BDS Finals Case Presentation - Excellent Grade
-
Upload
shamir-chandarana -
Category
Documents
-
view
19 -
download
1
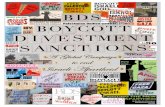
Transcript of BDS Finals Case Presentation - Excellent Grade
Background
Age: 59
Gender: Male
Occupation: Maintenance man at a student letting company
Presenting Complaint: Appearance of upper dentureLoose upper dentureUnable to eat with dentures inBleeding gumsOccasional sensitivity from upper canines
History Of Presenting Complaint:
Has lost his teeth progressively over the years due to neglectHas had his current set of dentures for over 5 yearsHasn’t worn his lower denture for over 5 years – bulky/poor retentionPrevious negative experiences with dentures and dentists
Initially requested a full clearance and F/F’s
Previous Dental History: Non-regular attender – LDV – 3 years agoPartially dentate
Background
Medical History High cholesterol (2004)– controlled with medicationIBS (2005) – occasionally gets symptoms controlled with medicationNo known allergies
Medications Prescribed medications:- Sulpiride – TDS when symptomatic, approximately 1/12- AtorvastatinNo over the counter medications
Social History Divorced - No childrenResides in PlymouthUsed to smoke 15 cigarettes per day for 30 years, stopped 7 years agoAlcohol consumption – approximately 8 units per week
Hobbies: Science fiction films
Family History No history of familial disease, dental or medical.
Patient Expectations To regain confidence in himself “To be able to eat foods I haven’t been able to eat in years”
Patient Anxiety: High
Examination
Extra-Oral Examination No facial swelling or asymmetry
No lymphadenopathy associated with the head and neck
No clicking, pain, discomfort, limitation or crepitus in movement of TMJ and musculature
Normal mouth opening
Low smile line with symmetrical and competent lips
Class I skeletal pattern
Examination Intra-Oral Examination
Soft tissues – numerous lingual varicosities on ventral surface of tongue, otherwise NAD
Gingivae – moderate phenotype, otherwise NAD
Static occlusion –
Incisal relationship – n/a
Molar relationship: n/a
Centre lines – n/a
Dynamic occlusion
Left & right lateral excursion – canine guidance
Incisal guidance – n/a
Summary Of Dentition
Charting
3 3
3 2 1 1 2 3
KEY:
Composite
Tooth Surface Loss SL
Caries
Denture Tooth
W
Examination
Basic Periodontal Examination (BPE)
Oral Hygiene RegimeBrushes approximately once per week with a manual toothbrush Uses fluoride toothpaste No interdental cleaning or mouthwash usage
DietAssessed via general discussions and in conjunction with a 3 day diet sheet:
Has on average 4 sugar hits a day Drinks tea and coffee without sugar
Caries Risk Assessment
High caries risk
Plaque Score 56.3% Bleeding Score 87.5%
X 2 X
X 4 X
Investigations and Justification
Radiographs Full Mouth Periapicals:• To check periapical pathology• To assess for carious lesions• To assess bone loss• Pre-treatment assessment to aid diagnosis
Sensibility Testing
Endo Cold Spray Electric Pulp Test
UR3 Positive Positive
UL3 Positive Positive
LR3 Positive Positive
LR2 Positive Positive
LR1 Positive Positive
LL1 Positive Positive
LL2 Positive Positive
LL3 Positive Positive
Percussion Testing All teeth negative response
Full Periodontal Assessment
6 point pocket chart, gingival recession, furcation grading, mobility score, suppuration, O’Leary plaque score, bleeding score
Diagnostic Study Models
To assess occlusion and aid treatment planning prior to treatment
Periapical Radiographs
Grade 1
UR3: Circular coronal radiolucency No periapical pathologySubgingival calculusModerate horizontal bone loss Maxillary antrum visible
Grade 1
UL3: Circular coronal radiolucency No periapical pathologySubgingival calculusModerate horizontal bone loss Maxillary antrum visible
Periapical Radiographs
Grade 2
LR3: Circular coronal radiolucency No periapical pathology
LR2: UnrestoredNo periapical pathology
LR1: UnrestoredNo periapical pathology
General:• Subgingival interproximal calculus• Moderate generalised horizontal bone
loss
Grade 2
LL1: UnrestoredNo periapical pathology
LL2: UnrestoredNo periapical pathology
General:• Subgingival interproximal calculus• Moderate generalised horizontal bone
loss
Grade 2
LL3: UnrestoredNo periapical pathology
General:• Subgingival interproximal calculus• Moderate generalised horizontal bone
loss
Full Periodontal Assessment
Initial Bleeding
87.5%
Initial Plaque 56.3% (O’Leary)
Pockets 7 pockets ≥4mm
Recession All teeth within class I, (Miller’s Index).
