Butterwick Hospice NewApproachComprehensive Report ... · Butterwick Hospice is operated by...
Transcript of Butterwick Hospice NewApproachComprehensive Report ... · Butterwick Hospice is operated by...

This report describes our judgement of the quality of care at this location. It is based on a combination of what wefound when we inspected and a review of all information available to CQC including information given to us frompatients, the public and other organisations
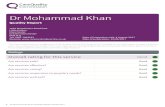
Ratings
Overall rating for this location Requires improvement –––
Are services safe? Requires improvement –––
Are services effective? Requires improvement –––
Are services caring? Good –––
Are services responsive? Requires improvement –––
Are services well-led? Requires improvement –––
Overall summary
Butterwick Hospice is operated by Butterwick Limited.The hospice was purposely built; is fully accessible andhas appropriate facilities for day-care, therapies andfamily support.
The hospice provides adult hospice services thatincludes; palliative and neurological day-care, familysupport services for adults, children and young people
and a home visiting service for palliative care and end oflife patients. The hospice does not have any inpatientbeds. We inspected this service using our comprehensiveinspection methodology.
We carried out a short-notice announced inspection on 3,4 and 10 March 2020. During the inspection, we visitedthe hospice at Bishop Auckland and the day-care facilityat Sedgefield community hospital. We also visited twopatients at home who were receiving care from the homecare team. We spoke with 15 staff including registered
ButtButtererwickwick HospicHospiceeQuality Report
Woodhouse Lane,Bishop AucklandDL14 6JUTel: 01388 603003Website: www.butterwick.org.uk/ourhospices/butterwickhospicebishopauckland/
Date of inspection visit: 03 to 04 March and 10 March2020Date of publication: 15/05/2020
1 Butterwick Hospice Quality Report 15/05/2020

nurses, health care assistants, reception staff, medicalstaff and senior managers. We spoke with seven patientsand relatives using day-care services and two patientsand their family members on home visits. During ourinspection, we observed patient care and interactionsand reviewed ten sets of patient records. We alsoreviewed other information and data about the hospiceand provided by the hospice to make our judgements.
To get to the heart of patients’ experiences of care andtreatment, we ask the same five questions of all services:are they safe, effective, caring, responsive to people'sneeds, and well-led? Where we have a legal duty to do sowe rate services’ performance against each key questionas outstanding, good, requires improvement orinadequate.
Throughout the inspection, we took account of whatpeople told us and how the provider understood andcomplied with the Mental Capacity Act 2005.
We rated the service as requires improvement overall. Werated safe, effective, responsive and well- led as requiresimprovement. We rated caring as good.
We found areas of practice that require improvement:
• Patient risks were not identified, assessed andmonitored in a consistent manner across all areas ofthe hospice and re-assessments were in-frequent.
• Health and safety risks were not consistently identifiedassessed and document. They were not alwaysescalated so they could not be adequately addressedand reviewed.
• Policies and processes regarding management ofmedicines did not meet the needs of all areas andwere therefore unfit for purpose. This had led toinconsistent practice in different areas.
• Not all staff and leaders were clear about their rolesand responsibilities in relation to governance andperformance.
• The provider had a large number of policies andprocedures that need to be brought up to date and inline with current guidance and best practice. This wasan ongoing piece of work.
• Staff and managers were not clear about theirresponsibilities in relation to ‘Duty of Candour’
• The hospice needed to improve the information itcollected and how it used it, to improve services and
patient outcomes. Audits were infrequent andfeedback and improvement actions were notmonitored. These were not always checked to see ifimprovements had been made or sustained.
• The hospice did not monitor waiting times in all partsof the service or monitor the impact of long waits onpatients.
We found good practice:
• The service had enough staff with the rightqualifications, skills, training and experience to keeppeople safe from avoidable harm and to provide theright care and treatment. Staff understood how toprotect patients from abuse and the service workedwell with other agencies to do so
• Staff recognised and reported incidents and nearmisses. Managers investigated incidents and sharedlessons learned with the whole team and the widerservice.
• Staff gave patients enough food and drink to meettheir needs and improve their health. Staff gavepatients and families practical support and advice tolive well.
• Staff supported patients to make informed decisionsabout their care and treatment. Staff treated patientswith compassion and kindness, respected their privacyand dignity, and took account of their individualneeds. Staff made reasonable adjustments to helppatients access services. They coordinated care withother services and providers.
• Leaders and staff actively and openly engaged withpatients, staff, the public and local organisations toplan and manage services. Staff felt respected,supported and valued and could raise concernswithout fear. All staff were committed to continuallylearning and improving services.
Following this inspection, we told the provider that itmust take some actions to comply with the regulationsand that it should make other improvements, eventhough a regulation had not been breached, to help theservice improve. We also issued the provider with threerequirement notices. Details are at the end of the report.
Ann Ford
Deputy Chief Inspector of Hospitals, North
Summary of findings
2 Butterwick Hospice Quality Report 15/05/2020

Our judgements about each of the main services
Service Rating Summary of each main service
Hospiceservices foradults Requires improvement –––
We rated the hospice as requires improvementoverall.We rated safe, effective, responsive and well-ledas requires improvement.We rated caring as good.
Summary of findings
3 Butterwick Hospice Quality Report 15/05/2020

Contents
PageSummary of this inspectionBackground to Butterwick Hospice 6
Our inspection team 6
Information about Butterwick Hospice 6
The five questions we ask about services and what we found 8
Detailed findings from this inspectionOverview of ratings 11
Outstanding practice 32
Areas for improvement 32
Action we have told the provider to take 33
Summary of findings
4 Butterwick Hospice Quality Report 15/05/2020

Butterwick Hospice
Services we looked atHospice services for adults
ButterwickHospice
Requires improvement –––
5 Butterwick Hospice Quality Report 15/05/2020

Background to Butterwick Hospice
Butterwick Hospice is operated by Butterwick Limited.The hospice opened in 1984 and is an independenthospice in Bishop Auckland, County Durham. It hasoutreach centres at Sedgefield community hospital,Weardale community hospital in Stanhope and theRichardson community hospital in Barnard Castle. Thehospice primarily serves the communities of the DurhamDales, Easington and Sedgefield clinical commissioninggroup areas.
Butterwick hospice provides adult hospice services whichincludes; palliative day care services with access tonursing care, physiotherapy and complementarytherapies, diversional therapies and social interaction. Italso provides a specialist neurological day care serviceand a palliative home care team which predominantlyprovides an overnight service. A family support workteam provides support and counselling to thosebereaved or affected by a life limiting illness. The family
support work team provides services to adults andchildren and young adults in the wider family. Theoutpatient complimentary therapies provision extends topatients with a life limiting diagnosis and carers.
The hospice has had a registered manager in post sinceDecember 2014 and is registered to provide the followingregulated activities;
· Nursing care,
· Personal care,
· Transport services,
· Triage and medical advice provided remotely,
· Treatment of disease, disorder or injury.
This was the first inspection of the hospice using thehospital inspection framework. CQC last inspection of thehospice was 10 June 2015, published: 28 August 2015. Itwas inspected using the adult social care framework andwas rated as Good across all domains.
Our inspection team
The team that inspected the service comprised a CQClead inspector,another CQC inspector, and a specialistadvisor with expertise in hospice services. The inspectionteam was overseen by Sarah Dronsfield, Head of HospitalInspection.
Information about Butterwick Hospice
The hospice is a purpose-built day-care facility in BishopAuckland, County Durham with outreach centres inSedgefield community hospital, Weardale communityhospital at Stanhope and the Richardson communityhospital at Barnard Castle.
During the inspection, we visited the Bishop Aucklandhospice site and the outreach day centre provided atSedgefield community hospital. We also went on twohome visits with the homecare team. We spoke with 15staff including registered nurses, health care assistants,family support counsellors, volunteers and senior
managers. We spoke with two patients using day-careservices and two patients and their family members onhome visits. During our inspection, we observed patientcare and interactions and reviewed 10 sets of patientrecords. We also reviewed other information and dataabout the hospice and provided by the hospice to makeour judgements.
Summaryofthisinspection
Summary of this inspection
6 Butterwick Hospice Quality Report 15/05/2020

There were no special reviews or investigations of thehospice ongoing by the CQC at any time during the 12months before this inspection. This was the hospice’s firstinspection using the current hospital inspectionframework.
Activity (April 2018 - March 2019)
• In the reporting period April 2018 - March 2019 thehospice provided services to 645 service users. Ofthese 524 were adults and 121 were children andyoung people accessing family support. Of the adults,44% were receiving services as palliative care patientsand 56% of patients had a life-limiting illness.
The hospice employed 6 registered nurses, 8 careassistants, three complementary therapists and threefamily support counsellors. The hospice also employedadministrative staff, volunteers and seven palliative homecare staff. The accountable officer for controlled drugs(CDs) was the registered manager.
Track record on safety
Zero - Never events
Clinical incidents: eight (in the last six months)
Zero - serious injuries
Zero - incidents of hospice acquired Meticillin-resistantStaphylococcus aureus (MRSA),
Zero - incidents of hospice acquired Meticillin-sensitivestaphylococcus aureus (MSSA)
Zero - incidents of hospice acquired Clostridium difficile(C. diff)
Zero - incidents of hospice acquired E. coli
Zero - complaints
Services accredited by a national body:
• Investors in people (2019)• “Disability Confident Employer Level 2”
Services provided at the hospice under service levelagreement:
• Physiotherapy• Pharmacy services• Chaplaincy services• Waste removal• Specialist equipment maintenance and testing• Infection prevention and control support
Summaryofthisinspection
Summary of this inspection
7 Butterwick Hospice Quality Report 15/05/2020

