Bone regeneration using a synthetic matrix containing enamel matrix derivate
-
Upload
david-schneider -
Category
Documents
-
view
215 -
download
2
Transcript of Bone regeneration using a synthetic matrix containing enamel matrix derivate
Bone regeneration using a syntheticmatrix containing enamelmatrix derivate
David SchneiderFranz E. WeberChristoph H. F. HammerleAndreas FeloutzisRonald E. Jung
Authors’ affiliations:David Schneider, Christoph H. F. Hammerle,Ronald E. Jung, Center for Dental and OralMedicine and Cranio-Maxillofacial Surgery, Clinicfor Fixed and Removable Prosthodontics and DentalMaterial Science, University of Zurich, Zurich,SwitzerlandFranz E. Weber, Department of Cranio-Maxillofacial Surgery, Section of OralBiotechnology & Bioengineering, UniversityHospital Zurich, Zurich, SwitzerlandAndreas Feloutzis, Private Practice, Maroussi,Greece
Corresponding author:Dr Ronald E. JungCenter for Dental and Oral Medicine and Cranio-Maxillofacial SurgeryClinic for Fixed and Removable Prosthodontics andDental Material ScienceUniversity of ZurichPlattenstrasse 11CH-8032 ZurichSwitzerlandTel.: þ 41 44 634 32 51Fax: þ 41 44 634 43 05e-mail: [email protected]
Key words: animal study, bioactive factor, bone regeneration, EMD, enamel matrix protein,
graft material, polyethylene glycols, RGD
Abstract
Purpose: The aim of the present study was to test whether the delivery of enamel matrix
derivate (EMD) via synthetic polyethylene glycol (PEG)-based hydrogels with and without
RGD sequences enhances bone formation in vivo.
Material and methods: In each of 10 rabbits, four titanium cylinders were placed on the
external cortical bones of their calvaria. The following four treatment modalities were
randomly allocated: One of the four cylinders was left empty (control), the other three were
filled with a combination of PEG matrix with hydroxyapatite/tricalciumphosphate (HA/TCP)
granules and EMD in a concentration of 100mg/ml (test 1) or 500mg/ml (test 2) or 500mg/ml
and RGD peptide (test 3). After 8 weeks, the animals were sacrificed and ground sections
were obtained for histological analysis. For statistical analysis, the Kruskal–Wallis test was
applied (Po0.05).
Results: The histomorphometric analysis revealed a statistically larger area fraction of
newly formed bone in the EMD 500/RGD group (54.8 � 14.5%) compared with the control
group (28.7 � 10.3%) and the EMD 500 group (31.2 � 14.1%) and non-significantly higher
area fraction compared with the EMD 100 group (38.2 � 10.4%). The percentage of
mineralized bone showed no statistically significant differences among the four groups.
The mean percentage of mineralized bone was 13.6 � 3.3% in the control group,
14.2 � 5.8% in the EMD 100 group, 11.69 � 5.9% in the EMD 500 group and 15.66 � 5.2%
in the EMD 500/RGD group. No statistically significant difference regarding the bone-to-
graft contact between the EMD 100 group (23 � 15.7%), the EMD 500 group
(22.2 � 14.6%) and the EMD 500/RGD group (21.6 � 8.8%) was observed.
Conclusions: The combination of a PEG matrix containing EMD with HA/TCP granules had
no effect on the formation of mineralized bone tissue in rabbit calvaria. The addition of
RGD peptide to the PEG/EMD 500 combination increased the area fraction of newly formed
bone compared with the other treatment groups. Further studies are indicated to study a
possible synergistic effect of EMD and RGD.
Tooth extraction is followed by a remodel-
ing processes of the alveolar ridge resulting
in partial loss of the buccal bone contour
(Araujo & Lindhe 2005). A large variety of
methods and materials for the regeneration
of lost alveolar bone have been described
(Hammerle & Karring 1998). Although
autologous bone is still considered to be
the ‘‘gold standard,’’ the limited availabil-
ity and the donor site morbidity have led to
a shift toward the use of xenogenic or
allogenic materials (Nkenke et al. 2001,
2002). Some of these materials are well
documented and have proven their efficacy
Date:Accepted 14 May 2010
To cite this article:Schneider D, Weber FE, Hammerle CHF, Feloutzis A,Jung RE. Bone regeneration using a synthetic matrixcontaining enamel matrix derivateClin. Oral Impl. Res 22, 2011; 214–222.doi: 10.1111/j.1600-0501.2010.01985.x
214 c� 2011 John Wiley & Sons A/S
and safety over a long period, but they are
associated with long healing periods be-
cause they lack osseoinductive properties
(Iezzi et al. 2007; Traini et al. 2007).
Grafting materials originating from animal
sources can cause difficulties in terms of
patient acceptance, immune response and a
possible transmission of infectious agents
that can never be completely excluded. As
a fully synthetic material, hydroxyapatite/
tricalciumphosphate (HA/TCP) overcomes
these shortcomings and has shown effec-
tiveness as a bone substitute for guided
bone regeneration (GBR) in several studies
(Froum et al. 2001; Schwarz et al. 2007;
Zafiropoulos et al. 2007; Artzi et al. 2008;
Cordaro et al. 2008)
The induction of bone formation re-
mains a challenge in tissue regeneration.
Numerous preclinical and clinical studies
have shown a positive effect of growth
factors and differentiation factors in hard
and soft tissue regeneration (Lynch et al.
1991; Howell et al. 1997; Cochran et al.
