Briefings on APCs - Revenue Cycle Advisor · Volume 18 Issue No. 1 JANUARY 2017 Briefings on APCs...
Transcript of Briefings on APCs - Revenue Cycle Advisor · Volume 18 Issue No. 1 JANUARY 2017 Briefings on APCs...

JANUARY 2017Volume 18 Issue No. 1
Briefings on APCs
New CPT codes introduced for dialysis circuit codingby Stacie L. Buck, RHIA, CCS-P, CIRCC, RCC
The coding manager’s role during the audit process
Rose T. Dunn, MBA, RHIA, CPA, FACHE, FHFMA, CHPS, writes about what coding manager should focus on during audits.
This month’s coding Q&A
Our experts answer questions about OPPS packaging, new 2017 CPT codes, modifiers -PN and -PO, and more.
2016 Briefings on APCs index
See what stories and topics Briefings on APCs covered in 2016.
P5
P8
P11
One area of CPT coding that saw big changes for 2017 is for dialysis circuit coding. The existing codes have all been deleted, and new codes have been created (36901-36909) for reporting these procedures.
Dialysis access maintenance codes are “inclusive” codes built on a progressive hierarchy with less intensive services bundled with the most intensive services performed in the arteriovenous fistula/arteriovenous graft (AVF/AVG). Only one primary code may be reported per session and add-on codes are also only reported one time per session.
The following components are included in codes 36901-36909:
• Accessing the AVF/AVG
• Placement of the catheter
• Vena cava
• Venous side branches (accessory)
• Through to arterial anastomosis (to evaluate peri-anastomosis or anastomosis)
• Contrast injections
• Fluoroscopy
• Radiological supervision and interpretation
• Closure of arteriotomy
Key terms
To ensure correct application of the new codes, it is imperative to have a clear understanding of some key terms:
Dialysis circuit: The dialysis circuit begins at the arterial anastomosis and extends to the right atrium. It is comprised of two segments (zones): the peripheral dialysis segment and the central dialysis segment.
INSIDE THIS ISSUE

HCPRO.COM © 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
2 |Briefings on APCs January 2017
Briefings on APCs (ISSN: 1530-6607 [print]; 1937-7428 [online]) is published monthly by HCPro, a division of BLR®. Subscription is an exclusive benefit for Basic members of HCPro’s Revenue Cycle Advisor. Basic membership rate: $595/year. • Briefings on APCs, 100 Winners Circle, Suite 300, Brentwood, TN 37027. • Copyright © 2017 HCPro, a division of BLR®. All rights reserved. Printed in the USA. Except where specifically encouraged, no part of this publication may be reproduced, in any form or by any means, without prior written consent of HCPro, a division of BLR, or the Copyright Clearance Center at 978-750-8400. Please notify us immediately if you have received an unauthorized copy. • For editorial comments or questions, call 781-639-1872 or fax 781-639-7857. For renewal or subscription information, call customer service at 800-650-6787, fax 800-785-9212, or email [email protected]. • Visit our website at www.hcpro.com. • Occasionally, we make our subscriber list available to selected companies/vendors. If you do not wish to be included on this mailing list, please write to the marketing department at the address above. • Opinions ex pressed are not necessarily those of BAPCS. Mention of products and services does not constitute endorsement. Advice given is general, and readers should consult professional counsel for specific legal, ethical, or clinical questions. Current Procedural Terminology (CPT) is copyright 2011 American Medical Association. All rights reserved. CPT is a registered trademark of American Medical Association; no fee schedules, basic units, relative values, or related listings are included in CPT. The AMA assumes no liability for the data contained herein. Applicable FARS/DFARS restrictions apply to government use.
EDITORIAL ADVISORY BOARD
Steven [email protected]
Kimberly Anderwood Hoy Baker, JD, CPCDirector of Medicare and ComplianceHCPro Danvers, Massachusetts
Dave Fee, MBAProduct Marketing Manager, Outpatient Products3M Health Information Systems Murray, Utah
Frank J. Freeze, LPN, CCS, CPC-HPrincipalThe Wellington Group Valley View, Ohio
Susan E. Garrison, CHCA, CHCAS, PCS, FCS, CPC, CPC-H, CCS-P, CHC, CPARExecutive Vice President of Healthcare Consulting ServicesMed Law Advisors, Inc. Atlanta, Georgia
Diane R. Jepsky, RN, MHA, LNCCEO & PresidentJepsky Healthcare Associates Sammamish, Washington
Lolita M. Jones, RHIA, CCSLolita M. Jones Consulting Services Fort Washington, Maryland
Jugna Shah, MPHPresidentNimitt Consulting Washington, D.C.
This document contains privileged, copyrighted information. If you have not purchased it or are not otherwise entitled to it by agreement with HCPro, a division of BLR, any use, disclosure, forwarding, copying, or other communication of the contents is prohibited without permission.
catheter placement(s), injection(s) of contrast, all necessary imaging from the arterial anastomosis and adjacent artery through the entire venous outflow including the inferior or superior vena cava, fluoro-scopic guidance, radiological supervision and interpre-tation and image documentation and report.