The five questions we ask about services and what we found
We always ask the following five questions of services.
Are services safe?We rated safe as requires improvement because:
• There were a number of environmental risks that the hospiceneeded to address. Some hand-wash basins were notcompliant with current guidance. Access to staff only parts ofthe building and hazardous substances were not alwayssecured.
• Although staff completed risk assessments when patients wereadmitted to the day-care service, there was no recognisedstandard or policy for how often patient risk assessmentsshould be redone.
• Records were not always complete or updated regularly.• The service did not have consistent systems and processes to
transcribe, administer, record and store medicines. Themedicines policies were not fit for purpose.
• Staff did not understand duty of candour. The duty of candourand incident policies did not completely reflect current bestpractice and legislation.
However, we also found the following areas of good practice:
• The service provided mandatory training in key skills to all staffand made sure everyone completed it.
• Staff understood how to protect patients from abuse and theservice worked well with other agencies to do so.
• The service had enough staff with the right qualifications, skills,training and experience to keep patients safe from avoidableharm and to provide the right care and treatment.
• Staff recognised and reported incidents and near misses.Managers investigated incidents and shared lessons learned.
Requires improvement –––
Are services effective?We rated effective as requires improvement because:
• Many of the service policies required reviewing and updating tobring them in line with best practice and national guidance.
• Overall the service did not have a systematic approach toaudits.
• Although data was collected, regarding patient outcomes, wewere unable to see how these could be used to improvepatients’ outcomes.
• Home-care staff were concerned that patients may have to waita long time for pain relief as they were currently unable toadminister medicines in patients’ homes.
Requires improvement –––
Summaryofthisinspection
Summary of this inspection
8 Butterwick Hospice Quality Report 15/05/2020

• There was no formal documentation for staff to use to supportthem in making and documenting best interest decisions.
However, we also found the following areas of good practice:
• Staff gave patients enough food and drink to meet their andmonitored patients regularly to see if they were comfortable orin pain.
• The service made sure staff were competent for their roles.• All those responsible for delivering care worked together as a
team to benefit patients.• Staff supported patients to make informed decisions about
their care and treatment.
Are services caring?We rated caring as good because:
• Staff treated patients with compassion and kindness, respectedtheir privacy and dignity, and took account of their individualneeds.
• Staff provided emotional support to patients, families andcarers to minimise their distress. They understood patients’personal, cultural and religious needs.
• Staff supported and involved patients, families and carers tounderstand their condition and make decisions about theircare and treatment. They ensured a family centred approachand offered support services to families including children andyoung people.
Good –––
Are services responsive?We rated responsive as requires improvement because:
• Managers did not monitor waiting times for neurological daycare services and patients could have extended waits, beforebeing able to access this service.
• Managers did not assess the impact of waiting time on patientswaiting to access the service.
• Although family support services had some targets in relation towaiting time from referral to assessment, they did not monitorwaiting times for access to treatment or assess the impact oflong waits.
However, we also found the found the following areas of goodpractice:
• The service took account of patients’ individual needs andpreferences. Staff made reasonable adjustments to helppatients access services and coordinated care with otherservices.
Requires improvement –––
Summaryofthisinspection
Summary of this inspection
9 Butterwick Hospice Quality Report 15/05/2020

• Patients could access the specialist palliative care servicesquickly when they needed them.
• It was easy for people to give feedback and raise concernsabout care received. The service acted on any concerns andcomplaints raised.
Are services well-led?We rated well-led as requires improvement because:
• Leaders did not fully understand and manage the priorities andissues the service faced.
• Leaders and teams did not have robust systems to manage allrisks and performance effectively.
• Leaders did not have effective governance processes,throughout the service. There were gaps in information andoversight.
• Not all staff at all levels were clear about their roles andaccountabilities.
• Clinical leads did not have regular opportunities to meet,discuss issues, propose improvements and learn from theperformance of the service.
However, we also found the following areas of good practice:
• The hospice had a strategic five-year plan for 2019-2024 whichoutlined its priorities and the enabling actions required.
• Leaders and staff actively and openly engaged with patients,staff, the public and local organisations to plan and manageservices.
• Staff felt respected, supported and valued and could raiseconcerns without fear.
• All staff were committed to continually learning and improvingservices.
Requires improvement –––
Summaryofthisinspection
Summary of this inspection
10 Butterwick Hospice Quality Report 15/05/2020

Overview of ratings
Our ratings for this location are:
Safe Effective Caring Responsive Well-led Overall
Hospice services foradults
Requiresimprovement
Requiresimprovement Good Requires
improvementRequires
improvementRequires
improvement
Overall Requiresimprovement
Requiresimprovement Good Requires
improvementRequires
improvementRequires
improvement
Detailed findings from this inspection
11 Butterwick Hospice Quality Report 15/05/2020

Safe Requires improvement –––
Effective Requires improvement –––
Caring Good –––
Responsive Requires improvement –––
Well-led Requires improvement –––
Are hospice services for adults safe?
Requires improvement –––
We rated safe as requires improvement.
Mandatory training
The service provided mandatory training in keyskills to all staff and made sure everyone completedit.
Nursing staff received and kept up-to-date with theirmandatory training. Training data showed thatmandatory training compliance was good, all moduleswere over the 75% compliance target.
Staff we spoke with all told us they were up to date withmandatory training and that they received alerts fromtheir manager when updates were due in the next month.Most mandatory training was completed online, andvolunteers told us they had also received appropriatetraining for their role.
Staff we spoke with who had been with the hospice for upto one year told us they had received an induction andenough training to ensure they felt competent to be ableto carry out their role. The first two weeks in their postwas as a supernumerary member of staff.
The mandatory training was comprehensive and met theneeds of patients and staff. Mandatory training included;health and safety, fire safety, information governance,record keeping, moving and handling, infection control,basic life support, adult and children’s safeguarding andmental capacity act and deprivation of liberty standards.
Managers monitored mandatory training and alerted staffwhen they needed to update their training.
Safeguarding
Staff understood how to protect patients from abuseand the service worked well with other agencies todo so. Staff had training on how to recognise andreport abuse and they knew how to apply it.
All staff received training at an appropriate level for theirrole on how to recognise and report abuse. Staff wespoke to told us they had received safeguarding training.
Staff knew how to make a safeguarding referral and whoto inform if they had concerns. They were able to explaintheir role in raising concerns, understood theirresponsibilities and were aware of who they could go tofor help and support.
Staff knew how to identify adults and children at risk of,or suffering, significant harm and worked with otheragencies to protect them. Staff provided a specificexample of a patient who had disclosed concerns aboutabuse, and we were assured that they had taken allcorrect and necessary action in relation to theinformation received.
Home-care staff we spoke with gave us examples of whenthey had raised concerns with their line manager ormembers of the multi-disciplinary team. They told us thecommunity nurses tended to take a lead when theyraised safeguarding concerns. They described how theyhad followed up to check the concerns had beenaddressed by the community nurse and alerted their ownmanagers of the issue.
Cleanliness, infection control and hygiene
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
12 Butterwick Hospice Quality Report 15/05/2020

The service, controlled infection risk well. Staff usedequipment and control measures to protectpatients, themselves and others from infection.They kept equipment and the premises visibly clean.
The hospice was clean and had suitable furnishingswhich were clean and well-maintained.
Cleaning records were up-to-date and demonstrated thatall areas were cleaned regularly. There was a process inplace to ensure flushing of water outlets on a weeklybasis.
Staff followed infection control principles including theuse of personal protective equipment (PPE). We observedstaff adhering to ‘bare below the elbow’, washing hands,using hand sanitiser and using PPE appropriately.
An infection control audit was undertaken annually by anexternal infection control and prevention matron, as partof a service level agreement. The latest audit in June 2019gave an overall score of 91% compliance. Areas forimprovement were display of hand washing posters, notall furniture was easily cleaned and not all patient washbowls had been washed and stored correctly.
Comments at the end of the audit indicated there wereareas of the hospice that needed to be upgraded and thatthese issues had been highlighted in previous years’audits. For example, it was recommended a carpet in thequiet room be re-placed with hard flooring, some clinicalhand washing basins needed upgrading as they did notmeet current recommendations, a bucket sink needed tobe removed from the laundry room and some otherdecorative features and furnishings in the quiet roomneeded repairing / replacing to make them easier toclean. There was also a need for a clinical hand washingbasin in the quiet room.
We could see from the audit action plan that any areasthat could be addressed were fed back to the clinicalteams for immediate action but there was no evidence ofongoing audit to check that actions were taken, andimprovements sustained. The action plan indicated thatupgrades to sink and environment would be addressedwhen funding allowed but these issues had not beenescalated to the risk register, despite beingrecommendations from previous years’ audits.
Although there was still no hand wash basin in the quietroom, we saw there was hand gel available.
A uniform audit in February 2020 showed 100%compliance with; bare below the elbow, no wrist watchesor inappropriate jewellery, nails – short, clean and nopolish, uniform correct and hair tied back. The only areafor action was staff carrying personal hand rub, 56% ofstaff were compliant. All clinical staff had their own handgel and the non-clinical staff and volunteers were usinggel at room entrances.
Feedback from a carers survey rated the generalcondition and cleanliness of the hospice premises asexcellent.
We observed a care worker using alcohol hand gel beforeassisting a patient to re-position. When checkingcatheters, disposable gloves were used, and the careworker washed their hands with soap and waterimmediately after completion of the task. Separatetowels were provided in the home environment for careworkers to use.
Home-care staff carried PPE and hand sanitiser withthem and told us they could top up whenever theyneeded to.
Cleaning cupboards onsite were secure and a referencefile with guidance for each substance used was stored inthese areas.
Environment and equipment
There were a number of environmental risks thatthe hospice needed to address. The hospice neededto upgrade the hand-wash basins where they werenot compliant with current guidance. We also founda number of risks where access to staff only parts ofthe building and hazardous substances was notsecured. However, equipment and premises werewell maintained, and staff managed clinical wastewell.
Patients could reach call bells and staff respondedquickly when called.
An infection control audit had identified that twohand-wash basins needed upgrading to be compliantwith current recommendations. The hand-wash basins inthe treatment room and domestic cupboard weredomestic basins (with overflows) which are unsuitable for
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
13 Butterwick Hospice Quality Report 15/05/2020