1999; Jung et al. 2003, 2005, 2008). The
regenerative potential also depends on the
method of application and release kinetics
of the bioactive substances from their car-
rier (Sigurdsson et al. 1996; Hunt et al.
2001).
Enamel matrix derivate (EMD) is an
extract from porcine tooth buds. It is com-
posed of several proteins, up to 90% of
which are amelogenins. The residual 10%
are proline-rich non-amelogenins. Enamel
matrix proteins are secreted by ameloblasts
during tooth formation and regulate en-
amel mineralization (Simmer & Fincham
1995). They are also secreted by epithelial
cells of the Hertwig’s root sheath during
root formation and affect the formation of
periodontal tissues, primarily acellular ce-
mentum (Hammarstrom 1997). Therefore,
EMD has been mainly used in periodontal
regenerative treatment, especially for furca-
tion and intrabony defects (Froum et al. 2001;
Tonetti et al. 2002; Donos et al. 2003; Jepsen
et al. 2004; Meyle et al. 2004; Sanz et al.
2004; Hoffmann et al. 2006).
Very little data are available regarding the
effect of EMD for periimplant bone regen-
eration (Casati et al. 2002). As matrix
proteins, EMD shows very low solubility
at physiological pH, but is soluble under
acidic conditions. Commercially available
EMD (Emdogains
, Institut Straumann AG,
Basel, Switzerland) is dissolved in a slightly
acidic propylene glycol alginate (PGA) gel.
One problem in applying Emdogains
for
periimplant bone regeneration is that its
PGA carrier gel is designed to collapse and
release the EMD at the tooth root under
physiological conditions and thus does not
provide space-keeping properties or the
retention of the protein in a larger volume.
The use of an optimized matrix as a deliv-
ery system for EMD could overcome this
problem. The combination of a bone sub-
stitute (e.g. HA/TCP) potentially provides
additional stability of the compound, help-
ing to keep the substances at the site of
bone regeneration.
Polyethylene glycol (PEG)-based hydro-
gels have been shown to be effective delivery
systems for bioactive substances because
these matrices allow optimal cell ingrowth
as well as retention and release of bioactive
proteins such as recombinant human bone
morphogenetic protein-2 (rhBMP-2) and
parathyroid hormone (PTH) (Lutolf et al.
2003; Jung et al. 2007a, 2007b, 2008). The
ingrowth of cells into these matrices can be
facilitated by the presence of RGD-contain-
ing peptides, an amino acid sequence com-
posed of arginine, glycine and aspartate.
RGD sequences are mainly found in extra-
cellular matrix proteins (e.g. fibronectin)
and mediate cell adhesion, cell migration
and signal transduction via binding to integ-
rins, a subgroup of cell surface receptors
(Akiyama 1996). The possible application
of EMD with an optimized carrier material
with and without RGD has not been in-
vestigated yet.
Hence, the aim of the present study was
to test if the delivery of EMD in different
concentrations via synthetic PEG-based
hydrogels with and without RGD se-
quences enhances bone formation in vivo.
Materials and methods
The present animal investigation was eval-
uated and approved by the responsible An-
imal Research Ethics Committee at the
University of Zurich, Switzerland.
Synthetic matrix and bioactive peptides
The synthetic matrix used as the carrier in
the present study was a PEG-based hydro-
gel (Institut Straumann AG, Basel, Swit-
zerland). This gel was formed by a reaction
of a 4-arm PEG with acrylate endgroups
with a linear PEG with thiol endgroups in
an aqueous buffer system (triethanola-
mine/HCl) (Elbert et al. 2001). The PEG
termini connected through a highly self-
selective addition reaction, forming an
elastic gel network. Immediately before
application, both PEG solutions were ster-
ile filtered and mixed with 0.15 g of HA/
TCP granulate in a distribution of 60% :
40% and a particle size of 400–700mm
(Straumann BoneCeramic, Institut Strau-
mann AG).
For the activated gels, stock solutions of
a lyophilized EMD and a nine amino acid
cys-RGD peptide (Bachem, Bubendorf,
Switzerland) in dilute (0.1%) acetic acid
were added first to the PEG-acrylate solu-
tion, resulting in the formation of covalent
bonds between the cystein residues and the
PEG-acrylate upon gelation, which was
started by adding the triethanolamine buf-
fer solution. The final concentrations for
the peptides were 350 mg/ml gel for cys-
RGD and 100 or 500mg/ml gel for EMD.
The surgical procedure, the histological
preparation, the histomorphometric and
statistic evaluation were performed accord-
ing to a previous animal study (Jung et al.
2007b).
Surgical procedure
The surgical procedure was performed in
10 adult New Zealand white rabbits. Dur-
ing a standardized surgical procedure, four
evenly distributed circular slits, 6 mm in
diameter and 1 mm in depth, were prepared
with a trephine bur bilaterally in the par-
ietal and frontal bones. Without removal
but after perforation of the external cortical
plate inside the created circles with a round
bur, specially designed 7 � 7 mm large
cylinders made of c.p. titanium with a
machined surface on their inside were
screwed into the slits.
One of the four cylinders served as a
control and was left empty. Another cylin-
der contained the EMD in a concentration
of 100mg/ml gel (test 1), and a third cylin-
der contained EMD in a concentration of
500 mg/ml gel (test 2). The fourth cylinder
contained EMD in a concentration of
500 mg/ml gel in combination with cys-
RGD (test 3). The position of the cylinders
in each animal was randomly assigned by
rotating the position of the treatment mod-
alities in a clockwise direction. After appli-
cation of the test substances into the
Schneider et al �Bone regeneration using a synthetic matrix and EMD
c� 2011 John Wiley & Sons A/S 215 | Clin. Oral Impl. Res. 22, 2011 / 214–222
cylinders, they were closed with a titanium
lid and the skin flap was adapted and
sutured for primary healing (Figs 1–3).
