Asthma Ppt
-
Upload
carmela-mae-sabellina-pis-an -
Category
Documents
-
view
8 -
download
1
description
Transcript of Asthma Ppt


Introduction:

• An estimated 300 million people worldwide suffer from asthma, with 250,000 annual deaths attributed to the disease. Workplace conditions, such as exposure to fumes, gases or dust, are responsible for 11% of asthma cases worldwide. About 70% of asthmatics also have allergies. The prevalence of asthma increased 75% from 1980-1994. Asthma rates in children under the age of five have increased more than 160% from 1980-1994. It is estimated that the number of people with asthma will grow by more than 100 million by 2025. Asthma accounts for approximately 500,000 hospitalizations each year.13 million school days are missed each year due to asthma.

Definition of terms:

• OrthopneaIs shortness of breath (dyspnea) which occurs when lying flat, causing the person to have to sleep propped up in bed or sitting in a chair.
• Spirometryis the most common of the Pulmonary Function Tests (PFTs), measuring lung function, specifically the measurement of the amount (volume) and/or speed (flow) of air that can be inhaled and exhaled. Spirometry is an important tool used for generating pneumotachographs which are helpful in assessing conditions such as asthma, pulmonary fibrosis, cystic fibrosis and COPD.

• c. Bronchodilators• is a substance that dilates the
bronchi and bronchioles, decreasing resistance in the respiratory airway and increasing airflow to the lungs. Bronchodilators may be endogenous (originating naturally within the body), or they may be medications administered for the treatment of breathing difficulties. They are most useful in obstructive lung diseases, of which asthma and chronic obstructive pulmonary disease are the most common conditions. Although this remains somewhat controversial, they might be useful in bronchiolitis. They are often prescribed but of unproven significance in restrictive lung diseases.

• d. Astmaticusan acute exacerbation of asthma that does not respond to standard treatments of bronchodilators and steroids. Symptoms include chest tightness, rapidly progressive dyspnea (shortness of breath), dry cough, use of accessory muscles, labored breathing and extreme wheezing. It is a life-threatening episode of airway obstruction considered a medical emergency. Complications include cardiac and/or respiratory arrest.

• e. Anticholinergics• is a substance that blocks
the neurotransmitter acetylcholine in the central and the peripheral nervous system. An example of an anticholinergic is dicycloverine, and the classic example is atropine. Anticholinergics are administered to reduce the effects mediated by acetylcholine on acetylcholine receptors in neurons through competitive inhibition. Therefore, their effects are reversible.

Etiology:

• Family history of fever, asthma and eczema is common.
• Viral upper infections frequently precipitate attacks. Contributing factors include an increase in sedentary lifestyle, with children remaining indoors, resulting an increase exposure to allergens amid poor ventilation. Increase air pollution has also been factor.

Types of asthma:

• Intrinsic • Intrinsic -
Idiosyncratic asthma is a result of neurological imbalances in the autonomic nervous system (ANS) in which the alpha and beta adrenergic as well as the cholinergic sites of the ANS are not properly coordinated.
• Extrinsic• Extrinsic - Allergic
asthma is a result of an antigen/antibody reaction on mast cells in the respiratory tract. This reaction causes the release of inflammatory mediators from mast cells which elicit the clinical response associated with an asthma attack.

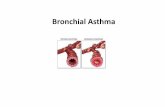
Pathophysiology:

Clinical manifestatio
ns:

• Cough, marked dyspnea, a tight feeling in the chest, and agitation develop as airway obstruction increases. The patient is unable to talk.
• Wheezing is characteristic as air passes through the narrowed bronchioles
• Breathing is rapid and labored, with use of accessory muscles and possible chest retraction
• Thick and tenacious or sticky mucus is coughed up
• Tachycardia occurs

• Hypoxia develops due to obstruction
• Respiratory acidosis develops in time due to air trapping, and marked fatigue causes decrease respiratory effort with weaker cough. This is aggravated by developing metabolic acidosis due to hypoxia, and from metabolic acid accumulating from increase metabolic activity and dehydration.
• Severe respiratory distress is evident. Hypoventilation leads to increasing hypoxemia and respiratory acidosis
• Respiratory is indicated by decreasing responsiveness, cyanosis, and arterial blood gas measurement indicating a PaO2 of above 50 mm Hg.