clinical settings. The quiet room needed to have a handwash basin installing. These recommendations had beenmade annually for the last three years but the hospicehad not added this to the risk register or taken any action.
The service had suitable facilities to meet the needs ofpatients’ families
The service had enough suitable equipment to help themto safely care for patients.
Staff disposed of clinical waste safely however, there werea number of risks regarding potential unauthorisedaccess to certain areas, chemicals and razors. We foundrazors in an unlocked cupboard in the bathroom, a keyhad been left in a door in the sluice, giving access to themains gas switch. In the area used by children there was akey left in the lock leading to a staircase giving access to aloft containing aerosols, other hazardous materials andaccess to a large drop of approximately four metres.
There was a maintenance programme in place forpremises and equipment and we found plannedmaintenance took place as needed. We checkedequipment such as hoists, oxygen and suction and foundthey were checked within the last 12 months. Equipmentwas labelled with when the next service or electrical testwas due.
There was a process in place to ensure flushing of wateroutlets on a weekly basis. We saw this was recorded onthe maintenance log for the hospice environment andequipment.
Staff cleaned equipment such as hoists and commodesafter each use and labelled them as clean and ready foruse. Staff checked and charged batteries on items such ashoists weekly.
The home care service did not provide any equipment foruse in patients’ homes other than disposable infectionprevention materials used by workers when caring forpatients. All equipment was provided by the local trustwho retained responsibility for maintenance andcollection of these. However, care workers told us that if apiece of equipment was found to be broken or notworking correctly, they would report this to the localdistrict nursing team.
When someone was using the hospice’s quiet room andchapel, they could not be observed from the corridor
outside which maintained their privacy and dignity.However, there was no alarm system in these rooms so ifa patient was using the space and fell ill, they could beunnoticed and unable to raise the alarm.
Quiet rooms and spaces that could be used by patients orvisiting children had ligature risks which had not beenindividually assessed. Ligature risks were blinds andstring bags. However, staff were aware of the risks andtold us that patients and visitors were not left alone inthese rooms. Managers had risk assessed this on anotherhospice premises and alerted staff in these areas.
The main hospice day room was bright and appearedclean. Chairs of varying heights with wipeable coveringwere available for patients to use. Corridors and signagewere dementia friendly including signs with pictures andtext.
Assessing and responding to patient risk
Although staff completed risk assessments whenpatients were admitted to the day-care service,there was no recognised standard or policy for howoften patient risk assessments should be redone.This meant frequency of risk assessments wasinfrequent and although some patients had beenformally reassessed regularly others had not.
Staff completed and updated risk assessments for eachpatient on admission to the service. Risk assessmentsincluded mouth-care, manual handling, falls, skin,nutrition and a carer needs assessment. Staff told us thatthey re-visited risk assessments and care plansthree-monthly. However, there was no policy or processto provide guidance to staff regarding frequency and itwas it clear from the records we looked at that thisstandard was not always adhered to. Although, one set ofrecords clearly showed a re-assessment had beencompleted after three months and a falls re-assessmenthad also been completed following a fall at home.Another patient who had attended the service since 2016did not have evidence of any re-assessments of theiroriginal risks but a recent new risk assessment had beenadded to this record regarding the patient’s mental healthand well-being.
Staff were trained to respond promptly to any suddendeterioration in a patient’s health. They were
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
14 Butterwick Hospice Quality Report 15/05/2020

knowledgeable about what action to take when anemergency arose. All staff were trained in basic lifesupport and the emergency response included using the999 service.
We found that where patients had do not attemptcardio-pulmonary resuscitation (DNACPR) in place, acopy of the form was kept at the front of patients notes.Patients who had these were asked to carry the originalon them when attending the hospice to ensure staffacted according to their wishes and advanced decisions.
We found generic patient risk assessments in each of theclinical areas. For example, in the physiotherapy roomand Sedgefield outreach centre we found assessmentsthat included choking, collapse, exposure to bodily fluids,use of oxygen and suction and anaphylaxis.
We did not see evidence of environmental riskassessments for all the risks we identified, such aswhether the relevant rooms were suitable or safe forchildren or for items such as window blinds which couldpotentially be a ligature risk. However, the hospice haddone a risk assessment of window blinds and cords as across location risk and had identified and implementedappropriate mitigations.
Before starting any complementary therapy, a therapistwould carry out a home visit to perform an assessment.This included; advising the patient of the treatmentsavailable and how often they could be carried out; theywould carry out a patch test to ensure it was safe to usetreatments and they would give the patient aninformation leaflet and contact number.
The service could access counselling and specialistmental health support, if staff were concerned about apatient’s mental health. Staff told us they could gaindirect access to counselling and family support and theycould refer into other primary care services and GPs whenneeded.
Staff would refer patients to GPs or mental health servicesfor mental health assessments for any patients thought tobe at risk of self-harm or suicide. Other patients could bereferred with conditions such as anxiety and depression.
Staff working in day-care received a morning handoverevery day. This was accompanied by a sheet giving detailsof patients and any specific needs or things for staff toconsider when providing care. Handover information
included all necessary key information to keep patientssafe. For example, food allergies and dietaryrequirements, risks, mobility, relevant medical history /condition and care interventions that would be requiredwere included.
Outreach service staff told us they held a briefing threetimes a week.
Staff were receiving alerts and information about thecorona virus outbreak and posters were on display forpatients and relatives.
Within the home-care service we found that patient helddocumentation was being replaced with a newer versionof a daily living and needs assessment and associatedrisk assessments. One of the home-care assistantsshowed us the new paperwork updated as animprovement action following a CQC inspection atanother location. They told us that staff had receivedinformation and talked through with managers how theyshould complete the documents. The HCA told us thenew documentation was being rolled out over the courseof their next visits.
The new documentation included a holistic assessmentof daily living activities and needs and included riskassessments for skin and a body map, mouth care,nutrition, and moving and handling.
Healthcare workers providing care to patients in theirown homes worked alone. They had an electronic loneworker system linked to a central call centre whichprovided extra security by logging workers in and out oftheir visits and provided an hourly call back service ifrequired. Additional backup was provided by a seniormember of staff who held an emergency telephonenumber on a rota. Hospice staff worked closely with thedistrict nursing team and Marie Curie support staff andwould contact them to provide extra support if required.
Staffing
The service had enough nursing and support staffwith the right qualifications, skills, training andexperience to keep patients safe from avoidableharm and to provide the right care and treatment.Managers regularly reviewed and adjusted staffinglevels and skill mix, and gave bank and agency staffa full induction.
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
15 Butterwick Hospice Quality Report 15/05/2020

The service had enough nursing and support staff to keeppatients safe.
The hospice employed six registered nurses, eight careassistants, three complementary therapists and threefamily support counsellors. The hospice also employedadministrative staff, volunteers and seven palliative homecare staff. The accountable officer for controlled drugs(CDs) was the registered manager.
There was a minimum staffing level of two registerednurses and two healthcare assistants for each clinic. Stafftold us they planned ahead for day care sessions andcould adjust staffing levels daily according to the needs ofpatients by requesting additional staff.
The service had low vacancy, turnover and sickness rates.
The hospice had its own pool of bank staff so additionalstaff were familiar with the service.
Managers made sure all bank and agency staff had a fullinduction and understood the service and what wasexpected of them.
Staff in the day care centres felt there were enough staffto deliver good, safe care. They told us they looked atpatient acuity for those patients attending for day careand were able to request an additional member of staff ifneeded. Staff told us they had plenty of time to spendwith patients and develop relationships. A member ofstaff explained that “people trust you, they have time toopen up to you.”
Home-care staff worked alone and primarily provided arespite service for a patient’s carer. There was a process inplace for them to contact the district nursing or localauthority home care team for help if necessary.Home-care staff told us this would usually only benecessary if something untoward happened or if apatient’s condition had changed unexpectedly.
There was a lone worker system in place to help keepstaff safe.
Records
Records were not always complete or updatedregularly. However, records were stored securelyand available to all staff providing care.
Staff had access to up-to-date, medical information onpatients’ care and treatment. However, this needed to be
requested from GPs who would download a summaryfrom their electronic system to share with the patient’sconsent. This information was not available in all of thecare records we looked at and there was no standardprocess regarding how often the hospice would requestan update from patients’ GPs.
The service did not have direct access to electronicpatient care records so could not access and downloadthis information directly.
Patient notes were stored securely, and all staff couldaccess them easily
Staff recorded daily evaluations of the care provided atthe day centre or in the patient’s home. Healthcareassistants providing day-care did not write directly inrecords but would bring anything relevant to theattention of nurses leading sessions who would recordthis.
We looked at nine sets of patient notes. These containedinitial care plans detailing people’s personal health,financial and spiritual needs. However, we saw that someof these plans dated back to 2016 and had not beenupdated since then. Others had been updated annually.Records of care were clear, and we could see that wherefurther assessment such as care plans for fatigue, anxiety,dyspnoea or pain were needed, these were appropriatelycompleted.
The hospice had not undertaken any recent recordsaudits
Medicines
The service did not have consistent systems andprocesses to safely transcribe, administer, recordand store medicines. The medicines policies andprocedures were not fit for purpose.
The hospice was reviewing medicine policies andprocedures as part of a whole system review of policiesand were aware the current medicine policies andprocedures were not fit for purpose.
Policies were inconsistent and staff were unable to followthem in some areas. Staff in some areas had introducednew ways of working to make areas of medicines
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
16 Butterwick Hospice Quality Report 15/05/2020

