C Blackwell Munksgaard 2003 Printed in Denmark. All rights ... articles/LR12/Pollanen... ·...
Transcript of C Blackwell Munksgaard 2003 Printed in Denmark. All rights ... articles/LR12/Pollanen... ·...
Periodontology 2000, Vol. 31, 2003, 12–31 Copyright C Blackwell Munksgaard 2003
Printed in Denmark. All rights reserved PERIODONTOLOGY 2000ISSN 0906-6713
Structure and function of thetooth–epithelial interface inhealth and diseaseM T. P, J I. S & V-J U
Introduction
Three types of mucous membranes (masticatory, lin-ing, and specialized) line the oral cavity and formthe structural boundary between the body and theexternal environment. Although each type of mu-cosa protects against mechanical and microbialdamage, the epithelia exhibit considerable differ-ences in their histology, thickness and differentiationsuitable for the functional demands of their location.Furthermore, the structure of different epithelia re-flects their effectiveness as a barrier to the penetra-tion of microbes and noxious agents into the deepertissues (141,160). Mucosal epithelia are composed ofcontinuously dividing and shedding populations ofkeratinocytes whose proliferation is confined to thebasal layer. The teeth, passing through the gingivalmasticatory mucosa, create a unique environmentalchallenge to the protective continuity. At the inter-face where the healthy gingiva meets the tooth sur-face the structural continuity is secured by the junc-tional epithelium attached to the tooth surface by adistinct mechanism known as the epithelial attach-ment apparatus (143). As opposed to the constantlyrenewing epithelia, teeth are units of nonsheddingsurfaces, which provide a solid substratum not onlyfor the attachment of the junctional epithelial cellsbut also for bacterial colonization and spreading inthe oral cavity. At the dentogingival junction the bac-terial colonies, exhibiting a variety of virulence fac-tors (68), pose a potential threat to the epithelialattachment. The attachment may be affected directlyby bacteria or indirectly through their ability to acti-vate inflammatory and immune processes, whichcontribute to the composition of the gingival crevicefluid (GCF) and thus to the conditions under which
12
the epithelial attachment apparatus is formed and/or maintained. In addition to the attachment, the re-newal rate and reparative capacity of the junctionalepithelial cells are equally important for the healthof the dentogingival junction. Accordingly, any de-generative episodes that involve the cells responsiblefor the attachment may gradually lead to the detach-ment of the junctional epithelium from the toothsurface and compromise the protective mucosalcontinuity.
Periodontal diseases are associated with bacterialplaque infecting the dentogingival margin and caus-ing inflammation in the underlying tissues (53,87).Logically, one of the main concerns of periodontalresearch has been to describe the inflammatory re-action in the adjacent tooth-supporting tissues andthe consequences it may have at the alveolar bonemargin (70,121,147). Less attention has been focusedon the effects of factors released from bacteria and/or from the inflammatory reaction on the junctionalepithelial cells. The precise mechanisms of epithelialdegeneration and/or activation leading to the de-tachment and apical migration of the junctional epi-thelial cells and consequent conversion of the gingi-val sulcus into an infected periodontal pocket havenot yet been discovered. This article deals with fac-tors associated with periodontal tissue protectionand destruction with special reference to the junc-tional epithelial cells.
Junctional epithelium
Schroeder and Listgarten first clarified the anatomyand histology of the dentogingival junction in theirmonograph: ‘Fine structure of developing epithelial
Tooth–epithelial interface in health and disease
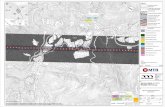
Fig. 1. Schematic illustration of the different epithelia atthe dentogingival junction. The junctional epithelium (JE)exhibits a distinct phenotype that allows the tissue to at-tach to the tooth surface and participate in the host de-fense in a number of ways.
attachment of human teeth’ (143). Since then,knowledge of the junctional epithelium has been re-viewed in numerous articles (90,142,144,161,168). Itis commonly accepted that the junctional epithel-ium exhibits several unique structural and func-tional features that contribute to preventing patho-genic bacterial flora from colonizing the subgingivaltooth surface. First, junctional epithelium is firmly
Fig. 2. Photomicrograph demonstrating the junctional ium into the sulcus. At the apical part of the junctionalepithelial DAT cells on the tooth surface (a). When the epithelium, cells (arrow) are seen to grow/proliferate intogingiva is displaced laterally the DAT cells are left on the the connective tissue (CT). A higher magnification (c) ofenamel (E) surface. The degeneration of the DAT cells ap- the apical part of the junctional epithelium. Note thepears to be a prerequisite for the apical advancement of dark-stained DAT cells along the cementum surface, thebacterial plaque (P). D Ω dentin. The junctional epithel- epithelial ‘finger’ proliferating apically and the absence ofium (JE) attached to tooth (to enamel or cementum (C) inflammatory infiltrate. Gingival epithelial cells grown onas in (b) forms a structural barrier against the bacterial decalcified dentin matrix (d) show apparent ability toplaque. Polymorphonuclear leukocytes that cover the extracellular collagenolysis (e).plaque (P) have migrated through the junctional epithel-
13
attached to the tooth and thus forms an epithelialbarrier against the plaque bacteria (Fig. 1 and 2a,b).Second, it allows the access of GCF, inflammatorycells and components of the immunological host de-fense to the gingival margin. Third, junctional epi-thelial cells exhibit rapid turnover, which contributesto the host–parasite equilibrium and rapid repair ofdamaged tissue (48). Although the importance of thejunctional epithelium in host defense is well recog-nized, an exact understanding of its role in thepathogenesis of periodontal diseases is largely miss-ing (Fig. 3). A major part of the older literature onjunctional epithelium describes its histological fea-tures at different stages of development or disease(113,141). More recent studies report on the distri-bution of cytoplasmic keratin filaments in the junc-tional epithelial cells, on different cell surface anti-gens and receptors, intercellular adhesion moleculesand details of the nonepithelial cells within the junc-tional epithelium and its nerve supply [for a reviewsee (142)]. These results consistently support theview that to be able to form a successful junctionbetween two dissimilar tissues and to respond in aflexible manner to the external environment, theepithelial cells responsible must have a distinct un-differentiated phenotype (160) (Fig. 4). The pheno-type of junctional epithelium, at least partly, reflectsa self-instructed adaptation of oral mucosa to the
Pöllänen et al.
existence of a solid tooth surface penetrating it(134,168). It is pertinent to suggest that the pheno-type required for epithelial adaptability may alsorender the cells vulnerable to the action of variousexogenous and endogenous agents. Since our under-standing of the pathogenic mechanisms that lead tofailure in junctional epithelium defense is limited,there is a clear need for fundamental research intothe junctional epithelial cells and their functionsunder different clinical conditions.
Epithelial attachment apparatus
The attachment of the junctional epithelium to thetooth is mediated through an ultramicroscopicmechanism defined as the epithelial attachment ap-paratus (143). It consists of hemidesmosomes at theplasma membrane of the cells directly attached tothe tooth (DAT cells) and a basal lamina-like extra-cellular matrix, termed the internal basal lamina, onthe tooth surface [Fig. 5 (80)]. By morphological cri-teria the internal basal lamina between the junc-tional epithelial DAT cells and the enamel is quitesimilar to the basement membrane between the epi-thelium and the connective tissue. However, by bio-chemical criteria the internal basal lamina differsessentially from the established basement mem-brane composition and thus from the external basallamina.
Fig. 3. The junctional epithelium (JE) is repeatedly or con-tinually exposed to bacterial challenges, which may leadto the failure of the junctional epithelium and eventuallyto subgingival plaque formation (brown), conversion ofthe gingival sulcus into a periodontal pocket and increasein the size of the inflammatory focus in the connectivetissue (gray).
14
The components of the internal basal lamina aresynthesized by the DAT cells in the absence of theimmediate vicinity of connective tissue (80,142).Internal basal lamina proteins include laminin andtype VIII collagen (128,130). Laminin, identified astype 5, is localized mainly to the optically electron-dense part of the internal basal lamina and it seemsto be associated with hemidesmosomes (69,93,100).Characteristically, the internal basal lamina lacks la-minin-1 and type IV collagen, which are componentsof true basement membranes (129,130). In addition,the internal basal lamina structure may involveother molecules that are unique to this structure (L.Häkkinen, unpublished results).
Hemidesmosomes have a decisive role in the firmattachment of the cells to the internal basal laminaon the tooth surface. Recent data suggest that thehemidesmosomes may also act as specific sites ofsignal transduction and, thus, participate in regula-tion of gene expression, cell proliferation and celldifferentiation (71). The intracellular part of hemi-desmosomes consists of at least two distinct pro-teins, the 230 kDa bullous pemphigoid antigen(BP230) and plectin, which is a high molecularweight cytomatrix protein (Fig. 5). These proteinsmediate the attachment of the epithelial cell cyto-plasmic keratin filaments to two transmembranecomponents of the hemidesmosome known as the180 kDa bullous pemphigoid antigen (BP180) anda6b4 integrin (71,174). The a6b4 integrin plays an im-portant role in the interaction of epithelial cells withthe extracellular matrix (101,127). This interactionutilizes the intracellular plectin connected throughthe b4-domain of the integrin to laminin-5 (ligandfor the a6b4 integrin) in the internal basal lamina(66,69,169). In general, the interaction between thedifferent components of the extracellular matrix andthe cell surface molecules linked to the intracellularcytoskeleton is fundamental for cell adhesion, cellmotility, synthetic capacity, tissue stability, regenera-tion and responses to external signals (175). Sincethe biochemical composition of internal basal lam-ina matrix differs from that of the true basementmembrane, the behavior of the attached DAT cellscannot be directly deduced from the data reportingon the behavior of basal cells that grow adjacent tothe external basal lamina (167).
Turnover of the junctional epithelial cells
The junctional epithelium is a stratified epitheliumcomposed of two strata, the basal layer facing theconnective tissue and the suprabasal layer extending
Tooth–epithelial interface in health and disease
to the tooth surface (Fig. 2 and 4). Coronally, close tothe sulcus, junctional epithelium is about 15 celllayers thick and narrows towards the apical part ofthe tissue. The turnover rate of junctional epitheliumis exceptionally rapid. In nonhuman primates it isabout 5 days and approximately twice the rate of theoral gingival epithelium (153). Previously it wasthought that only epithelial cells facing the externalbasal lamina were rapidly dividing. However, recentevidence indicates that a significant number of theDAT cells are, like the basal cells along the connec-tive tissue, capable of synthesizing DNA, which dem-
Fig. 4. Haematoxylin-eosin stainingof a clinically healthy human dento-gingival junction (a) shows an in-flammatory infiltrate in the connec-tive tissue (CT) lateral to the junc-tional epithelium (JE). Thejunctional epithelium exhibits widerintercellular spaces as compared tothe sulcular epithelium (SE). Thewide intracellular spaces allow theaccess of the components of the im-munological defense into the sulcus.DAT cells directly attached to thetooth are seen as a string lateral tothe enamel space (ES). Note the mostcoronal DAT cell («) that appears tobe supported only by the tooth andthus forms the medial wall of the sul-cus (see also schematic illustrationin Fig. 8). Reaction with a mono-clonal antibody to keratin 19 (b)shows that all the suprabasal junc-tional epithelial cells express thisprotein, as do the undifferentiatedbasal cells. The reaction with theantibody to keratin 10 shows thatterminal differentiation is a charac-teristic feature of the oral epithelium(OE) but not of the sulcular or junc-tional epithelia. The DAT cells alongthe tooth surface (d) are especiallyrich in K19.