Code 36901 describes a direct puncture of the dialysis circuit, followed by imaging of the entire graft/fistula from the arterial anastomosis and adjacent artery through entire venous outflow including the inferior or superior vena cava. All catheterizations are bundled, including those of the vena cava, venous side (acces-sory) branches, and the arterial anastomosis to evalu-ate the peri-anastomosis or anastomosis.
During some procedures, both antegrade and retro-grade punctures may be used for imaging. Code 36901 should not be used for a second puncture or any additional punctures directly into the dialysis circuit. This code includes all punctures made into the dialysis circuit and is assigned only one time per encounter. Repeat fistulagrams are not coded.
Should the catheter be advanced further to visualize the arterial anastomosis or the central veins, the catheter work is included with code 36901. However, the arterial inflow to the dialysis circuit is considered a
Peripheral dialysis segment: The peripheral segment begins at the arterial anastomosis and extends to the central dialysis segment, including the peri-anasto-motic region. This is the region of the dialysis circuit near the arterial anastomosis, including a short seg-ment of the parent artery, the anastomosis, and a short segment of the dialysis circuit immediately adjacent to the anastomosis. In the upper extremity, it extends through the axillary vein, and in the lower extremity, it extends through the common femoral vein.
Central dialysis segment: The central dialysis segment includes all draining veins central to the peripheral dialysis segment. In the upper extremity it includes veins central to the axillary and cephalic veins, includ-ing the subclavian and innominate veins through the superior vena cava. In the lower extremity it includes central veins to the common femoral vein, including the external and common iliac veins through the inferior vena cava.
Fistulagrams
Let’s first take a look at the definition of new code 36901: introduction of needle(s) and/or catheter(s), dialysis circuit, with diagnostic angiography of the dialysis circuit, including all direct puncture(s) and
Follow Us! Follow and chat with us about all things healthcare compliance, management, and reimbursement. @HCPro_Inc
QUESTIONS? COMMENTS? IDEAS?Contact Editor Steven Andrews at [email protected] or 781-639-1872, Ext. 3171.

HCPRO.COM© 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
Briefings on APCs | 3January 2017
separate vessel. If a more proximal inflow problem separate from the peripheral dialysis segment is suspected, additional catheter placement and imaging required for adequate evaluation of the artery may be separately reported. In this instance, when the catheter is selectively advanced from the dialysis circuit beyond the peri-anastomotic segment into the inflow artery, an additional catheter code may be reported, typically code 36215. This includes placement of the catheter retrograde into the inflow artery and into the aorta if necessary. Code 75710 may be reported be reported when a separate diagnostic evaluation is performed of the inflow artery.
When a fistulagram is performed through an existing access or when the catheter is maneuvered into the graft/fistula from an access that is not a direct punc-ture of the dialysis circuit, code 36901 is reported with modifier -52 (reduced services) appended.
Angioplasty
New codes for angioplasty include:
• 36902, introduction of needle(s) and/or catheter(s), dialysis circuit, with diagnostic an-giography of the dialysis circuit, including all direct puncture(s) and catheter placement(s), injection(s) of contrast, all necessary imaging from the arterial anastomosis and adjacent artery through the entire venous outflow including the inferior or superior vena cava, fluoroscopic guid-ance, radiological supervision and interpretation and image documentation and report; with trans-luminal balloon angioplasty, peripheral dialysis segment, including all imaging and radiological supervision and interpretation necessary to per-form the angioplasty
• Add-on code 36907, transluminal balloon an-gioplasty, central dialysis segment, performed through dialysis circuit, including all imaging and radiological supervision and interpretation re-quired to perform the angioplasty (List separate-ly in addition to code for primary procedure)
When coding therapeutic interventions in the dialysis circuit, recall this area is divided into two vessel
segments–the peripheral dialysis segment and the central dialysis segment. Only one code may be reported for each segment. The correct code is deter-mined by the most extensive procedure performed.
Code 36902 is assigned for angioplasty of the periph-eral dialysis segment and may only be reported one time for all angioplasty performed within this segment. When angioplasty of the central segment is performed, add-on code 36907 is assigned for angioplasty of the central veins (subclavian/ innominate/cava) and may only be reported one time for all angioplasty per-formed within that segment.
Note that all imaging, including a diagnostic fistulagram is bundled into the dialysis circuit angioplasty codes and 36901 should not be reported separately. Only one code from range 36901-36906 is allowed per session.
Stent
The new codes for stents are:
• 36903, introduction of needle(s) and/or catheter(s), dialysis circuit, with diagnostic an-giography of the dialysis circuit, including all direct puncture(s) and catheter placement(s), injection(s) of contrast, all necessary imaging from the arterial anastomosis and adjacent artery through the entire venous outflow including the inferior or superior vena cava, fluoroscopic guid-ance, radiological supervision and interpretation and image documentation and report; with trans-catheter placement of intravascular stent(s), pe-ripheral dialysis segment, including all imaging and radiological supervision and interpretation necessary to perform the stenting, and all angio-plasty within the peripheral dialysis segment
• Add-on code 36908, transcatheter placement of intravascular stent(s), central dialysis segment, performed through dialysis access circuit, includ-ing all imaging radiological supervision and inter-pretation required to perform the stenting, and all angioplasty in central dialysis segment (List sepa-rately in addition to code for primary procedure)
Code 36903 is assigned for stent placement in the peripheral dialysis segment and may only be reported

HCPRO.COM © 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
4 |Briefings on APCs January 2017
one time for all stents placed within this segment. When a stent is placed in the central segment, add-on code 36908 is assigned for stent placement in the central veins (subclavian/innominate/cava) and may only be reported one time for all stents placed within that segment. Note that angioplasty is bundled with each of these codes when performed in the same segment as stent placement.
