BB
-
Upload
uabsurgclrk -
Category
Health & Medicine
-
view
4.058 -
download
1
Transcript of BB

Benign Breast Disease:Surveillance, Diagnosis and Treatment
Helen Krontiras, M.D.Assistant Professor of Surgery
Co-Director UAB Breast Health Center
Co-Director Lynne Cohen Preventive Care Program for Women’s Cancers at UAB

Risk factors for breast cancer
Major– Gender– Genetic Predisposition– Histologic risk factors
• Personal history of breast cancer• Atypical hyperplasia• Lobular carcinoma in situ
– Age– Therapeutic radiation including breast tissue in the field

Hereditary Breast Cancer
90%
10%SporadicHereditary

Familial Breast Cancer Syndromes• BRCA 1
– Familial breast and ovarian cancer
• BRCA 2– Familial breast and ovarian cancer, with male breast
cancer and pancreatic cancers among others
• Li-Fraumeni (p53 or CHK2)– Sarcomas, brain tumors, adrenal cortical cancers and
breast cancer
• Cowden’s Disease (PTEN)– Breast cancer, thyroid cancer and skin lesions
• Peutz-Jeghers (tumor suppressor LKB1) – mucocutaneous melanotic pigmentation, intestinal polyposis and
increased risk of breast cancer among others

BRCA 1 and 2
• Autosomal dominant• 50% of familial breast cancer syndromes• The prevalence of BRCA mutations is 0.1% in the
general population • BRCA 1
– chromosome 17q21– 50-85% lifetime risk of breast cancer– 20-40% lifetime risk of ovarian cancer
• BRCA 2 – chromosome 13q12– 50-85% lifetime risk of breast cancer
• Increased risk of male breast cancer as well– 10-27% lifetime risk of ovarian cancer

Familial Breast Cancer
• Both maternal and paternal family histories are important
• Computational tools are available to predict the risk for clinically important BRCA mutations
• Respect confidentiality
• DNA testing is available for both genes
• Genetic counseling for those whom testing is considered

General Family History Risk Factors for Carrying a BRCA1 or BCRA2 Mutation
• Known BRCA1 or BRCA2 mutation
• Breast and ovarian cancer
• Early onset breast cancer
• Multiple breast primaries
• Male breast cancer
• Ashkenazi ancestry

Probability of developing breast cancer by age
From age 30 to age 40 . . . . . . .1 out of 257
From age 40 to age 50 . . . . . . .1 out of 67
From age 50 to age 60 . . . . . . .1 out of 36
From age 60 to age 70 . . . . . . .1 out of 28
From age 70 to age 80 . . . . . . .1 out of 24
Ever . . . . . . . . . . . . . . . . . . . . . .1 out of 8
Source: National Cancer Institute Surveillance, Epidemiology, and End Results Program, 1995-1997

Continuum of Breast Cancer Development
Normal HyperplasiaAtypical
hyperplasia
Ductal carcinoma
in situ
Invasive Ductal
carcinoma
RR 1.5-2.0 RR 4-5 RR 8-10

Benign breast diseaseProliferative breast diseaseRelative risk 1.5-2.0• Moderate or florid hyperplasia• Sclerosing adenosis• Intraductal papilloma• Apocrine metaplasia• Radial scar
Proliferative disease with atypiaRelative risk 4-5• Atypical lobular or ductal hyperplasia
LCISRelative risk 9-11• Lobular carcinoma in situ

Atypical Hyperplasia
Lobular carcinoma in situ
• Markers for increased risk• If found on core biopsy, surgical excision
necessary to rule out 30-50% incidence of coexisting cancer
• If found on excisional biopsy, no further surgical therapy warranted
• Management of AH and LCIS– Surveillance or,– Chemoprevention or, – Rarely Prophylactic surgery

Risk factors for breast cancer
Minor– Reproductive history
• Early menarche (<12)• Late childbearing (>30)• Nulliparity• Late Menopause (>55)
– Alcohol – Postmenopausal hormone use– Obesity

