Ben Miers, SPT Lauren Fackler, PT, DPT Christopher Hurley, PT, … · 2016-06-15 · subjective...
Transcript of Ben Miers, SPT Lauren Fackler, PT, DPT Christopher Hurley, PT, … · 2016-06-15 · subjective...
Application of Classification Systems and Multimodal Interventions for a 69-year-
old Patient with Cervical Disc Degeneration and Radicular Pain: A Case Report
Ben Miers, SPT
Lauren Fackler, PT, DPT
Christopher Hurley, PT, DPT, DSc, OCS, SCS, ATC
2
Title: Application of Classification Systems and Multimodal Interventions for a 69-year-old Patient
with Cervical Disc Degeneration and Radicular Pain: A Case Report
Background and Purpose: Neck pain most commonly appears idiopathically, and the source of pathology
is unknown in 50-80% of cases. The development of classification systems is to enhance patient outcomes
by providing direction for nonsurgical treatment approaches based on patient-specific presentation
characteristics from patient history and examination findings, experience gained by clinicians, and
evidence-based literature. The purpose of this case report is to demonstrate application of classification
systems purposed by multiple authors to direct a multimodal treatment approach for best clinical
management of a 69-year-old patient with cervical disc degeneration and radicular pain.
Case Description: A 69-year-old male presented with a chief complaint of neck and right arm pain and
was diagnosed with cervical disc degeneration. Subjective and objective findings of impaired cervical
range of motion, cervical joint hypomobility, radicular pain due to nerve root compression, adverse
mechanical neural tension (median nerve bias), scapular weakness, and poor postural awareness; as a result,
the patient was classified in Neck Pain with Radiculopathy and Centralization subcategories. The Neck
Disability Index (NDI) and PSFS (Patient- Specific Functional Scale) were used as outcome measures.
Outcomes: Clinically objective measurements were re-assessed at visit 11. The patient’s NDI improved
to 9/50 points which equals 18%, and PSFS improved to 5. Neither NDI nor PSFS were determined to be
clinically significant (MDC is equal to 10% in NDI and 2.1 points in PSFS).
Discussion: Application of classification systems and multimodal interventions are important to improve
patient outcomes and facilitate best clinical practice. Since the literature has not been able to conclusively
support classifications and multimodal interventions for patients with neck pain, research needs to further
validate both frameworks within practice.
3
Background
Neck pain most commonly appears idiopathically, and the source of pathology is
unknown in 50-80% of cases.1 The prevalence of neck pain is approximately 13%, with a
lifetime prevalence of nearly 50%.2 Evidence-based research has attempted to fill in the
gap of literature to enhance interventions for patients with neck pain. The development
of classification systems was used to enhance patient outcomes by providing direction
for nonsurgical treatment approaches based on patient-specific presentation
characteristics from patient history and examination findings, experience gained by
clinicians, and evidence-based literature.3 Childs et al. (2004) proposed a classification
system for patients with neck pain; and in 2008, researchers published Neck Pain:
Clinical Practice Guidelines Linked to the International Classification of Functioning,
Disability, and Health From the Orthopedic Section of the American Physical Therapy
Association (CPG) further illustrating 4 subgroups of patients diagnosed with neck pain:
neck pain with mobility deficits, neck pain with headaches, neck pain with movement
coordination impairments, and neck pain with radiating pain.4
Cervical radiculopathy (CR) is a common clinical diagnosis that is identified
within the neck pain with radiating pain4 or centralization3 subcategories. Radpasand
(2011) reported the incidence of CR is estimated to be approximately 85 per 100,000
people, with a higher rate in men than women (107.3 per 100,000 versus 63.4 per
100,000) and peak incidence in the sixth decade of life in both sexes.2 CR is caused by
impingement, irritation or inflammation of a nerve root leading to impairments such as:
pain, sensory or motor deficits, muscle weakness, numbness or tingling located in a
dermatomal pattern. Tanaka et al. (2000) suggested that radicular pain may be caused by
4
a posterolaterally herniated disc, osteophytes in the uncovertebral region, facet joint
osteoarthritis, ligamentum flavum, and foraminal stenosis as a result of disc space
narrowing. Researchers concluded that protruding discs and osteophytes in the
uncovertebral region were determined to cause nerve root compression anteriorly.
