Asthma Ppt
Transcript of Asthma Ppt

Asthma

Prevalence of Asthma Asthma affects 300 million adults and
children worldwide
Estimated prevalence of asthma is increasing 50% per decade
WHO: 15-20 million asthmatics in India
Children: 12% and Adults 5%’

Parts of the Respiratory System

The microscopic structure of the airwaysThe airways from the windpipe down to the smallest air passages that supply
the air sacs, have a similar microscopic structure
Ciliated columnar epithelium
Goblet cell
Basement membrane
Blood cellSmooth muscle layer
Spongy layer
Bronchial gland

Classification of the nervous system
Nervous system
Peripheral Central
Somatic Autonomic
Sympathetic Parasympathetic



Sympathetic receptors
Alpha- Beta-
1 2 1 2
Lungs

Where are beta receptors located?
Location Smooth muscle cells Mast cells Eosinophils Lymphocytes Nerve endings Epithelial cells
Relaxation
Anti-inflammatory
Mucus enhancement
Effects

Parasympathetic receptors
Muscarinic - M
M1, M2, M3
Smooth muscle
mucus glands
Ciliary epithelium
Blood vessels
Bronchoconstriction
Mucus secretions
Ciliary activity
Dilation Oedema

Inflammatory Cells
R B C s
E os in op h ils N eu trop h ils B asop h ils --> M as t ce lls
G ran u locytes
L ym p h ocytesT ce lls & B ce lls
M on ocytes - M ac rop h ag es
A g ran u locytes
W B C s P la te le ts
C e lls



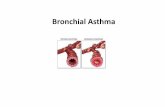
Asthma - Definition
Asthma is a Chronic inflammatory
disease characterized by
Airway hyperesponsiveness to a
variety of stimuli resulting in Bronchospasm
which reverses spontaneously - on treatment



Basic Cellular Mechanisms
FIRST EXPOSURE Sensitisation process
SECOND EXPOSURE Early allergic reaction Late allergic reaction

Allergic Response
SENSIT IZATION PH ASE
1st exposure
Enters the body
Allergen Body produces IgE antibodies
Antibodies + Allergens
Excess antibodiesBind to mast cells
Inflammatory mediators (histamine)(not released)
Produce
Y Y
YY
Y
YYY
YY
Y
Y
M astcell
Sensitization

Allergic Response
2nd exposure
IgE antibody
A llergen
Histamine
ChemotacticFactors
EA RLY ALLERG IC RESPON SE(EAR)
5-30 minutesafter exposure

Allergic Response
2nd exposure C hem otacticF actors
Migration & Activation
Basophils NeutrophilsEOSINOP HILS
Secondary Mediators ECP ; MBP
Damage to Epithelial cells (this exposes the parasympathetic nerves)
LATE A LLERG IC R ESPO N SE (LA R)
INFLAM M ATIO N
Mucus productionBronchoconstriction
Ciliary activityVasodilation
}
REDNESS, SWELLING
between 3-11 hours after exposure


Bronchospasm
Histamine
Leukotrienes
Acetylcholine


Effects of inflammation in the airways
Airway remodelling: the structural changes in the airways chronic untreated inflammation leads to irreversible changes in the structure of airways.
Fibrosis: Formation of fibrous tissue (destruction of lung tissue)
Goblet cell hyperplasia: Increase in the number of goblet cells
Neovascularization: Formation of new blood vessels
Smooth muscle cell hypertrophy: Increase in the size of smooth muscle cells
Basement Membrane Thickening Bronchial Gland Hyperplasia: Increase
in the cells of bronchial gland
Acute Effects Bronchoconstriction Plasma leakage Vasodilation Mucus secretion Nerve activation
Chronic Effects(Airway remodelling) Fibrosis Smooth muscle cell
hypertrophy Goblet cell hyperplasia New blood vessel
formation


Nocturnal Asthma
Nighttime symptoms of wheezing, cough, breathlessness is known as nocturnal asthma.
70% of deaths due to asthma occur
at night
Asthma attacks often occur
between2 and 4 am

Nocturnal Asthma
Causes of Nocturnal Asthma
Exposure to dust mite, animal dander
Gastro-oesophageal reflux
Post nasal drip
Decreased cortisol levels
Increased parasympathetic activity
Increased sensitivity to histamine


Diagnosing Asthma
Medical history
Physical examination
Measurements of lung function
Trial use of asthma medications

Peak Flow Meter
Diagnose asthma
To determine effectiveness of therapy
Identify factors which worsen asthma
Warn of an impending attack

Interpretation of PEFR
15-20% increase in the peak flow when
measured after administering a
bronchodilator, it indicates a significant
degree of reversible airflow obstruction.
Diurnal variability of >20% is indicative of
Asthma.

