Cancer Bone Metasis
-
Upload
bhartinder -
Category
Documents
-
view
225 -
download
0
description
Transcript of Cancer Bone Metasis

New therapeutic targets for cancerbone metastasisJing Y. Krzeszinski1 and Yihong Wan1,2
1 Department of Pharmacology, The University of Texas Southwestern Medical Center, Dallas, TX 75390, USA2 Simmons Cancer Center, The University of Texas Southwestern Medical Center, Dallas, TX 75390, USA
Review
Bone metastases are dejected consequences of manytypes of tumors including breast, prostate, lung, kidney,and thyroid cancers. This complicated process beginswith the successful tumor cell epithelial–mesenchymaltransition, escape from the original site, and penetrationinto the circulation. The homing of tumor cells to thebone depends on both tumor-intrinsic traits and variousmolecules supplied by the bone metastatic niche. Thecolonization and growth of cancer cells in the osseousenvironment, which awaken their dormancy to formmicro- and macro-metastasis, involve an intricate inter-action between the circulating tumor cells and localbone cells including osteoclasts, osteoblasts, adipo-cytes, and macrophages. We discuss the most recentadvances in the identification of new molecules andnovel mechanisms during each step of bone metastasisthat may serve as promising therapeutic targets.
Bone metastasisMore than 600 000 cases of cancer bone metastasis arediagnosed every year in the USA [1]. Bone is the third mostcommon site for metastatic disease (after lung and liver)and more prevalent in adult patients (>40 years of age)[2]. Notorious for causing severe pain, bone metastases arealso the major reasons for pathologic fracture, life-threat-ening hypercalcemia, spinal cord compression, immobility,and ultimate mortality in patients afflicted with advancedcancers in the breast, prostate, lung, kidney, thyroid, aswell as with hematologic malignancies such as myeloma[3].
Great progress has been made in the medical manage-ment of bone metastases including surgery approaches andradiation therapy, as well as targeted medical therapy.However, these strategies are at best only palliative and donot improve overall patient survival [4]. The challenges toidentify more effective and specific molecularly targetedtherapy to prevent and cure bone metastases as wellas enhance the quality of life in these patients remaindaunting.
Cancer bone metastasis refers to the ability of cancercells to leave a primary tumor, travel through circulation,and form a secondary tumor in the distant bone tissue. It
0165-6147/
� 2015 Elsevier Ltd. All rights reserved. http://dx.doi.org/10.1016/j.tips.2015.04.006
Corresponding author: Wan, Y. ([email protected]).Keywords: tumor-intrinsic factors; bone metastatic niche; bone microenvironment;macrometastasis; osteoclast; osteoblast.
360 Trends in Pharmacological Sciences, June 2015, Vol. 36, No. 6
comprises five steps: (i) escape from the primary tumor;(ii) invade into lymphatic and/or blood vessels; (iii) surviveand travel in the circulation; (iv) land on the bone; and(v) finally flourish in the new bone environment [5,6](Figure 1). Every step of cancer bone metastasis is tightlyregulated by tumor cells, with the cooperation and assis-tance from non-cancerous cells (Figure 1). In this review,potential new therapeutic targets in every step of cancermetastasis discovered over the past 2 years will bediscussed.
Escape from the original siteEpithelial to mesenchymal transition (EMT)
Tumor progression is often facilitated by both intrinsicgenetic changes and alterations in the local environment.Although still under debate, increasing evidence suggeststhat activation of the EMT process is essential to allowcarcinoma cells to undergo fundamental cytoskeleton re-organization to lose cohesiveness for single cell migrationand escape [7]. Numerous molecules have been reportedto be involved in this process. The classical marker of EMTis cadherin switching, in which E-cadherin is lost andN-cadherin is gained [8]. Transcription factors that regu-late junctional proteins such as E-cadherin, b-catenin [9]and integrin [10], along with miRNAs and alternativesplicing have been reported to play important roles inthe EMT [11].
EMT is commonly thought to promote general metasta-sis; however, Smith et al. proposed an interesting hypoth-esis that EMT activators, that also stimulate theexpression of RANKL, a major cytokine for the differenti-ation of the bone-resorbing osteoclasts from their myeloidprogenitors, could drive the tumor cells specifically to thebone. They found that the pro-EMT factor Snail couldusher prostate cancer cells to bone and stimulate tumor-bone vicious cycle through calcium and RANKL signaling[12]. Croset and colleagues also reported TWIST1, a well-known EMT-inducing transcription factor, as a contributorto breast cancer bone metastasis through upregulating theexpression of miR-10b, a proinvasive factor [13]. By com-paring immunohistochemical expression of EMT markers(i.e., E-cadherin, vimentin, NF-kB, Notch-1, ZEB1, andPDGF-D) in prostate cancer specimens (primary and bonemetastasis) containing both tumor and adjacent normaltissues, Sethi et al. identified Notch-1 as a signature genefor the acquisition of EMT in prostate cancer and its bonemetastases [11]. With the advances in profiling methodol-ogies, we expect to see more bone metastasis-specific

EMT
ECMdegrada�on
Angiogenesis
Intravasa�on
P2Y2
Integrins, cadherins,hA, etc.
Adhesion of tumorcells to the bone
SDF-1
CXCR4
RANK
TGF-β, IGFs, FGFs, etc.
RANKLPDGFR, CCL5, etc.
CXCR7, IL-11,IL-8, IGFBP2,DDR1, etc.
Bone-derivedgrowth factors
Osteoblas�c factors:ET1, BMP, FGF,PDGF, etc.
Osteoblas�c factors:PTHrP, interleukins,SRC, microRNAs, etc.
Lipidtrafficking
M1-M2macrophagepolariza�on
(A) Escape from the primary siteand invade into circula�on
(B) Survive in the circula�on
(C) Home to bone
(D) Thrive in the bone microenvironment
Platelet
Key:
Tumor cell NK cell Osteoclast Osteoblast Osteocyte Macrophage Adipocyte
TRENDS in Pharmacological Sciences
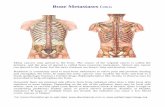
Figure 1. Multiple steps in cancer bone metastasis and the major regulatory factors in the tumor–bone microenvironment. The cellular basis of cancer progression includes
tumor cell local invasion, intravasation, survival in the circulation, extravasation, colonization, and proliferation in the bone. In the primary site, tumor cells undergo EMT,
ECM degradation, and angiogenesis to invade vascular or lymphatic circulation (A). After intravasation, a few tumor cells can survive from NK cell attack with the assistance
of platelets (B). Through communication between tumor-intrinsic factors and factors in the osseous environment, cancer cells extravasate to the bone and marrow.
Interactions between tumor cells and bone cells mediated by adhesion molecules are crucial for colonization (C). After landing, tumor cells start to interact with local cells,
including osteoclasts, osteoblasts, adipocytes, and macrophages, to thrive in bone and form micro- and macrometastases (D).
Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
targets to be identified during the EMT process, the signifi-cance of which awaits functional validations using variousmolecular genetic and pharmacological approaches.
Hypoxia
Low oxygen level (hypoxia) also increases the malignantbehavior of cancer cells, predominantly via hypoxia-inducible factors (HIFs) [14]. Independently of establishedprognostic parameters, intratumoral hypoxia serves as anadverse indicator for patient prognosis [15]. The activatedHIFs induce the expression of pluripotency-associatedtranscription factors (Oct-3/4, Nanog, and Sox-2) [16],glycolysis- and EMT-associated molecules [17,18], as wellas angiogenic factors such as vascular endothelial growthfactor (VEGF) [19]. Consequently, targeting the HIF sig-naling network and the altered metabolic pathways repre-sent a promising strategy to improve the efficacy of currenttherapies against aggressive and metastatic cancers.
C-X-C chemokine receptor type 4 (CXCR4), osteopontin(OPN), and interleukin-6 and -8 (IL6 and IL8) are hypoxia/HIF-inducible genes in the bone-specific metastatic genesignature in some cell types [20]. In breast cancer cells,HIF-1a and HIF-2a stimulate EMT by potentiating Notchsignaling to upregulate SNAIL1 and SLUG – two transcrip-tion repressors of E-cadherin [21–23]. Inhibiting HIF-1activity significantly suppresses breast cancer metastasisto bone in animal models, establishing HIF-1 as a promisingtherapeutic target [24]. Hypoxia also stabilizes growth ar-rest-specific 6 (GAS6)/AXL receptor tyrosine kinase signal-ing in metastatic prostate cancer [25]. Interestingly,transcutaneous CO2 application not only decreases HIF-1a and increases apoptosis, but also suppresses pulmonarymetastases in highly metastatic osteosarcoma cells, sug-gesting that reoxygenation via a novel transcutaneous CO2
treatment could be a therapeutic breakthrough for metas-tasis suppression in osteosarcoma patients [26].
361

Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
Cancer invasionDegradation of the extracellular matrix (ECM)
Invasion of carcinoma cells requires degradation of ECM,which forms the structural framework for most tissues andis composed of fibrous proteins (such as collagens, elastins,fibronectins, and laminins) and proteoglycans (such aschondroitin sulfate, heparan sulfate, keratan sulfate,and hyaluronic acid) [27]. Several genes related to theECM have elevated expression in highly metastatic tumors[28]. Transforming growth factor b (TGF-b) plays a crucialbut complicated role in not only the synthesis but alsothe degradation of ECM [29]. Various types of proteinasesare implicated in ECM degradation, but the major enzymesare considered to be matrix metalloproteinases (MMPs),which are Zn2+-endopeptidases that cleave the constitu-ents of the ECM. MMP-2 and MMP-9 are the predominantMMPs responsible for ECM protein degradation, and thusplay key roles in tumor development, growth, and metas-tasis [30]. miR-29c has recently been reported to suppresslung cancer cell adhesion to ECM and metastasis by tar-geting integrin b1 and MMP2, and thus represents a noveltherapeutic target for lung cancer metastasis [31].
Angiogenesis
After ECM degradation by MMPs, endothelial cells areattracted by the angiogenic stimuli produced by the tumorcells to migrate into the perivascular space and form newblood vessels [32]. This is a highly regulated process thatinvolves essential signaling pathways such as VEGF,VEGF receptors (VEGFRs), anti-angiogenic factors (e.g.,thrombospondin-1), pro-angiogenic factors (e.g., HIFs),Notch, and several ECM proteins [33]. Angiogenesis,regarded as a prerequisite for cancer metastasis, has beenstudied extensively. FDA-approved bevacizumab, a mono-clonal antibody against VEGF-A, was the first commerciallyavailable angiogenesis inhibitor that has been clinicallyused to treat metastatic colorectal, lung, breast, and renalcancers [34]. Cabozantinib, a dual inhibitor of VEGFR2and receptor tyrosine kinase MET, has exhibited beneficialeffects on radiographically evident bone metastases [35,36].Researchers have also generated other inhibitors forVEGFRs, including sunitinib, sorafenib, and cediranib[37], as well as aflibercept – a small recombinant proteinthat acts as a decoy receptor for VEGFs [38]. However, noneof these drugs have been proven to afford a survival advan-tage. This suggests that angiogenesis inhibitors may requirecoadministration of other therapies or dual-pathway block-ade to achieve clinical gains [36].
