ASTX660, a Novel Non-peptidomimetic Antagonist of cIAP1/2 ...ered using fragment-based drug design....
Transcript of ASTX660, a Novel Non-peptidomimetic Antagonist of cIAP1/2 ...ered using fragment-based drug design....

Small Molecule Therapeutics
ASTX660, a Novel Non-peptidomimeticAntagonist of cIAP1/2 and XIAP, PotentlyInduces TNFa-Dependent Apoptosis in CancerCell Lines and Inhibits Tumor GrowthGeorge A.Ward, Edward J. Lewis, Jong Sook Ahn, Christopher N. Johnson,John F. Lyons, Vanessa Martins, Joanne M. Munck, Sharna J. Rich, Tomoko Smyth,Neil T. Thompson, Pamela A.Williams, Nicola E.Wilsher, Nicola G.Wallis, andGianni Chessari
Abstract
Because of their roles in the evasion of apoptosis, inhibitor ofapoptosis proteins (IAP) are considered attractive targets foranticancer therapy. Antagonists of these proteins have thepotential to switch prosurvival signaling pathways in cancercells toward cell death. Various SMAC-peptidomimetics withinherent cIAP selectivity have been tested clinically and dem-onstrated minimal single-agent efficacy. ASTX660 is a potent,non-peptidomimetic antagonist of cIAP1/2 and XIAP, discov-ered using fragment-based drug design. The antagonism ofXIAP and cIAP1 by ASTX660 was demonstrated on purifiedproteins, cells, and in vivo in xenograft models. The compoundbinds to the isolated BIR3 domains of both XIAP and cIAP1with nanomolar potencies. In cells and xenograft tissue, direct
antagonism of XIAP was demonstrated by measuring its dis-placement from caspase-9 or SMAC. Compound-induced pro-teasomal degradation of cIAP1 and 2, resulting in downstreameffects of NIK stabilization and activation of noncanonicalNF-kB signaling, demonstrated cIAP1/2 antagonism. Treatmentwith ASTX660 led to TNFa-dependent induction of apoptosisin various cancer cell lines in vitro, whereas dosing in micebearing breast and melanoma tumor xenografts inhibitedtumor growth. ASTX660 is currently being tested in a phaseI–II clinical trial (NCT02503423), and we propose that itsantagonism of cIAP1/2 and XIAP may offer improved efficacyover first-generation antagonists that are more cIAP1/2 selective.Mol Cancer Ther; 17(7); 1381–91. �2018 AACR.
IntroductionEvasion of apoptosis is one of the hallmarks of cancer (1) and
can be achieved by overexpression of antiapoptotic proteins.Inhibitor of apoptosis proteins (IAP), such as cellular IAP (cIAP)1 and 2 and X-linked IAP (XIAP), are key regulators of antiapop-totic and prosurvival signaling pathways; XIAP directly inhibitscaspases, whereas cIAPs prevent the formation of proapoptoticsignaling complexes. This leads to suppression of apoptosisthrough both the extrinsic and intrinsic apoptosis pathways(2–4). Their deregulation, through amplification, overexpression,or loss of endogenous antagonists, occurs in various cancers and isassociated with tumor growth and poor prognosis, making themattractive targets for anticancer therapy (5).
The IAPs are characterized by their baculovirus IAP repeat (BIR)domains, which mediate protein:protein interactions; some
members of the family, such as cIAP and XIAP, also possess RING(Really Interesting New Gene) zinc finger domains with E3ubiquitin ligase activity (6, 7). The antiapoptotic activity of XIAPis mediated by its direct binding to and inactivation of caspases 3,7, and 9 via its BIR domains (8). IAP antagonists such as theendogenous second mitochondria-derived activator of caspases(SMAC), which is released from mitochondria on induction ofapoptosis, bind to the BIR domains of IAPs and can disruptinteractions such as those between XIAP and caspase-9 (9). Onbinding to other IAPs (cIAP1 and cIAP2), SMAC induces aconformational change, which activates their E3 ligase func-tion, leading to rapid autoubiquitination and proteasomaldegradation (10).
In response to TNFa, cIAPs ubiquitinate RIP1, promoting theformation of complexes (e.g., complex I), which activate survivalsignaling through the canonical NF-kB pathway. Simultaneously,formation of the death-inducing signaling complex (DISC),whichdrives apoptosis, is prevented. Antagonismand subsequentdegradation of the cIAP1/2 leads to the stabilization of NIK (NF-kB-inducing kinase), which activates the noncanonical NF-kBpathway, resulting in the production ofmultiple cytokines includ-ing TNFa. Removal of the cIAP1/2 also allows the DISC to form,leading overall to a switch in TNFa signaling from prosurvival toproapoptotic (11–15). This loss of cIAP1/2 combinedwith releaseof the XIAP-mediated block on caspases, which is essential for fullactivation of apoptosis, leads to a sustained proapoptotic effect inthe presence of TNFa via the extrinsic apoptosis pathway. Tumors
Astex Pharmaceuticals, Cambridge, United Kingdom.
Note: Supplementary data for this article are available at Molecular CancerTherapeutics Online (http://mct.aacrjournals.org/).
Corresponding Author: George A. Ward, Astex Pharmaceuticals, 430 Cam-bridge Science Park, Milton Road, Cambridge, CB4 0QA, United Kingdom.Phone: 44-122-322-6200; Fax: 44-122-322-6201; E-mail:[email protected]
doi: 10.1158/1535-7163.MCT-17-0848
�2018 American Association for Cancer Research.
MolecularCancerTherapeutics
www.aacrjournals.org 1381
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

with sufficient levels of TNFa in their environmentmay, therefore,be particularly susceptible to IAP antagonism (16). In addition,the antagonism of XIAP-mediated caspase inhibition promotesapoptosis induced by stimulation of the intrinsic apoptosis path-way by agents such as chemotherapeutics or DNA-damagingagents (17). This suggests that cIAP1/cIAP2/XIAP antagonists canbe used to promote apoptosis through both the extrinsic andintrinsic pathways.
IAPs have been therapeutically targeted by antisense oligonu-cleotides and antagonist small molecules (4). AEG35156, anantisense oligonucleotide targeted to XIAP, showed some evi-dence of clinical activity (18) and sensitized cancer cells tochemotherapeutic agents and TRAIL receptor agonists in preclin-ical models (3). The first generation of SMAC-mimetic IAPantagonists to enter the clinic, all containing alanine moietiesand inherently cIAP-selective, have shown some activity in pre-clinical models (19–22), but thus far limited single-agent efficacyin clinical trials (3, 4, 23–26).
We have previously reported the identification of lead com-pounds with activity against cIAP1 and XIAP by fragment-basedscreening and structure-based drug design (27, 28). Here, wedescribe the discovery and characterization of ASTX660, an antag-onist of cIAP1/2 and XIAP, which is currently being tested in aphase I–II clinical trial (NCT02503423). We hypothesize thatsuch IAP antagonism may lead to improved efficacy as a result ofthe more effective activation of apoptosis provided by blockingcIAP1/2 while releasing the XIAP block on caspases.