Degenerative changes of the intervertebral discs and nerve root impingement occur most
commonly at C5-C6 and C6-C7 spaces. Moreover, the frequency of cervical
radiculopathy was 26% for C6, 61% for C7, and 8% for C8.5
The primary focus for clinicians is to develop a method of treatment specific to
patients’ impairments and functional limitations. Classification systems allow for
clinicians to provide treatment interventions most likely to benefit patients with neck pain
based on homogeneous characteristics of each subcategory; although, little has been done
to examine proposed classification systems for patients with neck pain.3 Fritz and
Brennan (2007) reported that patients who received interventions matched within their
treatment subgroup had better outcomes than patients who received interventions that
were not matched to their subgroup.3 Therapists who treat patients with neck pain, or
other musculoskeletal conditions, acknowledge that a patient’s classification and
presentation can change based on advancing through stages of healing and therapeutic
process; therefore, treatment interventions can be modified and are not limited to
accommodate patients’ needs.6
Generally, single intervention strategies have provided suboptimal results and are
unsupported by most clinicians because it does not accurately represent the complexity of
patient conditions and demonstrate best clinical practice. Most clinicians believe that
prognoses have improved significantly for patients who were treated with a multifaceted
5
treatment approach. Many studies identify statically significant outcomes in pain relief
or improvements with patient function when using multimodal interventions versus single
interventions alone. 4 The literature supports the use of manipulation/mobilization,
exercise, and mechanical traction for patients with cervical radiculopathy or the
centralization classification. 6 Therefore, the purpose of this case report is to demonstrate
application of classification systems purposed by multiple authors to direct a multimodal
treatment approach for best clinical management of a 69-year-old patient with cervical
disc degeneration and radicular pain.
Case Description: Patient History and Systems Review
The patient was a 69-year-old male who presented with a chief complaint of neck
and right arm pain and was diagnosed with cervical disc degeneration. He was currently
retired after working as a tool and die maker for over 35 years. The patient reported that
his pain began approximately 4 months ago, where he started noticing pain in his arm and
along the right side of his neck and upper back. He stated that there was no particular
mechanism of injury or known etiology for painful symptoms. The patient mentioned that
he recently had an MRI which revealed protruded intervertebral discs in his neck;
however, the patient was unable to recall the levels of protrusion.
He experienced shooting pain into his right elbow, as well as the right upper back
and neck. Pain in his right arm was rated at 2/10 at rest but reached 9/10 on the Numeric
Pain Rating Scale (NPRS). The NPRS is an 11-point scale used to quantify the patient’s
level of pain, ranging from 0 (no pain) to 10 (worst pain imaginable). 4, 7, 8 The minimal
clinical important difference (MCID) has been reported to be 2 points.9 In addition, pain
6
in his upper back and neck was rated at 0/10 at the time of the evaluation, but increased
to 7/10 at its worst.
As a result, the patient reported that pain increased with driving for unspecified
durations, working at his computer, occasionally at night and sleeping on his stomach,
walking without quantifying a specific distance, and as the day progressed. Pain was at
its minimum in the morning, and it decreased with sitting upright and neutral arm
alignment. Ice and heat also helped relieve pain temporarily. The patient reported that he
was unable to participate in hobbies, such as, working with stained glass, performing sit-
ups while exercising, and using arms on aerobic cardiorespiratory equipment due to pain.
Significant factors that could have affected the patient’s current condition include a
history of hypertension and type II diabetes. The patient’s goals for physical therapy
involved decreasing painful symptoms and returning to his pre-morbid level of activity.
He stated that he wanted to participate in physical therapy before pursuing epidural
injections or operative treatment.
Clinical Impression #1
Based on subjective information, clinicians hypothesized that the patient was a good
candidate for physical therapy; however, there were significant areas to perform further
testing to rule in/out clinical hypotheses and direct treatment interventions. Due to
subjective report of shooting symptoms in the right upper extremity, neck and upper
back, it is important to differentially diagnose whether symptoms are derived from nerve
root or peripheral nerve compression. The patient has a diagnosis of cervical disc
degeneration, MRI results illustrating protruded intervertebral discs, and at an advanced
7
age; therefore, it is possible that the patient experiences cervical radiculopathy (CR) due
to cervical disc degeneration. The incidence of CR is to be approximately 107.9 per
100,000 men and peak incidence in the sixth decade of life.2 Further testing will be used
to rule in/out the ICD diagnosis of cervical disc disorder with radiculopathy according to
the CPG: Spurling’s maneuver, Upper limb tension tests (ULTT), outcomes of the neck
distraction test, decreased cervical rotation (< 60°) towards the affected side, and signs of
nerve root compression. 4 In addition to the previously stated tests and measures, it is
important to clear the shoulder complex due to symptoms in the right upper extremity and
pain associated with upper extremity usage with aerobic cardiorespiratory equipment.
Since the patient stated that his pain was elicited in sitting positions (driving, working
at the computer, and participating in stained glass work), a thorough postural assessment
is necessary to rule in/out biomechanical flaws that could lead to symptom exacerbation.
Moreover, the patient’s previous history of occupation might have contributed to disc
degeneration and radicular symptoms depending on his postural alignment and extensive
nature of profession.
Examination
Physical examination was performed to assess posture, active range of motion,
joint mobility, and symptom elicitation of the neck. The patient assumed a posture in
standing and sitting with a forward head relative to the plum line, mild increased thoracic
kyphosis (C6-T4), increased bilateral scapular protraction, and decreased lumbar lordosis.
Increased tone was present with palpation of the bilateral cervical paraspinal musculature.