As with percutaneous transluminal angioplasty, all imaging, including a diagnostic fistulagram, is likewise bundled into the dialysis circuit stent codes and 36901 should not be reported separately. Remember, only one code from range 36901-36906 is allowed per session.
Thrombectomy/Thrombolysis
We have three new codes for reporting thrombectomy/thrombolysis in this section:
• 36904, percutaneous transluminal mechanical thrombectomy and/or infusion for thrombolysis, dialysis circuit, any method, including all imaging and radiological supervision and interpretation, diagnostic angiography, fluoroscopic guidance, catheter placement(s), and intraprocedural phar-macological thrombolytic injection(s);
• 36905, percutaneous transluminal mechanical thrombectomy and/or infusion for thrombolysis, dialysis circuit, any method, including all imaging and radiological supervision and interpretation, diagnostic angiography, fluoroscopic guidance, catheter placement(s), and intraprocedural phar-macological thrombolytic injection(s); with trans-luminal balloon angioplasty, peripheral dialysis segment, including all imaging and radiological supervision and interpretation necessary to per-form the angioplasty
• 36906, percutaneous transluminal mechanical thrombectomy and/or infusion for thrombolysis, dialysis circuit, any method, including all imaging and radiological supervision and interpretation, diagnostic angiography, fluoroscopic guidance, catheter placement(s), and intraprocedural phar-macological thrombolytic injection(s); with trans-catheter placement of intravascular stent(s), peripheral dialysis segment, including all imaging
and radiological supervision and interpretation necessary to perform the stenting, and all angio-plasty within the dialysis circuit
Code 36904 describes thrombectomy/thrombolysis of the peripheral dialysis segment. It includes all work necessary to remove the thrombus, both mechanical and pharmacological. Use of a balloon to remove a thrombus (removal or the arterial plug) is considered part of the thrombectomy and should not be coded separately.
A separate stenosis treated with balloon angioplasty must be documented to report code 36905, which describes thrombectomy/thrombolysis of the AV graft/fistula with angioplasty of the peripheral dialysis segment instead of code 36904 when angioplasty is performed with thrombectomy.
Code 36906 is reported when thrombectomy/throm-bolysis of the AV graft/fistula occurs with angioplasty and stent placement in the peripheral dialysis segment at the same time.
Again, note that all imaging, including a diagnostic fistulagram, is bundled into the dialysis circuit throm-bectomy/thrombolysis codes and 36901 should not be reported separately and only one code from range 36901-36906 is allowed per session.
Embolization
Finally, let’s look at the add-on embolization code:
• Add-on code 36909, dialysis circuit permanent vascular embolization or occlusion (including main circuit or any accessory veins), endovascu-lar, including all imaging and radiological super-vision and interpretation necessary to complete the intervention (List separately in addition to code for primary procedure)
Add-on code 36909 describes embolization of the dialysis circuit and its collateral veins. Selective cath-eterization of any collateral veins is bundled and not reported separately. Code 36909 is reported only once per day for the entire dialysis circuit (peripheral and central segments) regardless of the number of branches and/or vessels embolized.

HCPRO.COM© 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
Briefings on APCs | 5January 2017
Conscious sedation (99151-99157)
Moderate conscious sedation is now reported sepa-rately for dialysis circuit interventions. Historically, the CPT Manual noted codes that include moderate conscious sedation using a bullseye symbol next to the codes and had provided a summary of CPT codes that included moderate conscious sedation in Appendix G of the manual. The bullseye is no longer utilized and the appendix has been removed. H
EDITOR’S NOTE:
Buck is president and senior consultant for RadRx of Stuart, Florida,
and provides coding, auditing, and education services for providers of
diagnostic and interventional radiology services on a nationwide ba-
sis. This article is adapted from Buck’s Cracking the IR Code: Your
Comprehensive Guide for Mastering Interventional Radiology 2017
Edition. For additional information, go to www.radrx.com. Opinions ex-
pressed are that of the author and do not represent HCPro or ACDIS.
The coding manager’s role during the audit processManagers should not assume that they can review every guideline, every item in Coding Clinic, or every coding-related issue targeted by the Office of Inspector General (OIG) or Recovery Audit Contractor (RAC).
A coding manager’s responsibilities include:
• Planning the coding audit process
• Organizing the resources necessary to conduct these audits, which will assess the coding staff’s skills
• Encourage staff members to learn more about disease processes and clinical interventions to improve their coding performance
An internal coding audit program is the monitoring effort that ties together all coding management func-tions. Managers must select topics that will allow them to develop an exemplary coding program. They should consider all available topics but select only those that are applicable to their setting and that will improve the team’s performance.
