BMI The Sloane Hospital - Care Quality Commission · BMI The Sloane Hospital Quality Report 125...
Transcript of BMI The Sloane Hospital - Care Quality Commission · BMI The Sloane Hospital Quality Report 125...

This report describes our judgement of the quality of care at this location. It is based on a combination of what wefound when we inspected and a review of all information available to CQC including information given to us frompatients, the public and other organisations
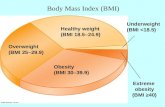
Ratings
Overall rating for this location Requires improvement –––
Are services safe? Good –––
Are services effective? Good –––
Are services caring? Good –––
Are services responsive? Requires improvement –––
Are services well-led? Requires improvement –––
Mental Health Act responsibilities and Mental Capacity Act and Deprivation of LibertySafeguardsWe include our assessment of the provider’s compliance with the Mental Capacity Act and, where relevant, MentalHealth Act in our overall inspection of the service.
We do not give a rating for Mental Capacity Act or Mental Health Act, however we do use our findings to determine theoverall rating for the service.
Further information about findings in relation to the Mental Capacity Act and Mental Health Act can be found later inthis report.
BMIBMI TheThe SloSloaneane HospitHospitalalQuality Report
125 Albemarle RoadBeckenhamKent BR3 5HSTel: 020 8466 4000Website: www.bmihealthcare.co.uk
Date of inspection visit: 2, 3 and 16 July 2019Date of publication: 11/10/2019
1 BMI The Sloane Hospital Quality Report 11/10/2019

Letter from the Chief Inspector of Hospitals
BMI The Sloane Hospital is operated by BMI Healthcare. The hospital has 32 beds spread over two wards. Facilitiesinclude two operating theatres and 12 consultant rooms in outpatients. There is a separate physiotherapy departmentconsisting of a gym, studio and five consulting rooms. The hospital provides surgery, medical care (endoscopy), servicesfor children and young people (from the age of three) and outpatients.
We inspected the hospital using our comprehensive inspection methodology. We carried out an unannouncedinspection between 2 - 3 &16 July 2019. Throughout the inspection, we took account of what people told us and howthe provider understood and complied with the Mental Capacity Act 2005.
The main service provided by this hospital was surgery. Where our findings on surgery, for example, managementarrangements, also apply to other services, we do not repeat the information but cross-refer to the surgery report. Wedid not rate medicine as endoscopy was the only service provided in medicine and it was managed within the hospital'ssurgical service, therefore the ratings have been integrated with the surgery ratings.
Following the inspection the hospital confirmed they had stopped providing services for children and young people.
Services we rate
Our rating of this hospital went down. We rated it as requires improvement overall because:
• Staff had not received training on how to care for children and young people.• The oversight and leadership of the service for children and young people was not sufficient or effective.• Children and young people were not always cared for in environments that were child friendly, risk assessed and met
their needs.• Managers did not monitor the effectiveness and performance of the endoscopy service.• Theatres did not have secure access to protect it from unauthorised access.
However:
• The hospital had made improvements since the last inspection in 2016. These included the installation of handhygiene sinks in patients' rooms and replacing carpets with wooden flooring that reduced the risk of infection.
• The hospital had systems for reporting, investigating and learning from incidents that occurred in the hospital andother BMI hospitals.
• The hospital provided mandatory training in key skills to all staff and made sure everyone completed it.• The hospital had effective systems to control the risk of infection and minimise the risk of harm to patients.• Staff had training in key skills, understood how to protect patients from abuse, and managed safety well.• The hospital used current evidence-based guidance and quality standards to plan the delivery of care and treatment
for patients. There were effective processes and systems in place to ensure guidelines and policies were updated andreflected best practice.
• Staff treated patients with compassion and kindness, respected their privacy and dignity, took account of theirindividual needs, and helped them understand their conditions. They provided emotional support to patients,families and carers.
• In all services people could access the service when they needed it and did not have to wait too long for treatment.• The hospital had improved engagement with patients and the community to plan and manage services.• Staff understood the service’s vision and values, and how to apply them in their work. Staff felt respected, supported
and valued.
Following this inspection, we told the provider that it should make improvements, even though a regulation had notbeen breached, to help the service improve.
Summary of findings
2 BMI The Sloane Hospital Quality Report 11/10/2019

Nigel AchesonDeputy Chief Inspector of Hospitals (London and South)
Summary of findings
3 BMI The Sloane Hospital Quality Report 11/10/2019

Our judgements about each of the main services
Service Rating Summary of each main service
Medical care(includingolderpeople'scare)
Medical services were a small proportion of thehospital activity. The main activity of the hospitalwas surgery.The endoscopy service was the main medicalservice and was integrated into operating theatreswhich is included in the surgery core servicereport. Where arrangements were the same wehave reported findings in the surgery report.We have not rated this service.
Surgery
Good –––
Surgery was the main activity of the hospital.Where our findings on surgery also apply to otherservices we do not repeat the information butcross refer to the surgery report. We rated thisservice as good overall because it was safe,effective, caring, responsive and well-led.
Services forchildren& youngpeople
Requires improvement –––
Services for children and young people were asmaller proportion of hospital activity.The main service provided for children and youngpeople was outpatient consultations andphysiotherapy. Surgery was only performed on 16and 17 year olds who met the criteria to follow theadult pathway.We rated this service as requiresimprovement overall because safe and effectivewere rated good, responsive was rated requiresimprovement and well-led inadequate. We did notrate caring as there were no children or youngpeople being treated on the days of the visit.
OutpatientsGood –––
We rated this service as good overall because itwas safe, caring, responsive and well-led. We donot rate effective in outpatients.
Summary of findings
4 BMI The Sloane Hospital Quality Report 11/10/2019

Contents
PageSummary of this inspectionBackground to BMI The Sloane Hospital 7
Our inspection team 7
Why we carried out this inspection 7
How we carried out this inspection 7
Information about BMI The Sloane Hospital 7
The five questions we ask about services and what we found 9
Detailed findings from this inspectionOverview of ratings 13
Outstanding practice 63
Areas for improvement 63
Summary of findings
5 BMI The Sloane Hospital Quality Report 11/10/2019

BMI The Sloane Hospital
Services we looked atMedical care, surgery, services for children and young people and outpatients.
BMITheSloaneHospital
Requires improvement –––
6 BMI The Sloane Hospital Quality Report 11/10/2019

Background to BMI The Sloane Hospital
BMI The Sloane Hospital is operated by BMIHealthcare. The hospital has been serving the localcommunity since 1981 when it was a nursing home and itbecame an acute hospital in 1982.
At the time of the inspection, a new executive directorhad recently been appointed and was going through theprocess to become the registered manager.
Our inspection team
The team that inspected the hospital comprised a CQCinspection manager, three CQC inspectors, an assistant
inspector, four specialist advisors with expertise insurgery, outpatients and children and young people. Theinspection team were overseen by Amanda Williams,Head of Hospital Inspection.
Why we carried out this inspection
We carried out this inspection as part of our independenthospital inspection programme. We followed up findingsfrom our 2016 inspection.
How we carried out this inspection
To get to the heart of patients’ experiences of care andtreatment, we ask the same five questions of all services:are they safe, effective, caring, responsive to people'sneeds, and well-led? Where we have a legal duty to do sowe rate services’ performance against each key questionas outstanding, good, requires improvement orinadequate.
During the inspection, we visited all wards and clinicalareas. We spoke with 31 staff including consultants anddoctors, managers, registered nurses, physiotherapists,pharmacists, hospital engineer, health care assistants,phlebotomy and administrative staff.
We also spoke with 12 patients and one relative. Inaddition, we observed three meetings; reviewed policyand procedure documents and 16 sets of patient records.
The hospital has been inspected once before in August2016 and was rated good.
Information about BMI The Sloane Hospital
The hospital has two wards and is registered to providethe following regulated activities:
• Diagnostic and screening procedures
• Surgical procedures
• Treatment of disease, disorder and injury
• Family planning services
Activity:
• In the reporting period, there were 662 inpatient and3,384 day-case episodes of care recorded at thehospital; of these 71% were privately funded and
Summaryofthisinspection
Summary of this inspection
7 BMI The Sloane Hospital Quality Report 11/10/2019

29% were NHS funded. Sixteen of the day cases wereyoung people aged 16-17. Only young people aged16-17 who meet the criteria to follow the adultpathway are admitted for invasive procedures.
• There were 32,000 outpatient total attendances inthe reporting period of which 84% were privatelyfunded and 16% NHS-funded. The children andyoung people service was a small proportion of thehospital’s activity. It accounted for 553 of 32,000attendances in the last year (March 2018 to February2019). Of these, 360 were aged between aged 3-15years and 193 were aged 16-17.
• There were 218 doctors who worked at the hospitalunder practising privileges including surgeons,anaesthetists and physicians. In addition, there werethree regular resident medical officers (RMOs) whoworked on a weekly rota. The hospitalemployed over 70 other staff, including 26 registerednurses and six care assistants and operatingdepartment practitioners (ODPs) as well as havingits own bank staff. The accountable officer forcontrolled drugs (CDs) was the executive director.
Track record on safety:
• No Never Events• One serious incident• No incidences of hospital acquired Meticillin-resistant
Staphylococcus aureus (MRSA)• No incidences of hospital acquired Meticillin-sensitive
staphylococcus aureus (MSSA)• No incidences of hospital acquired Clostridium difficile
(C. diff)• No incidences of hospital acquired Escherichia coli (E.
coli)
Services provided at the hospital under service levelagreement:
• Clinical and or non-clinical waste removal• Interpreting services• Grounds Maintenance• Laser protection service• Laundry• Maintenance of medical equipment• Pathology and histology• Residential medical officer (RMO) provision• GP service• Diagnostic imaging• Catering Services• Nurse Agency Provision
Summaryofthisinspection
Summary of this inspection
8 BMI The Sloane Hospital Quality Report 11/10/2019

The five questions we ask about services and what we found
We always ask the following five questions of services.
Are services safe?Our rating of safe remained the same. We rated safeas good because:
• Outpatients and surgery had enough staff with the rightqualifications, skills, training and experience to keep peoplesafe from avoidable harm and to provide the right care andtreatment.
• The service provided mandatory training in key skills to all staffand made sure everyone completed it.
• The service controlled infection risk well. Staff kept equipmentand the premises clean. They used control measures to preventthe spread of infection.
• Staff understood how to protect patients from abuse, and theservice worked well with other agencies to do so. Staff hadtraining on how to recognise and report abuse and they knewthe staff to contact for support.
• The service used systems and processes to safely prescribe,administer, record and store medicines.
• Staff kept detailed records of patients’ care and treatment.Records were clear, up-to-date and easily available to all staffproviding care.
• The hospital managed most patient safety incidents well. Staffrecognised some incidents and reported them appropriately.Managers investigated incidents and shared lessons learnedwith the whole team and the wider service. When things wentwrong, staff apologised and gave patients honest informationand suitable support.
However, we also found:
• In services for children and young people some risks inoutpatients had not been recognised and action taken tominimise them.
• The hospital did not have a service level agreement (SLA) withthe local NHS trust for transfers out in an emergency or if apatient’s condition deteriorated.
• The entrance to theatres was not secure to preventunauthorised access.
Good –––
Are services effective?Our rating of effective remained the same. We rated effectiveas good because:
Good –––
Summaryofthisinspection
Summary of this inspection
9 BMI The Sloane Hospital Quality Report 11/10/2019

• The majority of services provided care and treatment based onnational guidance and evidence-based practice.
• Staff assessed and monitored patients regularly to see if theywere in pain and gave pain relief in a timely way.
• In surgery, staff monitored the effectiveness of care andtreatment. They used the findings to make improvements andachieved good outcomes for patients.
• Staff followed national guidelines to make sure patients fastingbefore surgery were not without food for long periods
• Doctors, nurses and other healthcare professionals workedtogether as a team to benefit patients. They supported eachother to provide good care.
• Services had been adapted to meet the needs of patients andwere open in the evenings and weekend.
• Staff supported patients to make informed decisions abouttheir care and treatment. They followed national guidance togain patients’ consent.
However, we also found:
• Staff had not received any additional training to care forchildren and young people.
• There were no leaflets available aimed at children or youngpeople to promote healthy lifestyles.
Are services caring?We rated caring as good because:
• Staff treated patients with compassion and kindness, respectedtheir privacy and dignity, and took account of their individualneeds.
• Staff provided emotional support to patients, families andcarers to minimise their distress. They understood patients’personal, cultural and religious needs.
• Staff supported and involved patients, families and carers tounderstand their condition and make decisions about theircare and treatment.
Good –––
Are services responsive?Our rating of responsive went down. We rated responsiveas requires improvement because:
• The environment had not been adapted to meet the needs ofchildren and young people. In the outpatient clinic area therewere no toys.
• The hospital's complaints information had not been adjustedto meet the needs of children and young people.
However:
Requires improvement –––
Summaryofthisinspection
Summary of this inspection
10 BMI The Sloane Hospital Quality Report 11/10/2019

• The hospital planned and provided care in a way that met theneeds of many of the local people and the communities served.It also worked with others in the wider system and localorganisations to plan care.
• Staff made reasonable adjustments to help patients accessservices. They coordinated care with other services andproviders.
• People could access the service when they needed it andreceived the right care promptly. Waiting times from referral totreatment and arrangements to admit, treat and dischargepatients were in line with national standards.
• It was easy for adults to give feedback and raise concerns aboutcare received. The service treated concerns and complaintsseriously, investigated them and shared lessons learned with allstaff.
Are services well-led?Our rating of well-led went down. We rated well-led as requiresimprovement because:
• The day to day oversight and leadership of the service forchildren and young people was insufficient and ineffective.
• Information about the performance and quality and safety ofthe service for children and young people was not routinelycollected and discussed.
• The hospital did not have vision or strategy for the service forchildren and young people.
• The service for children and young were not a separate agendaitem at key quality and safety meetings.
• The issues we found in the service for children and youngpeople were not recorded on the risk register.
However:
• In surgery and outpatients, leaders had the skills and abilities torun the service. They understood and managed the prioritiesand issues the service faced. They were visible andapproachable in the service for patients and staff. Theysupported staff to develop their skills and take on more seniorroles.
• The hospital had a vision for what it wanted to achieve for mostservices and was developing its strategy to turn it into actionand involving all relevant stakeholders.
Requires improvement –––
Summaryofthisinspection
Summary of this inspection
11 BMI The Sloane Hospital Quality Report 11/10/2019

• In surgery and outpatients leaders operated effectivegovernance processes, throughout the service and with partnerorganisations. Staff at all levels were clear about their roles andaccountabilities and had regular opportunities to meet, discussand learn from the performance of the service.
• In endoscopy, effective governance processes were beingdeveloped and implemented.
• Leaders and staff actively and openly engaged with patients,staff, the public and local organisations to plan and manageservices. They collaborated with partner organisations to helpimprove services for patients.
Summaryofthisinspection
Summary of this inspection
12 BMI The Sloane Hospital Quality Report 11/10/2019

Overview of ratings
Our ratings for this location are:
Safe Effective Caring Responsive Well-led Overall
Medical care(including olderpeople's care)
N/A N/A N/A N/A N/A N/A
Surgery Good Good Good Good Good Good
Services for children &young people Good Good Not rated Requires
improvement Inadequate Requiresimprovement
Outpatients Good N/A Good Good Good Good
Overall Good Good Good Requiresimprovement
Requiresimprovement
Requiresimprovement
Notes
Detailed findings from this inspection
13 BMI The Sloane Hospital Quality Report 11/10/2019

Safe
EffectiveCaringResponsiveWell-led
Information about the serviceEndoscopy was the only medical service provided by thehospital. It was provided in theatres and integrated into thetheatre operating schedules. The main service provided bythis hospital was surgery. Where our findings on surgery–for example, management arrangements also apply toother services, we do not repeat the information butcross-refer to the surgery section.
The endoscopy unit is opened five days a week. Proceduresundertaken in the unit include gastroscopy, colonoscopy,oesophageal dilatation, prostatic biopsy and flexiblecystoscopy and bronchoscopy and video capsule. Duringthe inspection, we saw that majority of patients seen inendoscopy came for diagnostic colonoscopy or flexiblesigmoidoscopy. For the period Mach 2018 - February 20191,069 procedures were carried out at the hospital.
As endoscopy was under the management of theatreswhich is included in the surgery report we have not ratedmedical care.
Are medical care (including olderpeople's care) safe?
We did not rate this domain.
Mandatory training
The service provided mandatory training in key skills to allstaff and made sure everyone completed it.
• As of July 2019, compliance with mandatory training fortheatre clinical staff was 92.2% and for ward nursingstaff was 94.8%. This was above the corporatemandatory training target of 90% compliance for thistraining.
• Consultants and clinicians with practising privilegeswere not required to complete training using thehospital system but, assurance of mandatory trainingwas checked by the medical advisory committee.
For more information please see the surgery core servicereport.
Safeguarding
Staff understood how to protect patients from abuse andthe service worked well with other agencies to do so.
• Information provided by the hospital showed that94.7%% of theatre staff had completed safeguardingadults level one, 68.4% had completed level two and100% of staff had completed level 3. In theatres 100% ofstaff had completed safeguarding children level one,78.9% had completed level two and 100% of staff hadcompleted level three.
• On the ward 100% of nursing staff on the wards hadcompleted safeguarding adults level one, 95.6% hadcompleted level two and 100% of staff had completedlevel three. One hundred per cent of ward staff had alsocompleted safeguarding children level one, 95.6% hadcompleted level two and 100% of staff had completedlevel three.
For more information please see the surgery core servicereport.
Cleanliness, infection control and hygiene
The service controlled infection risk well. The service usedsystems to identify and prevent surgical site infections.They kept equipment and the premises visibly clean.
• Decontamination of endoscopy instruments took placeoff site by a fully accredited facility; accredited to ISO9001:2008, ISO 13485:2012, and compliant with MDD93/42 EEC through a bespoke Quality Management System.
Medicalcare(includingolderpeople'scare)
Medical care (including olderpeople's care)
14 BMI The Sloane Hospital Quality Report 11/10/2019