Mobility All teeth within Class 0 (Millers Index)
Furcation nil
Suppuration nil
KEYPocket Depth RecessionBleeding Pockets ≥4mm
Diagnoses / Problem List
Generalised (moderate) chronic periodontitis
Marginal Gingivitis with plaque retentive factors
Secondary Caries - LR3 B, UR3 B, UL3 B
Poor oral hygiene & dietary habits
Pathological Tooth Surface Loss – Attrition
Dentine Hypersensitivity – UR3, UL3, LL3, LL2
Arrested Caries – UR3B, LL2B
Acquired tooth loss – UL8-4, UL2-UR2, UR4-8, LR8-4, LL4-8
Dentures Unsatisfactory
Aesthetic concerns
Generalised gingival recession
Pre-Treatment Tooth Prognosis
Good ✔
Guarded | Questionable ?
Poor X
PERIO.
ENDO.
PROS. Overall
UR3 ✔ ✔ ✔ ✔
UL3 ✔ ✔ ? ?
PERIO.
ENDO. PROS. Overall
LR3 ✔ ✔ ✔ ✔
LR2 ? ✔ ✔ ?
LR1 ? ✔ ✔ ?
LL1 ? ✔ ✔ ?
LL2 ? ✔ ✔ ?
LL3 ? ✔ ? ?
✔
✔ ? ? ? ??
Guarded Teeth Justification
LR2-LL3 Periodontal, therefore overall prognosis guarded due to pockets greater than 4mm
UL3 + LL3 Active TSL (Grade III - Smith & Knight Index)
?
Treatment Aims
Aims Of Treatment
To educate patient about the importance of OH
To improve the oral-hygiene, dietary habits
Improve gingival & periodontal health
To arrest & secondary caries beneath failed restorations
To improve on anterior aesthetics
To regain posterior support
To improve function – ability to eat
To fill spaces from acquired tooth loss
To enable long term maintenance of oral/dental health
PATIENT FACTORS:- Realistic expectations- Patient motivation- Chair time- Home care and
maintenance- High caries risk
Education A Holistic approach - Explanation into caries progression and the aetiology of periodontal disease. Convey the importance of good OHI and keeping remaining teeth
Case Discussion..understanding the holistic needs of the patient
Primary Concerns
Appearance • “Stained fillings” – A thorough clinical examination revealed failed restorations.
① Caries removal + restorations with a better shade match improved aesthetics
Sensitivity
• Sensitivity due to exposed dentine in 6 of the patients 8 teeth• Options given:
① Leave, monitor, re-assess – rejected② Composite build ups
Unsatisfactory dentures
• Patient requested new set of upper dentures • Better Aesthetics / More retentive / Less bulky
• Treatment options ① Leave, monitor, re-assess - rejected② Bridgework (shortened dental arch) - rejected③ acrylic dentures④ cobalt chrome dentures⑤ implant retained dentures - rejected
Education • A Holistic approach • explanation into caries progression and the aetiology of periodontal disease.