Intravasation and extravasation
Blood vessels formed by tumor-induced local angiogenesisare generally leaky, with weak cell–cell junctions, throughwhich cancer cells can enter vasculature [39]. By compar-ing peripheral blood plasma in patients with breast cancerbone metastases to healthy volunteers, Martinez and col-leagues found that the plasma from patients can inducetrans-endothelial migration of MCF-7 cells (a humanbreast adenocarcinoma cell line). These findings indicatethat there are circulating factors in these patients thatmay promote intravasation, angiogenesis, survival, andEMT of circulating tumor cells [40].
362
Genes mediating specialized cancer cell extravasationrequired for bone metastasis have also been identified.A comparison of the expression profiles in bone-metastatichuman breast cancer sublines with the parental cell lineidentified several mediators of bone metastasis, in partic-ular CXCR4, IL-11, OPN, and MMP1, the combination ofwhich is sufficient to enhance osteolytic metastasis whenoverexpressed in the parental cell line [41]. Subsequently,several other profiling and microarray studies have beenpublished using different types of tumor cells, revealingseveral other potentially important bone metastasis tar-gets that require further functional characterization infuture research [42–45].
Survival in the circulationAfter intravasation, a few tumor cells are able to survive inthe circulation through the expression of various genes,cooperating with other cell types, and at the same timeevading immune system recognition to establish metasta-ses at distant sites upon extravasating from the vessels.Priming by platelets and surface shielding from naturalkiller (NK) cells are thought to be the major approachesthat circulating tumor cells (CTCs) utilize to survive anddevelop into metastasis [46]. Experimental models ofbreast cancer and melanoma show that platelets enhancemetastasis [47]. Interestingly, ATP released from plateletsis found to be required for platelet-dependent tumor celltransmigration; moreover, ATP-induced tumor cell extrav-asation and metastasis depends on the endothelial pur-inergic P2Y2 receptor [48]. It has also been shown thatplatelet-derived TGFb and direct platelet–tumor cell con-tacts synergistically activate the TGFb/Smad and NF-kBpathways in cancer cells, enabling the tumor cells formetastasis by transitioning to an invasive mesenchymal-like phenotype [49]. Tumor-intrinsic factors are alsoreported to assist tumor survival. Prostate cancer cellsevade NK cell immunity by secreting core2 b-1,6-N-acetylglucosaminyltransferase (C2GnT), a key enzyme inthe formation of core2 branched O-glycans [50]. CTCs haverecently attracted significant attention owing to their po-tential as an early prognostic marker for the clinical man-agement of metastatic breast cancer patients [51,52].Furthermore, analysis of patient-derived CTCs for thera-peutic gene targets could possibly lead to the developmentof personalized treatment regimens to prevent metastasis[53].
Homing to the boneTumor cells, bone cells, and tumor–bone interactions allhave been shown to contribute to the colonization of cancercells in bone.
Factors secreted from tumor cells
Different types of cancers exhibit different tropism todevelop metastases in different organs. Factors secretedby tumor cells can alter the microenvironment at distantorgan sites, generating pre-metastatic niches for subse-quent metastatic cancer cell colonization. There is ampleevidence showing that chemokines and their receptors playa key role in organ-specific cancer metastasis. The best-studied are CXCR4 and its ligand stromal-derived factor-1

Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
(SDF-1). SDF-1, produced by several bone marrow celltypes including osteoblast, is known to be important inhematopoietic stem cell homing to the bone marrow.CXCR4, expressed by multiple bone-metastatic tumorsincluding breast, prostate, and multiple myeloma, controlsthe metastatic destination of cancer cells by directing themto organs where SDF-1 is highly produced, such as bonemarrow [54]. This makes disruption of the CXCR4/SDF-1axis an attractive therapeutic strategy to prevent tumorcell spreading to bone. CTCE-9908, a peptide analog ofSDF-1 and a competitive inhibitor of CXCR4, reduces thesize of metastatic lesions derived from MDA-MB-231 hu-man breast cancer cells, following injection into the leftcardiac ventricle of nude mice [55]. Plerixafor/AMD3100, asmall-molecule CXCR4 antagonist, also delays metastaticoutgrowth of orthotopically transplanted 4T1 mouse breastcancer cells [56]. However, within the bone microenviron-ment, SDF-1 and CXCR4 appear to have conflicting roles.Genetic disruption of CXCR4 in the hematopoietic cellsturns to enhance osteoclast activity and thereby stimulatestumor cell growth in bone [57]. In short, the effects of theCXCR4/SDF-1 axis on tumor cell growth within the boneare not yet fully defined. Furthermore, there are theoreti-cal risks that blockade of this chemokine axis could impairmany important physiological processes that include stemcell homing, angiogenesis and immune cell trafficking[58]. As such, caution should be taken when designingtherapeutic strategies targeting CXCR4/SDF-1 to specifi-cally block the tumor cells.
Besides CXCR4, C-X-C motif chemokine 7 (CXCR7) hasalso been uncovered as a second SDF-1 receptor whichexerts a similar function to CXCR4 in tumor development[59]. Azab et al. found that inhibition of CXCR7 delayedtumor progression in multiple myeloma by specificallyabrogating the trafficking of angiogenic mononuclear cells,rather than through direct effects on tumors, demonstrat-ing a novel role of CXCR7 in the recruitment of angiogenicmononuclear cells to areas of multiple myeloma in the bonemarrow niche [60].
Similarly, C-X-C motif chemokine 10 (CXCL10) hasbeen reported to facilitate the trafficking of C-X-C chemo-kine receptor type 3 (CXCR3)-expressing cancer cells tobone, which augments its own production, enhances tumorgrowth, and at the same time promotes osteoclastic differ-entiation, indicating that the CXCL10/CXCR3 axis may beanother attractive therapeutic target for osteolytic metas-tasis [61].
Additional secretory proteins from metastatic tumor cellshave been discovered to function as autocrine or paracrinesignals that mediate crosstalk between different cell types tofacilitate tumor cell colonization in bone. Several cytokineproducts of breast cancers, such as parathyroid hormone-related protein (PTHrP) [62], IL-11 [63], and IL-8 [64], havebeen shown to modify host osseous environment to promoteosteoclast formation and bone colonization. More recently,adrenomedullin, a small peptide secreted by breast cancercells and increased by hypoxia, has been found to potentiateosteolytic responses to metastatic breast cancer cells. Over-expression of adrenomedullin in breast tumor cells acceler-ated osteolytic bone metastasis development, increasedosteoclast activity and decreased survival; whereas a
small-molecule adrenomedullin antagonist dramaticallysuppressed both tumor burden in bone and osteoclast activ-ity [65]. Insulin-like growth factor binding protein 2(IGFBP2) secreted from metastatic breast cancer cellsrecruits endothelia by modulating insulin-like growth factor1 (IGF1) activation of the IGF type-I receptor on endothelialcells; whereas c-Mer tyrosine kinase (MERTK) receptorcleaved from metastatic cells promotes endothelial recruit-ment by competitively antagonizing the binding of its ligandGAS6 to endothelial MERTK receptors. Interestingly,miRNA-126, targeting both IGFBP2 and MERTK, sup-presses metastatic endothelial recruitment, metastaticangiogenesis, and breast cancer metastatic bone coloniza-tion [66]. A set of miRNAs, including miR-126 and miR-135,were lost in the breast cancer cells with high bone metastaticpotential. Restoration of their expression in cancer cellssignificantly inhibits tumorigenesis and bone metastaticcolonization [67].
Three genes, encoding the cytokine IL-1b, the chemo-kine CXCL6 (GCP-2), and the protease inhibitor elafin(PI3), are positively associated with the occurrence ofskeletal metastases in animal models inoculated withhuman prostate cancer cells. Further studies showed thatIL-1b can promote skeletal colonization of prostate can-cer cells [68]. By performing mass spectrometry on con-ditioned media from isolated PCa-118b prostate tumorcells, which came from an osteoblastic bone lesion gener-ated by a patient-derived xenograft, Lee and colleaguesidentified 26 secretory proteins that may regulate pros-tate cancer bone colonization, including TGF-b2, growthdifferentiation factor 15 (GDF15), fibroblast growthfactor 3 (FGF3), fibroblast growth factor 19 (FGF19),C-X-C motif chemokine 1 (CXCL1), galectins, and b2-microglobulin [69].
In lung cancer bone metastases, inhibition of collagenreceptor discoidin domain receptor-1 (DDR1) reduces cellsurvival, homing, and bone colonization [70]. Receptor ofactivated protein C (EPCR) promotes tumor cell survivaland is negatively correlated with the clinical outcome inlung adenocarcinoma (AC) patients. Genetic silencing orantibody blockade of EPCR leads to strong abrogation ofbone metastasis [71]. Simultaneous silencing of histonedeacetylase 4 (HDAC4), paired-like homeodomain1 (PITX1),and roundabout axon guidance receptor homolog 1 (ROBO1)decreases bone metastatic ability of lung adenocarcinoma[72]. Hyperactive canonical WNT/TCF signaling throughLEF1 and HOXB9 enhances the competence of lung adeno-carcinoma to metastasize to the bone and brain [73]. Inaddition, overexpression of miR-335 in small cell lung cancer(SCLC) downregulates IGF1 receptor and RANKL, leadingto reduced bone metastases [74].
In melanomas, exosomes derived from highly metastatictumors have been shown to promote the mobilization of bonemarrow cells through upregulation of proinflammatorymolecules at pre-metastatic sites via the receptor tyrosinekinase MET. Moreover, these exosomes also induce vascularleakiness at pre-metastatic sites and reprogram bone mar-row progenitors toward a pro-vasculogenic phenotype. Con-sequently, the production and transfer of these exosomesincrease the incidence and burden of metastatic diseases[75].
363

Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
Hematopoietic stem cell (HSC) niche
The concept of the HSC niche was first proposed by RaySchofield in 1978 [76]. It is the microenvironment whereHSCs are thought to reside in the bone marrow, and hasbeen proposed to comprise several cell types such as vas-cular endothelium and endosteal osteoblasts [77,78]. Com-ponents of the HSC niche have also been indicated asfertile ground for the development of bone metastases.Some evidence supports the hypothesis that bone meta-static cancer cells disseminate in the same manner as howHSCs home to bone marrow – such as via the CXCR4/SDF1axis [79,80].