Materials and MethodsMaterials
ASTX660 as the hydrochloride salt was synthesized using achemical procedure similar to that used for AT-IAP (27). Thekey step involved the coupling reaction betweenmethyl-5-((R)-3-methyl-morpholin-4-ylmethyl)-piperazine-1-carboxylic acid tert-butyl ester and 2-chloro-1-{6-[(4-fluorophenyl)methyl]-5-(hydroxymethyl)-3,3-dimethyl-1H,2H,3H-pyrrolo[3,2-b]pyridin-1-yl}ethan-1-one (see Supplementary Materials and Methods);purity was determined as greater than 95% by high-performanceliquid chromatography. All other reagents were purchased fromSigma unless otherwise stated. BV-6 [(2S)-2-{[(2S)-1-[(2S)-2-cyclo-hexyl-2-[(2S)-2-(methylamino)propanamido]acetyl]pyrrolidin-2-yl]formamido}-N-{6-[(2S)-2-{[(2S)-1-[(2S)-2-cyclohexyl-2-[(2S)-2-(methylamino)propanamido]acetyl]pyrrolidin-2-yl]for-mamido}-3,3-diphenylpropanamido]hexyl}-3,3-diphenylpro-panamide] (14) was purchased from Selleckchem.
Protein production and crystallographyA XIAP-BIR3 construct (amino acids 250-354) was expressed in
E. coli, purified by affinity and size exclusion column chromatog-raphy, and crystallized at approximately 10 mg/mL as describedpreviously (27). Crystals were soaked with 5 mmol/L ASTX660in 5% DMSO overnight at room temperature prior to datacollection. The crystals had cell dimensions of approximately70 Å � 70 Å � 105 Å and belong to space group P4122. Thediffraction observed ranged from 1.7 to 3.0 Å.
Binding assaysInteraction between ASTX660 and the BIR3 domains of XIAP or
cIAP1 was determined by measuring the displacement of a fluo-rescent peptide tracer derived from SMAC (AbuRPFK(5&6FAM)-
amide; Peptide Synthetics Ltd) by fluorescence polarizationon a Pherastar plate reader (BMG Labtech). IC50 curves weregenerated using GraphPad Prism version 6 and fitted using thefour parameter logistic curve fit.
Cell linesThe human cell lines MDA-MB-231 and HEK293 were pur-
chased from the European Collection of Cell Cultures (ECACC);human melanoma cell lines, A375 and SK-MEL-28, were pur-chased from ATCC; and the diffuse large B-cell lymphoma cellline, WSU-DLCL2, was purchased from DSMZ. All were grown inDMEMmedium supplemented with 10% FBS and maintained at37�C in an atmosphere of 5% CO2 except WSU-DLCL2 cells,which were grown as above except in RPMI medium supplemen-ted with 10% FBS. All cell culture reagents were purchased fromInvitrogen unless stated otherwise. These cells lines were notpassaged for more than 6 months (or 30 passages) after authen-tication by the cell bank (short tandem repeat PCR) and wereroutinely screened for mycoplasma (MycoAlert, LONZA). Mela-noma cell lines screened at ChemPartner were purchased fromATCC, except COLO679 (ECACC), GAK (Japanese Collection ofResearch Bioresources),MMAC-SF (RikenCell Bank), andnormalhuman dermal fibroblasts (NHDF; LONZA), and were mycoplas-ma screened, short tandem repeat PCR verified, and not usedbeyond 10 passages.
Western blotsCell lysate samples were resolved by SDS-PAGE and immuno-
blotted as described previously (27) with antibodies specificfor XIAP (AF8221), cIAP1 (AF8181), and cIAP2 (AF8171) fromR&D Systems, and the following antibodies from Cell SignalingTechnology: cleaved caspase-3 (#9664), cleaved PARP (#9541),cleaved caspase-9 (#9505), phospho-p65 (S536; #3033),phospho-IkBa (Ser32; #2859), total IkBa (#4814), NF-kB1(p105/p50; #3035), NF-kB2 (p100/p52; #4882), SMAC(#2954), NIK (4994), and b-actin (#8457).
Immunoprecipitation with anti-XIAPEquivalent amounts of cell lysate were incubated overnight at
4�C with protein A/G magnetic beads (Pierce) coated with anti-XIAP polyclonal antibody (R&D Systems). The beads werewashed and boiled in SDS sample buffer containing DTT, beforeanalysis of the eluted proteins by Western blotting. Western blotsof the same lysate before immunoprecipitation were used forcomparison. Antagonism of XIAP by ASTX660 was monitored byWestern blotting for levels of SMAC immunoprecipitated byXIAP.
Meso Scale discovery assaysAn engineered HEK293 cell line (clonal isolate from stable
transfection with full-length FLAG-tagged XIAP expressionconstruct (RC207627) and a full-length untagged caspase-9construct (SC119362; Origene) were used to detect XIAPbinding to caspase-9. Cells were incubated with compoundfor 2 hours, lysed, and lysates added to streptavidin Meso ScaleDiscovery (MSD) plates coated with biotinylated anti-XIAPpolyclonal antibody (R&D Systems), before washing andprobing with anti–caspase-9 or anti-XIAP antibody (CellSignaling Technology), followed by the appropriate secondarydetection antibody.
Ward et al.
Mol Cancer Ther; 17(7) July 2018 Molecular Cancer Therapeutics1382
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

AnMSD plate-based assay was used to quantify levels of cIAP1in MDA-MB-231 after 2-hour ASTX660 treatment. Cells wereincubatedwith compound for 2 hours, washed, and lysed. Lysateswere applied to MSD plates as described previously (27).
Live cell imagingCells were imaged in real time using the IncuCyte ZOOM live
cell imager (Essen BioScience). Cells were incubated with com-pound in 0.1% (v/v) DMSO, with or without neutralizing anti-TNFa antibody (R&D Systems) for 5 days, and live images weretaken every 3 hours using a 10� objective. IncuCyte software wasused to calculate mean percent confluency from four nonover-lapping phase-contrast images of each well.
Induction of apoptosis wasmeasured over the first 24 hours byincluding the Essen BioScience IncuCyte Caspase-3/7 Reagent at afinal concentration of 2 mmol/L in all the wells. Apoptotic cellswere identified by the appearance of green-labeled nuclei, andgreen fluorescence was measured in real time in the green FL1channel of the IncuCyte ZOOM live cell microscope.
Apoptosis cytometry assaysAfter incubation of the cells with ASTX660 for the designated
length of time, cells were harvested by trypsinization, spundown, and 100 mL FACS buffer (PBS þ 1% FBS) was added.Cells were then added to a 96-well plate and 100 mL of 2�CellEvent reagent (Thermo Fisher Scientific; 4 mmol/L in FACSbuffer) was added. The plate was incubated in the dark for 30minutes before measuring fluorescent stained cells in a GuavaeasyCyte HT cytometer (Millipore). Cleaved caspase-3 stainingwas recorded in the FL1 channel, with unstained and DMSOcontrol wells being used to set the gated stained and unstainedcell populations.
Cell line viability screeningIn-house cell viability assays were set up using alamarBlue
reagent (Bio-Rad) as described previously (27). A human mela-noma cell line panel was analyzed at ChemPartner by CellTiter-Glo luminescent cell proliferation assay (Promega) after ASTX660treatment for 72 hours in the presence or absence of 1 ng/mLTNFa (R&DSystems).Datawere normalized to0.1%DMSO(v/v)control, and the drug response, measured as the area over thedose–response curve (activity area), was determined for each cellline (29).
In vivo studiesAll mice were purchased from Envigo. The care and treatment
of animals were in accordance with the United Kingdom Coor-dinating Committee for Cancer Research guidelines and withthe United Kingdom Animals (Scientific Procedures) Act 1986(30, 31). The study protocols were approved by the University ofCambridge Ethical Review Committee.