Histologic preparation
After 8 weeks, the rabbits were sedated
with barbiturates and sacrificed by an over-
dose of ketamin. The specimens were sec-
tioned in the frontal plane through the
middle of the cylinders. 200-mm-thick sec-
tions were obtained, ground and polished to
a uniform thickness of 60–80mm (Donath &
Breuner 1982). The specimens were surface-
stained with toluidine blue (Schenk et al.
1984). One central section was selected
to perform histomorphometric measure-
ments.
Histomorphometry
The mineralized bone tissue content was
assessed by applying standard morphome-
trical techniques (Weibel 1980; Gundersen
et al. 1988). Measurements were carried
out using a light microscope at a magnifi-
cation of � 160, using an optically super-
imposed eyepiece test grid composed of 100
points and 10 cycloid lines (Schenk &
Olah 1980). The graft to bone contact
was calculated by the number of intersec-
tions between graft particles and the
outlines of either mineralized bone or non-
mineralized tissue.
In order to respect not only the amount
of newly formed bone but also its extension
and distribution within the cylinders, a
quantitative evaluation of the area of bone
regeneration within the cylinders was per-
formed using a pixel count of histological
digital images in an image analysis program
(Adobes
Photoshop 7.0.1) (area of bone
regeneration [%]¼ pixel number of the
bone area � 100/total pixel number of the
cylinder) (Jung et al. 2008).
Statistical analysis
Mean values and standard deviations were
calculated based on point measurements or
cycloid measurements. The primary unit
for statistical analysis was the cylinder. All
values are displayed including the median.
Significant differences were identified by a
Kruskal–Wallis test and confirmed be-
tween groups by a Mann–Whitney U-
test. Statistical significance was set at
Po0.05. The statistical analysis was per-
formed using a statistical software package
(SPSS 16 for Windows).
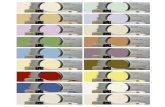
Fig. 1. Bone preparation: four circular slits (6 mm in diameter, 1 mm in depth) and five cortical perforation
holes.
Fig. 2. Titanium cylinders screwed into the slits.
Fig. 3. Closed cylinders after the augmentation procedure.
Schneider et al �Bone regeneration using a synthetic matrix and EMD
216 | Clin. Oral Impl. Res. 22, 2011 / 214–222 c� 2011 John Wiley & Sons A/S
Results
During the experiment, all animals showed
an uneventful healing in the area of sur-
gery. No reductions in body weights were
noted, and no postoperative infections were
observed. Upon specimen retrieval, 33 cy-
linders were found to be stable and in the
same position as at placement. However,
seven out of 40 cylinders were loose and
therefore excluded from further analysis
(two in the control group, two in test 1,
two in test 2 and one in the test 3 group).
Descriptive histology
The qualitative evaluation of the histologi-
cal specimens showed variable amounts
and patterns of bone formation in the four
treatment groups. The empty cylinders
(control group) presented a structure with
few trabeculae and large marrow spaces.
Adjacent to the inner walls of these cylin-
ders, the bone trabeculae were oriented in a
parallel manner. The bone formation was
limited to the lower third of the cylinders
(Fig. 4).
In cylinders containing the PEG matrix
with EMD in a concentration of 100mg/g
gel (test 1 group), the amount of newly
formed bone varied considerably. Similar to
the control group, the trabeculae neighbor-
ing the inner walls were aligned parallel to
the titanium surface. The extension of the
newly formed bone varied between the
lower to the upper third of the cylinders
(Fig. 5).
A similar situation was found in the
cylinders filled with PEG matrix with
EMD in a concentration of 500mg/g gel
(test 2 group). A large variety of new bone
was observed (Fig. 6).
The highest amount of newly formed
bone was observed in the group containing
EMD 500 mg/g combined with RGD (test 3
group). In most cases, the new bone
reached the upper third of the cylinders
and was evenly distributed among the
lower two thirds, embedding the HA/
TCP granules (Figs 7 and 8). All features
of lamellar bone structure (osteons, Haver-
sian canals, osteoblasts and -clasts, etc.)
could be observed.
Histomorphometry
The quantitative histomorphometric ana-
lysis revealed that the content of miner-
alized bone tissue was very similar in all
the groups (Fig. 9). Therefore, no signifi-
cant difference was detectable between the
groups (Table 1). The difference between
the means was highest between EMD
500 (11.7� 5.6%) and EMD 500/RGD
(15.7� 5.2%). On the other hand, the
quantitative evaluation of the area of bone
regeneration revealed a statistically signifi-
cant larger bone area in the EMD 500/RGD
(test 3) group compared with the control
Fig. 4. Histological section through an initially empty cylinder (control group) (original magnification � 10).
Fig. 5. Histological section through a cylinder containing polyethylene glycolþenamel matrix derivate 100
(test 1) (original magnification � 10).