15
onstrates their mitotic activity (133,135). At the co-ronal part of the junctional epithelium, the DAT cellstypically express a high density of transferrin recep-tors (131), which supports the idea of their activemetabolism and high turnover (172). The findingssuggest that the DAT cells have a more importantrole in tissue dynamics and reparative capacity ofthe junctional epithelium than has previously beenthought (143). Based on these data, alternativemodels for the turnover of DAT cells can be pro-posed (Fig. 6). The existence of a dividing populationof epithelial cells (DAT cells) in a suprabasal loca-
Pöllänen et al.
Fig. 5. A schematic illustration of a DAT cell shows thestructural and molecular composition of the epithelialattachment apparatus (EAA). N Ω nucleus of a DAT cell,IF Ω cytoplasmic keratin filaments (intermediate sizefilaments). The hemidesmosomes at the plasma mem-brane are associated with the a6b4 integrin that communi-cates with Ln-5 Ω laminin 5 located mainly in the internalbasal lamina, the extracellular domain (?) for BP180 is acollagenous protein (perhaps type VIII), that has not yetbeen definitely characterized. LL Ω lamina lucida, LD Ωlamina densa, SLL Ω sublamina lucida, IBL Ω internalbasal lamina.
tion, several layers from the connective tissue, is aunique feature of the junctional epithelium. The dis-tinct phenotype may result from specific permissiveor instructive signals provided by the internal basallamina matrix on the tooth surface. Therefore, anystructural or molecular changes in the internal basallamina can potentially influence the vital functionsof the DAT cells and contribute to the effectivenessor failure of the junctional epithelial defense or viceversa; changes in the cell metabolism, etc. may affectthe internal basal lamina.
Morphological studies of the internal basal laminaof teeth extracted because of advanced periodontitishave shown that remnants of the internal basal lam-ina can be detected even adjacent to severely de-generated DAT cells (111). Although the internalbasal lamina morphologically appears to be rela-tively resistant to external challenges its molecularstructures may still be altered, leading to changes ofthe DAT cell function. Indeed, it has been shown thatcertain matrix metalloproteinases from eukaryoticcells cleave laminin-5, exposing a cryptic molecular
16
site that triggers cell migration (49). It has not yetbeen shown, however, if bacterial proteinases canperform directly the same selective cleavage of lami-nin-5. Bacterial agents may thus indirectly triggermechanisms that lead to modulation of host cell be-havior. Hypothetically, even minor changes in cellmetabolism, biosynthetic activity or ability to divideand migrate may eventually lead to degenerationand detachment of the junctional epithelium/DATcells and allow pathogenic flora to grow on the ex-posed subgingival tooth surface. A wide variety ofbacterial species and their products, such as lipo-
Fig. 6. The mechanism of DAT cell turnover is not fullyunderstood. Considering the fact that the DAT cells areable to divide and migrate, three possible mechanismscan be proposed. These are (1) the daughter cells pro-duced by dividing DAT cells replace degenerating cells onthe tooth surface, (2) the daughter cells enter the exfoli-ation pathway and gradually migrate coronally betweenthe basal cells and the DAT cells to eventually break offinto the sulcus, or (3) epithelial cells move/migrate in thecoronal direction along the tooth surface and are replacedby basal cells migrating round the apical termination ofthe junctional epithelium.
Tooth–epithelial interface in health and disease
polysaccharides, lipoteichoic acids, short-chain fattyacids, and phospholipases, have been shown to af-fect adversely the metabolism of epithelial cells incultures, leading to changes in proliferation and/orproduction of cytokines and matrix metalloprotein-ases (43,44,64,118–120,156). Understanding of thepotential significance of these events in relation tothe pathogenesis of periodontal pocket formationcalls for further studies.
Junctional epithelium in theantimicrobial defense
Junctional epithelium consists of active populationsof cells and antimicrobial functions, which togetherform the first line of defense against microbial in-vasion into tissue (Fig. 7). Even though junctionalepithelial cell layers provide a barrier against bac-teria many bacterial substances, such as lipopolysac-charide, pass easily through the epithelium but haveonly limited access through the external basal lam-ina into the connective tissue (146). Both the inter-nal and external basal laminas act as barriers againstinfective agents.
Rapid turnover, as such, is an important factor inthe microbial defense of junctional epithelium (seebelow). Also, because the area covered by the divid-ing cells in the junctional epithelium is at least 50times larger than the area through which the epi-thelial cells desquamate into the gingival sulcus,there is a strong funnelling effect that contributes tothe flow of epithelial cells (145). Rapid shedding andeffective removal of bacteria adhering to epithelialcells is therefore an important part of the anti-microbial defense mechanisms at the dentogingivaljunction.
There is increasing evidence indicating that sev-eral specific antimicrobial defense systems exist inthe oral mucosa. Many epithelial cell types, includ-ing junctional epithelium, have been found to con-tain enzyme-rich lysosomes. Their fusion withplasma membrane is triggered by elevation of theintracellular calcium concentration (122,145). Inrats, the lysosomes have been demonstrated to con-tain cysteine proteinases (cathepsin B and H) activeat acidic pH (190). Porcine epithelial cells of Malas-sez share several characteristics with junctional epi-thelial cells and are able to produce several neutralproteinases, including collagen-degrading enzymesand a chymotrypsin-like proteinase (44). The role ofthese enzymes in the antibacterial mechanism hasnot yet been studied. Recently, it has been foundthat the junctional epithelial cells lateral to DAT cells
17
produce matrilysin (matrix metalloproteinase-7)(176). In Paneth cells of the mouse intestine this en-zyme is able to activate the precursor peptide of a-defensin, an important antimicrobial agent of mu-cosal epithelium (184). It is possible that a similaractive matrilysin/defensin system exists in junc-tional epithelium, as in other mucosa exposed tobacteria such as intestine, lungs and urogenitaltissues (88). Another possible effect by which matri-lysin contributes to the mucosal defense is the re-lease of bioactive molecules from the cell surfaceswhich play a role in the inflammatory reaction. Sucheffects are currently being actively explored.
Fig. 7. Several antimicrobial mechanisms exist in thejunctional epithelium. In the coronal part of the junc-tional epithelium quick cell exfoliation (1) because ofrapid cell division (2) and funnelling of junctional epi-thelial cells towards the sulcus hinder bacterial coloniza-tion (see text). Laterally, the (external) basement mem-brane forms an effective barrier against invading mi-crobes (3). Active antimicrobial substances are producedin junctional epithelial cells. These include defensins andlysosomal enzymes (4). Epithelial cells activated by mi-crobial substances secrete chemokines, e.g. interleukin-8 and cytokines, e.g. interleukins -1 and -6, and tumournecrosis factor-a that attract and activate professional de-fense cells, such as lymphocytes (LC) and polymorpho-nuclear leukocytes (PMN). Their secreted product, in turn,cause further activation of the junctional epithelial cells(5). CT Ω connective tissue.
Pöllänen et al.
Despite the selective barrier formed by the gingi-val basal laminas, components of the inflammatoryand immunological defense pass easily through thebasement membrane and epithelium into the sul-cus. Here they play an important role in restrictingbacterial access into the subgingival tissues (for a re-view see [81]) (Fig. 2a,b, 4a). Leukocytes, especiallythe polymorphonuclear leukocytes that migratethrough the junctional epithelium, comprise prob-ably the most important defense mechanism at thegingival margin (112). The cell surface carbohydrates(1) expressed by the junctional epithelial cells arethought to respond to extracellular molecularchanges in a manner which allows the cells to com-municate with their environment. The cells respondactively to bacterial infection by producing cell ad-hesion molecules (intercellular adhesion molecule-1) and chemotactic substances (chemokines such asC5a, leukotriene B4, lymphocyte function-associatedantigen-3 and interleukin-8) that facilitate the mi-gration of leukocytes through the junctional epithel-ium (16,28,99,171).
In the subsequent line of defense inflammatorymediators and antibodies produced by macro-phages, lymphocytes and plasma cells in the gingivaltissues restrict the spreading of bacterial infectioninto the connective tissue and systemic circulation.Significant amounts of lymphocytes may be presentalso within the junctional epithelium, thus contribu-ting to the protective functions of the tissue(148,149). Recently, it has been suggested thatsupplementary to system-derived antibodies andantibodies produced locally by plasma cells, thejunctional epithelial cells may also have a secretoryfunction (77).
The detachment of the DAT cellsfrom the tooth surface – (host vs.bacteria; battle for surface)
Role of the gingival crevice fluid
GCF is an exudate of varying composition found inthe sulcus/periodontal pocket between the toothand marginal gingiva. GCF contains components ofserum, inflammatory cells, connective tissue, epi-thelium, and microbial flora inhabiting the gingivalmargin or the sulcus/pocket (26, 37, 41, and articlesin this issue) (Fig. 8). In the healthy sulcus theamount of GCF is very small. However, its constitu-ents participate in the normal maintenance of func-tion of the junctional epithelium throughout its lat-
18
eral and vertical dimensions, including the most co-ronal DAT cells. During inflammation the GCF flowincreases and its composition starts to resemble thatof an inflammatory exudate (26). The increased GCFflow contributes to host defense by flushing bacterialcolonies and their metabolites away from the sulcus,thus restricting their penetration into the tissue.
The main route for GCF diffusion is through the(external) basement membrane and then throughthe relatively wide intercellular spaces of the variablethickness junctional epithelium into the sulcus. Al-though all the junctional epithelial cells are con-stantly exposed to the GCF and its various constitu-ents, the nutritional and other vital conditions in thedifferent parts of the junctional epithelium dependon a large number of local factors. Clearly, thechanges in the composition of the GCF caused eitherby bacteria, bacterial metabolites/enzymes or otherfactors, or the inflammatory reaction is likely to be
Fig. 8. The GCF passing through the junctional epitheliumdetermines the environmental conditions and providessufficient nutrients for the DAT cells to grow. At the gingi-val margin the GCF may become contamined so thatagents from the oral cavity and/or the plaque bacteriachallenge the most coronal DAT cells. Obviously, the con-ditions for DAT cell survival and adequate function at thecoronal part of the JE are different and more susceptibleof compromises than those for the basal cells living inthe vicinity of the connective tissue (CT) and the bloodcirculation.