A prostate cancer model suggests that HSCs colocalizewith prostate tumor cells at the endosteal bone surfacesin vivo and in vitro, indicating a niche competition [81]. Iftumor cells target HSC niche, then it is rational to hypoth-esize that bone metastasis can be altered by manipulatingthe size of the niche. Indeed, niche expansion by parathy-roid hormone (PTH) treatment resulted in significantlymore tumor cells in the bone marrow [82]. Although thedetailed mechanisms still remain unclear, several factorshave been implicated in how tumor cells hijack the HSCniche. Binding to the niche osteoclasts induces the expres-sion of TRAF family member-associated NF-kB activator(TANK) binding kinase 1 (TBK1) in prostate tumor cellsPC3 and C4-2B. An increased TBK1 level enhances tumorcell survival and drug resistance in the bone microenvi-ronment by inhibiting mTOR function [83]. Gas6, a ligandfor AXL and MER, is produced by the HSC niche. Gas6 canstimulate the survival of prostate tumor cells by inducingtumor dormancy through AXL [84]. Consistent with thisnotion, the Gas6/MER interaction also protects metastaticleukemia cells from chemotherapy-induced apoptosis [85].
Moreover, HSC-derived bone morphogenic proteins(BMPs), such as BMP2 and BMP6, can promote osteoblastdifferentiation [86]. Osteoblasts in turn maintain the end-osteal HSC niche, creating a positive feedback loop be-tween HSCs and osteoblasts, which leave an openopportunity for prostate cancer cells to alter the regulationof normal bone formation by HSCs through BMPs signal-ing pathway [87]. BMPs are also involved in both HSCquiescence and tumor cell dormancy, therefore represent-ing promising candidates for therapeutic targeting of bonemetastases [88,89].
Factors secreted from bone cells
One of the most interesting features of mammalian skele-ton is its ability to continuously remodel and renew itself.During this process of degrading and reforming bones,abundant factors are secreted from bone cells and bonematrix into the osseous environment.
TGF-b is one of the most abundant cytokines releasedfrom stromal cells. It stimulates tumor cell expression ofPTHrP, which activates osteoclasts [90]. Osteoclasts, inturn, resorb bone and release TGF-b from bone matrix topromote tumor cell proliferation and survival, forming a‘vicious cycle’. Inhibition of TGF-b with small molecules orneutralizing antibodies can reduce osteolytic lesion andtumor burden in tibial injection mouse models for bothbreast cancer and melanoma [91,92]. Interestingly, Li et al.suggested that loss of stromal TGF-b responsiveness in the
364
fibroblast instead promoted bone metastasis of prostatecancer cells, and this might be mediated by increasedexpression of cytokines CXCL1 and CXCL16, and thusaugment prostate cancer cell adhesion to the bone matrix[93].
High serum levels of IGFs are linked to high risk forbreast, prostate, and colorectal cancer. Studies in animalmodels and in humans have established crucial roles forIGFs in skeletal growth and development [94]. As for bonemetastases, neutralizing antibody against IGF type I re-ceptor (IGF-IR), but not to other bone-secreted factors suchas TGF-b, fibroblast growth factors (FGFs), or platelet-derived growth factors (PDGFs), blocks breast cancer boneanchorage. This supports a unique and important role ofbone-derived IGF-I in the crosstalk between the bonemicroenvironment and the cancer cells [95].
FGFs are a family of widely expressed polypeptideligands that regulate a broad spectrum of physiologicalprocesses via FGF receptors (FGFRs). FGF signaling hasbeen shown to mediate a positive feedback loop betweenprostate cancer cells and bone cells. Augmented expressionof FGF ligands and FGF receptors activates multiplemechanisms to promote prostate tumorigenesis and me-tastasis [96]. Two small-molecule tyrosine kinase inhibi-tors that can block FGFR function, dovitinib andnintedanib, are currently in clinical trials for metastaticcastration-resistant prostate cancer as well as for meta-static renal cell carcinoma (RCC) [96,97]. The antitumorand anti-bone-metastasis activity of dovitinib has beenshown to be mediated by FGFR1 inhibition in osteoblastsrather than in cancer cells, hence improving bone qualityand blocking cancer–bone interaction. This may accountfor clinical observations of dovitinib effects such as reduc-tions in lesion size and intensity on bone scans, lymph nodesize, and tumor-specific symptoms without proportionaldeclines in serum prostate-specific antigen level [98]. Thesestudies suggest that FGFR inhibition may represent apromising new therapeutic strategy to treat advancedcancers and bone metastasis.
Beyond these well-studied ‘classical’ bone secretedmolecules, several new factors have been recently identi-fied as key partners-in-crime for tumor bone metastasis.PDGF is secreted by bone stroma. Functional disruption ofPDGF receptor (PDGFR) can alter heterotypic tumor–stromal and tumor–matrix interactions in lung cancer,thereby preventing efficient engagement required for bonehoming and osseous colonization [99]. In addition, CCL5secreted from bone marrow MSCs can promote the migra-tion and invasion of hepatocellular carcinoma cells (HCCs),thus representing a potentially important factor in HCCbone metastasis [100].
Adhesion of tumor cells to bone cells
Adhesion between tumor cells and bone marrow stromalcells is crucial for cancer colonization in distant bonetissues. Integrins are a family of transmembrane receptorsthat function as the bridges for cell–cell and cell–ECMinteractions, thus playing major role in this adhesionprocess. So far, avb3 integrin has been the focus of moststudies. Various in vivo and in vitro experiments suggestthat avb3 integrin increases the potential of human and

(A) Osteoly�c lesion (B) Osteoblas�c lesion
TRENDS in Pharmacological Sciences
Figure 2. Illustration of osteolytic and osteoblastic bone metastatic lesions. Cancer
causes predominantly two types of bone metastatic lesions based on the
radiological appearance, with bone destruction being observed in osteolytic
bone metastatic lesions (A), while bone-forming phenotypes are observed in
osteoblastic bone metastatic lesions (B).
Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
murine breast cancer cells to form bone metastases[101–103]. ATN-161, a fibronectin-derived peptide knownto interfere with integrin avb1 and avb3 binding, hascompleted Phase I and II clinical trials [104]. In a preclini-cal animal model using intra-cardiac injection of MDA-MB-231 human breast cancer cells into nude mice, ATN-161treatment resulted in a remarkable reduction in the inci-dence and number of bone metastases, supporting a crucialrole for these integrin heterodimers in cancer osteotropism[105].
Cadherins are another family of cell adhesion moleculesthat have been implicated in the colonization of cancer cellsto distant organs. Cadherin-11 was originally identified inmouse osteoblasts and is known to regulate bone develop-ment [106]. It was later found that the level of cadherin-11expression increased when primary prostate cancer devel-oped into metastatic disease, especially in bone[107,108]. The same phenotype was also observed in breastcancer patients, indicating that cadherin-11 is specificallyassociated with bone metastasis of multiple cancers[109]. Cadherin-11 is proposed to mediate the binding oftumor cells to osteoblasts, thereby promoting cancer cellcolonization in bone [107,108].
Recently it was reported that heterotypic adherentjunctions (hAJs), that involve cancer-derived E-cadherinand osteogenic N-cadherin, play a key role in mediating theinteraction between cancer cells and osteogenic cellsin vitro and in vivo [110]. Interestingly, treatment withtrans-2-phenylcyclopropylamine hydrochloride (PCPA), aninhibitor of the chromatin-modifying protein lysinedemethylase 1 (LSD1), induced the expression of E-cad-herin and other epithelial markers. PCPA treatmentmarkedly suppressed the migration and invasion of tri-ple-negative breast cancer cells and attenuated bone me-tastasis without affecting lung infiltration, when MDA-MB-231 cells were injected directly into the blood circula-tion of nude mice [111]. There may be several possibleexplanations for these seemingly contrasting observations.First, cancer cell E-cadherin may play different roles in thepre- and post-metastatic sites – suppressing EMT in theprimary tumor but facilitating bone adhesion and coloni-zation in the bone metastatic niche. Second, other epithe-lial markers upregulated by PCPA may play different andperhaps more dominant roles compared to E-cadherin, driving the anti-metastatic outcome.
Protein glycosylation has also been suggested to modu-late bone metastasis. b-Galactoside a-2,3-sialyltransferase(ST3GAL6), an important factor in selectin ligand synthe-sis, was found to be highly expressed in multiple myelomacells and patients. Selectins are a family of cell adhesionmolecules that are composed of single-chain transmem-brane glycoproteins. Knockdown of ST3GAL6 attenuatedmultiple myeloma cell adhesion and migration in vitro, andreduced the ability of these cells to home to the bonemarrow in vivo, resulting in a reduction in tumor burdenand prolonged survival in an xenograft mouse model[112]. In an adhesion assay using a flow device, P-selectinwas found to induce strong adherence to cells expressingCXCR4, such as cancer cells, especially when SDF-1 iscoexpressed on the surface of bone marrow stromal cells.This indicates a potential synergistic effect of P-selectin
and SDF-1 in promoting cancer cell adhesion and bonecolonization [113].
CD44 is an adhesion molecule that binds to ECM andprimarily to hyaluronan (HA). It is recognized as a poten-tial cancer stem cell marker, and has also been suggestedto promote bone metastasis by enhancing tumorigenicity,cell motility, and HA production in a breast cancer xeno-graft model. As such, CD44–HA interaction has beensuggested as a potential novel target for therapeutic inter-vention for bone metastasis [114].
Bone microenvironment and macrometastasesBone provides a unique environment in which multiple celltypes co-reside and interact, including hematopoietic cellssuch as osteoclasts and immune cells, mesenchymal cellssuch as osteoblasts, osteocytes, and adipocytes, as well ascells forming the vasculature such as endothelial cells andpericytes. After successfully landing on bone, tumor cellsstart to mingle with the local bone cells and coerce themto create a hospitable environment for cancer cells tosurvive and thrive, using several different approachesand molecules.