Initial pharmacokinetic studieswere performed inmale BALB/cwild type as described previously (27). ASTX660 was eitherdissolved in saline and administered intravenously at 5 mg/kgin a dose volume of 5 mL/kg or dissolved in water adjusted to pH5.5 with NaOH and administered by oral gavage at 5 to 30mg/kgin 10 mL/kg. Blood samples were collected at various time pointsand plasma prepared by centrifugation. Further pharmacokineticand pharmacodynamic studies were performed using tumor-bearing immunocompromised animals (see below). Tumorswere excised at specific time points after oral dose and immedi-
ately snap frozen in liquid nitrogen before being stored at�80�Cprior to analysis.
MDA-MB-231 xenografts were prepared by subcutaneouslyinjecting 5 � 106 cells, suspended in 100 mL of serum-freemedium, into the right hind flank of male SCID (BALB/cJHan
�Hsd-Prkdcscid) mice. A375 xenografts were prepared by
subcutaneously injecting 5 � 106 cells, suspended in 100 mL ofa 1:1mixture of serum-freemedium andMatrigel (approximately10mg/mL, Corning), into the right hind flank of male nude mice(BALB/cOlaHsd-Foxn1nu). Subcutaneous xenograft tumors ofHEK293 expressing FLAG-taggedhumanXIAP and caspase-9wereprepared as described previously (27). Tumors were measuredusing digital calipers, and volumes were calculated by applyingthe formula for ellipsoid.
For tumor growth inhibition studies, tumor-bearing animalswere randomized into groups of 7 to 8 with the average tumorvolume of 100 mm3 (31 or 33 days after MDA-MB-231 cellinjection and 19 days after A375 injection). Mice were random-ized and oral ASTX660 treatment started on day 1. Controlanimals receivedwater. During the treatment period, tumors weremeasured at least twice a week, and the effect on body weight wasrecorded dailywhere possible. Statistical analyseswere performedusing GraphPad Prism version 6. The effects of treatments werecompared using one-way ANOVA and two-way ANOVA withDunnett multiple comparisons test against vehicle control. Dif-ferences were deemed statistically significant when P < 0.05.
Analysis of tumor sample pharmacodynamic markersXenograft tumor lysates were prepared by grinding the frozen
tissue to afine powderwith amortar/pestle under liquid nitrogen,and then adding ice-cold lysis buffer [1% Triton X-100, 150mmol/L NaCl, 20 mmol/L Tris�HCl pH 7.5, plus protease inhi-bitors (Roche), 50 mmol/L NaF and 1 mmol/L Na3V04], to theground-up tumor powder. Samples were vortexed and left on icefor 30 minutes. Lysates were cleared by centrifugation, andsamples of the supernatant removed for protein determinationby BCA assay (Pierce).
ForWestern blotting, equivalent amounts of protein lysate hadSDS sample buffer and a final concentration of 50 mmol/L DTTadded, before being boiled, and analyzed by Western blotting asdescribed above.
For immunoprecipitation assay of tumor lysates, equivalentamounts of xenograft lysate were incubated overnight at 4�Cwithprotein A/G magnetic beads (Pierce) coated with anti-XIAPpolyclonal antibody (R&D Systems) followed by Western blotanalysis. For the MSD assay, equivalent amounts of xenograftlysate (200 mg/well) were incubated overnight at 4�C in a strep-tavidin MSD plate coated with biotinylated anti-XIAP polyclonalantibody (R&D Systems), before washing and probing with anti-SMAC, anti–caspase-9, or anti-XIAP antibody (Cell SignalingTechnology) followed by the appropriate secondary detectionantibody.
Pharmacokinetic analysisCompound levels in plasma and tumor samples were mea-
sured and pharmacokinetic parameters were calculated asdescribed previously with the exception of sample bioanalysis,which was undertaken using reverse-phase liquid chromatogra-phy-mass spectrometry (MS), using a Qtrap 4000 MS (AB Sciex),coupled to an Agilent 1200 HPLC system (Agilent) or a QuattroPremier MS coupled to an Acquity UPLC system (Waters; ref. 27).
ASTX660 is an Antagonist of cIAP1/2 and XIAP
www.aacrjournals.org Mol Cancer Ther; 17(7) July 2018 1383
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

ResultsASTX660 is a novel IAP antagonist that targets the BIR3 domainof cIAP1/2 and XIAP
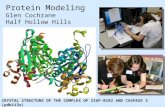
A fragment screen (28), subsequent structure-baseddrugdesigncampaign (27), and further optimization yielded ASTX660 (Fig.1A), a potent, non-peptidomimetic, orally bioavailable, antago-nist of cIAP1/2 and XIAP. ASTX660 potently inhibited the inter-actions between a SMAC-derived peptide and the BIR3 domainsof XIAP (BIR3-XIAP) and cIAP1 (BIR3-cIAP1)with IC50 values lessthan 40 and 12 nmol/L, respectively. The X-ray crystal structure ofASTX660 bound to BIR3-XIAP protein (PDB 5OQW) revealedthat this inhibitor binds to the surface of the protein by occupyingthe same 4 pockets (P1-P4) also recognized by the N-terminalsequence of the endogenous ligand SMAC (Fig. 1B) (32, 33). Thepiperazine ring occupies the P1 pocket, with the protonatednitrogen forming hydrogen bonds with the side chain of Glu314and the backbone carbonyl of Asp309. The methyl substituent isin van der Waals contact with the side chain of Trp310 and henceefficiently fills a small lipophilic subpocket in P1. The P2 pocket isoccupied by the morpholine ring, which stacks on the top of thecentral amide. The carbonyl of the central amide forms ahydrogenbondwith the backboneNHof Thr308. ASTX660 extends into theP3 pocket with a 4-azaindoline bicycle, which forms further vander Waals contacts with the side chain of Trp323, the backbonecarbonyl of Gly306, and the phenolic oxygen of the side chain ofTyr 324. Finally, the benzylic substituent grows from C-6 of theazaindoline into P4 (Fig. 1C).
ASTX660 potently antagonizes XIAP in cellsGiven the potent binding of ASTX660 to the isolated BIR3
domain of XIAP, we investigated the ability of ASTX660 toantagonize the effects of XIAP in cells. Both caspases and SMACbind to the BIR3 domain of XIAP in cells and so should bedisplaced by a XIAP antagonist. We measured the displacementof caspase-9 and SMAC in cells treated with ASTX660. TomeasureXIAP:caspase-9 binding, we generated a stably transfectedHEK293 cell line in which full-length XIAP (FLAG tagged) andcaspase-9 are overexpressed. This enabled us to observe theassociation of caspase-9 with XIAP. Two hours after addition ofASTX660 to this engineered cell line, the association between
XIAP and caspase-9 was potently inhibited with an EC50 value of2.8 nmol/L (Fig. 2A; Supplementary Table S1). To confirm theantagonism of endogenous XIAP by ASTX660, we also investi-gated the displacement of SMAC from XIAP in A375, melanomacells. Cell lysates, treated overnight with a range of ASTX660concentrations, were immunoprecipitated with anti-XIAP. A clearreduction in SMAC levels immunoprecipitated with XIAP wasobserved on treatment with concentrations of ASTX660 above0.01 mmol/L (Fig. 2B). Furthermore, exposure times as short as 5minutes to 1 mmol/L ASTX660 were sufficient to antagonize theinteraction of SMAC with XIAP in A375 cells (Fig. 2C).