Tooth–epithelial interface in health and disease
largest at the most coronal junctional epithelial cells.A considerable number of bacteria and host-de-
rived products found in the GCF have been associ-ated with the initiation and progression of peri-odontal disease. The bacterial agents include endo-toxins, hydrogen sulfide, butyric and propionicacids, bacterial collagenases and other proteases(e.g. trypsin-like), and a variety of enzymes, such ashyaluronidase and neuraminidase (37). Host-derivedagents include components associated with the in-flammatory reaction, such as factors of the comple-ment system, prostaglandins, different cytokines, in-tracellular enzymes, and products of tissue break-down such as lactate dehydrogenase, aspartateaminotransferase, polyamines, and collagen pep-tides (37,41,82). Furthermore, antimicrobial agentsand leukocyte-derived enzymes such as lysozyme,alkaline phosphatase, b-glucuronidase, cathepsin D,elastase, collagenase, and lactoferrin as well as os-teonectin and fibronectin are also found in the GCF.Indeed, the GCF contains a wide variety of biologic-ally active molecules with the potential capacity toaffect the growth of junctional epithelium/DAT cellsas well as oral bacteria, both competing for the toothsurface at the dentogingival interface (Fig. 8 and 9,Table 1).
Role of the polymorphonuclearleukocytes
Polymorphonuclear leukocytes form the most im-portant line of defense against bacterial plaque at thegingival margin (112). When the polymorphonuclearleukocytes reach the bacteria, they release the con-tents of their granules and may adhere to individualbacteria and phagocytose them. The polymorpho-nuclear leukocytes do not, however, appear to havethe capacity to remove dental plaque but rather forma protective wall against it. Therefore, polymorpho-nuclear leukocytes are a major contributor in thehost–parasite equilibrium but have a limited capacityto reclaim any tooth surface once lost to the plaquebacteria. On the other hand, activated polymorpho-nuclear leukocytes can cause tissue damage as a re-sult of a variety of enzymes, oxygen metabolites, andother components that are released from their gran-ules during the battle against microbes (3,179,187).The polymorphonuclear leukocytes have two maintypes of granules that contain agents that are effectivein killing the bacteria. The azurophilic (primary) gran-ules contain myeloperoxidase, lysozyme, elastase, ca-thepsin G, urokinase, acid hydrolases, and defensins,whereas the specific (secondary) granules contain
19
lactoferrin, elastase, and lysozyme (30). Activatedpolymorphonuclear leukocytes also generate hydro-gen peroxide (H2O2) and highly reactive oxygen rad-icals with the potential to destroy bacteria and gingi-val cells (21,30). The polymorphonuclear leukocytesare most effective in aerobic conditions close to thegingival margin (30), suggesting a different role forthem in anaerobic periodontal lesions. While di-recting their effects to the invading microbes thepowerful polymorphonuclear leukocyte substancesalso potentially affect the structural cells and extracel-lular matrix. Polymorphonuclear leukocytes may alsobecome activated in inflammatory lesions and releasespecifically their secondary granule contents duringtheir chemotactic migration (63,189). This phenom-enon may also take place in tissues such as the junc-tional epithelium. Therefore, the effects of the sec-ondary granule contents on gingival epithelium are ofspecial interest in research into the failure of the junc-tional epithelium and the formation of periodontalpockets.
Lactoferrin is an important antimicrobial proteinpresent in the secondary granules of polymorpho-nuclear leukocytes. It has high affinity for iron(5,32,85) and it acts on bacteria by causing iron de-
Fig. 9. The degeneration and detachment of DAT cells ex-poses the tooth surface and creates a subgingival nichesuitable for the colonization of anaerobic gram-negativebacteria and apical growth of dental plaque.
Pöllänen et al.
Table 1. Dental plaque and gingival crevice fluid (GCF) components associated with periodontal diseases
Dental plaque in vivo Human GCF/GCW
Cultured Periodontal PeriodontalCompound plaque bacteria Healthy disease Healthy disease
Alkaline phosphatase 60 mIU/site (25) 120 mIU/site (25)
Ammonia 14–86 m (176)
Butyric acid 9.1 mM (151) 0–0.2 m 2.6–14 m 0.08 m (19) 0.33–1.14 m
(104,105) (104,105) (19)
Hydrogen sulfide 539 n (115) 1–50 p.p.m. (98) 0.8 ng/mL (155) 4.2 ng/mL (155)
Interleukin-1b 23–150 ng/mL 86–882 ng/mL(95,117) (95,117)
Lactoferrin 600 mg/mL (46) 1500 mg/mL (46)
Lipoteichoic acid 50 mg ml (181)
Lipopolysaccharide 0.8–3.6 mg/mL 9.6–36 mg/mL(42,173) (42,173)
Prostaglandin E2 5 ng/mL (103) 10.5 ng/mL(103)
Propionic acid 113 m (151) 0.8–0.9 m 9.5–44 m 0.75 m (19) 0.98 m (19)(104,105) (104,105)
Transforming growth factor-a 226 pg/mL (95) 54 pg/mL (95)
Tumor necrosis factor-a 0.1–13 ng/mL(126)
GCW, gingival crevicular washing.
pletion, and thus reduction in bacterial cell divisionrate, glucose metabolism and macromolecular syn-thesis (7,178). Besides bacteriostatic activity, lacto-ferrin also has bactericidal effects, at least in vitro.Binding of lactoferrin to bacteria and their sub-sequent lysis has been reported in a number ofstudies (7,8,12,36). Furthermore, lactoferrin may ex-ert antimicrobial effects through interfering withbacterial attachment and colonization in the oralcavity (4,159,178). In addition to the effects de-scribed above, lactoferrin may also interfere with thehost defense not only by blocking complement acti-vation and inhibiting hydroxyl radical formation butalso by enhancing it by stimulating polymorpho-nuclear leukocyte recruitment to the infected sites(12). In the GCF from sites exhibiting gingival in-flammation or periodontal pockets the amount oflactoferrin is significantly elevated (1000–1500 mg/ml) as compared to the healthy sites (500 mg/ml)(2,46). While microbial multiplication is already sig-nificantly inhibited at low lactoferrin concentrations(50 mg/ml), even high amounts of lactoferrin ( 500mg/ml) seem to have no effect on epithelial cell divi-sion in model systems simulating the junctional epi-
20
thelium in vivo (118). High concentrations of lacto-ferrin do, however, hamper epithelial cell growth byinterfering with their adhesion and spreading. Themolecule may, thus, have a role in delaying the re-pair of the junctional epithelium/DAT cell popula-tion during severe inflammation.
Role of host proteinases andinflammatory mediators
Degradation of extracellular matrix during peri-odontal inflammation is a multistep process that in-volves several proteolytic enzymes. Different celltypes of periodontal tissue produce matrix metallo-proteinases (collagenases, stromelysins, gelatinases,membrane-type metalloproteinases), plasminogenactivator, cathepsins and elastase (17,165). In re-sponse to the bacteria and inflammatory cytokines,fibroblasts, junctional epithelial cells, osteoblasts/osteoclasts, macrophages, and polymorphonuclearleukocytes release proteinases that are involved inthe defense against microbes. At the same time theyalso contribute to periodontal tissue destruction bydegrading extracellular matrix and basement mem-
Tooth–epithelial interface in health and disease
brane components (17,60,132,158). In concert, ma-trix metalloproteinases are able to degrade all extra-cellular matrix proteins (17). Collagenases degradeinterstitial type collagen fibrils (I, II, III), whereasgelatinases, stromelysins, and membrane-typemetalloproteinases have the ability to degradefibronectin and gelatin (denatured collagen), andbasement membrane components including type IVcollagen, entactin, nidogen, and laminin (17,72,102).Neutrophil elastase and cathepsin G are capable ofdegrading basement membrane type IV collagen andlaminin, and also type VIII collagen, found in theinternal basal lamina (61,78). Proteinases of host ori-gin are thus capable of degrading all known extracel-lular components of connective tissue and epithel-ium including components of both the externalbasal lamina (basement membrane at the connec-tive tissue–junctional epithelium interface) and theinternal basal lamina at the epithelium–tooth inter-face. Therefore, these enzymes seem to have the po-tential to contribute to the lateral and apical prolifer-ation of the junctional epithelium into the connec-tive tissue (Fig. 2) as well as to epithelialdisintegration through degradation of the internalbasal lamina and increase in epithelial permeability.However, electron microscopic studies on DAT cellsattached to teeth extracted because of advancedperiodontitis do not support the idea that enzymaticdegradation of the epithelial attachment apparatusprecedes the degeneration of DAT cells (111). On thecontrary, the DAT cells in this material seemed to bemore severely affected than the epithelial attach-ment apparatus once produced and maintained bythe degenerating cells. This implies that it might bemore rewarding to focus the studies of pocket forma-tion on mechanisms that disturb the vital functionsof the DAT cells rather than on the destruction ofthe matrix components of the epithelial attachmentapparatus.
As described elsewhere in this issue, regulation ofproteinase activities is a complex process involvingactivation of latent precursor molecules as well asinhibition of the active enzymes. Therefore, the ac-tual damage caused by, for example, polymorpho-nuclear leukocyte proteinases may be limited in thepresence of proteinase inhibitors, such as a2 macro-globulin, a1 antitrypsin and tissue inhibitors ofmetalloproteinases, found in the junctional epithel-ium and in the gingival crevice. In fact, a recentstudy has demonstrated that there is only a limitedamount of active metalloproteinases in the pocketepithelium obtained from sites of periodontitis(140). Since the degradation of the extracellular ma-
21
trix by metalloproteinases plays a major role in theinflamed connective tissue, it is pertinent to ask howsignificant is the failing support of the connectivetissue to the integrity of the junctional epithelium.Obviously, a less effective connective tissue supportpredisposes the tissue to intraepithelial splits andcontributes to the lateral and apical proliferation ofthe epithelium. Together with increased per-meability of the junctional epithelium, this may alterthe nutritional conditions of the DAT cells on thetooth surface and expose them to agents from thedental plaque. Another area of junctional epitheliumbiology that has not been addressed in depth is thecomposition of the epithelial interstitial matrix andhow its degradation affects the behavior of junc-tional epithelial cells. Also, a limited proteolyticcleavage of matrix molecules, e.g. laminin, fibronec-tin and proteoglycan, may expose cryptic molecularsites with biological activity not possessed by the in-tact molecule (39). These active tissue fragmentsmay regulate cell adhesion, migration and prolifer-ation in inflamed tissue (175). For instance, while in-tact laminin-5 promotes formation of hemidesmo-somes and inhibits cell migration, its fragment pro-duced by a proteolytic cleavage promotes epithelialcell migration (49). Even though fragments offibronectin and collagen have been demonstrated inGCF their effects on junctional epithelium/pocketepithelium are unknown (38). In future, extracellularmatrix molecules and their fragments can be ex-pected to provide useful tools for prevention andmanagement of periodontal disease. For example,laminin-5 treatment of teeth or titanium dental im-plants may enhance long-term stability of epithelialattachment (35).
Cytokines, especially the interleukins -1 and -6,and tumor necrosis factor-a, and the arachidonicacid metabolite prostaglandin E2, have been stronglyassociated with periodontal disease [for a review see(47)]. These inflammatory mediators are secretedinto the GCF by both leukocytes and activated junc-tional epithelium cells and their amounts have beenshown to increase at sites exhibiting periodontaltissue destruction [Table 1; (95,103,109,117)]. In-terleukin-1, interleukin-6 and prostaglandin E2
stimulate bone resorption and contribute to peri-odontal tissue destruction also by inducing matrixmetalloproteinase (collagenase) production (47). In-terleukin-1 has been shown to promote fibroblastproliferation and production of other cytokines byperiodontal cells, and to activate the arachidonicacid pathway and thus production of prostaglandinE2 (27,34,110). Prostaglandin E2 in turn has an over-
Pöllänen et al.
all catabolic effect on gingival fibroblasts, as shownby suppressed DNA synthesis and collagen synthesis(6). Studies reporting the effects of inflammatorymediators on the junctional epithelium and its func-tions are not available today.