8
Goniometric measurements were taken and indicated restriction with cervical
extension and right lateral flexion greater than left as seen in Figure 1. Good to high
reliability has been reported with AROM measurements, when taken by the same
therapist, regardless of the use of goniometer versus a cervical range of motion
instrument.1 Cervical segmental mobility assessment was performed in supine due to lack
of position tolerance in prone where segmental mobility was quantified as hypomobile,
normal, or hypermobile. Such assessment strategies have demonstrated 100% accuracy
in isolating guilty segmental level of pathology. 1 Joint hypomobility was noted from C5-
T1 with posterior-anterior (PA) glides in which numbness sensations correlated with C6-
C7 dermatomal pattern or median nerve distribution during PA glides of C5-C6.
Thoracic segmental mobility was not assessed due to positional intolerance in prone.
Special tests, such as, Spurling’s test, vertebral artery insufficiency test, upper
limb tension tests, distraction test, were used to reproduce radicular symptoms or guide
treatment interventions. These tests are highly specific (86%, 86%, 90%) with the
exception of the upper limb tension test (22% specific and 97% sensitive) but less
sensitive (50%, 0%, 44%).4 Vertebral artery insufficiency test was negative; however,
Spurling’s test in cervical extension, right lateral flexion and rotation, upper limb tension
test (median nerve bias), and distraction test were all positive tests. The patient was
asked to perform repeated cervical extension motions based on centralization principles
with cervical retractions that are supported in the literature depending on patient
presentation. 4, 10 Pain was increased at end-range with cervical retractions, but
centralization and improvements in gross range of motion were noted as a result.
9
An examination of the right shoulder was performed to clear the glenohumeral,
acromioclavicular, and sternoclavicular joints. The patient was able to achieve full range
of motion at the shoulder with overpressure; although, there was moderate scapular
abduction and upward rotation during phase II and III during right shoulder flexion
within the scapular plane.22 Furthermore, manual muscle testing of the right shoulder
indicated 5/5 strength in all movements except shoulder abduction, external rotation, and
wrist flexion as seen in Figure 2. Manual muscle testing lacks sensitivity; although,
measurements were used as a myotome screen and gross strength assessment of the upper
extremity. 11, 12
Once consent was obtained by the patient to participate in this case study,
additional outcome measures, Neck Disability Index (NDI) and Patient-Specific
Functional Scale (PSFS), were immediately recorded after the third treatment session.
Ideally, quantifiable measures should have been issued during the initial examination;
however, clinicians were determining whether this patient was a suitable candidate for
the given case report.
The NDI is a common utilized outcome measure to capture perceived disability in
patients with neck pain. 4,9 The NDI contains 10 items – 7 related to activities of daily
living, 2 related to pain, and 1 related to concentration. Each item is scored from 0 to 5,
and the total score is expressed as a percentage, with higher scores corresponding to
greater disability. 4, 8, 9 Scores of 10-28% constitute mild disability, 30-48% indicate
moderate disability, 50-68% indicate severe disability, and 72% or greater signify
complete disability. Minimal detectable change (MDC) has been reported at 5.0 (10
percentage points) 1, 4, 9 and MCID is 5.0 or 7.0. 4 Research has found the test-retest
10
reliability of the NDI to be moderate intraclass correlation coefficient (ICC) of 0.68 13,
and the internal consistency to be high (alpha = 0.80-0.92). 1 On the initial measurement,
the patient’s NDI score was 13/50 points which equals 26%.
The PSFS is a practical alternative used to quantify a patient’s present functional
status rather change in functional status.14 The PSFS requires patients to list 3 activities
that are difficult as a result of their symptoms, injury, or disorder. The patient rates each
activity on an 11-point scale, with 0 representing the inability to perform the activity, and
10 representing the ability to perform the activity as well as they could prior to the onset
of symptoms. 4 The average of the 3 activities is the final score. The PSFS has been
evaluated for reliability and validity in patients with neck pain.14 The ICC value for test-
retest reliability in patients with cervical radiculopathy was 0.82. The MDC in that
population was determined to be 2.1 points and MCID of 2.0 points. 4 The patient’s initial
PSFS was determined to be 2.0 points.
Clinical Impression #2
Based on subjective and objective findings of impaired cervical range of motion,
cervical joint hypomobility, radicular pain due to nerve root compression, adverse
mechanical neural tension (median nerve bias), scapular weakness, and poor postural
awareness, the patient was classified in Neck Pain with Radiculopathy4 and/or
Centralization3-4 subgroups. According to the Childs et al (2008), the ICD diagnosis of
cervical disc disorder with radiculopathy can be made with reasonable certainty when the
patient presents with the following clinical findings: upper extremity symptoms, usually
radicular or referred pain, that are produced or aggravated with Spurling’s maneuver and
11
upper limb tension tests, and reduced with the neck distraction test, decreased cervical
range of motion (<60º) toward the involved side, signs of nerve root compression,
success with reducing upper extremity symptoms with initial examination and
intervention procedures. 4 Fritz and Brennan (2007) classified patients in the
centralization using the Classification Decision-Making Algorithm (CDMA) as seen in
Table 1.
