestigious cataract surgeons, finds thatthe intraoperative complications with foldableIOL`s are not significant but we do have to bealert as to problems arising from intraoperativehandling of the lenses, the instruments used tofold the lenses, the injectors and the forceps.Heavy or high density viscoelastics placedwithin the plastic injectors have led to breakageof the injector at the time of insertion. Inaddition, if the surgeon does not have enoughexperience with the injectors, he may scratchthe lens optic. Also, if we grasp the lenses withforceps without a stop at the tip, the optics canbe scratched at the time of folding.
Nicoli points out that tears may occur inlenses at the time of insertion. They may be:1) partial tears where vision is not affected
because they are not within the central zone;and 2) others have suffered significant tearsand have had to be removed during surgery,requiring that a new lens be inserted. Thesetears might have been due to the lack of lubri-cation with viscoelastic or because the sur-geon did not use the proper technique of inser-tion.
Importance of Warming AcrylicIOL's
Upon using acrylic lenses, they shouldbe warmed before folding and implantation.This measure provides easier folding and aslower unfolding. If we attempt to fold andimplant an acrylic IOL at room temperature,the lens presents resistance to folding and acertain resistance to unfolding.
Management of Complicationswith Array Multifocals
As emphasized by Fine and Hoffman,in situations in which the first eye has alreadyreceived an Array lens implant, complicationsmanagement must be directed toward findingthe way to implant an Array IOL in the secondeye. Under most circumstances, capsulerupture will still allow for implantation ofan Array lens as long as there is an intactcapsulorhexis. Under these circumstances,the lens haptics are implanted in the sulcus, andthe optic is prolapsed posteriorly through theanterior capsulorhexis. This is facilitated by acapsulorhexis that is slightly smaller than thediameter of the optic (Fig. 145) in order tocapture the optic in essentially an in-the-baglocation. If full sulcus implantation is used,then an appropriate change in the IOL powerwill have to be made to compensate for themore anterior location of the IOL within the

THE ART AND THE SCIENCE OF CATARACT SURGERY
262
eye. When vitreous loss occurs, a meticulousvitrectomy with clearing of all vitreous strandsmust be performed.
Iris trauma must be avoided because thepupil size and shape may affect the visualfunction of a multifocal IOL postoperatively.If the pupil measures less than 2.5 mm impair-ment of near visual acuity may ensue owing tothe location of the lens rings serving near visualacuity (Figs. 130, 131).
For patients with small postoperativepupil diameters affecting near vision, a mydri-atic pupilloplasty may be tried successfullyusing the Argon laser.
COMPLICATIONS WITHPOSTERIOR CAPSULE
RUPTURE
Maintaining the integrity of the posteriorcapsule is a must because the incidence ofretinal complications is higher when there isposterior capsular disruption. We specificallyrefer to cystoid macular edema and retinaldetachment.
The disruption of the posterior capsulemay occur at any stage of the operation, at thebeginning, in the mid stage upon removingthe nucleus and in the late stage when aspirat-ing the cortex. Adequate management canprovide satisfactory vision.
A tear in the posterior capsule is mostfrequent for surgeons who are beginning inthe process of transition or who are doingtheir first cases. It mostly occurs whenfinishing the nucleus and epinucleus removaland during the phase of aspiration of theresidual cortex. The tear is usually located at12 o’clock or nearby.
Higher Risks for PosteriorCapsule Tear
Carlos Nicoli, M.D., points out thatposterior capsular tears have an incidence ofapproximately 3%. This is the maximumacceptable. There is a much lower incidencewith surgeons of considerable experience.Above 3%, we must investigate what we aredoing wrong.
Nicoli emphasizes that there are alsosituations which we should detect at the timeof preoperative evaluation because they favora high risk of posterior capsule tear. Themost important are: 1) patients with historyof trauma who may have zonular dialysis;2) patients with pseudoexfoliation; 3) hardcataracts with large nuclei; 4) patients withlarger axial length; 5) posterior subcapsularcataracts have an inherent weakness of theposterior capsule. In the latter group, onemust be very careful not to performhydrodissection and delamination techniquesbecause they might stimulate the formationof a capsule tear not perceived by the sur-geon.
Capsule Rupture Early
When it occurs early, at the beginningof nucleus phacoemulsification, it does somore frequently with soft nuclei. The sur-geon miscalculates his maneuvers, is verystressed, applies too much phaco power or adisproportional vacuum all of which lead tofast aspiration and emulsification of part orthe whole nucleus, epinucleus and cortex.The posterior capsule comes along with allthese structures.
Another cause for capsule rupture early

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
263
is that the surgeon has sculpted deeply in asoft nucleus. By and large, tears occur in thecentral region and in a circular or oval shape(Fig. 151). In order to manage this complica-tion, Centurion advises to stop everything,do a so-called "dry vitrectomy" in which noinfusion is used or a limited vitrectomy withvery low flow system. It is also essential touse small amounts of viscoelastic under thenucleus fragments to push the vitreous andlens fragments away from the posterior cap-sule tear (Fig. 151). Nevertheless, if vitre-ous is already prolapsed, this must be solvedfirst. The experienced surgeon may thenproceed with phacoemulsification decreasingsignificantly the phaco power, or convert toan extracapsular (Fig. 144). If this complica-tion happens during the transition, the wisestdecision is to convert.
Capsule Rupture During MoreAdvanced Stages of Nucleus Removal
When using the «divide and conquer»or the chopping techniques, if there is acapsular tear during phacoemulsification ofone of the nucleus quadrants, the tear inthe posterior capsule may or may not beperceived by the surgeon. If thephacoemulsifier’s efficiency is reduced to theextent that aspiration no longer occurs, wemust always be suspicious that we have a tearin the posterior capsule and vitreous blockingthe port. In these cases, Centurion againrecommends to stop, inject viscoelastic, byall means identify the site and the size of thetear, perform anterior vitrectomy, inject vis-
Figure 151: Complications with Posterior CapsuleRupture
A disruption of the posterior capsule (H) isthe most severe intraoperative complication. If noimmediate action is taken, luxation of nucleus mate-rial (N) to the vitreous and retina may occur. Ifvitreous prolapse is present and it mixes with nucleusfragments, the vitreous should be addressed first. Tosolve this complication the surgeon must stop themaneuvers of nucleus removal. Proceed immediatelyto inject viscoelastic (V) under the nucleus fragmentsto push the vitreous and lens fragments away from theposterior capsule tear. In this figure, only a "trickle"of viscoelastic (V) is seen between the tear and thenucleus fragments. The rest of the viscoelastic isunderneath the nucleus attempting to push it awayfrom the tear. At this time it is indicated to performa well controlled anterior "dry vitrectomy" in whichno infusion is used or one with a very low flowsystem. If abundant nuclear material still remainsafter these measures are taken, the surgeon maychoose between converting to ECCE or very care-fully continuing with phacoemulsification decreas-ing significantly the phaco power. It depends on thesurgeon's experience.

THE ART AND THE SCIENCE OF CATARACT SURGERY
264
coelastic again, and proceed to luxation of theremaining parts of the nucleus into the ante-rior chamber with a bimanual maneuver (Fig.152). If the tear is fairly large and notsufficient posterior capsular support remains,an IOL may be placed in the sulcus if theanterior capsule is intact.
In case the surgeon does not feel safeenough to proceed with phacoemulsification,he can always convert to extracapsular aslong as the incision has been made in thelimbus and not in the cornea. He may alsoenlarge the limbal incision to remove the restof the nuclear pieces (Fig. 144).
In the presence of a large tear of theposterior capsule, it may be unrealistic andrisky to implant an IOL completely withinthe bag. As a matter of fact, some of the morefrequent cases of tears result in partial ab-sence of the upper half of the capsular bag. Insuch cases, after infusion of viscoelastic andvitrectomy and being sure that the anteriorcapsule is intact, you may implant a PMMAIOL by securing the superior haptic in thesulcus by a single suture as shown in Fig. 153and utilizing the remaining inferior part ofthe capsular bag as a support for the inferiorhaptics (Fig. 153). Some surgeons prefer toimplant both loops symmetrically in the sul-cus in such cases.
Nuclear Fragments DislocatedInto Vitreous
A non perceived or inadvertent majortear of the posterior capsule or of the zonulewhen beginning to manage the nucleus or halfway through the nucleus removal may leadto having pieces of nucleus or the entirenucleus fall into the vitreous. The mostimportant measure is to identify the loca-tion of the rupture and discontinue ultra-
sound energy. Then immediately proceed toclean the anterior chamber from all nucleusfragments present. If the nucleus or frac-tions of it are free or connected to capsularresidues and present in the anterior third ofthe vitreous chamber, viscoelastic may beplaced behind them for support and an ante-rior vitrectomy performed using a vitrectomyinstrument plus viscoelastic, trying to pull thenucleus into the anterior chamber and thenfinish the phacoemulsification. On the otherhand, if the nucleus is in a deeper locationwithin the vitreous cavity (Fig. 155), it isstrongly advised to perform only an anteriorvitrectomy for removal of the fragmentspresent in the anterior third of the vitreouscavity, remove the cortex and implant anintraocular lens as shown in Figs. 152, 153,156. Refer the patient to a posterior seg-ment surgeon. Do not attempt to remove anucleus which has fallen into the vitreousyourself unless you have experience withvitreoretinal surgery. The surgeon must seewhat he does and certainly doing attempts «inthe dark» may lead to very severe and irre-versible vitreoretinal lesions that definitelyjeopardize the outcome.
Capsule Rupture During CortexRemoval
Rupture of the posterior capsule whileremoving the cortex is frequently at 12o’clock and may be due to the use of veryhigh aspiration parameters, usually 400 to500 mm Hg (Figs. 71 and 128).
If the capsule is ruptured during theaspiration of cortex and vitreous enters theanterior chamber, the first step is to perform a"dry anterior vitrectomy" or an anterior vit-rectomy with very low flow system andproceed to implant the intraocular lens which

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
265
Figure 152 (left): Posterior Capsule Rupture- Surgeon Luxates a Lens Fragment intoAnterior Chamber
In the presence of a large posteriorcapsule rupture, an anterior vitrectomy is per-formed. Viscoelastic is infused in the anteriorchamber. One alternative is for the lens frag-ments (F) to be moved or luxated by the surgeonto the anterior chamber with a bimanual maneu-ver. An IOL (I) is placed in the sulcus to shieldthe defect. Safe phacoemulsification (P) maycontinue with very low ultrasound energy. Thesurgeon may decide not to continue with thephaco technique and convert to ECCE.
Figure 153 (right): Lens Placement overLarge Capsular Disruption.
A large capsular disruption hasoccurred resulting in partial absence ofthe upper half of the capsular bag. Onealternative is for the surgeon to implantthe IOL (L) with one haptic in the sulcus(S) above, and the other haptic withinthe remaining part of the capsular bag(C). The haptic in the sulcus above issecured by a single suture.

THE ART AND THE SCIENCE OF CATARACT SURGERY
266
may serve as a shield protecting the posteriorcapsule defect (Fig. 154). Aspirating the cor-tical residues at 12 o’clock is technicallydifficult (Fig. 128), but may be more difficultif there has been an incompletehydrodissection or a small capsulorhexis(Fig. 145). In Fig. 154, you may see that thesurgeon is aspirating the cortical residuesafter a posterior capsule rupture with an IOLplaced to protect the posterior capsule defectas a shield so that aspiration can continue.Then the cortical residues at the 12 o’clockposition are aspirated with a curved cannula.
In order to prevent posterior capsulerupture during the stage of cortex I/A, it isessential not to be aggressive in attempting toremove all the remaining cortex and not to dothe "vacuum cleaning" process. This is riskyand does not constitute the main source ofposterior capsule opacification postopera-tively.
Pars Plana Vitrectomy forDislocated Nucleus
Significant Factors Related toOutcome
Lihteh Wu, M.D., after reviewing theworld literature, reports that immediate parsplana vitrectomy offers no visual advantageover delayed vitrectomy. As a matter of fact,sometimes it is necessary to wait for theintraocular pressure to be controlled and forthe corneal edema to resolve. Borne,Tasman et al in a classic paper published in"Ophthalmology" in June 1996 in a retrospec-tive review of 121 eyes that underwent parsplana vitrectomy for removal of retained lensfragments as a result of phacoemulsification
Figure 154: Aspiration of Cortical Resi-due after Posterior Capsule Rupture.
The IOL (L) is placed to shield theposterior capsule defect (D) so that verylow flow aspiration can continue. Corticalresidues (R) at the 12:00 position are beingaspirated with a curved cannula (C).

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
267
referred to the Wills Eye Hospital concludedthat the timing of vitrectomy does not have astatistically significant impact on visual out-come. Neither the type of intraocular lens northe timing of lens implantation significantlyaltered the final visual acuity. Most eyes withretained lens fragments do well after vitrec-tomy, with the majority recovering good vi-
sion (Fig. 155). However, the risk of retinaldetachment (RD) is increased, and visualoutcome may be adversely affected if RDoccurs.
The Wills Eye Hospital team also em-phasized that during cataract surgery, the sur-geon must avoid aspirating (without cutting)any presenting vitreous gel. Attempts to
Figure 155: Complications of Posterior Capsule Rupture - Luxation of the NucleusInto the Vitreous Cavity
When the nucleus (C) or fragments are dislocated into the vitreous cavity (V), a parsplana vitrectomy is usually indicated for the extraction of lens nuclear fragments to avoidfuture complications. The surgical technique consists of a pars plana vitrectomy with threeports. The endoiluminator (E), the vitrectomy probe or the ultrasonic fragmentation probe(F) are inserted through pars plana sclerotomies. The infusion cannula (I) is inserted througha third sclerotomy to obtain a stable intraocular pressure during the procedure.Perfluorocarbon liquids (P) are sometimes used in the vitreous cavity to raise the nucleus forextraction.

THE ART AND THE SCIENCE OF CATARACT SURGERY
268
retrieve any lens fragments that have startedto dislocate posteriorly should be made onlywith vitrectomy handpieces. The use of lensloops, forceps, and other instruments thathave the potential to engage and pull onvitreous gel should not be used. A completelimbal vitrectomy should be performed be-fore any lens placement and the absence ofvitreous to the wound or other anterior struc-
tures should be confirmed at the time ofwound closure. Last, indirect ophthalmos-copy with scleral depression should be per-formed at the end of the procedure or by aretinal specialist to identify any retinal tearsbecause these will require at least laser orcryo retinopexy.
Figure 156 represents an IOL fixated tothe sulcus after vitrectomy.
Figure 156: Complications from Posterior Capsule Rupture - Implantation of theIntraocular Lens
The intraocular lens may be implanted depending on the situation: 1) In thecapsular bag if sufficient posterior capsule remains to serve as partial support, as long asthe anterior capsule is intact. This is shown in Figs. 152, 153, 154. 2) The secondalternative is to fixate the IOL in the sulcus or even sutured (S) to the sclera (IOL). In thisfigure, the IOL is shown sutured to the sclera at the level of the ciliary sulcus on both sides,following vitrectomy. After the vitrectomy is completed, it is recommended to keep theinfusion cannula (I) in place during the fixation of the intraocular lens and remove it at theend of the entire procedure. This will reassure a stable intraocular pressure during thesemaneuvers. IOL implantation at the time of vitrectomy is another alternative when the IOLwas not implanted after anterior vitrectomy and the anterior segment surgeon decided it wasbetter to do it later. The IOL is sutured to the sclera at the level of the ciliary sulcus, asshown in "S".

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
269
POSTOPERATIVE COMPLICATIONS
and related complications typical of the tran-sition period from extracapsular to pha-coemulsification. If vitreous loss occurs, theincidence of clinically significant CME in-creases up to 8%.
CME remains a significant cause ofunexpected poor visual acuity after un-eventful, uncomplicated cataract surgery.
Pathogenesis
Characteristically, fluorescein angiog-raphy demonstrates leakage from theparafoveal retinal capillaries and from opticnerve capillaries. If the patient is examinedright after fluorescein angiography, dye leak-age into the aqueous humor can be easilyseen; consequently, there is evidence of ageneralized increased ocular vascular perme-ability. Histopathological studies have dem-onstrated expansion of the extracellular spacein the outer plexiform layer of the fovea(Henle fibers), giving rise to cystoid spaces(Fig. 175 A). There may be also some degreeof subretinal fluid.
The pathogenesis of aphakic andpseudophakic CME is not known. Inflam-mation of the iris is considered an importantfactor in the pathogenesis; the irritated irisreleases a number of inflammatory mediatorsthat may be involved in CME. Inflammatorymediators, such as prostaglandins, diffuse
Despite the technological advancesthat have made cataract surgery an operationwith such a high rate of success, postopera-tive complications still occur although lessfrequently. For didactic purposes, we havedivided them into medical and surgical com-plications.
MEDICAL
Cystoid Macular Edema
Incidence
Professor Juan Verdaguer, M.D., fromChile points out that the incidence of thiscomplication has decreased due to improvedsurgical techniques and better management ofcomplications.
Although the incidence of angiographicCME has been estimated in about 20% inpseudophakic patients, clinically significantmacular edema with reduced visual acuityoccurs approximately in 1% of cases under-going uncomplicated extracapsular cataractsurgery.
CME is more common following com-plicated extracapsular and phacoemulsifi-cation procedures, particularly if the poste-rior capsule was ruptured, with vitreous lossand implantation of an anterior chamber lens

THE ART AND THE SCIENCE OF CATARACT SURGERY
270
into the vitreous cavity and into the retina,causing the disruption of the blood-retinalbarrier at the macular and optic nerve capil-laries.
Chronic iris irritation by entrapment ofiris to the wound with a peaked pupil, vitre-ous adherence to the wound with iris traction,anterior chamber intraocular lenses and irisclip lenses may trigger the release of theseinflammatory mediators.
Clinical Findings
The patient may complain of blurredvision four to six weeks after surgery, ormuch later in the postoperative period. In apatient who has undergone uncomplicatedcataract surgery, the surgeon will be sur-prised by an unexpected and uncorrectablereduced visual acuity, in the range of 20/30 -20/60. Most patients will have a white eyeand only a few will show some mild form ofanterior segment irritation. A few patientsmay show some vitreous inflammatory cells.
Clinically, CME may be easily over-looked, unless the macular area is carefullyexamined at the slit lamp with a Goldmancontact lens or similar. The macula appearsthickened, with intraretinal cystoid spaces, ina honeycomb pattern; the foveal reflex is lost(Figs. 157 A, B, C). A few patients showevidence of epiretinal membrane formation,with cellophane-like reflexes.
Fluorescein angiography is diagnostic.Early phases demonstrate a very slow leakagefrom the parafoveal retinal capillaries. In thelater frames, the dye fills the cystoid spaces;
the hyperfluorescent spaces are separated bya dark hypofluorescent stellate figure. Theangiographists should be aware of the prob-ably diagnosis to avoid missing the laterframes that will show this characteristic peta-loid or floral pattern (Fig. 157 B).
Late leakage of optic nerve capillariesis also demonstrable in the late frames; how-ever optic nerve swelling is usually not no-ticeable ophthalmoscopically.
Fluorescein angiography may be theonly means of making the diagnosis of CMEif the media is hazy.
Clinical Course
Most patients will experience sponta-neous recovery of visual acuity and resolutionof CME during the first year after surgery(Fig. 158). Patients with persistent CMEafter 6 months may develop permanentloss of vision ("chronic CME"). Thesepatients may develop a lamellar macular holeor pigment epithelial changes.
Treatment
Verdaguer clarifies that current thera-peutic intervention for prophylaxis and treat-ment of CME are based on blocking theinflammatory mediators that may be in-volved in CME, mainly the prostaglandins.
Prostaglandins are synthesized fromarachidonic acid released from cell mem-branes by phospholipase A 2. Cyclo-oxyge-nase converts arachidonic acid to cyclic inter-mediates and then to prostaglandins.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
271
Figure 157: Cystoid Macular Edema after Complicated Cataract Surgery withRupture of the Posterior Capsule and Anterior Chamber IOL
(A) Cystoid spaces at the macula and soft exudate inferonasal to the macula.(B) Late filling of cystoid spaces with fluorescein, in a petalloid pattern. Leakagefrom optic nerve capillaries. (C) Late frame of fluorescein angiography after 6months of topical treatment (sodium diclofenac + prednisolone acetate 1%) showsmarked improvement. (Courtesy of Prof. Juan Verdaguer, M.D.)

THE ART AND THE SCIENCE OF CATARACT SURGERY
272
Corticosteroids prevent the release ofarachidonic acid from cell membranes, byblocking phospholipase A 2. Non steroidalantiinflammatory drugs are cyclo-oxygenaseinhibitors, blocking the synthesis of prostag-landins.
Prophylactic Treatment
A randomized clinical trial by Flach etal demonstrated that cyclo-oxygenase inhibi-tors (COI) alone used prophylactically re-duced the incidence of CME after cataractsurgery. Ketorolac tromethamine 0.5% oph-thalmic solution was administrated threetimes daily beginning one day before surgeryand continued for 19 days postoperatively.Given the relatively low incidence of CME inuncomplicated cataract surgery, prophylactictreatment is seldom used.
Treatment of Chronic CME
Pooled data from randomized clinicaltrials indicate a treatment benefit in terms ofimproving final visual acuity by two or morelines. These studies report the efficacy of acombination of corticosteroid and cyclo-oxygenase inhibitors (COI, or NSAID's). Inall but one trial, COI was tested alone withgood results. Since there might be a synergis-tic effect, the following approach is sug-gested:1. Topical corticosteroids, prednisone ac-etate 1% four times daily + topical COI(diclofenac sodium 0.1% or flurbiprofen so-dium 0.03% or ketorolac tromethamine 0.5%)four times daily. The treatment is maintainedat least for two months, with careful monitor-ing of the intraocular pressure. If the patienthas a steroid pressure response, treatment
Figure 158: Cystoid Macular Edema after Uncomplicated ExtracapsularCataract Surgery
(A) Four months after surgery, visual acuity 20/100. (B) Three yearsafter surgery, visual acuity 20/25. Spontaneous improvement. (Courtesy ofProf. Juan Verdaguer, M.D.)

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
273
should be limited to topical COI. In case offavorable response, the regime is tapered veryslowly. If there is no response at two months,the following interventions could be consid-ered, without discontinuing the initial treat-ment.
2. Periocular steroid injections limitedto a maximum of three.
3. Carbonic anhidrase inhibitors maywork in a few patients but may be poorlytolerated.
4. Surgery should be considered only inpatients with surgical complications that havemodified the anatomy of the anterior segmentand only if a well conducted pharmacologicaltherapeutic trial has failed.
In patients with vitreous incarcerationin the wound, Nd:YAG vitreolysis may betried, but is difficult. An anterior vitrectomy,with repair of vitreous adhesion to the woundor iris may be the procedure of choice in thesecases. More extensive surgery may be re-quired if there is significant lens malposition.
Diabetes and Cystoid MacularEdema
Verdaguer is an authority on diabeticretinopathy. He emphasizes once again thatpatients with preexisting diabetic macularedema are at substantial risk for worsening ofthe macular edema following cataract sur-gery. Moreover, diabetics are probably moresusceptible to pseudophakic CME. The twoconditions, diabetic macular edema and post-surgical CME may, in fact, coexist in a givendiabetic patient. Patients with lipidic exu-dates, retinal hemorrhages, perifovealmicroaneurysms, diffuse or focal leakage atangiography will have a predominantly dia-betic macular edema. Patients without thesecharacteristics, a petaloid pattern of leakage
at the macula, and disc leakage, will have apredominantly postsurgical CME.
Treatment Recommendations
1. Optimize medical treatment.(metabolic control, arterial hypertension,dislipidemia, anemia).
2. Use topical steroids and COI, totreat the presumed pseudophakic CME.
3. Laser photocoagulation, focal orgrid, if there are leaking microaneurysms ordiffuse leakage, with lipid exudation and reti-nal hemorrhages.
PHOTIC MACULOPATHY
The intense illumination system ofmodern operating microscopes may inducephotochemical retinal injury. The first casesof phytotoxicity after uneventful cataract sur-gery were described by McDonald and Irvine(1983).
Photochemical vs PhotothermalDamage
Verdaguer clarifies that photochemicalinjury is different from photothermal damage(photocoagulation). Photocoagulation occursafter brief and intense light exposure; photo-chemical injuries develops after prolongedexposure at intensity too low to induce photo-coagulation. Photocoagulation induces animmediate visible reaction; photochemicaldamage is not immediately recognizable.
In photochemical injuries, light activa-tion of cell molecules generates oxygen sin-glets (free oxygen radicals). These are verytoxic and induce oxidation and damage of cellcomponents.

THE ART AND THE SCIENCE OF CATARACT SURGERY
274
Shorter wavelengths carry most energy(UV and blue visible light) and are morelikely to produce photochemical damage.
Incidence
Juan Verdaguer points out that theincidence of photoretinal injuries during ext-racapsular cataract surgery has been esti-mated at 7 to 28% in different series. Photicretinal injury did not develop after pha-coemulsification in one series, with carefullimiting of coaxial exposure time and micro-scope irradiance.
Risk Factors
The main risk factors associated withphotochemical damage are duration of theexposure (longer surgery time) and intensityof the operating microscope illumination.
Longer surgery times have been associ-ated with increased incidence of retinal pho-tochemical injuries. However, the complica-tion has occurred in short, uneventful proce-dures. Therefore, the skilled, rapid, experi-enced surgeon, should not disregard the dan-gers of photoxicity.
Clinical Findings
The patient may complain of a scotomathat may be central or paracentral, in corre-spondence to the retinal injury location. Afew patients may give a history of postopera-tive erithropsia. In other cases the maincomplaint may be unexpected poor visualacuity, if the injury is near the fovea.
Visible changes at the retina will beapparent 24 to 48 hours following exposure.In the early postoperative period the lesionappears a subtle creamy deep, pale oval le-sion, usually just below or above or temporal
to the center of the fovea. If the eye isinfraducted by a superior rectus suture, thelesion will be located below the macula.
Fluorescein angiography will show in-tense staining of the oval plaque. Cicatricialchanges are apparent within the first week,with pigmentary mottling and athropicchanges of the pigment epithelium within asharply demarcated oval area. The lesionshows a highly characteristic leopard-skinappearance.
The scotoma fades rapidly and thevisual acuity may improve, unless the lesionis large and involves the macula. Fluoresceinangiography will reveal changes restricted tothe oval scar, with window defects andblocked fluorescence corresponding to theareas of hyperpigmentation (Fig. 159).
Preventive Measures
The illuminating light should not bebrighter than necessary and the corneashould be covered whenever the surgeon isnot working intraocularly. A finger blockingthe light may suffice.
Indirect illumination, instead of co-axial illumination should be used duringclosure of surgical wound in extracapsularprocedures, since the risk is maximal follow-ing implantation of the lens, with the lightclearlu focused directly on the retina.
Tilting the microscope toward the sur-geon and infraduction of the globe maydisplace the light below the fovea.
Small incision phacoemulsificationtechnique is less likely to induce light toxic-ity, since the instruments remain in the visualaxis most of the time and operating times arereduced in the hands of experienced sur-geons. There is no treatment for thiscomplication.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
275
Photosensitizing agents, such ashidroxchloroquine,phenotiazines, allopurinal,etc., should be discontinued before surgery,since they may potentiate photic damage tothe retina.
AMINOGLYCOSIDETOXICITY
Aminoglycosides have been widelyused in the prophylaxis and treatment ofocular infections. Macular infarction is asevere complication that has been mainlyassociated with the administration of gen-tamicin, but has also been reported after useof amikacin and tobramycin.
Juan Verdaguer emphasizes thataminoglycoside toxicity may be related to:
1) Intravitreal injections in endoph-thalmitis treatment regimes. Toxicity mayfollow administration of gentamicin at rec-ommended doses. Verdaguer has seen thiscomplication after intravitreal injection of0.15 mg of gentamicin, a dose previouslyconsidered safe.
Treatment of post surgical endoph-thalmitis should include the intravitreous in-jection of an antibiotic which acts effectivelyagainst gram-positive organisms (vancomy-cin) and one that is effective against gramnegatives, since gram-negative endoph-thalmitis is much more common. Given thevery narrow safe therapeutic window ofaminoglycosides, a good choice would be acephalosporin such as ceftazidime. If thesurgeon is confronted with an acute postsurgi-
Figure 159: Photic Maculopathy after Extracapsular CataractSurgery - Cicatricial Stage
(A) Pigmentary mottling and cicatricial changes within anoval scar. (B) Typical leopard-skin appearance at angiography.(Courtesy of Prof. Juan Verdaguer, M.D.)

THE ART AND THE SCIENCE OF CATARACT SURGERY
276
cal endophthalmitis and ceftazidime is notavailable, an aminoglycoside should be in-cluded in the intravitreous injection, at thelowest effective dose (100 mg of gentamicinor 400 mg of amikacin). Even at these doses,toxicity cannot be ruled out.
2) Prophylactic intravitreous injec-tions in severe trauma cases. Verdaguerhas seen this complication after a prophylac-tic intravitreous tobramycin injection.Aminoglycosides should not be usedintravitreally for prophylactic purposes.Endophthalmitis is a treatable disease andaminoglycoside toxicity is not.(Campochiaro et at).
3) Following uncomplicated subcon-junctival injection after routine cataract sur-gery. Although this has been reported in theliterature, Verdaguer has never seen a case.The complication is believed to be associatedwith leakage of the antibiotic into the eyethrough the cataract wound (with or withoutsutures). The tunnelled, non-sutured wounds,create a one way valve, allowing subconjunc-tival antibiotics and access into the anteriorchamber. Subconjunctival antibiotic injec-tions, if used, should be placed in the quad-rant opposite to the wound.
4) Dilution errors in intravitreal injec-tions.
5) Inadvertent intraocular injection dueto confusion with miochol or other sub-stances. If the mistake is discovered dur-ing surgery, profuse anterior segment lavageshould be done, immediately. Immediatevitrectomy has also been recommended.
Clinical Findings
Vision is profoundly affected the dayfollowing surgery or the intravitreal injection.Usually, the retinal infarction affects the
macular area. (Intravitreal aminoglycosidestend to settle on the posterior pole in thesupine position). Examination reveals milkywhite opacification of the retina, a cherry redspot and a few blot retinal hemorrhages. Theappearance is similar to that seen in centralretinal artery occlusion, but limited to theposterior pole. It also differs from branchretinal arterial occlusion, since the infarctioninvolves the retina both above and below themacula. Fluorescein angiography revealssharply demarcated central area of occlusionof the retinal vessels and some perivascularleakage (Fig. 160).
Figure 160: Aminoglycoside Toxicity 2 Months afterIntravitreous Injection of Gentamicin
Vascular occlusion involving the temporal ves-sels (Macular infarction). (Courtesy of Prof. JuanVerdaguer, M.D.)