Role of bacterial products
It is plausible that several products released frombacteria during periodontal infection have junc-tional epithelium as their major target tissue. Eventhough there is ample evidence that bacterial sub-stances have a multitude of effects on several celltypes, ranging from activation of cell functions tocell death, the importance of specific substances ininitiation and progression of periodontal diseases isnot yet understood. We review here the literature ofthe main bacterial products and their potential ef-fects on the junctional epithelium.
In the early phase of plaque formation gram-posi-tive bacteria accumulate on the tooth surface closeto the most coronal junctional epithelium/DAT cellswhich may thus be exposed to the cell wall compo-nents of these typically supragingival bacteria;namely the peptidoglycan matrix, surface antigens,teichoic and lipoteichoic acids. Lipoteichoic acidsare genus- and species-specific molecules (45) thatare synthesized especially abundantly from sucroseat neutral pH (79,124). The precise functions oflipoteichoic acids in bacteria have not yet been es-tablished. However, they have been implicated ascarriers in cell wall synthesis, inhibitors of autolyticactivity and as reservoirs of cations (45,125). In theoral cavity lipoteichoic acids are thought to mediatebacterial adhesion to human cells and teeth(13,67,123).
If the bacterial plaque is allowed to grow, theamount of gram-negative bacteria increases. The cellwall of these bacteria is composed of a thin peptido-glycan layer and a bilayered outer membrane, whichcontains the major surface antigens including theporin proteins, and lipopolysaccharides (lipopolys-accharides/endotoxins) (55). The variation in thelipopolysaccharides between bacterial genera, spe-cies, and even within species (54,180,181) may ac-count for the reported differences in host responsesto lipopolysaccharides derived from different bac-terial populations.
From the periodontal point of view both lipotei-choic acids and lipopolysaccharides are interestingmolecules. They are released from the bacteria intothe extracellular environment during bacterial dis-ruption, and also during normal cell wall turnover
22
of living bacteria (42,45,55,56,68,150,173,181). Thus,varying amounts of lipoteichoic acids and lipopolys-accharides are present at the gingival margin wherethey may stimulate leukocyte function, increasecytokine and inflammatory mediator productionand activate the complement system as shown instudies in vitro (15,86,89,96). In addition to their roleas inflammation modulators lipoteichoic acids andlipopolysaccharides have been shown to affect peri-odontal tissues, e.g. by stimulating bone resorption(9,59,94). Furthermore, lipopolysaccharides appearto have the ability to increase epithelial permeabilityand penetrate healthy gingival sulcular epithelium(120,138,154). Lipopolysaccharides from Salmonellaenteritidis, Escherichia coli, Actinobacillus actino-mycetemcomitans, Porphyromonas gingivalis, Prevo-tella intermedia and Porphyromonas asaccharolyticahave been shown to stimulate human gingivalfibroblast proliferation at low (1 mg/mL) concen-trations and suppress their proliferation at higher (10 mg/mL) concentrations (11,31,65,74,83,84). Highconcentrations of lipopolysaccharides from non-oralbacteria (E. coli, 5000 mg/mL) have been shown toincrease the proliferation of basal cells of the junc-tional epithelium in an animal model (167). In hu-man epithelial cell and junctional epithelial tissuecultures lipopolysaccharides from oral pathogensshow only slight or no effects on the growth and mi-totic activity of the cells (120). This indicates thatlipopolysaccharides, despite their established role asmodulators of inflammation, may not significantlyharm the epithelial cells at the concentrations foundin dental plaque and GCF (below 50 mg/mL). There-fore, lipopolysaccharides do not appear to have a keyrole in DAT cell degeneration and detachment fromthe tooth surface.
When epithelial cells in different culture systemsare exposed to lipoteichoic acids from gram-positiveoral bacteria (Streptococcus sanguis and Streptococ-cus mutans, 10–50 mg/mL) their growth and mitoticactivity are consistently reduced (120). According tothese results, the lipoteichoic acids appear to havethe potential to interfere with the renewal of varioustypes of epithelial cells. As discussed before, a pro-longed inhibition of the renewal of the coronal junc-tional epithelium/DAT cells would most likely leadto their degeneration and detachment, and eventu-ally to subgingival colonization by gram-negativeperiodontal pathogens.
Periodontopathogenic bacteria release numerousproteolytic enzymes that are a prerequisite for thenormal metabolism of amino acids and for the sur-vival of these mainly asaccharolytic bacteria in the
Tooth–epithelial interface in health and disease
oral environment (for a review see [68]). Bacterialcollagenases, gelatinases, and trypsin- and chymo-trypsin-like enzymes have been shown to degradehost extracellular matrix macromolecules and base-ment membrane components in vitro suggestingthat also they have the potential to contribute toperiodontal tissue destruction, as do the host-de-rived proteinases (17,116). This is especially true inthe junctional epithelium, where the bacterial en-zyme concentrations are much higher than in theconnective tissue. Degradation of immunoglobulinsand complement proteins by bacterial proteinasesmay result in an incomplete host defense and thusfacilitate bacterial colonization and growth. Somebacterial proteinases are able to activate host matrixmetalloproteinases and thereby increase the totalproteolytic activity in the infected tissue (29,157).The complex interactions of bacterial and host-de-rived proteinases and their inhibitors, as well as thepresence of bacteria capable of degrading the pro-teinase inhibitors (24,107,139) make the exact roleof the bacterial proteloytic enzymes in periodontaltissue destruction difficult to study. It appears, how-ever, that the role, if any, of the bacterial enzymeson epithelial detachment and DAT cell viability/de-generation is primarily indirect and because ofchanges in the living conditions of these cells ratherthan of direct effects on the cells or on the epithelialattachment apparatus (111).
The oral cavity provides bacteria with a large num-ber of ecologic niches and substrates that can bemetabolized to different end products depending onthe bacterial population and the prevailing environ-mental conditions. Therefore, the composition of abacterial population and its virulence, associatedwith specific pathogenic mechanisms, reflects theinteraction of a large number of constantly changingvariables determined not only by the oral microfloraitself but also by the host. For example, the met-abolism of carbohydrates in dental plaque dependson the pH, the oxygen gradient, the amount andquality of available substrates, and most importantly,the bacterial composition of the plaque (92,185). Asa principal rule, cariogenic, supragingival plaquescontain a high percentage of streptococci, whereassubgingival plaques growing in periodontal pocketscontain high proportions of gram-negative an-aerobes (22,23,185). The main metabolic end prod-uct of the streptococcal plaque is lactic acid, whereasthe gram-negative bacteria produce butyric acidmore abundantly (68,91,106,164,185) (Fig. 10). It isnoteworthy that certain bacteria can take advantageof the metabolic end products released by other bac-
23
teria and thereby contribute to the production ofagents that are increasingly detrimental to the hosttissues. Anaerobic plaque bacteria, especially the as-accharolytic bacteria, utilize amino acids and pep-tides, derived either from diet or tissue/cell break-down, for their sources of energy. This requires thepresence of proteolytic enzymes that first degradethe macromolecules (proteins) into small peptidesor amino acids which are then further metabolizedby the bacteria (68,185). When amino acids are util-ized as an energy source, ammonia, sulfur-contain-ing compounds (hydrogen sulfide) and short-chainfatty acids, especially butyric and propionic acids,are formed (23,68,164).
Butyric and propionic acids are short-chain fattyacids containing four and three carbon atoms, re-spectively. They are produced by periodontopathog-enic bacteria, such as Porphyromonas, Fusobacteri-um, Prevotella and Treponema (18–20,22,51,97,164).As described above, the production of these acidsdepends on a variety of environmental factors in-cluding the proteolytic activity and the pH in thepocket. The maximal activity of proteolytic enzymesproduced by periodontal pathogens is at pH 7.0–8.0.Some periodontal bacteria (e.g. Prevotella interme-dia) are, however, capable of surviving and func-tioning over a much broader pH range and even ofraising the pH by producing ammonia, and therebymaking the environment more suitable for bacterialpopulations adapted to alkaline conditions (68). It isof particular interest that the concentrations of bu-tyric and propionic acids found in human plaqueand GCF correlate directly with the degree of gingivalinflammation and periodontal pocket depth (Table 1[19,104,105]). Furthermore, the application of milli-molar concentrations of these short-chain fatty acidsonto the healthy gingiva of beagle dogs has been re-ported to produce a marked gingival inflammatoryresponse (152). More recently, human studies haveshown that both food, which supports bacterial gen-eration of high levels of short-chain fatty acids (50m), and short-chain fatty acids (100 m) applieddirectly to healthy human gingiva elicit an inflam-matory response in the tissue. This response can bedemonstrated by increased GCF flow, subgingivaltemperature, polymorphonuclear leukocyte emi-gration, and elevated levels of inflammatory cyto-kines (interleukin-8) in the GCF (75,106,191). Short-chain fatty acids have also been shown to activateleukocytes to release inflammatory cytokines and ex-tend their lifetime (163,166). The activation of theinflammatory response and simultaneous inhibitionof the polymorphonuclear leukocyte function
Pöllänen et al.
(phagocytosis and degranulation) (106) can alter andprolong the inflammatory response and lead to moresevere tissue destruction.
In cell cultures, butyric and propionic acids, ap-plied in concentrations found in human plaque andGCF, have been shown to inhibit the proliferation ofboth fibroblasts and epithelial cells (33,119,151,156).Microbial populations producing these short-chainfatty acids may thus significantly impair the rapidrenewal of the junctional epithelium/DAT cells andthereby counteract one of the tissue’s main host pro-tective functions. Taken together, the current litera-ture suggests that butyric and propionic acids play arole in the initiation and progression of periodontalpocket formation by triggering and modifying the in-flammatory response and by hampering the turn-over and repair of the tissues at the dentogingivaljunction.
Utilization of amino acids by bacteria for their en-ergy needs, results in the formation of short-chainfatty acids, hydrogen sulfide and ammonia as by-products. Like the short-chain fatty acids, am-monium and hydrogen sulfide have potentially det-rimental effects on periodontal cells. Ammonium(20–80 m) has been shown to cause cell vacuoliz-ation in chondrocytes and to inhibit (2–10 m am-monium) collagen secretion by human gingivalfibroblasts in vitro (62,177). Whether or not the am-
Fig. 10. Oral bacteria produce short-chain fatty acids. En- glucose is abundant in aerobic (and low pH) conditionsvironmental factors such as the oxygen gradient, pH, sub- the metabolites on the left are the main products. In an-strate quality and quantity, and the presence of bacterial aerobic conditions at high pH and when lactose starch orenzyme inhibitors have a strong effect on the survival of amino acids are used as substrates, the metabolites on thebacteria and the metabolites produced. When sucrose or right hand side of the figure are increased.
24
monium levels produced by plaque bacteria signifi-cantly influence epithelial cells is not known.