By applying supportive evidence from the CPG4 and CDMA3, the following
interventions were recommended for patients in both subcategories: intermittent
mechanical cervical traction, thoracic spine thrust manipulation/non-thrust mobilization,
moist heat and soft tissue mobilization modalities, upper quarter and nerve mobilization,
range of motion and strengthening exercises (especially, the use of cervical retractions)
for the cervical spine, and patient education on postural awareness. As a result, a
multimodal approach using the previously stated interventions excluding thoracic spine
thrust manipulation and intermittent mechanical cervical traction was used for the
purpose of this case report.
Cleland et al (2007) proposed a clinical prediction rule (CPR) to identify patients
with neck pain likely to benefit from thoracic spine thrust manipulation and also,
attempted to examine the validity and application in 2010. Criteria include: symptom
duration of less than 30 days, no symptoms distal to the shoulder, subject reports that
looking up does not aggravate symptoms, Fear-avoidance Beliefs Questionnaire-Physical
Activity Scale (FABQ) score less than 12, diminished upper thoracic spine kyphosis (T3-
T5), and cervical extension of less than 30º. Subjects who met ≥ 3 of the 6 criteria
experienced a post-test probability of success ≥86%.15 From the subjective and objective
12
findings, it is probable to assume the patient met 2 of the 6 criteria at most which
decreases the probability of success to 71%.
Considering the findings reported, intermittent mechanical cervical traction is
supported in the literature for patients with neck pain experiencing radicular symptoms.
The CPG supports the use of a clinical prediction rule to identify patients likely to benefit
from intermittent mechanical cervical traction. The criteria are as follows: patient
reported peripheralization with lower cervical spine (C4-C7) mobility testing, positive
shoulder abduction sign, age ≥ 55 years, positive upper limb tension test (median nerve
bias utilizing shoulder abduction to 90º), and relief of symptoms with manual distraction
test. If at least 4 out of 5 criteria were present, the post-test probability of success with
cervical traction is approximately 90.2%. Although the patient presented with 4 out of 5
criteria, the administrators of this case report did not use intermittent mechanical cervical
traction. Instead of intermittent mechanical cervical traction, the use of manual traction
was agreed on by the student and licensed physical therapist associated with this case
report. The licensed physical therapist believed the patient exhibited nonverbal
psychosocial characteristics that would negatively impact patient prognosis with the use
of intermittent mechanical cervical traction as compared to manual traction.
Interventions
The patient was seen for a total of 13 sessions over a 6 week period of time.
Interventions were chosen based on impairments demonstrated by the patient and leading
evidence submitted in the literature. After the initial evaluation, the patient was informed
and educated on methods to enhance ergonomics for driving and sitting at the computer.
13
Initial evaluation was followed up with the patient being instructed and educated on
performing repeated cervical retractions in supine. Much of the literature is supportive of
cervical retractions for the use of decreasing pain and radicular symptoms, and
consequently, improving function.10 A home exercise program (HEP) including: bilateral
upper trapezius and levator scapulae stretches in sitting, bilateral pectoral stretches in
standing, scapular retractions in sitting, median nerve neuromobilizations, and proper
ergonomic strategies to improve postural awareness was administered to the patient.
After the patient was seen for 2 visits, the patient consented to participate in this case
report; therefore, NDI and PSFS were completed immediately. An initial subjective pain
rating using the NPRS, location and behavior of symptoms was collected before every
treatment session. This information was pertinent to rule in/out a pain source and
peripheralization or centralization of symptoms. Typically, the patient started each
session with moist heat applied for ten minutes to the cervical spine in sitting in order to
increase superficial tissue extensibility to enhance efficacy of other interventions.16 After
seven visits, moist heat was administered to the patient in supine due to increased
complaint of pain in sitting.
Manual therapy was included in therapy all 13 sessions; however, various
interventions were implemented when delivering manual therapy: soft tissue mobilization
(13 out of 13 sessions), manual cervical distraction (13 out of 13 sessions), and cervical
joint mobilizations (7 out of 13 sessions). Soft tissue mobilization was performed in
sitting that is illustrated by Meseguer et al17 utilizing positional inhibition of the right
upper trapezius and levator scapulae for three bouts of 90 seconds. Static manual
cervical distraction was used to mimic mechanical traction and decrease nerve root
14
compression. The distraction was dosed as a grade III joint distraction18 maintained for 7
to 15 minutes in supine. Normally, the patient expressed a 50 to 100% reduction of pain
and radicular symptoms after application of manual distraction. Cervical joint
mobilizations, lateral glides, were performed bilaterally (C4-C7) in supine at a rate of two
oscillations for 120 seconds. Lateral glides were used to facilitate appropriate lateral
flexion arthrokinematics at the facet joints. Much of the literature suggests that the use of
mobilizations when combined with other modalities or treatments produces greater short-
term and immediate effects in pain reduction for patients with neck pain. 19, 20, 21
The evidence supports the use of exercise in combination to manual therapy.