Spirometry
Patient blows into spirometer. The device measures and records maximum air flow, lung volume, and other parameters which are important in understanding the individual’s pulmonary (lung) function

FEV1
The spirometer mainly measures the FEV1 i.e.
the volume of air that a person can exhale out forcefully in the first second.
The FEV1 values are reduced in case of
asthmatics
Generally in mild cases it is <80% of the normal

Bronchodilator Reversibility testing
Diagnose asthma (Reversibility test)
Measure PEFR
Administer fast acting bronchodilator (Salbutamol 2 puffs)
Measure PEFR after 15-20 mins
15% improvement in peak flow reading

Two clinical properties of bronchodilators
Bronchodilation
Ability to dilate constricted bronchi
Bronchoprotection
Ability to prevent bronchi from going into
spasm after exposure to allergen or any
stimulus

Evaluation of bronchodilators
Bronchodilation Symptoms FEV1/PEFR
Bronchoprotection – can be assessed by methacholine challenge test PD20 /PD15






RELIEVERS Short acting 2 agonists
SalbutamolLevosalbutamol Terbutabaline
Anti-cholinergicsIpratropium bromide
XanthinesTheophylline Aminophylline
Adrenaline injections

PREVENTERSCorticosteroids
ORAL
Prednisolone, Betamethasone
INHALED
BeclomethasoneBudesonideFluticasone

PREVENTERS
Long acting 2 agonistsBambuterol – ORALSalmeterolFormoterol
Anti-leukotrienesMontelukast Zafirlukast

Xanthines
Theophylline SR
Mast cell stabilisers
Sodium cromoglycate
PREVENTERS

Classification of Severity-GINACLASSIFY SEVERITY
Clinical Features Before Treatment
SymptomsSymptoms NocturnalNocturnalSymptomsSymptoms FEVFEV1 1 or PEFor PEF
STEP 4STEP 4
Severe Severe PersistentPersistent
STEP 3STEP 3
Moderate Moderate PersistentPersistent
STEP 2STEP 2
Mild Mild PersistentPersistent
STEP 1STEP 1
IntermittentIntermittent
ContinuousContinuous
Limited physical Limited physical activityactivity
DailyDailyAttacks affect activityAttacks affect activity
> 1 time a week > 1 time a week but < 1 time a day but < 1 time a day
< 1 time a week< 1 time a week
Asymptomatic and Asymptomatic and normal PEF normal PEF between attacksbetween attacks
FrequentFrequent
> 1 time week> 1 time week
> 2 times a month> 2 times a month
2 times a month2 times a month2 times a month2 times a month
60% predicted60% predicted
Variability > 30%Variability > 30%
60 - 80% predicted 60 - 80% predicted
Variability > 30%Variability > 30%
80% predicted80% predicted
Variability 20 - 30%Variability 20 - 30%
80% predicted80% predicted
Variability < 20%Variability < 20%
The presence of one feature of severity is sufficient to place patient in that category.The presence of one feature of severity is sufficient to place patient in that category.

Goals of Asthma Therapy Minimal (ideally no) chronic symptoms Minimal (infrequent) exacerbations No emergency visits Minimal (ideally no) need for “as needed” use of
β2-agonist No limitations on activities, including exercise PEF circadian variation of less than 20 percent (Near) normal PEF Minimal (or no) adverse effects from medicine

Stepwise Approach to Asthma Therapy - AdultsStepwise Approach to Asthma Therapy - Adults
Alternative controller and reliever medications may be considered Alternative controller and reliever medications may be considered
Reliever: Rapid-acting inhaled β2-agonist prn
Preventer: Daily inhaledcorticosteroid
Preventer: Daily inhaled
corticosteroid Daily long-acting
inhaled β2-agonist
Preventer: Daily inhaled
corticosteroid Daily long –acting
inhaled β2-agonist plus (if needed)
When asthma is controlled, reduce therapy
Monitor
STEP 1:STEP 1:IntermittentIntermittent
STEP 2:STEP 2:Mild PersistentMild Persistent
STEP 3:STEP 3: Moderate Moderate PersistentPersistent
STEP 3:STEP 3: Moderate Moderate PersistentPersistent
STEP 4:STEP 4:Severe Severe
PersistentPersistentSTEP DownSTEP DownSTEP DownSTEP Down
Outcome: Asthma Control Outcome: Best Possible Results
Preventer:None
-Theophylline-SR -Anti-Leukotriene -Long-acting inhaled β2- agonist -Oral corticosteroid