Managers should consider whether any of their coders are new to the profession or team. Managers could monitor their performance to determine whether it is at an appropriate level. Coding quality is gauged in the 95%–96% range.
Managers must determine whether their new coders are meeting this level of proficiency. Conducting an audit of their current work can answer that question and lend insight regarding necessary corrective mea-sures. Remember that corrective measures are not intended to mean punitive actions but rather corrective
actions, which may include focused education, addi-tional reference materials, or closer monitoring.
External or internal audits that have identified weak-nesses and claim denials attributable to coding may signal other areas to monitor. Capturing denial reasons attributable to coding serves to identify ideal topics for in-services. Managers can use the findings to imple-ment education programs that can help reduce denials. Reducing coding denials is something tangible to demonstrate the value of your team members to upper management.
Managers also may consider auditing confusing conditions such as sepsis and septicemia or documenta-tion-driven services such as infusion, for which the combination of inadequate documentation of start and stop times and improper coding yields incorrect results.
Managers confronted with multiple appropriate issues to monitor should focus on one at a time until each is resolved and team members are performing at the level expected of them. Internal reviews should apply to all team members, including contractors, and all activities that the team members perform. If team members abstract data into the computer system, periodically review abstracted data for accuracy.
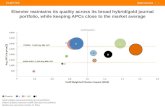
Review discharge dispositions if coders validate them. With many options of topics to monitor, managers should consider developing an internal audit calendar to help stay on track. Share this calendar with the team members and the compliance department so everyone is aware of each month’s focus (see Figure 1 on p. 7).

HCPRO.COM © 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
6 |Briefings on APCs January 2017
Considering the previous discussion, there are addi-tional components needed for a compliance plan. Let’s look at some examples.
Coding audits: Internal and external coding quality audits must be completed on a regular basis.
• Audit sample and frequency:
O Internal reviews for new coders: ■ 100% of the cases coded by a newly em-
ployed, experienced, and certified/creden-tial coder will be reviewed for the first two weeks. If the coder’s accuracy is not at least 95% at the end of the two-week period, the reviews will continue. If the newly hired coder is at 95% at the end of the two-week period, the frequency of reviews will be in accordance with this section of the plan.
■ 100% of all cases coded by a noncertified/credentialed, unexperienced, newly em-ployed coder will be reviewed until such time that the coder achieves a 95% accuracy rating for two consecutive weeks or 100 con-secutive cases, whichever is larger.
O External reviews (engaged by XYZ) for a cod-er’s first year with XYZ or if coder fails to achieve 95% accuracy:
■ Inpatient coding: Quarterly; 40 randomly se-lected discharges for each coder coding inpa-tient stays.
■ Outpatient coding: Quarterly; 30 random-ly selected noninvasive encounters for each coder coding noninvasive services, and 40 randomly selected invasive encounter for each coder coding invasive services.
■ Audit focus: Accuracy of:• Coding (capture and code assignment)• Present on admission (POA)• Diagnosis-related group (DRG) and am-
bulatory payment classification (APC)• Sequencing• Disposition• Query content and use
O External reviews: Coders in their second year and thereafter: Same as above but semiannual frequency.
O Internal reviews: Each month, the coding man-ager will review four randomly selected cases for each coder for the same components of the audit focus on accuracy that is listed above.
O Coding accuracy rate will be calculated using the code-over-code methodology. Reimburse-ment accuracy rate will be based on the accuracy of the DRGs and APCs derived using the case-over-case methodology.
• Audit focus:
O Data transfer: Review of the patient record to determine accurate code assignment with sub-sequent comparison with the appropriate claim form (e.g., UB-04, CMS 1500) to confirm codes are properly transferring to the claim
O Regulatory issues: Focus areas should include is-sues identified from the OIG Work Plan, RAC, Medicaid Integrity Contractor, and any specific payer (Medicare Advantage) foci
O Findings from these reviews must be utilized to improve coding and patient record documenta-tion practices and for coder, biller, physician, and other provider education, as appropriate
O Findings of these reviews will be reported to the compliance officer to direct any rebilling and/or refund activities and assess the need for further compliance-related actions
Denial management: Staff responsible for the final code assignments will review all claims denied (in part or total) based on codes assigned. Reviews of denied claims will be completed within 72 hours of receiving the denied claim and payer’s denial reason. All claims reviewed will be tracked in the denial management spreadsheet on the shared drive to facilitate identifying any trends or problem areas. A summary of the reviews will be provided each month to the subcommittee.
Now that we have an idea of some of the content of a coding compliance plan, we need to implement the plan.
Implementing the plan
The examples already outlined in this chapter provide the coding manager or HIM director with some of the components that should be addressed in the coding compliance plan in order to identify opportunities that

HCPRO.COM© 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
Briefings on APCs | 7January 2017
need to be mitigated before external governmental and nongovernmental reviews occur.
Entities that pay healthcare provider claims (payers) monitor the coding function because coding drives reimbursement. These payers capture the data on the claim for data and trend analyses and edit the claims for compliance with the many rules that govern coding. In the prior chapter, we discussed some of the rules.