Cancer cells influence bone cells mainly in two ways.Most often, the cancer cells manipulate the osteoclastlineage to increase osteoclast differentiation and activity.When this osteoclastic bone resorption supersedes osteo-blastic bone formation, osteolytic metastatic lesions occurin which the excessive bone degradation leaves ‘cavities’ inthe mineralized tissue where tumor cells reside, as oftenseen in X-ray images (Figure 2A). Sometimes, the cancercells also release substances to manipulate the osteoblastlineage to increase osteoblast differentiation and new bonedeposition. When this osteoblastic bone formation super-sedes osteoclastic bone resorption, osteoblastic metastaticlesions similar to sclerosis occur in which the excessivebone growth leaves ‘bulges’ in the mineralized tissue where
365

Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
tumor cells reside, which are also discernible in X-rayimages (Figure 2B). Although there is more bone deposi-tion in these osteoblastic lesions, their structure is abnor-mal, leading to weak bones and fractures. The distinctionbetween these two types of lesions is not absolute. Manypatients with bone metastases have both osteolytic andosteoblastic lesions, and individual metastatic lesion cancontain both osteolytic and osteoblastic components(Table 1). Mechanistically, osteoclasts have been shownto play a pro-metastatic role in both types of lesions.
Osteoclasts
In osteolytic bone metastases, tumor cells enhance osteo-clast formation by continuingly secreting pro-osteoclasto-genic factors including PTHrP, RANKL, interleukins,prostaglandin E, tumor necrosis factor (TNF), and macro-phage colony stimulating factor (MCSF). Conversely, oste-oclastic bone resorption releases growth factors, such asTGFb, IGFs, PDGFs, and BMPs, from the bone matrix toenhance tumor growth. This ‘tumor–osteoclast coopera-tion’ is the major foundation of the ‘vicious cycle’ hypothe-sis [115]. Clinically, anti-resorptive drugs have beenproven to be effective to slow down the process of cancerbone metastasis.
Bisphosphonates are a group of pyrophosphate analogsthat preferentially bind to calcium, which is mainlystored in bone in vertebrates. When attached to bone,bisphosphonates are ingested by osteoclasts and kill theosteoclasts [116]. Moreover, bisphosphonates can exertbeneficial effects not only via their anti-angiogenic proper-ties but also by their anticancer activity [117–121]. Thus,bisphosphonate therapy is currently a standard of care forpatients with malignant bone disease. This osteoclastpoisoning tactic has been used to restrict skeletal metas-tases for many tumor types, including prostate, breast,lung, and multiple myeloma [122]. Denosumab, a fullyhuman monoclonal antibody against RANKL, has alsobeen approved for the treatment of osteoporosis and fordelaying skeletal-related events in patients with bonemetastases secondary to breast or prostate cancer [123].
TGF-b is a major bone responder to tumor signals. Over-production of active TGF-b by osteoclastic bone resorption inthe skeletal metastasis setting not only increases tumor cellinvasiveness and angiogenesis but also induces immuno-suppression. Thus, blocking the TGF-b signaling pathway tointerrupt the vicious cycle between cancer and bone offers apromising therapeutic approach [124]. TGF-b neutralizingantibodies (1D11, Fresolimumab), tyrosine kinase inhibi-tors (LY2109761, LY2157299), and soluble decoy receptorproteins have been developed and tested in preclinicalstudies as well as in clinical trials for their efficacy ininhibiting cancer bone metastasis [125,126].
Table 1. Different bone lesions in cancer bone metastasis
Osteolytic Osteoblastic Mixed
Renal cell carcinoma
Melanoma
Multiple myeloma
Non-small cell
lung cancer
Thyroid cancer
Prostate cancer
Carcinoid
Small cell lung
cancer
Breast cancer
Gastrointerstinal
cancers
Squamous cancers
366
SRC (protooncogene SRC, Rous sarcoma) is an oncogeneencoding a tyrosine kinase that promotes cellular prolifer-ation, differentiation, motility, and survival. It is alsohighly expressed in osteoclasts and essential for the orga-nization of osteoclast cytoskeleton [127,128]. Moreover,SRC inhibits RUNX2 target genes, and thus negativelyimpacts upon osteoblast differentiation [129]. Owing to themultiple roles of SRC in osteoclasts, osteoblasts and tumorcells, targeting SRC has been the center of investigation.Dasatinib (a SRC inhibitor) and saracatinib (a dual inhibi-tor of SRC and ABL) are currently being evaluated inmultiple clinical trials for their efficacy in skeletal andmetastatic diseases [130,131].
Although the ability of these osteoclast inhibitor drugsin controlling bone metastases deterioration is encourag-ing, significant challenges lie ahead. First, the side effectsof currently approved drugs, such as osteonecrosis of thejaw (ONJ), hypocalcemia, and renal toxicity [132–134], arehard to ignore; second, and more importantly, in fact noneof these drugs can actually cure bone metastases or in-crease long-term survival, begging for better pharmacolog-ical strategies. Hence, researchers continue to investigatetumor influence on osteoclasts in the search for new andbetter therapeutic targets.
Identification of miRNAs that play key functions inbone-specific metastasis is a major breakthrough. Elland colleagues reported that miR-141 and miR-219 caninhibit osteoclast differentiation and experimental bonemetastases in a xenograft mouse model. Moreover, miR-16and miR-378 may have diagnostic potential as circulatingbiomarkers for osteolytic bone metastases [135]. Thesefindings highlight miRNAs as exciting new strategies forthe diagnosis and treatment of cancer skeletal metastasis.
Similarly, our laboratory has uncovered miR-34a asa potent suppressor of osteoclast differentiation, boneresorption, and skeletal metastasis, and it functionsthrough inhibiting the homeobox transcription factor Tgif2(TGFb inducible factor 2) [136]. Osteoclastic miR-34a over-expressing transgenic mice exhibit decreased osteoclasto-genesis and bone resorption, as well as higher bone mass,leading to resistance to osteoporosis and bone metastasis ofbreast cancer and melanoma. Conversely, miR-34a knock-out mice display enhanced osteoclastogenesis and boneresorption, leading to lower bone mass and exacerbatedcancer bone metastasis. Pharmacologically, systemic deliv-ery of a miR-34a mimetic via chitosan-based nanoparticleseffectively targets the circulating osteoclast progenitors toimpede the development of osteoporosis and cancer metas-tasis to the bone. These findings reveal miR-34a as a poten-tial therapeutic strategy to confer skeletal protectionand ameliorate bone metastasis of cancers [136]. Moreover,miR-34a was originally identified as a p53 target that isfrequently deleted in several types of human cancer [137],and pharmacological miR-34a treatment in mouse modelsexhibited efficacy to suppress tumor growth and lungmetastasis via the inhibition of CD44 [138]. Therefore,miR-34a therapy may confer multiple benefits at both pre-and post-metastatic sites in combating cancer malignancy.
Interestingly, recent studies reveal that specificmiRNAs are released from cancer cells within microvesiclesor exosomes, which can then be taken in by other local cells.

Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
For example, when overexpressed in bone metastatic lungcancer cells, miR-192 can be transferred to endothelial cellsto inhibit angiogenesis; systemic delivery of miR-192 candecrease osteolytic lesions in a mouse model [139]. Hence,both cell-intrinsic and exosome-delivered miRNAs repre-sent potential powerful therapeutic targets to attenuateosseous metastases of cancers.
Osteoblasts
Osteoblasts produce and deposit growth factors into thebone matrix, such as TGF-b and IGFs, which are inactiveuntil released and activated by osteoclastic bone resorptionin osteolytic metastases [140]. In addition to turning offosteoclast functions, it is proposed that another strategy toameliorate the bone loss is to turn on osteoblast functions[141]. Proteasome inhibitors are reported to promote boneformation by stimulating progenitor proliferation and oste-oblast differentiation. Bortezomib is the first FDA-approvedtherapeutic proteasome inhibitor, which demonstrates effi-cacy in the treatment of both multiple myeloma and lym-phomas in humans [142]. Interestingly, bortezomib has alsobeen shown to inhibit breast cancer osteolytic metastasis inpreclinical models [141]. Future clinical studies will benecessary to assess the therapeutic benefits of bortezomibon bone metastasis of solid tumors in patients.
In the osteoblastic bone metastases, there is also avicious cycle between tumor cells and osteoblasts. Tumorcells produce osteoblast-stimulating factors such as BMPs,FGFs and PDGF. Tumor cells also activate endothelin-1(ET-1), which downregulate Dkk1, a negative regulatorof osteoblastogenensis [143]. The activated osteoblastsproduce factors including IL-6, monocyte chemotactic pro-tein-1 (MCP-1), VEGF, and macrophage inflammatoryprotein-2 (MIP-2), which in turn assist cancer cell coloni-zation and amplification upon arrival in the bone microen-vironment. In particular, endothelins and their receptorsare emerging as plausible targets for osteoblastic bonemetastasis. Inhibition of ET-1 is reported to have dualsuppressive effects on both tumor cells and osteoblasts.ET-1 promotes cancer cell proliferation and invasion viaupregulating MMPs, inhibiting apoptosis, and enhancingVEGF-induced angiogenesis [144]. ET-1 also increasesosteoblast differentiation by reducing Dkk1. Both ET-1neutralizing antibodies and ET-A receptor antagonists(ABT-627) are under clinical evaluation [145,146]. The roleof osteoblasts in skeletal metastasis is less well defined –whether they are pro-metastatic or anti-metastatic maydepend on multiple factors such as the type of cancer cellsand whether the lesion is more osteolytic or osteoblastic.
Adipocytes
Adipocytes are another important component in the bonemarrow environment. The number of marrow adipocytesincreases greatly with aging and obesity, which are alsorisk factors for the development of metastatic cancers.Marrow adipocytes secrete hormones, cytokines, and fattyacids that may have profound effects on hematopoieticniches, neighboring bone cells, and inflammation, henceshaping the local milieu, hematopoiesis, and skeletal ho-meostasis [147]. It has been suggested that tumor cells canalso be attracted to marrow adipocytes and are affected by
adipokines. The interaction between these two cell typesmay create a chronic inflammatory environment that ispro-tumorigenic, as well as promoting the translocation ofadipocyte-stored lipids to the metastatic tumor cells, caus-ing increased motility in tumor cells [147–149].
Marrow adipocytes may promote tumor growth in bonein an FABP4-dependent manner. FABP4 is a cytosolic lipidchaperone that is predominantly expressed in adipocytes,macrophages, and endothelial cells. Adipocyte FABP4 istranscriptionally regulated by insulin and fatty acids, thelatter of which function as agonists for the nuclear receptorperoxisome proliferator associated receptor g (PPARg)[150]. Herroon et al. propose that FABP4 inhibition canblock lipid trafficking between marrow adipocytes andcancer cells, thus reducing the formation of tumor metas-tases in bone and marrow. These studies reveal adipocyteFABP4 as a potential driving mechanism for skeletalmetastasis [151]. Clearly, marrow adipocytes affect cancerbone metastasis; however, little is known about how ex-actly marrow fat cells modulate tumor colonization andmacrometastasis in the skeleton. Detailed genetic andmolecular studies will be necessary in the future to delin-eate the underlying mechanism and elucidate new thera-peutic targets for the fat–bone–cancer connection.