Exercises were used to facilitate upper cervical flexion, lower cervical extension, and
improved scapular retraction and upward rotation coupling motions. Exercises are dosed
and summarized in Figure 3. Cervical retractions are consistently being supported in the
literature to reduce pain and improve function. In addition to McKenzie’s philosophy of
repeated movements, Adbulwahab and Sabbahi (2000) suggests that there are statistically
significant improvements (P < .001) in H reflex amplitude of the flexor carpi radialis and
pain reduction after performing cervical tractions.10 Therefore, the patient performed 3
bouts of 10 repetitions of cervical retractions when radicular symptoms were experienced
and throughout the treatment session. The progression for cervical retractions was as
follows: retractions in supine, retractions in sitting, retractions with extension in sitting,
retractions with extension in sitting with overpressure.
Stretches were performed bilaterally for all 13 sessions and were dosed at 3 bouts
of 30 second holds. Muscles that were targeted included: pectoralis major, levator
scapulae, and upper trapezius. Stretching was performed to improve posture and
15
biomechanics of the cervical spine and shoulder complex. Stretching exercises are
considered “weak evidence” based on a single low quality random controlled trial. 4 In
addition to stretching, scapular retraction exercises were used to strengthen middle and
lower trapezius muscles in order to improve coupled motions during scapular upward
rotation.22 Exercises were administered at 2-3 bouts of 10 repetitions. A progression of
exercises is summarized in Figure 3.
Postural awareness was a very important aspect of patient education throughout
this case report to correct the patient’s posterior pelvic tilt, increased thoracic kyphosis,
protracted scapulae, upper cervical extension, and lower cervical flexion. The patient
was provided with visual, verbal, kinesthetic, and tactile cues to increase patient
participation, improve body positioning, and reduce radicular symptoms and compliant of
pain. The patient experienced an immediate reduction in radicular symptoms and
compliant of pain once posture changed. However, the patient would not maintain
optimal posture for more than 3 minutes after cues were given.
During the treatment process, the patient went on vacation in between visits 5 and
6, in addition, 12 and 13. Each trip required the patient to tolerate prolonged sitting
durations while flying and driving which aggravated neck and radicular pain. The patient
rated pain at 5-6 /10 on average and 10/10 at worst while on the plane and driving. Pain
peripheralized into his right forearm and was described as “burning and shooting”. When
the patient returned from the second vacation, he decided that he was going to receive an
epidural injection in the cervical spine. Therefore, clinicians believed that mechanical
intermittent cervical traction would be applied to observe whether the patient would
overcome the plateau of improvement in therapy. Treatment was applied as described by
16
Cleland et al. 23 Short-term benefits was experienced while the patient in this case report
was positioned in supine during and after traction was performed; however, symptoms
immediately returned once the patient transitioned to sitting and standing posture.
Furthermore, the patient received the epidural injection in between visit 12 and 13 where
he experienced a decreased in overall radicular and pain symptoms.
Outcomes
After participating in physical therapy for 12 visits without resorting to epidural
injection, the patient was able to perform tasks that included driving for 30-45 minutes,
working on stained glass, sitting for prolonged durations, and using the mouse at a
computer with moderate difficulty. Pain symptoms were localized in the right upper
neck. Once the epidural injection was administered between visit 12 and 13, the patient
had minimal residual pinching in the right upper extremity with positions against gravity
and sitting at the computer. Subjective report for treatment sessions 3, 11, and 13 are
represented by an NPRS score in Figure 4.
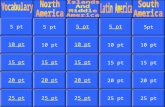
Overall, manual muscle testing scores improved to 5/5 and no complaint of pain
or tingling in all motions throughout bilateral extremities, as compared to 4+/5 right
shoulder abduction and 5/5 wrist flexion strength with noted tingling. Cervical extension
and right lateral flexion range of motion improved at visit 11 from 50 to 55 degrees and
32 to 34 degrees respectively. Cervical extension range of motion increased to 72
degrees and right lateral flexion decreased to 29 degrees by visit 13. Cervical extension
was determined to be clinically significant; however, right lateral flexion range of motion
17
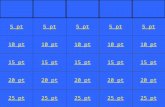
was not clinically significant. Cervical range of motion and manual muscle testing
measurements can be seen in Figure 1 and Figure 2.
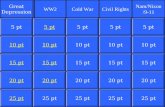
Clinically objective measurements were re-assessed at visit 11. The patient’s NDI
improved to 9/50 points which equals 18%, and PSFS improved to 5. Neither NDI nor
PSFS were determined to be clinically significant (MDC is equal to 10% in NDI and 2.1
points in PSFS). After the epidural injection and visit 13, the patient’s NDI was recorded
at 4/50 points which equals 8%, and PSFS was recorded at 8.3 points. Both NDI and
PSFS were found to be clinically significant between visits 11 and 13. Objective
measurements for NDI, PSFS, and NPRS can be observed in Figure 4.