Schneider et al �Bone regeneration using a synthetic matrix and EMD
c� 2011 John Wiley & Sons A/S 217 | Clin. Oral Impl. Res. 22, 2011 / 214–222
group (Fig. 10; Table 2). Among the groups
containing EMD, the most extended area of
bone formation was found in the EMD
500/RGD (test 3) group (54.8� 14.5%)
compared with the other EMD groups
(test 1: 38.2� 10.4%; test 2: 31.2�
14.1%). The area of bone formation was
significantly increased in the EMD 500-
containing groups, when RGD peptides
were added.
Regarding the bone-to-graft contact, the
EMD 100 group, the EMD 500 group and
the EMD 500/RGD group showed no statis-
tically significant difference (23� 15.7%,
22.2� 14.6% and 21.6� 8.8%, respec-
tively) (Fig. 11; Table 3).
Discussion
The results of the present study indicate
that the combination of a PEG matrix
containing enamel matrix protein (EMD)
with HA/TCP granules has a limited effect
on the formation of mineralized bone tissue
in the rabbit calvaria. However, the area
fraction of bone formation was signifi-
cantly increased by the addition of RGD
peptide to the PEG/EMD500 group with-
out affecting the graft to bone contact.
The topical application of enamel matrix
protein is well documented in periodontal
therapy and is effective in the regeneration
of periodontal tissues including bone. Ani-
mal and clinical studies have shown the
effectiveness of EMD in the treatment of
infrabony (Heijl et al. 1997; Froum et al.
2001; Tonetti et al. 2002; Cochran et al.
2003; Silvestri et al. 2003; Sanz et al. 2004;
Sculean et al. 2004) and furcation type
defects (Donos et al. 2003; Jepsen et al.
2004; Meyle et al. 2004; Hoffmann et al.
2006), providing superior clinical results
than open flap surgery alone and similar
results as by applying GTR techniques.
Although it stimulates osteoblasts in
vitro (Jiang et al. 2006), EMD has not
been tested clinically for the regeneration
of non-periodontal bone defects. In an ani-
mal study, EMD was combined with de-
proteinized bovine bone mineral (DBBM)
in one group and with a PGA carrier in
another and inserted into muscular tissue,
without contact to any bone tissue (Donos
et al. 2006). After 2 and 4 months, the
DBBM particles were encapsulated, regard-
less of the presence of PGA and no bone
formation was observed indicating that
neither EMD alone nor in combination
with PGA is able to induce bone formation.
A similar study in mice has shown that
EMD is not osteoinductive but it can be
osteoconductive in certain concentrations
in combination with demineralized freeze-
dried bone allograft (DFDBA) (Boyan et al.
2000). A comparative study in rabbits
with a similar design as the present study
showed that EMD had little effect on bone
formation in combination with b-TCP
Fig. 6. Histological section through a cylinder containing polyethylene glycolþenamel matrix derivate 500
(test 2) (original magnification � 10).
Fig. 7. Histological section through a cylinder containing polyethylene glycolþenamel matrix derivate
500þRGD (test 3) (original magnification � 10).
Schneider et al �Bone regeneration using a synthetic matrix and EMD
218 | Clin. Oral Impl. Res. 22, 2011 / 214–222 c� 2011 John Wiley & Sons A/S
compared with b-TCP alone (Murai et al.
2005). Using EMD alone or in combination
with DBBM for bone regeneration at the
lateral rat ramus, no effect on the forma-
tion of new bone under dome-shaped PTFE
capsules was observed compared with the
use of the capsule alone in another inves-
tigation (Donos et al. 2005). These results
are in agreement with the present study
revealing no effect of EMD in combination
with HA/TCP on bone regeneration, even
in higher dosages.
In a recent animal model, EMD has been
compared with rhBMP-2 and DFDBA for
the regeneration of critical-size calvaria
bone defects. It was shown that, without
the use of a bone substitute, unlike rhBMP-
2, both DFDBA and EMD did not lead to a
regeneration of the bone defect (Intini et al.
2008).
EMD has also been investigated for peri-
implant bone regeneration. An in vitro
study demonstrated a concentration-de-
pendent positive effect of EMD on human
osteoblast-like cells on a titanium surface
(Schwarz et al. 2004). In an animal study
with artificial dehiscence-type defects, it
was observed that the application of EMD
resulted in a similar amount of bone for-
mation as GBR with a resorbable mem-
brane (Casati et al. 2002). However, only
the combination of EMD and the mem-
brane showed a significantly higher area of
bone formation compared with the un-
treated control group in that study, suggest-
ing that EMD has the potential to
stimulate bone formation even in the
absence of periodontal ligament cells. The
addition of EMD into drill holes before
implant placement did not have a benefi-
cial effect on the osseointegration in
another animal study (Franke Stenport &
Johansson 2003). According to the observa-
tion of the growth pattern in the present
study, a layer of newly formed bone
was found on the inner wall of the titanium
cylinders in all groups. A difference in
the amount or the pattern of growth along
the titanium surface was not found among
the groups. The titanium surface appears
to be a guiding structure for the
cells involved in bone formation indepen-
dently of the presence or absence of EMD
or RGD.
The addition of RGD to the PEG–EMD
500 combination has led to a significant
increase in the area of bone formation
within the titanium cylinders. Several ex-
perimental studies have shown an in-
creased bone formation on RGD-coated
implant surfaces compared with uncoated
implants (Schaffner et al. 1999; Elmen-
gaard et al. 2005; Schliephake et al.