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
277
The condition is untreatable and irre-versible. Optic atrophy and atrophic andpigmentary retinal changes develop later.
POSTERIOR CAPSULEOPACIFICATION
Overview
Okihiro Nishi, M.D., is a renownedauthority on this subject because of his exten-sive research and revealing findings. Nishihas emphasized that posterior capsule opaci-fication (PCO) is the most frequent postop-erative complication associated with de-creased vision in cataract surgery. Itoccurswith an incidence of up to 50% within 5 yearsafter surgery.
Various mechanical, pharmaceuticaland immunologic techniques have been ap-plied in attempts to prevent PCO by removingor killing residual lens epithelial cells(LECs), but none has been confirmed to besatisfactorily practical, effective and safe forroutine clinical practice. Nishi emphasizesthat the most effective approach to reduce ordelay the incidence of PCO is by inhibitingthe migration of LECs and not by killing thecells.
Main Causes of PCO
Recent clinical, pathological and ex-perimental studies have emphasized that PCOis usually secondary to a proliferation andmigration of residual lens epithelial cells.(LECs).
How LECs Invade the PosteriorCapsule
Nishi has pointed out that residualLECs proliferate at the pre-equatorial germi-native zone and migrate posteriorly onto theposterior capsule postoperatively. In addi-tion, when the anterior capsule comes intocontact with the posterior capsule, the LECsunderneath the anterior capsule also mi-grate onto the posterior capsule abun-dantly, before the two capsules adhere andgrow together. The apposition of the anteriorcapsule and the posterior capsule can inducefibrotic PCO.
Role of IOL in PCO
When the IOL is in the capsular bagthe optic can separate both capsules, andinterferes with the LEC migration from theanterior capsular edge onto the posterior cap-sule. The inhibition of migrating LECs andthe separation of the capsules by the IOLoptic are the main reasons why the incidenceof PCO is significantly lower in eyes withan IOL than in those without one.
Specific Features of the AcrySofand PCO
Nishi points out that the AcrySof IOLreportedly has a significant low incidence ofPCO. His recent studies indicate that thiseffect may be due to the sharp and rectangularedge design of the AcrySof IOL. His histo-pathologic findings of the lens capsule con-

THE ART AND THE SCIENCE OF CATARACT SURGERY
278
taining an AcrySof IOL in rabbits disclosethat the lens capsule wrapped the IOL sofirmly that it conformed faithfully to therectangular sharp optic edge of the IOLand that migrating LECs were apparentlyinhibited at this capsular bend or anglecreated by the sharp edge and posteriorcapsule by contact. The creation of such abend or angle in the posterior capsule re-quires a well-centered CCC, smaller thanthe IOL optic, so that the CCC edge is inapposition to the optic.
On the other hand, the role of this lensmay be dependent not only on the rectangularedge design but also on the features of theIOL acrylic material, such as adhesiveness.The AcrySof IOL has triple the adhesivenessto a collagen film compared to a PMMA IOL.The adhesiveness may also help to facilitatethe creation of the bend. Moreover, theacrylic material itself may have effects on theinhibition of migrating LECs. This adhesive-ness property of the acrylic lens, which wedescribed as "tackiness" in Chapter 9 under"Advantages and Properties of AcrylicLenses" merits further investigation. This"tackiness" or adhesiveness seems to play arole in the positive effects of the AcrySoflens. If so, then this might be a factor ofparticular importance for the use of acryliclenses and designs of future IOL's.
From the analysis provided here, it isclear that the preventive effect on PCO of anAcrySof IOL may be both design and mate-rial dependent.
Role of Continuous CurvilinearCapsulorhexis in PCO
Nishi emphasizes that continuous cur-vilinear capsulorhexis (CCC) can contributeto reduce PCO because it facilitates the im-plantation of an IOL symmetrically in thecapsular bag maintaining it there withoutdecentration. It is extremely important tocreate a well-centered CCC of the correct sizefor the prevention of migrating LECs. TheCCC edge should be smaller than the IOLoptic and cover its margin (Fig. 145). Adecentered, oversized CCC or incompleteCCC with a radial tear (Fig. 146) may resultin the apposition of both capsules. Eventhough the defective area lies in a very lim-ited circumference, the LECs migrate fromthe edge of the anterior capsule onto theposterior capsule, causing PCO.
Main Factors that Reduce PCO
Nishi clarifies that there are three keyfactors that play an important role in reducingthe incidence of PCO: 1) the design of theIOL, which results in the creation of a sharpbend in the capsule. The discontinuous,rectangular bend or angle in the posteriorcapsule interferes with the proliferation ofLECs. 2) The material of the IOL, whichpoints to the benefits of some acrylic becauseof its adhesive properties andbiocompatibility (less fibrosis). 3) The surgi-cal technique which emphasizes a perfectly

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
279
centered CCC of smaller size than the IOLoptic.
In addition, Nishi strongly recom-mends a NSAID for 3 months postopera-tively, in order to reduce postoperative in-flammation with conversion of mononuclearcells into fibroblasts, and possibly prolifera-tion of residual LECs.
Visual Loss from PCO -Differential Diagnosis
It is often a rather difficult clinicaljudgment to determine if the capsule opacityis in fact responsible for the patient`s de-creased vision. The principal misdiagnosis isto believe that the capsule is responsible forthe problem when, in fact, the patient hasdeveloped a cystoid macular edema whichmay be difficult to detect because of theposterior capsular opacity. When in doubt, apre-capsulotomy fluorescein angiography isappropriate to determine if macular edema ispresent.
PERFORMING THE POSTERIORCAPSULOTOMY
Size of Capsulotomy
Some prestigious anterior segment sur-geons have advocated not dilating the pupilfor performing a YAG posterior capsulotomy.Many patients' pupillary openings are notlocated in the exact anatomical center of theiris. Once the pupil is dilated, it can bedifficult to identify where the true pupillaryopening was located.
Nevertheless, there are importantcontraindications to making a small capsulo-tomy. The most important are: 1) Difficultiesin the evaluation of the retinal fundus. 2) Thecenter of the capsulotomy may be clear fol-lowing treatment but the rest of the capsuleremains opaque, and sometimes with a crys-talloid appearance. Patients with maculardegeneration, for example, may see betterwhen the capsulotomy is wide enough toprevent contrast reducing haze from the re-sidual hazy peripheral capsule. In those casesit is better to dilate the pupil 4-5 mm preop-eratively in order perform a more effectivetreatment.
Dodick generally makes a capsuleopening the size of a normal pupil, 3-4 mm atthe most.
Posterior Capsulotomy LaserProcedure
Timing
Alice McPherson, M.D., was one ofthe first retina specialists to demonstrate thatretinal detachment could be precipitated byearly YAG laser posterior capsulotomy. Shehas advised waiting approximately 4-6months after cataract surgery to perform aYAG laser posterior capsulotomy. The priordictum to wait one year, was done to be sureall inflammation was finished, in order toavoid cystoid macular edema.
McPherson has pointed out that once acapsulotomy is performed, the pseudophakiceye is actually like an aphakic eye. Keepingthe patient`s posterior lens capsule in place as

THE ART AND THE SCIENCE OF CATARACT SURGERY
280
long as possible can reduce the tendency forvitreous traction on the periphery. After theYAG capsulotomy is done, any predisposingfactor can increase the potential for a retinaldetachment or cystoid macular edema.
Technique
Use the lowest level energy pulse thatwill open the capsule, usually 1 mJ. An
adequate opening can be made with 10 laserapplications or less, depending on howtaught the capsule is. A cruciate pattern isrecommended, starting in the periphery at 12o'clock, working down across the center ofthe capsule toward 6 o'clock, and completethe cross from 3 to 9 o'clock (Fig. 161). Thecapsule will usually retract further after com-pleting the capsulotomy.
Figure 161: Nd:YAG Laser Cruciate Pattern in Posterior Capsulotomy
For laser posterior capsulotomy, leave the pupil undilated becausemany pupils are not in the exact anatomical center of the iris. Leaving thepupil undilated allows the surgeon to open the capsule in exactly the correctlocation. Use a cruciate pattern as shown here to avoid pits in the center of theintraocular lens.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
281
Complications Following Nd:YAGPosterior Capsulotomy
Intraocular Pressure Elevation
The most common complication is atransient pressure elevation. This must beanticipated and treated prophylactically. Themost effective method is to instill one drop ofbrinzolamide or dorzolamide 30 minutes be-fore and one drop following the laser proce-dure. Patients at higher risk of developingtransient elevation of the intraocular pressureare those that have anterior chamber intraocu-lar lenses and patients with pre-existing glau-coma.
Retinal Detachment
A higher percentage of pseudophakicdetachments occurs in cases with a history offellow eye detachment, preexisting retinaldisease such as lattice degeneration and reti-nal holes, or in eyes with axial lengths above25 mm. Retinal detachments associated withNd:YAG laser posterior capsulotomy occurmost often within the first 6 months followingcapsulotomy.
Cystoid Macular Edema
It is not well-known yet whetherNd:YAG laser capsulotomy can induce theformation of cystoid macular edema (CME)in a quiet eye. Anterior segment inflamma-tion can occur after laser capsulotomy, andinflammation has been identified as an etio-logic factor for CME especially if laser treat-ment has been more intensive than the param-eters already established. In addition, pro-lapse of vitreous anteriorly through the capsu-
lotomy or a disruption of the anterior hyaloidmight produce posterior retinal traction, an-other possible cause for CME. Thus, a poten-tial relationship does exist. In suspiciouscases only a fluorescein angiogram after thetreatment may provide the answer.
POSTOPERATIVEASTIGMATISM INCATARACT PATIENTS
With present advances in small incisioncataract surgery, particularly with clear cor-neal incisions, postoperative astigmatism fol-lowing phacoemulsification should be mini-mal. A well trained surgeon creates an astig-matically neutral incision to prevent an in-duced astigmatism.
If astigmatism is present preoperatively,the surgeon addresses the problem at thetime of cataract surgery. By placing thecorneal incision in the indicated axis, preex-isting astigmatism and cataract surgery areperformed simultaneously. This latter subjectwhich we term "Refractive Cataract Surgery"is addressed at the beginning of Chapter 12(Cataract Surgery in Complex Cases).
MANAGEMENT
Astigmatism, either preexisting thatwas not fully corrected or induced may bemanaged after cataract surgery either withincisional refractive surgery (astigmatic kera-totomy) or with excimer laser (LASIK orPRK).
How to Proceed
Wait a minimum of three months fol-lowing surgery in order to deal with a stable

THE ART AND THE SCIENCE OF CATARACT SURGERY
282
astigmatism and do the adequate evaluation.The patient is examined with refraction,keratometry and corneal topography.
Techniques
The surgeon may perform either anexcimer laser procedures (Fig. 162 A-B) or anastigmatic keratotomy (AK) (Fig. 162-C) inorder to either enhance the effects of thecataract incision on any remaining astigma-tism or correct an astigmatism induced duringthe cataract operation, which is usually re-lated to large incision, planned extracapsular.
How These Techniques Work
LASIK or PRK may either flatten thesteep meridian or steepen the flat meridian.On the other hand, AK incisions work byflattening the steep axis. Tough not as accu-rate as when treating spherical corrections,myopic astigmatism treatment has been in-creasingly successful, on the order of 80% ofintended correction.
Procedure of Choice
Most surgeons prefer using astigmatickeratotomy (AK) because: 1) it is highlyeffective; 2) costs are much lower thanexcimer laser procedures.
If the astigmatism is larger than 1.5 Dagainst the rule, paired with-the-rule inci-sions are done because they can augment theastigmatism-reducing effect (Fig. 162-C)
Oshika et al in Japan reported a pro-spective evaluation of predictability and ef-fectiveness of arcuate keratotomy treatingcorneal astigmatism after cataract surgery in
Figure 162: Correcting Astigmatism Following CataractSurgery
Figures 162 A and B show the use of excimer laser inpostoperative astigmatism. The actual surgical procedure forastigmatism, either LASIK or PRK, is the same as forspherical ametropias. In LASIK, when treating simple orcompound myopic astigmatism, the excimer beam (L) alsoflattens the steep axis. Figure C shows the additional relaxingincisions that can be used in the postoperative period withastigmatic keratotomy (AK). The AK technique is the sameas described for congenital or idiopathic astigmatism, al-though not as predictable.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
283
104 eyes. They concluded that astigmatickeratotomy in pseudophakic eyes is less pre-dictable than that in eyes with idiopathicastigmatism, but the procedure is sufficientlyeffective in reducing the residual astigmatismafter cataract surgery. Individual nomogramsare necessary for astigmatic keratotomy ineyes with naturally occurring and postsurgi-cal astigmatism. In figure 164 we presentRichard Lindstrom's nomograms.
Key Factors in the Effects ofAstigmatic Keratotomy
These are related to the diameter of theoptical zone utilized (Fig. 163), and thelength and depth of the incisions. In correct-ing postoperative astigmatism a common
choice is a 7 mm optical zone to avoidvisual aberrations with a smaller opticalzone. The effect of these arcuate relaxingincisions is titrated by the length of the inci-sions (Fig. 164).
Highlights of AK Procedure
Anesthetize the eye with the topicalanesthetic of your choice. The center of thepupil is marked with the tip of a .12 mmforceps which has been painted with Gentianviolet. A 7 mm (or the diameter selected)optical zone marker (Fig. 163) is centeredover the pupil and pressed down. The axis ofthe steepest meridian is identified with twomarks, 180º apart, over the 7 mm opticalzone previously marked.
Figure 163: Marking the Central OpticalZone in Astigmatic Keratotomy
Following the marking of the visualaxis (V), and steep meridian, the optical zone,which will remain free of any incisions, isdelineated with this optical clear zone marker.The size of the optical zone (T) is determinedby the data specific to each patient's requiredcorrection (Nomogran in Fig. 164).

THE ART AND THE SCIENCE OF CATARACT SURGERY
284
Make one or two arcuate incisions(Fig. 162-C) in the 7 mm zone according tothe nomogram (Fig. 164). The wound isinspected and irrigated.
EXPLANTATION OFFOLDABLE IOL'S
RETAINING THE BENEFIT OFTHE SMALL INCISION
The problem arises once a flexibleIOL has been implanted and there is needto remove it. How can we proceed toexplant the IOL while retaining the benefitsof small incision cataract surgery? Jack
Dodick, M.D., and Susan Batlan, M.D.,recently developed a technique to solve thissituation.
The Most Common Indicationsfor Explantation
The most common indications for ex-plantation are dislocation or improper fixa-tion, chronic inflammation, anisometropia,improperly oriented haptics, a defective in-traocular lens, and haptic breakage.
Flexible intraocular lenses, which arebeing used with increasing frequency withsmall incision cataract surgery, are introducedinto the eye through a 3.0 to 3.4 mm wound.Explantation without enlarging the wound is
Find patient age group, then move right to find a result closest to refractive cylinder.To calculate the size of the transverse incision (when indicated) as compared to theamount of degrees of the Arcuate Keratotomies outlined above, you may use the
following equivalents:
30º arc= 2.0 mm 45º arc= 2.5 mm 60º arc= 3.0 mm 90º arc= 3.5 mm

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
285
certainly desirable in order to retain the ben-efit of the small incision.
Problems Presented byTraditional Techniques
Explantation has usually been a delicateproblem to handle. The techniques suggestedfor this purpose have been technically diffi-cult and risk compromising the corneal endot-helium and posterior lens capsule.
Most procedures for intraocular lensexplantation have included enlarging thewound and extruding the unfolded intraocularlens in one piece or bisecting the intraocularlens under viscoelastic with Vannas scissorsbefore removal through the wound. The needto enlarge the wound, however, defeats the
purpose of small incision cataract surgerybecause the original wound needs to be en-larged from 5.0 to 6.0 mm to facilitate in-traocular lens removal.
Description of New Technique
Because the average central anteriorchamber depth is usually 3.0 mm it is difficultto invert the intraocular lens to properly reori-ent the haptics. Further, removal of theintraocular lens in one piece is not possiblewithout enlarging the wound size, even if it isa flexible IOL.
Dodick and Batlan first deepen theanterior chamber and expand the lens capsulewith a superior quality viscoelastic. Theythen incise the IOL optic along its radius withGills' capsulotomy scissors (Fig. 165). This
Figure 165: Explantation of FoldableIOL While Maintaining a Small Incision -Stage 1
The small incision size can be main-tained in cases where it is necessary to re-move a foldable intraocular lens. First, theanterior chamber is deepened with viscoelas-tic. Gills capsulotomy scissors (S) are usedto partially incise the intraocular lens optic(L), along its radius. This radial incisionextends from the periphery of the optic to thecenter of the optic, as shown by the positionof the scissors in the illustration. The half-bisected optic will then hinge at the centerwhen explanted (see Fig. 166).

THE ART AND THE SCIENCE OF CATARACT SURGERY
286
maneuver allows the lens to be folded in half,and creates a lens with no part greater than3 mm in width. The superior haptic is thengrasped with Kelman-McPherson forceps andthe intraocular lens, with the optic folded inhalf, is gently pulled through the incision.The elastic properties of the flexible IOLenable the surgeon to deform the optic andremove the intraocular lens in one piece(Fig. 166)
By utilizing this technique for explanta-tion of a foldable IOL following small inci-sion cataract surgery, the surgeon does notcompromise the integrity of the originalwound, posterior lens capsule, or cornealendothelium.
RETINAL DETACHMENT
Risk Factors
Cataract extraction is a well-knownrisk factor for the development of arhegmatogenous retinal detachment (RRD).Anywhere from 20% to 40% of RRD occur ineyes that have undergone cataract surgery(Fig. 167).
Incidence
The incidence of RRD followingECCE and PCIOL implantation has beenreported to be between 0.25% and 1.7%. Theincidence of retinal detachment is less inpatients with uncomplicated phacoemulsifi-cation because this procedure is performedthrough a self-sealing, watertight small inci-sion with improved safety during the proce-dure. It is also significantly less invasive.
The rate of RD associated withphacoemulsification greatly increases in the
presence of rupture of the posterior capsuleparticularly when lens fragments are mixedwith the vitreous. What to do and what not todo is addressed in this same chapter underIntraoperative Complications of Pha-coemulsification - Posterior Capsule Rup-ture. This is an uncommon complication butit does occur in the initial stages of thelearning curve during the transition fromECCE to phacoemulsification.
Clinical Course of RD
Patients typically complain of photopsias,floaters, scotomas and blurry vision. Previousreports have emphasized the poorer outcomeof surgery for RRD in pseudophakic eyes ascompared to phakic eyes. These authors expe-rience is that peripheral capsular opacifica-tion, lenticular remnants and the optical ef-fects induced by the rim of the IOL impairvisualization of the small peripheral retinalbreaks by indirect ophthalmoscopy, therebyinterfering with the vitreoretinal surgeon'sbest performance.
In the present practice of clinical oph-thalmology, repair of retinal detachment isroutinely referred by the cataract surgeon to avitreoretinal surgeon.
POSTOPERATIVEENDOPHTHALMITIS
By definition, endophthalmitis refersto the presence of an inflammatory reaction inboth the anterior and posterior segments ofthe eye. Its etiology may be infectious ornoninfectious. The infectious nature of en-dophthalmitis is one of major concern toophthalmic surgeons. Fortunately, it has be-come a highly infrequent complication.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
287
Figure 166 (left): Explantation of Foldable IOLWhile Maintaining a Small Incision - Stage 2
The superior haptic (H) is then grasped withKelman-McPherson forceps (F) and the incised IOLis gently pulled through (arrow) the small 3.2 mmincision. The greatest width of the half-incised 6.0mm optic is now 3.0 mm and therefore will fitthrough the maintained small incision.
Figure 167 (right): Difference Between Phakicand Pseudophakic Detachments
Classic pseudophakic retinal detachmentsdiffer from phakic retinal detachments in twomajor ways. Retinal detachments (R) with anintraocular lens (L) following cataract surgery areusually associated with more anteriorly locatedmultiple breaks (M) along the posterior marginof the vitreous base (dotted line). Also withpseudophakos, these types of breaks tend to be inmultiple quadrants. On the other hand, phakicdetachments often tend to involve a single quad-rant with one tear. The second major differencebetween phakic and pseudophakic detachments isin the reduced ability of the surgeon to see theperipheral retina in the case of pseudophakos (notshown).

THE ART AND THE SCIENCE OF CATARACT SURGERY
288
The causes of infectious endoph-thalmitis include bacterial and fungal organ-isms. Depending on its time course, endoph-thalmitis may be further classified as acute orchronic. The speed with which the patientdevelops symptoms is directly proportional tothe virulence of the organism.
Relative Virulence of Organ-isms
Highly virulent organisms that arecommonly isolated include Staphylococcusaureus, Streptococci and Gram negativerods. Staphylococcus epidermidis is a littleless virulent and happens to be the mostcommon organism isolated. Propionibacte-rium acnes and fungi present in a moreindolent manner. Noninfectious causes in-clude retained lens fragments. According toProfessor Juan Verdaguer, the most com-mon endophthalmitis is the one produced bygram-negative organisms.
Clinical Findings and Sourceof Infection
In acute cases, the patient often com-plains of progressive worsening of vision,redness, ocular discharge and increasing ocu-lar pain. Examination often reveals eyelidedema, chemosis, corneal edema, intense celland flare, iris hyperemia, vitritis and hy-popyon. Visual loss is often secondary to therelease of toxins and the inflammatory reac-tion. The main sources of infection are thenormal bacterial flora in the lids and conjunc-tiva. Scrubbing the lids with povidone 5%just prior to surgery is an effective way ofreducing the bacterial load.
Management and VisualOutcome
The management of acute postopera-tive bacterial endophthalmitis has been influ-enced by the results of the EndophthalmitisVitrectomy Study. This study provides es-sential information for the understanding ofhow to proceed in the care of patients withthis potentially devastating complication. Itsguidelines are as follows: 1) A vitreousspecimen needs to be obtained for cultureand sensitivity as soon as possible (Fig. 168).2) Intravitreal amikacin (0.4 mg / 0.1 mL)and vancomycin (1.0 mg / 0.1 mL) mustbe injected after the specimen is obtained(Fig. 168). 3) If the initial visual acuity washands motion or better, study results suggestthat the visual outcome is the same whetheror not immediate pars plana vitrectomy isdone. 4) Vitrectomy is indicated in thoseeyes with initial visual acuity of light percep-tion or worse. Systemic antibiotics did notaffect the visual outcome of patients in thestudy. 5) The visual outcome was better inthose eyes with better visual acuity at presen-tation, underscoring the need for early di-agnosis.
In the cases where fungal or P. acnesendophthalmitis is suspected, a vitrectomy isusually indicated with the injection ofintravitreal antibiotics or antifungals.
INTRAOCULAR LENSDISLOCATION
Posterior dislocation of an IOL is anuncommon complication of cataract surgery.Its frequency appears to have increased in the

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
289
past few years as more surgeons enter into theinevitable steep learning curve of phacoemul-sification in which posterior capsule rupturesmay occur. The great emphasis given to theTransition into Phaco in Chapter 7 of thisVolume is precisely oriented toward facilitat-ing a successful and comfortable approach tothis procedure.
Symptomatology
The patient with intraocular lens dislocationoften complains of sudden loss of vision dueto the uncorrected aphakia. If complicationssuch as retinal detachment, cystoid macularedema or vitreous hemorrhage occur, the pa-tient may also complain of loss of vision. Ifthe IOL is mobile in the vitreous cavity, itmay be observed by the patient as a huge
floater. Posterior capsular rupture or zonulardialysis are usually present. The IOL may befreely mobile in the vitreous cavity, may befixed to the retina, or may be seen hangingwith one haptic attached to the posteriorcapsule, iris or ciliary body.
Management
Observation can be recommended if theIOL is not mobile and there are no retinalcomplications, but this would defeat the pur-poses of the operation. We can not expect thepatient to be satisfied with aphakic spectaclecorrection or contact lenses.
Several surgical options are available.These include removal, exchange or reposi-tioning of the IOL. Repositioning of the IOLinto the ciliary sulcus or over posterior capsu-
Figure 168: Technique of Vitreous Tapin Diagnosis and Intravitreal Adminis-tration of Antibiotics
A Ziegler knife (or equivalent) isinserted 3 mm posterior to the limbus tocreate a tract into the vitreous. The knifeis directed toward the mid-vitreous cav-ity. The knife is removed and a 22 gaugeneedle attached to a small syringe isinserted through the tract made by theknife. A vitreous specimen is obtainedfor culture and sensitivity studies. An-other syringe is attached to the needle andamikacin (0.4 mg / 0.1 mL) and vanco-mycin (1.0 mg / 0.1 mL) are injectedintravitreally immediately after the vitre-ous specimen is obtained.

THE ART AND THE SCIENCE OF CATARACT SURGERY
290
lar remnants with less than a total of 6 clockhours of inferior capsular support is not astable situation. Many of those repositionedIOLs will end up dislocating again.Transcleral suturing (Fig. 156) or IOL ex-change (removal of the dislocated IOL andplacement of a flexible open loop anteriorchamber IOL) is recommended in these cases.Current models of AC IOLs often do notresult in the same types of complications asolder models. Instead of risking anotherposterior dislocation of an IOL, these lensesshould be considered if adequate capsularsupport is lacking. The Kelman type ofanterior chamber lens has been a good optionfor years. The Nu-Vita aphakic IOL may besoon available. (The Nu-Vita phakic anteriorchamber IOL's have highly acceptable resultsin phakic patients). If the IOL is fixed inposition, out of the way, some surgeons leaveit alone and implant a second IOL.
The Role of Silicone Plate IOL's
Silicone plate lenses deserve specialattention because progressive contracture ofthe anterior capsulorhexis opening (“pursestring”) may occur more commonly whenthey are used. This increases the tension onthe IOL and causes it to bow posteriorly.Dehiscence anywhere in the capsular bagallows release of tension through expulsion ofthe implant. The anterior segment surgeonshould be advised to avoid implantation of aflexible silicone plate IOL if there is a breakin the posterior capsule, a radial notch or atear in the anterior capsular rim or zonulardialysis. Small capsulorhexis openingsshould be avoided in these cases.
BIBLIOGRAPHY
Bartz-Schmidt KU, Kirchhof B, Heimann K: Pri-mary vitrectomy for pseudophakic retinal detach-ment. Br. J Ophthalmol, 1996;80:346-349.
Borne, MJ., Tasman W., Regillo, C., Malecha, M.,Sarin, Lou: Outcomes of vitrectomy for retainedlens fragments. Ophthalmology, 1996;103:971-976.
Centurion V, Lacava AC, Sanchez JC, OliveiraMode, EA: IOL explantation. Faco Total by VirgilioCenturion.
Chan KC: An improved technique for managementof dislocated posterior chamber implants. Oph-thalmology, 1992 Jan; 99(1):51-57.
Endoophthalmitis Vitrectomy Study Group. Re-sults of the Endophthalmitis Vitrectomy StudyGroup. A randomized trial of immediate vitrec-tomy and of intravenous antibiotics for the treat-ment of post-operative bacterial endophthalmitis.Arch Ophthalmol 1995; 113:1479-1496.
Fastenberg DM, Schwartz PL, Shakin JL, GolupBM: Management of dislocated nuclear fragmentsafter phacoemulsification. Am J Ophthalmol 1991;112:535-539.
Gass JDM, Norton EWD: Cystoid macular edemaand papilledema following cataract extraction: afluorescein funduscopic and angiographic study.Arch Ophthalmol 1996; 79:646-661.
Gonzalez GA, Irvine AR: Posterior dislocation ofplate haptic silicone lenses [letter]. Arch Ophthalmol1996 Jun; 114(6):775-776.
Hayashi K, Yahashi H, Nakao F, Hayashi F: Re-duction in the area of the anterior capsule openingafter polymethilmethacrylate, silicone, and softacrylic intraocular lens implantation. Am JOphthalmol 1997; 123:441-7.

C h a p t e r 11: Complications of Phacoemulsification - Intraoperative and Postoperative
291
Joo CK, Shin JA, Kim JH: Capsular opening con-traction after continuous curvilinear capsulorhexisand intraocular lens implantation. J Cataract Re-fract Surg 1996 Jun; 22(5):585-590.
Learning DV: Practice styles and preferences ofASCRS members - 1994 survey. J Cataract Re-fract Surg 1995; 21:378-385.
Mittra RA, Connor TB, Han DP, et al: Removal ofdislocated intraocular lenses using pars plana vit-rectomy with placement of an open-loop, flesibleanterior chamber lens. Ophthalmology 1998;105(6):1011-1014.
Nishi, O: Prevention of posterior capsule opacifi-cation after cataract surgery: theoretical and prac-tical solutions. Atlas of Cataract Surgery, Editedby Masket S. & Crandall AS, published by MartinDunitz Ltd., 1999, 24:205-212.
Nishi, O: Removal of lens epithelial cells by ultra-sound in endocapsular cataract surgery. OphthalmicSurg. 1987; 18:577-80.
Nishi O, Nishi K, Fujiwara T, Shirasawa E: Effectsof diclofenac sodium and indomethacin on prolif-eration and collagen synthesis of lens epithelialcells in vitro. J Cataract Refract Surg 1995;21:461-5.
Oshika T, Shimazaki J, Yoshitomi F, Oki K, SakabeI, Matsuda S, Shiwa T, Fukuyama M, Hara Y:Arcuate keratotomy to treat corneal astigmatismafter cataract surgery: a prospective evaluation ofpredictability and effectiveness. Ophthalmology,1998; 105:2012-2016.
Powe NR, Schein OD, Gieser SC, et al: Synthesisof the literature on visual acuity and complicationsfollowing cataract extraction with intraocular lensinsertion. The Cataract Patient Outcome ResearchTeam. Arch Ophthalmol. 1994; 112:239-252.
Ravalico G, Tognetto D, Palomba MA, Busatto P,Baccara F: Capsulorhexis size and posterior cap-sule opoacification. J Cataract Refract Surg. 1996;22:98-103.
Schneiderman TE, Johnson MW, Smiddy WE, etal: Surgical management of posteriorly dislocatedsilicone plate haptic intraocular lenses. Am JOphthalmol 1997 May; 123(5):629-635.
Smiddy WE: Modification of scleral suture fixa-tion technique for dislocated posterior chamberintraocular lens implants [letter]. Arch Ophthalmol1998 Jul; 116(7):967.
Smiddy WE, Ibanez GV, Alfonso E, et al: Surgicalmanagement of dislocated intraocular lenses. JCataract Refract Surg 1995 Jan; 21(1):64-69.
Wilkinson CP: Pseudophakic retinal detachments.Retina 1985; 5:1-4.

THE ART AND THE SCIENCE OF CATARACT SURGERY
292

C h a p t e r 12: Cataract Surgery in Complex Cases
295
CATARACT SURGERYIN COMPLEX CASES
In previous chapters we have discussed
in depth how to evaluate the patient preop-eratively (Chapter 2), how to calculate thecorrect IOL power in standard and complexcases (Chapter 3), prevent major complica-tions such as infection (Chapter 4), and howto proceed with the operation by usingadequate, modern anesthesia and to make theoperating room efficient (Chapter 5). Whyphacoemulsification is so important (Chapter6), how to make the transition from ECCE tophacoemulsification with minimum risk tothe patient while minimizing mental andemotional trauma to the surgeon (Chapter 7),what are the best instruments and equipmentsto use in phacoemulsification (Chapter 8), areall essential experiences and information forthe modern cataract surgeon. In addition, youmay also find the state of the art phacoemul-sification techniques and facilitate yourunderstanding of each group of procedures sothat you can establish a basis for your ownselection of the procedure that will lead youto master phacoemulsification (Chapters 9and 10). Finally, a discussion of the mostimportant complications you may encounterin phacoemulsification and in plannedextracapsulars and how to manage them suc-cessfully is presented in Chapter 11.
Aims of this Chapter
Based on the tools and concepts pro-vided in Chapters 1-11, in this Chapter wecarefully consider, in depth, powerful tech-niques available today which allow the use ofphacoemulsification in the management ofcomplex, and more challenging cases.
Broadening of Indications
As emphasized by Miguel AngeloPadilha, M.D., F.B.C.S., one of Brazil’smost prestigious anterior segment surgeons,the progressive mastering of phacoemulsifi-cation (Chapter 9) by an increasing number ofsurgeons in various parts of the world allowsindications for this procedure to broaden rap-idly extending to the complex cases that werepreviously considered a contraindication tophaco. Patients with very hard cataracts,classified as “rock hard cataracts”, eyes withshallow anterior chamber, pseudoexfoliation,subluxated cataracts, cornea guttata, cornealdystrophies, corneal transparency alterations,as well as small pupils, were previously con-sidered contraindications to the use of thistechnique.

THE ART AND THE SCIENCE OF CATARACT SURGERY
296
In this chapter, we intend to provide thecataract surgeon with practical clinicalobservations, strategies and surgicaltechniques leading to safe and efficientmanagement of cataract surgery in specialsituations that we refer to as «the ComplexCases.» Although much of the focus is onphacoemulsification, many of the approachesto complex cases here presented are alsoapplicable to manual extracapsular.
Complex Cases Already Discussed inPrevious Chapters
They are: 1) Cataract surgery inpatients with diabetic retinopathy (pages21-27, Figs. 8-18). 2) In age-relatedmacular degeneration (pages 28-29, Figs.19-20). 3) In the presence of retinal breaks(pages 28-30, Fig. 21). 4) In uveitis (pages31,33, Fig. 22). 5) In adult strabismus withpartial amblyopia (page 33). 6) DeterminingIOL power in complex cases (pages 48-58,Figs. 24-32).
FOCUSING ON THEMAIN COMPLEXCASES
THE DIFFERENT TYPES OFVISCOELASTICS
Their Specific Roles
For years we have generally referred toviscoelastics (VES) as highly valuable pro-tective and space-maintaining substances.Joaquin Barraquer, M.D., referred to
viscoelastics years ago as his «third assis-tant.» Viscoelastics are very important forcataract surgery, whether in routine or com-plex cases. Their main uses are for maintain-ing the anterior chamber depth, protecting theendothelium, as aids during capsulorhexis,hydrodissection, phacoemulsification, withI/A, maintaining the capsular bag fully opena intraocular lens during insertion, unfolding,and positioning of the IOL.
They have a special place in this chap-ter because their adequate use has becomeeven more valuable and indispensable in themanagement of complex cases.
Cohesive and DispersiveViscoelastics
In the past few years, industry hasrefined viscoelastics, and made their proper-ties more specific so that we now have avail-able two main groups, each type better thanthe other for specific functions. As clarifiedby Buratto, these groups are: 1) cohesive,2) dispersive.
The Cohesive VES -Specific Properties
The better known cohesives are thosewith high viscosity, such as Healon GV,Healon, Provisc, Amvisc Plus, Amvisc, andBiolon. They are very useful in creatingspace and stabilizing the tissues, increasingmydriasis, supporting the nucleus duringcapsulorhexis, deepening the anterior cham-ber, separating synechiae, opening the capsu-lar bag and maintaining this space duringimplantation of the IOL.
The cohesive viscoelastics maintainspace really well because the molecules holdthemselves together. They are also quite easy

C h a p t e r 12: Cataract Surgery in Complex Cases
297
to remove. If you are trying to create a spacesuch as when opening the capsular bag, ordeepening the anterior chamber, then the co-hesive viscoelastics are going to work better.
The Dispersive VES-Specific Properties
The dispersive VES are those withlower viscosity and lower cohesiveness.They break up easily when injected into theeye and therefore disperse in small frag-ments. This group includes Viscoat (Alcon),Vitrax (Allergan) and the methylcelluloseproducts. These substances form a layer thatwill adhere and coat the posterior surface ofthe cornea to protect the endothelium duringphacoemulsification, or from other instru-mentation during manual ECCE. They help incapturing nuclear fragments. They are alsovaluable if the phacoemulsification tip acci-dentally catches the iris, in zonular disinser-tion and rupture of the posterior capsule.
The dispersive viscoelastics are ex-cellent coaters. If you aim to reduce thefriction between the intraocular lens optic andthe injector, so you are less likely to tear theintraocular lens, Lindstrom uses a dispersiveviscoelastic. Or, if you are operating on aneye with a dry or somewhat opaque surface,placing a few drops of the dispersive vis-coelastic on the surface clears the view sig-nificantly. If you tear the posterior capsule,but have not lost vitreous yet, if you againinject a dispersive viscoelastic, it can stay inthe eye over the tear and the capsule, to holdvitreous back and protect the capsule whileyou carefully remove the nuclear remnants ora little cortex. That can be very helpful.
But the dispersives are a little moredifficult to remove and they do not maintainspace as well. Consequently, the choice ofVES varies with the surgical requirements of
each particular case. Each surgeon must besufficiently trained to choose the most appro-priate substance for the individual patient andthe specific technique.
PHACOEMULSIFICATIONAFTER PREVIOUSREFRACTIVE SURGERY
The primary challenge in operating onpatients who have already had radial kerato-tomy (RK) or excimer laser surgery is selec-tion of the appropriate lens power. As thecorneal curvature is altered, the usual predic-tive formulas have also been altered. Stan-dard ultrasound A-scan technology and cor-neal curvature are still used to estimate theappropriate lens implant for reaching the tar-get refraction. In addition, if the fellow eyehas not had refractive surgery, that eye is alsomeasured.
We have already discussed this subjectin practical and specific terms for the clini-cian in pages 50-54 and presented the meth-ods and formulas most often used. Sincethere is no universally accepted formula tocalculate these patient’s IOL power accu-rately, we present here the method used by amaster cataract surgeon to solve this problem.
Jack Dodick, M.D., has found thefollowing procedure quite effective. He im-plants a specifically designated lens undertopical anesthesia with sutureless clear cor-neal wound. Following the operation, thepatient is taken to an autorefractor just min-utes after surgery. If there is a high ametropiapresent, the patient returns to the table, theeye is again prepped, the lens is removed andreplaced with one of the appropriate power. Inpatients with high myopia, for example, thesurgeon’s best judgment about lens implantpower can be considerably off target because

THE ART AND THE SCIENCE OF CATARACT SURGERY
298
of untoward circumstances like a staphyloma.In patients who have had RK, surgeons tendto underestimate the power of the lens im-plant.
Removing the lens does not present amajor problem. The challenge is to removethe lens without enlarging the small incisionand implant another through the same smallincision . If the original 6 mm or 5.5 mm optichas been implanted through a 3.2 mm inci-sion by folding; it is important to remove thelens without sacrificing the length of thewound. This is done quite simply by bisectingthe optic with Gills’ capsulotomy scissorsunder viscoelastic and removing the hingedtwo halves through the small incision. Thistechnique for removing the foldable lens ispresented in Figs. 165 and 166, Chapter 11.
PHACOEMULSIFICATIONIN HIGH MYOPIA
In patients with high myopia, pha-coemulsification is somewhat more challeng-ing than in other eyes. Patients with highmyopia have globes that are superelongatedand sclera that is thinned out. The minutethe phaco probe is inserted and the infusionstarts, the chamber deepens dramatically(Fig. 169). The probe must reach deep intothe eye to access the nucleus because the lensiris diaphragm may have moved considerablyback. Dodick has sought to overcome thisproblem by lowering the bottle height andreducing the flow, so that the lens is unlikelyto move to such a posterior location. Evenwhen this occurs, it is still quite possible with
Figure 169: Special Conditions of Pha-coemulsification in Patients with HighMyopia
Phacoemulsification in patientswith high myopia presents additional chal-lenges. Patients with high myopia haveglobes which are elongated (green arrows)and have thinner sclera. As the phacoemul-sification probe (P) is introduced into sucheyes, the lens (red arrow) and iris (bluearrow) move posteriorly by a considerableamount. The probe must then reach deeperinto the eye for lens extraction. Highvacuum and sectioning of the nucleus intopieces can allow the surgeon to bring thenucleus more anteriorly for easier removal.