Discussion
Classification systems are designed to direct treatment and improve outcomes by
grouping patients into subcategories of homogeneous subjective and objective findings.3
Although classification systems have been proposed by many researchers, validation and
application of such methods into practice has not advanced for patients with neck pain as
it has for patients with low back pain. The purpose of this case report was to apply
classification systems and multimodal interventions reported to improve outcomes of a
69 year-old patient with cervical disc degeneration with radicular pain. Most clinicians
that have used multimodal interventions, such as, manual therapy (joint mobilizations/
cervical or thoracic manipulations), exercise, and intermittent mechanical cervical
traction, have experienced positive outcomes. Cleland et al (2007) reported that 31 out of
43 subjects experienced successful short-term outcomes with a multimodal treatment
including: manual therapy, cervical traction, and deep neck flexor muscle strengthening
18
for at least 50% of visits (p < .001).24 In this case report, intermittent mechanical cervical
traction was substituted with manual cervical distraction; in addition, cervical and
thoracic manipulations were not utilized. Previous clinical experience led the supervising
therapist to believe that outcomes would be similar without the use of either intervention.
As a result, the student physical therapist’s plan of care was in accordance with the
licensed physical therapist.
Based on the classification decision-making algorithm3 (Table 1) and CPG 4, the
patient in this case report was classified in the Centralization and Neck Pain with
Radiating Pain subcategories. Fritz and Brennan3 reported that patients in this
classification using matched interventions were associated with fewer changes in NDI
and pain rating scores than other classifications which is essentially the outcome of the
patient in this case report before the administration of the epidural injection. However, in
the case of Fritz and Brennan, there was marked difference in patients in the
centralization classification receiving matched and nonmatched interventions (71.4% of
subjects achieved minimum detectable change in NDI as compared to 43.6% of subjects
receiving nonmatched interventions).3 The patient in this study experienced an 8%
change in NDI and 1.3 point change in PSFS out of a total of 12 visits which is not
considered to be clinically significant. The patient reported a 10% change in NDI and 5
point change in PSFS after receiving an epidural injection between visits 12 and 13 which
is considered clinically significant.
There are multiple limitations in this case report that might have affected patient
outcomes. First, the supervising and student therapist decided to implement mechanical
cervical distraction instead of intermittent mechanical cervical traction. Generally,
19
distraction of the cervical intervertebral joints is similar in theory to mechanical traction.
However, lack of parameters (force provided with distraction, approximate angle of pull,
and consistent duration of sustained distraction force for each session) excluding grade of
distraction may result in significant human error as compared to implemented mechanical
interventions. According to the CPR to identify patients likely to benefit from
intermittent mechanical cervical traction, the patient met 4 out of 5 criteria:
peripheralization with lower cervical spine (C4-C7) mobility testing, age ≥ 55 years,
positive upper limb tension test (median nerve bias utilizing shoulder abduction to 90º),
and relief of symptoms with manual distraction test. If patients meet 4 out of 5 criteria,
there is a 90.2% post-test probability of success with mechanical traction. For this reason
and validated supporting literature, mechanical traction most likely should have been
provided instead of manual cervical distraction. The second limitation is that NDI and
PSFS were completed by the patient after visit 3 rather than after the initial examination.
Outcomes and clinically significant measures may have been different in perception of
function.
Finally, this case report neglected to use either thoracic nonthrust
mobilization/manipulation or thrust mobilization/manipulation. Since the patient could
not tolerate joint mobility assessment of the thoracic spine supine due to pain,
observations should have been reassessed, modified and observed in sitting. Cleland et
al, (2007) reported that there was a Between-Group Change Score in NDI of 10.03 % in
patients who received thrust mobilization/manipulation as compared to those who
received nonthrust mobilization/manipulation.9 In contrast, Gross et al. (2010) suggested
that there was low evidence supporting thoracic manipulation for patients with neck
20
pain.19 The patient presented with degenerative changes in the cervical spine, and
researchers might have believed that degenerative processes could have affected the
thoracic spine which is a contraindication/precaution for thoracic manipulation. Thoracic
degeneration is unable to be ruled in without diagnostic testing; thus, the implementation
of thoracic nonthrust manipulation/mobilization might result in alternate outcomes.
Conclusion
The application of classification systems and multimodal interventions are
important to improve patient outcomes and facilitate best clinical practice. Since the
literature has not been able to conclusively support classifications and multimodal
interventions for patients with neck pain, research needs to further validate both
frameworks within practice. Although physical therapy outcomes were not determined to
be clinically significant in this case report, clinically significant outcomes were observed
after administration of an epidural injection. Further research should also investigate
evidence comparing outcomes for patients receiving manual cervical distraction versus
intermittent mechanical cervical traction.