Medical management:

laboratory and diagnostic exam:• Blood Tests - In the
laboratory evaluation of asthma it would be common to evaluate the patient’s blood count looking for “allergy cells” called eosinophils. The physician may also obtain a level of IgE, the immunoglobulin in the blood that is often elevated in allergic patients. • X-rays - are used to
detect emphysema, lung cancer and to show collapsed lungs or very obstructed airways.

• Sputum Exam - Examination of swabs of nasal mucus or chest phlegm (sputum) may be helpful in diagnosing asthma. Microscopic examination may identify abundant eosinophils that would be characteristic of allergy and asthma. The presence of pus cells called neutrophils would suggest an infectious process; for example, bronchitis or sinusitis. The physician may request a culture of the coughed sputum if pus cells are seen under the microscope.
• Pulmonary (Lung) Function Tests• Forced Expiratory Maneuver• The most important laboratory test the
physician performs in the diagnosis of asthma is pulmonary function testing. Before the testing begins the patient’s age, race, sex, height, and weight are recorded. From these statistics the expected normal values are determined. These are called the predicted normals and they are determined from statistical analysis of large groups of normal subjects.

• The most common test involves a device known as a spirometer, which measures the amount of air (volume) expelled by the patient as well as its speed as the air is exhaled forcefully. In this simple but extremely important maneuver the patient is asked to take a full deep breath in, then exhale fully and forcefully this is called a maximum forced expiratory maneuver. In tracing this maneuver the physician determines the maximum amount of air the patient can expel after the deepest inhalation. This amount is called the vital capacity.

• As air is expelled the airflow is measured throughout the maneuver until the patient is unable to exhale further. One extremely useful measurement is of the greatest flow that can be obtained after the patient has inhaled fully and forcefully exhaled. This is termed peak expiratory flow rate or “peak flow.” This important and easily performed. Flow rates are recorded at the beginning, middle, and end of the forced exhalation maneuver and so is the amount of air expelled each second. As air is exhaled by the lungs it is the large bronchial tubes (large airways) that empty first with the smaller passages (small airways) contributing a greater share as exhalation continues and ends. In one second a certain amount of air should normally be exhaled with an expected increase as time increases. The one-second measurement is often a good reflector of the large airways and measurements toward the middle and end of the breath usually determine the condition of smaller air passages.

Medication:• Anti-inflammatory drugs. This
is the most important type of therapy for most people with asthma because these asthma medications prevent asthma attacks on an ongoing basis. Steroids, also called "corticosteroids," are an important type of anti-inflammatory medication for people suffering from asthma. These asthma drugs reduce swelling and mucus production in the airways. As a result, airways are less sensitive and less likely to react to triggers.
• Bronchodilators. These asthma medications relieve the symptoms of asthma by relaxing the muscle bands that tighten around the airways. This action rapidly opens the airways, letting more air come in and out of the lungs. As a result, breathing improves. Bronchodilators also help clear mucus from the lungs. As the airways open, the mucus moves more freely and can be coughed out more easily.

Nursing management:

Assessment:• Subjective Data• Important Health Information• Past health history: Allergic
rhinitis or sinusitis; previous• asthma attack; exposure to
pollen, danders, feathers, mold,• dust, inhaled irritants, weather
changes, exercise, smoke;• sinus infections;
gastroesophageal reflux• Medications: Use of and
compliance with corticosteroids,• bronchodilators, cromolyn
sodium, anticholinergics, antibiotics;
• medications that may precipitate an attack in susceptible
• asthmatics such as aspirin, nonsteroidal
• antiinflammatory drugs, _-adrenergic blockers
• Functional Health Patterns• Health perception–health
management: Family history of allergies
• or asthma; recent upper respiratory infection or sinus
• infection• Activity-exercise: Fatigue,
decreased or absent exercise tolerance;
• dyspnea, cough, productive cough with yellow or green
• sputum; chest tightness, feelings of suffocation, air hunger
• Sleep-rest: Interrupted sleep, insomnia
• Coping–stress tolerance: Fear, anxiety, emotional distress, stress
• in work environment or in the home