ASTX660 binds to and leads to the degradation of cIAP1/2 andstabilization of NIK in cells
Binding of an IAP antagonist to the BIR3 domain of cIAP1/2induces a conformational change, which activates the protein'subiquitin ligase activity from the C-terminal RING domain (34).This leads to rapid autoubiquitination and proteasomal degra-dation of cIAP1/2 (14). To demonstrate the antagonism of cIAPsby ASTX660, levels of cIAP1 were measured in the human breastcancer cell line, MDA-MB-231, after treatment with ASTX660.Measurement of cIAP1 using an immunosorbent assay MSDdetection platform demonstrated that ASTX660 induced degra-dation of cIAP1, with an EC50 of 0.22 nmol/L after 2 hours oftreatment (Fig. 3A; Supplementary Table S1). Further investiga-tion demonstrated a similar effect in A375 cells where cIAP1 levelsdropped rapidly after treatment with 1 mmol/L ASTX660 andremained significantly decreased for up to 48 hours after additionof the compound (Fig. 3B). The human diffuse large B-celllymphoma cell line, WSU-DLCL2, which has high basal cIAP2,was used to demonstrate the effect of ASTX660 treatment onantagonism of both cIAP1 and cIAP2 over a range of times andconcentrations (Fig. 3C). ASTX660 treatment of WSU-DLCL2cells leads to significant cIAP1 and cIAP2 degradation after 1and 4 hours. Levels of cIAP2 were restored by 24 hours possiblydue to resistance previously observed with IAP antagonists afterprolonged treatment in a high NF-kB signaling background(35). TNFa-induced levels of cIAP2 are also antagonized inA375 and SK-MEL-28 melanoma cell lines after ASTX660treatment (see Fig. 4B).
Figure 1.
ASTX660 is a novel antagonist of cIAP1/2 and XIAP. A, Chemical structure of non-peptidomimetic cIAP1/2 and XIAP antagonist, ASTX660, derived by fragment-based drug discovery. B and C, X-ray crystal structure of ASTX660 (in green) in complex with XIAP-BIR3 (PDB 5OQW). The Connolly surface of the proteinin B is colored by electrostatic potential (red, negative; blue, positive; gray, neutral). Hydrogen bonds between ligand and protein in C are shown as dashed red lines.
Ward et al.
Mol Cancer Ther; 17(7) July 2018 Molecular Cancer Therapeutics1384
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

Degradation of cIAPs leads to the stabilization of NIK andactivation of the noncanonical NF-kB pathway. The effects ofASTX660 treatment on NIK levels and NF-kB signaling were alsoinvestigated. On treatment of MDA-MB-231 cells with ASTX660,the rapid degradation of cIAP1was accompanied by a concomitantincrease in the levels ofNIK at 2hours, which remained increased at6 hours (Fig. 3D). The effect of NIK stabilization on noncanonicalNF-kB signaling was further demonstrated by the depletion of NF-kB2p100and the increase inp52after24and48hoursof treatmentwith ASTX660. In addition, although canonical NF-kB signalingmarkers [phospho-p65 or NF-kB1 (p105/p50)] remained largelyunaltered, levels of phospho-IkBawere rapidly increased posttreat-ment and remained above basal levels up to 48 hours aftertreatment (Fig. 3D). Together, these data suggest that ASTX660binds to cIAP1 and 2, leading to their degradation and downstreameffects on NF-kB signaling and apoptosis induction.
The mechanism by which ASTX660 induces apoptosis in celllines is TNFa dependent
Effects of ASTX660 treatment on cell viability and apoptosiswere investigated further in MDA-MB-231 cells. Overall viability
of this cell line was reduced with an EC50 of 1.8 nmol/L (Sup-plementary Table S1), whereas cleavage of PARP and caspase-3,detected by Western blot 24 hours after treatment with ASTX660,indicated apoptosis was induced byASTX660 treatment (Fig. 3D).These effects were investigated further by measuring cell viabilityand induction of cleaved capsase-3 in real time. Loss of viabilitywas observed soon after treatment with 0.1 mmol/L ASTX660 (Fig.4A), and this was reversed on additionof a neutralizing anti-TNFaantibody, indicating that the effects of ASTX660 were TNFadependent and that this cell line produces autocrine TNFa levelssufficient for this ASTX660-induced response. The loss of viabilitywas paralleled by an induction of apoptosis indicated by anincrease in levels of cleaved caspase-3, an effect that, again, wasreversed by the addition of the neutralizing anti-TNFa antibody(Fig. 4A; Supplementary Fig. S1).
Induction of apoptosis was further studied in two melanomacell lines, A375 and SK-MEL-28. Although addition of 1 mmol/LASTX660 to these cell lines led to a degradation of both cIAP1 andcIAP2, apoptosis was only observed in the presence of TNFa asdemonstrated by an increase in the levels of cleaved PARP,caspase-3, and caspase-9, again indicating the dependence on
Figure 2.
ASTX660 treatment leads to potent antagonism of XIAP in cells. A, An engineered HEK293 cell line overexpressing XIAP and caspase-9 was treated for 2 hourswith indicated concentrations of ASTX660. XIAP:caspase-9 binding was measured by immunoprecipitation of FLAG-tagged XIAP and quantitation of XIAP-associated caspase-9 using an MSD plate–based assay. Results show the mean of duplicate values. B, A375 cells were treated for 16 hours with the indicatedconcentrations of ASTX660. Endogenous XIAP antagonism was measured by Western blotting cell lysates for SMAC levels bound to XIAP followingimmunoprecipitation with anti-XIAP (top). Total XIAP and SMAC levels were determined by Western blots of cell lysates before immunoprecipitation (bottom).C, A375 cell lysates were treated with 1 mmol/L ASTX660 for the indicated times. XIAP antagonism was measured by Western blotting for SMAC levels afterimmunoprecipitation with anti-XIAP (top). Total XIAP and SMAC levels were determined by Western blots of cell lysates before immunoprecipitation (bottom).
ASTX660 is an Antagonist of cIAP1/2 and XIAP
www.aacrjournals.org Mol Cancer Ther; 17(7) July 2018 1385
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

TNFa (Fig. 4B; Supplementary Fig. S2). Activity of caspase-3, asa marker of apoptosis, was further investigated in these mel-anoma cell lines by measuring the cleavage of a caspase-3substrate using flow cytometry. Treatment with ASTX660 orTNFa (1 ng/mL) alone showed no effect on caspase-3 activity,in either the A375 or SK-MEL-28 cells; however, when bothtreatments were combined, the activity of caspase-3 was greatlyincreased at time points up to 72 hours, indicating induction ofapoptosis (Fig. 4C).
Effects of ASTX660 treatment on cellular viability were alsoinvestigated in a wider panel of 33melanoma cell lines (Fig. 4D).Addition of TNFa increased or potentiated the inhibitory effect ofASTX660 for the majority of cell lines, but not necessarily for all,suggesting that at least in these cell lines, sufficient levels ofendogenous TNFa are produced. NHDF cell viability was notsignificantly altered by ASTX660 treatment (Fig. 4D).
ASTX660 is orally bioavailable in mice and demonstratesprolonged antagonism of XIAP and cIAP1 in vivo
The pharmacokinetic parameters of ASTX660 were evaluatedfollowing intravenous andoral administration tomice. Followingintravenous administration of ASTX660 at 5 mg/kg to maleBALB/c mice, a moderate mean clearance of 41 mL/minute/kgwas observed with a large volume of distribution of 2.7 L/kg.ASTX660was orally bioavailable (34%) following administrationat 10 mg/kg to mice.
ASTX660 distributed into MDA-MB-231 (Fig. 5A) tumor xeno-grafts. ASTX660 was detectable in tumors up to 168 hours after asingle oral dose of 20mg/kg, andAUClast was 129mmol/L/h/mL. Incontrast, plasma exposure achieved an AUClast 14.3 mmol/L/h/mLand concentrations were below the limit of detection after 48hours. A rapid reduction in cIAP1 levels coupled with antagonismof the XIAP:SMAC interaction was detected from 30 minutes
Figure 3.