Macrophages
Macrophages, derived from myeloid progenitors, are alsoan important component of bone marrow. Genetic dissec-tion suggests that cathepsin K (CTSK) from macrophages,in addition to osteoclasts, plays a key role in promotingprostate cancer progression in bone [152]. Macrophagesare classified into two main subsets that can be distin-guished by their regulation of inflammation: M1 macro-phages that generally promote inflammation, and M2macrophages that typically suppress inflammation andassist tissue repair [153]. When associated with tumors,M1 macrophages have been proposed to be anti-tumorigenicby releasing reactive oxygen species, nitrogen intermedi-ates, and inflammatory cytokines to kill cancer cells;while M2 macrophages are generally considered to bepro-tumorigenic by releasing a variety of growth factors,such as FGFs and VEGF, that promote tumor growth andinvasion [154]. Rac2, a small GTPase, that facilitates mac-rophage M1 to M2 polarization, was reported to promotetumor metastasis [155].
Hiraoka et al. used clodronate-packaged liposomes(Cl2MDP-LIP) to deplete monocytes and macrophages,in addition to osteoclasts, to broadly assess the effects ofthese cells on cancer metastasis in a metastatic lung cancercell cardiac injection mouse model. They found that target-ing both macrophage and osteoclast by CI2MDP-LIP treat-ment showed a more pronounced reduction in the numberand size of bone metastatic lesions compared to the soleosteoclast-targeting agent reveromycin A [156]. Anotherstudy showed that anti-CD115 antibody can deplete tu-mor-associated macrophages, leading to decreased osteo-lytic bone lesions in nude mice transplanted with MDA-MB-231 human breast cancer cells via cardiacinjection [157].
By contrast, elevated expression of hyaluronan synthase2 (HAS2) in metastatic tumor cells was shown to be crucial
367

Table 2. Molecular targets and current drugs for cancer bone metastasis
Molecular targets Mechanisms Agents/drugs Refs
Escape of cancer cells from the original site
Snail Stimulates EMT and the tumor–bone vicious cycle [12]
TWIST1 Promotes breast cancer bone metastasis through
mir-10b
[13]
Notch1 Signature gene for the acquisition of EMT in prostate
cancer bone metastases
[11]
HIF1 Induced by hypoxia to stimulate EMT Transcutaneous CO2
treatment
[24–26]
Invasion of cancer cells
MMP2/MMP9 Cleave the constituents of the ECM [30]
miR-29c Suppresses lung cancer cell adhesion to ECM and
metastasis
[31]
VEGF receptors Essential for angiogenesis Bevacizumab
Cabozantinib
Sunitinib, sorafenib,
and cediranib
Aflibercept
[34]
[35,36]
[37]
[38]
P2Y2 Important for ATP-induced tumor cell extravasation [48]
C2GnT Protects cancer cells from NK cell immunity [50]
Homing to the bone
Tumor cell secreted factors
CXCR4/SDF-1 axis Attract cancer cells to the HSC niche CTCE-9908
Plerixafor/AMD3100
[54,55]
[56]
CXCR7 Promotes tumor progression by recruiting angiogenic
mononuclear cells
[60]
CXCL10/CXCR3 axis Enhance tumor growth and osteoclast differentiation [61]
Adrenomedullin Increases osteoclast activity [65]
IGFBP2, MERTK Recruit endothelia microRNA-126 [66]
TGF-b2, GDF15, FGF3,
FGF19, CXCL1, galectins
and b2-microglobulin
Highly expressed in the conditioned medium from
isolated osteoblastic bone lesion cancer cells
[69]
DDR1 Associated with cancer cell survival and homing on bone [70]
EPCR Promotes cancer cell survival [71]
HDAC4, PITX1, ROBO1 Promote lung adenocarcinoma bone metastasis [72]
Canonical WNT/TCF Enhance both bone and brain metastasis [73]
HSC niche
PTH Expands HSC niche [82]
TBK1 Inhibits mTOR function and enhances cancer cell
survival
[83]
Gas6 Induces cancer cell dormancy [84,85]
BMP2, 6 Promote osteoblast differentiation, maintain HSC niche,
and regulate cancer cell dormancy
[86–89]
Bone cell secreted factors
IGFs Modulate both bone microenvironment and cancer cells [94,95]
FGFs Mediate a positive feedback loop between cancer cells
and bone cells
Dovitinib
Nintedanib [96–98]
PDGFR Associated with cancer bone-homing and osseous
colonization
[99]
CCL5 Promotes cancer cell migration and invasion [100]
Adhesion of tumor cells to bone cells
avb3 integrin Promotes cancer bone colonization ATN-161 [101–105]
Cadherin-11 Mediates binding of cancer cells to osteoblasts [106–109]
hAJs Mediate the interaction between cancer cells and
osteogenic cells
[110]
ST3GAL6 Generates single-chain transmembrane glycoproteins;
participates in cancer cell adhesion and migration [112]
P-selectin Induces strong adherence to cells expressing CXCR4 [113]
CD44 Binds to ECM and primarily to HA [114]
Bone microenvironment and macrometastasis
Osteoclast
Calcium/RANKL/TGFb Main factors of tumor–osteoclast vicious cycle Bisphosphonates
Denosumab
1D11, Fresolimumab
LY2109761, LY2157299
[116–122]
[123]
[124–126]
Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
368

Table 2 (Continued )
Molecular targets Mechanisms Agents/drugs Refs
SRC Promotes osteoclasts and inhibits osteoblasts Dasatinib
saracatinib [127–131]
miR-16, miR-378 Potential circulating biomarkers for osteolytic bone
metastasis
[135]
miR-34a Inhibits osteoclast differentiation by suppressing Tgif2,
and impedes cancer progression at both pre- and post-
metastatic sites as a p53 target and a CD44 inhibitor
[136–138]
miR-192 Inhibits angiogenesis and decrease osteolytic lesions [139]
Osteoblast
Proteasome inhibitors Promote bone formation Bortezomib [141,142]
ET-1 Promotes cancer cell invasion and osteoblast
differentiation
ABT-627 [143–146]
Adipocyte
FABP4 Regulates lipid trafficking between marrow adipocytes
and cancer cells
[150,151]
Macrophage
Rac2 Facilitates macrophage M1 to M2 polarization [155]
HAS2 Increases secretion of PDGFs from macrophages [158]
Box 1. Experimental models for bone metastasis imaging
The development of experimental animal models for the imaging
and quantification of cancer bone metastasis has significantly
facilitated our research endeavor. These are mainly transplantation
mouse models using luciferase-labeled bone metastasis-prone cell
lines, such as MDA-MB-231 human breast cancer cell sublines [41],
4T1.2 mouse mammary tumor cell line [159], B16-F10 mouse
malignant melanoma cell line [160], and the TSU-Pr1-B1/B2 human
bladder cancer cell line [161]. These cell lines can develop bone
metastasis when injected intracardiacally and in some cases
orthotopically. Recently, GFP-labeled bone metastasis-prone cell
lines, such as human lung cancer H460 cells [162] and human
prostate cancer PC-3 cells [163], have been generated to image bone
metastasis when a single highly-fluorescent subcutaneously grow-
ing tumor is transplanted by surgical orthotopic implantation. In
addition, GFP-labeled mouse melanoma B16 and human melanoma
LOX cell lines [164], as well as in vivo-selected highly metastatic
MDA-MB-435-GFP human breast cancer cells [165], can also develop
bone metastasis. Interestingly, PC3-GFP cells have been used to
show that fluorescence-guided surgery significantly reduced recur-
rence of experimental prostate cancer bone metastasis compared
with bright-light surgery; and the combination of fluorescence-
guided surgery and zoledronic acid increased disease-free survival
versus bright-light surgery and zoledronic acid [166]. Challenges for
future investigation will be to establish genetic animal models that
recapitulate the entire process of cancer bone metastasis, as well as
patient-derived cancer cell xenograft models that can predict
patient-specific propensity for bone metastasis as well as patient-
specific efficacy of potential treatments.
Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
for the interaction between tumor cells and macrophages inbone, resulting in an increased secretion of PDGFs frommacrophages, which then activated stromal cells and pro-moted cancer cells self-renewal. Thus, HAS2 inhibitors wereproposed as potential anti-metastatic agents that disrupt amacrophage-tumor paracrine growth factor loop within thismicroenvironment [158].
The contribution of macrophages to tumor growth,progression, and metastasis has been the subject of intenseinvestigation in the past few years. However, there islittle direct evidence that clearly demonstrates a suppres-sive effect of macrophages on bone metastasis, mainlybecause most strategies for depletion and/or inhibition ofmacrophages, as well as for manipulating macrophageintrinsic factors, also target osteoclasts at the same time.
Concluding remarksCancer bone metastasis is a highly complicated processthat involves not only tumor cells themselves but alsomultiple other cell types at both pre-metastatic andpost-metastatic sites. Potential molecular markers havebeen identified in the early stages of metastasis to diagnoseor predict skeletal metastatic events in advanced cancers(Table 2). For the subsequent steps of cancer homing andmacrometastasis in bone, accumulating evidence hasrevealed an intricate network by which tumor cells interactwith many local bone cells to form a vicious cycle andorchestrate successful skeletal metastasis (Table 2).
This cancer–bone feedforward loop provides ampleopportunities for therapeutic targeting to prevent andtreat bone metastasis of advanced cancers. Because mostcurrent regimens only attenuate the progression of exist-ing bone metastasis, and do not confer long-term survival,a therapeutic strategy targeting the early stages will behighly desirable to inhibit EMT, eradicate cancer stemcells, halt the dissemination of circulating tumor cells,as well as to prevent bone colonization and micrometas-tasis formation. The major goals and challenges for futureinvestigation reside in the following aspects: (i) early bio-markers, ideally circulating factors, for the prediction and
diagnosis of metastatic disease need to be identified andclinically validated; (ii) genetic or humoral factors thatallow the assessment of cancer cell dormancy need to beexplored; (iii) better characterization of the mechanisms bywhich osteoclasts, osteoblasts, marrow adipocytes, andmacrophages influence bone metastasis of various cancersis required; (iv) therapeutic approaches that can simulta-neously target multiple components in multiple steps dur-ing cancer bone metastasis are needed to more effectivelyprevent and eliminate cancer malignancy; (v) pharmacolog-ical agents that specifically target the mechanismsemployed by the tumor cells and their interaction with nichecells, without overtly interfering normal physiological
369

Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
functions, will promise less side effects and an improvedquality of life for the patients; and, finally (vi) new andalternative experimental animal models need to be estab-lished, such as genetic models that can recapitulate theentire process of cancer bone metastasis, as well as pa-tient-derived cancer cell xenograft models that can predictpatient-specific propensity for bone metastasis as well aspatient-specific efficacy of potential treatments (Box 1).Increasing numbers of molecular targets and mechanismsare being discovered by researchers, which will lead togreater understanding of the etiology of cancer bone metas-tasis. These new advances will ultimately facilitate innova-tions for not only effective and safe agents to treat but alsoefficient diagnostic approaches to predict and finally preventcancer bone metastasis.