Convey the importance of good OHI and keeping remaining teeth
Definitive Treatment Plan
Phase 1 – Short-Term Management
1 Dietary analysis and diet advice
2 OHI, supra-gingival debridementFluoride mouthwash and interdental cleaning aidsFluoride Varnish Application on susceptible sites (arrested caries)Prescription of high fluoride toothpaste
3 Root Surface Debridement (RSD) on pockets ≥ 4mm – with 2 month review
4 Composite restorations – UR3, UL3, LL3
Phase 2 – Medium Term Management
5 Diagnostic wax-up’s of LL1-3 to match anatomy of LR1-3
6 Composite build ups – LL1-3 LR3 DB, UR3, UL3
7 Upper acrylic RPD – Kennedy Classification I mod ILower cobalt-chrome RPD – Kennedy Classification I
Phase 3 – Long Term Management
8 6 monthly dental recall appointments 3 monthly periodontal maintenance appointments
Phase 1 – Short-Term
1 2 3 4 5 6 7 8 9 100
20
40
60
80
100Plaque Score Bleeding Score
Appointments
%
2 Month Periodontal Review
Pockets ≥4mm reduced from 70 No. of bleeding sites reduced 251
KEYPocket Depth Recession Bleeding
Phase 2 - Lower Composite Build-ups
Diagnostic wax ups
requested for LL1-3
Optosil putty
matrix used to create
stent
Rubber dam placement
Total-Etch Bonding
Technique
Composite (shade A4) build up
Polishing
Clinical Stages
Phase 2 – Lower CoCr RPD Design
Saddles To replace missing teethLR4-7, LL4-7
Support Tooth-mucosal support 1) From underlying mucosa 2) From abutment teethCingulum rest encompassing mesial aspect – similar to RPI
Retention DirectOn abutment teeth- Gingivally approaching roach clasps
IndirectKennedy bar connector on cingulum of LR2 and LL2
Bracing Reciprocating action of framework above survey line on LR3/LL3
Connectors Kennedy Bar- Lingual bar + continuous barHygiene - Avoided minor connectors + incisal rests to prevent food packing / plaque trapping
Post-Treatment Tooth Prognosis
Good ✔
Guarded | Questionable ?
Poor X
PERIO.
ENDO.
PROS. Overall
UR3 ✔ ✔ ✔ ✔
UL3 ✔ ✔ ✔ ✔
PERIO.
ENDO. PROS. Overall
LR3 ✔ ✔ ✔ ✔
LR2 ✔ ✔ ✔ ✔
LR1 ✔ ✔ ✔ ✔
LL1 ✔ ✔ ✔ ✔
LL2 ✔ ✔ ✔ ✔
LL3 ✔ ✔ ✔ ✔
Improvements Justification
LR2-LL3 First round of RSD successful. Pockets reduced to 3mm or less
UL3 + LL3 Composite build ups to stabilise and protect against further tooth surface loss – restored function. Long term success dependent on review/monitoring
Maintenance and Recall
Maintenance
Home:• Regular interdental cleaning• Maintaining good OHI and diet• Denture hygiene
Professional:• Reinforce home regime
Recall
Dental Recall:• 6 month recall interval – high caries risk• Monitor/assess for caries and restorations
clinically and radiographically.• Biannual fluoride varnish application
Periodontal Health Recall:• 3 monthly periodontal screening• Full periodontal assessment & 6 point
pocket chart (if indicated)• Plaque and bleeding scores
Monitor:• Review Upper and lower dentures • Lower build ups – staining / repairs• UL3B/LL2B arrested caries
Case Reflection
What went well…① I felt I understood the patients concerns and motivations, and this enabled me to produce a result which helped his confidence.
② Patient specific OH education, the patient now has a meticulous OHI regime at home and understands why
③ It was rewarding to hear that once I had fitted his dentures, he hadn’t taken them out to eat a single meal
④ The 7 pockets ≥4mm healed well within the first round of RSD.
⑤ I was really happy with the final result from my composite build ups and dentures.
⑥ I am happy I decided to go with the modified Kennedy bar design.
Challenges / What could I have done differently..
① I could have requested articulated diagnostic wax-ups for the upper canines also, and build them out more mesially occlusal stop + more stable occlusion. This may have ensured canine guidance.
② I worked closely with the patient and the technician in order to improve the denture design. I realised my limitations and consequently sought to seek additional advice to achieve the best possible result for the patient.
③ I could have used the Altered Cast Technique for a functional impression of the lower alveolar ridges.
Learning Experience
I now understand the importance photography skills and taking good clinical photos: 1) for the patient records and the dento-legal perspective 2) to be able to self-critique my own work to improve upon for future cases
The importance of listening to the patients concerns and taking them into consideration when treatment planning.
The importance of good communication with the lab. For the lower denture I was in constant communication with the chrome department at Phoenix and I think this helped in the final result of the denture
Over the course of this treatment plan and my final year at PDS, I feel I have grown as a clinician and as a professional and hopefully I can transfer these qualities going forward in my career
“Thank you for everything Shamir, these are the best dentures I have ever had, I can’t describe how happy I am with them.