Antagonism of cIAP1 by ASTX660 leads to its degradation in cancer cells. A, MDA-MB-231 cells were treated with the indicated concentrations of ASTX660for 2 hours, lysed, and relative levels of cIAP1 measured using an MSD plate–based assay. Results show the mean of duplicate values. B, A375 cells were treatedwith 1 mmol/L ASTX660 for the indicated times and cIAP1 or XIAP levels analyzed by SDS-PAGE followed by immunoblotting. b-Actin was used as an internalcontrol. C, WSU-DLCL2 cells were treated with the indicated concentrations of ASTX660 for the indicated times. Levels of cIAP1 and cIAP2 were analyzedby SDS-PAGE followed by immunoblotting. D, MDA-MB-231 cells were treated with the indicated concentrations of ASTX660 for 2, 6, 24, and 48 hours, lysed, andequal amounts of total protein were then analyzed by SDS-PAGE followed by immunoblotting with the indicated antibodies.
Ward et al.
Mol Cancer Ther; 17(7) July 2018 Molecular Cancer Therapeutics1386
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

and for up to 3 days following a single dose in the tumors in thesame experiment (Fig. 5B). Further experiments with Westernblotting analyses confirmed rapid cIAP1 degradation in MDA-MB-231 xenograft tumors after treatment and a concomitantinduction of apoptosis within one hour as demonstrated by anincrease in cleaved PARP and cleaved caspase-3 (Fig. 5C). Adecrease in association of XIAP and SMAC was also observed inxenograft tumor tissue, again after one hour of treatment (Fig.5D), indicating antagonismofXIAPbyASTX660. The antagonisticeffects onXIAPwere investigated further in a tumormodel derivedfrom HEK293 cells genetically engineered to express XIAP andcaspase-9 (Supplementary Fig. S3). In this model, a single dose ofASTX660 disrupted the interaction between XIAP and caspase-9or SMAC for at least 3 days. Tumor ASTX660 concentrationspersisted over the duration of the study.
ASTX660 causes growth inhibition of MDA-MB-231 and A375xenograft tumors in vivo
The dose- and schedule-dependent antitumor effects ofASTX660 were investigated in the MDA-MB-231 breast cancerxenograft model (Fig. 6A and B; Supplementary Fig. S4A andS4B). Daily oral administration of ASTX660 at 5, 10, and20 mg/kg significantly inhibited tumor growth (P < 0.05 fromdays 15, 18, and 11, respectively; Fig. 6A). An intermittentschedule (cycles of 7 consecutive days of dosing followed by7 days of dose-holiday) at 20 mg/kg also achieved significanttumor growth inhibition, and its effects were equivalent to thecontinuous schedule in the same model (both P < 0.05 vs.vehicle treatment from day 8; Fig. 6B). The activity of ASTX660was further investigated in an A375 melanoma xenograftmodel in nude mice (Fig. 6C; Supplementary Fig. S4C-i). Daily
Figure 4.
TNFa triggers ASTX660-induced apoptosis in cell lines. A, Viability (top) and apoptosis (bottom) were measured in breast cancer MDA-MB-231 cells aftertreatment with 0.1 mmol/L ASTX660 using IncuCyte ZOOM live cell imaging. Anti-TNFa antibody at concentrations of 1 or 10 mg/mL was added to neutralizeTNFa in the cell supernatant to monitor effects on the cell survival. B, Melanoma cell lines, A375 and SK-MEL-28, were treated with 1 mmol/L ASTX660 plus orminus 1 ng/mL TNFa for 24 hours. Cells were then lysed, and equal amounts of total protein were analyzed by SDS-PAGE followed by immunoblottingwith the indicated antibodies. C, A375 or SK-MEL-28 cells were treated with 1 mmol/L ASTX660 for 25 hours in the presence or absence of 1 ng/mL TNFa.Cleaved caspase-3 activity was measured by cytometry. D, Effect of 72-hour ASTX660 treatment on the viability of 33 melanoma cell lines [plus NHDF cells (�),included as a control]. Data generated by CellTiter-Glo in triplicate, in the presence or absence of 1 ng/mL TNFa, were normalized to 0.1% DMSO (v/v) control,and the drug response, measured as the area over the dose–response curve (activity area), was determined for each cell line (29).
ASTX660 is an Antagonist of cIAP1/2 and XIAP
www.aacrjournals.org Mol Cancer Ther; 17(7) July 2018 1387
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

oral administration of ASTX660 at 10 and 20 mg/kg causedsignificant tumor growth inhibition in an A375 model (bothP < 0.05 from day 8), although in vitro, this cell line was onlysensitive to ASTX660 in the presence of TNFa in vitro (Fig. 4Band C).
In all three studies, the ASTX660 treatmentswerewell tolerated,and no excessive bodyweight loss or significant adverse effectswere observed (Supplementary Fig. S4A-i, S4B-I, and S4C-i). It hasbeen suggested that antagonizing multiple IAPs may lead toreduced tolerability in vivo (20, 36). To investigate the inflamma-tory effects of ASTX660, we tested the compound ex vivo onperipheral blood mononuclear cells (PBMC) from 2 healthyhuman donors. We observed no substantial evidence of increasein secretion of proinflammatory cytokines (TNFa, IL1b, IL2, IL6,IL8, IFNg , and MCP-1) in a multiplexed cytokine assay (MSD)after a 48-hour treatment with 10 mmol/L of ASTX660 or with10 mmol/L LCL161 (see Supplementary Table S2). This was incontrast to the bivalent antagonist, BV-6 (Genentech; ref. 14),which causes rapid cIAP1/2 depletion, potently antagonizes XIAP(37), and induced cytokine elevation in the same PBMC assays(Supplementary Table S2).
DiscussionAntagonism of IAPs is considered a promising therapeutic
approach for activating apoptosis pathways in cancer, and anumber of IAP antagonists have undergone evaluation in earlyclinical trials (38). However, despite several observations ofobjective clinical response, single-agent activity in the clinic hasbeen limited (39). The N-terminal sequence (AVPI) of the endog-enous protein SMAC provided the starting point for the firstgeneration of peptidomimetic IAP antagonists. The AVPI peptideshows cIAP1 selectivity (�200-fold over XIAP) due to differentialinteractions formed by the alanine residue in the P1 pocket of theBIR3 domains of XIAP and cIAP1. We have shown that thisintrinsic selectivity is retained in the first generation of SMACmimetics currently in the clinic (27). Given its function in inhibit-ing caspase activation, it has been proposed that XIAP antagonismplays a key role in the activation of apoptosis through both theintrinsic and extrinsic pathways (2, 40). An IAP antagonist withincreased XIAP potency may lead to improved efficacy due tomore effective activation of apoptosis provided by releasing theXIAP block on caspases (38, 45). An increased therapeutic
A
B D
C
1
10
100
1,000
10,000
0 24 48 72 96 120 144 168
Mea
n A
STX6
60 c
once
ntra
�on
(nm
ol/L
)
Time a�er single dose (h)
Plasma
Tumor
0102030405060708090100110
0102030405060708090
100110
0 24 48 72 96 120 144 168
cIAP
1 Le
vel
(% v
ehic
le c
ontr
ol)
XIAP
:SM
AC B
indi
ng(%
veh
icle
con
trol
)
Time (h)
XIAP:SMAC (IP)
cIAP1 Level
6 h 24 hVehicle control
cIAP1
Cleaved PARP
Cleaved Caspase-3
1 h
XIAP
β-Ac�n
SMAC
SMAC
XIAP
6 h 24 hVehicle control 1 h
Figure 5.