C h a p t e r 12: Cataract Surgery in Complex Cases
299
high vacuum to bring the nucleus up into thepupillary plane earlier than with a normal oremmetropic eye. Phaco chop helps further bycutting the nucleus in several pieces andbringing these pieces up into the pupillaryplane with high vacuum.
The challenges in calculating the cor-rect IOL power in high myopia are discussedon page 50.
CHALLENGES OFPHACOEMULSIFICATIONIN HYPEROPIA
The challenge in hyperopia is some-what different. Dodick refers to these ascrowded eyes because all of the small ana-tomical structures are in a smaller, confinedspace. Positive pressure is more likely tooccur. Dodick makes two fundamental ad-justments in technique when dealing with anextremely hyperopic eye. First, he dehydratesthe vitreous with an osmotic agent such asMannitol. Secondly, he tries to compress theeye and to express some of the unboundwater in the vitreous with a compressivedevice like an Honan balloon (Fig. 96). Heleaves this Honan balloon on at about 35 to40 mm Hg for 20 to 30 minutes. These twopreparatory steps help reduce the volume ofthe eye and soften the eye prior to nucleusremoval.
The challenges in calculating the cor-rect IOL power in high hyperopia are pre-sented on page 48. The pros and cons ofpiggyback lenses in very high hyperopia arediscussed on page 49.
REFRACTIVE CATARACTSURGERY
Why and When Do RefractiveCataract Surgery
Richard Lindstrom, M.D. has be-come an advocate of what he calls «refractivecataract surgery», by which we mean tryingto improve the patient’s astigmatism at thetime of cataract surgery.
In his extensive research and clinicalexperience, about 70% of the cataract patientsthat he operates have less than one diopter ofastigmatism preoperatively and about 30%have more than one. He does not make anyastigmatic corrections in those that have lessthan one diopter. That is good enough for20/30 uncorrected visual acuity. Lindstrombecomes somewhat more aggressive withastigmatism when there are two diopters ormore before the cataract operation. His goalis to reduce it to one diopter; not to try tocorrect it all, just to get it down into areasonable range. He advises making thecombined operation for cataract and astigma-tism only when performing phacoemulsifi-cation.
As a matter of fact, he advises againstit if the phacoemulsification incision, isenlarged to place a 6.5 or 7 millimeter opticPMMA IOL or when a planned ECCE isperformed. In such cases, he recommends,doing the cataract surgery, see what you get,and then fix it later if there is a problem.Most patients adapt to glasses. This is be-

THE ART AND THE SCIENCE OF CATARACT SURGERY
300
cause with an incision of this size, it is almostimpossible to plan the refractive operation.The range of effect on astigmatism with suchincisions is significant. With a planned extra-capsular wound one patient might change adiopter and another might change four diopt-ers.
TECHNIQUE FORREFRACTIVE CATARACTSURGERY
Surgical Principles
Lindstrom’s surgical principles andtechnique are as follows:
1) Move the cataract 3 mm tunnelincision to the steeper meridian (Fig. 170).He thinks of this small wound as an astig-matic keratotomy. This will reduce thepresent astigmatism by 0.50 diopters. If thepatient has 1 diopter of plus cylinder at axis90, and a 3 mm cataract incision is made ataxis 90, he/she will end up with only a 1/2diopter of cylinder. If they have +1 diopter at180 and the 3 mm cataract/IOL incision ismoved over to the temporal side where thesteeper meridian is located, they will end upwith only +1/2 diopter of astigmatism at 180ºwhich is good enough for 20/20 vision uncor-rected. Lindstrom’s approach is to makethem better, not to correct all the astigmatism.If they have 1.5 diopters, they will end upwith 1 diopter cylinder and that is acceptable.But if they have 2 diopters to begin with, theywill end up with 1.5 diopters and that isoutside his goal. Lindstrom’s outcome goalis 1 diopter astigmatism or less.
2) If more than 1.0 diopter of astigma-tism would remain, Lindstrom applies the
principles of astigmatic keratotomy at thetime of surgery. He does this very conserva-tively. The cataract wound becomes oneastigmatic keratotomy. On the opposite side,at a 7 mm optical zone, he will make a small2 mm corneal incision to correct 1 diopter ora 3 mm long incision to correct 2 diopters ofastigmatism in the cataract age group. Thisbecomes a second astigmatic keratotomy(Fig. 170).
If the patient preoperatively has 3diopters of astigmatism, Lindstrom placesthe 3 mm cataract/IOL incision again on thesteeper meridian. This brings the astigmatismdown to 2-1/2. If he wants the patient to endup with 1/2 diopters instead of 2 1/2 dioptersof astigmatism, he makes a small 3 mm, non-perforating corneal incision with a diamondknife on the opposite side of the cataractincision at a 7 mm optical zone (Fig. 170).
Surgical Procedure
Lindstrom sets the depth of the dia-mond blade at 600 microns. In that area onthe average the cornea is about 650 micronsthick so it is a very safe setting so as not toperforate the cornea. This incision can bedone at the very beginning of the surgery.The first thing to do is make this little tinycut. The other alternative is to complete thecataract operation, firm up the eye, and makethat tiny cut at the end, but that may be moredifficult.
The exact location of this cut in thecornea is 3.5 mm from the center of thecornea. By using a 7 mm optical zone, thecut is really 3.5 mm from the center of thecornea. The diameter of the cornea is 12 mm.The limbus is 6 mm from the center.

C h a p t e r 12: Cataract Surgery in Complex Cases
301
Why Straight Cuts Instead ofArcuate
Lindstrom uses a 7 mm optical zonemarker that has little marks on it for 30, 45,60 and 90 degrees. At a 7 mm zone a 30degree arcuate cut is equivalent to a 2 mmstraight cut and a 45 degree arcuate cut isequivalent to a 3 mm straight cut (Fig. 171).Lindstrom finds that it is safer and easier
Figure 170 (above)): Technique for Refractive Cata-ract Surgery
Dr. Lindstrom places the 3 mm cataract tunnelincision (C) in the steeper meridian to reduce pre-opastigmatism when present in a cataract patient. Furtherreduction of astigmatism may be obtained with acorneal incision (A) placed opposite the cataract inci-sion in the same axis at the 7 mm optical zone(dotted line). The example shows a patient with pre-op3 diopters of plus cylinder at axis 145º (inset). Thecorneal cataract incision is placed in this axis and mayreduce the pre-op astigmatism by 0.50 diopters. The 3mm straight corneal incision placed opposite the cata-ract incision in the same axis at the 7 mm optical zoneshould reduce astigmatism further by 2.0 diopters. Thetwo together will reduce astigmatism a total of 2.5diopters.
Figure 171 (below): Length of Straight CornealIncision Related to Arcuate Incision
At the 7 mm optical zone (dotted line), a 30ºarcuate cut is equivalent to a 2 mm straight cut(A). At the 7 mm optical zone, a 45º arcuatecut is equivalent to a 3 mm straight cut (B).Dr. Lindstrom finds that it is safer and easier tomake such small incisions straight rather thanarcuate.

THE ART AND THE SCIENCE OF CATARACT SURGERY
302
just to make these small incisions straightinstead of arcuate. With this technique hetries to make things safe and better for thepatient, not perfect, and without doing anyharm. This means trying to bring a patientfrom 3.5 diopters of astigmatism down toone, in order to improve the quality of his/hervision. He finds that he can enhance theresults to the point now where about 85% to90% of the patients will have 1 diopter or lessof astigmatism.
Lindstrom finds that these tiny inci-sions programmed as outlined here are a verypowerful tool and seem to be very safe. He
has not observed any major complicationssuch as poor wound healing, infection orperforation.
Full Refractive Correction ofthe Cataract Patient
By selecting the correct IOL powereven in complex cases as outlined in pages45-54, correcting the preexisting astigmatismas discussed here and further enhancementwith the use of toric foldable IOL’s if neces-sary (see Chapter 9), we have the means tocreate in our patients the truly refractivecataract operation.
CATARACT AND GLAUCOMA
Age related cataract and primaryopen-angle glaucoma or chronic angle clo-sure glaucoma often coexist in the olderpopulation. With increasing longevity this isbecoming more prevalent. The managementof such cases has been controversial becausemedical or surgical therapy of one conditionoften affects the other.
Most of the concepts and techniquespresented in this chapter are based on theexperiences and observations of Maurice H.Luntz, M.D., Chief of the Glaucoma Serviceat the Manhattan Eye and Ear Hospital inNew York.
Overview - AlternativeApproaches
When cataract and glaucoma coexistbut the glaucoma is uncontrolled or poorlycontrolled, one approach is to give priority tocontrol of the glaucoma either with addi-tional medication or if this is not possible,
with laser trabeculoplasty or filtration sur-gery. Luntz believes that this approach hasits drawbacks. Medical therapy for glaucomamay necessitate miotics, which tend to reducevisual acuity regardless of preexisting lensopacities, and may encourage an accelerationof cataract progression. Surgical therapy ofglaucoma may be associated with increasedlens opacification, especially if the surgery iscomplicated by inadvertent lens trauma buteven in the absence of lens trauma. Subse-quent cataract extraction, even if a function-ing bleb and good drainage are obtained,results in loss of the bleb in approximately10% of eyes, and inability to restore controlof the glaucoma.
When the indications for cataract ex-traction are present but the glaucoma is con-trolled medically, the most common approachhas been to remove the cataract and continuemedical management of the glaucoma. In-traocular pressure is more easily controlled insome eyes after lens extraction but a signifi-cant number of these patients will require

C h a p t e r 12: Cataract Surgery in Complex Cases
303
glaucoma surgery as early as 3-6 months afterstandard cataract extraction . The patient thenfaces a second surgical procedure with itsattendant risks soon after the first operation.
An alternative approach is combinedcataract and glaucoma surgery. Most sur-geons are now oriented toward this approach.Excellent results are reported with extracap-sular cataract extraction and trabeculectomy(Luntz and Stein, 1988; Simmons, 1992) andphacoemulsification with trabeculectomy.The combined procedure is used in thosepatients in whom IOP runs above the upperlimit of the target IOP for that patient, or inwhom good control of IOP necessitates theuse of three or more different drugs. In thosepatients in whom IOP is well controlled usingno more than two different drugs, phacoemul-sification alone will generally maintain ad-equate postoperative control.
COMBINED CATARACTSURGERY ANDTRABECULECTOMY
In this chapter, we will first presentthe evolution of the different types of Com-bined Procedures for Cataract Extraction andTrabeculectomy as described by Luntz, toprovide you with an instant mental picture ofthe different approaches to this problem, thelatest being combining phacoemulsificationwith a tunnel incision and trabeculectomy.Considering that this Volume covers all ma-jor, widely accepted cataract surgery proce-dures, we present the advanced techniques incombined surgery for glaucoma with pha-coemulsification as well as with planned ext-racapsular. The evolution of the differenttypes of combined cataract extraction-trab-eculectomy is presented in Figs. 172, 173,
174, 175, the combined extracapsular ex-traction with trabeculectomy step by step inFigs. 176 through 181, and phacoemulsifica-tion combined with trabeculectomy step bystep in Figs. 182 through 187.
Indications
The indications based on Luntz’s ob-servations are: 1) Any eye with open angleglaucoma and cataract in which surgery isrequired for the cataract, even if the glaucomacan be medically controlled but requires morethan two medications to do so. If combinedsurgery is not done, many of these eyes willrequire glaucoma surgery at a later date,exposing the patient to two surgical proce-dures where one would have sufficed. Anexception to this are those patients in whomIOP with three medications runs in the verylow teens (10-11mm Hg).
2) Eyes with uncontrolled glaucomarequiring glaucoma surgery and significantcataract with corrected vision of 20/40 or less,reading 6-pt. print or less or with poor glaretolerance.
Evolution of the Incision forCombined Cataract Extractionand Trabeculectomy
The combined operation for cataractand glaucoma constitutes two procedures per-formed at the same surgical session. Thetechnique for each procedure remains un-changed but the surgical incision needs to bemodified using either separate incisions foreach procedure (Fig. 172) or combining theincisions for each operation into one com-pound incision (Figs. 173, 174, 175).

THE ART AND THE SCIENCE OF CATARACT SURGERY
304
A. Extracapsular CataractExtraction with Trabeculectomy
1. Separate Incisions
The cataract and trabeculectomy inci-sions are made separately at different sites.The cataract incision is made in the cornea andis a single 11 mm chord length corneal cataractincision. A 3 mm x 3 mm lamellar scleraltrabeculectomy flap is made separately in theupper nasal quadrant in the sclera under fornixor limbus based conjunctival flap (Fig. 172).This approach has the disadvantage that itnecessitates a corneal cataract wound forextracapsular surgery. This type of incision isno longer popular because of its tendencytoward higher levels of astigmatism in theearly postoperative phase before the cornealsutures are removed. This approach is a goodtechnique for those surgeons using a smallcorneal incision for phacoemulsification com-bined with trabeculectomy (Fig. 187).
2. Compound Incision
By the term «compound incision» we meanthat the surgeon combines a limbal 2-planecataract incision of 9.5 mm or 10 mm chordlength with a 3 mm x 3 mm 1/2 thicknesslamellar scleral flap for the trabeculectomy(Fig. 173). Luntz prefers to place a trab-eculectomy flap in the center of the cataractincision and this is a generally favored tech-nique (Fig. 173). When the trabeculectomyflap is placed in the center of the cataractincision and the cornea-scleral trabeculectomyblock measuring (2 mm x 2 mm) is removedfrom the scleral bed before removing thecataract, the total surface area of the cataractincision is increased at the site of maximumthickness of the lens during extraction for
intracapsular surgery or of a nuclear extrac-tion for extracapsular surgery, thus facilitat-ing their removal. This allows the use of anincision of smaller cord length - namely, 9.5mm instead of the usual 11 mm chord length(Fig. 173).
Luntz points out that a matter ofgreat importance in the architecture of thiscompound incision is that the continuity ofthe limbal scleral incision for the cataractremoval is broken in the center by the intru-sion of the trabeculectomy flap with its tworadial incisions which are placed 3 mm apart.By breaking the continuity of the limbalscleral incision (the cataract portion of theincision) we introduce an element of instabil-ity into the incision. Part of the incision isparallel to the limbus (the cataract incision)and part of the incision is radial to the limbus(the trabeculectomy incision). Where the twomeet at each side of the trabeculectomyscleral flap the incision, when stressed post-operatively (for example by squeezing of theeyelid or distortion of the globe) they canshift horizontally, vertically or obliquely,causing postoperative oblique or against therule astigmatism. The ability of the incisionto shift vertically is magnified if the cataractand trabeculectomy incisions meet at the lim-bus at a 90º angle. To minimize this effect,Luntz recommends that the cataract incisionshould be curved into the trabeculectomyincision forming a convex curve on each sideof the cataract trabeculectomy incision junc-tion (Fig. 173). This curving of the incisionreduces any tendency for vertical shift. Thiscan be enhanced by careful attention to place-ment of the interrupted sutures at the time ofsuturing the incision. Additional stability isimparted to the incision by placing the inter-rupted 10-0 nylon sutures radially in thecataract portion of the incision, and by plac-ing the sutures in the curved junction between

C h a p t e r 12: Cataract Surgery in Complex Cases
305
Figure 172 A (left): Evolution of Types ofCombined Cataract Extraction-Trabeculec-tomy Surgery - Type 1- Individual SurgicalSites - Surgeon’s View
The first method of combined cataractextraction with trabeculectomy involves twoseparate surgical sites. The cataract surgery isperformed through a corneal incision (C). Thetrabeculectomy is performed by a standard tech-nique at the limbus. Note separate 3 mm by 3mm scleral flap (F) and 2 mm by 2 mm trab-eculectomy window (W). Iridectomy (I). Lim-bus based conjunctival flap.
Figure 172 B (right): Evolution ofTypes of Combined Cataract Extrac-tion-Trabeculectomy Surgery - Type1- Individual Surgical Sites - CrossSection View
In this cross-section view, youcan instantly identify the anatomicalstructures involved in the combined pro-cedure when using two individual surgi-cal sites. Note the scleral trabeculec-tomy flap (F) separate from corneal cata-ract incision (C). Trabeculectomy win-dow (W). Iridectomy (I). Limbus basedconjunctival flap.

THE ART AND THE SCIENCE OF CATARACT SURGERY
306
the cataract and trabeculectomy portions at45º to the incision line (Fig. 173).
Although this is a relatively stablecompound incision, it is not as stable as asingle unbroken incision and will inducemore astigmatism, particularly oblique andagainst the rule astigmatism, than would beexpected with a simple, unbroken cataractincision. An unbroken incision can beachieved by making the incision for the cata-ract surgery separate from the trabeculectomy(Fig. 172) or by using a large scleral beveland combining both the trabeculectomy andthe cataract wound within the unbroken inci-sion (Figs. 174, 175).
Figure 173 A (above) : Evolution of Types ofCombined Cataract Extraction-Trabeculectomy- Type 2- Combined Incision - Surgeon’s View
A combination of the cataract extractionand trabeculectomy incisions is seen in thissurgeon’s view. Note the limbus based two-planecataract incision (C) with cord length of 9.5 mmand centrally placed 3 mm by 3 mm scleral flap (F).Note the 2 mm by 2 mm trabeculectomy window(W). The junction of the cataract incision andscleral flap is convex in shape (arrow) for a morestable wound closure. Iridectomy (I). Fornix basedconjunctival flap.
Figure 173 B (below): Evolution of Types of Com-bined Cataract Extraction-Trabeculectomy - Type 2-Combined Incision - Cross Section View
This cross section view allows prompt identifica-tion of the tissues and technique involved as explained inFig. 173 A. Compare the site of the cataract incision(limbus-based) and the combined scleral flap (F) withcataract incision in contrast with the individual surgicalsites incision shown in Fig. 172 B.

C h a p t e r 12: Cataract Surgery in Complex Cases
307
Figure 174 A (left): Evolution of Types ofCombined Extracapsular Cataract Extrac-tion-Trabeculectomy - Type 3- Single, Unbro-ken Tunnel Incision - Surgeon’s View
Development of the scleral tunnel inci-sion for phacoemulsification has simplified theincision for combined extracapsular cataract ex-traction and trabeculectomy. A 9.5 mm to 10 mmcord length, 1/2- scleral thickness groove (S) isplaced 1.5 mm posterior to the surgical limbus. Ascleral tunnel is dissected to the limbus, penetrat-ing into the anterior chamber in the center of thegroove incision and widened on each side overthe full 10 mm length of the groove using acrescent knife and corneo-scleral scissors (C)(See Fig.178). The resulting scleral flap (F) isreflected. A trabeculectomy window (W) is per-formed under this scleral flap, contained withinthe scleral bed. Iridectomy (I) shown in Fig. 174-B. Fornix based conjunctival flap.
Figure 174 B (right): Evolution of Types ofCombined Extracapsular Cataract Extraction-Trabeculectomy - Type 3- Single, UnbrokenTunnel Incision - Cross Section View
The angled view of the structures involvedin the tunnel incision shows the difference in thissurgical approach to the two previous types ofincision (Figs. 172-B and 173-B). The anatomicalstructures and technique of incision are explainedin figure legend of Fig. 174 A.

THE ART AND THE SCIENCE OF CATARACT SURGERY
308
3. Combining the cataract-trabeculectomy into a single,unbroken incision
Instead of making the cataract por-tion of the incision at the limbus, the cataractincision is moved posteriorly to a position1.5 mm or 2 mm posterior and parallel to thelimbus. This is the preferred incision forextracapsular cataract surgery with trab-eculectomy (Fig. 174).
A trabeculectomy block of 2 mmx 2 mm can be excised out of this scleral-corneal bevel (Figs. 179, 180) without thenecessity of cutting a separate trabeculectomyflap in the sclera (Fig. 173). The end result isa trabeculectomy block dissected within thescleral cataract incision which is a simple,unbroken incision (Fig. 180) adding signifi-cantly to the stability of the scleral incisionand reducing the amount of postoperativeastigmatism.
B. Phacoemulsification withTrabeculectomy
This is presently the preferred tech-nique for those with experience in pha-coemulsification surgery. It results in theleast level of postoperative astigmatism andrapid visual rehabilitation.
The most popular incision is similarto the one shown in Fig. 177 except that thepocket incision is made to a chord lengthbetween 3.1 mm and 6 mm rather than the10 mm chord length incision used for extra-capsular extraction. The chord length of thisincision will depend on the size and type ofintraocular lens used. Thus, for a foldablesilicone or acrylic IOL, a 3.5 or 4 mm chordlength will be used; whereas, for a PMMA
lens a 5.5 or 6 mm chord length incisionwould be used.
The trabeculectomy block is removedfrom the scleral bevel within the incision asdescribed previously in Figs. 179, 180. (Fordetails of the surgical technique see Pha-coemulsification Cataract Incision with Trab-eculectomy later in this chapter, Figs. 182,187.
Intraocular Lens Implants
Luntz considers that the indicationsfor implanting an intraocular lens are thesame in glaucoma patients as in non-glau-coma patients. The posterior chamber in-traocular lens is preferable. Anterior chamberlenses (Kelman-Multiflex - Editor) have beensuccessfully used where a posterior chamberlens cannot be safely used, for example,where the anterior and posterior capsule havebeen extensively torn and will not support aposterior chamber intraocular lens in the bagor in the sulcus. (This subject is discussed indetail in pages 118-123 - Editor).
Preoperative Preparation
Pilocarpine drops should be stopped24-48 hours before surgery in order to facili-tate pupillary dilatation at the time of surgery.If preoperative intraocular pressure is high itshould be reduced prior to surgery with intra-venous Mannitol (1.5 g./kg. body weight) orwith oral glycerine 75 cc. Topical steroids(Prednisolone 1% q.i.d.) and topical nonste-roidal antiinflammatory drops are given 24-hours before surgery and continued for 1 to 2weeks after surgery. This reduces postopera-tive inflammation and may diminish the inci-dence of cystoid macular edema.

C h a p t e r 12: Cataract Surgery in Complex Cases
309
Figure 175 A (right): Evolution of Types of Com-bined Cataract Extraction-Trabeculectomy - Type4 - Tunnel Incision for Phacoemulsification andTrabeculectomy
A 1/2- scleral thickness, 6 mm cord lengthgroove (S) is made 1.5 mm posterior to the limbus. Ascleral tunnel (T) (its margins denoted by dotted lines)is dissected to the limbus. The corneal incision forintroduction of the phacoemulsification probe andtrabeculectomy window (W) are located within theresulting scleral bed. Iridectomy (I). Fornix basedconjunctival flap.
Figure 175 B (left): Evolution of Types ofCombined Cataract Extraction-Trab-eculectomy - Type 4 - Tunnel Incisionfor Phacoemulsification and Trabeculec-tomy - Section View
Compare this cross section viewwith the one shown in Fig. 174 B. Thescleral tunnel flap is much smaller. Thecataract incision (C) in Fig. 174 B is muchlarger. This figure shows in cross sectionwhat is described in the surgeon’s view inFig. 175 A.

THE ART AND THE SCIENCE OF CATARACT SURGERY
310
SURGICAL TECHNIQUESSTEP BY STEP
The following is a summary of thetwo main procedures step-by-step as recom-mended by Luntz.
ECCE and TrabeculectomyWith Single, Unbroken TunnelIncision
Conjunctival - Tenon’s Flap(Fornix-based) (5x-7x Magnification)
If Mitomycin is to be used Luntzprefers to apply it to the conjunctival surfacebefore raising the conjunctival-Tenon’s flap(see section on antimetabolites further in thischapter).
A superior rectus bridal suture is op-tional. The fornix-based conjunctival-Tenon’sflap with a 12 mm cord length is raised at thesuperior limbus. The flap is dissected posteri-orly to further expose the sclera. Adequatehemostasis and clearing of the sclera is ob-tained.
Luntz considers that the fornix-basedconjunctival flap has many advantages com-pared to a limbus-based flap:
1) There is better exposure and visual-ization of the operative field.
2) The possibility of damaging theconjunctival flap during dissection, particu-larly producing a «buttonhole» is eliminated.
3) A fornix-based flap is technicallyeasier to dissect than a limbus-based flap,especially when operating in an area ofscarred conjunctiva, either from previous sur-gery or trauma. It also offers better exposureof the surgical area.
4) The fornix-based conjunctiva flapadheres and scars at the limbus. As a result,the bleb forms posteriorly producing a dif-fuse, well-vascularized «low-profile» blebwell behind the limbus. There is less possi-bility of developing a thin «high-profile»avascular anterior bleb which overhangs thecornea, which has the added risk of micro-scopic perforations of hypoxic conjunctivaand possible intraocular infection.
5) The posteriorly situated bleb andthe scar at the limbus allow safe and earlycontact lens fitting if a contact lens is re-quired.
6) Tenon’s fascia is minimally trau-matized.
Scleral-Corneal Incision(7x-10x Magnification)
A 1/2-thickness scleral groove is cutin the exposed sclera using a diamond knifeblade or a crescent knife blade 1.5 mm poste-rior to the surgical limbus, extending for 9.5to 10 mm cord length parallel to the limbus(Fig. 176). At the center point of the incision(12:00 o’clock position) a crescent knifeblade is used to dissect a scleral tunnel justanterior to the corneal vascular arcade whichis then dissected to each side across the cordlength of the incision (Fig. 176). A 3.1 mmkeratome is introduced into the «tunnel» at 12o’clock and advanced to the anterior limit ofthe tunnel in the cornea (Fig. 176). Pressingthe point of the keratome downward towardthe iris, the keratome is advanced and pen-etrates the cornea into the anterior chamberwith the tip of the keratome 45º to the irisplane (Fig. 177). At this point, the directionof the keratome tip is changed to run parallelto the iris surface and the keratome is ad-vanced fully into the anterior chamber to

C h a p t e r 12: Cataract Surgery in Complex Cases
311
complete the 3.1 mm incision (Fig. 177).The keratome is removed and the anteriorchamber filled with viscoelastic. Using aSuperblade, a paracentesis incision is made atthe 9:00 o’clock and 3:00 o’clock meridians.
Figure 176 (above): Combined ExtracapsularCataract Extraction - Trabeculectomy Proce-dure With Single, Unbroken Tunnel Incision- Steps 1 and 2
A 12 mm cord length, fornix basedconjunctival flap (C) is reflected. A 1/2 thicknessvertical scleral groove incision (S) is made witha diamond knife or crescent knife (not shown),1.5 mm posterior to the limbus for a cord lengthof 9.5 to 10 mm, parallel to the limbus. At thecenter the groove (12 o’clock position), a cres-cent knife blade (K), is used to dissect a scleraltunnel to just anterior to the corneal vasculararcade. The sclera is then dissected to each sideacross the length of the groove (arrows - dottedlines).
Figure 177 (below): Combined Extracap-sular Cataract Extraction - Trabeculec-tomy Procedure With Single, UnbrokenTunnel Incision - Step 3
A 3.1 mm keratome (K) is introducedinto the tunnel at the 12 o’clock position andadvanced to the anterior limit of the tunnel inthe cornea (inset - 1). The tip of the keratomeis depressed and advanced into the anteriorchamber. At this point, the direction of thekeratome tip is changed to run parallel to theiris surface and the keratome is fully ad-vanced into the anterior camber (inset -2 ) tocomplete the 3.1 mm incision. The keratomeis removed and the anterior chamber is filledwith viscoelastic.

THE ART AND THE SCIENCE OF CATARACT SURGERY
312
Anterior Capsulotomy(10x Magnification)
A 27-gauge needle with the tip bent to90º is introduced into the anterior chamberand a can-opener capsulotomy or preferablya large capsulorhexis, depending on thesurgeon’s preference is performed.
Completion of Sclero-CornealIncision (10x Magnification)
The scleral flap is lifted and microsurgi-cal corneal-scleral scissors are introducedinto the scleral-corneal incision cutting to theleft and right, completing the incision into theanterior chamber for the entire cord length ofthe original scleral groove (Fig. 178). Thefinal result is a 9.5 to 10 mm cord length
incision into the anterior chamber with a 1.5 -2 mm wide scleral-corneal bevel (Fig. 174).
Trabeculectomy(10x Magnification)
The anterior chamber is filled withviscoelastic . A 2 mm x 2 mm block of tissueis excised from the scleral-corneal bevel atthe 12:00 o’clock position using a Luntz-Dodick microsurgical punch (Katena). Theposterior limit of the excised scleral-cornealblock reaches to the scleral spur (Figs. 179,180).
The trabeculectomy opening located inthe center of the scleral-corneal incision re-duces resistance of the scleral bevel to pas-sage of the lens nucleus from the eye andfacilitates its removal.
Figure 178: Combined Extracapsular Cataract Ex-traction - Trabeculectomy Procedure - Step 4
After an anterior capsulotomy orcapsulorhexis has been performed, the scleral flap (F)is lifted and corneal-scleral scissors (D) are intro-duced into the previous 3.1 mm incision. The cataractincision is extended to the left and right (arrow) usingthe scissors. This produces a 9.5 to 10 mm cord lengthincision into the anterior chamber with a 2mm-widescleral-corneal bevel. The anterior chamber is thenfilled with viscoelastic.

C h a p t e r 12: Cataract Surgery in Complex Cases
313
Figure 179 (left): Combined ExtracapsularCataract Extraction - Trabeculectomy Proce-dure - Step 5
This cross section shows the scleral-cornealbevel (T). An approximately 2 by 2mm block oftissue is excised from the scleral-corneal bevel(T) at the 12 o’clock position using a KellyDescemets punch (P) or Vannas scissors. Theposterior limit of the excised block reaches tothe scleral spur (arrow).
Figure 180 (right): Combined Extracapsu-lar Cataract Extraction - TrabeculectomyProcedure - Step 6
This surgeon’s view shows the initial1/2-thickness scleral groove incision (S), thecompleted 9.5 to 10mm scleral-corneal bevelincision (C), the approximately 2mm by 2mmtrabeculectomy window (W) and reflectedscleral flap (F). (See Figure 174 B forcorresponding cross section view). The sur-geon then performs an extracapsular cataractextraction and IOL insertion using his/her pre-ferred technique. A peripheral iridectomyunder the trabeculectomy is essential.

THE ART AND THE SCIENCE OF CATARACT SURGERY
314
Removal of the Lens Nucleusand Cortex. Insertion of IOL
The surgeon proceeds with extracapsu-lar cataract extraction and insertion of an IOLusing his/her preferred technique.
Iridectomy (10x Magnification)
Following insertion of the IOL a pe-ripheral iridectomy is made within the trab-eculectomy opening ensuring that the base ofthe iridectomy is wider than the trabeculec-tomy opening (Fig. 173-A). This is achievedby grasping the iris near its root at the centerof the trabeculectomy opening, bringing it outof the eye and moving to the left, cutting
midway across the iris from the right sidewith a Vannas or DeWecker scissors, and thenmoving the iris to the right and completingthe iridectomy cut.
Closure of the Cataract-Trabeculec-tomy Incision (5x Magnification)
Closure is achieved using interrupted10-0 nylon sutures, one interrupted suture oneither side of the trabeculectomy openingleaving the trabeculectomy opening and adja-cent scleral bevel unsutured (Fig. 181). Theinterrupted sutures are placed through thefull thickness of the scleral flap at the limbusand through the posterior scleral incision(Fig. 181). The sutures are not tightly tied,
Figure 181: Combined Extracapsular CataractExtraction - Trabeculectomy Procedure - Step 7
This surgeon’s view shows closure of theincision with two interrupted 10-0 nylon suturesplaced through the full thickness of the scleral flap atthe limbus and through the posterior scleral incisionon each side of the trabeculectomy opening (dottedline). A running uninterrupted 10-0 Nylon suturecloses the conjunctival incision (not shown).