In our example plan, we encourage our coding team to strive for coding quality and data integrity. Changing a single digit or character of the code to achieve a complication or comorbidity or major comorbidity that yields greater reimbursement for an organization may be tempting.
However, such an action would be fraudulent because it implies that the patient record contains sufficient documentation to support the codes that were assigned. Knowingly doing so routinely can create patterns that suggest to oversight entities that an organization engages in questionable practices, and these patterns are often caught when claims data trending analyses are performed.
Upon observation of such practices, oversight and payer entities may request copies of patient records for their auditors to review. Facilities may incur financial and licensure penalties, negative publicity, and con-
tinuing oversight by government agencies if fraudulent activity is confirmed. Some entities may be required to develop and submit for approval and monitoring a corporate integrity agreement (CIA). If the fraudulent activity is determined to be intentional by one or more coders, the coders may lose their certifications and credentials.
Corporate integrity agreements
According to Joan Hogarth and Roselyn Tyson of the American Health Lawyers Association, a category of Health Law Wiki, the CIA is an enforcement tool used by the OIG within the Department of Health and Human Services (HHS) to improve the quality of healthcare and to promote compliance with healthcare regulations. Similarly, the term integrity agreement or IA is used for smaller healthcare providers such as physicians.
The CIA is usually entered into contemporaneously with a civil settlement between the government and a healthcare provider (individual and entity) who has been the subject of investigations arising under the False Claims Act as amended in 1986 or who has been found guilty in acts of defrauding Medicare, Medicaid, or any other federal healthcare programs. “A provider or entity consents to these obligations as part of the civil settlement and in exchange for the OIG’s agree-
Anywhere Hospital Coding Compliance Calendar
January: CC/MCC capture for inpatient records; contract
coders and new coder reviews
February: Discharge disposition and abstracting accuracy;
contract coders and new coder reviewsMarch: New CPT codes; contract coders and new coder
reviews
April: Modifier usage for outpatient surgery and ED coding
(E/M and infusions); contract coders and new coder reviewsMay: Random selection for all team members June: Surgical inpatients; contract coders and new coder
reviewsJuly: Observation and pregnancy encounters; contract cod-
ers and new coder reviews
August: Chemotherapy and clinic encounters; contract
coders and new coder reviewsSeptember: CC/MCC capture; contract coders and new
coder reviews
October: OIG Workplan topics; contract coders and new
coder reviewsNovember: Random selection for all team members December: New ICD codes; contract coders and new
coder reviews Source: Rose T. Dunn, MBA, RHIA, CPA, FACHE, FHFMA, CHPS

HCPRO.COM © 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
8 |Briefings on APCs January 2017
ment not to seek an exclusion of that healthcare provider or entity from participation in Medicare, Medicaid, and other federal healthcare programs.” (See http://oig.hhs.gov/fraud/cias.asp.)
CIAs are negotiated and monitored through the Office of Counsel to the Inspector General. They are detailed agreements that are constructed to mirror the Federal Sentencing Guidelines of 1995 while remaining indi-vidualized to reflect (i) the scope and size of the healthcare provider and (ii) the specific charges that gave rise to that particular CIA.
A CIA allows a provider who has engaged in fraudu-lent conduct to continue participating in federal healthcare programs. The average time period for a CIA is typically five years. If the healthcare provider breaches the CIA, the OIG reserves the right to
impose additional sanctions including stipulated penalties and permissive exclusion pursuant to its authority under 42 U.S.C.1320a-7(b)(7), according to the American Health Lawyers Association. H
EDITOR’S NOTE:
This article is excerpted from JustCoding’s Practical Guide to Cod-
ing Management by Rose T. Dunn, MBA, RHIA, CPA, FACHE, FHF-
MA, CHPS. Dunn is a past president of the American Health
Information Management Association (AHIMA) and recipient of its
1997 Distinguished Member and 2008 Legacy awards. In 2011, she
served as the interim CEO of AHIMA and received a Distinguished
Service Award from its board of directors. Dunn is the chief operat-
ing officer of First Class Solutions, Inc., a health information man-
agement (HIM) consulting firm based in St. Louis. Opinions
expressed are that of the author and do not necessarily represent
HCPro, ACDIS, or any of its subsidiaries.
OPPS packaging changes for 2017
Q Packaging continues to grow each year under the OPPS. Is CMS still packaging
based on date of service?
A The OPPS is a prospective payment system which involves paying a lump sum for a com-
plete service. We have watched as packaging has ex-panded each year in order to truly have a prospective payment.
With the initiation of composite and comprehensive APCs, more services have become packaged into other services, along with supplies and drugs being packaged into procedures.
For 2017, the big packaging change is that items and services with status indicators of Q1 (status indicator STV packaged codes) and Q2 (status indicator T packaged codes) will be packaged at the claim level and not based on the date of service.
If a patient stays overnight as an outpatient or is receiving observation services, then any Q1 and Q2 items on the claim, regardless of the date of service, will be packaged based on the OPPS standard packag-ing rules, but at the claim level.
For example, if a patient has a procedure and has to stay overnight, all of the Q1/Q2 services that were provided will package into the separately payable procedures/services, even if the procedure was per-formed on the first day and Q1/Q2 services were provided on the second day.