Orally administered ASTX660 treatment modulates pharmacodynamic markers in a MDA-MB-231 xenograft model. A, SCID mice bearing MDA-MB-231xenograft were treated with a single 20 mg/kg dose of ASTX660 and compound concentrations in plasma or tumor samples analyzed. B, In the same tumorsamples, levels of cIAP1 and XIAP:SMAC association were determined by MSD assay. C, Mice bearing MDA-MB-231 xenograft tumors received a single oraldose of ASTX660 at 30 mg/kg. Animals were sacrificed at the indicated time points, and protein levels in tumors were measured by immunoblotting of whole-celllysates. D, In the same tumor lysates, XIAP:SMAC association was analyzed by anti-XIAP immunoprecipitation. Each sample represents individual animals.MSD assay values represent mean � SEM from 3 animals.
Ward et al.
Mol Cancer Ther; 17(7) July 2018 Molecular Cancer Therapeutics1388
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

window may also be achieved between efficacious dose and theonset of cytokine-induced toxicity that results from cIAP antag-onism. Cytokine release syndrome has been reported as the dose-limiting toxicity in aphase I dose escalation studyof cIAP-selectiveantagonist LCL161 (23), and such effects have also beendescribedin detail in preclinical toxicity studies with another cIAP1/2antagonist GDC-0152 (41). A true antagonist of cIAP1/2 andXIAP couldbetter explore the clinical potential of IAP antagonism.
To develop such a compound, we have applied our fragment-based drug discovery approach (Pyramid�) to specificallyidentify nonalanine leads with a cIAP1–cIAP2–XIAP profile,avoiding the intrinsic selectivity resulting from peptidomimetic
approaches basedon theAVPI tetrapeptide (27, 28). A subsequentlead optimization campaign focused on reducing off-target activ-ities and improving pharmacokinetic properties, resulting inASTX660, a potent nonpeptidic IAP antagonist, structurally dis-tinct from IAP antagonists previously reported. The resulting IAPantagonism of ASTX660 was demonstrated both in vitro andin vivo. ASTX660 binds to both cIAP1 and XIAP with low nano-molar potency, and this inhibition translates to cells, wherepotent cIAP1/2 antagonism was demonstrated by their degrada-tion,which occurs on the induction of autoubiquitinylation uponantagonist binding; at the same time, antagonism of XIAP wasmeasuredbydisplacement of SMACand casapse-9.Moreover, our
A B
0
100
200
300
400
500
600
0 7 14 21 28
Tum
or v
olum
e (m
m3 )
Day
Vehicle control
20 mg/kg ASTX660 q.d.
20 mg/kg ASTX660 q.d.x 7/no dose x 7
0
100
200
300
400
500
600
700
0 7 14 21 28
Tum
or v
olum
e (m
m3 )
Day
Vehicle control20 mg/kg ASTX66010 mg/kg ASTX6605 mg/kg ASTX660
0
100
200
300
400
500
600
700
800
0 7 14
Tum
or v
olum
e (m
m3 )
Day
Vehicle control20 mg/kg ASTX66010 mg/kg ASTX660
C
Figure 6.
Orally administered ASTX660 inhibits growth of MDA-MB-231 and A375 xenograft tumors. Each data point represents mean � SEM from 8 animals unlessotherwise indicated. A, ASTX660 was orally administered to SCID mice, bearing MDA-MB-231 xenografts, at 20, 10, and 5 mg/kg once daily for 25 days. Controlanimals received water. B, Comparison of the effects of varying ASTX660 administration schedule on MDA-MB-231 tumors. One group of tumor-bearinganimals was treated with ASTX660 for 28 consecutive days (q.d., n¼ 7), and another was given 2 cycles of 7 consecutive days of dosing followed by 7 days of dose-holiday (q.d. � 7/no dose � 7). On dosing days, both treatment groups received ASTX660 once daily at 20 mg/kg. The unconnected symbols represent thedosing events (red square: q.d. and blue triangle: q.d. � 7/no dose � 7). The control group received water as vehicle once daily for 25 consecutive days.C, A375-bearing nude mice were orally treated with 10 or 20 mg/kg of ASTX660 for 14 consecutive days.
ASTX660 is an Antagonist of cIAP1/2 and XIAP
www.aacrjournals.org Mol Cancer Ther; 17(7) July 2018 1389
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

data also confirm here that ASTX660 has potent long-lastingantagonism of cIAP1 and XIAP in vivo following oral administra-tion accompanied by significant inhibition of xenograft tumorgrowth. In the assays used here, ASTX660 demonstrated potenciesof 2.8 and 0.22 nmol/L, respectively, for XIAP and cIAP1 antag-onism (12.7-fold difference). In contrast, other clinical stagemonovalent SMACmimetics do not achieve this level of potencyfor XIAP (range, 10–35 nmol/L) or this balance of antagonism(39-227 fold difference) under the same conditions (see Supple-mentary Table S1), making ASTX660 a novel compound forfurther investigating the effects of IAP antagonism.
There are several potential advantages to antagonizing XIAP inaddition to cIAP1/2. Aberrantly high levels of XIAP have beenlinked to poor prognosis in a number of tumor types, includingdiffuse large B-cell lymphoma, renal cell carcinoma, bladdercancer, and colorectal cancer (42–45), while overexpression ofXIAP in response to chemotherapy and radiotherapy has beenproposed to contribute to resistance to these treatments (42, 46,47). In addition, XIAP levels have also been implicated in mod-ulating responses to immunotherapy, with increased levels inHodgkin lymphoma preventing cytotoxic lymphocyte–mediatedcytotoxicity by blocking granzyme B–induced apoptosis (48) andupregulation of XIAP in inflammatory breast cancer drivingresistance to antibody-dependent cell-mediated cytotoxicity(49), further indicating potential for a molecule that potentlyantagonizes XIAP. Furthermore, the role of XIAP in both extrinsicand intrinsic apoptosis suggests that a potent XIAP inhibitor, suchas ASTX660, might also be expected to show increased synergywith activators of both these apoptotic pathways, such as che-motherapeutics, radiotherapy, or TRAIL agonists, compared witha more cIAP-selective antagonist (2). It has been suggested thatcertain bivalent compounds that potently antagonize cIAP andXIAP are not well tolerated in vivo as they induce an excessivecytokine-mediated proinflammatory phenotype (20, 36). How-ever, we have demonstrated that, unlike the bivalent compounds,ASTX660 does not elicit a toxic cytokine signature, suggesting thatthe IAP antagonist properties of this compound are not a disad-vantage in this respect.
ASTX660 is currently being tested in a phase I–II study insubjects with advanced solid tumors and lymphomas(NCT02503423). Further studies with this novel compound willallow the true clinical potential of an IAP antagonist to beexplored both as a single agent and in combination.
Disclosure of Potential Conflicts of InterestG.A. Ward, E.J. Lewis, J.S. Ahn, C.N. Johnson, J.F. Lyons, V. Martins,
J.M. Munck, S.J. Rich, T. Smyth, N.T. Thompson, P.A. Williams, N.E. Wilsher,N.G. Wallis, and G. Chessari are employees of Astex Pharmaceuticals.