C h a p t e r 12: Cataract Surgery in Complex Cases
315
but tied to achieve tissue apposition without«crimping» the scleral flap and are «buried»in the sclera. It is desirable to inflate theanterior chamber with balanced salt solutionto achieve a good positive intraocular pres-sure before tying these sutures.
An alternative is to use one horizontalsuture through the scleral flap and scleral-corneal bevel on either side of the trabeculec-tomy opening.
Closure of the Conjunctivo-Tenons’Flap (5X Magnification)
An uninterrupted 10-0 nylon suturerunning from the limbal sclera to conjunctivacloses the conjunctival incision. These su-tures should be tightly tied, particularly if anantimetabolite is used.
Phacoemulsification WithTrabeculectomy
This procedure is shown in Figs. 182through 187.
Conjunctivo-Tenons’ Flap(5x-7x Magnification)
A 6 mm fornix-based flap is raised inthe same way as described previously for thecombined extracapsular extraction and trab-eculectomy. Luntz’ technique when usingantimetabolites is that if mitomycin is to be
used it is applied before raising the conjuncti-val flap.
Scleral-Corneal Incision (7x-10xMagnification)
Luntz performs a 1/2-thickness verticalscleral groove, 5.5 mm or 6.0 mm cordlength, depending on the diameter of the IOLto be used, or 3.5 mm cord length if a foldableIOL is used, which is cut in the exposedsclera in the superior half of the globe,1.5 mm posterior to the limbus using a cres-cent blade or diamond blade (Fig.182). Thecrescent knife then dissects under the anteriorlip of the groove to within the corneal vascu-lar arcade extending the dissection on eitherside to the limits of the incision (Fig. 182).
Using a Superblade, a paracentesis inci-sion is made at the 9:00 o’clock and 3:00o’clock meridians.
A 2.5 mm keratome is inserted into thescleral-corneal incision at the 12:00 o’clockmeridian advancing the keratome to the edgeof the incision just anterior to the cornealvascular arcade (Fig. 183). The tip of thekeratome is pushed toward the anteriorchamber, it is withdrawn slightly and theanterior chamber is penetrated with thekeratome tip 45º to the iris plane. At thispoint, the keratome tip is raised so that thekeratome advances fully into the anteriorchamber parallel to the iris plane producing a2.5 mm «tunnel» incision (Figs. 183, 177Insets).

THE ART AND THE SCIENCE OF CATARACT SURGERY
316
Figure 182 (left): Combined Phacoemulsifica-tion Cataract Extraction - Trabeculectomy Pro-cedure - Steps 1 and 2
A 6mm cord length fornix based conjuncti-val flap is reflected. A 1/2 thickness vertical scleralgroove incision is made with a diamond knife orcrescent knife (not shown) at 1.5mm posterior andparallel to the limbus for a cord length of 6mm fora 5.5 or 6.0mm diameter IOL, or 3.5mm if afoldable IOL is used (Fig. 40 B). At the center ofthe groove incision (12 o’clock position), a cres-cent knife blade (K) is used to dissect a scleraltunnel to just anterior to the corneal vascular ar-cade. The sclera is then dissected to each sideacross the length of the groove (arrows).
Figure 183 (right): Combined Phacoemulsifi-cation Cataract Extraction - TrabeculectomyProcedure - Step 3
A 2.5mm keratome (K) is introduced intothe tunnel at the 12 o’clock position and advancedto the anterior limit of the tunnel in the cornea(See Fig. 177, inset 1). The tip of the keratome isdepressed and advanced into the anterior cham-ber. At this point, the direction of the keratome tipis changed to run parallel to the iris surface andthe keratome is fully advanced into the anteriorchamber (See Fig. 177, inset 2) to complete the2.5mm incision. The keratome is removed and theanterior chamber is filled with viscoelastic. Thecataract is then removed.

C h a p t e r 12: Cataract Surgery in Complex Cases
317
Corneal «Tunnel» Incision andSeparate Trabeculectomy
(7x-10x Magnification)
For cataract and glaucoma surgery the3.0 - 3.5 mm tunnel intracorneal incisionplaced in the temporal cornea can be usedwith a trabeculectomy performed separatelyand superiorly (Fig. 187).
Capsulorhexis, Phacoemulsifi-cation, Nucleofractis, Infusion/ As-piration and IOL Insertion (10x-15xMagnification)
Using the scleral corneal tunnel inci-sion (Fig. 184), the surgeon performs theabove procedures according to his/her pre-ferred method.
Trabeculectomy is not performed priorto lens removal in order to maintain a water-tight «tunnel» incision for the phacoemulsifi-cation.
The 2.5 mm tunnel incision is enlargedto a 6 mm incision for insertion of a 6 mmIOL. If a 5 mm IOL is used, a 5 mm incisionis made; and if a foldable lens is used theincision can be reduced to 3.5 mm.
Trabeculectomy (10x-15xMagnification)
Following insertion of the IOL the ante-rior chamber is filled with viscoelastic and atrabeculectomy is made within the scleralbevel of the tunnel incision using the sametechnique as described in Figs. 175 and 179.The next step is an iridectomy insuring thatthe iridectomy base is wider than the trab-eculectomy opening, as previously described(Fig. 184).
Figure 184: Combined PhacoemulsificationCataract Extraction - Trabeculectomy Proce-dure - Step 4
This figure shows the final configuration of thecombined Phacoemulsification Cataract Extrac-tion - Trabeculectomy incision. (See Figure 175B for the corresponding cross section view).The scleral-corneal incision has been extendedfor its full length. In this figure, a cord length of6mm is illustrated. The IOL is then inserted.Trabeculectomy (W) is performed by removingan approximately 2mm by 2mm block of thescleral-corneal bevel down to the scleral spur(see Figure 179). Iridectomy is performed (I).The sclera is shown lifted here to reveal thescleral tunnel (T) (its margins denoted by dottedlines). Initial scleral groove incision (S).

THE ART AND THE SCIENCE OF CATARACT SURGERY
318
Closure of the Incision(5x Magnification)
An interrupted 10-0 nylon suture isplaced through the scleral incision on eitherside of the trabeculectomy as described inFig. 185. The trabeculectomy and adjoiningscleral-corneal bevel is left open without su-tures. The knots should be buried. Thescleral flap can also be left unsutured butLuntz has found a high incidence of postop-erative bleeding and hyphema in these eyes.The 3.5mm incision or the 6 mm scleral flapare left unsutured only if the surgeon antici-pates that freer drainage of aqueous throughthe trabeculectomy opening will be requiredearly in the postoperative period. However,the disadvantage of an unsutured scleral flap,particularly the 6 mm scleral flap, is that theanterior chamber may be shallow or flat in theimmediate postoperative period. To overcomethis problem, one or two releasable 10-0nylon sutures should be used (Figs. 186 A-B).These have the advantage that the anteriorchamber is very unlikely to shallow postop-eratively, because the scleral incision is par-tially sutured, and, at the same time, thesutures can be easily removed in the postop-erative period if and when more drainagethrough the filtering procedure is required.The releasable sutures are placed as follows:the 10-0 nylon suture (Luntz prefers a CU-5needle) is loaded backwards in the needleholder. The suture is placed through theposterior lip of the scleral incision and thenthrough the anterior lip of the incision (poste-rior lip of the trabeculectomy flap) and exteri-orized through the anterior lip. A second biteis taken at the limbus and into adjacent corneain a radial direction and is exteriorized. Athird bite is then taken at the point where thesuture exits from the cornea, and this bite in
the cornea is horizontal to the limbus(Fig. 186). The free end of this nylon sutureentering into the posterior lip of the scleralincision is held with tying forceps. Threethrows are made, and the tying forceps thenengages the portion of the suture that isexteriorized between the anterior lip of thescleral incision and the limbus. This portionof the suture is then pulled through the threeloops held in the other tying forceps, and abow knot is tightened, apposing the two lipsof the scleral incision. The free end of thenylon suture from the bow tie is cut, and thefree end of the nylon suture on the cornea iscut. The radial and horizontal suture in thecornea eliminates a free end of nylon sutureon the cornea behaving as a windshield wiper.Two such releasable nylon sutures are placedin the incision at the same locations as shownfor the interrupted sutures in Fig. 185. (Theabove technique is the method described byAllan E. Kolker, M.D.).
Conjunctival Closure(5x Magnification)
The conjunctiva is closed with anuninterrupted 10-0 nylon suture as previouslydescribed.
(Editor’s Note: in patients with glau-coma and cataract, one of the most difficultproblems to deal with is the management ofthe small pupil. This important subject isdiscussed separately in this same chapter.)
Antimetabolites in CombinedProcedures
Luntz believes that antimetabolitesshould be used routinely in combined cataractand trabeculectomy as the result is better.

C h a p t e r 12: Cataract Surgery in Complex Cases
319
Figure 185 (left): Combined Phacoemulsifi-cation Cataract Extraction - TrabeculectomyProcedure - Step 5
This surgeon’s view shows closure ofthe 6mm incision with two interrupted 10-0nylon sutures placed through the full thicknessof the scleral flap at the limbus and through theposterior scleral incision on each side of thetrabeculectomy opening (dotted line). If prop-erly valvulated to prevent loss of the anteriorchamber, the 6mm scleral flap can be leftunsutured, which will result in a bigger drop inintraocular pressure. A running uninterrupted10-0 Nylon suture closes the conjunctival inci-sion (not shown).
Figure 186 A-B (right): Technique forPlacement of Releasable Sutures
(A) The 10-0 nylon suture ispassed through both lips of the scleral flap,through the limbus radially into the corneaand then through the cornea parallel to thelimbus (to prevent the “windshield wiper”effect of a radial suture. Figure (B) showsthe technique for tying the bow. Theportion of suture between the anterior lipof the scleral flap and the limbus is pulledup into a bow and tied to the free end of thesuture at the posterior lip of the scleralflap. (This technique was introduced byAlan Kolker, M.D., and is reproducedwith his permission).

THE ART AND THE SCIENCE OF CATARACT SURGERY
320
Choice of Antimetabolite
Surgeons in general will vary in theirchoice of an appropriate antimetabolite de-pending on the age of the patient and theirown personal experience. For the combinedcataract and trabeculectomy procedure, Luntzuses mitomycin-C routinely, as the results ofthe procedures are better with the use of anantimetabolite. There is a remote possibilityof teratogenesis and the development of can-cer many years following application of thisdrug. For this reason, and particularly so inchildren, an informed consent is requiredbefore Mitomycin-C is applied.
When using Mitomycin, Luntz’ pre-ferred technique is to soak a Weck cell spongeinto a solution of 0.4% Mitomycin-C. Thesoaked Weck cell sponge is placed on theconjunctival surface at the site selected forsurgery. It is held on the conjunctiva for one-minute and then replaced with a freshlysoaked Weck cell sponge for a further one-minute, and this is repeated a third or fourthtime giving a total application time of three orfour minutes. Following this, the conjuncti-val surface is vigorously lavaged with bal-anced salt solution to remove all traces of thedrug.
Some surgeons have used a topicalapplication of 5-FU intraoperatively with aWeck cell sponge soaked in the drug,similar to the way Mitomycin-C is used.The effectiveness of this method is stillundecided.
Results of Combined CataractSurgery and Trabeculectomy
In Luntz’ experience, the results ofcombined cataract surgery and trabeculec-tomy have been consistently good. In a studycombining extracapsular cataract extractionwith posterior chamber intraocular lens im-plant and trabeculectomy, 38 eyes were fol-lowed for up to 46 months, with a mean of16.4 months. The average preoperative in-traocular pressure was 20.5 mm Hg and theaverage postoperative pressure was 14.5 mmHg, a statistically significant change. Themean number of medications preoperativelywas 2.3 and postoperatively at the end of thefollow-up period this had still dropped to amean of 1.42.
There was no significant change in thevisual field graded from the preoperative tothe postoperative level. Visual acuity,which averaged 20/120 preoperatively,improved to an average of 20/50postoperatively.
Simmons et al (1992), have also re-ported good results with few complicationsusing extracapsular cataract extraction withposterior chamber intraocular lens and trab-eculectomy (as well as phacoemulsificationand trabeculectomy -Editor).
In Luntz’ studies, the complicationsassociated with combined ECCE and trab-eculectomy (and (phacoemulsification andtrabeculectomy) were surprisingly few and ofno greater severity than would have been

C h a p t e r 12: Cataract Surgery in Complex Cases
321
expected from the cataract surgery or theglaucoma surgery alone. Intraoperative com-plications specific to the combined operationwere not observed. The complications thatwere seen were similar to those associatedwith a trabeculectomy or extracapsular cata-ract extraction alone.
Immediate postoperative problemsconsisted of corneal edema of mild degreewhich rapidly resolved, and iritis whichcaused no long-term problems. Contrary towhat was anticipated, the performance of aradial iridectomy and its repair by suturingthe iris when this procedure was chosen bythe surgeon did not cause an increase in the
level of postoperative iritis. None of thepatients had shallow or flat anterior chamberspostoperatively, which can be attributed togood apposition and closure of the cataractwound.
When using antimetabolites, if a sig-nificant leak from the conjunctival wounddoes occur this will in most cases requiresurgical repair. Surgical repair entails re-suturing the incision. In severely affectedeyes, the conjunctiva at the site of the leakbecomes friable and normal conjunctiva isrotated from the fornix or moved across as aflap from the adjacent temporal or nasalconjunctiva.
Figure 187 : An Alternative Technique of Pha-coemulsification Using “Tunnel” IntracornealIncision Combined with Separate Trabeculec-tomy
In cases of combined phako and glaucomasurgery, a 3.0 - 3.5mm “tunnel” intracornealincision (C) is placed in the temporal cornea toperform the phacoemulsification and foldable lensimplantation. Trabeculectomy is performed in thestandard manner separately and superiorly with3mm by 3mm scleral flap (F) and 2mm by 2mmtrabeculectomy window (W).

THE ART AND THE SCIENCE OF CATARACT SURGERY
322
PHACOEMULSIFICATIONIN DISEASED CORNEAS
PHACOEMULSIFICATIONAND IOL IMPLANTATIONIN THE PRESENCE OFOPAQUE CORNEA
OverviewMost of the concepts and techniques
presented on this subject are based on theextensive clinical experience and research ofProfessor Miguel Angel Padilha, of Brazil.For many years, a triple procedure involvinga corneal transplant, cataract extraction andintraocular lens implantation regularly en-tailed an open sky extracapsular cataract ex-traction. This technique exposed the openeye for a long period of time, while thesurgeon performed the anterior capsulotomy,extraction of the cataract nucleus, aspirationof the cortical material and the implantationof the intraocular lens. Only then is thedonor’s cornea placed and adequately su-tured. During this period, the eye is subjectedto considerable risk, including the greatlyfeared complication of expulsive hemor-rhage.
Padilha’s Timing and Technique
When the cornea is opaque to theextent of preventing visualization of the ante-rior chamber, no other alternative is left thanto proceed with the surgical timing and steps
described above: a corneal trephining first,followed by open sky extracapsular extrac-tion, intraocular lens implantation and sutur-ing the donor cornea to the recipient’s corneato complete the operation.
If the cornea is reasonably transpar-ent, allowing the surgeon to visualize thestructures of the anterior chamber (Fig. 188)Padilha’s procedure of choice is removal ofthe cataract by phacoemulsification firstwhich is a pressurized, much safer system,continued by IOL implantation and last, com-pleting the penetrating graft, as first recom-mended by Enrique Malbran, M.D., fromArgentina in 1995.
Step 1: Incomplete trephining of themoderately opaque cornea reaching halfdepth (Fig. 188). Step 2: Viscoelastic isinjected into the anterior chamber through aside port incision. A Valvulated self-sealingscleral tunnel incision 2 mm posterior to thelimbus, is performed, as shown in Fig. 40-B.Step 3: CCC with a bent needle used as acystotome and long Kelman-McPherson for-ceps, preceded by injection of viscoelastic(Figs. 97, 44, 45). Step 4: The remainingphases of phacoemulsification are completedin a routine way, followed by the implantationof an PMMA or foldable intraocular lens,depending on the experience of the surgeon(Fig. 189). A miotic agent is injectedintracamerally. Step 5: Padilha checks thehermetic closure of the sclero-corneal tunnel.The wound may or may not be closed with ahorizontal suture depending on how sure the

C h a p t e r 12: Cataract Surgery in Complex Cases
323
Figure 188: Phacoemulsification in OpaqueCorneas - Stage 1
The surgeon first proceeds to do anincomplete trephining of the affected corneawith the trephine gauged to enter only 1/2 thecorneal depth (T). Next, the surgeon proceedswith the injection of viscoelastic (V) through anancillary incision (A). Through a scleral-corneal tunnel incision, a valvulated self-seal-ing wound 2 mm posterior from the limbus(W), a circular capsulorhexis (C) is performed.The remaining phases of phacoemulsificationare completed in a routine way.
Figure 189: Phacoemulsification inOpaque Corneas - IOL Insertion -Stage 2
Following phacoemulsification,and I/A of the cortical remains, the ante-rior chamber is again filled with vis-coelastic. The next step is the implanta-tion of a PMMA or a foldable intraocu-lar lens (L), depending on the preferenceof the surgeon. Tunnel incision (W).

THE ART AND THE SCIENCE OF CATARACT SURGERY
324
surgeon is of its complete sealing. He pro-ceeds with the removal of the opaque cornealbutton using a disposable Beaver knife andCastroviejo’s scissors (Fig. 190). The sur-geon completes the procedure by bringingtogether the edges of the donor and recipientcorneas, using 16 interrupted 10.0 nylonmonofilament sutures. This approach un-doubtedly reduces the long period of timeduring which the eye remains exposed, thusmaking surgery much safer.
Specific Recommendations
1) Padilha strongly recommends thatthe phaco procedure not be done using a clearcornea incision. Complications or difficultiesmay arise at the time of performing thepenetrating graft. Consequently, use thesclero-corneal tunnel incision shown in Fig.40-B.
2) The technique of phacoemulsifica-tion must be endocapsular, within the capsu-lar bag, using the surgeon’s procedure ofchoice for management and disassemblingthe nucleus. This is with the purpose ofpreventing additional damage to the cornealendothelium. If necessary, the nucleus maybe dislocated into the anterior chamber whereit can be removed or into the iris plane(using Lindstrom’s iris-plane techniques -Figs. 136-139, Chapter 10). But repeatedlylubricating the cornea with dispersive vis-coelastic.
3) If corneal edema deriving from thecorneal disease itself is present and interfereswith visualization of the intraocular maneu-vers, the corneal epithelium may be com-pletely removed to facilitate the surgeon’sadequate view of surgical maneuvers andinstrumentation. (Editor’s Note: placing dis-persive viscoelastic over the cornea will fur-ther facilitate the inner view by the surgeon).
Figure 190: Phacoemulsification in OpaqueCorneas - Completing the PenetratingKeratoplasty - Stage 3
Following the IOL implantation (L),through the tunnel incision (W), the surgeoncompletes the trephining of the cornea and pro-ceeds with the removal of the corneal button (T)with a disposable knife and Castroviejo orBarraquer scissors (S). The surgeon completesthe procedure by placing 16 radial interrupted10-0 nylon sutures in the donor recipient.

C h a p t e r 12: Cataract Surgery in Complex Cases
325
PHACOEMULSIFICATION,IOL IMPLANTATION ANDFUCHS’ DYSTROPHY
Preoperative Evaluation
These patients demand a meticulouspreoperative evaluation before cataract sur-gery. This should not be limited to a goodbiomicroscopic examination with the slitlamp. Specular microscopy and cornealpachymetry may provide additional informa-tion of value to decide if a cataract extractionis sufficient or if a triple procedure is the mostappropriate. These diagnostic examinationsshould be made if the equipment is available.
In the majority of patients, however, adetailed biomicroscopy may be sufficient todetermine the amount of guttata and the ex-tension of the corneal edema.
Role of SpecularBiomicroscopy and Pachymetry
In performing specular biomicros-copy, counting the endothelial cells is notsufficient to guarantee that an eye with cor-neal disease will withstand surgical traumawithout developing further corneal edema,or even worse, bullous keratopathy in thefuture. Analysis of the cell morphology pro-vides important additional information forpredicting the nature of postoperative compli-cations after phacoemulsification or any otherintraocular surgery.
Pachymetry offers a dynamicevaluation of these same corneas. Repetitivemeasures of the thickness of the diseasedcornea may demonstrate how well its fluidsystem functions.
If there is considerable corneal edema,with an endothelial cell count of less than500/mm2 and a central pachymetry up to 610micra, the procedure of choice is performingcombined surgery consisting of penetratingkeratoplasty, cataract extraction and IOLimplantation.
Special Precautions DuringPhacoemulsification
1) The presence of cornea guttata orFuchs’ dystrophy is not a contraindication tophacoemulsification, but it does requireadditional specific precautions. The surgeonmust significantly decrease turbulence andmaintain the anterior chamber with asufficient quantity of BSS and viscoelastic toprevent contact between the nuclearfragments and the endothelium, particularlyat the stage of aspiration of cortical remnants.
2) In corneas with Fuchs’ dystrophy, itis very important to use dispersiveviscoelastic for better adherence to andprotection of the diseased endothelium. Beattentive in case the viscoelastic comes outthrough the wound. This makes it necessaryto reintroduce it fairly often during thesurgical procedure. This should be donethrough the sideport incision (Fig. 191). Thephaco or the I/A tip should be keptfunctioning within the anterior chamberavoiding its removal and reinsertion back andforth through the main incision. This couldlead to additional trauma.
3) During phacoemulsification, themaneuvers should be very delicate, usingtechniques that reduce the time and power ofthe ultrasound. Padilha considers that thephaco fracture or “divide-and-conquer”techniques, are the most indicated. When

THE ART AND THE SCIENCE OF CATARACT SURGERY
326
emulsifying the last quadrant the surgeonmust prevent fragments from moving intothe anterior chamber and touching theendothelium (Fig. 192). The idealprocedure is to maintain a high vacuumpower (150 mmHg or higher), keeping nucle-
ar fragments attached to the titanium tip andset in motion the pulse system of theequipment. If such fragments should moveinto the anterior chamber, dispersiveviscoelastic substance should be used toprevent their touching the endothelium(Fig. 192).
Figure 191 (left): Phacoemulsification inFuchs’ Dystrophy - Use of Viscoelastic
In such altered corneas it is veryimportant to use dispersive viscoelastics (V)for better adherence to and protection of thediseased corneal endothelium. The lateralparacentesis or sideport incision (L) shouldbe used for the intracameral injection ofviscoelastic. The phaco tip introducedthrough the primary incision is not to bereinserted in and out, back and forth (T)for intraocular maneuvers . This could addtrauma.
Figure 192 (right): Phacoemulsificationin Fuchs’ Dystrophy - Ideal Procedure
During phacoemulsification, themaneuvers should be very delicate, de-creasing the power of ultrasound to theminimum desirable, and using techniquesthat reduce the time of ultrasound. Theideal procedure is to maintain a highvacuum power (150 mmHg or more), keep-ing lens fragments attached to the phaco tip(P), and use the pulse system of the equip-ment. If such fragments should tend tomove into the anterior chamber (white ar-row), the dispersive viscoelastic (V) shouldbe once more irrigated into the anteriorchamber to protect the endothelium.

C h a p t e r 12: Cataract Surgery in Complex Cases
327
4) At the time of lens implantation,the first step should be the introduction of acohesive viscoelastic (VE) inside thecapsular bag to maintain the posteriorcapsule well distended, especially if afoldable lens is to be implanted (Fig. 193).The next step is to lubricate the injector withdispersive viscoelastic to facilitate thedelivery of the lens from inside the injectorwith the bag.
At the end of surgery, the aspiration ofthe cohesive VE will be easier and faster thanthe dispersive VE. In order to protect thecornea from any damage, the dispersive VEshould not be removed aggressively althoughall VES should be removed. Administrationof carbonic anhydrase inhibitors andbetablockers during the immediatepostoperative period is always recommendedto inhibit elevation of intraocular pressure,especially in cases with some cornealdisease.
Figure 193: Phacoemulsification in Fuchs’ Dystrophy -IOL Implantation
At the time of IOL implantation (L) the first stepshould be the introduction of viscoelastic in the anteriorchamber and the capsular bag (C) as presented in Fig. 191 tokeep the bag well distended, especially if a foldable lens is tobe implanted.

THE ART AND THE SCIENCE OF CATARACT SURGERY
328
PHACOEMULSIFICATION IN SMALL PUPILS
Pharmacological Mydriasis
Phacoemulsification requires that thepupil be well dilated. Adequate exposureof the lens and the anterior capsule isessential. Padilha first tries to obtain apharmacological mydriasis. He uses acombination of Phenylephrine 10%,Tropicamide 1% ( Mydriacyl R ), and aprostaglandin inhibitor such asIndomethacin or Flurbiprofen 0.03%(Ocufen R ), which is administered every 15minutes during 1 hour before surgery.Among the two inhibitors, Padilha prefersOcufen R, for better maintenance ofthe mydriasis. This pharmacologicalcombination is administered if, of course, nocardiovascular contraindications exist.
If this combination of medications isnot effective, unpreserved adrenaline 1:1000diluted in 10 ml of BSS may be injected intothe anterior chamber at the beginning ofsurgery.
Mechanical Dilatation withViscoelastics
In the presence of iris adhesions to theanterior lens capsule, Luntz mechanicallyseparates them using a viscoelastic passedthrough a cannula. Once the synechiae havebeen separated, intracameral Epinephrine(adrenaline) is injected and in many instancesthe pupil will dilate adequately.
Mechanical Strategies
In patients who have a certain degree ofiris atrophy that may be related to advancedsenility, post uveitis, trauma or the long termuse of miotics in glaucomatous eyes, thefollowing options are available to obtain ad-equate exposure of the lens and the anteriorcapsule.
1. Stretching the Pupil
The pupil in most patients can bestretched to an adequate dilatation using twoKuglin hooks as advocated by MauriceLuntz, M.D. One Kuglin hook is insertedinto a preformed temporal paracentesis andadvanced to the opposite nasal pupil marginwhere the Kuglin hook engages the pupilmargin (Fig. 194). The second Kuglin hookenters the anterior chamber through a pre-formed nasal paracentesis, is advanced acrossthe anterior chamber to the opposite temporalpupillary edge, which it engages (Fig. 194).Both Kuglin hooks are now pushed towardthe limbus, stretching the pupil horizon-tally until maximal stretching is achieved.There will inevitably be some small sphinctertears.
Both Kuglin hooks are now removedfrom the anterior chamber and re-entered intothe anterior chamber through two preformedkeratome incisiona one at 12 o’clock and theother at 6 o’clock (Fig. 195). One Kuglinhook is advanced across the anterior chamberto engage the pupil margin at 6 o’clock, and

C h a p t e r 12: Cataract Surgery in Complex Cases
329
Figure 194 (left): Stretching the PupilHorizontally with Two Kuglin Hooks
One Kuglin hook is inserted through atemporal paracentesis and advanced to theopposite nasal pupil margin and engages thepupil margin. The second Kuglin hook entersthe anterior chamber through a nasal paracen-tesis, and is advanced across the anteriorchamber to the opposite temporal pupillaryedge, which it engages. Both Kuglin hooksare now pushed toward the limbus, stretch-ing the pupil horizontally until maximalstretching is achieved.
Figure 195 (right): Stretching the Pupil Verti-cally with Two Kuglin Hooks
Both Kuglin hooks are now re-positionedthrough keratome incisions at 12 and 6 o’clock.One Kuglin hook is advanced across the anteriorchamber to engage the pupil margin at 6 o’clock,and the second Kuglin hook engages the pupilmargin at 12 o’clock. Both Kuglin hooks arepushed toward the limbus facing each otherthereby stretching the pupil vertically. Oncethe maximal vertical extension is achieved, theKuglin hooks are removed.

THE ART AND THE SCIENCE OF CATARACT SURGERY
330
the second Kuglin hook engages the pupilmargin at 12 o’clock. Both Kuglin hooks areagain pushed toward the limbus, facing eachother, at 6 and 12 o’clock, thereby stretchingthe pupil vertically (Fig. 195). Once the maxi-mal vertical extension is achieved, the Kuglinhooks are retracted. Intracameral epinephrineis injected, followed by intracameral vis-coelastic. In those eyes in which the pupilmargin in not significantly fibrosed and nottoo spastic, this maneuver can achieve asufficiently dilated pupil to proceed with pha-coemulsification. The technique usingKuglin hooks has also been advocated byMiguel Padilha, M.D.
2) Mechanical Pupillary Dilators
In those cases in which the pupilmargin is fibrosed or very spastic, one of thefollowing procedures may be necessary.
A) Plastic Iris Hooks (Alcon-Grieshaber) are inserted through four para-centesis incisions in the cornea (Fig. 196) asadvocated by Luntz as well as Padilha. Thehooks engage the pupil margin at the 10:00o’clock, 2:00 o’clock, 4:00 o’clock and 8:00o’clock meridians, and the pupil is forciblyenlarged by pulling the hooks outward andfixing their positions. Metal hooks are alsoavailable but Luntz considers that plastichooks are less traumatic to the pupil.
Figure 196: Alcon-Grieshaber Flexible Iris Re-tractor for Small Pupil
The flexible iris retractor is a safe alternativefor temporary iris fixation in cases where dilatationcannot be achieved pharmacologically and when thepupil is not fibrosed and can be stretched. Theretractor is made of prolene and a flexible tab (H)made of nylon holds the hook in position once in theeye. Four self-sealing 0.5 mm stab paracentesisincisions are made in the peripheral cornea at the10:00, 2:00, 4:00 and 8:00 o’clock meridians. Thehooks (H) are inserted through the paracentesis inci-sions (P) and engage the iris at the pupil margin(arrow - 1). The pupil is forcibly enlarged by pullingthe hooks outward (arrow - 2). The final position ofthe hooks is fixed by adjusting the flexible nylon tabtoward the eye (arrow - 3). Inset shows surgeon’sview of the final configuration of the retractors andthe resulting pupil shape.

C h a p t e r 12: Cataract Surgery in Complex Cases
331
When the pupil margins are heavilyfibrosed this method will not achieve ad-equate pupil dilation, or the pupil margin maybe severely traumatized.
Padilha considers that, of all the avail-able mechanical resources, the one that hascontributed the most safety and satisfaction inthe management of small pupils is the flexibleiris retractor (Alcon-Grieshaber) (Fig. 196).These retractors are extremely useful, even ifplacing them requires extra time. After theplacement of the first or the second retractor,the anterior chamber may need to be refilled
with viscoelastic to facilitate the introductionof the other two.
B) The Beehler Pupil Dilator
Padilha uses this instrument when theother options outlined above have not beeneffective. This dilator, made by Moria, inFrance, allows dilatation in three directionswith only one maneuver (Fig. 197). More-over, it provokes a discrete retraction of theiris in the direction of the corneal or scleraltunnel incision.
Figure 197: Phacoemulsification in Small Pupils -Beehler’s Pupil Dilator
The Beehler’s pupil dilator (B) allows dilation inthree directions with only one maneuver. Three arms (A)extend from inside the instrument and exert distention on themargins of the pupil. The same instrument also stimulates adiscrete retraction of the iris in the direction of the corneal orscleral tunnel incision (T).

THE ART AND THE SCIENCE OF CATARACT SURGERY
332
C) The Silicone Expander Ring
In more severe cases, Padilha uses asilicone ring with an indentation, which fitsall along the edge of the pupil. This presentssome advantages. Using this technique theiris fits like a tire around the ring, which islike an iron wheel (Fig. 198). Among itsdisadvantages is the fact that it can loosenitself easily with intraocular maneuvers dur-ing the phaco procedure. Known asGraether’s pupil expander (EagleVision#1540) it has three components: the pre-loaded expander, a disposable insertor and aglide retractor of the iris. (The use of this ringis controversial - Editor).
Figure 198: Phacoemulsification in Small Pupils -Adjustment of the Silicone Expander Ring
Once the silicone expander ring (E) is inposition, Padilha slides out the iris retractor glide(not shown) and adjusts the final placement of thesilicone expander using two Sinskey hooks (H).
Padilha emphasizes that stretchingmaneuvers using mechanical dilators mayinduce a certain degree of iris atony. Thispredisposes the iris margins to insinuate intothe titanium tip, during the phaco maneuvers,leading to injury of the sphincter and the iristissue. The same can occur with sector iridec-tomies, which can also predispose the iris tothe development of synechiae to the anteriorcapsule during the postoperative period, re-quiring the administration of miotic drops forsome time.