Is ultrasound included in new spinal epidural CPT codes?
Q I notice the parenthetical remarks under-neath the new 2017 CPT spinal epidural
injection codes (62321, 62323, and 62327) indi-cate that fluoroscopy, CT, and ultrasound codes are not to be reported with the code. However, the code descriptors only include flu-oroscopy and CT, without any mention of ultra-sound (76942). Is ultrasound included in the description for 62321?
A Ultrasound is not included in the code descrip-tor for the spinal injections, however, ultra-
sound is not used in these procedures since the spine is too bony. Adequate visualization cannot be achieved via ultrasound due to the bony prominences of the spine.

HCPRO.COM© 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
Briefings on APCs | 9January 2017
Our radiology machine still uses film
Q We have one older radiology machine that still uses film. We are working on re-
placing it and don’t use it very much. Is there anything special that we need to do when re-porting studies done on “old faithful”?
A With the advent of more advanced and comput-erized technology in the radiology realm, most
of the studies performed presently are done with the more advanced technology.
Beginning in January 2017, CMS has created modifier -FX (X-ray taken using film) to identify those proce-dures performed with older technology. Section 1833(t)(16)(F)(iv) of the Social Security Act contains provi-sions for a reduction in payment of 20% for those x-ray services utilizing film for 2017. The reduction will be applied when the service is separately payable. This modifier is mandatory for hospital reporting when the service involves film.
Using modifier –PN for nonexcepted services
Q We have an off-campus provider based department that is “non-excepted,” so we
have to report modifier –PN (nonexcepted ser-vice provided at an off-campus outpatient, pro-vider-based department of a hospital). Is that for just the services that would be paid under the OPPS if the department were “excepted”?
A The -PN modifier should be reported on each claim line. The purpose of this modifier is
two-fold:1. Identification of the nonexcepted services
provided2. Trigger the payment rate under the Medicare
Physician Fee Schedule
This modifier should also be reported on claims lines for separately payable drugs, clinical laboratory tests, and therapy services. However, the modifier does not trigger a payment adjustment for these services. These specific services are paid either at the same amount in
a physician’s office (average sales price +plus6% for drugs) or under the same fee schedule for OPPS hospitals and physician offices.
Excepted outpatient provider-based departments should continue to report modifier -PO (services, procedures and/or surgeries provided at off-campus provider-based outpatient departments), which has been mandatory since January 1, 2016.
For more information, see Transmittal 3685.
Reporting modifiers –PO and –PN together
Q I have a follow-up question to the non-ex-cepted services modifier (-PN). We have
some patients that visit more than one provid-er-based department (we call them clinics) on the same day and we have to combine the ser-vices from both clinics on one claim. Can we report both the -PO and the -PN modifiers on the same claim?
A Yes, modifiers -PN and–PO can be reported on the same claim, but not the same line item. So if
a patient is seen at two clinics and services are provid-ed at each clinic, append modifier -PN to those servic-es provided in the nonexcepted provider-based department (clinic) and modifier -PO to those services provided in the excepted off-campus provider based department.
It would be highly unlikely that the same service would be provided in both departments to the same patient on the same day. Should that occur, review the docu-mentation very carefully to insure that the duplicated service was medically necessary before reporting the service multiple times.
Remember too that a dedicated ED and an on-campus provider-based department are not subject to either modifier. So in your example, if the patient was seen in the ED and an off-campus provider-based department on the same day, the modifier is only applicable to the services in that off-campus provider-based department.

HCPRO.COM © 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
10 |Briefings on APCs January 2017
How do we report stem cell acquisition?
Q We started providing allogenic hemato-poietic stem cell transplants on an outpa-
tient basis for some of our patients. Until just recently, none of them were Medicare patients, but now we have some patients that meet the physician-established criteria for the trans-plant being done as an outpatient. We know that Medicare doesn’t separately pay for the donor acquisition services so we can’t bill them separately. How do we include this on the claim to ensure that the cost of all compo-nents of this service are reported?
A Stakeholders discussed concerns about report-ing these services on an outpatient claim to
ensure that the specific and unique costs were identi-fied on an outpatient claim during OPPS rulemaking last year.
CMS discussed in detail in the 2017 OPPS final rule that this is a very unique situation and they are
making special accommodation by establishing a new comprehensive APC (C-APC) for this service. CPT code 38240 (hematopoietic progenitor cell [HPC]; allogeneic transplantation per donor) is assigned to new C-APC 5244.
In order to ensure the cost of the services is recognized on the outpatient claims, hospitals are required to report revenue code 0815 when billing the donor acquisition services associated with the transplantation.