Hydrogen sulfide is a highly toxic compound thatcauses adverse effects on human tissues (eyes andrespiratory tract) at concentrations of 50 p.p.m. (50mg/mL) and above (14). Hydrogen sulfide has beendetected in the GCF collected from gingival sulcus/pocket and its amount has been shown to increasein gingival inflammation (155). In the concentrationsfound in dental plaque (1–50 ppm) hydrogen sulfidehas been shown to be toxic to HeLa cells (98). Inter-estingly, oxidation of hydrogen sulfide results in sul-fate formation and detoxification of the compound,whereas its toxicity is increased in the presence ofshort chain hydrocarbons, ethanol and/or proteins(14). Considering the protein-rich, short-chain fattyacid-containing and anaerobic conditions in thesubgingival space, hydrogen sulfide appears to be apotential candidate to cause significant damage tothe junctional epithelium/DAT cells on the toothsurface during periodontal disease progression.
Role of risk factors for periodontaldisease
It is clear that periodontal diseases are primarilycaused by bacterial infections and that a number ofrisk factors contribute to the susceptibility of indi-
Tooth–epithelial interface in health and disease
viduals to these infections, and to the pathogenesisand severity of the disease. These factors includesmoking, diabetes, immunosuppression, genetic fac-tors, stress and age (136). Studies on how the riskfactors influence disease progression have mainlybeen focused on the inflammatory reaction(10,52,57,58,76,108,114,137,162,186,188). The con-clusion from these studies is that a sound inflam-matory host response is needed for successful peri-odontal defense. Factors that modify this responsemay either cause an overwhelming reaction or aninadequate reaction, both of which may acceleratetissue destruction. It is interesting that periodontalrisk factors, such as hyperglycaemia and chemicalcompounds released from tobacco, have harmful ef-fects on the renewing capacity of both fibroblastsand bone cells (40,50,170) However, very little isknown about the influences of any of the risk factorson oral gingival/sulcular or junctional epithelium(64). From the defense point of view, it would be im-portant to examine whether these factors also impairthe turnover or other defense mechanisms of thejunctional epithelium and thus contribute to the de-generation of the dentoepithelial junction.
It is also quite possible that a specific response ofjunctional epithelial cells to bacterial or host sub-stances is a key factor in the pathogenesis of certainforms of periodontal diseases. One example could belocalized juvenile periodontitis, where a rapid apicalgrowth of the junctional epithelium is associatedwith a typically distributed pocket formation. A localjunctional epithelial cell defect might in this case re-sult, for example, in a decreased ability of the DATcells to form hemidesmosomes. In fact, in Kindlersyndrome a defect in the formation of hemidesmo-some-associated fibers consisting of type VII colla-gen leads to detachment of skin and gingival epithel-ium and to early onset periodontitis (183).
Conclusions
The precise mechanisms that lead to the degenera-tion and detachment of the junctional epitheliumfrom the tooth surface and to the conversion of agingival sulcus into an infected periodontal pockethave not been established. The destructive mechan-isms may involve many of the modalities of both thehost defense and microbial virulence. Studies of thedegeneration process of the junctional epithelialcells themselves are, however, largely missing. Thejunctional epithelium consists of distinct popula-
25
tions of cells at different anatomical locations. Allthese cells have a responsive phenotype that allowsthem to exhibit specific functions in periodontal de-fense and to take or lose an active role during peri-odontal disease progression. The junctional epithel-ium is firmly attached to the tooth by the suprabasalDAT cell/internal basal lamina structure, and to theconnective tissue by the basal cell/external basallamina complex. Environmental conditions differessentially in these two locations and even similarpathogenic challenges may become modified andcause considerably different cellular responses.While the coronal DAT cells grow close to the bac-terial plaque the apical and lateral parts of the junc-tional epithelium are likely to be influenced by theconnective tissue and the inflammatory reaction.The GCF provides the most coronal DAT cells withthe necessary conditions to survive but it also con-tains a variety of biologically active molecules withthe potential capacity to affect their vital functionsand behavior. Although the significance of the vari-ous components of the GCF to the failure of thejunctional epithelium and its DAT cells calls forfurther studies there are a few candidates that are ofparticular interest today. Among these are the poly-morphonuclear leukocyte products that may havedirect influences on DAT cell survival and/or theiradhesion and bacterial lipoteichoic acids and meta-bolic end products, such as propionic and butyricacids that may interfere with cell division and thusthe turnover and reparative capacity of the junc-tional epithelium. Similarly, inflammatory factorsand components associated with periodontal riskfactors may reach high concentrations in the GCFand severely interfere with the junctional epithel-ium’s normally protective functions.
When the physiology of the junctional epitheliumand its molecular reactions during different externalchallenges are known in more detail the tissue’s rolein the failure of the healthy dentogingival junctionand the reasons that make some individuals suscep-tible to periodontal diseases will be better under-stood.
References1. Abe Y, Hara Y, Saku T, Kato I. Histological study of lectin
binding in regenerated rat junctional epithelium. J Peri-odontal Res 1995: 30: 238–244.
2. Adonogianaki E, Muoghal NA, Kinane DF. Lactoferrin inthe gingival crevice as a marker for PMN-leukocytes inperiodontal disease. J Clin Periodontol 1993: 20: 26–31.
3. Altman LC, Baker C, Fleckman P, Luchtel D, Oda D. Neu-trophil mediated damage to human gingival epithelialcells. J Periodontal Res 1992: 27: 70–79.
Pöllänen et al.
4. Alugupalli KR, Kalfas S. Inhibitory effect of lactoferrin onthe adhesion of Actinobacillus actinomycetemcomitansand Prevotella intermedia to fibroblasts and epithelialcells. Acta Pathol Microbiol Scand 1995: 103: 154–160.
5. Anderson BF, Baker HM, Dodson EJ, Norris GE, RumballSV, Waters JM, Baker EN. Structure of human lactoferrinat 3.2 Å resolution. Proc Natl Acad Sci USA 1987: 84: 1769–1773.
6. Arai H, Nomura Y, Kinoshita M, Shimizu H, Ono K, GotoH, Takigava M, Nishimura F, Washio N, Kurihara H, Muray-ama Y. Response of human gingival fibroblasts to prosta-glandins. J Periodontal Res 1995: 30: 303–311.
7. Arnold RR, Brewer M, Gauthier JJ. Bactericidal activity ofhuman lactoferrin: sensitivity of a variety of microorgan-isms. Infect Immun 1980: 28: 893–989.
8. Arnold RR, Russell JE, Champion WJ, Brewer M, GauthierJJ. Bactericidal activity of human lactoferrin: differen-tiation from the stasis of iron deprivation. Infect Immun1982: 35: 792–799.
9. Bab IA, Sela MN, Ginsburg I, Dishon T. Inflammatorylesions and bone resorption induced in the rat periodon-tium by lipoteichoic acid of Streptococcus mutans. In-flammation 1979: 3: 345–358.
10. Ballieux RE. Impact of mental stress on the immune re-sponse. J Clin Periodontol 1991: 18: 427–430.
11. Bartold PM, Narayanan AS, Page RC. Platelet-derivedgrowth factor reduces the inhibitory effects of lipopolysac-charide on gingival fibroblast proliferation. J PeriodontalRes 1992: 27: 499–505.
12. Baveye S, Elass E, Mazurier J, Spik G, Legrand D. Lactofer-rin: a multifunctional glycoprotein involved in the modu-lation of the inflammatory process. Clin Chem Lab Med1999: 37: 281–286.
13. Beachey EH, Simpson WA. The adherence of group Astreptococci to oropharyngeal cells: the lipoteichoic acidadhesin and fibronectin receptor. Infection 1982: 10: 107–111.
14. Beauchamp ROJ, Bus JS, Popp JA, Boreiko CJ, AndjelkovichDA. A critical review of the literature on hydrogen sulfidetoxicity. Crit Rev Toxicol 1984: 13: 25–97.
15. Bhakdi S, Klonisch T, Nuber P, Fischer W. Stimulation ofmonokine production by lipoteichoic acids. Infect Immun1991: 20: 4614–4620.
16. Bickel M. The role of interleukin-8 in inflammation andmechanisms of regulation. J Periodontol 1993: 64: 456–460.
17. Birkedal-Hansen H. Role of cytokines and inflammatorymediators in tissue destruction. J Periodontal Res 1993: 28:500–510.
18. Borthen L, Heimdahl A, Lindqvist L, Nord C. Determi-nation of volatile fatty acids in saliva and faeces by gas-liquid chromatography: a rapid method for detectionof antibiotic-induced changes in the oropharyngeal andgastrointestinal microflora. Int J Microbiol 1983: 1: 35–45.
19. Botta GA, Radin L, Costa A, Schito G, Blasi G. Gas-liquidchromatography of the gingival fluid as an aid in peri-odontal diagnosis. J Periodontal Res 1985: 20: 450–457.
20. Bricknell K, Grinenko V, Carlton D, Newman M. GLC rapidanalysis of bacteria in plaque. J Periodontal Res 1978: 57:abstract 1106.
21. Carlsson J. Growth and nutrition as ecological factors. In:Kuramitsu, H, Ellen, R, editors. Oral Bacterial Ecology: TheMolecular Basis. Norfolk: Horizon Scientific Press, 2000:Chapter 2, 67–130.
26
22. Carlsson J. Metabolic activities of oral bacteria. In: Thylstr-up, A, Fejerskov, O, editors. Textbook of Cariology. Copen-hagen: Munksgaard, 1986: 74–106.
23. Carlsson J. Microbiology of plaque-associated periodontaldisease. In: Lindhe, J, editor. Textbook of Clinical Periodon-tology. Copenhagen: Munksgaard, 1989: 129–152.
24. Carlsson J, Herrmann BF, Höfling JF, Sundqvist GK. Degra-dation of the human proteinase inhibitors alpha-1-anti-trypsin and alpha-2-macroglobulin by Bacteroides gingi-valis. Infect Immun 1984: 43: 644–648.
25. Chapple ILC, Socransky SS, Dibart S, Glenwright HD, Mat-thews JB. Chemiluminescent assay of alkaline phospha-tase in human gingival crevicular fluid: investigations withan experimental gingivitis model and studies on thesource of the enzyme within crevicular fluid. J Clin Peri-odontol 1996: 23: 587–594.
26. Cimasoni G. Crevicular Fluid Updated. Monographs inOral Sciences. Basel: Karger, 1983: 45–102.
27. Clemens MJ.In: Read, AP, Brown, T, editors. Cytokines. Ox-ford: Bio Scientific Publishers, 1991: 1–121.
28. Crawford J. Distribution of ICAM-1, LFA-3, and HLA-DRin healthy and diseased ginigval tissues. J Periodontal Res1992: 27: 291–298.
29. DeCarlo AA Jr, Windsor LJ, Bodden MK, Harber GJ, Birked-al-Hansen B, Birkedal-Hansen H. Activation and novelprocessing of matrix metalloproteinases by a thiol-pro-teinase from the oral anaerobe Porphyromonas gingivalis.J Dent Res 1997: 76: 1260–1270.