• All instruments were packed in sealed cases followinguse and sent for decontamination off site. They were‘tracked and traced’ daily through a register ofinstruments. On receipt of clean scopes the serialnumber for each scope was logged and then allocatedto a patient. This was noted and recorded on the teambrief. Staff followed the pathway for the management ofendoscopes.
• The theatres and patient rooms we visited were visiblyclean. Daily cleaning schedules in the theatres andwards were in place. We saw the daily cleaningschedules were generally up to date and signed.
For more information please see the surgery core servicereport.
Environment and equipment
The design, maintenance and use of facilities, premisesand equipment kept people safe. Staff were trained to usethem.
• The theatre department consisted of two main theatres,one of which had laminar flow, an anaesthetic room anda three bedded recovery bay. Endoscopy was carriedout in one of the main theatres.
• Resuscitation trolleys were located on the wards and inthe theatre. On the wards we saw there were some gapsin the daily checks and trolleys were within easy accessfor staff. The stock was checked, and all items were indate. In theatres the resuscitation trolley was completewith daily checks and all drugs in date. There was adefibrillator, suction and oxygen all available andworking.
For more information please see the surgery core servicereport.
Assessing and responding to patient risk
Staff completed and updated risk assessments for eachpatient and removed or minimised risks.
• In line with theatres, endoscopy staff used the WorldHealth Organisation (WHO) 5 steps to safer surgery,surgical checklist, which was designed to preventavoidable mistakes. This included checks such aspatient identify, allergies and ensuring the consent formhad been signed. The 5 steps to safer surgery checklistwas audited monthly, including endoscopy, and wereviewed the audits for December 2018, January andFebruary 2019 and saw that they were 100% compliant.
• It was hospital policy that consultants were required tobe available to attend emergencies within 30 minutes.
• The theatre department had an out of hours on callteam which included an anaesthetist who was availableto deal with emergency surgery.
• The hospital had a procedure and equipment formanaging a suspected gastrointestinal bleed and staffwere aware of it.
• All endoscopy patients were triaged using apre-admission medical screening tool. It covered keysafety areas such as venous thromboembolism (VTE),pressure areas, nutrition, pain were completed usingnational risk assessment tools.
• The hospital did not have a service level agreement totransfer acutely unwell patients to a local NHS trust.However, there was a standard operating procedure(SOP) for critically ill transfer; If a patient needed to betransferred urgently staff were to call 999 for anambulance.
For more information please see the surgery core servicereport.
Nurse staffing
The service was in the process of recruiting nursing andsupport staff with the right qualifications, skills, trainingand experience to keep patients safe from avoidable harmand to provide the right care and treatment.
• The hospital had experienced difficulties recruitingstaff for theatres, including endoscopy, and at time ofthe inspection a dedicated health care support workerand a bank nurse were covering endoscopy.
For more information please see the surgery core servicereport.
Medical staffing
The service had enough medical staff with the rightqualifications, skills, training and experience to keeppatients safe from avoidable harm and to provide the rightcare and treatment.
• We saw a list of consultants who carried out endoscopyprocedures and the hospital had a lead consultant forthe service.
• The RMO provided a 24-hour 7 day a week service on athree-week rotational basis. All RMOs were selected
Medicalcare(includingolderpeople'scare)
Medical care (including olderpeople's care)
15 BMI The Sloane Hospital Quality Report 11/10/2019

specifically to enable them to manage a varied patientcaseload and requirements. The RMOs were providedunder contract with an external agency that providedtraining and support.
For more information please see the surgery core servicereport.
Records
Staff kept detailed records of patients’ care and treatment.Records were clear, up-to-date, stored securely and easilyavailable to all staff providing care.
• Records we reviewed were complete and up to date,they were a mix of paper and electronic. They includethe pre-assessment formed part of the patient record.
• All records were stored securely, and computers werelocked when not in use.
For more information please see the surgery core servicereport.
Medicines
The service used systems and processes to safely prescribe,administer, record and store medicines.
• We saw that all medicines in the theatre departmentwere stored securely in locked trolleys, cupboards andfridges with stock medications stored in lockedcupboards in the key code locked clinical room.
For more information please see the surgery core servicereport.
Incidents
The service managed patient safety incidents well. Staffrecognised and reported incidents and near misses.
• Between February 2018 and end of March 2019 therewere 12 incidents related to endoscopy. There were noserious incidents or Never Events. The majority of theincidents were related to communication and we couldsee action had been taken in response to them.
• We saw learning from incidents was shared at the dailycomm cell meetings. Information we reviewed showedthat learning from never events at other BMI hospitalshad been shared with all theatre staff.
Safety Thermometer (or equivalent)
The service used monitoring results to improve safety.
• During the reporting period March 2018 to March 2019hospital data showed the service was 100% harm free,with no pressure ulcer, no catheter or urinary tractinfections or venous thromboembolism episodes andno patient falls.
Are medical care (including olderpeople's care) effective?
We did not rate this domain.
The service was developing policies and procedures toensure care and treatment was based on national guidanceand evidence-based practice. Managers checked to makesure staff followed guidance.
• The hospital’s draft local endoscopy standardoperational procedure (SOP) was informed by a range ofnational guidance including the joint advisory group(JAG) accreditation standards, the 'BritishGastroenterology Society Quality and Safety Standards'and 'HTM01 06: Decontamination of Flexibleendoscopes'.
• The endoscopy service did not have JAG accreditationbut, was working towards achieving it. The ‘JAGreadiness site visit report’ in January 2019 identifiedactions that needed to be completed. An action planhad been developed in response to the report and wewere provided with an update of the actions. We sawthat many of them were in progress with some actionsalready completed.
Nutrition and hydration
Staff followed national guidelines to make sure patientsfasting before surgery were not without food for longperiods.
• Depending on the type of procedure, patients weregiven written specific instructions for preparation fortreatment including diet and fluids. For examplepatients undergoing colonoscopy were given writteninstructions about diet restriction and bowelpreparation.
• Information about fluids and diet was included in thedraft endoscopy standard operating procedure (SOP).
Pain relief
Staff assessed and monitored patients regularly to see ifthey were in pain and gave pain relief in a timely way.
Medicalcare(includingolderpeople'scare)
Medical care (including olderpeople's care)
16 BMI The Sloane Hospital Quality Report 11/10/2019

• We were told, and it was documented in the hospital’sdraft local endoscopy operational standard operationalprocedure that patients were offered a choice of topicalanaesthetic (throat spray), analgesia or intravenoussedation/analgesia, where clinically appropriate.
• Outpatients kept a stock of pain-relieving medication,such as paracetamol. Should stronger medication berequired, the patient was referred to their own GP or thein-house service. In more urgent cases, the consultant inclinic or RMO could write a prescription is stronger painrelief was required.
Competent staff
The hospital provided evidence that staff working inendoscopy were competent to carry out their role.
• During the inspection the we were told staff had notreceived any specific training on endoscopy and they'learnt on the job' However, following the inspection thehospital provided evidence of completed competencyforms for staff.
• All consultants working with the hospital had practisingprivileges which required consultants to have an up todate General Medical Council (GMC) registration,evidence of indemnity insurance and revalidationcertificate. These were reviewed and highlighted atMedical Advisory Committee (MAC) meetings.
• Consultants only performed surgical procedures whichthey undertook in the NHS. As all the consultants heldNHS contracts they maintained their skills by working intheir trust and had their appraisals completed by theirNHS Medical Director.
• The service had a lead consultant who chaired theendoscopy user group. We were provided with a list ofconsultants and the specific endoscopic proceduresthey carried out.
Multidisciplinary working
Doctors, nurses and other healthcare professionals workedtogether as a team to benefit patients.
• We observed good working relationships betweendoctors and nurses and different staff groups intheatres.
For more information please see the surgery core service.
Seven-day services
Key services were available seven days a week to supporttimely patient care.
• Theatres ran from Monday -Saturday 7.30 am - 9.00 pm,with the evening session commencing at 5.30 pm. Theyoccasionally over-ran.
• The resident medical officer was available 24-hours,seven days a week.
For more information please see the surgery core servicereport.
Health promotion
Staff gave patients practical support and advice to leadhealthier lives.
• In pre-assessment patients had access to a variety ofleaflets which included smoking cessation, alcoholdependency, and venous thromboembolism (VTE) anda guide to pain control.
Consent, Mental Capacity Act and Deprivation ofLiberty Safeguards
Staff supported patients to make informed decisions abouttheir care and treatment. They followed national guidanceto gain patients’ consent.
• Consent training was included within the mandatorytraining and both theatre and ward staff were 100%compliant. The hospital told us that training in theMental Capacity Act 2005 and Deprivation of LibertiesSafeguards (DoLS) was included in safeguardingvulnerable adults level 2 training.
• We are aware of one incident in endoscopy where apatient had been through pre-assessment but, whenthey arrived for their procedure it was clear they didn’tunderstand why they were there and did not havecapacity to consent. Staff recognised this and tookappropriate action to cancel the procedure and arrangefor it to take place in a hospital that could meet theirneeds.
Are medical care (including olderpeople's care) caring?
We did not rate this domain.
Compassionate care
Medicalcare(includingolderpeople'scare)
Medical care (including olderpeople's care)
17 BMI The Sloane Hospital Quality Report 11/10/2019

Staff treated patients with compassion and kindness,respected their privacy and dignity, and took account oftheir individual needs.
• Patients’ privacy and dignity was maintained during theprocedure. Depending on the procedure patients weregiven either a gown and shorts to wear and did notchange out of their clothes until necessary.
• The hospital used the Family and Friends survey but, itwas anonymous, and they were unable to extractfeedback specific to the endoscopy service.
For more information please see the surgery core servicereport.
Emotional support
Staff provided emotional support to patients to minimisetheir distress.
• In theatres all staff were observed to treat patients withdignity and respect. Staff made sure patients werecomfortable and had the opportunity to voice anyconcerns.
For more information please see the surgery core servicereport.
Understanding and involvement of patients and thoseclose to them
Staff involved patients, and those close to them indecisions about their care and treatment.
• We observed staff give explanations to patient who werewaiting for endoscopy procedures.
• Information about fees was available but limited. In theminutes of the March 2019 Medical Advisory Committeethere was reference to the costs of procedures beingmade more transparent to patients who were self-funding.
For more information please see the surgery core servicereport.
Are medical care (including olderpeople's care) responsive?
We did not rate this domain.
Service delivery to meet the needs of local people
The service planned and provided care in a way that metthe needs of local people.
• The service worked with their stakeholders such as theircommissioners in the planning and development of theservice.
• The endoscopy was integrated into theatres andpatients were cared for in the same areas as otherpatients undergoing surgical procedures.
• All patients’ rooms were single en-suite and there wereno restricted visiting times for patients and endoscopiclists for male and females were done separately.
• The endoscopy unit did not have Joint Advisory Groupon gastrointestinal endoscopy (JAG) accreditation but,was working towards achieving it.
Meeting people’s individual needs
The service took account of patients’ individual needs andpreferences.
• Staff told us they rarely had vulnerable patients usingthe service. However, staff had received training on howto care for patients living with dementia and it was partof the pre-assessment to carry out dementiaassessment on all patients over 65, with or without adiagnosis of dementia.
• The service had separate lists for women and men toensure their privacy was not compromised.
• The hospital had an open visiting policy, this meantfamily and friends could provide support andassistance.
• The hospital had a chaperone policy in place andnotices encouraging patients to ask for a chaperonewere visible on the wards. Chaperone training wasavailable through a BMI e-learning package.
Access and flow
People could access the service when they needed it andreceived the right care promptly.
• The hospital told us there were no delays in accessingthe service for patients who were insured or privatelyfunded. For NHS-funded patients they were meeting thereferral to treatment times.
• Between January 2018 – January 2019 eight procedureswere cancelled. Five of these were related to medicalreasons, two were patient choice and one was due tothe patient not receiving the information about theiradmission date.
Medicalcare(includingolderpeople'scare)
Medical care (including olderpeople's care)
18 BMI The Sloane Hospital Quality Report 11/10/2019

Learning from complaints and concerns
It was easy for people to give feedback and raise concernsabout care received. The service treated concerns andcomplaints seriously, investigated them and shared lessonslearned with all staff.
• Information was available the BMI leaflet 'How did wedo today?' to inform patients, relative and visitors onhow they could raise any concerns.
• Between January 2018 - January 2019 there were twocomplaints about the service. The complaints wereabout communication and we could see action hadbeen taken in relation to one but action in relation tothe second one had not been recorded.
Are medical care (including olderpeople's care) well-led?
We did not rate this domain.
Leadership
Clinical leaders in post understood and managed thepriorities and issues the service faced.
• The senior management team were supported by fiveclinical services managers which included theatres andthe wards. The theatre manager, who had recently takenup the post and had been with the hospital for less thansix months at the time of the inspection, had oversightof the endoscopy service. There was a lead consultantfor the service.
• During the inspection we were told the hospital hadrecently recruited a lead scrub nurse and it was plannedthat they would take on the day to day management ofthe service. Following the inspection the hospitalconfirmed they had a lead endoscopy nurse in post.
Vision and strategy
The service had a vision for what it wanted to achieve and astrategy to turn it into action. The vision and strategy werefocused on sustainability of services.
• The hospital is part of BMI Healthcare. The hospital’svision and strategy were driven by BMI Healthcare whichwas to ‘offer the best patient experience and bestoutcomes in the most cost-effective way from ourcomprehensive UK network of acute care hospitals”.
• The hospital had a five-year vision for 2015 to 2020which was achieved through their eight strategicobjectives and priorities.
• The strategy for the endoscopy service was evolving.The executive director told us that the longer-term planfor the service was to have an independent endoscopysuite situated on the ambulatory care ward. This wouldenable the service to expand in terms of numbers andfree up theatre time for other surgical procedures. Thevision was reflected in the notes of the endoscopy user’sgroup minutes June 2019.
Culture
Staff felt respected, supported and valued. The serviceprovided opportunities for development. The service hadan open culture.
• All staff we spoke with described the hospital as‘friendly’ and like a ‘family’.
• The theatre manager and the wards manager workedclinically and were proud of their staff and department.
• Staff told us the executive team were visible andapproachable and they felt listened to by the seniorteam.
Governance
The service governance processes were evolving.Substantive nursing staff were learning about their role andresponsibilities.
• The hospital had a clinical governance committee whichwas responsible for clinical oversight of patient safetyissues, incidents, complaints, risk register and audits.
• The endoscopy user group was relatively new, it metquarterly and was still evolving. The purpose of thegroup was ‘To ensure the unit’s Endoscopy Service fullycomplies with BMI`s policies, the British Society ofGastroenterology (BSG) quality and safety standardsand other statutory and regulatory requirements; and toprovide a coordinated approach to service delivery andservice development.’ The group fed into the clinicalgovernance committee.
• The lead consultant chaired the meeting and workforce,environment and facilities, and JAG accreditation werediscussed.
For more information please see the surgery core servicereport.
Managing risks, issues and performance
Medicalcare(includingolderpeople'scare)
Medical care (including olderpeople's care)
19 BMI The Sloane Hospital Quality Report 11/10/2019

The service used systems to manage performance. Theyidentified and escalated some of the relevant risks andissues and identified actions to reduce their impact.
• The risk register contained one risk related toendoscopy; light bulbs exceeding their hours of safeusage which had been resolved. Some of the potentialrisks such as not having a dedicated manager and staffnot having training were not included on the register.
• The hospital had some mechanisms to monitorperformance. However, the June 2019 minutes of theendoscopy user group indicated that consultants werenot regularly submitting their data and only one audithad been carried out.
• Incidents and complaints about the service werereviewed at the Medical Advisory Committee (MAC) aspart of the governance report. The governance reportwas a standing agenda items and we could see evidenceof reference to endoscopy in the reports.
• Daily issues about the service were discussed at thedaily comm cell meetings. The daily comms cellmeetings were held Monday to Friday and wereattended by representatives for each department. Themeeting covered a range of subjects including riskreview, recent incidents, health and safety update,training compliance review, and any concerns thataffected the hospital. This was cascaded to staff, so theygained a wider view of risk, issues and generalperformance within the hospital.
• The hospital’s monthly bulletin included informationabout changes in legislation, NICE guidance, andMedicines & Healthcare Products Regulatory Agency(MHRA) alerts.
Managing information
The service collected reliable data and analysed it. Data ornotifications were submitted to external organisations asrequired.
• During the inspection we observed staff treated patientidentifiable information in line with the General DataProtection Regulations (GDPR).
• Staff had secure access to the hospital’s intranet whichgave them access to a range of policies, procedures andguidance and their training and personal developmentrecords.
• Consultants had access to a BMI ‘Consultant App’ whichgave them remote login to clinics and theatre lists on asmartphone. The app enabled consultants to accessclinic and operating theatre data. The application wasdownloaded using BMI credentials. No data was storedon the phone and a time out was applied for security.
Engagement
The service engaged with patients and staff.
• There was effective engagement with staff through arange of mechanisms including ‘Sloane says’ a staff onlymeeting and the ED open forum.
• Since the last inspection the hospital had introducedpatient journey meetings to aid communication,teamwork and collaboration across all departments toidentify how to improve the service provided to patients.The meeting had representatives from all departmentsand a patient representative attending the bi monthlymeetings.
Medicalcare(includingolderpeople'scare)
Medical care (including olderpeople's care)
20 BMI The Sloane Hospital Quality Report 11/10/2019

Safe Good –––
Effective Good –––
Caring Good –––
Responsive Good –––
Well-led Good –––
Information about the serviceThe main service provided by this hospital was surgery.Where our findings on, for example, managementarrangements also apply to other services, we do notrepeat the information but cross-refer to the surgerysection.
In this section we cover the hospital’s arrangements fordealing with risks that might affect its ability to provideservices (such as staffing problems, power cuts, fire andflood) in the overall safety section and the informationapplies to all services unless we mention an exception.
The hospital is registered for 32 inpatient beds, all weresingle rooms with 30 rooms providing en-suite facilitiesacross two wards:
• Cator ward had 16 rooms for inpatient and day casepatients
• Langley ward had 12 rooms which could accommodateinpatient and day case patients. Two rooms had beenre-designated for ambulatory care patients which couldaccommodate six patients and a room had been setaside for meeting with ambulatory patients.
As part of the inspection of surgical services we inspectedCator and Langley wards. However, Langley Ward wasclosed on the first day of the inspection as it was beingrefurbished. On the second day of the inspections threerooms were used for day patients.
The hospital does not have critical care facilities. In anemergency, the hospital transfers patients to a nearby NHStrust.
The surgical service had two operating theatres, one withlaminar flow (a system of circulating filtered air to reduce
the risk of airborne contamination). In addition, there weretwo anaesthetic rooms and a three-bay recovery. Thedepartment operated Monday to Saturday between 7.30am and 9.00 pm.
The inpatient and day-case activity for the period March2018 to February 2019 comprised both privately fundedand NHS-funded patients.
Inpatient activity was 72.5% (480) privately funded and27.5% (182) NHS-funded patients. Day case activity was71% (2,399) privately funded and 29% (985) NHS-fundedpatients.
During the period March 2018 to February 2019 there were662 inpatient and 3,384 day case patients.
Are surgery services safe?
Good –––
Our rating of safe stayed the same. We rated it as good.
Mandatory training
The service provided mandatory training in key skills to allstaff and made sure everyone completed it.
• As of July 2019, compliance with mandatory training fortheatre clinical staff was 92.2% and for ward nursingstaff was 94.8%. This was higher than the corporatemandatory training policy which states a target of 90%compliance for this training.
• As of February 2019, compliance with mandatorytraining for staff working across the whole hospital was90.7%. This was similar to the corporate mandatorytraining policy states a target of 90% compliance for thistraining.
Surgery
Surgery
Good –––
21 BMI The Sloane Hospital Quality Report 11/10/2019

• The hospital had a corporate mandatory trainingprogramme, which included but was not limited totopics such as infection prevention and control, movingand handling, fire safety, conflict resolution, health andsafety, and information governance. The mandatorytraining matrix identified the mandatory trainingrequired dependant on job role.
• The resident medical officers (RMOs) received theirmandatory training from their agency and were notallowed to work at the hospital unless this had beencompleted.
• The RMOs, the Director of Clinical Services, resus leadand ward sister were trained in advanced life support(ALS). Other clinical staff were trained in immediate lifesupport (ILS) or adult basis life support.
• Staff told us they completed training through thecorporate learning system ‘BMI Learn’; which was anonline resource of training modules, e-learning courses,and some face-to-face sessions.
• Staff could view their individual training needs, currentcompliance and access e-learning courses through thehospital’s electronic training system. The system alsoalerted both managers and staff when mandatorytraining was due to be completed.
• Staff we spoke with told us they were up-to-date withmost of the statutory and mandatory training.
Safeguarding
Staff understood how to protect patients from abuse andthe service worked well with other agencies to do so. Staffhad training on how to recognise and report abuse andthey knew how to apply it.
• The service had a corporate safeguarding adults’ policywhich incorporated Mental Capacity, Deprivation ofLiberty Safeguards (DoLS) and PREVENT advice. Thepolicy included what action staff should take if they hadconcerns a patient had undergone female genitalmutilation (FGM). At the time of the inspection the policywas under review. The policy had been due for review inNovember 2018. The hospital also had a standardoperating procedure (SOP) for safeguarding adults andsafeguarding children which was due for review in June2020. Staff had access to the hospitals safeguardingpolicy’s for children and adults via the hospitals intranet.
Following our inspection, the hospital advised that theBMI Safeguarding adults policy was reviewed andupdated in June 2019 and circulated to staff in July2019.
• Safeguarding adults and children was part of themandatory training programme for staff and differentlevels of training were provided according to the jobrole. Nursing staff we spoke with told us theirsafeguarding training was up to date. Data provided bythe hospital showed that 94.7%% of theatre staff hadcompleted safeguarding adults level one, 68.4% hadcompleted level two and 100% of staff had completedlevel 3. A 100% of theatre staff had completedsafeguarding children level one, 78.9% had completedlevel two and 100% of staff had completed level three. A100% of nursing staff on the wards had completedsafeguarding adults’ level one, 95.6% had completedlevel two and 100% of staff had completed level three. A100% of ward staff had also completed safeguardingchildren level one, 95.6% had completed level two and100% of staff had completed level three.
• The director of clinical services (DCS) was the hospitalsafeguarding lead for vulnerable adults and childrenand trained to level three. Staff also had access to theBMI regional safeguarding lead who was trained to levelfour.
• Staff we spoke with had a good understanding of theirresponsibilities in relation to safeguarding of vulnerableadults and children and could explain how to respondto and escalate a concern or make a referral.
• Safeguarding information and contact numbers weredisplayed as a reminder and easy access for staff on thewards.
• The hospital reported no safeguarding concerns duringthe period March 2018 to March 2019.
Cleanliness, infection control and hygiene
The service controlled infection risk well. The service usedsystems to identify and prevent surgical site infections.They kept equipment and the premises visibly clean
• At the last inspection we had concerns there were nohand hygiene sinks in patients’ rooms and Langley wardhad carpet flooring which posed a risk for infectioncontrol. On this occasion we found the situation had
Surgery
Surgery
Good –––
22 BMI The Sloane Hospital Quality Report 11/10/2019