management safer. However, the policies had not yetbeen reviewed and the new practices had not beenformally accepted and rolled out across all teams andcentres.
Some policies and or procedures appeared to be havewritten for a specific area of the hospice withoutconsideration of other teams or settings. For example, theprocedure for transcribing of medicines to beadministered by staff appeared to have been written forthe children’s inpatient unit. The procedure did not meetthe needs of staff in the day-care setting or thoseproviding care in patients’ homes.
There was a clear need for a robust transcribingprocedure and supporting policies to be in place forsome of the current patients. We met a patient who couldnot administer their own medicine but attended thehospice on a rolling programme. There was also thepotential that as patients’ conditions progressed, theywould become unable to self-administer because of adecline in either their motor or cognitive skills.
There were mixed messages from staff in day caresettings as to whether they transcribed and administeredmedicines or not. In one setting, nurses told us practicewas to transcribe a patient’s medicines onto a medicineadministration record (MAR) and two nurses checked themedicine and the patient identity before administering.This practice was not fully supported by the hospicepolicies. Other nurses told us they did not need toadminister medicines as patients kept their ownmedicines and self-administered.
There was no formal or consistent risk assessment forself-administration of medicines in the hospiceenvironment although we did see that this had beenconsidered in some of the admission documentation.
Health care assistants in the home-care team told us theydid not give medicines, however they also told us thatthey felt it would be beneficial to be able to administer ‘asrequired’ pain medicines when a patient was strugglingto self-administer. They described a process where theywould ring a community nurse or a family member toattend the patient if they required pain relief. Staff wereconcerned that a patient could potentially be in pain ordiscomfort for lengthy periods if nurses or family
members were unable to come immediately. Managerswere aware of this concern and were reviewing whattraining, policies and procedures would be needed forhome-care staff to be able to do this.
The service had systems to ensure staff knew aboutpatient safety alerts and incidents. These were cascadedto all staff though emails and handovers.
The hospice had a controlled drug (CD) cabinet for anypatient medicines that fell into this category and othermedicines were kept by the patient. A controlled drugregister was used to record CDs being added to the storeand for medicines taken out and given back to thepatient. The key to the cupboard was kept securely whereit could be accessed by the registered nurses who neededit.
The registered manager was the accountable officer forCDs. The hospice held a current Home Office licence forcontrolled drugs.
Incidents
Staff did not understand duty of candour. The dutyof candour and incident policies did not completelyreflect current best practice and legislation or guidestaff to make appropriate judgements regardinglevel of harm and when to implement duty ofcandour. However, staff recognised and reportedincidents and near misses. Managers investigatedincidents and shared lessons learned with the wholeteam and ensured that actions from patient safetyalerts were implemented and monitored.
Staff we spoke with knew how and when to reportincidents. Although written policy information aboutbeing open with patients and duty of candour wasunclear, it was clear from examples that staff gave us,their first responsibility was to patients and families. Staffdid not understand the legal requirements of duty ofcandour and when this should be implemented.
The Duty of Candour (DoC) is a legal duty to inform andapologise to patients if there have been mistakes in theircare that has led to moderate or significant harm. Theincident policy did not guide staff in judging level of harmor indicate when duty of candour should beimplemented. However, managers were aware of thelimitations of the current policies and these were beingreviewed.
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
17 Butterwick Hospice Quality Report 15/05/2020

Managers had just implemented a weekly incident reviewgroup and had held their first two meetings. They felt themeetings had been worthwhile and would give them amuch better oversight of all incidents across the hospicelocations to be able to identify any themes, sharelearning and make improvements. The group looked atall new incidents and followed up any outstandingactions from previous incidents. There were six newincidents in the first and second week of the reviewstaking place and one of these was a fall at the hospice.The incident review had clearly identified areas ofpractice to be reviewed as part of the incidentinvestigation.
There were eight incidents reported during thesix-months before this inspection.
The service had no never events in the previous 12months. Never events are serious Incidents that arewholly preventable because guidance or safetyrecommendations that provide strong systemicprotective barriers are available at a national level andshould have been implemented by all healthcareproviders.
Managers investigated incidents thoroughly while beingsupportive of staff involved. A ‘look back’ exercise wasundertaken for any emergency transfers or emergencysituations such as deterioration of a patient to ensurestaff were able to debrief and to determine if there wereany opportunities for learning.
Staff told us they received feedback from investigation ofincidents and learning was shared through teammeetings and at handovers.
There was evidence that changes had been made as aresult of feedback. Managers and staff were able to tell usabout the action taken involving the transport service.
Home-care staff told us about an incident that hadoccurred in the patient’s home and how they had firstinformed the carer and then how they reported theincident to their line manager.
Are hospice services for adults effective?(for example, treatment is effective)
Requires improvement –––
We rated effective as requires improvement.
Evidence-based care and treatment
Many of the service policies required reviewing andupdating to bring them in line with best practice andnational guidance.
There was an ongoing review of all policies to bring themup to date and in line with best practice and nationalguidance. The policies had all been risk rated, prioritisedfor review and allocated to named individuals to lead theimprovement.
At handover meetings, staff routinely referred to thepsychological and emotional needs of patients, theirrelatives and carers.
Nutrition and hydration
Staff gave patients enough food and drink to meettheir needs and improve their health. They usedspecial feeding and hydration techniques whennecessary. The service made adjustments forpatients’ religious, cultural and other needs.
Staff made sure patients had enough to eat and drink,including those with specialist nutrition and hydrationneeds
Staff used a nationally recognised screening tool tomonitor patients at risk of malnutrition.
Specialist support from staff such as dietitians andspeech and language therapists were available forpatients who needed it.
The hospice held a current food hygiene certificate andscored five out of a possible five. Staff food hygienetraining certificates were on display in the kitchen. Stafftold us they were able to cater for a variety of religiousand cultural needs, and we saw a folder in the kitchenproviding detail on main world religions and the dietaryneeds and preferences of followers of those faiths.
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
18 Butterwick Hospice Quality Report 15/05/2020

Patients attending the day hospice were offered a rangeof hot and cold drinks, served by a volunteer.
The kitchen provided a full hot meal for patients. Kitchenstaff held a full list of each patient’s allergies, and copiesof any special dietary needs. Where this included pureedfood or liquid food, a copy of the relevant speech andlanguage assessment was held in the kitchen. Adaptivecups, mugs and cutlery was available and a list of peoplerequiring assistance to eat was held by staff. Nurses andhealthcare assistants’ competency to assist patients withfeeding was assessed by the hospice.
Feedback from a carers survey rated the quality ofcatering and access to food and drink at other times asexcellent.
Pain relief
Staff assessed and monitored patients regularly tosee if they were comfortable or in pain. They tookaction to make patients more comfortable and toassist them taking pain relieving medicines whenneeded.
Staff supported patients to self-administer pain reliefwhen they needed it and in one area of the hospice, staffadministered pain relief to patients when needed. Wherestaff administered pain relief, they recorded thisaccurately and evaluated the effect of the medicine given.
Home-care staff expressed a concern that they wereunable to administer pain relief in patients’ homes.Although they had a system in place to contact a familymember or a member of the district nursing team toattend the home to do this, they felt that this could resultin a delay and patients would have to wait for painrelieving medicine.
Service managers were aware home-care staff would liketo be able to administer pain relief in patients’ home andthey were undertaking a review of what training andpolicy adjustments would be needed to enable staff to dothis.
We observed a care worker supporting a patient in theirown home ask more than once if the patient was in anypain. The patient said they weren’t, but their bodylanguage and general demeanour made the care worker
think the patient was in some pain that they were notdisclosing. They made a note asking the district nurse toreview the patient and conduct a thorough painassessment.
Patient outcomes
Overall the service did not have a systematicapproach to audits which could be used to checkimprovement over time. Some data was collectedregarding patient outcomes, but we were unable tosee how these could be used to improve patients’outcomes. In some areas of the service, staffmonitored the effectiveness of care and treatmentand used the findings to make improvements andachieve good outcomes for patients.
Managers and staff did not carry out a comprehensiveprogramme of repeated audits to check improvementover time. However, there was a programme of a smallnumber of annual audits which included infection controlaudits and record keeping.
There was no evidence that managers used informationfrom the audits to improve care and treatment.
The service collected some outcome information forpatients. For example, The Phase of illness (POI) andAustralian Karnofsky Performance Status (AKPS) werescored on each patient on admission and two to threeweekly after. While this information was analysed by thehospice it was difficult to draw any conclusions from thisother than the patients participating were relativelystable, as the data showed little change.
The hospice team wanted to work on the training andimplementation of the Integrated Palliative care OutcomeScale (IPOS) which is a measure of global symptomburden as reported by patients. It was planned that thisinformation would be used to direct discussion within theclinical team, to ensure the current patient care plan is upto date and ensure the hospice approach is patientcentred. However, this work had not started.
The hospice collected information using the SupportTeam Assessment Schedule (STAS) on a weekly basis toassess clinical outcomes and intermediate outcomes ofpalliative care. STAS has nine core items coveringphysical, psychosocial, spiritual, communication,planning, family concerns and service aspects. Toevaluate the effectiveness of holistic intervention of
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
19 Butterwick Hospice Quality Report 15/05/2020