2005). Because RGD sequences play an
important role in cell adhesion, cell migra-
tion and signal transduction (Pierschbacher
& Ruoslahti 1984; Akiyama 1996), it can
be assumed that these properties are bene-
ficial for the formation of new bone in
connection with the bone substitute HA/
TCP. However, although RGD has been
suggested to be a mediator for osteoblast
adhesion to HA (Okamoto et al. 1998), the
bone-to-HA/TCP contact appears not to
have been influenced by RGD in the pre-
sent study. The fact that the bone-to-graft
contact is not influenced by the presence of
the RGD peptides might indicate their
absence from the HA/TCP surface, most
likely due to the fact that the cys-RGD
peptides were allowed to covalently bind to
the PEG hydrogel by their addition to the
Fig. 8. Histological section through a cylinder containing polyethylene glycolþenamel matrix derivate
500þRGD (test 3), detail (original magnification � 160).
Fig. 9. The percentage of mineralized bone generated within the cylinders in each group is displayed. The lines to
the right of the values indicate the median of the group. No significant differences between the groups were observed.
Table 1. Percentage of mineralized bone
Condition Number ofsamples
Mean(%)
SD
Empty 8 13.6 3.3EMD 100 8 14.2 5.8EMD 500 8 11.7 5.9EMD 500/RGD 9 15.7 5.2
EMD, enamel matrix derivate.
Schneider et al �Bone regeneration using a synthetic matrix and EMD
c� 2011 John Wiley & Sons A/S 219 | Clin. Oral Impl. Res. 22, 2011 / 214–222
PEG acrylate solution before their first
contact with the HA/TCP particles.
According to a recent in vitro study
(Lutolf et al. 2003), the ingrowth of osteo-
blasts into the PEG matrix is facilitated by
the presence of RGD. This might explain
the finding that the addition of RGD to
500 mg/ml EMD significantly increased the
area of newly formed bone. It can be
speculated that the presence of RGD
within the PEG gel facilitates the ingrowth
of osteoblasts and leads to a broader dis-
tribution of the bone tissue within the
cylinders. Thus, also in this animal model,
the presence of RGD peptides in the matrix
is beneficial for bone formation.
The same study design and the same
carrier (PEG) were used to investigate the
effect on bone formation of rhBMP-2 (Jung
et al. 2008) and PTH (Jung et al. 2007a).
Therefore, a comparison of these sub-
stances and those used in the present study
can be performed. Compared with PTH
(53.5� 22.7%), the mean area of newly
formed bone was similar in the present
study in the EMD 500/RGD group
(54.8� 14.5%). The percentage of miner-
alized bone, however (15.7� 5.2%), was
lower than observed in the investigations
with BMP (30.2� 7.6%) and PTH
(19.6� 6%).
Based on the comparison of these three
studies, it appears that the effect on bone
regeneration was similar between EMD
and PTH, whereas rhBMP-2 revealed al-
most twice as much newly formed bone
compared with either EMD or PTH. All
three bioactive factors reveal a favorable
ingrowth and distribution of newly formed
bone within the entire titanium cylinder.
This might indicate a good matrix structure
given by the PEG hydrogel.
Conclusion
It can be concluded that the combination of
a PEG matrix containing enamel matrix
protein (EMD) with HA/TCP granules has
no effect on the percentage of mineralized
bone tissue in the rabbit calvaria compared
with spontaneous healing, independent of
the EMD concentration. However, the ad-
dition of RGD peptide to the PEG/EMD
500 group revealed an increased area
fraction of new bone compared with the
other treatment groups. Further studies are
Fig. 10. Area fraction of newly formed bone within the cylinder. The lines to the right of the values indicate the
median of the group. Application of the Kruskal–Wallis test revealed a significant difference between the four
groups (P¼ 0.004). Significant differences between groups determined by the Mann–Whitney U-test are
indicated nnPo0.05.
Table 2. Area fraction of newly formed bone
Condition Number of samples Mean (%) SD
Empty 8 28.7 10.3EMD 100 8 38.2 10.4EMD 500 8 31.2 14.1EMD 500/RGD 9 54.8 14.5
EMD, enamel matrix derivate.
Fig. 11. Surface fraction of bone-to-graft contact. The lines to the right of the values indicate the median of the
group. No significant differences between the groups were observed.
Table 3. Surface fraction of bone to graft contact
Condition Number of samples Mean (%) SD
EMD 100 8 23 15.7EMD 500 8 22.2 14.6EMD 500/RGD 9 21.6 8.8
EMD, enamel matrix derivate.
Schneider et al �Bone regeneration using a synthetic matrix and EMD
220 | Clin. Oral Impl. Res. 22, 2011 / 214–222 c� 2011 John Wiley & Sons A/S
indicated to investigate a possible synergis-
tic effect of EMD and RGD.
Acknowledgements: The authors
express their gratitude to Aart
Molenberg (PhD, Institut Straumann
AG) and Michel Dard (PhD, Institut
Straumann AG) for providing expertise
and support. The animal care by F.
Nicholls (University Hospital, Zurich,
Switzerland) and the technical
assistance by J. Fierz and A.
Tchouboukov are also highly
acknowledged.
References
Akiyama, S.K. (1996) Integrins in cell adhesion and
signaling. Human Cell 9: 181–186.
Araujo, M.G. & Lindhe, J. (2005) Dimensional ridge
alterations following tooth extraction. An experi-
mental study in the dog. Journal of Clinical
Periodontology 32: 212–218.
Artzi, Z., Weinreb, M., Carmeli, G., Lev-Dor, R.,
Dard, M. & Nemcovsky, C.E. (2008) Histomor-
phometric assessment of bone formation in sinus
augmentation utilizing a combination of autoge-
nous and hydroxyapatite/biphasic tricalcium
phosphate graft materials: at 6 and 9 months in
humans. Clinical Oral Implants Research 19:
686–692.