improved. Hand hygiene sinks had been installed inCator ward and were in the process of being installed inLangley ward. Laminate flooring had been installed onLangley ward.
• The theatres and patient rooms we visited were visiblyclean. However, we did observe a staff member carryingdirty linen through the ward. We observed domesticstaff cleaning throughout the day and undertaking thisin a methodical and unobtrusive way. Daily cleaningschedules in the theatres and wards were in place. Wesaw the daily cleaning schedules were generally up todate and signed.
• Staff followed the hospital’s policy and were bare belowthe elbow and used personal protective equipment(PPE). All patient rooms on Cator ward had sinks andsoap, anti-bacterial gels were available on Langley ward.There were hand washing facilities in the theatres whichincluded the anaesthetic rooms, theatres and recoverybays.
• The hospital had an identified an infection preventionand control lead (IPC) and we attended the IPC linkmeeting during the inspection which had representationfrom different departments across the hospitalincluding the wards and theatre.
• Observational hand hygiene audits for March 2019demonstrated a compliance of 100% in the theatres andon the wards.
• The hospital undertook monthly departmental healthand safety checks and infection prevention and controlaudits to minimise the risk of the spread of infection toand between patients.
• The hospital reported no incidents of surgical siteinfections in the 12 month period January 2018 toDecember 2018.
• The hospital reported no incidents of MRSA, MSSA, CDifficle or E. Coli in the 12-month period January 2018 toDecember 2018.
• Patients were screened for Meticillin-ResistantStaphylococcus Aureus (MRSA) on routinely if they had ahospital admission in the last 18 months or had MRSA inthe past as part of their pre-operative assessment.
• Patient led assessments of the care environment(PLACE) 2018 for cleanliness was 99.8% which wasbetter than the BMI Healthcare average 98.8%. PLACE isan annual assessment of the non- clinical aspects of thepatient environment.
Environment and equipment
The design, maintenance and use of facilities, premisesand equipment kept people safe. Staff were trained to usethem.
• The theatre department consisted of two main theatres,one of which had laminar flow, an anaesthetic room anda three bedded recovery bay. The entrance to thetheatre department was through the main corridorwhich could be easily accessed as there was noelectronic card swipe access to the theatre to preventunauthorised access. This was raised at the time of theinspection. The hospital advised they were installingelectronic card swipe access to two sets of doors, oneset of double doors in main corridor situated beforetheatre department an on the main theatre departmentdoors. This would provide enhanced security for theboth hospital ward areas and the theatre department.The installation lead time was booked and was plannedto be completed in the 1st week of August 2019.Arrangements were put into immediate effect to ensurethe theatre reception was staffed from 8.00 am untiltheatre closed with the theatre administration assistantand porters to maintain a security checking presence.Whilst lack of a secure entrance to the hospital hadbeen identified on the risk register, the risk tounauthorised access to the theatres was not identifiedon the risk register.
• The inpatient wards consisted of two wards. Cator wardhad 16 rooms for inpatient and day case patients.Langley ward had 12 rooms which could accommodateinpatient and day case patients. Two rooms had beenre-designated for ambulatory care patients which couldaccommodate six patients and a room had been setaside for meeting with ambulatory patients.
• Electrical medical equipment (EME) were labelled withasset numbers and the dates of the most recent serviceor test, which provided a visual check that they hadbeen examined to ensure they were safe to use. Wewere also shown records that provided evidence ofrecent maintenance inspections. This indicated that thehospital complied with guidelines contained in the HSE‘maintaining portable electrical equipment HSG107’(2013) and Medicines and Healthcare ProductsRegulatory Agency’s ‘Managing Medical Devices’ (April2015).
• The theatre department ordered operating equipmentfrom a BMI central hub, we a saw there was a record ofthe equipment that that been ordered. In the warming
Surgery
Surgery
Good –––
23 BMI The Sloane Hospital Quality Report 11/10/2019

air cabinet, we saw that stock rotation was in place andtemperatures recorded. However, theatres did not havean ultra sound machine for nerve blocks which did notreflect best practise. Following the inspection thehospital confirmed that an ultrasound machine wasnow available.
• In theatres we saw the 'difficult airways trolley' had dailychecks in place which met the recommendations of thedifficult airways society.
• Resuscitation trolleys were located on the wards and inthe theatre. On the wards we saw there were some gapsin the daily checks and trolleys were within easy accessfor staff. The stock was checked, and all items were indate. In the theatre the resuscitation trolley wascomplete with daily checks and all drugs in date. Therewas a defibrillator, suction and oxygen all available andworking.
• Disposable items of equipment were disposed ofappropriately, either in clinical waste bins or sharpsinstrument containers. Sharps management compliedwith Health and Safety (sharps instruments inhealthcare) regulation 2013. Sharps boxes wereobserved to be signed by staff and dated andassembled properly.
• Staff understood their responsibility to ensure theysegregated and disposed of clinical waste appropriatelyClinical waste bins were clearly labelled and weobserved staff kept the rooms used to store clinicalwaste clean and tidy to minimise infection risk. Therewas a contract in place with an external supplier todispose of clinical waste, which was stored securelyuntil collected.
• The patient led assessments of the care environment(PLACE) for 2018 for the condition, appearance andmaintenance 92.7% the same as the BMI Healthcareaverage 92.7%
Assessing and responding to patient risk
Staff completed and updated risk assessments for eachpatient and removed or minimised risks. However, thehospital did not have a not have a service level agreement(SLA) with the local NHS trust for transfers out in anemergency or if a patient’s condition deteriorated.
• The hospital did not have a service level agreement(SLA) with the local NHS trust for transfers out in anemergency or if a patient’s condition deteriorated. Astandard operating procedure (SOP) for critically ill
transfer out was in place for staff to follow. If a patientneeded to be transferred urgently staff were to call 999for an ambulance. The hospital advised there had beensafe transfers out. The hospital was in the process ofbuying portable ventilators for anaesthetists to travelwith the acutely unwell. This had been identified on therisk register.
• There was an admission policy setting out agreedcriteria for admission to the hospital. All patients wereadmitted to the surgical service under the care of anamed consultant. Patients had to meet certain criteriabefore the hospital would accept them for surgery, thisminimised the risk of harm to the patient due to lack ofappropriate facilities.
• Comprehensive assessments were carried out onpatients at pre-assessment and staff continued tomonitor these before and after their surgery. Key safetyareas such as venous thromboembolism (VTE), pressureareas, nutrition, pain were completed using national riskassessment tools.
• All patient records we looked at showed people wereassessed using the National Early Warning System(NEWS). Each chart recorded the necessary observationssuch as pulse, temperature and respirations.
• Staff were able to describe how they would escalateconcerns about a deteriorating patient. The RMOprovided medical cover 24 hours a day, seven days aweek. This meant concerns regarding a patient could beescalated at any time of the day. The RMO could contactthe relevant consultant as they were required bytelephone in the event of any concerns about patientcare.
• During this inspection we observed the theatre teamused the World Health Organisation (WHO) 5 steps tosafer surgery, surgical checklist, which was designed toprevent avoidable mistakes. This included checks suchas patient identify, allergies and ensuring the consentform had been signed. The 5 steps to safer surgerychecklist was audited monthly and we reviewed theaudits for December 2018, January and February 2019and saw that they were 100% compliant.
• The hospital had a sepsis screening tool and sepsis carepathway. Sepsis training was part of the mandatorytraining care and communication of the deterioratingpatient (CCDP) module. Data provided by the hospitalshowed 73.6% of theatre staff and 86.9% of ward staffhad completed the training.
Surgery
Surgery
Good –––
24 BMI The Sloane Hospital Quality Report 11/10/2019

• The practicing privileges agreement for all consultantsensured there was 24-hour clinical support when theyhad patients in the hospital. This included makingalternative arrangements for a named consultant toattend to patients in an emergency if they were notavailable. There was always a resident medical officer(RMO) on site who completed advanced life supporttraining, who was able to provide first line emergencytreatment.
• Patients who had concerns following discharge,including day surgery could call the hospital or thecorporate BMI 24-hour telephone advice line or access‘live support’ on the BMI website. The hospital also hada 48 hour follow up call service and staff on the wardwere scheduled to provide this.
• Theatre staff attended a safety huddle each morning,where the operating list was discussed. This was toensure all patient needs and risks for that day wereidentified. We observed a huddle during our inspectionand noted effective communication with all staffinvolved.
• Nursing staff on the wards undertook handoverbetween each shift (day shift to night shift, and viceversa), which included an update on all patientscurrently admitted and highlighted any specificconcerns such as infection risks to all staff.
• Staff used the situation, background, and assessment,(SBAR) communication tool for handover from theatreto ward staff when a patient returned from theatre. Ithelped remind staff of the areas to be covered. Staffprinted handover notes, which they updated during thehandover. All the patients were discussed and actionsoutstanding for patients were allocated.Situation-Background-Assessment-Recommendation(SBAR) is a communication tool designed to supportstaff sharing clear, concise and focused information.
• Theatre and wards staff completed adult basic lifesupport, immediate or advanced life support trainingdepending on their role. Data provided by the hospitalshowed that 62.5% of theatre staff had completed adultbasic life support training, 81.8% of theatre staff and100% of ward staff had completed adult immediate lifesupport and 50% (one of two staff identified) of wardstaff had completed adult advanced life support.Immediate life support training for theatre staff wasbelow the target of 90%.
• The mandatory training matrix identified the followingstaff to be trained in adult advanced life support as
registered practitioners selected by the hospital to leadthe resus team and/or the hospital scenarios. The resusOfficers, RMO, recovery or anaesthetic practitionersselected by hospital (2 -3 per department to cover hoursthat are open).
Nursing and support staffing
The service had enough nursing and support staff with theright qualifications, skills, training and experience to keeppatients safe from avoidable harm and to provide the rightcare and treatment.
• Staffing was monitored daily to ensure staffing levelsand the skill mix of staff met the projected acuity andnumbers of patients.
• The theatre department staffing comprised of 10.60 fulltime equivalent (FTE) theatre nursing staff and 4.00 FTEoperating department practitioners (ODPs) and healthcare assistants (HCAs).
• There were ongoing difficulties with the recruitment oftheatre staff and this was recorded on the hospital’s riskregister. Senior theatre staff told us they used regularbank and agency staff to ensure continuity of care. Staffwe spoke with told us that the transfer of patients to andfrom theatre was an issue. The theatre department hada dedicated porter, but when they were absent theOPD’s had to collect patients from the ward and thiswould delay theatre. Following the inspection, thehospital advised the porter had been absent on the dayof the inspection.
• The theatre department used the theatre utilisation tool(TUT). The tool is designed to automate analysis of anumber of key theatre department process measures.The TUT increases the efficiency of the department byrefining staff allocation to patient numbers andprocedure mix and therefore reducing staffing costs,creating capacity for additional caseload, improvingpatient safety and ultimately increasing satisfaction forpatients, consultants and staff. The theatres also usedthe BMI Resource Model in theatres which incorporatedthe Association of Perioperative Practice (AFPP)guidelines for safer staffing.
• Workforce planning for the theatres was currently donetwo weeks in advance, but there were plans to aim for amonthly rota.
Surgery
Surgery
Good –––
25 BMI The Sloane Hospital Quality Report 11/10/2019

• In recovery there were a minimum of two nurses, whichis in line with the British Anaesthetic and RecoveryNurses Association (BARNA) and the Royal College ofAnaesthetists (RCOA) recommendations.
• Wards staffing comprised of 12.40 FTE registered nursesand 1FTE (HCA). On the wards a senior nurse was incharge as a contact point for staff, consultants andpatients 24 hours a day, seven days a week.
• On the wards nurse staffing levels and skill mix wereplanned according to patient admissions which wereknown in advance. Staffing levels were calculated usingthe electronic BMI Healthcare Nursing Dependency andSkill Mix Planning Tool.
• A minimum of two registered nurses were always onduty on the wards, one of whom was substantive, plus ahealth care assistant (HCA). Nursing staff numbers weredetermined by the numbers of patients booked foradmission and could be adjusted to the flow of patientsas admission times were staggered.
• Agency nurses underwent hospital orientation andinduction. In theatres the use of bank and agency staffbetween April 2018 and March 2019 was between 21%and 10% each month for nursing staff, and between 15%and 1% for OPD and HCA staff. On the wards over thesame period the use of bank and agency staff fornursing staff was between 17% and 7% each month and3% and 1% for HCA staff. The overall reliance on agencyand bank staff had improved over the 12-month periodand senior staff told us they always tried to book thesame staff that were familiar with the hospital. On thewards nursing staff told us agency staff mainly coverednights and bank staff supported day and night shifts.
Medical staffing
The service had enough medical staff with the rightqualifications, skills, training and experience to keeppatients safe from avoidable harm and to provide the rightcare and treatment.
• The hospital had 218 doctors with practicing privilegesfor more than six months. Between April 2018 and March2019, the number of episodes of care carried out bydoctors with practicing privileges were: 5.96% (13) ofdoctors carried out 100 or more episodes of care, 21%(46) of doctors carried out between 10 and 99 episodesof care, 11.9% (26) of doctors carried between 1 and 9episodes of care, 61% (133) of doctors undertook noepisodes of care.
• A requirement for all consultants and anaesthetists’consultants engaged under BMI practising privilegeswas that they remained available for their own patients(both by phone and, if required, in person). Consultantsand anaesthetists were required to confirm suitablecover arrangements if they are unavailable or on annualleave (buddy system).
• Under their practising privileges consultants wererequired to visit their patients at least once per day. Allthe patients we spoke with told us they had seen theirconsultant post-surgery and patients who wereinpatients had seen them daily and or prior to theirdischarge.
• The day to day medical service was provided by aresident medical officer (RMO) who dealt with anyroutine and emergency situations in consultation withthe relevant consultant. Out of hours, consultantsprovided either telephone advice or attended in person.
• The RMO provided a 24-hour 7 day a week service on athree-week rotational basis. All RMOs were selectedspecifically to enable them to manage a varied patientcaseload and requirements. The RMOs are providedunder contract with an external agency that providedtraining and support.
• The theatre department had an out of hours on callteam which included and anaesthetist who wasavailable to deal with emergency surgery.
Records
Staff kept detailed records of patients’ care and treatment.Records were clear, up-to-date, stored securely and easilyavailable to all staff providing care.
• Patient individual care records were written andmanaged to ensure that they were accurate, complete,legible, up to date and stored securely. Staff had accessto computers and these were password protected andwe observed that these were locked when not in use.This was in line with the Data Protection Act 1998.
• Patients care pathways commenced at pre-operativeassessment prior to admission for surgery. Thepre-operative assessment was fully completed andformed part of the paper record.
• GP’s were sent discharge letters electronicallyimmediately after discharge with details of thetreatment, including follow up care and medicinesprovided.
Surgery
Surgery
Good –––
26 BMI The Sloane Hospital Quality Report 11/10/2019

• Where appropriate, patient care records containedstickers identifying equipment and implants usedduring surgery. This meant that they could clearly betracked and traced.
• Staff used specific care pathway paperwork for eachpatient which ensured they kept records appropriate.For example, patients admitted for knee surgery hadtheir clinical entries recorded in the ‘Primary kneereplacement care pathway’ documentation. Carerecords contained pre-operative assessments, recordsfrom the surgical procedure and anaesthetic, recoveryobservations, nursing and medical staff notes anddischarge checklists and assessments. The records alsoincluded multidisciplinary clinical notes, includingthose from physiotherapists.
• Theatre staff maintained a log of implants on theirprosthetics register to enable traceability if an incidentoccurred. Theatre personnel retained a sticker fromeach implant in the register as well as in the patientnotes.
• We reviewed six sets of medical records and found thatrisk assessments for venous thromboembolism (VTE),pressure areas, nutrition, pain had been completedusing national risk assessment tools. Patients allergieswere also recorded.
• The hospital undertook quarterly health documentationaudits these included ensuring all notes were securewithin the file and filed in order. Documents werelegible, there was evidence of informed consent,completed operation note, completion of clinical riskassessments for VTE, pressure areas, moving andhandling, bed rails, and falls and that all entries bynursing staff and consultants were signed and dated.The audit undertaken in December 2018 demonstratedrecord compliance was 91.5%. An action plan had beenput in place to address areas were documentation wasnot achieving 100%.
• We saw that safety checks undertaken during surgery,using the World Health Organisation (WHO) ‘Five Stepsto Safer Surgery', were held within the patient’s notes.
• Information governance was part of the mandatorytraining programme which all staff were required toattend. Compliance for theatres staff was 100% andwards staff was 86.9% which was below the hospital’starget was 95% of staff having completed the training
Medicines
The service used systems and processes to safely prescribe,administer, record and store medicines.
• The pharmacy team completed a programme of regularaudits for missed doses, controlled drugs and medicinesreconciliation.
• Pharmacy staff visited wards each day and conductedmedicines reconciliation. (Medicines reconciliation isthe process of ensuring that the list of medicines aperson is taking is correct.) Staff could access medicinessupplies and advice out of hours.
• We saw controlled drugs (CD) were stored, recorded,and handled appropriately with two nurses signingwhen controlled drugs were being administered. Wenoted no discrepancy in signing in the CD book.
• Access to the pharmacy during opening hours was bydesignated pharmacy staff only. There were specificprocedures for other named staff to gain emergencyaccess to the pharmacy out of hours, with the residentmedical officer (RMO) and senior nurse holding separatekeys meaning that single access was not possible
• All medicines on the wards and in the theatredepartment were stored securely in locked trolleys,cupboards and fridges with stock medications stored inlocked cupboards in the key code locked clinical room.
• We reviewed a selection of medications stored on thewards and the theatre department and found all to bewithin expiry date.
• Staff monitored fridge temperatures on the wards dailyto confirm that the fridge temperatures were in range,however no action was taken when the readings wereout of range. Following the inspection the hospitaladvised they are now recording the actions they takewhen fridge readings are out of range.
• There was no fridge in the anaesthetic room soemergency drugs were stored in a cool pack.
• Staff had to access medication guidance, for examplethe hospital’s medicines policy and current BritishNational Formularies.
• The pharmacy manager represented BMI with the localCCG’s and liaised with them on a regular basis regardingissues with prescribing and adherence to formulary.
Incidents
The service managed patient safety incidents well. Staffrecognised and reported incidents and near misses.
• The hospital reported no incidents classified as neverevents across the theatres and wards in the
Surgery
Surgery
Good –––
27 BMI The Sloane Hospital Quality Report 11/10/2019

twelve-month period from January 2018 to December2019. Never events are serious patient safety incidentsthat should not happen if healthcare providers follownational guidance on how to prevent them. Each neverevent type has the potential to cause serious patientharm or death but neither need have happened for anincident to be a never event.
• The hospital used an electronic incident reportingsystem so all clinical and non-clinical incidents werereported and logged directly onto the incident reportingdatabase. Staff said they were encouraged to reportedincidents and had individual feedback. Nursing staff toldus learning from incidents was disseminated to staffthrough their departmental meetings as well as thecomm cell to prevent recurrence.
• The hospital reported 248 clinical incidents in thetwelve-month period January 2018 to December ofwhich 72.5% (180) related to the theatres and inpatients.Of the 248 incidents 73.7% (183) were categorised as noharm, 24% (60) were categorised as low harm, 1.6% (4)were categorised as moderate harm, and 0.4% (1)incident was categorised as severe harm.
• The hospital provided the details of the last three rootcause analysis investigations (RCA), two of whichoccurred in 2017 and related to theatre and inpatientservices. One incident occurred in June 2017 and theseverity of harm identified as low for a patient beinganesthetised without having signed a consent form forthe procedure. The other incident in October 2017related to the escalation of a deteriorating patient andsubsequent death of the patient. The investigationsidentified the root causes, that duty of candour hadbeen applied, the lessons learned, arrangements forshared learning which included presenting key findingand shared learning at MAC (Medical AdvisoryCommittee) meetings and an action plan which detailedwhat actions were taken to prevent reoccurrence.
• From November 2014, providers are required to complywith the duty of candour Regulation 20 of the Healthand Social Care Act 2008 (Regulated Activities)Regulations 2014. The duty of candour is a regulatoryduty relates to openness and transparency and requiresproviders of health and social care services to notifypatients (or other relevant persons) of certain ‘notifiablesafety incidents’ and provide reasonable support to thatperson. Staff we spoke with were aware of theirresponsibility to apologise and be open and honest andshare the information with the patient and their carers.
Safety Thermometer (or equivalent)
The service used monitoring results to improve safety. Staffcollected safety information and shared it with staff.However, the service did not display safety informationpatients and visitors to view.
• The hospital measured safety performance andsubmitted safety data to the BMI Healthcareorganisation.
• During the reporting period March 2018 to March 2019hospital data showed the service was 100% harm free,with no pressure ulcer, no catheter or urinary tractinfections or venous thromboembolism episodes andno patient falls.
• The service did not display safety information on theward for patients and visitors to view.
Are surgery services effective?
Good –––
Our rating of effective stayed the same.We rated it as good.
Evidence-based care and treatment
The service provided care and treatment based on nationalguidance and evidence-based practice. Managers checkedto make sure staff followed guidance.
• Policies, procedures and guidelines had beendeveloped in line with national policy. These includedThe Royal College of Surgeons standards for consultantled surgical care, the Association of Anaesthetists ofGreat Britain and Ireland (AAGBI), National Institute forHealth and Care Excellence (NICE) guidelines.
• All the BMI corporate Policies, procedures andguidelines were available to all staff through thehospital's intranet system and staff demonstrated theyknew how to access them.
• Staff running the pre-operative assessment clinicfollowed NICE guidance to ensure that staff had relevanttests prior to surgery to minimise the risk ofcomplications or harm.
• The hospital used different care pathways for daypatients, inpatients, patient undergoing hip or kneereplacement. The assessments used by staff were basedon national tools such as the malnutrition screeningtool (MUST) and the News Early Warning Scores (NEWS).
Surgery
Surgery
Good –––
28 BMI The Sloane Hospital Quality Report 11/10/2019