palliative patients accessing Day Hospice services. Thisinformation showed that although over time somepatients scores deteriorated, the majority remainedstable and all patients remained in the lower range withscores between 0-25. Scores in this range indicated thatpatients had minimal problems with a low likelihood ofadmission to hospital
The hospice had a number of key performance indicatorsthat it needed to achieve and report to commissioners ona quarterly basis. From October to December 2019 100%of patients in day-care / outpatients had a care plan inplace.
For the hospice at home service performance for: arecord was made as to whether patient has a care planwas 100%.
The family support team had 100% compliance withwritten assessment of needs and action plan agreed withpatient.
The physiotherapists and complementary therapists usedassessments to chart the outcomes for their patients andto change care plans where needed to improve individualpatient outcomes. However, they did not collate this datafor monitoring purposes or to track trends over time.
The family support team evaluated individual sessionsand the bereavement groups they provided. Evaluationforms were given to service users after each sessionwhich helped the counsellors evaluate the sessionresources used and how useful / enjoyable the childrenand young people found them. Individual evaluationforms could be used to inform the next session andresults were collated on an annual basis to ensureresources were acceptable to the children and youngpeople.
From September 2018 to April 2019, the service hadprovided six groups of six weeks duration to children andyoung people. The groups were accessed by 41 childrenand young people and attendance was 100%. Thechildren reported positive outcomes such as feelinghappier at school, arguing with the teacher less, enjoyedmaking new friends who had also lost someone, thingswere better at home and that its okay to be sadsometimes when you’ve lost someone you love.
There were family support services evaluations from Julyto September 2019 and October to December 2019. Theservice sent evaluations to all patients on discharge(adults and children.) Out of 36 evaluations sent 28 werereturned and all feedback was positive.
Positive outcomes reported by patients using the familysupport services included: “Always felt lighter afterwards”,“It really helped more than I could have hoped for”, “Mycounsellor was amazing, really helped me so much”,“Before I started counselling, I wasn’t sure about it anddidn’t think it would help. After a couple of weeks, Irealised it was helping and would encourage anyone togo.”
Anecdotal evidence and patient feedback indicated thatfollowing the group programmes given by the familysupport team, members of the group had continued tomeet and effectively made their own support systems inthe community.
Feedback from a carers survey indicated that relatives feltinvolvement with the hospice had a positive impact ontheir loved one’s quality of life and overall, they were verysatisfied with care.
Competent staff
The service made sure staff were competent for theirroles. Managers appraised staff’s work performanceand held supervision meetings with them to providesupport and development.
Staff were experienced, qualified and had the right skillsand knowledge to meet the needs of patients.
Staff told us the training and support they receivedenabled them to carry out their roles competently. Stafftold us they accessed much of their training online.
Managers gave all new staff an induction tailored to theirrole when they started work. Staff told us they were givena workbook to complete over a twelve-week period andthat these were signed off by a senior member of thenursing team when completed and assessed ascompetent.
Staff had the opportunity to discuss training needs withtheir line manager and were supported to develop their
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
20 Butterwick Hospice Quality Report 15/05/2020

skills and knowledge. Managers gave staff the time andopportunity to develop their skills and knowledge.Managers were providing bitesize training for staff tofacilitate access.
Managers made sure staff received any specific trainingfor their role. Nursing staff, including health careassistants received additional training regarding topicssuch as; mouthcare, catheter care, tracheostomy care,blood pressure, blood glucose and continence care.
There was a clinical educator who visited the hospice oneday a week to support the learning and developmentneeds of staff and to deliver training sessions. Staff told usthey had recently had a session regarding lone workersafety. Staff told us they could make requests for refreshertraining to address their learning needs.
Senior staff told us they assessed the competence ofsupport staff through observation and discussion.
Managers supported staff to develop through yearly,constructive appraisals of their work. Qualified nursesincluding the registered manager were supportedthrough revalidation. A six-month review had recentlybeen introduced in response to feedback from staff.
The hospice was continuing to develop competencies forstaff roles and had begun to ask staff to complete these.However, we saw in staff appraisals that they had askedfor refresher training in topics such as catheter care butthat these had not been provided yet.
Hospice data showed that compliance with annualappraisals was 65.5% against a target of 75%. This figurewas explained to some extent by new starters and leavershowever four of eight bank staff were overdue theirappraisal, two of these staff had been appraised, one wasa new starter and the other had a documented reason fortheir appraisal being overdue.
Managers had recently sought help from a partnerorganisation to develop a policy for clinical supervision.Four members of staff within Butterwick Ltd had beentrained to be facilitators for other members of staff. Thepolicy stated that staff would access clinical supervisionfour times a year.
Complementary therapy staff told us they weresupported to access regular, constructive clinicalsupervision of their work.
Members of the family support team were trained todegree level and demonstrated a high commitment toongoing training and development. This was necessary tomaintain a high level of expertise and to maintainregistration as a counsellor. The clinical lead for theservice had strong links with the local college which was asource of many of the volunteers. The service supportedstudents to achieve their client hours.
All counselling staff including volunteer counsellorsreceived clinical supervision once a month. The leadcounsellors accessed their counselling supervisionthrough an external provider, and they providedsupervision for the volunteers.
There were compulsory bi-monthly supervision meetingswith lone workers who provided the home-care service.
We checked four staff files and four volunteer files. Allcontained evidence of safe recruitment practicesincluding current disclosure and barring checks andevidence of nursing qualifications where appropriate. Noall contained copies of annual appraisals, although thesewere provided later by the hospice services manager.
Multidisciplinary working
All those responsible for delivering care workedtogether as a team to benefit patients. Theysupported each other to provide good care andcommunicated effectively with other agencies.
Staff worked across health care disciplines and with otheragencies when required to care for patients. Home-carestaff regularly liaised with specialist nurses, othercharities, community nursing teams, Marie Curie andsocial care teams. Community nurses sometimes visitedpatients at the hospice if they needed to makeassessments or provide treatment.
Nursing staff, family support and therapy staff workedtogether to provide the best experience possible forpatients and their families.
Staff referred patients for mental health assessmentswhen they showed signs of mental ill health ordepression.
We saw staff working well together as part of a team tomeet the individual needs of their patients.
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
21 Butterwick Hospice Quality Report 15/05/2020

There were many examples of multi-disciplinary workingand nursing staff could describe how they were able torefer directly to allied health professionals and medicalstaff within the hospice and within acute and primarycare settings.
Home-care staff talked about how they communicatedwith community nursing and other care providers toensure patients received the best care possible.
Staff working in day-care received a morning handoverevery day. This was accompanied by a sheet giving detailsof patients and any specific needs or things for staff toconsider when providing care.
The hospice held a multidisciplinary meeting to reviewneurological patients waiting to access services, howeverthis was only scheduled to meet once a quarter and overthe last year had only met twice due to diary constraints.
Seven-day services
Home-care services were available seven days aweek to support timely patient care.
Home-care services were offered seven days a week andthe managers had an on-call system to support staff ifneeded during out of hours periods.
Health promotion
Staff gave patients and families practical supportand advice to live well.
The service had relevant information promoting healthylifestyles and support.
Staff assessed each patient’s health when admitted andprovided support for any individual needs to live ahealthier lifestyle. This support was extended to family,loved ones and carers.
Consent and Mental Capacity Act
Staff supported patients to make informed decisionsabout their care and treatment. They knew how tosupport patients who lacked capacity to make theirown decisions or were experiencing mental illhealth. However, there was no formaldocumentation for staff to use to support them inmaking and documenting best interest decisions.
Staff gained consent from patients for their care andtreatment in line with legislation and guidance. Staffasked for and documented consent for photos andinformation sharing.
Staff were aware of patients who had documentedadvanced decisions including do not attemptcardio-pulmonary resuscitation (DNACPR). Copies ofDNACPR records were held at the front of patients notesand patients carried the original on their person.
Staff understood how and when to assess whether apatient had the capacity to make decisions about theircare. Although new patients accessing the service usuallyhad full mental capacity, staff recognised that patientscould use the service over a long time and mentalcapacity could fluctuate.
Patients were asked for verbal consent for therapeuticinterventions and this was usually documented at thestart of a course of treatment.
Staff told us that if patients could not give consent, theywould make decisions in their best interest, taking intoaccount wishes and known daily activities or practices.However, there was no documentation available tosupport staff to do this.
Relevant staff understood Gillick Competence and FraserGuidelines and supported children who wished to makedecisions about their treatment.
Staff received training in the Mental Capacity Act andDeprivation of Liberty Safeguards.
Are hospice services for adults caring?
Good –––
We rated caring as good.
Compassionate care
Staff treated patients with compassion andkindness, respected their privacy and dignity, andtook account of their individual needs.
Staff were discreet and responsive when caring forpatients. Staff took time to interact with patients and
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
22 Butterwick Hospice Quality Report 15/05/2020

those close to them in a respectful and considerate way.We observed staff all had good communication skills andhad a caring approach when interacting and engagingwith patients.
Patients said staff treated them well and with kindness.The hospice took part in the Friends and Family Test andcollated quarterly reports from the feedback. FromOctober to December 2019 the response rate was 85%and 100% of respondents were extremely likely torecommend the service.
The hospice collected feedback from carers following thedeath of their loved one to evaluate the care they weregiven. From a survey sent to six patients who hadreceived home-care from July to September 2019 fourwere returned. Feedback showed that staff alwaysintroduced themselves, they were knowledgeable abouttheir patients and treated them with respect and dignity.Relatives had confidence in the staff providing care totheir loved ones and relatives and patients had time toask questions. Staff made an effort to meet patients’individual needs and wishes, treated relatives withcourtesy and respected privacy.
Some examples of feedback from patients were; “Thankyou for all the time you have given me, the patience youhave shown me and above all the kindness.” “ButterwickHospice has helped me more than words can sayphysically, mentally, emotionally and they continue to doso”. “The treatment I have had is second to none and theyhave gone out of their way, this includes all staff andhelpers.”
Staff understood and respected the individual needs ofeach patient and showed understanding and anon-judgmental attitude when caring for or discussingpatients with mental health needs.
Staff understood and respected the personal, cultural,social and religious needs of patients and how they mayrelate to care needs
Staff felt they were cared for by their colleagues andmanagers and that this helped them to provide good careto patients and families.
Staff told us how developing close relationships withpatients and their families was important in deliveringcare. They felt rewarded that they were able to deliver agood standard of care and were able to honour patients’wishes at end of life.
We saw that staff were aware of and understood patients’interests and hobbies. They used this knowledge toinform conversations and social interactions that werewarm and caring.
We saw that staff had good rapport with patients andrelatives and listened, with genuine interest to how theyhad been over the period since their last contact. We sawthat relationships were well- developed and caring andthat patients were trusting of staff and able to disclosetheir concerns and fears.
We saw a volunteer treating patients with compassionand kindness, taking the time to have long conversationswith them and asking about their interests and theirfamilies. A volunteer told us that they felt a huge sense ofachievement being able to take the time to speak topeople and make them a drink, and that it could “makeall the difference” to someone that day.
We observed care delivered in a patient’s home. The careworker obtained verbal permission to re-position thepatient and checked what else they could do to helpthem several times. The care worker and patientdiscussed the patient’s interests, their shared taste inmusic and the patient’s forthcoming plans.
Emotional support
Staff provided emotional support to patients,families and carers to minimise their distress. Theyunderstood patients’ personal, cultural and religiousneeds.
Staff gave patients and those close to them help,emotional support and advice when they needed it
Staff undertook training on bereavement and loss anddemonstrated empathy when having difficultconversations
Staff understood the emotional and social impact that aperson’s care, treatment or condition had on theirwell-being and on those close to them
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
23 Butterwick Hospice Quality Report 15/05/2020