30. Dennison DK, Van Dyke TE. The acute inflammatory re-sponse and the role of phagocytic cells in periodontalhealth and disease. Periodontol 2000 1997: 14: 54–78.
31. Derenzis FA, Chen S-Y. Ultrastructural study of culturedhuman gingival fibroblasts exposed to endotoxin. J Peri-odontol 1983: 54: 86–90.
32. Derisbourg P, Wieruszeski JM, Montreuil J, Spik G. Primarystructure of glycans isolated from human leukocyte lacto-transferrin. Biochem J 1990: 269: 821–825.
33. Eftimiadi C, Valente S, Mangiante S, Mangiante PE, Nied-erman R. Short chain fatty acids produced by anaerobicbacteria inhibit adhesion and proliferation of periodontalligament fibroblasts. Minerva Stomatol 1993: 42: 481–485.
34. El Attar TM, Lin HS. Prostaglandin E2 antagonizes gingivalfibroblast proliferation stimulated by interleukin-1 beta.Prostaglandin Leukotrienes Essential Fatty Acids 1993: 49:847–850.
35. El-Ghannam A, Starr L, Jones J. Laminin-5 coating en-hances epithelial cell attachment, spreading, and hemi-desmosome assembly on Ti-6A1–4V implant material invitro. J Biomed Mater Res 1998: 41: 30–40.
36. Ellison RT, Giehl TJ, La Force FM. Damage of the outermembrane of enteric gram-negative bacteria by lactofer-rin and transferrin. Infect Immun 1988: 56: 2774–2781.
37. Embery G, Waddington R. Gingival crevicular fluid: bio-markers of periodontal tissue activity. Adv Dent Res 1994:8: 329–336.
38. Embery G, Waddington RJ, Hall RC, Last KS. Connectivetissue elements as diagnostic aids in periodontology. Peri-odontol 2000 2000: 24: 193–214.
39. Engel J. Domains in proteins and proteoglycans of theextracellular matrix with functions in assembly and cellu-lar activities. Int J Biol Macromol 1991: 13: 145–151.
40. Fang MA, Frost PJ, Iida-Klein A, Hahn TJ. Effects of nic-otine on cellular function in UMR 106–01 osteoblast-likecells. Bone 1991: 12: 283–286.
Tooth–epithelial interface in health and disease
41. Fine DH, Mandel ID. Indicators of periodontal disease ac-tivity: an evaluation. J Clin Periodontol 1986: 13: 533–546.
42. Fine DH, Mendieta C, Barnett ML, Furgang D, Naini A.Endotoxin levels in periodontally healthy and diseasedsites: Correlation with levels of gram-negative bacteria. JPeriodontol 1992: 63: 897–901.
43. Firth JD, Putnis EE, Larjava H, Uitto V-J. Bacterial phos-pholipase C upregulates matrix metalloproteinase expres-sion by cultured epithelial cells. Infect Immun 1997: 65:4931–4936.
44. Firth JD, Sue ES, Putnis EE, Oda D, Uitto VJ. Chymotryp-sin-like enzyme secretion is stimulated in cultured epi-thelial cells during proliferation and in response to Actino-bacillus actinomycetemcomitans. J Periodontal Res 1996:31: 345–354.
45. Fischer W. Physiology of lipoteichoic acids in bacteria. In:Rose, AH, Tempest, DW, editors. Advances in MicrobialPhysiology. London: Academic Press Limited. 1988: 233–302.
46. Friedman SA, Mandel ID, Herrera MS. Lysozyme and lac-toferrin quantitation in the crevicular fluid. J Periodontol1983: 54: 347–350.
47. Gemmell E, Marshall RI, Seymour GJ. Cytokines andprostaglandins in immune homeostasis and tissue de-struction in periodontal disease. Periodontol 2000 1997:14: 112–143.
48. Genco RJ. Consensus report on periodontal diseases:pathogenesis and microbial factors. In: Genco, RJ, editor.Annals of Periodontology. Chicago: American Academy ofPeriodontology, 1996: 926–932.
49. Giannelli G, Falk-Marzillier J, Schiraldi O, Stetler-Steven-son WG, Quaranta V. Induction of cell migration by matrixmetalloproteinase-2 cleavage of laminin-5. Science 1997:277: 225–228.
50. Goldstein S. Cellular and molecular biological studies ondiabetes mellitus. Pathol Biol 1984: 32: 99–106.
51. Gorbach SL, Mayhew JW, Bartlett JG, Thadepalli H, Onder-donk AB. Rapid diagnosis of anaerobic infections by directgas-liquid chromatography of clinical specimens. J ClinInvest 1976: 57: 478–484.
52. Greenspan JS, Greenspan D, Winkler JR, Murray PA. Ac-quired immunodeficiency syndrome: oral and periodontalchanges. In: Genco, RJ, editor. Contemporary Periodontics.St. Louis: CV Mosby, 1990: 298–321.
53. Haffajee AD, Socransky SS. Microbial etiological agents ofdestructive periodontal diseases. Periodontol 2000 1994: 5:78–111.
54. Hamada S, Koga T, Nishihara T, Fujiwara T, Okahashi N.Characterization and immunobiologic activities of lipo-polysaccharides from periodontal bacteria. Adv Dent Res1988: 2: 284–291.
55. Hammond BF. Bacterial structure and function. In: Schus-ter, GS, editor. Oral Microbiology and Infectious Diseases.Philadelphia: B.C.. Decker Inc., 1990: 25–43.
56. Hancock IC. Bacterial surface composition and properties.In: Newman, HN, Wilson, M, editors. Dental Plaque Re-visited, Oral Biofilms in Health and Disease. Cardiff: Bio-line, 1999: 37–48.
57. Hart TC, Kornman KS. Genetic factors in the pathogenesisof periodontitis. Periodontol 2000 1997: 14: 202–215.
58. Hart TC, Shapira L, Van Dyke TE. Neutrophil defects asrisk factors for periodontal diseases. J Periodontol 1994:65: 521–529.
27
59. Hausmann E, Nair BC, Dziak R. Bacterial componentswhich result in bone loss. In: Genco, RJ, Merhagen, SE,editors. Host Parasite Interactions in Periodontal Diseases.Washington D.C.: American Society for Microbiology,1982: 151–159.
60. Heath JK, Gowen M, Meikle MC, Reynolds JJ. Human gin-gival tissues in culture synthesize three metalloproteinasesand a metalloproteinase inhibitor. J Periodontal Res 1982:17: 183–190.
61. Heck LW, Blackburn WD, Irwin MH, Abrahamson DR.Degradation of basement membrane laminin by humanneutrophil elastase and cathepsin G. Am J Pathol 1990:136: 1267–1274.
62. Helgeland K. Inhibitory effect of NH4Cl on secretion ofcollagen in human gingival fibroblasts. Scand J Dent Res1984: 92: 419–435.
63. Henson PM. The immunologic release of constituentsfrom neutrophil leukocytes, mechanisms of release duringphagocytosis and adherence to nonphagocytable surfaces.J Immunol 1971: 107: 1547–1557.
64. Hill M. Cell renewal in oral epithelia. In: Hill, M, editor.The Structure and Function of Oral Mucosa. Oxford: Perga-mon Press, 1984: 53–81.
65. Hill SJ, Ebersole JL. The effect of lipopolysaccharide ongrowth factor-induced mitogenesis in human gingivalfibroblasts. J Periodontol 1996: 67: 1274–1280.
66. Hirako Y, Owaribe K. Hemidesmosomes and their uniquetransmembrane protein BP180. Microsc Res Tech 1998: 43:207–217.
67. Hogg SD, Manning JE. Inhibition of adhesion of viridansstreptococci to fibronectin coated hydroxyapatite beads bylipoteichoic acid. J Appl Bacteriol 1988: 65: 483–489.
68. Holt SC, Bramanti TE. Factors in virulence expression andtheir role in periodontal disease pathogenesis. Crit RevOral Biol Med 1991: 2: 177–281.
69. Hormia M, Sahlberg C, Thesleff I, Airenne T. The epithel-ium–tooth interface – a basal lamina rich in laminin-5 andlacking other known laminin isoforms. J Dent Res 1998: 77:1479–1485.
70. Ishikawa I, Nakashima K, Koseki T, Nagasawa T, WatanabeH, Arakawa S, Nitta H, Nishihara T. Induction of the im-mune response to periodontopathic bacteria and its rolein the pathogenesis of periodontitis. Periodontol 20001997: 14: 79–111.
71. Jones JCR, Hopkinson SB, Goldfinger LE. Structure and as-sembly of hemidesmosomes. Bioessays 1998: 20: 488–494.
72. Kähäri V-M, Saarialho-Kere U. Matrix metalloproteinasesin skin. Exp Dermatol 1997: 6: 199–213.
73. Kainulainen T, Hakkinene L, Hamidi S, Larjava K, Kallioin-en M, Peltonen J, Salo T, Larjava H, Oikarinen A. Essentialrole of laminin-5 during re-epithelialization of wounds. JHistochem Cytochem 1998: 46: 353–360.
74. Kamin S, Harvey W, Wilson M, Schutt A. Inhibition offibroblast proliferation and collagen synthesis by capsularmaterial from Actinobacillus actinomycetemcomitans. JMed Microbiol 1986: 22: 245–249.
75. Kashket S, Zhang J, Niederman R. Gingival inflammationinduced by food and short-chain carboxylic acids. J DentRes 1998: 77: 412–417.
76. Kenney EB, Kraal JH, Saxe SR, Jones J. The effect of ciga-rette smoke on human oral polymorphonuclear leuco-cytes. J Periodontal Res 1977: 12: 227–234.
77. Kinane DF, Lappin DF, Kouoluri O, Buckley A. Humoral
Pöllänen et al.
immune responses in periodontal disease may have mu-cosal and systemic immune features. Clin Exp Immunol1999: 115: 534–541.
78. Kittleberger R, Neale TJ, Francky KT, Greenhill NS. Cleav-age of type VIII collagen by human neutrophil elastase.Biochim Biophys Acta 1992: 1139: 295–299.
79. Knox KW, Wicken AJ. Effect of growth conditions on lipotei-choic acid production. In: Shockman, GD, Wicken, AJ, edi-tors. Chemistry and Biological Activities of Bacterial SurfaceAmphiphiles. New York: Academic Press Inc 1981, 229–237.
80. Kobayashi K, Rose GG, Mahan CJ. Ultrastructure of thedento-epithelial junction. J Periodontal Res 1976: 11: 313–330.
81. Kornman KS, Page RC, Tonetti MS. The host response tothe microbial challenge in periodontitis: assembling theplayers. Periodontol 2000 1997: 14: 33–53.
82. Lamster IB, Gribic JT. Diagnosis of periodontal diseasebased on analysis of the host response. Periodontol 20001995: 7: 83–99.
83. Larjava H, Uitto V-J, Eerola E, Haapasalo M. Inhibition ofgingival fibroblast growth by Bacteroides gingivalis. InfectImmun 1987: 55: 201–205.
84. Layman DL, Diedrich DL. Growth inhibitory effects of en-dotoxins from Bacteroides gingivalis and intermedius onhuman gingival fibroblasts in vitro. J Periodontol 1987: 58:387–392.