C h a p t e r 12: Cataract Surgery in Complex Cases
333
TRAUMATIC CATARACTS
Overview
The complex repair of an eye injury isbest when a team which shares anterior andposterior segment skills work together inprimary and secondary management.
Almost all bad results following oculartrauma occur in injuries involving the poste-rior segment, particularly when the lens isalso damaged
Assessment of the Injured Eye
The circumstances of the injury and theearly clinical assessment give important in-formation that will determine the early man-agement and help to predict complications.
As pointed out by Michael Roper-Hall, M.D., an accurate history is essential.This can be very helpful in indicating thenature and extent of injury. The true historyis sometimes elusive, especially when chil-dren are involved, or there is potential forlitigation.
The injuries that cause traumatic cata-ract occur not only from serious penetratingtrauma, but also from blunt injury. Mostblunt injuries are not severe enough to causerupture of the sclera. In evaluating andmanaging all blunt injuries, it is important torecognize that each ocular tissue, from thecornea to the posterior choroid, may havebeen damaged by the impact. Therefore,management is based on identifying the af-fected tissues, understanding the pathophysi-ology of events that can occur after a bluntinjury, and anticipating possible secondarycomplications.
Highlights of Examination
The ophthalmologist must examine thepatient carefully. The examination shouldbegin with an assessment of the visualfunction, if there is light perception or lightprojection. The prognosis is better if there isgood light projection. Then the eye shouldbe examined in the usual way with the directophthalmoscope and the slit lamp. In manycases the fundus cannot be visualized be-cause of the presence of opaque media: cor-nea, lens, and vitreous hemorrhage. Thepresence of a foreign body must be definitelyexcluded. It is important to search for ana-tomically related trauma. Individual in-traocular structures are not often damagedalone.
In severe injuries, the full extent ofdamage is obscured by blood or opacities inthe media . Special assessment is neededbefore planning surgery to establish the ex-tent of damage and the visual potential.There may be no light perception in thepresence of a complete vitreous hemorrhage -until the hemorrhage clears. In such casesdiagnostic imaging is invaluable.
Diagnostic Imaging
B-scan ultrasonography should beused to identify the presence of a foreignbody and where is it precisely located, theamount of vitreous hemorrhage present andthe condition of the retina. Ultrasound imag-ing also demonstrates changes in lens posi-tion; posterior rupture of the lens; cyclitic

THE ART AND THE SCIENCE OF CATARACT SURGERY
334
membrane; hemorrhage into the vitreous;separation of the vitreous from the retina; andretinal detachment, which are obscured todirect examination (Fig. 199).
Combined Injuries of Anterior andPosterior Segment
A damaged lens mixed with blood andvitreous needs prompt and adequate surgery.Failure to remove this debris encouragesfibrosis with a cyclitic membrane causingciliary body detachment and hypotony even-tually leading to retinal detachment and ph-thisis bulbi.
Traumatic Cataracts in thePresence of Anterior SegmentPenetrating Wounds
Main Objectives
In anterior segment injuries the initialobjectives are watertight repair of the cornealwound, restoring normal depth to the anteriorchamber, intensive antibiotic treatment toprevent infection and intense antiinflamma-tory therapy from the very start. The furthergoals are to manage the cataract adequately,reduce secondary damage by minimizing ex-cessive corneal scarring; assuring a clear,adequately sized and cosmetically and opti-cally desirable pupillary opening; and pre-venting further damage to the anterior cham-ber angle that could result in glaucoma.
Often all of these objectives can beachieved at the time of initial wound repairalthough in some cases further surgicalprocedures are needed. The traumatic injurymay have caused a lens anterior capsular
defect either from a blunt rupture or a sharplaceration.
MANAGEMENT OFTRAUMATIC CATARACT
Robert Stegmann, M.D., has very ex-tensive experience in trauma cases. He be-lieves that the prognosis for a traumatic cata-ract can be the same as for a routine senilecataract if the traumatic cataract is handledproperly. This excludes cases in which thereis damage to the posterior segment, the vitre-ous has become cloudy, or the retina is dam-aged from the same trauma, or where infec-tion has occurred.
Small Wounds in AnteriorCapsule
In many cases a penetrating wound inthe cornea and lens is small, the lens materialstill remains within the capsule and, eventhough cloudy, it may not escape through thetiny capsular tear (Fig. 200). Prof. GioraTreister from Israel recommends that in suchcases, the lens be left alone during the firstsurgical intervention. He repairs the primarywound and goes no further at this timebecause generally these are the worst condi-tions for operating on the eye. The tissues areswollen and irritated, and perhaps even in-fected. The trauma may have occurred atnight. In case of unexpected complications,the most experienced surgeons are not onduty.
If it is not absolutely necessary to gofurther with the initial procedure, Treisterrecommends that it will suffice to close theprimary wound and to concentrate on properreconstruction later.

C h a p t e r 12: Cataract Surgery in Complex Cases
335
Figure 199 (above): Importance of Diagnostic Imaging inTraumatic Cataracts
In addition to studying the cataract itself, B-scanultrasonography demonstrates changes in lens position; pos-terior rupture of the lens; cyclitic membrane; hemorrhageinto the vitreous; separation of the vitreous from the retina;and retinal detachment, which are obscured to direct exami-nation. Figure 199 shows a polaroid photo of a B-scanultrasound.
Figure 200 (below): Traumatic Cataract from Small Penetrating Wound in theCornea and Lens
This cross section of the anterior segment of the eye shows a damaged lenswith an anterior capsular tear (T). The lens is cloudy but lens material has still notescaped through the capsular tear. In such cases, Dr. Treister repairs the primarycorneal wound (W) at this time and goes no further (assuming that the posteriorsegment of the eye is not involved in the trauma). A few days later when the eye isless irritated, lens extraction and IOL insertion can be performed.

THE ART AND THE SCIENCE OF CATARACT SURGERY
336
If Anterior Capsule More WidelyDamaged
If the anterior capsule is more widelydamaged and lens material is present in theanterior chamber, (Fig. 201) Treister re-moves all the lens material during the firstsurgical intervention and examines the poste-rior segment with the indirect ophthalmo-scope. If the trauma is confined to the anteriorsegment, the vitreous is clear, the retina isattached without retinal tears and no foreignbody is seen, a posterior chamber lens isimplanted .
Timing for Primary LensExtraction
John Alpar, M.D., who has extensiveexperience with traumatic cataracts, consid-ers that a primary lens extraction shouldoccur any time the lens is so damaged that itsparticles are mixed with anterior chamber orvitreous material. The lens should also beremoved in cases of subluxated lens follow-ing trauma. The advantages of a primaryoperation in these cases are that postopera-tive inflammation is reduced, rehabilitationtime is faster, and later examinations, includ-ing the evaluation of the retina, are easier toperform.
Figure 201: Traumatic Cataract with Anterior Capsule WidelyDamaged
Lens material is present in the anterior chamber. Viscoelastic hasbeen injected into the anterior chamber. The AC is irrigated (blue arrow)with BSS and the debris, pigment residues, fibrin and lens material (D) arewashed out of the eye (red arrow). Lens damage shown in (L).

C h a p t e r 12: Cataract Surgery in Complex Cases
337
The most important indications forprimary operation are signs that point to thelikelihood of a ruptured posterior capsulewith vitreous already entering the chamber.
More Extensive DamageAffecting Posterior Capsule
In case of perforation of the lens withan opening also in the posterior capsule,Treister as well as Stegmann in SouthAfrica remove the vitreous from the anteriorchamber (if present) with a vitrector to-gether with the lens material but try to pre-serve the posterior lens capsule, or part of it,for sulcus-placed posterior IOL implantation.
Specific Problems withTraumatic Cataracts
Paul Koch, M.D., points out thatzonules are often torn and there may besignificant risk of collapse of the posteriorcapsule as well as vitreous prolapse aroundthe equator of the lens. Consequently, in thepreoperative evaluation with the slip lamp,look carefully for evidence of zonulysis.
HIGHLIGHTS OFSURGICAL TECHNIQUE
The Incision
A sclero-corneal tunnel (Fig. 40-B) isdefinitely the incision to be used. A cornealtunnel incision is contraindicated. Theconjunctiva must be treated very delicately.Some of these patients may develop second-
ary glaucoma and might need a filteringoperation at a later date.
Anterior Capsulorhexis
In many cases the anterior capsule hasbeen perforated. A CCC may be quite diffi-cult and sometimes risky. Paul Koch hasadvocated that a better way to open theunsupported part of the anterior capsule rup-tured zonules is to use capsule scissors. Apuncture can be made in the anterior capsule,scissors introduced with one blade throughthe puncture, and a snip capsulotomy per-formed. Koch points out that pulling inwardto create a capsulorhexis with a needle orforceps could be dangerous, dislocating thelens beyond the point of recovery.
Other parts of the capsule, where thezonules are intact, may be opened in the usualfashion.
The circular anterior capsulotomyshould be made large enough so that thenucleus can be floated out of the bag withhydrodissection. Typically this occurs easilybecause the nucleus is white, soft and fluffy.
In performing the anterior capsulotomy,if the cataract is white, the use of Trypan Blueas shown in Figs. 101 and 102, page 173 mayincrease the possibility for performing asuccessful capsulotomy.
Lens Removal
In the presence of traumatic cataract,phacoemulsification is done in the anteriorchamber. Once the nucleus enters the anteriorchamber, viscoelastic can be placed aboveand below it, protecting the cornea and push-ing the flaccid capsule as far posteriorly as

THE ART AND THE SCIENCE OF CATARACT SURGERY
338
possible. In a young patient the nucleus isusually very soft and is amenable to manydifferent options. For a patient with an intactcapsulorhexis, phaco-aspiration of thenucleus is safe and effective. If an anterior orposterior capsular tear is present, then manualaspiration with a Simcoe-style cannula af-fords greater control. «Dry» aspiration of thesoft nucleus under viscoelastic material offersexcellent control, especially in the most com-plicated cases, as advocated by Snyder andOsher.
Role of Intracapsular TensionRing in Traumatic Cataracts
This is an important advance incataract surgery. The ring is a relatively
recent development, as advocated by RobertJ. Cionni, M.D., in the U.S. and OkihiroNishi, M.D., in Japan. This device maintainsthe shape of the bag during and followingextracapsular surgery or phacoemulsificationin traumatic cases or in patients with sublux-ation or pseudoexfoliation. It has importantimplications in terms of preventing IOL dislo-cation, decentration, tilting, further zonulardehiscence, and posterior capsule opacifica-tion. The capsular tension ring (orintracapsular ring), is an open circularPMMA haptic (Fig. 202). It can distribute theforces inside the capsular bag, thereby mak-ing it possible to perform surgery safer, anddecentration of the IOL is prevented.
In the management of traumatic cata-racts, the ring is placed in the bag for support,
Figure 202: Concept of IntracapsularTension Ring in Traumatic Cataracts andSubluxated Lenses
(A) The intracapsular tension ring(R) is an open circular PMMA ring inserted(arrows) into the capsular bag (C) via aninjector (I) through a 3.5 mm incision. Bothends have a small eyelet (E) for bettermaneuverability with a hook during implan-tation. The ring lies at the equator of thecapsular bag and so maintains the capsularbag shape. An IOL can then be implantedinto the capsular bag with the ring in place.(B) Shows an isolated view of the entirecapsular bag with the ring (R) and IOL (L)in place, with haptics of the IOL (H) prop-erly positioned within the distended bag.The intracapsular ring distributes the forces(arrows) inside the capsular bag, therebymaking it possible to work safely. Asym-metrical collapse of the bag anddecentration of the IOL is prevented.

C h a p t e r 12: Cataract Surgery in Complex Cases
339
provided that there is an intact anterior capsu-lotomy and posterior capsular bag. In somecases it will be easy to place it prior toemulsification of the nucleus, while in otherpatients it is better to place it prior to corticalaspiration. This will stabilize the capsule andsupport the areas lacking zonules. Once thecapsule is secure, the cortex can be removedand the implant placed. If necessary the ringcan be sutured transsclerally..
Removal of Cortex
After nucleus removal, before proceed-ing with cortical aspiration, inspect the poste-rior capsule carefully to be sure that there areno tears as a result of the injury, particularly ablunt injury, where tears might be hidden.
If the capsule is intact, proceed as usual,following the principles and techniques out-lined in Figs. 127 and 128. In case of doubtabout the effects of automated irrigation-aspiration, you may use the manual aspirationwith the Simcoe-type cannula, as shown inFig. 128. This allows a greater degree ofcontrol.
Selection of IOL
Traumatic cataracts may be associ-ated at a late date with some vitreoretinalcomplications. PMMA and acrylic lenses arewell tolerated by the eye and preferred by thevitreoretinal surgeons. Since traumatic cata-racts are not uncommonly associated withsome degree of traumatic mydriasis, a 6.0mm or larger diameter IOL optic is a prudentchoice.
IOL Implantation
With the support and stability of anintracapsular tension ring, the placement of
the IOL in the capsular bag is indicated anddesirable. If an intracapsular ring is notavailable and only a small area of zonulardehiscence is present, slowly unfolding theimplant or very gently placing a rigid lenswith soft loops will minimize the stress on theintact remaining zonules.
Ciliary sulcus placement of a posteriorchamber implant is still possible in the settingof a posterior capsular tear or zonular dialysis(Figs, 153, 154, 156). If the anteriorcapsulorhexis is intact, yet a severe posteriorcapsule break exists, the haptics should beplaced in the sulcus. It may be possible tocapture the lens optic posteriorly into thecapsulorhexis. This will provide adequatesupport and will prevent the lens from subse-quently dislocating.
If the capsulorhexis is incompetent orlarger than the implant optic, sulcus fixationwith a large diameter implant can be utilized.
Selection of Viscoelastic inTraumatic Cataracts
In those eye centers where the two maintypes of viscoelastics are available (disper-sive and cohesive), the following are goodchoices as advocated by Snyder and Osher:1) When the hyaloid face is partly exposed, ahighly retentive (dispersive) viscoelasticagent such as Viscoat (Alcon) or Vitrax(Allergan), may tamponade the vitreous andkeep it back. The dispersive agents alsoprotect the endothelium well. This may beparticularly important in cases in which theendothelial cell density has been reduced bythe trauma. 2) On the other hand, the spaceretaining qualities and ease of removal typicalof highly cohesive viscoelastic agents, suchas Healon GV (Pharmacia & Upjohn), makethese agents more appropriate for the lensimplantation stage of the procedure.

THE ART AND THE SCIENCE OF CATARACT SURGERY
340
Phacoemulsification Advan-tages in Traumatic Cataract
Traumatized eyes with potentiallyweakened zonules are at greater risk for su-prachoroidal hemorrhage. Maintaining aclosed system as provided by phacoemulsifi-
cation reduces the risk of expulsive hemor-rhage. In addition, a closed system allowscompartmentalization within the anterior seg-ment. If the posterior capsule is broken or if azonular dehiscence is present, viscoelastictamponade of the vitreous can be best main-tained in the setting of a closed system.
PHACOEMULSIFICATION INSUBLUXATED CATARACTS
Strategic Management
Phacoemulsification is performed in atotally closed system, where the ultrasoundtip blocks the incision, allowing the volumeof aspirated masses to equal the volume ofliquid injected into the anterior chamber, thusmaintaining stable intraocular pressurethroughout the surgery. The space availablefor disassembling the cataract is extremelysmall, limited anteriorly by the cornealendothelium and, posteriorly, by the posteriorcapsule.
If the zonules sustaining the crystal-line lens are weak, broken or nonexistent, inpart or totally, or when the posterior capsuleis ruptured, a delicate and risky situation mayarise unless we are ready to manage it effec-tively.
MANAGEMENT DEPENDING ONSIZE OF ZONULAR DIALYSIS
When confronted with a zonularrupture, Padilha recommends adopting thefollowing strategies: 1) If duringbiomicroscopy at the office, under mydriasisand with a slit lamp, a small or moderatezonular dialysis is detected, which does not
extend to more than 45º of the crystallinelens circumference, and we can see anexcellent red retinal reflex, it is almostcertain that a phacoemulsification can beaccomplished safely.
The hydrodissection must separate thelens capsule from the cortex by injectingbalanced salt solution (BSS) under the ante-rior capsule, and the hydrodelamination mustattain consistent detachment of the nucleusfrom the epinucleus (Fig. 203).
The sharp separation of these structureswill significantly reduce the tension on thefragile zonules during disassembling of thenucleus and aspiration of the residual cortex.
2. a) If the damage to the zonular fibersextends to more than 45º and the cataract hasa hard nucleus with a retinal reflex turningbrown, or b) the dialysis extends to 180º,the insertion of an intracapsular tension ring(Fig. 202) will be extremely useful to bettersupport the crystalline bag throughout thesurgical procedure, reducing the chances ofdislocation of the cataract into the vitreous.This is true even in cases of soft cataract. Theuse of the intracapsular tension ring is alsovalid for cases with pseudoexfoliation andectopia lentis – as in the Marfan syndromeand others.

C h a p t e r 12: Cataract Surgery in Complex Cases
341
3. On the other hand, if there is avery extensive damage to the zonular fiberswith a dialysis of more than 180º, Padilhaconsiders that phacoemulsification or even aplanned extracapsular extraction may not besufficiently safe, even with the help of theintracapsular tension ring (Fig. 202), espe-
cially in cases of hard cataracts. In thesepatients, Padilha advocates performing anintracapsular extraction associated with aKelman anterior chamber implant, or aposterior chamber lens fixated to the sclera(Fig. 156). He considers this to be a moreprudent solution.
Figure 203: Subluxated Cataracts - Hydrodissection
The cannula (C) is positioned under the anterior capsule (A) and the BSS isinjected separating the cortex from the nucleus and epinucleus. This maneuver isrepeated in order to create a clear cleavage plane. Too much irrigation must beavoided. Otherwise, it may produce a dangerous blocking of the nucleus against themargins of the anterior capsulotomy. This could give rise to a sudden dislocation ofthe cataract into the vitreous (V) by creating a tear of the posterior capsule (P).

THE ART AND THE SCIENCE OF CATARACT SURGERY
342
Special Precautions withSubluxated Cataracts
Padilha points out that some importantissues should be considered when subluxatedcataracts are approached.
Anterior Capsulotomy
Anterior capsulotomy should beperformed as a continuous curvilinearcapsulorhexis (CCC). The surgeon needs touse extreme caution starting with a bentneedle and completing it with this sameinstrument or with the Uttrata’s or similarforceps.
If any problem arises at the time ofthe anterior capsule perforation with the cys-totome (bent-needle) the surgeon may beginthe capsulorhexis with a pinch-type forcepssuch as the Kershner capsulorhexis cysto-tome-forceps (Rhein Medical). The maneu-vers should be executed very carefully andsmoothly so as to prevent further damage tothe zonules. The diameter of this capsulo-tomy should not be very large. Reaching theequatorial region must be avoided at all costs.(Editor’s Note: I also refer you to the discus-sion of Traumatic Cataracts complicated bysome zonular dialysis, in which Paul Kochrecommends using scissors to perform theanterior capsulotomy so as to not exhertfurther pressure on the weakened zonuleswith the maneuvers of a standardcapsulorhexis.)
Characteristics of ViscoelasticsUsed
Another important issue involves theuse of viscoelastic substances. It is importantto combine one viscoelastics with cohesive
properties, with another of dispersiveproperties, which scatters and adheres to in-struments or tissues. While the latter willprotect the damaged zonular area, by adher-ing to adjacent tissues of that region andhelping prevent an eventual escape of thevitreous, the cohesive viscoelastic will pressdown upon the anterior face of the crystallinelens, transforming it into a convex surface,and facilitate making the CCC. Such convex-ity will help channel the zonular tear in thedirection of the center of the capsule andnot toward the periphery because of the cen-trifugal force generated above the surface(Fig. 204). (Editor’s Note: A very cleardefinition of the qualities of the cohesive andthe dispersive viscoelastics, and how theydiffer from one another, is presented at thebeginning of this Chapter).
Additional Measures to ReduceRisks
1) Padilha recommends that the pha-coemulsification incision, whether in clearcornea or a scleral tunnel, should be placedas far away (circumferentially) as possiblefrom the damaged zonular region. This is toprevent extension of the zonular dialysis bythe insertion and withdrawal of instruments inthe interior of the eye precisely in the mostaffected area. If the zonular rupture is locatedin the superior quadrants a superior temporalincision will make surgery more demandingand risky.
2) To further reduce risks, Padilhaadvises the use of disposable plastic flexibleiris retractors, which will help sustain andstabilize the crystalline bag. The flexiblehooks are anchored in the borders of theCCC, in exactly the way we use them in

C h a p t e r 12: Cataract Surgery in Complex Cases
343
Figure 204 (left): Subluxated Cataracts - Use ofDispersive Viscoelastic
An important issue involves the use of vis-coelastic substances. These substances should havecharacteristics such as viscosity, pseudoplasticity,coatability and elasticity, which will allow variousmaneuvers during the surgical procedure. This viewshows a cannula (C) inserted under the iris (I) in theregion where a zonular dialysis (ZD) is present,injecting a dispersive viscoelastic, closing the dam-aged zonular area and lessening the chances of aneventual vitreous escape.
Figure 205 (right): Subluxated Cataracts - Help-ing Support of Capsular Bag with Flexible IrisRetractors
To provide more support to the capsular bag,flexible iris retractors (F) are fastened to the bordersof the anterior capsulotomy (C). The retractors areinserted through four opposite ancillary incisions.Once the retractors are in position (F), thecapsulorhexis (C) is carefully put on stretch, withoutmuch traction. Then the surgeon may proceed withphacoemulsification using very low parameters suchas vacuum less than 150 mmHg, low irrigation andreduced ultrasound power (less than 70%). Phacoprobe (P).

THE ART AND THE SCIENCE OF CATARACT SURGERY
344
order to dilate small pupils (Figs. 205 and196) except that the retractors are placed inthe margins of the anterior capsulotomyinstead of the margins of the pupil.
3) During disassembling of the nucleus,maneuvers to rotate the nucleus should bereduced to a minimum. In order to prevent theneed for these maneuvers, hydrodissectionand hydrodelamination should done carefullybut thoroughly.
4) Padilha recommends that theintracapsular tension ring be introduced afterthe hydrodelamination is completed andbefore emulsification (Fig. 202). This is an-other very important measure to provide sup-port to the capsular bag. Usually the ring isheld by a long Kelman-McPherson forcepsand introduced clockwise. When operating onthe right eye using a superior sclero- cornealtunnel incision, the ring is moved 1 hour inthe direction of 3 o’clock and 6 o’clock. Aspatula—preferably Koch’s spatula—is usedto facilitate the insertion of the ring in thecorrect position inside the bag. These ringscome in different sizes. They are producedby Morcher GmbH, Germany, and Corneal,France, and will be commercially availablethrough Alcon in the near future.
If an accidental cataract subluxationoccurs during a conventional cataract sur-gery, the surgery must be interrupted and thering should be introduced as described above.In these cases, Padilha prefers to implant aone-piece intraocular lens, all PMMA, insidethe capsular bag and to make its length coin-cide with the meridian where the zonularrupture occurred.
Increasing the Safety ofPosterior Lens Implantation inExtensive Zonular Disinsertion
In those cases where a more extensivezonular disinsertion is present, it is importantto create safer conditions to implant a lens inthe posterior chamber. Variations and con-stant improvements of this technique havebeen presented at various meetings and pub-lications by many authors, especially Drs.Jorge Villar-Kuri, from Mexico, RobertOsher, from the United States, YoshihiroTokuda, from Japan, Charlotta Zetterstrom,from Sweden, among others.
Some guidelines are basic and veryimportant in these extreme situations,including cases of Marfan’s syndrome. Thesurgeon should always opt for a smallcapsulorhexis using a bent needle, and carryout the hydrodissection very carefully.
Padilha considers there are at leastthree options in order to increase the safetyof the posterior chamber lens implantation.The first consists in totally removing thecapsular bag following removal of thecataract. This could be indicated in certainsituations where the lens is too dislocatedeither superiorly or inferiorly, and vitreousloss is present. Following a generous anteriorvitrectomy using an automated vitrector,the intraocular lens is sutured to the sclera,(Fig. 156).

C h a p t e r 12: Cataract Surgery in Complex Cases
345
Fixation of the Anterior Capsule tothe Ciliary Sulcus
The second option to increase thesafety of the posterior lens implantation andto prevent it from dislocating is to actuallysuture the anterior capsule to the ciliary sul-cus. This is done so that when the IOL issutured and implanted, it will remain in place.
This technique involves making two incisionsin the anterior capsule, through the smallCCC (Fig. 206), as in the intercapsular tech-nique advocated some years ago by Sourdilleand Galand. The borders of the free edge ofthe capsule should be folded and sutured tothe sclera at the opposite side of the luxation,as suggested by Villar-Kuri . The step-by-step technique is shown in Figs. 206-210.
Figure 206 (above): Subluxated Cataracts- Fixation of the Anterior Capsule to theCiliary Sulcus - Stage 1
Once the capsular bag is filled withviscoelastic, the anterior capsulotomy (C) isenlarged to the left and right using Vannasscissors (V). This allows the capsule todistend and allow more space for theinsertion of the IOL.
Figure 207 (below): Subluxated Cata-racts - Fixation of the Anterior Capsuleto the Ciliary Sulcus - Stage 2
A prolene 10-0 suture (P) is care-fully inserted in the anterior chamber andthrough the anterior capsule flap (C) thathas been created with the scissors, in acurved “U”. Take care to ensure that theendothelium is not touched. Scleral flapin the inferior part of the globe for finalfixation of sutures (F).

THE ART AND THE SCIENCE OF CATARACT SURGERY
346
Figure 208 (above): Subluxated Cataracts - Fixa-tion of the Anterior Capsule to the Ciliary Sulcus -Stage 3
Viscoelastic is reinjected in the anterior cham-ber. Through an inferior triangular scleral flap (F), 2.0mm from the limbus, the surgeon introduces a straight,long, 25 gauge needle (N), emerging through theprimary incision (M), with its bevel up. Into its borethe surgeon inserts the C7 needle (magnified inset),and slowly pulls the long needle until it goes out of theglobe through the inferior scleral flap.
Figure 209 (center): Subluxated Cataracts -Fixation of the Anterior Capsule to the CiliarySulcus - Stage 4
The suture is used to pull up the anteriorcapsule (C) to the inferior scleral bed (S). Theknot is buried inside the sclera, closing thescleral flap (F) with a 10-0 nylon suture (N).
Figure 210 (below): Subluxated Cataracts - Fixa-tion of the Anterior Capsule to the Ciliary Sulcus -Last Stage
At this point the anterior capsule (C) is fixed tothe ciliary sulcus to permit more space and safety forthe IOL insertion. Finally, the IOL of the surgeon’schoice (L) is implanted, placing it in a position perpen-dicular to the disinsertion. The primary incision isclosed with a horizontal 10-0 nylon suture (N).

C h a p t e r 12: Cataract Surgery in Complex Cases
347
CATARACT SURGERY IN CHILDHOOD
Previous Controversies NowResolved
Cataract surgery in the pediatric patientand the post op management of these childrenis still a complex problem, but significantlyless than up to five years ago. The difficultcontroversies previously existing regardingfinding solutions for their visual recoveryhave been solved in most cases. These con-troversies are:
1) Age and Timing for Surgery
Bilateral Cataracts
It is now generally agreed that earlycataract surgery in bilateral cataracts andimmediate optical correction can preventotherwise irreversible deprivation amblyopiain the child born with dense cataracts. Un-less this is done, children with bilateral cata-racts who undergo surgery later in childhoodor in their teens recover only limited visualacuity, usually an average of no better than20/60. Optimum optical correction followingsurgery is more effectively done today withIOL implantation.
In infants with bilateral cataracts, de-spite an increased complication rate, surgerymust be performed within the first months ofage to avoid irreversible amblyopia.
Cataract surgery in children over theage of 1 year is less complex with a highersuccess rate and with fewer complications inthe postoperative period. It is best to performsurgery in both eyes at the same «sitting».Sterility must be maintained during the whole
procedure in bilateral cases. This requireschanging all instruments and sterile clothingof the surgeon, nurse and patient betweeneyes. Patching is not indicated. Generalanesthesia is used in all cases.
Unilateral Cataracts
Unilateral congenital cataract presents amore challenging problem, since even a mildcataract will cause irreversible deep amblyo-pia in one eye if not treated. Treatment isbased on surgery within two months of life,prompt optical correction with intraocularlens implantation and aggressive occlusiontherapy with frequent follow-up have beensuccessful in several series.
Preconditions to be Met forUseful Vision
In cases of unilateral cataracts, ifcataract surgery with IOL implantation is notdone very early in life, the chances ofachieving good vision are slim. It is possibleto achieve useful vision in some childrenwith monocular congenital cataracts providedcertain important preconditions are met. Themost important is the age at which the surgeryis undertaken along with equally importantimmediate optical correction and occlusiontherapy as emphasized by Noel Rice, M.D.at Moorfields Eye Hospital in London andEugene Helveston, M.D. in the U.S. yearsago. These preconditions continue to bevalid. It is essential first to provide a focusedimage and second, eliminate suppression.
This «triumverate» or «troika» oftreatment is the key to success. To a great

THE ART AND THE SCIENCE OF CATARACT SURGERY
348
extent, the ophthalmologist depends on otherprofessionals who determine when the cata-ract is identified and referral takes place. Ifthe child does not present to the ophthalmolo-gist within the optimal period for surgery andoptical rehabilitation, clearly the ophthalmicsurgeon is considerably constrained in thequality of care he/she can provide. Timing isabsolutely the key. If the surgeon decides tooperate on a unilateral cataract, the familyneeds to expect the very high likelihood ofonly a helper eye, and not an eye that willhave very good vision. It is important toacknowledge this limitation.
Role of Parents
Their role is absolutely essential forachieving a good result. The surgeon wouldbe wise to take this factor into considerationbefore undertaking treatment. Parents whodo not understand what they and the childneed to go through for pre and postoperativemanagement to prevent and «conquer» am-blyopia, become the first contraindication tosurgery. This is particularly important inunilateral cataracts in which prolonged am-blyopia treatment is essential.
Importance of AsymmetricalVisual Input
The period of sensitivity of the visualsystem and its responsiveness to the develop-ment of vision through having a good visualinput in humans is still not precisely deter-mined, but we know that it is most respon-sive during early infancy, and it falls offrapidly during the first year of life. Theclinical research made by Rice at Moorfieldsand Von Noorden in the U.S. determined
that the implications of asymmetrical inputinto the visual system are vitally important,particularly in relation to unilateral congeni-tal cataracts.
When Should We Not Operate?
Any unilateral lenticular opacity that ismoderately severe will cause amblyopia. Ifmanagement as here described is not pos-sible very early in life, it may be best if weadvise against it. Very mild unilateral len-ticular opacity, may be best left alone. Re-moving a small unilateral cataract that causesa small degree of amblyopia creates aphakia,which may lead to even more amblyopia,unless we implant the adequate IOL andundertake aggressive occlusion therapy.
Preoperative Evaluation
History
In the workup of a child with cataract,a detailed history is necessary. It is impor-tant to determine whether the cataract isprogressive, particularly in older children.Contrary to some earlier teaching, we nowknow that bilateral cataracts are often pro-gressive. Frequently, in children from ages3 to 6 and even of high school age, vision isgradually diminished bilaterally because ofprogressive congenital cataracts.
As pointed out by CharlottaZetterstrom, M.D., PhD, of Stockholm,Sweden, in a clinically healthy child, anextensive preoperative evaluation to establishthe cause for the cataract is not routinelynecessary. Congenital cataracts are fre-quently inherited as an autosomal dominanttrait but a recessive inheritance also occurs.