21
References
1. Heintz MM, Hegedus EJ. Multimodal management of mechanical neck pain using a treatment based classification system. J MANUAL MANIPULATIVE THER. 2008; 16(4):217-224.
2. Radpasand M. Use of a multimodal conservative management protocol for the treatment of a patient with cervical radiculopathy. Journal of Chiropractic Medicine. 2011;10(1):36-46.
3. Fritz JM, Brennan GP. Preliminary Examination of a Proposed Treatment-Based Classification System for Patients Receiving Physical Therapy Interventions for Neck Pain. Phys Ther. 2007;87(5):513-524.
4. Childs JD, Cleland JA, Elliott JM, Teyhen DS, Wainner RS, Whitman JM, Sopky BJ, Godges JJ, Flynn TW. Neck Pain: Clinical Practice Guidelines Linked to the International Classification of Functioning, Disability, and Health From the Orthopaedic Section of the American Physical Therapy Association. J Orthop Sports Phys Ther. 2008; 38(9): A1-A34.
5. Tanaka N, Fujimoto Y, An HS, Ikuta Y, Yasuda M. The Anatomic Relation Among the Nerve Roots, Intervertebral Foramina, and Intervertebral Discs of the Cervical Spine. Spine. 2000; 25(3): 286-291.
6. Childs JD, Fritz JM, Piva SR, Whitman JM. Proposal of a Classification System for Patients with Neck Pain. J Orthop Sports Phys Ther. 2004; 34(11): 686-700.
7. Childs JD, Piva SR, Fritz JM. Responsiveness of the Numeric Pain Rating Scale in Patients with Low Back Pain. Spine. 2005; 30(11): 1331-1334.
8. Cleland JA, Childs JD, Whitman JM. Psychometric Properties of the Neck Disability Index and Numeric Pain Rating Scale in Patients With Mechanical Neck Pain. Arch Phys Med Rehabil. 2008;89(1):69-74.
9. Cleland JA, Glynn P, Whitman JM, Eberhart SL, MacDonald C, Childs JD. Short-Term Effects of Thrust Versus Nonthrust Mobilization/Manipulation Directed at the Thoracic Spine in Patients With Neck Pain: A Randomized Clinical Trial. Phys Ther. 2007;87(4):431-440.
10. Abdulwahab SS. Sabbahi M. Neck Retractions, Cervical Root Decompression, and Radicular Pain. J Orthop Sports Phys Ther. 2000; 30(1): 4-12.
11. Waldrop MA. Diagnosis and Treatment of Cervical Radiculopathy Using a Clinical Prediction Rule and a Multimodal Intervention Approach: A Case Series. J Orthop Sports Phys Ther. 2006; 36(3): 152-159.
12. Bertilson BC, Grunnesjo M, Strender L. Reliability of clinical tests in the assessment of patients with neck/shoulder problems – impact of history. Spine. 2003; 28(19): 2222-2231.
22
13. Cleland JA, Whitman JM, Fritz JM, et al. The Reliability and construct validity of the Neck Disability Index and Patient Specific Functional Scale in patients with cervical radiculopathy. Spine. 2006; 31: 598-602.
14. Westway MD, Stratford PW, Binkley JM. The Patient-Specific Functional Scale: Validation of Its Use in Persons with Neck Dysfunction. J Orthop Sports Phys Ther. 1998; 27(5): 331-338.
15. Cleland JA, Childs JD, Fritz JM, et al. Development of a clinical prediction rule for guiding treatment of a subgroup of patients with neck pain: use of thoracic spine manipulation, exercise, and patient education. Phys Ther. 2007; 87:9-23.
16. Robertson VJ, Ward AR, Jung P. The effect of heat on tissue extensibility: A comparison of deep and superficial heating. Arch Phys Med Rehabil. 2005; 86(4):819-825.
17. Meseguer AA, Fernández-de-las-Peñas C, Navarro-Poza J, Rodríguez-Blanco C, Gandia JJB. Immediate effects of the strain/counterstrain technique in local pain evoked by tender points in the upper trapezius muscle. Clinical Chiropractic. 2006;9(3):112-118.
18. Kisner C, Colby LA. Therapeutic Exercise: Foundations and Techniques 5th ed. Philadelphia, PA: F.A. Davis Company: 113-117.
19. Gross A, Miller J, D’Sylva J, et al. Manipulation or mobilisation for neck pain: A Cochrane Review. Man Ther. 2010;15(4):315-333.
20. Miller J, Gross A, D'Sylva J, et al. Manual therapy and exercise for neck pain: A systematic review. Man Ther. 2010;15(4):334-354.
21. D’Sylva J, Miller J, Gross A, et al. Manual therapy with or without physical medicine modalities for neck pain: a systematic review. Man Ther. 2010;15(5):415-433. DOI: 10.1016/j.math.2010.04.003.