A patient receiving care in their own home told us theteam had been fantastic. They said they had felt wellsupported physically and emotionally by staff theydescribed as excellent.
A patient attending neurological day-care explained thatmany of the patients knew each other very well havingattended for several years, and that they were ‘like family’,as were the staff. Staff had a clear rapport with patientsand patients told us that it was good to see the same staffas they felt they didn’t have to repeat themselves.
One patient told us that the social aspect of day care wasalmost as important to them as all the other patients hadsimilar experiences and they all supported each other.They told us “it is important to me psychologically tocome here.”
Staff received emotional support from other staff andmanagers through supervision, debriefings and generalconversation and felt this enabled them to supportpatients better.
The family support team provided emotional supportthrough; one to one counselling for adults and children,social groups for adults and a bereavement group forchildren.
Feedback from patients for the family support team wasextremely positive and patients made comments such as“the counsellor was an amazing support, she was lovelyand made me feel secure and counselling has given methe tools to improve my emotional health”
Hospice staff offered complementary therapy to patientsand their families. This could be given in their own homesif necessary
Understanding and involvement of patients andthose close to them
Staff supported and involved patients, families andcarers to understand their condition and makedecisions about their care and treatment. Theyensured a family centred approach and offeredsupport services to families including children andyoung people.
Staff made sure patients and those close to themunderstood their care and treatment
Staff talked with patients, families and carers in a waythey could understand, using communication aids wherenecessary.
Patients and their families could give feedback on theservice and their treatment and staff supported them todo this.
Staff supported patients to make advanced decisionsabout their care
Staff supported patients to make informed decisionsabout their care
Patients gave positive feedback about the service.
Staff could give examples of how they used patientfeedback to improve daily practice.
We saw staff who were very sensitive to patients’communication needs. They interacted with patients whofound it difficult to communicate using appropriatelanguage and enabling them to respond with non-verbalcues.
We saw staff interacting with family members as partnersin care. They treated family members with respect andvisibly valued their opinion and instructions as they werethe people who knew the patient best.
We spoke to three patients attending neurologicalday-care. All confirmed that they had a goodunderstanding of their condition and were able to makeinformed decisions. They told us that the physiotherapythey received was vital to their well-being and thecomplementary therapies additionally helped to lift theirmood.
We observed a care worker supporting a patient in theirown home. The patient’s immediate relative was presentand all three had a detailed discussion about how thepatient had been feeling that day and any changes intheir condition or treatment. The relative told us they feltentirely involved in their loved one’s care.
Staff assessed the health needs of carers when a patiententered the service and signposted to other supportservices where necessary.
Are hospice services for adultsresponsive to people’s needs?
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
24 Butterwick Hospice Quality Report 15/05/2020

(for example, to feedback?)
Requires improvement –––
We rated responsive as requires improvement.
Service delivery to meet the needs of local people
The service planned and provided care in a way thatmet the needs of local people and the communitiesserved. It also worked with others in the widersystem and local organisations to plan care.
Managers planned and organised services, so they metthe needs of the local population
Facilities and premises were appropriate for the servicesbeing delivered
The service had systems to help care for patients in needof additional support or specialist intervention
The hospice had identified that there was a highincidence of neurological conditions and in particular;Multiple Sclerosis (MS) in the local population. As a result,the team worked with the NHS MS nurse specialist toprovide a more tailored service for these patients. Twoday-care places at each of the hospice’s locations werering-fenced for neurological patients and the hospiceprovided one neurological group session per week. Halfof the hospice’s patients had a non-cancer diagnosis.
The hospice was situated in an area that waspredominantly populated by people identifying as WhiteBritish. However, there were people from a range of othercommunities and ethnicities living in the hospicecatchment area. We asked two members of staffproviding clinical care, both confirmed they had nevercared for someone identifying as being from a black orethnic minority. One person told us they had worked forthe hospice for over ten years and nobody fitting thisdescription had used the hospice.
We asked leaders if they had done any work aroundhidden voices or barriers to using hospice services andwere told this was not something that had beenundertaken.
Meeting people’s individual needs
The service took account of patients’ individualneeds and preferences. Staff made reasonableadjustments to help patients access services. Theycoordinated care with other services and providers.
Staff made sure patients living with mental healthproblems, learning disabilities and dementia, receivedthe necessary care to meet all their needs.
The nurse from the hospice visited patients at home tomake an assessment of whether the hospice could meettheir needs before accepting them as a day patient. Thishome visit also ensured the patient had enoughinformation about the service to decide for themselves ifthe service could meet their needs and would be ofbenefit to them.
The hospice was designed to meet the needs of patients;although primarily a day care centre the hospice was ableto provide quiet rooms and a bed for patients whoneeded to rest during the day.
There were rooms available for the family support teamto work with children and young people. These had beenthoughtfully furnished with decoration, toys and activitiesfor children of varying ages. The rooms for children andyoung people were away from the adult day centre areaand staff told us children, young people and families wereescorted to these areas from the reception area.
Family support and counselling was tailored toindividuals and family needs and staff were flexible withthe hours they worked. Services were delivered incommunity or school settings, at the hospice or in thehome and could be delivered in the evenings toaccommodate the needs of others.
The team used tools developed specifically for children tomeasure emotional pain and also to evaluate the servicethey received.
Staff told us how they made adjustments to ensureprivacy for the patient was maintained when delivering asession at home. For example, they told us of occasionswhen they had delivered support at home and taken asupport worker with them to care for children and youngpeople, so they were able to work with a parent. On otheroccasions a support worker had been needed to care fora sick adult while the counsellor worked with anothermember of the family.
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
25 Butterwick Hospice Quality Report 15/05/2020

All staff had attended a ‘Dementia friends’ session during2019 to help them consider the needs of people sufferingwith dementia.
The service did not have information leaflets available inalternative languages however managers said they wouldsource these as and when needed. The hospice did nothave any current patients whose first language was notEnglish.
Managers told us that staff, patients, loved ones andcarers could get help from interpreters or signers whenneeded.
Although the hospice did not have any patients with awide range of protected characteristics, staff andmanagers described individualised care to all theirpatients and did not believe there were barriers topatients accessing their services. The hospice servicesmanager had recognised that the hospice needed toconsider ways in which it could improve its marketing toensure equal access to all groups.
Patients were given a choice of food and drink to meettheir cultural and religious preferences.
Staff told us that if a patient being cared for at homeexpressed a wish to die in a hospice setting, the homecare team would refer this to the district nursing team,who could arrange a transfer to one of three localhospices.
The service offered complementary therapies to patientsin their own home and in day care. This offer wasextended to wider family members and not just to thepatient. Family support services also provided services topeople in their own homes where needed.
The hospice had recently ceased provision of transport byhospice volunteers and this was now provided by anexternal company.
The hospice provided a chapel for prayer and quietreflection. Iconography was Christian andnon-removable. There were a number of other quietrooms and interview rooms that could be used by otherfaiths, however the hospice did not have any items suchas texts or prayer mats for use by patients or their familiesfor other religions.
The hospice’s service level agreement for the provision ofchaplaincy services was only for the provision of Christianchaplains, however leaders told us they did have contactdetails for other faith leaders if required.
Staff told us about celebration days they had held inresponse to national events or for patients’ interestexamples given were a St Patrick’s day celebration, Easterand Christmas celebrations and a ladies’ world cup day.
Staff told that one of the things they liked most aboutworking at the hospice was that they were able to providepatient led, person centred care. Activities were organisedaround patients’ interests and included things such asbingo, Thai chi, quizzes and themed days like beach days.
Access and flow
People could access most of the services when theyneeded it and received the right care in a timely way.Patients could access the specialist palliative careservice when they needed it. However, managers didnot monitor waiting times for neurological day careservices and patients could have extended waitsbefore being able to access this service.
Referral to the hospice services could be made by anyhealthcare professional and referral criteria were in place.For the home-care service patients had to be receivingcare from a community nursing team and the communitynursing service needed to be aware of the referral.
Referrals into the complementary therapy service couldbe made by any healthcare professional but treatmentwould not commence until the patient’s generalpractitioner had given their approval.
Referral criteria for the family support service were clearand staff had a seven-day standard for referral to firstcontact and courtesy calls were to be made if a client hadnot been seen by five weeks. The hospice did not providedata to show how many patients waited more than fiveweeks, actual length of waits or longest waits.
Referrals to the home care service were submitted onpaper by other health professionals. People were not ableto self-refer. These were then prioritised by the careco-ordinator based on urgency. District nurses spoke atleast weekly to the care co-ordinator about the needsand changes in the condition of those receiving theservice, and this was incorporated into visit planning.
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
26 Butterwick Hospice Quality Report 15/05/2020