• The hospital offered an advanced recovery programmewhich meant that patients were assisted out of bed assoon as possible following their operation. This helpedto prevent post-operative complications and encourageearly rehabilitation.
• The clinical audit programme was set by the BMIHealthcare group. Audits included the World HealthOrganisation (WHO) surgical safety checklist, infectionprevention and medicines management. This meant thehospital was bench marked against other BMI hospitalswithin the BMI healthcare group.
Nutrition and hydration
Staff followed national guidelines to make sure patientsfasting before surgery were not without food for longperiods.
• Patients were advised about fasting times prior tosurgery at pre- operative assessment. Patients told usthat on admission staff would check to ensure they hadfollowed the fasting guidelines. Staff told us fasting wasusually six to eight hours for food, and two hours forclear fluids prior to surgery.
• Nursing staff completed assessments in nutrition andhydration. Staff used the Malnutrition Universal ScoringTool (MUST) on at pre-assessment risk assessment priorto admission.
• Intravenous fluids were prescribed when required. Fluidbalance charts were used to monitor patient’s hydrationstatus.
Pain relief
Staff assessed and monitored patients regularly to see ifthey were in pain and gave pain relief in a timely way.
• Pain relief on the wards was well managed. Patientsprescribed pain relief to be given ‘when required’ wereable to request this when they needed it. Patients toldus they were asked by staff on the comfort rounds if theywere in any pain and medicines were provided in linewith the patients’ prescriptions.
• In theatres we observed that patients were asked aboutpain and pain relief was offered.
• Staff assessed patients’ pain as part of the national earlywarning score (NEWS). This ensured that painmanagement was monitored, and patients receivedpain control medicine in a timely way. In four out of thesix patient notes we saw patients had been asked aboutpain.
• The resident medical officer (RMO) could prescribeadditional pain relief or nursing staff would speak to thepatient’s consultant.
• Post-operative pain relief was discussed with patients atpre-operative assessment and they were giveninformation about pain control and anaesthesia.
• The hospital provided details of two quarterly painmanagement audits undertaken in July and November2018. Both audits showed that all the patients notes hadevidence that the nursing team had assessed thepatients pain levels frequently.
Patient outcomes
Staff monitored the effectiveness of care and treatment.
• The hospital participated in the National Joint Registry(NJR) to collect information on orthopaedic jointreplacement operations, to monitor the performance ofimplants and the effectiveness of different types ofsurgery.
• The hospital submitted data to the NHS patientreported outcome measure (PROMS) programme for hipand knee replacement and cataract surgery andsubmits data monthly. For the period April 2017 toMarch 2018 hip and knee replacement pre-operativequestionnaire completion was 83.7% and thepost-operative questionnaire the responses rate was75.6%.
• As part of the BMI Healthcare organisation the hospitalcontributed to the Private Healthcare InformationNetwork (PHIN). Data was submitted in accordance withlegal requirements which were regulated by theCompetition and Markets Authority (CMA).
• The hospital also submitted data to the National Breastand Implant Register, however the hospital advised thishad not been updated since 2017 due to no staff havingauthorised access to input to the register. The hospitaladvised that since this had been identified, steps havebeen taken to request access to the register. All recordssince the last data input were kept in theatre in hardcopy format but, had yet to be submitted to the register.
• From January 2018 to December 2018 there was oneunplanned transfer of an inpatient to another hospital.During the same period there were eight unplannedreturns to theatre and three unplanned readmissionswithin 28 days of discharge.
• The day after discharge patients had a telephone followup call by ward staff, this ensured contact was made
Surgery
Surgery
Good –––
29 BMI The Sloane Hospital Quality Report 11/10/2019

with patients to confirm that were supported postoperatively and to determine any potential problems,which may impede an expected good outcome. Allpost-operative calls from patients for advice weredocumented and reviewed daily by ward manager fortrends or patterns.
Competent staff
The service made sure staff were competent for their roles.Managers appraised staff’s work performance.
• Staff told us they participated in the appraisals process.BMI Sloane appraisal year runs from October toSeptember. In the current appraisal year 70% of nursingstaff and 100% of operating department practitioners(OPD) registered and health care assistants (HCA)working in the theatres had an appraisal. On the wards100% of nursing staff and health care assistants (HCA)had an appraisal.
• Nursing staff told us there were opportunities forlearning and development and they had access toregular training updates these included paediatric basiclife support, controlled drugs and medicinemanagement workshops. Staff completed theire-learning whilst on duty and were not expected tocomplete their training in their own time or to come intowork on their day off to complete. Nursing staff told usthey had monthly scenarios to practice differentsituations. These have included for example managing apatient with sepsis. At the end of the scenario staff aredebrief and additional training is identified.
• Registered staff we spoke with confirmed they weresupported by the hospital with revalidation
• In the theatres bank and agency staff were utilised. Stafftold us that they had two agency staff they used forconsistency and had a pool of four bank staff.
• Nursing staff told us they felt supported by theconsultants while they were on site and if they neededto contact them out of hours.
• The RMO told us they were able to access consultants ifthey needed advice and the agency that employedthem undertook regular appraisals. However, it was notclear who was responsible for providing the RMOs withclinical supervision.
• All consultants working with the hospital had practisingprivileges which required consultants to have an up to
date General Medical Council (GMC) registration,evidence of indemnity insurance and revalidationcertificate. These were reviewed and highlighted atMedical Advisory Committee (MAC) meetings.
• Consultants only performed surgical procedures whichthey undertook in the NHS. As all the consultants heldNHS contracts they maintained their skills by working intheir trust and had their appraisals completed by theirNHS Medical Director.
Multidisciplinary working
Doctors, nurses and other healthcare professionals workedtogether as a team to benefit patients.
• We observed that multidisciplinary (MDT) working wasevident on the wards; The RMO, pharmacists and nursein charge reviewed patients who stayed overnight.
• Nursing, theatre staff and the RMO told us it was easy tocontact a consultant if they needed advice. Theconsultant had overall responsibility for a patient’s care.
• There was clear communication between theatre staffto ward staff. To aid safe and effective handovers of care,between the ward, theatre staff used a written Situation,background, Assessment, Recommendation (SBAR)handover tool.
• Physiotherapy staff were mobilised in-patient’spost-surgery to aid effective recovery which includedfollow up at outpatient clinics.
• Pre-operative assessment staff told us they liaised withconsultants and anaesthetists if there were anyconcerns about tests results or medications the patientwas taking.
• Patients GP were sent a letter when the hospitaldischarged a patient.
Seven-day services
Key services were available seven days a week to supporttimely patient care.
• The theatres ran from Monday to Friday from 7.30 am to9.00 pm and 8.30 am to 6.30 pm on Saturdays. Theatrestaff were on-call should there be any unplannedreturns to theatre. On call staff were able to contactconsultants and consultant anaesthetists.
• Nursing cover was available on the wards during the dayand overnight for patients who required an overnightstay seven days per week.
Surgery
Surgery
Good –––
30 BMI The Sloane Hospital Quality Report 11/10/2019

• The RMO was always on-call and was based at thehospital, should staff need to escalate concerns about apatient.
• Consultants as part of their practicing privileges wereavailable by phone and, if required, in person when theyhad inpatients in the hospital.
• Two pre- operative assessment clinics ran from Mondayto Friday. Staff told us there were plans to offerpre-operative assessment clinics in the evening and ona Saturday morning. Pre-operative assessments werealso offered on the telephone.
• Physiotherapy staff supported effective recovery andrehabilitation by providing sessions to inpatients daily,including at weekends.
• The pharmacy was open Monday to Friday 8.00 am to4.00 pm. There was one clinical pharmacist and oneassistant or pharmacy technician available duringopening hours. The RMO and senior nurse in chargewere permitted joint access to the pharmacy out ofthese hours. The 'on call' pharmacist provided supportremotely or came in when controlled drugs wereneeded out of hours for theatres or where theconsultant has added a new medicine that was notalready available from the out of hours cupboard.
• Diagnostic imaging services provided an on-call serviceoutside normal hours and at weekends for any inpatientemergencies or urgent radiological advice.
Health promotion
Staff gave patients practical support and advice to leadhealthier lives.
• Physiotherapy staff encouraged patients to mobiliseearly post surgery to help prevent post-surgerycomplications and encourage independence.
• In pre-assessment patients had access to a variety ofleaflets which included smoking cessation, alcoholdependency, and venous thromboembolism (VTE) anda guide to pain control.
• Patient menus included meals labelled as healthychoices.
Consent, Mental Capacity Act and Deprivation ofLiberty Safeguards
Staff supported patients to make informed decisions abouttheir care and treatment. They followed national guidanceto gain patients’ consent.
• Staff had access to the BMI policies regarding consent,mental capacity act and deprivation of libertysafeguards and knew where to find them on the BMIintranet. Staff told us they would followed the hospitalspolicy and procedures when a patient could not givetheir consent.
• Patients told us that the consultants had discussed thebenefits and risk of surgery before signing the consentforms. In all the records we reviewed the consent formshad been completed correctly.
• Staff we spoke with were clear about theirresponsibilities in relation to gaining consent. Patienttold us that staff would gain their consent beforepost-operative observations and when performingtherapeutic treatment.
• Consent training was included within the mandatorytraining and both theatre and ward staff were 100%compliant. The hospital told us that training in theMental Capacity Act 2005 and Deprivation of LibertiesSafeguards (DoLS) was included in safeguardingvulnerable adults level 2 training.
Are surgery services caring?
Good –––
Our rating of caring stayed the same. We rated it as good.
Compassionate care
Staff treated patients with compassion and kindness,respected their privacy and dignity, and took account oftheir individual needs.
• Staff were seen to be considerate and empathetictowards patients. During our inspection we spoke withsix patients and their relatives who were all very positiveabout their care and treatment. They told us the nurseswere kind, caring and listened to their concerns.
• In theatres all staff were observed treating patients withdignity and respect. Staff made sure patients werecomfortable and had the opportunity to air anyconcerns. We observed staff asking a partially sightedpatient if they would like anything when they woke upfrom their anaesthetic for example their glasses ordimmed lighting.
Surgery
Surgery
Good –––
31 BMI The Sloane Hospital Quality Report 11/10/2019

• Patients reported that staff were polite, courteous andattentive; relatives who visited them felt welcomed. Weobserved clinical and housekeeping staff introducedthemselves to patients and patients were treated withkindness and respect.
• The privacy and dignity of patients was maintained withthe use of closed doors. The hospital told us they hadtwo dignity champions.
• Patients informed us that staff were attentive andhelpful. Patients told us call bells were answeredquickly. Patients were encouraged to tell staff if theyrequired any assistance or pain relief and we saw thisbeing done.
• Relatives felt that staff kept them involved and informedabout their relative’s care and they had confidence thattheir relatives were cared for well.
• We saw notices on display in the hospital advisingpatients to let staff know if they wished for a chaperone.
• Hospital wide Friends and Family Test (FFT) scores forinsured and self-pay patients for the period May 2018 toMay 2019 ranged from 93% – 100%. The scores for NHSpatients for the same period ranged from 98% -100%.
• The patient led assessments of the care environment(PLACE) for 2018 for privacy, dignity and wellbeing scorewas 82.4% which was lower than the BMI Healthcareaverage of 85.8%.
• Staff encouraged patients to complete patientsatisfaction questionnaires to review and improvepatient experience. The monthly report showed patientresponse rates, rating within categories and rankingagainst all BMI hospitals. In May 2019 BMI SloaneHospital was rated 43 out of 55 BMI hospitals nationally.
Emotional support
Staff provided emotional support to patients to minimisetheir distress.
• Staff in all areas showed sensitivity and support topatients and understood the emotional impact of themhaving to be admitted for surgery. One patient we spokewith told us their consultant had phoned them threedays before their operation, so they could ask furtherquestions as they were anxious about their surgery.They told us this gave them additional reassurance.
• People were given appropriate information and supportto cope emotionally with their care, treatment.Additional information was provided at pre-operativeassessment and they were signposted to other supportservices.
• The hospital had open visiting hours on the ward andrelatives and carers could visit at any time to offersupport.
• Patients told us staff regularly checked on theirwellbeing and to ensure their comfort.
• Patients were able to telephone the ward afterdischarge, for further help and advice on their returnhome.
• Staff had access to a number of local religiousorganisation hey could contact if patients requestedthis.
Understanding and involvement of patients and thoseclose to them
Staff involved patients, and those closed to them indecisions about their care and treatment.
• Patients told us that they were involved in their careplanning and that they were given the opportunity toask questions about care and treatment. All the patientsmet with their consultant and the anaesthetist prior tothe operation. We observed therapy staff gave leaflets toa patient to support the verbal information provided.
• Patients told us they were given clear explanationsabout the risks and benefits of the planned treatmentand patients understood how their recovery wouldprogress. This happened through discussion with theirconsultant and pre-operative assessment nurses.
• All the patients we spoke with were either non-NHSfunded or NHS funded. However, none of the patientswhen asked said finances had been discussed withthem.
• All patients had named consultants which were writtenon the doors of their rooms.
• Patients we spoke with knew they could contact thehospital if they felt unwell after they were dischargedfrom the hospital. The ward staff performed follow uptelephone calls 48 hours post discharge. A nurse wasrostered to call patients to check that they had noproblems or complications.
• Patients felt that they were given relevant informationabout their diagnosis and treatment and that they werehelped to make informed decisions about their care.
Surgery
Surgery
Good –––
32 BMI The Sloane Hospital Quality Report 11/10/2019

Are surgery services responsive?
Good –––
Our rating of responsive stayed the same. We rated it asgood.
Service delivery to meet the needs of local people
The service planned and provided care in a way that metthe needs of local people.
• The hospital worked with local clinical commissioninggroups (CCG) and NHS trust to provide a range ofelective services, these included hip and kneereplacements.
• Private patients were able to book appointmentsthrough the BMI Healthcare website, which also had a‘live chat’ support function. NHS funded patients whorequired surgical procedures could book through thenational choose and book portal, this also gave patientsa greater choice of hospital and appointment date andtime.
• The inpatient and day-case activity for the period March2018 to February 2019 comprised both non-NHS fundedand NHS funded patients. During the same period therewere 662 inpatient and 3,384 day-case patients.Inpatient activity was 72.5% (480) non-NHS funded and27.5% (182) NHS funded patients. Day case activity was71% (2,399) non-NHS funded and 29% (985) NHS fundedpatients.
• There were no facilities for emergency admissions;commissioners and the local NHS trust were aware ofthis.
• The hospital pre-planned all admissions. They acceptedpatients for treatment who were assessed as being atlow risk of complications and whose post-operative carecould be met.
• Pre-operative assessments were completed at least twoweeks prior to admission and no less than 5 days. Underexceptional circumstances pre-admission assessmentcould be undertaken no less than 72 hours withapproval of the Director of Clinical services. NHSpatients' pre -surgery assessments occurred within amaximum of 16 weeks prior to the patients anticipatedsurgical date.
Meeting people’s individual needs
The service took account of patients’ individual needs andpreferences.
• Patient admissions were pre-planned so that staff couldassess patient needs prior to treatment. Staff told usthat pre-operative assessment clinics were ran flexiblyto accommodate individual patients’ requirements. Forexample, for patients who wanted an early appointmentthey would start the clinic at 6.30 am. The hospital wasalso looking to introduce evening and Saturday morningpre-operative assessment clinics.
• The hospital used the care pathways for surgicalpatients. The pathways promoted effective patient carebased on evidence based practice and ensured thatindividual patient’s needs were recognised. They alsoprovided flexibility to enable day case patients theoption to stay overnight according to need. One patientwho was a day case told us they did not get back fromthe theatre until later the previous evening, and theyhad stayed in overnight and were being discharged laterin the day.
• The hospital had an open visiting policy, this meantfamily and friends could provide support andassistance.
• Catering services were outsourced to an externalprovider. A variety of meals were available for patients tochoose. There were allergy aware menus and menuswith healthier choice which included vegetarian andgluten free. The staff provided support with meals asneeded. Hot and cold drinks and snacks were readilyavailable. Patients we spoke with were generally happywith the choices they had been offered.
• Patient led assessments of the care environment(PLACE) 2018 for food and hydration was 93.3% similarto BMI Healthcare average of 93.8%.
• Staff told us they could access interpreters. Translationservices were provided through a telephoneinterpretation service.
• The hospital had a chaperone policy in place andnotices encouraging patients to ask for a chaperonewere visible on the wards. Chaperone training wasavailable through e-Learning.
• On the wards there were information boards withinformation for staff on how to support people withdementia. A dementia box was available on the ward
Surgery
Surgery
Good –––
33 BMI The Sloane Hospital Quality Report 11/10/2019

which staff could access to help to support a patientwith dementia. On the wards 95.7% of nursing staff and100% of the theatre staff had completed dementiaawareness training.
• Patient Led Assessments of the Care Environment(PLACE) 2018 for dementia was 78.9% which was lowerthan the BMI Healthcare average of 79.4% and fordisability this was 78.4%, which was lower than the BMIHealthcare average score 83.3%.
• The hospitals website provided information aboutpaying for treatment. Patients were able to pay forthemselves. Treatment could also be funded throughprivate medical insurance. The hospital also providedservices for patient funded through the NHS.
• The hospital was unable to treat bariatric patients asthey did not have bariatric equipment
Access and flow
People could access the service when they needed it andreceived the right care promptly.
• Admissions to the hospital could only be made byconsultants who had admitting rights. The hospital hada clear exclusion criterion for planned and unplannedadmission, these included patients requiring criticalcare level two or three, termination of pregnancy,infectious diseases, mental health, acute cardiology andchildren under 16 years of age. This meant the hospitalonly admitted patients they had the facilities andexpertise to care for.
• NHS patients were usually referred by their GP’s orthrough spot purchase contracts with the NHS.
• In the twelve-month period January 2018 to December2018 the hospital treated a total of 4,030 patients aged18 to 75+ years, of these 662 were inpatients and 3,368were day cases.
• In the twelve-month period January 2018 to December2018 the hospital carried out 1214 surgical procedure.Over this period the hospital cancelled 12 proceduresfor non-clinical reasons. Five of the patients wereoffered appointments within 28 days.
• Between June 2018 and June 2019, a total of 63 patientshad their procedure or appointment cancelled on theday. Of these 39.6% (25) were day case patients and23.8% (15) were inpatients. Of these 55% (22) werecancelled due to clinical reasons, 22.5% (9) patients
were cancelled due to lack of staffing or unavailableequipment, 12.5% (5) patients cancelled theirprocedures, and 5% (2) procedures were cancelled bythe consultants.
• There were morning, afternoon and evening operatingsessions. The evening session ran from 5.30 pm to 9.00pm and included both inpatients and day cases. Theatreand ward staff told us the evening surgery sessionsometimes overran, with patients returning to the wardafter 9.00 pm. Occupancy rates on the wards meant thatany day case patient who required an overnight staycould do so.
Learning from complaints and concerns
It was easy for people to give feedback and raise concernsabout care received. The service treated concerns andcomplaints seriously, investigated them and shared lessonslearned with all staff.
• The hospital executive director oversaw themanagement of complaints. The handling of complaintswas monitored to ensure that complaints were dealtwithin the time frame set out in the BMI complaintspolicy. Where there were time extensions in dealing withcomplaints, the reasons for the extension was recorded.Complaints could be raised in person, by telephone, orin writing and are recorded onto BMI Healthcareelectronic complaints reporting system.
• Complaints were discussed at the daily 'comms cell'meetings, weekly senior management meetings, atmonthly clinical governance meetings and heads ofdepartment meetings and cascaded to all departments.
• Staff told us they tried to resolve complaints andconcerns at the time where ever possible.
• Across the hospital 214 complaints were raised bypatients during the twelve-month period January 2018to December 2019. One complaint had been referred tothe Independent Healthcare Complaints AdjudicationService (ISCAS). The hospital advised they had twocomplaints following short notice surgical cancellationswhere it was identified that the cancellations could havebeen avoided. Theatre staffing, and equipment are nowreviewed in advance.
• Between October 2018 and March 2019 there were 13complaints related to theatres (7), the wards (4), and
Surgery
Surgery
Good –––
34 BMI The Sloane Hospital Quality Report 11/10/2019