Boyan, B.D., Weesner, T.C., Lohmann, C.H., An-
dreacchio, D., Carnes, D.L., Dean, D.D., Co-
chran, D.L. & Schwartz, Z. (2000) Porcine fetal
enamel matrix derivative enhances bone forma-
tion induced by demineralized freeze dried bone
allograft in vivo. Journal of Periodontology 71:
1278–1286.
Casati, M.Z., Sallum, E.A., Nociti, F.H. Jr., Caf-
fesse, R.G. & Sallum, A.W. (2002) Enamel matrix
derivative and bone healing after guided bone
regeneration in dehiscence-type defects around
implants. A histomorphometric study in dogs.
Journal of Periodontology 73: 789–796.
Cochran, D.L., King, G.N., Schoolfield, J., Velas-
quez-Plata, D., Mellonig, J.T. & Jones, A. (2003)
The effect of enamel matrix proteins on perio-
dontal regeneration as determined by histological
analyses. Journal of Periodontology 74: 1043–
1055.
Cochran, D.L., Schenk, R., Buser, D., Wozney, J.M.
& Jones, A.A. (1999) Recombinant human bone
morphogenetic protein-2 stimulation of bone for-
mation around endosseous dental implants. Jour-
nal of Periodontology 70: 139–150.
Cordaro, L., Bosshardt, D.D., Palattella, P., Rao, W.,
Serino, G. & Chiapasco, M. (2008) Maxillary
sinus grafting with bio-oss or straumann bone
ceramic: histomorphometric results from a rando-
mized controlled multicenter clinical trial. Clin-
ical Oral Implants Research 19: 796–803.
Donath, K. & Breuner, G. (1982) A method for the
study of undecalcified bones and teeth with at-
tached soft tissues. The Sage-Schliff (sawing and
grinding) technique. Journal of Oral Pathology
11: 318–326.
Donos, N., Bosshardt, D., Lang, N., Graziani, F.,
Tonetti, M., Karring, T. & Kostopoulos, L. (2005)
Bone formation by enamel matrix proteins and
xenografts: an experimental study in the rat ra-
mus. Clinical Oral Implants Research 16: 140–
146.
Donos, N., Glavind, L., Karring, T. & Sculean, A.
(2003) Clinical evaluation of an enamel matrix
derivative in the treatment of mandibular degree II
furcation involvement: a 36-month case series.
International Journal of Periodontics and Re-
storative Dentistry 23: 507–512.
Donos, N., Kostopoulos, L., Tonetti, M., Karring, T.
& Lang, N.P. (2006) The effect of enamel matrix
proteins and deproteinized bovine bone mineral on
heterotopic bone formation. Clinical Oral Im-
plants Research 17: 434–438.
Elbert, D.L., Pratt, A.B., Lutolf, M.P., Halstenberg,
S. & Hubbell, J.A. (2001) Protein delivery from
materials formed by self-selective conjugate addi-
tion reactions. Journal of Controlled Release 76:
11–25.
Elmengaard, B., Bechtold, J.E. & Soballe, K. (2005)
In vivo study of the effect of RGD treatment on
bone ongrowth on press-fit titanium alloy im-
plants. Biomaterials 26: 3521–3526.
Franke Stenport, V. & Johansson, C.B. (2003) En-
amel matrix derivative and titanium implants.
Journal of Clinical Periodontology 30: 359–363.
Froum, S.J., Weinberg, M.A., Rosenberg, E. & Tar-
now, D. (2001) A comparative study utilizing
open flap debridement with and without enamel
matrix derivative in the treatment of periodontal
intrabony defects: a 12-month re-entry study.
Journal of Periodontology 72: 25–34.
Gundersen, H.J., Bendtsen, T.F., Korbo, L., Mar-
cussen, N., Moller, A., Nielsen, K., Nyengaard,
J.R., Pakkenberg, B., Sorensen, F.B. & Vesterby,
A. (1988) Some new, simple and efficient stereo-
logical methods and their use in pathological
research and diagnosis. APMIS 96: 379–394.
Hammarstrom, L. (1997) Enamel matrix, cemen-
tum development and regeneration. Journal of
Clinical Periodontology 24: 658–668.
Hammerle, C.H. & Karring, T. (1998) Guided bone
regeneration at oral implant sites. Periodontology
2000 17: 151–175.
Heijl, L., Heden, G., Svardstrom, G. & Ostgren, A.
(1997) Enamel matrix derivative (EMDOGAIN)
in the treatment of intrabony periodontal defects.
Journal of Clinical Periodontology 24: 705–714.
Hoffmann, T., Richter, S., Meyle, J., Gonzales, J.R.,
Heinz, B., Arjomand, M., Sculean, A., Reich, E.,
Jepsen, K., Jepsen, S. & Boedeker, R.H. (2006) A
randomized clinical multicentre trial comparing
enamel matrix derivative and membrane treat-
ment of buccal class II furcation involvement in
mandibular molars. Part III: patient factors and
treatment outcome. Journal of Clinical Perio-
dontology 33: 575–583.
Howell, T.H., Fiorellini, J., Jones, A., Alder, M.,
Nummikoski, P., Lazaro, M., Lilly, L. & Co-
chran, D. (1997) A feasibility study evaluating
rhBMP-2/absorbable collagen sponge device for
local alveolar ridge preservation or augmentation.