AcknowledgmentsWe thank all the investigators whose studies have contributed to theunderstanding of cancer bone metastasis but could not be cited here dueto space limitation. Y.W. is a Virginia Murchison Linthicum Scholar inMedical Research. This work was supported in part by the CancerPrevention Research Institute of Texas (CPRIT) (RP130145, Y.W.), theUS Department of Defense (W81XWH-13-1-0318, Y.W.), NationalInstitutes of Health (NIH, R01DK089113, Y.W.), Mary Kay Foundation(#073.14, Y.W.), Simmons Cancer Center (Y.W.), Welch Foundation(I-1751, Y.W.), UT Southwestern Endowed Scholar Startup Fund (Y.W.),NIH T32 Training Grant (J.Y.K.), and a National Cancer Institute (NCI)Cancer Center Support Grant (5P30CA142543).
References1 Randall, R.L. (2014) A promise to our patients with metastatic bone
disease. Ann. Surg. Oncol. 21, 4049–40502 Davila, D. et al. (2015) Evaluation of osseous metastasis in bone
scintigraphy. Semin. Nucl. Med. 45, 3–153 Quinn, R.H. et al. (2014) Contemporary management of metastatic
bone disease: tips and tools of the trade for general practitioners.Instr. Course Lect. 63, 431–441
4 Taubenberger, A.V. (2014) In vitro microenvironments to study breastcancer bone colonisation. Adv. Drug Deliv. Rev. 79–80C, 135–144
5 Jandial, R. (2013) Metastatic Cancer: Clinical and BiologicalPerspectives, CRC Press
6 Leber, M.F. and Efferth, T. (2009) Molecular principles of cancerinvasion and metastasis. Int. J. Oncol. 34, 881–895
7 Lamouille, S. et al. (2014) Molecular mechanisms of epithelial–mesenchymal transition. Nat. Rev. Mol. Cell Biol. 15, 178–196
8 van Roy, F. and Berx, G. (2008) The cell–cell adhesion moleculeE-cadherin. Cell. Mol. Life Sci. 65, 3756–3788
9 Peifer, M. et al. (1992) The vertebrate adhesive junction proteins beta-catenin and plakoglobin and the Drosophila segment polarity genearmadillo form a multigene family with similar properties. J. CellBiol. 118, 681–691
10 Hynes, R.O. (2002) Integrins: bidirectional, allosteric signaling machines.Cell 110, 673–687
11 Sethi, S. et al. (2010) Molecular signature of epithelial–mesenchymaltransition (EMT) in human prostate cancer bone metastasis. Am. J.Transl. Res. 3, 90–99
12 Smith, B.A. et al. (2014) Abstract C60: Snail transcription factorcontributes to bone metastasis in prostate and breast cancer cells.Cancer Epidemiol. Biomark. Prev. 23, C60
13 Croset, M. et al. (2014) TWIST1 expression in breast cancer cellsfacilitates bone metastasis formation. J. Bone Miner. Res. 29, 1886–1899
14 Semenza, G.L. (2010) Defining the role of hypoxia-inducible factor 1 incancer biology and therapeutics. Oncogene 29, 625–634
15 Vaupel, P. (2009) Prognostic potential of the pre-therapeutic tumoroxygenation status. Adv. Exp. Med. Biol. 645, 241–246
16 Mathieu, J. et al. (2011) HIF induces human embryonic stem cellmarkers in cancer cells. Cancer Res. 71, 4640–4652
17 Jing, S-W. et al. (2013) Hypoxia suppresses E-cadherin and enhancesmatrix metalloproteinase-2 expression favoring esophageal carcinoma
370
migration and invasion via hypoxia inducible factor-1 alpha activation.Dis. Esophagus 26, 75–83
18 Yang, M-H. et al. (2008) Direct regulation of TWIST by HIF-1alphapromotes metastasis. Nat. Cell Biol. 10, 295–305
19 Stoeltzing, O. et al. (2003) Regulation of hypoxia-inducible factor-1alpha, vascular endothelial growth factor, and angiogenesis by aninsulin-like growth factor-I receptor autocrine loop in humanpancreatic cancer. Am. J. Pathol. 163, 1001–1011
20 Lu, X. and Kang, Y. (2010) Hypoxia and hypoxia-inducible factors:master regulators of metastasis. Clin. Cancer Res. 16, 5928–5935
21 Chen, J. et al. (2010) Hypoxia potentiates Notch signaling in breastcancer leading to decreased E-cadherin expression and increased cellmigration and invasion. Br. J. Cancer 102, 351–360
22 Lundgren, K. et al. (2009) Hypoxia, Snail and incomplete epithelial-mesenchymal transition in breast cancer. Br. J. Cancer 101, 1769–1781
23 Xing, F. et al. (2011) Hypoxia-induced Jagged2 promotes breast cancermetastasis and self-renewal of cancer stem-like cells. Oncogene 30,4075–4086
24 Dunn, L.K. et al. (2009) Hypoxia and TGF-beta drive breast cancerbone metastases through parallel signaling pathways in tumor cellsand the bone microenvironment. PLoS ONE 4, e6896
25 Mishra, A. et al. (2012) Hypoxia stabilizes GAS6/Axl signaling inmetastatic prostate cancer. Mol. Cancer Res. 10, 703–712
26 Harada, R. et al. (2013) Reoxygenation using a novel CO2 therapydecreases the metastatic potential of osteosarcoma cells. Exp. CellRes. 319, 1988–1997
27 Gilkes, D.M. et al. (2014) Hypoxia and the extracellular matrix:drivers of tumour metastasis. Nat. Rev. Cancer 14, 430–439
28 Eckhardt, B.L. et al. (2005) Genomic analysis of a spontaneous modelof breast cancer metastasis to bone reveals a role for the extracellularmatrix. Mol. Cancer Res. 3, 1–13
29 Hubmacher, D. and Apte, S.S. (2013) The biology of the extracellularmatrix: novel insights. Curr. Opin. Rheumatol. 25, 65–70
30 Coussens, L.M. et al. (2002) Matrix metalloproteinase inhibitors andcancer: trials and tribulations. Science 295, 2387–2392
31 Wang, H. et al. (2013) miRNA-29c suppresses lung cancer celladhesion to extracellular matrix and metastasis by targetingintegrin b1 and matrix metalloproteinase2 (MMP2). PLoS ONE 8,e70192
32 Papetti, M. and Herman, I.M. (2002) Mechanisms of normal andtumor-derived angiogenesis. Am. J. Physiol. Cell Physiol. 282,C947–C970
33 Dimova, I. et al. (2014) Angiogenesis in cancer – general pathways andtheir therapeutic implications. J. BUON 19, 15–21
34 Couzin-Frankel, J. and Ogale, Y. (2011) FDA. Once on ‘fast track’;avastin now derailed. Science 333, 143–144
35 Fay, A.P. et al. (2015) Current role of cabozantinib in metastaticcastration-resistant prostate cancer. Expert Rev. Anticancer Ther.15, 151–156
36 Schweizer, M.T. and Carducci, M.A. (2013) From bevacizumab totasquinimod: angiogenesis as a therapeutic target in prostate cancer.Cancer J. 19, 99–106
37 Petrillo, M. et al. (2012) Novel targets for VEGF-independent anti-angiogenic drugs. Expert Opin. Investig. Drugs 21, 451–472
38 Chu, Q.S-C. (2009) Aflibercept (AVE0005): an alternative strategy forinhibiting tumour angiogenesis by vascular endothelial growthfactors. Expert Opin. Biol. Ther. 9, 263–271
39 Weis, S.M. and Cheresh, D.A. (2011) aV integrins in angiogenesis andcancer. Cold Spring Harb. Perspect. Med. 1, a006478
40 Martinez, L.M. et al. (2014) Changes in the peripheral blood and bonemarrow from untreated advanced breast cancer patients that areassociated with the establishment of bone metastases. Clin. Exp.Metastasis 31, 213–232
41 Kang, Y. et al. (2003) A multigenic program mediating breast cancermetastasis to bone. Cancer Cell 3, 537–549
42 Conti, A. et al. (2014) Mapping protein signal pathway interaction insarcoma bone metastasis: linkage between rank, metalloproteinasesturnover and growth factor signaling pathways. Clin. Exp. Metastasis31, 15–24
43 Sieh, S. et al. (2014) Paracrine interactions between LNCaP prostatecancer cells and bioengineered bone in 3D in vitro culture reflectmolecular changes during bone metastasis. Bone 63, 121–131

Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
44 Wang, H. et al. (2013) Gene expression markers in circulating tumorcells may predict bone metastasis and response to hormonaltreatment in breast cancer. Mol. Clin. Oncol. 1, 1031–1038
45 Welch, D.R. (2004) Microarrays bring new insights into understandingof breast cancer metastasis to bone. Breast Cancer Res. 6, 61–64
46 Palumbo, J.S. et al. (2007) Tumor cell-associated tissue factor andcirculating hemostatic factors cooperate to increase metastaticpotential through natural killer cell-dependent and-independentmechanisms. Blood 110, 133–141
47 Coupland, L.A. et al. (2012) Platelets and P-selectin control tumor cellmetastasis in an organ-specific manner and independently of NKcells. Cancer Res. 72, 4662–4671
48 Schumacher, D. et al. (2013) Platelet-derived nucleotides promotetumor-cell transendothelial migration and metastasis via P2Y2receptor. Cancer Cell 24, 130–137
49 Labelle, M. et al. (2011) Direct signaling between platelets and cancercells induces an epithelial–mesenchymal-like transition and promotesmetastasis. Cancer Cell 20, 576–590
50 Okamoto, T. et al. (2013) Core2 O-glycan-expressing prostate cancercells are resistant to NK cell immunity. Mol. Med. Rep. 7, 359–364
51 Giuliano, M. et al. (2014) Circulating tumor cells as early predictors ofmetastatic spread in breast cancer patients with limited metastaticdissemination. Breast Cancer Res. 16, 440
52 Giuliano, M. et al. (2015) Circulating and disseminated tumor cellsfrom breast cancer patient-derived xenograft-bearing mice as a novelmodel to study metastasis. Breast Cancer Res. 17, 3
53 Mumford, B.S. and Robertson, G.P. (2014) Circulating melanoma cellsin the diagnosis and monitoring of melanoma: an appraisal of clinicalpotential. Mol. Diagn. Ther. 18, 175–183