pre-operative assessment (7). All the complaints hadbeen responded to and closed. There were noconsistent trends or themes in the complaints that werereported.
• There was a daily duty manager at the hospital whopatients or visitors could speak with if they had anyconcerns or compliments.
• Information was available the BMI leaflet 'How did wedo today?' to inform patients, relatives and visitors onhow they could raise any concerns.
Are surgery services well-led?
Good –––
Our rating of well-led stayed the same. We rated it as good.
Leadership
Managers had the skills and abilities to run the service.They understood and managed the priorities and issuesthe service faced.
• There was a clear leadership structure. An executivedirector (ED) had overall accountability for the hospitaland was supported by senior management teammembers, director of clinical services (DCS), director ofoperations (DO), sales and marketing manager,commercial finance manager, and the medical advisorycommittee (MAC) chair.
• The senior management team were supported by fiveclinical services managers which included theatres andthe wards. The theatre manager and ward manager hadrecently come into post and had been with the hospitalfor less than six months at the time of the inspection.
• The leaders had the skills, knowledge and experiencethey needed for their roles.
• The department managers that we spoke with had agood understanding of the challenges to quality andsustainability and were able to identify the actionsneeded to address them.
• Staff were positive about the local leadership. Staff toldus they felt supported by their line-manger to do theirjobs despite challenges, especially of capacity andrecruitment
• Consultant medical staff told us they had a goodworking relationship with the staff and seniormanagement to deliver care and meet patients’ needs.
Vision and strategy
The service had a vision for what it wanted to achieve and astrategy to turn it into action. The vision and strategy werefocused on sustainability of services.
• BMI Sloane is part of BMI Healthcare. The hospital’svision and strategy were driven by BMI Healthcare whichwas to ‘offer the best patient experience and bestoutcomes in the most cost-effective way from ourcomprehensive UK network of acute care hospitals”.
• The hospital had a five-year BMI Sloane operationalplan 2015-2020 which set out the hospitals vision toalign with the BMI Healthcare company vision “toprovide outstanding care to our local population, withhigh performing, caring and progressive team.” Thehospital identified it’s eight strategic objective andpriorities as being people, patients, communication,growth, governance, efficiency, facilities’, andinformation.
• Most of the staff we spoke with knew of BMI’s vision toprovide the best possible patient experience andoutcome. In the theatres and on the wards, we saw staffworking together to achieve this.
• The hospitals strategy was to review the current servicesit provided and possibly expand the endoscopy serviceand ambulatory care service.
Culture
Staff felt respected, supported and valued. The serviceprovided opportunities for development. The service hadan open culture.
• There was a culture of honesty, and transparency. Staffwere encouraged to report incidents and learning fromincidents was cascaded. We saw evidence of senior staffcarrying out duty of candour responsibilities whichdetailed the involvement and support of patients orrelatives in root cause analysis investigation reports.
• The hospital had trained two members of staff in July as‘freedom to speak up champions, as part of a BMI-wideinitiative. While some junior staff could not recall thenames of the hospital champions, we saw examples ofpublicity posters and emails distributed as part of theinformation campaign. The champions form part of aconfidential support network for staff who may want toreport a problem but don’t feel confident to raise theissue alone.
Surgery
Surgery
Good –––
35 BMI The Sloane Hospital Quality Report 11/10/2019

• The theatre manager and the wards manager workedclinically and were proud of their staff and department.
• Nursing staff told us there was good team work and peersupport. Staff were committed to delivering a goodservice.
• Staff were enthusiastic about the care and services theyprovided for patients. Some of the staff we spoke withhad worked at the hospital for many years anddescribed the hospital as a good place to work.
• The hospital had nominated two staff as the freedom tospeak up guardians and they were due to undertaketraining at the end of July.
• There were opportunities for further learning anddevelopment, nursing staff told us there wereopportunities for them to progress.
• On the wards we saw multidisciplinary working whichinvolved patients, therapists and nursing staff workingtogether to achieve good outcomes for patients.
• Patients acknowledged a positive and caring ethos andwere mostly happy with their care.
Governance
The service operated effective governance processes. Staffwere clear about their roles and accountabilities and hadregular opportunities to meet, discuss and learn from theperformance of the service.
• The hospital had effective governance process andworked within the BMI Hospital Committee Terms ofReference. Governance and risk performance werediscussed through the committee meeting structureincluding monthly heads of department (HoD), clinicalgovernance, Health & Safety and quarterly MedicalAdvisory Committee. Agendas of meetings followed astandardised format, with action listed and a namedindividual and timeframe for completion. Senior leadersreport into the corporate BMI healthcare regional andnational clinical governance structure.
• The hospital’s clinical governance committee ensuredthere was clinical oversight of for example patient safetyissues, incidents, complaints, risk register and audits.There was also a standing agenda item to reviewexternal and national guidance and new legislation,such as National Institute of Health and Care Excellence(NICE) guidance. This ensured the hospital implementedand maintained best practice, and any issues affecting
safety and quality of patient care were known,disseminated managed and monitored. We reviewedfour sets of minuets were well attended by the SMT,HoDs and clinical leads.
• Medical Advisory Committee (MAC) meetings were heldbi-monthly. MAC minutes showed there was there wasrepresentation from all the surgical disciplines at theMAC meeting. The role of the MAC was advisory andincluded ensuring that all consultants were skilled,competent, and experienced to perform the treatmentsundertaken. Practising privileges were granted forconsultants to carry out specified procedures using ascope of practice document, these were reviewedbiannually.
• The theatre and ward managers attended the monthlyHoD, and clinical governance meetings. We review bothward and theatre department meetings, but it was notclear from these minutes whether information wasalways being shared with the frontline staff.
Managing risks, issues and performance
The service used systems to manage performanceeffectively. They mostly identified and escalated relevantrisks and issues and identified actions to reduce theirimpact.
• The hospital had a risk register which was regularlyreviewed and updated to ensure risks were monitoredand appropriately managed. Heads of departmentsmanaged departmental risk registers which fed into thehospital register.
• The hospital had 38 risks identified across alldepartments, four of the risks related to theatres andone related to the wards. The hospital had identified itsfive top risks two of which related to the theatres andthe ward. The risk register included the majority ofconcerns we found during the inspection with theexception of the secure access to the theatredepartment.
• The daily 'comms cell' meetings Monday to Friday wereattended by representatives for each department. Themeeting covered a range of subjects including riskreview, recent incidents, health and safety update,training compliance review, and any concerns thataffected the hospital. This was cascaded to staff, so theygained a wider view of risk, issues and generalperformance within the hospital.
Surgery
Surgery
Good –––
36 BMI The Sloane Hospital Quality Report 11/10/2019

• The hospital had an audit programme that supportedthe hospital to ensure patient safety. Incidents, nearmisses and complaints are monitored for trend andimprovements actioned through action plans. Lessonslearned were cascaded to staff.
• The hospital’s monthly bulletin included informationabout changes in legislation, NICE guidance, andMedicines & Healthcare Products Regulatory Agency(MHRA) alerts.
Managing information
The service collected reliable data and analysed it. Data ornotifications were submitted to external organisations asrequired.
• Service performance measures were reported andmonitored by the hospital, BMI Healthcare and localcommissioners. These included data and notificationsthat required submission to external bodies.
• The hospital had access to patients' NHS treatmentrecords.
• Information technology systems were used effectively tomonitor and improve the quality of care. For example,the incident and complaints recording system providedthe hospital with a platform to monitor and assess risksand assess trends.
• Staff had secure access to the hospital’s intranet whichgave them access to a range of policies, procedures andguidance and their training and personal developmentrecords.
• Consultants had access to a BMI ‘Consultant App’ whichgave them remote login to clinics and theatre lists on asmartphone. The app enabled consultants to accessclinic and operating theatre data. The application wasdownloaded using BMI credentials. No data was storedon the phone and a time out was applied for security.
• BMI had group policies and processes in placegoverning Information Governance, Security andPersonal Data Protection. All data controllerregistrations for the processing of personal data weremaintained in accordance with the requirements of theUK Information Commissioners Office.
• The Groups Information Security and Governancepolicies were compliant with ISO/IEC27002 the Code ofPractice for Information Security Management, withsecurity risk management and regular independentauditing undertaken to satisfy these requirements.
• BMI held and maintained formal certification to ISO/IEC27001:2013 relating to the operation andmanagement of its Information Security ManagementSystem (Certificate Number: CI/144541S). BMI managesits information security obligations based on continualimprovement with Information Security Managementforming a key part of the BMI Information ManagementCommittee function.
• BMI annually submitted, and was compliant with, theNHS HSCIC / NHS Digital Information GovernanceStatement of Compliance - IG Toolkit. BMI was alsocompliant with the Payment Card Industry Data SecurityStandard – PCI-DSS (PCI Security Standards Council).
Engagement
The service engaged with patients and staff.
• The hospital had introduced patient journey meetingsto aid communication, teamwork and collaborationacross all departments to identify how to improve theservice provided to patients. The meeting hadrepresentatives from all departments and a patientrepresentative attending the bi monthly meetings. Anoutcome from the meetings was that dignity championshad been appointed in the theatres and on the wardsand dignity boards were displayed in the hospital diningroom.
• The hospital gathered patients’ feedback which wasmonitored monthly through the patient satisfactiondashboard. The top most improved satisfaction scoreform March 2018 to March 2019 was the number ofpatients who had received a follow up call which hadincreased by 33.8% from 49.2% in March 2018 to 83% inMarch 2019.
• The hospital encouraged staff to attend staff forums,including the ED open forum and ‘Sloane Says’meetings.
• Information was shared with staff daily at the dailycommunication cell (comm cell) meeting,representatives from each department fed back to theirteams through daily brief and handover meetings.Information is also cascaded by email, and monthlydepartmental meetings.
• The annual BMiSay employee survey for 2018 showedthat 67% of staff at BMI Sloane were satisfied workingfor BMI healthcare and 98% were committed to doingtheir very best for BMI Healthcare.
Surgery
Surgery
Good –––
37 BMI The Sloane Hospital Quality Report 11/10/2019

• BMI healthcare had recently introduced a new longservice award that rewarded staff who had worked forBMI healthcare. The long service award was given everyfifth anniversary from five to forty years for more thanfive years.
Learning, continuous improvement and innovation
The service was committed to continually learning andimproving services. They had a good understanding ofquality improvement methods and the skills to use them.
• The hospital had a rolling refurbishment plan whichincluded installing hand hygiene sinks and laminateflooring on Langley ward.
• Two rooms on Langley wards had been re-designatedfor ambulatory care patients which could accommodatesix patients and a room had been set aside for meetingwith ambulatory patients.
• Members of the senior team were encouraged tocomplete the ILM management courses and theintroduction of leadership training to facilitate,encourage and allow managers to develop within theirrole.
Surgery
Surgery
Good –––
38 BMI The Sloane Hospital Quality Report 11/10/2019

Safe Good –––
Effective Good –––
Caring Not sufficient evidence to rate –––
Responsive Requires improvement –––
Well-led Inadequate –––
Information about the serviceServices for children and young people focused mainly onoutpatients, with a small number of surgical cases beingcarried out.
The hospital did not have paediatric nurse on site all thetime, however it had a service level agreement with anearby BMI hospital to provide paediatric nursing supportover the phone and in person as defined by the agreement.
The hospital did not perform interventional procedureson children and young people younger than 16 as therewas no paediatric nurse on site. Patients aged three to 16were only permitted to have consultations with specialists.If interventions were needed they were referred to othersites with paediatric nurses present. The exception to thisrule was in physiotherapy where there was a paediatricphysiotherapist who cared for children and youngpeople children and young people aged from six to 18years. Children and young people aged 16 and 17 wereassessed prior to surgery to determine whether they weresafe to have surgery on site without a paediatric nursepresent.
Children and young people were cared for in the sameareas within the hospital as adults. There was aninconsistent approach to making the waiting roomssuitable for children and young people. As part of theinspection of children and young people services weinspected both hospital inpatient wards, the outpatient,pre-assessment areas and the physiotherapy department.
The main service provided by this hospital was surgery.Where our findings on surgery, for example, managementarrangements, also apply to other services, we do notrepeat the information but cross-refer to the surgery report.
Activity
The children and young people service accounted forabout 553 of 32,000 attendances in the last year (March2018 to February 2019). Of these, 360 were aged betweenaged 3-15 years and 193 were aged 16-17.
Are services for children & young peoplesafe?
Good –––
We rated safe as good.
Mandatory training
The service provided mandatory training in key skills to allstaff and made sure everyone completed it.
• The service had an induction package that included allmandatory training, in a range of formats includinge-learning and face-to-face. Training and competencylevels were monitored for agency and bank staff as wellas permanent staff. Managers explained they recordedand monitored training compliance using the "BMIlearn" tool. There were a few mandatory coursesrelating to the care of children and young people, theseincluded paediatric resuscitation and safeguardingtraining at various levels depending on specific job role.
• Nurses said they felt the training they received wassuitable and supported them to carry out their role.
• Four members of theatre staff had completed PILStraining, which was 80% compliance with assignedtraining. 12 ward nurses had completed PaediatricImmediate Life Support (PILS) training. This was 100%
Servicesforchildren&youngpeople
Services for children & youngpeople
Requires improvement –––
39 BMI The Sloane Hospital Quality Report 11/10/2019

compliance assigned PILS training. PILS training istraining aimed at giving healthcare professionals theskills and knowledge to treat seriously ill children orchildren whose heart is stopping.
Safeguarding
Staff understood how to protect patients from abuse andthe service worked well with other agencies to do so. Staffhad training on how to recognise and report abuse andthey knew how to apply it.
• Ward staff mandatory training figures showed all 23nurses had completed their level one childsafeguarding, 22 nurses had completed their level twosafeguarding and one nurse had completed level threesafeguarding. This was 100% compliance with trainingassigned to each individual. One ward nurse had notcompleted their female genital mutilation (FGM)training.
• Theatre staff mandatory training figures showed that all19 staff had completed their level one childsafeguarding, 15 members of the team had completedlevel two safeguarding and one member of the teamhad completed level three safeguarding. This was 100%compliance with training assigned to each individual.Three members of theatre staff had outstanding FGMmandatory training.
• Physiotherapy had two members of staff trained to levelthree safeguarding and ensured one was alwaysworking when children were present in the department.
• Ward staff and physiotherapists were able to giveexamples of when they would highlight safeguardingconcerns and knew who to raise them to. Physiotherapystaff were able to recall times they had raisedsafeguarding concerns.
• The hospital’s policies on children and youngpeople children and young people safeguarding were indate and made accessible to staff through notice boardsor online. Staff were aware where to find the policiesshould they need them.
• Managers followed safe practices for recruiting staff andallowed delays if needed to make sure all checks hadbeen completed.
Cleanliness, infection control and hygiene
The service controlled infection risk well. Staff usedequipment and control measures to protect patients,themselves and others from infection. They keptequipment and the premises visibly clean.
• In response to the previous ward inspection there wasan ongoing programme to ensure each room hadhandwashing facilities. This work was not yet completedwith some rooms only having hand washing facilities inthe bathroom.
• Staff used “I am clean” stickers to indicate they hadcleaned the equipment recently and it was ready for useby another patient.
• All staff in clinical areas were “bare below the elbows”,had their hair tied back and wore clinically appropriateclothing.
• There were regular hand hygiene audits carried out inthe hospital in all the areas children and young peoplewere treated. Observational hand hygiene audits forMarch 2019 demonstrated a compliance of 100% in thetheatres and on the wards
Environment and equipment
Generally the design, maintenance and use of facilities,premises and equipment kept people safe. Staff weretrained to use them.
• Resuscitation trolleys were appropriately located in thewards and outpatient department, with specificpaediatric ‘grab bags’ in reception and thephysiotherapy department. ‘Grab bags’ are bags thatcontain specific equipment needed in an emergency toallow procedures to be carried out on children. Therewas no signage around the resuscitation trolleyreminding staff of the location of the nearest ‘grab bag’,but all staff we spoke with knew its location.
• Equipment in the paediatric grab bag in reception wasincomplete. The contents had been checked andsigned, but some items were missing; one was out ofdate and others were inappropriate for use. Thisincluded no small cannulas for accessing children’sveins and suction equipment that did not fit the suctionmachine. This had not been noted during the bag’sregular checks. We raised this with staff and the issueswith equipment were immediately resolved. Thehospital was carrying out an investigation to find outhow this had happened.
• We raised concerns about security of theatres, whereyoung adults were operated on. Hospital managers
Servicesforchildren&youngpeople
Services for children & youngpeople
Requires improvement –––
40 BMI The Sloane Hospital Quality Report 11/10/2019

were aware of the risk and there was a business case inplace to improve the security. In response to ourconcerns they made arrangements to ensure the theatrereception was manned from 8.00 am until theatreclosed to maintain a secure environment. A permanentswipe card system was due for installation in the weekcommencing 1st August 2019.
• Young people were cared for on the same wards asadults. Adults and young people were cared for in singlerooms on the wards.
• Physiotherapy staff completed a daily environment riskassessment to make sure the environment of thewaiting and treatment rooms were safe for children andyoung people. Posters in the waiting room remindedparents and carers of their responsibility to take care oftheir children and that there were doors between thewaiting room and any staircases.
• Outpatient staff were introducing a daily riskassessment to make sure the environment in thewaiting room was safe for children and young people.There were no notices in the waiting areas to warnparents or carers of the risk of open staircases. While weacknowledge the waiting areas had to haveunobstructed access for fire safety reasons, there wereno notices to remind parents of the potential risks.
Assessing and responding to patient risk
Staff completed and updated risk assessments for eachpatient and removed or minimised risks.
• The hospital did not have a service level agreement totransfer critically unwell patients. All staff were aware ofthis and they were able to detail how they wouldtransfer a critically ill patient, by dialling 999 and makingthe operator aware they were not a critical care centre.This was highlighted on the hospital risk register andwas being progressed by the clinical services manager.This risk was reduced by only allowing children andyoung people under the age of 16 to have consultationsin the hospital and screening children and youngpeople aged 16 and 17 to check suitability to enter theadult pathway if having surgery.
• Information provided by the hospital showed that threechildren under the age of three had been treated in theprevious year, the hospital should only accept childrenand young people age three and above for consultation.We asked about this during the inspection and senior
staff were unable to confirm if it was correct. They toldus they were not aware of the visits and they had notbeen highlighted to anybody and as such noinvestigation, action plan or changes had been made.
• There were strict criteria for the treatment of childrenand young adults within the hospital. The criteriaincluded that young people aged 16 and 17 would onlybe admitted for routine uncomplicated elective surgicalprocedures and that procedure bookings were not to beconfirmed until the pre-assessment team had assessedthem to be “clinically appropriate”. The risk assessmentshown to us was thorough and screened patients forother illnesses and potential care issues that could leadto complications. The risk assessment providedinstructions for where to book children and youngpeople if they were unsuitable for treatment at thehospital.
• No children and young people under the age of 16 werepermitted to have any invasive procedures.
• Pre-assessment staff assessed young people to makesure they were safe to follow an adult surgical pathway.These checks included the young person and theirparent/guardian being informed there was not apaediatric specialist on site at the time of surgery andbeing offered to have treatment elsewhere.
• The hospital had processes to minimise the risk of nothaving a paediatric nurse on site at the time of surgery.They included communication with the paediatric nurselead for the area to ensure they were aware of surgerytimings to ensure they were available for support ifrequired.
• The hospital used the national early warning scoresystem (NEWS) to detect any potential deterioration inpatients. It was hospital policy to screen young peopleat the pre-assessment stage to ensure they were able tofollow an adult pathway. Accordingly, the paediatricversion of the NEWS was not employed.
• Physiotherapy staff completed specific children andyoung people risk assessments before a child or youngperson receive any physiotherapy treatment.
• Staff followed the five safer steps to surgery and theycompleted the World Health Organisation’s (WHO)checklists. The WHO checklist is a checklist developedto decrease errors, adverse events and increaseteamwork and communication in surgery. For detailedinformation about WHO compliance please refer tosurgery.
Servicesforchildren&youngpeople
Services for children & youngpeople
Requires improvement –––
41 BMI The Sloane Hospital Quality Report 11/10/2019