International Journal of Periodontics and Re-
storative Dentistry 17: 124–139.
Hunt, D.R., Jovanovic, S.A., Wikesjo, U.M., Woz-
ney, J.M. & Bernard, G.W. (2001) Hyaluronan
supports recombinant human bone morphoge-
netic protein-2 induced bone reconstruction of
advanced alveolar ridge defects in dogs. A pilot
study. Journal of Periodontology 72: 651–658.
Iezzi, G., Degidi, M., Scarano, A., Petrone, G. &
Piattelli, A. (2007) Anorganic bone matrix re-
trieved 14 years after a sinus augmentation pro-
cedure: a histologic and histomorphometric
evaluation. Journal of Periodontology 78: 2057–
2061.
Intini, G., Andreana, S., Buhite, R.J. & Bobek, L.A.
(2008) A comparative analysis of bone formation
induced by human demineralized freeze-dried
bone and enamel matrix derivative in rat calvaria
critical-size bone defects. Journal of Perio-
dontology 79: 1217–1224.
Jepsen, S., Heinz, B., Jepsen, K., Arjomand, M.,
Hoffmann, T., Richter, S., Reich, E., Sculean,
A., Gonzales, J.R., Bodeker, R.H. & Meyle, J.
(2004) A randomized clinical trial comparing
enamel matrix derivative and membrane treat-
ment of buccal class II furcation involvement in
mandibular molars. Part I: study design and re-
sults for primary outcomes. Journal of Perio-
dontology 75: 1150–1160.
Jiang, J., Goodarzi, G., He, J., Li, H., Safavi, K.E.,
Spangberg, L.S. & Zhu, Q. (2006) Emdogain-gel
stimulates proliferation of odontoblasts and osteo-
blasts. Oral Surgery, Oral Medicine, Oral Pathol-
ogy, Oral Radiology, and Endodontology 102:
698–702.
Jung, R.E., Cochran, D.L., Domken, O., Seibl, R.,
Jones, A.A., Buser, D. & Hammerle, C.H. (2007a)
The effect of matrix bound parathyroid hormone
on bone regeneration. Clinical Oral Implants
Research 18: 319–325.
Jung, R.E., Glauser, R., Scharer, P., Hammerle,
C.H., Sailer, H.F. & Weber, F.E. (2003) Effect of
rhBMP-2 on guided bone regeneration in humans.
Clinical Oral Implants Research 14: 556–568.
Jung, R.E., Hammerle, C.H., Kokovic, V. & Weber,
F.E. (2007b) Bone regeneration using a synthetic
matrix containing a parathyroid hormone peptide
combined with a grafting material. The Interna-
tional Journal of Oral & Maxillofacial Implants
22: 258–266.
Jung, R.E., Schmoekel, H.G., Zwahlen, R., Koko-
vic, V., Hammerle, C.H. & Weber, F.E. (2005)
Platelet-rich plasma and fibrin as delivery systems
for recombinant human bone morphogenetic
protein-2. Clinical Oral Implants Research 16:
676–682.
Jung, R.E., Weber, F.E., Thoma, D.S., Ehrbar, M.,
Cochran, D.L. & Hammerle, C.H. (2008) Bone
morphogenetic protein-2 enhances bone forma-
tion when delivered by a synthetic matrix con-
Schneider et al �Bone regeneration using a synthetic matrix and EMD
c� 2011 John Wiley & Sons A/S 221 | Clin. Oral Impl. Res. 22, 2011 / 214–222
taining hydroxyapatite/tricalciumphosphate.
Clinical Oral Implants Research 19: 188–195.
Lutolf, M.P., Weber, F.E., Schmoekel, H.G.,
Schense, J.C., Kohler, T., Muller, R. & Hubbell,
J.A. (2003) Repair of bone defects using synthetic
mimetics of collagenous extracellular matrices.
Nature Biotechnology 21: 513–518.
Lynch, S.E., Buser, D., Hernandez, R.A., Weber,
H.P., Stich, H., Fox, C.H. & Williams, R.C.
(1991) Effects of the platelet-derived growth fac-
tor/insulin-like growth factor-I combination on
bone regeneration around titanium dental im-
plants. Results of a pilot study in beagle dogs.
Journal of Periodontology 62: 710–716.
Meyle, J., Gonzales, J.R., Bodeker, R.H., Hoffmann,
T., Richter, S., Heinz, B., Arjomand, M., Reich,
E., Sculean, A., Jepsen, K. & Jepsen, S. (2004) A
randomized clinical trial comparing enamel ma-
trix derivative and membrane treatment of buccal
class II furcation involvement in mandibular mo-
lars. Part II: secondary outcomes. Journal of
Periodontology 75: 1188–1195.
Murai, M., Sato, S., Koshi, R., Yokoyama, K., Ikeda,
K., Narukawa, M., Takayama, T., Yoshinuma, N.
& Ito, K. (2005) Effects of the enamel matrix
derivative and beta-tricalcium phosphate on bone
augmentation within a titanium cap in rabbit
calvarium. Journal of Oral Science 47: 209–217.
Nkenke, E., Radespiel-Troger, M., Wiltfang, J.,
Schultze-Mosgau, S., Winkler, G. & Neukam,
F.W. (2002) Morbidity of harvesting of retromolar
bone grafts: a prospective study. Clinical Oral
Implants Research 13: 514–521.
Nkenke, E., Schultze-Mosgau, S., Radespiel-Troger,
M., Kloss, F. & Neukam, F.W. (2001) Morbidity
of harvesting of chin grafts: a prospective study.