54 Hirbe, A.C. et al. (2010) The CXCR4/SDF-1 chemokine axis: apotential therapeutic target for bone metastases? Curr. Pharm.Des. 16, 1284–1290
55 Richert, M.M. et al. (2009) Inhibition of CXCR4 by CTCE-9908inhibits breast cancer metastasis to lung and bone. Oncol. Rep. 21,761–767
56 Smith, M.C.P. et al. (2004) CXCR4 regulates growth of both primaryand metastatic breast cancer. Cancer Res. 64, 8604–8612
57 Hirbe, A.C. et al. (2007) Disruption of CXCR4 enhancesosteoclastogenesis and tumor growth in bone. Proc. Natl. Acad. Sci.U.S.A. 104, 14062–14067
58 Lapidot, T. and Kollet, O. (2002) The essential roles of the chemokineSDF-1 and its receptor CXCR4 in human stem cell homing andrepopulation of transplanted immune-deficient NOD/SCID andNOD/SCID/B2m(null) mice. Leukemia 16, 1992–2003
59 Burns, J.M. et al. (2006) A novel chemokine receptor for SDF-1 and I-TAC involved in cell survival, cell adhesion, and tumor development.J. Exp. Med. 203, 2201–2213
60 Azab, A.K. et al. (2014) CXCR7-dependent angiogenic mononuclearcell trafficking regulates tumor progression in multiple myeloma.Blood 124, 1905–1914
61 Lee, J-H. et al. (2012) CXCL10 promotes osteolytic bone metastasis byenhancing cancer outgrowth and osteoclastogenesis. Cancer Res. 72,3175–3186
62 Yin, J.J. et al. (1999) TGF-beta signaling blockade inhibits PTHrPsecretion by breast cancer cells and bone metastases development. J.Clin. Invest. 103, 197–206
63 Kang, Y. et al. (2005) Breast cancer bone metastasis mediated by theSmad tumor suppressor pathway. Proc. Natl. Acad. Sci. U.S.A. 102,13909–13914
64 Bendre, M.S. et al. (2002) Expression of interleukin 8 and notparathyroid hormone-related protein by human breast cancer cellscorrelates with bone metastasis in vivo. Cancer Res. 62, 5571–5579
65 Siclari, V.A. et al. (2014) Tumor-expressed adrenomedullin acceleratesbreast cancer bone metastasis. Breast Cancer Res. 16, 1693
66 Png, K.J. et al. (2012) A microRNA regulon that mediates endothelialrecruitment and metastasis by cancer cells. Nature 481, 190–194
67 Tavazoie, S.F. et al. (2008) Endogenous human microRNAs thatsuppress breast cancer metastasis. Nature 451, 147–152
68 Liu, Q. et al. (2013) Interleukin-1b promotes skeletal colonization andprogression of metastatic prostate cancer cells with neuroendocrinefeatures. Cancer Res. 73, 3297–3305
69 Lee, Y-C. et al. (2015) Secretome analysis of an osteogenic prostatetumor identifies complex signaling networks mediating cross-talk of
cancer and stromal cells within the tumor microenvironment. Mol.Cell Proteomics 14, 471–483
70 Valencia, K. et al. (2012) Inhibition of collagen receptor discoidin domainreceptor-1 (DDR1) reduces cell survival, homing, and colonization inlung cancer bone metastasis. Clin. Cancer Res. 18, 969–980
71 Anton, I. et al. (2012) Receptor of activated protein C promotesmetastasis and correlates with clinical outcome in lungadenocarcinoma. Am. J. Respir. Crit. Care Med. 186, 96–105
72 Luis-Ravelo, D. et al. (2014) A gene signature of bone metastaticcolonization sensitizes for tumor-induced osteolysis and predictssurvival in lung cancer. Oncogene 33, 5090–5099
73 Nguyen, D.X. et al. (2009) WNT/TCF signaling through LEF1 andHOXB9 mediates lung adenocarcinoma metastasis. Cell 138, 51–62
74 Gong, M. et al. (2014) miR-335 inhibits small cell lung cancer bonemetastases via IGF-IR and RANKL pathways. Mol. Cancer Res. 12,101–110
75 Peinado, H. et al. (2012) Melanoma exosomes educate bone marrowprogenitor cells toward a pro-metastatic phenotype through MET.Nat. Med. 18, 883–891
76 Schofield, R. (1978) The relationship between the spleen colony-forming cell and the haemopoietic stem cell. Blood Cells 4, 7–25
77 Kiel, M.J. et al. (2005) SLAM family receptors distinguishhematopoietic stem and progenitor cells and reveal endothelialniches for stem cells. Cell 121, 1109–1121
78 Xie, Y. et al. (2009) Detection of functional haematopoietic stem cellniche using real-time imaging. Nature 457, 97–101
79 Mu ller, A. et al. (2001) Involvement of chemokine receptors in breastcancer metastasis. Nature 410, 50–56
80 Taichman, R.S. et al. (2002) Use of the stromal cell-derived factor-1/CXCR4 pathway in prostate cancer metastasis to bone. Cancer Res.62, 1832–1837
81 Shiozawa, Y. et al. (2011) Human prostate cancer metastases targetthe hematopoietic stem cell niche to establish footholds in mouse bonemarrow. J. Clin. Invest. 121, 1298–1312
82 Calvi, L.M. et al. (2003) Osteoblastic cells regulate the haematopoieticstem cell niche. Nature 425, 841–846
83 Kim, J.K. et al. (2013) TBK1 regulates prostate cancer dormancythrough mTOR inhibition. NEO 15, 1064–1074
84 Shiozawa, Y. et al. (2010) GAS6/AXL axis regulates prostate cancerinvasion, proliferation, and survival in the bone marrow niche. NEO12, 116–127
85 Shiozawa, Y. et al. (2010) GAS6/Mer axis regulates the homing andsurvival of the E2A/PBX1-positive B-cell precursor acute lymphoblasticleukemia in the bone marrow niche. Exp. Hematol. 38, 132–140
86 Jung, Y. et al. (2008) Hematopoietic stem cells regulate mesenchymalstromal cell induction into osteoblasts thereby participating in theformation of the stem cell niche. Stem Cells 26, 2042–2051
87 Joseph, J. et al. (2012) Disseminated prostate cancer cells can instructhematopoietic stem and progenitor cells to regulate bone phenotype.Mol. Cancer Res. 10, 282–292
88 Grassinger, J. et al. (2007) Bone morphogenetic protein (BMP)-7 butnot BMP-2 and BMP-4 improves maintenance of primitive peripheralblood-derived hematopoietic progenitor cells (HPC) cultured inserum-free medium supplemented with early acting cytokines.Cytokine 40, 165–171
89 Kobayashi, A. et al. (2011) Bone morphogenetic protein 7 in dormancyand metastasis of prostate cancer stem-like cells in bone. J. Exp. Med.208, 2641–2655
90 Johnson, R.W. et al. (2011) TGF-beta promotion of Gli2-inducedexpression of parathyroid hormone-related protein, an importantosteolytic factor in bone metastasis, is independent of canonicalHedgehog signaling. Cancer Res. 71, 822–831
91 Bandyopadhyay, A. et al. (2006) Inhibition of pulmonary and skeletalmetastasis by a transforming growth factor-beta type I receptorkinase inhibitor. Cancer Res. 66, 6714–6721
92 Mohammad, K.S. et al. (2011) TGF-beta-RI kinase inhibitor SD-208reduces the development and progression of melanoma bonemetastases. Cancer Res. 71, 175–184
93 Li, X. et al. (2012) Loss of TGF-b responsiveness in prostate stromalcells alters chemokine levels and facilitates the development of mixedosteoblastic/osteolytic bone lesions. Mol. Cancer Res. 10, 494–503
94 Yakar, S. et al. (2010) IGF-1 and bone: New discoveries from mousemodels. J. Bone Miner. Res. 25, 2543–2552
371

Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
95 Hiraga, T. et al. (2012) Bone-derived IGF mediates crosstalk betweenbone and breast cancer cells in bony metastases. Cancer Res. 72,4238–4249
96 Corn, P.G. et al. (2013) Targeting fibroblast growth factor pathways inprostate cancer. Clin. Cancer Res. 19, 5856–5866
97 Motzer, R.J. et al. (2014) Dovitinib versus sorafenib for third-linetargeted treatment of patients with metastatic renal cell carcinoma:an open-label, randomised phase 3 trial. Lancet Oncol. 15, 286–296
98 Wan, X. et al. (2014) Prostate cancer cell-stromal cell crosstalk viaFGFR1 mediates antitumor activity of dovitinib in bone metastases.Sci. Transl. Med. 6, 252ra122
99 Catena, R. et al. (2011) PDGFR signaling blockade in marrow stromaimpairs lung cancer bone metastasis. Cancer Res. 71, 164–174
100 Bai, H. et al. (2014) CCL5 secreted from bone marrow stromal cellsstimulates the migration and invasion of Huh7 hepatocellularcarcinoma cells via the PI3K–Akt pathway. Int. J. Oncol. 45, 333–343
101 Felding-Habermann, B. et al. (2001) Integrin activation controlsmetastasis in human breast cancer. Proc. Natl. Acad. Sci. U.S.A.98, 1853–1858
102 Sloan, E.K. et al. (2006) Tumor-specific expression of alphavbeta3integrin promotes spontaneous metastasis of breast cancer to bone.Breast Cancer Res. 8, R20
103 Zhao, Y. et al. (2007) Tumor alphavbeta3 integrin is a therapeutictarget for breast cancer bone metastases. Cancer Res. 67, 5821–5830
104 Cianfrocca, M.E. et al. (2006) Phase 1 trial of the antiangiogenicpeptide ATN-161 (Ac-PHSCN-NH2), a beta integrin antagonist, inpatients with solid tumours. Br. J. Cancer 94, 1621–1626
105 Khalili, P. et al. (2006) A non-RGD-based integrin binding peptide(ATN-161) blocks breast cancer growth and metastasis in vivo. Mol.Cancer Ther. 5, 2271–2280
106 Kawaguchi, J. et al. (2001) Targeted disruption of cadherin-11 leads toa reduction in bone density in calvaria and long bone metaphyses. J.Bone Miner. Res. 16, 1265–1271
107 Huang, C-F. et al. (2010) Cadherin-11 increases migration andinvasion of prostate cancer cells and enhances their interactionwith osteoblasts. Cancer Res. 70, 4580–4589
108 Chu, K. et al. (2008) Cadherin-11 promotes the metastasis of prostatecancer cells to bone. Mol. Cancer Res. 6, 1259–1267