85. Legrand D, Mazurier J, Colavizza D, Montreuil J, Spik G.Properties of the iron-binding site of the N-terminal lobeof human and bovine lactotransferrins. Importance of theglycan moiety and of the non-covalent interactions be-tween the N- and C-terminal lobes in the stability of theiron binding site. Biochem J 1990: 266: 575–581.
86. Lindemann RA, Economou JS, Rothermel H. Productionof interleukin-1 and tumour necrosis factor by human pe-ripheral monocytes activated by periodontal bacteria andextracted lipopolysaccharides. J Dent Res 1988: 67: 1131–1135.
87. Loe H, Theilade E, Jensen SB. Experimental gingivitis inman. J Periodontol 1965: 36: 177–187.
88. Lopez-Boado YS, Wilson CL, Hooper LV, Gordon JI, Hultgr-en SJ, Parks WC. Bacterial exposure induces and activatesmatrilysin in mucosal epithelial cells. J Cell Biol 2000: 148:1305–1315.
89. Loppnow H, Brade H, Rietschel ET, Flad H-D. Induction ofcytokines in mononuclear and vascular cells by endotoxinand other bacterial products. Meth Enzymol 1994: 236: 3–10.
90. Luke D. The structure and functions of the dentogingivaljunction and periodontal ligament. Br Dent J 1992: 172:187–190.
91. Macfarlane GT, Gibson GR. Microbiological aspects of theproduction of short-chain fatty acids in the large bowel.In: Cummings, JH, Rombeau, JL, Sakata, T, editors. Physio-logical and Clinical Aspects of Short-Chain Fatty Acids.Cambridge: Cambridge University Press, 1995: 87–106.
92. Marsh PD, Bradshaw DJ. Microbial community aspects ofdental plaque. In: Newman, HE, Wilson, M, editors. DentalPlaque Revisited-Oral Biofilms in Health and Disease. Car-diff: Bioline, 1999: 237–253.
93. Masunaga T, Shimizu H, Ishiko A, Tomita Y, Aberdam D,Ortonne JP, Nishikawa T. Localization of laminin-5 in theepidermal basement membrane. J Histochem Cytochem1996: 44: 1223–1230.
28
94. Millar SJ, Goldstein EG, Levine MJ, Hausmann E. Modu-lation of bone metabolism by two chemically distinct lipo-polysaccharide fractions from Bacteroides gingivalis. InfectImmun 1986: 51: 302–306.
95. Mogi M, Otogoto J, Ota N, Inagaki H, Minami M, Kojima K.Interleukin 1beta, interleukin 6, beta2-microglobulin, andtransforming growth factor-alpha in gingival crevicularfluid from human periodontal disease. Arch Oral Biol1999: 44: 535–539.
96. Monefeldt K, Tollefsen T. Effects of streptococcal lipotei-choic acid on complement activation in vitro. J Clin Peri-odontol 1993: 20: 186–192.
97. Moore WE, Holdeman LV, Smibert RM, Hash DE, Burmeis-ter JA, Ranney RR. Bacteriology of severe periodontitis inyoung adult humans. Infect Immun 1982: 38: 1137–1148.
98. Morhart RE, Mata LJ, Sinskey AJ, Harris RS. A microbio-logical and biochemical study of gingival crevice debrisobtained from Guatemalan Mayan Indians. J Periodontol1970: 41: 644–649.
99. Mukaida N, Harada A, Yasumoto K, Matsushima K. Prop-erties of pro-inflammatory cell type specific leukocytechemotactic cytokines, interleukin-8 (IL-8) and monocytechemotactic and activating factor (MCAF). Microbiol Im-munol 1992: 36: 773–789.
100. Mullen LM, Richards DW, Quaranta V. Evidence that lami-nin-5 is a component of the tooth surface internal basallamina, supporting epithelial cell adhesion. J PeriodontalRes 1999: 34: 16–24.
101. Murgia C, Blaikie P, Kim N, Dans M, Petrie HT, GiancottiFG. Cell cycle and adhesion defects in mice carrying a tar-geted deletion of the integrin beta4 cytoplasmic domain.EMBO J 1998: 17: 3940–3951.
102. Murphy G, Knäuper V. Relating matrix metalloproteinasestructure to function: why the ‘hemopexin’ domain? Ma-trix Biol 1997: 15: 511–518.
103. Nakashima K, Roehrich N, Cimasoni G. Osteocalcin,prostaglandin E2 and alkaline phosphatase in gingival cre-vicular fluid: their relations to periodontal status. J ClinPeriodontol 1994: 21: 327–333.
104. Naleway C, Chou H, Manos T, Goodman C, Robinson P,Singer R. Assessment of the potential relationship betweenlevels of short chain fatty acids found in subgingivalplaque and periodontal health. J Dent Res 1989: 68: ab-stract 121.
105. Niederman R, Buyle-Bodin Y, Lu B-Y, Robinson P, NalewayC. Short-chain carboxylic acid concentration in humangingival crevicular fluid. J Dent Res 1997: 76: 575–579.
106. Niederman R, Zhang J, Kashket S. Short-chain carboxylic-acid-stimulated, PMN-mediated gingival inflammation.Crit Rev Oral Biol Med 1997: 8: 269–290.
107. Nilsson T, Carlsson J, Sundqvist G. Inactivation of key fac-tors of the plasma proteinase cascade systems by Bacter-oides gingivalis. Infect Immun 1985: 50: 467–471.
108. Noble RC, Penny BB. Comparison of leukocyte count andfunction in smoking and non-smoking young men. InfectImmun 1975: 12: 550–555.
109. Offenbacher S, Odle BM, Van Dyke TE. The use of crevic-ular fluid prostaglandin E2 levels as a predictor of peri-odontal attachment loss. J Periodontal Res 1986: 21: 101–112.
110. O’Garra A. Peptide regulatory factors. Interleukins and theimmune system. Part 1. Lancet 1989: 1: 943–946.
111. Overman DO, Salonen JI. Characterization of the human
Tooth–epithelial interface in health and disease
junctional epithelial cells directly attached to the tooth inperiodontal disease. J Dent Res 1994: 73: 1818–1823.
112. Page RC, Offenbacher S, Schroeder HE, Seymour GJ, Korn-man KS. Advances in the pathogenesis of periodontitis:summary of developments, clinical implications and fu-ture directions. Periodontol 2000 1997: 14: 216–248.
113. Page RC, Schroeder HE. Pathogenesis of inflammatoryperiodontal disease. A summary of current work. Lab In-vest 1976: 33: 235–249.
114. Payne JB, Johnson GK, Reinhardt RA, Dyer JK, Maze CA,Dunning DG. Nicotine effects on PGE2 and IL-1 beta re-lease by LPS treated human monocytes. J Periodontal Res1996: 31: 99–104.
115. Persson S, Claesson R, Carlsson J. The capacity of subgin-gival microbiotas to produce volatile sulphur compoundsin human serum. Oral Microbiol Immunol 1989: 4: 169–172.
116. Potempa J, Banbula A, Travis J. Role of bacterial protein-ases in matrix destruction and modulation. Periodontol2000 2000: 24: 153–192.
117. Preiss DS, Meyle J. Interleukin-1beta concentration of gin-gival crevicular fluid. J Periodontol 1994: 65: 423–428.
118. Pöllänen MT, Häkkinen L, Overman DO, Salonen JI. Lacto-ferrin impedes epithelial cell adhesion in vitro. J Peri-odontal Res 1998: 33: 8–16.
119. Pöllänen MT, Overman DO, Salonen JI. Bacterial metabo-lites sodium butyrate and propionate inhibit epithelial cellgrowth in vitro. J Periodontal Res 1997: 32: 326–334.
120. Pöllänen MT, Salonen JI, Grenier D, Uitto V-J. Epithelialcell response to challenge of bacterial lipoteichoic acidsand lipopolysaccharides in vitro. J Med Microbiol 2000: 49:245–252.
121. Reynolds JJ, Meikle MC. Mechanisms of connective tissuedestruction in periodontitis. Periodontol 2000 1997: 14:144–157.
122. Rodriguez A, Webster P, Ortego J, Andrews N. Lysosomesbehave as Ca2π-regulated exocytic vesicles in fibroblastsand epithelial cells. J Cell Biol 1997: 137: 93–104.
123. Rolla G, Iverson OJ, Bonesvoll P. Lipoteichoic acid-the keyto adhesiveness of sucrose-grown Streptococcus mutans.Adv Exp Med Biol 1978: 107: 607–617.
124. Rolla G, Oppermann RV, Bowen WH, Ciardi JE, Knox KW.High amounts of lipoteichoic acid in sucrose-inducedplaque in vivo. Caries Res 1980: 14: 235–238.
125. Rose RK, Hogg SD, Shellis RP. A quantitative study of cal-cium binding by isolated streptococcal cell walls andlipoteichoic acid: comparison with whole cells. J Dent Res1994: 73: 1742–1747.
126. Rossomando EF, White LB, Hadjimichael J. Immunomag-netic separation of tumour necrosis factor alpha. II. In situprocedure for the human gingival space. J Chromatogr1992: 27: 19–26.
127. Ryan MC, Lee K, Miyashita Y, Carter WG. Targeted disrup-tion of the LAMA3 gene in mice reveals abnormalities insurvival and late stage differentiation of epithelial cells. JCell Biol 1999: 145: 1309–1323.
128. Salonen J, Oda D, Funk SE, Sage H. Synthesis of type VIIIcollagen by epithelial cells of human gingiva. J PeriodontalRes 1991: 26: 355–360.
129. Salonen J, Pelliniemi LJ, Foidart JM, Risteli L, Santti R. Im-munohistochemical characterization of the basementmembranes of the human oral mucosa. Arch Oral Biol1984: 29: 363–368.
29
130. Salonen J, Santti R. Ultrastructural and immunohisto-chemical similarities in the attachment of human oral epi-thelium to the tooth in vivo and to an inert substrate inan explant culture. J Periodontal Res 1985: 20: 176–184.
131. Salonen J, Sewon L, Paunio K. Immunohistochemicallocalization of epithelial cells expressing transferrin recep-tors in normal and diseased human dento-gingival junc-tion. J Periodontal Res 1988: 23: 182–186.
132. Salonen J, Uitto VJ, Pan YM, Oda D. Proliferating oral epi-thelial cells in culture are capable of both extracellular andintracellular degradation of interstitial collagen. Matrix1991: 11: 43–55.
133. Salonen JI. Proliferative potential of the attached cells ofhuman junctional epithelium. J Periodontal Res 1994: 29:41–45.
134. Salonen JI, Kautsky MB, Dale BA. Changes in cell pheno-type during regeneration of junctional epithelium of hu-man gingiva in vitro. J Periodontal Res 1989: 24: 370–377.
135. Salonen JI, Pöllänen MT. Junctional epithelial cells directlyattached to the tooth. Acta Med Dent Helv 1997: 2: 137–140.
136. Salvi GE, Lawrence HP, Offenbacher S, Beck JD. Influenceof risk factors on the pathogenesis of periodontitis. Peri-odontol 2000 1997: 14: 173–201.