There were a number of performance targets regardingaccess and flow that were reported to commissionersevery quarter; for the day care service from October toDecember 2019 100% of patients were contacted withinfive working days of referral; for the hospice at homeservice preferred place of care was achieved in 100% ofcases and the family support and bereavement servicecontacted patients within seven days of referral occurredfor 92% and 90% of patients in the last two quarters.
Day care place occupancy was also monitored for each ofthe day care centres. We could see that this fluctuatedand at Bishop Auckland this ranged between 80 and 93%from July to September 2019. For the same periodoccupancy was 73 to 100% at Weardale, 106 and 135% atthe Richardson and 84 to 95% at Sedgefield.
From July to September 2019 the palliative home careteam delivered 2,597 hours of respite care
From July to September 2019 the family support servicehad 67 referral and 185 people accessed the service.
From July to September 2019 the neurological day careservice delivered sessions to 153 people with 122accessing physiotherapy and 117 accessingaromatherapy.
Hospice managers could not tell us how many patientswere waiting to access the neurological day service orhow long they had waited. Managers did not monitorwaiting times for neurological day-care services and onepatient told us they had waited ‘a couple of years toaccess the service’. Managers told us the neurological dayservice provided by the hospice at its Bishop Aucklandsite was heavily oversubscribed.
There was no clear rationale regarding some patientsaccessing a rolling programme while other patients hadlong waits. It was unclear what the rationale was for thelength of time between patients being on and off theprogramme. The hospice managers told us patientssometimes waited longer than usual in-between therapy,to enable new patients to access the service. However,this had not been systematically reviewed or monitoredto establish consistent waiting times, either for thepatients on the programme or those waiting to access it.
The hospice had set up a multi-disciplinary team meetingto review waiting patients to see if they needed to accessservices earlier, however this was led by the MS nurse and
only met every six months. Other neurological specialistsdid not receive an invite, leading to the possibility thatpeople with a non-MS diagnosis could potentially wait formuch longer before they could access the service.
Staff supported patients when they were referred ortransferred between services. Staff were able to giveexamples of how they had supported patients and orfamily members when they had suffered a medical ormental health crisis.
A care co-ordinator organised all home visits. Visits for theweekend were scheduled on Friday, so it was not possibleto organise a weekend visit at short notice. However, asthe care co-ordinator held an emergency phone, theywere able to re-prioritise staff at weekends if a patienthad passed away.
The home care service had identified the team couldprovide 8000 hours of patient care per year and theymonitored performance against this. The team told usthat if they were unable to fulfil a visit, they would askcolleagues at another home care organisation if theywould be able to pick this up.
The hospice had recently taken the decision to stopproviding a transport service for its patients. This hadbeen communicated directly with each patient using theservice and alternative methods of transport had beendiscussed. The hospice had worked with a charity toprovide some transport and had signposted patients toother patient transport services such as those providedthrough GP surgeries or other voluntary agencies. Staffhad identified that patients would benefit from a leafletto give clear information on how to access transport, butthey had not done this yet.
The family support team provided services to childrenand young people and their families, staff told theyprovided interventions for children as young as six years.For younger children the service provided guidance,information and signposting to parents to help themaccess more appropriate services.
The services accepted referrals from members of thehospice team, other healthcare professionals, teachersand they would also accept self-referral. Family supportservices were provided at the hospice, in schools andcommunity groups and in the home.
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
27 Butterwick Hospice Quality Report 15/05/2020

The team also provided teaching sessions to otherprofessionals. For example, they had run a sessionregarding loss and grief with a group of teachers to helpthem understand and support children in school, whohad been bereaved.
From 1 April 2018 to 31 January 2019 the family supportservice had seen 261 individuals, 105 of these werechildren. They had provided 1,369 counselling sessions(984 for adults and 385 for children and young people).They had held 250 adult support groups and 123 groupsfor children and young people)
The family support team used a needs-based waiting listfor their services and the clinical lead told us the waitinglist for counselling was 14-16 weeks.
Learning from complaints and concerns
It was easy for people to give feedback and raiseconcerns about care received. The service treatedconcerns and complaints seriously, investigatedthem and shared lessons learned with all staff.
Patients, relatives and carers knew how to complain orraise concerns
The service clearly displayed information about how toraise a concern in patient areas.
Managers investigated complaints and identified themes
Staff knew how to acknowledge complaints and patientsreceived feedback from managers after the investigationinto their complaint.
The hospice had not received any complaints in theprevious twelve months. We checked the last twocomplaints which dated back to 2017. One was partiallyupheld and related to concerns by a patient about notfeeling welcome at a group they attended, and thesecond was a complaint about staff behaviour. Neithercomplaint file was complete, with copies of alldocuments missing in the first instance, and a copy of thefinal letter missing from the second. Although the secondcomplaint was a personnel matter that would have beendealt with confidentially there was no evidence in the fileto say how or if this was addressed
Managers shared feedback from complaints with staffand learning was used to improve the service
Are hospice services for adults well-led?
Requires improvement –––
We rated well-led as requires improvement.
Leadership
Leaders did not fully understand and manage thepriorities and issues the service faced. A lack of aleadership structure at local level with unclearresponsibilities and links into the clinical services ofthe other locations had led to issues such asdisjointed policies, a lack of a robust auditprogramme and ineffective management of waitinglists. However, managers were visible andapproachable in the service for patients and staff.They supported staff to develop their clinical skills.
The Butterwick hospice was led by a director of patientcare who was also responsible for two other hospicelocations. A hospice services manager led the team at thissite. The individual services were led by a home-carecoordinator, two lead nurses and the family support leadpractitioner.
The hospice services manager told us they had been ableto access training to help them with their role and theyhad been supported in developing their role.
Responsibilities of the lead nurses were not always clear,and they were sometimes unsure as to whether theyshould / could make changes in their area. They werealso not clear about their role in supporting appraisalsand supervision for the staff who reported to them daily.
This lack of clarity had contributed to the differences inpractice between sites and services. For example, we sawdifferences in documentation and differences inadministration and transcribing of medicines.
The service leads did not receive managementsupervision and there was not a forum for lead nurses /practitioners to get together to discuss clinical issues.This was likely to have contributed to multiple policiesand procedures fitting the needs of one clinical servicebut not those of another.
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
28 Butterwick Hospice Quality Report 15/05/2020

Local managers liked to be visible to staff and patientsand staff described their leaders and line managers assupportive and caring. They gave examples of whenmanagers had supported them with the death of apatient and with balancing caring commitments at home.
Local leaders were proud to work at the hospice and wereproud of their staff and volunteers and their commitmentto providing high quality patient care.
Staff told us they were very happy with their local leaders,and the visibility / approachability of the director ofpatient care. However, they commented that they rarelysaw the chief executive or board members at the BishopAuckland site. One member of staff told us they would behappier if executive leads spent more time meetingpatients and speaking to staff, so they had a goodunderstanding of the services they led.
Volunteer staff told us they felt isolated from seniorleaders of the organisation and staff at the Stockton sitewhich they felt was due to the complementary therapymanager post becoming vacant.
Vision and strategy
The hospice had a strategic five-year plan for2019-2024 which outlined its priorities and theenabling actions required.
The hospice had a mission statement “to improve thequality of life for those who have a life limiting illness, andtheir families, and to offer positive support for everychallenge they may encounter during their illness. To seedeath as part of life’s journey.”
The hospice team wished to provide compassionate,dignified care and support where it was needed the most.The strategy expressed the values of care, compassion,dignity, support and community.
Priorities were defined as having the right workforce; theright environment for patients; volunteers and staff, toensure openness and transparency; to have the resourcesand capacity to meet demand with the central aim ofproviding the best quality of care and quality of life forpatients.
Each strategic priority was underpinned by enablingactions.
Culture
Staff felt respected, supported and valued. Theywere focused on the needs of patients receivingcare. The service provided opportunities for careerdevelopment and had an open culture wherepatients, their families and staff could raiseconcerns without fear.
Staff described the culture as open and told us theywould have no fear about raising concerns. Staff hadconfidence in their managers and leaders said they wouldbe able to approach them if they had anything theywanted to discuss. There was a clear sense of teamworkacross day hospice staff and everyone spoke very highlyof their colleagues.
Staff told us of concerns and ideas for improvements theyhad raised with managers. Senior nursing staff felt theywere able to make changes and develop practice in theirown area of responsibility. However, this had led to someinconsistencies in practice.
Examples of concerns staff had raised included policiesand processes regarding administration of medicines andthe quality of risk assessments. These concerns had beenreviewed and managers had agreed that improvementsneeded to be made. Work was ongoing to make thechanges needed.
Managers needed to ensure they consulted with clinicalstaff in all areas regarding any updates to clinical policiesand procedures to ensure the needs of all services wereincorporated.
Governance
Leaders did not have effective governanceprocesses, throughout the service. Not all staff at alllevels were clear about their roles andaccountabilities. Clinical leads did not have regularopportunities to meet, discuss issues, proposeimprovements and learn from the performance ofthe service.
There was a defined governance and committeestructure in place for senior managers within theorganisation. However, clinical leads did not receivemanagement supervision or have a forum where theycould meet to discuss clinical or practical service issues,
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
29 Butterwick Hospice Quality Report 15/05/2020