109 Tamura, D. et al. (2008) Cadherin-11-mediated interactions with bonemarrow stromal/osteoblastic cells support selective colonization ofbreast cancer cells in bone. Int. J. Oncol. 33, 17–24
110 Wang, H. et al. (2015) The osteogenic niche promotes early-stage bonecolonization of disseminated breast cancer cells. Cancer Cell 27, 193–210
111 Ferrari-Amorotti, G. et al. (2014) Suppression of invasion andmetastasis of triple-negative breast cancer lines by pharmacologicalor genetic inhibition of slug activity. NEO 16, 1047–1058
112 Glavey, S.V. et al. (2014) The sialyltransferase ST3GAL6 influenceshoming and survival in multiple myeloma. Blood 124, 1765–1776
113 Hedges, E.A. et al. (2014) Modulation of selectin-mediated adhesion offlowing lymphoma and bone marrow cells by immobilized SDF-1. Int.J. Mol. Sci. 15, 15061–15072
114 Hiraga, T. et al. (2013) Cancer stem-like cell marker CD44 promotesbone metastases by enhancing tumorigenicity, cell motility, andhyaluronan production. Cancer Res. 73, 4112–4122
115 Guise, T.A. (2002) The vicious cycle of bone metastases. J.Musculoskelet. Neuronal Interact. 2, 570–572
116 Li, B. et al. (2014) Treatment and prevention of bone metastases frombreast cancer: a comprehensive review of evidence for clinicalpractice. J. Clin. Med. 3, 1–24
117 Misso, G. et al. (2012) Evaluation of the in vitro and in vivoantiangiogenic effects of denosumab and zoledronic acid. CancerBiol. Ther. 13, 1491–1500
118 Santini, D. et al. (2002) Pamidronate induces modifications ofcirculating angiogenetic factors in cancer patients. Clin. CancerRes. 8, 1080–1084
119 Santini, D. et al. (2003) Zoledronic acid induces significant and long-lasting modifications of circulating angiogenic factors in cancerpatients. Clin. Cancer Res. 9, 2893–2897
120 Santini, D. et al. (2007) Repeated intermittent low-dose therapy withzoledronic acid induces an early, sustained, and long-lasting decreaseof peripheral vascular endothelial growth factor levels in cancerpatients. Clin. Cancer Res. 13, 4482–4486
372
121 Vincenzi, B. et al. (2003) Bisphosphonates: new antiangiogenicmolecules in cancer treatment? Ann. Oncol. 14, 806–807
122 Wu, S. et al. (2007) The use of bisphosphonates in cancer patients.Acta Oncol. 46, 581–591
123 Drooger, J.C. et al. (2013) Denosumab in breast cancer treatment.Eur. J. Pharmacol. 717, 12–19
124 Massague, J. (2008) TGFbeta in Cancer. Cell 134, 215–230125 Buijs, J.T. et al. (2011) TGF-b in the bone microenvironment: role in
breast cancer metastases. Cancer Microenviron. 4, 261–281126 Connolly, E.C. et al. (2012) Complexities of TGF-b targeted cancer
therapy. Int. J. Biol. Sci. 8, 964–978127 Koreckij, T. et al. (2009) Dasatinib inhibits the growth of prostate
cancer in bone and provides additional protection from osteolysis.Br. J. Cancer 101, 263–268
128 Saad, F. and Lipton, A. (2010) SRC kinase inhibition: targeting bonemetastases and tumor growth in prostate and breast cancer. CancerTreat. Rev. 36, 177–184
129 Marzia, M. et al. (2000) Decreased c-Src expression enhances osteoblastdifferentiation and bone formation. J. Cell Biol. 151, 311–320
130 Gucalp, A. et al. (2011) Phase II trial of saracatinib (AZD0530), an oralSRC-inhibitor for the treatment of patients with hormone receptor-negative metastatic breast cancer. Clin. Breast Cancer 11, 306–311
131 Hannon, R.A. et al. (2010) Effects of the Src kinase inhibitor saracatinib(AZD0530) on bone turnover in healthy men: a randomized, double-blind, placebo-controlled, multiple-ascending-dose phase I trial. J. BoneMiner. Res. 25, 463–471
132 Brown, J.E. and Coleman, R.E. (2012) Denosumab in patients withcancer-a surgical strike against the osteoclast. Nat. Rev. Clin. Oncol.9, 110–118
133 Coleman, R.E. (2012) Bone cancer in 2011: prevention and treatmentof bone metastases. Nat. Rev. Clin. Oncol. 9, 76–78
134 Khosla, S. et al. (2007) Bisphosphonate-associated osteonecrosis of thejaw: report of a task force of the American Society for Bone andMineral Research. J. Bone Miner. Res. 22, 1479–1491
135 Ell, B. et al. (2013) Tumor-induced osteoclast miRNA changes asregulators and biomarkers of osteolytic bone metastasis. Cancer Cell24, 542–556
136 Krzeszinski, J.Y. et al. (2014) miR-34a blocks osteoporosis and bonemetastasis by inhibiting osteoclastogenesis and Tgif2. Nature 512,431–435
137 Hermeking, H. (2007) p53 enters the microRNA world. Cancer Cell 12,414–418
138 Liu, C. et al. (2011) The microRNA miR-34a inhibits prostate cancerstem cells and metastasis by directly repressing CD44. Nat. Med. 17,211–215
139 Valencia, K. et al. (2014) miRNA cargo within exosome-like vesicletransfer influences metastatic bone colonization. Mol. Oncol. 8, 689–703
140 Guise, T.A. (2009) Breaking down bone: new insight into site-specificmechanisms of breast cancer osteolysis mediated by metalloproteinases.Genes Dev. 23, 2117–2123
141 Jones, M.D. et al. (2010) A proteasome inhibitor, bortezomib, inhibitsbreast cancer growth and reduces osteolysis by downregulatingmetastatic genes. Clin. Cancer Res. 16, 4978–4989
142 Richardson, P.G. et al. (2005) Bortezomib or high-dosedexamethasone for relapsed multiple myeloma. N. Engl. J. Med.352, 2487–2498
143 Clines, G.A. et al. (2007) Dickkopf homolog 1 mediates endothelin-1-stimulated new bone formation. Mol. Endocrinol. 21, 486–498
144 Carducci, M.A. and Jimeno, A. (2006) Targeting bone metastasis inprostate cancer with endothelin receptor antagonists. Clin. CancerRes. 12, 6296s–6300s
145 Chiao, J.W. et al. (2000) Endothelin-1 from prostate cancer cells isenhanced by bone contact which blocks osteoclastic bone resorption.Br. J. Cancer 83, 360–365
146 Pinto, A. et al. (2012) Targeting the endothelin axis in prostatecarcinoma. Tumour Biol. 33, 421–426
147 Hardaway, A.L. et al. (2014) Bone marrow fat: linking adipocyte-induced inflammation with skeletal metastases. Cancer MetastasisRev. 33, 527–543
148 Gazi, E. et al. (2007) Direct evidence of lipid translocation betweenadipocytes and prostate cancer cells with imaging FTIRmicrospectroscopy. J. Lipid Res. 48, 1846–1856

Review Trends in Pharmacological Sciences June 2015, Vol. 36, No. 6
149 Tokuda, Y. et al. (2003) Prostate cancer cell growth is modulated byadipocyte-cancer cell interaction. BJU Int. 91, 716–720
150 Furuhashi, M. and Hotamisligil, G.S. (2008) Fatty acid-bindingproteins: role in metabolic diseases and potential as drug targets.Nat. Rev. Drug Discov. 7, 489–503
151 Herroon, M.K. et al. (2013) Bone marrow adipocytes promote tumorgrowth in bone via FABP4-dependent mechanisms. Oncotarget 4,2108–2123
152 Herroon, M.K. et al. (2013) Macrophage cathepsin K promotesprostate tumor progression in bone. Oncogene 32, 1580–1593
153 Lawrence, T. and Natoli, G. (2011) Transcriptional regulation ofmacrophage polarization: enabling diversity with identity. Nat.Rev. Immunol. 11, 750–761
154 Zhang, M. et al. (2014) A high M1/M2 ratio of tumor-associatedmacrophages is associated with extended survival in ovariancancer patients. J. Ovarian Res. 7, 19
155 Joshi, S. et al. (2014) Rac2 controls tumor growth, metastasis and M1-M2 macrophage differentiation in vivo. PLoS ONE 9, e95893
156 Hiraoka, K. et al. (2008) Inhibition of bone and muscle metastases oflung cancer cells by a decrease in the number of monocytes/macrophages. Cancer Sci. 99, 1595–1602
157 Fend, L. et al. (2013) Therapeutic effects of anti-CD115 monoclonalantibody in mouse cancer models through dual inhibition oftumor-associated macrophages and osteoclasts. PLoS ONE 8, e73310
158 Okuda, H. et al. (2012) Hyaluronan synthase HAS2 promotes tumorprogression in bone by stimulating the interaction of breast cancerstem-like cells with macrophages and stromal cells. Cancer Res. 72,537–547
159 Lelekakis, M. et al. (1999) A novel orthotopic model of breast cancermetastasis to bone. Clin. Exp. Metastasis 17, 163–170
160 Uluckan, O. et al. (2008) APT102, a novel adpase, cooperates withaspirin to disrupt bone metastasis in mice. J. Cell. Biochem. 104,1311–1323
161 Chaffer, C.L. et al. (2005) Upregulated MT1–MMP/TIMP-2 axis in theTSU-Pr1-B1/B2 model of metastatic progression in transitional cellcarcinoma of the bladder. Clin. Exp. Metastasis 22, 115–125
162 Yang, M. et al. (1998) Widespread skeletal metastatic potential ofhuman lung cancer revealed by green fluorescent protein expression.Cancer Res. 58, 4217–4221
163 Yang, M. et al. (1999) A fluorescent orthotopic bone metastasis modelof human prostate cancer. Cancer Res. 59, 781–786
164 Yang, M. et al. (1999) Genetically fluorescent melanoma bone andorgan metastasis models. Clin. Cancer Res. 5, 3549–3559
165 Miwa, S. et al. (2014) Tumor-targeting Salmonella typhimurium A1-Rprevents experimental human breast cancer bone metastasis in nudemice. Oncotarget 5, 7119–7125
166 Miwa, S. et al. (2014) Fluorescence-guided surgery of prostate cancerbone metastasis. J. Surg. Res. 192, 124–133
373