• Resuscitation simulations were practiced within thehospital three times a year. This was provided throughan external provider and simulations wereunannounced. These scenarios were followed up with areport detailing any areas for improvement. A recentexample provided simulated a ten-year-old patientsuffering an asthma attack in the outpatientdepartment.
• The Resident Medical Officer (RMO) was trained toadvanced levels of paediatric resuscitation. The RMOwas available on site at all times, staying on siteovernight. The hospital had three RMOs working on arotational basis to make sure they were not overworkedor overtired.
Nurse staffing
• In line with BMI policy, the hospital did not have apaediatric trained nurse on site but, had anarrangement to access paediatric nursing advice orsupport from another hospital close by. This risk wasalso reduced by following procedures to screen childrenand young people for suitability to have treatment atthe site.
Medical staffing
The service had paediatricians available on Saturdays torun their clinics. In the week children and youngpeople were seen by specialists such as dermatologists ona consultation only basis.
• For more detailed findings on medicines please see theSafe section in the surgical report.
Records
Staff kept detailed records of patients’ care and treatment.Records were clear, up-to-date and stored securely.
• All 10 records we reviewed were complete. Theyincluded pre-assessment checks, appropriatelycompleted consent forms, surgical notes, ward notesand discharge paperwork. Notes also clearly identifiedwhen a patient had any allergies.
• Staff in pre-assessment demonstrated how youngpeople were identified to theatre staff on computersystems as well as in physical notes created prior to theprocedure.
• We saw discharge paperwork in all sets of notes that wereviewed. The discharge paperwork was clear andsummarised what was found in the notes and in all
cases gave medication recommendations. In all notesthere was a record of an attempt of contact follow upapproximately 48 hours after surgery. This was notedwhen contact had not been successfully made.
Medicines
Notes reflected that pain relief was administered andmonitored after surgery. When required young people weredischarged with pain relief and a discharge summarydetailing how and when to take them.
• For our detailed findings on medicines please see thesafe section in surgery.
Incidents
Staff did not always recognise issues that needed to bereported and managed. However, they were able to providesome examples of learning from incidents.
• Staff were able to explain the way incidents werereported and the various routes, including face to facemeetings and emails that they would expect to receivefeedback. Staff told us they shared learning betweenhospitals within the hospital group, allowing for learningfrom incidents at other BMI hospitals.
• Staff did not always remove and report safety issues. Anexample of this was the paediatric ‘grab bag’ detailedearlier.
• Staff were able to provide an example of an incidentwhen a young person was in theatres without the leadpaediatric nurse being aware of this. The procedure wascancelled and the patient moved to another hospital.Staff could detail the learning and changes in processesthat arose from this this event. Changes to practice werereflected in notes checked dated after the incident.
Safety Thermometer (or equivalent)
For our detailed findings on safety monitoring please seethe safe section in surgery.
Are services for children & young peopleeffective?
Good –––
We rated effective as good.
Evidence-based care and treatment
Servicesforchildren&youngpeople
Services for children & youngpeople
Requires improvement –––
42 BMI The Sloane Hospital Quality Report 11/10/2019

The service provided care and treatment based on nationalguidance and evidence-based practice.
• Pre-assessment staff followed strict criteria for youngpeople to have surgery at the hospital. If there wereconcerns about a patient’s condition or co-existingconditions these would be discussed with the leadpaediatric nurse for the area and the patient transferredto another hospital with more support. Notes reviewedevidenced venous thromboembolism (VTE) riskassessments, as per assessment criteria. VTE meansblood clotting in the veins.
• There was a children and young person operationalmanual that defined training and staffing needs for thecare of children and young people. This was brokendown into age groups and type of interaction forexample consultation only or interventional work suchas surgery. This was aimed at making sure children andyoung people were cared for by the right person at theright time. This manual also stated the consentprocedure for children and young people and thepre-assessment, admission and discharge pathways.The document referenced up to date guidance from avariety of agencies and made reference to best practiceand national guidance for the care of children andyoung people.
• There was more focus on children and young person inphysiotherapy compared with outpatients and clinicalareas. During our inspection we found that staff on thewards, theatre and outpatients were unaware ofthe child and young person's pathway and could notdefine their roles within it. In contrast to this, staff inphysiotherapy and pre-assessment knew their roles inthe pathway and the mechanisms in place to ensurethey were safely treated.
Nutrition and hydration
At the time of inspection there were no children beingtreated therefore nutrition and hydration could not beassessed.
• Staff told us fasting prior to surgery was usually six toeight hours for food, and two hours for clear fluids priorto surgery.
Pain relief
At the time of inspection, no children were being treatedand therefore immediate pain management could not beassessed.
• However, we saw that pain management wasdocumented in patients notes post operatively. Painchecks were evidenced in post-operative care notes anddischarge paperwork made clear reference to how andwhen to take pain relief if required.
Patient outcomes
• The provider did not collate audit data to monitor theoutcomes of children and young people afterappointments or procedures.
• The paediatric lead nurse knew of the overarchingpaediatric audit but, thought it was out of date andneeded repeating. Following our inspection, thehospital confirmed that the audit was in date and duefor re-audit in Autumn 2019.
Competent staff
The service made sure staff were competent for their roles.Managers appraised staff’s work performance and heldsupervision meetings with them.
• Training surrounding children and young people'scare was limited to life support and safeguarding. Asthere were no paediatric nurses permanently employedby the hospital training did not extend beyondmandatory courses for nurses.
• Managers were able to evidence and check staffcompetency using the “BMI learn” software. This heldthe training records for permanent members of staff.Managers were also able to detail how they ensuredbank or agency staff training records were checked tomake sure they were competent and safe to practice intheir role. The IT software flagged to managers when amember of staff required an update and staff describedhaving time to carry out their training.
• Staff we spoke with said they felt there was goodencouragement for development, with some of themprogressing from clinical members of the team tomanagement level. Examples of heads of departmentbeing put on leadership courses were given.
• The clinical services manager detailed the system inplace to identify when nurses were due for revalidationand the process in place should the nurse miss theirdeadline.
• In physiotherapy a member of the team detailed howtheir training was coordinated with other BMI hospitalsto run larger training sessions, with specific learningdirected towards children and young people. This was
Servicesforchildren&youngpeople
Services for children & youngpeople
Requires improvement –––
43 BMI The Sloane Hospital Quality Report 11/10/2019

funded by the hospital. The paediatric physiotherapisttold us in addition to the mandatory training they hadattended courses and training with specialist focuson children and young people's care. An example of thistraining was a course about the muscle growth ofchildren.
Multidisciplinary working
Doctors, nurses and other healthcare professionals workedtogether across sites to maintain safety.
• Pre-assessment staff, the wards and the theatre teamwere able to communicate with the lead paediatricnurse based off site should they have any concernsabout a child or young person. Discussions of thisnature were documented in patient notes in line withthe service level agreement the paediatric nurse hadwith the hospital.
Seven-day services
Services were made available outside of school hours tosupport patient care.
• Paediatricians had dedicated Saturday clinics to seepatients on the weekend, outside of school hours. Otheroutpatient clinics had timings throughout the week thatincluded evenings to allow children and youngpeople to attend.
• The physiotherapy department had Saturday andevening clinics, outside of school hours. These werestaffed by a member of the team trained to treatpaediatric patients.
Health promotion
There were no specific leaflets designed to help promotehealthy lifestyles to children.
• During the inspection there were no children beingtreated therefore staff interactions could not bereviewed.
Consent, Mental Capacity Act
• Patients with mental capacity problems would bereferred elsewhere in line with hospital guidelines.
• We saw the hospital had a specific consent formfor children and young people. The form had both aplace for their parent or guardian to sign and for thechild or young person to sign if they wanted to. In the
records we viewed these were all signed. The use of thisform was laid out in the hospital's children and youngpeople operational manual, which explained howand when it should be used.
Are services for children & young peoplecaring?
Not sufficient evidence to rate –––
We have not rated caring as during the inspectionno children or young people were being treated thereforewe could not assess whether care was compassionate.
Compassionate care
During the inspection there were no children being treatedtherefore we could not assess whether compassionate carewas provided.
• The hospital only had one format of friends and familytest on the ward that young people and adults could fillout. They were unable to separate out responses fromchildren or young people.
Emotional support
During the inspection there were no children being treatedtherefore we could not assess whether emotional supportwas provided.
Understanding and involvement of patients and thoseclose to them
Staff supported and involved patients, families and carersto understand their condition and make decisions abouttheir care and treatment.
• Pre-assessment staff completed their risk assessmentand checks consulting both the patient and their parentor guardian when the patient was under the age of 18. Inthe first instance this was completed with a telephoneconsultation but was able to be extended to a face toface consultation if required. This allowed children andyoung people and their families to be involved in thediscussion about their care.
Are services for children & young peopleresponsive?
Servicesforchildren&youngpeople
Services for children & youngpeople
Requires improvement –––
44 BMI The Sloane Hospital Quality Report 11/10/2019

Requires improvement –––
We rated responsive as requires improvement.
Service delivery to meet the needs of local people
• The outpatient clinic area was not child friendly forexample there were no toys available and waiting roomswere open to staircases without signs to alert parents tothis. The hospital has since told us that toys wereremoved from the waiting room as the waiting time forpatients was less than 10 minutes.
• We saw that the tea/coffee machines had notices toalert parents and patients that they contained hotwater.
• Young people undergoing procedures were cared for onadult wards. However, they did not stay overnight andall rooms were single occupancy.
• In the physiotherapy department there were toys andbooks for children, the waiting room had a door thatcould be closed to separate it from the stair case. Tea/coffee machines had notices to alert people they werehot.
• Wi-Fi was available throughout the hospital and wasfree to use for all people on the premises.
Meeting people’s individual needs
Staff referred children and young people to other services ifthey were unable to accommodate their needs. Theycoordinated care with other services and providers.
• The hospital had criteria for young people to beassessed and treated, if patients did not meet thecriteria they were referred to another hospital nearbythat could accommodate their needs. This was overseenby the paediatric lead nurse who covered threehospitals that were located close together.
• The catering team explained how they would speakwith young people to assess their personal preferences.
• All ward rooms had a television provided free of chargefor patients admitted.
• There was a chaperoning policy specifically for childrenand young people. This policy set out the needfor children and young people to be offered a
chaperone for examinations but left the ultimatedecision to the patient and parent or guardian. Thepolicy laid out the processes for recording the decisionto, or not to, have a chaperone.
Access and flow
People could access the service when they needed it andreceived the right care promptly.
• Paediatric clinics were scheduled at appropriate timesthroughout the week to avoid school hours. Forexample, the paediatricians’ clinics were scheduled forSaturdays and the physiotherapy team had a paediatricphysiotherapist working evenings and on Saturdays.
• All children or young children seen at the hospital wereprivately funded, there were no waiting lists. Any delaysto treatment were due to the risk assessments beingcarried out.
Learning from complaints and concerns
It was possible for people to give feedback and raiseconcerns about care received. The service treated concernsand complaints seriously, investigated them and sharedlessons learned with all staff. However, the hospital had novariation to the complaints procedure to make it childfriendly if needed.
• Managers showed evidence of discussion about acomplaint related to a young person’s care beingdelayed; we saw the evidence of learning from thecomplaint and the changes made to practice in light ofit. This change in practice was then evidenced in thenotes checked dated after the resolution.
Are services for children & young peoplewell-led?
Inadequate –––
We rated well-led as inadequate.
Leadership
Leaders were in place to run the children and youngperson's service. However, the service was small incomparison to the adult service and there was littleeffective day to day management. In physiotherapy therewas more effective day to day management of children andyoung people's pathways.
Servicesforchildren&youngpeople
Services for children & youngpeople
Requires improvement –––
45 BMI The Sloane Hospital Quality Report 11/10/2019

• The paediatric nurse who was in place to overseethe children and young people's services was based atanother hospital and attended the site four times a year.The paediatric lead nurse was available to call ifconcerns arose and nurses knew who they needed tocontact. Since inspection we were informed from theend of July 2019 the paediatric lead nurse will be on siteonce every two weeks.
• Due to the paediatric lead not being present on site,there was little day to day monitoring of the service. Thelack of oversight was evident in discussions with nursingstaff and the concerns we found with the paediatric grabbag.
• The director of clinical services had oversight of theheads of department on site, training and competenciesand the governance of the hospital. They were able tooutline the process that children and youngpeople should follow in the hospital and were aware ofthe incident where processes had not been followedand the changes implemented from this.
• The physiotherapy department had a more definedstructure for children and young people's pathways.Responsibilities were clearly defined as there was anamed lead physiotherapist who took responsibility forthe care of children and young people.
Vision and strategy
The service did not have a vision for children and youngpeople's services.
• In senior team meetings children and young peoplewere not a stand-alone agenda item however, anyincidents or complaints relating to the service werediscussed at governance meetings.
• Following the inspection, we have been informed thatthe lead paediatric nurse will now be routinely involvedin the monthly clinical governance meetings
Culture
• Staff said there was a ‘family feel’ to the organisationand they felt supported. Many of them had worked atthe hospital for a long time.
• There was evidence, discussed earlier, of answering andresolving complaints and using that learning to improvepatient pathways in the future.
• Since inspection we have been provided with thephysiotherapy department clinical governance minutesthat show discussion about children and youngpeople's services.
Governance
The children and young people's service was lacking aneffective governance process, with members of staff unableto locate protocols immediately. The hospital did notroutinely discuss the service at key meetings.
• Young people undergoing procedures as day case wereon the adult pathway and staff followed all adultpolicies.
• Hospital governance and Medical Advisory Committee(MAC) meeting agendas made no reference to childrenand young people's services. The only specific instanceof services being discussed in minutes provided by thehospital was in a MAC meeting following an incident anddoctors were asking for clarification on the assessmentcriteria. At the time of inspection this had been rectifiedand clarification given.
Managing risks, issues and performance
• The hospital had a risk register. There were no directissues relating to children and young people on theregister, although we found some concerns during theinspection.
Managing information
The service did not demonstrate reliable data collectionand analytics with regards to children and young people.
• During the inspection we were informed of threechildren aged below three years old who had beentreated in the hospital in the last year which was not inline with their policy or statement of purpose. Astatement of purpose lays out the broad types ofservices a healthcare institution will offer. Whenmanagers were asked about this they were eitherunaware of the data or were unable to answer how ithad happened and believed it could have beenmisinformation provided to us.
• The service initially provided us with incorrect dataregarding the number of young people who hadundergone surgery between 1st March 2018 to 1stFebruary 2019. This raised concerns about the reliability
Servicesforchildren&youngpeople
Services for children & youngpeople
Requires improvement –––
46 BMI The Sloane Hospital Quality Report 11/10/2019

of the data for the service. When asked, the service wasable to give accurate information about surgicalpatients and was launching an investigation as to howthis data had been collated.
Engagement
• The hospital collaborated with partner organisations tohelp improve services for patients. The hospital engagedwith partner hospitals to share the lead paediatric nursebased at another BMI hospital.
Learning, continuous improvement and innovation
There was evidence of learning from when things had gonewrong.
• Managers were able to provide evidence from anincident where there was a near miss with a patientnearly being treated before being appropriatelypre-assessed. The procedure was cancelled and movedto another hospital with appropriate support. Since thisincident the young person pre-assessment pathway hasbeen clarified to consultants and documentation ofproposed treatment has been standardised.
Servicesforchildren&youngpeople
Services for children & youngpeople
Requires improvement –––
47 BMI The Sloane Hospital Quality Report 11/10/2019

Safe Good –––
Effective
Caring Good –––
Responsive Good –––
Well-led Good –––
Information about the serviceThe outpatient department (OPD) is located on the firstfloor of the main hospital complex and comprises 12consulting rooms and a treatment room. Two of theconsulting rooms are designated and specially equippedfor dealing with eye (Ophthalmic) disease and ear, noseand throat (ENT) conditions.
The department is responsible for a phlebotomy (bloodtesting) service and surgical pre-assessment clinic, whichoccupy adjoining rooms. The hospital pharmacy and aGP service are also located on the same floor and sharewaiting areas with OPD. The GP service is operated byanother registered provider and is not included in thisinspection.
Diagnostic imaging services are based on the groundfloor of the hospital and includes MRI, CT, DigitalMammography and Ultrasound. This service is operatedby another registered provider and is not included in ourinspection.
There is a separate outpatient physiotherapy departmentconsisting of a gym, a studio and five physiotherapyconsulting rooms.
The OPD hold clinics every week for adults and children,in a wide range of specialities. Of the 24 specialismsoffered, the five with the largest percentage of patientsare general surgery, orthopaedics, ophthalmology, ENTand gastroenterology.
This report focusses on outpatient services for adults. Ourreport on services for children and young people isshown in a separate section. During the inspection, wespoke with 14 staff including a consultant, manager,registered nurses, physiotherapists, pharmacists, hospital
engineer, health care assistants, phlebotomy andadministrative staff. We spoke with six patients and onerelative. In addition, we reviewed policy and proceduredocuments and 10 sets of patient records.
Activity (March 2018 to February 2019)
• There were 32,000 attendances in the reportingperiod; of these 84% were funded through medicalinsurance or privately and 16% were NHS-funded.
Are outpatients services safe?
Good –––
Our rating of safe stayed the same. We rated it as good.
Mandatory training
The service provided mandatory training in key skills toall staff and made sure everyone completed it. Staffcompleted mandatory training using a combination ofonline learning and practical skills sessions.
• Online training utilised computer software was providedby BMI Healthcare, who also stipulated the topics to becovered each year. These included basic or intermediatelife support skills training, infection prevention andcontrol, information governance, safeguarding (adultsand children), fire safety and manual handling. Duty ofCandour, documentation and other legal aspects topicswere integral parts of the information governancemodule.
• We were shown data that indicated outpatientdepartment staff had achieved 100% compliance. The
Outpatients
Outpatients
Good –––
48 BMI The Sloane Hospital Quality Report 11/10/2019

outpatient manager explained that compliance statuswas reported to the monthly head of departmentmeeting and benchmarked with other BMI hospitals as akey performance target.
• We saw training status displayed on a large ‘dashboard’sited in the staff corridor leading to the canteen. Thislocation was used for the daily briefing and meant thatmanagers and any passing staff could easily checkdepartmental performance. In addition, the hospitalemployed a clinical educator who coordinated trainingand maintained oversight of individual training status.
• Staff we spoke with were positive about the trainingprovided and were confident they would be supportedto attend additional training if requested.
Safeguarding
Staff understood how to protect patients from abuse andthe service worked well with other agencies to do so. Staffhad training on how to recognise and report abuse, andthey knew how to apply it.
• Patients we spoke with said they felt safe and werealways treated respectfully by staff.
• Both adult and child safeguarding training was providedand we saw that outpatient nurses and physiotherapistswere trained to level two and key clinical staff at thehospital trained to level three. Safeguarding roles andtraining were aligned with BMI healthcare policy andnational guidance contained in the ‘SafeguardingChildren and young people: roles and competencies forhealthcare staff, published by the Royal College ofPaediatrics and Child Health in 2014.
• Staff we spoke with demonstrated a good awareness ofwhat to do if they had safeguarding concerns and whoto contact should they require advice. Staff correctlynamed the director of clinical services as the lead forsafeguarding at the hospital. We saw laminated postersdisplayed in the department showing ‘flow chart’prompts on how to report any safeguarding concerns.These were up to date and clearly described keyindividuals at local and corporate level and includedtheir contact details.
• Outpatient staff could not recall any recent safeguardingconcerns. We were told that last year, one patientattending an appointment disclosed that a child wasleft at home alone. Staff described the reporting stepstaken, which resulted in the case being referred to thepolice.
• Female genital mutilation and child sexual exploitationawareness were incorporated into safeguarding trainingwhich was delivered as part of the statutory andmandatory training programme as well as in inductioncourses for new staff.
• The service had a well-defined recruitment pathway andprocedures to help ensure that the relevant recruitmentchecks had been completed for all staff. This included adisclosure and barring service (DBS) check every twoyears, photo-ID confirmation, occupational healthclearance, references and qualification and professionalregistration check.
Cleanliness, infection control and hygiene
The service controlled infection risk well. Staff usedequipment and control measures to protect patients,themselves and others from infection. They keptequipment and the premises visibly clean.
• Since our last inspection, the hospital had commenceda programme of replacing the handwashing sinks to aversion fully compliant with department of healthguidance (HBN 00-10 Part C ‘sanitary assemblies’ andHealth Building Note 00-09 ‘infection control in the builtenvironment’). We saw examples of the new sinksinstalled and the outpatient manager identified theones in the department still to be upgraded.
• In addition, carpeted flooring throughout thedepartment had been replaced by a seamless floorcovering which complied with department of health‘Health Building Note 00-10 Part A - Flooring’.
• We checked a variety of consulting, therapy and exerciserooms along with utility and store areas. Overall, alldepartments we visited had achieved a high standard ofcleanliness and hygiene. Rooms and store areas weretidy and free from clutter.
• In therapy rooms and equipment stores, wide use wasmade of ‘I am clean’ stickers. These showed the dateand time the article was cleaned along with the name ofthe person who cleaned it. We saw these details hadbeen completed in all cases, which meant staff couldquickly identify items that were ready for use.
• Chairs in waiting areas, consultation and examinationrooms were covered with ‘easy-clean’ fabric, whichcomplied with guidance on Health Building Note 00-09‘infection control in the built environment’ (Section3.133).
Outpatients
Outpatients
Good –––
49 BMI The Sloane Hospital Quality Report 11/10/2019