Authors' ContributionsConception and design: G.A. Ward, J.F. Lyons, N.T. Thompson, N.G. Wallis,G. ChessariDevelopment of methodology: G.A. Ward, E.J. Lewis, C.N. JohnsonAcquisition of data (provided animals, acquired and managed patients,provided facilities, etc.): G.A. Ward, E.J. Lewis, J.S. Ahn, C.N. Johnson,V. Martins, J.M. Munck, S.J. Rich, P.A. Williams, N.E. WilsherAnalysis and interpretation of data (e.g., statistical analysis, biostatistics,computational analysis): G.A. Ward, E.J. Lewis, J.S. Ahn, C.N. Johnson,V. Martins, J.M. Munck, S.J. Rich, T. Smyth, N.T. Thompson, P.A. Williams,N.E. Wilsher, N.G. Wallis, G. ChessariWriting, review, and/or revision of the manuscript:G.A. Ward, C.N. Johnson,J.F. Lyons, V. Martins, T. Smyth, P.A. Williams, N.E. Wilsher, N.G. Wallis,G. ChessariAdministrative, technical, or material support (i.e., reporting or organizingdata, constructing databases): G.A. Ward, V. MartinsStudy supervision: J.F. Lyons, N.T. Thompson
AcknowledgmentsWe warmly acknowledge scientific discussions with many Astex colleagues.
We also thank Anne Cleasby for critical discussions and crystallographicsupport.
The costs of publication of this articlewere defrayed inpart by the payment ofpage charges. This article must therefore be hereby marked advertisement inaccordance with 18 U.S.C. Section 1734 solely to indicate this fact.
Received September 8, 2017; revised January 4, 2018; acceptedApril 16, 2018;published first April 25, 2018.
References1. Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell
2011;144:646–74.2. Fulda S, Vucic D. Targeting IAP proteins for therapeutic intervention in
cancer. Nat Rev Drug Discov 2012;11:109–24.3. Dubrez L, Berthelet J, Glorian V. IAP proteins as targets for drug develop-
ment in oncology. Onco Targets Ther 2013;9:1285–304.4. Bai L, Smith DC, Wang S. Small-molecule SMAC mimetics as new cancer
therapeutics. Pharmacol Ther 2014;144:82–95.5. Hunter AM, LaCasse EC,KornelukRG. The inhibitors of apoptosis (IAPs) as
cancer targets. Apoptosis 2007;12:1543–68.6. Deveraux QL, Reed JC. IAP family proteins–suppressors of apoptosis.
Genes Dev 1999;13:239–52.7. Vaux DL, Silke J. IAPs, RINGs and ubiquitylation. Nat Rev Mol Cell Biol
2005;6:287–97.8. Eckelman BP, Salvesen GS, Scott FL. Human inhibitor of apoptosis
proteins: why XIAP is the black sheep of the family. EMBO Rep 2006;7:988–94.
9. Du C, Fang M, Li Y, Li L, Wang X. Smac, a mitochondrial protein thatpromotes cytochrome c-dependent caspase activation by eliminating IAPinhibition. Cell 2000;102:33–42.
10. Feltham R, Bettjeman B, Budhidarmo R, Mace PD, Shirley S, Condon SM,et al. Smac mimetics activate the E3 ligase activity of cIAP1 protein bypromoting RING domain dimerization. J Biol Chem 2011;286:17015–28.
11. MahoneyDJ, CheungHH,MradRL, Plenchette S, SimardC, Enwere E, et al.Both cIAP1 and cIAP2 regulate TNFalpha-mediated NF-kappaB activation.Proc Natl Acad Sci U S A 2008;105:11778–83.
12. Bertrand MJ, Milutinovic S, Dickson KM, Ho WC, Boudreault A, Durkin J,et al. cIAP1 and cIAP2 facilitate cancer cell survival by functioning as E3ligases that promote RIP1 ubiquitination. Mol Cell 2008;30:689–700.
13. MicheauO, Tschopp J. Induction of TNF receptor I-mediated apoptosis viatwo sequential signaling complexes. Cell 2003;114:181–90.
14. Varfolomeev E, Blankenship JW, Wayson SM, Fedorova AV, Kayagaki N,Garg P, et al. IAP antagonists induce autoubiquitination of c-IAPs, NF-kappaB activation, and TNFalpha-dependent apoptosis. Cell 2007;131:669–81.
15. Vince JE, Wong WW, Khan N, Feltham R, Chau D, Ahmed AU, et al. IAPantagonists target cIAP1 to induce TNFalpha-dependent apoptosis. Cell2007;131:682–93.
16. Petersen SL,Wang L, Yalcin-Chin A, Li L, PeytonM,Minna J, et al. AutocrineTNFalpha signaling renders human cancer cells susceptible to Smac-mimetic-induced apoptosis. Cancer Cell 2007;12:445–56.
17. Obexer P, Ausserlechner MJ. X-linked inhibitor of apoptosis protein - acritical death resistance regulator and therapeutic target for personalizedcancer therapy. Front Oncol 2014;4:197.
18. Dean E, Jodrell D, Connolly K, Danson S, Jolivet J, Durkin J, et al. Phase Itrial of AEG35156 administered as a 7-day and 3-day continuous
Ward et al.
Mol Cancer Ther; 17(7) July 2018 Molecular Cancer Therapeutics1390
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

intravenous infusion in patients with advanced refractory cancer. J ClinOncol 2009;27:1660–6.
19. Cai Q, Sun H, Peng Y, Lu J, Nikolovska-Coleska Z, McEachern D, et al. Apotent and orally active antagonist (SM-406/AT-406) ofmultiple inhibitorof apoptosis proteins (IAPs) in clinical development for cancer treatment.J Med Chem 2011;54:2714–26.
20. Condon SM, Mitsuuchi Y, Deng Y, LaPorte MG, Rippin SR, Haimowitz T,et al. Birinapant, a smac-mimetic with improved tolerability for thetreatment of solid tumors and hematological malignancies. J Med Chem2014;57:3666–77.
21. Flygare JA, BeresiniM, BudhaN, ChanH, Chan IT, Cheeti S, et al. Discoveryof a potent small-molecule antagonist of inhibitor of apoptosis (IAP)proteins and clinical candidate for the treatment of cancer (GDC-0152).J Med Chem 2012;55:4101–13.
22. Hennessy EJ, Adam A, Aquila BM, Castriotta LM, Cook D, Hattersley M,et al. Discovery of a novel class of dimeric Smac mimetics as potent IAPantagonists resulting in a clinical candidate for the treatment of cancer(AZD5582). J Med Chem 2013;56:9897–919.
23. Infante JR, Dees EC,Olszanski AJ, Dhuria SV, Sen S, Cameron S, et al. PhaseI dose-escalation study of LCL161, an oral inhibitor of apoptosis proteinsinhibitor, in patients with advanced solid tumors. J Clin Oncol 2014;32:3103–10.
24. DiPersio JF, ErbaHP, Larson RA, Luger SM, TallmanMS, Brill JM, et al. OralDebio1143 (AT406), an antagonist of inhibitor of apoptosis proteins,combined with daunorubicin and cytarabine in patients with poor-riskacute myeloid leukemia–results of a phase I dose-escalation study.Clin Lymphoma Myeloma Leuk 2015;15:443–9.
25. Amaravadi RK, Schilder RJ, Martin LP, Levin M, Graham MA, Weng DE,et al. A phase I study of the SMAC-mimetic birinapant in adults withrefractory solid tumors or lymphoma.Mol Cancer Ther 2015;14:2569–75.
26. Noonan AM, Bunch KP, Chen JQ, Herrmann MA, Lee JM, Kohn EC, et al.Pharmacodynamic markers and clinical results from the phase 2 study ofthe SMACmimetic birinapant in women with relapsed platinum-resistantor -refractory epithelial ovarian cancer. Cancer 2016;122:588–97.