Clinical Oral Implants Research 12: 495–502.
Okamoto, K., Matsuura, T., Hosokawa, R. & Aka-
gawa, Y. (1998) RGD peptides regulate the spe-
cific adhesion scheme of osteoblasts to
hydroxyapatite but not to titanium. Journal of
Dental Research 77: 481–487.
Pierschbacher, M.D. & Ruoslahti, E. (1984) Cell
attachment activity of fibronectin can be dupli-
cated by small synthetic fragments of the mole-
cule. Nature 309: 30–33.
Sanz, M., Tonetti, M.S., Zabalegui, I., Sicilia, A.,
Blanco, J., Rebelo, H., Rasperini, G., Merli, M.,
Cortellini, P. & Suvan, J.E. (2004) Treatment of
intrabony defects with enamel matrix proteins or
barrier membranes: results from a multicenter
practice-based clinical trial. Journal of Perio-
dontology 75: 726–733.
Schaffner, P., Meyer, J., Dard, M., Wenz, R., Nies,
B., Verrier, S., Kessler, H. & Kantlehner, M.
(1999) Induced tissue integration of bone implants
by coating with bone selective RGD-peptides in
vitro and in vivo studies. Journal of materials
science. Materials in Medicine 10: 837–839.
Schenk, R. & Olah, A.J. (1980) Histomorphometrie.
In: Kuhlencordt, F. & Bartelheimer, H., eds.
Handbuch Der Inneren Medizin, 437–494. Ber-
lin: Springer.
Schenk, R.K., Olah, A.J. & Herrmann, W. (1984)
Preparation of calcified tissues for light micro-
scopy. In: Dickson, G.R., ed. Methods of Calci-
fied Tissue Preparation, 1–56. Amsterdam:
Elsevier.
Schliephake, H., Scharnweber, D., Dard, M., Sew-
ing, A., Aref, A. & Roessler, S. (2005) Functiona-
lization of dental implant surfaces using adhesion
molecules. Journal of Biomedical Materials Re-
search. Part B, Applied Biomaterials 73: 88–96.
Schwarz, F., Herten, M., Ferrari, D., Wieland, M.,
Schmitz, L., Engelhardt, E. & Becker, J. (2007)
Guided bone regeneration at dehiscence-type
defects using biphasic hydroxyapatiteþbeta
tricalcium phosphate (bone ceramic) or a
collagen-coated natural bone mineral (biooss
collagen): an immunohistochemical study in
dogs. The International Journal of Oral and
Maxillofacial Surgery 36: 1198–1206.
Schwarz, F., Rothamel, D., Herten, M., Sculean, A.,
Scherbaum, W. & Becker, J. (2004) Effect of
enamel matrix protein derivative on the attach-
ment, proliferation, and viability of human
SaOs(2) osteoblasts on titanium implants. Clin-
ical Oral Investigations 8: 165–171.
Sculean, A., Donos, N., Schwarz, F., Becker, J.,
Brecx, M. & Arweiler, N.B. (2004) Five-year
results following treatment of intrabony defects
with enamel matrix proteins and guided tissue
regeneration. Journal of Clinical Periodontology
31: 545–549.
Sigurdsson, T.J., Nygaard, L., Tatakis, D.N., Fu, E.,
Turek, T.J., Jin, L., Wozney, J.M. & Wikesjo,
U.M. (1996) Periodontal repair in dogs: evaluation
of rhBMP-2 carriers. International Journal
of Periodontics and Restorative Dentistry 16:
524–537.
Silvestri, M., Sartori, S., Rasperini, G., Ricci, G.,
Rota, C. & Cattaneo, V. (2003) Comparison of
infrabony defects treated with enamel matrix
derivative versus guided tissue regeneration with
a nonresorbable membrane. Journal of Clinical
Periodontology 30: 386–393.
Simmer, J.P. & Fincham, A.G. (1995) Molecular
mechanisms of dental enamel formation. Critical
Reviews in Oral Biology and Medicine 6:
84–108.
Tonetti, M.S., Lang, N.P., Cortellini, P., Suvan,
J.E., Adriaens, P., Dubravec, D., Fonzar, A., Four-
mousis, I., Mayfield, L., Rossi, R., Silvestri, M.,
Tiedemann, C., Topoll, H., Vangsted, T. & Wall-
kamm, B. (2002) Enamel matrix proteins in the
regenerative therapy of deep intrabony defects.
Journal of Clinical Periodontology 29: 317–325.
Traini, T., Valentini, P., Iezzi, G. & Piattelli, A.
(2007) A histologic and histomorphometric eva-
luation of anorganic bovine bone retrieved 9 years
after a sinus augmentation procedure. Journal of
Periodontology 78: 955–961.
Weibel, E.R. (1980) Stereological Methods: Practical
Methods for Biological Morphometry. New York:
Academic Press.
Zafiropoulos, G.G., Hoffmann, O., Kasaj, A., Will-
ershausen, B., Weiss, O. & Van Dyke, T.E. (2007)
Treatment of intrabony defects using guided tissue
regeneration and autogenous spongiosa alone or
combined with hydroxyapatite/beta-tricalcium
phosphate bone substitute or bovine-derived xe-
nograft. Journal of Periodontology 78: 2216–2225.
Schneider et al �Bone regeneration using a synthetic matrix and EMD
222 | Clin. Oral Impl. Res. 22, 2011 / 214–222 c� 2011 John Wiley & Sons A/S