propose improvements and learn from performance ofthe service. This had led to teams adopting differentpractices in different settings and policies or procedureswhich met the needs of one service but not another.
There was a regular manager meeting, but this was notalways attended by a representative from day care oroutreach services and reports or updates from thoseservices were not always included in the minutes fromthe meetings.
There had not been any local staff meetings at thehospice for several months until they were reinstated on 5March 2020. The minutes indicated there was goodengagement with staff and there had been theopportunity for staff to raise concerns or propose ideas inrelation to cost savings or efficiencies. It did not appearthat the outreach services had been represented at themeeting.
There were gaps in systems and processes to supportmanagers and leaders in maintaining effectivegovernance and oversight. For example, the local hospicemanager could not directly access; Disclosure and barringservice (DBS) checks, registration or training information.However, Butterwick Ltd was working with partnerorganisations to help them modernise and implementnew systems to address this.
There was no monitoring or oversight of patient waitinglists and there was no consistent assessment of any riskto patients who waited for long periods to accessneurological day services or family support.
Although the service had recently introduced a system forensuring all their employed staff had up to dateregistration, DBS, mandatory training and appraisals, thiswas not in place for staff not directly employed, such asphysiotherapists who were employed by an NHS trust.
Clinical leads were not all clear about their roles andresponsibilities.
Managers told us the new governance structure had beenimplemented during 2019 but this was not fullyembedded. It had been intended that there would becertain agenda items discussed at all meetings to ensurea flow of information from service to board. However, wenoted that incidents and complaints were not on theagenda for staff or manager meetings, but activity,staffing, policies and contract updates were.
The hospice produced a ‘Quality Account’ each year’ withpriorities and objectives but there did not appear to bean action plan or recorded meeting minutes thatindicated whether the priority objectives had been met.
Although there was a system in place for reviewing andprioritising the re-writing of out of date policies, this wasnew and there was still a lot of work to do with bringingall policies and procedures up to date. Managers neededto ensure clinical staff were consulted with updatedpolicies to make sure they met needs of all clinical areas.
Managing risks, issues, performance and managinginformation
Leaders and teams did not have robust systems tomanage all risks and performance effectively. Theyidentified risks and issues but did not alwaysdocument identified actions to reduce their impact.Risks were not always escalated to a risk register foroversight and monitoring of actions.
Although the hospice used agreed targets to monitorperformance it did not produce comparative data overtime. This meant the management team could notmonitor its own performance over time, usingappropriate control limits.
There were gaps in performance data, for examplewaiting times to access neurological day services was notmonitored. This meant some patients could wait monthsor years to access the service while others accessed a rollon roll off service. The gaps in information meant therewas limited data and a lack of knowledge which couldhave been used to improve access to the service.
Clinical leads were not clear about their role in managingrisks, issues and performance which meant some riskswere not identified or escalated appropriately.
Not all risks we identified or known to staff were recordedon the organisation’s risk register. For example, the issueswith handwash basins and other recommendations frominfection control audits were not on the risk registerdespite being recommended at the annual audit for thelast three years. This meant there was no monitoring ofmitigations or any chance of the issues being escalatedfor action /allocation of funding to correct.
There was also some confusion in clinical areas regardingrisk assessments. Although there was a process of
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
30 Butterwick Hospice Quality Report 15/05/2020

assessing risks locally, the risks we saw documented,were in the main, clinical risks. Mitigations were aroundgeneral management of those risks, for example patientswith a tracheostomy, or exposure to bodily fluids.
Environmental / equipment risk assessments such asstorage of oxygen or child safety were not documented.For example, although oxygen was stored safely andsecurely it was not evident that a formal risk assessmenthad been completed around this. Therefore, we could notbe assured that staff were aware of the risks associatedwith the storage and use of oxygen.
Managers were clear about their biggest risks andidentified these as funding, staffing and meetingstandards.
Staff received training regarding confidentiality,information governance and data protection. Theregistered manager was the Caldicott lead for thehospice. A Caldicott lead is a senior person responsiblefor protecting the confidentiality of people's health andcare information and making sure it is used properly.
The hospice services manager identified a need for theservices to be able to develop or access IT systems forpatient records and for performance information. Thehospice was looking for ways in which electronic systemscould be developed.
Engagement
Leaders and staff actively and openly engaged withpatients, staff, the public and local organisations toplan and manage services. They collaborated withpartner organisations to help improve services forpatients.
Staff were clearly engaged with the organisation andwhat it stood for, they told us that managers weresupportive, and communication was good. Staff andmanagers told us about weekly team briefs, serviceupdates, staff supervision and a monthly informationexchange. The chief executive or another senior managerpersonally delivered the information exchange at thedifferent hospice sites.
Staff were given opportunities to propose; ideas for costefficiencies, fundraising ideas and to make othersuggestions. Suggestion boxes were available for staff touse.
However, there was no formal staff survey in place or anyformal staff recognition or awards. Other than longservice, where a volunteer had been in post for ten yearsand received an addition to their name badge, there wereno staff or volunteer annual awards or thank you cardsystem.
Managers told us that they were making a concertedeffort to improve staff recognition and had introducedrecognising and naming staff noted for examples of goodpractice at the regular information exchange.
Managers and staff welcomed feedback from serviceusers and their families. The hospice services managermade themselves available to patients to hear theirfeedback on the services they received.
The service collected patient, relative and other serviceuser feedback through surveys, formal and informalevaluations of services and by collating correspondenceand thankyou cards.
The hospice had identified from a local joint needsassessment that there was a high incidence ofneurological conditions and in particular; MS in the localpopulation. As a result, the hospice team had workedwith commissioners, the MS society and the NHS MSnurse specialist to provide and tailor a service for thesepatients.
Learning, continuous improvement and innovation
All staff were committed to continually learning andimproving services.
Managers and staff were open to service improvementand wanted to develop their services to provide the bestpossible care.
Hospiceservicesforadults
Hospice services for adults
Requires improvement –––
31 Butterwick Hospice Quality Report 15/05/2020

Outstanding practice
The family support team had worked extremely hard toprovide an accessible service for families with children,who had suffered a bereavement. Staff were extremelyresponsive and tailored their approach to meet the
individual needs of children, young people and theirfamilies to ensure they could access the service. Theycould access the service at home, at the hospice, inschools and community groups.
Areas for improvement
Action the provider MUST take to improve
• The provider must ensure that risks to patients areidentified, assessed and monitored consistentlythroughout the hospice, and that assessments andcare plans are updated regularly. Patient records mustbe kept up to date. Regulation 12 and 17.
• The provider must ensure that health and safety risksto staff and patients are identified, assessed anddocumented consistently throughout the hospice, andthat they are escalated appropriately so they can bereviewed, and appropriate mitigating actions can betaken. Regulation 12.
• The provider must ensure there are policies, systemsand processes in place to ensure the safe andconsistent management of medicines across allhospice settings. To include; transcribing,administration, recording and storage medicines.Regulation 12.
• The provider must take prompt action to ensure staffand managers are clear about their responsibilitiesunder ‘duty of candour’ to ensure they meet regulationstandards and ensure regulatory requirements arereflected in policies and processes. Regulation 20.
• The provider must continue its work to bring policiesand procedures in line with current guidance and bestpractice. To include a review of documentation tosupport staff making and documenting best interestdecisions. Regulation 17.
• The provider must monitor waiting times for allaspects of its services to inform potential serviceimprovements. Regulation 17.
Action the provider SHOULD take to improve
• The provider should consider how it could promote itsservices to minority groups to ensure its services areaccessible to diverse groups. Regulation 10.
• The provider should review how it collects patientoutcome data how this information can be used toimprove services and patient care.
• The provider should review its audit programme toensure it can demonstrate achievement of safestandards and how it can use this information to makeimprovements over time.
• The provider should explore how staff in thehome-care setting can be supported to assist patientswho need help with administration of pain-relievingmedicine.
• The provider should ensure staff at all levels are clearabout their roles and responsibilities to support arobust governance, performance and improvementframework and that they are given the opportunity tomeet, discuss issues, propose improvements and learnfrom the performance of the service.
Outstandingpracticeandareasforimprovement
Outstanding practice and areasfor improvement
32 Butterwick Hospice Quality Report 15/05/2020

Action we have told the provider to takeThe table below shows the legal requirements that were not being met. The provider must send CQC a report that sayswhat action they are going to take to meet these requirements.
Regulated activity
Treatment of disease, disorder or injury Regulation 12 HSCA (RA) Regulations 2014 Safe care andtreatment
The hospice did not always assess the risks to the healthand safety of service users and did not always mitigateidentified risks.
Risks to patients were not identified, assessed andmonitored consistently throughout the hospice.Assessments and care plans were not updated regularly,and patient records were not always up to date
The hospice did not always ensure the premises weresafe to use for their intended purpose. Not all health andsafety risks to staff and patients were identified,assessed and documented consistently throughout thehospice. This meant they were not always escalated,reviewed and mitigated appropriately.
The hospice did not ensure the proper and safemanagement of medicines. The provider did not haverobust policies, systems and processes in place to ensurethe safe and consistent management of medicinesacross all hospice settings.
Regulated activity
Treatment of disease, disorder or injury Regulation 17 HSCA (RA) Regulations 2014 Goodgovernance
The hospice did not have effective systems or processesto assess, monitor and improve the quality and safety ofthe services provided.
Many of the hospice policies and procedures were out ofdate or unfit for purpose.
Regulation
Regulation
This section is primarily information for the provider
Requirement noticesRequirementnotices
33 Butterwick Hospice Quality Report 15/05/2020

The hospice did not monitor the length of time patientswaited for services or consider the impact this may haveon service users.
The hospice did not have effective systems or processesto assess, monitor and mitigate the risks relating to thehealth, safety and welfare of service users and otherswho may be at risk. This meant risks were not alwaysidentified and documented so they could be reviewed,and mitigations put in place.
The hospice did not maintain securely an accurate,complete and contemporaneous record in respect ofeach service user.
Patient records were not always complete or hold up todate information.
Regulated activity
Treatment of disease, disorder or injury Regulation 20 HSCA (RA) Regulations 2014 Duty of candour
Staff and managers were not clear about theirresponsibilities under ‘duty of candour’ to ensure theymeet regulation standards. Regulatory requirementswere not reflected. in hospice policies and processes.
Regulation
This section is primarily information for the provider
Requirement noticesRequirementnotices
34 Butterwick Hospice Quality Report 15/05/2020

Action we have told the provider to takeThe table below shows the legal requirements that were not being met. The provider must send CQC a report that sayswhat action they are going to take to meet these requirements.
This section is primarily information for the provider
Enforcement actionsEnforcementactions
35 Butterwick Hospice Quality Report 15/05/2020