137. Salvi GE, Yalda B, Collins JG, Jones BH, Smith FW, ArnoldRR, Offenbacher S. Inflammatory mediator response as apotential marker for periodontal diseases in IDDM pa-tients. J Periodontol 1997: 68: 127–135.
138. Salzman AL, Wang H, Wollert PS, Vandermeer TJ,Compton CC, Denenberg AG, Fink MP. Endotoxin-inducedileal mucosal hyperpermeability in pigs: role of tissue aci-dosis. Am J Physiol 1994: 266: G633–G646.
139. Sandholm L. Proteases and their inhibitors in chronic in-flammatory periodontal disease. J Clin Periodontol 1986:13: 19–26.
140. Sarment DP, Korostoff J, D’Angelo M, Polson AM, FeldmanRS, Billings PC. In situ localization and characterization ofactive proteases in chronically inflamed and healthy hu-man gingival tissues. J Periodontol 1999: 11: 1303–1312.
141. Schroeder H. Differentiation of Human Oral Epithelia. Ba-sel: Karger 1981.
142. Schroeder H. The junctional epithelium. Origin, structure,and significance. Acta Med Dent Helv 1996: 1: 155–167.
143. Schroeder H, Listgarten M. Fine Structure of the Develop-ing Epithelial Attachment of Human Teeth. Monographs indevelopmental biology. Basel: Karger 1971/1977.
144. Schroeder H, Listgarten M. The gingival tissues: the archi-tecture of periodontal protection. Periodontol 2000 1997:13: 91–120.
145. Schroeder HE. Ultrastructure of the junctional epitheliumon the human gingiva. Helv Odontol Acta 1969: 13: 65–83.
146. Schwartz J, Stinson FL, Parker RB. The passage of triatedbacterial endotoxin across intact gingival crevicular epi-thelium. J Periodontol 1972: 43: 270–276.
147. Schwartz Z, Goultschin J, Dean D, Boyan BD. Mechanismsof alveolar bone destruction in periodontitis. Periodontol2000 1997: 14: 158–172.
148. Seguier S, Godeau G, Brousse N. Immunohistological andmorphometric analysis of intra-epithelial lymphocytesand Langerhans cells in healthy and diseased human gin-gival tissues. Arch Oral Biol 2000: 45: 441–452.
149. Seguier S, Godeau G, Leborgne M, Pivert G, Brousse N.Immunohistologic and morphometric analysis of cyto-
Pöllänen et al.
toxic T lymphocytes in gingivitis. J Periodontol 1999: 70:1383–1391.
150. Shapiro L, Lodato FM, Jr, Courant PR, Stallard RE. Endo-toxin determinations in gingival inflammation. J Peri-odontol 1972: 43: 591–596.
151. Singer RE, Buckner BA. Butyrate and propionate: import-ant components of toxic dental plaque extracts. Infect Im-mun 1981: 32: 458–463.
152. Singer RE, Buckner BA, Meckel AH, Leonard GJ. Propi-onate and butyrate induction of gingival inflammation inthe beagle. J Dent Res 1980: 59: Abstract 670.
153. Skougaard MR. Cell renewal, with special reference to thegingival epithelium. Adv Oral Biol 1970: 4: 261–288.
154. Snyderman R. Role for endotoxin and complement inperiodontal tissue destruction. J Dent Res 1972: 51: 356–361.
155. Solis-Gaffar MC, Rustogi KN, Gaffar A. Hydrogen sulfideproduction from gingival crevicular fluid. J Periodontol1980: 51: 603–606.
156. Sorkin BC, Niederman R. Short chain carboxylic acids de-crease human gingival keratinocyte proliferation and in-crease apoptosis and necrosis. J Clin Periodontol 1998: 25:311–315.
157. Sorsa T, Ingman T, Suomalainen K, Haapasalo M, Konttin-en Y, Lindy O, Saari H, Uitto VJ. Identification of proteasesfrom periodontopathogenic bacteria as activators of latenthuman neutrophil and fibroblast-type interstitial col-lagenases. Infect Immun 1992: 60: 4491–4495.
158. Sorsa T, Uitto V-J, Suomalainen K, Vauhkonen M, Lindy S.Comparison of interstitial collagenases from human gin-giva, sulcular fluid and polymorphonuclear leukocytes. JPeriodontal Res 1988: 23: 386–393.
159. Soukka T, Tenovuo J, Rundegren J. Agglutination of Strep-tococcus mutans serotype c cells but inhibition of Porphyr-omonas gingivalis autoaggregation by human lactoferrin.Arch Oral Biol 1993: 38: 227–232.
160. Squier CA. Keratinization of the sulcular epithelium – apointless pursuit? J Periodontol 1981: 52: 426–429.
161. Stern I. Current concepts of the dentogingival junction:the epithelial and connective tissue attachment to thetooth. J Periodontol 1981: 52: 465–476.
162. Sternberg EM, Chrousos GP, Wilder RL, Gold PW. Thestress response and the regulation of inflammatory dis-ease. Ann Intern Med 1992: 117: 854–866.
163. Stringer RE, Hart CA, Edwards SW. Sodium butyrate delaysneutrophil apoptosis: role of protein biosynthesis in neu-trophil survival. Br J Haematol 1996: 92: 169–175.
164. Summanen P, Baron EJ, Citron DM, Strong C, Wexler HM,Finegold SM. Advanced identification methods. In: Hoff-man, S, editor. Wadsworth Anaerobic Bacteriology Manual.Belmont, California: Star Publishing Co., 1993: 65–94.
165. Suomalainen K, Sorsa T, Uitto V-J, Vauhkonen M, LindyS. Characteristics of neutral proteases present in inflamedgingiva. Scand J Dent Res 1989: 97: 346–354.
166. Swartwout S, Niederman R. Bacterial metabolite mediateddifferential human PMN gene expression. J PeriodontalRes 1997: 32: 196–199.
167. Takata T, Miyauchi M, Ogava I, Ito H, Kobayashi J, Nikai H.Reactive change in proliferative activity of the junctionalepithelium after topical application of lipopolysaccharide.J Periodontol 1997: 68: 531–535.
168. Ten Cate AR. The role of epithelium in the development,structure and function of the tissues of tooth support. OralDis 1996: 2: 55–62.
30
169. Thorup AK, Dabelsteen E, Schou S, Gil SG, Carter WG, Re-ibel J. Differential expression of integrins and laminin-5 innormal oral epithelia. APMIS 1997: 105: 519–530.
170. Tipton DA, Dabbous MK. Effects of nicotine on prolifer-ation and extracellular matrix production of human gingi-val fibroblasts in vitro. J Periodontol 1995: 66: 1056–1064.
171. Tonetti M, Imboden M, Gerber L, Lang N, Laissue J, MullerC. Localized expression of mRNA for phagocyte-specificchemotactic cytokines in human periodontal infections.Infect Immun 1994: 62: 4005–4014.
172. Trowbridge IS, Omary B. Human cell surface glycoproteinrelated to cell proliferation is the receptor for transferrin.Proc Natl Acad Sci USA 1981: 78: 3039–3043.
173. Tzamouranis A, Matthys J, Ishikawa I, Cimasoni G. In-crease in endotoxin concentration in gingival washingsduring experimental gingivitis in man. J Periodontol 1979:50: 175–177.
174. Uitto J, Pulkkinen L. Molecular complexity of the cu-taneous basement membrane zone. Mol Biol Rep 1996: 23:35–46.
175. Uitto V-J, Larjava H. Extracellular matrix molecules andtheir receptors: an overview with special emphasis onperiodontal tissues. Crit Rev Oral Biol Medical 1991: 2:323–354.
176. Uitto VJ, Salonen JI, Firth JD, Jousimies-Somer H, Saarial-ho-Kere U. Matrilysin (matrix metalloproteinase-7) ex-pression in human junctional epithelium. J Dent Res 2002:81: 241–246.
177. van Steenbergen TJM, van der Mispel LMS, de Graaff J.Effects of ammonia and volatile fatty acids produced byoral bacteria on tissue culture cells. J Dent Res 1986: 65:909–912.
178. Visca P, Berlutti F, Vittorioso P, Dalmastri C, Thaller MC,Valenti P. Growth and adsorption of Streptococcus mutans6715–13 to hydroxyapatite in the presence of lactoferrin.Med Microbiol Immunol 1989: 178: 69–79.
179. Weiss SJ. Tissue destruction by neutrophils. N Engl J Med1989: 320: 365–376.
180. Whitfield C, Amor PA, Koplin R. Modulation of the surfacearchitecture of gram-negative bacteria by the action ofsurface polymer: lipid A-core ligase and by determinantsof the polymer chain length. Mol Microbiol 1997: 23: 629–638.
181. Wicken AJ, Knox KW. Chemical composition and prop-erties of amphiphiles. In: Shockman, GD, Wicken, AJ, edi-tors. Chemistry and Biological Activities of Bacterial Sur-face Amphiphiles. New York: Academic Press Inc., 1981: 1–9.
182. Wicken AJ, Knox KW. Lipoteichoic acids: a new class ofbacterial antigen. Science 1975: 187: 1161–1167.
183. Wiebe CB, Larjava HS. Abnormal deposition of type VIIcollagen in Kindler syndrome. Arch Dermatol Res 1999:251: 6–13.
184. Wilson CL, Ouellette AJ, Satchell DP, Ayabe T, Lopez-BoadoYS, Stratman JL, Hultgren SJ, Matrisian LM, Parks WC.Regulation of intestinal alpha defensin activation by themetalloproteinase matrilysin in innate host defence.Science 1999: 286: 113–117.
185. Wilson JT. Metabolism of bacteria. In: Schuster, GS, editor.Oral Microbiology and Infectious Disease. Toronto: B.C..Decker Inc., 1990: 57–67.
186. Wilson RM, Reeves WG. Neutrophil phagocytosis and kill-ing in insulin-dependent diabetes. Clin Exp Immunol1986: 63: 478–484.
Tooth–epithelial interface in health and disease
187. Wilton JMA. Crevicular neutrophils: protective or damag-ing?. In: Lehner, T, Cimasoni, G, editors. Borderland Be-tween Caries and Periodontal Disease III. Geneva: EditionsMedecine et Hygiene, 1986: 71–85.
188. Winkler JR, Grassi M, Murray PA. Clinical description andetiology of HIV-associated periodontal diseases. In: Rob-ertson, PB, Greenspan, JS, editors. Perspectives on OralManifestations of AIDS. Littleton: MA.. PSG Publishing,1988: 49–70.
189. Wright DG, Gallin JI. Secretory responses of human neu-trophils: exocytosis of specific (secondary) granules by hu-
31
man neutrophils during adherence in vitro and duringexudation in vivo. J Immunol 1979: 123: 285–294.
190. Yamaza T, Kido MA, Kiyoshima T, Nishimura Y, HimenoM, Tanaka T. A fluid-phase endocytotic capacity and intra-cellular degradation of a foreign protein (horseradish per-oxidase) by lysosomal cysteine proteinases in the rat junc-tional epithelium. J Periodontal Res 1997: 82: 651–660.
191. Zhang J. Gingival inflammation induced by food and shortchain carboxylic acids. DMSc Thesis, Harvard University,1996.