Gail Model
• Developed at the National Cancer Institute by Dr. Mitchell Gail in 1989
• Individualized risk prediction– Individual’s estimated 5-year and lifetime risk are calculated and
compared to women the same age and race who are of average risk
• Increased risk is defined as a 5-year risk of 1.7% or greater– Equates to the risk of an average 60 year old woman
• Gail Modelhttp://www.cancer.gov/bcrisktool/



Limitations of Gail Model
• Not used in those with prior history of breast cancer or LCIS
• May underestimate risk with family history suggestive of a gene mutation
– Other models exist for this patient population
• Validity in women under 35 years of age is unknown
• Validity in non-Caucasians is unknown

SurveillanceAverage Risk for Breast Cancer
• Mammography– Annual screening beginning at age 40
• Clinician breast examination– Annual evaluation beginning with GYN exams
• Self breast examination – Regular, breast self-awareness

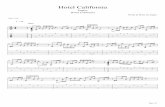
Mammography
• Screening mammogram– Asymptomatic patients– Two view examination of
each breast• Craniocaudal• Mediolateral oblique
• Compare with previous mammograms
RCC LCC
RMLO LMLO

Mammography
• Diagnostic mammogram– Evaluate physical
examination findings– Evaluate abnormalities
on screening • Spot compression• Magnification views• Additional projections• Sonography

Benefits of Screening Mammography
• Randomized trials show reduction in mortality by at least 24%
• Cancer detected in 2-3 of every 1000 women who undergo regular screening mammography

Limitations of Screening Mammography
• Interval cancer rate 10-20%• Biopsy positive predictive value (PPV2)
25%-40%• Dense breasts• Blind areas of the breast• Breast compression• “DCIS dilemma”

Ultrasound
• Adjunct to mammography
• Not a screening tool• Used for problem
solving– Cystic vs solid– Evaluate palpable
abnormalities

Clinical Breast Exam
• Recommended annually for all women 20 years and older
• Inspection of nipple and skin• Palpation of nodal basins
– Cervical, supraclicular, infraclavicular, and axilla
• Systematic examination of the entire breast– Include tissue over sternum– Inframammary fold– Retroareolar area

Self Breast Exam
• Inexpensive, noninvasive • 5-7 days after the onset of menses or on the
same day of the month for postmenopausal women
• New changes should be brought to the attention of primary care provider
• Randomized controlled trials have shown no reduction in mortality from breast cancer among women who performed monthly BSE

Options for Management of Women at Moderate Risk for Breast Cancer
• Surveillance
• Chemoprevention– Tamoxifen
• Lifestyle modification

ChemopreventionTamoxifen
• Consider for women at increased risk
• Currently only FDA approved medication for risk reduction for breast cancer
• Selective estrogen receptor modulator
• 50% reduction in breast cancer risk– 86% with atypical hyperplasia– 56% with lobular carcinoma in situ
Fisher et al, J Natl Cancer Inst 1998

Prevents Breast Cancer
& Inhibits RecurrenceIncreases
Thromboembolic Events
Increases Incidence ofUterine Cancer
Preserves
Bone Density
Lowers
Circulating Cholesterol
Tamoxifen Actions
Increases incidence of hot flashes
Increases incidence vaginal dryness

Options for Management of Women at Increased Risk for Inherited Breast Cancer
• Surveillance– Breast self examination
• Monthly Beginning at age 18
– Clinical breast examination• Semiannually at age 25
– Mammogram and MRI • Annually starting at age 25 or 10 years younger than the youngest
affected relative
• Chemoprevention– Tamoxifen
• Prophylactic surgery– Bilateral Total Mastectomy– Bilateral Oopherectomy

Breast MRI
• Approved for breast by FDA in 1991
• Contrast enhanced (Gadolinium)
• Current data only supports its use for screening in women who are at increased risk for an inherited breast cancer

Rationale for MRI Screening of Populations at Increased Risk for Inherited Breast Cancer
• 80% lifetime risk• Develop cancer at an
early age when breasts are dense
• Grow rapidly– 50% “interval
cancers”
• Median size 1.7 cm– 50% have spread to
lymph nodes

Palpable Mass
• Thorough history and physical examination– Onset, duration, change over time– Breast cancer risk factors
• Dominant mass– Discrete or poorly defined– Cystic or solid
• Persistent through the menstrual cycle• Distinct from surrounding tissue• Asymmetric with respect to the opposite side