22. Levangie PK, Norkin CC. Joint Structure & Function: A Comprehensive Analysis 4th ed. Philadelphia, PA: F.A. Davis Company: 256-267.
23. Cleland JA, Whitman JM, Fritz JM, Palmer JA. Manual Physical Therapy, Cervical Traction, and Strengthening Exercises in Patients with Cervical Radiculopathy: A Case Series. J Orthop Sports Phys Ther. 2005; 35(12): 802-811.
24. Cleland JA, Fritz JM, Whitman JM, Heath R. Predictors of short-term outcome in people with a clinical diagnosis of cervical radiculopathy. Phys Ther. 2007;87(12):1619-1632.
23
Figure 1. This figure describes cervical active range of motion measurements at initial examination, Visit 11, and Visit 13.
Active Range of Motion Cervical spine (Degrees)
Initial Evaluation Visit 11 Visit 13 Flexion 60 63 52
Extension 50 55 72 R Lateral Flexion 32 34 32 L Lateral Flexion 44 42 29
R Rotation 64 71 72 L Rotation 66 72 67
Figure 2. This figure describes shoulder and wrist manual muscle testing scores at initial examination, Visit 11, and Visit 13.
MMT Shoulder Score out of 5
Initial Evaluation Visit 11 Visit 13 Flexion 5 5 5
Extension 5 5 5 Abduction 4+ 5 5
External Rotation 4 5 5 Internal Rotation 5 5 5
Wrist Score out of 5
Initial Evaluation Visit 11 Visit 13 Flexion 5* 5 5
Extension 5 5 5 Radial Deviation 5 5 5
Ulnar Deviation 5 5 5 * = denotes tingling in the right upper extremity with particular movement.
Figure 3. This figure describes a series of exercises with parameters per each visit. (x) = treatment was performed that visit, YTB = yellow theraband, YSC = yellow sport cord, RSC = red sport cord, ( ) # = associated dumbbell weight, ov = overpressure, and ext. = extension with overpressure.
Exercise Parameters Visit 1 Visit 2 Visit 3 Visit 4 Visit 5 Upper trapezius stretch 3 x 30 sec hold x x x x
Levator Scapulae stretch 3 x 30 sec hold x x x x Supine Cervical Retractions 2 x 10 repetitions x x x x Sitting Scapular Retractions 2 x 10 repetitions x x x x, YTB Standing Pectoral Stretch 3 x 30 sec hold x x x x
Rows with Sport Cord 2 x 10 repetitions x x x x, RSC Shoulder Extensions with Sport Cord 2 x 10 repetitions x x x x, RSC
Cervical Retractions in Sitting 2 x 10 repetitions x x x x
24
Shoulder Scaption PRE 2 x 10 repetitions x x x x Supine Pectoral Stretch on Foam Roll 3 minute hold x x
Standing Trunk Rotation 2 x 10 repetitions x, YSC x, YSC Wall push-ups 2 x 10 repetitions x x
Thread the needle 2 x 10 repetitions x x Supine Shoulder Protraction 2 x 10 repetitions
Supine Shoulder Flexion 2 x 10 repetitions Isolated Trunk Rotations 2 x 10 repetitions Isolated Pelvic Rotations 2 x 10 repetitions
Median nerve glides 2 x 10 repetitions Transverse Abdominis (TA)
Contractions 2 x 10 repetitions Marching with TA Contractions 2 x 10 repetitions
Modified Marching with TA Contractions 2 x 10 repetitions
Supine Abdominal Crunch 2 x 10 repetitions Supine oblique crunch with pelvic
rotation 2 x 10 repetitions
Figure 3 continued.
Visit 6 Visit 7 Visit 8 Visit 9 Visit 10 Visit 11 Visit 12 Visit 13
x x x x x x x x x x x x x x x x x x
x, YTB x x x x x
x, RSC
x, RSC
x, RSC x, RSC x, RSC x, RSC x, RSC x, RSC
x, RSC
x, RSC
x, RSC x, YSC x, RSC x, RSC x, YSC x, RSC
x x, ov x x x x,ov,ext x x x, 3# x, 3# x, 2# x x
x x,
YSC x,
YSC x,
YSC x x x x x x
x, 3# x, 3# x, 3# x, 2# x, 2# x, 3#
x x x x x x x x x x x
25
x
Figure 4. This figure describes outcome measures: NDI, PSFS, and NPRS for visits 3, 11, and 13.
Outcome Measures Visit 3 Visit 11 Visit 13 Neck Disability Index (points) 13/50 9/50 4/50
(%) 26 18 8
PSFS Score Driving in car 2 3 9
Using computer mouse 4 5 7 Stained glass 0 2 9
Average Score (points) 2 3.3 8.3
Severe NPRS Score (points) 9/10 6/10 1/10 MDC for NDI = 5 points or 10% MDC for PSFS = 2.1 points MDC for NPRS = 2.0 points Table 1. Proposed Clinical Decision-Making Algorithm for Patients with Neck Pain developed by Fritz and Brennan.