CMS is implementing a claim edit that requires both CPT code 38240 and revenue code 0815 for the donor acquisition services to be reported on the outpatient claim. Revenue code 0815 is to be used in this sce-nario, replacing revenue code 0819. CMS will update the Medicare Claims Processing Manual (Pub. 100-04, Chapter 4, Section 231.11 and Chapter 3, section 90.3.1) to reflect the new billing guidelines for this service. H
Contributors
Shannon E. McCall, RHIA, CCS, CCS-P, CPC,
CPC-I, CEMC, CCDS
Director of coding and HIM
HCPro
Danvers, Massachusetts
Laurie L. Prescott, RN, MSN, CCDS, CDIP,
AHIMA-approved ICD-10 trainer
CDI education specialist
HCPro
Danvers, Massachusetts
Shelley C. Safian, PhD, MAOM/HSM, CCS-P,
CPC-H, CHA, AHIMA-approved ICD-10 trainer
Safian Communications Services
Orlando, Florida
Lori-Lynne A. Webb, CPC, CCS-P, CCP, CHDA,
CDIP, COBGC, AHIMA-approved ICD-10 trainer
President
Webb Services
Boise, Idaho
Denise Williams, RN, CPC-H
Senior vice president of revenue integrity services
Revant Solutions
Fort Lauderdale, Florida
We would like to thank the following contributors for answering the questions that appear on pages 8–10.

HCPRO.COM© 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
Briefings on APCs | 11January 2017
See what stories and topics Briefings on APCs covered in 2016. To find a specific story, search on www.revenuecycleadvisor.com or www.justcoding.com.
BillingBilling therapy services in support of comprehensive APC services. Aug., p. 4.
CMS adds laboratory drug testing codes, revises IMRT and SRS guidance. June, p. 1.
CMS eases provider burden and reporting
CMS finalizes self-identified overpayments rule for services including Part B. Oct., p. 1.
CMS proposes Part B drug payment test with flat-fee add-on, value-based purchasing tools. May, p. 1.
Define outpatient CDI nuances. June, p. 4.
Determine how Bipartisan Budget Act impacts off-campus departments, modifier -PO. April, p. 7.
Linking diagnoses and procedures to documentation in outpatient settings. Oct., p. 4.
More HIM professionals needed to manage an increasing workload, responsibilities. July, p. 1.
Overcome billing and coding challenges for comprehensive observation services. Oct., p. 7.
Reporting CMS’ modifiers related to Advance Beneficiary Notifications. June, p. 7.
Reporting modifiers for services performed in the postopera-tive period. Aug., p. 8.
requirements in CLFS final rule. Aug., p. 1.
Review your electronic order templates to protect against audits and ensure compliance. Nov., p. 1.
Coding Q&AAccurate coding and billing for biosimilars. Feb., p. 12.
Adhering to provider-based rules. May, p. 12.
Billing circumcision during a delivery. Feb., p. 10.
Billing PHP claims on a weekly basis. Aug., p. 11.
Billing with condition code W2. April, p. 12.
Can inpatient-only procedures be done on outpatients? Nov., p. 10.
Certain pathology services get new status
Changes in heart failure documentation requirements. July, p. 10.
Charging for foreign body removal in the ED. April, p. 12.
Charging separately for each lumen. May, p. 12.
Claims with influenza getting returned. Dec., p. 10.
Clarifying edits with other departments. May, p. 10.
CMS makes changes to drug codes in July update. Aug., p. 12.
Codes for reporting smoking cessation services. Oct., p. 11.
Coding complications during delivery. Jan., p. 11.
Coding weeks of gestation for pregnant patients. April, p. 11.
Correct billing for low-dose CT scans. Jan., p. 11.
Defining therapeutic services. June, p. 10.
Definitions of ancillary bedside procedures. Nov., p. 11.
Determine how to report bedside procedures. July, p. 10.
Determine reimbursement for corneal tissue. March, p. 11.
Determine whether to report hypertension with headache in ICD-10-CM. April, p. 11.
Determining type of heart failure. May, p. 10.
Documentation requirements for bedside procedures. July, p. 11.
Eye procedures performed during the same session. July, p. 12.
Getting a MAC to consider additional diagnoses. May, p. 11.
Guidelines for reporting blepharoptosis tissue removal. Aug., p. 10.
Have modifier−JW requirements changed? Oct., p. 10.
How do we apply modifier –CT? March, p. 10.
How do we receive payment for Inflectra? Nov., p. 11.
indicators in July. Aug., p. 10.
Instrumentation for foreign body removal. May, p. 10.
Linking symptoms with diagnoses in documentation. July, p. 9.
Making a plan to monitor drug reimbursement. Nov., p. 12.
Modifier use during twin deliveries. Feb., p. 11.
Necessary documentation for conditions during delivery. Jan., p. 12.
New HCPCS codes for July. July, p. 12.
New HCPCS codes for October. Oct., p. 12.
New pass-through items in 2016. Jan., p. 10.
Nonreportable services for observation patients. Oct., p. 12.
Noting pregnant patient admission without delivery. March, p. 10.
Payments for Composite APCs. March, p. 10.
2016 Briefings on APCs Index

HCPRO.COM © 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
12 |Briefings on APCs January 2017
Payments for observation Composite APC. June, p. 10.
Processing drug screening claims. July, p. 10.
Receiving payment for Nuwiq. June, p. 11.
Report twins born on different dates. Feb., p. 12.
Reporting facility E/M along with hyperbaric oxygen therapy. Aug., p. 11.
Reporting HCPCS codes for biosimilars. July, p. 11.
Reporting HCPCS codes for drug screening. June, p. 12.
Reporting IMRT services accurately. March, p. 12.