Palpable Masses
• Suspicious masses – Hard or firm – Indistinct, irregular
borders – Attached to the skin or
deep fascia
• Benign masses – Mobile– Well demarcated– Soft
•Accuracy of physical examination alone is limited•Correct in 60-85% of cases •More difficult in younger women

• 8 out of 10 lumps are NOT cancer
• Most are lumps are benign conditions– Fibroadenoma– Cyst– Fibrocystic disease

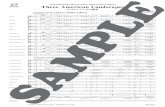
Changing frequencies of discrete breast lumps with age
% o
f to
tal
<20 21-30 31-40 41-50 51-60 >60
10
20
30
50
40
60
70
90
80
0
Cancer
Benign breast changeFibroadenoma
Cyst
Abscess
Dixon 1995Age

Algorithm to Evaluate Dominant Mass or Thickening
< 30 yrs. > 30 yrs. Menopausal
Breast US,considermammo
Bilateralmammo, ± US,FNA/core
Bilateralmammograms
Cyst or classicfibroadenoma
Other Cyst thatresolves
Diagnosticbenign cytology
Non-diagnostic
Observe,biopsy if itchanges
Biopsy Observe,biopsy ifit recurs
Observe,biopsy if itchanges
Biopsy FNA,biopsy

Palpable Mass
• Any discrete solid mass should prompt a surgical referral for tissue diagnosis– Even if mammogram is negative
• If the clinical examination and mammogram are normal but the patient says she can feel a lump, follow-up clinical examination in 2-3 months
• Diffuse nodularity without a discrete mass should be followed clinically at a different point in the menstrual cycle

Palpable Mass
• Triple test diagnosis– Physical examination– Mammography and/or ultrasound– Cytology or histology
• There is 0.5% probability of malignancy when all three are benign
Donnegan, NEJM 1992

Abnormal Mammogram
Increased use of screening mammogram
has resulted in in the identification of a large
number of subclinical abnormalities – Mass– Calcifications
• Clustered
• Pleomorphic
• Grouped
• Linear
• Branching
– Architectural distortion

BIRADS
• Category 0: Need Additional Imaging Evaluation• Category 1: Negative• Category 2: Benign Finding• Category 3: Probably Benign Finding. Short
Interval Follow-Up Suggested • Category 4: Suspicious Abnormality. Biopsy
Should Be Considered• Category 5: Highly Suggestive of Malignancy.
Appropriate Action Should Be Taken • Category 6: Known Malignancy
American College of Radiology (ACR) Breast Imaging Reporting and Data System Atlas
(BI-RADS® Atlas). Reston, Va: © American College of Radiology; 2003.

Abnormal Mammogram
• Careful physical examination• Diagnostic imaging often obviates the
need for biopsy in patients with normal physical examination– 50% of indeterminate lesions are found to be
unequivocally benign or can be followed with interval mammography
• Patients with new findings that cannot be resolved should be referred to a specialist

• Core biopsy (preferred) or excisional biopsy for BIRADS 4 or 5
• Surgical excision indicated after benign core biopsy for atypical hyperplasia, LCIS, radial scar, nondiagnostic specimen, discordant result

Nipple Discharge
• Common symptom but uncommon presentation of breast cancer
• Likelihood of discharge being associated with carcinoma increases with age– 32% of women over 60– 7% of women under 60
• Physical examination– Evaluate for palpable masses
• Cytology not useful in evaluating nipple discharge
• Imaging

Nipple Discharge
• Physiologic Discharge– With compression– Bilateral – Multiple ducts
• Pathologic Discharge– Spontaneous– Unilateral – Single duct– Bloody
DDx• Extensive nipple manipulation• Vigorous aerobic exercise• Stress• Pregnancy
DDx
• Intraductal papilomatosis
• Duct ectasia
• Intraductal mastitis
• Cancer

Nipple Discharge
• Physiologic– Reassure– Follow-up to assure symptoms resolve and no
new symptoms
• Persistent nonlactional galactorrhea– Medical evaluation
• Pathologic– Surgical referral – Bilateral mammogram

The key to any breast complaint is follow-up