C h a p t e r 12: Cataract Surgery in Complex Cases
349
It is important, to rule out metabolic disor-ders, genetically transmitted syndromes, in-trauterine infections and ocular conditionswith associated anomalies.
Examination
The workup of the congenital cataractpatient continues with the office examina-tion. Infants with congenital cataracts gener-ally resist having their eyes examined, anddo not cooperate with the examining physi-cian. This causes considerable stress in thefamily. The ophthalmologist must use spe-cial examination techniques. First, the lightshould be turned down to low levels ofillumination, which causes the eyes to openimmediately. Direct illumination is used todetermine the extent of the opacity.
The red reflex should first be deter-mined by direct ophthalmoscopy with thepupil undilated. The cataract is often mostdense in the central part of the lens and afterdilatation it seems to be less significant.While the newborn child is awake it is alsoimportant to assess visual function, if pos-sible, with a Teller acuity card. Watch for theability to fix and follow with an object thatattracts attention. Clarify with the parentswhether they have had any visual interactionwith the child.
Children with significant bilateral con-genital cataracts may seem to have delayeddevelopment as well as obviously impairedvisual behavior. Children with monocularcataracts often present with strabismus,which however may not develop until severeirreparable visual loss has occurred. Chil-dren with monocular cataract are almost al-ways detected much later than cases withbilateral cataract. The presence of nystagmus
at the age of 2-3 months generally indicates apoor visual prognosis.
Complete examination of infants withdilated pupils often requires sedation or gen-eral anesthesia and can be performed duringthe same anesthesia as the surgery although,if possible, days before surgery, so that thesurgeon can be better informed to enablehim/her to make adequate decisions, and toinform the parents properly.
Measurement of the corneal diameter,intraocular pressure using a handheld tonom-eter, type and density of the cataract byphotography, are all part of a good examina-tion in these patients. Zetterstrom empha-sizes that when the clarity of the mediapermits, indirect ophthalmoscopy may revealpersistent fetal vessels or other posterior seg-ment abnormalities that may have an impacton the visual outcome. A-scan measurementof the axial length, and keratometer readingsare done. These are essential measurementsfor contact lens and IOL power calculation.Newborn eyes with congenital cataract areshorter and have a smaller corneal diametercompared to controls (Fig. 31 and text pages54-56).
A B-scan ultrasound is also performedin cases in which visualization of the retina isimpossible, in order to determine whetherthere are retinal abnormalities, masses, or thepresence of hypoplastic primary vitreous.Helveston considers it important to deter-mine the intraocular pressure because there isa significant relationship between reducedcorneal diameter, intraocular pressure, andthe presence of glaucoma. One of the mostserious problems in the management of con-genital cataracts, particularly bilateral con-genital cataracts, is the glaucoma that mayoccur 5 to 10 years after successful cataract

THE ART AND THE SCIENCE OF CATARACT SURGERY
350
surgery treatment. This glaucoma resembleschronic simple glaucoma in the adult patient.While the intraocular pressure may showonly a modest increase, glaucoma in childrencan be extremely resistant to successful treat-ment. If not controlled, it can cause the sametype of atrophy in the optic nerve that occursin chronic simple glaucoma.
The Special Case of LamellarCataracts
Saunders, the founder of Moorfield’sEye Hospital, determined 200 years ago thatlamellar cataracts often do not interfere at allor at a rather insignificant level with visualdevelopment. The lamellar cataract lookscentral and quite dense on retroillumination,but is revealed under slit-lamp illuminationas definitely lamellar. Children with lamellarcataracts usually achieve very good vision ifthese cataracts are operated on much later inlife, even late in childhood or the teens ortwenties. Patients do not usually developnystagmus and often achieve normal or nearnormal vision. The corollary is that there isno need to operate on these children in earlyinfancy. The prognosis is better if operatedwhen older, when visual development iscomplete. An accurate calculation of IOLpower can be made, with a better visualresult.
In his clinical research, Rice observedthat in many children with lamellar cataracts,if ophthalmoscopy is undertaken even with areasonably dilated pupil, the view of thefundus is often extremely obscured; in fact,there may not even be any red reflex. If eyesare examined fully, however, it can alwaysbe seen that there is clear cortex. If there is areasonable view of the peripheral fundus
through the peripheral lens, there is no indi-cation for precipitous and early surgery.Such cases can be treated very conserva-tively.
These patients often have vision suffi-ciently reduced in primary and early second-ary school years to benefit from cataractremoval and IOL implantation between ages5 and 15 or even a little earlier.
Rubella Cataracts
These cataracts used to be an importantsource of blindness. Rubella cataracts tend tobe bilateral and progressive and result in amembranous type of partially resolved cata-ract, posterior synechiae, and chronic uveitis.For the past 25 years, since rubella immuni-zation has been available, rubella cataractshave been virtually nonexistent. The keypoint in managing these rubella cataracts isnot to aspirate them incompletely becauseeventually the eyes are lost. The process ofaspiration reactivates the virus.
The Need for Close Monitoring
These children should be closely moni-tored. This includes evaluating visual devel-opment to be sure it is proceeding in asatisfactory manner. The surgeon’s responsi-bility is to both nurture the process of sightand to help prevent amblyopia. Otherwise,the outcome will be poor because of insuffi-cient attention to the anti-amblyopia treat-ment.
Preoperative Considerations
The most important relates to the cal-culation and selection of the type of IOL to

C h a p t e r 12: Cataract Surgery in Complex Cases
351
be used and its correct power. The methodand the considerations relating to IOL powercalculation in pediatric cataracts is amply andclearly presented in pages 54, 55, 56 and Fig.31, page 56.
The Decision to Implant IOL’sin Children with CataractSurgery
How to optically correct patients withbilateral congenital cataracts and monocularcongenital cataract has been a major subjectof controversy for many years. Some distin-guished ophthalmic surgeons 20 years agowere strongly against performing surgery inmonocular congenital cataract followed bytreatment of amblyopia with a contact lens.Visual results were so bad that children withthis problem must be amblyopic by nature,they thought, and the psychological damageto the children and the parents by forcingsuch treatment was to be condemned.
Surgery of bilateral congenital cata-racts at a very early age followed by correc-tion with spectacles and sometimes withcontact lenses usually ended with no betterthan 20/60 vision bilaterally. This was againa source for the belief that congenital cata-racts either unilateral or bilateral were bynature associated with amblyopia, profoundin cases of monocular cases and fairly strongin bilateral cataracts.
When posterior chamber IOL implanta-tion in adults became established as theprocedure of choice, strong influences withinophthalmology were adamantly opposed totheir use in children for the following rea-sons: 1) the eye grows in length with conse-quent significant change in refraction. It wasconsidered impossible to predict such change
and consequently, the accurate IOL poweradequate for each child. 2) There wasopacification of the posterior capsule in mostcases. This required a second operation forposterior capsulotomy and the presence of anIOL would impede proper surgical maneu-vers.
The situation has now significantlychanged. The previous failures with spec-tacles and contact lenses, the new develop-ments in technology and surgical techniquesand the fresh insight of surgeons of a newgeneration have led us to discard the previousthinking and to consider the implantation ofposterior chamber IOL’s a very positive de-velopment in children. This has been madepossible by the following developments: 1)new medications that effectively prevent and/or control inflammation. 2) The introductionof posterior capsule capsulorhexis byGimbel in North America promptly fol-lowed by Everardo Barojas in Mexico andLatin America (Fig. 30). 3) High viscosityviscoelastics to facilitate intraocular surgeryin smaller eyes. 4) New, more appropriateIOL’s for children and implantation in thecapsular bag. 5) Refined technology thatleads to a more precise calculation of the IOLpower.
A «Major» Controversy No More
The controversy as to whether to im-plant IOL’s or not in the management ofcataract surgery in children has been almostresolved. At present, most surgeons placeintraocular lenses, whether treating congeni-tal cataracts or traumatic cataracts, followingevidence that they can be safely tolerated inmost children. The informed consent discus-sion with the parent or guardian, however,should include the fact that intraocular lenses

THE ART AND THE SCIENCE OF CATARACT SURGERY
352
have still not been approved by the FDA foruse in children. This is a matter of particularimportance in the U.S.
The previously existing controversy ofthe timing of the IOL implantation in chil-dren has also been resolved as a conse-quence of experience. Intraocular lens im-plantation may be significantly easier at thetime of cataract extraction than at a later date,since iridocapsular adhesions and fusion ofthe anterior and posterior capsular flaps makea subsequent secondary implant proceduremore challenging.
Surgical Technique
The Incision
A sclero-corneal tunnel 3.5 to 3.8 mmwide is the procedure of choice (Fig. 40-B).Manage the conjunctiva very carefully incase the patient develops secondary glaucomalater in life. Because the sclera is soft andelastic in children, it is hard to achieve a self-sealing incision. Consequently, the incisionshould be sutured.
The Anterior Chamber and Pupil
High-viscosity viscoelastic material isused because the anterior chamber is shallowin these small eyes. If the pupil is small,stretching the pupil with flexible iris retrac-tors (Alcon-Grieshaber) can be very helpful(Fig. 198). They are placed before the con-tinuous anterior capsulorhexis is performed.
Anterior Capsulorhexis
This is an important step to assure inthe bag placement of the IOL. Its size shouldbe smaller than the IOL optic. Zetterstrom
points out that the anterior capsule is thickand elastic in children and a capsular tear caneasily extend out to the equator.
A central puncture is made with a cysto-tome and the leading edge of the capsule isgrasped with forceps. Several repeatedgrasps are recommended to avoid extensionto the equator and to assure maximal control.The capsulorhexis should be kept small be-cause it usually enlarges due to the inherentelasticity of the capsule. (See figures 97, 98,99, 100 for CCC with cystotome and 45, 46with forceps).
Nucleus Removal
After an appropriate hydrodissection,the removal of the nucleus and cortex in themajority of cases can be performed using anI/A probe with a 0.5 mm orifice, because forthe most part the congenital cataract is usu-ally very soft. Occasionally the cataract ishard and has to be disassembled and re-moved. All the lens cortical material must beaspirated in order to reduce postoperativeinflammation (Fig. 128, page 206). Prolifera-tion of cells leading to a secondary cataractformation is more aggressive in the youngerchild.
Posterior Capsulorhexis
In children a posterior capsulorhexiscombined with an anterior vitrectomy arenecessary to produce a clear optical axis andreduce the need for a secondary operation.The diameter of the posterior capsulorhexismust be at least 3.5 to 4.0 mm or it will tendto close. Moreover, the anterior and poste-rior capsules must be separated with the useof additional viscoelastic. This maneuverwill push the vitreous back and prevent its

C h a p t e r 12: Cataract Surgery in Complex Cases
353
prolapse into the anterior chamber (Fig. 211).Posterior capsulorhexis is performed by mostsurgeons before IOL implantation, as pre-sented here. Nevertheless, some surgeons doit after IOL implantation, as shown in Fig. 30,page 52. The latter procedure may be cum-bersome.
Anterior Vitrectomy
This important step is performed aftercompleting posterior capsulorhexis and aimsat removing 1/3 of the anterior vitreous gelbefore there is any vitreous presentation. It is
performed using a vitrectomy probe, asshown in Fig. 212. Special care should begiven to removing any vitreous present in theanterior chamber. A so-called “dry” vitrec-tomy, without infusion of fluid, is safelyperformed between the anterior and posteriorcapsulorhexis. Viscoelastic is removed toavoid elevated intraocular pressure after sur-gery.
Using this method it is possible to im-plant an IOL in the capsular bag duringprimary surgery or in the ciliary sulcus if asecondary implantation is scheduled in thefuture.
Figure 211: Cataract Surgery in Children - Importance of Posterior Capsulorhexis
When the capsular bag is empty of all lens material, viscoelastic is injected to fill thecapsular bag and a posterior continuous capsulorhexis (P) is performed, always smaller than theanterior capsulorhexis (A). A combination of cystotome first followed by forceps is the techniquepreferred by most surgeons. High viscosity viscoelastic (V) is injected to separate both capsulesand to keep the vitreous out of the way.

THE ART AND THE SCIENCE OF CATARACT SURGERY
354
IOL Implantation
Primary IOL implantation into the cap-sular bag is the procedure of choice. The riskof contact with vascular tissue and the possi-bility of inducing chronic inflammation isreduced as compared with implantation in thesulcus. For IOL implantation it is importantto extend the incision to 3.5 or 3.8 mm tofacilitate the implantation of a foldableacrylic IOL. Viscoelastic is injected betweenthe anterior and posterior capsules to separatethem. The acrylic lens is folded and insertedby the same technique used in the adult eye(Fig. 213).
Figure 212 (above): Cataract Surgery in Children- Anterior Vitrectomy
With the anterior chamber filled with vis-coelastic an anterior dry (that is, without infusion)vitrectomy is performed to avoid vitreous (V) rem-nants in the anterior chamber. This step should helpeliminate any vitreous gel in the anterior chamberand near the posterior capsule. The vitrectomyprobe (B) is inserted under the anteriorcapsulorhexis (A) and at the margin of the posteriorcapsulorhexis (P), always with the tip facing up,taking care not to touch any one of both capsules.This maneuver is preferably performed before theIOL implantation.
Figure 213 (right): Cataract Surgery in Chil-dren - Intraocular Lens Implantation
The anterior chamber and capsular bag arefilled with viscoelastic. IOL (L) implantationwithin the capsular bag is the procedure of choice.It is important to use an acrylic lens. Anteriorcapsule (A). Posterior capsule (P).

C h a p t e r 12: Cataract Surgery in Complex Cases
355
The Posterior Approach toCataract Extraction in Children
This has become a second option, andcertainly not the procedure of choice. Withsignificant advances in cataract removal inchildren through the anterior approach, thetwo or three port pars plana vitrectomy withremoval of the posterior capsule and lensmaterial and IOL fixation in the sulcus is leftfor cases in which a vitreoretinal operation isrequired as the primary procedure. This is therealm of the vitreoretinal surgeon. The ante-rior segment surgeon feels uncomfortablewith this approach particularly when the tech-nique done through the anterior segment isnow so effective and the main controversiesrelated to this surgery are almost a problem ofthe past.
CATARACT SURGERYIN UVEITIS
This is, indeed, one of the most delicateand complex situations in cataract surgery. Inthis volume it is fully discussed in pages 31-33 and Fig. 22 (Chapter 2).
BIBLIOGRAPHY
Alio JL, Chipont E: Cataract surgery in patientswith uveitis. Cataract Surgery in Complicated Casesby Buratto, 2000; 15:193-206.
Belfort Jr., R: Cataract surgery in patients withuveitis. Highlights of Ophthalmology Bi-MonthlyJournal, Vol. 27, Nº 4, 1999.
Buzard K, Lindstrom RL: Refractive cataract sur-gery. Highlights of Ophthalmology Bi-MonthlyLetter. 1994; Vol. 22, Nº 11-12, pp. 111-116.
Centurion V, Lacava AC, De Lucca ES, Barbosa R:High myopia and cataract. Faco Total by VirgilioCenturion.
Colvard DM, Kratz RP: Cataract surgery utilizingthe erbium laser. In: Fine IH, ed.Phacoemulsification: New Technology and Clini-cal Application (Thorofare, NJ: Slack, 1996),161-80.
Dodick, JM: YAG laser phacolysis in new cataracttechniques. Boyd’s World Atlas Series of Ophthal-mic Surgery of HIGHLIGHTS, 1995; 5-130-131.
Dodick, JM, Christian J: Experimental studies onthe development and propagation of shoch wavescreated by the interaction of short Nd:YAG laserpulses with a titanium target: possible implica-tions for Nd:YAG laser phacolysis of thecataractous human lens. J Cataract Refract Surg1991; 17:794-7.
Fenzl RE, Gills III JP, Gills JP: Piggybackintraocular lens implantation. Current Opinion inOphthalmology, Feb. 2000, Vol. 11, Nº 1.
Kershner RM: Refractive cataract surgery. CurrentOpinion in Ophthalmology, Feb. 1998, Vol. 9, Nº 1.

THE ART AND THE SCIENCE OF CATARACT SURGERY
356
Khater TT, Koch DD: Pediatric cataracts. CurrentOpinion in Ophthalmology, Feb. 1998, Vol. 9 Nº 1.
Koch DD, Lindstrom RL: Controlling astigmatismin cataract surgery. Seminars in Ophthalmology,December 1992; Vol. 7, Nº 4 pp 224-233.
Lacava AC, Sanchez JC, Centurion V: High hyper-opia, cataract, polipseudophakic or piggyback, FacoTotal by Virgilio Centurion.
Management of aphakia in childhood. Focal Points,American Academy of Ophthalmology, nMarch1999 (3 Sections) Vol. XVII, Nº 1.
Neto Murta J, Quadrado M: Pediatric lens implan-tation: technique and results. Atlas of CataractSurgery, Edited by Masket S. & Crandall AS,published by Martin Dunitz Ltd., 1999, 33:291-300.
Zetterstrom C.: Cataract surgery in the pediatriceye. Cataract Surgery in Complicated Cases byBuratto, 2000; 1:1-14.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
359
Overview
Although phacoemulsificationfollowed by implantation of a foldable IOL isthe “state of the art” technique and theoperation of choice for many surgeons andpatients, planned extracapsular extractionwith an 8 mm incision and implantation of arigid posterior chamber IOL is still used for avast number of patients.
As a matter of fact, if we consider theday-to-day practice as performed by the ma-jority of clinical ophthalmologists world-wide, planned extracapsular technique with a8 mm incision and posterior chamber, in-the-bag implantation of a rigid PMMA lens orsome other type of manual extracapsularcontinue to be: 1) the cataract surgical proce-dure performed on the largest number ofpatients who undergo cataract surgery; 2) thesurgical technique done by the majority ofclinical ophthalmologists throughout theworld regardless of whether they are techni-cally able to do phacoemulsification.
There are many first class surgeons whocan perform a superior quality phacoemulsifi-cation but for a large number of patients theyneed to do manual ECCE. This is particularlytrue in less economically advanced societies.
A good example of this situation is theexperience of Everardo Barojas, M.D.,from Mexico, one of Latin America’s mostrespected ophthalmic surgeons and teachers.He performs a first class phacoemulsificationand teaches the technique to his residents.But in his extensive work with patients in the
THE PRESENT ROLE OFMANUAL EXTRACAPSULARS
rural communities which he spontaneouslyserves, he does the “envelope extracapsulartechnique” initiated in the 1960’s by Baikoffand revived in 1982 by Galand. All hisresidents learn how to perform the plannedextracapsular with 8 mm incision, the enve-lope extracapsular, as well as phacoemulsifi-cation.
Barojas and collaborators have se-lected the “envelope extracapsular” proce-dure for rehabilitation of large numbers ofpatients at a time considering cost, time ittakes, safety and good results.
Advances in Manual Extracap-sular
In the past few years, the technique ofplanned ECCE has progressively andsubstantially improved. In addition, smallincision or medium-small incision manualextracapsulars have stimulated the interest ofa good number of clinical ophthalmologists indifferent regions who have chosen to do thesemanual techniques instead of undergoing thelearning process of phacoemulsification eventhough some of these “small incision” manualextracapsulars are not easy to do. Thesetechniques are presented in this Chapter.
Advances in extracapsular surgery arerelated to better instruments, viscoelastics,the application of nuclear fragmentation tech-niques, advances in IOL technology, irrigat-ing solutions and the methods to minimizeinfection and postoperative inflammation aspresented in Chapter 4 of this Volume. The

THE ART AND THE SCIENCE OF CATARACT SURGERY
360
application of these advances is a long stepforward for manual extracapsular as well asphacoemulsification, which is a mechanicalextracapsular. As a matter of fact, a goodnumber of steps used in phacoemulsification,such as continuous circular capsulorhexishave been incorporated into the modernmethods of ECCE. All of these factors makemanual extracapsular a very good operation.The essential difference with phaco regardingresults is that with a very well done phaco andtopical anesthesia the patient has almost im-mediate visual rehabilitation and minimal in-flammation, in contrast to a very well per-formed ECCE in which final visual recoverymay take 6-8 weeks, although the visualacuity is practically the same at the end of thisperiod. There may also be more inflamma-tion with ECCE.
Regional Predominance ofPhacoemulsification
Phacoemulsification is predominant es-sentially in the U.S. and Western Europe,where it has become the number one tech-nique for most ophthalmic surgeons. Inmany instances, this is because their patientsdemand and expect a very rapid visual reha-bilitation and have the economic means toreceive the benefit of the high technologyrequired for phaco. In other geographicalregions, phacoemulsification continues togain ground, but essentially in teaching cen-ters and private practice.
Because manual planned ECCE is stillextensively used, we have selected ProfessorJoaquin Barraquer, M.D., from Barcelonato present his technique of a flawless plannedextracapsular. There is no one better suitedfor this task.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
361
EDITOR’S NOTE:
Professor Joaquin Barraquer is one of the world’s top master surgeons. He wasone of the key pioneers of ophthalmic surgery under the microscope which led to thedevelopment of microsurgery. The ASCRS selected him as “one of the world`s mostoutstanding innovators.” The III International Congress on Advances in Ophthalmol-ogy, 2000 declared him “Ophthalmologist of the Millennium.”
PERFORMING A FLAWLESS
PLANNED EXTRACAPSULAR CATARACT EXTRACTION
With an 8 mm Incision and
Posterior Chamber IOL Implantation
by Professor Joaquin Barraquer, M.D., F.A.C.S.
ANESTHESIA
At the Barraquer Ophthalmology Cen-ter in Barcelona, we continue to find generalanesthesia administered by an expert anesthe-siologist the procedure of choice even withambulatory surgery. With this type of anes-thesia, the surgeon does not need to dependon the cooperation of the patient. Hypotonyof the eye is excellent. The surgeon canperform the complete procedure with opti-mum control and safety.
Nevertheless, because many eye cen-ters and clinical ophthalmologists throughoutthe world routinely use local anesthesia, bothtechniques are here described.
General Anesthesia(as Performed at the BarraquerOphthalmology Center)
Pre-induction
Midazolam (1-5 mg, intravenous,anxiolytic).
Induction
Propophyl (1-3 mg/kg, intravenous, hypnotic)Succinylcholine (1 mg/kg, intravenous, mus-cular relaxant for orotracheal intubation).

THE ART AND THE SCIENCE OF CATARACT SURGERY
362
Adjunct Medications
Analgesics: alfentanil (0.5-1.0 mg) orpentazocine (15-30 mg) intravenous.
Neuroleptics: droperidol (2.5-5.0 mg,intravenous)
Vagolyptics: atropine (0.5-1.0 mg, in-travenous)
Curare: atracurium besylate (0.25-0.50 mg, intravenous as muscle relaxant)
Antiemetics: ondansetron (4 mg) and/ormetoclopramide (10 mg) intravenous.
Maintenance
Halogenated ethers for inhalation anes-thesia (sevoflurane or isoflurane), occasion-ally complemented by nitrogen protoxide(N
2O) 50%.
Ventilation
Spontaneous respiration, if possible,depending on the type of patient and surgery.Assisted or controlled ventilation if neces-sary.
Monitoring
Electrocardiogram (EKG)Pulsioximetry (Oxygen saturation)Non-invasive blood pressure (NIBP)
every 3 minutes.Capnography (expired CO
2) and respi-
ratory frequency.Muscular relaxation.
Awakening and Recovery
Oxygenation 100% and control of vitalsigns. Cholinesterase inhibitors (neostig-mine and/or edrophonium) if curare has beenused.
Local Anesthesia
With this type of anesthesia very goodhypotony and akinesia can be achieved. Ifsedation is adequate but not excessive, mini-mal patient cooperation will be sufficient.Barraquer believes an expert anesthesiologistshould always be available to ensure that thepatient is controlled, even if local anesthesiais used.
Sedation
Propophyl, alfentanil, midazolam. Thedosage depends upon the patient’s weightand age.
The patient should be oxygenated dur-ing the anesthetic and surgical procedurebecause sedation causes respiratory depres-sion.
Peribulbar Injection
Two injections are administered: Ante-equa-tor injection - Inferotemporal Site.
1. An inferotemporal injection at the inter-section of the temporal lateral third andthe two medial thirds of the inferior orbit,just anterior to the equator (Fig. 214). A23 gauge needle 25 mm long is used.
2. A superonasal injection (Fig. 215). A 25gauge needle 16 mm long is used.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
363
Figure 214 (right): Peribulbar LocalAnesthesia
Inferotemporal injection anterior to theequator. The needle is advanced justanterior to the equator of the globe, alongthe inferior orbit, but not into the musclecone. The anesthetic solution is injectedat this site. The beveled side of the needletip is directed toward the globe.
Figure 215 (left): Peribulbar Post-equatorSuperonasal Injection.
The needle is directed posteriorlybehind the globe outside the muscle conetoward the area of the superior orbital fis-sure. The anesthetic solution is injected justpast the equator.

THE ART AND THE SCIENCE OF CATARACT SURGERY
364
Technique for PeribulbarInjection
First, the inferior temporal rim of theorbit is identified by palpation, and the eye-ball is displaced with the finger. The needle isalways introduced in the direction of the orbituntil it touches bone. At this point the needleis lowered, following the rim of the bone.Three to 4 cc of local anesthesia are injected.Then the same maneuver is performed at thesuperior nasal point. Massage is applied to theglobe for a few seconds. A Honan balloon isplaced over the globe with a pressure of about40 mm for 5 to 10 minutes (Fig. 96).
Anesthetic Medications
5 cc lidocaine 2%, plus 5 cc buvicaine0.75%, plus hyaluronidase 100 UI plusadrenaline 1:200 000 (3 to 4 cc in the injec-tion inferiorly and 3 to 4 cc in the injectionsuperiorly. This combination lasts for almost2 hours).
Monitoring
Electrocardiogram (EKG)Pulsioximetry (Oxygen saturation)Non-invasive blood pressure (NIBP)
every 3 minutes.Muscular relaxation
Extracapsular CataractExtraction with an 8 mmIncision (ECCE)
At the beginning of the operation, thepupil must be adequately dilated (8mm ormore. We use cyclopegics and tropicamideevery 30 minutes, beginning 3 hours beforesurgery. Diclophenac is added to reduce thetendency for the surgical maneuvers to causepupillary constriction. Atropine is not recom-mended because we want prompt recupera-tion of normal pupillary reaction the first dayafter surgery.
Incision
A traction suture is applied in the supe-rior rectus muscle. A fornix-based conjuncti-val flap is prepared. The conjunctiva is sepa-rated at the limbus either with a razorbladeknife or with Wescott scissors. If the scissorsare used, the dissection is completed with thesame scissors.
Light bipolar diathermy is used to co-agulate the bleeding vessels, especially in theanterior part of the sclera and at the sclerocor-neal limbus, where the incision will be madeto extract the nucleus and to introduce theIOL.
An 8 mm-groove is made approxi-mately 0.5 mm from the limbus with a dia-

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
365
mond knife, a Desmarres scarifier, a dispos-able knife, or a razorblade knife. The depth ofthe groove is approximately two-thirds of thescleral thickness and represents the first stepof a two-plane incision to be completed later.This two-plane incision facilitates better ap-position of the wound edges, thereby improv-ing wound closure and reducing postopera-tive astigmatism induced by the sutures. Thesurgeon should avoid overlapping thewound edges. (Fig 216).
Continuous CurvilinearCapsulorhexis
A viscoelastic substance is introducedin the anterior chamber through a paracente-sis (Fig. 217) to maintain adequate depth andto facilitate the deep, horizontal incision (sec-ond step) and anterior capsulorrhexis. Thehorizontal incision is started with a dispos-able knife at one of the ends of the predeter-mined groove and continued over approxi-
Figure 216: Incision - Stage 1
A non-penetrating perpendicular incision is performed 0.5 mm behindthe limbus with a diamond blade knife (K). The incision extends from 2 to 10o’clock (arrow) for a length of 8 mm. This is the first plane of the two-planeincision A paracentesis is made at the limbus (A.) To simplify Figures 216and 217, the fornix-based conjunctival flap has not been represented in theseillustrations.

THE ART AND THE SCIENCE OF CATARACT SURGERY
366
mately 3 mm (Fig. 217). After thecapsulorrhexis has been done, as shownin Fig. 219 A, B and C, the deep plane ofthe incision is completed with scissors(Fig. 218). Care must be taken to ensure that
Figure 217 (above): Incision - Stage 2
A viscoelastic substance is injected with acannula through a paracentesis to fill the anteriorchamber. This will maintain the anterior chamberdepth and increase dilation of the pupil. At one endof the non-penetrating limbal incision, a horizontalbeveled incision is made (D). This will begin thesecond plane of the two-plane incision. Fixationforceps (F).
Figure 218 (below): Incision - Stage 3
The two-plane horizontal beveled inci-sion is completed (red arrow) with Barraquer’sscissors (S) in the deep layers of the groove.
the lid speculum does not exert pressure onthe eye, which might induce protrusion orrupture of the posterior capsule.
The capsulorrhexis can be performedby perforating the center of the capsule with a

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
367
needle, or cystotome, which is an insulininjection needle, conveniently bent near itsbase to produce adequate angulation for bet-ter maneuvering (Fig. 97). The bend close tothe tip of the needle makes a little hook usedto exert traction on the capsule fragment.Cystotomes are also available commercially.Another way of performing a capsulorrhexisis to tear the central part of the anterior
capsule with adequate forceps such as Uttrataforceps. We usually prefer the forceps to thecystotome (Fig. 219 A, B,C).
Once the center of the capsule has beenruptured or torn, a small flap of capsulartissue is grasped and pulled in either a clock-wise or counterclockwise direction to elimi-nate the central part of the anterior capsule(Fig. 219 A,B,C). We attempt to create a
Figure 219 A-C: The Continuous Curvilinear Anterior Capsulorhexis Technique - Stages 1 - 3
(A) After the tear is started in the center of the anterior capsule, traction is exerted at the 10:00meridian (X) on the operculum that is doubled on itself. Uttrata forceps (N) are used to grasp the underside ofthe capsular flap (C) and the tear is extended in a counterclockwise direction (blue arrow) to produce acircumferential capsular rupture (red arrow). (B) The tear is continued with the Uttrata forceps in the samedirection (blue arrow) to complete the circular tear (red arrow). (C)The capsulorrhexis is completed, and thecircular operculum is removed.

THE ART AND THE SCIENCE OF CATARACT SURGERY
368
circular opening 5.5mm to 6 mm in diameter(Fig. 220). In cases of very large nuclei, ofcapsular pseudoexfoliation, or when somephacodonesis is present, we prefer to con-struct a capsulorrhexis with a slightly largerdiameter in order to avoid traction on thezonules when the nucleus is brought into theanterior chamber. In these cases a largecapsulorrhexis facilitates mobilization and ro-tation of the nucleus (Fig. 221).
Figure 220 (above): Continuous Cur-vilinear Anterior Capsulorrhexis -Standard Size
The regular curve of the capsu-lar opening is less prone to radial tearsthan the irregular edges of the openingthat result form the can-opener and en-velope techniques.
Figure 221 (below): Large ContinuousCurvilinear Anterior Capsulorrhexis
This illustration depicts a largeCCC, adequate for removing a large and/orhard nucleus.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
369
Hydrodissection
Next is the hydrodissection. Balancedsaline solution (BSS+) with epinephrine (di-lution 0.06%) is injected with a thin cannula(25 G) between the anterior capsule and thelens cortex (Fig. 222) to separate the nucleus,which tends to pass through thecapsulorrhexis into the anterior chamber.
Subsequently, the nucleus is rotated with thesame cannula in clockwise or counterclock-wise direction, depending on where thenucleus has entered the anterior chamber. Thenucleus is lifted slightly during the rotationmaneuver to complete the displacement intothe anterior chamber (Figs. 223, 224). As thecapsule is an elastic structure, even largenuclei can pass through a relatively small
Figure 222 (left): Hydrodissection of the LensCapsule from the Cortex - Stage 1
After the continuous curvilinear anteriorcapsulorrhexis has been completed, a cannula (C)is inserted in the anterior chamber. The tip of thecannula is placed between the anterior capsuleand the lens cortex at the locations represented.Fluid is injected (arrows) at these locations toseparate the capsule from the cortex. The result-ing fluid waves can be seen (W). These wavescontinue posteriorly to separate the posterior cap-sule form the cortex.
Figure 223 (right): Hydrodissection - Stage 2
A 25 gauge needle (A) is introduced paral-lel to the edge of the nucleus (N), and a solution ofBSS+ and epinephrine is injected. This hydraulicforce (arrow) produces a cleavage plane betweenthe posterior capsule and the posterior surface ofthe nucleus. The nucleus passes into the anteriorchamber without tearing the capsulorrhexis.

THE ART AND THE SCIENCE OF CATARACT SURGERY
370
capsulorrhexis without tearing the capsulewhen a continuous circular capsulotomywithout notches is performed.
Other methods of opening the capsuleare: 1) the envelope technique, which uses amore or less straight incision between thecentral and superior third. 2) The can-openertechnique produces small, less circular cap-sule ruptures. These techniques, which arebased on lineal incisions, however, may resultin a higher incidence of rupture or tearing ofthe posterior capsule during the cleaning ma-neuvers of the capsular bag.
Removal of Nucleus
Once the nucleus has passed into theanterior chamber, gentle compression is ap-plied 1mm to 2mm from the inferior limbus(Fig. 224) with a round-tipped or blunt instru-ment. The nucleus is displaced upwards(Fig. 224), resulting in some gaping of theincision. Simultaneously, the scleral lip of theincision is depressed with another instrumentsuch as Colibri or Adson forceps to facilitatethe expulsion of the nucleus (Fig. 224). Ex-pression of the nucleus should never be at-tempted while the nucleus is still inside thecapsular bag because zonular rupture mayoccur, necessitating the continuation of sur-gery as an unplanned intracapsular extraction.
Removal of Cortex - Irrigationand Aspiration
The anterior chamber is irrigated withBSS+ and epinephrine (0.06% dilution) toremove persistent residual lens matter or epi-nuclear elements. A nylon 10-0 cross suture isapplied in the central part of the incision to
maintain adequate anterior chamber depthduring irrigation and aspiration of the cortexthat remains adherent to the capsular bag. Anaspiration probe with a 0.3mm opening at thetip is used. This probe has a special coverwith two lateral openings at the inferior endfor irrigation to maintain the anterior chamberdepth while the cortical lens matter is aspi-rated (Fig. 225). The height of the bottle isadjusted from 20cm to 78cm to increase orreduce the irrigation in relation to the depth ofthe chamber. An adequate chamber depthmakes it possible to work with greater safety,although excessive irrigation may result iniris prolapse through the wound. This can becorrected by reducing the height of the bottle.For aspiration of the lens matter, a variablevacuum with an upper limit of 450mmHg isapplied.
Once all the lens matter has been re-moved, the anterior capsule is “polished”using the same probe and a low vacuumpower between 20mmHg and 60mmHg toavoid capsular retraction and rupture. Care-ful, exhaustive cleaning of most of the poste-rior capsule surface is essential in order topostpone as long as possible the opacificationof the capsule and the subsequent Nd: YAGlaser capsulotomy. The surgeon must be care-ful not to be aggressive during this step ofaspiration-irrigation of the cortex so as toavoid posterior capsule rupture or zonulesrupture during these maneuvers. If this shouldoccur, vitrectomy would be required, and theIOL would have to be placed in the sulcus.
If irrigation-aspiration equipment is notavailable, the lens matter can be removedmanually. A cannula and syringe are used togently irrigate, mobilize the lens matter, andaspirate it in the four quadrants. A curved

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
371
Figure 224 (left): Removal ofNucleus
Once the nucleus is in the an-terior chamber, nucleoexpression isperformed. Slight compression is ex-erted with a blunt instrument 1 or2mm over the inferior limbus (H). thenucleus is displaced upwards, separat-ing the lips of the incision. Simulta-neously, another instrument (F) is usedto depress the scleral lip of the incisionin order to facilitate the expulsion ofthe nucleus.
Figure 225 (right): Removal of theResidual Cortex
The aspiration probe has anopening 0.3 mm in diameter at theupper end. It also has a cover or sleevewith two inferior lateral openings forirrigation to maintain the depth of theanterior chamber during aspiration ofthe lens matter.