• Domestic staff cleaned the outpatient andphysiotherapy departments daily and we sawcompleted checklists indicating that rooms and toiletshad been cleaned. Outpatient and physiotherapy staffhad the responsibility for ensuring that each consultingor therapy room was clean and prepared for use. Theycompleted a daily cleanliness checklist and ensuredeach room was correctly stocked. These forms werecollated and audited by the department manager.
• We saw disposable curtains in use throughout thedepartment and these were marked with the datechanged. This complied with Health Building Note 00-09‘infection control in the built environment’ and indictedthat staff routinely changed curtains to help reduce thechances of germs passing from one person or object toanother.
• The hospital’s hand decontamination policy was currentand described when staff should wash their hands. Wesaw staff in outpatient following the policy and adheringto the World Health Organisation’s ‘Five moments forhand hygiene’. Antimicrobial hand-gel dispensers wereplaced at reception desks or mounted on walls atstrategic points in the department. These contained geland we observed staff using the product as they movedaround outpatients.
• All medical and clinical staff we observed during theinspection were ‘bare below the elbows’ in accordancewith good practice standards such as those shown innational institute of health and care excellence (NICE)clinical guideline 139.
• We saw ample supplies of personal protectiveequipment such as aprons and gloves in dispensers onwalls and we saw these items being used. Gloves werereadily available in wall mounted storage bins. The binswere divided into the full range of sizes. This meant staffhad convenient access to correctly fitting gloves, whichconsequently reduced the chance of accidental tearing.
• Fluid spillage kits were also readily available.• Sharps boxes were managed in accordance with the
Health and Safety (Sharp Instruments in Healthcare)Regulations 2013 (the Sharps Regulations). Clearlymarked and secure containers were placed in eachconsulting room and other areas where medical sharpswere used. Instructions for staff on the safe disposal ofsharps were displayed on the walls above the bins.
• The hospital had introduced ‘reusable’ sharpscontainers, which reduced the environmental impactassociated with single-use plastic containers. outpatientstaff expressed pride in this innovation anddemonstrated their safe use and features.
• Waste in the clinic rooms was separated and placed indifferent coloured bags to identify the various categoriesof waste. Portering staff removed the clinical waste atthe end of clinic and placed them in bulk storage bins.We saw that waste was correctly separated and kept inlocked and labelled bulk storage bins, on the hospitalpremises until collected. This complied withdepartment of health ‘Technical Memorandum (HTM)07-01, control of substance hazardous to health andHealth and Safety at Work regulations’.
• Our observations were supported by local audit scoresand the 2018 patient-led assessment of the careenvironment survey. This showed the trust scored99.9%, for cleanliness, which was better than theEngland average of 98.5%.
Environment and equipment
The design, maintenance and use of facilities, premisesand equipment kept people safe. Staff were trained touse them. Staff managed clinical waste well.
• The outpatient and physiotherapy environments weobserved supported the safe delivery of diagnosis,treatment and therapy. For example, consultationrooms were well lit, air-conditioned and equipped withsufficient stocks of sterile consumables held inpurpose-built trolleys.
• Corridors, rooms and toilets were spacious with doorswide enough to accommodate people usingwheelchairs. Entryways to the hospital had droppedkerbs to assist wheelchair users or those with limitedmobility reach the building. The entrance to thephysiotherapy building utilised a low-incline, non-slipramp with handrails. Lift access was provided to the firstfloor of the hospital. Disabled parking spaces and a‘drop off' bay were sited close to the main entrance anddoors were automated, again assisting people livingwith less mobility.
• Each consultation or therapy room had a call buttonmodule fitted next to the clinician’s desk. Two differentlycoloured and shaped buttons were provided: one wasan emergency assistance alarm and the other tosummon a nurse or reception colleague to assist with
Outpatients
Outpatients
Good –––
50 BMI The Sloane Hospital Quality Report 11/10/2019

chaperoning or another task. The system included anaudible alert, a display screen at the reception stationand signal lights in the corridor. These gave an ‘at aglance’ indication of the area and room where the callwas made. These features helped to ensure thatcolleagues could provide rapid assistance whenneeded. In addition, emergency alerts automaticallyactivated pagers carried by the residential medicalofficer and senior clinical staff. These displayed thelocation of the area where the emergency alarm hadbeen activated so they could also render aid.
• Purpose-made emergency trolleys were sited in boththe outpatient and physiotherapy departments. Theseincluded portable oxygen, suction, defibrillator andmedication along with laminated prompt sheets andequipment checklist. The trolley in outpatient containedresuscitation items designed for use with adults and thephysiotherapy department had equipment bags forboth adults and children.
• These were stocked and checked daily on log sheets,which were collected by managers and auditedmonthly. Every device we checked functioned correctlyand each consumable item was ‘in date’, which wasconsistent with the logs maintained by outpatient staff.This indicated that department staff had an active focuson ensuring these items were ready for immediate useshould an emergency occur.
• In outpatients, clear signage was provided to show thelocation of the trolley if it was moved away from thenormal charging point. The department sister explainedthat the trolley had, on occasion been wheeled closer toa diagnostic room as part of routine risk mitigation.
• Patient examination couches, furniture and equipmentwere labelled with asset numbers and service orcalibration dates. This helped to provide assurance thatitems were controlled and maintained in accordancewith manufacturer recommendations and policyguidelines. We saw equipment logs maintained by thehospital engineer that helped senior managers keepoversight of the servicing and repair status of each item.
• Staff told us that the medical equipment was wellmaintained and none cited any problems in obtainingsufficient items for use. The store areas we visitedappeared clean and well-organised, with plentifulshelving and items clearly labelled.
• Overall, the facilities we saw were kept in gooddecorative order. We saw clear direction signs andinformation posters as well as room identification signs.
The name of the consultant using the room could beeasily changed and the door sign also showed ‘free’ orbusy’, which helped ensure patient privacy and dignitycould be maintained.
• A routine fire alarm test was conducted during ourinspection. Fire safety and evacuation equipment wasavailable throughout the department and we sawevidence that an external specialist contractor hadcompleted fire equipment safety checks.
• Safety signage and an interlock was fitted to the door ofthe ophthalmology room where diagnostic laserprocedures took place. This helped to keep staff andpatients safe by deterring people from entering whenprocedures were underway.
• A Laser Protection Officer from a local NHS trustoversaw the safe working of the Laser equipment in thedepartment, with a dedicated nurse from outpatient asliaison.
• The 2018 patient led assessment of the careenvironment survey showed the trust scored 93%, forcondition, appearance and maintenance, which wasjust less than the England average of 94%. Managersacknowledged the challenges of the hospitalconstruction, which was originally four large houses.Funding had been approved for upgrades to theflooring, both lifts and other aspects of the buildingsuch as the access ramp to the physiotherapydepartment. Managers explained that a planned ‘rollingrefurbishment’ programme was in place.
Assessing and responding to patient risk
Outpatient staff acted to minimise patient risk andquickly acted upon patients at risk of deterioration.Immediate or emergency assistance could be summonedby the use of the alarms fitted to each room and toilet.
• Medical assistance was provided by the residentmedical officer (RMO) and the patient’s consultant.
• Nursing staff told us they had good support from theRMO or consultant and senior clinicians whenever apatient’s deterioration was observed.
• There were clear and known protocols in place for thetransfer of patients to the local NHS accident andemergency facility by ambulance.
• An orthopaedic consultant explained that he was easilyable to refer any patients to other specialists at the
Outpatients
Outpatients
Good –––
51 BMI The Sloane Hospital Quality Report 11/10/2019

hospital, including a consultant physician who livedlocally and conducted twice weekly sessions at thehospital. This meant he could quickly access advice forany patients he was concerned about.
• Less urgent referrals could also be made to the in-houseGP service or the patient’s own GP.
• Nursing staff gave us examples of diagnostic clinicswhere potential risks were identified and the changesmade to mitigate these. This included pre-positioningemergency equipment and ensuring a trained staffmember remained with the patient.
Nurse staffing
The service had enough nursing and support staff withthe right qualifications, skills, training and experience tokeep patients safe from avoidable harm and to providethe right care and treatment. Managers regularlyreviewed and adjusted staffing levels and skill mix, andgave bank and agency staff a full induction.
• The outpatient clinics were staffed by registered nursesand health care assistants (HCA). The physiotherapydepartment comprised of receptionist, manager andphysiotherapists operating an appointment system andrehabilitation classes.
• Nursing cover was calculated dependent on the numberof clinics running and the numbers of patients attendingclinic as well as other factors such as procedure supportand chaperoning. There was always a minimum of twoqualified nurses on duty. HCAs assisted in clinics.
• The sister completed staffing rotas four weeks inadvance and there was a mix of early and late shifts, inresponse to planned clinics.
• According to data supplied by the hospital, outpatientshad no unfilled shifts during the last three months.Managers stated that when agency staff were requiredthey tried to utilise identified individuals and blockbookings to ensure continuity. We met an agencyphlebotomist and saw that the supervisor hadcompleted an induction checklist for this individual.
• We observed two of the daily “comm cell” briefingsessions conducted by the executive director, wherestaffing status was discussed with the senior team andresources allocated or moved as needed. We saw thatthis was a standing item on the meeting agenda.
• The outpatient manager explained that she was awayfrom the department on secondment to a sisterhospital. To bridge the gap the senior managementteam had recently promoted a registered nurse into asisters' post.
Medical staffing
Outpatient clinics were timetabled to suit eachspecialist’s availability and obligation as part of theconsultant’s practicing privileges contract. Every clinicwas run by a consultant who saw each patient on theirappointment list.
• Consultants in clinic could be assisted by the RMO incases where urgent or additional medical support wasrequired.
• Outpatient staff told us if a consultant had to cancel aclinic due to unforeseen circumstances then they (oradministration office staff) would telephone patients toinform them and either re-arrange the appointment oroffer an alternative consultant.
• Patients we spoke with said they had been able to getan appointment with their chosen consultant and withminimal delay.
• The executive director and chair of the hospital’smedical advisory committee (MAC) managed practicingprivileges and contracts for consultants.
Records
Staff kept detailed records of patients’ care andtreatment. Records were clear, up-to-date, storedsecurely, tracked and easily available to all staff providingcare. In the patient notes we reviewed we saw asatisfactory standard of record keeping. The recordscontained required information such as admissiondetails, progress notes and consent to treatment.
• Managers stated that the hospital had a dedicatedmedical records department with responsibility forfiling, storing and maintaining the medical record foreach patient treated. Files were prepared in advance ofoutpatient clinics using appointment lists generated byan electronic patient administration system. Staffshowed us that NHS and private patient notes weremanaged in the same way.
• Once the patient was discharged, the medical recordsdepartment was also responsible for scanning the files
Outpatients
Outpatients
Good –––
52 BMI The Sloane Hospital Quality Report 11/10/2019

onto a secure electronic database for archiving.Authorised outpatient staff were able to access thedatabase and print archived medical records ifrequested by a consultant, even during a clinic.
• In outpatients, we saw file cabinets located in an alcoveaway from public areas of the department. All cabinetswere kept locked and clearly labelled with colouredsigns showing clinic days. Staff operated a rolling filesystem which helped nursing and medical records staffallocate files into the correct cabinet for patients due toattend and patients who had been seen that day.
• The hospital supplied information that showed in thelast three months, no patients were seen in outpatientswithout all relevant medical records being available.Staff confirmed these figures when we spoke to them.
• Physiotherapy patient notes were recorded and storedseparately from the patients’ main file. Managersexplained that a pilot project was underway toamalgamate these records.
• Outpatient staff collated test results and included themin the medical record prior to the patient attendingclinic. We saw that histology results were received inpaper form and blood results using a secure networkprinter. Diagnostic images and reports were provideddirectly to the consultant a computer service that couldbe securely accessed from the clinic, another BMIhospital, or other authorised terminals.
• Patient notes were retained by the hospital. Completionof accurate and contemporaneous medical recordsformed part of the practicing privileges agreement for allconsultants. Consultants were registered as datacontrollers and any breaches in information securitywere reported to the senior managers at to corporatelevel.
Medicines
Outpatients, supported by the hospital pharmacy, usedeffective systems and processes to safely prescribe,administer, record and store medicines. The departmentdid not hold any controlled drugs.
• Medicines were stored in a designated room with doorssecured by mechanical code locks. Within the room, themedicines were stored in a locked cupboard that wasaccessed by keys held by the registered nurse in charge.This was in line with standards for good medicinesmanagement and helped to prevent unauthorisedaccess to medicines.
• Medicines requiring refrigeration were stored in lockedfridges. We saw the temperature of medicine fridges wasmonitored daily and the fridge temperature remainedwithin range. Ambient temperature of the room was alsochecked and recorded. Records were submitted topharmacy each month for auditing and archival. Thesemeasures provided assurance that medication wasstored within the manufacturer’s recommendedtemperature range to maintain their function and safety.
• Flammable medicines were kept in a lockable fireproofcabinet.
• Emergency medicines were available on resuscitationtrolleys which were secure, sealed and checkedregularly.
• Stock medicines were removed from the cupboards atthe start of clinic and placed in locked consultationrooms. During clinic, any stock kept in the consultationroom was the responsibility of the consultant.
• Outpatients held two types of prescription forms forprescribers to use: private prescription pads printed bythe BMI group and NHS FP 10 prescriptions. Both typeshad numbered pages and were held in labelled pouchescontaining an ‘issue and receipt’ record. Each pouchwas numbered to correspond with a consultation room.
• The nurse in charge kept the pouches in a lockedcupboard. Each prescription had a serial number on it.The nurse in charge gave a pouch to each consultant atthe start of clinic, who kept the pad with them. The padswere then checked and stored in a locked room at theend of clinic. Issue and receipt records were submittedto pharmacy each month for auditing and archival.These measures helped to reduce the chance ofprescription forms being lost or stolen.
• Consultants wrote prescriptions at the time of thepatient’s visit and these could be dispensed from thehospital pharmacy which was conveniently located nextto outpatients.
• We saw copies of the British National Formulary (BNF)Issue 77 in pharmacy and outpatient. This was the latestedition in print. The BNF is updated in book form twice ayear and details all medicines that are prescribed in theUK, with information about indications and dosages,contraindications, cautions and side effects. Thisindicted that an effective level of support was providedto the consultant in clinic. In addition, electronicversions of the BNF and hospital formularies wereavailable and we saw computer terminals in eachconsulting room.
Outpatients
Outpatients
Good –––
53 BMI The Sloane Hospital Quality Report 11/10/2019

• Medicine related alerts and recalls were communicatedvia email to the nurse in charge. The pharmacy staff alsodelivered a paper copy, and these were cascaded to allprescribers.
• There was good clinical pharmacy support and thepharmacist and the nurse in charge jointly managedmedicine stock levels.
• The pharmacy was open Monday to Friday 8 am to 5pm. There is one clinical pharmacist and one assistantor pharmacy technician available during opening hours.The RMO and senior nurse on duty had out of hoursaccess to the pharmacy and we saw the arrangementsin place to allow secure access and recordkeeping ofany medication dispensed.
• The hospital stored medical gases safely. Withinoutpatient and physiotherapy departments, we saw ‘indate’ cylinders of oxygen securely stored in holders.Regulators appeared clean and the cylinders were readyfor immediate use. In the hospital engineering section,we saw bulk cylinders stored in purpose-built rooms.The medical gas cylinder storage rooms were compliantwith department of health ‘Technical Memorandum02-0’. Additional cylinders were chained and locked toan external wall, but the valves had plastic covers andappeared to be dust and oil free. Overall, this indicatedthe hospital followed ‘the code of practice 44: thestorage of gas cylinders (2016)’ and ‘Technicalinformation sheet 36 (2017)’ from the BritishCompressed Gases Association.
Incidents
The service managed patient safety incidents well. Staffrecognised and reported incidents and near misses.Managers investigated incidents and shared lessonslearned with the whole team and the wider service. Whenthings went wrong, staff apologised and gave patientshonest information and suitable support. Managersensured that actions from patient safety alerts wereimplemented and monitored.
• In the reporting period, the department logged 68clinical incidents and no non-clinical incidents. We didnot identify any common themes from the incidents,and all involved different clinical specialities. The rate ofclinical incidents per 100 attendances was 0.2% whichwas lower than other independent hospitals we holdrecords for.
• Outpatients reported no serious incidents or neverevents. Never events are serious, preventable patientsafety incidents that should not occur if healthcareproviders implemented existing national guidance orsafety recommendations. Providers are obliged toreport never events for any patient receivingNHS-funded care. The occurrence of never events canhighlight potential weaknesses in how an organisationmanages fundamental safety processes.
• Staff reported incidents using a commercial softwarepackage linked to the corporate intranet. Outpatientstaff we spoke with confirmed they had received trainingand felt confident about using the system.
• Managers understood their obligations under Duty ofCandour (DoC). This statutory duty, under the Healthand Social Care Act (Regulated Activities Regulations2014) requires providers of health and social careservices to notify patients (or other relevant persons) ofcertain safety incidents and provide them withreasonable support.
• The software would not allow an incident to be ‘closed’until the duty of candour section of the file wascompleted. This facility gave senior managers assurancethat duty of candour was being followed by thosedealing with the incident report.
• Staff could describe how learning from incidents tookplace at local, regional and national (corporate) level.Governance meeting minutes and team meetingrecords we saw confirmed there was dissemination oflearning. We reviewed three investigation reports andsaw evidence of learning from that was shared acrossthe hospital through emails and team meetings.
• In addition, we observed a daily ‘Comm Cell’ meetingled by the duty manager. Every department wasrepresented and as part of the standing agenda, weheard the team discuss recent incidents or complaintsand share learning points. Managers stated that anupdated spreadsheet showings actions and an image ofthe comms display board was emailed to all staff afterthe meeting.
Safety Thermometer (or equivalent)
The service used monitoring results to improve safety.Staff collected safety information and shared it with staffand patients. The safety thermometer is used to recordthe prevalence of patient harms and to provideimmediate information and analysis for frontline teamsto monitor their performance in delivering harm free care.
Outpatients
Outpatients
Good –––
54 BMI The Sloane Hospital Quality Report 11/10/2019

• We observed safety performance charts included in the‘Com Cell’ display. These showed current safetythermometer information about key indicators such asfalls and staffing levels.
• Safety performance was reported monthly to the BMIgroup. During the reporting period, date provided by thehospital showed the service was 100% harm free.
• We did not see safety information displayed inoutpatients or physiotherapy departments. Thisinformation was, however, available in annual reportingpublished on the BMI healthcare website for prospectivepatients to view.
Are outpatients services effective?
We do not rate effective in outpatients.
Evidence-based care and treatment
The service provided care and treatment based onnational guidance and evidence-based practice. Bothdepartments followed BMI corporate and nationalguidance. Managers checked to make sure staff followedguidance. New and updated guidance was evaluated andshared with staff.
• Clinical and therapy staff could access national andcorporate guidelines through the BMI group intranet.There were sufficient computer terminals provided todo this and we saw staff and a consultant using theresources.
• BMI used standardised care pathways based on currentbest practice and National Institute for Health and CareExcellence guidance (NICE). The hospital routinelyreviewed the effectiveness of care and treatment byusing performance dashboards as well as local audits.These were benchmarked against the results of otherhospitals in the group as well as national indicators.
• Audits included environmental, handwashing andinfection control checks were routinely performed andthe results of these were shared among staff. Weobserved examples of the results shared on staff noticeboards and the ‘Com Cell’ display.
Nutrition and hydration
• During our inspection, we saw outpatient staff offeringtea or coffee to patients.
Pain relief
Staff assessed and monitored patients regularly to see ifthey were in pain and gave pain relief in a timely way.
• Staff described a pain assessment tool where patientswere asked to score discomfort based on a range from0-10, however we did not observe any instances in clinicwhere patients complained of pain. The use of a painscoring system allowed staff to give appropriatemedication or support with alternative painmanagement techniques and review the effectiveness ofthe intervention.
• Staff said they had used pictogram assessment aids inthe past. These are aids designed to help people withlimited language abilities describe their level ofdiscomfort.
• Outpatient’s kept a stock of pain-relieving medication,such as paracetamol. Should stronger medication berequired, the patient was referred to their own GP or thein-house service. In more urgent cases, the consultant inclinic or RMO could write a prescription is stronger painrelief was required.
Patient outcomes
Staff monitored the effectiveness of care and treatment.They used the findings to make improvements. Thehospital measured performance using a variety of clinicaland business indicators which enabled the seniormanagement team to benchmark performance againstother hospitals in the BMI group.
• These included an internal audit programme andparticipation in initiatives such as the national jointregister and the private healthcare information network(PHIN).
• The hospital also used a propriety computerisedreporting system to provide data on patients whorequired readmission, transfer to another hospital,unplanned return to theatre, infections, incidentsrelating to a thrombolytic event or other significantevents.
• Staff told us that diagnostic test results, includingdiagnostic imaging, were available promptly.
Competent staff
The service made sure staff were competent for theirroles. Managers appraised staff’s work performance andheld supervision meetings with them to provide supportand development.
Outpatients
Outpatients
Good –––
55 BMI The Sloane Hospital Quality Report 11/10/2019