• Objective Data• General• Restlessness or exhaustion,
confusion, upright or forwardleaning
• body position• Integumentary• Diaphoresis, cyanosis
(circumoral, nailbed)• Respiratory• Wheezing, crackles, diminished
or absent breath sounds, and• rhonchi on auscultation;
hyperresonance on percussion;• sputum (thick, white,
tenacious), ↑ work of breathing with use
• of accessory muscles; intercostal and supraclavicular retractions;
• tachypnea with hyperventilation; prolonged expiration
• Cardiovascular• Tachycardia,
pulsus paradoxus, jugular venous distention, hypertension
• or hypotension, premature ventricular contractions

Intervention:• The immediate nursing care of the patient with asthma depends on
the severity of the symptoms. The patient may be treated successfully as an outpatient if asthma symptoms are relatively mild, or he or she may require hospitalization and intensive care for acute and severe asthma.
• The patient and family are often frightened and anxious because of the patient’s dyspnea. Thus, an important aspect of care is a calm approach. The nurse assesses the patient’s respiratory status by monitoring the severity of symptoms, breath sounds, peak flow, pulse oximetry, and vital signs. The nurse obtains a history of allergic reactions to medications before administering.
• Medications and identifies the patient’s current use of medications.• The nurse administers medications as prescribed and monitors the
patient’s responses to those medications. Fluids may be administered if the patient is dehydrated, and antibiotic agents may be prescribed if the patient has an underlying respiratory infection.
• If the patient requires intubation because of acute respiratory failure, the nurse assists with the intubation procedure, continues close monitoring of the patient, and keeps the patient and family informed about procedures.

Promoting home and community based care:

Teaching Patients Self-Care. • A major challenge is to implement basic asthma
management principles at the community level (Reinke, 2000). Key issues include education of health care providers, establishment of programs for asthma education (for patients and providers), use of outpatient follow-up care for patients, and a focus on chronic management versus acute episodic care. The nurse is pivotal to achieving all of these objectives.

• Patient teaching is a critical component of care for the patient
with asthma (Plaut, 2001). Multiple inhalers, different types of inhalers, anti-allergy therapy, anti-reflux medications, and avoidance measures are all integral for long-term control. This complex therapy requires a patient–provider partnership to determine the desired outcomes and to formulate a plan to achieve those outcomes. The patient then carries out daily therapy as part of self-care management, with input and guidance by the health care provider.

• Before a partnership can be established, the patient needs to understand the following:
• The nature of asthma as a chronic inflammatory disease
• • The definition of inflammation and bronchoconstriction
• • The purpose and action of each medication• • Triggers to avoid, and how to do so• • Proper inhalation technique• • How to perform peak flow monitoring (Chart 24-
5)• • How to implement an action plan• • When to seek assistance, and how to do so

• Lung and Blood Institute. The nurse should obtain current educational
• materials for the patient based on the patient’s diagnosis,
• causative factors, educational level, and cultural factors.

Continuing Care• The nurse who has contact with the patient in the hospital,
clinic, school, or office uses the opportunity to assess the patient’s respiratory status and ability to manage self-care to prevent serious exacerbations. The nurse emphasizes adherence to the prescribed therapy, preventive measures, and the need to keep follow-up appointments with the primary health care provider. A home visit to assess the home environment for allergens may be indicated for the patient with recurrent exacerbations.
• The nurse refers the patient to community support groups.• In addition, the nurse reminds the patient and family about
the importance of health promotion strategies and recommended health screening.

Evaluation :

Click icon to add picture
REFERENCES:
Novales, Dionesia. Handbook of Common Communicable and Infectious Diseases. Quezon City: C & E Publishing Inc. 2008Longworth, David. Handbook of Infectious Disease. Springhouse, Pennsylvania: Springhouse Corporation. 2001Cuevas, Frances Pricilla, et. Al., Public Health Nursing in the Philippines. Publications Committee, National League of the Philippine Government Nurses, Inc.2007.Porth,C.M.(2005). Pathophysiology: Concept of Altered Health States, Lippincott Williams and WilkinsKarch, A.M.(2012). Nursing Drug Guide. Lippincott Williams and WilkinsBlack, J.M & Hawks, J.H.(2009). Medical-Surgical Nursing: Clinical Management foe Positive Outcomes. Singapore: Elsevier Pte Ltd.