THE ART AND THE SCIENCE OF CATARACT SURGERY
372
probe tip is used for the superior quadrants(Fig. 226). The posterior capsule may also bepolished manually using this technique at theend of the procedure. In cases of centralcapsular fibrosis, posterior capsulorrhexis canbe performed at the end of the procedure or ata later stage in a Nd: YAG laser capsulotomy.
A viscoelastic is injected in the capsularbag and the anterior chamber. The surgeonshould check carefully to ensure that thecapsular bag is completely filled with vis-coelastic. The preplaced cross-point suture isremoved from the wound.
IOL Implantation
The lens is grasped at the superior rimof the optics with straight forceps. With aslight inclination, the inferior haptic is intro-duced into the capsular bag (Fig. 227). Theoptic is centered with the capsulorrhexis androtated using a Sinskey hook until the supe-rior haptic is in the correct position inside thebag. The IOL should be implanted horizon-tally. Introduction of the superior haptic maybe easier if it is grasped with thin forcepswithout teeth (Fig. 228). The haptic is guided
Figure 226: Irrigation/Aspiration of the Residual Cortex (modification by Malbran).
The residual cortex (C) is removed from the capsular bag with a curved irrigation/aspiration probe. A slightly curved tip is used to gently aspirate the residual cortex nasallyand temporally. The residual cortex located in the difficult-to-reach areas of the superiorcapsular bag is removed using a curved irrigation/aspiration probe tip.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
373
Figure 227 (left): Intraocular Lens Implanta-tion.
After the cataract is removed and vis-coelastic is injected into the anterior chamber andthe capsular bag, the PMMA (L) lens is graspedwith forceps (F). The inferior haptic (H) is placedin the capsular bag (C) inferiorly. Forceps areused to introduce the optic part into the capsularbag.
Figure 228 (right): IOL Implantation
The superior haptic (H) is graspedwith straight forceps and bent inferiorly (redarrow) so that the elbow of the haptic can bedirected (blue arrow) into the capsular bag(C) superiorly.

THE ART AND THE SCIENCE OF CATARACT SURGERY
374
toward the center of the capsulorrhexis androtated 90 degrees. The forceps are removedfrom the capsulorrhexis, and the IOL settlesin the capsular bag. The capsulorrhexis isclearly seen in front of the optic part of theIOL (Fig. 229). Generally, PMMA lenses areused, and the preferred diameter of the opticis 6.5 mm.
Acetylcholine 1% is applied to induce4 mm of miosis. Subsequently, a peripheraliridectomy is performed.
Suturing and Aspiration of theViscoelastic
The incision is closed with 5 to 7 nylonradial sutures. The knots must be buried in thesclera (Fig. 229).
The viscoelastic material is aspirated.The anterior chamber is restored to normaldepth with 1% acetylcholine (lyophilized ace-tylcholine dissolved in BSS) The conjuncti-val flap is repositioned to cover the incision.The two extremities of the flap are anchoredwith 10-0 nylon sutures.
Figure 229: Conclusion of the Operation
Cross-sectional view. The IOL occu-pies its normal position within the capsularbag. The incision is sutured with 10-0 nylon,preferably radial sutures, and the knots areburied in the sclera. The fornix-based con-junctival flap is repositioned to cover thewound. The flap is anchored with 10-0 nylonsutures at the two ends of the incision (notshown in this illustration).

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
375
THE MANUAL, SMALL INCISIONEXTRACAPSULARS
There is a significant learning curve, andexperience is required.
The proposed Mini-Nuc technique mustbe performed under positive intraocular pres-sure during all stages of surgery. The desiredIOP is achieved during surgery with the useof an anterior chamber maintaining system,and controlled by the height of the BSS bottle(Anterior Chamber Mainteiner (ACM) inFig. 230).
Importance of ConstantIrrigation and Positive 100% IOP
The principle of maintaining positiveIOP during cataract surgery is graduallybecoming acceptable to more surgeons, eventhose performing phacoemulsification. In themini-nuc technique, positive IOP exists 100%of the operating time. Any fluid lost duringintraoperative maneuvers is promptly recov-ered because of the large internal diameter ofthe ACM tubing (“A” in Figs. 230-231). Thesteady flow ensures a constant depth of theanterior chamber. This flow continuouslywashes all debris: blood, pigment, and left-over cortical material from the eye with lowturbulence and low fluctuation of anteriorchamber depth. Consequently, less postop-erative inflammatory reaction occurs.
There is significant interest about thesemethods. They allow successful removal ofthe cataract through a small incision andmanually, without the need to use mecha-nized equipment.
We hereby present the three mostwidely accepted: 1) Michael Blumenthal’sMini-Nuc (Israel); 2) David McIntyre’sPhaco Section (USA); and 3) FranciscoGutierrez C., Manual Phacofragmentation.
THE MINI-NUC TECHNIQUE
This procedure caught-on in the mindsof many clinical ophthalmologists since itsinception, 10 years ago. Blumenthal hascontinuously worked at improving themethod he created and its results.
Principles of the Mini-NucTechnique
The procedure requires only a smallincision and no stitches. It has proven to besafe surgery. It is possible to use topicalanesthesia, and rehabilitation is speedy.Moreover, it is cost-effective. There are somedisadvantages, however, of manual ECCE. Itis not an easy technique to learn and perform.

THE ART AND THE SCIENCE OF CATARACT SURGERY
376
The BSS bottle can be used as a reser-voir of pharmacological drugs to be infusedcontinuously into the eye. These drugs mayinclude adrenaline 1:1,000,000, to keep thepupil dilated, antibiotics, and any other drugthe surgeon wishes to use. The length ofsurgery is not critical as the constant positiveIOP keeps the aqueous blood barrier intact;and the ciliary processes and choroidal,retinal, and iris vessels are not exposed to ahypotonic environment at any time. Thishelps to prevent exudate formation or aworse complication, expulsive hemorrhage.
Blumenthal considers that positive IOPprovides not only a safe milieu and preventscomplications; it is a precondition for con-trolled surgery. Because the internal architec-ture of the eye is not disturbed, plannedmaneuvers can be carried out safely.
SURGICAL TECHNIQUE
Anesthesia, Paracentesis, ACM
Lidocaine 4% drops are instilled 15minutes before surgery 3-4 times. At presentEsrecain gel is used with each Lidocainedrop. A total of 0.2-0.3 cc of Marcaine 0.5%with adrenaline is injected subconjunctivallybetween 11:00 and 2:00 in the limbal area,where diathermy will be applied. During sur-gery, 0.2-0.3 cc of intraocular non-preservedLidocaine is injected into the tube of theACM. It will reach the eye in diluted form.This is very efficient, cost-effective ocularanesthesia.
Two paracenteses are performed at10:30 and 2:30 by stiletto knife (identified as“D” in Fig. 230). Moderate beveled incisions
are made in clear cornea just at the edge of theblood vessels. The same stiletto knife is usedfor an incision just anterior to the limbus inthe clear cornea for the purpose of inducingthe ACM cannula (5149 oval Visitec) in the6 o'clock area (identified as “A” in Fig. 230).
Paracentesis Incision and Fixa-tion of ACM
The most important aspect of the bev-eled tunnel paracentesis incision to intro-duce the ACM is its length. The incisionshould be at least 2 mm long before the knifepenetrates the AC, and will be 1 mm wide(Fig. 230-A).
The ACM is introduced into the tunnel-shaped paracentesis, beveled edge up. Whenit reaches the AC, it is turned beveled edgedown, and the ACM flow is directed towardsthe iris. The ACM is introduced 2.0 - 2.5 mminto the AC, and not more. The shallower thedepth of the AC, the greater care the surgeonshould take not to exceed these limits. (Inthe illustrations, the cannula is shown beveledup for clarity but at surgery it should be keptbeveled down toward the iris.)
Height of BSS Bottle
Normally, the BSS bottle should belocated 40 to 50 cm above the eye, keepingthe IOP at 30-40 mm Hg. If intraocularbleeding occurs, raising the bottle will stopthe bleeding. If a posterior capsule tear oc-curs, the bottle should be lowered to 20 cm.The BSS bottle should be lowered evenfurther to 10-15 cm when suturing, in orderto achieve the best adaptation of the incisionedges.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
377
The most important concept to keep inmind is that the height of the BSS bottle canbe changed depending upon the situation. Itdoes not need to be standardized, and thesurgeon can adjust it according to his/her owntechnique, and varying needs during surgery.
Capsulorhexis
The ACM and positive IOP push thecrystalline lens backward reducing the forceof the zonules exerting pressure on the ante-rior capsule toward the periphery. This facili-tates capsulorhexis performed by a cysto-tome, and avoids unintended tears toward theperiphery of the crystalline lens. Forceps in-troduced through the paracentesis cornealtunnel produce outflow of BSS thus reduc-
Figure 230: Creation of the Special Sclero-Cor-neal Pocket Tunnel Incision - Stage 1
The Anterior Chamber Maintainer (A) is inplace, introduced through a tunnel in clear corneawhich is at least 2mm in length and 1mm wide, nearand parallel to the limbus. The height of the BSSbottle, connected to the maintainer, controls the in-traocular pressure. Two 1mm paracentesis incisions(D) are made at 10:30 and 2:30 just anterior to thelimbus, for instrument access. The main external in-cision, 0.3mm in depth and 4-5mm long, 1mm be-hind the limbus is made. A crescent knife (C) dis-sects the tunnel, first 1mm in sclera, then 2-3mmforward into clear cornea (1), then extending later-ally (2) to produce the pockets (P) on both sides.While performing the pockets, the crescent knife ifretracted laterally and backward (3), creating theexternal incision extensions (E) on both sides. Inset(F) shows the cross section of a scleral tunnel inci-sion made under low intraocular pressure which iswavy and uneven. Inset (G) shows incision qualitywhich is smooth and even, as achieved under highintraocular pressure from anterior chamber main-taining system.
ing the AC depth and causing the zonules topull the anterior capsule more forcefully.Blumenthal believes that althoughcapsulorhexis can be done successfully usingforceps with viscoelastic material or evenBSS only, positive IOP in the anterior cham-ber provides the best precondition for suc-cessful and controlled capsulorhexis per-formed through the paracentesis using a cys-totome.
Conjunctiva
A conjunctival flap is cut 1 mm fromthe limbus between 11:00 and 2:00. The1 mm of conjunctiva attached to the limbusfacilitates the postoperative healing process.

THE ART AND THE SCIENCE OF CATARACT SURGERY
378
Healing of conjunctiva to conjunctiva occursquickly and is stable, unlike the healing pro-cess between conjunctiva and limbus. Theattached conjunctiva also makes it possible toglue the edges of the conjunctiva by coagula-tion
Sclerocorneal Pocket PrimaryIncision and Tunnel
Precondition for Utmost ControlledDissection
The main reason the ACM is intro-duced at the beginning of surgery is to keepthe IOP between 30 and 40 mm Hg to makethe eye coats taut. The importance of thisprecondition for the utmost controlled dissec-tion in the sclera and cornea should not beunderestimated (Fig. 230). Most unintendedmisdirected scleral dissection, premature en-trance to the anterior chamber, or failure toachieve a full-size scleral pocket tunnel occuras complications of dissection in soft, floppytissue.
The sclerocorneal tunnel architectureof the primary incision which Blumenthalprefers for manual ECCE begins with anexternal straight scleral incision 4 to 6 mmlong and 0.3 mm deep (Fig. 230). It shouldbe performed 1 mm behind the limbus at thesurgeon’s choice of location, either 12:00 ortemporal. As the external incision is cutstraight, the distance of this incision variesgradually from the limbus. It is 1 mm behindthe limbus at 12:00, while on both sides theexternal incision is further away form thecurved limbus, up to 1.5 mm to 2 mm
At the bottom of the 0.3 mm deepexternal cut, dissection is extended anteriorlyuntil it engages the limbal tissues, whichresist dissection more than scleral or cornealtissues. In overcoming this extra resistance,the surgeon must take care not to press for-ward too forcefully, which might cause un-controlled forward corneal dissection andpremature perforation of the AC. Control oflamellar dissection at all stages is critical.
Dissection continues forward for about2 mm in clear cornea. As the dissectionapproaches the lateral edge of the tunnel, theknife is swept sideways 45 degrees, resultingin a funnel-shaped tunnel (identified as C 2,3 in Fig. 230) . Thus the internal aspect of thetunnel is about 25% larger than the externalincision. While the crescent knife is at thelateral edge of the straight external part of theincision, dissection should be carried ob-liquely backward. In this way the crescentknife forms a lateral pocket on both sides(identified as C 1, 2, 3 in Fig. 230), extendingbackward for 1 mm on each side. A back-ward incision 90 degrees to the limbus suchas hereby described, does not induce astig-matic effect. With practice the result shouldbe a well-constructed pocket sclerocornealtunnel (Fig. 230).
Now the keratome is slid into thetunnel (identified as I-K 4 in Fig. 231) with aslight side to side movement to preventpremature perforation of the anterior cham-ber. When the tip of the keratome reaches theend of the tunnel, the keratome is then tilteddownward to enter the anterior chamber.After entering the anterior chamber, thekeratome is moved laterally and forward

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
379
(Fig. 231-K-4). This combination of move-ments directs the internal incision in curvedfashion parallel to the limbus. The procedureis repeated on the other edge of the tunnel.Thus the extreme edges of the internal inci-sion (temporal and nasal points of entry of theAC), are 3.5 to 4.0 mm from the lateralpoints of the external incision. A commonerror in constructing this tunnel occurs whenthe keratome, instead of moving laterally andanteriorly, is directed laterally and backward,thereby creating a much smaller tunnel. Themore funnel shaped the tunnel is, the lessastigmatism induced, and the less potentialthere is for BSS leakage from the AC eitherduring or after surgery. All these movementsare performed while the eye is fixated withBonn forceps, away from the tunnel incision.
Hydrodissection and NucleusDislocation
Hydrodissection is performed throughone of the two paracenteses located at10:30 and 2:30 (Fig. 230). ProfessorBlumenthal uses a 1 cc syringe attached to acannula. A 3-5 cc syringe should not be used,as a sudden surplus of BSS in the crystallinelens might burst the posterior capsule. Thecannula should be introduced under the ante-rior capsule at the 12:00 position. No morethan 0.1 cc to 0.3 cc of BSS is injected,engulfing the lens contents instantly byhydrodissection. In most cases the nucleustilts forward into the AC at the 12:00 position,as the BSS fluid accumulates first at this
Figure 231 - Creation of the Special Sclero-Cor-neal Pocket Tunnel Incision - Stage 2
A keratome (K) enters the anterior chamberto accomplish the internal corneal incision (I - bluedotted line) curved shape, parallel to the limbus. Thekeratome must be moved in a direction slightly awayfrom the surgeon while moving it laterally (4-arrow)to produce this curved configuration of the internalcorneal incision. Lateral scleral pockets (P). Ante-rior chamber maintainer (A). The distance from theexternal to internal incision is about 3.5mm to 4mm.Internal incision (I) length is about 7mm.

THE ART AND THE SCIENCE OF CATARACT SURGERY
380
location (Fig. 232). In cases where thenucleus is not partially dislocated anteriorly,one or two Sinskey hooks are introduced atone or both paracenteses located at 11:00 and2:00. Uneven pressure by one hook while thenucleus is rotated causes the nucleus to tiltand gradually to dislocate anteriorly. Thesurgeon should make sure that the nucleustilts up toward the wound. If it does not, thelens should be rotated further until this align-ment is achieved. When the tilt is not suffi-cient in the surgeon’s judgment, the bent partof a cannula should be introduced under the
lens while BSS is injected. This will cause thenucleus to move gradually anteriorly com-pletely into the AC (Fig. 232). The use of toomuch force during this maneuver can causethe lens to suddenly touch the endothelium.
Blumenthal does not remove cortex atthe center of the lens anteriorly because thiscortex protects the endothelium from therough nucleus during movements in the AC.The lens does not need to be completelydislocated to the AC before extraction canbegin. When the nucleus is free after rotation,it can remain partially in the bag and partiallyin the AC (Fig. 232).
Figure 232: Hydrodissection of the Nucleus and Epinucleus
The anterior chamber maintainer (A) connected to a BSS bottle maintains and con-trols intraocular pressure during the circular capsulorhexis. A hydrodissector cannula (H) isintroduced through a paracentesis (D) under the anterior capsule at the 12:00 o’clock position.Injection of fluid (blue arrows) causes the superior nucleus and epinucleus to become luxatedanteriorly (arrow - 1,2,3), tilting it forward into the anterior chamber. The nucleus and epi-nucleus are now partly in the anterior chamber and partly in the bag, ready for expression.Main sclero-corneal pocket incision (I) is shown in cross section.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
381
Nucleus Expression Using Glide andHigh IOP
Before the lens glide is introducedunder the nucleus, the surgeon must firstassess whether viscoelastic material is neededin addition to the ACM. Blumenthal consid-ers using viscoelastic in shallow chambersand in patients with glaucoma that may havea small pupil. The glide should not be inducedforcefully as it might engage the nucleusitself rather than slide under it (Fig. 233). Theglide should not move too far inferiorly or itmay tear the posterior capsule. If a glide is
not used, the nucleus may not move in acontrolled way towards the incision.
To move the nucleus (with its epi-nucleus) into the wound, slight external pres-sure should be exerted with a closed forcepsor other instrument on the glide inside thetunnel in a stroking pattern. The strokes mayneed to be repeated a few times until thenucleus is pushed forward by fluid from theACM to engage the mouth of the sclerocor-neal tunnel (Fig. 234). At first, BSS still leaksaround both sides of the nucleus. Stroking iscontinued until the nucleus is well lodged inthe inner aspect of the sclerocorneal pocket,
Figure 233: Technique of Nucleus ExpressionUsing Glide and High IOP - Surgeon’s View
A lens glide (G) is introduced through theincision to a position just under the superior edgeof the tilted nucleus and epinucleus within the an-terior chamber. High intraocular pressure from theanterior chamber maintainer causes the nucleus andepinucleus (N)(shown in ghost views) to move to-ward (1-arrow) the open incision. Slight pressurefrom a firm instrument (not shown) placed withinthe incision on top of the glide may be used to ini-tiate the movement of the nucleus toward the inci-sion as it is forced out of the opening by the highintraocular pressure. As the epinucleus and nucleus(N) enter the incision tunnel, the epinucleus (E) maystrip off within the scleral pockets (P). The hardcore nucleus continues to exit the incision with theflow of BSS under pressure (2-arrow). If a largenucleus will not exit the eye, chipping off a smalltriangular piece of nucleus will facilitate expres-sion of the nucleus (inset below). Anteriorcapsulorhexis (C).

THE ART AND THE SCIENCE OF CATARACT SURGERY
382
and no leakage is observed. Continued pres-sure should not be made in the tunnel whenthe nucleus is engaged, as pressure in thetunnel would open the tunnel and new leak-age would begin, preventing nucleus expres-sion.
Now pressure is shifted out of the tun-nel, posteriorly, onto the sclera. This slightlychanges the position of the nucleus in thetunnel to allow expression. The nucleusrocks from side to side, and rotates slightly onits axis while finding its way out of the tunnel(Fig. 234).
The amount of pressure to induce canbe assessed by observing the depth of the AC,
which should not change. If the AC col-lapses, stop pressing and allow it to reform.
The preceding description is accuratewhen the tunnel is large enough to allow thenucleus to pass through the tunnel. Duringthis move, it sheds any remnants of epi-nuclear material; in this way the smallestpossible nucleus is delivered. The remnantsof the epinucleus are observed as leftover inthe AC; they are soft and easily expressed bythe hydrostatic pressure itself (Fig. 235).Their progress is helped by gentle strokes inthe tunnel, causing BSS to flow out of theeye. The BSS on its way out engulfs the softepinucleus and flushes the epinucleus out.
Figure 234: Technique of Nucleus Expression Using Glide and High IOP - Cross Section View
This cross section view shows lens glide (G) in place for nucleus expression. High in-traocular pressure from the anterior chamber maintainer (A-arrow) causes the nucleus and epi-nucleus (1) to move toward (red arrow) the open incision. As the epinucleus and nucleus enter theincision tunnel, the epinucleus (E) may strip off within the scleral pockets as the hard core nucleus(N) continues to exit (2) the incision with the flow of BSS under pressure.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
383
Should the nucleus proper be too large to beexpressed, the surgeon has two choices: (1)Enlarge the inside aspect of the tunnel, notthe external incision; or (2) Perform chipping.Part of the nucleus is exposed in the incision.A 25 gauge needle is introduced into thenucleus, chipping off a small triangularpiece. The smallest new diameter of thenucleus can be made small enough for thenucleus to be expressed.
Epinucleus and Cortex Extraction
Epinucleus
Continuous flow and positive IOP in-flate the capsular bag after nucleus extraction.The soft epinucleus left behind in the AC isusually hydroexpressed spontaneously. To fa-cilitate this maneuver a spatula can beintroduced through the tunnel (Fig. 235). Incases where the epinucleus is left in thecapsular bag, manipulation in the bag right
Figure 235: Expression of Epinucleus
If the epinucleus (1) remained in thescleral tunnel pockets, it may be hydroex-pressed (2-red arrow) using slight instrumentstrokes of a small spatula (S) placed insidethe tunnel. Anterior chamber maintainer (A)provides pressure to facilitate this expression.Lens glide (G). Note remaining cortex (C)within the capsular bag.

THE ART AND THE SCIENCE OF CATARACT SURGERY
384
and left by the spatula will release the epi-nucleus from its adherence to the cortex andallow it to be flushed out.
The Cortex
Blumenthal recommends aspiratingthe cortex manually; aspiration is bettercontrolled using a 5 cc syringe and cannula(Fig. 236). The cannula should be introducedfrom one of the paracentesis sites and notfrom the tunnel because introducing a can-nula through the tunnel may allow BSS toescape. The resulting instability of the poste-rior capsule would be unfavorable forsmooth aspiration of the cortex. Using the
paracentesis port for aspiration allows theamount of BSS aspirated or lost to be instan-taneously replaced by the anterior chambermaintainer.
IOL Implantation
The leading haptic is inserted into theAC and under the anterior capsule at 6:00o'clock (Fig. 237). The anterior chamber maybecome shallow for a short period during thismaneuver. For this reason a strong IOL holderis recommended so that the leading loop canbe directed under the capsule even in thepresence of a shallow AC. When the leadingloop is stable under the capsule, the IOL
Figure 236: Cortex Removal and Water JetTechnique to Remove Residual Cortex
A special cannula with a 0.4mm pore(J), connected to a 5cc syringe is introducedthrough a paracentesis (D), where it is used toaspirate the cortex (B). Next, a hydrodissectorcannula (H) is introduced through the paracen-tesis (D) and is used to create a water jet burstof BSS (blue arrows) directed to the posteriorcapsule. This forces any cortical material leftover to free itself from its attachments to thecapsule, either in the posterior capsule or lo-cated in the equator of the lens bag. This pres-sure and that from the anterior chamber main-tainer (A) forces these pieces out of the eye.Anterior capsulorhexis (C).

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
385
holder is released, but not before forcepsgrasp the trailing loop outside the eye toprevent the IOL from springing out of the bagat 6:00. A modified Sinskey hook is insertedthrough one of the paracenteses, usually at10:00 for right-handed surgeons and the lensis manipulated into the bag. The trailing loopis introduced into the AC first. Then the IOLis rotated while pushing backward (Fig. 238).Thus the trailed loop enters the bag
(Fig. 238). Blumenthal prefers to have holesin the loops and one hole in the haptic nearthe optic for manipulating the lens into thecapsular bag. Blumenthal has seen no illeffects resulting from haptic holes.
When to Use Viscoelastic
In cases where any difficulty arisesduring implantation, especially in young
Figure 237: Intraocular Lens Implantation Technique - Stage 1
The intraocular lens is introduced into the anterior chamber using an IOL holder, with the distal hapticdirected posterior to the anterior capsule, and into the 6:00 capsular bag (arrow). When this is achieved, the IOLholder is released, not before forceps (F) grasp the trailing loop outside the eye to prevent the IOL from springingout of the bag at 6 o’clock. The anterior chamber maintainer (A) keeps the capsular bag ballooned during implan-tation. Anterior capsulorhexis (C).

THE ART AND THE SCIENCE OF CATARACT SURGERY
386
people, or if the anterior chamber is shallow,the use of viscoelastic material is indicated. Itis easier to introduce the IOL into the AC inthe presence of viscoelastic, but manipulationof the lens into the final preferred position ismore easily achieved in the presence of BSS.Viscoelastic is not contraindicated duringmanual small incision Mini-Nuc ECCE whileusing the anterior chamber maintaining sys-tem, but the BSS flow should be reduced orstopped. It is better to activate the ACMsystem during aspiration of the viscoelastic.This keeps turbulence and fluctuation to aminimum.
Pupil Enlarged by Increased IOP
Deepening the AC with the ACM andincreasing the IOP from 10 mm Hg to 30-40mm Hg, pushes the iris back and sideways,dilating the pupil mechanically beyond thepharmacological effect of the dilatationdrugs. In certain cases the pupil stays extradilated at the end of surgery because of aphenomenon known as reverse pupillaryblock. No long-term ill effects arise from this.After a few minutes the reverse pupillaryblock subsides, as pressure in the posteriorchamber rises above that existing in the AC.The block can also be broken mechanically
Figure 238: Intraocular Lens Implan-tation Technique - Stage 2
With the distal haptic already lo-cated within the capsular bag at 6 o’clock,the forceps (F) moves the proximal hapticlaterally (1-arrow). A Sinsky hook (S)placed through the paracentesis (D) en-gages the haptic hole (H) in the loop.While rotating the lens (2-arrow), theproximal haptic is introduced into the an-terior chamber, compressed with the hook,directed behind the anterior capsule (3-ar-row) and into the bag in one motion. An-terior chamber maintainer (A). Anteriorcapsulorhexis (C).

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
387
by introducing a spatula under the iris. Thepupil immediately becomes smaller, and theiris moves forward.
Advantages of the Continuous Flowof BSS during Manual ECCE
Removes debris: The anterior chamberis washed throughout surgery. All pigmentdebris is washed out, reducing to a minimumpossible ill effects during the postoperativeperiod.
Stops bleeding: When bleeding occursin the tunnel or in the anterior chamber duringsurgery, it can be stopped by increasing theIOP. Moreover, no blood accumulates duringsurgery, as it is washed out by the continuousflow.
Frees cortex remnants: These rem-nants find their way out of the eye due to thecontinuous flow through the AC. The rest areaspirated by a 5 cc syringe with a cannulaattached. The aspiration is usually performedat the final stage of the surgery before theACM is pulled from the eye.
Removes viscoelastic: Viscoelastic ma-terial can and sometimes must be used duringthe surgery. It can be flushed out by fluidfrom the ACM or aspirated. Leftover quanti-ties of viscoelastic are removed from theirhidden locations with short bursts of BSSproduced by a 1 cc syringe and cannula.
Cleans posterior capsule: A 1 cc sy-ringe attached to the hydrodissector cannulais used to create an intermittent water jeteffect on the posterior capsule to clean it fromattached cortical material (Fig. 233). This
procedure is much more effective when theACM is used. The freed cortical material isaspirated whenever it is separated form thecapsule. Aspiration of cortical material di-rectly from the posterior capsule involvesmuch more dangerous manipulation, as mostcapsule tears occur during this stage of thesurgery.
Prevents inflow : Hypotony, even if itoccurs for a very short period, can causeinflow from outside the eye into the eye. Withthe ACM system, its active flow preventsforeign material from washing into the AC.By the same mechanism bacteria are partiallyprevented from entering the eye. If an instru-ment does carry bacteria to the AC, the bacte-ria may be washed out reducing the likeli-hood of endophthalmitis.
Complications
Posterior capsule tear: Tears in theposterior capsule are mostly caused by suc-tion with the aspiration cannula. The presenceof the AC maintaining system during unin-tended tear of the posterior capsule pushes thevitreous face backward. In 70% of cases ofunintended tear of the posterior capsule, thevitreous face stays intact. When the vitreousface is intact, BSS does not enter the vitreousbody, even if the IOP is 40 mm Hg.
The hypothesis that vitreous hydrateswhen in contact with BSS is not true. Hydra-tion occurs only if the vitreous face is broken.During manual ECCE there is little turbu-lence or fluctuation; most of the time there isno movement at all. The amount of BSS used

THE ART AND THE SCIENCE OF CATARACT SURGERY
388
throughout one modern ECCE procedure dur-ing 10 minutes of surgery is only 20 cc to 30cc The amount of flow during each minute ofthe surgery is 2 cc to 3 cc. This amountproduces the least possible turbulence. Con-trolled aspiration using a 5 cc syringe in thepresence of a posterior capsule tear can beperformed without vitreous engagement, andaspiration of cortical material in the presenceof posterior capsule tear is continued until thecapsule bag is free of cortex, without enlarg-ing the tear.
The steady condition allows the sur-geon to perform the most delicate maneuverpossible, aspiration of cortical material lyingon the vitreous face. This maneuver can bedone only if the vitreous remains still, with nofluctuation.
Vitreous involvement: When vitreousenters the AC through a posterior capsuletear, vitrectomy must be performed. An exist-ing ACM is a great advantage at this stage.Because an imbalance of inflow and outflowwould aggravate the situation, Blumenthalrecommends the paracentesis entrance for thevitrectome tip. Steady conditions during vit-rectomy ensure the procedure can be per-formed in a controlled manner. Because theposterior capsule does not move in an uncon-trolled fashion, enlarging the size of the tearcan be avoided. Enlarging the posterior cap-
sule tear during vitrectomy reduces the optionof choosing the bag as the best fixation sitefor the IOL.
Locating vitreous strands is anothervery important aspect of the art of vitrectomy.Two-handed vitrectomy, during which thesurgeon has a spatula in one hand and thevitrectome in the other, enables the surgeon tosearch for and locate vitreous fibers. Gettingrid of all the vitreous strands, whether largeor small, is essential. A quiet milieu allowsthe surgeon to search with the spatula care-fully for strands over the iris and at theopening sites of the paracenteses and thetunnel. Eyes after such vitrectomy withoutstrands in the AC have a very low rate ofCME or iris deformation. In cases where thesmallest vitreous strands remain, on the otherhand, the incidence of CME is much higher.
Expulsive Hemorrhage Minimized byPositive IOP: This rare phenomenon can bereduced to a minimum in routine cataractsurgery, and in complicated or traumatic eyesby using continuous positive IOP during sur-gery. No hypotony occurs to cause leakagefrom, or rupture of choroidal or retinal bloodvessels, especially when they are arterioscle-rotic. Therefore expulsive hemorrhage or par-tial choroidal hemorrhage is mostly pre-vented.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
389
THE SMALL INCISION PHACO SECTION MANUAL EXTRACAPSULAR TECHNIQUE
Overview
We here present the Phaco Sectioncataract technique as developed by DavidMcIntyre, M.D. one of the most talented andexpert cataract surgeons in the U.S. Wedescribe the evolution of his cataract surgerytechnique, present highlights of the procedurehe has been using for 10 years, suggest how asurgeon can make the transition to the 5.5 mmwound Phacosection, and outline his surgicalprocedure step by step.
At present McIntyre continues to usea 5.5 mm, non-sutured self-sealing, corneo-scleral tunnel incision placed temporally undera peritomy, through which extracapsularcataract surgery is performed and a posteriorchamber intraocular lens (IOL) is placed in thecapsular bag. The intraocular lens is a 5.5 mmround, one-piece polymethylmethacrylate(PMMA) IOL placed in the bag, presentlymanufactured by Surgidev.
McIntyre uses an anterior chambermaintainer, capsulorhexis and the nucleus issectioned into 2 or 3 fragments, occasionally 4,with few exceptions in ages under 50-55.
Evolution of Technique
McIntyre’s surgical technique has hada complex evolution. In 1974, he made thetransition from intracapsular to extracapsular
surgery, using Kelman's phacoemulsificationtechnique. During the past 20 years he hasdevised a number of instruments and modifiedtechniques, resulting in extracapsular surgerywith smaller and smaller incisions. Currentlythe incision is self-sealing and just large enoughfor the IOL implantation.
From the perspective of results withpatients, McIntyre has found no reason toreturn to the emulsification of the cataractnucleus with ultrasonic energy(phacoemulsification). At the same time he haspersonally attempted to develop a number ofmechanical devices to aid in cortex aspiration.With each device he has reaffirmed that he hasgreater control over the operation when he usesa completely manual technique.
Indications
McIntyre strongly believes that a basicadvantage of the Phaco-Section is itsapplicability to all degrees of hardness ofnucleus, from soft (+) to moderate (++), tofairly hard (+++) and to hard (++++), with trulyminimal variations.
PHACO SECTION MOSTIMPORTANT FEATURES
The three separate tissue zones of thelens are shown in Fig. 239 to enhance theunderstanding of how Phaco Section works.