• All new staff had an induction package, which includedcore competencies and knowledge that was signed offby their line manager. We saw examples of these duringour visit.
• Staff confirmed hospital data showing that 100% hadreceived an appraisal in the past year. Regular appraisalallowed the hospital to identify and monitor staffperformance and personal development.
• There was a robust performance management systemin place, in line with BMI group policy.
• There were processes in place for confirmation orpracticing privileges. Consultants were offered privilegesby the executive director and medical advisorycommittee only after hospital had received thenecessary assurance documentation.
• All appraisals were shared with the NHS trust in which aconsultant worked. Where the executive directorprovided information for NHS appraisals, they routinelylooked at data relating to that particular surgeon’spractice such as surgical site infections, complaints andmortality or morbidity.
• The trust had recruitment policies and procedurestogether with job descriptions for all grades of staff.Managers described how the trust completedrecruitment checks to ensure new staff wereexperienced, qualified, competent and suitable for theirrole. All new employees undertook trust and localinduction with additional support and training whenrequired.
• We saw electronic systems that assisted managersmonitor the status of staff requiring validation andcontinuing registration with professional bodies.Registered nurses we spoke with told us the trustsupported them in preparing for revalidation, which is aprocess all nurses and midwives must complete torenew their registration.
Multidisciplinary working
Doctors, nurses and other healthcare professionalsworked closely together as a team to benefit patients.They supported each other to provide safe care. We saweffective multi-disciplinary working between allprofessions and grades of staff.
• There was evidence of close collaboration betweendepartments such as pharmacy and engineering. We
also observed examples of respectful and positiveworking relations between consultants, nursing andphlebotomy staff, physiotherapists, pharmacy andadministrators.
• People we spoke with consistently praised the “familyfeel” of outpatients and we heard positive feedbackfrom staff of all grades about the excellent teamworkwithin the hospital.
• At meetings such as the ‘Com Cell’ briefing, we sawproactive engagement between all members of themultidisciplinary team. These meetings were wellorganised and attended by representatives from clinicaland operational departments.
• BMI hospitals were organised into ‘hubs’ and we alsosaw examples of multidisciplinary teamwork betweensites. For example, the outpatient manager had beenseconded to another hospital on a developmental taskand we saw staff at various grades providing leave cover.
Seven-day services
Although key services at the hospital were available sevendays a week, outpatients and physiotherapy departmentsoperated six days a week during daytime hours.
• Outpatients was open from 8 am to 8 pm Monday toFriday and from 8 am to 12 pm on Saturday. Managersexplained that arrangements could be made to extendSaturday hours, if for example a consultant had a largenumber of appointments.
• Physiotherapy was open from 8 am to 8 pm Monday toThursday; 8 am to 5 pm on Friday and from 8.30 am to 1pm on Saturday.
Health promotion
Staff gave patients practical support and advice to leadhealthier lives.
• We saw a variety of information and advice leaflets ondisplay in outpatients and physiotherapy. These werecontained in wall-mounted or desk-top racks sited inwaiting areas and consultation rooms and includedadvice on topics such as smoking cessation and alcoholdependency.
• The physiotherapy department provided a range ofclasses open to patients and the general public. Theseincluded pilates, yoga for lower back pain, ‘joint school’,back to the gym sessions and ski fit classes.
Outpatients
Outpatients
Good –––
56 BMI The Sloane Hospital Quality Report 11/10/2019

• The physiotherapy manager explained that thesecourses had proved popular, with the pilates class“being oversubscribed”. The team also worked localsports clubs and schools in the locality.
Consent, mental capacity act and deprivation ofliberty safeguards
Staff supported patients to make informed decisionsabout their care and treatment. They followed nationalguidance to gain patients’ consent. They knew how tosupport patients who lacked capacity to make their owndecisions or were experiencing mental ill health. Theyused to agree personalised measures that limit patients'liberty.
• Clinical staff understood how and when to assesswhether a patient had the capacity to make decisionsabout their care. Staff could describe their roles andresponsibilities under the Mental Health Act 1983 andthe Mental Capacity Act 2005. They knew how to supportpatients experiencing mental ill health and those wholacked the capacity to make decisions about their care.
• These aspects were included in mandatory trainingmodules for ‘documentation and legal aspects’ andduty of candour. According to data provided by thehospital 97% of staff had completed the former topicand 98.3% the latter. This exceeded corporate targets of95%
• We reviewed a sample of patient guides on display inoutpatients and found these contained clearexplanations about the services offered, what to expect,record keeping and data protection. These detailshelped patients to make informed decisions about theirtreatment.
• We saw, and patients told us that verbal consent wasalways sought prior to carrying out a task such as takingblood or a applying a dressing.
• During our visit, the physiotherapist running arehabilitation class made sure she had verbal consentfrom class participants before we commenced ourobservation.
Major incident awareness and training
Outpatient staff described participating in medicalemergency simulations such as fire drills and a collapsedpatient. Staff reported the learning experience in positiveterms.
• The hospital had a back-up generator in the engineeringcompound which was tested weekly and we sawrecords showing this. The hospital engineer stated thatthe generator was capable of powering all electricalservices for the hospital. This meant staff could continueto provide full care and facilities to patients should apower interruption occur.
Are outpatients services caring?
Good –––
Our rating of caring stayed the same. We rated it as good.
Compassionate care
Staff treated patients with compassion and kindness,respected their privacy and dignity, and took account oftheir individual needs. We observed staff introducingthemselves by name and addressing the patients in arespectful and dignified manner.
• All staff wore name badges that clearly showed theirname and role. This indicated the hospital activelyconsidered ways to inform patients and relatives aboutwho was providing care and whom they could seekadvice from.
• Consulting and therapy room doors were kept closed,and staff knocked before entering rooms to maintainpatients’ privacy. Consultants conducted appointmentsin private clinic rooms with the doors closed, withobvious signs on the door indicating the name of theconsultant, and whether the room was in use.
• Patients and relatives commented very positively aboutthe care provided to them by the staff.
• We saw ‘thank you’ cards on display in outpatients andphysiotherapy that included comments about staffhelpfulness and kindness. Managers stated that thefeedback helped to encourage and inform staff aboutthe value of their work.
• A patient told us that staff and their consultant had thetime to explain things in detail and allowed time for anyquestions. Patients reported feeling part of thedecision-making about their treatment and care.
• We saw posters displayed in waiting areas and eachconsulting room informing patients of their right torequest a chaperone for any consultation, examination
Outpatients
Outpatients
Good –––
57 BMI The Sloane Hospital Quality Report 11/10/2019

or treatment. Staff told us they offered patients achaperone before any intimate examination orprocedure and were able to anticipate requests basedon the clinic schedule.
• In outpatients we saw a comment card system forpatients to feedback about their experience in thedepartment. Managers stated this was part of patientexperience surveys conducted for BMI healthcare by anindependent company. The results are collated, and amonthly report provided to the hospital, which werecascaded to department teams. The monthly reportshowed patient response rates, rating within categoriesand benchmarking against other BMI hospitals.
• Managers explained that the results of the patientsurvey were discussed at bi-monthly patient satisfactionmeetings and actions logged for implementation.Patient representatives were invited to attend thisforum.
• The hospital participated in the ‘friends and family test’(FFT), which asks people if they would recommend theservices they have used. The FFT provides a mechanismto highlight both good and poor patient experience.According to date supplied by the hospital, the averagescore over the last three months was 97%. Responserates averaged 30% and the hospital was working toimprove this figure. In outpatients, administrative stafffrom the booking office visited patients in the waitingrooms to encourage them to fill out cards before theyleft the department.
Emotional support
Staff provided emotional support to patients, familiesand carers to minimise their distress. They understoodpatients’ personal, cultural and religious needs.
• Patients told us that staff and consultants working in theoutpatient clinics were approachable and “had the timeto explain everything”. Information such as side effectsof medicine were also made clear.
• We saw relatives being invited to accompany patientsinto consultation rooms, which indicated that thehospital encouraged a friend or partner to attend theappointment in order to provide emotional support.
Understanding and involvement of patients andthose close to them
Staff supported and involved patients, families and carersto understand their condition and make decisions abouttheir care and treatment.
• We saw staff photographs and names displayed in themain foyer.
• In each waiting area and at reception desks we sawsigns advising patients about the fees charged and whoto ask for further information. The wall posters includedclear advice about ancillary charges such as blood testsand the displays at reception desks showed the pricesfor splints and other used consumable items.
• During the group exercise class we saw thephysiotherapist answering questions and supportingthe patients with information and advice.
Are outpatients services responsive?
Good –––
Our rating of responsive stayed the same. We rated it asgood.
Service delivery to meet the needs of local people
The service planned and provided care in a way that metthe needs of local people and the communities served. Italso worked with others in the wider system and localorganisations to plan care.
• A wide range of outpatient services were available tomeet the needs of the client group. Private and NHSpatients did not experience long wait times to see theirchosen consultant.
• The environment provided was appropriate and patientcentred, with comfortable and sufficient seating, toiletand refreshment facilities.
• Evening and Saturday outpatient clinics were routinelyoffered, which afforded additional choice andconvenience to patients and particularly those thatworked or had childcare commitments during the week.
• Outpatient clinics were supported by diagnosticservices on site. These were operated by anotherprovider. and included Magnetic Resonance Imaging(MRI) scans, x-ray, Computerised Tomography (CT) scansand ultrasound scans. These facilities were available toNHS and private patients and were open at the sametimes as outpatient and physiotherapy departments.
Outpatients
Outpatients
Good –––
58 BMI The Sloane Hospital Quality Report 11/10/2019

Meeting people’s individual needs
The service was inclusive and took account of patients’individual needs and preferences. Staff made reasonableadjustments to help patients access services. Theycoordinated care with other services and providers.
• Free car parking was provided on-site for theconvenience of visitors. The consultation and therapyclinics we visited were in buildings that were wheelchairaccessible and suitable for use by people with limitedmobility. The hospital had dropped curbs or accessramps at entrances and automatic doors to help makeentering the building easier. Corridors, lifts, clinic roomsand toilets were spacious with doors wide enough to fitwheelchairs.
• Free Wi-Fi was provided for patients and visitors and theoutpatient department had hearing loops installed tohelp improve the way hearing aids worked for peoplewho used them.
• We saw arrangements in place to provide food and drinkfor patients who were in the department.
• Each waiting area included beverage making facilitiesfor tea, coffee and cool water along with a variety ofindividually wrapped biscuits. The beverage stationswere attended at regular intervals by catering staff whoreplenished supplies and crockery.
• Managers explained that should a clinic overrununexpectedly, staff were able to order a snack from thecaterers for any patients having to wait for an extendedtime in the department.
• On the first day of our inspection, we saw two cateringteam staff delivering freshly made cakes and fruit snacksto their outpatient colleagues. They explained this was aweekly gesture of appreciation from the cateringdepartment.
• In addition to local facilities, BMI Healthcare offeredpatients ‘live support’ on the BMI website. This is anonline chat facility using a secure connection. Patientscan also request information at any time using websitefacilities.
• Interpreting services were provided through a contractservice and outpatient staff told us they were normallymade aware of whether English was not a patient’s firstlanguage in the patient’s referral letter and would planaccordingly.
• Similarly, if a patient was identified as having needsassociated with dementia or learning difficulties, thenthey would work with a relative or carer to ensure thepatient was comfortable during visits to thedepartment.
• Evening and Saturday outpatient clinics were routinelyoffered, which afforded additional choice andconvenience to patients and particularly those thatworked or had childcare commitments during the week.
Access and flow
People could access the service when they needed it andreceived the right care promptly. Waiting times fromreferral to treatment and arrangements to admit, treatand discharge patients were in line with nationalstandards.
• GPs referred the majority of new patients attending thedepartment. We were told that physiotherapy andreferrals from other registered practitioners were alsoaccepted by insurers.
• All the patients we spoke to told us they were happywith the length of time they had waited to be seenfollowing referral and had been offered timesconvenient to them. The hospital exceeded the target of92% for NHS patients beginning treatment within 18weeks of referral for each month in the reporting period.
• Follow up appointments were arranged according to therequest of consultants and the needs of patients.
• The imaging department used picture archiving andcommunication system (PACS) technology. This enabledthe hospital to quickly store, retrieve, distribute andview high-quality medical images. For example, thedepartment was able to share images with radiologistsat the local NHS hospital, if the need arose.
Learning from complaints and concerns
It was easy for people to give feedback and raise concernsabout care received. The service treated concerns andcomplaints seriously, investigated them and sharedlessons learned with all staff. The service includedpatients in the investigation of their complaint.
• The hospital received 62 complaints between April 2018and March 2019. Staff at all levels described an openand honest culture and a willingness to acceptresponsibility for any shortcomings.
Outpatients
Outpatients
Good –––
59 BMI The Sloane Hospital Quality Report 11/10/2019

• All written complaints were acknowledged within twodays of receipt. The timescale for a response was 20days or, where it was a complex situation requiringlonger time to investigate, a holding letter was sent.
• The provider met their own timescales.• There was a robust system in place for capturing
learning from complaints and incidents. This was donein a variety of ways, including the daily ‘Comms Cell’departmental briefing, weekly senior managementmeetings and monthly clinical governance meetings.
• Any complaints attributable to individuals or teamswere recorded onto the electronic complaints reportingsystem and shared with the individuals appropriately.Where complaints involved clinical care, the consultantresponsible for the patients’ care was contacted andinvolved in the investigation.
• All complaints were reported to the provider via theregional reporting structure. This enabled BMIHealthcare hospitals to learn from complaints within thegroup.
Are outpatients services well-led?
Good –––
Our rating of well-led stayed the same. We rated it asgood.
Leadership
Leaders had the skills and abilities to run the service.They understood and managed the priorities and issuesthe service faced. They were visible and approachable inthe service for patients and staff. They supported staff totake on more senior roles and to develop.
• We saw good examples of local leadership inoutpatients, physiotherapy and other departments wevisited such as pharmacy. Staff we spoke with said theyfelt well supported, valued and that that their opinionscounted.
• The outpatient manager had been seconded to anotherhospital on a development task, which had promptedthe senior management team into appointing a deputylead. One of the outpatient nurses had just beenpromoted into post and was establishing early prioritiesfor her new role.
• Outpatient staff agreed that senior managers werehighly visible and frequently visited the department.They said they felt free to raise any issues with themdirect or through their line manager.
Vision and strategy
The service had a vision for what it wanted to achieve anda strategy to turn it into action, developed with relevantstakeholders. The vision and strategy were focused onsustainability of services. Leaders and staff understoodand knew how to apply them and monitor progress.
• As part of the BMI group, the hospital shared thecorporate vision” Serious about health. Passionateabout care” and strategy “to offer the best patientexperience and best outcomes in the most cost-effectiveway”.
• The hospital had an operational plan to align with thecompany and had eight strategic priorities: beingpeople, patients, communication, growth, governance,efficiency, facilities and information.
• Outpatient managers and staff were clear about thevision of the organisation and committed to workingtowards achieving the goals.
Culture
Staff felt respected, supported and valued. They werefocused on the needs of patients receiving care. Theservice had an open culture where patients, their familiesand staff could raise concerns without fear.
• Staff said that they enjoyed coming to work and thatthey were passionate about the care they gave topatients. They spoke in positive terms aboutmultidisciplinary team working in order to provide highquality care and understood the hospital structure andwho to contact if they had any questions or concerns.
• We saw that the senior management team were visibleand approachable. All reported that either the executivedirector and director of clinical services would visit thedepartment daily and engage with staff.
• Staff told us they felt confident to share ideas and tohighlight any concerns, incidents, or errors and learnfrom the subsequent investigations.
• The requirements related to duty of candour were metthrough the processes for investigating incidents andreviewing and responding to complaints. Staff were ableto tell us how important it was to be open and honestwith people when things went wrong.
Outpatients
Outpatients
Good –––
60 BMI The Sloane Hospital Quality Report 11/10/2019

Governance
Leaders operated effective governance processes,throughout the service and with partner organisations.Staff at all levels were clear about their roles andaccountabilities and had regular opportunities to meet,discuss and learn from the performance of the service.
• We reviewed the minutes of meetings, whichdemonstrated that regular team and managementmeetings took place. The minutes documented howinformation on incidents and complaints wereinvestigated and any learning shared and good practicepromoted.
• The hospital had a risk register and managers updatedthis accordingly. The outpatient’s manager was aware oftheir department’s risks, and they were correctlyrecorded on the hospitals risk register.
• Managers knew they were responsible for performanceof their departments and received regular feedbackfrom the senior management team.
• A Laser Protection Officer from a local NHS foundationtrust oversaw safety in the OPD. Staff told us they alwayswere available for advice.
Managing risks, issues and performance
Leaders and teams used systems to manage performanceeffectively. They identified and escalated relevant risksand issues and identified actions to reduce their impact.They had plans to cope with unexpected events. Staffcontributed to decision-making to help avoid financialpressures compromising the quality of care.
• The hospital had a risk register and managers updatedthis accordingly. The outpatient’s manager was aware oftheir department’s risks, and they were correctlyrecorded on the hospitals risk register.
• There were good structures for reporting against thegovernance framework in place for all BMI Healthcarehospitals with regional and national benchmarkingagainst other BMI Healthcare hospitals.
• The provider had an electronic incident reportingsystem that fully linked complaints, incidents and riskreporting.
• The safety records were monitored monthly by thesenior management team. Lessons learned werediscussed and disseminated across the organisation.
• There were clear lines of accountability andresponsibility with explicit and effective informationflow pathways.
• The hospital participated in the BMI group auditprogramme. Incidents, near misses and complaints arealso monitored and analysed to help identifyimprovements. Lessons learned were cascaded to allstaff through regular briefings, team meetings and amonthly hospital bulletin, which includedannouncements about NICE guidance or equipmentsafety alerts.
Managing information
The service collected reliable data and analysed it. Staffcould find the data they needed, in easily accessibleformats, to understand performance, make decisions andimprovements. The information systems were integratedand secure. Data or notifications were consistentlysubmitted to external organisations as required.
• Service performance measures were monitored bysenior management at the hospital and BMI group.These included data and notifications that requiredsubmission to external bodies such as NHScommissioners and regulators.
• Information technology systems were widely used tomonitor and improve the quality of care. Staff hadample access to intranet resources which included BMIgroup policies, procedures, training and personalrecords.
Engagement
Leaders and staff actively and openly engaged withpatients, staff, equality groups, the public and localorganisations to plan and manage services. Theycollaborated with partner organisations to help improveservices for patients.
• At all levels, the staff we spoke to expressed pride intheir teams and the services they provided. Staff saidthat they enjoyed coming to work and that they werepassionate about the care they gave to patients.
• We saw daily briefings led by the executive director thatwere used to acknowledge individual contributions,celebrate success, discuss incidents and share learning.Notes from the meeting were emailed to all staffafterwards.
Learning, continuous improvement and innovation
Outpatients
Outpatients
Good –––
61 BMI The Sloane Hospital Quality Report 11/10/2019

All staff were committed to continually learning andimproving services. They had a good understanding ofquality improvement methods and the skills to use them.Staff told us there was good internal promotion andopportunities to undertake further training andeducation.
• The hospital used a corporate clinical benchmarkingsystem which ensured the hospital regularly reviewed itsclinical performance and benchmarked this againstother hospitals. This helped the service work towardscontinuous improvement.
• The hospital had introduced patient journey meetingsto aid communication, teamwork and collaborationacross all departments to identify how to improve theservice provided to patients. Patient satisfaction datawas actively sought and acted upon to help improveservices.
• BMI healthcare had recently introduced a new awardthat recognised long service.
• Pharmacy had responded to consultant enquiries andproduced VTE and corporate medication incidentmonitoring, in collaborating with BMI hospitals locallyand nationally.
Outpatients
Outpatients
Good –––
62 BMI The Sloane Hospital Quality Report 11/10/2019

Areas for improvement
Action the provider SHOULD take to improveIn medicine, the hospital should:
• Further develop the systems to monitor and improvethe endoscopy service.
In surgery, the hospital should:
• Continue to develop a service level agreement (SLA)with the local NHS trust for transfers out in anemergency or if a patient’s condition deteriorates.
• Continue to work to secure theatres fromunauthorised access.
• Continue to support staff to achieve the hospital’smandatory training target of 90% compliance.
• Progress the work to transfer the backlog of data to theNational Breast and Implant Register and move tosubmitting it in a timely way.
Outstandingpracticeandareasforimprovement
Outstanding practice and areasfor improvement
63 BMI The Sloane Hospital Quality Report 11/10/2019











![Bob sloane tucker_mays_finding_executive_jobs_in_the_current_economy[1]](https://static.fdocuments.in/doc/165x107/5461db44b1af9f86228b4c62/bob-sloane-tuckermaysfindingexecutivejobsinthecurrenteconomy1.jpg)