Reporting multiple ultrasounds during the same session. April, p. 12.
Reporting ultrasounds during the same session. June, p. 10.
Reporting unspecified versus other specified schizophrenia in ICD-10-CM. Nov., p. 12.
Requirements for TOB 013X reporting. Oct., p. 12.
Rules for authenticated operative reports. Feb., p. 11.
Should we report mitomycin since it’s already packaged? Nov., p. 10.
Status indicators changing in 2016. June, p. 12.
Tobacco use in pregnant patients. Feb., p. 10.
Using modifier -L1 to receive lab payments. April, p. 10.
Value code reporting requirements in 2016. Feb., p. 10.
We don’t always get payment for lab claims. April, p. 10.
CPT codingDigestive system has most changes for surgical procedures in relatively minor CPT update. Feb., p. 1.
AMA updates genitourinary sections for new technology and terminology. March, p. 1.
Pay attention to the hierarchy when reporting drug adminis-tration services. March, p. 4.
Training tool: CPT codes for shoulder surgery. June, p. 6.
Determine the most appropriate laterality modifier. July, p. 5.
Training tool: CPT codes for reporting craniectomies and craniotomies. Sept., p. 12.
Review proper procedures for applying modifier -52. Feb., p. 4.
ICD-10AHA Coding Clinic for ICD-10 covers orthopedic and cardiovascular coding. Feb., p. 8.
Challenges and opportunities in data analytics. Aug., p. 6.
Impact of ICD-10 on physician workflow: The unforeseen consequences. May, p. 4.
Post-implementation survey shows time spent coding increases for most ICD-10 record types. April, p. 1.
Putting the specific into unspecified. Dec., p. 8.
Survey respondents share challenges, successes. April, p. 6.
Training tool: ICD-10-CM codes for disorders of the skin and subcutaneous tissue. April, p. 9.
Updated 2017 ICD-10-CM guidelines come ‘with’ controver-sial changes. Nov., p. 4.
OPPSAdditional changes in the 2017 OPPS final rule. Dec., p. 7.
CMS aligns packaging logic, deletes laboratory modifier. Dec., p. 5.
CMS backs off some burdensome proposals but imposes negative payment update in latest rule. Jan., p. 1.
CMS implementing site-neutral payment policies in 2017. Dec., p. 1.
CMS looks to enact site-neutral payment policies for off-campus departments. Sept., p. 1.
CMS proposes aligning packaging logic. Sept., p. 5.
CMS proposes removing six codes from inpatient-only list, seeks TKA comments. Sept., p. 9.
CMS shifts 2-midnight rule responsibility to QIOs, finalizes packaging expansion. Jan., p. 5.
OPPS has first negative payment update. Jan., p. 4.
Tips for sending CMS comments. Sept., p. 11.
OPPS AdvisorAccuracy is paramount for providers when reporting CMS’ new modifiers for 2016. Jan., p. 7.
CMS issues new drug reporting requirement while providers wait on Part B payment model. July, p. 7.
CMS surprises with Part B drug payment model that puts the onus on providers. May, p. 6.
Data accuracy is key for CMS to set payment rates, but guidance must be standardized. March, p. 7.
Forecasting financials based on CMS’ latest proposals. Sept., p. 8.
Making a checklist to prepare for the OPPS final rule. Nov., p. 8.

HCPRO.COM© 2017 HCPro, a division of BLR. For permission to reproduce part or all of this newsletter for external distribution or use in educational packets, contact the Copyright Clearance Center at copyright.com or 978-750-8400.
Briefings on APCs | 13January 2017
Las Vegas, Nevada | May 9–12, 2017
3586
4
Visit hcmarketplace.com/ACDIS2017 for complete details, including agenda and hotel information.
Join us in Las Vegas for a big anniversary of the nation’s first and only national conference dedicated to the CDI profession.
The 10th annual ACDIS Conference features unparalleled networking, the ACDIS Achievement Awards, and 50 sessions in the following tracks:
• Clinical and coding• Management and leadership• Quality and regulatory• Outpatient and risk-adjusted CDI• Physician engagement• CDI expansion
WHAT’S HOT IN 2017?Our popular interactive conference app returns, featuring Twitter notifications, conference materials, a session planner, and audience polls.
This year’s lineup of speakers includes YouTube sensation ZDoggMD, as well as CMS, American Hospital Association, and Recovery Auditor representatives!
Register now at hcmarketplace.com/ACDIS2017 and save $100!*Save $200 now if you are an ACDIS member.
Visit: hcmarketplace.com/ACDIS2017 | Call: 800-650-6787 | Email: [email protected]
Don’t miss our rocking, inspirational keynote
Zubin Damania, MDaka ZDoggMD





![Australian Wheeled APCs Austrian Wheeled APCs … Wheeled APCs australian_wheeled_apcs.htm[5/10/2017 9:46:16 PM] Weapons Variant,” which I have, unfortunately, have not been able](https://static.fdocuments.in/doc/165x107/5aafc8647f8b9a25088de9a9/australian-wheeled-apcs-austrian-wheeled-apcs-wheeled-apcs-australianwheeledapcshtm5102017.jpg)