THE ART AND THE SCIENCE OF CATARACT SURGERY
390
The following are the most importantfeatures of McIntyre’s Phaco-Section surgicalprocedure.
Capsulorhexis
This is performed through the incompletetunnel incision that is perforated only by thecystotome.
McIntyre believes capsulorhexisoffers several advantages in smallincision phacosection technique. First,a 6 mm capsulorhexis is large enoughto allow the management of almost allnuclei by the phacosection technique(Fig. 241). Secondly, the capsulorhexisactually gives a stronger margin to thecapsulectomy than any of the "can-opener" techniques. Consequently,there is considerably less risk of tearsof the capsulectomy margin extendingaround the equator and to the posteriorcapsule.
Third, the use of air providessignificant benefit in the capsulorhexis.Air is maintained in the anteriorchamber very easily after the punctureincision of the cystotome needle(Fig. 241). The presence of air in theanterior chamber makes visualization
and control of the fragment of anterior capsulemuch easier for the surgeon. Lying on thesurface of the cataract as it is torn around thecircle, the fragment is very easily visualized.
And finally, and perhaps mostimportantly, when the fluid is removed fromthe anterior chamber and is replaced with an airbubble, the magnification effect of the corneais almost entirely neutralized, so that it is easyto understand the actual dimensions. When theanterior chamber is filled with fluid, the corneabecomes a 15% magnifier on average, makingthe capsulorhexis appear much larger than itreally is.
Completing the Tunnel Incision
After the capsulorhexis has beencompleted, the surgeon must complete thetunnel primary incision into the anteriorchamber. There is a paracentesis just to the
Figure 239: The Three Tissue Zones of the Lens
This anterior globe cross section shows the three separatetissue zones of the lens. Portions of the lens are shown removed toreveal the three dimensionality of these tissue zones. The rigidnucleus (N) is in the center. The second zone is the epinucleus (E),a firm or heavy gelatin material which is difficult to aspirate. Thethird and outer zone is the cortex (C) which is soft gelatin that is easyto aspirate, and lies just under the capsule (D). Note the 6 mmdiameter circular capsulorhexis, which is large enough to allow themanagement of almost all nuclei by the phacosection technique.Air (A) is used to fill the anterior chamber during capsulorhexis tomaintain the chamber depth and to eliminate the magnificationeffect of the corneal curvature.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
391
right end of the tunnel incision, but the tunnelhas been perforated only by a needle (thecystotome) up to this point. McIntyre enlargesthe primary incision by grasping the margin ofthe scleral lip with a colibri forceps and passinga 15-degree supersharp blade through thecystotome puncture to slightly enlarge theincision. Then, with the double-bevelledcrescent knife, he enlarges the opening into theanterior chamber to the full length of the tunnelincision, which is 5.5 mm to 6 mm (Fig. 241).
The Dynamics of the Self-SealingIncision
McIntyre uses an analogy to help explainthe dynamics of the self-sealing incision.Shallowness of the tunnel is important inpreventing frequent hyphema. Deep tunnelstend to have frequent hyphemas; superficialtunnels tend not to result in frequent hyphema.McIntyre’s analogy is a great circle, which isthe shortest distance between two points on thesurface of the sphere, a common concept usedin navigation (Fig. 240). On the eye the endsof an incision can be connected by a great circlearound the globe. If any pressures and tractionoccur, there is a tendency for a wrinkle todevelop that connects the two ends of theincision along the great circle.
Consequently, if a scleral flap is fashionedfollowing the curve of the limbus, that scleralflap must be sutured in position because anydeformity of the globe will cause the eye towrinkle along the great circle connecting thetwo ends of the incision. The scleral flapwould become a free, non-supporting structure.In contrast, a frown-type incision that has a
concavity facing the great circle that connectsthe two ends of the incision does not allow anystretching or raising of the flap. This is thereason the superficial layer of dissection in atunnel has a very firm, unyielding geometrywhich to resists deformity or increasedpressure within the globe. As long as theincision is concave to the great circle, asatisfactory self-sealing tunnel can be created.With the exception of children, the tunnelincision is sutured only in approximately 1of 300 cases.
Anterior Chamber Maintainer
The anterior chamber maintainer thatMcIntyre uses is a threaded or screw-like tipof metal tubing attached to a silicone tube,which is then attached to the hub of a needle. Itcan be plugged into a fluid source and has aflexible connection with the eye (Fig. 241).The internal diameter of the metal tubing is 0.6mm. The threaded outer surface of the tube isable to grasp the corneal paracentesis veryfirmly so that when this has been screwed intothe cornea it will hold in that position evenwhen the eye is rotated rather vigorously.
At the conclusion of the procedure itmust be unscrewed to be removed. During itsintroduction the silicone tube and the maintainertip itself have a stylette passed into them; theresulting rigidity allows the turning process,and a rounded point at the tips allows it to easilypass through the paracentesis. The fluid sourcefor the chamber maintainer is balanced saltsolution (BSS), which contains additionalantibiotics for prophylactic purposes and issupported on an electric IV (intravenous) pole

THE ART AND THE SCIENCE OF CATARACT SURGERY
392
so that the static height, and thereby thegravitational force, on the fluid that is enteringthe anterior chamber can be easily adjusted.The infusion tubing that comes from the BSSbottle to the table also has a roller valve so thatthe assistant can turn the maintainer system onand off as needed throughout the procedure.
Aspiration of the Anterior Cortex andEpinucleus
With the tunnel completely opened andwith the chamber maintainer operating and itspressure somewhat elevated, the surgeon doesthe preliminary aspiration of the cortex and
Figure 240: Straight vs Frown Shaped Scleral Incision
A "great circle" on a sphere, or in this case on an eye, is the circumferential line (L) produced by a plane(P) which passes through the center (C) of the sphere. The great circle shown on this eye is one which passes throughthe area of a planned incision marked by endpoints (A) and (B). The key to the concept of the great circle is that itis geometrically the shortest distance between two points which lie on that circle. If the surface incision (D - top inset)forms a concave shape that does not cross the great circle (dotted line), then the superficial flap is quite rigid. If theincision (E - bottom inset) forms a convex shape from the great circle (dotted line), then there will be no support forthe flap. Note the resulting gape of the incision.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
393
epinucleus overlying the anterior surface ofthe firm central nucleus using a 21-gaugecannula (Fig. 241). McIntyre is careful tocreate a gutter or furrow around theequatorial area of the nucleus, thus allowingit to more easily come up from the remainingepinuclear "bowl". This is performedwithout any hydrodissection.
Most experienced surgeons are awareof a complication that is frequentlydisastrous for the patient: the combinationof posterior capsule tearing or rupturingwith loss of vitreous and with portions ofnucleus retained in the posterior segment.
McIntyre believes that thiscomplication indicates potential loss ofcontrol by the surgeon during portions ofthe operation when aspiration is being used.During removal of the lens material, thecataract should be seen as being formed ofthree separate tissue zones (Fig. 239). Startingfrom the center is the nucleus, a rigid materialthat is too viscous to allow aspiration. Thesecond zone is the epinucleus or, as it is oftencalled, the epinuclear bowl. The epinucleus isa relatively firm gelatinous material with anintermediate degree of viscosity, which can beaspirated with sufficient vacuum. The thirdzone is the peripheral cortex, which lies justunder the capsule surface. This gelatinouszone is of a very low viscosity and is freelyaspirated.
This perspective of the three zones of thecataract clearly reveals an important safetyfactor in aspiration. Whether using manual ormechanical methods, the surgeon has morecontrol when aspirating from the less viscouscortex toward the highly viscous nucleus.
On the other hand, there is a potential lossof control and an extreme danger whenaspirating from the more viscous element, suchas the epinucleus, toward the peripheral cortex.In this circumstance when the aspirating
Figure 241: Aspiration of Anterior Cortex and Anterior Epi-nucleus
The following illustration depicts the surgeon's view of aleft eye. Temporal (3 o'clock) is at the bottom and nasal (9 o'clock)is at the top. First, an anterior chamber maintainer (M) is insertednasally. A 6 mm circular capsulorhexis (A) is performed. The 5.5mm frown shaped scleral tunnel (T) incision is completed. Aspecially sharpened 21 gauge cannula (D) is introduced through aparacentesis made to the right of the scleral tunnel incision. Insetshows detail of the tip of the cannula. The port of the cannula isdirected posteriorly to aspirate the central cortex (C), andepinucleus (E) overlying the anterior surface of the firm nucleus (N).A furrow is created around the equatorial area of the nucleus.
instrument clears a portion of the viscousepinuclear material, the cortex will then movethrough the aspirating system at a much greatervelocity, challenging the control of the surgeonto avoid impaction and probable tearing of theposterior capsule.
Phacosection
Following the preliminary aspiration ofcortex and epinucleus from the front surface of

THE ART AND THE SCIENCE OF CATARACT SURGERY
394
the nucleus, McIntyre does a hydrodissectionof only the central hard nucleus using a 27-gauge, slightly narrowed and slightly curvedcannula (Fig. 242). With this hydrodissectionhe also tilts forward the margin of the nucleusnearest the incision. Then the nucleus itselfcan be divided into a number of fragmentsusing the technique called Phacosection(Fig. 243). This term, which McIntyre findsvery useful, originated with Peter Kansas inNew York. The procedure involves dividingthe nucleus into a number of fragments, thenumber being determined by the size andhardness of the nuclear material, usually 2 or 3,occasionally 4. Each of these fragments is thenindividually surrounded by a layer of heavyviscoelastic material (Fig. 244) and simplyextracted from the anterior chamber with theirprotective viscoelastic coating using a pairof instruments designed for this purpose(Fig. 245).
Removal of Epinucleus andCortical Cleanup
Following the removal of the dividednucleus particles, the epinucleus is then remo-ved as a second stage. The epinucleus ishydrodissected from its attachment to theperipheral cortex (Fig. 246). In most cases theepinucleus is a continuous structure which canbe hydrodissected, brought forward into theanterior chamber, and hydraulically expressed.The epinucleus is not removed by aspiration.
The third stage of the cataract tissueremoval is simple aspiration of the residualcortex. The only stages of the procedureperformed by aspiration are the preliminaryaspiration of the anterior cortex and epinucleus,and then the final cleanup of the residualperipheral cortex. In this way the process ofaspirating from a more viscous to a less viscous
Figure 242: Hydrodissection of the Nucleus
A 27 gauge cannula (F) placedthrough the paracentesis is used to hydrodissectthe nucleus (N). The cannula is rotated (ar-row) under the margin of the nucleus nearestthe scleral tunnel incision to tilt it forward. Asmall amount of viscoelastic material may beused to maintain this tilt. Note the epinuclearbowl (E) in which the nucleus sets. Chambermaintainer (M).

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
395
medium is avoided. Thereby, the surgeonavoids losing control and destroying thecontinuity of the posterior capsule.
Transition from ExtracapsularExtraction to Phacosection
McIntyre believes it is easier forthe ophthalmic surgeon who isaccustomed to standard, conventionallarge-incision extracapsular surgery tomake the transition to small-incisionphacosection (5.5 mm) than tophacoemulsification. The smallincision phacosection technique offersthe surgeon some very distinct advantageson his/her patient’s behalf in comparisonwith the conventional large-incisionplanned extracapsular. These advantagesare: more safely, a much more rapidrecovery, a much more durable eye during
Figure 243 (left): Phacosection of the Nucleus
A spatula (S) is introduced through thescleral tunnel incision (T) and placed behind thenucleus (N). A single cutter (R), also introducedthrough the tunnel incision, is used to section(arrow) the nucleus. The anterior chamb er con-tains viscoelastic with the anterior chamber main-tainer (M) turned off during this sectioning.
Figure 244 (above): Surrounding NuclearPieces with Viscoelastic
Each fragment of nucleus is in-dividually surrounded by a layer of heavyviscoelastic material via a cannula throughthe tunnel incision. The viscoelastic (V) isshown being placed between the two hardnucleqr fragments (N). This will assist inprotecting intraocular structures during theirremoval. The anterior chamber maintainer(M) is still turned off.

THE ART AND THE SCIENCE OF CATARACT SURGERY
396
Protocol for Phacosection Surgery
The total small incision self-sealingphacosection cataract procedure with lensimplantation can be summarized in the followingsteps:
1) A standard patient preparation withwide dilation of the pupil. Peribulbar anesthesiafollowed by 40 minutes of oculopression with anequivalent of 30 mm pressure. The patient isdraped with isolation of the lid margins andinsertion of the speculum.
2) A nasal limbal paracentesis is followedby insertion of the anterior chamber maintainer,which is then turned on (Fig. 241).
3) A temporal limbus based conjunctivalflap of 3 to 4 mm width is made with mechanicaldissection of the limbus and limited bipolarcautery of the episcleral vessels.
4) A 6 mm frown incision is marked withcalipers on the surface of the sclera, avoiding anymajor scleral vessels (Fig. 240).
5) A superficial scleral tunnel is dissectedwith a crescent blade. A paracentesis is createdto the right side of the incision tunnel. Thenperforation is made through the base of the tunnelinto the anterior chamber at the center of thetunnel with a hooked cystotome.
6) The anterior chamber maintainer isturned off. The anterior chamber is inflated withair through the cystotome, and a capsulorhexis ofapproximately 6 mm diameter is created.
7) The chamber maintainer is turned on.Perforation is made through the central tunnelpuncture with a 15 degree super sharp blade,followed by the crescent blade to enlarge theinternal aspect of the tunnel incision to its fulldimension.
8) Any remaining air bubbles and thecapsule fragment are aspirated through the tunnelincision with a 21-gauge cannula. The chambermaintainer is elevated to increase the hydrostaticpressure. Preliminary aspiration of the anteriorcortex and the epinucleus down to the face of thenucleus is done with the 21-gauge cannula throughthe paracentesis (Fig. 241).
9) Hydrodissection of the firm centralnucleus is done with a 27-gauge cannula throughthe paracentesis, tilting forward the equator of thenucleus adjacent to the tunnel (Fig. 242).Hydrodissection is intended to elevate the smallestidentifiable nucleus and to tilt forward only theequator that lies directly in front of the tunnelincision.
10) The anterior chamber maintainer isturned off. The anterior chamber is deepenedwith viscoelastic of high viscosity; a small amountis injected behind the nucleus to hold it in the tiltedposition if necessary. With a cutting board and asingle nucleus cutter the surgeon reaches into theanterior chamber (Fig. 243). Depending on thesize and hardness of the nucleus, the surgeondecides how many cuts in the nucleus will beneeded. With the single cutter he then makes one,two, or three cuts as required. The two instrumentsare withdrawn.
11) Additional viscoelastic is injectedand the cannula is used to position the first fragmentof the cut nucleus that appears most readilyaccessible for removal (Fig. 244).
12) With the shield of viscoelastic inplace, the surgeon reaches into the anteriorchamber with the two nucleus extractinginstruments, which look very much like a pair ofspoons. The two spoons surround the fragment ofnucleus and remove it from the anterior chamber(Fig. 245).

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
397
13) Additional viscoelastic is used toisolate each individual fragment as it is removedwith the extracting instruments. The averagevolume of viscoelastic required is .25 ml.
14) The chamber maintainer is turnedon. Hydrodissection of the epinucleus is donewith the 27-gauge cannula and balanced saltsolution (BSS). The entire epinucleus ishydroexpressed with or without the irrigatingspoon (Fig. 246).
15) The residual peripheral cortex isaspirated with the straight and curved cannulasthrough the paracentesis.
16) The posterior capsule is polishedwith the straight side ported aspirating cannulaturned posteriorward and introduced through thetunnel incision.
17) This is followed by inspection,irrigation, and positioning of the intraocular lens
on the introduction forceps. The IOL is introducedunder an assisting 30-gauge cannula with theleading haptic placed directly into the nasalcapsular bag. The lens optic is steadied with the30-gauge cannula as the introduction forceps areremoved. The trailing haptic is placed under theincision into the capsular bag with a Dusek forceps.The lens is rotated, its position is confirmed, andthe haptics are placed in the horizontal position.
18) The conjunctival incision is sealedwith bipolar cautery. The corneal margins of theparacentesis are hydrated with a 30-gauge cannula.The chamber maintainer is removed. The marginsof the ACM paracentesis are hydrated with BSS.
19) Absence of iris incarceration isconfirmed. Final re-deepening and inspection ofthe anterior chamber is done through theparacentesis.
20) Finally, medications and dressingare applied.

THE ART AND THE SCIENCE OF CATARACT SURGERY
398
Figure 246 (left): Hydrodissection andHydroexpression of Remaining Epi-nucleus
The remaining epinucleus (E) ishydrodissected as shown using the special21 gauge cannula (D) introduced throughthe tunnel incision. BSS is being injectedthrough the 27 gauge cannula (F) as well asthe anterior chamber maintainer (M). Work-ing through the tunnel at this point assuresthat leakage will control excessive anteriorchamber pressure. When the epinucleus hasbeen hydrodissected and is floating in theanterior chamber, its removal (arrow) isfacilitated with the irrigating spoon (notshown). The residual peripheral cortex (C)is then aspirated via cannula through theparacentesis.
Figure 245 (right): Nuclear Fragment Re-moval
A spatula (S) introduced through thetunnel incision is inserted under the viscoelastic-coated nuclear fragment (N). The extractinginstrument (X), shaped somewhat like an in-verted spoon, is inserted over the nuclear frag-ment. Then, to extract the fragment, the spatula(S) is rotated upwards (red arrow) causing thetips of the instruments to approach one another ina pincer-like fashion. Both instruments with theincluded nuclear fragment are then removedfrom the anterior chamber in a straight horizontalmovement (blue arrow), thus preventing boththe instrument and the nuclear fragment fromcontacting the corneal endothelium. Note re-maining nuclear fragment (F) still within epi-nuclear bowl (E). Anterior chamber maintainer(M) is still off during this extraction.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
399
the immediate postoperative period, and a majorreduction in the astigmatism effects of thesurgery.
If the surgeon decides to make a transitionfrom the traditional large incision extracapsulartechnique this should be done in a very orderlyway with the following steps: 1)Begin usingthe standard incision technique with which thesurgeon is already familiar. 2) After completingthe large incision with pre-placed sutures if thatis the surgeon's custom, begin to practice thecapsulorhexis. 3) When comfortable with thecapsulorhexis technique, begin to aspirate downonto the surface of the nucleus, tilt the nucleusforward, perform the phacosectioningtechnique, and extract the particles of thenucleus. This is still done through the full-sizeextracapsular incision with which the surgeonis familiar.
4) When the surgeon is completelycomfortable with all these steps, then he/shecan begin to change the incision technique.McIntyre suggests that the size of the incisioncan first be reduced to about 7.5 mm. A frownincision can be made, but closed with twosimple interrupted sutures. 5) When the surgeonis confident this is performed satisfactorily, he/she can consider moving the incision site to thetemporal limbus and can progressively reducethe linear dimension of the tunnel. 6) When thetunnel is approximately 6.5 to 6 mm, thesurgeon will probably continue to put onesuture in the center of the tunnel just to maintainconfidence.
At this point, the surgeon is in fact doingthe current small incision phacosectiontechnique, and will find it is perfectly safe toeliminate the use of sutures except in specialcircumstances.

THE ART AND THE SCIENCE OF CATARACT SURGERY
400
THE SMALL INCISION MANUALPHACOFRAGMENTATION
The small incision manualphacofragmentation (MPF) that we herebypresent has been designed and developed byFrancisco Gutierrez C., M.D., of Spain. Itis performed with a 3.2 mm clear cornealincision, which is the same size as in pha-coemulsification. This manual phaco frag-mentation (MPF) can also be done with a 3.5mm scleral tunnel incision, which is the sameincision size for phaco when we utilize thescleral tunnel technique (Figs. 247 and 248).
Benefits of (MPF)
As advocated by Dr. Gutierrez C., thistechnique provides several important benefits,as follows:
1) It can be performed with a small 3.2mm incision if done in clear cornea and with a3.5 mm incision if done with a scleral tunnel,thereby resulting in minimum astigmatism andrapid recovery (Figs. 247 and 248).
2) It functions well with hard and softnuclei.
3) It requires a low investment in theequipment and instrumentation.
4) Presumably, it provides a very goodbackup when complications arise and pha-coemulsification must be discontinued. Thistechnique helps the phacoemulsification sur-geon in the event of an accidental rupture of theposterior capsule. Also, the instrumentationfacilitates extracting the nuclear fragments from
the AC through the small incision, avoiding theneed to enlarge it and convert the surgery to anECCE.
5) Presumably it is a method easier tomaster than phaco.
6) No less important, it requires no su-tures or stitches.
Experiences with Other PhacoFragmentation Techniques
In order to overcome the two main draw-backs of phaco: 1) difficult learning curve and2) high cost of equipment, a good number andvariety of techniques for manualphacofragmentation have been used in the past.The limitations of these techniques have beenrelated to not being able to sufficiently reducethe size of the incision because: 1) the instru-mentation was coarse; 2) the nuclear frag-ments that were to be extracted from the ante-rior chamber were too large, usually becausethe nucleus was divided into two or three pieces.
Why Use Gutierrez' Technique?
Positive Features of Instrumentation
The phacofragmentor designed byGutierrez, is manufactured by the Englishfirm of John Weiss & Son Ltd., a subsidiary ofthe Swiss multinational Haag-Streit. With it

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
401
the nucleus is broken into very small 2 x 2 mmpieces that can be extracted through a 3.2 or 3.5mm incision (Fig. 247). This results in apractically neutral postsurgical residual astig-matism.
The racquet-shaped design of thefragmentor (see P and B in Fig. 247) keeps thenuclear fragments within the racquet, avoidingtheir dispersion as they are removed from theAC.
The phacofragmentor or nucleotome hasa straight ophthalmic handle, with a 45º angleat its end, which is 8 mm long and 2 mm wideand racquet-shaped. The racquet is divided infour parts by three transverse bars two millime-ters apart (Fig. 247) which keep the smallpieces within the racquet. Other importantinstruments are:
• A spatula with a straight ophthalmichandle, whose end is adapted to the dimensions
and angle of the nucleotome and serves assupport for phacofragmentation (see "S" inFig. 247).
• Two straight-handled, ophthalmic ma-nipulators, left and right, with a basket end,which serve to collect the nuclear fragmentsduring the nuclear fragmentation (Fig. 250).
• Anterior chamber maintainers werepioneered years ago by Strampelli as well asJoaquin Barraquer, and their use is alwaysemphasized by Michael Blumenthal for hisMini-Nuc cataract extraction technique. TheGutierrez AC maintainer (ACM) maintainscontinuous irrigation with BSS in the anteriorchamber, creating positive pressure that stabi-lizes the AC depth. During the stages of theoperation in which the maintainer is used, theamount of viscoelastic utilized is less, therebyreducing costs.
Figure 247: Manual MultiphacofragmentationTechnique - Stage 1 - Fragmentation
Following creation of a 3.5mm scleral tun-nel (I) or 3.2mm corneal incision, continuous cir-cular capsulorhexis, and hydrodissection of thenucleus, the nucleus is luxated into the anteriorchamber. After the nucleus is luxated into theanterior chamber, a high density viscoelastic isinjected into the area surrounding the nucleus to fillthe anterior chamber. The spatula (S) is placedbeneath the nucleus (N). The nucleotome, (orphacofragmentor) (P) is placed on top of the nu-cleus. With the nucleus sandwiched between thetwo instruments (inset), the nucleotome is presseddownward toward the spatula (arrow). This sec-tions the nucleus into four fragments (1,2,3,4)between the cross bars (B) of the racket shapednucleotome.

THE ART AND THE SCIENCE OF CATARACT SURGERY
402
Surgical Technique
It is important to have good pharmaco-logical mydriasis because the pupil may con-tract during surgery.
Incision: This method can be performedthrough a 3.2 mm corneal incision (clear cor-neal) (Fig. 247) or through a 3.5 mm scleraltunnel incision (scleral tunnel) 2 mm awayfrom the corneal-scleral limbus (Fig. 248). Thepreparatory incision is made without penetrat-ing the anterior chamber (AC).
Capsulotomy: A continuous circularcapsulorhexis is performed with a cystotomethrough a superotemporal paracentesis. Thiscapsulorhexis should be sufficiently wide (ap-proximately 6 mm) to allow an easy luxation ofthe nucleus into the AC. The AC maintainer isused during this step and when aspirating theanterior cortex and epinucleus in soft and me-
dium-soft nuclei, before hydrodissection.Nucleus Hydrodissection and Lux-
ation: After entering the AC with a 3.2 mmbeveled blade, balanced salt solution (BSS) isinjected with a Binkhorst cannula through thecorneal or scleral incision between the anteriorcapsule and the cortex at 12 o'clock.
The BSS must be injected slowly andcontinuously until the "wave" of dissection isvisible on the posterior capsule. Injection ofBSS is continued until luxation of the nucleusbegins. If the luxation of the nucleus into theAC is partial, it may be completed by rotatingthe nucleus with a cannula, cystotome or spatula.
Nuclear Fragmentation: Once thenucleus has been luxated into the AC, high-density viscoelastic is injected into the sur-rounding area to fill the AC. The nucleus isthen fragmented by placing the spatula beneaththe nucleus and the nucleotome on top of it
Figure 248 - Manual Multiphacofrag-men-tation Technique - Stage 2 - Extraction
While the nuclear fragments (A)remain with the nucleotome (P), the spatula(S) and nucleotome are extracted (arrow)from the anterior chamber through the inci-sion (I). Notice the remaining nucleus (N)with center removed, within the anteriorchamber. This procedure is repeated untilthe whole nucleus is fragmented and ex-tracted. With hard nuclei, after capturing thenuclear fragments (A) with both instruments(P) and (S), space can be gained by extract-ing nuclear fragments (A) using only thenucleotome (P), as hard fragments will re-main within the nucleotome (P) without thesupport of the spatula (S), thus reducingcorneal injury.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
403
(Fig. 247). Pressure is then created by slowlypressing the nucleotome downward toward thespatula until the part of the nucleus in it isfragmented into four pieces (Fig. 247). Thepieces remain within the nucleotome, andwith the help of the spatula are extractedfrom the AC using a "sandwich" technique(Figs. 248 and 249). This maneuver is repeateduntil the whole nucleus is fragmented.
During nuclear fragmentation it is im-portant to refill the AC with high-density vis-coelastic as needed to protect the corneal en-dothelium and facilitate safe manipulation dur-ing surgery.
Manipulation of Nuclear Fragments:There are right and left manipulators to dis-place the remaining fragments of the nucleus tothe center of the AC to facilitate their fragmen-tation and subsequent removal (Fig. 250).
Cortex Extraction and Nucleus Re-moval: The lens cortex is aspirated with a two-way Simcoe irrigation-aspiration cannula(Fig. 251). If small pieces of the nucleusremain in the AC, they can be removed accord-ing to their hardness in different ways: with thenucleotome and the spatula together (sandwich- Figs. 247, 248, 249) or only with the
Figure 249: Manual MultiphacofragmentationTechnique - Stage 2A - Extraction
This cross section shows the extractionconfiguration seen in the surgeon’s view of Figure2. Notice the nuclear fragments (A) sandwichedbetween the nucleotome (P) and spatula (S) asthey are extracted (arrow) from the chamber. Partof the nucleus (N) remains in the anterior chamberand will be extracted in the same manner.

THE ART AND THE SCIENCE OF CATARACT SURGERY
404
Figure 250 - Manual Multiphaco-fragmen-tation Technique - Stage 3 - Manipulationof Nuclear Fragments
Left (L) and right (R) curvedmanipulators (M) are used to displace (ar-rows) the remaining fragments of the nucleus(N) to the center of the anterior chamber.From there they will be fragmented and ex-tracted in a similar fashion with thenucleotome and spatula.
Figure 251 - Manual Multiphacofragmen-tation Technique - Stage 5 - Removal of SoftNuclear Fragments and Cortex
Following removal of the nucleus,the lens cortex and any soft residual nuclearfragments (FS) can then be aspirated and ex-tracted from the anterior chamber with a Simcoeirrigation-aspiration cannula (A). A Charleuxcannula may also be used (not shown). Lenscortex beneath the hard-to-reach incision areacan be aspirated with a Binkhorst cannula (B) asshown.

C h a p t e r 13: Manual Extracapsular Techniques of Choice - Planned ECCE - Small Incision ECCE
405
nucleotome, removing the spatula from the AConce the surgeon has grasped the nuclearfragment. Removal can also be accomplishedusing a two-way (I/A) Simcoe or Charleuxcannula (Fig. 251), or with gentle BSS irriga-tion of the AC aided by a fine cannula.
Intraocular Lens Implant and WoundClosure: Viscoelastic is injected into the cap-sular bag and a foldable lens is implanted.Sutures are not usually required.
Complications
In Dr. Gutierrez C. experience, com-plications are rare. There is always the possi-bility for mild corneal edema if much in-traocular manipulation is done and for a smallhemorrhage in the anterior chamber if theinstrumental manipulation may causes smalldamage to the iris.
Dr. Gutierrez C. recommends thatophthalmologists beginning to use this methodinitially practice with incisions larger than3.5 mm, progressively reducing the size as theymaster the technique.

THE ART AND THE SCIENCE OF CATARACT SURGERY
406

C h a p t e r 14: The New Cataract Surgery Developments
409
THE NEW CATARACT SURGERY
DEVELOPMENTS
Overview
At present, there are four main avenuesof development for new techniques in cata-ract surgery. Those who advocate them con-sider that they might be better than pha-coemulsification. They are:
1) The Laser Techniques
Two groups of procedures are donewith laser:
a) The Dodick Laser Photolysis Sys-tem: This is the only one that has beenapproved by the FDA in the United States andis also clinically available in Europe. Thissystem is manufactured by Laser Corp., basedin Salt Lake City, Utah.
b) The Paradigm Nd:YAG Laser Sys-tem, also known on the “Phantom”. This isunder investigational development by Para-digm Medical Industries also of Salt LakeCity.
2) The Catarex System, beingdeveloped by Richard Kratz et al.
3) The Phaco Tmesis System, ofAziz Anis.
4) Warm Water Jet Technology.
DODICK’S PHOTOLYSIS SYS-TEM
Dodick et al use a Q-switched Nd:YAGlaser. The pulsed laser and a specially de-signed probe to use this energy are utilized forremoval of the cataractous crystalline lens.The probe has a quartz-clad fiber. Theproximal end of the quartz fiber is connectedto the laser source. The fiber enters the probethrough the probe’s infusion port and thedistal end terminates in front of a titaniumtarget inside the tip of the probe. This targetis an essential element of the device (Fig.252).
The titanium target acts as a trans-ducer, causing optical breakdown and plasmaformation to occur in the aspiration chamber,and sending out acoustic shock waves config-ured by the target’s shape to be maximized atthe aspirating tip. At the aspirating tipnuclear material is shattered by the acousticwaves and evacuated out of the eye.

THE ART AND THE SCIENCE OF CATARACT SURGERY
410
Figure 252: Dodick’s Laser Photolysis
The laser fibre (L) terminates in front of a titaniumtarget (T) which absorbs the emitted pulsed YAG laser energy(L). The resultant optical breakdown and plasma formationcreate shock waves which travel to the mouth of the aspirationport shattering the lens material. Suction occurs there and thecataract is aspirated out of the eye.
Surgical Technique
As described by Kanellopoulos et al a1.4 mm clear-cornea incision is made forinsertion of the Dodick photolysis laser-aspi-ration probe. A second, 0.9 mm corneal inci-sion is made to provide irrigation or infusionthrough a second probe. The infusion andaspiration are done after a 6 mm CCC isperformed. The laser delivers pulsing photicenergy, which creates a shock wave thatemanates from the probe tip in a focused
cone. These shock waves break down thesubstance of the cataract (Fig. 252). Thefragmented particles of the cataract are thenaspirated out of the eye.
The same probe is used to aspiratethe cortex.
At present, the incision needs to beenlarged for insertion of a foldable IOL.Industry is working on making foldablelenses that can be introduced into the eye withincisions smaller than the 2.8 mm minimumused now.

C h a p t e r 14: The New Cataract Surgery Developments
411
Advantages
According to Dodick, photolysis hastwo primary advantages. One is that it willallow smaller incisions and two, it generatesno heat. One of the disadvantages of classicphaco is that the wound may be damaged byheat. With laser photolysis, we will not haveany wound burns.
Photolysis is felt to offer more protec-tion of the corneal endothelium and presum-ably it is a somewhat simpler procedure thanphaco.
THE CATAREX SYSTEM
This system is under investigationaldevelopment under the leadership of RichardP. Kratz, Shoeila Mirhashemi, MichaelMittelstein and John Sorensen. Through theyears, Kratz has made several major contri-butions to improve the techniques of pha-coemulsification.
Catarax is a different technology thatmay important advantages over phaco andECCE.
Potential Advantages and Tech-nique
Lindstrom is participating in the in-vestigational work in animals. As he de-scribes it, it only requires a 1.0 to 1.4 mmincision. The surgeon makes a one millimeterincision in the anterior capsule with di-athermy, just inside the edge of the iris wherehe makes the wound. Then he puts in adevice that looks somewhat like a blenderblade into the eye that works through a vortexaction. This basically breaks up the lens,allowing aspiration.
The potential advantage of Catarexseems to be that there should be no corneal
endothelial cell loss, in contrast to phaco,which even in good hands, may have a fourpercent endothelial cell loss or more. WithCatarex, since all maneuvering is done insidethe capsule with its tight seal, the endothe-lium should have no damage. The otherpotential advantage is that by working insidethe capsule this procedure might decreaseposterior capsular tears and eliminate irisdamage. All these potential advantagesshould provide us a safer operation.
Another potential advantage is that itis hoped Catarex may be easier thanphacoemulsification, which is a difficultoperation. If so, this would be a very positiveadvance from the perspective of public healthand the availability to many people that whocannot have phaco at present. Hopefully, thecost would be less.
Aziz PhacoTmesis
PhacoTmesis uses a spinning needlethat also has ultrasound. It is a very powerfulcutting tool.
Water Jet Technology
If you heat water to the right tempera-ture, about 55 to 60 degrees centigrade, youcan appear to melt the lens. There are severalcompanies working on a water jet type tech-nology to remove cataracts with basicallyheated balanced salt solution. It appears thatthis can be done without damaging the sur-rounding tissues from the heat either by usingan endocapsular method or by having shortpulses of the heated material directed at thecataract with cool material circulating in theanterior chamber.
The latter two methods mentionedabove seem to be brilliant ideas but it isunclear whether they can be translated intopractical reality.

THE ART AND THE SCIENCE OF CATARACT SURGERY
412
BIBLIOGRAPHY
Anis, AY: PhacoTmesis. Atlas of Cataract Sur-gery, Edited by Masket S. & Crandall AS, pub-lished by Martin Dunitz Ltd., 1999, 12:89-96.
Colvard DM, Kratz RP: Cataract surgery utilizingthe erbium laser. In: Fine IH, ed. Phacoemulsifica-tion: New Technology and Clinical Application(Thorofare, NJ: Slack, 1996), 161-80.
Dodick, JM: The Nd:YAG laser phacolysis tech-nique. Boyd’s World Atlas Series of OphthalmicSurgery of HIGHLIGHTS. 1995; 5:130-131.
Dodick JM, Christian J: Experimental studies onthe development and propagation of shock wavescreated by the interaction of short Nd:YAG laserpulses with a titanium target: possible implica-tions for Nd:YAG laser phacolysis of the catarac-tous human lens. J Cataract Refract Surg 1991;17:794-7.
Kanellopoulos AJ, Dodick JM, Brauweiler P,Alzner, E: Dodick photolysis for cataract surgery.Early experience with the Q-switchedneodymium:YAG laser in 100 consecutive patients.Ophthalmology, 1999;106:2197-2202.
Kratz RP, Mirhashemi S, Mittelstein M, SorensenJT: The Catarex technology. Atlas of Cataract Sur-gery, Edited by Masket S. & Crandall AS, pub-lished by Martin Dunitz Ltd., 1999, 11:85-88.