27. Tamanini E, Buck IM, Chessari G, Chiarparin E, Day JEH, Frederickson M,et al. Discovery of a potent nonpeptidomimetic, small-molecule antago-nist of cellular inhibitor of apoptosis protein 1 (cIAP1) and X-linkedinhibitor of apoptosis protein (XIAP). J Med Chem 2017;60:4611–25.
28. Chessari G, Buck IM, Day JE, Day PJ, Iqbal A, Johnson CN, et al. Fragment-based drug discovery targeting inhibitor of apoptosis proteins: discovery ofa non-alanine lead series with dual activity against cIAP1 and XIAP. J MedChem 2015;58:6574–88.
29. Barretina J, Caponigro G, Stransky N, Venkatesan K, Margolin AA, Kim S,et al. The cancer cell line encyclopedia enables predictive modelling ofanticancer drug sensitivity. Nature 2012;483:603–7.
30. Workman P, Aboagye EO, Balkwill F, Balmain A, Bruder G, Chaplin DJ,et al. Guidelines for the welfare and use of animals in cancer research. Br JCancer 2010;102:1555–77.
31. Hollands C. The Animals (scientific procedures) Act 1986. Lancet 1986;2:32–3.
32. Liu Z, Sun C, Olejniczak ET, Meadows RP, Betz SF, Oost T, et al. Structuralbasis for binding of Smac/DIABLO to the XIAP BIR3 domain. Nature2000;408:1004–8.
33. Wu G, Chai J, Suber TL, Wu JW, Du C,Wang X, et al. Structural basis of IAPrecognition by Smac/DIABLO. Nature 2000;408:1008–12.
34. Dueber EC, Schoeffler AJ, Lingel A, Elliott JM, Fedorova AV, Giannetti AM,et al. Antagonists induce a conformational change in cIAP1 that promotesautoubiquitination. Science 2011;334:376–80.
35. Petersen SL, Peyton M, Minna JD, Wang X. Overcoming cancer cellresistance to Smac mimetic induced apoptosis by modulating cIAP-2expression. Proc Natl Acad Sci U S A 2010;107:11936–41.
36. Lawlor KE, Khan N, Mildenhall A, Gerlic M, Croker BA, D'Cruz AA, et al.RIPK3 promotes cell death and NLRP3 inflammasome activation in theabsence of MLKL. Nat Commun 2015;6:6282.
37. Muller-Sienerth N, Dietz L, Holtz P, Kapp M, Grigoleit GU, Schmuck C,et al. SMACmimetic BV6 induces cell death in monocytes and maturationof monocyte-derived dendritic cells. PLoS One 2011;6:e21556.
38. Derakhshan A, Chen Z, Van Waes C. Therapeutic small moleculestarget inhibitor of apoptosis proteins in cancers with deregulation ofextrinsic and intrinsic cell death pathways. Clin Cancer Res 2017;23:1379–87.
39. Fulda S. Promises and challenges of smac mimetics as cancer therapeutics.Clin Cancer Res 2015;21:5030–6.
40. Ndubaku C, Varfolomeev E, Wang L, Zobel K, Lau K, Elliott LO, et al.Antagonism of c-IAP and XIAP proteins is required for efficient inductionof cell death by small-molecule IAP antagonists. ACS Chem Biol 2009;4:557–66.
41. Erickson RI, Tarrant J, Cain G, Lewin-Koh SC, Dybdal N, Wong H, et al.Toxicity profile of small-molecule IAP antagonist GDC-0152 is linked toTNF-alpha pharmacology. Toxicol Sci 2013;131:247–58.
42. Hussain AR, Uddin S, Ahmed M, Bu R, Ahmed SO, Abubaker J, et al.Prognostic significance of XIAP expression in DLBCL and effect of itsinhibition on AKT signalling. J Pathol 2010;222:180–90.
43. Ramp U, Krieg T, Caliskan E, Mahotka C, Ebert T, Willers R, et al. XIAPexpression is an independent prognostic marker in clear-cell renal carci-nomas. Hum Pathol 2004;35:1022–8.
44. Li M, Song T, Yin ZF, Na YQ. XIAP as a prognostic marker of earlyrecurrence of nonmuscular invasive bladder cancer. Chin Med J 2007;120:469–73.
45. XiangG,WenX,WangH,ChenK, LiuH. Expression ofX-linked inhibitor ofapoptosis protein in human colorectal cancer and its correlation withprognosis. J Surg Oncol 2009;100:708–12.
46. Xiong Z, Fu Z, Shi J, Jiang X, Wan H. HtrA1 down-regulation Inducescisplatin resistance in colon cancer by increasing XIAP and activating PI3K/Akt pathway. Ann Clin Lab Sci 2017;47:264–70.
47. Holcik M, Yeh C, Korneluk RG, Chow T. Translational upregulation of X-linked inhibitor of apoptosis (XIAP) increases resistance to radiationinduced cell death. Oncogene 2000;19:4174–7.
48. Kashkar HSJ, Hombach A, Deggerich A, Yazdanpanah B, Uterm€ohlen O,Heimlich G, et al. XIAP targeting sensitizes Hodgkin lymphoma cells forcytolytic T-cell attack. Blood 2006;108:3434–40.
49. Ravi RFE, Jain A, Pham V, Yoshimura K, Prouser T, Jalla S, et al.Resistance of cancers to immunologic cytotoxicity and adoptive immu-notherapy via X-linked inhibitor of apoptosis protein expression andcoexisting defects in mitochondrial death signaling. Cancer Res 2006;108:1730–9.
www.aacrjournals.org Mol Cancer Ther; 17(7) July 2018 1391
ASTX660 is an Antagonist of cIAP1/2 and XIAP
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848

2018;17:1381-1391. Published OnlineFirst April 25, 2018.Mol Cancer Ther George A. Ward, Edward J. Lewis, Jong Sook Ahn, et al. Lines and Inhibits Tumor Growth
-Dependent Apoptosis in Cancer CellαXIAP, Potently Induces TNFASTX660, a Novel Non-peptidomimetic Antagonist of cIAP1/2 and
Updated version
10.1158/1535-7163.MCT-17-0848doi:
Access the most recent version of this article at:
Material
Supplementary
http://mct.aacrjournals.org/content/suppl/2018/04/25/1535-7163.MCT-17-0848.DC1
Access the most recent supplemental material at:
Cited articles
http://mct.aacrjournals.org/content/17/7/1381.full#ref-list-1
This article cites 49 articles, 13 of which you can access for free at:
Citing articles
http://mct.aacrjournals.org/content/17/7/1381.full#related-urls
This article has been cited by 1 HighWire-hosted articles. Access the articles at:
E-mail alerts related to this article or journal.Sign up to receive free email-alerts
Subscriptions
Reprints and
To order reprints of this article or to subscribe to the journal, contact the AACR Publications Department at
Permissions
Rightslink site. Click on "Request Permissions" which will take you to the Copyright Clearance Center's (CCC)
.http://mct.aacrjournals.org/content/17/7/1381To request permission to re-use all or part of this article, use this link
on March 29, 2020. © 2018 American Association for Cancer Research. mct.aacrjournals.org Downloaded from
Published OnlineFirst April 25, 2018; DOI: 10.1158/1535-7163.MCT-17-0848







![PROSTAGLANDINS, PEPTIDOMIMETIC COMPOUNDS, AND …2 PROSTAGLANDINS, PEPTIDOMIMETIC COMPOUNDS, AND RETINOIDS. cascade [4] (Scheme 1.1). The first pathway to be identified starts with](https://static.fdocuments.in/doc/165x107/5fa972d89278580d002e033c/prostaglandins-peptidomimetic-compounds-and-2-prostaglandins-peptidomimetic-compounds.jpg)